Abstract
Objectives
Monkeypox, a zoonotic orthopoxvirus, has spread to many countries in recent months, involving mostly men who have sex with men with multiple partners. Clinical presentation includes skin lesions, systemic signs, and less frequent skin superinfections or anorectal and ophthalmic involvements. We aim to detail cases of myocarditis attributable to monkeypox, an entity that has been poorly described.
Methods
This is a descriptive case series reporting three cases of myocarditis that occurred in patients infected with monkeypox in France in 2022.
Results
Patients were adult men with no medical history who had skin lesions with positive polymerase chain reaction for monkeypox virus. A few days after the onset of cutaneous signs, patients developed acute chest pain, elevated cardiac markers, and biological inflammatory syndrome compatible with myocarditis. Two patients presented electrocardiogram abnormalities and decreased ejection fraction associated with kinetic disturbances on transthoracic electrocardiography. The last patient had normal transthoracic electrocardiography and normal electrocardiogram, but cardiac magnetic resonance imaging showed segmental inferolateral acute myocarditis. Patients were hospitalized and received cardioprotective treatment. One received antiviral treatment with tecovirimat. Symptoms and laboratory abnormalities rapidly resolved in all patients.
Discussion
These cases suggest an association between monkeypox infections and cardiac inflammatory complications. The development of chest pain in an infected patient should not be underestimated and should lead to prompt investigations for myocarditis. Monkeypox infection should also be included in the differential diagnosis of myocarditis, particularly in at-risk patients such as men who have sex with men with multiple partners in whom complete examination for skin or mucosal lesions should thus be performed.
Keywords: Complication, Epidemic, Monkeypox, Myocarditis, Virus
Introduction
Monkeypox, a zoonotic orthopoxvirus, has spread to many countries outside the known endemic areas in recent months [1]. The current epidemic has mainly involved men who have sex with men with multiple partners. Clinical presentation includes skin lesions, systemic signs, and less frequent skin superinfections or severe and painful anorectal or ophthalmic involvements [[2], [3], [4]]. Myocarditis is a focal or diffuse inflammation of the myocardium that can result in acute arrhythmia, dilated cardiomyopathy, and heart failure [5,6]. Viruses such as adenovirus, parvovirus B19, HIV, or enterovirus are known to cause myocarditis. Only five cases of myocarditis attributed to monkeypox have been described, all in 2022 during the current epidemic, with possible differential causes of myocarditis [3,7,8]. We describe here three new cases of acute myocarditis attributable to monkeypox.
Methods
This is a case series describing three cases of myocarditis attributable to monkeypox in France in 2022. Cases were identified during a call for observations in a national meeting for the coordination of epidemiological risks. Diagnostic criteria for myocarditis were not predefined and remained at the discretion of clinicians. A review of medical records was conducted to detail the cases retrospectively. Each patient had been previously informed that clinical-biological information could be used for research, without oral opposition.
Results
Patient 1, a 21-year-old man, developed a fever with anal pain four days after the last unprotected homosexual intercourse, with several sexual intercourses with at-risk partners during the previous month. Monkeypox polymerase chain reaction (PCR) on swabs from anal pustules was positive. Two days later, acute chest pain radiating into the arms and jaw appeared. Electrocardiogram revealed elevation of the ST segment in inferior leads. High-sensitivity troponin T reached 4040 pg/mL (N < 58.9), creatine kinase (CK) 418 U/L (N, 39–308) and C-reactive protein (CRP) 27 mg/L (N < 6). Contrast chest computed tomography scan excluded pulmonary embolism. Transthoracic echocardiography (TTE) showed a nondilated, nonhypertrophied left ventricle with segmental hypokinesis of inferior and inferolateral walls, and left ventricular ejection fraction was estimated at 56%. Cardioprotective treatment with bisoprolol and ramipril was initiated. There was no recurrence of pain, and high-sensitivity troponin T decreased to 2200 pg/mL on day 1. No other sexually transmitted infection or other cause of myocarditis was found (normal serum protein electrophoresis; no declared toxic consumption; negative HIV and syphilis serologies; negative PCRs for Epstein-Barr virus, Cytomegalovirus, and parvovirus B19; and negative nasopharyngeal SARS-CoV-2 PCR). Coronary explorations were not performed given the patient's young age, the absence of comorbidity or family history of cardiovascular disease, and the rapidly favourable outcome. Cardiac magnetic resonance imaging (MRI) was performed four weeks later and demonstrated no evidence of cardiac inflammation.
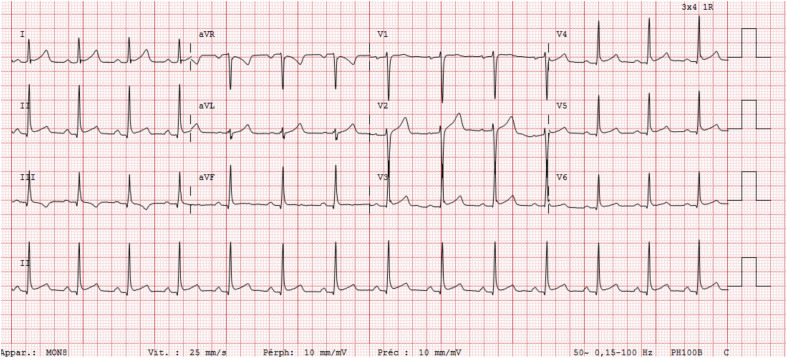
Patient 2, a 25-year-old man with no medical history, developed pustules on the face and penis a few days after unprotected sexual intercourse. Five days later, he reported constant chest pain and palpitations. Monkeypox PCR on skin lesions was positive. The electrocardiogram showed a discrete elevation of the ST segment in the inferior and anterior territories, with possible undershift of the PQ segment (Fig. 1 ). Blood analyses showed increased high-sensitivity troponin T (700 pg/mL; N < 58.9), CK (318 U/L; N, 39–308), and CRP (39 mg/L; N < 6) levels. TTE showed impaired left ventricular ejection fraction (45%) with inferolateral akinesia. The evolution was rapidly favourable under bisoprolol and ramipril. No other STI or other cause of myocarditis was found after medical examination and biological assessment (identical to patient 1). For the same reasons as in the first case, coronary explorations were not performed.
Fig. 1.
Electrocardiogram of patient 2.
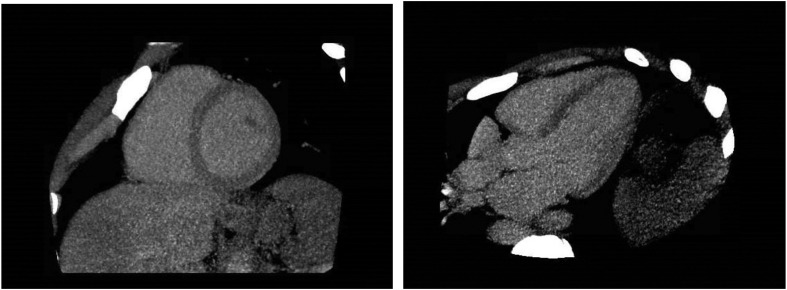
Patient 3, a 32-year-old man with no medical history, developed erosive cutaneous lesions on the penis approximately one week after unprotected heterosexual intercourse. Three days later, he presented retrosternal chest pain and fever. Monkeypox PCR on skin lesions and pharynx were positive and negative in serum. Laboratory analyses showed increased high-sensitivity troponin T (2035 pg/mL; N < 58.9), CK (2295 U/L; N, 39–308), and CRP (115 mg/l; N < 6) levels. Electrocardiogram and TTE were normal. Cardioprotective treatment with bisoprolol and antiaggregation and antiviral treatment with tecovirimat were initiated. No other sexually transmitted infection or aetiology of myocarditis was found (negative blood PCRs for HIV, Herpes Simplex viruses, Cytomegalovirus, Varicella-Zoster virus, parvovirus B19 and Herpes Human viruses 6 & 8; slightly detectable Epstein-Barr virus DNA in blood <500 copies/mL; negative nasopharyngeal multiplex PCR; negative serologies for intracellular bacteria; negative screening for toxics consumption; isolated antinuclear antibodies with low titer 1/80; normal angiotensin-converting enzyme; unconsumed complement; and normal serum protein electrophoresis). Chest pain stopped on day 2 and high-sensitivity troponin T levels normalized on day 4. Cardiac-CT scanner showed normal coronary arteries but reflected acute myocarditis. Cardiac MRI, performed 11 days after the onset of chest pain, showed segmental myocarditis involving the inferolateral segment (Fig. 2 ).
Fig. 2.
Key pictures of cardiac magnetic resonance imaging of patient 3.
Discussion
In these three cases, the history began with typical monkeypox lesions confirmed by PCR. A few days later, patients presented acute chest pain, fever, elevated cardiac markers, and biological inflammatory syndrome, without other systemic signs. Typical electrocardiogram and TTE abnormalities associated with myocarditis were identified in two patients. Cardiac MRI showed segmental myocarditis in the third patient. Myocarditis was attributed to monkeypox in all, and no differential diagnosis was found. The outcome was rapidly favourable in all patients after cardioprotective treatment, regardless of the use of antiviral treatment.
Only five cases of myocarditis attributed to monkeypox had been previously described. Two were described in a series of 528 human monkeypox infections diagnosed in 16 countries in 2022 [3]. One occurred in a patient infected with HIV with 780 CD4 cells per cubic millimetre; the second patient had no medical history. Their symptoms lasted less than 7 days. Recently, three other case reports of myocarditis attributed to monkeypox were reported [7,8]. Patients were immunocompetent and presented with clinical presentation compatible with myocarditis and recently confirmed monkeypox infections. Two patients had ventricular repolarization abnormalities on electrocardiogram with normal TTE, including one in whom cardiac MRI confirmed the myocarditis. The third patient had a normal electrocardiogram and TTE. One patient was treated with tecovirimat. The outcome was rapidly favourable in all. However, differential causes of myocarditis were not discussed in two of these five patients, one had no additional investigation for other causes of elevated cardiac markers although he had a family history of coronary disease, one had a concomitant active syphilitic infection, and the last one had had a paucisymptomatic SARS-CoV2 infection two months before.
In summary, findings from our present case series suggest the possibility of an association between monkeypox and acute myocarditis, as previously suggested. However, our cases were important to describe because differential diagnoses were explored and deemed unlikely, whereas the presence of other possible causes of myocarditis in previously reported cases (or the deferral of explorations for differential diagnoses) suggested that causality between monkeypox and myocarditis is questionable.
Thus, this series highlights the importance of not underestimating chest pain in monkeypox-infected patients. We should not be completely reassured by the favourable outcome of myocarditis in these patients, given the low number of cases reported: larger studies with appropriate designs are needed to confirm an association between monkeypox infections and myocarditis and to assess the risk of progression towards complications (such as arrhythmia or long-term cardiomyopathy). In the meantime, patients infected with monkeypox should be advised to consult a doctor rapidly if they experience chest pain. Furthermore, monkeypox should be considered if myocarditis is diagnosed in at-risk patients in countries experiencing epidemics.
Author contributions
M.D. contributed to conceptualization, data curation, methodology, validation, visualization, writing the original draft, and review and editing. T.G. contributed to conceptualization, writing the original draft, and review and editing. M.G. contributed to data curation, writing the original draft, and reviewing and editing. G.F.G., P.L.N, A.K., V.J., L.B., and Y.Y. contributed to writing the original draft and review and editing. M.-H.A. and Cd.L.P.d.V. contributed to conceptualization, data curation, methodology, validation, visualization, writing the original draft, and review and editing.
Transparency declaration
The authors declare that they have no conflicts of interest.
Handling Editor: L. Leibovici
References
- 1.World Health Organization. 2022. https://www.who.int/emergencies/situations/monkeypox-oubreak-2022 [Google Scholar]
- 2.Mailhe M., Beaumont A.-L., Thy M., Le Pluart D., Perrineau S., Houhou-Fidouh N., et al. Clinical characteristics of ambulatory and hospitalized patients with monkeypox virus infection: an observational cohort study. Clin Microbiol Infect. 2023;29:233–239. doi: 10.1016/j.cmi.2022.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thornhill J.P., Barkati S., Walmsley S., Rockstroh J., Antinori A., Harrison L.B., et al. Monkeypox virus infection in humans across 16 countries —April–june 2022. N Engl J Med. 2022;387:679–691. doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 4.Bryer J., Freeman E.E., Rosenbach M. Monkeypox emerges on a global scale: a historical review and dermatologic primer. J Am Acad Dermatol. 2022;87:1069–1074. doi: 10.1016/j.jaad.2022.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lampejo T., Durkin S.M., Bhatt N., Guttmann O. Acute myocarditis: aetiology, diagnosis and management. Clin Med Lond Engl. 2021;21:e505–e510. doi: 10.1016/j.jaad.2022.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sozzi F.B., Gherbesi E., Faggiano A., Gnan E., Maruccio A., Schiavone M., et al. Viral myocarditis: classification, diagnosis, and clinical implications. Front Cardiovasc Med. 2022;9 doi: 10.3389/fcvm.2022.908663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Nava G., Kadlecik P., Filardo T.D., Ain D.L., Cooper J.D., McCormick D.W., et al. Myocarditis attributable to monkeypox virus infection in 2 patients, United States, 2022. Emerg Infect Dis. 2022;28:2508–2512. doi: 10.3201/eid2812.221276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinho A.I., Braga M., Vasconcelos M., Oliveira C., Santos L.D., Guimarães A.R., et al. Acute myocarditis: a new manifestation of Monkeypox infection? JACC Case Rep. 2022;4:1424–1428. doi: 10.1016/j.jaccas.2022.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]