Reply to the Editor:
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Since our Y-incision/rectangular patch technique was presented and published in 2021, concern has been raised that our aortic annular enlargement (AAE) technique does not enlarge the “true” aortic annulus and left ventricular outflow tract (LVOT). Is this the case, and should we be concerned?
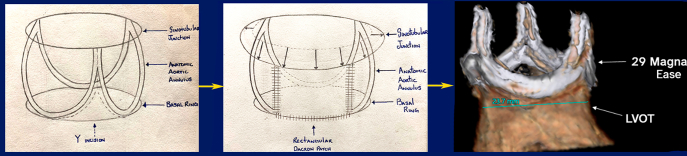
There has been widespread confusion over the definition of the aortic annulus. Robert Anderson, a cardiac embryologist and anatomist, defines the aortic root as the structure between the virtual basal ring and the sinotubular junction.1 Inside the aortic root, the crown-like structure through which the cusps of the aortic valve attach to the aortic wall is defined as the aortic annulus.1 We call it the anatomic aortic annulus. In contrast, the virtual basal ring of the aortic root can be measured by echocardiogram and computed tomography aortogram and is also called an aortic annulus. For surgical aortic valve replacement (SAVR), we place the sutures on the anatomic aortic annulus to secure the prosthetic valve, not the virtual basal ring. The goal of AAE is to enlarge the anatomic aortic annulus and the root to accommodate a larger valve inside the aortic root, with the inner diameter of the prosthetic valve matching the diameter of the basal ring (Figure 1).
Figure 1.
Y-incision enlarges the anatomic aortic annulus for a larger valve sitting as a crown sits on a head.
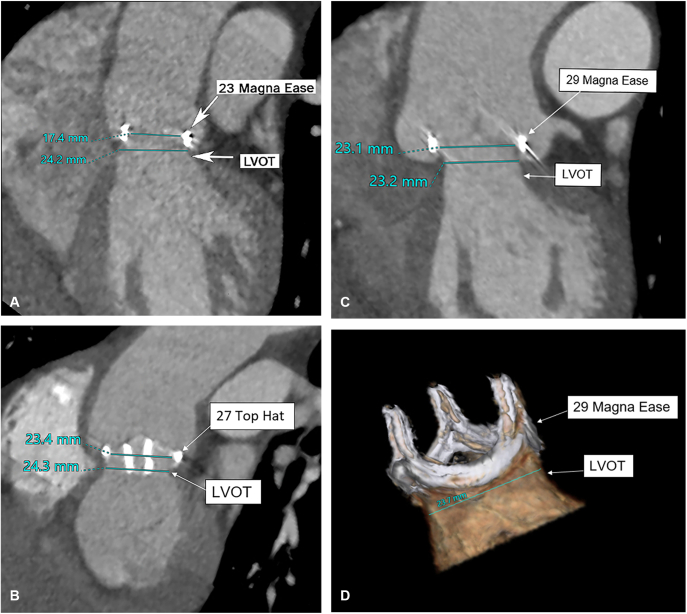
There is also confusion regarding the labeling of the bioprosthetic valve. The inner diameter of the bioprosthetic valve is 5 to 7 mm smaller than the labeled size (defined by a historical American Society for Artificial Internal Organs conference for a stented bioprosthesis as the distance between 2 parallel lines located at the outside border of the struts) after implantation because of the sewing ring, strut material, and aortic annular tissue protruding inside the sewing ring of the valve (Figure 2, A).2 After SAVR, the inner diameter of the prosthetic valve becomes the new “basal ring” of the prosthetic valve, which can be 5 to 7 mm smaller than the patient's native basal ring2 (Figure 2, A). This is why it is necessary to upsize the prosthetic valve by 3 to 4 valve sizes to have an inner diameter matching the patient's native basal ring, especially in active patients2 (Figure 2, B and C).
Figure 2.
Three cases of aortic valve replacement in 3 patients, all of whom had a 23-mm basal ring. The first case had a size 23 Magna Ease implanted without aortic annular enlargement. The inner diameter was 17 mm on computed tomography aortogram (CTA), and left ventricular outflow tract (LVOT) was 24 mm (A). The second case had a size 27 (the largest size) Top Hat mechanical valve (CarboMedics) implanted after Y-incision aortic annular enlargement. The inner diameter of the size 27 Top Hat valve was 23 mm and LVOT was 24 mm based on the blood flow with contrast on CTA (B). The third case had a size 29 Magna Ease (Edwards Lifesciences) implanted after Y-incision aortic annular enlargement. The inner diameter of the size 29 Magna Ease was 23 mm and the LVOT was 23 mm based on the blood flow with contrast on CTA (C), and the bioprosthetic valve sitting on the LVOT like a crown on a head (D).
I agree with Dr Said3 that the fundamental conceptual difference between our AAE technique and traditional AAE techniques, including Nicks, Manougian, and Konno, is that our technique does not enlarge the basal ring and LVOT as in the traditional techniques. In patients with aortic valve stenosis, the basal ring and LVOT are of normal size, but the aortic valve is stenotic. The goal of the traditional techniques is not to enlarge the basal ring or LVOT per se in patients with aortic valve stenosis only but to enlarge the anatomic aortic annulus by incising into the LVOT. The further the incision into the LVOT, the greater the enlargement of the anatomic aortic annulus, and the larger the prosthetic valve implanted. Our AAE technique enlarges the anatomic aortic annulus and root with a Y-incision without incising into the basal ring or LVOT. This allows us to place prosthetic valves upsized by 3 to 4 sizes above (supra-annular)2 or inside the residual anatomic annulus (intra-annular) and the patch (such as intra-annular implantation of St Jude mechanical valve).4 The upsized valve has an inner diameter close to the diameter of patient's native basal ring. This is confirmed by the blood flow through the LVOT and prosthetic valve on postoperative computed tomography aortogram (Figure 2, B and C). The prosthetic valve over the LVOT is like a crown on a head with perfect match (Figure 2, D). Despite the large-size valve implanted, the postoperative mean gradient across the aortic valve (7 mm Hg) is still greater than that across the LVOT (2 mm Hg), which remains the same as the preoperative LVOT gradient.2 The normal basal ring and LVOT do not need to be enlarged, since we do not place a prosthetic valve in the basal ring or LVOT. The same concept applies when a total root replacement is used in an extra-anatomic fashion to implant a larger valve for a small aortic annulus/root. There is also no need to enlarge the basal ring and LVOT for the total root replacement.5 Not enlarging the basal and LVOT is not a weakness of our technique, but rather it simplifies the operation of AAE by avoiding violating any surrounding structures of the aortic root. In patients with aortic valve stenosis and subannular or LVOT stenosis simultaneously, such as subaortic web or hypertrophic obstructive cardiomyopathy, we recommend resection of subannular web or myectomy AND Y-incision AAE with SAVR.
Because the distance between the nadirs of the left and noncoronary cusps is slightly different among patients and the largest size valve available varies by valve type, the upsizing of the prosthetic or bioprosthetic valve is variable. However, we predominately upsize by 3 to 4 valve sizes.2 The “roof” technique is to resolve the kink between the enlarged root and native ascending aorta. Fifty percent of patients in our early series had no “roof” technique but with no hemodynamical significance.2 With our AAE technique, the aortic root is extensively enlarged (from 27 to 40 mm), the sinotubular junction is effaced, the valve-to-coronary distance is 4 to 6 mm despite a much larger valve is used, and the proximal ascending aorta is enlarged.2 The patients who receive a bioprosthesis are well prepared for potential future valve-in-valve transcatheter aortic valve replacement. Currently, the Y-incision AAE technique is our first choice for all aortic annular enlargement at our institution, and SAVR with AAE increased to 50% of all aortic valve replacements in 2022 with median valve size of 27.
References
- 1.Anderson R.H. The surgical anatomy of the aortic root. Multimed Man Cardiothorac Surg. 2007;2007 doi: 10.1510/mmcts.2006.002527. mmcts.2006.002527. [DOI] [PubMed] [Google Scholar]
- 2.Yang B., Ghita C., Makkinejad A., Green C., Wu X. Early outcomes of the Y-incision technique to enlarge the aortic annulus 3 to 4 valve sizes. J Thorac Cardiovasc Surg. July 3, 2022 doi: 10.1016/j.jtcvs.2022.07.006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Said S.M., Jahanyar J. Yang technique for aortic annular enlargement and the “lemon on a stick.”. J Thorac Cardiovasc Surg Tech. 2022;16:21. doi: 10.1016/j.xjtc.2022.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang B., Naeem A. A Y incision and rectangular patch to enlarge the aortic annulus by three valve sizes. Ann Thorac Surg. 2021;112:e139–e141. doi: 10.1016/j.athoracsur.2021.01.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clemence J., Jr., Yang B. Aortic root replacement of small roots to prepare for transcatheter aortic valve replacement. Ann Thorac Surg. 2022;114:e303–e305. doi: 10.1016/j.athoracsur.2021.12.023. [DOI] [PubMed] [Google Scholar]