Abstract
A notable rise in health-related disability for which evidence-based rehabilitation is beneficial is evident in low-to-middle income countries. This scoping review aimed to systematically identify and map the most common functioning problems associated with health conditions that contribute most to disability in South Africa using the International Classification of Functioning, Disability and Health (ICF) framework. Peer-reviewed evidence published from January 2006 to December 2021 was systematically searched from five databases. Some 268 studies reporting on functioning problems (impairments, activity limitations, and participation restrictions) in South African adults (>18 years) related to 10 health conditions were included. A total of 130 different functioning problems were mapped to the ICF. The most prevalent problems (top 20) were related to mobility, pain, and mental health but spanned across several ICF domains and were mostly in patients at primary care. The high prevalence and wide range of functioning problems may be particularly burdensome on an already strained primary health care (PHC) system. This points towards targeted planning of innovative strategies towards strengthening rehabilitation service delivery at primary care to address these complexities where there is an inadequate rehabilitation workforce.
Keywords: functioning, ICF, primary care, rehabilitation, South Africa
1. Introduction
Functioning of individuals is recognised as an important indicator of population health and well-being [1]. Functioning refers to the ability to perform daily activities and participation in personal, work and community settings [2]. Ageing, trauma and diseases, especially non-communicable chronic diseases (NCDs) impairs functioning [3], in the short-term, long-term, or episodically. Suboptimal functioning influences an individual’s perception of their health condition negatively [4]. Therefore, functioning problems compound the effect on perception of health and quality of life in people who are already living with morbidity associated with a chronic condition [4].
Morbidity at a national level is often described using Global Burden of Disease (GBD) metrics such as Years Lived with Disability (YLDs) [5]. The YLDs reflect the total years lived with a chronic condition disease [6]. YLDs are increasing at a higher rate in low- and middle- income countries (LMICs), compared to high- income countries (HICs) [7]. In South Africa (SA), YLDs due to health conditions that contribute to most disability increased by about 270% from 1990–2017, with a further 6% predicted increase from 2017–2022 [8]. Thus, health systems in LMICs need to adapt in response to the epidemiological transitioning reflective of high levels of morbidity and functioning problems [9].
To prepare countries, especially LMICs, the WHO launched initiatives to strengthen rehabilitation as the key health strategy aimed at addressing functioning problems [10]. These WHO initiatives include a package of evidence-based rehabilitation interventions that should be prioritized for integration into the health systems [11]. Additionally, the WHO developed the Rehabilitation Competency Framework (RCF) which ensures that the rehabilitation workforce has the required competencies and is capable of addressing its population’s rehabilitation needs [12]. Since the healthcare experiences and rehabilitation needs of the populations vary widely between countries, country specific functioning profiles are needed to effectively plan and integrate rehabilitation services into local health systems.
Strengthening rehabilitation into the health system of LMICs is challenging. As a case example, South Africa, classified as a upper-middle-income country, has a high disease burden inclusive of communicable and non-communicable diseases [13]. The health system is already constrained and fragmented. Two decades post-Apartheid, racial and political divides continue to affect the quality and access to healthcare by different population groups. The private health sector provides healthcare services to 16% of South Africa’s mostly affluent population. The remaining 84% of South Africa’s poorer population receives healthcare from the public sector which uses 48% of the allocated national healthcare budget [14]. The limited public sector resources has to fund many competing health needs considering the high burden of disease. Furthermore, one in five adult South Africans present with multimorbidity [15] and associated functioning problems are notable but rarely addressed, especially at primary care level where only 6% of the total rehabilitation workforce work [16]. Thus, integrating rehabilitation services will require strong advocacy supported by relevant data on functioning needs to inform service planning.
South Africa is currently reforming towards a National Health Insurance (NHI) policy [17]. The policy promises that disability and rehabilitation services will be “fully integrated into primary health care (PHC) with a view to increasing care, treatment and rehabilitation” [18]. An important first step was to include rehabilitation in the country’s PHC standard treatment guidelines (STGs), which are the crux of packages of care [19]. Due to competing demands on the limited healthcare budget in South Africa, crucial information regarding the functioning problems is required to guide policy makers in prioritizing, costing, and designing rehabilitation services fit for the local population. Since many stakeholders are involved in the NHI planning and implementation process, standardisation of terminologies are important [2].
The International Classification of Functioning, Disability, and Health (ICF) provides standard terminology for describing functioning [2]. This framework can be used to indicate functioning problems that include body impairments, activity limitations or participation restrictions that result from an individual with a health condition interacting with contextual factors such as environmental and personal factors [2]. The focus is removed from the health condition an individual presents with to what they have difficulty doing—for example, being more concerned with whether a person has difficulty walking rather than whether the person has HIV or stroke. The ICF is aetiologically neutral meaning and serves to classify data on functioning across health conditions [2].
Comprehensive comparable data on functioning across health conditions in LMICs, particularly South Africa, is scarce. The growing body of literature that applies the minimal generic ICF set [20] (a minimum generic set of ICF domains suitable for describing functioning) or the ICF Rehabilitation Core Set [21] is largely based in high income countries (HICs). The findings may not be generalizable to South Africa’s context with limited access to quality healthcare services [22] and different profiles of chronic conditions contributing to most disability [7]. Instruments used to capture disability statistics during South Africa population surveys or censuses, such as the Washington Group Short Set on Functioning (WG-SS) [23], do not include all critical ICF domains. This may result in under-identifying or underreporting of functioning problems. The World Bank Model Disability Survey (MDS), while more comprehensive, is quite new and to date has not been implemented in South Africa [24]. Country-level planning is often based on the GBD studies estimates of disability at country and global levels [24]. However, a gap exists in detailed descriptions of the functioning problems required to plan rehabilitation services.
Clinical data on functioning in South African adult populations is available but is siloed into the different health conditions or specific functioning problem [25]. A composite and comprehensive mapping of this data compared across health conditions will provide country level data on functioning which is useful for rehabilitation service planning [26]. The main aim of this review was to summarize and synthesize the status of peer-reviewed literature regarding the most common functioning problems presenting in the adult population in South Africa. This was done by describing the most prevalence types of functioning problems (impairments, activity limitations and participation restrictions). These functioning problems were associated with the top 10 conditions contributing most to years lived with disability in South Africa and for which evidence-based rehabilitation interventions to address associated disability exist [8]. The most prevalent functioning problems were mapped to the ICF framework.
2. Materials and Methods
A scoping review of the current evidence regarding functioning problems associated with the priority conditions in South Africa was conducted according to a predefined protocol [27], in line with the methodological framework developed by Arksey and O’Malley [28]. Corresponding guidance contained in the Joanna Briggs Institute Reviewers’ Manual was also considered [29]. The ICF framework guided our review to allow a standardised analysis of the identified impairments, activity limitations, and participation restrictions associated with priority conditions in South Africa, to determine which were most common. We reported the scoping review according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) guidelines (Supplementary File S1) [30].
The main research questions for this review were: (i) “What is the spectrum of functioning problems associated with conditions contributing most to YLDs in South Africa?”; (ii) “Which are the ICF domains and categories dominantly affected by the most prevalent functioning problems in adult South Africans?”
Eligibility of the research questions was informed by the Population, Exposure, Context, Outcome design (PECOd) framework [29]. This included the population (P) of patients >18 years with exposure (E) to at least one of the conditions contributing to the greatest YLD, as indicated by GBD 2019 data, within the context (C) of South Africa [8]. The outcomes (O) were the functioning problems investigated using all peer-reviewed study designs (D).
2.1. Search Method
The bibliographic databases of PubMed/MEDLINE, SCOPUS, Web of Science, EbscoHost (CINAHL and Africawide Information), and SABINET were searched for articles published from 1 January 2006 to 31 December 2021. This date range was selected to focus on current functioning problems, considering that constant improvements in clinical care, public health and technology may affect rates of disability [31]. A re-run of the searches was conducted in June 2022 to complete search of new studies that may have been published since the previous searches run in August 2021. Studies were considered eligible if full texts were available, reporting information regarding type and/or prevalence of the impairments, activity limitations or participation restrictions associated with the health condition. The languages of publication were restricted to English and Afrikaans, the most common languages for scholarly communication in South Africa.
Grey literature, including theses and dissertations, were not reviewed as we were looking for complete, peer-reviewed published data only. We excluded impairments which were not indicated for rehabilitation, for example, neck stiffness in Tuberculous meningitis or internal impairments such as vomiting. We excluded health related quality of life assessments as they focus on the individual’s values and expectations following disease or injury [32] rather than functioning problems in terms of impairments, activity limitations and participation restrictions.
The search strategies were drafted and refined with the assistance of a librarian from Stellenbosch University. An initial search was conducted in PubMed. Key search terms regarding functioning including “activity limitation”, “functional impairment”, “functional loss”, “disability”, and “participation restriction” were used in varying combinations with the search terms for the listed health conditions. After analysing text words contained in titles and abstracts, and index words selected to describe key articles, additional search terms were added to the search strategy. Similar searches of the remaining electronic databases were done by adapting the various combinations of identified key words to the unique searching features of the databases. We used a wide search to include Title, Abstract and Key Words fields, to avoid missing important articles whose titles may not reflect the content of the article. The final search strategies for the five databases are provided (Supplementary File S2). We manually reviewed the reference lists of eligible studies for studies that may have been missed during the initial database searches.
All database search results were transferred to Rayyan reference management software [33]. Deduplication of all retrieved articles was done in Rayyan prior to the initial phase of screening by title and abstract.
2.2. Study Selection
After deduplication, one reviewer (MYC) reviewed all the titles and abstracts using pre-determined criteria and consulted a second reviewer (KB) or third reviewer (QAL) when unsure. One reviewer (MYC) further reviewed the full texts of the eligible articles to check that they had the required information. The reasons for excluding ineligible studies after reviewing the full texts were documented. There was no need to contact any authors of the included studies for further data clarification or additional information during the eligibility assessment as all data were clear.
2.3. Charting the Data
To ensure consistency and clarity of charted data, the reviewers held discussions to determine the variables, and nature and extent of the information to be extracted from the eligible studies. A custom data extraction form (available online: http://osf.10/7h6xz accessed on 15 March 2022) was initially developed in Microsoft Excel and revised iteratively after being piloted on a sample of 33 full text articles on stroke. The data extraction process was however cumbersome and time-consuming as it involved clicking across several columns in Excel and having to copy and paste every data entry. The potential for several errors and omissions during data entry and ICF classification existed, which would have affected the validity of our results [34]. Additionally, we encountered difficulty in filtering the layers of information—several health conditions needed to be considered to get an overview of functioning problems compared across health conditions, and each health condition was often associated with several functioning problems. These practical difficulties and concerns led to the design and development of a secure, web-based software application named Rehab4all [35]. One reviewer (MYC) subsequently extracted data from all eligible studies using the Rehab4all application while a second reviewer (QAL) checked for accuracy.
Data items included the first author and year of publication, study design, setting (rural, urban, or semi-urban), level of care (rehabilitation centre, PHC facility, specialized hospital), health condition (using the International Classification of Diseases 11th revision: ICD-11 [36] in combination with the GBD Institute for Health Metrics [37]), multimorbidity (the co-existence of two or more chronic health conditions in an individual), study design and description of sample population, including sex, and mean age. Details regarding outcome measures used to evaluate function, and the type and prevalence of functioning problems as reported in the articles, were recorded. Where several similar words or synonyms were found to report the same presenting functioning problem, the most familiar word in the South African layman language was selected—for example, “fatigue” and “exhaustion” were represented by “tiredness”. The presenting functioning problems were categorised into major groups based on similar functioning as listed in the Box 1 below.
Box 1. The presenting functioning problems were categorized into major groups based on similar functioning.
| Balance and coordination problems Behaviour problems Bowel and bladder problems Communication problems Fine motor skill problems IADLs problems Joint mobility/stiffness Mental disorders Mobility problems Muscle function/paralysis Pain (acute, chronic, unspecified) |
Physical capacity problems Respiratory problems Self-care problems Sensory problems Skin problems Swallowing problems Swelling Vision problems Weight problems Working and schooling problems Sexuality problems |
Prevalence statistics reporting on different recall periods (point, annual or lifetime) of the functioning problems were extracted. In longitudinal studies, where both baseline and post-intervention prevalence were reported, the baseline was considered as this is when the patient potentially begins to receive rehabilitation. Even for conditions like fractures or Tuberculosis, where rehabilitation is started after medical interventions, baseline data were considered as this time point present the worst-case scenario required for strategic planning [38]. There was no need to contact any authors for further details regarding unclear or incomplete data.
2.4. Quality Assessment
We did not appraise methodological quality or risk of bias of the included studies, in line with guidance on scoping review methodology [29].
2.5. Data Analysis
2.5.1. Type of Functioning Problems
One reviewer (MYC) deductively coded the presenting functioning problems reported in the included studies, using the ICF framework with assistance of the Rehab4all application. The first-level classifications in the ICF are coded with a letter referring to the different components, where b = body functions (nine domains) and s = body structures (nine domains), and d = activities and participation (10 domains). The various components can be further coded with a number referring to second-level domains, third-level categories, and fourth-level qualifiers. Because of the use of the Rehab4all application, human error in coding was minimised. A second reviewer (QAL) checked for completeness and accuracy of the coding. Where the presenting functioning problem reported in the study could not be straightforwardly coded, the main concepts from the assessment tool or outcome measures used to evaluate functioning and vulnerability were used to derive the activity limitation or impairment using ICF linking rules [39].
2.5.2. Prevalence of the Functioning Problems
The pooled prevalence of the identified impairments, activity limitations and/or participation restrictions were calculated. The top 20 most prevalent functioning problems were based on pooled prevalence if at least 5 articles provided prevalence statistics.
3. Results
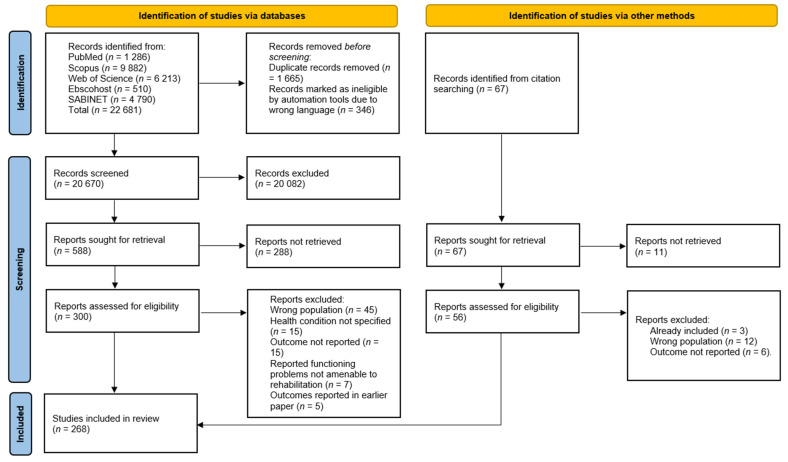
A total of 268 studies met the eligibility criteria. The process of selection of articles at each phase and the reasons for excluding articles are detailed in the PRISMA flow diagram (Figure 1) [40].
Figure 1.
PRISMA flow diagram.
3.1. Study Characteristics
The sample sizes totalled to 242,085 study participants. The mean age for the included sample could not be calculated as some studies did not report age as a mean (i.e., either reported the median or ranges of age groups). Almost half of the studies (47%) were conducted at primary care level (which included the out-patient clinics of secondary or tertiary hospitals), 22% were conducted in in-patient wards at hospitals, 13% in the community, 9% in specialized hospitals, 7% in rehabilitation facilities while 3% did not report the care level. The geo-location was not reported in 23% of the articles, while 62% of the studies were carried out in urban settings, 11% in rural settings and 3% in peri-urban settings. Most of the studies (43%) were descriptive cross-sectional studies, 28% were cohort studies, 10% were case studies/series, 7% were randomized control trials, while case–control studies, quantitative surveys, quasi-experimental studies, and reviews made up the remaining 12%.
Most studies reported on functioning problems associated with HIV and associated Tuberculosis, stroke, and diabetes mellitus (Table 1).
Table 1.
Number of articles according to the top ten health conditions contributing to greatest disability in South Africa.
| Condition | Sub-Category | No of Articles (n) | Subtotals |
|---|---|---|---|
| HIV | HIV only [41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163] | 126 | |
| HIV with TB [164,165,166,167,168,169,170,171,172,173] | 10 | ||
| HIV with Kaposi’s sarcoma [174,175] | 2 | ||
| HIV with Cryptococcal Meningocele [176] | 1 | 139 | |
| Tuberculosis | TB, unspecified [148,177,178,179,180,181,182,183,184,185,186,187,188,189,190] | 15 | |
| TB, MDR [191,192,193,194,195,196,197,198,199,200] | 10 | ||
| TB, pulmonary [201,202,203] | 3 | ||
| TB, spinal [204,205,206] | 3 | ||
| TB, tuberculoma [207] | 1 | ||
| TB, meningitis [208] | 1 | 33 | |
| Stroke | Stroke, unspecified [148,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227,228,229,230,231] | 24 | 24 |
| Diabetes Mellitus | DM, Type unspecified [232,233,234,235,236,237,238,239] | 8 | |
| DM, Type II [240,241,242,243,244,245,246] | 7 | ||
| DM, Type I [241,242] | 2 | ||
| DM with hypertension [247] | 1 | ||
| DM with HIV [248] | 1 | 19 | |
| Spinal pain | Neck pain [249,250,251,252,253,254,255,256] | 8 | |
| LBP, mechanical [252,254,257,258,259,260] | 6 | ||
| LBP, pathological [261,262,263] | 3 | 17 | |
| Fracture/dislocation | Lower limb fracture/dislocation [264,265,266,267,268] | 5 | |
| Upper limb fracture/dislocation [269,270,271,272,273] | 5 | ||
| Pathological fracture(s) [274,275] | 2 | ||
| Spinal fracture(s) [276,277] | 2 | ||
| Rib fracture(s) [278] | 1 | ||
| Skull/cranial fracture(s) [279] | 1 | ||
| Fracture, unspecified [280] | 1 | 17 | |
| Arthritis | Rheumatoid arthritis [281,282,283,284,285] | 5 | |
| OA, hip [286] | 1 | ||
| OA, knee [287] | 1 | ||
| OA, other [237] | 1 | 8 | |
| Burns | Burns only [288,289,290,291,292] | 5 | |
| Burns with amputation [293] | 1 | 6 | |
| Hearing loss | Hearing loss [293,294,295] | 3 | 3 |
| Headaches | Headache, cervicogenic [296] | 1 | |
| Headache, unspecified [254] | 1 | 2 |
DM—diabetes mellitus, HIV—human immunodeficiency virus, LBP—low back pain, OA—osteoarthritis, TB—tuberculosis, TB, MDR—multidrug resistant tuberculosis. Background color: Pathological-blue, Arthritis—blue; Hearing loss -blue, Headache—unshaded and LBP-shaded.
3.2. Prevalence of the Top 20 Functioning Problems
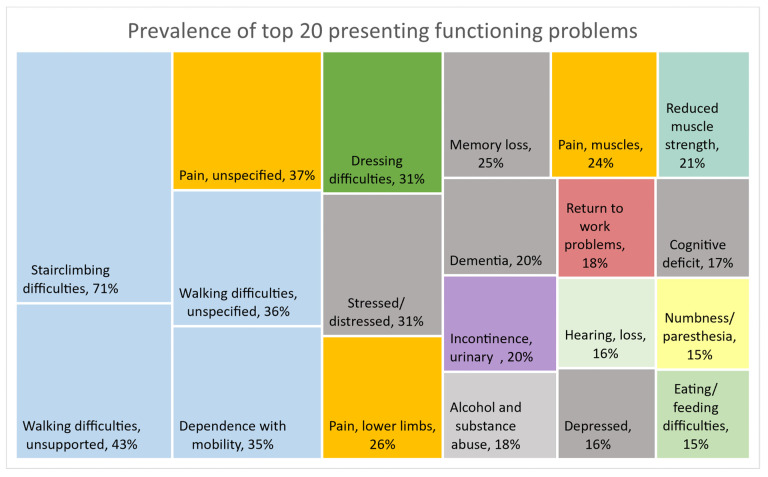
A total of 130 different presenting functioning problems, described by nature and/or body area, were identified from the literature. The reported functioning problems were mostly associated with HIV, Tuberculosis, Diabetes Mellitus and Stroke, and the reported prevalence ranged from 0.1 to 97%. Figure 2 provides an overview of the prevalence of the top 20 functioning problems, considered if at least five articles provided prevalence data, to provide an overview of the most prevalent presenting functioning problems. Mobility problems (shaded blue)—which included difficulty with stairclimbing (70.6%) and difficulties with unsupported walking (43.4%)—and walking difficulties—which were not further described (36.4%)—were most prevalent. Similarly, pain (shaded yellow) of unspecified nature (37.3%), muscle pain (24.3%) and pain that affected the lower limbs (26.4%) had high prevalence. Mental health problems (shaded grey) such as stress, depression, loss of memory and cognitive deficit had prevalence ranging between 15.9% and 30.7%. Respiratory symptoms were not highly prevalent in these populations.
Figure 2.
Prevalence (calculated if statistics from at least five articles were available) of top 20 functioning problems from at least 5 articles.
3.3. Breakdown of the Most Prevalent Problems
The most prevalent functioning problems (the top 20) mostly fell under mobility, pain, and mental categories of the ICF. To further understand these three most prevalent groups of problems, we report on the other functioning problems that fell under these categories regardless of the number of articles that reported them.
3.3.1. Mobility Problems
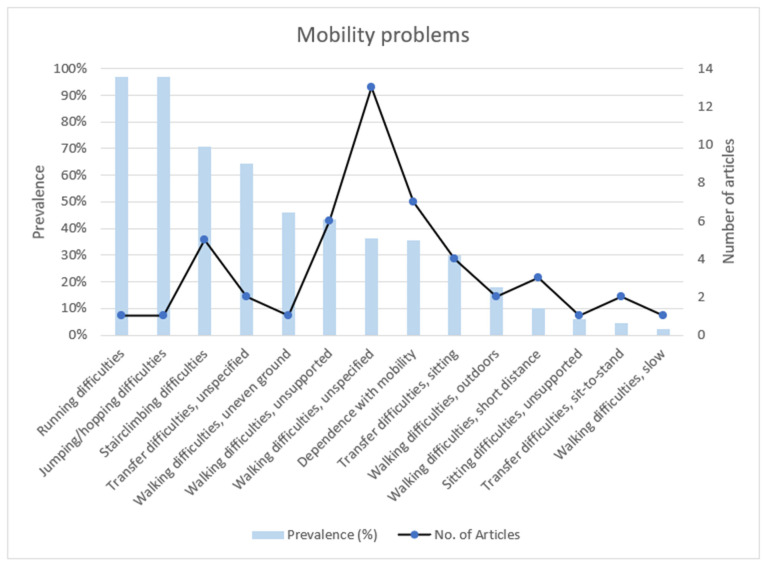
Figure 3 highlights the number of articles and prevalence reported for mobility problems. Articles that reported on mobility problems mostly reported on walking difficulties without giving further description of the problem. The most prevalent mobility problems were difficulties with high-level functioning activities such as jumping/hopping (97%), running (97%) and stairclimbing (70.6%). However, of these high-level functioning activities, only stairclimbing was reported on by at least 5 articles (6 articles). Walking with unsteady gait and standing difficulties were reported by 4 and 3 articles, respectively, but without reporting the prevalence. Related to mobility problems, were falls (7.1% from 7 articles), fear of falling (20%, from 1 article) and balance problems (2.7%, from 4 articles).
Figure 3.
Prevalence and number of articles reporting on mobility problems.
3.3.2. Pain Problems
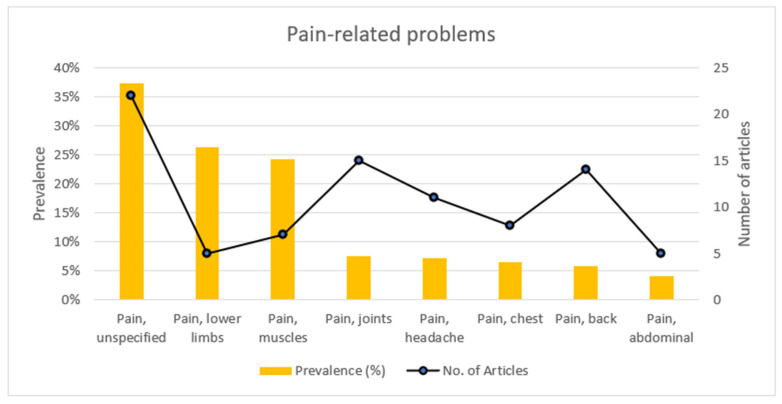
Figure 4 highlights the number of articles and prevalence reported for pain-related problems. Articles reporting on pain mostly reported on the prevalence of pain but did not specify the nature of the pain or the body area affected. The body area reported to have the highest prevalence of pain (26.4%) were the lower limbs. Pain of muscular origin had a higher prevalence than joint pain (24.3% versus 7.5%). Allodynia and pain of the upper limbs were reported by one article each but without reporting the prevalence.
Figure 4.
Prevalence of, and number of articles reporting on, pain-related problems.
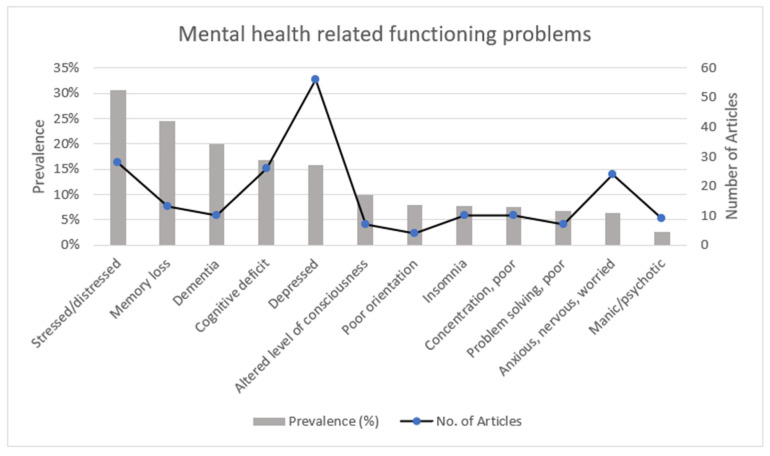
3.3.3. Mental Health Problems
The most reported mental health problem (shown in Figure 5) was being depressed, reported on by 56 articles. The most prevalent mental health related functioning problem was stress (30.7%). Associated behavioural problems included alcohol and substance abuse, which had a prevalence of 18% and was reported by 31 articles. Suicidal ideation had a low prevalence of 2.3% and was reported on by 13 articles.
Figure 5.
Prevalence of, and number of articles reporting on, mental health related functioning problems.
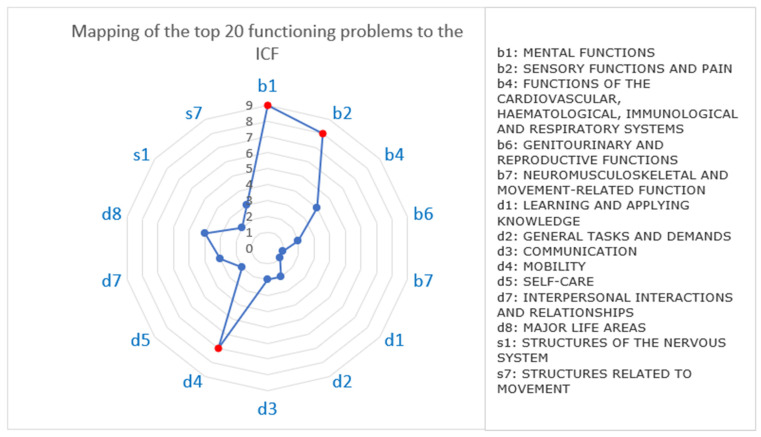
3.4. Mapping to the ICF
The top 20 presenting functioning problems were mapped to the ICF domains and categories using the outcome measures used in the studies (Table 2). For example, Parker et al. [139] used the Brief Pain Inventory to explore the impact of pain on sleep. The identified functioning problems covered five of the nine body function domains, two of the nine body structure domains and six of the 10 activity limitation and participation domains. Most of the presenting functioning problems affected b1 mental functions (n = 9), b2 sensory functions and pain (n = 8), and d4 mobility (n = 7) (Figure 6). Some functioning problems spanned across several ICF domains—for example, unspecified pain and return to work problems spanned across seven, cognitive deficits and depression spanned across six and five domains, respectively. Most studies provided sufficient information to code the identified functioning problems as far as the fourth level. For example, to add further detail on mobility problems, the walking distance was specified, e.g., d4501 walking long distance, the location was specified, e.g., d4600 moving around within the home. No ICF code was found to indicate walking speed.
Table 2.
Mapping of top 20 presenting functioning problems to the ICF according to related outcome measures.
| Problem | ICF Domain | ICF Code/Category | Outcome Measures |
|---|---|---|---|
| Stairclimbing difficulties | d4 MOBILITY | d455 moving around | Barthel Index (BI); [211,216,217] Rivermead Motor Assessment scores of Gross function (RMA-G); Nottingham extended activities of daily living (NEADL) scale [297] |
| Walking difficulties, unsupported | d4 MOBILITY | d450 Walking d465 Moving around using equipment |
Rivermead Mobility Index (RMI); [215] Berg Balance Scale (BBS); [215] Postural Assessment Scale for Stroke Patients (PASS); [215] self-report; [76] Use of assistive devices [227] |
| Pain, unspecified | b1 MENTAL FUNCTIONS | b134 Sleep functions b152 Emotional functions |
Wisconsin Brief Pain Questionnaire (WBPQ); [125] Beck Depression Inventory (BDI); [139] Pain Catastrophizing Scale (PCS); [150,249] Hopkins Symptoms Checklist-25 (HSCL-25); [150] Neuropathic Diagnostic Questionnaire (DN4) [249] |
| b2 SENSORY FUNCTIONS AND PAIN | b270 Sensory functions related to temperature and other stimuli b280 Sensation of pain |
Brief Pain Inventory (Xhosa) (BPI-Xhosa); [298] WBPQ; [125,150] Brief Neuropathy Screening Tool (BNST); [150,299] Visual Analogue Scale (VAS), [280] Numeric Pain Rating Scale (NPRS); [249] Brief Peripheral Neuropathy Screen (BPNS) [75] | |
| s7 STRUCTURES RELATED TO MOVEMENT | s750 Structure of lower extremity | ASAMI score, the Foot Function Index (FFI), radiographic outcomes; [300] The Lower Extremity Functional Scale (LEFS) [75] | |
| d2 GENERAL TASKS AND DEMANDS | d240 Handling stress and other psychological demands | HSCL-25 [150] | |
| d4 MOBILITY | d450 Walking | (BPI [130]; Karnofsky Performance Scale (KPS) [125] | |
| d7 INTERPERSONAL INTERACTIONS AND RELATIONSHIPS | d710 Basic interpersonal interactions | BPI [130] | |
| d8 MAJOR LIFE AREAS | d820 School education d845 Acquiring, keeping, and terminating a job |
BPI [130] | |
| Walking difficulties, unspecified | b2 SENSORY FUNCTIONS AND PAIN | b235 Vestibular functions | Self-report [76] |
| d4 MOBILITY | d450 Walking | Self-report [76] | |
| Dependence with mobility | d4 MOBILITY | d450 Walking d465 Moving around using equipment |
Rankin scores; [301] BI; [211] Timed-up-and-go-test; [182] BBS; [215] Nurick classification [205] |
| Dressing difficulties | d5 SELF-CARE | d540 Dressing | BI; [211] World Health Organization’s Disability Assessment Schedule 2.0 (WHODAS 2.0) [209] |
| Stressed/distressed | b1 MENTAL FUNCTIONS | b126 Temperament and personality functions | Questionnaire on Stress in Diabetes—Revised (QSD-R); [244] Breslau PTSD screener [61] |
| d2 GENERAL TASKS AND DEMANDS | d240 Handling stress and other psychological demand | Primary Care PTSD Screen (PC-PTSD); [179] The Kessler Psychological Distress Scale (K-10); [179] Mini-International Neuropsychiatric Interview (MINI); [135] Hopkins Symptom Checklist (HSCL); [101] Composite International Diagnostic Interview (CIDI); [78] CIDI [111] | |
| d7 INTERPERSONAL INTERACTIONS AND RELATIONSHIPS | d750 Informal social relationships | Questionnaire on Stress in Diabetes—Revised (QSD-R) [244] | |
| Pain, lower limbs | b2 SENSORY FUNCTIONS AND PAIN | b280 Sensation of pain | BPI-Xhosa; [138] NPRS; [291] BPNS; [64] Visual Analogue Scale (VAS) [280] |
| s7 STRUCTURES RELATED TO MOVEMENT | s750 Structure of lower extremity | BPI-Xhosa; [57,138] Burn Specific Pain and Anxiety scale (BSPAS) [291] | |
| Memory loss | b1 MENTAL FUNCTIONS | b117 Intellectual functions b144 Memory functions b164 Higher-level cognitive functions |
WHODAS 2.0; [209] International HIV Dementia Scale (IHDS); [93] Neuropsychological (NP) test battery; [132] The revised signs and symptoms checklist for persons with HIV disease (SSC-HIVrev); [146] The International Classification of Functioning, Disability and Health (ICF) [128] |
| Pain, muscles | b2 SENSORY FUNCTIONS AND PAIN | b280 Sensation of pain | ICF; [128] WHODAS 2.0; [107] self-report; [265] SSC-HIVrev [79] |
| Reduced muscle strength | b4 FUNCTIONS OF THE CARDIOVASCULAR, HAEMATOLOGICAL, IMMUNOLOGICAL AND RESPIRATORY SYSTEMS | b455 Exercise tolerance functions | ICF; [128] |
| b7 NEUROMUSCULOSKELETAL AND MOVEMENT-RELATED FUNCTION | b710 Mobility of joint functions b730 Muscle power functions |
ICF; [128] Oxford Scale of muscle strength; [42] isokinetic dynamometry; [269,283] sphygmomanometer [283] | |
| s7 STRUCTURES RELATED TO MOVEMENT | s750 Structure of lower extremity s720 Structure of shoulder region |
ICF; [128] isokinetic dynamometry [269,283] | |
| Dementia | b1 MENTAL FUNCTIONS | b117 Intellectual functions b144 Memory functions b147 Psychomotor functions b152 Emotional functions |
NP test battery; [132] IHDS; [80,155,200] mini-mental state examination (MMSE), Montreal cognitive assessment (MOCA), Simioni symptom questionnaire (SSQ) and cognitive assessment tool-rapid version (CAT-rapid) [95] |
| Incontinence, urinary | b6 GENITOURINARY AND REPRODUCTIVE FUNCTIONS | b620 Urination functions | Self-report [198] BI; [211,217] Survey of Autonomic Symptoms (SAS) [75] |
| Alcohol and substance abuse | b1 MENTAL FUNCTIONS | b117 Intellectual functions b130 Energy and drive functions b152 Emotional functions |
MINI; [155] Alcohol Use Disorder Identification Test (AUDIT); [91,147,189] CAGE questionnaire; [54] Alcohol, Smoking and Substance Involvement Screening Test questionnaire (ASSIST) [102] |
| Return to work problems | b1 MENTAL FUNCTIONS | b117 Intellectual functions b130 Energy and drive functions b144 Memory functions b152 Emotional functions b167 Mental functions of language |
Return to work questionnaire [212,226] |
| b2 SENSORY FUNCTIONS AND PAIN | b210 Seeing functions b280 Sensation of pain |
Return to work questionnaire; [212,226] BPI [212,226] |
|
| b4 FUNCTIONS OF THE CARDIOVASCULAR, HAEMATOLOGICAL, IMMUNOLOGICAL AND RESPIRATORY SYSTEMS | b455 Exercise tolerance functions | Return to work questionnaire [212,226] | |
| b6 GENITOURINARY AND REPRODUCTIVE FUNCTIONS | b620 Urination functions | Return to work questionnaire [212,226] | |
| d3 COMMUNICATION | d330 Speaking | Return to work questionnaire [212,226] | |
| d4 MOBILITY | d445 Hand and arm use d450 Walking d470 Using transportation |
Return to work questionnaire [212,226] | |
| d8 MAJOR LIFE AREAS | d845 Acquiring, keeping, and terminating a job | Return to work questionnaire [212,226,250] | |
| Cognitive deficit | b1 MENTAL FUNCTIONS | b117 Intellectual functions b140 Attention functions b144 Memory functions b147 Psychomotor functions b156 Perceptual functions b160 Thought functions b164 Higher-level cognitive functions |
NP test battery; [157] MoCA; [156] Tampa Scale for Kinesiophobia-11 (TSK-11); PCS; [250] NeuroScreen Performance [157]; IHDS; [80,155,200] MMSE, SSQ and cognitive assessment tool-rapid version (CAT-rapid); [95] Bedside Executive Screening Test (BEST) [245] |
| b3 VOICE AND SPEECH FUNCTIONS | b330 Fluency and rhythm of speech functions | NP test battery; [45,157,171] | |
| b4 FUNCTIONS OF THE CARDIOVASCULAR, HAEMATOLOGICAL, IMMUNOLOGICAL AND RESPIRATORY SYSTEMS | b435 Immunological system functions | Laboratory assessments for immune markers TYMP and NGAL [58] | |
| d4 MOBILITY | d475 Driving | NP test battery and driving simulations [82] | |
| d8 MAJOR LIFE AREAS | d820 School education | NP test battery; [157] | |
| s1 STRUCTURES OF THE NERVOUS SYSTEM | s110 Structure of brain | Brain imaging [302] | |
| Hearing, loss | b2 SENSORY FUNCTIONS AND PAIN | b167 Mental functions of language b230 Hearing functions |
Otoscopy, tympanometry, pure-tone audiometry, and distortion product otoacoustic emissions [66,105,184,191,197] |
| d1 LEARNING AND APPLYING KNOWLEDGE | d166 Reading | South African Sign Language (SASL) [303] | |
| d3 COMMUNICATION | d330 Speaking | SASL [303] | |
| Depressed | b1 MENTAL FUNCTIONS | b126 Temperament and personality functions b130 Energy and drive functions b134 Sleep functions b147 Psychomotor functions b152 Emotional functions |
NP test battery; Patient Health Questionnaire (PHQ-9); [154] Centers for Epidemiologic Studies Depression Scale (CES-D) [108,144] Hospital Anxiety and Depression Scale (HADS) [243] Beck Depression Inventory—Second Edition (BDI II) [133] |
| b2 SENSORY FUNCTIONS AND PAIN | b280 Sensation of pain | PHQ-9; [154] | |
| b4 FUNCTIONS OF THE CARDIOVASCULAR, HAEMATOLOGICAL | b455 Exercise tolerance functions | PHQ-9; [154] | |
| d7 INTERPERSONAL INTERACTIONS AND RELATIONSHIPS | d710 Basic interpersonal interactions d770 Intimate relationships |
Edinburgh Postnatal Depression Scale (EPDS) [60,131] | |
| d8 MAJOR LIFE AREAS | d845 Acquiring, keeping, and terminating a job d850 Remunerative employment |
BPI [57] | |
| Numbness/paraesthesia | b2 SENSORY FUNCTIONS AND PAIN | b265 Touch function b270 Sensory functions related to temperature and stimuli b280 Sensation of pain b840 Sensation related to the skin |
Total Neuropathy Score (TNSr) [64] SCC- HIVrev; [304] Assessment of fine touch, pin-prick and vibration sense for neuropathy symptom score (NSS) and neuropathy disability score (NDS); [192] AIDS Clinical Trials Group BPNS [56] |
| s1 STRUCTURES OF THE NERVOUS SYSTEM | s120 Spinal cord and related structures | Radiological imaging | |
| Eating/feeding difficulties | d5 SELF-CARE | d550 Eating | National Institute of Health Stroke Scale, (NIHSS); [217] WHODAS 2.0; [209] South African dysphagia screening tool (SADS); [213] Self-report [215] |
Figure 6.
Mapping of the top 20 presenting functioning problems to the ICF domains.
4. Discussion
This scoping review established the current evidence from peer-reviewed literature on the types and prevalence of functioning problems contributing to most disability in South African adult populations. The most prevalent functioning problems presenting in the South African adult population when mapped to the ICF were mostly mobility-, pain-, and mental health-related. Most studies were found to be at primary care level highlighting the complexities of functioning problems brought about by the associated health conditions experienced by adult patients seen at this level of care.
The prevalence of functioning problems associated with health conditions in the current study was found to be comparable to studies conducted in similar low-resource settings. For example, the current study reported a high prevalence of 70.2% for stairclimbing difficulties compared to Matter et al. [305] who reported 66.7% of adults in Botswana and 65.1% in Swaziland with difficulty with walking or climbing steps. Functional limitations do not always culminate into functioning problems where social support and the required assistive devices are readily available [306]. Thus, it is imperative to scale-up rehabilitation services in low-resource settings to cater for the specific population needs [26].
A total of 130 different functioning problems were identified. The current disease-oriented approach to health care and highly fragmented health care system often leads to ineffective and sub-optimal rehabilitation care [14]. A person-centred approach will effectively address the wide array of functioning problems associated with health conditions [307]. Most functioning problems are inter-related, therefore, by addressing one functioning problem, it is possible to address the other affected domains. For example, addressing balance problems caused by vestibular or muscle weakness may address walking problems that could in turn solve selfcare and participation issues. The identified functioning problems can be used to create awareness among rehabilitation clinicians of the contextual presenting functioning problems to identify, assess, and provide targeted patient-centred treatment plans. An understanding of individual functioning will provide a clearer picture of the burden associated with a health condition and the impact of the health condition on a persons’ life roles or livelihood [308]. Patients too will have better awareness of their own functioning and rehabilitation needs which may have otherwise been dismissed as normal during illness or ageing, empowering them to become informed decision-makers in their healthcare. Thus, rehabilitation clinicians can work with patients to successfully re-integrate patients into their communities [307].
Mapping the identified functioning problems to the ICF highlighted that most functioning problems spanned across several domains and categories of the ICF. For example, pain spanned affected eight different domains of the ICF, which included mobility, interpersonal relationships and major life areas of education and employment. Rehabilitation alone cannot address the full range of educational, social, and development issues [10]. Collaboration with other sectors (such as labour and transport) is required to address the full spectrum of rehabilitation needs. However, rehabilitation remains the key health strategy with the distinctive role of restoring optimal function and alleviating the effects of living with a health condition, in addition to promotive, preventative, curative and palliative roles. South Africa’s NHI drive supports the strengthening of rehabilitation as a health strategy by improving the access and quality of rehabilitation services particularly at primary care [309]. The current study findings are potentially useful in informing the relevant stakeholders and policymakers regarding rehabilitation service planning and strengthening of rehabilitation services.
Rehabilitation service planning: This reasonable approximation of rehabilitation needs within the South African adult population provided by this review may be useful in forecasting the rehabilitation workforce capacity and workforce competencies required in these contexts. Our study findings suggest that at least 7 in 10 adult patients have a functioning problem amenable to rehabilitation—and mostly in patients seeking primary care. This provides a sobering picture of the reality of the complexity and immensity of rehabilitation needs resulting from the high prevalence and wide range of functioning problems in the adult populations presenting to primary care. Yet, only 6–20% of PHC facilities provide rehabilitation services in South Africa [16]. The NHI seeks to provide adequate and relevantly skilled health workers especially at primary care [18]. Thus, the established priority functioning problems associated with health conditions may be useful indicators of rehabilitation need requisite for human resource planning, with respect to both quality and quantity.
The rehabilitation workforce needs to be competent in the knowledge, skills and attitudes required to serve the specific population needs of these low resourced settings. This is especially so for recently qualified community service therapists who are often the sole rehabilitation providers at PHC in South Africa [310]. The WHO’s RCF [311] may be operationalized based on these context-relevant rehabilitation needs. Rehabilitation continuous development and undergraduate rehabilitation curricula may be revised to fill the identified gaps in skills, knowledge and attitudes required to address these key functioning problems presenting in the South African populations. Similarly, clinical practice guidelines which have been reported to be inadequate or contextually irrelevant may be developed [312]. Because CPG need to be brief and succinct to improve uptake among busy clinicians [313], they may be based on these most prevalent functioning problems and continuously revised to adapt to the changing population demographics. This helps to ensure that the scope of such guidelines is suited to the context and needs of South African populations.
Meanwhile, innovative strategies such as task shifting or sharing may be more feasible in low-resource settings which remain chronically plagued by inadequate human resources or additional staff [314,315]. The descriptions of priority functioning problems identified through the current study may provide guidance on the bare minimum skills or knowledge related to mobility, pain and mental health required by each health care provider. The already available primary care workers are favourably positioned to provide the spectrum of care required to meet the increasing and diverse demands of the population’s health needs [316]. Depending on the level of cadre, training may be provided to ensure adequate identification, referral, or basic management (such as patient education).
Strengthening rehabilitation services: The limited resources in LMICs require that financial resource planning be determined by priority needs. The contextual mapping of the most prevalent functioning problems provided in this study will help ensure that patients access the needed rehabilitation services without suffering financial hardship. It may be useful to have allocated funding within the health systems for rehabilitation of functioning problems. For example, in our study, mobility problems were found to be the most prevalent functioning problem. Many factors contribute to mobility problems requiring collaboration between all health care professionals including all disciplines of rehabilitation at primary care [317]. Foremost is the need for assistive devices, which have been reported to be inadequate in most poorly resourced public healthcare facilities in LMICs, one study [318] reporting that 36% of people requiring assistive devices in Zimbabwe acquired them but two thirds of these having to source them privately. Having funding allocated to mobility problems would ensure acquisition of adequate assistive devices and other rehabilitation services. Thus, the findings from this study will prove valuable in building a rehabilitation investment case for funders, healthcare managers and policymakers to make informed decisions with regard to providing both adequate finance and rehabilitation health workforce in support of strengthening rehabilitation at primary care. In the South African context, the ICF framework has been approved for integration into the coding system for the NHI, in addition to the ICD-11 and International Classification of Health Interventions (ICHI). Therefore, the priority functioning problems, mapped to the ICF, and the identified outcome measures will be useful in informing this process.
Mental health-related functioning problems were also found to be, not only highly prevalent in South African adult populations, but also the most reported-on in the reviewed literature. This could have been because mental health is a separate niche of study for specialized professionals including psychologists and psychiatrists. However, there is still lack of prioritisation of resources and policies in response to mental disorders especially at PHC in LMICs including South Africa [319]. The current initiative of clinical guidelines designed to support primary care health workers’ clinical decision-making, namely Primary Care 101, makes little or no reference to rehabilitation in the identification and management of mental health problems [320]. The role of psychosocial rehabilitation is mostly assigned to an auxiliary social worker. However, other health rehabilitation disciplines play significant roles in preventing the onset of mental health problems and facilitating recovery for those experiencing mental health problems, including workplace based mental health programs [321], cognitive rehabilitation interventions, family support and social networks, and physical activity interventions to promote functional independence [322]. Additionally, improved mental health literacy among the patients and caregivers may lead to better treatment planning and health outcomes.
4.1. Strengths and Limitations of the Study
The scoping review provided a comprehensive mapping of functioning problems reported in published scientific literature for adult populations in low resource settings. The ICF which is a standard framework for reporting health and functioning states was used. While our study reported comprehensively on our methodology, the repeatability in other countries will be affected by the availability of relevant peer-reviewed publications on functioning problems related to specified health conditions.
The use of the web-based application Rehab4all enabled a transparent process of extracting the data used. Additionally, this will allow continued updating of evidence as advances in healthcare or reduced health inequities will influence the profile of priority functioning problems in the populations. For example, hearing loss may no longer be a priority functioning loss as new drug treatments with less ototoxic side-effects, e.g., Bedaquiline versus Kanamycin become more available in low-resource settings [197]. Other countries may access or contribute to the data to provide better comparisons of contextually similar settings.
The calculated prevalence was dependent on the number of articles provided. Not all functioning problems were reported on by several articles thus affecting the validity of our results. A statistician or data scientist can be engaged to employ more advanced techniques to analyse the burden of the identified functioning problems and control for confounding factors such as publication bias.
The high proportion of HIV-related functioning problems in effect reflects how the sub-Saharan region continues to be the greatest contributor to the HIV epidemic despite decreased incidence, therefore, there continues to be global research interest and funding opportunities towards HIV-related research. South Africa’s public sector health research funding remains below the proposed 2% of the national health budget [323]. However, more research is needed in other health conditions.
4.2. Further Research
Additional research such as a qualitative study may be important to validate the study findings and fill the gaps in findings especially regarding participation restrictions. Cross-sectional studies may be done to determine the prevalence of the functioning problems that were reported qualitatively such as in case studies or case series.
Environmental factors were not considered in this review as this requires a more extensive review of the barriers and facilitators of functioning within the selected contexts.
The prevalence of multimorbidity is high in South Africa [15]. The review could be taken further into understanding the functioning problems associated with common multimorbidity patterns. Authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
Considering the enormity of the review, we pragmatically selected the top ten health conditions contributing to greatest disease burden in South Africa based on the GBD 2019 estimates [8]. Thus, we may have missed notable health conditions in South Africa such as neurodegenerative disorders that are especially associated with HIV and ageing. Except for dementia, the lack of standardized and widely accepted screening and diagnostic tools/criteria which facilitate epidemiological studies of other common neurodegenerative conditions, e.g., Guillain Barre Syndrome or Parkinsonism may be reason for the lack of evidence regarding their prevalence in South Africa [324]. Similarly, our review was limited to adult populations. As a result, genetic diseases which are more highly prevalent in children and young adults were not included. Perhaps future reviews may address these health conditions and/or populations.
5. Conclusions
The study has provided an example of how other poorly resourced countries can leverage on already published evidence on functioning problems as a first step in a transparent process towards informed planning in strengthening rehabilitation within health systems. The scoping review has identified the most prevalent functioning problems associated with health conditions contributing to most disability in South Africa. The wide range of highly prevalent functioning problems were mostly reported in populations at primary care. The most common problems were associated with mobility, mental health, and pain. This points towards targeted planning of innovative strategies towards strengthening rehabilitation service delivery at primary care to address these complexities where there is an inadequate rehabilitation workforce.
Early detection of these key functioning problems by the health system at primary care can be facilitated by routine screening for the identified functioning problems through available and contextually appropriate easy to use tools. The country’s PHC system can be re-engineered to provide health promotion and prevention services that target the key functioning problems. This can be achieved through effective knowledge dissemination and self-management strategies within the communities as well as training for the available primary care cadre to provide brief interventions or appropriate referral for rehabilitation care. These moderate changes to will ultimately result in improved population health outcomes and achieving universal health coverage for disadvantaged populations in poorly resourced settings.
Acknowledgments
The authors wish to thank Alvina Matthee of the Faculty of Medicine and Health Sciences Library, University of Stellenbosch for guidance in developing the literature search strategy. We also thank Denric Blaauw for the development of the Rehab4all application.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192315636/s1. File S1: Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist; File S2: Full electronic search strategy for all databases.
Author Contributions
M.Y.C. was the major contributor in drafting and writing the manuscript as part of her thesis in fulfillment of the requirements of her doctoral degree. Conceptualization, Q.A.L.; Methodology, Q.A.L., K.B. and M.Y.C.; Software, Q.A.L.; Validation, Q.A.L. and K.B.; Formal Analysis, M.Y.C. and Q.A.L.; Investigation, M.Y.C. and Q.A.L.; Data Curation, M.Y.C. and Q.A.L.; Writing—Original Draft Preparation, M.Y.C.; Writing—Review and Editing, Q.A.L. and K.B.; Visualization, M.Y.C. and Q.A.L.; Supervision, Q.A.L. and K.B.; Project Administration, M.Y.C.; Funding Acquisition, Q.A.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions of Rehab4all application developed.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Medical Research Council of South Africa (Grant SU-PT-15/10-000005) and the National Research Foundation Chair Initiative (UID 115461).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stucki G., Bickenbach J. Functioning: The Third Health Indicator in the Health System and the Key Indicator for Rehabilitation. Eur. J. Phys. Rehabil. Med. 2017;53:134–138. doi: 10.23736/S1973-9087.17.04565-8. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . How to Use the ICF: A Practical Manual for Using the International Classification of Functioning, Disability and Health (ICF). Exposure Draft for Comment. World Health Organization; Geneva, Switzerland: 2013. [Google Scholar]
- 3.Barua A., Hazarika J., Basilio M.A., Soans S.J., Colin M., Kamath A. Functional Impairments: A Study in Elderly Individuals. J. Int. Med. Sci. Acad. 2011;24:61–63. [Google Scholar]
- 4.Duntava A., Borisova L.V., Mäkinen I.H. The Structure of Health in Europe: The Relationships between Morbidity, Functional Limitation, and Subjective Health. SSM—Popul. Health. 2021;16:100911. doi: 10.1016/j.ssmph.2021.100911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD 2019 Diseases and Injuries Collaborators Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vos T., Flaxman A.D., Naghavi M., Lozano R., Michaud C., Ezzati M., Shibuya K., Salomon J.A., Abdalla S., Aboyans V., et al. Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries 1990-2010: A Systematic Analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jesus T.S., Landry M.D., Hoenig H. Global Need for Physical Rehabilitation: Systematic Analysis from the Global Burden of Disease Study 2017. Int. J. Environ. Res. Public Health. 2019;16:980. doi: 10.3390/ijerph16060980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Louw Q., Grimmer K., Berner K., Conradie T., Bedada D.T., Jesus T.S. Towards a Needs-Based Design of the Physical Rehabilitation Workforce in South Africa: Trend Analysis [1990–2017] and a 5-Year Forecasting for the Most Impactful Health Conditions Based on Global Burden of Disease Estimates. BMC Public Health. 2021;21:913. doi: 10.1186/s12889-021-10962-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madden R., Ferreira M., Einfeld S., Emerson E., Manga R., Refshauge K., Llewellyn G. New Directions in Health Care and Disability: The Need for a Shared Understanding of Human Functioning. Aust. N. Z. J. Public Health. 2012;36:458–461. doi: 10.1111/j.1753-6405.2012.00889.x. [DOI] [PubMed] [Google Scholar]
- 10.Stucki G., Bickenbach J., Gutenbrunner C., Melvin J. Rehabilitation: The Health Strategy of the 21st Century. J. Rehabil. Med. 2018;50:309–316. doi: 10.2340/16501977-2200. [DOI] [PubMed] [Google Scholar]
- 11.Rauch A., Negrini S., Cieza A. Toward Strengthening Rehabilitation in Health Systems: Methods Used to Develop a WHO Package of Rehabilitation Interventions. Arch. Phys. Med. Rehabil. 2019;100:2205–2211. doi: 10.1016/j.apmr.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Mills J.A., Cieza A., Short S.D., Middleton J.W. Development and Validation of the WHO Rehabilitation Competency Framework: A Mixed Methods Study. Arch. Phys. Med. Rehabil. 2021;102:1113–1123. doi: 10.1016/j.apmr.2020.10.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson L.F., Meyer-Rath G., Dorrington R.E., Puren A., Seathlodi T., Zuma K., Feizzadeh A. The Effect of HIV Programs in South Africa on National HIV Incidence Trends, 2000–2019. J. Acquir. Immune Defic. Syndr. 2022;90:115–123. doi: 10.1097/QAI.0000000000002927. [DOI] [PubMed] [Google Scholar]
- 14.Maphumulo W.T., Bhengu B.R. Challenges of Quality Improvement in the Healthcare of South Africa Post-Apartheid: A Critical Review. Curationis. 2019;42:1901. doi: 10.4102/curationis.v42i1.1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roomaney R.A., van Wyk B., Cois A., Wyk V.P. Van One in Five South Africans Are Multimorbid: An Analysis of the 2016 Demographic and Health Survey. PLoS ONE. 2022;17:e0269081. doi: 10.1371/journal.pone.0269081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conradie T., Berner K., Louw Q. Describing the Rehabilitation Workforce Capacity Data in the Public Sector of Three Rural Provinces in South Africa. Int. J. Environ. Res. Public Health. 2022;19:12176. doi: 10.3390/ijerph191912176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Achoki T., Sartorius B., Watkins D., Glenn S.D., Kengne A.P., Oni T., Wiysonge C.S., Walker A., Adetokunboh O.O., Babalola T.K., et al. Health Trends, Inequalities and Opportunities in South Africa’s Provinces, 1990–2019: Findings from the Global Burden of Disease 2019 Study. J. Epidemiol. Community Health. 2022;76:471–481. doi: 10.1136/jech-2021-217480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.South African National Department of Health . National Health Act: National Health Insurance Policy: Towards Universal Health Coverage | South African Government. NDoH; Pretoria, South Africa: 2017. [Google Scholar]
- 19.Conradie T., Charumbira M., Bezuidenhout M., Leong T., Louw Q. Rehabilitation and Primary Care Treatment Guidelines, South Africa. Bull. World Health Organ. 2022;100:689–698. doi: 10.2471/BLT.22.288337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cieza A., Oberhauser C., Bickenbach J., Chatterji S., Stucki G. Towards a Minimal Generic Set of Domains of Functioning and Health. BMC Public Health. 2014;14:218. doi: 10.1186/1471-2458-14-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prodinger B., Cieza A., Oberhauser C., Bickenbach J., Üstün T.B., Chatterji S., Stucki G. Toward the International Classification of Functioning, Disability and Health (ICF) Rehabilitation Set: A Minimal Generic Set of Domains for Rehabilitation as a Health Strategy. Arch. Phys. Med. Rehabil. 2016;97:875–884. doi: 10.1016/j.apmr.2015.12.030. [DOI] [PubMed] [Google Scholar]
- 22.Bright T., Wallace S., Kuper H. A Systematic Review of Access to Rehabilitation for People with Disabilities in Low-and Middle-Income Countries. Int. J. Environ. Res. Public Health. 2018;15:2165. doi: 10.3390/ijerph15102165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitra S., Chen W., Hervé J., Pirozzi S., Yap J. Invisible or Mainstream? Disability in Surveys and Censuses in Low- and Middle-Income Countries. Soc. Indic. Res. 2022;163:219–249. doi: 10.1007/s11205-022-02879-9. [DOI] [Google Scholar]
- 24.Sabariego C., Fellinghauer C., Lee L., Kamenov K., Posarac A., Bickenbach J., Kostanjsek N., Chatterji S., Cieza A. Generating Comprehensive Functioning and Disability Data Worldwide: Development Process, Data Analyses Strategy and Reliability of the WHO and World Bank Model Disability Survey. Arch. Public Health. 2022;80:6. doi: 10.1186/s13690-021-00769-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Banks L.M., Kuper H., Polack S. Poverty and Disability in Low-And Middleincome Countries: A Systematic Review. PLoS ONE. 2017;12:e0189996. doi: 10.1371/journal.pone.0189996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gutenbrunner C., Bickenbach J., Melvin J., Lains J., Nugraha B. Strengthening Health-Related Rehabilitation Services at the National Level. J. Rehabil. Med. 2018;50:317–325. doi: 10.2340/16501977-2217. [DOI] [PubMed] [Google Scholar]
- 27.Charumbira M.Y., Berner K., Louw Q.A. Functioning Problems Associated with Conditions with Greatest Disease Burden in South Africa and Zimbabwe: A Scoping Review Protocol. F1000Research. 2022;11:371. doi: 10.12688/f1000research.110314.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arksey H., O’Malley L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 29.Peters M.D.J., Godfrey C., McInerney P., Munn Z., Tricco A.C., Khalil H. Chapter 11: Scoping Reviews (2020 Version); Aromataris, E., Munn, Z., Eds. [(accessed on 28 May 2020)]. Available online: https://reviewersmanual.joannabriggs.org/
- 30.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018;169:467–474. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 31.Groce N.E. Global Disability: An Emerging Issue. Lancet Glob. Health. 2018;6:e724–e725. doi: 10.1016/S2214-109X(18)30265-1. [DOI] [PubMed] [Google Scholar]
- 32.Karimi M., Brazier J. Health, Health-Related Quality of Life, and Quality of Life: What Is the Difference? PharmacoEconomics. 2016;34:645–649. doi: 10.1007/s40273-016-0389-9. [DOI] [PubMed] [Google Scholar]
- 33.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Munn Z., Tufanaru C., Aromataris E. Data Extraction and Synthesis. Am. J. Nurs. 2014;114:49–54. doi: 10.1097/01.NAJ.0000451683.66447.89. [DOI] [PubMed] [Google Scholar]
- 35.Charumbira M.Y., Blaauw D., Berner K., Louw Q.A. Development of an Innovative Strategy to Determine Functioning Problems Attributed to Health Conditions in Low Resource Settings. Digit. Health. 2022 doi: 10.1177/20552076221144213. Submitted . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harrison J.E., Weber S., Jakob R., Chute C.G. ICD-11: An International Classification of Diseases for the Twenty-First Century. BMC Med. Inform. Decis. Mak. 2021;21:206. doi: 10.1186/s12911-021-01534-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Institute for Health Metrics and Evaluation University of Washington GBD Compare | IHME Viz Hub. [(accessed on 11 March 2021)]. Available online: https://vizhub.healthdata.org/gbd-compare/
- 38.Vollmar H.C., Ostermann T., Redaèlli M. Using the Scenario Method in the Context of Health and Health Care—A Scoping Review Data Collection, Quality, and Reporting. BMC Med. Res. Methodol. 2015;15:89. doi: 10.1186/s12874-015-0083-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maritz R., Baptiste S., Darzins S.W., Magasi S., Weleschuk C., Prodinger B. Linking Occupational Therapy Models and Assessments to the ICF to Enable Standardized Documentation of Functioning. Can. J. Occup. Ther. 2018;85:330–341. doi: 10.1177/0008417418797146. [DOI] [PubMed] [Google Scholar]
- 40.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bantjes J., Kagee A. Suicide Prevention in HIV Treatment Centres: Population Attributable Risk Analysis of Treating Common Mental Disorders. AIDS Behav. 2021;25:1864–1872. doi: 10.1007/s10461-020-03116-5. [DOI] [PubMed] [Google Scholar]
- 42.Benjamin N.A., Jelsma J. An Innovative Approach to Reducing Pain in Patients with Peripheral Neuropathy Related to HIV: A Single Case Study. Afr. J. Disabil. 2014;3:1–4. doi: 10.4102/ajod.v3i1.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cholera R., Pence B.W., Gaynes B.N., Bassett J., Qangule N., Pettifor A., Macphail C., Miller W.C. Depression and Engagement in Care Among Newly Diagnosed HIV-Infected Adults in Johannesburg, South Africa. AIDS Behav. 2017;21:1632–1640. doi: 10.1007/s10461-016-1442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spies G., Fennema-Notestine C., Archibald S.L., Cherner M., Seedat S. Neurocognitive Deficits in HIV-Infected Women and Victims of Childhood Trauma. AIDS Care. 2012;24:1126–1135. doi: 10.1080/09540121.2012.687813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Spies G., Fennema-Notestine C., Cherner M., Seedat S. Changes in Cognitive Function in Women with HIV Infection and Early Life Stress. AIDS Care. 2017;29:14–23. doi: 10.1080/09540121.2016.1204417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Spies G., Kader K., Kidd M., Smit J., Myer L., Stein D.J., Seedat S. Validity of the K-10 in Detecting DSM-IV-Defined Depression and Anxiety Disorders among HIV-Infected Individuals. AIDS Care. 2009;21:1163–1168. doi: 10.1080/09540120902729965. [DOI] [PubMed] [Google Scholar]
- 47.Stanton A.M., Lee J.S., Wirtz M.R., Andersen L.S., Joska J., Safren S.A., Van Zyl R., Conall S. Tobacco Use and Health-Related Quality of Life Among Individuals with Depression Who Are Receiving Treatment for HIV in Cape Town, South Africa. Int. J. Behav. Med. 2021;28:417–430. doi: 10.1007/s12529-020-09951-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Säll L., Salamon E., Allgulander C., Owe-Larssson B. Psychiatric Symptoms and Disorders in HIV Infected Mine Workers in South Africa. Afr. J. Psychiatry. 2009;12:206–212. doi: 10.4314/ajpsy.v12i3.48495. [DOI] [PubMed] [Google Scholar]
- 49.Troeman Z.C.E., Spies G., Cherner M., Archibald S.L., Fennema-notestine C., Theilmann R.J., Spottiswoode B., Stein D.J., Seedat S. Impact of Childhood Trauma on Functionality and Quality of Life in HIV-Infected Women. Health Qual. Life Outcomes. 2011;9:84. doi: 10.1186/1477-7525-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tshifularo M., Govender L., Monama G. Otolaryngological, Head and Neck Manifestations in HIV-Infected Patients Seen at Steve Biko Academic Hospital in Pretoria, South Africa. S. Afr. Med. J. 2013;103:464. doi: 10.7196/SAMJ.6786. [DOI] [PubMed] [Google Scholar]
- 51.Uys H. Prevalence and Clinical Presentation of HIV Positive Female Psychiatric Inpatients. Afr. J. Psychiatry. 2013;16:23–28. doi: 10.4314/ajpsy.v16i1.4. [DOI] [PubMed] [Google Scholar]
- 52.Venter W.D.F., Moorhouse M., Sokhela S., Fairlie L., Mashabane N., Masenya M., Serenata C., Akpomiemie G., Qavi A., Chandiwana N., et al. Dolutegravir plus Two Different Prodrugs of Tenofovir to Treat HIV. N. Engl. J. Med. 2019;381:803–815. doi: 10.1056/NEJMoa1902824. [DOI] [PubMed] [Google Scholar]
- 53.Venter W.D.F., Sokhela S., Simmons B., Moorhouse M., Fairlie L., Mashabane N., Serenata C., Akpomiemie G. Dolutegravir with Emtricitabine and Tenofovir Alafenamide or Tenofovir Disoproxil Fumarate versus Efavirenz, Emtricitabine, and Tenofovir Disoproxil Fumarate for Initial Treatment of HIV-1 Infection (ADVANCE): Week 96 Results from a Randomised, Phase 3. Lancet HIV. 2020;7:e666–e676. doi: 10.1016/S2352-3018(20)30241-1. [DOI] [PubMed] [Google Scholar]
- 54.Cichowitz C., Maraba N., Hamilton R., Charalambous S., Hoffmann C.J. Depression and Alcohol Use Disorder at Antiretroviral Therapy Initiation Led to Disengagement from Care in South Africa. PLoS ONE. 2017;12:e0189820. doi: 10.1371/journal.pone.0189820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vermaak J.R., Dave J.A., Levitt N., Heckmann J.M. Sensory Neuropathy and Metabolic Risk Factors in Human Immune Deficiency Virus Infected South Africans Receiving Protease Inhibitors. AIDS Res. Ther. 2015;12:30. doi: 10.1186/s12981-015-0073-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wadley A.L., Cherry C.L., Price P., Kamerman P.R. HIV Neuropathy Risk Factors and Symptom Characterization in Stavudine-Exposed South Africans. J. Pain Symptom Manag. 2011;41:700–706. doi: 10.1016/j.jpainsymman.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 57.Wadley A.L., Mitchell D., Kamerman P.R. Resilience Does Not Explain the Dissociation between Chronic Pain and Physical Activity in South Africans Living with HIV. PeerJ. 2016;4:e2464. doi: 10.7717/peerj.2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Williams M.E., Ipser J.C., Stein D.J., Joska J.A., Naudé P.J.W. The Association of Immune Markers with Cognitive Performance in South African HIV-Positive Patients. J. Neuroimmune Pharmacol. 2019;14:679–687. doi: 10.1007/s11481-019-09870-1. [DOI] [PubMed] [Google Scholar]
- 59.Witten J.A., Thomas K.G.F., Westgarth-taylor J., Joska J.A., Witten J.A., Thomas K.G.F., Westgarth-taylor J., Witten J.A., Thomas K.G.F., Westgarth-taylor J., et al. Executive Dyscontrol of Learning and Memory: Findings from a Clade C HIV-Positive South African Sample. Clin. Neuropsychol. 2015;29:956–984. doi: 10.1080/13854046.2015.1108455. [DOI] [PubMed] [Google Scholar]
- 60.Wong M., Myer L., Zerbe A., Phillips T., Petro G., Claude A., Remien R.H., Shiau S., Brittain K., Abrams E.J. Depression, Alcohol Use, and Stigma in Younger versus Older HIV-Infected Pregnant Women Initiating Antiretroviral Therapy in Cape Town, South Africa. Arch. Womens Ment. Health. 2017;20:149–159. doi: 10.1007/s00737-016-0688-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yemeke T.T., Sikkema K.J., Watt M.H., Ciya N., Robertson C., Joska J.A. Screening for Traumatic Experiences and Mental Health Distress Among Women in HIV Care in Cape Town, South Africa. J. Interpers. Violence. 2020;35:4842–4862. doi: 10.1177/0886260517718186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dos Santos M., Wolvaardt G. Integrated Intervention for Mental Health Co-Morbidity in HIV-Positive Individuals: A Public Health Assessment. Afr. J. AIDS Res. 2016;15:325–331. doi: 10.2989/16085906.2016.1229683. [DOI] [PubMed] [Google Scholar]
- 63.Van Coppenhagen B., Duvenage H.S. Prevalence of Depression in People Living with HIV and AIDS at the Kalafong Provincial Tertiary Hospital Antiretroviral Clinic. S. Afr. J. Psychiatry. 2019;25:1–6. doi: 10.4102/sajpsychiatry.v25i0.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van der Watt J.J., Benatar M.G., Harrison T.B., Carrara H., Heckmann J.M. Isoniazid Exposure and Pyridoxine Levels in Human Immunodeficiency Virus Associated Distal Sensory Neuropathy. Int. J. Tuberc. Lung Dis. 2015;19:1312–1319. doi: 10.5588/ijtld.15.0467. [DOI] [PubMed] [Google Scholar]
- 65.Cobbing S. A Home-Based Rehabilitation Intervention for Adults Living With HIV: A Randomized Controlled Trial. J. Assoc. Nurses AIDS Care. 2017;28:105–117. doi: 10.1016/j.jana.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 66.van der Westhuizen Y., Swanepoel D.W., Heinze B., Hofmeyr L.M. Auditory and Otological Manifestations in Adults with HIV/AIDS. Int. J. Audiol. 2013;52:37–43. doi: 10.3109/14992027.2012.721935. [DOI] [PubMed] [Google Scholar]
- 67.Woollett N., Cluver L., Bandeira M., Brahmbhatt H. Identifying Risks for Mental Health Problems in HIV Positive Adolescents Accessing HIV Treatment in Johannesburg. J. Child Adolesc. Ment. Health. 2017;29:11–26. doi: 10.2989/17280583.2017.1283320. [DOI] [PubMed] [Google Scholar]
- 68.Chiliza N., Du Toit M., Wasserman S. Outcomes of HIV-Associated Pneumocystis Pneumonia at a South African Referral Hospital. PLoS ONE. 2018;13:e0201733. doi: 10.1371/journal.pone.0201733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cross H.M., Combrinck M.I., Joska J.A. HIV-Associated Neurocognitive Disorders: Antiretroviral Regimen, Central Nervous System Penetration Effectiveness, and Cognitive Outcomes. S. Afr. Med. J. 2013;103:758. doi: 10.7196/SAMJ.6677. [DOI] [PubMed] [Google Scholar]
- 70.Cullen C., Bch M.B., Sa F., Ophth M. Case Report: Successful Treatment of Bilateral Visual Loss Caused by Idiopathic Optic Neuritis in an HIV-Infected Patient. S. Afr. J. HIV Med. 2011;12:29–32. doi: 10.4102/sajhivmed.v12i4.169. [DOI] [Google Scholar]
- 71.Daniels A.K., Van Niekerk R.L. Van The Impact of a Therapeutic Exercise Intervention on Depression and Body Self-Image in HIV-Positive Women in Sub-Saharan Africa. HIV/AIDS—Res. Palliat. Care. 2018;10:133–144. doi: 10.2147/HIV.S167005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Desmond K., Milburn N., Richter L., Tomlinson M., Greco E., van Heerden A., van Rooyen H., Comulada W.S., Rotheram-Borus M.J. Alcohol Consumption among HIV-Positive Pregnant Women in KwaZulu-Natal, South Africa: Prevalence and Correlates. Drug Alcohol Depend. 2012;120:113–118. doi: 10.1016/j.drugalcdep.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dolan R., Maritz D., Wallis L., Parak M. Bilateral Lower Motor Neuron Facial Nerve Palsy Due to HIV Seroconversion. S. Afr. J. HIV Med. 2011;12:39–40. doi: 10.4102/sajhivmed.v12i1.212. [DOI] [Google Scholar]
- 74.Dreyer A.J., Nightingale S., Heaps-Woodruff J.M., Henry M., Gouse H., Paul R.H., Thomas K.G.F., Joska J.A. Rates of Cognitive Impairment in a South African Cohort of People with HIV: Variation by Definitional Criteria and Lack of Association with Neuroimaging Biomarkers. J. Neurovirol. 2021;27:579–594. doi: 10.1007/s13365-021-00993-x. [DOI] [PubMed] [Google Scholar]
- 75.Dudley M.T., Borkum M., Basera W., Wearne N., Heckmann J.M. Journal of the Neurological Sciences Peripheral Neuropathy in HIV Patients on Antiretroviral Therapy: Does It Impact Function ? J. Neurol. Sci. 2019;406:116451. doi: 10.1016/j.jns.2019.116451. [DOI] [PubMed] [Google Scholar]
- 76.Berner K., Strijdom H., Essop M., Webster I., Morris L., Louw Q. Fall History and Associated Factors among Adults Living with HIV-1 in the Cape Winelands, South Africa: An Exploratory Investigation. Open Forum Infect. Dis. 2019;6:ofz401. doi: 10.1093/ofid/ofz401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Edwards A., Siedner M.J., Nash S., Neuman M., Danaviah S., Smit T., Gareta D., Kowal P., Seeley J. HIV Serostatus, Inflammatory Biomarkers and the Frailty Phenotype among Older People in Rural KwaZulu-Natal, South Africa. Afr. J. AIDS Res. 2020;19:177–185. doi: 10.2989/16085906.2020.1790398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Freeman M., Nkomo N., Kafaar Z., Kelly K. Factors Associated with Prevalence of Mental Disorder in People Living with HIV/AIDS in South Africa. AIDS Care. 2007;19:1201–1209. doi: 10.1080/09540120701426482. [DOI] [PubMed] [Google Scholar]
- 79.Friend-du Preez N., Peltzer K. HIV Symptoms and Health-Related Quality of Life Prior to Initiation of HAART in a Sample of HIV-Positive South Africans. AIDS Behav. 2010;14:1437–1447. doi: 10.1007/s10461-009-9566-6. [DOI] [PubMed] [Google Scholar]
- 80.Ganasen K.A., Fincham D., Smit J., Seedat S., Stein D. Utility of the HIV Dementia Scale (HDS) in Identifying HIV Dementia in a South African Sample. J. Neurol. Sci. 2008;269:62–64. doi: 10.1016/j.jns.2007.12.027. [DOI] [PubMed] [Google Scholar]
- 81.Goodkin K., Hardy D.J., Singh D., Lopez E. Diagnostic Utility of the International HIV Dementia Scale for HIV-Associated Neurocognitive Impairment and Disorder in South Africa. J. Neuropsychiatry Clin. Neurosci. 2014;26:352–358. doi: 10.1176/appi.neuropsych.13080178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gouse H., Masson C., Henry M., Thomas K.G.F., Robbins R., Kew G., London L., Joska J.A., Marcotte T.D. The Impact of HIV-Associated Neurocognitive Impairment on Driving Performance in Commercial Truck Drivers. AIDS Behav. 2021;25:689–698. doi: 10.1007/s10461-020-03033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haas A.D., Kunzekwenyika C., Hossmann S., Manzero J., Van Dijk J., Manhibi R., Verhey R., Limacher A., Von Groote P.M., Manda E., et al. Original Research: Symptoms of Common Mental Disorders and Adherence to Antiretroviral Therapy among Adults Living with HIV in Rural Zimbabwe: A Cross-Sectional Study. BMJ Open. 2021;11:49824. doi: 10.1136/bmjopen-2021-049824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hakkers C.S., Beunders A.J.M., Ensing M.H.M., Barth R.E., Boelema S., Devillé W.L.J., Tempelman H.A., Coutinho R.A., Hoepelman A.I.M., Arends J.E., et al. The Montreal Cognitive Assessment–Basic (MoCA-B) Is Not a Reliable Screening Tool for Cognitive Decline in HIV Patients Receiving Combination Antiretroviral Therapy in Rural South Africa. Int. J. Infect. Dis. 2018;67:36–40. doi: 10.1016/j.ijid.2017.11.024. [DOI] [PubMed] [Google Scholar]
- 85.Hansrod F., Spies G., Seedat S. Type and Severity of Intimate Partner Violence and Its Relationship with PTSD in HIV-Infected Women. Psychol. Health Med. 2015;20:697. doi: 10.1080/13548506.2014.967702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hattingh Z., Le Roux M., Nel M., Walsh C. Assessment of the Physical Activity, Body Mass Index and Energy Intake of HIV-Uninfected and HIV-Infected Women in Mangaung, Free State Province. S. Afr. Fam. Pract. 2014;56:196–200. doi: 10.1080/20786204.2014.936663. [DOI] [Google Scholar]
- 87.Bhigjee A.I., Moodley A.A., Roos I., Wells C., Ramdial P., Esser M. The Neuromyelitis Optica Presentation and the Aquaporin-4 Antibody in HIV-Seropositive and Seronegative Patients in KwaZulu-Natal, South Africa. S. Afr. J. HIV Med. 2017;18:1–7. doi: 10.4102/sajhivmed.v18i1.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Heinze B.M., Vinck B.M., Hofmeyr L.M., Swanepoel D.W. Auris Nasus Larynx Vestibular Involvement in Adults with HIV/AIDS. Auris Nasus Larynx. 2014;41:160–168. doi: 10.1016/j.anl.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 89.Hitchcock S., Meyer H., Gwyther E. Neuropathic Pain in AIDS Patients Prior to Antiretroviral Therapy. S. Afr. Med. J. 2008;98:889–892. [PubMed] [Google Scholar]
- 90.Hoare J., Westgarth-taylor J., Fouche J.-P., Spottiswoode B., Paul R., Thomas K., Stein D., Joska J. A Diffusion Tensor Imaging and Neuropsychological Study of Prospective Memory Impairment in South African HIV Positive Individuals. Metab. Brain Dis. 2012;27:289–297. doi: 10.1007/s11011-013-9422-2. [DOI] [PubMed] [Google Scholar]
- 91.Huis in ‘t Veld D., Pengpid S., Colebunders R., Skaal L., Peltzer K. High-Risk Alcohol Use and Associated Socio-Demographic, Health and Psychosocial Factors in Patients with HIV Infection in Three Primary Health Care Clinics in South Africa. Int. J. STD AIDS. 2017;28:651–659. doi: 10.1177/0956462416660016. [DOI] [PubMed] [Google Scholar]
- 92.Joska J.A., Fincham D.S., Stein D.J., Paul R.H., Seedat S. Clinical Correlates of HIV-Associated Neurocognitive Disorders in South Africa. AIDS Behav. 2010;14:371–378. doi: 10.1007/s10461-009-9538-x. [DOI] [PubMed] [Google Scholar]
- 93.Joska J.A., Sa F., Westgarth-Taylor J., Hoare J., Thomas K.G.F., Ph D., Paul R., Ph D. Validity of the International HIV Dementia Scale in South Africa. AIDS Patient Care STDS. 2011;25:95–101. doi: 10.1089/apc.2010.0292. [DOI] [PubMed] [Google Scholar]
- 94.Joska J.A., Westgarth-Taylor J., Hoare J., Thomas K.G.F., Paul R., Myer L., Stein D.J. Neuropsychological Outcomes in Adults Commencing Highly Active Anti-Retroviral Treatment in South Africa: A Prospective Study. BMC Infect. Dis. 2012;12:39. doi: 10.1186/1471-2334-12-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Joska J.A., Witten J., Thomas K.G., Robertson C., Casson-Crook M., Roosa H., Creighton J., Lyons J., McArthur J., Sacktor N.C. A Comparison of Five Brief Screening Tools for HIV-Associated Neurocognitive Disorders in the USA and South Africa. AIDS Behav. 2016;20:1621–1631. doi: 10.1007/s10461-016-1316-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Joska J.A., Dreyer A.J., Nightingale S., Combrinck M.I., De Jager C.A. Prevalence of HIV-1 Infection in an Elderly Rural Population and Associations with Neurocognitive Impairment. AIDS. 2019;33:1765–1771. doi: 10.1097/QAD.0000000000002257. [DOI] [PubMed] [Google Scholar]
- 97.Joska J.A., Landon J.W., Paul R.H., Stein D.J., Flisher A.J. Characterization of HIV-Associated Neurocognitive Disorders Among Individuals Starting Antiretroviral Therapy in South Africa. AIDS Behav. 2011;15:1197–1203. doi: 10.1007/s10461-010-9744-6. [DOI] [PubMed] [Google Scholar]
- 98.Bongongo T., Tumbo J., Govender I. Depressive Features among Adult Patients Receiving Antiretroviral Therapy for HIV in Rustenburg District, SA. S. Afr. J. Psychiatry. 2013;19:31. doi: 10.4102/sajpsychiatry.v19i2.418. [DOI] [Google Scholar]
- 99.Kader R., Govender R., Seedat S., Koch J.R., Parry C. Understanding the Impact of Hazardous and Harmful Use of Alcohol and/or Other Drugs on ARV Adherence and Disease Progression. PLoS ONE. 2015;10:e0125088. doi: 10.1371/journal.pone.0125088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kagee A., Martin L. Symptoms of Depression and Anxiety among a Sample of South African Patients Living with HIV. AIDS Care. 2010;22:159–165. doi: 10.1080/09540120903111445. [DOI] [PubMed] [Google Scholar]
- 101.Kagee A. Psychological Distress among Persons Living with HIV, Hypertension, and Diabetes. AIDS Care. 2010;22:1517–1521. doi: 10.1080/09540121.2010.484458. [DOI] [PubMed] [Google Scholar]
- 102.Kaswa R., De Villiers M. Prevalence of Substance Use amongst People Living with Human Immunodeficiency Virus Who Attend Primary Healthcare Services in Mthatha, South Africa. S. Afr. Fam. Pract. 2020;62:a5042. doi: 10.4102/safp.v62i1.5042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kekwaletse C.T., Morojele N.K. Alcohol Use, Antiretroviral Therapy Adherence, and Preferences Regarding an Alcohol-Focused Adherence Intervention in Patients with Human Immunodeficiency Virus. Patient Prefer. Adherence. 2014;8:401–413. doi: 10.2147/PPA.S55547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Khoza-shangase K. Vestibular Function in a Group of Adults with HIV/AIDS on HAART. Afr. J. Infect. Dis. 2017;12:7–14. doi: 10.21010/ajid.v12i1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Khoza-Shangase K. An Analyisis of Auditory Manifestations in a Group of Adults with AIDS Prior to Antiretroviral Therapy. Afr. J. Infect. Dis. 2011;5:11–22. [PMC free article] [PubMed] [Google Scholar]
- 106.Khoza-Shangase K., Jade Van Rie K. Pathological Vestibular Symptoms Presenting in a Group of Adults with HIV/AIDS in Johannesburg, South Africa. S. Afr. J. Infect. Dis. 2017;32:43–53. doi: 10.1080/23120053.2016.1216816. [DOI] [Google Scholar]
- 107.Kietrys D., Myezwa H., Galantino M.L., Parrott J.S., Davis T., Levin T., O’Brien K., Hanass-Hancock J. Functional Limitations and Disability in Persons Living with HIV in South Africa and United States: Similarities and Differences. J. Int. Assoc. Provid. AIDS Care. 2019;18:232595821985055. doi: 10.1177/2325958219850558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kitshoff C., Campbell L., Naidoo S. The Association between Depression and Adherence to Antiretroviral Therapy in HIV-Positive Patients, KwaZulu-Natal, South Africa. S. Afr. Fam. Pract. 2012;54:145–150. doi: 10.1080/20786204.2012.10874194. [DOI] [Google Scholar]
- 109.Breuer E., Stoloff K., Myer L., Seedat S., Stein D.J., Joska J. Reliability of the Lay Adherence Counsellor Administered Substance Abuse and Mental Illness Symptoms Screener (SAMISS) and the International HIV Dementia Scale (IHDS) in a Primary Care HIV Clinic in Cape Town, South Africa. AIDS Behav. 2012;16:1464–1471. doi: 10.1007/s10461-011-0067-z. [DOI] [PubMed] [Google Scholar]
- 110.Mahomed W., Audiology M.A., Heinze B., Vinck B., Stoltz A. Faculty of Humanities Audiovestibular Profile of HIV Positive Adults. upSpace; Ottawa, ON, Canada: 2018. p. 1300. [Google Scholar]
- 111.Martin L., Fincham D., Kagee A. Screening for HIV-Related PTSD: Sensitivity and Specificity of the 17-Item Posttraumatic Stress Diagnostic Scale (PDS) in Identifying HIV-Related PTSD among a South African Sample. Afr. J. Psychiatry. 2009;12:270–274. doi: 10.4314/ajpsy.v12i4.49041. [DOI] [PubMed] [Google Scholar]
- 112.Masenyetse L.J., Manda S.O., Mwambi H.G. An Assessment of Adverse Drug Reactions among HIV Positive Patients Receiving Antiretroviral Treatment in South Africa. AIDS Res. Ther. 2015;12:6. doi: 10.1186/s12981-015-0044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mashinya F., Alberts M., Van Geertruyden J., Colebunders R. Tobacco Use among ARV Treated HIV Infected Rural South Africans: Prevalence and Its Determinants. Afr. J. Phys. Health Educ. Recreat. Danc. 2015;21:768–776. [Google Scholar]
- 114.Mathebula S.D., Makunyane P.S. Loss of Amplitude of Accommodation in Pre-Presbyopic HIV and AIDS Patients under Treatment with Antiretrovirals. Afr. Vis. Eye Health. 2017;76:1–6. doi: 10.4102/aveh.v76i1.411. [DOI] [Google Scholar]
- 115.Meel B.L. HIV/AIDS, Psychiatric Disorder and Sexual Assault in Transkei: A Case Report. Med. Sci. Law. 2006;46:181–183. doi: 10.1258/rsmmsl.46.2.181. [DOI] [PubMed] [Google Scholar]
- 116.Menezes C.N., Maskew M., Sanne I., Crowther N.J., Raal F.J. A Longitudinal Study of Stavudine-Associated Toxicities in a Large Cohort of South African HIV Infected Subjects. BMC Infect. Dis. 2011;11:244. doi: 10.1186/1471-2334-11-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Millar A., Joubert K., Naude A. Prevalence of Hearing Loss and Tinnitus in a Group of Adults with Human Immunodeficiency Virus. S. Afr. J. Commun. Disord. 2020;67:1–7. doi: 10.4102/sajcd.v67i1.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Millar A., Joubert K., Naude A. Prevalence of Peripheral Vestibular Impairment in Adults with Human Immunodeficiency Virus. J. Audiol. Otol. 2021;25:36–42. doi: 10.7874/jao.2020.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mogambery J.C., Dawood H., Wilson D., Moodley A. HIV-Associated Neurocognitive Disorder in a KwaZulu-Natal HIV Clinic: A Prospective Study. S. Afr. J. HIV Med. 2017;18:1–5. doi: 10.4102/sajhivmed.v18i1.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Breuer E., Stoloff K., Myer L., Seedat S., Stein D.J., Joska J.A. The Validity of the Substance Abuse and Mental Illness Symptom Screener (SAMISS) in People Living with HIV/AIDS in Primary HIV Care in Cape Town, South Africa. AIDS Behav. 2014;18:1133–1141. doi: 10.1007/s10461-014-0698-y. [DOI] [PubMed] [Google Scholar]
- 121.Mokhele I., Nattey C., Jinga N., Mongwenyana C., Fox M.P., Onoya D. Prevalence and Predictors of Postpartum Depression by HIV Status and Timing of HIV Diagnosis in Gauteng, South Africa. PLoS ONE. 2019;14:e0214849. doi: 10.1371/journal.pone.0214849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Moodley K., Bill P.L.A., Bhigjee A.I., Patel V.B. A Comparative Study of Motor Neuron Disease in HIV-Infected and HIV- Uninfected Patients. J. Neurol. Sci. 2019;397:96–102. doi: 10.1016/j.jns.2018.12.030. [DOI] [PubMed] [Google Scholar]
- 123.Morojele N.K., Nkosi S., Kekwaletswe C.T., Shuper P.A., Manda S.O., Myers B., Parry C.D. Utility of Brief Versions of the Alcohol Use Disorders Identification Test (AUDIT) to Identify Excessive Drinking Among Patients in HIV Care in South Africa. J. Stud. Alcohol Drugs. 2017;78:88–96. doi: 10.15288/jsad.2017.78.88. [DOI] [PubMed] [Google Scholar]
- 124.Morris T., Naidoo P., Cloete K.J., Harvey J., Seedat S. No Association Between Cumulative Traumatic Experiences and Sex in Risk for Posttraumatic Stress Disorder Among Human Immunodeficiency Virus–Positive Adults. J. Nerv. Ment. Dis. 2013;201:504–509. doi: 10.1097/NMD.0b013e31829482d7. [DOI] [PubMed] [Google Scholar]
- 125.Mphahlele N.R., Mitchell D., Kamerman P.R. Pain in Ambulatory HIV-Positive South Africans. Eur. J. Pain. 2012;16:447–458. doi: 10.1002/j.1532-2149.2011.00031.x. [DOI] [PubMed] [Google Scholar]
- 126.Mupawose A., Broom Y. Assessing Cognitive-Linguistic Abilities in South African Adults Living with HIV: The Cognitive Linguistic Quick Test. Afr. J. AIDS Res. 2010;9:147–152. doi: 10.2989/16085906.2010.517481. [DOI] [PubMed] [Google Scholar]
- 127.Myer L., Smit J., Le Roux L., Parker S., Stein D.J., Seedat S. Common Mental Disorders among HIV-Infected Individuals in South Africa: Prevalence, Predictors, and Validation of Brief Psychiatric Rating Scales. AIDS Patient Care STDS. 2008;22:147–158. doi: 10.1089/apc.2007.0102. [DOI] [PubMed] [Google Scholar]
- 128.Myezwa H., Stewart A., Musenge E., Nesara P. Assessment of HIV-Positive in-Patients Using the International Classification of Functioning, Disability and Health (ICF) at Chris Hani Baragwanath Hospital, Johannesburg. Afr. J. AIDS Res. 2009;8:93–105. doi: 10.2989/AJAR.2009.8.1.10.723. [DOI] [PubMed] [Google Scholar]
- 129.Naidoo P., Premdutt R. Do Challenges Still Exist amongst HIV/AIDS Patients in Managing Their Condition? A Cross-Sectional Study of 297 Participants in the Ethekwini Metro of Kwazulu-Natal, South Africa. Afr. J. AIDS Res. 2019;18:198–204. doi: 10.2989/16085906.2019.1648305. [DOI] [PubMed] [Google Scholar]
- 130.Narasimooloo C., Naidoo S.S., Gaede B.M. Adequacy of Pain Management in HIV-Positive Patients. S. Afr. Fam. Pract. 2014;53:71–76. doi: 10.1080/20786204.2011.10874063. [DOI] [Google Scholar]
- 131.Brittain K., Mellins C.A., Phillips T., Zerbe A., Abrams E.J., Myer L., Remien R.H. Social Support, Stigma and Antenatal Depression Among HIV-Infected Pregnant Women in South Africa. AIDS Behav. 2017;21:274–282. doi: 10.1007/s10461-016-1389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Narsi K., Tomita A., Ramlall S. Neuropsychological Functioning and Cognitive Reserve in Newly HIV Diagnosed Antiretroviralnaïve South African Adults from Peri-Urban and Informal Settlements. PLoS ONE. 2021;16:e0260260. doi: 10.1371/journal.pone.0260260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Nel A., Kagee A. The Relationship between Depression, Anxiety and Medication Adherence among Patients Receiving Antiretroviral Treatment in South Africa. AIDS Care. 2013;25:948–955. doi: 10.1080/09540121.2012.748867. [DOI] [PubMed] [Google Scholar]
- 134.Nöthling J., Martin C.L., Laughton B., Cotton M.F., Seedat S. Maternal Post-Traumatic Stress Disorder, Depression and Alcohol Dependence and Child Behaviour Outcomes in Mother–Child Dyads Infected with HIV: A Longitudinal Study. BMJ Open. 2013;3:e003638. doi: 10.1136/bmjopen-2013-003638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Olley B.O. Psychological Distress in the First Year after Diagnosis of HIV Infection among Women in South Africa. Afr. J. AIDS Res. 2006;5:207–215. doi: 10.2989/16085900609490381. [DOI] [PubMed] [Google Scholar]
- 136.Olley B.O., Seedat S., Stein D.J. Persistence of Psychiatric Disorders in a Cohort of HIV/AIDS Patients in South Africa: A 6-Month Follow-up Study. J. Psychosom. Res. 2006;61:479–484. doi: 10.1016/j.jpsychores.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 137.Pappin M., Wouters E., Booysen F.L.R. Anxiety and Depression amongst Patients Enrolled in a Public Sector Antiretroviral Treatment Programme in South Africa: A Cross-Sectional Study. BMC Public Health. 2012;12:244. doi: 10.1186/1471-2458-12-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Parker R., Jelsma J., Stein D.J. Pain in AmaXhosa Women Living With HIV/AIDS: Translation and Validation of the Brief Pain Inventory e Xhosa. J. Pain Symptom Manag. 2016;51:126–132.e2. doi: 10.1016/j.jpainsymman.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 139.Parker R., Jelsma J., Stein D.J. Pain in AmaXhosa Women Living with HIV/AIDS: A Cross-Sectional Study of Ambulant Outpatients. BMC Women’s Health. 2017;17:31. doi: 10.1186/s12905-017-0388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Pathai S., Lawn S.D., Weiss H.A., Cook C., Sa F., Bekker L., Gilbert C.E. Increased Ocular Lens Density in HIV-Infected Individuals With Low Nadir CD4 Counts in South Africa: Evidence of Accelerated Aging. JAIDS J. Acquir. Immune Defic. Syndr. 2013;63:307–314. doi: 10.1097/QAI.0b013e31828ad759. [DOI] [PubMed] [Google Scholar]
- 141.Pathai S., Lawn S.D., Weiss H.A., Cook C., Bekker L., Gilbert C.E. Retinal Nerve Fibre Layer Thickness and Contrast Sensitivity in HIV-Infected Individuals in South Africa: A Case-Control Study. PLoS ONE. 2013;8:e73694. doi: 10.1371/journal.pone.0073694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Cassimjee N., Motswai P.K. Neuropsychological Profiles of Adults and Older Adults with HIV. S. Afr. J. Psychol. 2017;47:35–45. doi: 10.1177/0081246316646296. [DOI] [Google Scholar]
- 143.Pathai S., Gilbert C., Weiss H.A., Cook C., Wood R., Bekker L., Lawn S.D. Frailty in HIV-Infected Adults in South Africa. JAIDS J. Acquir. Immune Defic. Syndr. 2013;62:43–51. doi: 10.1097/QAI.0b013e318273b631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Peltzer K., Szrek H., Ramlagan S., Leite R., Chao L.-W. Depression and Social Functioning among HIV-Infected and Uninfected Persons in South Africa. AIDS Care. 2015;27:41–46. doi: 10.1080/09540121.2014.946383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Peltzer K., Rodriguez V.J., Jones D. Prevalence of Prenatal Depression and Associated Factors among HIV-Positive Women in Primary Care in Mpumalanga Province, South Africa. SAHARA-J J. Soc. Asp. HIV/AIDS. 2016;13:60–67. doi: 10.1080/17290376.2016.1189847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Peltzer K. HIV-Related Symptoms and Management in HIV and Antiretroviral Therapy Patients in KwaZulu-Natal, South Africa: A Longitudinal Study. J. Soc. Asp. HIV/AIDS. 2013;10:96–104. doi: 10.1080/17290376.2013.870119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Peltzer K., Phaswana-Mafuya N., Petros G. Hazardous Alcohol Use among Persons Living with Human Immunodeficiency Virus Infection in the Eastern Cape, South Africa. J. Psychol. Afr. 2009;19:247–251. doi: 10.1080/14330237.2009.10820287. [DOI] [Google Scholar]
- 148.Pengpid S., Peltzer K. Mental Morbidity and Its Associations with Socio-Behavioural Factors and Chronic Conditions in Rural Middle- and Older-Aged Adults in South Africa. J. Psychol. Afr. 2020;30:257–263. doi: 10.1080/14330237.2020.1767956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pienaar M., Van Rooyen F.C., Walsh C.M. Reported Health, Lifestyle and Clinical Manifestations Associated with HIV Status in People from Rural and Urban Communities in the Free State Province, South Africa. S. Afr. J. HIV Med. 2017;18:a465. doi: 10.4102/sajhivmed.v18i1.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Pillay P., Wadley A.L., Cherry C.L., Karstaedt A.S., Kamerman P.R., Cherry C.L. Psychological Factors Associated With Painful Versus Non-Painful HIV-Associated Sensory Neuropathy. AIDS Behav. 2018;22:1584–1595. doi: 10.1007/s10461-017-1856-9. [DOI] [PubMed] [Google Scholar]
- 151.Pinillos F., Dandara C., Swart M., Strehlau R., Kuhn L., Patel F., Coovadia A., Abrams E. Case Report: Severe Central Nervous System Manifestations Associated with Aberrant Efavirenz Metabolism in Children: The Role of CYP2B6 Genetic Variation. BMC Infect. Dis. 2016;16:56. doi: 10.1186/s12879-016-1381-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ramirez-Avila L., Regan S., Giddy J., Chetty S., Ross D., Katz J.N., Freedberg K.A., Walensky R.P., Losina E., Bassett I.V. Depressive Symptoms and Their Impact on Health-Seeking Behaviors in Newly-Diagnosed HIV-Infected Patients in Durban, South Africa. AIDS Behav. 2012;16:2226–2235. doi: 10.1007/s10461-012-0160-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Chetty S., Naidu K. Clinical Presentation of HIV-Infected Patients in a Psychiatric Hospital in South Africa. Afr. J. Infect. Dis. 2018;12:29–36. doi: 10.21010/ajid.v12i2.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Rane M.S., Hong T., Govere S., Thulare H., Moosa M., Celum C., Drain P.K. Depression and Anxiety as Risk Factors for Delayed Care-Seeking Behavior in Human Immunodeficiency Virus–Infected Individuals in South Africa. Clin. Infect. Dis. 2018;67:1411–1418. doi: 10.1093/cid/ciy309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Robbins R.N., Remien R.H., Mellins C.A., Joska J.A., Stein D.J. Screening for HIV-Associated Dementia in South Africa: Potentials and Pitfalls of Task-Shifting. AIDS Patient Care STDS. 2011;25:587–593. doi: 10.1089/apc.2011.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Robbins R.N., Joska J.A., Thomas K.G.F., Stein D.J., Linda T., Mellins C.A., Remien R.H. Exploring the Utility of the Montreal Cognitive Assessment to Detect HIV-Associated Neurocognitive Disorder: The Challenge and Need for Culturally Valid Screening Tests in South Africa. Clin. Neuropsychol. 2013;27:437–454. doi: 10.1080/13854046.2012.759627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Robbins R.N., Gouse H., Brown H.G., Ehlers A., Leu C., Remien R.H., Mellins C.A., Joska J.A. A Mobile App to Screen for Neurocognitive Impairment: Preliminary Validation of NeuroScreen Among HIV-Infected South African Adults. JMIR Mhealth Uhealth. 2018;6:e5. doi: 10.2196/mhealth.9148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Roos R., Myezwa H., Van Aswegen H., Musenge E. Effects of an Education and Home-Based Pedometer Walking Program on Ischemic Heart Disease Risk Factors in People Infected with HIV: A Randomized Trial. J. Acquir. Immune Defic. Syndr. 2014;67:268–276. doi: 10.1097/QAI.0000000000000299. [DOI] [PubMed] [Google Scholar]
- 159.Roos R., Myezwa H., Van Aswegen H. Factors Associated with Physical Function Capacity in an Urban Cohort of People Living with the Human Immunodeficiency Virus in South Africa. S. Afr. J. Physiother. 2019;75:1–7. doi: 10.4102/sajp.v75i1.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Schlebusch L., Vawda N. HIV-Infection as a Self-Reported Risk Factor for Attempted Suicide in South Africa. Afr. J. Psychiatry. 2010;13:280–283. doi: 10.4314/ajpsy.v13i4.61877. [DOI] [PubMed] [Google Scholar]
- 161.Schutte C., Ranchhod N., Kakaza M., Pillay M. AIDS-Related Progressive Multifocal Leukoencephalopathy (PML): A Retrospective Study from Pretoria, South Africa. S. Afr. Med. J. 2013;103:399. doi: 10.7196/SAMJ.6386. [DOI] [PubMed] [Google Scholar]
- 162.Sebothoma B., Khoza-Shangase K. Investigation of the Interaction between Hearing Function and Comorbidities in Adults Living with Human Immunodeficiency Virus. Int. J. Environ. Res. Public Health. 2021;18:12177. doi: 10.3390/ijerph182212177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Shearer K., Evans D., Xhosa B., Hirasen K., Bracken C., Mahomed K., Long L., Fox M.P. Low Prevalence of Depressive Symptoms among Stable Patients on Antiretroviral Therapy in Johannesburg, South Africa. PLoS ONE. 2018;13:e0203797. doi: 10.1371/journal.pone.0203797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Auld S.C., Kornfeld H., Maenetje P., Mlotshwa M., Chase W., Vangu T., Torigian D.A., Wallis R.S., Churchyard G., Bisson G.P. Pulmonary Restriction Predicts Long— Term Pulmonary Impairment in People with HIV and Tuberculosis. BMC Pulm. Med. 2021;21:19. doi: 10.1186/s12890-020-01368-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Candy S., Chang G., Andronikou S. Acute Myelopathy or Cauda Equina Syndrome in HIV-Positive Adults in a Tuberculosis Endemic Setting: MRI, Clinical, and Pathologic Findings. Am. J. Neuroradiol. 2014;35:1634–1641. doi: 10.3174/ajnr.A3958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gounden S., Perumal R., Magula N. Extrapulmonary Tuberculosis in the Setting of HIV Hyperendemicity at a Tertiary Hospital in Durban, South Africa. South. Afr. J. Infect. Dis. 2018;33:57–64. doi: 10.1080/23120053.2017.1403207. [DOI] [Google Scholar]
- 167.Khan M., Pillay T., Moodley J., Ramjee A., Padayatchi N. Pregnancies Complicated by Multidrug-Resistant Tuberculosis and HIV Co-Infection in Durban, South Africa. Int. J. Tuberc. Lung Dis. 2007;11:706–708. [PubMed] [Google Scholar]
- 168.Marais S., Roos I., Mitha A., Patel V., Bhigjee A.I. Posttubercular Syringomyelia in HIV-Infected Patients: A Report of 10 Cases and Literature Review. J. Neurol. Sci. 2018;395:54–61. doi: 10.1016/j.jns.2018.09.034. [DOI] [PubMed] [Google Scholar]
- 169.Mntonintshi M., O’Mahony D., Mabunda S., Namugenyi K.A.F. Undiagnosed Tuberculosis in Patients with HIV Infection Who Present with Severe Anaemia at a District Hospital. Afr. J. Prim. Health Care Fam. Med. 2017;9:1–6. doi: 10.4102/phcfm.v9i1.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Makapi N., Morare T., Rose D.M., Appels O. Oesophageal Tuberculosis with Concomitant Candidiasis: A Rare Cause of Dysphagia. BMJ Case Rep. 2019;12:e231435. doi: 10.1136/bcr-2019-231435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ramlall S., Lessells R.J., Naidu T., Sandra Mthembu S., Padayatchi N., Burns J.K., Tomita A. Neurocognitive Functioning in MDR-TB Patients with and without HIV in KwaZulu-Natal, South Africa. Trop. Med. Int. Health. 2020;25:919–927. doi: 10.1111/tmi.13444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Stek C., Allwood B., Du Bruyn E., Buyze J., Schutz C., Thienemann F., Lombard A., Wilkinson R.J., Meintjes G., Lynen L. The Effect of HIV-Associated Tuberculosis, Tuberculosis-IRIS and Prednisone on Lung Function. Eur. Respir. J. 2020;55:1901692. doi: 10.1183/13993003.01692-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wilson D., Ch B., Hurtado R.M., Digumarthy S. Case 18-2009: A 24-Year-Old Woman with AIDS and Tuberculosis with Progressive Cough, Dyspnea, and Wasting. N. Engl. J. Med. 2009;360:2456–2464. doi: 10.1056/NEJMcpc0902226. [DOI] [PubMed] [Google Scholar]
- 174.Patel N., Naidoo P., Mosiane P., Jann-Kruger C. HIV/AIDS-Associated Kaposi’s Sarcoma of the Gastrointestinal Tract: A Pictorial Spectrum. S. Afr. Med. J. 2016;106:986. doi: 10.7196/SAMJ.2016.v106i10.11277. [DOI] [PubMed] [Google Scholar]
- 175.Sebitloane H., Moodley J. Disseminated AIDS-Associated Kaposi’s Sarcoma in Pregnancy. SAMJ. 2006;96:602–603. [PubMed] [Google Scholar]
- 176.Loyse A., Moodley A., Rich P., Molloy S.F., Bicanic T., Bishop L., Rae W.I.D., Bhigjee A.I., Loubser N.D., Michowicz A.J., et al. Neurological, Visual, and MRI Brain Scan Findings in 87 South African Patients with HIV-Associated Cryptococcal. J. Infect. 2015;70:668–675. doi: 10.1016/j.jinf.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 177.Allwood B.W., Stolbrink M., Baines N., Louw E., Wademan D.T., Lupton-Smith A., Nel S., Maree D., Mpagama S., Osman M., et al. Persistent Chronic Respiratory Symptoms despite TB Cure Is Poorly Correlated with Lung Function. Int. J. Tuberc. Lung Dis. 2021;25:262. doi: 10.5588/ijtld.20.0906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Peltzer K., Louw J. Prevalence of Suicidal Behaviour & Associated Factors among Tuberculosis Patients in Public Primary Care in South Africa. Indian J. Med. Res. 2013;138:194–200. [PMC free article] [PubMed] [Google Scholar]
- 179.Peltzer K., Naidoo P., Matseke G., Louw J., Mchunu G., Tutshana B. Prevalence of Post-Traumatic Stress Symptoms and Associated Factors in Tuberculosis (TB), TB Retreatment and/or TB–HIV Co-Infected Primary Public Health-Care Patients in Three Districts in South Africa. Psychol. Health Med. 2013;18:387–397. doi: 10.1080/13548506.2012.726364. [DOI] [PubMed] [Google Scholar]
- 180.Wessels J., Walsh C.M., Nel M. Smoking Habits and Alcohol Use of Patients with Tuberculosis at Standerton Tuberculosis Specialised Hospital, Mpumalanga, South Africa. Health SA Gesondheid. 2019;24:a1146. doi: 10.4102/hsag.v24i0.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Zarrabi A.D., Heyns C.F. Clinical Features of Confirmed Versus Suspected Urogenital Tuberculosis in Region With Extremely High Prevalence of Pulmonary Tuberculosis. Urology. 2009;74:41–45. doi: 10.1016/j.urology.2008.12.083. [DOI] [PubMed] [Google Scholar]
- 182.Van Aswegen H., Roos R., McCree M., Quinn S., Mer M. Investigation of Physical and Functional Impairments Experienced by People with Active Tuberculosis Infection: A Feasibility Pilot Study. Afr. J. Disabil. 2019;8:a515. doi: 10.4102/ajod.v8i0.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Balkema C.A., Irusen E.M., Taljaard J.J., Koegelenberg C.F.N. Tuberculosis in the Intensive Care Unit: A Prospective Observational Study. Int. J. Tuberc. Lung Dis. 2014;18:824–830. doi: 10.5588/ijtld.13.0044. [DOI] [PubMed] [Google Scholar]
- 184.Khoza-shangase K. Hearing Function of Gold Miners with and without a History of Tuberculosis Treatment: A Retrospective Data Review. Braz. J. Otorhinolaryngol. 2020;86:294–299. doi: 10.1016/j.bjorl.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Louwagie G., Kanaan M., Morojele N.K., Van Zyl A., Moriarty A.S., Li J., Siddiqi K., Turner A., Mdege N.D., Omole O.B., et al. Effect of a Brief Motivational Interview and Text Message Intervention Targeting Tobacco Smoking, Alcohol Use and Medication Adherence to Improve Tuberculosis Treatment Outcomes in Adult Patients with Tuberculosis: A Multicentre, Randomised Controlled Tri. BMJ Open. 2022;12:e056496. doi: 10.1136/bmjopen-2021-056496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Myers B., Carney T., Rooney J., Malatesta S., White L.F., Parry C.D.H., Bouton T.C., Ragan E.J., Horsburgh C.R., Warren R.M., et al. Alcohol and Tobacco Use in a Tuberculosis Treatment Cohort during South Africa’s COVID-19 Sales Bans: A Case Series. Int. J. Environ. Res. Public Health. 2021;18:5449. doi: 10.3390/ijerph18105449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Peltzer K., Naidoo P., Matseke G., Louw J., Mchunu G., Tutshana B. Prevalence of Psychological Distress and Associated Factors in Tuberculosis Patients in Public Primary Care Clinics in South Africa. BMC Psychiatry. 2012;12:89. doi: 10.1186/1471-244X-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Peltzer K. Longitudinal Analysis of HIV Risk Behaviour Patterns and Their Predictors among Public Primary Care Patients with Tuberculosis in South Africa. SAHARA-J J. Soc. Asp. HIV/AIDS. 2018;15:1–6. doi: 10.1080/17290376.2018.1433057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Peltzer K., Louw J., Mchunu G., Naidoo P., Matseke G., Tutshana B. Hazardous and Harmful Alcohol Use and Associated Factors in Tuberculosis Public Primary Care Patients in South Africa. Int. J. Environ. Res. Public Health. 2012;9:3245–3257. doi: 10.3390/ijerph9093245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Peltzer K., Naidoo P., Louw J., Matseke G., Zuma K., Mchunu G., Tutshana B., Mabaso M. Screening and Brief Interventions for Hazardous and Harmful Alcohol Use among Patients with Active Tuberculosis Attending Primary Public Care Clinics in South Africa: Results from a Cluster Randomized Controlled Trial. BMC Public Health. 2013;13:1. doi: 10.1186/1471-2458-13-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Appana D., Joseph L., Paken J. An Audiological Profile of Patients Infected with Multi-Drug Resistant Tuberculosis at a District Hospital in KwaZulu-Natal. S. Afr. J. Commun. Disord. 2016;63:1–12. doi: 10.4102/sajcd.v63i1.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Conradie F., Mabiletsa T., Sefoka M., Mabaso S., Louw R., Evans D., Van Rie A. Prevalence and Incidence of Symmetrical Symptomatic Peripheral Neuropathy in Patients with Multidrug-Resistant TB. S. Afr. Med. J. 2013;104:24. doi: 10.7196/samj.6455. [DOI] [PubMed] [Google Scholar]
- 193.Harris T., Bardien S., Schaaf H.S., Petersen L., De Jong G., Fagan J.J. Aminoglycoside-Induced Hearing Loss in HIV-Positive and HIV-Negative Multidrug-Resistant Tuberculosis Patients. S. Afr. Med. J. 2012;102:363. doi: 10.7196/SAMJ.4964. [DOI] [PubMed] [Google Scholar]
- 194.Hong H., Dowdy D.W., Dooley K.E., Francis H.W., Budhathoki C., Han H., Farley J.E. Aminoglycoside-Induced Hearing Loss Among Patients Being Treated for Drug-Resistant Tuberculosis in South Africa: A Prediction Model. Clin. Infect. Dis. 2020;70:917–924. doi: 10.1093/cid/ciz289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Hong H., Dowdy D.W., Dooley K.E., Francis H.W., Budhathoki C., Han H.-R., Farley J.E. Prevalence of Pre-Existing Hearing Loss Among Patients With Drug-Resistant Tuberculosis in South Africa. Am. J. Audiol. 2020;29:199–205. doi: 10.1044/2020_AJA-19-00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Jacobs T.Q., Lecturer A.R. Adverse Effects Profile of Multidrug-Resistant Tuberculosis Treatment in a South African Outpatient Clinic Adverse Effects Profile of Multidrug-Resistant Tuberculosis Treatment in a South African Outpatient Clinic. S. Afr. Fam. Pract. 2012;54:531–539. doi: 10.1080/20786204.2012.10874288. [DOI] [Google Scholar]
- 197.Khoza-shangase K., Prodromos M. Impact of Drug-Resistant Tuberculosis Treatment on Hearing Function in South African Adults: Bedaquiline versus Kanamycin. Afr. J. Commun. Disord. 2021;68:a784. doi: 10.4102/sajcd.v68i1.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Padayatchi N., Daftary A., Moodley T., Madansein R., Ramjee A. Case Series of the Long-Term Psychosocial Impact of Drug- Resistant Tuberculosis in HIV-Negative Medical Doctors. Int. J. Tuberc. Lung Dis. 2010;14:960–966. [PubMed] [Google Scholar]
- 199.Ramma L., Ibekwe T.S. Cochleo-Vestibular Clinical Findings among Drug Resistant Tuberculosis Patients on Therapy-a Pilot Study. Int. Arch. Med. 2012;5:3. doi: 10.1186/1755-7682-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Tomita A., Ramlall S., Naidu T., Mthembu S.S., Padayatchi N., Burns J.K. Neurocognitive Impairment Risk Among Individuals With Multiple Drug–Resistant Tuberculosis and Human Immunodeficiency Virus Coinfection. J. Nerv. Ment. Dis. 2019;207:307–310. doi: 10.1097/NMD.0000000000000962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Daniels K.J., Irusen E., Pharoah H., Hanekom S. Post-Tuberculosis Health-Related Quality of Life, Lung Function and Exercise Capacity in a Cured Pulmonary Tuberculosis Population in the Breede Valley District, South Africa. S. Afr. J. Physiother. 2019;75:a1319. doi: 10.4102/sajp.v75i1.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Ehrlich R.I., Adams S., Baatjies R., Jeebhay M.F. Chronic Airfl Ow Obstruction and Respiratory Symptoms Following Tuberculosis: A Review of South African Studies. Int. J. Tuberc. Lung Dis. 2011;15:886–891. doi: 10.5588/ijtld.10.0526. [DOI] [PubMed] [Google Scholar]
- 203.Louw J.S., Mabaso M., Peltzer K. Change in Health-Related Quality of Life among Pulmonary Tuberculosis Patients at Primary Health Care Settings in South Africa: A Prospective Cohort Study. PLoS ONE. 2016;11:e0151892. doi: 10.1371/journal.pone.0151892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Dunn R., Zondagh I., Candy S. Spinal Tuberculosis. Magnetic Resonance Imaging and Neurological Impairment. Spine. 2011;36:469–473. doi: 10.1097/BRS.0b013e3181d265c0. [DOI] [PubMed] [Google Scholar]
- 205.Dunn R., Van Der Horst A., Lippross S. Tuberculosis of the Spine—Prospective Neurological and Patient Reported Outcome Study. Clin. Neurol. Neurosurg. 2015;133:96–101. doi: 10.1016/j.clineuro.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 206.Marais S., Roos I., Mitha A., Mabusha S.J., Patel V., Bhigjee A.I. Spinal Tuberculosis: Clinicoradiological Findings in 274 Patients. Clin. Infect. Dis. 2018;67:89–98. doi: 10.1093/cid/ciy020. [DOI] [PubMed] [Google Scholar]
- 207.Marais S., Roos I., Mitha A., Patel V., Kalincik T., Bhigjee A.I. Presentation and Outcome of Patients with Intracranial Tuberculoma in a High HIV Prevalence Setting. Int. J. Tuberc. Lung Dis. 2020;24:224–232. doi: 10.5588/ijtld.19.0386. [DOI] [PubMed] [Google Scholar]
- 208.Wait J.W., Schoeman J.F. Behaviour Profiles After Tuberculous Meningitis. J. Trop. Pediatr. 2010;56:166–171. doi: 10.1093/tropej/fmp080. [DOI] [PubMed] [Google Scholar]
- 209.Arowoiya A.I., Elloker T., Karachi F., Mlenzana N., Jacobs-Nzuzi Khuabi L.-A., Rhoda A. Using the World Health Organization’s Disability Assessment Schedule (2) to Assess Disability in Community-Dwelling Stroke Patients. S. Afr. J. Physiother. 2017;73:1–7. doi: 10.4102/sajp.v73i1.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Knox M., Stewart A., Richards C.L. Six Hours of Task-Oriented Training Optimizes Walking Competency Post Stroke: A Randomized Controlled Trial in the Public Health-Care System of South Africa. Clin. Rehabil. 2018;32:1057–1068. doi: 10.1177/0269215518763969. [DOI] [PubMed] [Google Scholar]
- 211.Mamabolo V., Mudzi W., Stewart A., Olorunju S., Singh A. A Study to Determine Post Discharge Functional Improvements in Patients with Stroke. S. Afr. J. Occup. Ther. 2009;39:15–18. [Google Scholar]
- 212.Ntsiea M.V., Van Aswegen H., Lord S., Olorunju S.S. The Effect of a Workplace Intervention Programme on Return to Work after Stroke: A Randomised Controlled Trial. Clin. Rehabil. 2015;29:663–673. doi: 10.1177/0269215514554241. [DOI] [PubMed] [Google Scholar]
- 213.Ostrofsky C., Seedat J. The South African Dysphagia Screening Tool (SADS): A Screening Tool for a Developing Context. S. Afr. J. Commun. Disord. 2016;63:1–9. doi: 10.4102/sajcd.v63i1.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Penn C., Barber N., Fridjhon P. Early Recovery Profiles of Language and Executive Functions after Left Hemisphere Stroke in Bilingualism. Aphasiology. 2016;31:741–764. doi: 10.1080/02687038.2016.1258538. [DOI] [Google Scholar]
- 215.Puckree T., Naidoo P. Balance and Stability—Focused Exercise Program Improves Stability and Balance in Patients After Acute Stroke in a Resource-Poor Setting. PM&R. 2014;6:1081–1087. doi: 10.1016/j.pmrj.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 216.Rhoda A., Mpofu R., De Weerdt W. Activity Limitations of Patients with Stroke Attending Out-Patient Facilities in the Western Cape, South Africa. S. Afr. J. Physiother. 2011;67:16–22. doi: 10.4102/sajp.v67i2.41. [DOI] [Google Scholar]
- 217.Rhoda A., Smith M., Putman K., Mpofu R., DeWeerdt W., DeWit L. Motor and Functional Recovery after Stroke: A Comparison between Rehabilitation Settings in a Developed versus a Developing Country. BMC Health Serv. Res. 2014;14:82. doi: 10.1186/1472-6963-14-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Scheffler E., Mash R. Surviving a Stroke in South Africa: Outcomes of Home-Based Care in a Low-Resource Rural Setting. Top. Stroke Rehabil. 2019;26:423–434. doi: 10.1080/10749357.2019.1623473. [DOI] [PubMed] [Google Scholar]
- 219.Titus A.W., Hillier S., Louw Q.A., Inglis-Jassiem G. An Analysis of Trunk Kinematics and Gait Parameters in People with Stroke. Afr. J. Disabil. 2018;7:1–6. doi: 10.4102/ajod.v7i0.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Blackwell Z., Littlejohns P. A Review of the Management of Dysphagia: A South African Perspective. J. Neurosci. Nurs. 2010;42:61–70. doi: 10.1097/JNN.0b013e3181ce5c86. [DOI] [PubMed] [Google Scholar]
- 221.Wasserman S., de Villiers L., Bryer A. Community-based care of stroke patients in a rural African setting. S. Afr. Med. J. 2009;99:579–583. [PubMed] [Google Scholar]
- 222.De Villiers L., Badri M., Ferreira M., Bryer A. Stroke Outcomes in a Socio-Economically Disadvantaged Urban Community. S. Afr. Med. J. 2011;101:345–348. doi: 10.7196/SAMJ.4588. [DOI] [PubMed] [Google Scholar]
- 223.Van Wyk A., Eksteen C.A., Rheeder P. The Effect of Visual Scanning Exercises Integrated Into Physiotherapy in Patients With Unilateral Spatial Neglect Poststroke. Neurorehabil. Neural Repair. 2014;28:856–873. doi: 10.1177/1545968314526306. [DOI] [PubMed] [Google Scholar]
- 224.Van Zyl M., Pillay B., Kritzinger A., Lekganyane M., Kritzinger A. Significance of Speech Production Errors on Cross- Linguistic Processing in Sepedi-English Individuals with Bilingual Aphasia: A Case Series Analysis. Top. Stroke Rehabil. 2019;26:294–306. doi: 10.1080/10749357.2019.1593612. [DOI] [PubMed] [Google Scholar]
- 225.Comley-White N., Mudzi W., Musenge E. Effects of Shoulder Strapping in Patients with Stroke: A Randomised Control Trial. S. Afr. J. Physiother. 2018;74:1–11. doi: 10.4102/sajp.v74i1.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Duff N., Ntsiea M.V., Mudzi W. Factors That Influence Return to Work after Stroke. Occup. Health South. Africa. 2014;20:6–12. [Google Scholar]
- 227.Hartley T., Burger M., Esterhuizen T.M., Inglis-Jassiem G. Functional Outcome of Stroke Inpatients According to Human Immunodeficiency Virus Status: A Feasibility Study. Afr. J. Disabil. 2020;9:1–9. doi: 10.4102/ajod.v9i0.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Hartley T., Burger M., Inglis-Jassiem G. Post Stroke Health-Related Quality of Life, Stroke Severity and Function: A Longitudinal Cohort Study. Afr. J. Disabil. 2022;11:1–10. doi: 10.4102/ajod.v11i0.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Joseph C., Rhoda A. Activity Limitations and Factors Influencing Functional Outcome of Patients with Stroke Following Rehabilitation at a Specialised Facility in the Western Cape. Afr. Health Sci. 2013;13:646–654. doi: 10.4314/ahs.v13i3.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Joseph C., Rhoda A., Conradsson D.M. Levels and Patterns of Physical Activity in Stroke Survivors with Different Ambulation Status Living in Low-Income Areas of Cape Town, South Africa. Top. Stroke Rehabil. 2020;27:494–502. doi: 10.1080/10749357.2020.1741242. [DOI] [PubMed] [Google Scholar]
- 231.Khalema D., Goldstein L.N., Lucas S. A Retrospective Analysis of Time Delays in Patients Presenting with Stroke to an Academic Emergency Department. S. Afr. J. Radiol. 2018;22:1–6. doi: 10.4102/sajr.v22i1.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Bongongo T. An Assessment of Erectile Dysfunction among Male Diabetics Attending Temba Community Health Centre, Pretoria. S. Afr. Fam. Pract. 2019;61:229–233. doi: 10.1080/20786190.2019.1658935. [DOI] [Google Scholar]
- 233.Cairncross J.P., Steinberg W.J., Labuschagne M.J. Prevalence of Eye Pathology in a Group of Diabetic Patients at National District Hospital Outpatient Department in Bloemfontein, South Africa. Afr. J. Prim. Health Care Fam. Med. 2017;9:1–7. doi: 10.4102/phcfm.v9i1.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Hlayisi V., Petersen L., Ramma L. High Prevalence of Disabling Hearing Loss in Young to Middle-Aged Adults with Diabetes. Int. J. Diabetes Dev. Ctries. 2019;39:148–153. doi: 10.1007/s13410-018-0655-9. [DOI] [Google Scholar]
- 235.Kemp T., Rheeder P. The Prevalence and Associations of Erectile Dysfunction in a South African Male Diabetic Urban Population. J. Endocrinol. Metab. Diabetes S. Afr. 2015;20:134–139. doi: 10.1080/16089677.2015.1090185. [DOI] [Google Scholar]
- 236.Mabaso R.G., Oduntan O.A. Risk Factors for Visual Impairment and Blindness amongst Black Adult Diabetics Receiving Treatment at Government Healthcare Facilities in Mopani District, Limpopo Province, South Africa. Afr. J. Prim. Health Care Fam. Med. 2014;6:1–8. doi: 10.4102/phcfm.v6i1.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Shukla A., Kumar K., Singh A. Association between Obesity and Selected Morbidities: A Study of BRICS Countries. PLoS ONE. 2014;9:e94433. doi: 10.1371/journal.pone.0094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Webb E.M., Rheeder P., Roux P. Screening in Primary Care for Diabetic Retinopathy, Maculopathy and Visual Loss in South Africa. Ophthalmologica. 2016;235:141–149. doi: 10.1159/000443972. [DOI] [PubMed] [Google Scholar]
- 239.Van Vuuren J.J., Pillay S. Major Depressive Disorder in Patients with Diabetes Mellitus in Pietermaritzburg, South Africa. S. Afr. Med. J. 2019;109:58–61. doi: 10.7196/SAMJ.2018.v109i1.13356. [DOI] [PubMed] [Google Scholar]
- 240.Mendenhall E., Norris S.A. When HIV Is Ordinary and Diabetes New: Remaking Suffering in a South African Township. Glob. Public Health. 2015;10:449–462. doi: 10.1080/17441692.2014.998698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Pillay S., Aldous C., Mahomed F. Diabetic Patients Served at a Regional Level Hospital: What Is Their Clinical Picture? J. Endocrinol. Metab. Diabetes S. Afr. 2015;20:50–56. doi: 10.1080/16089677.2015.1030856. [DOI] [Google Scholar]
- 242.Pillay S., Naidoo K.H., Msimang K. The Spectrum of Hearing Abnormalities in Patients Living with Diabetes Mellitus. S. Afr. Med. J. 2021;111:1006–1017. doi: 10.7196/SAMJ.2021.v111i10.15863. [DOI] [PubMed] [Google Scholar]
- 243.Ramkisson S., Pillay B.J., Sartorius B. Anxiety, Depression and Psychological Well-Being in a Cohort of South African Adults with Type 2 Diabetes Mellitus. S. Afr. J. Psychiatry. 2016;22:1–9. doi: 10.4102/sajpsychiatry.v22i1.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Ramkisson S., Pillay B.J., Sartorius B. Psychosocial Stress in South African Patients with Type 2 Diabetes. J. Insul. Resist. 2016;1:1–7. doi: 10.4102/jir.v1i1.17. [DOI] [Google Scholar]
- 245.De Wet H., Levitt N., Tipping B. Executive Cognitive Impairment Detected by Simple Bedside Testing Is Associated with Poor Glycaemic Control in Type 2 Diabetes. S. Afr. Med. J. 2007;97:1074–1076. [PubMed] [Google Scholar]
- 246.Le Roux M., Walsh C., Reid M., Raubenheimer J. Diabetes-Related Knowledge, Attitude and Practices (KAP) of Adult Patients with Type 2 Diabetes Mellitus in the Free State Province, South Africa. S. Afr. J. Clin. Nutr. 2018;32:83–90. doi: 10.1080/16070658.2018.1468536. [DOI] [Google Scholar]
- 247.Kagee A. Symptoms of Depression and Anxiety among a Sample of South African Patients Living with a Chronic Illness. J. Health Psychol. 2008;13:547–555. doi: 10.1177/1359105308088527. [DOI] [PubMed] [Google Scholar]
- 248.Berkowitz N., Okorie A., Goliath R., Levitt N., Wilkinson R.J., Oni T. The Prevalence and Determinants of Active Tuberculosis among Diabetes Patients in Cape Town, South Africa, a High HIV/TB Burden Setting. Diabetes Res. Clin. Pract. 2018;138:16–25. doi: 10.1016/j.diabres.2018.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Basson C.A., Stewart A., Mudzi W., Musenge E. Effect of Neural Mobilization on Nerve-Related Neck and Arm Pain: A Randomized Controlled Trial. Physiother. Can. 2020;72:408–419. doi: 10.3138/ptc-2018-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Cresswell C., Galantino M.L., Myezwa H. The Prevalence of Fear Avoidance and Pain Catastrophising amongst Patients with Chronic Neck Pain. S. Afr. J. Physiother. 2020;76:a1326. doi: 10.4102/sajp.v76i1.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Demyttenaere K., Bruffaerts R., Lee S., Posada-Villa J., Kovess V., Angermeyer M.C., Levinson D., de Girolamo G., Nakane H., Mneimneh Z., et al. Mental Disorders among Persons with Chronic Back or Neck Pain: Results from the World Mental Health Surveys. Pain. 2007;129:332–342. doi: 10.1016/j.pain.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 252.Igumbor E., Puoane T., Gansky S., Plesh O. Pain as a Reason for Primary Care Visits: Cross-Sectional Survey in a Rural and Periurban Health Clinic in the Eastern Cape, South Africa. S. Afr. Fam. Pract. 2012;54:256–263. doi: 10.1080/20786204.2012.10874224. [DOI] [Google Scholar]
- 253.Lang T., Parker R., Burgess T. Cervico-Mandibular Muscle Activity in Females with Chronic Cervical Pain. S. Afr. J. Physiother. 2013;69:3–8. doi: 10.4102/sajp.v69i3.26. [DOI] [Google Scholar]
- 254.Rauf W., Meyer H., Marcus T., Becker P. Prevalence of Chronic Pain in Patients Attending Primary Healthcare Facilities in South-West Tshwane. S. Afr. Fam. Pract. 2013;55:85–89. doi: 10.1080/20786204.2013.10874308. [DOI] [Google Scholar]
- 255.Soal L.J., Bester C.M., Shaw B.S., Yelverton C. Changes in Chronic Neck Pain Following the Introduction of a Visco-Elastic Polyurethane Foam Pillow and/or Chiropractic Treatment. Health SA Gesondheid. 2019;24:1–6. doi: 10.4102/hsag.v24i0.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Watson E.D., Coopoo Y. Telephone versus Usual Care in Management of Acute Whiplash Associated Disorder: A Pilot Study. S. Afr. J. Res. Sport. Phys. Educ. Recreat. 2016;38:259–267. [Google Scholar]
- 257.Kluge J., Hall D., Louw Q., Theron G., Grové D. Specific Exercises to Treat Pregnancy-Related Low Back Pain in a South African Population. Int. J. Gynecol. Obstet. 2011;113:187–191. doi: 10.1016/j.ijgo.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 258.Kruger P., Billson J., Wood P.S., Du Toit P.J. The Effect of Chronic Low Back Pain on Daily Living and Fear-Avoidance Beliefs in Working Adults. Afr. J. Phys. Health Educ. Recreat. Danc. 2015;21:300–314. [Google Scholar]
- 259.Major-Helsloot M.E., Crous L.C., Grimmer-Somers K., Louw Q.A., Major-Helsloot M.E., Grimmer-Somers K. Management of LBP at Primary Care Level in South Africa: Up to Standards? Afr. Health Sci. 2014;14:698–706. doi: 10.4314/ahs.v14i3.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Mattison M.C., Ross N.A. Comparing Fatigue Responses between Healthy Individuals and Asymptomatic Low Back Pain Sufferers—Implications for Return-to-Work: A Pilot Study. Ergon. SA. 2017;28:2. doi: 10.4314/esa.v28i2.2. [DOI] [Google Scholar]
- 261.Kelly A., Younus A., Lekgwara P. Minimally Invasive Spinal Surgery in Spinal Tuberculosis—A Case Report Series. Interdiscip. Neurosurg. Adv. Tech. Case Manag. 2021;23:101010. doi: 10.1016/j.inat.2020.101010. [DOI] [Google Scholar]
- 262.Younus A., Kelly A. Lumbar Unifacet Dislocation without an Associated Fracture—A Case Report and Literature Review. Interdiscip. Neurosurg. Adv. Tech. Case Manag. 2021;23:100973. doi: 10.1016/j.inat.2020.100973. [DOI] [Google Scholar]
- 263.Younus A., Kelly A., Lekgwara P. Evaluating Patient Outcome Post Tubular Lumbar Microdiscectomy. Interdiscip. Neurosurg. Adv. Tech. Case Manag. 2021;23:100975. doi: 10.1016/j.inat.2020.100975. [DOI] [Google Scholar]
- 264.Adam S., Godlwana L., Maleka D. Effect of Pre-Fracture Mobility on the Early Post-Operative Functional Outcome in Elderly Patients with a Hip Fracture. S. Afr. J. Physiother. 2013;69:13–18. doi: 10.4102/sajp.v69i3.28. [DOI] [Google Scholar]
- 265.Butler I., Tipping B., Bhaga R. Atypical Femoral Fractures. J. Endocrinol. Metab. Diabetes S. Afr. 2013;18:125–127. doi: 10.1080/22201009.2013.10872316. [DOI] [Google Scholar]
- 266.Ferreira N., Marais L.C. Bicondylar Tibial Plateau Fractures Treated with Fine-Wire Circular External Fixation. Strateg. Trauma Limb Reconstr. 2014;9:25. doi: 10.1007/S11751-014-0185-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Gdeh D., Haffejee M., Nel M. Frequency of Erectile Dysfunction Following Pelvic Fracture Among Patients Admitted to Two Wits Teaching Hospitals, South Africa. Sudan J. Med. Sci. 2018;13:144. doi: 10.18502/sjms.v13i3.2953. [DOI] [Google Scholar]
- 268.Gross T., Huettl T., Audigé L., Frey C., Monesi M., Seibert F.J., Messmer P. How Comparable Is So-Called Standard Fracture Fixation with an Identical Implant? A Prospective Experience with the Antegrade Femoral Nail in South Africa and Europe. Injury. 2010;41:388–395. doi: 10.1016/j.injury.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 269.Bhatia D.N., de Beer J.F., van Rooyen K.S., du Toit D.F. The Reverse Terrible Triad of the Shoulder: Circumferential Glenohumeral Musculoligamentous Disruption and Neurologic Injury Associated with Posterior Shoulder Dislocation. J. Shoulder Elb. Surg. 2007;16:e13–e17. doi: 10.1016/j.jse.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 270.Fleming M.A., Dachs R., Maqungo S., du Plessis J.P., Vrettos B.C., Roche S.J. Angular Stable Fixation of Displaced Distal-Third Clavicle Fractures with Superior Precontoured Locking Plates. J. Shoulder Elb. Surg. 2015;24:700–704. doi: 10.1016/j.jse.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 271.Held M., Jordaan P., Laubscher M., Singer M., Solomons M. Conservative Treatment of Fractures of the Proximal Phalanx: An Option Even for Unstable Fracture Patterns. Hand Surg. 2013;18:229–234. doi: 10.1142/S0218810413500287. [DOI] [PubMed] [Google Scholar]
- 272.Leijnen D., Med M.S., Viljoen J.T., Sci M.E., Kirby J.H., Chb M.B., Med S., Viviers P.L., Chb M.B., Sc M., et al. Frozen Shoulder or Missed Posterior Dislocation? S. Afr. J. Sport. Med. 2015;27:58–59. doi: 10.17159/2413-3108/2015/v27i2a494. [DOI] [Google Scholar]
- 273.Midgley R. Case Report: The Casting Motion to Mobilize Stiffness Technique for Rehabilitation after a Crush and Degloving Injury of the Hand. J. Hand Ther. 2016;29:323–333. doi: 10.1016/j.jht.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 274.Arendse R., Brink P., Beighton P. Hereditary Bone Dysplasia with Pathological Fractures and Nodal Osteoarthropathy. Skeletal Radiol. 2009;38:1197–1203. doi: 10.1007/s00256-009-0794-7. [DOI] [PubMed] [Google Scholar]
- 275.Chetty M., Stephen L.X.G., Roberts T. Osteoporosis-Pseudoglioma Syndrome in South Africa. S. Afr. Med. J. 2016;106:100. doi: 10.7196/SAMJ.2016.v106i6.11008. [DOI] [PubMed] [Google Scholar]
- 276.Conradie M., Conradie M.M., Scher A.T., Kidd M., Hough S. Vertebral Fracture Prevalence in Black and White South African Women. Arch. Osteoporos. 2015;10:1. doi: 10.1007/s11657-015-0203-x. [DOI] [PubMed] [Google Scholar]
- 277.Ramnarain A., Govender S. Fibular Allograft and Anterior Plating for Dislocations/Fractures of the Cervical Spine. Indian J. Orthop. 2008;42:83–86. doi: 10.4103/0019-5413.38587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Oosthuizen G.V., De Wet J., Bruce J.L., Clarke D.L. Rib Fracture Fixation in a South African Public Trauma Service. S. Afr. J. Surg. 2017;55:4–8. [PubMed] [Google Scholar]
- 279.Enicker B., Madiba T.E. Cranial Injuries Secondary to Assault with a Machete. Injury. 2014;45:1355–1358. doi: 10.1016/j.injury.2014.04.036. [DOI] [PubMed] [Google Scholar]
- 280.Awolola A.M., Campbell L., Ross A. Pain Management in Patients with Long-Bone Fractures in a District Hospital in KwaZulu-Natal, South Africa. Afr. J. Prim. Health Care Fam. Med. 2015;7:1–5. doi: 10.4102/phcfm.v7i1.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Gous E., Ally M.M.T.M., Meyer P.W.A., Suleman F.E. Simple Erosion Narrowing Score of the Hands as a Predictor of Cervical Spine Subluxation in Rheumatoid Arthritis. S. Afr. J. Radiol. 2020;24:1–6. doi: 10.4102/sajr.v24i1.1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Lombard L.A., du Plessis L.M., Visser J. Body Composition of Rheumatoid Arthritis Patients in the City of Cape Town, South Africa. Clin. Rheumatol. 2014;33:467–476. doi: 10.1007/s10067-013-2414-0. [DOI] [PubMed] [Google Scholar]
- 283.Nolte K. Land- and Water-Based Exercises in Rheumatoid Arthritis Patients: A Series of Case Reports. S. Afr. J. Sport. Med. 2011;23:69–70. doi: 10.17159/2078-516X/2011/v23i3a335. [DOI] [Google Scholar]
- 284.Prioreschi A., Makda M.A., Tikly M., McVeigh J.A. In Patients with Established RA, Positive Effects of a Randomised Three Month WBV Therapy Intervention on Functional Ability, Bone Mineral Density and Fatigue Are Sustained for up to Six Months. PLoS ONE. 2016;11:e0153470. doi: 10.1371/journal.pone.0153470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Solomon A., Christian B.F., Woodiwiss A.J., Norton G.R., Dessein P.H. Burden of Depressive Symptoms in South African Public Healthcare Patients with Established Rheumatoid Arthritis: A Case-Control Study. Clin. Exp. Rheumatol. 2011;29:506–512. [PubMed] [Google Scholar]
- 286.Younus A., Kelly A. Hip Spine Syndrome—A Case Series and Literature Review. Interdiscip. Neurosurg. Adv. Tech. Case Manag. 2021;23:100960. doi: 10.1016/j.inat.2020.100960. [DOI] [Google Scholar]
- 287.Frimpong E., Mcveigh J.A., Van Der Jagt D., Mokete L., Kaoje Y.S. Light Intensity Physical Activity Increases and Sedentary Behavior Decreases Following Total Knee Arthroplasty in Patients with Osteoarthritis. Knee Surg. Sport. Traumatol. Arthrosc. 2019;27:2196–2205. doi: 10.1007/s00167-018-4987-2. [DOI] [PubMed] [Google Scholar]
- 288.Cloake T., Haigh T., Cheshire J., Walker D. ScienceDirect The Impact of Patient Demographics and Comorbidities upon Burns Admitted to Tygerberg Hospital Burns Unit, Western Cape, South Africa. Burns. 2016;43:411–416. doi: 10.1016/j.burns.2016.08.031. [DOI] [PubMed] [Google Scholar]
- 289.Eyal A.S., Kemp M., Luvhengo T. A 10-Year Audit of Burns at Kalafong Hospital. Burns. 2007;33:393–395. doi: 10.1016/j.burns.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 290.Kinoo S.M., Singh B. Complex Regional Pain Syndrome in Burn Pathological Scarring: A Case Report and Review of the Literature. Burns. 2017;43:e47–e52. doi: 10.1016/j.burns.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 291.Morris L.L. Pain and Anxiety Experiences of South African Adult Burn Injury Patients. S. Afr. J. Physiother. 2010;66:6–9. doi: 10.4102/sajp.v66i1.56. [DOI] [Google Scholar]
- 292.Den Hollander D., Albert M., Strand A., Hardcastle T.C. Epidemiology and Referral Patterns of Burns Admitted to the Burns Centre at Inkosi Albert Luthuli Central Hospital, Durban. Burns. 2014;40:1201–1208. doi: 10.1016/j.burns.2013.12.018. [DOI] [PubMed] [Google Scholar]
- 293.Ablort-morgan C., Allorto N.L., Rode H. ScienceDirect Rehabilitation of a Bilateral Upper Limb Amputee in a Resource Restricted Burn Service. Burns. 2016;42:e81–e85. doi: 10.1016/j.burns.2016.01.027. [DOI] [PubMed] [Google Scholar]
- 294.Govender S.M., de Jongh M. Identifying Hearing Impairment and the Associated Impact on the Quality of Life among the Elderly Residing in Retirement Homes in Pretoria, South Africa. S. Afr. J. Commun. Disord. 2021;68:1–9. doi: 10.4102/sajcd.v68i1.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Louw C., Swanepoel D.W., Eikelboom R.H., Hugo J. Prevalence of Hearing Loss at Primary Health Care Clinics in South Africa. Afr. Health Sci. 2018;18:313–320. doi: 10.4314/ahs.v18i2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Olivier B., Pramod A., Maleka D. Trigger Point Sensitivity Is a Differentiating Factor between Cervicogenic and Non-Cervicogenic Headaches: A Cross-Sectional, Descriptive Study. Physiother. Can. 2018;70:323–329. doi: 10.3138/ptc.2017-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Rouillard S., De Weerdt W., De Wit L., Jelsma J. Functioning at 6 Months Post Stroke Following Discharge from Inpatient Rehabilitation. S. Afr. Med. J. 2012;102:545–548. doi: 10.7196/SAMJ.5488. [DOI] [PubMed] [Google Scholar]
- 298.Parker R., Stein D.J., Jelsma J. Pain in People Living with HIV/AIDS: A Systematic Review. J. Int. AIDS Soc. 2014;17:18719. doi: 10.7448/IAS.17.1.18719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Maritz J., Benatar M., Dave J.A., Harrison T.B., Badri M., Levitt N.S., Heckmann J.M. HIV Neuropathy in South Africans: Frequency, Characteristics, and Risk Factors. Muscle Nerve. 2010;41:599–606. doi: 10.1002/mus.21535. [DOI] [PubMed] [Google Scholar]
- 300.Naude J.J., Manjra M.A., Birkholtz F., Barnard A., Tetsworth K., Glatt V., Hohmann E. Functional Outcomes and Quality of Life Following Complex Tibial Fractures Treated with Circular External Fixation: A Comparison between Proximal, Midshaft, and Distal Tibial Fractures. Strateg. Trauma Limb Reconstr. 2021;16:32–40. doi: 10.5005/jp-journals-10080-1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Wasserman S., de Villiers L., Bryer A., de Villiers L., Bryer A., de Villiers L., Bryer A. Stroke Care in a Rural African Setting. Int. J. Stroke. 2009;4:151. doi: 10.1111/j.1747-4949.2009.00275.x. [DOI] [PubMed] [Google Scholar]
- 302.Spies G., Ahmed-Leitao F., Fennema-Notestine C., Cherner M., Seedat S. Effects of HIV and Childhood Trauma on Brain Morphometry and Neurocognitive Function. J. Neurovirol. 2016;22:149–158. doi: 10.1007/s13365-015-0379-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Penn C., Commerford A., Ogilvy D. Spatial and Facial Processing in the Signed Discourse of Two Groups of Deaf Signers with Clinical Language Impairment. Clin. Linguist. Phon. 2007;21:369–391. doi: 10.1080/02699200701267476. [DOI] [PubMed] [Google Scholar]
- 304.Nicholas P.K., Voss J., Wantland D., Lindgren T., Huang E., Holzemer W.L., Cuca Y., Moezzi S., Portillo C., Willard S., et al. Prevalence, Self-Care Behaviors, and Self-Care Activities for Peripheral Neuropathy Symptoms of HIV/AIDS. Nurs. Health Sci. 2010;12:119–126. doi: 10.1111/j.1442-2018.2009.00505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Matter R.A., Eide A.H. Access to Assistive Technology in Two Southern African Countries. BMC Health Serv. Res. 2018;18:792. doi: 10.1186/s12913-018-3605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Maart S. Ph.D. Thesis. University of Cape Town; Cape Town, South Africa: 2015. Disability in Under-Resourced Areas in the Western Cape, South Africa: A Descriptive Analytical Study. [Google Scholar]
- 307.Jesus T.S., Bright F., Kayes N., Cott C.A. Person-Centred Rehabilitation: What Exactly Does It Mean? Protocol for a Scoping Review with Thematic Analysis towards Framing the Concept and Practice of Person-Centred Rehabilitation. BMJ Open. 2016;6:e011959. doi: 10.1136/bmjopen-2016-011959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Üstün T.B., Chatterji S., Bickenbach J., Kostanjsek N., Schneider M. The International Classification of Functioning, Disability and Health: A New Tool for Understanding Disability and Health. Disabil. Rehabil. 2003;25:565–571. doi: 10.1080/0963828031000137063. [DOI] [PubMed] [Google Scholar]
- 309.Zondi T., Day C. Measuring National Health Insurance: Towards Universal Health Coverage in South Africa. S. Afr. Health Rev. 2019;2019:55–68. [Google Scholar]
- 310.Ned L., Cloete L., Mji G. The Experiences and Challenges Faced by Rehabilitation Community Service Therapists within the South African Primary Healthcare Health System. Afr. J. Disabil. 2017;6:1–11. doi: 10.4102/ajod.v6i0.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.World Health Organization . Rehabilitation Competency Framework. World Health Organization; Geneva, Switzerland: 2020. Electronic Version. [Google Scholar]
- 312.Kredo T., Abrams A., Young T., Louw Q., Volmink J., Daniels K. Primary Care Clinical Practice Guidelines in South Africa: Qualitative Study Exploring Perspectives of National Stakeholders. BMC Health Serv. Res. 2017;17:608. doi: 10.1186/s12913-017-2546-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Stander J., Grimmer K., Brink Y. Factors Influencing Clinical Practice Guideline Uptake by South African Physiotherapists: A Qualitative Investigation of Barriers and Facilitators. J. Eval. Clin. Pract. 2020;26:728–737. doi: 10.1111/jep.13182. [DOI] [PubMed] [Google Scholar]
- 314.WHO . Task Shifting: Global Recommendations and Guidelines. WHO; Geneva, Switzerland: 2008. [Google Scholar]
- 315.WHO . Rehabilitation in Health Systems. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 316.Hone T., Macinko J., Millett C. Revisiting Alma-Ata: What Is the Role of Primary Health Care in Achieving the Sustainable Development Goals? Lancet. 2018;392:1461–1472. doi: 10.1016/S0140-6736(18)31829-4. [DOI] [PubMed] [Google Scholar]
- 317.Singh R., Küçükdeveci A.A., Grabljevec K., Gray A. The Role of Interdisciplinary Teams in Physical and Rehabilitation Medicine. J. Rehabil. Med. 2018;50:673–678. doi: 10.2340/16501977-2364. [DOI] [PubMed] [Google Scholar]
- 318.Kuper H., Smythe T., Kujinga T., Chivandire G., Rusakaniko S. Should Disability-Inclusive Health Be a Priority in Low-Income Countries? A Case-Study from Zimbabwe. Glob. Health Action. 2022;15:2032929. doi: 10.1080/16549716.2022.2032929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Mapanga W., Casteleijn D., Ramiah C., Odendaal W., Metu Z., Robertson L., Goudge J. Strategies to Strengthen the Provision of Mental Health Care at the Primary Care Setting: An Evidence Map. PLoS ONE. 2019;14:e0222162. doi: 10.1371/journal.pone.0222162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Petersen I., Fairall L., Bhana A., Kathree T., Selohilwe O., Brooke-Sumner C., Faris G., Breuer E., Sibanyoni N., Lund C., et al. Integrating Mental Health into Chronic Care in South Africa: The Development of a District Mental Healthcare Plan. Br. J. Psychiatry. 2016;208:s29. doi: 10.1192/bjp.bp.114.153726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Hoosain M., Plastow N.A. Protocol: Workplace-Based Occupational Therapy for Mental Health in Africa: A Scoping Review Protocol. BMJ Open. 2022;12:e054821. doi: 10.1136/bmjopen-2021-054821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Plastow N.A., van Niekerk L., Cloete L., Leibbrandt D. Collaborative Capacity Development to Complement Stroke Rehabilitation in Africa [Internet] AOSIS; Cape Town, South Africa: 2021. The Effect of Interventions to Support Mental Health Post-Stroke in Africa: A Systematic Review; pp. 133–169. [Google Scholar]
- 323.Barnabé M.A., Gordon R., Ramjee G., Loots G., Blackburn J.M. National Expenditure on Health Research in South Africa: How Has the Landscape Changed in the Past Decade? S. Afr. Med. J. 2020;110:274–283. doi: 10.7196/SAMJ.2020.v110i4.14349. [DOI] [PubMed] [Google Scholar]
- 324.Lekoubou A., Echouffo-Tcheugui J.B., Kengne A.P. Epidemiology of Neurodegenerative Diseases in Sub-Saharan Africa: A Systematic Review. BMC Public Health. 2014;14:653. doi: 10.1186/1471-2458-14-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions of Rehab4all application developed.