Abstract
Simple Summary
Germline BRCA1 and BRCA2 pathogenic variant carriers are recognized to be at increased risk for multiple cancers including breast, ovarian, pancreatic, and prostate cancer, with risk management recommendations for these cancers included in BRCA1/2 guidelines. Currently, it is remains uncertain whether BRCA1/2 carriers are also at an increased risk for gastric cancer. Herein, we review the accumulating evidence that suggests BRCA1/2 carriers are at increased risk for gastric cancer, particularly among BRCA2 carriers. We also review existing literature addressing BRCA1/2-associated gastric carcinogenesis and potential avenues for therapeutic intervention. Lastly, we present gastric cancer risk management considerations for BRCA1/2 carriers as currently no such recommendations exist.
Abstract
Carriers of a pathogenic germline variant (PV) in BRCA1 or BRCA2 are at increased risk for a number of malignancies, including breast, ovarian, pancreatic, and prostate cancer. In this review, we discuss emerging evidence that BRCA2 PV carriers, and likely also BRCA1 PV carriers, are also at increased risk for gastric cancer (GC), highlighting that GC may be part of the BRCA1/2 cancer risk spectrum. While the pathogenesis of GC among BRCA1/2 PV carriers remains unclear, increasing evidence reveals that GCs are often enriched with mutations in homologous recombination-associated genes such as BRCA1/2, and that GC prognosis and response to certain therapies can depend on BRCA1/2 expression. Given the strength of data published to date, a risk management strategy for GC among BRCA1/2 PV carriers is needed, and herein we also propose a potential strategy for GC risk management in this population. Moving forward, further study is clearly warranted to define the mechanistic relationship between BRCA1/2 PVs and development of GC as well as to determine how GC risk management should be factored into the clinical care of BRCA1/2 carriers.
Keywords: breast cancer susceptibility gene, DNA damage, hereditary breast and ovarian cancer syndrome, pathogenic germline variants, stomach cancer
1. Introduction
DNA damage resulting in double-strand breaks (DSBs) creates genomic instability and initiates the DNA damage response to allow for repair of these DSBs [1,2]. The two primary processes of DNA DSB repair are non-homologous end joining (NHEJ) and homologous recombination (HR). In NHEJ the broken ends of DNA are directly ligated [3,4], which can result in small nucleotide deletions at the DSB site or larger deletions and chromosomal rearrangement if multiple DSBs are simultaneously present [2,3,4]. Conversely, HR is less error prone as it involves the use of a homologous DNA sequence as a template to restore lost genetic information at the site of a DSB [1,2].
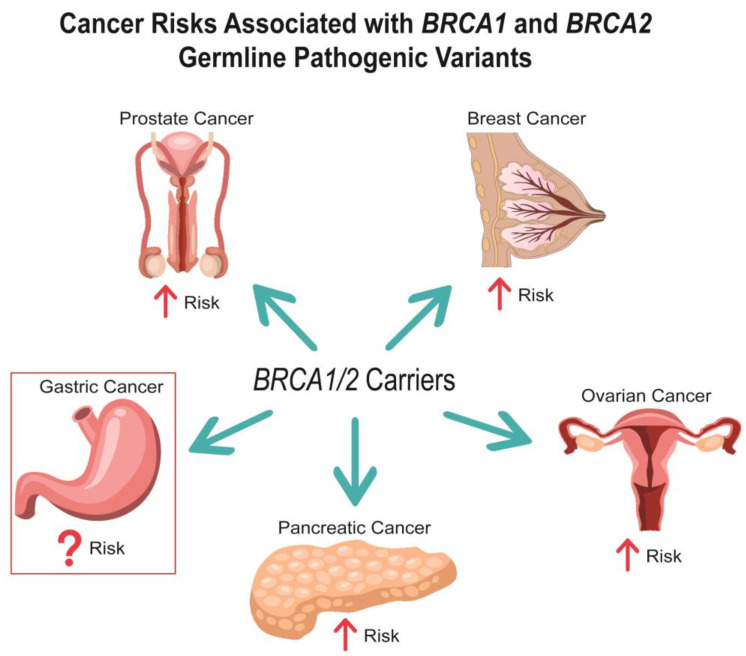
Breast cancer susceptibility gene one (BRCA1) and two (BRCA2), are well established tumor suppressor genes that play a pivotal role in promoting HR in response to DNA damage [5,6,7]. Indeed, pathogenic germline variants (PVs) in either of these genes leads to an increase in NHEJ, which can in turn promote genomic instability and tumorigenesis [2,3,4,8,9,10,11]. BRCA1 was first described as a hereditary breast and ovarian cancer susceptibility gene in 1994, followed by BRCA2 in 1995 [12,13]. Since then, the risks for breast and ovarian cancer in BRCA1/2 PV carriers have been well characterized (Figure 1). Importantly, cancer risks differ between BRCA1 and BRCA2 PVs as well as by sex. For instance, female BRCA1 PV carriers are at a higher risk for breast and ovarian cancer than BRCA2 PV carriers [14]. Meanwhile, male BRCA1/2 PV carriers are at a much lower absolute risk for breast cancer than females [15], although the relative breast cancer risk compared to the general population is higher in male versus female BRCA1/2 carriers. In addition to breast and ovarian cancer, an increased risk for prostate cancer in BRCA2 PV carriers as well as pancreatic cancer in both male and female BRCA1/2 PV carriers has been recognized [15,16]. Currently, there are guidelines that outline risk management strategies for all the aforementioned cancers in BRCA1/2 PV carriers [17,18,19,20].
Figure 1.
Cancer Risks Associated with BRCA1 and BRCA2 Germline Pathogenic Variants.
There is mounting evidence that BRCA1/2 PV carriers also have an elevated risk of gastric cancer (GC) [15,16,21,22,23,24,25,26,27,28]. Indeed, a recent study showed a cumulative risk as high as 21.3% for BRCA1 and 19.3% for BRCA2 PV carriers by age 85, however this study was performed in a Japanese population where risk of GC is increased at baseline [16]. Importantly, despite this potential increased GC risk, there are currently no recommended GC surveillance guidelines for BRCA1/2 PV carriers. Furthermore, while mechanistic implications of BRCA1/2 in GC pathogenesis remain obscure, there is evidence that GC may be enriched for mutations in genes associated with HR and confer a tumor mutation signature associated with HR deficiency [29,30,31]. Additionally, BRCA1/2 expression levels may be prognostic for chemotherapy response in GC [29,30,31,32,33,34,35,36,37].
Given the emerging evidence for increased GC risk in BRCA1/2 PV carriers, it is critical, and timely, that the existing literature is evaluated to help guide development of risk management strategies and identify potential areas of future investigation. Therefore, the intent of this review is 3-fold. (1) To summarize what is currently known about the risk of GC in BRCA1/2 PV carriers. (2) Describe the evidence of HR deficiency and altered BRCA1/2 expression in GC pathogenesis. (3) Identify potential strategies for gastric surveillance in BRCA1/2 PV carriers.
2. Gastric Cancer Risk in BRCA1/2 Carriers
Over the last three decades there have been multiple studies that examined risk of GC among BRCA1/2 PV carriers. While the majority of these studies analyzed BRCA1 and BRCA2 PV carriers as separate populations, other studies evaluated BRCA1/2 carriers as a combined cohort. When presenting the data from studies examining GC risk in BRCA1/2 PV carriers, we have divided this data between BRCA1 PV carriers, BRCA2 PV carriers, and study populations comprised of both BRCA1 and BRCA2 PV carriers. Of note, in the majority of these BRCA1/2 studies, individuals did not necessarily undergo multigene panel testing, and thus it is possible that some of the observed cases of GC were driven by PVs in genes increasing risk of GC other than BRCA1/2.
2.1. Gastric Cancer Risk among BRCA1 PV Carriers
Several studies have provided compelling evidence that germline BRCA1 PVs may increase risk of GC (Table 1). In a 1999 study by Johannsson et al. [27] examining the incidence of malignant tumors in 29 Swedish families (n = 1145 relatives) with a proband carrying a germline BRCA1 PV, incidence of GC was increased among all individuals (standardized morbidity rate (SMR) 2.76, 95% CI 1.01–6.00) and women in isolation (SMR 5.16, 95% CI 1.14–13.22), but not among men (SMR 1.43, 95% CI 0.17–5.15). In a 2001 study by Risch et al. [38] involving 649 patients in Canada with ovarian cancer, including 39 BRCA1 PV carriers, risk of GC was increased 6-fold in first-degree relatives of BRCA1 PV carriers compared to relatives of non-carriers (incidence 4.9% vs. 0.8%; RR 6.2, 95% CI 2.0–19). One year later, Brose et al. [39] similarly found that age-adjusted GC risk was seven times higher among BRCA1 PV carriers (n = 483) from two U.S. centers compared to the general population (5.5% vs. 0.8%, 95% CI 3.4–7.5%). In a 2012 study by Moran et al. [23] involving 268 BRCA1-associated families in England, risk of GC was increased in BRCA1-positive families compared to the general population (RR 2.4, 95% CI 1.2–4.3), although notably this risk was driven by GC diagnosed among 1184 potential BRCA1 PV carriers that had not undergone BRCA1/2 testing. More recently in 2022, Li et al. [15] examined cancer risk among 3184 families in the multinational Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA) with at least one family member having a BRCA1 PV, noting increased risk of GC among 8884 BRCA1 PV carriers (RR 2.17, 95% CI 1.25–3.77), particularly including those less than 65 years old (RR 3.50, 95% CI 2.01–6.10). By age 80, the absolute risk of developing GC among BRCA1 PV carriers was 0.7% (95% CI 0.3–1.7) for females and 1.6% (95% CI 0.7–4.0) for males [15]. Furthermore, in a 2022 case–control study in Japan by Momozawa et al. [16] involving 63,828 patients with at least one of 14 different cancer types and 37,086 controls, BRCA1 PVs were again associated with increased risk of GC (OR 5.2, 95% CI 2.6–10.5). The average age of GC diagnosis was 62.3 ± 12.0 among BRCA1 PV carriers compared to 65.7 ± 10.5 among non-carriers of BRCA1/2 PVs (p = 0.14), and cumulative GC risk was 21.3% (95% CI 6.9–33.4%) by age 85 in BRCA1 PV carriers compared to just below 5% for individuals without a BRCA1/2 PV [16]. Notably, the high cumulative GC risk for all subsets of patients in this study likely reflects the elevated incidence of GC in East Asian countries [40]. Furthermore, sex-specific GC risks were not calculated in this study.
Table 1.
Select Studies Reporting Gastric Cancer Risk in BRCA1 Carriers.
| Author | Year | Population Location | Patient Population | Comparator Cohort | Risk Estimates | Gastric Cancer Risk Increased? |
|---|---|---|---|---|---|---|
| Gastric Cancer Risk in BRCA1 PV Carriers | ||||||
| Ford et al. [41] | 1994 | North America and Western Europe | 464 BRCA1 PV carriers | General Population | 1 observed case vs. 0.76 cases expected; RR 1.11, p > 0.05 | No |
| Johannsson et al. [27] | 1999 | Sweden | 1145 relatives from 29 families with a proband with a BRCA1 PV | General Population | All: SMR 2.76, 95% CI 1.01–6.00; F: SMR 5.16, 95% CI 1.14–13.22; M: SMR 1.43, 95% CI 0.17–5.15 | Yes |
| Risch et al. [38] | 2001 | Canada | 39 BRCA1 PV carriers and 291 FDRs | 4378 FDRs of ovarian cancer patients without BRCA1 or BRCA2 PVs | Incidence: 4.9% vs. 0.8%; RR 6.2, 95% CI 2.0–19 | Yes |
| Brose et al. [39] | 2002 | United States | 483 BRCA1 PV carriers | General Population | Age-adjusted lifetime risk: 5.5% vs. 0.8%, 95% CI 3.4–7.5% | Yes |
| Thompson et al. [42] | 2002 | North America and Western Europe | 2245 BRCA1 PV carriers | General Population | RR 1.56, 95% CI 0.91–2.68 | No |
| Schlebusch et al. [26] | 2010 | South Africa | 793 individuals from 26 families with a BRCA1 PV | General Population | 7 cases observed vs. 6.62 cases expected, p = 0.8829 | No |
| Moran et al. [23] | 2012 | England | 631 BRCA1 PV carriers and 1184 FDRs from 268 families with a BRCA1 PV | General Population | RR 2.4, 95% CI 1.2–4.3 | Yes |
| Mersch et al. [43] | 2014 | United States | 613 BRCA1 PV carriers | General Population | SIR 1.736, 95% CI 0.023–9.661 | No |
| Li et al. [15] | 2022 | Multinational (>10 countries) | 8884 BRCA1 PV carriers | General Population | RR 2.17, 95% CI 1.25–3.77 | Yes |
| BRCA1 PVs amongst gastric cancer patients | ||||||
| Ławniczak et al. [44] | 2016 | Poland | 317 patients with GC | 4570 controls | Mutation rate: 0.63% vs. 0.48%; OR 1.3, 95% CI 0.3–5.6 | No |
| Momozawa et al. [16] | 2022 | Japan | 10,705 cases of GC | 37,086 controls | OR 5.2, 95% CI 2.6–10.5 | Yes |
| Meta-analysis | ||||||
| Lee et al. [45] | 2021 | North America, Western Europe, South Africa | Meta-analysis, including 5 studies pertaining to BRCA1 PVs, all of which are cited in this sub-section of Table 1 [23,28,38,42,43] | Varied by study | BRCA1 PVs were not associated with increased risk of GC (RR 1.70, 95% CI 0.93–3.09) | No |
Abbreviations: CI—confidence interval; F—female; FDR—first degree relative; GC—gastric cancer; M—male; OR—odds ratio; PV—pathogenic variant; RR—relative risk; SIR—standardized incidence ratio; SMR—standardized morbidity rate.
In contrast, there are other studies suggesting that GC risk may not be increased among germline BRCA1 PV carriers. In a 1994 study by Ford et al. [41] of 33 families with linkage to BRCA1 (including 464 BRCA1 PV carriers) in North America and Western Europe in the Breast Cancer Linkage Consortium (BCLC), only one carrier was found to have GC, which did not significantly vary from what was expected (0.76 cases expected) based on population metrics (RR 1.11, p > 0.05). Several years later, a 2002 study comprised of 699 families in Western Europe and North America with at least one member carrying a BRCA1 PV noted that risk of GC was not statistically significantly higher among 2245 BRCA1 PV carriers compared to the general population (RR 1.56, 95% CI 0.91–2.68) [42]. Likewise, a 2010 study by Schlebusch et al. [26] involving South African families with history of breast and/or ovarian cancer noted that risk of GC was not increased among 26 families (n = 793 relatives) with a BRCA1 PV compared to the general population (7 cases observed vs. 6.62 expected, p = 0.8829). In 2014, a study by Mersch et al. [43] similarly noted that GC risk was not increased among 613 BRCA1 PV carriers (standardized incidence ratio (SIR) 1.736, 95% CI 0.023–9.661). Two years later, a 2016 study in Poland demonstrated that founder BRCA1 PVs were not detected more frequently among 317 patients with GC compared to 4570 controls (0.63% vs. 0.48%; OR 1.3, 95% CI 0.3–5.6) [44]. Most recently, in a 2021 meta-analysis by Lee et al. [45], BRCA1 PVs were not associated with increased risk of GC (RR 1.70, 95% CI 0.93–3.09) based on the collective analysis of data from five studies, all of which are cited above [23,26,38,42,43]; notably, the 2022 studies by Li et al. [15] and Momozawa et al. [16], which both noted an association between BRCA1 PVs and increased GC risk, were published after this 2021 meta-analysis. Thus, accounting for all evidence published to date, it seems most likely that BRCA1 PV carriers are at a modestly increased risk for GC, although further study is warranted to more clearly define this relationship.
2.2. Gastric Cancer Risk among BRCA2 PV Carriers
A majority of studies have found that GC risk is increased among germline BRCA2 PV carriers (Table 2). In a 1999 study by the BCLC involving 173 families with BRCA2 PVs in Western Europe, the United States, and Canada (n = 3728 relatives), BRCA2 PV carriers were at increased risk for GC compared to the general population (RR 2.59, 95% CI 1.46–4.61) [28]. Shortly thereafter, in a 2001 study involving 70 Ashkenazi Jewish patients with gastrointestinal (GI) malignancies, the BRCA2 Ashkenazi Jewish founder PV (6174delT) was enriched among patients with GC compared to the general Ashkenazi Jewish population (5.7% vs. 1.2%; OR 5.2, 95% CI 1.2–22) [25]. The following year, Tulinius et al. [46] examined the effect of a single Icelandic founder BRCA2 PV (999del5) on cancer risk among families of 995 breast cancer patients in Iceland, 90 of whom tested positive for the BRCA2 founder. GC risk was increased among male first-degree relatives of BRCA2-positive probands (RR 2.40, 95% CI 1.29–4.05), male second-degree relatives of BRCA2-positive probands (RR 1.91, 95% CI 1.33–2.63), female second-degree relatives of BRCA2-positive probands (RR 3.08, 95% CI 2.09–4.34), and female second-degree relatives of all probands (RR 1.39, 95% CI 1.17–1.61) [46]. That same year, Jakubowska et al. [24] published a study based in Poland revealing that BRCA2 PVs were observed more frequently among 29 families with at least one female breast cancer diagnosed before the age of 50 and one male GC diagnosed before the age of 55 compared to 248 breast-ovarian cancer families (20.7% vs. 6.9%, p < 0.025). In 2003, the same authorship group published a similar study revealing that BRCA2 PVs were found more frequently in 34 Polish women with ovarian cancer and a family history of GC (mean age of GC diagnosis of 59 years, range: 33–76) compared to 75 Polish women with ovarian cancer and a family history of ovarian but not GC (23.5% vs. 4.0%; OR 7.4, 95% CI 1.8–30) [47]. Several years later, the aforementioned 2010 study by Schlebusch et al. [26] examining cancer prevalence among South African breast-ovarian cancer families revealed that prevalence of GC was increased among 43 families (n = 1264 relatives) with a BRCA2 PV compared to the general population (24 cases observed vs. 11.17 expected, p = 0.0001). Along the same lines, risk of GC was increased among BRCA2 families (RR 2.7, 95% CI 1.3–4.8) in the 2012 study by Moran et al. [23], which included 222 BRCA2 families comprised of 517 individuals that tested positive for a BRCA2 PV and 1009 non-tested first-degree relatives of BRCA2 PV carriers. More recently, in the 2021 meta-analysis by Lee et al. [45], BRCA2 PVs were associated with increased risk of GC (RR 2.15, 95% CI 1.98–2.33) based on analysis of six studies, each of which is cited in this subsection [23,26,38,43,48]. In the 2022 multinational study by Li et al. [15], which included 2157 BRCA2 families, BRCA2 PV carriers (n = 6095) were again found to be at increased risk of GC (RR 3.69, 95% CI 2.40–5.67). While the relative risk of GC was higher among females compared to males (6.89 vs. 2.76, p = 0.04), both male and female BRCA2 PV carriers had an absolute risk of developing GC by age 80 of 3.5% [15]. Finally, BRCA2 PVs were associated with increased risk of GC (OR 4.7, 95% CI 3.1–7.1) in the 2022 study by Momozawa et al. [16] in a Japanese population. Among BRCA2 PV carriers, the average age of GC diagnosis was 64.5 ± 9.7, and the cumulative risk of GC was 19.3% (95% CI 11.9–26.0%) by age 85. [16]
Table 2.
Select Studies Reporting Gastric Cancer Risk in BRCA2 Carriers.
| Author | Year | Population Location | Patient Population | Comparator Cohort | Risk Estimates | Gastric Cancer Risk Increased? |
|---|---|---|---|---|---|---|
| Gastric Cancer Risk in BRCA2 PV Carriers | ||||||
| Breast Cancer Linkage Consortium [28] | 1999 | Europe and North America | 1152 confirmed or probable BRCA2 PV carriers from 173 families * | General Population | RR 2.59, 95% CI 1.46–4.61 | Yes |
| Johannsson et al. [27] | 1999 | Sweden | 728 relatives from 20 families with a proband with a BRCA2 PV | General Population | All: SMR 1.63, 95% CI 0.34–4.75; F: SMR 1.37, 95% CI 0.03–7.64; M: 1.79, 0.22–6.48 | No |
| Risch et al. [38] | 2001 | Canada | 21 BRCA2 PV carriers and 160 FDRs | 4378 FDRs of ovarian cancer patients without BRCA1 or BRCA2 PVs | Incidence: 1.8% vs. 0.80%; RR 2.3, 95% CI 0.30–18 | No |
| Tulinius et al. [46] | 2002 | Iceland | 90 families with a proband with a BRCA2 PV | General Population | F FDRs: RR 1.78, 95% CI 0.57–4.10; F SDRs: RR 3.08, 95% CI 2.09–4.34; M FDRs: RR 2.40, 95% CI 1.29–4.05; M SDRs: RR 1.91, 95% CI 1.33–2.63 | Yes |
| van Asperen et al. [48] | 2005 | Netherlands | 1811 individuals with a 50% probability of having a BRCA2 PV | General Population | RR 1.2, 95% CI 0.6–2.0 | No |
| Schlebusch et al. [26] | 2010 | South Africa | 1264 individuals from 43 families with a BRCA2 PV | General Population | 24 cases observed vs. 11.17 cases expected, p = 0.0001 | Yes |
| Moran et al. [23] | 2012 | England | 517 BRCA2 PV carriers and 1009 FDRs from 222 families with a BRCA2 PV | General Population | RR 2.7, 95% CI 1.3–4.8 | Yes |
| Mersch et al. [43] | 2014 | United States | 459 BRCA2 PV carriers | General Population | SIR 1.755, 95% CI 0.023–9.763 | No |
| Li et al. [15] | 2022 | Multinational (>10 countries) | 6095 BRCA2 PV carriers | General Population | RR 3.69, 95% CI 2.40–5.67 | Yes |
| BRCA2 PVs amongst gastric cancer patients | ||||||
| Figer et al. [25] | 2001 | Israel | 35 Ashkenazi Jewish patients with GC | General Ashkenazi Jewish Population | Mutation rate: 5.7% vs. 1.2%; OR 5.2, 95% CI 1.2–22 | Yes |
| Jakubowska et al. [24] | 2002 | Poland | 29 breast cancer patients from families with ≥1 female breast cancer diagnosed before age 50 and ≥1 male GC diagnosed before age 55 | 248 breast-ovarian cancer families | Mutation rate: 20.7% vs. 6.9%, p < 0.025 | Yes |
| Jakubowska et al. [47] | 2003 | Poland | 34 women with ovarian cancer and family history of GC | 75 women with ovarian cancer and family history of ovarian cancer but not GC | Mutation rate: 23.5% vs. 4.0%; OR 7.4, 95% CI 1.8–30 | Yes |
| Momozawa et al. [16] | 2022 | Japan | 10,705 cases of GC | 37,086 controls | OR 4.7, 95% CI 3.1–7.1 | Yes |
| Meta-analysis | ||||||
| Lee et al. [45] | 2021 | North America, Western Europe, South Africa | Meta-analysis, including 6 studies pertaining to BRCA2 PVs, all of which are cited in this sub-section of Table 2 [23,25,28,38,43,49] | Varied by study | BRCA2 PVs were associated with increased risk of GC (RR 2.15, 95% CI 1.98–2.33) | Yes |
* In a cohort of families with BRCA2 PVs, probable BRCA2 PV carriers were defined as men with breast cancer, females with breast cancer diagnosed < 60 years old, and females with ovarian cancer (excluding known non-carriers). Abbreviations: CI—confidence interval; F—female; FDR—first degree relative; GC—gastric cancer; M—male; OR—odds ratio; PV—pathogenic variant; RR—relative risk; SDR—second degree relative; SIR—standardized incidence ratio; SMR—standardized morbidity rate.
There are only a few studies that have not found an elevated risk of GC among BRCA2 PV carriers. In the 1999 study by Johannsson et al. [27], GC risk was not increased among 20 BRCA2-associated families (n = 728 relatives) compared to the general population (SMR 1.63, 95% CI 0.34–4.75). Similarly, in the 1999 study by Risch et al. [38], in which BRCA2 PVs were identified in 21 of 649 women with ovarian cancer, no association was found between risk of GC and presence of a BRCA2 PV (RR 2.3, 95% CI 0.30–18). Similarly, GC risk was not increased among individuals with a 50% probability of having a BRCA2 PV (n = 1811) in a 2005 study based in the Netherlands (RR 1.2, 95% CI 0.6–2.0) [48]. Finally, in the aforementioned 2014 study by Mersch et al. [43], risk of GC was not increased among 459 BRCA2 PV carriers compared to the general population (SIR 1.755, 95% CI 0.023–9.763). Despite the handful of studies to the contrary, the constellation of evidence cited above, highlighted by the 2021 meta-analysis by Lee et al. [45] and 2022 studies by Li et al. [15] and Momozawa et al. [16], strongly suggests that BRCA2 PV carriers are at increased risk for GC.
2.3. Gastric Cancer Risk among Cohorts Comprised of BRCA1 and BRCA2 PV Carriers
Four studies analyzed risk of GC among cohorts comprised of both BRCA1 and BRCA2 PV carriers, with the majority noting increased GC risk in this combined population (Table 3). In a 2004 study by Bermejo et al. [49] among families with at least three generations in the Swedish Family-Cancer Database that met eligibility criteria for BRCA1 or BRCA2 PV testing (n = 130,487), development of GC by age 70 occurred twice as frequently in families with breast and ovarian cancer (1.88%, 95% CI 1.05–3.12%) compared to the general population (0.92%). Similarly, in a 2019 study in Korea among first- and second-degree relatives of high risk breast cancer patients (n = 2555, including 377 BRCA1/2 PV carriers), the proportional incidence of a family history of GC was higher among BRCA1/2 PV carriers compared to patients without a BRCA1/2 PV (13.8% vs. 7.4%; OR 1.666, 95% CI 1.183–2.345) [50]. Most recently, in a 2020 study using data from The Cancer Genome Atlas (TCGA) and a Chinese academic center, the proportional incidence of GC among male BRCA1/2 PV carriers with tumors (n = 294) was higher than that among non-BRCA1/2 carrying males with tumors (n = 4577) (11.9% vs. 5.5%, p < 0.001) in a subgroup analysis of the TCGA population [21]. On the other hand, in a 2012 study of 238 high-risk breast cancer patients in Korea (including 49 BRCA1/2 PV carriers), the proportional incidence of a family history of GC did not vary between patients without BRCA1/2 PVs and BRCA1/2 PV carriers (24.7% vs. 20.5%; RR 0.947, 95% CI 0.822–1.091) [51]. Altogether, three of the four studies noted an increased risk of GC in this combined population of BRCA1/2 carriers, further substantiating germline BRCA1/2 PVs as a risk factor for GC.
Table 3.
Select Studies Reporting Gastric Cancer Risk in Combined Populations of BRCA1 and BRCA2 Carriers.
| Author | Year | Population Location | Patient Population | Comparator Cohort | Risk Estimates | Gastric Cancer Risk Increased? |
|---|---|---|---|---|---|---|
| Gastric Cancer Risk in BRCA1/2 PV Carriers | ||||||
| Bermejo et al. [49] | 2004 | Sweden | 10,359 individuals from families with breast and ovarian cancer | General Population | Incidence: 1.88% (95% CI 1.05–3.12%) vs. 0.92% | Yes |
| Noh et al. [51] | 2012 | Korea | 49 BRCA1/2 PV carriers | 189 high-risk breast cancer patients without BRCA1/2 PVs | Proportional incidence of a family history of GC: 24.7% for comparator cohort vs. 20.5% for BRCA1/2 PV carriers; RR 0.947, 95% CI 0.822–1.091 | No |
| Kim et al. [50] | 2019 | Korea | 377 BRCA1/2 PV carriers | 2178 high-risk breast cancer patients without BRCA1/2 PVs | Proportional incidence of a family history of GC: 13.8% vs. 7.4%; OR 1.666, 95% CI 1.183–2.345 | Yes |
| Sun et al. [21] | 2020 | Multinational (>10 countries) | 294 male BRCA1/2 PV carriers with tumors | 4577 male patients with tumors who were not carriers of BRCA1/2 PVs | Proportional incidence of GC: 11.9% vs. 5.5%, p < 0.001 | Yes |
Abbreviations: CI—confidence interval; GC—gastric cancer; OR—odds ratio; PV—pathogenic variant; RR—relative risk.
3. BRCA1/2-Associated Gastric Cancer
3.1. Classical Pathways of Gastric Carcinogenesis
The two major subtypes of gastric adenocarcinoma are the intestinal type and diffuse type, and these two subtypes have different mechanisms of carcinogenesis [52,53]. The Correa cascade is the classic mechanism for the development of intestinal type GC. Typically, in this pathway GC evolves from long-term gastric inflammation due to chronic or atrophic gastritis leading to intestinal metaplasia, followed by dysplasia, and eventually carcinoma [52]. H. pylori is a well-established pathogen that can promote progression through this pathway via promotion of chronic gastritis [54]. Another pathogen associated with gastric carcinogenesis is the Epstein–Barr virus [55], which has been associated with approximately 9% of GCs, including both intestinal and diffuse type [56]. In contrast to intestinal type GC, diffuse GC (DGC) occurs independent of the Correa cascade. DGC is poorly differentiated with a lack of intercellular adhesion and often histologically characterized by signet-ring cells [53].
Several studies have reported the presence of germline BRCA1 and BRCA2 mutations in cases of GC [22,29,31,57,58,59], as well as others that noted somatic BRCA1/2 mutations [22,30]. To our knowledge, there are no reports investigating a mechanistic role of BRCA1/2 mutations in GC pathogenesis. Thus, which of these classical pathways of GC pathogenesis might be relevant to BRCA1/2-associated GC remains to be determined.
3.2. Homologous Recombination Deficiency in Gastric Cancer
There is increasing evidence that GCs may be enriched for mutations in genes associated with HR [29,30,31]. A 2015 study by Alexandrov et al. reported that 7–12% of GCs assessed from TCGA, International Cancer Genome Consortium, and previously published articles, had a tumor mutation signature associated with HR deficiency [30]. Importantly, the authors noted a GC with a somatic BRCA2 mutation that presented a HR deficient tumor mutation signature [30]. Furthermore, germline mutations in BRCA1/2 HR pathway interaction partners, PALB2 and RAD51C, were also shown to confer a tumor mutation signature enriched for HR deficiency in four cases of GC [29]. While this same study noted three cases of GC with a germline BRCA1 mutation, the tumor mutation signatures were not reported [29]. Lastly, a study looking at 207 Japanese patients with GC noted a high frequency of germline mutations in HR associated genes [31]. Of the 207 patients, 10.6% harbored a BRCA2 mutation, 9.7% with an ATM mutation, 4.3% with a PALB2 mutation, 4.3% with a RAD50 mutation, as well as 3.9% with a BRCA1 mutation [31].
3.3. Prognostic Value of BRCA1/2 Expression in Gastric Cancer
Three different groups independently published similar findings in 2013 looking at BRCA1 protein expression via immunohistochemistry as a potential prognostic indicator in GC [32,33,34]. Of note, these studies did not check for the presence of germline or somatic BRCA1 mutations. Chen et al., evaluated BRCA1 protein expression in surgically resected GC tissue from 637 patients [32]. The investigation found that lack of BRCA1 expression was associated with poor tumor differentiation, advanced-stage disease, and decreased overall survival (OS) compared to patients with BRCA1 expression in their GC [32]. Zhang and colleagues described similar findings, reporting that of 125 GC tissue samples 21.4% showed a loss of BRCA1 expression [33]. Importantly, the loss of BRCA1 expression was found to be significantly associated with DGC, a higher tumor grade, advanced clinical stage, and a lower 2-year survival rate compared to patients with positive BRCA1 expression [33]. The findings of the previous two groups were further corroborated by Kim et al., who demonstrated that the tumors of patients with sporadic GC and low to negative BRCA1 nuclear expression were associated with advanced-stage disease and perineural invasion [34]. Furthermore, disease-free survival (DFS) of patients with low to negative BRCA1 expression was significantly decreased compared to patients with high expression [34]. Converse to these findings, a study by Wang et al. reported that GC tumors with high nuclear expression of BRCA1 were associated with a worse OS [35]. However, high cytoplasmic expression was associated with a better OS [35]. These findings suggests that BRCA1 expression and protein localization may be an informative marker of GC prognosis. Nonetheless, future studies to validate such a hypothesis are needed.
Only a few studies have evaluated BRCA2 protein expression as a prognostic marker in GC. Wang et. al., detected BRCA2 expression exclusively in the cytoplasm of both normal and GC tumor cells [35]. Importantly, GC tumors with high expression of cytoplasmic BRCA2 were associated with a better OS [35]. A more recent study in 2022 was able to detect both cytoplasmic and nuclear BRCA2 protein expression in GC tumor tissues [36]. The investigators showed that positive nuclear BRCA2 expression was correlated with DGC and a lower OS [36]. Correlations for cytoplasmic expression of BRCA2 were not reported [36]. Given the limited number of studies, additional investigations are needed to determine if BRCA2 protein expression and its cellular localization has prognostic value in GC.
3.4. Potential Therapeutic Interventions in BRCA1/2 Associated Gastric Cancer
The emerging evidence of HR deficiency and altered expression of BRCA1/2 proteins in GC suggests a potential role for the employment of DNA damaging chemotherapeutic agents in BRCA1/2-associated GC. Such approaches have been shown to be efficacious in treatment of breast and ovarian cancers of BRCA1/2 carriers [60,61,62,63,64,65,66], as well pancreatic cancers with an inactivation of BRCA1, BRCA2, or PALB2 and an HR deficiency tumor mutation signature [67].
Regarding BRCA1 expression, Chen et al. found that patients with GC and negative BRCA1 expression saw a greater OS benefit compared to patients with positive BRCA1 expression when administered platinum-based adjuvant chemotherapy [32]. Kim et al., demonstrated that patients with stage III GC and negative BRCA1 nuclear expression saw a significant increase in OS and DFS when given a fluoropyrimidine combined with platinum-based adjuvant chemotherapy compared to patients with positive BRCA1 nuclear expression [34]. Interestingly, the combined fluoropyrimidine and platinum-based adjuvant treatment seemed to confer a better OS and DFS than fluoropyrimidine alone in the stage III patients with negative BRCA1 nuclear expression [34]. This perhaps further implicates a role for platinum-based DNA damaging agents in GC when BRCA1 expression is reduced or absent. Lastly, Moiseyenko et al. showed that GC patients with tumor tissue samples that had low BRCA1 transcript levels had a significantly higher overall response and clinical benefit compared to those with high BRCA1 transcript levels when administered a combination of platinum-based agents, fluoropyrimidines, and anthracyclines [37]. However, this study did not find a significant improvement in PFS or OS in this cohort [37]. Separate from the transcript analyses, the investigators described two patients with a BRCA1 germline PV and loss of heterozygosity (LOH) in GC tumor samples [37]. The authors note that these two patients both appeared to show an enhanced sensitivity to platinum-based chemotherapy by means of tumor size reduction [37]. Taken together, this evidence begins to implicate a potential chemotherapeutic role for DNA damaging agents such as platinum-based compounds when BRCA1 expression is altered in GC. Of note, we were unable to identify similar studies of BRCA2 expression and response to chemotherapy in the context of GC.
While the studies presented here suggest improved responsiveness of BRCA1/2-associated GCs to platinum-based intervention, other DNA damaging agents such as PARP inhibitors (PARPi) may also prove useful as PARPi have shown selective killing of BRCA1/2 mutant tumor cells [68,69]. Additionally, clinical trials have shown promise in treatment of BRCA1/2 PV carriers in other cancers [61,62,63,64]. Given the emerging risk of GC in germline BRCA1/2 PV carriers, future studies and clinical trials are crucial to more clearly determine the chemotherapeutic agents that are the most efficacious in the treatment of GC when BRCA1/2 expression is altered and/or in the presence of germline BRCA1/2 PVs. Furthermore, such studies involving germline BRCA1/2 PV carriers should also take into consideration locus-specific LOH status as a study by Maxwell et al. indicated that the absence of locus-specific LOH may predict primary resistance to DNA damaging agents [70]
4. Gastric Surveillance Considerations in BRCA1/2 Carriers
4.1. Non-Gastric Surveillance in BRCA1/2 Carriers
Before pondering the potential for GC surveillance in BRCA1/2 PV carriers, it is relevant to first review the risk management recommendations for other malignancies associated with BRCA1/2 PVs, including breast, ovarian, prostate, and pancreatic cancer [71,72]. For breast cancer surveillance, National Comprehensive Cancer Network (NCCN) guidelines recommend that female BRCA1/2 PV carriers are taught breast awareness at age 18 and undergo clinical breast exams every 6–12 months starting at age 25, annual breast magnetic resonance imaging (MRI) from age 25–30, and annual mammogram and breast MRI from age 30–75, supplemented with discussion of the option of risk-reducing mastectomy [71]. Male BRCA1/2 PV carriers are recommended to undergo annual breast exams starting at age 35, with consideration of annual mammogram starting at age 50 for men with gynecomastia [71]. For risk reduction of ovarian cancer in this population, NCCN guidelines recommend risk-reducing salpingo-oophorectomy (RRSO), typically between age 35–40 and after completion of childbearing, noting that it is reasonable to delay RRSO until age 40–45 among BRCA2 PV carriers [71]. For prostate cancer surveillance, NCCN guidelines recommend prostate cancer screening starting at age 40 for BRCA2 PV carriers, and that BRCA1 PV carriers begin shared decision-making surrounding prostate-specific antigen screening at age 40 with consideration of surveillance at annual intervals [72]. Last, based on growing evidence that BRCA1/2 PVs increase risk of pancreatic cancer, guidelines have recommended pancreatic cancer surveillance with endoscopic ultrasound (EUS) or MRI for those carriers with a first- or second-degree family member with pancreatic cancer [71,73]. However, recent data has explored pancreatic cancer surveillance in BRCA1/2 carriers without a family history of pancreatic cancer [74,75], and newly released American Society for Gastrointestinal Endoscopy (ASGE) guidelines now recommend that all BRCA1/2 PV carriers undergo pancreatic cancer surveillance starting at age 50 [76].
4.2. Gastric Surveillance in Other Hereditary Gastric Cancer Risk Syndromes
A number of hereditary cancer predisposition syndromes are associated with elevated risk of GC, which has led to a multitude of syndrome-specific guidelines for GC surveillance [77]. Patients with hereditary diffuse gastric cancer syndrome (HDGC) due to a PV in CDH1 or CTNNA1 have the highest lifetime cumulative risk of GC [57,78,79]. In HDGC, if gastrectomy is declined or delayed, guidelines recommend annual upper endoscopy with targeted and non-targeted gastric biopsies [78]. Patients with Lynch syndrome, who have a lifetime risk of GC of up to 9%, are recommended to undergo upper endoscopy starting at age 30–40, with biopsies of the antrum and body performed to rule out H. pylori and gastric intestinal metaplasia, followed by repeat upper endoscopy every 2–4 years thereafter [80]. Likewise, patients with familial adenomatous polyposis (FAP) are recommended to undergo upper endoscopy with ampulla visualization starting at age 20–25, with the interval of subsequent studies based on the Spigelman stage of duodenal polyposis or gastric pathology, which can range from 3 months to 5 years [80]. For patients with gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS), who have an estimated risk of developing intestinal-type gastric adenocarcinoma of 12–25%, expert opinion recommends annual upper endoscopy starting at age 15 and consideration of risk-reducing total gastrectomy in their 30s [80,81,82]. In the setting of Peutz-Jeghers syndrome, which carries a 29% risk of GC by age 65, patients are recommended to undergo baseline upper endoscopy at age 8–10 followed by repeat study every 2–3 years, or again at age 18 and every 3 years thereafter if no characteristic polyps are found at baseline [83]. Similarly, patients with juvenile polyposis syndrome, who have a lifetime GC risk of up to 21–30%, are directed to undergo initial upper endoscopy between age 12–15 followed by repeat study every 1–3 years, or again at age 18 and every 1–3 years going forward if no polyps are found at baseline [80,83].
4.3. Gastric Cancer Risk Management in BRCA1/2 Carriers
Despite mounting evidence that GC risk is increased among BRCA1/2 PV carriers, at this time BRCA1/2 guidelines do not recommend any specific surveillance for GC. Discussion of the potential merits of surveillance and other strategies for GC risk management is certainly warranted by the organizations that develop and implement BRCA1/2 surveillance guidelines (i.e., NCCN), and GC risk should be addressed in future guideline iterations. However, until that time, we favor the following strategy for GC risk management in BRCA1/2 PV carriers:
H. pylori testing and treatment—It currently remains unknown whether H. pylori plays a role in gastric carcinogenesis among BRCA1/2 PV carriers, and it also remains uncertain whether BRCA1/2 PV carriers have increased prevalence of H. pylori. However, H. pylori is a well-documented GC risk factor that is treatable, and as with other hereditary GC risk syndromes, such as Lynch syndrome, we believe that it would be reasonable to test for H. pylori (either non-invasively or via gastric biopsy) among BRCA1/2 PV carriers at least one-time, with treatment and confirmation of eradication if H. pylori is present.
Perform careful upper endoscopy concurrently when endoscopic ultrasound is performed for pancreatic cancer surveillance—As current ASGE guidelines recommend that all BRCA1/2 PV carriers initiate pancreatic cancer surveillance at age 50, it is likely that an increasing number of BRCA1/2 PV carriers will be undergoing EUS for pancreatic cancer surveillance [76]. We believe that if a BRCA1/2 PV carrier is already undergoing an EUS for pancreatic cancer surveillance, a standard upper endoscopy should also be performed concurrently with careful inspection for upper GI neoplasia.
Low threshold for upper endoscopy for upper GI symptom investigation—In other hereditary syndromes associated with increased GC risk, the threshold of most clinicians for performing upper endoscopy for evaluation of upper GI symptoms is lower than for the general population. We would recommend that the threshold for upper endoscopy in BRCA1/2 PV carriers with upper GI symptoms be similarly low.
Consider regular gastric surveillance in BRCA1/2 PV carriers with a family history of GC—If a BRCA1/2 PV carrier has a family history of GC in a carrier of the BRCA1/2 PV, we believe that a baseline surveillance upper endoscopy can be offered at age 50, or 10 years prior to the youngest GC diagnosis, and then can be repeated at an interval of 3 years.
While the above considerations are based on our professional opinion, further study and expert discussion is urgently warranted to construct an optimal, evidence-based risk management strategy for GC risk among BRCA1/2 PV carriers, particularly as the incidence of GC in this population will likely increase over time as improvements in the detection and treatment of other at-risk malignancies (i.e., breast, ovarian, prostate, pancreatic) prolongs the overall lifespan of this cohort.
5. Conclusions
A growing body of evidence indicates that risk of GC is increased among BRCA2 PV carriers, and likely also among BRCA1 PV carriers. Furthermore, increasing evidence implicates a potential role of HR associated genes (e.g., BRCA1/2) and their altered expression in GC pathogenesis, which may have important prognostic and therapeutic implications. Moreover, the strength of the data published to date warrants that the organizations charged with developing cancer surveillance guidelines consider providing an evidence-based risk management strategy for GC among BRCA1/2 PV carriers. Altogether, the emerging clinical evidence and remaining questions surrounding pathogenesis and optimal risk management strategies make GC among BRCA1/2 PV carriers an intriguing area for further research.
Author Contributions
Conceptualization, K.H.B., B.A.N., B.W.K. and K.N.M. Writing—original draft preparation, K.H.B. and B.A.N. Writing—review and editing, B.W.K. and K.N.M. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no relevant conflict of interest. BWK discloses research support from Epigenomics, Freenome, Guardant Health, Immunovia, Janssen Pharmaceuticals, and Universal Diagnostics, as well as non-funded research collaborations with Ambry, Myriad, GeneDx, and Invitae.
Funding Statement
This research was funded by DeGregorio Family Foundation Grant Award (BWK) and the Basser Center Men and BRCA Program (KNM and BWK).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ackerson S.M., Romney C., Schuck P.L., Stewart J.A. To Join or Not to Join: Decision Points Along the Pathway to Double-Strand Break Repair vs. Chromosome End Protection. Front. Cell Dev. Biol. 2021;9:708763. doi: 10.3389/fcell.2021.708763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ranjha L., Howard S.M., Cejka P. Main steps in DNA double-strand break repair: An introduction to homologous recombination and related processes. Chromosoma. 2018;127:187–214. doi: 10.1007/s00412-017-0658-1. [DOI] [PubMed] [Google Scholar]
- 3.Stinson B.M., Moreno A.T., Walter J.C., Loparo J.L. A Mechanism to Minimize Errors during Non-homologous End Joining. Mol. Cell. 2020;77:1080–1091. doi: 10.1016/j.molcel.2019.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang H.H.Y., Pannunzio N.R., Adachi N., Lieber M.R. Non-homologous DNA end joining and alternative pathways to double-strand break repair. Nat. Rev. Mol. Cell Biol. 2017;18:495–506. doi: 10.1038/nrm.2017.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prakash R., Zhang Y., Feng W., Jasin M. Homologous recombination and human health: The roles of BRCA1, BRCA2, and associated proteins. Cold Spring Harb. Perspect. Biol. 2015;7:a016600. doi: 10.1101/cshperspect.a016600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powell S.N., Kachnic L.A. Roles of BRCA1 and BRCA2 in homologous recombination, DNA replication fidelity and the cellular response to ionizing radiation. Oncogene. 2003;22:5784–5791. doi: 10.1038/sj.onc.1206678. [DOI] [PubMed] [Google Scholar]
- 7.Walsh C.S. Two decades beyond BRCA1/2: Homologous recombination, hereditary cancer risk and a target for ovarian cancer therapy. Gynecol. Oncol. 2015;137:343–350. doi: 10.1016/j.ygyno.2015.02.017. [DOI] [PubMed] [Google Scholar]
- 8.Snouwaert J.N., Gowen L.C., Latour A.M., Mohn A.R., Xiao A., DiBiase L., Koller B.H. BRCA1 deficient embryonic stem cells display a decreased homologous recombination frequency and an increased frequency of non-homologous recombination that is corrected by expression of a BRCA1 transgene. Oncogene. 1999;18:7900–7907. doi: 10.1038/sj.onc.1203334. [DOI] [PubMed] [Google Scholar]
- 9.Holloman W.K. Unraveling the mechanism of BRCA2 in homologous recombination. Nat. Struct. Mol. Biol. 2011;18:748–754. doi: 10.1038/nsmb.2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Venkitaraman A.R. Functions of BRCA1 and BRCA2 in the biological response to DNA damage. J. Cell Sci. 2001;114:3591–3598. doi: 10.1242/jcs.114.20.3591. [DOI] [PubMed] [Google Scholar]
- 11.Venkitaraman A.R. Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell. 2002;108:171–182. doi: 10.1016/S0092-8674(02)00615-3. [DOI] [PubMed] [Google Scholar]
- 12.Miki Y., Swensen J., Shattuck-Eidens D., Futreal P.A., Harshman K., Tavtigian S., Liu Q., Cochran C., Bennett L.M., Ding W., et al. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science. 1994;266:66–71. doi: 10.1126/science.7545954. [DOI] [PubMed] [Google Scholar]
- 13.Wooster R., Bignell G., Lancaster J., Swift S., Seal S., Mangion J., Collins N., Gregory S., Gumbs C., Micklem G. Identification of the breast cancer susceptibility gene BRCA2. Nature. 1995;378:789–792. doi: 10.1038/378789a0. [DOI] [PubMed] [Google Scholar]
- 14.Kuchenbaecker K.B., Hopper J.L., Barnes D.R., Phillips K.A., Mooij T.M., Roos-Blom M.J., Jervis S., van Leeuwen F.E., Milne R.L., Andrieu N., et al. Risks of Breast, Ovarian, and Contralateral Breast Cancer for BRCA1 and BRCA2 Mutation Carriers. J. Am. Med. Assoc. 2017;317:2402–2416. doi: 10.1001/jama.2017.7112. [DOI] [PubMed] [Google Scholar]
- 15.Li S., Silvestri V., Leslie G., Rebbeck T.R., Neuhausen S.L., Hopper J.L., Nielsen H.R., Lee A., Yang X., McGuffog L., et al. Cancer Risks Associated with BRCA1 and BRCA2 Pathogenic Variants. J. Clin. Oncol. 2022;40:1529–1541. doi: 10.1200/JCO.21.02112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Momozawa Y., Sasai R., Usui Y., Shiraishi K., Iwasaki Y., Taniyama Y., Parsons M.T., Mizukami K., Sekine Y., Hirata M., et al. Expansion of Cancer Risk Profile for BRCA1 and BRCA2 Pathogenic Variants. JAMA Oncol. 2022;8:871–878. doi: 10.1001/jamaoncol.2022.0476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dullens B., de Putter R., Lambertini M., Toss A., Han S., Van Nieuwenhuysen E., Van Gorp T., Vanderstichele A., Van Ongeval C., Keupers M., et al. Cancer Surveillance in Healthy Carriers of Germline Pathogenic Variants in BRCA1/2: A Review of Secondary Prevention Guidelines. J. Oncol. 2020;2020:9873954. doi: 10.1155/2020/9873954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aslanian H.R., Lee J.H., Canto M.I. AGA Clinical Practice Update on Pancreas Cancer Screening in High-Risk Individuals: Expert Review. Gastroenterology. 2020;159:358–362. doi: 10.1053/j.gastro.2020.03.088. [DOI] [PubMed] [Google Scholar]
- 19.Bancroft E.K., Page E.C., Castro E., Lilja H., Vickers A., Sjoberg D., Assel M., Foster C.S., Mitchell G., Drew K., et al. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: Results from the initial screening round of the IMPACT study. Eur. Urol. 2014;66:489–499. doi: 10.1016/j.eururo.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Segal N., Ber Y., Benjaminov O., Tamir S., Yakimov M., Kedar I., Rosenbaum E., Sela S., Ozalvo R., Shavit-Grievink L., et al. Imaging-based prostate cancer screening among BRCA mutation carriers—Results from the first round of screening. Ann. Oncol. 2020;31:1545–1552. doi: 10.1016/j.annonc.2020.06.025. [DOI] [PubMed] [Google Scholar]
- 21.Sun P., Li Y., Chao X., Li J., Luo R., Mei L., He J. Clinical characteristics and prognostic implications of BRCA-associated tumors in males: A pan-tumor survey. BMC Cancer. 2020;20:994. doi: 10.1186/s12885-020-07481-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ichikawa H., Wakai T., Nagahashi M., Shimada Y., Hanyu T., Kanu Y., Muneoka Y., Ishikawa T., Takizawa K., Tajima Y., et al. Pathogenic germline BRCA1/2 mutations and familial predisposition to gastric cancer. JCO Precis. Oncol. 2018;2:18–00097. doi: 10.1200/PO.18.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moran A., O’Hara C., Khan S., Shack L., Woodward E., Maher E.R., Lalloo F., Evans D.G. Risk of cancer other than breast or ovarian in individuals with BRCA1 and BRCA2 mutations. Fam. Cancer. 2012;11:235–242. doi: 10.1007/s10689-011-9506-2. [DOI] [PubMed] [Google Scholar]
- 24.Jakubowska A., Nej K., Huzarski T., Scott R.J., Lubinski J. BRCA2 gene mutations in families with aggregations of breast and stomach cancers. Br. J. Cancer. 2002;87:888–891. doi: 10.1038/sj.bjc.6600562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Figer A., Irmin L., Geva R., Flex D., Sulkes J., Sulkes A., Friedman E. The rate of the 6174delT founder Jewish mutation in BRCA2 in patients with non-colonic gastrointestinal tract tumours in Israel. Br. J. Cancer. 2001;84:478–481. doi: 10.1054/bjoc.2000.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schlebusch C.M., Dreyer G., Sluiter M.D., Yawitch T.M., van den Berg H.J., van Rensburg E.J. Cancer prevalence in 129 breast-ovarian cancer families tested for BRCA1 and BRCA2 mutations. S. Afr. Med. J. 2010;100:113–117. doi: 10.7196/SAMJ.3235. [DOI] [PubMed] [Google Scholar]
- 27.Johannsson O., Loman N., Moller T., Kristoffersson U., Borg A., Olsson H. Incidence of malignant tumours in relatives of BRCA1 and BRCA2 germline mutation carriers. Eur. J. Cancer. 1999;35:1248–1257. doi: 10.1016/S0959-8049(99)00135-5. [DOI] [PubMed] [Google Scholar]
- 28.Breast Cancer Linkage Consortium Cancer risks in BRCA2 mutation carriers. J. Natl. Cancer Inst. 1999;91:1310–1316. doi: 10.1093/jnci/91.15.1310. [DOI] [PubMed] [Google Scholar]
- 29.Sahasrabudhe R., Lott P., Bohorquez M., Toal T., Estrada A.P., Suarez J.J., Brea-Fernandez A., Cameselle-Teijeiro J., Pinto C., Ramos I., et al. Germline Mutations in PALB2, BRCA1, and RAD51C, Which Regulate DNA Recombination Repair, in Patients with Gastric Cancer. Gastroenterology. 2017;152:983–986.e6. doi: 10.1053/j.gastro.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alexandrov L.B., Nik-Zainal S., Siu H.C., Leung S.Y., Stratton M.R. A mutational signature in gastric cancer suggests therapeutic strategies. Nat. Commun. 2015;6:8683. doi: 10.1038/ncomms9683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ichikawa H., Nagahashi M., Shimada Y., Hanyu T., Ishikawa T., Kameyama H., Kobayashi T., Sakata J., Yabusaki H., Nakagawa S., et al. Actionable gene-based classification toward precision medicine in gastric cancer. Genome Med. 2017;9:93. doi: 10.1186/s13073-017-0484-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen W., Wang J., Li X., Li J., Zhou L., Qiu T., Zhang M., Liu P. Prognostic significance of BRCA1 expression in gastric cancer. Med. Oncol. 2013;30:423. doi: 10.1007/s12032-012-0423-5. [DOI] [PubMed] [Google Scholar]
- 33.Zhang Z.Z., Liu Y.J., Yin X.L., Zhan P., Gu Y., Ni X.Z. Loss of BRCA1 expression leads to worse survival in patients with gastric carcinoma. World J. Gastroenterol. 2013;19:1968–1974. doi: 10.3748/wjg.v19.i12.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim J.W., Cho H.J., Kim M., Lee K.H., Kim M.A., Han S.W., Oh D.Y., Lee H.J., Im S.A., Kim T.Y., et al. Differing effects of adjuvant chemotherapy according to BRCA1 nuclear expression in gastric cancer. Cancer Chemother. Pharmacol. 2013;71:1435–1443. doi: 10.1007/s00280-013-2141-x. [DOI] [PubMed] [Google Scholar]
- 35.Wang G.H., Zhao C.M., Huang Y., Wang W., Zhang S., Wang X. BRCA1 and BRCA2 expression patterns and prognostic significance in digestive system cancers. Hum. Pathol. 2018;71:135–144. doi: 10.1016/j.humpath.2017.10.032. [DOI] [PubMed] [Google Scholar]
- 36.Pádua J.D.B., Mariano C.F.A., Fabro A.T., Tirapelli D.P.D.C., Sankarankutty A.K., Dos Santos J.S., Brunaldi M.O. Prognostic Value of the Immunohistochemical Expression of RAD51 and BRCA2 in Gastric Adenocarcinoma. J. Histochem. Cytochem. 2022;70:199–210. doi: 10.1369/00221554211065834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moiseyenko V.M., Volkov N.M., Suspistin E.N., Yanus G.A., Iyevleva A.G., Kuligina E.S., Togo A.V., Kornilov A.V., Ivantsov A.O., Imyanitov E.N. Evidence for predictive role of BRCA1 and bTUBIII in gastric cancer. Med. Oncol. 2013;30:545. doi: 10.1007/s12032-013-0545-4. [DOI] [PubMed] [Google Scholar]
- 38.Risch H.A., McLaughlin J.R., Cole D.E., Rosen B., Bradley L., Kwan E., Jack E., Vesprini D.J., Kuperstein G., Abrahamson J.L., et al. Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am. J. Hum. Genet. 2001;68:700–710. doi: 10.1086/318787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brose M.S., Rebbeck T.R., Calzone K.A., Stopfer J.E., Nathanson K.L., Weber B.L. Cancer risk estimates for BRCA1 mutation carriers identified in a risk evaluation program. J. Natl. Cancer Inst. 2002;94:1365–1372. doi: 10.1093/jnci/94.18.1365. [DOI] [PubMed] [Google Scholar]
- 40.Sung H., Ferlay J., Siegel R., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 41.Ford D., Easton D.F., Bishop D.T., Narod S.A., Goldgar D.E. Risks of cancer in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Lancet. 1994;343:692–695. doi: 10.1016/S0140-6736(94)91578-4. [DOI] [PubMed] [Google Scholar]
- 42.Thompson D., Easton D.F., Breast Cancer Linkage Consortium Cancer Incidence in BRCA1 mutation carriers. J. Natl. Cancer Inst. 2002;94:1358–1365. doi: 10.1093/jnci/94.18.1358. [DOI] [PubMed] [Google Scholar]
- 43.Mersch J., Jackson M.A., Park M., Nebgen D., Peterson S.K., Singletary C., Arun B.K., Litton J.K. Cancers associated with BRCA1 and BRCA2 mutations other than breast and ovarian. Cancer. 2015;121:269–275. doi: 10.1002/cncr.29041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ławniczak M., Jakubowska A., Bialek A., Lubinski J., Jaworska-Bieniek K., Kaczmarek K., Starzynska T. BRCA1 founder mutations do not contribute to increased risk of gastric cancer in the Polish population. Hered. Cancer Clin. Pract. 2016;14:3. doi: 10.1186/s13053-015-0043-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee Y.C., Lee Y.L., Li C.Y. BRCA Genes and Related Cancers: A Meta-Analysis from Epidemiological Cohort Studies. Medicina. 2021;57:905. doi: 10.3390/medicina57090905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tulinius H., Olafsdottir G.H., Sigvaldason H., Arason A., Barkardottir R.B., Eglisson V., Ogmundsdottir H.M., Tryggvadottir L., Gudlaugsdottir S., Eyfjord J.E. The effect of a single BRCA2 mutation on cancer in Iceland. J. Med. Genet. 2002;39:457–462. doi: 10.1136/jmg.39.7.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jakubowska A., Scott R., Menkiszak J., Gronwald J., Byrski T., Huzarski T., Gorski B., Cybulski C., Debniak T., Kowalska E., et al. A high frequency of BRCA2 gene mutations in Polish families with ovarian and stomach cancer. Eur. J. Hum. Genet. 2003;11:955–958. doi: 10.1038/sj.ejhg.5201064. [DOI] [PubMed] [Google Scholar]
- 48.van Asperen C.J., Brohet R.M., Meijers-Heijboer E.J., Hoogerbrugge N., Verhoef S., Vasen H.F., Ausems M.G., Menko F.H., Gomez Garcia E.B., Klijn J.G., et al. Cancer risks in BRCA2 families: Estimates for sites other than breast and ovary. J. Med. Genet. 2005;42:711–719. doi: 10.1136/jmg.2004.028829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bermejo J.L., Hemminki K. Risk of cancer at sites other than the breast in Swedish families eligible for BRCA1 or BRCA2 mutation testing. Ann. Oncol. 2004;15:1834–1841. doi: 10.1093/annonc/mdh474. [DOI] [PubMed] [Google Scholar]
- 50.Kim H., Choi D.H., Park W., Im Y.H., Ahn J.S., Park Y.H., Nam S.J., Kim S.W., Lee J.E., Yu J.H., et al. The association between non-breast and ovary cancers and BRCA mutation in first- and second-degree relatives of high-risk breast cancer patients: A large-scale study of Koreans. Hered. Cancer Clin. Pract. 2019;17:1. doi: 10.1186/s13053-018-0103-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Noh J.M., Choi D.H., Baek H., Nam S.J., Lee J.E., Kim J.W., Ki C.S., Park W., Huh S.J. Associations between BRCA Mutations in High-Risk Breast Cancer Patients and Familial Cancers Other than Breast or Ovary. J. Breast Cancer. 2012;15:283–287. doi: 10.4048/jbc.2012.15.3.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Correa P. Human gastric carcinogenesis: A multistep and multifactorial process—First American Cancer Society Award Lecture on Cancer Epidemiology and Prevention. Cancer Res. 1992;52:6735–6740. [PubMed] [Google Scholar]
- 53.Ansari S., Gantuya B., Tuan V.P., Yamaoka Y. Diffuse gastric cancer: A summary of analogous contributing factors for its molecular pathogenicity. Int. J. Mol. Sci. 2018;19:2424. doi: 10.3390/ijms19082424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Polk D.B., Peek R.M., Jr. Helicobacter pylori: Gastric cancer and beyond. Nat. Rev. Cancer. 2010;10:403–414. doi: 10.1038/nrc2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cancer Genome Research Atlas Network Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tavakoli A., Monavari S.H., Mohammadi F.S., Kiani S.J., Armat S., Farahmand M. Association between Epstein-Barr virus infection and gastric cancer: A systematic review and meta-analysis. BMC Cancer. 2020;20:493. doi: 10.1186/s12885-020-07013-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hansford S., Kaurah P., Li-Chang H., Woo M., Senz J., Pinheiro H., Schrader K.A., Schaeffer D.F., Shumansky K., Zogopoulos G., et al. Hereditary Diffuse Gastric Cancer Syndrome: CDH1 Mutations and Beyond. JAMA Oncol. 2015;1:23–32. doi: 10.1001/jamaoncol.2014.168. [DOI] [PubMed] [Google Scholar]
- 58.Lu C., Xie M., Wendl M.C., Wang J., McLellan M.D., Leiserson M.D., Huang K.L., Wyczalkowski M.A., Jayasinghe R., Banerjee T., et al. Patterns and functional implications of rare germline variants across 12 cancer types. Nat. Commun. 2015;6:10086. doi: 10.1038/ncomms10086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Halpern N., Grinshpun A., Boursi B., Golan T., Margalit O., Aderka D., Friedman E., Laitman Y., Hubert A., Kadouri L., et al. Clinical Characteristics and Prognosis of Gastric Cancer Patients with BRCA 1/2 Germline Mutations: Report of Ten Cases and a Literature Review. Onco Targets Ther. 2020;13:11637–11644. doi: 10.2147/OTT.S276814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Byrski T., Huzarski T., Dent R., Gronwald J., Zuziak D., Cybulski C., Kladny J., Gorski B., Lubinski J., Narod S.A. Response to neoadjuvant therapy with cisplatin in BRCA1-positive breast cancer patients. Breast Cancer Res. Treat. 2009;115:359–363. doi: 10.1007/s10549-008-0128-9. [DOI] [PubMed] [Google Scholar]
- 61.Fong P.C., Boss D.S., Yap T.A., Tutt A., Wu P., Mergui-Roelvink M., Mortimer P., Swaisland H., Lau A., O’Connor M.J., et al. Inhibition of poly (ADP-ribose) polymerase in tumors from BRCA mutation carriers. N. Engl. J. Med. 2009;361:123–134. doi: 10.1056/NEJMoa0900212. [DOI] [PubMed] [Google Scholar]
- 62.Ledermann J., Harter P., Gourley C., Friedlander M., Vergote I., Rustin G., Scott C., Meier W., Shapira-Frommer R., Safra T., et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N. Engl. J. Med. 2012;366:1382–1392. doi: 10.1056/NEJMoa1105535. [DOI] [PubMed] [Google Scholar]
- 63.Sandhu S.K., Schelman W.R., Wilding G., Moreno V., Baird R.D., Miranda S., Hylands L., Riisnaes R., Forster M., Omlin A., et al. The poly (ADP-ribose) polymerase inhibitor niraparib (MK4827) in BRCA mutation carriers and patients with sporadic cancer: A phase 1 dose-escalation trial. Lancet Oncol. 2013;14:882–892. doi: 10.1016/S1470-2045(13)70240-7. [DOI] [PubMed] [Google Scholar]
- 64.Balmaña J., Tung N.M., Isakoff S.J., Grana B., Ryan P.D., Saura C., Lowe E.S., Frewer P., Winer E., Baselga J., et al. Phase I trial of olaparib in combination with cisplatin for the treatment of patients with advanced breast, ovarian and other solid tumors. Ann. Oncol. 2014;25:1656–1663. doi: 10.1093/annonc/mdu187. [DOI] [PubMed] [Google Scholar]
- 65.Pennington K.P., Walsh T., Harrell M.I., Lee M.K., Pennil C.C., Rendi M.H., Thornton A., Norquist B.M., Cadadei S., Nord A.S., et al. Germline and Somatic Mutations in Homologous Recombination Genes Predict Platinum Response and Survival in Ovarian, Fallopian Tube, and Peritoneal Carcinomas. Clin. Cancer Res. 2014;20:764–775. doi: 10.1158/1078-0432.CCR-13-2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Telli M.L., Timms K.M., Reid J., Hennessy B., Mills G.B., Jensen K.C., Szallasi Z., Barry W.T., Winer E.P., Tung N.M., et al. Homologous Recombination Deficiency (HRD) Score Predicts Response to Platinum-Containing Neoadjuvant Chemotherapy in Patients with Triple-Negative Breast Cancer. Clin. Cancer Res. 2016;22:3764–3773. doi: 10.1158/1078-0432.CCR-15-2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Waddell N., Pajic M., Patch A.M., Chang D.K., Kassahn K.S., Bailey P., Johns A.L., Miller D., Nones K., Quek K., et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature. 2015;518:495–501. doi: 10.1038/nature14169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Farmer H., McCabe N., Lord C.J., Tutt A.N., Johnson D.A., Richardson T.B., Santarosa M., Dillon K.J., Hickson I., Knights C., et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–921. doi: 10.1038/nature03445. [DOI] [PubMed] [Google Scholar]
- 69.Bryant H.E., Schultz N., Thomas H.D., Parker K.M., Flower D., Lopez E., Kyle S., Meuth M., Curtin N.J., Helleday T. Specific killing of BRCA2-deficient tumours with inhibitors of poly (ADP-ribose) polymerase. Nature. 2005;434:913–917. doi: 10.1038/nature03443. [DOI] [PubMed] [Google Scholar]
- 70.Maxwell K.N., Wubbenhorst B., Wenz B.M., De Sloover D., Pluta J., Emery L., Barrett A., Kraya A.A., Anastopoulos I.N., Yu S., et al. BRCA locus-specific loss of heterozygosity in germline BRCA1 and BRCA2 carriers. Nat. Commun. 2017;8:319. doi: 10.1038/s41467-017-00388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.National Comprehensive Cancer Network Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic. Version 1.2023—7 September 2022. [(accessed on 1 October 2022)]. Available online: https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf.
- 72.National Comprehensive Cancer Network Prostate Cancer Early Detection. Version 1.2022—16 February 2022. [(accessed on 1 October 2022)]. Available online: https://www.nccn.org/professionals/physician_gls/pdf/prostate_detection.pdf.
- 73.Goggins M., Overbeek K.A., Brand R., Syngal S., Del Chiaro M., Bartsch D.K., Bassi C., Carrato A., Farrell J., Fishman E.K., et al. Management of patients with increased risk for familial pancreatic cancer: Updated recommendations from the International Cancer of the Pancreas Screening (CAPS) Consortium. Gut. 2020;69:7–17. doi: 10.1136/gutjnl-2019-319352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Katona B.W., Long J.M., Ahmad N.A., Attalla S., Bradbury A.R., Carpenter E.L., Clark D.F., Constantino G., Das K.K., Domcheck S.M., et al. EUS-based Pancreatic Cancer Surveillance in BRCA1/BRCA2/PALB2/ATM Carriers without a Family History of Pancreatic Cancer. Cancer Prev. Res. 2021;14:1033–1040. doi: 10.1158/1940-6207.CAPR-21-0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang L., Domchek S.M., Kochman M.L., Katona B.W. Reaching beyond family history as inclusion criteria for pancreatic cancer surveillance in high-risk populations. Genes Cancer. 2022;13:49–51. doi: 10.18632/genesandcancer.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sawhney M.S., Calderwood A.H., Thosani N.C., Rebbeck T.R., Wani S., Canto M.I., Fishman D.S., Golan T., Hidalgo M., Kwon R.S., et al. ASGE guideline on screening for pancreatic cancer in individuals with genetic susceptibility: Summary and recommendations. Gastrointest. Endosc. 2022;95:817–826. doi: 10.1016/j.gie.2021.12.001. [DOI] [PubMed] [Google Scholar]
- 77.Long J.M., Ebrahimzadeh J., Stanich P.P., Katona B.W. Endoscopic Surveillance in Patients with the Highest Risk of Gastric Cancer: Challenges and Solutions. Cancer Manag. Res. 2022;14:2953–2969. doi: 10.2147/CMAR.S277898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Blair V.R., McLeod M., Carneiro F., Coit D.G., D’Addario J.L., van Dieren J.M., Harris K.L., Hoogerbrugge N., Oliveira C., van der Post R.S., et al. Hereditary diffuse gastric cancer: Updated clinical practice guidelines. Lancet Oncol. 2020;21:e386–e397. doi: 10.1016/S1470-2045(20)30219-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Coudert M., Drouet Y., Delhomelle H., Svrcek M., Benusiglio P.R., Coulet F., Clark D.F., Katona B.W., van Hest L.P., van der Kolk L.E., et al. First estimates of diffuse gastric cancer risks for carriers of CTNNA1 germline pathogenic variants. J. Med. Genet. 2022;59:1189–1195. doi: 10.1136/jmg-2022-108740. [DOI] [PubMed] [Google Scholar]
- 80.National Comprehensive Cancer Network Genetic/Familial High-Risk Assessment: Colorectal. Version 1.2022—8 June 2022. [(accessed on 1 October 2022)]. Available online: https://www.nccn.org/professionals/physician_gls/pdf/genetics_colon.pdf.
- 81.Foretová L., Navratilova M., Svoboda M., Grell P., Nemec L., Sirotek L., Obermannova R., Novotny I., Sachlova M., Fabian P., et al. GAPPS—Gastric Adenocarcinoma and Proximal Polyposis of the Stomach Syndrome in 8 Families Tested at Masaryk Memorial Cancer Institute—Prevention and Prophylactic Gastrectomies. Klin. Onkol. 2019;32:109–117. doi: 10.14735/amko2019S109. [DOI] [PubMed] [Google Scholar]
- 82.Worthley D.L., Phillips K.D., Wayte N., Schrader K.A., Healey S., Kaurah P., Shulkes A., Grimpen F., Clouston A., Moore D., et al. Gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS): A new autosomal dominant syndrome. Gut. 2012;61:774–779. doi: 10.1136/gutjnl-2011-300348. [DOI] [PubMed] [Google Scholar]
- 83.Boland C.R., Idos G.E., Durno C., Giardiello F.M., Anderson J.C., Burke C.A., Dominitz J.A., Gross S., Gupta S., Jacobson B.C., et al. Diagnosis and Management of Cancer Risk in the Gastrointestinal Hamartomatous Polyposis Syndromes: Recommendations from the US Multi-Society Task Force on Colorectal Cancer. Am. J. Gastroenterol. 2022;117:846–864. doi: 10.14309/ajg.0000000000001755. [DOI] [PubMed] [Google Scholar]