Abstract
Background
The deadly COVID-19 pandemic has swept the globe since December 2019. Due to the significant risk of infection, frontline health workers had to use Personal Protective Equipment and hand hygiene products, to help prevent transmission of infection. The present study aims to compare the adverse skin responses between healthcare workers (HCW) and non-healthcare workers (NHCW).
Materials and methods
A descriptive, cross-sectional study of HCW and NHCW throughout the country wa executed. A self-structured questionnaire was utilized to gather data from 404 HCWs and 826 NHCWs during a two-month period using multistage sampling. STATA (v16) was used to analyse the data.
Results
41.87% of the study participants experienced adverse skin reactions, which were more prevalent amongs HCW (65.10%) than NHCW (30.51%). The most frequently reported skin condition was skin dryness (34.39%), followed by skin peeling (11.71%). Users of alcohol-based hand sanitizers (ABHS) were more likely to get itch (8.13%), whereas soap water users were more likely to suffer from skin peeling (35.74%) and rash (7.46%). There was a significant (p < 0.001) association between occupation and adverse skin responses, with HCW being 3.5 times more likely to have adverse skin manifestations than NHCW.
Conclusion
The research showed that healthcare workers were at a greater risk to developing skin reactions than the overall population with frequent use of hand hygiene measures being a significant risk factor.
Keywords: Hand wash, Hand hygiene, Skin problem, Skin reaction, Sanitizer
Hand wash, Hand Hygiene, Skin problem, Skin Reaction, Sanitizer.
1. Introduction
COVID-19 was declared a global pandemic by the World Health Organization on March 11, 2020, signifying the spread of a major global infectious disease [1]. As of this writing, the total number of confirmed cases worldwide has climbed to 250, 154, 972 [2] and claimed about 5,054,267 lives despite intensive public health precautions [2]. As the disease spread, governments began to recognize the pressure it had on the economy and health care sector. Accelerated public health campaigns were thus put into motion in all forms of mass media. With social distancing, facial masks, immaculate hand hygiene, and vaccinations forming the pillars of the preventive strategy.
Hand hygiene is of utmost importance after facial masks as a measure of infection control to prevent contamination of hands directly via 'respiratory droplets from coughs and sneezes or indirectly via touching infected fomites. The CDC recommends hand hygiene by either using soap and water or ABHS (Alcohol Based Hand Sanitizer) [3]. Hand sanitizers with an alcohol concentration of at least 60% ethanol or 70% isopropyl alcohol can be used in place of soap and water to inactivate SARS-CoV-2 [3].
As healthcare and non-healthcare professionals, began to adopt strict hygiene protocols with frequent hand washing with soap and water or ABHS, a series of adverse effects linked to the use of cleansing agents began to emerge. Numerous individual studies looking into the healthcare and general population separately revealed an increase in the incidence of adverse skin reactions in both groups [4, 5, 6, 7, 8, 9, 10]. In Wuhan (China), 74.5% of health professionals developed hand eczema, with an increased frequency of handwashing as a significant predictor [4]. Similar studies in Germany [5], Turkey [6], and India [7] also revealed a rise in hand eczema reported by healthcare workers at 90.4%, 50.5%, and 65.5% respectively. Studies into the non-healthcare population group also saw a rise in hand hygiene reactions due to increased hand washing and the use of sanitisers. 24 new cases of hand eczema were diagnosed in urgent care in a study in Milan [8], 16 new cases were reported in 10 days in a survey India [9] and nearly half the participants in a study in Saudi Arabia experienced skin reactions, particularly people those with a history of eczema [10]. But very limited research was carried out to compare the risks in both the groups side by side [11, 12].This study aims to explore these adverse effects within both the groups identify potential risk factors and propose appropriate changes in an attempt to prevent or reduce these effects.
2. Materials and Methods
2.1. Study participants and study site
This cross-sectional study surveyed healthcare workers (HCW) and non-healthcare workers (NHCW) across Bangladesh in a period of two months (May and June 2021).
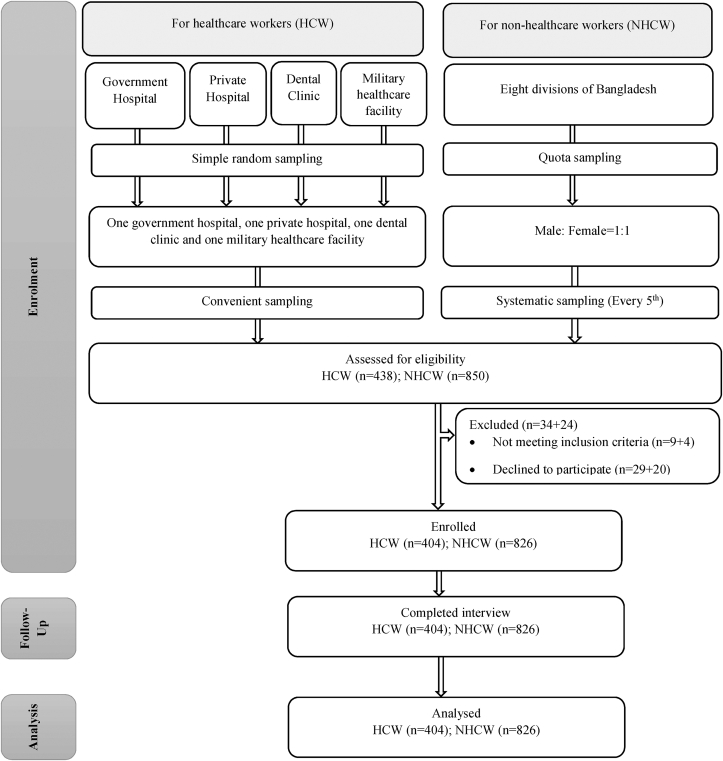
Sample size estimation was done using the formula: n = , where Zα/2 = critical value of the normal distribution at α/2 (for a confidence level of 95%, α is 0.05 and the critical value is 1.96), Zβ = critical value of the normal distribution at β (for a power of 80%, β is 0.2 and the critical value is 0.84), p1 = assumed prevalence of adverse skin reactions among HCW = 0.55 [12], and p2 = assumed prevalence of adverse skin reactions among NHCW = 0.45 [12]. The calculated sample size was 389 in each group. However, we recruited 404 HCW and 826 NHCW (a total of 1230 participants) to ensure adequate power for the study (see Figure 1).
Figure 1.
STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) flow chart of study participants. A total of 1288 individuals (438 HCW & 850 NHCW) were assessed for eligibility. 58 individuals (34 HCW & 24 NHCW) were excluded for not meeting the inclusion criteria leaving a final sample of 1230 (404 HCW & 826 NHCW).
Initially, one government hospital, one private hospital, and one dental clinic were picked at random from a list of hospitals and dental clinics in each of the eight divisions (Dhaka, Chittagong, Rajshahi, Barisal, Mymensingh, Rangpur, Khulna, and Sylhet). A similar list was used to pick a military health-care institution. If any institution refused to participate that institution was excluded from the sampling frame and another institution was chosen randomly according to the inclusion criteria. Later, using the convenient sampling approach, 404 HCW were chosen from these institutions.
Secondly, 826 consenting general citizens (NHCW) were interviewed at public locations across the eight divisions using a fixed-step approach on a random route sample (every fifth person). To establish a representative sample of the general population per city, a quota sampling approach based on gender was applied (using data from the Bangladesh Bureau of Statistics). If a male subject is needed to fulfil the quota, every fifth person is contacted until a male is found.
2.2. Data collection
Volunteers were recruited and trained at each of the research locations. After informed written consent, volunteers conducted face-to-face interviews with subjects. A telephone interview was considered for health care personnel on COVID duty or who were isolated at home and informed verbal consent was taken from them. The HCW included registered physicians, nurses, technicians, and assistants whereas NHCW were included in the general population. Due to the genetic and cultural diversity, foreign nationals were excluded.
2.3. Study instrument
The researchers developed an initial questionnaire based on their review of existing studies. It was then pretested on 30 respondents, and the final version was accepted based on their recommendations. The final questionnaire retrieved information regarding respondents' sociodemographic characteristics (age, sex, occupation, place of employment, average work hours in the previous month), hand hygiene product type, and frequency of usage (1–4, 5–10, 11–15, 16–20, >20). Additionally, the questionnaire included questions about the history of COVID-19 infection and vaccinations. Moreover, respondents were asked about any new skin problems associated with the usage of hand hygiene products. The researchers compiled a list of frequent and relevant dermatological problems from the responses. All the reporting was done according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [13].
2.4. Ethical consideration
The Institutional Review Board of North South University approved (Approval no 2021/OR-NSU/IRB/1001) the research protocol. Wherever feasible, the 1964 Declaration of Helsinki and later modifications and comparable ethical standards were followed. Data collection was voluntary, and no incentive was offered to participants. Data were only accessible to the authors and were not disclosed anywhere.
2.5. Statistical analysis
We used Stata (version 16; StataCorp, College Station, TX, USA) for data analysis. A histogram, a normal Q-Q plot, and the Kolmogorov-Smirnov test were used to check for normality in continuous data. Arithmetic mean was used for quantitative data as a measure of center, and standard deviation was used as measure of dispersion. Two independent sample t-test (for continuous variables) and Pearson's chi-square (χ2) test (for categorical variables) were used to explore the bivariate relationship between outcome and predictor variables. Finally, variables with a p-value of ≤0.2 in the bivariate analysis were imputed into a binary logistic regression model to investigate the factors associated with adverse skin reactions among hand hygiene product users. All p-values were considered statistically significant if < 0.05.
3. Results
3.1. Baseline characteristics of study participants
Table 1 depicts the background characteristics of the study population. Out of the entire study cohort, 826 (67.17%) were non-healthcare workers (NHCW) & 404 (32.83%) were healthcare workers (HCW). 56.83% of the respondents were male and 51.79% were literate up to graduate level. 38% of the NHCW worked for more than 32 h a week which mainly included private job holders (39%) and labourers (21%) but in the other hand, the 59.65% of the HCW worked greater than 32 h a week. 75.53% of the entire study cohort used ABHS, while 69.35% used soap water. When asked about daily use frequency, 30.81% of the cohort reported that they had cleansed their hands 1 to 4 times a day, while 35.01 % reported that they had used hand hygiene products 5 to 10 times a day. 19.95% of the HCW cleansed their hands greater than 20 times a day, while only 4.68% of the NHCW did the same. 31.22% of the entire cohort had a prior history of COVID-19 infection. Among HCW, 65.84% were infected and among NHCW, only 14.29% were infected. 60.89% of the study cohort was fully vaccinated.
Table 1.
Background characteristics of study population.
| Characteristics | Entire study cohort (n = 1230) | NHCW (n = 826) | HCW (n = 404) | |||
|---|---|---|---|---|---|---|
| Age, years (mean ± SD) | 29.45 ± 11.53 | 29.45 ± 13.18 | 29.46 ± 7.06 | |||
| Gender | ||||||
| Male | 699 | (56.83%) | 417 | (50.48%) | 282 | (69.8%) |
| Female | 531 | (43.17%) | 409 | (49.52%) | 122 | (30.2%) |
| Educational Status | ||||||
| Illiterate | 23 | (1.87%) | 23 | (2.78%) | - | |
| Primary | 73 | (5.93%) | 69 | (8.35%) | 4 | (0.99%) |
| Secondary | 116 | (9.43%) | 88 | (10.65%) | 28 | (6.93%) |
| Higher Secondary | 205 | (16.67%) | 157 | (19.01%) | 48 | (11.88%) |
| Graduate | 637 | (51.79%) | 377 | (45.64%) | 260 | (64.36%) |
| Post-graduate | 176 | (14.31%) | 112 | (13.56%) | 64 | (15.84%) |
| Marital Status | ||||||
| Unmarried | 655 | (53.3%) | 514 | (62.23%) | 141 | (34.99%) |
| Married | 552 | (44.91%) | 299 | (36.2%) | 253 | (62.78%) |
| Widow∖Divorced∖Separated | 22 | (1.79%) | 13 | (1.57%) | 9 | (2.23%) |
| Religion | ||||||
| Islam | 891 | (72.44%) | 560 | (67.8%) | 331 | (81.93%) |
| Hindu | 289 | (23.5%) | 230 | (27.85%) | 59 | (14.6%) |
| Buddhism | 41 | (3.33%) | 28 | (3.39%) | 13 | (3.22%) |
| Other | 9 | (0.73%) | 8 | (0.97%) | 1 | (0.25%) |
| Occupation | ||||||
| Business | 59 | (4.8%) | 59 | (7.14%) | - | |
| Government Job | 30 | (2.44%) | 30 | (3.63%) | - | |
| Private Job | 123 | (10%) | 123 | (14.89%) | - | |
| Labourer | 52 | (4.23%) | 52 | (6.3%) | - | |
| Medical Student | 46 | (3.74%) | 46 | (5.57%) | - | |
| Non-medical Student | 411 | (33.41%) | 411 | (49.76%) | - | |
| Unemployed | 103 | (8.37%) | 103 | (12.47%) | - | |
| Other | 2 | (0.16%) | 2 | (0.24%) | - | |
| Doctor | 301 | (24.47%) | - | 301 | (74.5%) | |
| Nurse | 35 | (2.85%) | - | 35 | (8.66%) | |
| Medical Technologist | 31 | (2.52%) | - | 31 | (7.67%) | |
| Other Healthcare Worker | 37 | (3.01%) | - | 37 | (9.16%) | |
| Work hour (hours/week) | ||||||
| <8 | 249 | (26.32%) | 190 | (35.06%) | 59 | (14.6%) |
| 8 to 16 | 141 | (14.9%) | 84 | (15.5%) | 57 | (14.11%) |
| 16 to 24 | 40 | (4.23%) | 24 | (4.43%) | 16 | (3.96%) |
| 24 to 32 | 70 | (7.4%) | 39 | (7.2%) | 31 | (7.67%) |
| 32 to 48 | 151 | (15.96%) | 72 | (13.28%) | 79 | (19.55%) |
| 48 to 56 | 197 | (20.82%) | 133 | (24.54%) | 64 | (15.84%) |
| >56 | 98 | (10.36%) | - | 98 | (24.26%) | |
| Hand hygiene product | ||||||
| Alcohol based sanitizer | 929 | (75.53%) | 572 | (69.25%) | 357 | (88.37%) |
| Soap water | 853 | (69.35%) | 592 | (71.67%) | 261 | (64.6%) |
| Detergent solution/Savlon solution/Bleaching powder solution | 15 | (1.22%) | 9 | (1.09%) | 6 | (1.49%) |
| Daily use frequency (times/day) | ||||||
| 1 to 4 | 367 | (30.81%) | 306 | (38.73%) | 61 | (15.21%) |
| 5 to 10 | 417 | (35.01%) | 279 | (35.32%) | 138 | (34.41%) |
| 11 to 15 | 214 | (17.97%) | 135 | (17.09%) | 79 | (19.7%) |
| 16 to 20 | 76 | (6.38%) | 33 | (4.18%) | 43 | (10.72%) |
| >20 | 117 | (9.82%) | 37 | (4.68%) | 80 | (19.95%) |
| H/O COVID-19 infection | 384 | (31.22%) | 118 | (14.29%) | 266 | (65.84%) |
| Vaccination Status | ||||||
| Not vaccinated | 347 | (28.21%) | 316 | (38.26%) | 31 | (7.67%) |
| Received first dose | 134 | (10.89%) | 99 | (11.99%) | 35 | (8.66%) |
| Fully vaccinated | 749 | (60.89%) | 411 | (49.76%) | 338 | (83.66%) |
SD, standard deviation; NHCW, non-healthcare workers; HCW, healthcare workers; Data are presented as n (%) unless otherwise indicated.
3.2. Prevalence of adverse skin reactions
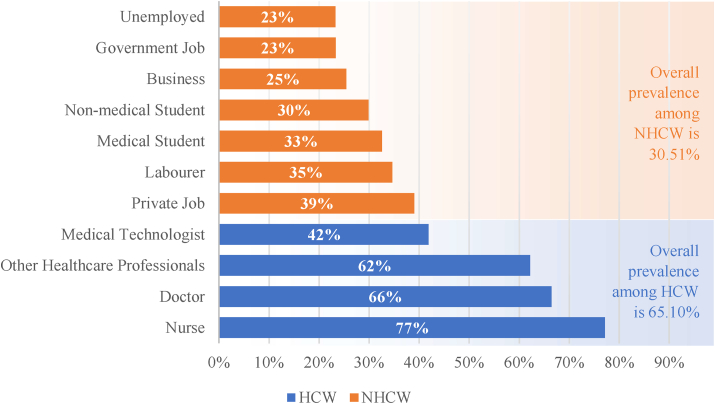
Overall prevalence of adverse skin reactions in our study population was 41.9% (Table 2). Figure 2 depicts that healthcare workers (65.10%) had a higher prevalence of adverse skin reactions compared to non-healthcare workers (30.51%). Among the HCW, nurses (77%) had the highest prevalence of adverse skin reactions, followed by doctors (66%) and other health care professionals (62%). On the other hand, among the NHCW, private job holders (39%) had the highest prevalence of adverse skin reactions, followed by labourers (35%) and medical students (33%).
Table 2.
Factors associated with adverse skin reactions among the hand sanitizer users.
| Factors | Adverse skin reactions (n = 515, 41.9%)a | Bivariate analysis |
Multivariate analysis |
|||||
|---|---|---|---|---|---|---|---|---|
| Crude OR (95% CI) | p-valueb | Adjusted OR (95% CI) | p-valueb | |||||
| Age, years | ||||||||
| ≤21 | 110 | (21.36%) | Reference | <0.001 |
Reference | 0.004 |
||
| 22-26 | 159 | (30.87%) | 2.14 | (1.56─2.93) | 0.63 | (0.36─1.1) | ||
| 27-34 | 135 | (26.21%) | 2.42 | (1.74─3.38) | 0.48 | (0.25─0.89) | ||
| ≥35 |
111 |
(21.55%) |
1.29 |
(0.93─1.78) |
0.41 |
(0.23─0.75) |
||
| Gender | ||||||||
| Male | 287 | (55.73%) | Reference | 0.508 |
Reference | |||
| Female | 228 | (44.27%) | 1.08 | (0.86─1.36) | 1.92 | (1.37─2.7) | <0.001 | |
| Educational Status | ||||||||
| Illiterate | 7 | (1.36%) | Reference | 0.168 |
Reference | 0.384 |
||
| Primary | 31 | (6.02%) | 1.69 | (0.62─4.6) | 1.21 | (0.4─3.68) | ||
| Secondary | 43 | (8.35%) | 1.35 | (0.51─3.53) | 0.85 | (0.27─2.64) | ||
| Higher Secondary | 73 | (14.17%) | 1.26 | (0.5─3.21) | 0.60 | (0.19─1.89) | ||
| Graduate | 288 | (55.92%) | 1.89 | (0.77─4.65) | 0.71 | (0.23─2.22) | ||
| Post-graduate | 73 | (14.17%) | 1.62 | (0.63─4.14) | 0.89 | (0.28─2.82) | ||
| Marital Status | ||||||||
| Unmarried | 241 | (46.89%) | Reference | <0.001 |
Reference | 0.246 |
||
| Married | 266 | (51.75%) | 1.60 | (1.27─2.1) | 1.24 | (0.86─1.77) | ||
| Widow∖Divorced∖Separated | 7 | (1.36%) | 0.80 | (0.32─1.99) | 0.59 | (0.19─1.83) | ||
| Religion | ||||||||
| Islam | 387 | (75.15%) | Reference | 0.006 |
Reference | 0.020 |
||
| Hindu | 99 | (19.22%) | 0.68 | (0.51─0.89) | 1.03 | (0.69─1.53) | ||
| Buddhism | 24 | (4.66%) | 1.84 | (0.97─3.47) | 1.71 | (0.76─3.88) | ||
| Other | 5 | (0.97%) | 1.63 | (0.43─6.1) | 14.5 | (1.52─139.86) | ||
| Occupation | ||||||||
| NHCW | 252 | (30.51%) | Reference | <0.001 |
Reference | <0.001 |
||
| HCW | 263 | (65.10%) | 4.25 | (3.3─5.47) | 3.50 | (2.23─5.49) | ||
| Work hour (hours/week) | ||||||||
| <8 | 85.00 | (19.45%) | Reference | <0.001 |
Reference | <0.001 |
||
| 8 to 16 | 64.00 | (14.65%) | 1.60 | (1.5─2.45) | 1.62 | (1─2.64) | ||
| 16 to 24 | 17.00 | (3.89%) | 1.43 | (0.72─2.81) | 1.30 | (0.61─2.75) | ||
| 24 to 32 | 37.00 | (8.47%) | 2.16 | (1.26─3.7) | 1.88 | (1.03─3.43) | ||
| 32 to 48 | 66.00 | (15.1%) | 1.50 | (0.99─2.27) | 1.24 | (0.75─2.04) | ||
| 48 to 56 | 97 | (22.2%) | 1.87 | (1.28─2.74) | 2.38 | (1.46─3.87) | ||
| >56 | 71 | (16.25%) | 5.07 | (3.3─8.49) | 2.51 | (1.34─4.7) | ||
| Hand hygiene products | ||||||||
| Alcohol based sanitizer | 427 | (82.91%) | 2.06 | (1.56─2.72) | <0.001 | 1.40 | (0.93─2.1) | 0.107 |
| Soap water | 365 | (70.87%) | 1.13 | (0.88─1.45) | 0.325 | 0.97 | (0.69─1.37) | 0.88 |
| Detergent/Savlon solution/bleaching powder solution | 8 | (1.55%) | 1.59 | (0.57─4.42) | 0.371 | 1.21 | (0.33─4.43) | 0.76 |
| Daily use frequency (times/day) | ||||||||
| 1 to 4 | 103 | (20%) | Reference | <0.001 | Reference | 0.001 | ||
| 5 to 10 | 205 | (39.81%) | 2.48 | (1.84─3.34) | 1.98 | (1.33─2.95) | ||
| 11 to 15 | 108 | (20.97%) | 2.61 | (1.84─3.71) | 1.96 | (1.22─3.15) | ||
| 16 to 20 | 44 | (8.54%) | 3.52 | (2.12─5.86) | 1.84 | (0.97─3.5) | ||
| >20 | 55 | (10.68%) | 2.27 | (1.48─3.49) | 0.92 | (0.53─1.61) | ||
| H/O COVID-19 infection | 232 | (45.05%) | 3.04 | (2.37─3.9) | <0.001 | 1.83 | (1.29─2.61) | 0.001 |
| Vaccination Status | ||||||||
| Not vaccinated | 114 | (22.14%) | Reference | <0.001 | Reference | 0.590 | ||
| Received first dose | 55 | (10.68%) | 1.42 | (0.94─2.15) | 1.16 | (0.68─1.99) | ||
| Fully vaccinated | 346 | (67.18%) | 1.75 | (1.34─2.29) | 0.98 | (0.64─1.51) | ||
Data are presented as n (%).
Significant p-values (<0.05) are in boldOR, odds ratio; CI, confidence interval; NHCW, non-healthcare workers; HCW, healthcare workers.
Figure 2.
Adverse skin reactions among Healthcare Workers (HCW) and Non-Healthcare Workers (NHCW) according to profession. Overall prevalence of adverse skin reactions among HCW and NHCW is 65.10% and 30.51%, respectively. The predominant group with the most adverse skin reactions among HCW were nurses and among NHCW were private job holders.
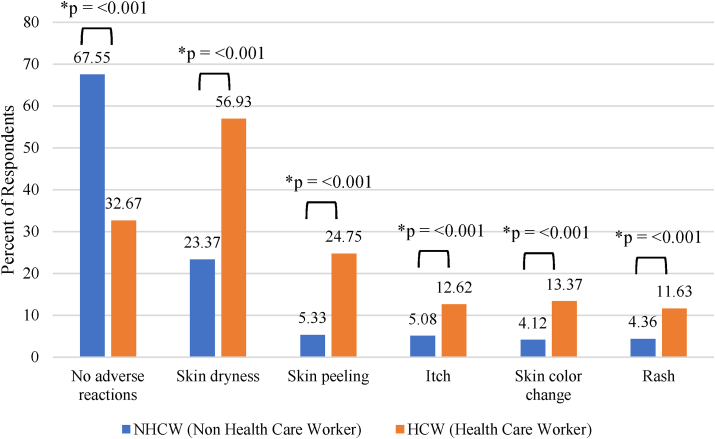
3.3. Types of adverse skin reactions
Figure 3 depicts the types of adverse skin reactions and their frequencies following hand hygiene product use among the study population. Over half of the cohort reported no adverse reactions (56.1%), among which the majority were NHCW (67.55%). Adverse skin reactions were reported by 41.87% of the study population, which were more common among HCW (65.10%) compared to NHCW (30.51%). Skin dryness was the commonest reported skin problem (34.39%) followed by skin peeling (11.71%).
Figure 3.
Types of adverse skin reactions among Healthcare Workers and Non-Healthcare Workers. Skin dryness was the most prevalent type of adverse skin reaction followed by skin peeling in both HCWs and NHCWs. However, HCWs were significantly more prone to all types of adverse skin reactions compared to NHCWs.
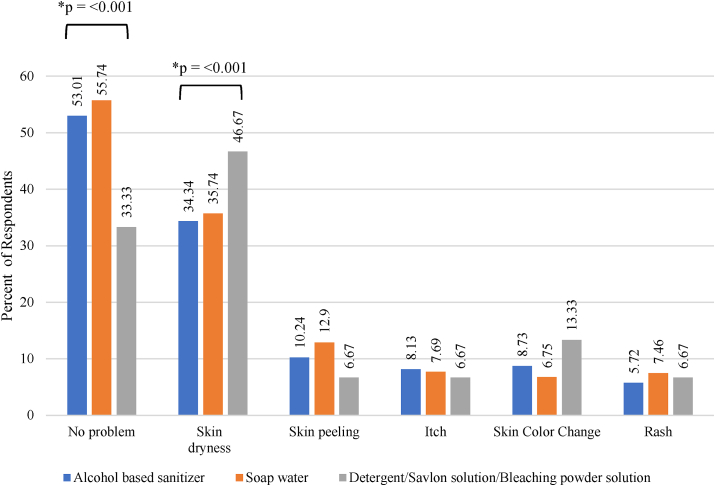
3.4. Hand hygiene product use and adverse skin reactions
Figure 4 reveals study participants using soap water were significantly more protected from developing adverse reactions (55.74%) compared to those using ABHS (53.01%) and detergent/savlon solution/bleaching powder solution (33.33%). Detergent/savlon solution/bleaching powder solution users were significantly more prone to developing skin dryness (46.67%). Prevalence of skin colour change was also higher in detergent/savlon solution/bleaching powder solution users (13.33%). On the other hand, ABHS users were more likely to develop itch (8.13%), and soap water users were susceptible to skin peeling (35.74%) and rash (7.46%).
Figure 4.
Adverse skin reactions according to hand hygiene product use. Participants using soap water were significantly more protected from developing adverse reactions than two other groups. Skin dryness was significantly higher and skin color change were also more common among detergent/savlon solution/bleaching powder solution users. Skin peeling and itch were more common among soap water and alcohol-based sanitizer users, respectively.
3.5. Factors associated with adverse skin reactions
Unadjusted and adjusted results of binary logistic regression of the study variables are presented in Table 2. Age had a significant association with adverse skin reactions during both bivariate and multivariate analysis.
The multivariate analysis showed HCW were 3.5 times more likely to suffer from adverse skin manifestations than NHCW. Females were 1.92 times more likely to have adverse skin reactions compared to men. When compared to the group that worked fewer than 8 h per week, those who worked between 48 and 56 h and those who worked more than 56 h were 2.38 times and 2.51 times more likely to experience adverse skin reactions, respectively. ABHS use was significantly associated with developing adverse reactions in bivariate analysis (Crude OR: 2.06; 95% CI: 1.56–2.72. p < 0.001). Although it loses significance in the multivariate analysis, ABHS users were 40% more likely to develop adverse skin reactions, whereas soap water users were 3% less likely. The daily use frequency of hand hygiene products had a significant (p < 0.001) association with adverse skin manifestations. The group that used ABHS 5 to 10 times per day had almost two times the risk of having adverse skin responses compared to the group that used ABHS 1 to 4 times per day. Subjects who had a history of COVID-19 infection were nearly two times more likely to develop adverse skin reactions than those who did not (p = 0.001).
4. Discussion
Skin reactions are common adverse effect of hand hygiene product use. With increased hand hygiene measures to prevent COVID-19 transmission, healthcare workers and the general public were at increased risk of adverse skin reactions. The present study explored the prevalence and types of adverse skin reactions that occurred following hand hygiene product use during COVID-19 pandemic and compared the results between HCW and NHCW.
Our current study showed that of the 41.8% of participants reporting skin reactions, HCWs (65.10 %) were recorded to have more frequent adverse responses than NHCWs (30.51 %). There was significant association between occupation and adverse skin reactions, with HCWs being 3.5 times more likely to suffer from adverse skin manifestations than NHCWs. Our findings were consistent with a population-based survey in Saudi Arabia [11] and a prospective cross-sectional study carried out in Thailand [12] which found skin changes to be common during the pandemic in both healthcare workers and the general population with healthcare workers being at a greater risk. This could be due to the higher frequency of cleansing and increased use of alcohol-based products as revealed in previous studies [11, 12]. The long working hours of HCW compared to NHCW could also be an important factor. This has been supported by a multiple logistic regression model, which showed a significant association between work hours (hours/week) and adverse skin reactions.
The increased risk of dermatological problems linked to frequent handwashing has been evidenced in studies even before the current outbreak. During the strict hygiene practices in the 2014 Ebola pandemic, an increase in the diagnosis of hand eczema was also seen in HCW [14]. The randomised trial in Ebola revealed soap to be more triggering than ABHS [14]. This contradicts our study, which showed participants using soap water to be more protected from developing adverse reactions (55.74%) compared to those using ABHS (53.01%) and detergent/savlon solution/bleaching powder solution (33.33%). This could be the result of more frequent use of hand sanitisers in comparison to soap and water which is less easily accessible or portable than sanitiser. This can be further supported by the fact that the study participants who used ABHS 5 to 10 times per day had early twice the risk of developing unfavourable skin reactions than those using ABHS 1 to 4 times daily. ABHS was also associated with an increased risk of hand eczema in the 2020 study in Thailand [12]. ABHS have a low irritating potential and are more tolerable, but they tend to make the skin dry and more susceptible to contact dermatitis [15]. In general, while using ABHS, it is better to avoid ones with allergenic surfactants, preservatives, fragrances, or dyes [16]. ABHS, with added moisturisers, is beneficial in ameliorating hand dryness associated with frequent hand hygiene [16].Moreover, ethanol is preferable for the formulation since it is less irritating than isopropyl alcohol despite equal effectiveness [17]. In our current study, the most typical skin problem was also skin dryness (34.39%), followed by skin peeling (11.71%). Skin dryness was also the most frequently described reaction in the previous studies carried out in Germany [5], Saudi Arabia [11], India [7], and Thailand [12]. The WHO and the American Contact Dermatitis Society also advocate the use moisturisers after hand cleansing to help alleviate the most reported adverse reaction of dry skin [16, 18].
When exploring the association between gender and adverse skin reactions in our study, females were almost twice as likely to have adverse skin reactions than men. It is believed that the incidence of self-reporting in females could be a result of their thinner epidermis [19] and hormonal changes leading to inflammatory sensitivity [20, 21]. There was no statistically significant association between COVID-19 vaccination status and hand hygiene-related adverse skin conditions. Subjects with a history of COVID-19 infection were nearly two times more likely to suffer from undesirable cutaneous manifestations. However, why such an association exists still owes an explanation and demands further studies to explore the matter.
4.1. Limitations
It's essential to note some of our study's limitations as well as the methods we used to solve them. Firstly, while carrying out the study, the hand hygiene technique was not considered. The WHO and American Contact Dermatitis Society recommend cleansing by gentle patting rather than rubbing to minimise mechanical trauma to the skin barrier [16, 18]. The effect of gloves usage and water temperature during handwashing with soap was also not considered in the study [16, 22]. Wearing gloves when hands are still wet can increase the risk of skin irritation due to the increased chance of entrapment of irritants and so effect adverse reaction [23]. Due to our study's cross-sectional nature, we cannot infer causality for the associations that we have presented in this paper. However, by presenting AORs using multiple regression models, we attempted to account for the potential effect of confounders. All the problems presented in this study were self-reported by the respondents, which may have led to self-reporting bias. In order to minimize this, all our data collectors were medical students with adequate training and followed a predefined neutral script. We also acknowledge that the findings of our study may not be generalizable due to our sample size. To make the sample representative and reduce selection bias, the healthcare workers were selected from randomly selected healthcare facilities, and non-healthcare workers were selected by quota sampling across all the divisions of Bangladesh.
5. Conclusion
Our research revealed healthcare workers to be at a significantly higher risk of developing adverse skin reactions from hand hygiene product use than the overall population. Also, a higher frequency of hand hygiene product use was a risk factor for adverse skin reactions. Although limiting the frequency may reduce the incidence of adverse skin reactions but might not always be practically feasible while adhering to strict infection control protocols. It is thus important to educate everyone about rational hand hygiene techniques and the inclusion of protective measures in their hand hygiene practices.
Declaration
Author contribution statement
Simanta Roy: Conceived and designed the experiments; Wrote the paper.
Mohammad Azmain Iktidar: Conceived and designed the experiments; Analyzed and interpreted the data.
Aishik Dipta Saha: Performed the experiments; Wrote the paper.
Sreshtha Chowdhury, Syed Md. Sayeem Tanvir: Contributed reagents, materials, analysis tools or data.
Syeda Tasnim Tabssum Hridi: Analyzed and interpreted the data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
Supplementary content related to this article has been published online at https://doi.org/10.1016/j.heliyon.2022.e12295.
References
- 1.Fouad N.A. In chief’s introduction to essays on the impact of COVID-19 on work and workers. J Vocat Behav. 2020 Jun;119 doi: 10.1016/j.jvb.2020.103441. 2020/05/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus disease (COVID-19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [cited 2021 Dec 2]. Available from:
- 3.Core practices | HICPAC | CDC. https://www.cdc.gov/hicpac/recommendations/core-practices.html#anchor_1556561902 [cited 2021 Dec 2]. Available from:
- 4.Lan J., Song Z., Miao X., Li H., Li Y., Dong L., et al. Skin damage among health care workers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82(5):1215. doi: 10.1016/j.jaad.2020.03.014. May 1 [cited 2022 Oct 16] Available from:/pmc/articles/PMC7194538/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guertler A., Moellhoff N., Schenck T.L., Hagen C.S., Kendziora B., Giunta R.E., et al. Onset of occupational hand eczema among healthcare workers during the SARS-CoV-2 pandemic: comparing a single surgical site with a COVID-19 intensive care unit. Contact Dermatitis. 2020;83(2):108. doi: 10.1111/cod.13618. Aug 1 [cited 2022 Oct 16] Available from:/pmc/articles/PMC7283680/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Erdem Y., Altunay I.K., Aksu Çerman A., Inal S., Ugurer E., Sivaz O., et al. The risk of hand eczema in healthcare workers during the COVID-19 pandemic: do we need specific attention or prevention strategies? Contact Dermatitis. 2020;83(5):422. doi: 10.1111/cod.13632. Nov 1 [cited 2022 Oct 17] Available from:/pmc/articles/PMC7300646/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jindal R., Pandhi D. Effect of hand hygiene practices in healthcare workers on development of hand eczema during coronavirus-19 pandemic: a cross sectional online survey. Indian J Dermatol. 2021;66(4):440. doi: 10.4103/ijd.IJD_973_20. Jul 1 [cited 2022 Oct 16] Available from:/pmc/articles/PMC8530052/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giacalone S., Bortoluzzi P., Nazzaro G. The fear of COVID-19 infection is the main cause of the new diagnoses of hand eczema: report from the frontline in Milan. Dermatol Ther. 2020;33(4) doi: 10.1111/dth.13630. Jul 1 [cited 2022 Oct 16] Available from:/pmc/articles/PMC7267079/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh M., Pawar M., Bothra A., Choudhary N. Overzealous hand hygiene during the COVID 19 pandemic causing an increased incidence of hand eczema among general population. J Am Acad Dermatol. 2020;83(1):e37. doi: 10.1016/j.jaad.2020.04.047. Jul 1 [cited 2022 Oct 16] Available from:/pmc/articles/PMC7161474/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zahrallayali A., Al-Doboke A., Alosaimy R., Alabbasi R., Alharbi S., Fageeh S., et al. The prevalence and clinical features of skin irritation caused by infection prevention measures during COVID-19 in the Mecca region, Saudi Arabia. Clin Cosmet Investig Dermatol. 2021;14 doi: 10.2147/CCID.S309681. https://pubmed.ncbi.nlm.nih.gov/34285535/ [cited 2022 Oct 16] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alsaidan M.S., Abuyassin A.H., Alsaeed Z.H., Alshmmari S.H., Bindaaj T.F., Alhababi A.A. The prevalence and determinants of hand and face dermatitis during COVID-19 pandemic: a population-based survey. Dermatol Res Pract. 2020;2020 doi: 10.1155/2020/6627472. [cited 2022 Oct 16] Available from:/pmc/articles/PMC7726962/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Techasatian L., Thaowandee W., Chaiyarit J., Uppala R., Sitthikarnkha P., Paibool W., et al. Hand hygiene habits and prevalence of hand eczema during the COVID-19 pandemic. J Prim Care Community Health. 2021;12 doi: 10.1177/21501327211018013. [cited 2022 Oct 16] Available from:/pmc/articles/PMC8138294/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. The Lancet. 2007;370(9596) doi: 10.1016/S0140-6736(07)61602-X. https://pubmed.ncbi.nlm.nih.gov/18064739/ Oct [cited 2021 Nov 28] Available from: [DOI] [PubMed] [Google Scholar]
- 14.Wolfe M.K., Wells E., Mitro B., Desmarais A.M., Scheinman P., Lantagne D. Seeking clearer recommendations for hand hygiene in communities facing Ebola: a randomized trial investigating the impact of six handwashing methods on skin irritation and dermatitis. PLoS One. 2016;11(12) doi: 10.1371/journal.pone.0167378. Dec 1 [cited 2022 Oct 16] Available from:/pmc/articles/PMC5193384/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Houben E., de Paepe K., Rogiers V. Skin condition associated with intensive use of alcoholic gels for hand disinfection: a combination of biophysical and sensorial data. Contact Dermatitis. 2006;54(5) doi: 10.1111/j.0105-1873.2006.00817.x. https://pubmed.ncbi.nlm.nih.gov/16689810/ May [cited 2022 Oct 17] Available from: [DOI] [PubMed] [Google Scholar]
- 16.Rundle C.W., Presley C.L., Militello M., Barber C., Powell D.L., Jacob S.E., et al. Hand hygiene during COVID-19: recommendations from the American contact dermatitis society. J Am Acad Dermatol. 2020;83(6) doi: 10.1016/j.jaad.2020.07.057. https://pubmed.ncbi.nlm.nih.gov/32707253/ Dec 1 [cited 2022 Oct 17] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balato A., Ayala F., Bruze M., Crepy M.N., Gonçalo M., Johansen J., et al. European Task Force on Contact Dermatitis statement on coronavirus disease-19 (COVID-19) outbreak and the risk of adverse cutaneous reactions. J Eur Acad Dermatol Venereol. 2020;34(8) doi: 10.1111/jdv.16557. https://pubmed.ncbi.nlm.nih.gov/32356382/ Aug 1 [cited 2022 Oct 17] Available from: [DOI] [PubMed] [Google Scholar]
- 18.Beiu C., Mihai M., Popa L., Cima L., Popescu M.N. Frequent hand washing for COVID-19 prevention can cause hand dermatitis: management tips. Cureus. 2020;12(4) doi: 10.7759/cureus.7506. Apr 2 [cited 2022 Oct 17] Available from: /pmc/articles/PMC7195203/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sandby-Møller J., Poulsen T., Wulf H.C. Epidermal thickness at different body sites: relationship to age, gender, pigmentation, blood content, skin type and smoking habits. Acta Derm Venereol. 2003;83(6) doi: 10.1080/00015550310015419. https://pubmed.ncbi.nlm.nih.gov/14690333/ [cited 2022 Oct 17] Available from: [DOI] [PubMed] [Google Scholar]
- 20.Lee C.H., Maibach H.I. The sodium lauryl sulfate model: an overview. Contact Dermatitis. 1995;33(1):1–7. doi: 10.1111/j.1600-0536.1995.tb00438.x. https://pubmed.ncbi.nlm.nih.gov/7493454/ [cited 2022 Oct 17] Available from: [DOI] [PubMed] [Google Scholar]
- 21.Farage M.A. Vulvar susceptibility to contact irritants and allergens: a review. Arch Gynecol Obstet. 2005;272(2) doi: 10.1007/s00404-005-0732-4. https://pubmed.ncbi.nlm.nih.gov/15906051/ [cited 2022 Oct 17] Available from: [DOI] [PubMed] [Google Scholar]
- 22.Michaels B., Gangar V., Schultz A., Arenas M., Curiale M., Ayers T., et al. Water temperature as a factor in handwashing efficacy. Food Serv. Technol. 2002;2(3) https://onlinelibrary.wiley.com/doi/full/10.1046/j.1471-5740.2002.00043.x Sep 1 [cited 2022 Oct 17] Available from: [Google Scholar]
- 23.Kilpatrick C., Allegranzi B., Pittet D., Kilpatrick C. WHO first global patient safety challenge: clean care is safer care, contributing to the training of health-care workers around the globe. Int J Infect Control. 2011;7(2) https://ijic.info/article/view/6515 [cited 2022 Oct 17] Available from: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.