Dear editor:
Lai et al.1 and Komiya et al.2 sequentially reported in this journal the changes in tuberculosis (TB) infection before and after the COVID-19 pandemic in Taiwan and Japan. The results of both studies showed that the number of patients newly diagnosed with TB has significantly decreased since the COVID-19 outbreak.1 , 2 Lai et al. suggested that interventions regarding the COVID-19 pandemic in infection control such as city lockdown, wearing masks, etc. had a positive impact on TB incidence. Komiya et al. considered that the statistical decrease in TB incidence after the COVID-19 outbreak was likely influenced by the decrease in the number of Mycobacterium tuberculosis (M. tuberculosis) tests and might not reflect the true incidence of TB in Japan.
TB is a seasonal infectious disease caused by M. tuberculosis infection. It is currently the second leading cause of death from a single infectious disease after COVID-19.3, 4, 5, 6 China is the third largest country in terms of the estimated number of TB cases (7.4% of global infections).4 Unlike other countries, the Chinese government has been implementing strict infection control measures for respiratory infectious diseases since January 2020 until now. However, no study is available on changes in TB infection before and after the COVID-19 pandemic in mainland China. To fill the gap, we therefore evaluated the trends in TB infection before and after the COVID-19 pandemic, which may help guide the implementation of clinical prevention strategies.
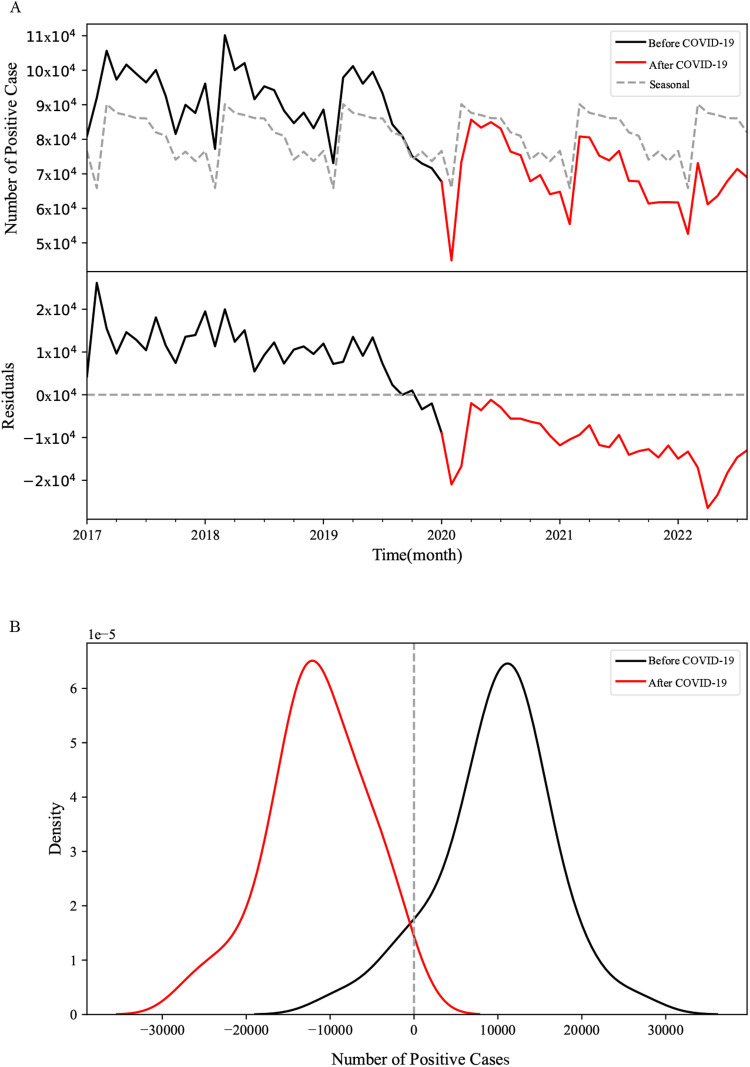
National surveillance data on TB infection provided by the National Health Commission of the People's Republic of China in mainland China were collected from January 1, 2017 to August 31, 2022. The results showed that there was a significant seasonality in the number of TB infection, in which the positive detection rate was highest in March and lowest in February (Fig. 1 A). In addition, there was a decreasing trend in the number of TB infection over the last 5 years (Fig. 1A). To discuss whether the COVID-19 outbreak has decreased the inflection of the TB, we removed the seasonal component, a redundant component usually caused by the weather and holidays that occurred similarly every year, to get a much more reliable result. The seasonal component is calculated by averaging the same month of every year, so it's a function of the month, independent of the year.
Fig. 1.
The monthly new cases of TB before and after the COVID-19 outbreak. A) the raw monthly new cases of TB (solid line) and the seasonal component (dash line) in the upper panel, and the residual after removing the seasonal component in the lower panel. B) the residual distributions before (black) and after (red) the outbreak. They illustrated that the outbreak decreased the number of new cases significantly (P-value < from the student's t-test on the two distributions in Figure B). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.).
In this function, the N (y, m) is the number of new cases in the year (y) and the month (m). And the adjusted series will be . After the seasonal adjustment, a t-test was used to test the difference between the adjusted number of new cases before and after the COVID-19 outbreak. Results from the analysis of the number of positive TB infections revealed a significant difference in the number of TB infections before and after the COVID-19 outbreak in mainland China (Fig. 1A and 1B; P < 0.0001). Additionally, we also observed that the adjusted value of TB infections had a local minimal value in February 2020 and April 2022, respectively, which coincided with the time of household isolation implemented by the Chinese government through a society-wide lockdown from January 24, 2020 to May 2020 and from April to May 2022. The main cause might be that the government imposed the lockdowns in many areas during these two time periods and restricted access to hospitals, especially for people with non-emergency symptoms. In this case, the physicians might be deprived of the opportunity to suspect TB infection and to test for M. tuberculosis. It implies an increase in the number of undiagnosed, untreated TB patients, which will lead to an increase in the number of deaths due to TB and a potential risk of community transmission. Besides, absence of immune stimulation due to decreased TB diagnoses and relative decrease in vaccine uptake may lead to "immune debt", which may negatively impact and potentially make the population more vulnerable in the next epidemic season.7
Otherwise, the COVID-19 pandemic brought about lifestyle changes, including encouragement to wear masks, wash hands, maintain social distance, and suspend mass gatherings. These preventive measures against transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may have contributed to the decline in many types of infectious diseases, especially respiratory infectious diseases. This short-term positive impact is welcome. Whereas, the majority of TB observed worldwide is secondary (reactivated) TB, which usually develops after decades due to reactivation of latent TB infection.8 , 9 Thus, infection control measures enacted after the COVID-19 outbreak to prevent the spread of SARS-CoV-2 would not be expected to show a real impact on the number of TB infections until decades later. Nevertheless, the COVID-19 pandemic influenced the epidemiological trend of TB infections in mainland China. It may be mainly attributed to a series of strict measures taken during the COVID-19 pandemic, as well as the increased awareness of self-protection and protective measures taken by people, which also reduced the chance of TB infection. The global pandemic is still ongoing and the situation of epidemic prevention and control is still severe, despite the fact that COVID-19 still occurs in some cities in mainland China and is generally under control, so the long-term epidemiological trend of TB deserves our continuous attention.
In conclusion, there has been a devastating impact on access to TB diagnosis, treatment, and the burden of TB due to the COVID-19 pandemic. Intensive efforts are urgently needed to mitigate and reverse the negative impact of the COVID-19 pandemic on TB.
Author contributions
Haiyan Yang and Fang Liu designed the study. Jie Xu and Yujia Wang conducted data collection. Jie Xu conducted statistical analyses. Jie Xu wrote the manuscript. All the authors approved the final version of the manuscript.
Data availability statement
The data that support the findings of this study are included in this article and available from the corresponding author upon reasonable requests.
Funding
This study was supported by the grant from National Natural Science Foundation of China (No. 82273696). The funder has no role in the data collection, data analysis, preparation of manuscript and decision to submission.
Declaration of Competing Interest
The authors declare that they have no any potential conflict of interest regarding this submitted manuscript.
References
- 1.Lai C.C., Yu W.L. The COVID-19 pandemic and tuberculosis in Taiwan. J Infect. 2020;81(2):e159–ee61. doi: 10.1016/j.jinf.2020.06.014. PubMed PMID: 32534000. Pubmed Central PMCID: PMC7286835. Epub 2020/06/14. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Komiya K., Yamasue M., Takahashi O., Hiramatsu K., Kadota J.I., Kato S. The COVID-19 pandemic and the true incidence of Tuberculosis in Japan. J Infect. 2020;81(3):e24–ee5. doi: 10.1016/j.jinf.2020.07.004. PubMed PMID: 32650109. Pubmed Central PMCID: PMC7338857. Epub 2020/07/11. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luies L., du Preez I. The echo of pulmonary tuberculosis: mechanisms of clinical symptoms and other disease-induced systemic complications. Clin Microbiol Rev. 2020 Sep 16;33(4) doi: 10.1128/CMR.00036-20. PubMed PMID: 32611585. Pubmed Central PMCID: PMC7331478. Epub 2020/07/03. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeremiah C., Petersen E., Nantanda R., Mungai B.N., Migliori G.B., Amanullah F., et al. The WHO global tuberculosis 2021 report - not so good news and turning the tide back to End TB. Int J Infect Dis. 2022 Mar 20 doi: 10.1016/j.ijid.2022.03.011. PubMed PMID: 35321845. Pubmed Central PMCID: PMC8934249. Epub 2022/03/25. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong Y., Wang L., Burgner D.P., Miller J.E., Song Y., Ren X., et al. Infectious diseases in children and adolescents in China: analysis of national surveillance data from 2008 to 2017. Bmj. 2020 Apr 2;369:m1043. doi: 10.1136/bmj.m1043. PubMed PMID: 32241761. Pubmed Central PMCID: PMC7114954 at http://www.icmje.org/coi_disclosure.pdf and declare: support from the China Ministry of Science and Technology, National Natural Science Foundation of China, China Scholarship Council, and Peking University Health Science Centre for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work. Epub 2020/04/04. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thorpe L.E., Frieden T.R., Laserson K.F., Wells C., Khatri G.R. Seasonality of tuberculosis in India: is it real and what does it tell us? Lancet. 2004;364(9445):1613–1614. doi: 10.1016/S0140-6736(04)17316-9. 30-Nov 5PubMed PMID: 15519633. Epub 2004/11/03. eng. [DOI] [PubMed] [Google Scholar]
- 7.Cohen R., Ashman M., Taha M.K., Varon E., Angoulvant F., Levy C., et al. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now. 2021;51(5):418–423. doi: 10.1016/j.idnow.2021.05.004. PubMed PMID: 33991720. Pubmed Central PMCID: PMC8114587. Epub 2021/05/16. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mori T., Leung C.C. Tuberculosis in the global aging population. Infect Dis Clin North Am. 2010;24(3):751–768. doi: 10.1016/j.idc.2010.04.011. PubMed PMID: 20674802. Epub 2010/08/03. eng. [DOI] [PubMed] [Google Scholar]
- 9.Furin J., Cox H., Pai M. Tuberculosis. Lancet. 2019 Apr 20;393(10181):1642–1656. doi: 10.1016/S0140-6736(19)30308-3. PMID: 30904262. Epub 2019/03/25. eng. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are included in this article and available from the corresponding author upon reasonable requests.