Abstract
The antidiabetic effects of quercetin and metformin are well known. However, their synergistic effect in reversing the symptoms of diabetes-induced endothelial dysfunction remains unknown. In this study, we have investigated their synergistic effect in streptozotocin (STZ)-nicotinamide induced diabetic rats. Seventy-five rats were divided into five groups; normal control, diabetic control, treatment groups (10 mg/kg quercetin, 180 mg/kg metformin, and combined). The plasma glucose and lipid levels, liver enzymes, ex-vivo studies on aortic rings, histology of liver, kidney, pancreas, abdominal aorta and thoracic aorta, and immunohistochemical studies were carried out. The findings revealed that the combination of quercetin and metformin showed a greater antidiabetic effect than either drug, and rendered protection to the endothelium. The combination effectively reversed the hyperglycemia-induced endothelial dysfunction in diabetic rats. Furthermore, it also reversed the dysregulated expression of eNOS, 3-nitrotyrosine, VCAM-1, CD31 and SIRT-1. Overall, the present study's findings demonstrate that quercetin potentiates the activity of metformin to control the complications associated with diabetes.
Subject terms: Endocrine system and metabolic diseases, Cardiology
Introduction
The endothelium is a permeable barrier between the bloodstream and the outer vascular wall, regulating the vascular tone and structure. Endothelial dysfunction in the diabetic state is a well-established response arising from cardiovascular risk factors. There is decreased synthesis of nitric oxide in dysregulated endothelium. In addition, its availability may be reduced significantly in association with an imbalance between the relaxation and contraction factors of the endothelium.
Diabetes mellitus is a chronic metabolic disease associated with poor glycemic control, sedentary lifestyle, and obesity1. It is typically the consequence of insulin resistance in which the adipose or muscle cells do not respond effectively to normal insulin levels produced by β-cells of the pancreas2. According to the International Diabetes Federation report, about 327 million adults were affected with diabetes in 2017. The number is expected to rise to 438 million by 20453. More than 90% of diabetic cases were diagnosed with type-2 diabetes mellitus (T2DM). Uncontrolled diabetes leads to macrovascular and microvascular complications4. The macrovascular complications include ischemic heart disease, stroke, and foot gangrene, while the microvascular include retinopathy, nephropathy, and autonomic neuropathy4. Vascular disease risk reduction constitutes only to a smaller proportion. However, the key parameter, namely, glycosylated haemoglobin (HbA1C) levels, are lowered. These observations indicate that other major disease markers carry significant importance, which needs to be carefully considered to control T2DM5. However, reducing the glycemic level remains significant in lowering chronic cardiovascular risks. The current treatment options available in the market are expensive and have numerous side effects, including hypoglycemia, abdominal discomfort, and cell death6. Therefore, there has been a renewed interest in searching for newer promising diabetes treatment options.
Quercetin is a phytochemical that belongs to the class of flavonoids7. It is rich in tea, broccoli, and onion, exhibiting antioxidant and anti-inflammatory properties7. There exists a large body of evidence on Quercetin on its potential in ameliorating diabetes and related symptoms. Numerous studies have reported quercetin’s potential as an antidiabetic agent that have demonstrated improved endothelial function8. Quercetin is the most active flavonoid that exhibits normoglycemic properties via interacting with the 11β–Hydroxysteroid dehydrogenase type 1 (11β-HSD1) enzyme9. Quercetin has also been proven to enhance insulin production by 44–70% in isolated rat islets by improving the islet function10. The suggested mechanism includes the alteration of the Ca2+ fluxes and cyclic nucleotide metabolism in the islet cells10. Quercetin also promotes the regeneration of pancreatic islets, thus enhancing insulin production10,11.
Metformin was originally developed from a natural toxic compound, galegine, isolated from Galega officinalis. There have been numerous studies that have been carried out on the molecule ever since. In addition, several studies in the early 1950s had reported on the high efficacy and safety of metformin as an anti-diabetic agent12. Although it effectively reduces the elevated blood glucose in T2DM patients, its exact mechanism is still unknown13. Metformin suppresses glucose secretion in the liver and enhances its uptake by skeletal muscle14,15. Metformin reduces free fatty acid (FFA) levels and thus offers cardioprotection16,17. It also reduces blood pressure in humans and diabetic rats15.
There are no reported long-term studies on the effect of quercetin along with metformin on diabetes. Quercetin and metformin individually show improvements in vascular function. Their combination is expected to possess either additive or synergistic action. In this study, we report the synergistic effect of quercetin and metformin in streptozotocin-nicotinamide induced diabetic rats.
Results
Effect of treatment on oral glucose tolerance and plasma glucose
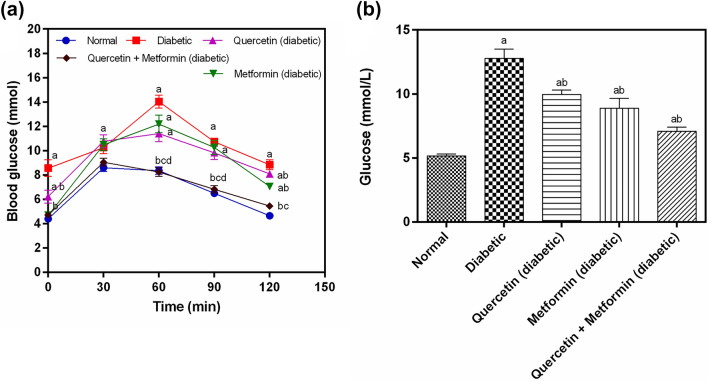
The fasting blood glucose levels were significantly (p < 0.05) higher in diabetic than the normal rats. The treatment with quercetin, metformin and quercetin + metformin significantly reduced the blood glucose levels in diabetic rats compared to the non-diabetic control (Fig. 1a). Among the treatment groups, rats treated with quercetin + metformin showed the highest reduction in blood glucose levels compared to quercetin and metformin alone. Besides this, quercetin + metformin-treated rats showed a glucose profile similar to the normal control (Fig. 1a).
Figure 1.
Effect of test compounds on, (a) oral glucose tolerance test, (b) on plasma glucose in diabetic rats. Data represent mean ± SEM. The alphabet, ‘a’ shows a significant difference in comparison with normal control (p < 0.05). The alphabet, ‘b’ shows a significant difference in comparison to diabetic control (p < 0.05). The alphabet, ‘c’ shows a significant difference in comparison with a quercetin treatment group (p < 0.05). The alphabet, ‘d’ shows a significant difference in comparison with the metformin treatment group (p < 0.05).
The plasma glucose level was significantly higher (p < 0.05) in the diabetic control group than in the normal control. The oral treatment with quercetin, Metformin, and quercetin + Metformin for 30 days significantly reduced (p < 0.05) the plasma glucose level in diabetic rats compared to diabetic control. The significantly highest reduction in plasma glucose was noticed in rats treated with quercetin + metformin compared to diabetic control (Fig. 1b).
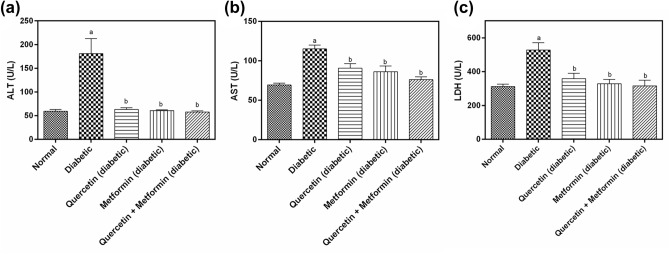
Effect of treatment on alanine aminotransferase (ALT), aspartate aminotransferase (AST), plasma creatinine (CR) and lactate dehydrogenase (LDH)
The plasma ALT, AST, and LDH levels were significantly higher (p < 0.05) in diabetic control compared with normal control. The treatment with quercetin, Metformin, and quercetin + Metformin for 30 days significantly reduced (p < 0.05) the plasma ALT, AST and LDH levels in diabetic rats as compared to diabetic control (Fig. 2).
Figure 2.
Effect of test compounds on, (a) plasma alanine aminotransferase (ALT), (b) plasma aspartate aminotransferase (AST), (c) plasma lactate dehydrogenase (LDH) in diabetic rats. Data represent mean ± SEM. The alphabet, ‘a’ shows a significant difference in comparison with normal control (p < 0.05). The alphabet, ‘b’ shows a significant difference in comparison to diabetic control (p < 0.05).
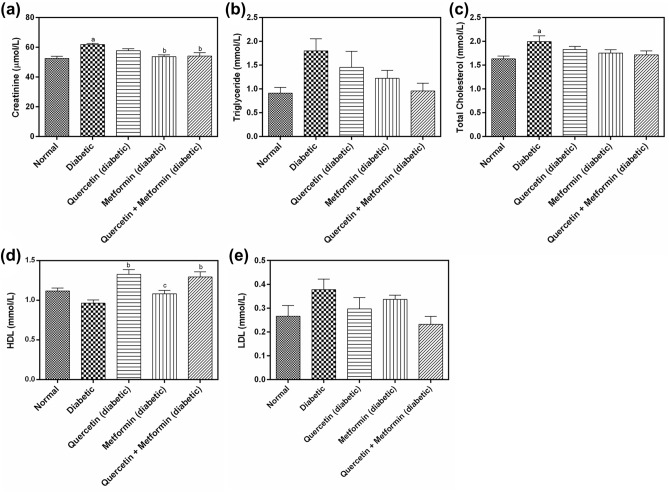
Effect of treatment on lipid profile
The mean triglyceride (TG), total cholesterol (TC), and low-density lipoprotein (LDL) levels were significantly higher (p < 0.05) in diabetic control as compared to normal control. In contrast, the high-density lipoprotein (HDL) level was low. Quercetin, metformin and quercetin + metformin treatments showed a reduction in CR, TG, TC and LDL levels compared to diabetic control. The quercetin + metformin was most effective among others. The HDL levels were significantly higher in quercetin, metformin, and quercetin + metformin treatment (Fig. 3).
Figure 3.
Effect of test compounds on plasma, (a) creatinine, (b) triglyceride (TG), (c) total cholesterol (TC), (d) high density lipoprotein (HDL), and (e) low density lipoprotein (LDL) in diabetic rats. Data represents mean ± SEM. The alphabet, ‘a’ shows a significant difference in comparison with normal control (p < 0.05). The alphabet, ‘b’ shows a significant difference in comparison to diabetic control (p < 0.05).
Ex vivo studies with rat aortic rings
Quercetin, metformin, and their combination increased the ACh-induced endothelium-dependent relaxation, SNP-induced endothelium-independent relaxation, and reduced the α 1-adrenergic agonist PE-induced contraction in diabetic rat aortic rings ex-vivo but had minimal effect in normal rat aortic rings (Tables 1, 2 and 3). The diabetic rats’ aorta did not relax upon the addition of acetylcholine (an endothelium-dependent vasorelaxant, Table 1), and sodium nitroprusside (an endothelium-independent vasodilator, Table 2). Phenylepinephrine (PE, α 1- adrenergic agonist) enhanced the contraction of the aorta from the diabetic rats (Table 3).
Table 1.
Effect of test compounds on phenylephrine (PE) induced contraction in aortae.
| Treatment groups | Phenylephrine (PE) induced contraction in aortae | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aortae with perivascular adipose tissue (PVAT) | Aortae without PVAT | |||||||||||||||
| Endothelium intact | Endothelium Denuded | Endothelium intact | Endothelium Denuded | |||||||||||||
| Abdominal aortae | Thoracic aortae | Abdominal aortae | Thoracic aortae | Abdominal aortae | Thoracic aortae | Abdominal aortae | Thoracic aortae | |||||||||
| Emax | pEC50 | Emax | pEC50 | Emax | pEC50 | Emax | pEC50 | Emax | pEC50 | Emax | pEC50 | Emax | pEC50 | Emax | pEC50 | |
| Normal | 104.9 ± 3.6 | 4.6 ± 0.1 | 102.9 ± 3.9 | 5.1 ± 0.2 | 111.2 ± 5.2 | 5.5 ± 0.2 | 113.6 ± 5.7 | 5.2 ± 0.1 | 113.9 ± 3.1 | 4.9 ± 0.1 | 109.9 ± 2.3 | 5.3 ± 0.1 | 131.6 ± 1.4 | 5.5 ± 0.3 | 120.9 ± 4.7 | 5.0 ± 0.1 |
| Diabetic | 142.9 ± 3.4a | 5.9 ± 0.4 | 141.0 ± 4.1a | 5.7 ± 0.2 | 157.4 ± 6.1 | 5.9 ± 0.2 | 153.7 ± 5.2a | 5.8 ± 0.3 | 146.7 ± 4.9a | 5.5 ± 0.3 | 158.3 ± 2.3a | 5.8 ± 0.3 | 176.3 ± 5.7a | 5.9 ± 0.3 | 168.4 ± 5.5a | 6.0 ± 0.3 |
| Quercetin (diabetic) | 126.6 ± 2.0b | 5.3 ± 0.2 | 129.4 ± 4.2 | 5.5 ± 0.2 | 139.9 ± 3.8 | 5.7 ± 0.2 | 134.9 ± 4.5b | 5.6 ± 0.2 | 134.9 ± 4.5b | 5.3 ± 0.2 | 130.1 ± 3.2b | 5.6 ± 0.1 | 150.6 ± 4.4b | 5.31 ± 0.3 | 144.7 ± 5.7b | 6.1 ± 0.9 |
| Metformin (diabetic) | 126.1 ± 3.4b | 5.6 ± 0.3 | 127.6 ± 4.3 | 5.3 ± 0.2 | 130.4 ± 5.5 | 5.8 ± 0.2 | 130.8 ± 6.8b | 5.5 ± 0.2 | 132.3 ± 6.3b | 5.44 ± 0.2 | 127.4 ± 1.7b | 5.4 ± 0.2 | 142.9 ± 4.5b | 5.5 ± 0.3 | 137.1 ± 6.1b | 5.7 ± 0.2 |
| Quercetin + Metformin (diabetic) | 115.5 ± 5.0bcd | 5.1 ± 0.1 | 112.1 ± 4.0bc | 5.3 ± 0.1 | 120.5 ± 3.8 | 5.6 ± 0.2 | 122.1 ± 4.6b | 5.4 ± 0.1 | 125.1 ± 1.9b | 5.3 ± 0.1 | 119.7 ± 3.9b | 5.5 ± 0.1 | 139.9 ± 6.5bc | 5.1 ± 0.3 | 132.0 ± 6.5b | 5.9 ± 0.2 |
Data represent mean ± SEM.
The alphabet, ‘a’ shows a significant difference in comparison with normal control (p < 0.05).
The alphabet, ‘b’ shows a significant difference in comparison to diabetic control (p < 0.05).
The alphabet, ‘c’ shows a significant difference in comparison with a quercetin treatment group (p < 0.05).
The alphabet, ‘d’ shows a significant difference in comparison with the metformin treatment group (p < 0.05).
Table 2.
Effect of test compounds on acetylcholine (Ach) induced relaxation in aortae.
| Treatment groups | Acetylcholine (Ach) induced relaxation in aortae | |||||||
|---|---|---|---|---|---|---|---|---|
| Aortae with perivascular adipose tissue (PVAT) | Aortae without PVAT | |||||||
| Endothelium intact | Endothelium intact | |||||||
| Abdominal aortae | Thoracic aortae | Abdominal aortae | Thoracic aortae | |||||
| Rmax | pEC50 | Rmax | pEC50 | Rmax | pEC50 | Rmax | pEC50 | |
| Normal | 104.8 ± 4.2 | 5.2 ± 0.1 | 105.2 ± 4.4 | 5.6 ± 0.1 | 101.6 ± 0.7 | 5.4 ± 0.2 | 104.6 ± 5.0 | 5.4 ± 0.1 |
| Diabetic | 62.9 ± 4.3a | 3.4 ± 0.2 | 64.6 ± 3.0a | 3.6 ± 0.2 | 64.5 ± 4.5a | 3.5 ± 0.2 | 69.2 ± 6.2a | 3.5 ± 0.2 |
| Quercetin (diabetic) | 83.4 ± 2.5b | 4.8 ± 0.1 | 84.7 ± 2.2b | 4.8 ± 0.1 | 79.3 ± 1.2ab | 4.5 ± 0.2 | 81.2 ± 1.9ab | 4.8 ± 0.2 |
| Metformin (diabetic) | 83.0 ± 1.4b | 4.8 ± 0.1 | 87.2 ± 4.2b | 5.2 ± 0.2 | 84.4 ± 4.7ab | 4.6 ± 0.2 | 84.6 ± 2.1ab | 4.8 ± 0.1 |
| Quercetin + Metformin (diabetic) | 96.8 ± 2.2bcd | 5.0 ± 0.1 | 95.3 ± 3.8b | 5.1 ± 0.1 | 93.8 ± 2.4b | 5.1 ± 0.1 | 100.2 ± 2.6bcd | 5.2 ± 0.1 |
Data represent mean ± SEM.
The alphabet, ‘a’ shows a significant difference in comparison with normal control (p < 0.05).
The alphabet, ‘b’ shows a significant difference in comparison to diabetic control (p < 0.05).
The alphabet, ‘c’ shows a significant difference in comparison with a quercetin treatment group (p < 0.05).
The alphabet, ‘d’ shows a significant difference in comparison with the metformin treatment group (p < 0.05).
Table 3.
Effect of test compounds on sodium nitroprusside (SNP) induced relaxation in aortae.
| Treatment groups | Sodium nitroprusside (SNP) induced relaxation in aortae | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aortae with perivascular adipose tissue (PVAT) | Aortae without PVAT | |||||||||||||||
| Endothelium intact | Endothelium Denuded | Endothelium intact | Endothelium Denuded | |||||||||||||
| Abdominal aortae | Thoracic aortae | Abdominal aortae | Thoracic aortae | Abdominal aortae | Thoracic aortae | Abdominal aortae | Thoracic aortae | |||||||||
| Rmax | pEC50 | Rmax | pEC50 | Rmax | pEC50 | Rmax | pEC50 | Rmax | pEC50 | Rmax | pEC50 | Rmax | pEC50 | Rmax | pEC50 | |
| Normal | 105.9 ± 2.0 | 6.16 ± 0.1 | 103.8 ± 1.1 | 5.9 ± 0.1 | 105.5 ± 1.8 | 5.8 ± 0.1 | 105.2 ± 1.7 | 5.3 ± 0.1 | 108.2 ± 1.7 | 6.0 ± 0.2 | 108.5 ± 2.3 | 6.50 ± 0.1 | 108.5 ± 1.4 | 6.3 ± 0.1 | 112.2 ± 1.8 | 6.6 ± 0.1 |
| Diabetic | 92.6 ± 2.1 | 5.7 ± 0.2 | 92.2 ± 0.7 | 5.3 ± 0.2 | 90.1 ± 1.4 | 5.0 ± 0.1 | 91.5 ± 0.8 | 5.2 ± 0.1 | 86.2 ± 1.4 | 5.4 ± 0.19 | 92.6 ± 0.6 | 5.3 ± 0.7 | 92.2 ± 1.9 | 5.6 ± 0.3 | 93.4 ± 0.8a | 5.3 ± 0.1 |
| Quercetin (diabetic) | 94.9 ± 1.0 | 6.0 ± 0.1 | 96.4 ± 0.7 | 6.0 ± 0.1 | 99.0 ± 0.4a | 5.5 ± 0.0 | 97.6 ± 0.9 | 5.4 ± 0.1 | 97.3 ± 3.5 | 5.9 ± 0.1 | 103.7 ± 1.3 | 5.85 ± 0.1 | 97.8 ± 0.6 | 5.9 ± 0.3 | 98.7 ± 0.5 | 6.2 ± 0.1 |
| Metformin (diabetic) | 96.9 ± 0.5 | 5.9 ± 0.2 | 97.2 ± 0.7 | 5.6 ± 0.1 | 96.9 ± 0.3 | 5.6 ± 0.1 | 96.4 ± 1.0 | 5.5 ± 0.1 | 93.9 ± 1.7 | 6.0 ± 0.1 | 99.8 ± 0.8 | 6.4 ± 0.1 | 101.9 ± 1.1 | 6.3 ± 0.1 | 104.8 ± 1.0 | 6.1 ± 0.1 |
| Quercetin + Metformin (diabetic) | 99.3 ± 0.8 | 6.1 ± 0.2 | 99.7 ± 1.5 | 6.0 ± 0.1 | 103.4 ± 1.0b | 6.0 ± 0.1 | 100.7 ± 1.1 | 5.6 ± 0.2 | 98.6 ± 0.9 | 5.9 ± 0.1 | 103.0 ± 1.5 | 6.2 ± 0.1 | 103.0 ± 1.0 | 6.2 ± 0.1 | 108.4 ± 1.2 | 6.1 ± 0.1 |
Data represent mean ± SEM.
The alphabet, ‘a’ shows a significant difference in comparison with normal control (p < 0.05).
The alphabet, ‘b’ shows a significant difference in comparison to diabetic control (p < 0.05).
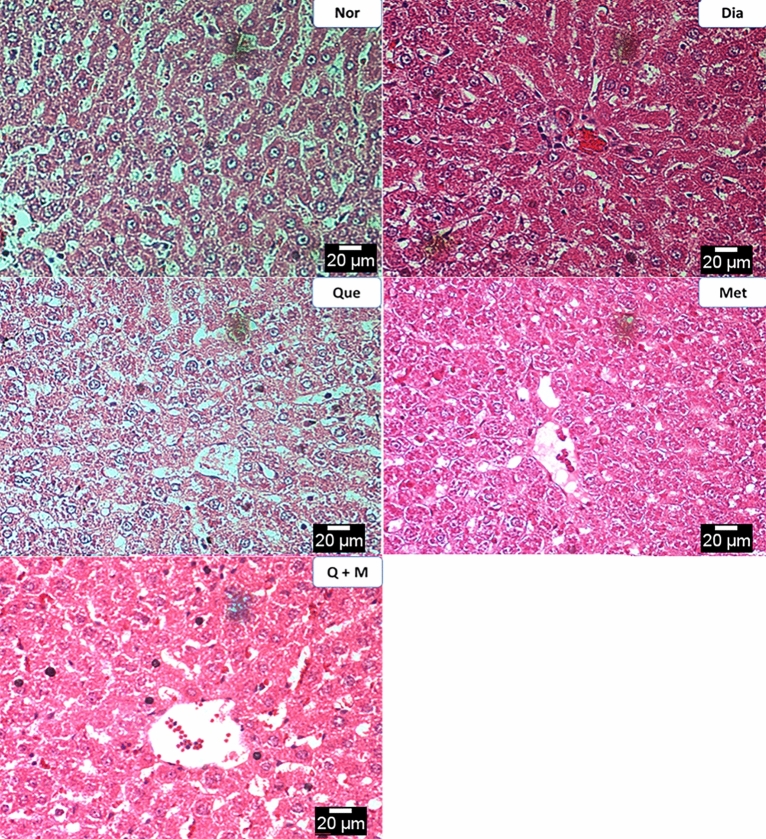
Histological analysis
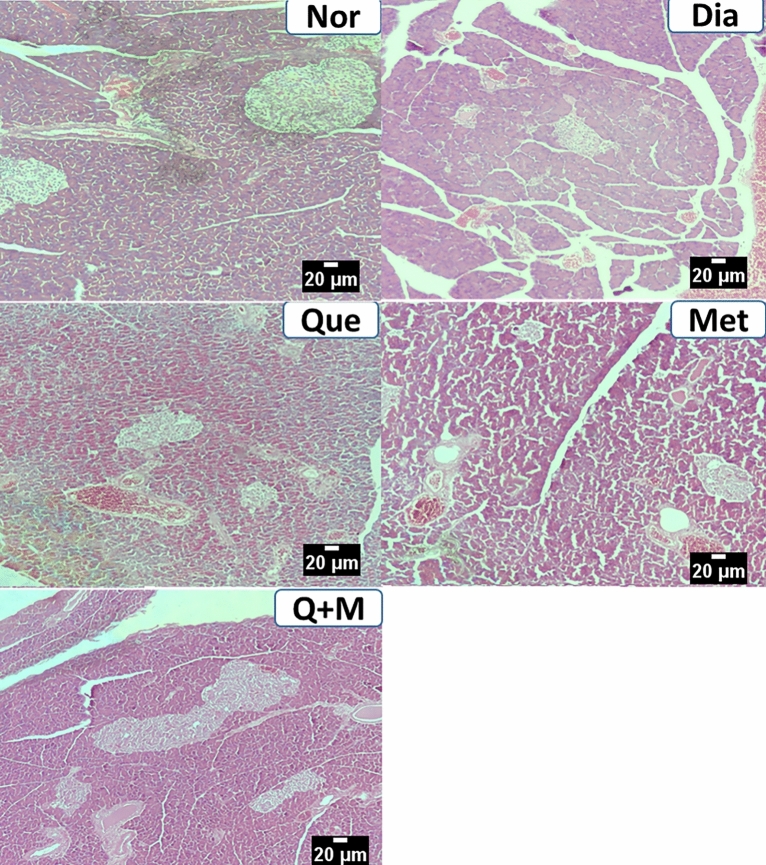
Liver
Control groups showed mild edematous liver parenchyma with intact architecture and minimal inflammation of periportal areas. Treatment with STZ caused predominantly degenerative changes in the hepatocytes, including fatty, feathery, and hydropic types. The diabetic rats treated with metformin or quercetin showed minimal degenerative changes indicating their protective effect on the hepatocytes. However, the diabetic rats treated with a combination of metformin and quercetin showed very minimal degenerative changes, indicating a better protective effect on the hepatocytes than these drug’s independent effects, as shown in Fig. 4.
Figure 4.
The effect of test compounds on liver histology in diabetic rats. Nor Normal, Dia Diabetic, Que Quercetin treated, Met Metformin treated, Q + M Quercetin + metformin treated diabetic rats.
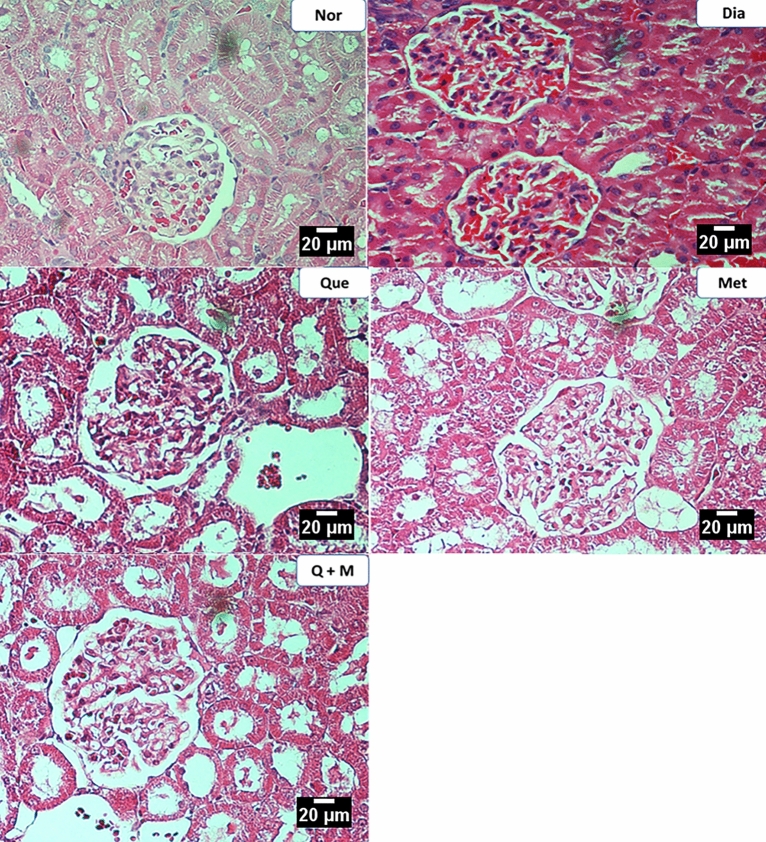
Kidney
Normal control observed renal parenchyma with mild interstitial oedema near glomeruli. The diabetic rats showed predominant changes in the glomerulus, such as (1) basement membrane thickening, (2) mesangial proliferation, and (3) thickened blood vessels in the interstitium with mild inflammation. The metformin or quercetin treated rats showed similar changes in the diabetic group. However, the diabetic rats treated with the combination of metformin and quercetin showed only very mild glomerular changes indicating a better protective effect on the kidneys (Fig. 5).
Figure 5.
The effect of test compounds on kidney histology in diabetic rats. Nor Normal, Dia Diabetic, Que Quercetin treated, Met Metformin treated, Q + M Quercetin + metformin treated diabetic rats.
Pancreas
The rats in the control group showed normal exocrine and endocrine cell proportions. The exocrine acinar cells were arranged in lobules, endocrine islet cells were found embedded inside the lobules of acinar cells and were enclosed by a thin capsule. Treatmenrt with STZ caused a drastic reduction of the volume of islets per lobule and showed focal areas of pale eosinophilic material and a small number of atrophic cells. This eosinophilic material was also seen surrounding the small blood vessels. The diabetic rats treated with metformin or quercetin showed mild degenerative changes. An occasional islet showed lymphocytic insulitis. The group treated with a combination of metformin and quercetin showed islets with several cells but with a lesser volume compared to the control. Only mild infiltration of inflammatory cells and eosinophilic deposits were observed in this group (Fig. 6).
Figure 6.
The effect of test compounds on pancreas histology in diabetic rats. Nor Normal, Dia Diabetic, Que Quercetin treated, Met Metformin treated, Q + M Quercetin + metformin treated diabetic rats.
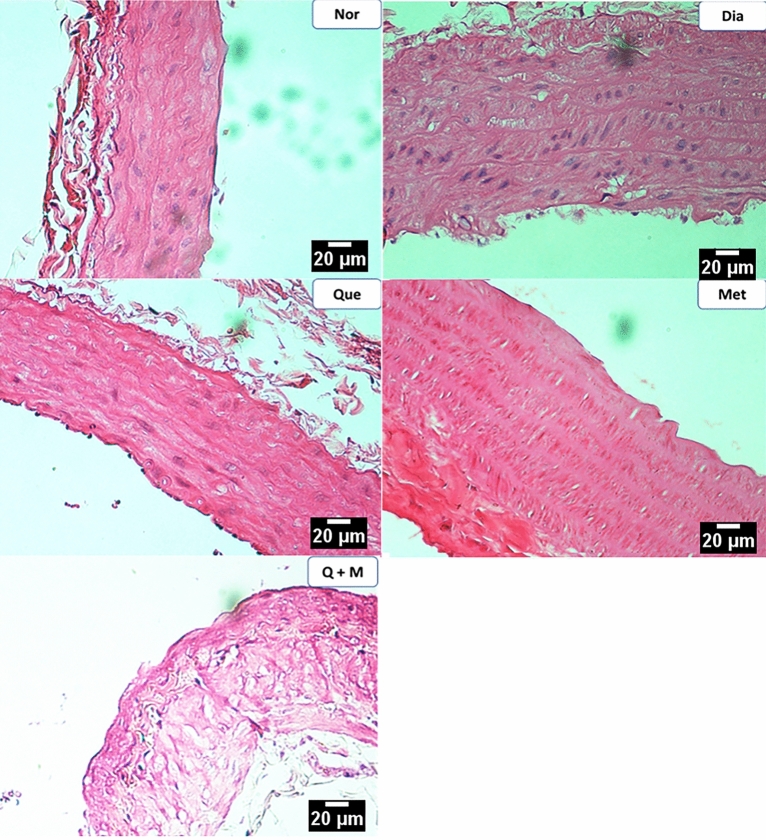
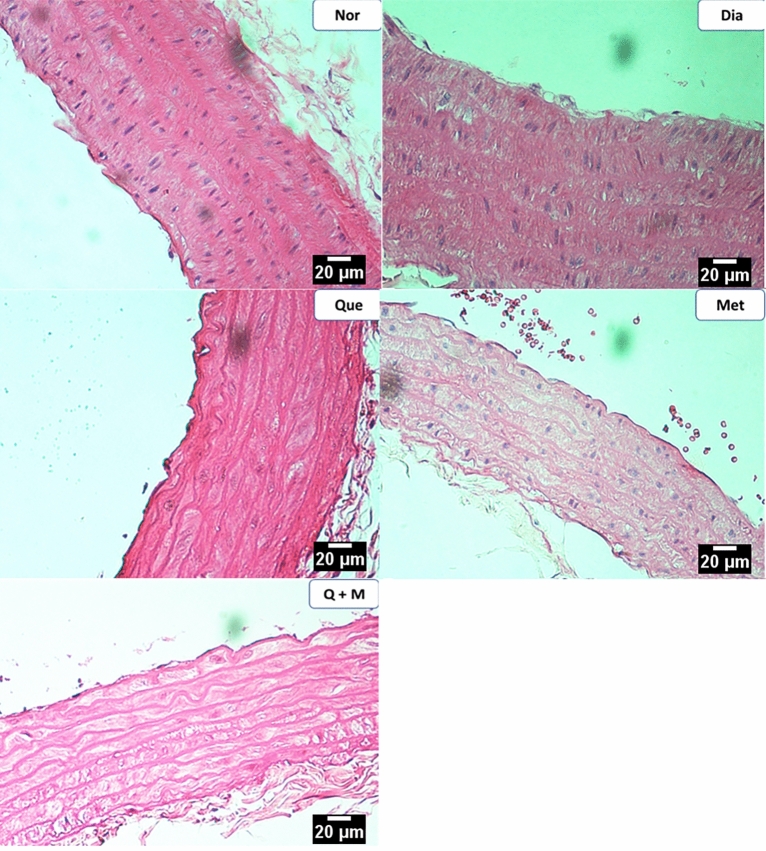
Abdominal and thoracic aortae
The rats in the control group showed a typical blood vessel architecture. STZ treatment caused focal fat depositions in tunica intima and mild tunica media enlargement. The diabetic rats treated with metformin or quercetin showed a mild degree of fatty deposits in the tunica intima focally, indicating the protective effect on the arteries. The diabetic rats treated with a combination of metformin and quercetin showed minimal fatty changes indicating a better protective effect on the aortae (Figs. 7, 8).
Figure 7.
The effect of test compounds on abdominal aortae histology in diabetic rats. Nor Normal, Dia Diabetic, Que Quercetin treated, Met Metformin treated, Q + M Quercetin + metformin treated diabetic rats.
Figure 8.
The effect of test compounds on thoracic aortae histology in diabetic rats. Nor Normal, Dia Diabetic, Que Quercetin treated, Met Metformin treated, Q + M Quercetin + metformin treated diabetic rats.
Immunohistochemistry
The expression levels of eNOS, 3-nitrotyrosine, VCAM-1, CD31, and SIRT1 in abdominal aortae were comparatively improved with quercetin + metformin combined treatment individual treatments. In diabetic rats, the 3-nitrotyrosine, VCAM-1, and CD31 expression were strong with 3 + density in s80% of the endothelium; however, eNOS and SIRT1 levels were less (between zero to 1 + density) in 10% of the endothelium. The sections of the normal control group showed a 2 + density of the endothelium of eNOS, 1 + in 30–40% of the endothelium of SIRT1, and minimal to 1 + density in 10–40% of endothelium for 3-nitrotyrosine, VCAM-1 and CD31 expression (Fig. S1).
The expression levels of eNOS, 3-nitrotyrosine, VCAM-1, and CD31 observed in thoracic aortae were similar to the levels in observed in the abdominal aortae except that SIRT1 expressed at high density with 3 + in 80% of the endothelium of diabetic rats and lower in normal control (1 + density in 10–40% of endothelium). The combination of quercetin + metformin improved the levels compared to individual treatment (Fig. S2).
Discussion
Hyperglycemia is the major contributing factor for dyslipidemia and endothelial dysfunction, proceed to cardiovascular complications18. Thus, targeting hyperglycemia, dyslipidemia, and endothelial dysfunction is a promising therapeutic approach. Besides this, a combination of drugs and natural products would treat complex diseases. In this milieu, the first-choice antidiabetic drug “metformin” was investigated along with a flavonoid “quercetin” in the treatment of hyperglycemia, dyslipidemia, and endothelial dysfunction in diabetic rat models. As per our knowledge, this is the first report on the synergistic effect of metformin and quercetin in diabetes.
The treatment with quercetin or metformin reduced the plasma glucose levels in diabetic rats. However, the diabetic rats treated with the combination of quercetin and metformin showed the most significant activity in reversing the elevated blood glucose levels compared to the treatment with quercetin or metformin alone. Both quercetin and metformin are well known for lowering plasma glucose levels and improving liver gluconeogenesis and serum lipid parameters3,19,20. The antihyperglycemic effect of metformin + quercetin has not been reported so far. The synergistic effect between quercetin and resveratrol in reversing hyperglycemia and endothelial dysfunction were reported21.
Dyslipidemia associated with diabetes is an important risk factor for endothelial dysfunction, which leads to atherosclerosis, myocardial infarction and coronary diseases22. The present study revealed that the combination of quercetin + metformin is more effective in reversing the lipid levels in diabetic rats than either quercetin or metformin alone. Garimella et al.23 showed that metformin treatment improves the lipid profile of individuals with T2DM. Mariee and co-workers showed that quercetin treatment significantly decreased triglycerides, total cholesterol, serum low-density lipoprotein, and high-density lipoprotein levels24. However, the effect of quercetin + metformin combination on lipid profile has not been investigated so far.
Quercetin, metformin and their combination reversed the elevated levels of liver enzymes, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) in diabetic rats. Moreover, plasma lactate dehydrogenase (LDH) levels were improved with combination treatment compared with individual treatments and control. The mechanism by which the combination therapy reverses the diabetic complications are not fully understood. Still, it could be due to the restoration of genes involved in glucose/lipid metabolism, liver function, cardiovascular system, and inflammation/immunity, which were altered by STZ-nicotinamide injection. Histological studies supported these results. Quercetin and metformin showed a synergistic effect in protecting hepatocytes and glomeruli.
Endothelium, a permeable barrier between the bloodstream and the outer vascular wall, regulates the vascular tone and structure. Endothelial cells synthesize and secrete nitric oxide (NO) through the action by endothelial NO synthase (eNOS). Under normal conditions, endothelium induces the production and release of NO. The cardiovascular protective effect of NO is mediated by preventing leukocyte adhesion, migration of leukocytes into the arterial wall, proliferation of the muscle cell, platelet adhesion, aggregation, and adhesion molecule expression. In diabetic conditions, the endothelium loses its protective role and becomes a pro-atherosclerotic structure. Perivascular adipose tissue (PVAT) plays a crucial role in regulating vascular functions. PVAT is known to release an unknown PVAT- released relaxation factor (PVAF) in rat aortae and other arteries25. In rat aortae, PVAT alters the relaxation responses to blood vessels by NO release and involving hydrogen peroxide production by PVAT. Therefore, PVAT has similar properties as that of the endothelium in regulating vascular tone and functions. In diabetic conditions, PVAT undergoes functional and structural alterations that impact vascular functions26. In this study, quercetin, metformin, and the combination increased the ACh-induced endothelium-dependent relaxation, SNP-induced endothelium-independent relaxation and reduced the α1-adrenergic agonist, PE-induced contraction in diabetic rat aortic rings ex vivo but did not have such effect in normal rat aortic rings. ACh and SNP showed reduced responses in aorta relaxation, whereas PE enhanced the aorta contraction in diabetic rats8. Increased production of superoxide anions inhibits the endothelial relaxation and enhanced the α1- receptor-induced contractions. These actions are mediated via either enhancing the vascular smooth muscle contraction or decreasing the nitric oxide level8.
Quercetin is reported to protect the eNOS levels in hyperglycemic conditions. It has been reported in the literature that metformin improves endothelial function through upregulation of eNOS15,27–31. Immunohistochemical studies revealed that eNOS (in abdominal and thoracic aortae) was downregulated in diabetic rats. The treatment of diabetic rats with test compounds (quercetin, metformin, and the combination) upregulated the eNOS levels (abdominal and thoracic aortae) compared to the untreated diabetic control. There was no significant difference in the activity of test compounds on eNOS levels in either abdominal or thoracic aortae.
Nitrotyrosine content is higher in endothelial cells of diabetic patients and thus induces endothelial dysfunction. The increase in NAD(P)H oxidase–induced O2 − production in diabetic conditions initiate oxidative/nitrative stress. Inactivation of NO by O2 − anion is associated with reduced NO bioavailability and thus causes endothelial dysfunction32. Immunohistochemical studies revealed that vascular tissues (abdominal and thoracic aortae) in diabetic control rats contain significantly elevated levels of 3-nitrotyrosine, compared to that in normal control. Nitrotyrosine (in abdominal and thoracic aortae) was highly upregulated in diabetic rats. The treatment with test compounds (quercetin, metformin, and the combination) reversed the elevated nitrotyrosine levels (abdominal and thoracic aortae) in diabetic rats. There was no significant difference in the activity of test compounds on nitrotyrosine levels in abdominal aortae versus thoracic aortae.
Vascular cell adhesion protein-1 (VCAM-1) facilitates the adhesion of lymphocytes, monocytes, basophils, and eosinophils to the surface of the endothelial cells, which promotes migration through the endothelium33. In this study, increased oxidative stress was associated with increased VCAM-1 in both abdominal and thoracic aortae. The combination therapy reverses the diabetes induced endothelial dysfunction through downregulation of the expression of VCAM-1 levels (abdominal and thoracic aortae) as compared to that in diabetic control. However, there was no significant difference in the VCAM-1 levels in abdominal versus thoracic aortae.
CD31 is a member of the immunoglobulin family, designated as PECAM-1 (platelet endothelial cell adhesion molecule 1). It is present in the endothelial intercellular junction. CD31 facilitates adhesion between endothelial cells (EC) and the inflammatory cells during inflammatory conditions and angiogenesis34–36. It has been reported that an increase in the CD31 number is associated with cardiovascular risk35. The treatment of diabetic rats with test compounds (quercetin, metformin, and combination) downregulated the CD31 levels in the abdominal and thoracic aortae.
Hyperglycemia in diabetes decreases SIRT-1 expression and thus activates p53 by increasing its acetylation. It has been reported that activation of SIRT-1 prevents hyperglycemia-induced vascular cell senescence and thereby improves vascular function in diabetic conditions37. In addition, the reductions in SIRT-1 deacetylation of eNOS can impair endothelium-dependent dilation (EDD)38. Quercetin, in diabetes, activates SIRT-1 leading to eNOS phosphorylation, NO production and intracellular cGMP in endothelial progenitor cells. It is reported that quercetin upregulates SIRT-1. Metformin has been shown to improve endothelial function and protect the macro-and microvasculature in diabetes14,39. It has been suggested that SIRT-1 is a key target for the endothelial-protective action of metformin. In this study, the treatment in diabetic rats with test compounds (quercetin, metformin, and combination) and the SIRT-1 levels (abdominal and thoracic aortae) in diabetic rats were found to be upregulated compared to those treated to diabetic control. There was no significant difference in the activity of test compounds on SIRT-1 levels in either abdominal or thoracic aortae.
In conclusion, the combination of quercetin with metformin showed a greater antidiabetic effect compared with metformin or quercetin individually. In addition, the combination effectively reversed the hyperglycemia-induced endothelial dysfunction in diabetic rats and regulated the expression of eNOS, 3-nitrotyrosine, VCAM-1, CD31 and SIRT-1 markers. Overall, the results from this study suggest that quercetin potentiates the activity of metformin to control diabetes.
Methods
Animals
Male Sprague Dawley rats (8 weeks old, 180 –220 g weight) were purchased from Animal Resource Unit, Faculty of Veterinary Medicine, University Putra Malaysia and housed 7 days for acclimatization (24 ± 1 °C, 50 ± 5% humidity and with a 12 h light/12 h dark cycle) before the experiments. All the rats had free access to standard rat chow (Gold Coin Feedmills, Malaysia) and reverse osmosis water. The experimental protocol was approved (Approval No.: PhD 4.11/JCM-46/2011) by the Research & Ethics Committee, International Medical University, Malaysia. All methods involving rats were carried out in accordance with standard conventional guidelines and regulations. We have also conducted the experiments in accordance with ARRIVE guidelines. Experimental animals were euthanized by cervical dislocation method which is one of the common methods for euthanasia.
Experimental design and induction of type 2 diabetes
Seventy-five rats were divided into five groups (15 rats in each group). The group of rats fed with a standard diet was referred to as normal control. The other rats were fasted 6–8 h prior to inducing diabetes. The diabetes was induced by intraperitoneal injection of streptozotocin (STZ; 60 mg/kg body weight, Amresco, USA) followed by nicotinamide (120 mg/kg body weight, Sigma-Aldrich, Malaysia) in a 15-min interval. On the 7th day after the injection, the plasma glucose levels in rats were greater than 11.0 mmol/l and were confirmed, diabetic. The rats were maintained in this condition for 7 to 8 weeks. Then, the rats were treated for 30 days with quercetin, Metformin, and quercetin + Metformin. The plasma glucose levels in all rats were determined at the baseline and the end of the treatment period.
Treatment with quercetin, metformin, and quercetin + metformin
Quercetin and metformin solutions were prepared in 1% (w/v) carboxymethyl cellulose (Sigma-Aldrich, Malaysia) and given orally once a day to the type 2 diabetes rats for 30 days. The rats in (1) quercetin group received quercetin 10 mg/kg body weight, (2) metformin group received 180 mg metformin per kg body weight, (3) quercetin + metformin group received 10 mg quercetin followed by 180 mg metformin per kg body weight, and (4) diabetic control received 1% (w/v) carboxymethyl cellulose. The dose of quercetin (10 mg kg−1 of body weight), was fixed based on our previous study that was conducted in our laboratory40. Similarly, the dose of metformin (180 mg metformin per kg body weight) was decided based on previously published studies that were conducted on rats under similar conditions41. Moreover, as the optimal response dose has been already established, we had decided to employ a single dose of quercetin and metformin based on previous reported studies.
Oral glucose tolerance test
After 30 days of treatment, the diabetic rats were fasted for 12 h and given an oral glucose load of 3 g/kg body weight through gastric intubation. The blood glucose levels were checked at intervals of 30 min up to 120 min by using the Accu-chek Performa blood glucose test strips (Roche Diagnostics, Germany).
Biochemical analysis
Blood was collected through the retro-orbital sinus of rats (after 30-day treatment), and the plasma was separated following the routine procedure. The plasma was analyzed for (1) aspartate aminotransferase (AST), (2) alanine aminotransferase (ALT), (3) lactate dehydrogenase (LDH), (4) glucose, (5) creatinine (CR), (6) total cholesterol (TC), (7) high-density lipoprotein (HDL), (8) low-density lipoprotein (LDL), and (9) triglycerides (TG) using Siemens Dimension Xpand Plus (Faculty of Veterinary Medicine, University Putra Malaysia).
Ex-vivo studies with rat aortic rings
The rats were euthanized by cervical dislocation method which is one of the common methods for euthanasia. The descending thoracic and abdominal aortae rings of the rats (~ 3–5 mm) were carefully removed as described by Boutouyrie et al.42. The aortae associated perivascular adipose tissue (PVAT) and endothelium (ED) were removed and categorized as indicated below. PVAT + ED: aortae rings with undamaged PVAT and intact ED. PVAT ˗ ED: aortae rings with undamaged PVAT and no ED. ˗ PVAT + ED: aortae rings with intact ED and no PVAT. ˗ PVAT ˗ ED: aortae rings without ED and PVAT. The isometric tension, effect of phenylephrine, acetylcholine and sodium nitroprusside on aortic rings were investigated.
Measurement of isometric tension
The inner glass-jacketed organ bath vessel was filled with 7 ml of Krebs physiological salt solution (KPSS (g/l); NaCl: 6.96; NaHCO3: 2.10; MgSO4: 0.29; KCl: 0.35; KH2PO4: 0.14; CaCl2: 0.350; glucose: 2.0; EDTA: 0.022) and bubbled continuously with 95% oxygen and 5% carbon dioxide at 37 °C. The aortic rings were then hooked on to an isometric force–displacement transducer (AD Instruments, Australia) and left in the Krebs solution at a tension of 1.5 g for 90 min for equilibrating and stabilizing the aortic rings. The aortic response output from the transducer was amplified and recorded in gram tension throughout the experiment using the Power Lab recording system (AD Instruments, Australia). After the equilibration, aortic rings were immersed in potassium chloride solution (80 mM) for 5 min to fix a baseline contractile response. The percentage of the KCl contraction was used to express the contractile response to phenylephrine. This step was repeated 3 times over intervals of 5 min. Then, the tissue was challenged with phenylephrine (10 μM), and the contraction was observed until it reached a plateau. Following this, acetylcholine (10 μM) was added, and the relaxant response was observed. The endothelium is considered intact if the percentage ACh-induced relaxation was higher than 50% of the initial phenylephrine-induced contraction. If the relaxation induced by acetylcholine was less than 50%, the endothelium was considered to be denuded.
Effect of phenylephrine, acetylcholine, and sodium nitroprusside on aortic rings
After establishing the endothelium integrity, the tissues were treated with increasing concentrations of phenylephrine (1 nM to 1 µM) at intervals of 4 min between contractions that lasted for 5 min. After the test, the tissues were washed several times using Krebs solution until the tension reached the basal levels in about 30 min. This test was performed to investigate the maximum contraction of tissue.
Simultaneously, to determine the maximum endothelial-dependent relaxation in rat aortae, the tissues were pre-contracted with phenylephrine (10 µM) before being exposed to cumulative acetylcholine concentrations (1 nM to 1 µM).
Besides this, after washing with Krebs solution, the tissues were subjected to pre-contractions with a similar concentration of phenylephrine before they were exposed to cumulative concentrations of sodium nitroprusside (1 nM to 1 µM). This process establishes the maximum endothelial-independent relaxation in the rat's aortae.
Histological analysis
After the 30 days treatment, the pancreas, liver, kidneys, and aortae were removed from the sacrificed rats. They were cleaned for adipose and connective tissues and fixed in 10% neutral buffered formalin. After fixation, the organs were embedded in paraffin to be cut into thin sections of ~ 4 μm. The appropriate sections were fixed on the glass slides and stained with hematoxylin and eosin. The stained slides were examined under a light microscope.
Immunohistochemistry
The tissue sections were mounted on glass slides and treated serially with xylene and ethanol (decreasing gradient). After water and 1 × amplifying immunohistochemistry (ICH) buffer wash, the slides were submerged in 1 × epitope unmasking solution and autoclaved. The autoclaved slides were cooled and washed with 1 × ICH buffer for 5 min with rocking. The wet tissue on slides was covered with 1–3 drops of peroxidase block and incubated at 28 °C for 30 min. Then, the tissue slides were washed with 1 × ICH buffer and kept in antibody amplifier™ and amplifying antibody dilution buffer (~ 3 ml) overnight at 4 °C. The tissue slides were washed with 1 × ICH buffer, covered with 1–3 drops of labelled polymer, and incubated at 28 °C for 30 min. The tissue sections were repeatedly covered with labelled polymer during incubation to avoid drying. After incubation, the slides were washed and stained with diaminobenzidine (DAB) solution and counter stained using 1% (w/v) hematoxylin. The stained slides were examined under a light microscope. The following monoclonal antibodies (Abcam, Malaysia) were used in this experiment. eNOS (ab50010; 1:100 dilution), nitrotyrosine (ab10282; 1:100 dilution), VCAM-1 (ab134047; 1:500 dilution), CD-31 (ab119339; 1:100 dilution), and SIRT-1 (ab110304; 1:200 dilution).
Statistical analysis
All results are stated as mean ± standard error of the mean (SEM). The phenylephrine dose–response curves were plotted as a percentage of high K+ solution-induced contraction per mg tissue weight against the phenylephrine concentration (log scale). The acetylcholine dose–response curves were plotted as a percentage of phenylephrine (0.1 µM) contraction per mg tissue weight against acetyl concentration (log scale). The sodium nitroprusside dose–response curves were plotted as a percentage of phenylephrine (0.1 µM) contraction per mg tissue weight against sodium nitroprusside concentration (log scale). The graphs were plotted using non-linear regression. Two-way ANOVA test followed by Bonferroni post-test were used to analyze the statistical significance for differences in responses among the different groups. A significant difference was accepted when the p-value was less than 0.05. All statistical analysis were performed using GraphPad Prism software (version 5; GraphPad Software Inc., USA).
Supplementary Information
Acknowledgements
Jestin Chellian was supported by a research grant (IMU 243/2011) from the International Medical University, Kuala Lumpur, Malaysia. We would like to thank Prof Dr Mak Joon Wah School of Postgraduate Studies and Research, International Medical University, Malaysia, Prof Dr Francis I Achike, College of Medicine, Texas A&M University, USA and Prof Dr Mohd Rais Bin Mustafa, Department of Pharmacology, Universiti Malaya, Malaysia for their supervision, technical advice and guidance.
Author contributions
J.C. performed the entire study, collected data, and wrote the draft manuscript; M.R.P. and K.K.M. involved in editing the manuscript; D.K.C. and P.K. conducted animal studies, data interpretation and manuscript editing; P.K. performed histopathological analysis; M.R.P. supervised the entire study. All authors revised the manuscript critically for intellectual content and have approved the final version.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jestin Chellian, Email: jestin_chellian@imu.edu.my.
Mallikarjuna Rao Pichika, Email: mallikarjunarao_pichika@imu.edu.my.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-25739-5.
References
- 1.Ahmad E, et al. Type 2 diabetes. Lancet. 2022 doi: 10.1016/S0140-6736(22)01655-5. [DOI] [PubMed] [Google Scholar]
- 2.Madempudi RS, et al. Probiotics in the management of diabetes. In: Brandelli A, et al., editors. Probiotics Advanced Food and Health Applications. Academic press; 2022. pp. 407–424. [Google Scholar]
- 3.Madempudi RS, et al. Efficacy of UB0316, a multi-strain probiotic formulation in patients with type 2 diabetes mellitus: A double blind, randomized, placebo-controlled study. PLoS ONE. 2019;11:e0225168. doi: 10.1371/journal.pone.0225168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chawla A, et al. Microvasular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J. Endocrinol. Metab. 2016;4:546–551. doi: 10.4103/2230-8210.183480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldberg RB. Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J. Clin. Endocrinol. Metab. 2009;9:3171–3182. doi: 10.1210/jc.2008-2534. [DOI] [PubMed] [Google Scholar]
- 6.Marín-Peñalver JJ, et al. Update on the treatment of type 2 diabetes mellitus. World J. Diabetes. 2016;17:354–395. doi: 10.4239/wjd.v7.i17.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, et al. Quercetin, inflammation and immunity. Nutrients. 2016;3:167. doi: 10.3390/nu8030167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dagher O, et al. Therapeutic potential of quercetin to alleviate endothelial dysfunction in age-related cardiovascular diseases. Front. Cardiovasc. Med. 2022;8:658400. doi: 10.3389/fcvm.2021.658400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torres-Piedra M, et al. A comparative study of flavonoid analogues on streptozotocin–nicotinamide induced diabetic rats: Quercetin as a potential antidiabetic agent acting via 11β-Hydroxysteroid dehydrogenase type 1 inhibition. Eur. J. Med. Chem. 2010;6:2606–2612. doi: 10.1016/j.ejmech.2010.02.049. [DOI] [PubMed] [Google Scholar]
- 10.Abdelmoaty MA, et al. Confirmatory studies on the antioxidant and antidiabetic effect of quercetin in rats. Indian J. Clin. Biochem. 2010;2:188–192. doi: 10.1007/s12291-010-0034-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vessal M, et al. Antidiabetic effects of quercetin in streptozocin-induced diabetic rats. Comp. Biochem. Physiol. C. Toxicol. Pharmacol. 2003;3:357–364. doi: 10.1016/S1532-0456(03)00140-6. [DOI] [PubMed] [Google Scholar]
- 12.Triggle CRA, et al. Metformin: Metformin: Is it a drug for all reasons and diseases? Metabolism. 2022;133:155223. doi: 10.1016/j.metabol.2022.155223. [DOI] [PubMed] [Google Scholar]
- 13.Sartoretto JL, et al. Metformin treatment restores the altered microvascular reactivity in neonatal streptozotocin-induced diabetic rats increasing NOS activity, but not NOS expression. Life Sci. 2005;21:2676–8269. doi: 10.1016/j.lfs.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 14.Majithiya JB, Balaraman R. Metformin reduces blood pressure and restores endothelial function in aorta of streptozotocin-induced diabetic rats. Life Sci. 2006;22:2615–2624. doi: 10.1016/j.lfs.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto T, et al. metformin normalizes endothelial function by suppressing vasoconstrictor prostanoids in mesenteric arteries from OLETF rats, a model of type 2 diabetes. Am. J. Physiol. Circ. Physiol. 2008;3:1165–1176. doi: 10.1152/ajpheart.00486.2008. [DOI] [PubMed] [Google Scholar]
- 16.Sena CM, et al. metformin restores endothelial function in aorta of diabetic rats. Br. J. Pharmacol. 2011;2:424–437. doi: 10.1111/j.1476-5381.2011.01230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheang WS, et al. metformin protects endothelial function in diet-induced obese mice by inhibition of endoplasmic reticulum stress through 5’ adenosine monophosphate-activated protein kinase-peroxisome proliferator-activated receptor pathway. Arterioscler. Thromb. Vasc. Biol. 2014;4:830–836. doi: 10.1161/ATVBAHA.113.301938. [DOI] [PubMed] [Google Scholar]
- 18.Association AD. Standards of medical care in diabetes–2012. Diabetes Care. 2012;1:S11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen S, et al. Therapeutic effects of quercetin on inflammation, obesity, and type 2 diabetes. Mediat. Inflamm. 2016;2016:1–5. doi: 10.1155/2016/9340637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bjornstad P, et al. metformin improves insulin sensitivity and vascular health in youth with type 1 diabetes mellitus: Randomized controlled trial. Circulation. 2018;25:2895–2907. doi: 10.1161/CIRCULATIONAHA.118.035525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang DK, Kang HS. Anti-diabetic effect of co-treatment with quercetin and resveratrol in streptozotocin-induced diabetic rats. Biomol. Ther. (Seoul) 2018;2:130–138. doi: 10.4062/biomolther.2017.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petrie JR, et al. Diabetes, hypertension, and cardiovascular disease: Clinical insights and vascular mechanisms. Can. J. Cardiol. 2018;5:575–584. doi: 10.1016/j.cjca.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garimella S, et al. Effect of Metformin on lipid profile of type II diabetes. Int. J. Intg. Med. Sci. 2016;11:449–453. [Google Scholar]
- 24.Mariee AD, et al. Protective effect of dietary flavonoid quercetin against lipemic-oxidative hepatic injury in hypercholesterolemic rats. Pharm. Biol. 2012;8:1019–1025. doi: 10.3109/13880209.2012.655424. [DOI] [PubMed] [Google Scholar]
- 25.Miao CY, Li ZY. The role of perivascular adipose tissue in vascular smooth muscle cell growth. Br. J. Pharmacol. 2012;3:643–658. doi: 10.1111/j.1476-5381.2011.01404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qi XY, et al. Perivascular adipose tissue (PVAT) in atherosclerosis: A double-edged sword. Cardiovasc. Diabetol. 2018;1:134. doi: 10.1186/s12933-018-0777-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaliora AC, et al. Dietary antioxidants in preventing atherogenesis. Atherosclerosis. 2006;1:1–17. doi: 10.1016/j.atherosclerosis.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 28.Gargiulo P, et al. metformin decreases platelet superoxide anion production in diabetic patients. Diabetes Metab. Res. Rev. 2002;2:156–159. doi: 10.1002/dmrr.282. [DOI] [PubMed] [Google Scholar]
- 29.Bellin C, et al. Generation of reactive oxygen species by endothelial and smooth muscle cells: Influence of hyperglycemia and metformin. Horm. Metab. Res. 2006;11:732–739. doi: 10.1055/s-2006-955084. [DOI] [PubMed] [Google Scholar]
- 30.Faure P, et al. An insulin sensitizer improves the free radical defense system potential and insulin sensitivity in high fructose-fed rats. Diabetes. 1999;2:553–557. doi: 10.2337/diabetes.48.2.353. [DOI] [PubMed] [Google Scholar]
- 31.Scarpello JH, Howlett HC. Metformin therapy and clinical uses. Diabetes Vasc. Dis. Res. 2008;3:157–167. doi: 10.3132/dvdr.2008.027. [DOI] [PubMed] [Google Scholar]
- 32.Magenta A, et al. Nitric oxide, oxidative stress, and p66Shc interplay in diabetic endothelial dysfunction. Biomed. Res. Int. 2014 doi: 10.1155/2014/193095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krieglstein CF, Granger DN. Adhesion molecules and their role in vascular disease. Am. J. Hypertens. 2001;S3:44S–54S. doi: 10.1016/S0895-7061(01)02069-6. [DOI] [PubMed] [Google Scholar]
- 34.Zhou Z, et al. Antibody against murine PECAM-1 inhibits tumor angiogenesis in mice. Angiogenesis. 1999;2:181–188. doi: 10.1023/A:1009092107382. [DOI] [PubMed] [Google Scholar]
- 35.DeLisser HM, et al. Involvement of endothelial PECAM-1/CD31 in angiogenesis. Am. J. Pathol. 1997;3:671–677. [PMC free article] [PubMed] [Google Scholar]
- 36.Chiva-Blanch G, et al. High adherence to the Nordic diet is associated with lower levels of total and platelet-derived circulating microvesicles in a Norwegian population. Nutrients. 2019;5:1114. doi: 10.3390/nu11051114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Orimo M, et al. Protective role of SIRT1 in diabetic vascular dysfunction. Arterioscler. Thromb. Vasc. Biol. 2009;6:889–894. doi: 10.1161/ATVBAHA.109.185694. [DOI] [PubMed] [Google Scholar]
- 38.Donato AJ, et al. SIRT-1 and vascular endothelial dysfunction with ageing in mice and humans. J. Physiol. 2011;18:4545–4554. doi: 10.1113/jphysiol.2011.211219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mather KJ, et al. Improved endothelial function with metformin in type 2 diabetes mellitus. J. Am. Coll. Cardiol. 2001;5:1344–1350. doi: 10.1016/S0735-1097(01)01129-9. [DOI] [PubMed] [Google Scholar]
- 40.Machha A, et al. Quercetin, a flavonoid antioxidant, modulates endothelium-derived nitric oxide bioavailability in diabetic rat aortas. Nitric Oxide. 2007;16(4):442–447. doi: 10.1016/j.niox.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 41.Gad MZ, et al. Effects of pioglitazone and metformin on carbohydrate metabolism in experimental models of glucose intolerance. Int. J. Diabetes Metab. 2010;18:132–138. [Google Scholar]
- 42.Boutouyrie P, et al. In vivo/in vitro comparison of rat abdominal aorta wall viscosity: Influence of endothelial function. Arterioscler. Thromb. Vasc. Biol. 1997;7:1346–1355. doi: 10.1161/01.ATV.17.7.1346. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.