Abstract
Cartilage is used as a grafting material for tympanoplasty. The rigidity of the cartilage is the main concern. There are debates regarding slicing the cartilage when it is used as a graft. Therefore, this systematic review and meta-analysis aimed to compare the hearing results of full vs. partial-thickness cartilages in patients undergoing cartilage tympanoplasty. We systematically searched google scholar, PubMed, Cochrane, Ovid, Scopus, and gray literature including the references of the selected studies, and conference abstracts which were published up to 6 May 2020. The search syntax for identifying studies was: ((Cartilage) AND (tympanoplasty) AND (thickness)). The literature search found 1047 articles. After eliminating duplicates, 908 studies remained; from these, we excluded observational studies, reviews, case reports, and non-randomized trials, and 12 studies remained. Finally, only 5 articles were included for analysis. The pooled standardized mean difference (SMD) for the post-operative gap was −0.87 95% CI: (−1.66, −0.08) (I2 = 87.1%, p < 0.001). The pooled SMD of the reduction in gap in the full-thickness group was 2.84, 95% CI (1.39–4.3), I2 = 93.2%, p < 0.001). The pooled SMD of the reduction in gap in the partial-thickness group was 4.02, 95% CI (1.97–6.02), I2 = 95.3%, p < 0.001). The pooled results of this systematic review showed that partial-thickness cartilage graft has better hearing outcomes than full-thickness in patients undergoing cartilage tympanoplasty.
Keywords: Tympanoplasty, Cartilage, Fascia, Hearing
Introduction
Traditionally, skin, fascia, vein, perichondrium, and dura mater were used for tympanoplasty[1], while in 1595, tympanoplasty using cartilage as a grafting material was introduced by Utech which is indicated in patients with retraction pockets, recurrent perforations, and atelectatic ears.[2] Cartilage use has excellent results for the reconstruction especially in patients with middle ear pathology, and eustachian tube dysfunction [3]. One critical point in the case of cartilage tympanoplasty is the thickness of the cartilage which could affect hearing results [4]. Based on this point using cartilage, Zahnert et al. recommended the best thickness of the cartilage for tympanoplasty as 0.5 mm compared to the full-thickness[5], while Dornhoffer et al. reported better outcome in patients who underwent tympanoplasty using full-thickness cartilages [3].
There are controversies regarding using different cartilage thicknesses for patients who are candidates for cartilage tympanoplasty. Therefore, we designed this systematic review and meta-analysis to compare the hearing results of full vs. partial-thickness cartilage grafts in patients undergoing cartilage tympanoplasty.
Methods
Literature Search
We systematically searched google scholar, PubMed, Cochrane, Ovid, Scopus, and gray literature including the references of the selected studies, and conference abstracts which were published up to 6 May 2020.
The inclusion criteria were:
Randomized clinical trials
The studies that compared the hearing results and the graft take in the type 1 cartilage tympanoplasty between full-thickness cartilage and partial-thickness cartilage
Exclusion criteria were: case reports, cohort studies, and case–control studies.
Search Strategy and Data Extraction
The search syntax for identifying studies was:
((Cartilage) AND (tympanoplasty) AND (thickness)).
Two independent researchers evaluated the studies and extracted the data. Data regarding the name of the first authors, publication year, number of cases in each group of the study, pre-operative and post-operative gap, hearing gain, graft take, surgical technique (endoscopic or microscopic), and method of cartilage slicing were extracted.
Risk of Bias Assessment
We evaluated the risk of potential biases using the Cochrane Collaboration for assessing the risk.[6]
Statistical Analysis
All statistical analyses were performed using STATA version 13.0 (Stata Corp LP, College Station, TX, USA). We used the inverse variance with random effects model.
The standardized mean difference (SMD) was calculated for comparisons. For the graft take variable, the pooled prevalence was calculated. Inconsistency (I2) was calculated to determine heterogeneity.
Results
The literature search found 1047 articles that were assessed. After eliminating duplicates, 908 studies remained; from these, we excluded observational studies, reviews, case reports, and non-randomized trials. Finally, 12 studies remained. After the full-text evaluation, only 5 articles were included for analysis (Fig. 1). The other 7 articles didn’t compare full-thickness with partial-thickness and only used one type of cartilage in those clinical trials.
Fig. 1.
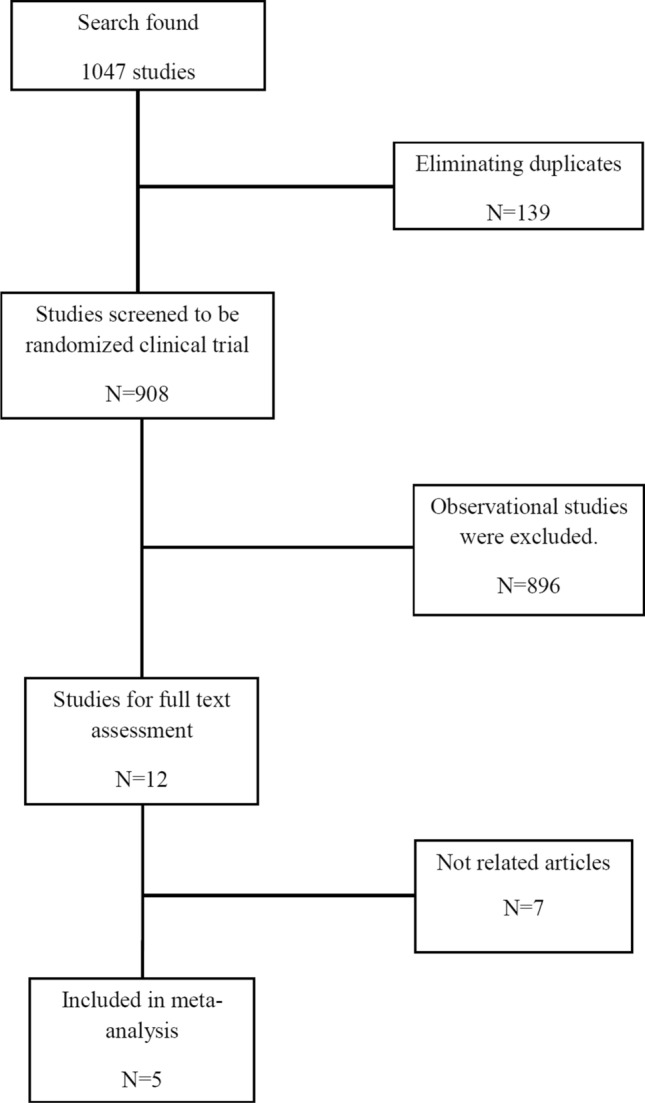
Flow diagram summarizing the selection of the studies
Included articles were published between 2007 and 2020 and the follow-up duration varied between 2 and 9 months (Table 1). Totally, 113 patients were evaluated in the full-thickness group (group A) and 114 in the partial-thickness group (group B).
Table 1.
Characteristics of the included articles
| First author | Publication year | Study duration | Follow up duration | Method of cartilage slicing | Surgical technique |
|---|---|---|---|---|---|
| Guindi1 | 2016 | July 2014 and February 2015 | 6 months | Slicing the tragal cartilage with a surgical scalpel blade No. 11 while held between two glass slides | Not mentioned |
| Atef4 | 2007 | January 2003 and March 2004 | 8–9 months | The tragal cartilage disk was bisected to half of its thickness using a No. 15 scalpel under microscopic magnification | Microscopic |
| Sadek7 | 2019 | February 2017 to November 2017 | 3 months |
Kurz® Precise Cartilage Splitter 0.5 mm thickness tragal cartilage obtained |
Microscopic |
| Mokbel8 | 2013 | July 2004 to July 2010 | Not mentioned |
Partial thickness (0.2 mm) where thinning of the cartilage was done by a special instrument called Conchotome (Kurz Co. Germany) |
Microscopic |
| Parelkar9 | 2020 | February 2014 to September 2015 | 2 months | The tragal cartilage was sliced to a partial thickness (∼0.4 mm) | Endoscopic |
Characteristics of the included articles are summarized in Table 1. Pre-operative and post-operative gap and reduction in the gap are shown in Table 2. The quality assessment of the included studies is also shown in Table 3.
Table 2.
Main findings of the included studies
| Group A Full thickness |
Group B Partial thickness |
|
|---|---|---|
| Guindi1 | ||
| Number | 15 | 15 |
| Pre-operative gap | 30.15 ± 5.42 | 30.22 ± 6.49 |
| Post-operative gap | 20.44 ± 5.34 | 10.74 ± 4.29 |
| Reduction in gap | 9.71 | 19.48 |
| Graft take | 14 (93.33%) | 14 (93.33%) |
| Atef4 | ||
| Number | 28 | 29 |
| Pre-operative gap | 21.3 ± 3.72 | 22.07 ± 2.62 |
| Post-operative gap | 10.44 ± 2.21 | 10.28 ± 1.65 |
| Reduction in gap | 10.85 | 11.79 |
| Graft take | 27 (96.4%) | 28 (96.5%) |
| Sadek7 | ||
| Number | 15 | 15 |
| Pre-operative gap | 43.6 ± 11.8 | 40.5 ± 8.8 |
| Post-operative gap | 31.9 ± 8.9 | 27.3 ± 4.9 |
| Reduction in gap | 11.7 | 13.2 |
| Graft take | 14 (93.8%) | 14 (93.8%) |
| Mokbel8 | ||
| Number | 30 | 30 |
| Pre-operative gap | 29.3 ± 2.55 | 29.7 ± 2.74 |
| Post-operative gap | 13.8 ± 2.40 | 9.9 ± 2.08 |
| Reduction in gap | 15.5 | 19.8 |
| Graft take | 30 (100%) | 30 (100%) |
| Parelkar9 | ||
| Number | 25 | 25 |
| Pre-operative gap | 40.80 ± 7.46 | 39.40 ± 7.95 |
| Post-operative gap | 26.72 ± 8.08 | 26.40 ± 8.6 |
| Reduction in gap | 14.08 | 13 |
| Graft take | 22 (88%) | 17 (68%) |
Table 3.
Quality assessment of the included studies
| First author | Sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessor | Incomplete outcome data | Selective outcome reporting | Others |
|---|---|---|---|---|---|---|---|
| Guindi1 | Yes | unclear | No | No | Unclear | Yes | Yes |
| Atef4 | Yes | unclear | Yes | Yes | Unclear | Yes | Yes |
| Sadek7 | Yes | unclear | No | No | Unclear | Yes | Yes |
| Mokbel8 | Yes | unclear | No | No | Unclear | Yes | Yes |
| Parelkar9 | Yes | unclear | No | No | Unclear | Yes | Yes |
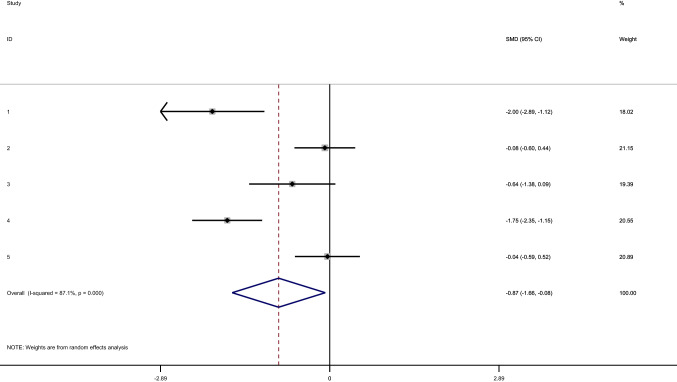
The pooled SMD for the post-operative gap (group B–group A) was −0.87 95% CI: (−1.66, −0.08) (I2 = 87.1%, p < 0.001) (Fig. 2).
Fig. 2.
The pooled SMD of the post-operative gap
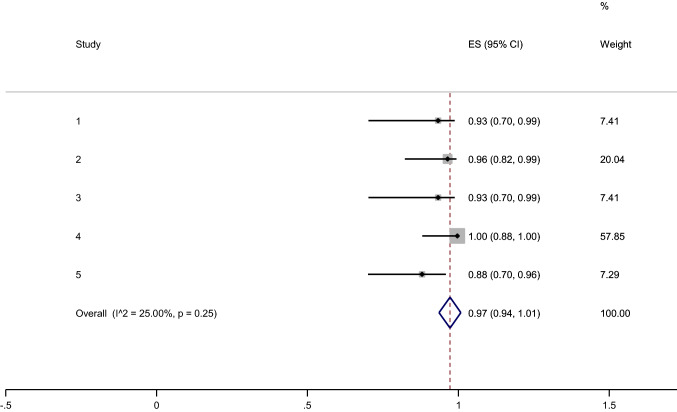
The pooled frequency of graft take in group A (full-thickness) was 97%, 95% CI: (94–100%) (I2:25%, p = 0.25) (Fig. 3).
Fig. 3.
The pooled frequency of graft take in group A (full thickness)
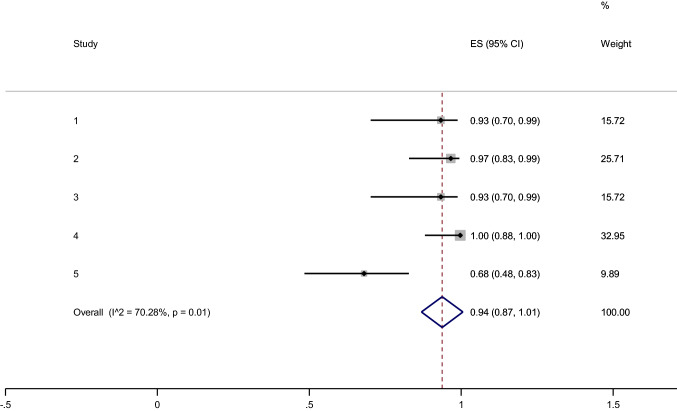
The pooled frequency of graft take in group B (partial-thickness) was 94%, 95% CI: (87–100%) (I2:70.2%, p = 0.01) (Fig. 4).
Fig. 4.
The pooled frequency of graft take in group B (partial thickness)
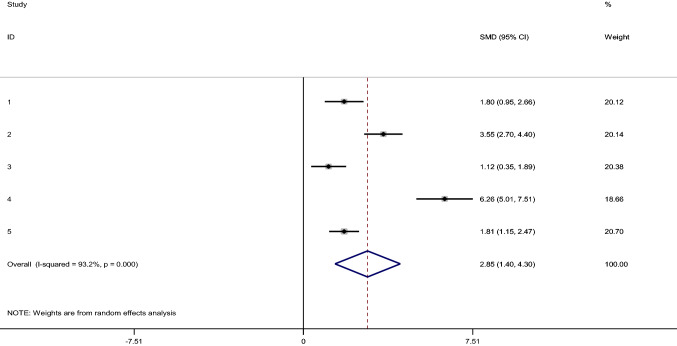
The pooled SMD of the reduction in gap in group A (full-thickness) was 2.84, 95% CI (1.39–4.3), I2 = 93.2%, p < 0.001) (Fig. 5).
Fig. 5.
The pooled SMD of the reduction in gap in group A (full thickness)
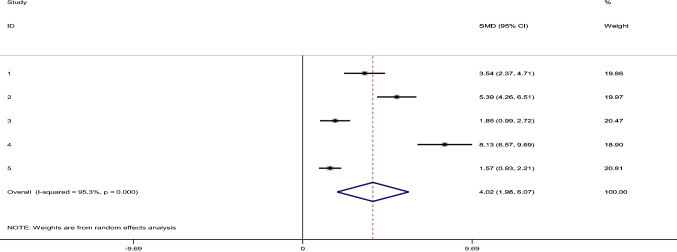
The pooled SMD of the reduction in gap in group B (partial-thickness) was 4.02, 95% CI (1.97–6.02), I2 = 95.3%, p < 0.001) (Fig. 6).
Fig. 6.
The pooled SMD of the reduction in gap in group B (partial thickness)
Discussion
To our knowledge, this is the first systematic review and meta-analysis evaluating the hearing results of full vs. partial-thickness cartilage in patients undergoing cartilage tympanoplasty type I.
The results showed that hearing results (post-operative gap) after implanting partial-thickness cartilage improved more significantly than the full-thickness group (The pooled SMD for the post-operative gap was −0.87 95% CI: (−1.66, −0.08)).
Two authors Guindi et al. and Mokbel et al.[1, 7] reported significantly better hearing outcomes in patients who had partial-thickness cartilage grafts than the full-thickness group, while the other three individual studies did not find significant difference regarding the hearing outcome (post-operative gap) [4, 8, 9]. The pooled results of this systematic review showed that partial-thickness cartilage graft has better outcomes than full-thickness.
The results also showed that the pooled frequency of graft-take in the full-thickness group was 97% and in the partial-thickness group was 94% which is indicative of good graft take in both groups. The frequency of graft-take in group A ranged between 88–100% in included studies and 68–100% in group B. This finding could be based on the rigid quality of the cartilage that prevents infection or middle ear pressure change [7].
Atef et al.[4] reported that most patients had subtotal perforation (20 in full-thickness and 19 in partial-thickness groups). In the full-thickness group, 6 patients had posterior perforation, and 2 patients had anterior perforation. Also, in the partial-thickness group, 9 patients had posterior perforation, and 1 patient had anterior perforation. The average size of the perforation was not exactly mentioned in the other studies.
One of the cautions in interpreting the results of this systematic review is the method of slicing and the thickness of the slices in the partial-thickness group. In previous studies, some authors believed that applying a cartilage graft of 0.5 mm had better outcomes [5].
All included studies used tragal cartilage for full-thickness, and partial-thickness graft except for Mokbel et al.[7] that did not report where the cartilage graft was harvested from.
By comparing the hearing results of the fascia graft, full-thickness graft, and partial-thickness graft (0.5 mm), Nemade and Dabhokar found that the best balance between stability and acoustic sensitivity is observed in the partial-thickness graft group [10].
In another study, Murbe et al. reported better sound transmission properties in patients with partial-thickness cartilage grafts [11]. On the other hand, Atef et al. found that partial-thickness cartilages are not superior to full-thickness cartilages graft [4].
By following one thousand patients, Dornhoffer preferred the application of full-thickness of cartilages instead of partial-thickness as cartilage thinning will cause curves which would be difficult to use [3].
After the introduction of tympanoplasty by Wullstein and Zöllner, a wide range of grafts were used while temporalis fascia was the most acceptable graft [12, 13].
Previously, the beliefs about conductive hearing loss in patients who underwent cartilage tympanoplasty made its usage difficult but the comparison of different grafts showed better hearing results or no inferiority [4].
Gerber et al. reported no superiority regarding the hearing results of cartilage versus fascia graft, while others reported superiority of cartilage grafts to other types of grafts in tympanoplasty [14–16].
The suggestion about slicing the cartilage due to hearing loss based on thick rigid cartilage use, makes the application of thinned cartilage grafts possible. In 2000, Zahnert et al. found that the best cartilage thickness was 0.5 mm compared to 0.7–1 mm[5] while Lee et al. suggested cartilage thickness of 0.1–0.2 mm.[17]
This systematic review and meta-analysis have some limitations. The cartilage thickness was not the same in the partial-thickness group. Furthermore, the duration of the follow-up period was not the same in all studies and was sometimes too short. Also, the number of included studies was not too much.
Conclusion
The pooled results of this systematic review showed that partial-thickness cartilage graft has better hearing outcomes than full-thickness cartilage graft in patients undergoing cartilage tympanoplasty.
Acknowledgements
The research was fully sponsored by Otorhinolaryngology Research Center of the Tehran, University of Medical Sciences. This manuscript has not been previously published and is not under consideration in the same or substantially similar form in any other peer-reviewed media.
Funding
Researchers received no specific funding, grants, or other support.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guindi SS, Abd el-moez MK, Hussein MA, Magdy IM. Evaluation of healing and hearing results of full thickness cartilage graft versus partial thickness cartilage graft in tympanoplasty. Med J Cairo Univ. 2016;84:679–84. [Google Scholar]
- 2.Utech H. Uber diagnostische und therapeutische Moglichkeiten der Tympanotomie bei Schalleitungstorungen. Z Laryn Rhinol. 1959;38:212–221. [PubMed] [Google Scholar]
- 3.Dornhoffer J. Cartilage tympanoplasty: Indications, techniques, and outcomes in A 1,000-patient series. Laryngoscope. 2003;113(11):1844–1856. doi: 10.1097/00005537-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Atef A, Talaat N, Fathi A, Mosleh M, Safwat S. Effect of the thickness of the cartilage disk on the hearing results after perichondrium/cartilage island flap tympanoplasty. ORL. 2007;69(4):207–211. doi: 10.1159/000101540. [DOI] [PubMed] [Google Scholar]
- 5.Zahnert T, Hüttenbrink K-B, Mürbe D, Bornitz M. Experimental investigations of the use of cartilage in tympanic membrane reconstruction. Otol Neurotol. 2000;21(3):322–328. doi: 10.1016/s0196-0709(00)80039-3. [DOI] [PubMed] [Google Scholar]
- 6.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mokbel KM, Thabet E-SM. Repair of subtotal tympanic membrane perforation by ultrathin cartilage shield: evaluation of take rate and hearing result. Eur Arch Otorhinolaryngol. 2013;270(1):33–36. doi: 10.1007/s00405-011-1903-5. [DOI] [PubMed] [Google Scholar]
- 8.Sadek AA, Talaat MM. Half-thickness tragal cartilage slicing improves the sound transmission properties in endoscopic myringoplasty among Egyptians. Egypt J Neck Surge Otorhinolaryngol. 2019;5(1):1–9. doi: 10.21608/ejnso.2019.57899. [DOI] [Google Scholar]
- 9.Parelkar K, Thorawade V, Marfatia H, Shere D. Endoscopic cartilage tympanoplasty: full thickness and partial thickness tragal graft. Braz J Otorhinolaryngol. 2020;86(3):308–314. doi: 10.1016/j.bjorl.2018.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nemade SV, Dabholkar JP. Healing and hearing results of temporalis fascia graft Vs cartilage graft (Full thickness and half thickness) in type I tympanoplasty. Online J Otolaryngol. 2014;4(3):1–19. [Google Scholar]
- 11.Mürbe D, Zahnert T, Bornitz M, Hüttenbrink KB. Acoustic properties of different cartilage reconstruction techniques of the tympanic membrane. Laryngoscope. 2002;112(10):1769–1776. doi: 10.1097/00005537-200210000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Wullstein H. Funktionelle Operationen im mittelohr mit hilfe des freien Spaltlappen-transplantates. Archiv für Ohren-, Nasen-und Kehlkopfheilkunde. 1952;161(2–6):422–435. doi: 10.1007/BF02129204. [DOI] [Google Scholar]
- 13.Zöllner F. The principles of plastic surgery of the sound-conducting apparatus. J Laryngol Otol. 1955;69(10):637–652. doi: 10.1017/S0022215100051240. [DOI] [PubMed] [Google Scholar]
- 14.Gerber MJ, Mason JC, Lambert PR. Hearing results after primary cartilage tympanoplasty. Laryngoscope. 2000;110(12):1994–1999. doi: 10.1097/00005537-200012000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Milewski C. Composite graft tympanoplasty in the treatment of ears with advanced middle ear pathology. Laryngoscope. 1993;103(12):1352–1356. doi: 10.1288/00005537-199312000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Duckert LG, Müller J, Makielski KH, Helms J. Composite autograft" shield" reconstruction of remnant tympanic membranes. Am J Otol. 1995;16(1):21–26. [PubMed] [Google Scholar]
- 17.Lee CF, Chen JH, Chou YF, Hsu LP, Chen PR, Liu TC. Optimal graft thickness for different sizes of tympanic membrane perforation in cartilage myringoplasty: a finite element analysis. Laryngoscope. 2007;117(4):725–730. doi: 10.1097/mlg.0b013e318031f0e7. [DOI] [PubMed] [Google Scholar]