Abstract
Depression is one of the most common mood disorders in the late-life population and is associated with poor quality of life and increased morbidity, disability and mortality. Nevertheless, in older adults, it often remains undetected and untreated. This narrative review aims at giving an overview on the main definitions, clinical manifestations, risk and protective factors for depression in the elderly, and at discussing the main reasons for its under/misdiagnosis, such as cognitive decline and their overlapping symptomatology. A practical approach for the global and multidisciplinary care of the older adult with depression, derived from cross-checking evidence emerging from the literature with everyday clinical experience, is thus provided, as a short and flexible “pocket” guide to orient clinicians in recognizing, diagnosing and treating depression in the elderly.
Keywords: late-life depression, older adults, mood disorders, geriatric depression
Introduction
Depression is one of the most common mood disorders in the late-life population.1,2 The prevalence of depressive disorder in the over 60 years old population is about 5.7%.3 However, it increases with age, to reach the peak of 27% in over-85 individuals.1 Interestingly, the prevalence still increases and reaches the 49% in those living in communities or nursing homes,4,5 regardless of the severity or the definition of depression considered.1
Late-life depression (LLD) can be distinguished according to the age at which the first depression occurred. Early-onset depression (EOD) identifies the persistence or recurrence in old age of a depression previously diagnosed throughout adulthood, while late-onset depression (LOD) represents a depressive disorder developed de novo in old age.6
DSM 5 identifies a cluster of depressive symptoms, namely depressed mood, loss of interest and pleasure, weight loss or gain, fatigue, insomnia or hypersomnia, psychomotor agitation or retardation, decreased concentration, thoughts of death and/or suicide and worthlessness.3
However, LLD is characterized by an atypical cluster of symptoms, ie somatic symptoms which are predominant compared to mood symptoms, so it is important to be aware of this particular clinical presentation in order to not underestimate LLD.
Moreover, the complex spectrum of Late-Life Depression (LLD) goes beyond the main diagnostic entities of unipolar depressive disorders, such as Major Depressive Disorder (MDD) and persistent depressive disorder.7 Relevant depressive symptoms which do not fulfill the criteria for a diagnosis of depression have nevertheless a significant clinical relevance, because of their association with poorer quality of life and increased disability; however, they are often undetected and untreated, despite a very small chance of spontaneous remission.8
Depressive symptoms produce clinically significant distress and impairment in daily life, notching social, familiar, and occupational areas of functioning. Depression is entangled in a bidirectional relationship with somatic morbidity finally resulting in an increase in patients’ burden of disability and frailty and augmenting mortality.9 In fact, besides being a risk factor and a predictor of poor prognosis for many conditions, like diabetes, cancer, cardiovascular diseases, dementia,10–12 depression can be precipitated and perpetuated by chronic medical conditions typical of the aging process. A longitudinal study of 3214 healthy elderly individuals proved that Mild Cognitive Impairment (MCI), as well as smoking and mobility, vision, and subjective memory impairments, can significantly increase the risk of depression.13
Thus, the diagnosis of depression is challenging in elderly people, since it often presents with multifaceted and more somatic symptoms compared to adults,14 thus resembling a “real” medical organic disease.5
Also, treatment is demanding, because of the complexity of older patients, who more frequently have a pharmacological-resistant depression and require a multidimensional and, possibly, a multi-professional equipe taking charge.
The objective of this review is, on the one hand, to explain the strong impact of geriatric depression on individual and caregivers’ quality of life and the difficulties in recognizing and prescribing the adequate treatment and, on the other hand, to propose a practical approach for the global and multi-disciplinary care of the older adult with depression, from diagnosis up to the definition of a customized treatment. In order to do so, a short and flexible “pocket” guide is here proposed as a tool to orient clinicians in recognizing, diagnosing and treating depression in the elderly. To the best of our knowledge, there is no tool currently available, such as the here proposed pocket guide, thought to be flexible and easily adaptable to the most disparate clinical contexts.
Reviewing the Literature on Geriatric Depression: Definitions, Risk and Protective Factors, Symptomatology and Clinical Variants
Geriatric Depression Syndrome: Characterization and Symptomatology
While the depression severity appears to remain stable across the lifespan, what really differentiates depression in middle and old age concerns qualitative differences in the clinical presentation of the symptomatology (Table 1).
Table 1.
Depression Symptoms in Younger and Older Adults: Typical and Atypical Presentation
| Symptoms and Clinical Presentation | Older Adults | Younger Adults | |
|---|---|---|---|
| DSM* 5 core symptoms | Depressed mood | ↓ | ↑ |
| Anhedonia | ↑ | ↓ | |
| Somatic symptoms | Loss of appetite | Hyperphagia | |
| Insomnia | Hypersomnia | ||
| Physical tiring/lack of energy | Fatigue | ||
| Cognitive deficits | Poor concentration | ||
| GI** complaints | – | ||
| Psychomotor retardation | Agitation | ||
Abbreviations: *DSM, Diagnostic and Statistical Manual of Mental disorders; **GI, gastrointestinal.
As an example, considering depressed mood (sadness or dysphoria) and loss of interest (anhedonia), which are the two core symptoms of Major Depressive Disorder (MDD) according to the DSM 5, they can be manifested differently in older adults compared younger people,15 as well as inappropriate guilt or feelings of worthlessness.16 Notably, regarding the first of these two core symptoms (ie depressed mood), feelings of dysphoria or sadness are frequently absent in older adults,7 underlying a specific variant of geriatric depression indicated as “depression without sadness”,17 characterized by lack of interest, sleep difficulties, lack of hope, loss of appetite and thoughts of death.
On the contrary, symptoms like lack of vigor and withdrawal, which are referred to the second core symptom of MDD, are usually more pronounced. In fact, “loss of interest” is usually pronounced, since older adults tend to be more apathetic.18 Suicidal thoughts are frequent in LLD, together with state of anxiety, especially in the morning.19
What characterizes even more LLD is a shift towards somatic symptoms,18 which become prominent and vary in their manifestations compared to early onset depression, although the criteria symptoms remain the same. For example, while increased appetite and overeating may frequently occur in younger individuals, loss of appetite and weight are more common in late life.20 Similarly, considering that sleep duration declines with age, decreased sleep is more common in LLD compared to hypersomnia, which is more typically experienced by younger depressed adults.18 Fatigue is expressed both as physical tiring and lack of energy rather than a mental symptom, while the “poor concentration” symptom could be manifested more as a broader cognitive impairment where memory loss is related to executive dysfunction.21 In general, older people manifest more vague and gastrointestinal somatic complaints, together with hypochondriasis.22 Lastly, psychomotor retardation is more common in LLD than agitation, leading to disturbances in speech, facial expression, fine motor behavior, and gross locomotor activity, which exceed the general slowdown observed in normal aging.23
It is therefore clear that one of the main challenges in recognizing the diagnostic features of geriatric depression is the overlap of its typical symptoms with those of other comorbid physical or neurologic conditions and, in general, with the typical signs of frailty (ie, weight loss, psychomotor slowing and exhaustion).
In fact, the somatic symptoms that in younger adults are indicative of depression, in the elderly may be correlated with aging and may not be indicative of a specific pathology, as well as could be due to other comorbid conditions. Thus, while including somatic symptoms in geriatric screening for depression regardless of their etiology (inclusive approach) may lead to false positives,24 it remains true that they cannot be completely excluded from the diagnostic framework (as the exclusive approach, instead, proposes), as aging and its associated conditions do not necessarily justify all these aspects. An alternative is represented by the aetiological approach, in which somatic symptoms are considered only if they are not primarily due to another medical condition.25 In general, a good clinical practice is to ask people about their mood when they refer to non-specific physical complaints, as to assess the presence of mood problems that older adults tend not to autonomously express, as previously stated.
Geriatric Depression Syndromes
Because of its peculiar features and complexity, different specific variants of geriatric depression have been proposed to better frame its presentations.
Among these, the “depletion syndrome”,26 characterized by lack of interest, sleep difficulties, lack of hope, loss of appetite and thoughts of death, described the common condition of “depression without sadness” seen in older adults.
Another condition is referred to as “reversible dementia”. In some cases, in fact, older patients suffering from a severe depression development with marked cognitive impairment can induce the clinicians to misdiagnose dementia.27 However, in these patients, the cognitive symptomatology recedes with the remission of depression, even if a part of them subsequently develops a proper dementia.28 The label of “pseudodementia” this condition was addressed as, is no longer used, because of the complex relationship between depression and dementia, which represents an interaction between pathological processes, with more than one illness masquerading as another.29
In fact, the complex entanglement involving aging-related processes, network dysfunction and depressive symptoms is also supported by the fact that two distinct syndromes regarding LOD can be recognized, ie the “depression-executive dysfunction syndrome” (DED) and vascular depression. DED30 develops in patients whose fronto-striatal pathways are affected by aging-related or pathological changes. It is marked by psychomotor retardation, loss of interest, suspiciousness, lack of insight and pronounced disability, but rather mild vegetative symptoms and less prominent depressive ideation.31 Moreover, individuals affected by this syndrome have impaired performance in tests of executive functioning (namely verbal fluency, response inhibition, problem solving, cognitive flexibility, working memory and ideomotor planning).32 Vascular depression, instead, is characterized by psychomotor slowing, lack of initiative and apathy, and it is typically observed in patients with a medical history of hypertension and cognitive impairment.31 The “vascular depression” hypothesis postulates that cerebrovascular disease may predispose, precipitate, or perpetuate some geriatric depressive disorders,31 disrupting networks supporting affective and cognitive functions.32
Risk and Protective Factors
The identification of factors that can increase or protect from the risk of developing depression in the elderly population is crucial in order to promote prevention strategies, but also for the best comprehensive approach to this disease. The literature has shown that suffering from a chronic disorder4,33–35 or cognitive impairment,36 having a weak social, emotional and supportive network,5,37 living isolated, taking care of relatives with chronic disease,38 losing a partner,39 can facilitate the rising of depressive symptoms. Furthermore, gender differences, well known in younger patients, persists also into late life, so being a woman can represent a risk factor.40 On the other hand, having a high level of self-esteem,41 resilience42 and sense of control,41 keeping a healthy lifestyle43 and having a medium/high level of cognitive reserve44 represent protective factors for the rising of depression in elderly age. Table 2 provides a detailed overview of the main risk and protective factors involved in geriatric depression.
Table 2.
Risk and Protective Factors for Depression in Elderly
Recognizing Geriatric Depression in the Elderly: A Current Challenge
Depression in older adults is often under- or misdiagnosed and thus undertreated or inappropriately treated. Reasons for underdiagnosis are several and include psychosocial factors too. The first issue concerns the prejudice that depression is a normal phase of aging, because of the medical and situational conditions typical of older age, such as the limitations imposed by functional disability, health concerns and psychological stressors as decreasing social contacts, transitions in key social roles (ie, retirement) and grief.15 Although, mood deflection is certainly understandable, it does not imply that it should be neglected, nor that it is not treatable, especially when it is a source of suffering and impairs functioning. Another barrier for depression recognition involves stigmatization. In fact, some individuals are reluctant to accept a diagnosis of depression, and often both patients and clinicians may hope to find a “medical illness” in order to avoid the stigma of a psychiatric diagnosis.20 Moreover, older adults are less likely to express mood problems, like dysphoria or worthlessness, and may describe their symptoms in a more “somatic” way.7 In general, older adults often find physical illness to be more acceptable than psychiatric illness.45 At the same time, physicians may lack screening for depression because of more urgent physical problems or because they wrongly attribute depressive symptoms to comorbid medical illness.46
In addition to underdiagnosis, another factor that contributes to undertreatment is misdiagnosis. As previously stated (Table 1), in the elderly depression has an atypical presentation, including persistent complaints of pain, headache, fatigue, apathy, agitation, insomnia, weight loss, low attention and other nonspecific symptoms which can overlap with or be confused with other physical illnesses and dementia. This can lead clinicians to pursue an expensive medical workup, when they may not be able to recognize these problems as being part of a depressive episode. At the same time, older adults may relate their symptoms to a medical condition, thus not seeking the proper help.18 Thus, it is necessary to gain insight on variability in the presentation of specific depressive symptoms across the lifespan.
Confounding Factors: Cognitive Impairment and Depression in Older Adults
Another specific challenge in the accurate diagnosis of depression concerns its entanglement with cognitive impairment and dementia. In fact, there is a substantial overlapping in the clinical presentation of late-life depression and early-stage dementia: a subjective perception of memory loss, as well as psychomotor retardation and a lack of motivation in answering at cognitive tests are typically observed in depressed older adults, and can be interpreted as signs of dementia.47 Moreover, in older adults, depression is commonly accompanied by cognitive deficits, which are present in 20 to 50% of cases.48,49 On the other hand, depressive symptoms are a common neuropsychiatric symptom of Alzheimer’s Disease (AD).50 Still, given the prevalence of both syndromes in the older population, they can also independently co-occur, and the two diagnoses are not mutually exclusive.36
Geriatric depression is characterized by cognitive deficits involving executive functions, such as problem solving, planning, decision-making and inhibition, along with selective and sustained attention and working memory impairment.51 Other deficits, involving some aspects of episodic memory and visuospatial functions, may be secondary to executive dysfunction.28 These symptoms remain significant even after the remission of the depressive symptomatology.52 In a 10-year longitudinal study, Ly et al53 have shown that depressed older adults perform worse than compared healthy controls in cognitive tasks, maybe for the neurotoxic effects of depression and reduced cognitive reserve.
The relationship between late-life depression and cognitive decline is even more complex, considering that, besides mimicking each other, they also can coexist and be mutually a risk factor.
On the one hand, in fact, older adults with dementia can develop pure depressive symptoms. Clinical depression in these cases can be either reactive to the diagnosis or a relapse of a previously diagnosed depression.54 Olin et al proposed diagnostic criteria for “depression of Alzheimer’s disease”, including the presence of at least three significant depressive symptoms during the same two-week period that represents a significant perturbation from previous functioning, when all the criteria of AD are fulfilled.55
On the other hand, Ly et al53 found that late-onset depression, but not EOD, was associated with a more rapid cognitive decline over time. These findings suggest that EOD, whose symptoms are persistent or recurrent in old age, is a vulnerability factor that alters cognitive abilities even in healthy aging, representing a risk factor for dementia.21 On the contrary, LOD could be a real harbinger of dementia. In particular, highly educated people are more likely to show depressive symptoms as initial presentation of dementia, probably because cognitive reserve may delay the onset of cognitive, but not depressive, symptomatology.56
Reviewing the Literature on Therapeutic Approaches to Depression in the Elderly
The effective management of geriatric depression builds upon different strategies, involving both pharmacological and non-pharmacological options that have to be considered based on the patient’s characteristics and psychosocial environment, in order to shape a tailored and comprehensive intervention. In fact, the most effective approach is the biopsychosocial one, combining pharmacotherapy, psychotherapy and an array of lifestyle and social environment’s personalized modifications. These therapies and good practices have shown to be effective, resulting in improved quality of life, enhanced functional capacity, possible improvement in medical health status, increased longevity, and lower health care costs.14
Pharmacological Treatment of Depression in Older Adults
Late-life depression compared with that of younger patients shows a lower response rate to antidepressants, nonetheless several treatment options exist.
When prescribing drugs, including psychotropic drugs, to older adults’ attention should be paid to pharmacokinetic and pharmacodynamic changes associated with aging. In fact, drug distribution varies, due to the increase in body fat that leads to an increasing distribution volume and elimination of half-life for lipophilic drugs. Renal filtration rate decrease enhances the problem of drug elimination. In addition, hepatic metabolism, besides being affected by aging, is also influenced by other concomitant drugs that induce or inhibit cytochrome P-450 metabolic enzymes.
In the choice of antidepressant treatment, the patient’s previous response to treatment should be considered, as well as his/her other comorbidities and medications, in order to minimize the risk of side effects and drug–drug interactions. In addition, somatic symptoms associated with depression like anxiety, psychotic symptoms, insomnia/hypersomnia, hyperphagia/poor nutrition should be considered.
The second-generation antidepressants, ie Selective Serotonin Reuptake Inhibitors (SSRIs) and Selective Norepinephrine Reuptake Inhibitors (SNRIs), are considered the first-line treatment options for depression in the elderly, because of their efficacy,57 tolerability and safety profile. Except for paroxetine, they have lower anticholinergic effects than older antidepressants (ie tricyclics) and are thus well tolerated by patients with cognitive impairment or cardiovascular disease. SSRIs are also good for improving cognition,58 while SNRIs are a good first choice in comorbid neuropathic pain. Most frequent SSRIs and SNRIs side effects include hyponatremia,59 nausea and gastro-intestinal bleeding,60 so periodic blood exams are recommended. Another second-generation antidepressant is mirtazapine that improves appetite being useful for anorexia,61 and whose sedative side effect can be useful for insomnia.62 A novel antidepressant, vortioxetine, a multimodal serotonin modulator, seems to be promising for elderly people since it also has a positive effect on cognition, independently of the improvement in depression.63
When psychotic symptoms coexist, the addition of antipsychotics to antidepressants may be more effective than antipsychotics or antidepressants monotherapy, as reported by Meyers et al,64 who found that the combination treatment of olanzapine plus sertraline was not only more effective than monotherapy but also equally tolerated.
Psychotherapy in Geriatric Depression
As for younger adults, also for older people psychotherapeutic approaches are to be encouraged, even in the presence of cognitive decline, since that treatment’s versatility gives the therapist the opportunity to adapt it to the patient’s needs and characteristics and to his/her physical and emotional environment.
In the following paragraphs a brief overview of the principal psychotherapy approaches available for older persons with depression is shortly provided.
Problem Adaptation Therapy (PATH)
PATH is a home-delivered psychosocial intervention, which has shown to lead to significant positive results in elderly with depression, by providing help in emotional regulation.65,66 This kind of therapy puts the focus on strategies personalized on each patient’s needs (ie memory and organizational deficits, behavioral/functional limitations, interpersonal tension, social isolation and anhedonia).65 PATH looks to lessen the negative impact of emotions by improving pleasurable activities, using a problem-solving approach and integrating environmental adaptations and compensatory strategies, for instance using calendars, checklists and strategies to sustain or shift attention.
Engage Therapy
This stepped therapy targets behavioral domains grounded on neurobiological constructs using simple and efficient behavioral techniques.31 The intervention aims at modulating patient’s response using the “reward exposure” strategy, working on three main behavioral domains, ie “negativity bias” (negative valence system dysfunction), “apathy” (arousal system dysfunction), and “emotional dysregulation” (cognitive control dysfunction), and add strategies targeting these domains.
Problem Solving Therapy (PST)
PST is an 8-week intervention that consists in a seven-step process to solve problems, including problem orientation that directs patient attention to one problem at a time, problem definition that helps patients select relevant information to determine what the root problem is, goal setting that focuses attention to the desired outcome, brainstorming that helps patients consider different ways for reaching the goal, decision-making, to evaluate the alternative solutions likelihood and picking the best choice, and action planning that involves a step-by-step plan for the patient to implement his/her solution.67
Supportive Therapy
This home-delivered psychotherapy focuses on nonspecific therapeutic factors as facilitating expression of affect, conveying empathy, highlighting successful experiences, and imparting optimism. Supportive Therapy reduces depression and disability in older patients with major depression, cognitive impairment, and disability.65
Interpersonal Therapy
Interpersonal Therapy is a psychodynamic therapy that focuses on complicated grief, role transition, role dispute/interpersonal conflicts, and interpersonal deficits.68 During the first phase of treatment, therapists help patients to explore and understand depressive symptoms through a psychoeducational approach. In later phases, problems are identified and understood in the interpersonal context. In the final phase, the therapist focuses on the gains and limitations of therapy and the prevention of relapses.68
Computerized Cognitive Remediation (CCR)
CCR has demonstrated improvements in mood and self-reported function in depressed patients similar to those obtained through the Problem Solving Therapy.81 CCR is suitable for patients with an MMSE score of at least 24/30.68 It makes use of a video game to treat depression (EVO), personalized, self-administered and continuously adapted to the patients’ aptitude both at baseline and progress in treatment.67 Unlike Problem Solving Therapy, the EVO participants showed generalization to untrained measures of working memory and attention, as well as negativity bias. CCR is relatively inexpensive and can be used at the patients’ homes, thus minimizing barriers to access of care, common in older adults.31
Electroconvulsive Therapy (ECT)
An effective treatment for depression in elderly population, available from mental health specialists, is electroconvulsive therapy (ECT).69 In ECT, an electrical stimulus is given for a brief period to produce a generalized seizure. The treatment is effective especially for psychotic depression, severe suicidality, treatment-refractory depression, catatonia, and depression with severe weight loss and anorexia, moreover, is indicated for older old (≥80 years).70 A meta-analysis of the cognitive effects of ECT suggests its relative safety and the transient character of its effects on cognition.71 Compared to antidepressants, ECT induces a higher speed of remission.72
Practical Guidance for Depression Diagnosis and Treatment in the Elderly: A Pocket Guide for the Daily Clinical Management
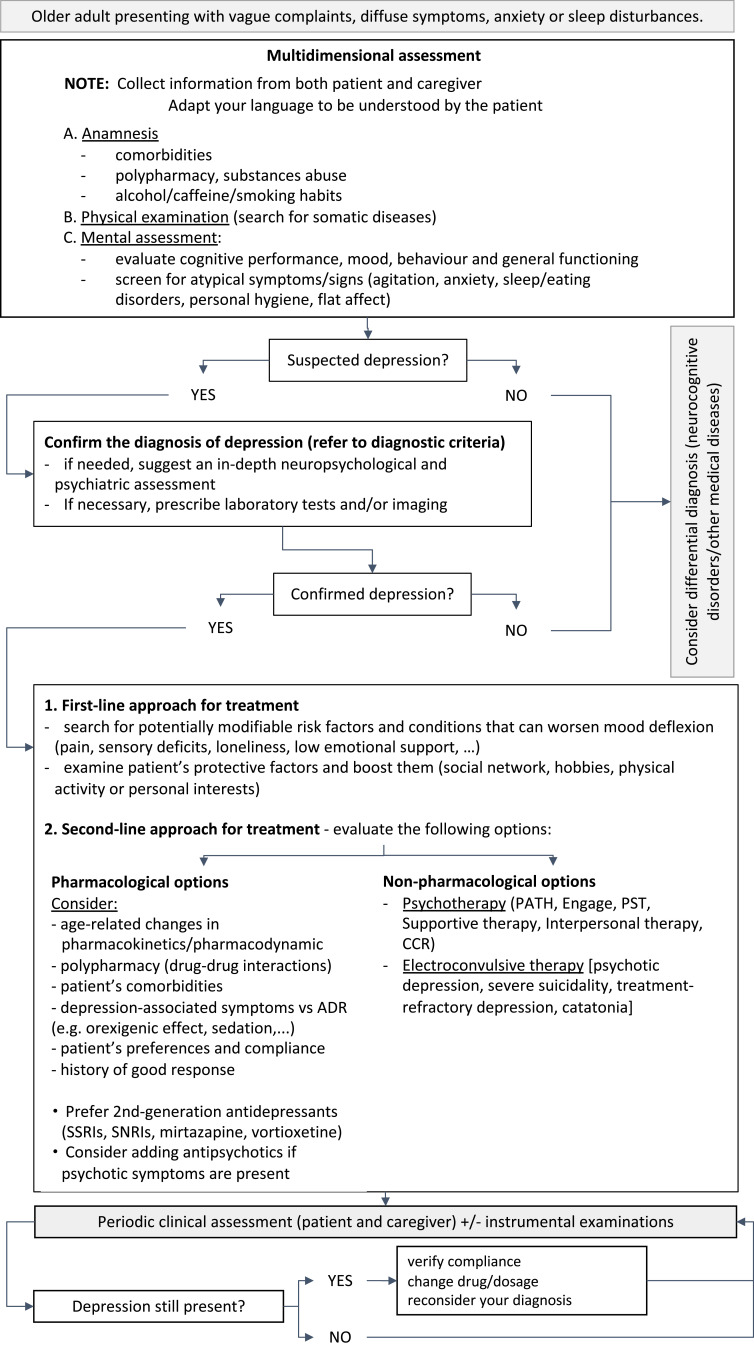
If the proper recognition of geriatric depression remains at current challenge, the key aspects and main evidence presented here, along with a long interdisciplinary team clinical experience, lead to the identification of some guidelines to optimize the recognition and the adequate differential diagnosis of depression in the elderly. All the contents discussed below are summarized in the pocket guide, as a practical reference for a comprehensive diagnostic procedure in everyday clinical practice (see Figure 1).
Figure 1.
Pocket guide for the assessment and management of geriatric depression in everyday clinical practice.
Clinicians should carefully consider depression among possible differential diagnosis, particularly when: patients refer to their attention with vague complaints as pain, fatigue and diffuse symptoms and/or suffer from anxiety or sleep disturbances; some clues are evident, such as poor personal hygiene, flat affect and slumped posture; the patient tends to frequently use healthcare resources, as calls or visits to practitioners.46,48
In these cases, an accurate screening for the underlying risk factors and a collection of anamnestic data, which include medical, psychological and cognitive remote and recent history, is crucial to evaluate all potential contributing or protecting factors. Furthermore, to assess the individual’s protective factors (that mainly deal with aspects related to social network, hobbies, physical activity or personal interests) will also have a positive clinical implication in the management and treatment of depressive symptoms from a non-pharmacological point of view, by knowing the activities that could be pleasant and stimulating, as well as his or her personal resources.
Moreover, caregivers and families can be helpful, since they may provide information about the patient’s mood, behavior and general functioning. In fact, they could notice relevant changes that are not reported by the patient, especially if she or he has poor insight, as in the case of the co-occurrence of cognitive impairment.
When talking to patients, instead, it is important to adequate to the social and cultural background of older adults. As discussed in the previous sections, they are not used to deal with mental health issues and to verbally express concerns about their mood. Thus, the clinician should prefer to use expressions such as “Are you feeling low/down?” instead of directly asking “Are you depressed?” in order to address the stigma, and discuss mental health referral in the broader context of other medical conditions to increase the acceptability.38 At the same time, all the healthcare professionals should promote the sensitization of the elderly to mood disorders and more generally to mental health, so that they can themselves become more attentive and aware in recognizing their emotional and psychological difficulties.
Clinicians can count on several validated tools to quantitatively assess the presence and severity of depression, namely self-report scales, clinician rating scales and structured interviews. Despite their popularity and their clear advantages, some considerations have to be taken into account when dealing with older adults. First of all, these tools were mostly developed for young adults, so they do not always catch the appropriate features for the elderly.73 This also falls on their validity and reliability, which are strictly related to the population they are based on.74 Self-reports are widely used because of their quickness and ease of administration. However, they are susceptible to some respondent’s characteristics, such as low educational attainment or cognitive impairment, which can influence the true comprehension of questions or of the response format.75 In general, in the case of older adults with cognitive impairment, it is preferable to avoid self-reports and use alternative assessment methods that include direct observation and family reports.7 Moreover, especially for patients with comorbidities, items with somatic content may need further clarifications, since somatic symptoms could be misattributed to depression.76 Lastly, visual impairment can obstacle the completion of self-report scales: in these cases, the clinician can either propose an enlarged copy of the scale or administrate it orally. The use of clinician rating scales overcomes some of these issues, since they are based on the direct observation of a trained professional. If clinician rating scales offer a more accurate measurement of depression, it has been found that they are less sensitive in detecting changes in mild forms of depression.77 Structured interviews offer the possibility to facilitate the comprehension of questions, as well as to deeper investigate aspects that need to be better clarified, as the nature of somatic symptoms; however, because of the time and skills requested for their administration, their utility is limited.78 Overall, there is no single superior assessment method; rather, it is important that clinicians are aware of their strengths and shortcomings and informed about the psychometric properties of the main tools, so that they can choose the most appropriate instrument depending on the characteristics of the individuals. Moreover, using multiple methods and sources of information (ie, multidimensional assessment) has been shown to be the most effective approach.78
When depressive symptoms are detected and a diagnosis of LLD is probable, among all the other factors, also the domestic and family context has to be looked at, that is, whether there are dynamics that can exacerbate the depressive symptomatology of the patient. This could be the case, for example, of a dysfunctional interaction in the patient-caregiver dyad or of some psycho-affective characteristics of the caregiver himself (for example, if he or her is depressed as well), likewise tensions in family relationships or other health or financial issue of relevant psychological impact.
Lastly, it is important to exclude somatic causes of depression and to characterize a depressive episode or symptoms through patient history, clinical examination, laboratory tests, and/or imaging. In fact, LLD can per se be distinguished into a proper LOD or the recurrence of an EOD and, as stated, this has some clinical implications. Alternatively, depression can be secondary to a general medical condition or to a substance or medication use, considering that multimorbidity and polypharmacy are extremely common conditions among older adults.79 Moreover, depressive symptoms could be the manifestation of a cerebrovascular disease or of a prodromal stage of AD, thus having a primarily organic origin. It is also important, in any case, to repeat when possible both the instrumental examinations (namely imaging techniques for the investigation of regional brain glucose metabolism, as FDG-PET) and the administration of cognitive and/or psychological screening tools in order to re-evaluate the overall diagnosis at a follow-up after 6–9 months. In fact, since LLD is a treatable and reversible condition, when a diagnosis of depression is made and a pharmacological or non-pharmacological treatment has been proposed, there should be evidence of efficacy. Otherwise, the question arises if the depressive symptoms observed were secondary to another cause (so, the diagnosis was incorrect) or the therapeutic approach chosen was not the most suitable one.
Depression and Cognitive Impairment: How to Address Differential Diagnosis?
Whereas depressive and cognitive disorders often coexist in the elderly, it is crucial to distinguish a geriatric depression that includes cognitive deficits from a mild dementia with depressive symptoms. What needs to be determined from a clinical point of view, in particular, is whether or not the picture observed will evolve into dementia.
Time is a first important criterion: while in the case of dementia symptoms will develop with a slow progression over several years, depressive symptomatology onset can be dated with more precision and the progression of symptoms is more rapid.48,80 Another relevant cue concerns awareness. Patients with reversible dementia complain more about their cognitive disturbances, highlighting their failures and disability and precisely describing the pattern of their deficits; older adults with dementia, on the contrary, usually lack insight and their description of cognitive loss is vague.80
From a neuropsychological point of view, evidence has been described about a different characterization of cognitive profiles of patients with AD and depression that can be striking in the differential diagnosis.
First of all, patients with LLD show a prominent dysexecutive profile, with a slight impairment in global cognition.21 Conversely, a broader cognitive impairment, with significant deficits of orientation, language, praxis and memory is typical of AD.81 Secondly, although a memory disturbance is visible in both AD and LLD, they have a different functional origin. The episodic memory impairment of AD, due to hippocampal damage, is defined by a recall deficit that does not improve with cueing or recognition testing, since storage processes are primarily affected.82 Depression, instead, leads to an insufficient allocation of attentional resources and executive dysfunction that affect encoding or retrieval strategies,83 without a pure storage deficit. Thus, a differential diagnosis can be made with specific memory testing based on effective and specific encoding of information and retrieval facilitation with cueing.82 Inefficacy of cueing and a flat learning curve despite exposure is typical of AD, while an improvement with exposure and a normal recall with retrieval cues are distinctive features of depression.36
In general, patients with depression have a suboptimal cognitive performance due to poor motivation that leads them to give up the task more easily, not pay enough attention and use ineffective strategies, so their overall performance is more influenced by the cognitive load of the task and the extent to which it relies on executive functions.83
In addition to all the steps that have to be gone through, and the factors that have to be taken into account for a comprehensive assessment that includes depression among the differential hypothesis, some general guidelines are here suggested about organizational aspects that can be implemented to improve the detection of depressive symptoms in the elderly.
First, given the predominance of somatic symptoms in late-life depression, as well as their tendency to focus more on their physical (rather than mental) issues, it is plausible that older adults who suffer from depression do not spontaneously refer to a mental health professional at first, but to other figures, such as general practitioners, physicians or other health professionals. For this reason, it would be important to improve the knowledge about late-life depression presentation, as well as the capacity to carry out screening activities, of specialists of other disciplines. In fact, although a formal diagnosis of depression is not part of their role, they could improve the detection of potential cases because of their position, as it is the case of occupational and physical therapists, nurses or general practitioners.45
Furthermore, different professional figures, as psychiatrists, geriatricians, psychologists and neuropsychologists, often have to interface with older adults’ depressive symptoms in the presence of multimorbidity and/or cognitive deficits, and thus answer questions concerning the differential diagnosis of depression. It is of paramount importance for each specialist to evaluate individuals in their whole complexity. In this regard, a multidimensional assessment should always be provided, in order to take into account all the aspects discussed above, such as risk and protective factors, medical and psychological history, social context and recent life events. Moreover, when appropriate, specialists should choose a multidisciplinary approach, referring patients to other professionals that can have a role in the differential diagnosis or in identifying the most appropriate therapeutic option. When possible, it would be a valuable resource for figures with different and complementary competences to work together.
For example, in the specific case of older adults with depressive symptoms with a subjective perception or signs of cognitive impairment, geriatricians and neuropsychologists could manage outpatient visits and consultations in wards together, considering the tangled characteristics of LLD discussed above. In this way, these professional figures can provide a first screening of cognitive functioning and the characterization of some deficits that will help in the differential diagnosis between depression and dementia. Moreover, this synergy can help to consciously investigate the presence of a mood disorder and, where necessary, to offer to the patient a more accurate psychological and cognitive assessment, targeted medical investigations and therefore a tailored treatment.
In case older adults are aware of having a mood problem, they mainly refer to the psychiatrist. Notwithstanding the crucial role and competence of psychiatrists in this context, it is still important for them to consider older adults in their whole complexity. In this regard, they should provide a multidimensional assessment that takes into account all the aspects previously stated (ie, risk and protective factor, medical and psychological history, social context, recent life events…) and, when appropriate, have a multidisciplinary approach, referring patients to other professionals that can have a role in the differential diagnosis or in identifying the most appropriate therapeutic approach.
Another professional figure that frequently has to cope with the differential diagnosis of depression are geriatricians, since in their clinical practice they consult with patients who show signs or have a subjective perception of cognitive or neuropsychiatric problems. Both in outpatient visits and in consultations in wards, it could be a valuable resource for the geriatricians to be assisted by a neuropsychologist. For the characteristics of LLD discussed above, it would be beneficial for patients if the geriatrician and the psychologist/neuropsychologist could work together in the assessment of older adults, both for the outpatient visits and for the consultation inwards.
In this way, these professional figures can synergistically provide a first screening of cognitive functioning and the characterization of some deficits that will help in the differential diagnosis between depression and dementia. Moreover, it can help to consciously investigate the presence of a mood disorder and, where necessary, to offer the patient a more accurate psychological and cognitive assessment, targeted medical investigations and therefore a tailored treatment.
In conclusion, as a general indication, it is overall important to periodically screen older adults for depression. Furthermore, patients who already are in treatment for depression need to be periodically re-evaluated, since the persistence of a depressive symptomatology suggests that the therapeutic approach chosen (pharmacological or not) should be revised.
Conclusions
This review, beyond reviewing depression, its clinical main characterizations and current challenges had the goal to propose a few guidelines born from the “every-day” clinical activity carried-out on this population. A “pocket guide” has been produced in order to hopefully orient clinicians in their daily clinical management of depression and in sensitizing different professionals to a comprehensive, global and multidisciplinary assessment of a complex disorder affecting complex individuals such as the elderly are. Shortly, after a first multidimensional assessment, clinicians are provided with clinical cues orienting their diagnostic process. Whereas the diagnosis of depression is confirmed, by also excluding other co-occurrent/different pathologies (ie cognitive decline), a first- and second-line therapeutic approaches are suggested, including both pharmacological and non-pharmacological options. Lastly, follow-ups and periodic clinical assessments are strongly recommended to monitor individuals over time.
Finally, by considering not only the risk, but also the protective factors that may help people in facing depression along late life, this review also indirectly encourages clinicians in promoting active social, cognitive and psycho-affective lifestyles in the elderly, as crucial, modifiable factors that may significantly influence the natural course of their aging.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sjöberg L, Karlsson B, Atti AR, Skoog I, Fratiglioni L, Wang HX. Prevalence of depression: comparisons of different depression definitions in population-based samples of older adults. J Affect Disord. 2017;221:123–131. doi: 10.1016/j.jad.2017.06.011 [DOI] [PubMed] [Google Scholar]
- 2.Blazer DG. Depression in late life: review and commentary. J Gerontol a Biol Sci Med Sci. 2003;58(3):249–265. doi: 10.1093/gerona/58.3.M249 [DOI] [PubMed] [Google Scholar]
- 3.Global Health Data Exchange (GHDx). The Institute for Health Metrics and Evaluation (IHME). Whasington. Available from; 2022. https://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/d780dffbe8a381b25e1416884959e88b. Accessed June 10, 2022. [Google Scholar]
- 4.Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr Scand. 2006;113(5):372–387. doi: 10.1111/j.1600-0447.2006.00770.x [DOI] [PubMed] [Google Scholar]
- 5.Park M, Unützer J. Geriatric depression in primary care. Psychiatr Clin North Am. 2011;34(2):469. doi: 10.1016/j.psc.2011.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rhebergen D, Stek M. Late-life depression. In: Sinclair AJ, Morley JE, Vellas B, Cesari M, editors. M Pathy’s Principles and Practice of Geriatric Medicine. John Wiley & Sons Ltd; 2022:71. [Google Scholar]
- 7.Balsamo M, Cataldi F, Carlucci L, Padulo C, Fairfield B. Assessment of late-life depression via self-report measures: a review. Clin Interv Aging. 2018;13:2021–2044. doi: 10.2147/CIA.S178943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meeks TW, Vahia IV, Lavretsky H, Kulkarni G, Jeste DV. A tune in “a minor” can “b major”: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J Affect Disord. 2011;129(1–3):126–142. doi: 10.1016/j.jad.2010.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rotella F, Mannucci E. Diabetes mellitus as a risk factor for depression. A meta-analysis of longitudinal studies. Diabetes Res Clin Pract. 2013;99(2):98–104. doi: 10.1016/j.diabres.2012.11.022 [DOI] [PubMed] [Google Scholar]
- 11.Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JP. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ. 2015;2:350. [DOI] [PubMed] [Google Scholar]
- 12.Wu Q, Kling JM. Depression and the risk of myocardial infarction and coronary death: a meta-analysis of prospective cohort studies. Medicine. 2016;95(6):e2815. doi: 10.1097/MD.0000000000002815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weyerer S, Eifflaender-Gorfer S, Wiese B, et al. Incidence and predictors of depression in non-demented primary care attenders aged 75 years and older: results from a 3-year follow-up study. Age Ageing. 2013;42(2):173–180. doi: 10.1093/ageing/afs184 [DOI] [PubMed] [Google Scholar]
- 14.Birrer RB, Vemuri SP. Depression in later life: a diagnostic and therapeutic challenge. Am Fam Physician. 2004;69(10):2375–2382. [PubMed] [Google Scholar]
- 15.Melrose S. Late life depression: nursing actions that can help. Perspect Psychiatr Care. 2019;55(3):453–458. [DOI] [PubMed] [Google Scholar]
- 16.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallo JJ, Rabins PV. Depression without sadness: alternative presentations of depression in late life. Am Fam Physician. 1999;60(3):820–826. [PubMed] [Google Scholar]
- 18.Schaakxs R, Comijs HC, Lamers F, Beekman AT, Penninx BW. Age-related variability in the presentation of symptoms of major depressive disorder. Psychol Med. 2017;47(3):543–552. doi: 10.1017/S0033291716002579 [DOI] [PubMed] [Google Scholar]
- 19.Triolo F, BelvederiMurri M, Calderón-Larrañaga A, et al. Bridging late-life depression and chronic somatic diseases: a network analysis. Transl Psychiatry. 2021;11(1):557. doi: 10.1038/s41398-021-01686-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson BD, Kessel EM, Klein DN, Shankman SA. Depression symptom dimensions and asymmetrical frontal cortical activity while anticipating reward. Psychophysiology. 2018;55(1):e12892. doi: 10.1111/psyp.12892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Invernizzi S, Simoes Loureiro I, KandanaArachchige KG, Lefebvre L. Late-life depression, cognitive impairment, and relationship with alzheimer’s disease. Dement Geriatr Cogn Disord. 2021;50(5):414–424. [DOI] [PubMed] [Google Scholar]
- 22.Hegeman JM, Kok RM, van der Mast RC, Giltay EJ. Phenomenology of depression in older compared with younger adults: meta-analysis. Br J Psychiatry. 2012;200(4):275–281. doi: 10.1192/bjp.bp.111.095950 [DOI] [PubMed] [Google Scholar]
- 23.Bennabi D, Vandel P, Papaxanthis C, Pozzo T, Haffen E. Psychomotor retardation in depression: a systematic review of diagnostic, pathophysiologic, and therapeutic implications. Biomed Res Int. 2013;2013:158746. doi: 10.1155/2013/158746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Husain-Krautter S, Ellison JM. Late life depression: the essentials and the essential distinctions. Focus. 2021;19(3):282–293. doi: 10.1176/appi.focus.20210006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koenig HG, George LK, Peterson BL, Pieper CF. Depression in medically ill hospitalized older adults: prevalence, characteristics, and course of symptoms according to six diagnostic schemes. Am J Psychiatry. 1997;154(10):1376–1383. [DOI] [PubMed] [Google Scholar]
- 26.Gallo JJ, Rabins PV, Lyketsos CG, Tien AY, Anthony JC. Depression without sadness: functional outcomes of nondysphoric depression in later life. J Am Geriatr Soc. 1997;45(5):570–578. doi: 10.1111/j.1532-5415.1997.tb03089.x [DOI] [PubMed] [Google Scholar]
- 27.Brodaty H, Connors MH. Pseudodementia, pseudo-pseudodementia, and pseudodepression. Alzheimers Dement. 2020;12(1):e12027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morimoto SS, Kanellopoulos D, Manning KJ, Alexopoulos GS. Diagnosis and treatment of depression and cognitive impairment in late life. Ann N Y Acad Sci. 2015;1345(1):36–46. doi: 10.1111/nyas.12669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Casey DA. Depression in older adults: a treatable medical condition. Prim Care. 2017;44(3):499–510. doi: 10.1016/j.pop.2017.04.007 [DOI] [PubMed] [Google Scholar]
- 30.Alexopoulos GS, Borson S, Cuthbert BN, et al. Assessment of late life depression. Biol Psychiatry. 2002;52(3):164–174. doi: 10.1016/S0006-3223(02)01381-1 [DOI] [PubMed] [Google Scholar]
- 31.Alexopoulos GS. Mechanisms and treatment of late-life depression. Transl Psychiatry. 2019;9(1):188. doi: 10.1038/s41398-019-0514-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Steffens DC, McQuoid DR, Payne ME, Potter GG. Change in hippocampal volume on magnetic resonance imaging and cognitive decline among older depressed and nondepressed subjects in the neurocognitive outcomes of depression in the elderly study. Am J Geriatr Psychiatry. 2011;19(1):4–12. doi: 10.1097/JGP.0b013e3181d6c245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mills TL. Comorbid depressive symptomatology: isolating the effects of chronic medical conditions on self-reported depressive symptoms among community-dwelling older adults. Soc Sci Med. 2001;53(5):569–578. doi: 10.1016/S0277-9536(00)00361-0 [DOI] [PubMed] [Google Scholar]
- 34.Pan A, Keum N, Okereke OI, et al. Bidirectional association between depression and metabolic syndrome: a systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012;35(5):1171–1180. doi: 10.2337/dc11-2055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feng J, Pan CW. Risk factors for depression in the elderly: an umbrella review of published meta-analyses and systematic reviews. J Affect Disord. 2022;307:37–45. doi: 10.1016/j.jad.2022.03.062 [DOI] [PubMed] [Google Scholar]
- 36.Leyhe T, Reynolds CF, Melcher T, et al. A common challenge in older adults: classification, overlap, and therapy of depression and dementia. Alzheimers Dement. 2017;13(1):59–71. doi: 10.1016/j.jalz.2016.08.007 [DOI] [PubMed] [Google Scholar]
- 37.Yokoyama E, Kaneita Y, Saito Y, et al. Association between depression and insomnia subtypes: a longitudinal study on the elderly in Japan. Sleep. 2010;33(12):1693–1702. doi: 10.1093/sleep/33.12.1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hernández Gómez MA, Fernández Domínguez MJ, Blanco Ramos MA, et al. Depresión y sobrecargaen el cuidado de personas mayores [Depression and burden in the caretaking of elderly]. Rev Esp Salud Publica. 2019;93:e201908038. [PubMed] [Google Scholar]
- 39.Schoevers RA, Deeg DJ, van Tilburg W, Beekman AT. Depression and generalized anxiety disorder: co-occurrence and longitudinal patterns in elderly patients. Am J Geriatr Psychiatry. 2005;13(1):31–39. doi: 10.1097/00019442-200501000-00006 [DOI] [PubMed] [Google Scholar]
- 40.Olsen CDH, Möller S, Ahrenfeldt LJ. Sex differences in quality of life and depressive symptoms among middle-aged and elderly Europeans: results from the SHARE survey. Aging Ment Health. 2021;1–8. doi: 10.1080/13607863.2021.2013434 [DOI] [PubMed] [Google Scholar]
- 41.Tang T, Jiang J, Tang X. Psychological risk and protective factors associated with depression among older adults in mainland China: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2022;37(1). doi: 10.1002/gps.5637 [DOI] [PubMed] [Google Scholar]
- 42.Fontes AP, Neri AL. Resilience in aging: literature review. CienSaude Colet. 2015;20(5):1475–1495. doi: 10.1590/1413-81232015205.00502014 [DOI] [PubMed] [Google Scholar]
- 43.Tsutsumimoto K, Makizako H, Doi T, et al. Prospective associations between sedentary behaviour and incident depressive symptoms in older people: a 15-month longitudinal cohort study. Int J Geriatr Psychiatry. 2017;32(2):193–200. doi: 10.1002/gps.4461 [DOI] [PubMed] [Google Scholar]
- 44.Coin A, Devita M, Bizzotto M, et al. The association between cognitive reserve and depressive mood in older inpatients: gender and age differences. Exp Aging Res;2022. 1–10. doi: 10.1080/0361073X.2022.2041324 [DOI] [PubMed] [Google Scholar]
- 45.Vieira ER, Brown E, Raue P. Depression in older adults: screening and referral. J Geriatr Phys Ther. 2014;37(1):24–30. doi: 10.1519/JPT.0b013e31828df26f [DOI] [PubMed] [Google Scholar]
- 46.Reynolds CF, Lenze E, Mulsant BH. Assessment and treatment of major depression in older adults. Handb Clin Neurol. 2019;167:429–435. [DOI] [PubMed] [Google Scholar]
- 47.Dias NS, Barbosa IG, Kuang W, Teixeira AL. Depressive disorders in the elderly and dementia: an update. Dement Neuropsychol. 2020;14(1):1–6. doi: 10.1590/1980-57642020dn14-010001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Myrick L. Recognizing and treating late-life depression. JAAPA. 2019;32(7):51–53. doi: 10.1097/01.JAA.0000558392.18267.d3 [DOI] [PubMed] [Google Scholar]
- 49.Sheline YI, Barch DM, Garcia K, et al. Cognitive function in late life depression: relationships to depression severity, cerebrovascular risk factors and processing speed. Biol Psychiatry. 2006;60(1):58–65. doi: 10.1016/j.biopsych.2005.09.019 [DOI] [PubMed] [Google Scholar]
- 50.Asmer MS, Kirkham J, Newton H, et al. Meta-analysis of the prevalence of major depressive disorder among older adults with dementia. J Clin Psychiatry. 2018;79(5):17r11772. doi: 10.4088/JCP.17r11772 [DOI] [PubMed] [Google Scholar]
- 51.ValiengoLda C, Stella F, Forlenza OV. Mood disorders in the elderly: prevalence, functional impact, and management challenges. Neuropsychiatr Dis Treat. 2016;12:2105–2114. doi: 10.2147/NDT.S94643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Riddle M, Potter GG, McQuoid DR, Steffens DC, Beyer JL, Taylor WD. Longitudinal cognitive outcomes of clinical phenotypes of late-life depression. Am J Geriatr Psychiatry. 2017;25(10):1123–1134. doi: 10.1016/j.jagp.2017.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ly M, Karim HT, Becker JT, et al. Late-life depression and increased risk of dementia: a longitudinal cohort study. Transl Psychiatry. 2021;11:147. doi: 10.1038/s41398-021-01269-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hughes AJ, Bhattarai JJ, Paul S, Beier M. Depressive symptoms and fatigue as predictors of objective-subjective discrepancies in cognitive function in multiple sclerosis. MultSclerRelatDisord. 2019;30:192–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Olin JT, Schneider LS, Katz IR, et al. Provisional diagnostic criteria for depression of Alzheimer disease. Am J Geriatr Psychiatry. 2002;10(2):125–128. doi: 10.1097/00019442-200203000-00003 [DOI] [PubMed] [Google Scholar]
- 56.Geerlings MI, Schoevers RA, Beekman AT, et al. Depression and risk of cognitive decline and Alzheimer’s disease. Results of two prospective community-based studies in The Netherlands. Br J Psychiatry. 2000;176:568–575. doi: 10.1192/bjp.176.6.568 [DOI] [PubMed] [Google Scholar]
- 57.Nelson JC, Delucchi K, Schneider LS. Anxiety does not predict response to antidepressant treatment in late life depression: results of a meta-analysis. Int J Geriatr Psychiatry. 2009;24(5):539–544. doi: 10.1002/gps.2233 [DOI] [PubMed] [Google Scholar]
- 58.Nelson JC. Diagnosing and treating depression in the elderly. J Clin Psychiatry. 2001;62(Suppl 24):18–22. [PubMed] [Google Scholar]
- 59.De Picker L, Van Den Eede F, Dumont G, Moorkens G, Sabbe BG. Antidepressants and the risk of hyponatremia: a class-by-class review of literature. Psychosomatics. 2014;55(6):536–547. doi: 10.1016/j.psym.2014.01.010 [DOI] [PubMed] [Google Scholar]
- 60.de Abajo FJ. Effects of selective serotonin reuptake inhibitors on platelet function: mechanisms, clinical outcomes and implications for use in elderly patients. Drugs Aging. 2011;28(5):345–367. doi: 10.2165/11589340-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 61.Fox CB, Treadway AK, Blaszczyk AT, Sleeper RB. Megestrol acetate and mirtazapine for the treatment of unplanned weight loss in the elderly. Pharmacotherapy. 2009;29(4):383–397. doi: 10.1592/phco.29.4.383 [DOI] [PubMed] [Google Scholar]
- 62.Ancoli-Israel S, Ayalon L. Diagnosis and treatment of sleep disorders in older adults. Am J Geriatr Psychiatry. 2006;14(2):95–103. doi: 10.1097/01.JGP.0000196627.12010.d1 [DOI] [PubMed] [Google Scholar]
- 63.Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Int Clin Psychopharmacol. 2012;27(4):215–223. doi: 10.1097/YIC.0b013e3283542457 [DOI] [PubMed] [Google Scholar]
- 64.Meyers BS, Flint AJ, Rothschild AJ, et al.; STOP-PD Group. A double-blind randomized controlled trial of olanzapine plus sertraline vs olanzapine plus placebo for psychotic depression: the study of pharmacotherapy of psychotic depression (STOP-PD). Arch Gen Psychiatry. 2009;66(8):838–847. doi: 10.1001/archgenpsychiatry.2009.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kiosses DN, Ravdin LD, Gross JJ, Raue P, Kotbi N, Alexopoulos GS. Problem adaptation therapy for older adults with major depression and cognitive impairment: a randomized clinical trial. JAMA Psychiatry. 2015;72(1):22–30. doi: 10.1001/jamapsychiatry.2014.1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kok RM, Reynolds CF. Management of depression in older adults: a review. JAMA. 2017;317(20):2114–2122. doi: 10.1001/jama.2017.5706 [DOI] [PubMed] [Google Scholar]
- 67.Anguera JA, Gunning FM, Areán PA. Improving late life depression and cognitive control through the use of therapeutic video game technology: a proof-of-concept randomized trial. Depress Anxiety. 2017;34(6):508–517. doi: 10.1002/da.22588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kierman GL, Weissman MK. Interpersonal Psychotherapy of Depression: A Brief, Focused, Specific Strategy. 1st ed. Jason Aronson; 1994. [Google Scholar]
- 69.Van Damme A, Declercq T, Lemey L, Tandt H, Petrovic M. Late-life depression: issues for the general practitioner. Int J Gen Med. 2018;11:113–120. doi: 10.2147/IJGM.S154876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kellner CH. Electroconvulsive Therapy: stayin’ Alive, Stayin’ Well. Acta Psychiatr Scand. 2021;144(3):215–217. doi: 10.1111/acps.13352 [DOI] [PubMed] [Google Scholar]
- 71.Kumar S, Mulsant BH, Liu AY, Blumberger DM, Daskalakis ZJ, Rajji TK. Systematic review of cognitive effects of electroconvulsive therapy in late-life depression. Am J Geriatr Psychiatry. 2016;24(7):547–565. doi: 10.1016/j.jagp.2016.02.053 [DOI] [PubMed] [Google Scholar]
- 72.Spaans HP, Sienaert P, Bouckaert F, et al. Speed of remission in elderly patients with depression: electroconvulsive therapy v. medication. Br J Psychiatry. 2015;206(1):67–71. doi: 10.1192/bjp.bp.114.148213 [DOI] [PubMed] [Google Scholar]
- 73.Jeste ND, Hays JC, Steffens DC. Clinical correlates of anxious depression among elderly patients with depression. J Affect Disord. 2006;90(1):37–41. doi: 10.1016/j.jad.2005.10.007 [DOI] [PubMed] [Google Scholar]
- 74.Laflamme L, Vaez M, Lundin K, Sengoelge M. Prevention of suicidal behavior in older people: a systematic review of reviews. PLoS One. 2022;17(1):e0262889. doi: 10.1371/journal.pone.0262889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vaughan L, Corbin AL, Goveas JS. Depression and frailty in later life: a systematic review. Clin Interv Aging. 2015;10:1947–1958. doi: 10.2147/CIA.S69632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Linden M, Borchelt M, Barnow S, Geiselmann B. The impact of somatic morbidity on the Hamilton depression rating scale in the very old. Acta Psychiatr Scand. 1995;92(2):150–154. doi: 10.1111/j.1600-0447.1995.tb09559.x [DOI] [PubMed] [Google Scholar]
- 77.Blais M, Baer L. Understanding Rating Scales and Assessment Instruments. Handbook of Clinical Rating Scales and Assessment in Psychiatry and Mental Health. Humana Press; 2010. [Google Scholar]
- 78.Edelstein BA, Drozdick LW, Ciliberti CM. Chapter 1 - assessment of depression and bereavement in older adults. In: Handbook of Assessment in Clinical Gerontology. 2nd ed. Academic Press; 2010. [Google Scholar]
- 79.Calderón-Larrañaga A, Santoni G, Wang HX, et al. Rapidly developing multimorbidity and disability in older adults: does social background matter? J Intern Med. 2018;283(5):489–499. doi: 10.1111/joim.12739 [DOI] [PubMed] [Google Scholar]
- 80.Wells CE. Pseudodementia. Am J Psychiatry. 1979;136(7):895–900. [DOI] [PubMed] [Google Scholar]
- 81.Crowe SF, Hoogenraad K. Differentiation of dementia of the Alzheimer’s type from depression with cognitive impairment on the basis of a cortical versus subcortical pattern of cognitive deficit. Arch Clin Neuropsychol. 2000;15(1):9–19. doi: 10.1093/arclin/15.1.9 [DOI] [PubMed] [Google Scholar]
- 82.Frasson P, Ghiretti R, Catricalà E, et al. Free and cued selective reminding test: an Italian normative study. Neurol Sci. 2011;32(6):1057–1062. doi: 10.1007/s10072-011-0607-3 [DOI] [PubMed] [Google Scholar]
- 83.Gasser AI, Salamin V, Zumbach S. Dépression de la personneâgéeoumaladied’Alzheimerprodromique: quelsoutils pour le diagnostic différentiel? [Late life depression or prodromal Alzheimer’s disease: which tools for the differential diagnosis?]. Encephale. 2018;44(1):52–58. doi: 10.1016/j.encep.2017.03.002 [DOI] [PubMed] [Google Scholar]