Abstract
The impact of the global COVID-19 pandemic, including the indirect effect of policy responses, on psychological distress has been the subject of much research. However, there has been little consideration of how the prevalence of psychological distress changed with the duration and repetition of lockdowns, or the rate of resolution of psychological distress once lockdowns ended. This study describes the trajectories of psychological distress over multiple lockdowns during the first two years of the pandemic across five Australian states for the period May 2020 to December 2021 and examines whether psychological distress trajectories varied as a function of time spent in lockdown, or time since lockdown ended.
A total of N = 574,306 Australian adults completed Facebook surveys over 611 days (on average 940 participants per day). Trajectories of psychological distress (depression and anxiety) were regressed on lockdown duration and time since lockdown ended. Random effects reflecting the duration of each lockdown were included to account for varying effects on psychological distress associated with lockdown length.
The prevalence of psychological distress was higher during periods of lockdown, more so for longer lockdowns relative to shorter lockdowns. Psychological distress increased rapidly over the first ten weeks of lockdowns spanning at least twelve weeks, though less rapidly for short lockdowns of three weeks or less. Psychological distress levels tended to stabilise, or even decrease, after ten consecutive weeks of lockdown. After lockdown restrictions were lifted, psychological distress rapidly subsided but did not return to pre-lockdown levels within four weeks, although continued to decline afterwards.
In Australia short lockdowns of pre-announced durations were associated with slower rises in psychological distress. Lockdowns may have left some temporary residual population effect, but we cannot discern whether this reflects longer term trends in increasing psychological distress. However, the findings do re-emphasise the resilience of individuals to major life stressors.
Keywords: Depression, Anxiety, Mental health, Trajectories, COVID-19, Australia
Highlights
-
•
We study psychological distress trajectories within and across COVID-19 lockdowns.
-
•
Distress increased with lockdown duration, especially 12-week or longer lockdowns.
-
•
Distress stabilises after ten weeks of consecutive lockdown.
-
•
Distress steadily declines after removing lockdown restrictions.
1. Introduction
Both the COVID-19 pandemic itself and the government policy responses introduced to limit the spread of the virus (such as ‘lockdowns’) were associated with significant life stressors including illness and bereavement, isolation and loneliness, loss of employment, and economic uncertainty (Hertz-Palmor et al., 2021; Wu, Yao, Deng, Marsiglia, & Duan, 2021). Many studies examined population mental health during the initial phase of the pandemic, drawing upon data from representative cohorts that surveyed the same individuals prior to, and then at multiple time points during the pandemic. These studies showed that, after an initial deterioration in population mental health at the onset of the pandemic, there was evidence of recovery (Daly & Robinson, 2021; Pierce et al., 2020). A subsequent meta-analysis of longitudinal studies conducted in Europe and North America in the first year of the pandemic, 2020, confirmed that lockdown had a negative impact on population levels psychological distress, although the effect size was small (Robinson, Sutin, Daly, & Jones, 2022).
Research examining the effect of lockdowns on population mental health face several challenges. Worsening mental health over time may reflect the effect of COVID-19 lockdowns or may be the continuation of longer-term population trends (e.g., Butterworth, Watson, & Wooden, 2020; Twenge & Cooper, 2020). Studies drawing on longitudinal cohort studies with multiple pre-COVID measurement occasions have adjusted for underlying trends, and still found small but significant worsening of mental health during the pandemic (Pierce et al., 2020). Another challenge is to disentangle the mental health consequences of lockdowns from the direct effects of the pandemic (such as fear of catching the virus, Chandola, Kumari, Booker, & Benzeval, 2020). Studies using quasi-experimental designs (e.g., difference-in-difference) to contrast the mental health of people in areas that were and were not exposed to lockdowns (e.g., Butterworth, Schurer, Trinh, Vera-Toscano, & Wooden, 2022; Serrano-Alarcón, Kentikelenis, Mckee, & Stuckler, 2022) have demonstrated that lockdowns had a modest negative effect on overall mental health.
Although the existing research provides important insights into the average effects of lockdown restrictions on mental health, it usually only includes a limited number of observations during COVID-19. As a result of this limited temporal resolution, such studies provide no information about two key issues, namely (i) how mental health changes over the course of lockdown, and (ii) how quickly mental health recovers after lockdowns are lifted. Lockdowns may have cumulative effects on psychological distress; depression and anxiety may continue to rise with longer lockdowns, or there may be patterns of stabilisation or improvement that cannot be detected from a single COVID measurement occasion. Even surveys that have included multiple measures during the pandemic still may not include adequate measurement occasions to capture the variability in lockdown duration for individuals in different locations. As a result, estimates relying on such comparisons will fail to detect acute or transient changes in psychological distress and so may underestimate the total, or maximal, effect of lockdown.
Another body of research conducted during the COVID-19 pandemic has adopted a surveillance or monitoring approach (e.g., Botha, Butterworth, & Wilkins, 2022; Fancourt, Steptoe, & Bu, 2021). These studies have recruited representative cross-sectional samples at regular occasions throughout the pandemic (as regularly as weekly), using consistent measures over time. This approach provides an opportunity to examine how population mental health has changed over time, and in relation to changes in lockdown status. For example, the COVID-19 Behaviour Tracker Global Survey drew fortnightly representative surveys from existing online panels in 15 different countries for more than 12 months. Linking this data to details of the stringency of local policy responses (Oxford COVID-19 Government Response Tracker) showed how population mental health was associated with policy stringency: mental health was worse at the times policies were strictest (Aknin et al., 2022).
This impact of the pandemic and lockdowns is unsurprising as negative life events are well known to be associated with adverse impacts on mental wellbeing and increased psychological distress (Frijters, Johnston, & Shields, 2011; Jeong et al., 2016). However, the impact of significant life stressors is often transient, with mental health and subjective wellbeing recovering to baseline levels for most individuals (Kettlewell et al., 2020). Similar transient effects have also been found in pre-COVID research of the mental health effects of quarantine (Jeong et al., 2016). Understanding whether any lockdown mental health impact is transient and the trajectory of this may help determine policy and service responses to future pandemics.
Over the course of the pandemic, different Australian states had very different lockdown experiences. All states experienced multiple lockdowns, although the duration of lockdowns varied considerably: sometimes lasting for as little as a week or, as in the case of Melbourne in the state of Victoria (VIC) extending for up to 4 months. Victoria experienced the most severe and extended lockdown restrictions of any region in the world in 2020 of 112 consecutive days, while New South Wales (NSW) experienced a 106-day lockdown in the second half of 2021. Given Australia's aggressive suppression strategy, there were also many shorter lockdowns (introduced at the first sign of community transmission) with the duration of these lockdowns often pre-determined and announced by policy makers. Studies with high frequency data collection (e.g., daily or weekly) are required to evaluate how psychological distress is affected by different lockdown durations.
The aim of the present study is to investigate the mental health effects of COVID-19 policy responses based on daily data from five Australian states. We examined 1) trajectories of change, 2) recovery during and after lockdowns, and 3) the effect on mental health of lockdown duration and the number of lockdowns experienced. The main source of data used in this paper was the Global COVID-19 Trends and Impact Survey (UMD Global CTIS), which recruited a new random sample of Facebook users each day, stratified by country and region, and assessed COVID symptoms, depression, anxiety, and financial stress among other items (Astley et al., 2021; Kreuter et al., 2020). As such, it provides the type of high frequency dataset needed to estimate the changes in psychological distress that occurred within lockdown, as well as after the restrictions lifted, for each Australian state throughout the pandemic.
2. Material and methods
2.1. Sampling method
We use data from the UMD Global CTIS, which was a partnership between the University of Maryland and Facebook. Facebook users were invited to take off-platform surveys of COVID-19-related symptoms beginning April 23rd, 2020. Approved by the UMD IRB (1,587,016–10), the survey and sampling strategy was designed by the University of Maryland Joint Program in Survey Methodology. The survey participants provided their written informed consent to UMD to participate in the survey. The anonymised data was obtained for this paper under a data use agreement (DUA) between the University of Maryland and the University of Sydney. Full details of the methods of the stratified survey collection are described in Kreuter et al. (2020). Briefly, every day a unique random sample of Facebook users over 18 years old (stratified by region) was invited to consent and participate via an invitation at the top of their Facebook News Feed (i.e., a repeated cross-sectional survey design). Probability sampling on existing attributes (e.g., region, age, gender) based on internal Facebook data was used to ensure new users were included each wave and to reduce survey fatigue. In low density geographical regions, users may be sampled again once a month (in high density regions users are sampled every 2–6 months), but survey responses cannot be linked longitudinally.
Participants reported on their COVID-19 symptoms, psychological distress, and financial concerns (the complete list of survey variables is available at https://gisumd.github.io/COVID-19-API-Documentation/docs/indicators/indicators. Survey weights were developed from the United Nations Population Division 2019 World Population Projections for age and gender, and used to minimize errors of representation, including coverage, sampling and non-response bias in each geographic region. The resulting weighted estimates aim to represent the general population of adults in each state rather than Facebook users per se. More details on the sampling frame, non-response modelling to reduce nonresponse and coverage bias, and post-stratification to represent the general adult population are available at https://covidmap.umd.edu/document/css_methods_brief.pdf.
The average daily sample size for each State, stratified by age and gender is shown in Supplementary methods in the Appendix (Table A1). Tasmania, Northern Territory, and the Australian Capital Territory were not included in the analysis as the average number of users sampled in those regions was less than 20 percent of the average sample size in the other states, and the sampling dates did not extend over the same period.
2.2. Psychological distress
Psychological distress was measured by two items on depression and anxiety taken from the Kessler-10 (K10) (Kessler et al., 2003):
“During the last 7 days, how often did you feel so depressed that nothing could cheer you up?” (5 = “All of the time”, 4 = “most of the time”, 3 = “some of the time”, 2 = “a little of the time”, 1 = “none of the time”).
“During the last 7 days, how often did you feel so nervous that nothing could calm you down?” (5 = “All of the time”, 4 = “most of the time”, 3 = “some of the time”, 2 = “a little of the time”, 1 = “none of the time”).
The K10 is a widely used instrument in Australia, in both epidemiology and clinical reporting. The administration of the K10 to monitor mental health outcomes is mandated for patients of public mental health services in the Australian State of NSW (Andrews & Slade, 2001; Hickie, Andrews, & Davenport, 2002), and evidence of internal consistency ( = 0.93), test-retest reliability (ICC = 0.86, r = 0.76), factorial validity, convergent and discriminant validity, and treatment sensitivity has been provided (Berle et al., 2010; Kessler et al., 2002; Merson, Newby, Shires, Millard, & Mahoney, 2021; Slade, Grove, & Burgess, 2011; Sunderland, Mahoney, & Andrews, 2012a, 2012b). The psychometric properties of the instrument are invariant across the adult lifespan (Sunderland, Hobbs, Anderson, & Andrews, 2012a, 2012b). We report the population weighted proportions of adults responding “most” or “all of the time” to each question as the population prevalence of depression and anxiety, respectively.
2.3. Lockdown dates
After an initial national lockdown from the end of March 2020 to mid-May 2020, Australia successfully reduced COVID-19 cases to negligible levels (as few as 3 new cases a day according to the 7-day trailing average, www.covidlive.com.au). Australian data in the UMD Global CTIS is only available from early May 2020, towards the end of the first national lockdown. Subsequently different states in Australia underwent distinct episodes of lockdowns of varying length over 2020 and 2021 (see Table 1). By the end of 2021, Melbourne (VIC) and Sydney (NSW) had experienced 272 and 150 days of lockdown respectively, while Queensland (QLD) (and the rest of Australia) had remained relatively free of restrictions. This makes NSW and VIC a good case-study to examine the impact of extended lockdowns on the prevalence of depression and anxiety in the population, relative to its temporal trend as well as by comparisons with the rest of Australia. The lockdown dates and durations for each State are summarised in Table 1.
Table 1.
Lockdown characteristics, by state.
| State | Lockdown | Start | End | Duration |
|---|---|---|---|---|
| Victoria (VIC) | 1 | 2020-03-31 | 2020-05-12 | 42 days |
| 2 | 2020-07-09 | 2020-10-28 | 111 days | |
| 3 | 2021-02-12 | 2021-02-17 | 5 days | |
| 4 | 2021-05-27 | 2021-06-10 | 14 days | |
| 5 | 2021-07-15 | 2021-07-27 | 12 days | |
| 6 | 2021-08-05 | 2021-10-22 | 78 days | |
| New South Wales (NSW) | 1 | 2020-03-31 | 2020-05-15 | 45 days |
| 2 | 2020-12-17 | 2021-01-09 | 23 days | |
| 3 | 2021-06-26 | 2021-10-10 | 106 days | |
| Queensland (QLD) | 1 | 2020-03-31 | 2020-05-02 | 32 days |
| 2 | 2021-01-08 | 2021-01-11 | 3 days | |
| 3 | 2021-03-29 | 2021-04-01 | 3 days | |
| 4 | 2021-06-29 | 2021-07-03 | 4 days | |
| 5 | 2021-07-31 | 2021-08-08 | 8 days | |
| South Australia (SA) | 1 | 2020-03-31 | 2020-05-11 | 41 days |
| 2 | 2020-11-19 | 2020-11-22 | 3 days | |
| 3 | 2021-07-21 | 2021-07-28 | 7 days | |
| Western Australia (WA) | 1 | 2020-03-23 | 2020-04-27 | 35 days |
| 2 | 2021-01-31 | 2021-02-05 | 5 days | |
| 3 | 2021-04-24 | 2021-04-27 | 3 days | |
| 4 | 2021-06-29 | 2021-07-03 | 4 days |
Note: Lockdown dates were sourced from State Premier announcements and news reports, and curated by Anthony Macali.
Note we excluded the initial national lockdown in the analyses below, as data collection only commenced towards the end of the first lockdown period. Furthermore, the second lockdown listed for NSW was restricted to a single local government area (LGA), representing fewer than 65,000 people (less than 0.8 percentage points of the NSW population), so was excluded from the analyses.
2.4. Modelling
The outcome variables were the daily prevalence of depression and anxiety. For duration of lockdown the main explanatory variable was the cumulative number of weeks spent to date in the current lockdown (“week”). To estimate the post-lockdown trajectory, we used the number of weeks in the post-lockdown period since the most recent lockdown ended, top-coded as a maximum of 5 weeks (“postweek”). To capture the non-linear trajectory of weekly changes in depression and anxiety with lockdown duration, the cumulative lockdown week (or post lockdown week) was modelled with cubic regression splines, using the mgcv package (version 1.8) by Wood et al. (Wood, 2004; Wood, Pya, & Säfken, 2016) running in R (version 4.1, R Core Team, 2013). We included varying coefficients (i.e., random effects) for the total duration of each lockdown to correctly account for variations in trajectory due to the total length of each lockdown (“duration”). We present the predicted population-level estimates of prevalence as a function of time in lockdown. The marginal effects of each lockdown duration were calculated to allow comparison between lockdown trajectories with different durations.
The linear effect of time since the start of the pandemic (“month”) was entered into each model to control for trends in levels of psychological distress over the pandemic (Butterworth et al., 2022). State fixed effects were included to capture average differences between regions in Australia (“State”) and the potential cumulative effect of new lockdowns (“number”) in each state.
Formally the daily prevalence of each outcome () was modelled for each days of the pandemic for each State (NSW, VIC, QLD, SA, WA) as:
Where is the population estimate of daily prevalence of psychological distress in each State, is the underlying trend in levels of psychological distress in Australia, is the fixed estimate for average differences in psychological distress in each State over the pandemic, is the trend in psychological distress over different lockdown numbers in each State, is a smooth function(s) for the non-linear trend in psychological distress over lockdown weeks, and is the random effect (slope) of lockdown duration for each durations.
is a penalized cubic regression spline of the form:
With equally spaced knots for over the range of .
The marginal effects of each lockdown duration and number were calculated by holding all other effects constant. We obtained the change in (i.e., prevalence) at different values of (lockdown duration or number) by using the delta method. In brief, was estimated at given values of (holding all other constant). For each we determined the change in by , where is an arbitrary value less than the range of . The results express the average change in at each , marginalising over all other .
In sensitivity analyses we also included the number of daily new infections and daily financial concerns as confounding variables (see Appendix Section 2). Appropriate model diagnostic information is available in Appendix Section 3.
3. Results
The demographic features of Facebook users in our sample of 574,306 who responded to either the depression or anxiety item between April 2020 and December 2021 are shown in Table 2.
Table 2.
Summary statistics, overall and by state.
| Characteristic | Australia N = 5,743,061 |
VIC N = 1,594,651 |
NSW N = 1,446,051 |
QLD N = 1,280,281 |
SA N = 632,831 |
WA N = 789,251 |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Female | 348,842 (61%) | 95,083 (60%) | 86,968 (60%) | 79,591 (62%) | 39,602 (63%) | 47,598 (60%) |
| Male | 225,464 (39%) | 64,382 (40%) | 57,637 (40%) | 48,437 (38%) | 23,681 (37%) | 31,327 (40%) |
| Age | ||||||
| 18-24 | 60,800 (11%) | 17,927 (11%) | 15,878 (11%) | 13,989 (11%) | 5949 (9.4%) | 7057 (8.9%) |
| 25-44 | 217,775 (38%) | 64,480 (40%) | 57,974 (40%) | 48,544 (38%) | 19,394 (31%) | 27,383 (35%) |
| 45-64 | 203,992 (36%) | 54,320 (34%) | 49,133 (34%) | 45,348 (35%) | 25,260 (40%) | 29,931 (38%) |
| 65+ | 91,739 (16%) | 22,738 (14%) | 21,620 (15%) | 20,147 (16%) | 12,680 (20%) | 14,554 (18%) |
| Region | ||||||
| City | 287,802 (51%) | 77,990 (50%) | 66,058 (47%) | 63,066 (50%) | 34,149 (55%) | 46,539 (60%) |
| Town | 182,543 (33%) | 52,848 (34%) | 50,782 (36%) | 41,921 (34%) | 16,624 (27%) | 20,368 (26%) |
| Rural | 89,470 (16%) | 24,432 (16%) | 24,094 (17%) | 19,976 (16%) | 10,889 (18%) | 10,079 (13%) |
| Fear of infection | 191,607 (43%) | 60,749 (48%) | 49,565 (46%) | 39,668 (40%) | 18,857 (38%) | 22,768 (37%) |
| Financial concerns | 144,856 (25%) | 42,148 (26%) | 37,656 (26%) | 32,724 (26%) | 14,867 (23%) | 17,461 (22%) |
| Depressed | 36,795 (6.4%) | 12,019 (7.5%) | 9494 (6.6%) | 7669 (6.0%) | 3744 (5.9%) | 3869 (4.9%) |
| Anxious | 24,057 (4.2%) | 7683 (4.8%) | 6101 (4.2%) | 5268 (4.1%) | 2508 (4.0%) | 2497 (3.2%) |
1n (%). Tasmania, Australian Capital Territory, Northern Territory were excluded due to small sample size.
Most responses were from females (61%) and/or adults aged 25–64 (74%), living in a city or town (84%), and over half came from VIC or NSW (53%). Compared to Australian 2021 census data (see Table A2), females are relatively oversampled, along with middle-aged adults (45–64). The survey weights provided by UMD Global CTIS were included in all models to adjust for disproportionate sampling over age groups and gender. Fear of infection was highest in VIC (48%) and lowest in WA (37%), (4, N = 574,306) = 3774, p < .0001. Financial concerns were similar in VIC, NSW and QLD (26%) but lower in SA and WA, (4, N = 574,306) = 685, p < .0001. The proportion of people feeling depressed was highest in VIC (7.5%), followed by NSW (6.6%), (4, N = 574,306) = 706, p < .0001. Anxiety prevalence was also highest in VIC (4.8%) relative to other states, (4, N = 574,306) = 374, p < .0001.
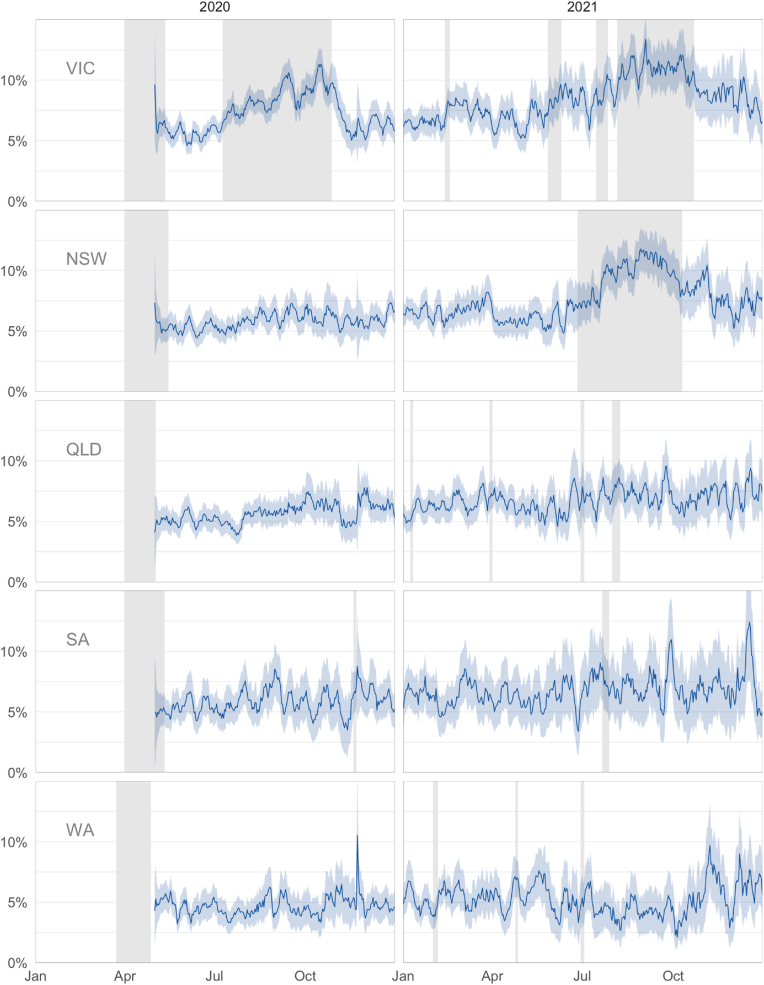
3.1. Depression
The daily prevalence of depression, as estimated by a weighted proportion of the population, is shown in Fig. 1 for each state over the course of the COVID-19 pandemic. A linear regression of depression prevalence on time (month) revealed the average monthly increase in prevalence over the pandemic was positive and significant in each state: [95%CI] = 0.11 [0.1, 0.12], 0.1 [0.09, 0.11], 0.08 [0.07, 0.1], 0.16 [0.15, 0.17], 0.04 [0.03, 0.06] percentage points for NSW, QLD, SA, VIC, WA, respectively. Lockdown had a significant effect on increasing the prevalence of depression in each State except WA: [95%CI] = 2.49 [2.27, 2.7], 0.46 [0.13, 0.8], 0.65 [0.01, 1.28], 2.36 [2.2, 2.53], 0.18 [−0.38, 0.74] percentage points for NSW, QLD, SA, VIC, WA, respectively.
Fig. 1.
Daily population prevalence of depression (±95% CI) by state and year.Note: Daily population weighted estimates of depression prevalence (±95%CI shaded) in each Australian State between the end of April 2020 and December 2021. Grey shaded regions indicate lockdown periods in each State.
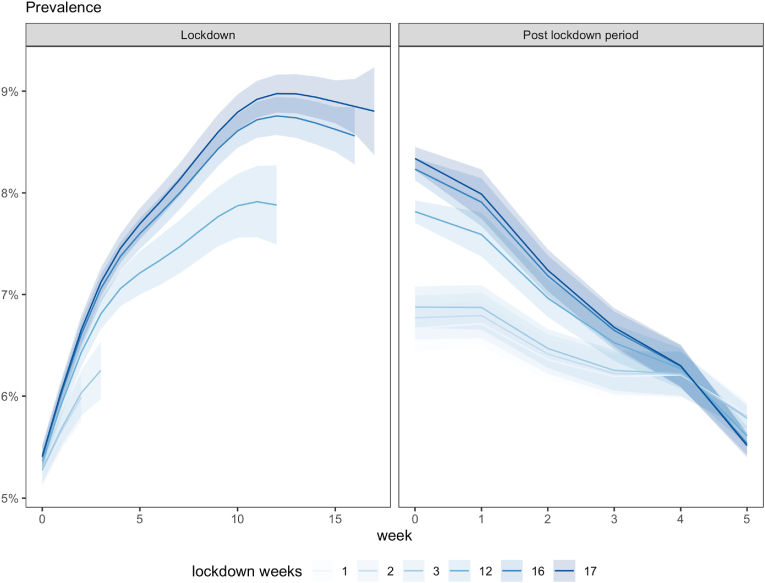
Fig. 2 reports the estimated trajectories for depression by lockdown duration. The estimated depression prevalence increased week on week over a lockdown before peaking in week 10 (adjusted R-squared = 76%, F = 55.46, p < .001). Including the random effect of lockdown duration in the lockdown model explained only an additional 0.2 percentage points of variance (adjusted R-squared = 76.2%, F = 29.32, p < .001).
Fig. 2.
Effect of lockdown on population prevalence of depression (±95% CI). Note: Figure shows the estimated effect of lockdown on the population prevalence of depression as a function of time (weeks). In the lockdown period (left), the Week 0 estimate represents the average prevalence in the period immediately prior to lockdown (left). In the post lockdown period (right), Week 0 represents the average depression during the prior lockdown and the Week 5 estimate represents the average prevalence after the 4th week post-lockdown period and before the next lockdown.
The smooth trajectories in the post lockdown period shows the prevalence of depression lowered rapidly in the initial two weeks after lockdown on average, before approaching stable levels (adjusted R-squared = 72%, F = 22.34, p < .001). Including the random effect of lockdown duration in the post-lockdown model explained an additional 2 percentage points of variance (adjusted R-squared = 74%, F = 217.37, p < .001). The prevalence fell to 6 percent by 4 weeks post-lockdown regardless of lockdown duration. Note however the week 5 post lockdown estimate falls below the week 4 post lockdown estimate, indicating depression levels still had further to fall after four weeks.
The varying effect of lockdown duration plotted in Fig. 2 shows that short lockdowns (1–3 weeks) tended to have less impact on prevalence levels over the same initial period of a lockdown than longer lockdowns. The marginal effect of lockdown duration (over all states and lockdown numbers) is compared in Table 3.
Table 3.
Marginal effect of lockdown duration on depression.
| lockdown length (weeks) | marginal delta (%) | SE | lower 95%CI | upper 95%CI |
|---|---|---|---|---|
| 1 | 0.36 | 0.05 | 0.27 | 0.46 |
| 2 | 0.38 | 0.05 | 0.29 | 0.47 |
| 3 | 0.40 | 0.04 | 0.31 | 0.48 |
| 12 | 0.55 | 0.04 | 0.48 | 0.63 |
| 16 | 0.62 | 0.04 | 0.54 | 0.71 |
| 17 | 0.64 | 0.04 | 0.56 | 0.73 |
Table 3 shows the marginal effect of lockdown duration on prevalence of depression is greater for longer lockdowns than shorter lockdowns. Depression prevalence increases by between 0.36 and 0.4 percentage points per week over short lockdowns, but a faster increase of 0.55–0.64 percentage points occurs for longer lockdowns. Comparison of the 95% confidence intervals shows the rate of increase in each case is significantly greater than the short lockdowns.
The number of new lockdowns (“number”) had different and even opposite cumulative effects on depression prevalence in some states.
The marginal estimates (Table 4) show the percent prevalence of depression increases by 0.45–0.465 percentage points with each additional lockdown in VIC and NSW, was also positive in QLD but in SA ranged around zero and was negative in WA. Comparison of the 95% confidence intervals shows the cumulative effect of each additional lockdown was significantly greater in VIC and NSW than any of the other states.
Table 4.
Marginal effect of lockdown number on depression.
| State | marginal delta (%) | SE | lower 95%CI | upper 95%CI |
|---|---|---|---|---|
| Victoria | 0.45 | 0.03 | 0.39 | 0.51 |
| New South Wales | 0.46 | 0.06 | 0.35 | 0.58 |
| Queensland | 0.08 | 0.03 | 0.01 | 0.15 |
| South Australia | −0.07 | 0.10 | −0.27 | 0.13 |
| Western Australia | −0.22 | 0.05 | −0.33 | −0.12 |
3.2. Anxiety
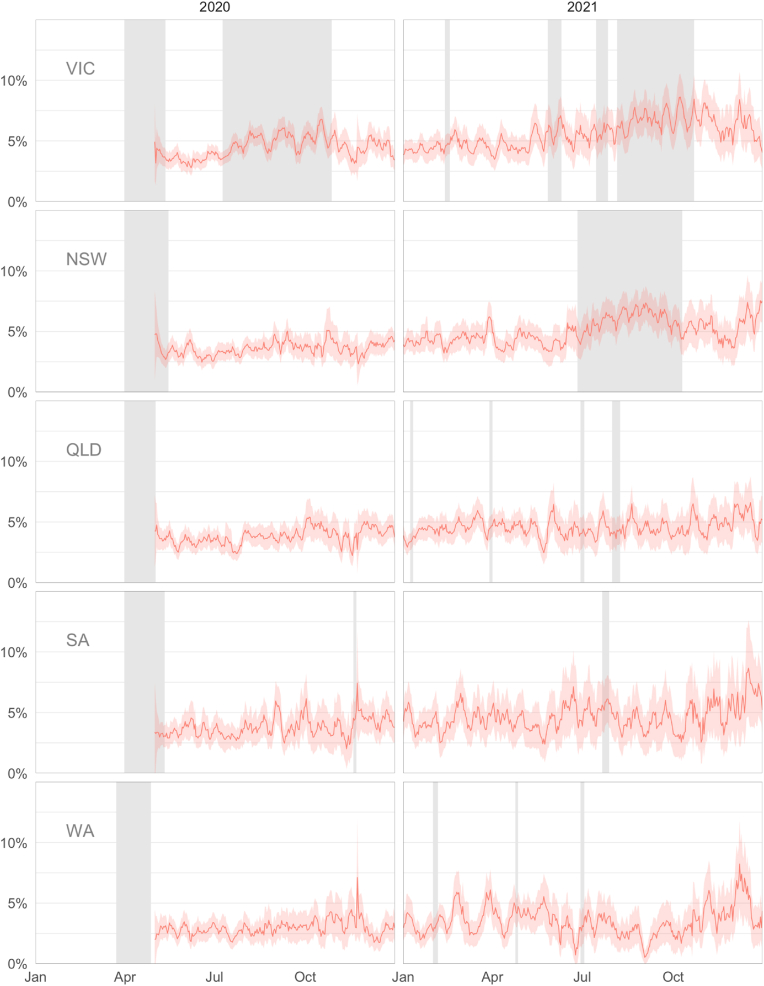
Fig. 3 shows the daily prevalence of anxiety, as a weighted proportion of the population, for each state over the course of the COVID-19 pandemic. Changes in anxiety prevalence using this one question were much more modest during lockdown periods as compared to depression.
Fig. 3.
Daily population prevalence of anxiety (±95% CI) by state and year. Note: Daily population weighted estimates of anxiety prevalence (±95% CI shaded) in each Australian State between the end of April 2020 and December 2021. Grey shaded regions indicate lockdown periods in each State.
A linear regression of anxiety prevalence on time (month) by lockdown revealed the average monthly increase in prevalence over the pandemic was positive and significant in each state: [95%CI] = 0.11 [0.1, 0.12], 0.07 [0.06, 0.08], 0.08 [0.07, 0.09], 0.14 [0.13, 0.14], 0.05 [0.03, 0.06] percentage points for NSW, QLD, SA, VIC, WA, respectively. There were some differences between states in the effect of lockdown on anxiety with lockdown increasing anxiety in each state except QLD and WA [95%CI] = 1.03 [0.88, 1.19], −0.38 [−0.65, −0.1], 0.89 [0.37, 1.42], 1.01 [0.89, 1.12], 0.11 [−0.4, 0.62] percentage points for NSW, QLD, SA, VIC, WA.
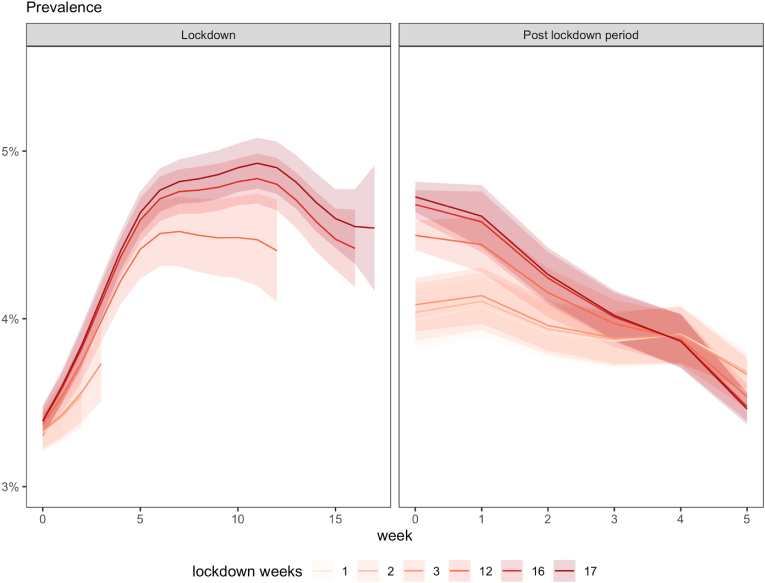
The estimated trajectories in Fig. 4 show similar patterns for the different lockdown durations, to the differences we observed for depression. The model estimates show anxiety prevalence increased rapidly week-on-week for the first 5 weeks, before falling after 10 weeks (adjusted R-squared = 65%, F = 33.53, p < .001). Adding the random effect of lockdown duration explained an additional 0.1 percentage points of variance (F = 10.01, p < .001).
Fig. 4.
Effect of lockdown on population prevalence of anxiety (±95%CI). Note: Figure shows the estimated effect of lockdown on the population prevalence of anxiety as a function of time (weeks). In the lockdown period (left), the Week 0 estimate represents the average prevalence in the period immediately prior to lockdown. In the post-lockdown period (right), Week 0 represents the average anxiety during the prior lockdown and the Week 5 estimate represents the average prevalence after the 4th week post-lockdown period and before the next lockdown.
The estimates of the post lockdown period further show the prevalence of anxiety declining over the four-week period modelled here (adjusted R-squared = 61.6%, F = 6.20, p < .001), and continuing to decline after this four-week period as indicated by the post-lockdown Week 5 estimate. Adding the random effect of lockdown duration explained an additional 1.1 percentage points of variance (F = 85.71, p < .001).
The varying effect of lockdown duration plotted in Fig. 4 shows that short lockdowns (1–3 weeks) tended to have less impact on anxiety prevalence over the same period than longer lockdowns, but this effect was not significantly different in the estimated marginal effects of different lockdown durations in Table 5.
Table 5.
Marginal effect of lockdown duration on anxiety.
| lockdown length (weeks) | marginal delta (%) | SE | lower 95%CI | upper 95%CI |
|---|---|---|---|---|
| 1 | 0.09 | 0.04 | 0.02 | 0.17 |
| 2 | 0.10 | 0.04 | 0.03 | 0.17 |
| 3 | 0.11 | 0.04 | 0.04 | 0.18 |
| 12 | 0.18 | 0.03 | 0.11 | 0.24 |
| 16 | 0.21 | 0.04 | 0.14 | 0.28 |
| 17 | 0.22 | 0.04 | 0.15 | 0.29 |
As with depression, the cumulative number of lockdowns had differential effects on anxiety prevalence (Table 6). Anxiety increased with each additional lockdown in VIC and NSW, whereas for the other states anxiety either decreased (QLD, WA) or there was no evidence of change (SA).
Table 6.
Marginal effect of lockdown number on anxiety.
| State | marginal delta (%) | SE | lower 95%CI | upper 95%CI |
|---|---|---|---|---|
| Victoria | 0.20 | 0.03 | 0.15 | 0.25 |
| New South Wales | 0.11 | 0.05 | 0.02 | 0.21 |
| Queensland | −0.12 | 0.03 | −0.18 | −0.07 |
| South Australia | −0.04 | 0.08 | −0.21 | 0.12 |
| Western Australia | −0.22 | 0.04 | −0.31 | −0.13 |
4. Discussion
This study is, to our knowledge, the first to describe how psychological distress rose and fell across multiple lockdowns, and assess whether mental wellbeing recovered following lockdowns.
4.1. Key results
Using high temporal resolution daily survey data from Australian respondents, we found that the prevalence of psychological distress tended to increase over the course of the pandemic in almost all states. The consistent increase we demonstrated was not reported in a meta-analysis by Robinson et al. (2022), in which most studies which found that symptoms of psychological distress tended to decline over the pandemic in European and North American countries after an initial rise, as health and wellbeing improved after an initial adverse response. Our data did not capture the immediate pandemic period and so there may also have been an initial increase in psychological distress that we may have not measured. However, this general trend may not represent a COVID-19 effect as there were increasing baseline rates of psychological distress in the community reported in the years prior to the pandemic (see Butterworth et al., 2020). This shifting baseline contaminates estimates of the average lockdown effect in other studies relying on comparisons between two timepoints unless carefully controlled. However, by considering the long-term trend in daily psychological distress enabled us to distinguish the temporal effects of lockdown and its alleviation.
Our results suggest that psychological distress, primarily depression and to a lesser extent anxiety, increased over lockdown periods, with lockdowns of 12 weeks or more producing a more rapid increase than shorter lockdowns. Lockdowns of one, two or three weeks had little to no impact on psychological distress prevalence, potentially because their short and limited duration was often communicated to the public prior to their imposition We found that the effect of lockdowns on psychological distress was not permanent, with the levels of psychological distress prevalence declining to near, but still slightly elevated, pre-lockdown levels within four weeks following the end of lockdown, and continued to decline over the subsequent post-lockdown period.
The results from this study are therefore consistent with previous work demonstrating poorer mental health during lockdown. However, our findings suggest that this adverse mental health effect was likely only experienced in the case of lockdowns lasting more than three weeks, and most of the increase in psychological distress was transitory once lockdowns ended. However, a residual effect of lockdown may remain. We also found (see Appendix Section 2) that at least part of the association between lockdown duration and psychological distress was mediated by financial concerns.
4.2. Strengths
A key strength of this study is that the data came from five States in one country where there is a relatively homogeneous health and social care systems, and social and population structures who experienced similar Federal economic responses to the pandemic. The state variation in lockdown timing and duration enables some of these effects to be at least partially controlled, and the specific effects of lockdown be more evident. However, the degree of restriction within each lockdown varied although we could discern no pattern of association between this and psychological distress. The temporal resolution of these data is the only available that we are aware of that can address our trajectory questions. Although the samples are large it is very likely that some respondents responded multiple times and these people will contribute more to the findings.
4.3. Limitations
Despite considerable effort in survey design, including stratified probabilistic sampling over a large sampling frame and adjustments to population controls including age group, region and gender, sampling bias may still be present in this dataset. In particular, as an internet-based social media user group, the survey is a nonrandom sample of the population in the countries/territories covered by UMD-CTIS. As such, any stable, time-invariant differences between people may contribute to bias in the current results, such as unadjusted differences in education or rurality (Bradley et al., 2021; but see Astley et al., 2021). The effect of such bias is likely to be restricted to the estimation of the intercept in the models used here, and not interact with the trajectories or slopes over time. Of more concern would be the presence of time-varying differences. For example, working people might have elevated levels of psychological distress and only find time to respond during lockdown and not after work responsibilities have resumed. Such time-varying effects on the outcome could bias the trajectories of psychological distress. That said, the representativeness of longitudinal studies, particularly over a long period of time with frequent follow-up, would also be affected by selection and attrition.
4.4. Generalizability and interpretation
Overall, these high temporal resolution data from a very large sample, although limited to only two psychological distress questions, provide a guide to how psychological distress rises and falls in the population over the course of repeated lockdowns. These findings may be useful for public health communication, and, assuming that demand for mental health services follows the same pattern, for policy makers and clinicians. They also remind us how resilient people are in general to major life stressors (Kettlewell et al., 2020), an observation often missing from the social discourse. An interesting avenue for future research is to examine the potential value of collecting related data from social media outlets to understand the consequences of government policy in large populations. Another possibility is to examine different sub-populations, such as age groups and gender, to study whether lockdown duration impacted the psychological distress trajectories of these groups in different ways.
Ethical statement
The UMD Global CTIS was a partnership between the University of Maryland and Facebook. The survey and sampling strategy was designed by the University of Maryland Joint Program in Survey Methodology, and full details of the methods of the stratified survey collection are described in Kreuter et al. (2020). The UMD Global CTIS data collection was approved by the UMD IRB (1,587,016–10).
Author statement
Ferdi Botha: Conceptualization, Methodology, Writing – Original Draft, Writing – Review & Editing, Project administration, Funding acquisition. Peter Butterworth: Conceptualization, Methodology, Writing – Original Draft, Writing – Review & Editing. Richard W. Morris: Conceptualization, Methodology, Software, Formal analysis, Data Curation, Writing – Original Draft, Writing – Review & Editing, Visualization, Project administration, Funding acquisition. Nick Glozier: Conceptualization, Methodology, Writing – Original Draft, Funding acquisition.
Declaration of competing interest
None.
Acknowledgement
We are grateful to three anonymous referees for helpful comments and suggestions. This research was supported by the Australian Government through the Australian Research Council's Centre of Excellence for Children and Families over the Life Course (Project ID CE200100025).
1.0 Supplementary methods
Daily sampling rate
The daily sampling rate of Facebook users who responded to either the depression or anxiety item between April 2020 and December 2021 is shown in Table A1 for each state, stratified by age group and gender:
Table A1.
Total respondents and average per day.
| State | Age | Total respondents (%) |
Average respondents per day |
||
|---|---|---|---|---|---|
| Females | Males | Females | Males | ||
| Victoria | 18–24 | 11,665 (65%) | 6262 (35%) | 19 | 10 |
| 25–44 | 39,705 (62%) | 24,775 (38%) | 65 | 41 | |
| 45–64 | 31,856 (59%) | 22,464 (41%) | 52 | 37 | |
| 65+ | 11,857 (52%) | 10,881 (48%) | 19 | 18 | |
| New South Wales | 18–24 | 10,464 (66%) | 5414 (34%) | 17 | 9 |
| 25–44 | 35,830 (62%) | 22,144 (38%) | 59 | 36 | |
| 45–64 | 29,227 (59%) | 19,906 (41%) | 48 | 33 | |
| 65+ | 11,447 (53%) | 10,173 (47%) | 19 | 17 | |
| Queensland | 18–24 | 9721 (69%) | 4268 (31%) | 16 | 7 |
| 25–44 | 31,656 (65%) | 16,888 (35%) | 52 | 28 | |
| 45–64 | 27,720 (61%) | 17,628 (39%) | 45 | 29 | |
| 65+ | 10,494 (52%) | 9653 (48%) | 17 | 16 | |
| South Australia | 18–24 | 3978 (67%) | 1971 (33%) | 7 | 4 |
| 25–44 | 12,547 (65%) | 6847 (35%) | 21 | 11 | |
| 45–64 | 16,214 (64%) | 9046 (36%) | 27 | 15 | |
| 65+ | 6863 (54%) | 5817 (46%) | 11 | 10 | |
| Western Australia | 18–24 | 4594 (65%) | 2463 (35%) | 8 | 4 |
| 25–44 | 17,431 (64%) | 9952 (36%) | 29 | 16 | |
| 45–64 | 18,063 (60%) | 11,868 (40%) | 30 | 19 | |
| 65+ | 7510 (52%) | 7044 (48%) | 12 | 12 | |
Australian demographics (age and sex)
Table A2 shows age and sex distributions from the 2021 national Census for Australia and each state, for comparison with the demographic features of Facebook users in our sample (Table 2).
Table A2.
National Census data 2021
| Characteristic | Australia N = 25,422,788 | VIC N = 6,503,491 | NSW N = 8,072,163 | QLD N = 5,156,138 | SA N = 1,781,516 | WA N = 2,660,026 |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Females | 12,877,635 (51%) | 3,302,528 (51%) | 4,087,995 (51%) | 2,615,736 (51%) | 902,924 (51%) | 1,337,171 (50%) |
| Males | 12,545,154 (49%) | 3,200,963 (49%) | 3,984,166 (49%) | 2,540,404 (49%) | 878,592 (49%) | 1,322,855 (50%) |
| Age | ||||||
| 18-24 | 2,150,360 (11%) | 554,388 (11%) | 674,712 (11%) | 444,934 (11%) | 148,273 (10%) | 217,581 (11%) |
| 25-44 | 7,112,430 (36%) | 1,894,231 (37%) | 2,245,196 (36%) | 1,389,541 (35%) | 461,947 (33%) | 751,844 (37%) |
| 45-64 | 6,256,922 (31%) | 1,573,432 (31%) | 1,978,732 (31%) | 1,289,431 (32%) | 451,788 (32%) | 661,700 (32%) |
| 65+ | 4,378,094 (22%) | 1,092,833 (21%) | 1,424,141 (23%) | 875,603 (22%) | 356,325 (25%) | 428,619 (21%) |
*n (%).
2.0 Supplementary results
In follow-up sensitivity analyses we included the number of daily new infections and daily financial concerns as explanatory variables.
Each variable was added to the model as a penalized cubic regression spline, and we calculated the marginal effects of each lockdown duration as before. The results, when compared to the marginal effects in the main report, indicate the mediating effect of each variable (financial concerns or new infections) on the effect of lockdown duration.
2.1 Financial concern
Financial concerns during lockdown have been shown to be a significant mediating factor of psychological distress for various disadvantaged groups (Botha et al., 2022). Financial concern was measured by a single item:
“How worried are you about your household’s finances in the next month?” (Very, somewhat, not too worried, not at all)
We included the weighted percentage of people reporting they were “very” or “somewhat” worried about their household finances as representing financial concern.
Table A3.
Marginal effect of lockdown length on depression after including financial concerns
| lockdown length (weeks) | marginal delta (%) | SE | lower 95%CI | upper 95%CI |
|---|---|---|---|---|
| 1 | 0.08 | 0.05 | −0.01 | 0.17 |
| 2 | 0.10 | 0.04 | 0.01 | 0.19 |
| 3 | 0.12 | 0.04 | 0.04 | 0.20 |
| 12 | 0.28 | 0.03 | 0.21 | 0.34 |
| 16 | 0.35 | 0.04 | 0.27 | 0.42 |
| 17 | 0.36 | 0.04 | 0.29 | 0.44 |
Adding financial concerns improved the fit with depression prevalence (explained deviance increased from 76.1% to 79.1%). In comparison to Table 3 (Marginal effect of lockdown duration on depression), the marginal effect of lockdown duration on depression prevalence was reduced by approximately 0.28 percentage points after including financial concerns. The remaining effect was indistinguishable from zero for short duration lockdowns (e.g., 1 week), and the effect at longer durations is almost half that observed without financial concerns (e.g., 0.36 v 0.64 during 17-week lockdown). Nevertheless, lockdowns of 2-week or longer tended to increase depression prevalence, with or without accounting for financial concerns.
Table A4.
Marginal effect of lockdown length on anxiety after including financial concerns
| lockdown length (weeks) | marginal delta (%) | SE | lower 95%CI | upper 95%CI |
|---|---|---|---|---|
| 1 | −0.12 | 0.04 | −0.20 | −0.04 |
| 2 | −0.11 | 0.04 | −0.19 | −0.04 |
| 3 | −0.11 | 0.04 | −0.18 | −0.03 |
| 12 | −0.04 | 0.04 | −0.11 | 0.03 |
| 16 | −0.02 | 0.04 | −0.09 | 0.06 |
| 17 | −0.01 | 0.04 | −0.09 | 0.07 |
Adding financial concerns improved the fit with anxiety prevalence (explained deviance increased from 65.2% to 69.5%). Comparing the marginal effect of lockdown duration on anxiety prevalence with and without financial concerns in the model (e.g., Table 4. Marginal effect of lockdown duration on anxiety), reveals financial concerns substantially mediated anxiety over varying lockdown durations. After accounting for financial concerns, short lockdowns up to 3-weeks tended to reduce anxiety, while the effect of longer lockdowns was indistinguishable from zero.
2.2 Fear of infection
Other factors such as daily media reports of the rate of new infections, or announcement of temporary changes in government support could also drive changes in psychological distress on a daily basis. Even people who have not directly experienced pandemic-related stressors such as infection, bereavement or job loss can nevertheless be negatively affected by the fear of experiencing them, often fueled by exposure to a continuous deluge of negative media coverage of the spreading infection rates in the community (Bower et al., 2021; Digby, Winton-Brown, Finlayson, Dobson, & Bucknall, 2021; Garfin, Silver, & Holman, 2020). In Australia, the number of new infections was reported daily at official government press conferences, which were widely reported and tracked in the media. Thus like lockdown, their impact on psychological distress may be transient and shortlived – difficult to detect without daily measurements of both. However controlling for daily changes in the salient influence of infection rate when estimating trends in distress has not been widely done.
Although the UMD Global CTIS included a single item measuring fear of infection, the responses were only collected between May 1st, 2020 and May 20th, 2021, which excludes the extended lockdown period in NSW. Because of the restricted availability of this item, we adopted another measure as a proxy for fear of infection. Daily case numbers (new infections) reported by each State Government for the entire pandemic period were collected and curated by Anthony Macali at covidlive. com.au, and downloaded from www.covidlive.com.au/covid-live.csv on the 01-15-2022.
The correlation between (log) daily cases and responses to the fear of infection item over 2020 in VIC (i.e., the time period both were available over an extended lockdown period) was Pearson 0.931.
Table A5.
Marginal effect of lockdown length on depression after including new infections
| lockdown length (weeks) | marginal delta (%) | SE | lower 95%CI | upper 95%CI |
|---|---|---|---|---|
| 1 | 0.35 | 0.05 | 0.25 | 0.44 |
| 2 | 0.36 | 0.05 | 0.27 | 0.46 |
| 3 | 0.38 | 0.05 | 0.29 | 0.47 |
| 12 | 0.51 | 0.04 | 0.43 | 0.59 |
| 16 | 0.57 | 0.05 | 0.48 | 0.66 |
| 17 | 0.58 | 0.05 | 0.49 | 0.68 |
Adding new infections improved the fit with depression prevalence (explained deviance increased from 76.1% to 76.7%). The marginal effect of lockdown duration on depression prevalence was very similar with and without new infections in the model (compare to Table 3. Marginal effect of lockdown duration on depression).
Table A6.
Marginal effect of lockdown length on anxiety after including new infections
| lockdown length (weeks) | marginal delta (%) | SE | lower 95%CI | upper 95%CI |
|---|---|---|---|---|
| 1 | 0.09 | 0.04 | 0.02 | 0.17 |
| 2 | 0.10 | 0.04 | 0.03 | 0.17 |
| 3 | 0.11 | 0.03 | 0.05 | 0.18 |
| 12 | 0.21 | 0.03 | 0.16 | 0.26 |
| 16 | 0.25 | 0.03 | 0.19 | 0.31 |
| 17 | 0.26 | 0.03 | 0.20 | 0.32 |
Adding new infections improved the fit with anxiety prevalence (explained deviance increased from 65.2% to 66.1%). The marginal effect of lockdown duration on anxiety prevalence was very similar with and without new infections in the model (compare to Table 5. Marginal effect of lockdown duration on anxiety).
Overall, the results including mediating variables indicated almost all the effect of lockdown on anxiety was mediated by financial concerns, as well as a substantial portion of the effect of lockdown on depression. Indeed, once financial concerns were explained, short lockdowns tended to decrease anxiety prevalence and had little further impact on depression. By contrast, new infections (a proxy for fear of infection) had little mediating impact on depression or anxiety.
Model diagnostics
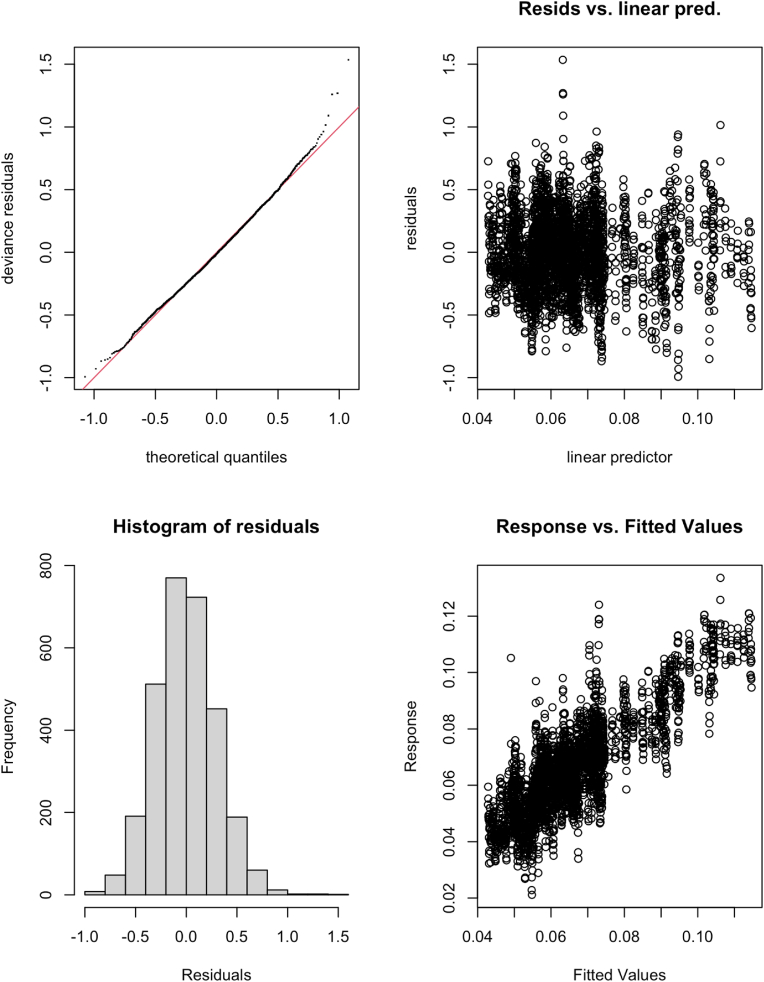
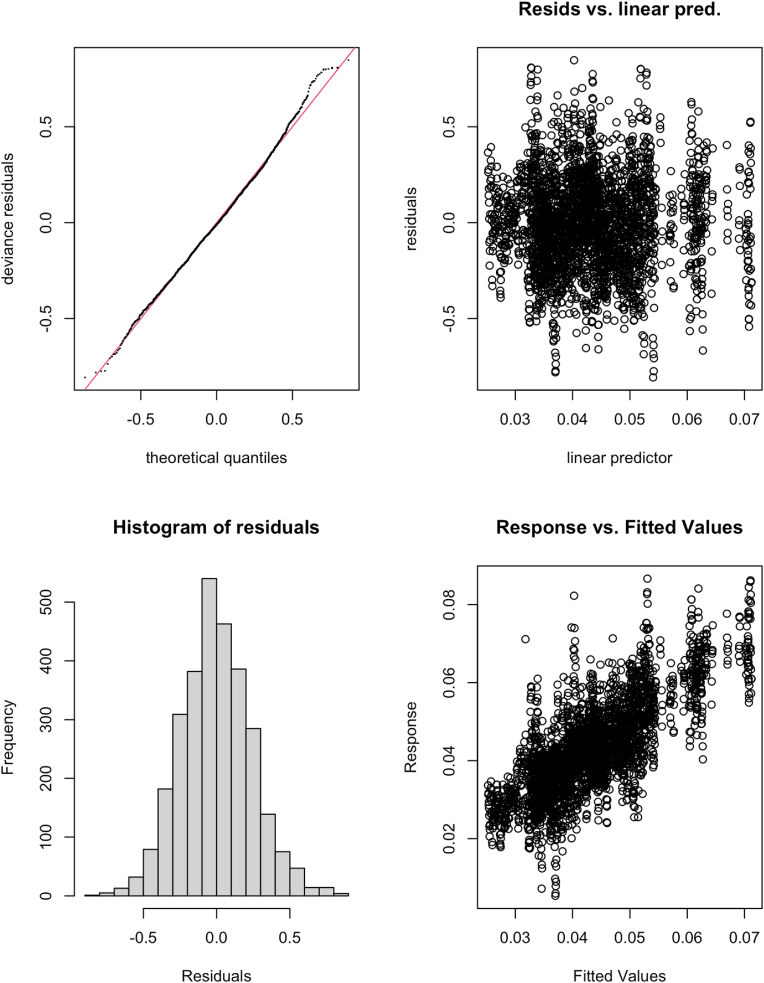
Model fits were checked and assessed for oversmoothing, as well as violation of the distributional assumptions.
The k-index represents the adequacy of the basis dimension for the fit (Wood, 2017; section 5.9). The further below 1, the more likely there is a missed pattern left in the residuals. The k-index for the random effect of lockdown duration were below 1 in the models of depression (k-index = 0.5) and anxiety (k-index = 0.52).
Four residual plots were also inspected for each fit, with plots of deviance residuals against approximate theoretical quantiles of the deviance residual distribution according to the fitted model. The Q-Q plot (top left) indicated some deviation in the tails of the distribution from normal, however there were no identifiable pattern in the residual vs predicted scatterplot, and the histogram of residuals was approximately normal.
Effect of lockdown duration on depression model.
Effect of lockdown duration on anxiety model.
Data availability
Data will be made available on request.
References
- Aknin L.B., Andretti B., Goldszmidt R., Helliwell J.F., Petherick A., De Neve J.-E., et al. Policy stringency and mental health during the COVID-19 pandemic: A longitudinal analysis of data from 15 countries. The Lancet Public Health. 2022;7(5):e417–e426. doi: 10.1016/S2468-2667(22)00060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Slade T. Interpreting scores on the Kessler psychological distress scale (K10) Australian & New Zealand Journal of Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842X.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Astley C.M., Tuli G., Mc Cord K.A., Cohn E.L., Rader B., Varrelman T.J., et al. Global monitoring of the impact of the COVID-19 pandemic through online surveys sampled from the Facebook user base. Proceedings of the National Academy of Sciences. 2021;118(51) doi: 10.1073/pnas.2111455118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berle D., Starcevic V., Milicevic D., Moses K., Hannan A., Sammut P., et al. The factor structure of the Kessler-10 questionnaire in a treatment-seeking sample. The Journal of Nervous and Mental Disease. 2010;198(9):660–664. doi: 10.1097/NMD.0b013e3181ef1f16. [DOI] [PubMed] [Google Scholar]
- Botha F., Butterworth P., Wilkins R. Protecting mental health during periods of financial stress: Evidence from the Australian Coronavirus Supplement income support payment. Social Science & Medicine. 2022;115158 doi: 10.1016/j.socscimed.2022.115158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower M., Smout S., Ellsmore S., Donohoe-Bales A., Sivaprakash P., Lim C., et al. COVID-19 and Australia's mental health: An overview of academic literature, policy documents, lived experience accounts, media and community reports. The University of Sydney; Australia's Mental Health Think Tank. 2021. https://ses.library.usyd.edu.au/bitstream/handle/2123/26777/AustraliasMentalHealthThinkTank-EvidenceSummary-COVID-MentalHealth.pdf Retrieved from.
- Bradley V.C., Kuriwaki S., Isakov M., Sejdinovic D., Meng X.-L., Flaxman S. Unrepresentative big surveys significantly overestimated US vaccine uptake. Nature. 2021;600(7890):695–700. doi: 10.1038/s41586-021-04198-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butterworth P., Schurer S., Trinh T.-A., Vera-Toscano E., Wooden M. Effect of lockdown on mental health in Australia: Evidence from a natural experiment analysing a longitudinal probability sample survey. The Lancet Public Health. 2022 doi: 10.1016/S2468-2667(22)00082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butterworth P., Watson N., Wooden M. Trends in the prevalence of psychological distress over time: Comparing results from longitudinal and repeated cross-sectional surveys. Frontiers in Psychiatry. 2020:1345. doi: 10.3389/fpsyt.2020.595696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandola T., Kumari M., Booker C.L., Benzeval M. The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychological Medicine. 2020:1–10. doi: 10.1017/S0033291720005048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. Journal of Psychiatric Research. 2021;136:603–609. doi: 10.1016/j.jpsychires.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digby R., Winton-Brown T., Finlayson F., Dobson H., Bucknall T. Hospital staff well-being during the first wave of COVID-19: Staff perspectives. International Journal of Mental Health Nursing. 2021;30(2):440–450. doi: 10.1111/inm.12804. [DOI] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frijters P., Johnston D.W., Shields M.A. Life satisfaction dynamics with quarterly life event data. The Scandinavian Journal of Economics. 2011;113(1):190–211. doi: 10.1111/j.1467-9442.2010.01638.x. [DOI] [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology. 2020;39(5):355. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertz-Palmor N., Moore T.M., Gothelf D., DiDomenico G.E., Dekel I., Greenberg D.M., et al. Association among income loss, financial strain and depressive symptoms during COVID-19: Evidence from two longitudinal studies. Journal of Affective Disorders. 2021;291:1–8. doi: 10.1016/j.jad.2021.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickie I.B., Andrews G., Davenport T.A. Measuring outcomes in patients with depression or anxiety: An essential part of clinical practice. Medical Journal of Australia. 2002;177(4):205–207. doi: 10.5694/j.1326-5377.2003.tb05056.x. [DOI] [PubMed] [Google Scholar]
- Jeong H., Yim H.W., Song Y.-J., Ki M., Min J.-A., Cho J., et al. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiology and Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.-L., et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., et al. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kettlewell N., Morris R.W., Ho N., Cobb-Clark D.A., Cripps S., Glozier N. The differential impact of major life events on cognitive and affective wellbeing. SSM-Population Health. 2020;10 doi: 10.1016/j.ssmph.2019.100533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter F., Barkay N., Bilinski A., Bradford A., Chiu S., Eliat R., et al. Partnering with a global platform to inform research and public policy making. Survey Research Methods. 2020;14:159–163. doi: 10.18148/srm/2020.v14i2.7761. [DOI] [Google Scholar]
- Merson F., Newby J., Shires A., Millard M., Mahoney A. The temporal stability of the Kessler psychological distress scale. Australian Psychologist. 2021;56(1):38–45. doi: 10.1080/00050067.2021.1893603. [DOI] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2013. R: A language and environment for statistical computing.http://www.R-project.org/ Retrieved from. [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano-Alarcón M., Kentikelenis A., Mckee M., Stuckler D. Impact of COVID-19 lockdowns on mental health: Evidence from a quasi-natural experiment in England and Scotland. Health Economics. 2022;31(2):284–296. doi: 10.1002/hec.4453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T., Grove R., Burgess P. Kessler psychological distress scale: Normative data from the 2007 Australian national survey of mental health and wellbeing. Australian and New Zealand Journal of Psychiatry. 2011;45(4):308–316. doi: 10.3109/00048674.2010.543. [DOI] [PubMed] [Google Scholar]
- Sunderland M., Hobbs M.J., Anderson T.M., Andrews G. Psychological distress across the lifespan: Examining age-related item bias in the Kessler 6 psychological distress scale. International Psychogeriatrics. 2012;24(2):231–242. doi: 10.1017/S1041610211001852. [DOI] [PubMed] [Google Scholar]
- Sunderland M., Mahoney A., Andrews G. Investigating the factor structure of the Kessler psychological distress scale in community and clinical samples of the Australian population. Journal of Psychopathology and Behavioral Assessment. 2012;34(2):253–259. doi: 10.1007/s10862-012-9276-7. [DOI] [Google Scholar]
- Twenge J.M., Cooper A.B. 2020. The expanding class divide in happiness in the United States, 1972–2016. Emotion. [DOI] [PubMed] [Google Scholar]
- Wood S.N. Stable and efficient multiple smoothing parameter estimation for generalized additive models. Journal of the American Statistical Association. 2004;99(467):673–686. doi: 10.1198/016214504000000980. [DOI] [Google Scholar]
- Wood S.N. Generalized additive models. Chapman and Hall; Boca Raton, FL: 2017. [Google Scholar]
- Wood S.N., Pya N., Säfken B. Smoothing parameter and model selection for general smooth models. Journal of the American Statistical Association. 2016;111(516):1548–1563. doi: 10.1080/01621459.2016.1180986. [DOI] [Google Scholar]
- Wu S., Yao M., Deng C., Marsiglia F.F., Duan W. Social isolation and anxiety disorder during the COVID-19 pandemic and lockdown in China. Journal of Affective Disorders. 2021;294:10–16. doi: 10.1016/j.jad.2021.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.