Dear Editor,
In 2020, widespread attention was turned to evaluate the supply and demand for mechanical ventilation in combination with critical care workforce staffing strategies to accommodate surges in COVID-19 critical illness (Tsai et al., 2022). Beyond critical care demand, oxygen therapy is a predominant first-line intervention for hypoxemic respiratory failure across a broad range of settings, including delivery via nasal cannula. Thus, we examine longitudinal oxygen utilization during the first 24 months of the COVID-19 pandemic to quantify oxygen consumption increases inclusive of high-flow nasal cannula (HFNC) use for patients hospitalized with COVID-19 in a large and diverse integrated health system.
Methods
Data were drawn from a prospective, cross-sectional, observational study conducted in collaboration with the Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS): COVID-19 Registry. We analyzed the volume of oxygen used, types of oxygen support, and the volume of hospitalized patients with and without COVID-19 over a 2-year period (April 2020 and March 2022) in a 4,457-bed integrated health system of 26 adult acute care hospitals serving rural, suburban and urban populations in the Southern region of the United States. The VIRUS registry was approved by the Baylor Scott & White Research Institute Institutional Review Board. We followed the STROBE reporting guideline.
Results
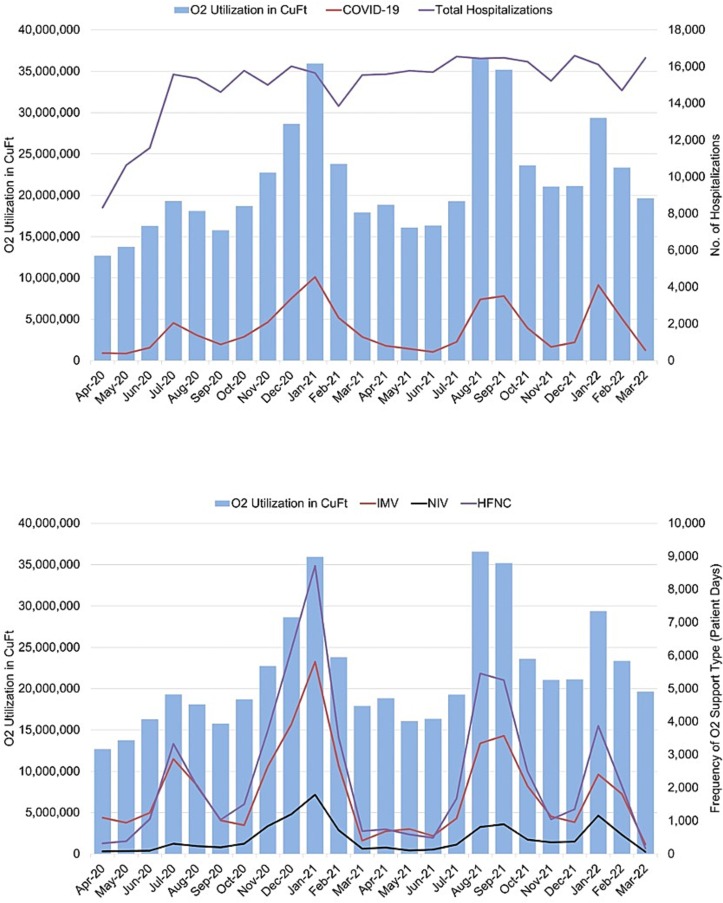
Oxygen consumption peaks coincided with peaks in COVID-related hospitalization, including up to a 134 % increase in volume of oxygen used (Fig. 1 a). The predominant type of oxygen support for patients with COVID-related hospitalizations was delivered via HFNC (Fig. 1b). High levels of oxygen consumption coincide with high levels of HFNC use for patients hospitalized with COVID-19. Reciprocal changes in HFNC use during non-peak periods of COVID-19 hospitalizations coincided with lower volumes of oxygen utilization. Widespread adoption of HFNC within an integrated health system setting is discernible within the first 6 months. Furthermore, the dual increase in hospitalization volumes due to COVID-19 and oxygen flow rates for HFNC of 30–60 L/min (compared with 20–30 L/min for noninvasive and invasive mechanical ventilation), illustrate a sustained high demand for medical grade oxygen.
Fig. 1.
a. Oxygen utilization and hospitalization volumes (April 2020 – March 2022). b. Oxygen utilization and oxygen support types for COVID-19 hospitalizations (April 2020 – March 2022) Abbreviations: O2 = CuFt = cubic feet; O2 = oxygen; IMV = invasive mechanical ventilation; NIV = non-invasive mechanical ventilation; HFNC = high-flow nasal cannula.
Discussion
Oxygen therapy is a potentially scarce resource in the context of a long-term respiratory pandemic. While oxygen scarcity is a known challenge in low-resource settings (Fowler et al., 2008), the COVID-19 pandemic has introduced the relevance of oxygen conservation strategies at a global level to consider disaster management beyond short-term access problems to oxygen supply associated with natural disasters (e.g., hurricanes) (Blakeman and Branson, 2013). Similar to Days of Cash On Hand (DCOH) metrics, oxygen supply affects the solvency and viability of healthcare delivery, with some hospitals reporting less than a 48-hour supply of oxygen in reserve (Parkinson, 2021). Further, the demand for high-flow oxygen therapy has been established as a non-invasive intervention for respiratory failure as early concerns related to efficacy and aerosolization were tempered by favorable outcomes. The combination of a respiratory virus pandemic with clinical practice pattern changes creates a sustained change in demand for medical oxygen with increases in average and peak utilization.
Ethical statement
The VIRUS registry was approved by the Baylor Scott & White Research Institute Institutional Review Board. The approval number is #020-119. The ClinicalTrials.gov identifier for the VIRUS registry is NCT04323787. The reporting of this study conforms to the STROBE statement.
Author contributions
Concept and design: Arroliga, White, Danesh, Jimenez.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of manuscript: White, Danesh, Arroliga, Jimenez.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: All authors.
Obtained funding: Danesh.
Administrative, technical, or material support: Danesh, Arroliga.
Supervision: Danesh, Arroliga.
Name and location of the institution where the study was performed:
Baylor Scott & White Health, Texas, United States.
Name, date and location of any meeting or forum where research data were previously presented, and who presented:
The full-length Research Letter and Fig. 1a have not been previously presented. An abbreviated meeting abstract version with Fig. 1b has been submitted to the American Thoracic Society (ATS) 2023 meeting for consideration. Status as of November 21, 2022: Under review with ATS meeting abstract reviewers for decisions in mid-January 2023 for meeting abstract publication in May 2023.
Sources of financial support:
This work was partially funded by the Cardiovascular Research Review Committee of the Baylor Healthcare System Foundation, Society of Critical Care Medicine, and the Gordon and Betty Moore Foundation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Blakeman T.C., Branson R.D. Oxygen supplies in disaster management. Resp. Care. 2013;58(1):173–183. doi: 10.4187/respcare.02088. [DOI] [PubMed] [Google Scholar]
- Fowler R.A., Adhikari N.K.J., Bhagwanjee S. Clinical review: critical care in the global context–disparities in burden of illness, access, and economics. Crit. Care. 2008;12(5):225. doi: 10.1186/cc6984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkinson N. Oxygen supplies tight in Southern US states. In. Gas World. 2021: gasworld.com. Retrieved from https://www.gasworld.com/oxygen-supplies-tight-in-southern-us-states/2021613.article.
- Tsai T.C., Orav E.J., Jha A.K., Figueroa J.F. National estimates of increase in US mechanical ventilator supply during the COVID-19 pandemic. JAMA Netw. Open. 2022;5(8) doi: 10.1001/jamanetworkopen.2022.24853. [DOI] [PMC free article] [PubMed] [Google Scholar]