Abstract
Background
The COVID-19 pandemic demanded intensive care units (ICUs) globally to expand to meet increasing patient numbers requiring critical care. Critical care nurses were a finite resource in this challenge to meet growing patient numbers, necessitating redeployment of nursing staff to work in ICUs.
Objective
Our aim was to describe the extent and manner by which the increased demand for ICU care during the COVID-19 pandemic was met by ICU nursing workforce expansion in the late 2021 and early 2022 in Victoria, Australia.
Methods
This is a retrospective cohort study of Victorian ICUs who contributed nursing data to the Critical Health Information System from 1 December 2021 to 11 April 2022. Bedside nursing workforce data, in categories as defined by Safer Care Victoria’s pandemic response guidelines, were analysed. The primary outcome was ‘insufficient ICU skill mix’—whenever a site had more patients needing 1:1 critical care nursing care than the mean daily number of experienced critical care nursing staff.
Results
Overall, data from 24 of the 47 Victorian ICUs were eligible for analysis. Insufficient ICU skill mix occurred on 10.3% (280/2725) days at 66.7% (16/24) of ICUs, most commonly during the peak phase from December to mid-February. The insufficient ICU skill mix was more likely to occur when there were more additional ICU beds open over the ‘business-as-usual’ number. Counterfactual analysis suggested that had there been no redeployment of staff to the ICU, reduced nursing ratios, with inability to provide 1:1 care, would have occurred on 15.2% (415/2725) days at 91.7% (22/24) ICUs.
Conclusion
The redeployment of nurses into the ICU was necessary. However, despite this, at times, some ICUs had insufficient staff to cope with the number and acuity of patients. Further research is needed to examine the impact of ICU nursing models of care on patient outcomes and on nurse outcomes.
Keywords: Critical care nursing, Intensive care unit, Staffing levels, Workforce, Workload management
1. Introduction
The coronavirus 2019 (COVID-19) pandemic has had an unprecedented effect on the number of severely ill patients admitted to intensive care units (ICUs) globally. Consequently, surge models evolved to expand ICU capacity including space, beds, equipment, and deployment of staff.[1], [2], [3], [4], [5], [6], [7] Early analyses in Australia suggested that treble the number of ICU beds might be required to accommodate the predicted surge in the critically ill population, but doing so would necessitate a 269% increase in registered nurses over the baseline.8 In April 2020, to monitor ICU demand and capacity, the Critical Health Resource Information System (CHRIS) was developed as a collaboration between The Australian and New Zealand Intensive Care Society (ANZICS) and Ambulance Victoria and funded by The Australian Government Department of Health.9 In May 2020, Safer Care Victoria developed the ‘Coronavirus (COVID-19) Intensive Care Unit Surge Workforce Models Of Care Delivery’ guideline to address structured ICU workforce surge planning, which were updated in September 2021 (V2).10
ICU workforce shortages, particularly nursing, provided an ongoing discussion as a potential key limiter to ICU capacity, however, workforce data were not collected in CHRIS. Consequently, through collaboration and consultation with the Victorian ICU Nurse Unit Managers Community of Practice, nursing workforce data were added in November 2021, reflecting the categories of surge workforce as outlined by the Safer Care Victoria Guidelines (V2).10 The extent to which workforce redeployment and workforce expansion occurred, and the potential effect on delivery of 1:1 care for critically ill patients within the ICU, has not been described. This is important as there is substantial evidence that the number of critical care nurses impacts patient outcomes, nurse outcomes, and health services.11 , 12 For example, low levels of critical care nurses are associated with increased patient mortality, increased nosocomial infections, and higher hospital costs.12 Additionally, poor ICU nurse staffing levels can affect nurse wellbeing, including increasing burnout, depersonalisation, and emotional exhaustion.13 Thus, we sought to quantify the critical care nursing deficit associated with the pandemic surge–related increase in ICU capacity.
2. Objectives
Our aim was, firstly, to describe the extent and manner by which the increased demand for ICU care during the COVID-19 pandemic was met by ICU nursing workforce expansion in late 2021 and early 2022 in Victoria; secondly, to quantify provision of redeployed non-critical care nursing staff working in ICUs; and thirdly, to attempt to identify factors associated with insufficient provision of critical care nursing staff.
3. Methods
3.1. Design and setting
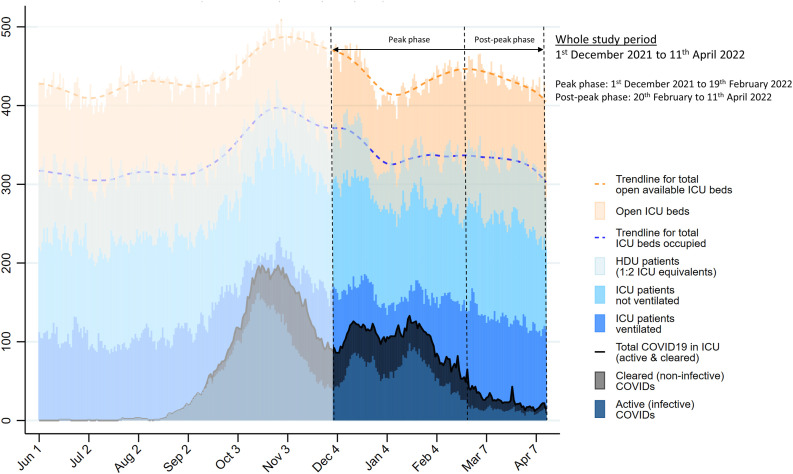
We conducted a retrospective cohort study at Victorian public and private, adult and paediatric hospital ICUs between 1st December 2021 and 11th April 2022. This study period was after the peak of the delta wave (peak in mid-October 2021 of 2257 new community cases reported in Victoria) and during the omicron wave (peak in mid-January 2022 of 51,144 new community cases reported in Victoria).14 Associated hospital admission data for all of 2021 and until the end of the study period is in Fig. 1 .
Fig. 1.
Study period (1st December 2021 to 11th April 2022) where nursing skill mix information was available, shown against the overall number of patients in all 45 active Victorian ICUs, open ICU beds and numbers of COVID-19 patients in the ICU between 1st Jun 2021 and 11th April 2022. The trendline for mean daily occupied ICU beds in all Victorian hospitals is shown by the blue dotted line and represents all ICU equivalent patients (i.e., all patients requiring 1:1 nursing + [0.5 x the number of patients requiring 1:2 nursing within ICU]). ICU, intensive care unit. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3.2. Data source
All data were extracted from CHRIS. ICU staff entered ‘snapshot’ aggregated census information about local critical care resources, demand and activity, between two and four times per day. No individual patient or outcome data were entered. ICU Nurse Unit Managers (NUM) at all Victorian hospitals were also invited to voluntarily collect additional information about nurse staffing skill mix at least once and up to four times per day. The number of staff providing direct patient care at the timepoint considered was entered. ICU nursing skill mix was categorised into four groups as defined by the Safer Care Victoria guidelines V2.10
-
•
Group One: experienced critical care nursing staff including clinical nurse specialists, associate nurse unit managers, postgraduate critical care nurses and nurses with 5+ years of current/continuous ICU experience
-
•
Group Two: early career critical care nursing staff including foundation year/transition to ICU speciality nurses, 2021 postgraduate ICU students (employment study model), nurses with critical care experience not normally working in ICU pre-pandemic
-
•
Group Three: redeployed nursing staff with no ICU experience (novice to ICU)
-
•
Group Four: registered undergraduate students of nursing, enrolled nurses and allied health staff providing direct patient care
The mean daily values for each nursing skill mix group were extracted. For the purposes of the study, Groups One and Two were considered as critical care registered nurses (CCRN). Groups Three and Four were considered as non-critical care registered nurses (non-CCRN). Both these groups reflect ICU nursing expansion as Group Three were redeployed nursing staff novice to ICU and Group Four were staff that would not normally be responsible for direct patient care of an allocated ICU patient.
The following data were also extracted as daily mean values for each hospital: the number of patients requiring 1:1 critical care nursing and invasive mechanical ventilation,15 the number of high-dependency patients requiring 1:2 critical care nursing,15 the number of patients with COVID-19 within each ICU and in other wards outside of ICU, the daily number of open ICU beds, the baseline number of open ICU beds prior to the pandemic, the number of critical care staff unavailable due to COVID-19 illness/exposure, and the ICU Activity Index. The ICU Activity Index is a calculated ‘score’ which indicates the acuity level within each ICU. A value over two represents a very busy ICU which is potentially under strain.9 Daily mean occupancy was calculated as [the total number of 1:1 nursed patients + (0.5 × 1:2 high-dependency patients)] divided by the total daily number of open ICU beds.
3.3. Outcomes
The primary outcome was ‘insufficient ICU skill mix’. This outcome was met whenever a site had more patients needing 1:1 critical care nursing care than the mean daily number of CCRN staff. For instance, a site that had 10 patients who required 1:1 critical care nursing and only had nine CCRNs available would be considered as having ‘insufficient skill mix’ on that day. The number of high-dependency patients requiring 1:2 nursing within the ICU was not considered in this calculation.
Two secondary outcomes were considered. The secondary outcome of ‘insufficient ventilated skill mix’ was met whenever a site had more patients needing invasive mechanical ventilation than the number of CCRN staff. The secondary outcome of ‘reduced ICU nursing ratio’ was met whenever there were more ‘ICU equivalent’ patients than the total number of bedside nursing staff. For instance, a site with 10 patients who required 1:1 critical care nursing and six high-dependency patients who required 1:2 nursing (i.e., 13 ‘ICU equivalents’) and a total of 12 or fewer nursing staff involved in direct patient care (from all four groups) would be classified as having ‘reduced ICU nursing ratio’ for that day.
3.4. Sample size
A convenience sample based on the number of hospitals who contributed data for more than 2 months during the 5-month study period was chosen.
3.5. Statistical analysis
Data are presented as the percentage (number/proportion) for categorical data or median (interquartile range) for continuous data. All continuous data were assessed for normality and found to be nonparametrically distributed. Chi-square, Wilcoxon rank-sum and Kruskal–Wallis tests were used to compare groups depending on the type of data, and number of groups examined. After assessing for colinearity, mixed-effects logistic regression was used to determine variables independently associated with the primary outcome, with site entered as a random effect with a random intercept per facility applied. A P value of <0.05 was considered statistically significant. All data were analysed using Stata version 16.1, College Station, Texas. No imputation for missing data was performed.
Following the main analysis which assessed the impact of observed redeployment of staff into ICUs during the study period, a counterfactual analysis was conducted to assess hypothetical nursing ratios that would have been present in the absence of any redeployed noncritical care trained staff. This analysis recalculated nursing ratios assuming the daily number of critical care–trained staff (Groups One and Two) and the number of patients present within each ICU remained unchanged, but there were zero redeployed staff present from Groups Three and Four. This was in recognition of the fact that without redeployment of nursing staff within the ICU to meet the additional demand for ICU beds, nursing ratios would have been even lower than measured.
3.6. Subgroups
Outcomes for all ICUs for the whole study period are reported and for two time periods: peak (1st December 2021 to 19th February 2022) and post-peak (20th February to 11th April 2022, after daily Victorian ICU director cluster demand meetings were ceased and switched to twice weekly) phases. Outcomes are also reported by hospital type. Hospitals were classified into one of five groups as tertiary, metropolitan, rural/regional, private, or paediatric.
3.7. Funding and ethics
The study was self-funded by the researchers and was approved as a low-risk project by the Human Research and Ethics Committee of the Alfred Hospital (HREC 246/22).
4. Results
All 47 ICUs in Victoria contributed daily data about ICU resources and activity. Of these, 32 hospitals also provided information on nursing skill mix. Eight were excluded because of contributing fewer than 2 months' staffing data each, leaving 24 participating ICUs over the 132-day study period. These 24 participating ICUs represent 71% (344/486) of all the baseline ICU beds in Victoria. In total, nursing skill mix data were available for 86% (2725/3168) of all days. At least 20 of the 24 hospitals contributed nursing skill mix data on 89% (118/132) of the days, but there were only 4 days when all 24 hospitals contributed data. Appendix table 1 shows the basic characteristics and number of ICU beds at study hospitals. All hospital types were represented.
ICU capacity, patient needs, and staffing data were highly variable (Fig. 1; Table 1 ). In summary, the median number of open ICU beds was 8, with a maximum of 65; the median daily number of ventilated patients was 2.5, with a maximum of 46.7, and the median daily number of COVID-19 patients in each ICU was 1, with a maximum of 32.3. The total daily number of patients and open ICU beds in all Victorian ICUs between 1st June 2021 and 11th April 2022, and the study period (1st December 2021 to 11th April 2022) over which nursing skill mix data were available for contributing hospitals are shown in Fig. 1. The daily number of all 1:1 nursed, ventilated, and COVID-19 patients in the 24 study hospital ICUs during the study period are shown in Appendix fig. 1.
Table 1.
Staffing and activity characteristics of ICUs on days with and without insufficient ICU skill-mix (more patients needing 1:1 critical care nursing than available CCRNs: primary study outcome).
| Primary outcome: Insufficient ICU skill-mix | All days | No | Yes | P value |
|---|---|---|---|---|
| Days with more patients needing 1:1 nursing than CCRNs, % (number) | - | 89.7% (2445/2725) | 10.3% (280/2725) | N/A |
| Secondary outcome: Insufficient ventilated skill-mix | 0.7% (19/2725) | 0% (0/2445) | 6.8% (19/280) | N/A |
| Secondary outcome: Reduced ICU nursing ratio | 3% (82/2725) | 1.8% (43/2445) | 13.9% (39/280) | <0.001 |
| Mean daily CCRNs per site | 8 (5-17) [1, 70] | 8 (5-17) [2, 70] | 8 (4-23) [1, 58] | 0.33 |
| Group 1 (CCRN nurses - experienced) | 7 (4-13) [1, 48] | 7 (4-13) [1, 48] | 6 (3-19) [1, 43] | 0.98 |
| Group 2 (CCRN nurses - early career) | 2 (1-4) [0, 33] | 2 (1-4) [0, 33] | 2 (1-5) [0, 30] | 0.62 |
| Mean daily non-CCRNs per site | 1 (0-2) [0, 31] | 0 (0-2) [0, 20] | 4 (2-7) [0, 31] | <0.001 |
| Group 3 (non-CCRN redeployed nurses) | 0 (0-2) [0, 31] | 0 (0-2) [0, 20] | 4 (2-7) [0, 31] | <0.001 |
| Group 4 (RUSONs, enrolled nurses & allied health) | 0 (0-0) [0, 4] | 0 (0-0) [0, 4] | 0 (0-0) [0, 2] | <0.001 |
| Critical care staff unavailable due to COVID-19 illness or furlough | 1.6 (0-4) [0, 131.8] | 1.5 (0-4) [0, 131.8] | 2 (0-5) [0, 61] | 0.63 |
| Open available ICU beds | 8 (5.5-15.5) [0, 65.3] | 8 (5.5-15) [0, 63.8] | 11.8 (5-27.2) [4, 65.3] | 0.001 |
| ICU beds open over 'business as usual' | -2 (-4-0.3) [-23, 19.3] | -2 (-4-0) [-23, 17.8] | 1 (-2-2.6) [-18, 19.3] | <0.001 |
| Vacant ICU beds | 1.8 (0.8-3) [0, 12.7] | 2 (1-3) [0.1, 12.7] | 1 (0.2-1.8) [0, 8.3] | <0.001 |
| ICU occupancy | 83% (64-93.5) [0, 200] | 81% (60-92) [0, 200] | 96% (88.6-100) [66.7, 150] | <0.001 |
| Activity Index | 1.1 (0.6-1.5) [0, 2.8] | 1 (0.5-1.5) [0, 2.8] | 1.6 (1.2-1.9) [0.7, 2.6] | <0.001 |
| Days with Activity Index > 2.0, % (number) | 6.5% (178/2725) | 5.1% (125/2445) | 18.9% (53/280) | <0.001 |
| 'ICU equivalent' patients | 6.5 (3.5-14) [0, 63.8] | 6 (3.3-13.3) [0, 62] | 10.8 (5-26) [2.7, 63.8] | <0.001 |
| Patients in ICU needing 1:1 critical care nursing | 5 (2-13.3) [0, 62.3] | 4.5 (1.5-12.8) [0, 60] | 9.8 (5-24.8) [2.5, 62.3] | <0.001 |
| Ventilated patients | 2.5 (0.7-7) [0, 46.7] | 2 (0.5-6.5) [0, 43.8] | 6 (2-16.2) [0, 46.7] | <0.001 |
| COVID-19 patients in each ICU | 1 (0-3) [0, 32.3] | 0.5 (0-2) [0, 31] | 3 (1-9) [0, 32.3] | <0.001 |
| HDU patients (1:2 nursing) in each ICU | 2.3 (0.7-4.3) [0, 14] | 2.5 (1-4.5) [0, 14] | 0 (0-2) [0, 12] | <0.001 |
| COVID-19 patients on the hospital ward | 6 (0-16.8) [0, 173] | 6 (0-16) [0, 173] | 10.1 (0-23) [0, 119.5] | 0.10 |
Data reported are median (interquartile range) [minimum, maximum] daily values per site (unless otherwise stated).
CCRN, critical care registered nurse; COVID-19, coronavirus disease 2019; HDU, high-dependency unit; ICU, intensive care unit; RUSON, Registered undergraduate student of nursing.
Table 1 shows a comparison of days when there was insufficient ICU skill mix compared to days when this was not present. Insufficient ICU skill mix occurred more commonly when there were more ICU beds open, lower numbers of vacant ICU beds, higher occupancy and ICU activity, more patients requiring 1:1 nursing, more ventilated patients, more COVID-19 patients, and lower numbers of high-dependency patients.
Overall, insufficient ICU skill mix occurred on 10.3% (280/2725) days at 66.7% (16/24) of ICUs, most commonly during the peak phase from December to mid-February (Table 2 ). Insufficient ventilated skill mix occurred on 0.7% (19/2725) days overall at 37.5% (9/24) of ICUs and was more common during the peak phase. Reduced nursing ratios occurred on 3% (82/2725) of days at 75% (18/24) of ICUs but were equally common in both phases. Counterfactual analysis suggested that had there been no redeployment of nursing staff to ICU, reduced nursing ratios would have occurred on 15.2% (415/2725) of days at 91.7% (22/24) of ICUs and more commonly during the peak phase.
Table 2.
Outcomes for the whole study period (1st December 2021 to 11th April 2022) and for peak (1st December 2021 to 19th February 2022) and post-peak (20th February to 11th April 2022) phases, showing the number of days on which the outcome was observed and the number of ICUs where this outcome occurred.
| Outcomes | Time Period | Days with this outcome |
ICUs with this outcome |
P value for |
||
|---|---|---|---|---|---|---|
| Proportion | Number | Proportion | Number | difference between phases | ||
| Primary outcome: Insufficient ICU skill-mix | ||||||
| Whole study period (1st December 2021 to 11th April 2022) | 10.3% | 280/2725 | 66.7% | 16/24 | ||
| Peak phase (1st December 2021 to 19th February 2022) | 14.3% | 242/1690 | 62.5% | 15/24 | <0.001 | |
| Post peak phase (20th February 2022 to 11th April 2022) | 3.7% | 38/1035 | 45.8% | 11/24 | ||
| Secondary outcome: Insufficient ventilated skill-mix | ||||||
| Whole study period (1st December 2021 to 11th April 2022) | 0.7% | 19/2725 | 37.5% | 9/24 | ||
| Peak phase (1st December 2021 to 19th February 2022) | 1.1% | 18/1690 | 33.3% | 8/24 | 0.003 | |
| Post peak phase (20th February 2022 to 11th April 2022) | 0.1% | 1/1035 | 4.2% | 1/24 | ||
| Secondary outcome: Reduced ICU nursing ratio | ||||||
| Whole study period (1st December 2021 to 11th April 2022) | 3.0% | 82/2725 | 75% | 18/24 | ||
| Peak phase (1st December 2021 to 19th February 2022) | 3.0% | 51/1690 | 70.8% | 17/24 | 0.86 | |
| Post peak phase (20th February 2022 to 11th April 2022) | 3.0% | 31/1035 | 45.8% | 11/24 | ||
| Counterfactual analysis: Days with reduced ICU nursing ratio if there had been no redeployment of nurses into ICU | ||||||
| Whole study period (1st December 2021 to 11th April 2022) | 15.2% | 415/2725 | 91.7% | 22/24 | ||
| Peak phase (1st December 2021 to 19th February 2022) | 19.9% | 336/1690 | 91.7% | 22/24 | <0.001 | |
| Post peak phase (20th February 2022 to 11th April 2022) | 7.6% | 79/1035 | 70.8% | 17/24 | ||
ICU, intensive care unit.
Insufficient ICU skill mix = Days with more patients needing 1:1 critical care nursing than available critical care registered nurses (CCRNs), % (number).
Insufficient ventilated skill mix = Days with more ventilated patients than available critical care registered nurses (CCRNs), % (number).
Reduced ICU nursing ratio = Days with less than 1:1 overall critical care nursing ratio, % (number).
Table 3 shows that after adjusting for confounders, days with insufficient ICU skill mix were more likely to occur when there were more additional ICU beds open over the ‘business-as-usual’ number, when there was higher occupancy and higher numbers of COVID-19 patients within the ICU. The strongest factor was when additional ICU beds were open over the ‘business as usual’ number. Insufficient ICU skill mix was less likely to occur in rural/regional sites and when there were relatively higher numbers of COVID-19 patients on the general wards outside of ICU.
Table 3.
Mixed effects multivariable logistic regression (with site as a random effect). Factors associated with having more patients needing 1:1 critical care nursing than CCRNs.
| Odds Ratio (95% CI) | P value | |
|---|---|---|
| Hospital type | ||
| Tertiary | Reference group | |
| Metropolitan | 7.40 (0.34 - 160.8) | 0.20 |
| Rural/regional | 0.02 (0.00 - 0.80) | 0.038 |
| Private | 1.12 (0.06 - 22.48) | 0.94 |
| Daily number of critical care staff unavailable due to COVID-19 illness or furlough | 1.02 (1.00 - 1.04) | 0.044 |
| Number of baseline 'business as usual' ICU beds | 0.94 (0.82 - 1.08) | 0.39 |
| Daily ICU beds open over 'business as usual' | 1.28 (1.16 - 1.41) | <0.001 |
| Daily ICU occupancy (%) | 1.08 (1.06 - 1.09) | <0.001 |
| Daily number of ventilated patients | 1.05 (0.97 - 1.13) | 0.23 |
| Daily number of COVID-19 patients in each ICU | 1.13 (1.07 - 1.20) | <0.001 |
| Daily number of COVID-19 patients on the hospital ward | 0.98 (0.97 - 0.99) | 0.002 |
COVID-19, coronavirus disease 2019; ICU, intensive care unit.
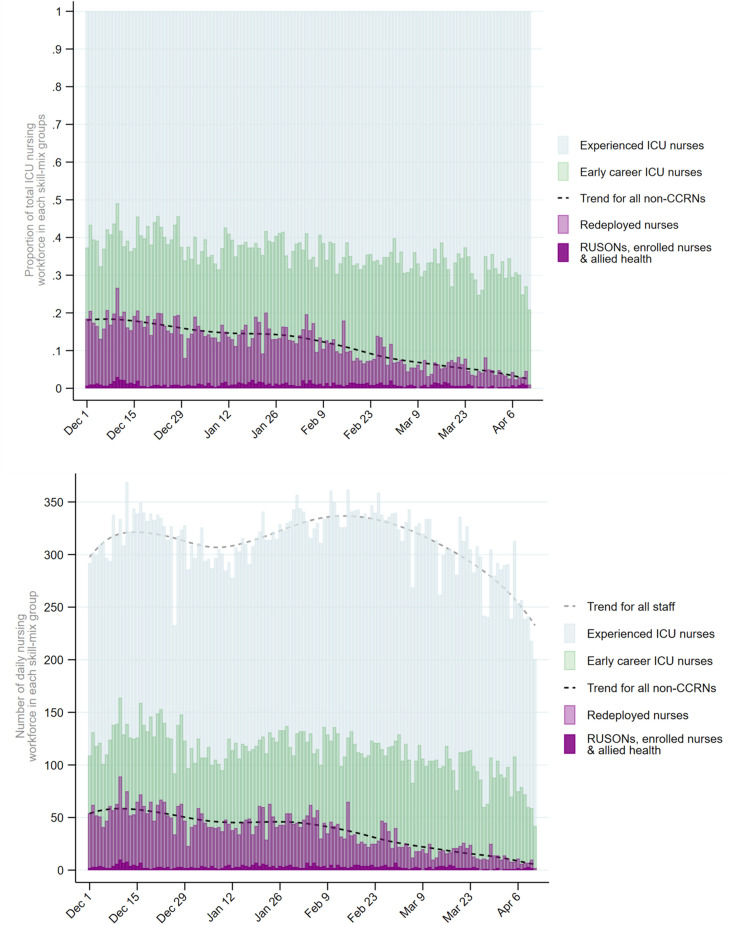
Fig. 2 shows a declining daily number and proportion of non-CCRNs over the study period. Appendix fig. 2 shows a progressive decline in the daily number and proportion of ICUs which had insufficient ICU skill mix. The 10th of December was the day with the highest proportion of the workforce who were non-CCRNs (27%) and the greatest proportion/number of ICUs with insufficient ICU skill mix (40%, 8/20). During the peak phase, there were fewer CCRNs, more non-CCRNs, higher occupancy and activity levels, and higher numbers of ventilated and COVID-19 patients than during the post-peak phase (Appendix table 2). Insufficient ICU skill mix was most commonly observed in tertiary and metropolitan ICUs and was rare in rural/regional, private, and paediatric ICUs (Appendix Table 3).
Fig. 2.
Nursing skill mix distribution at study ICUs between 1st December 2021 and 11th April 2022. Over the study period which began during a period of high demand for ICU beds due to the COVID-19 pandemic, there was a decline in the number and proportion of the ICU nursing workforce who were redeployed nurses from areas outside ICU (light purple) or staff without critical care experience (dark purple). ICU, intensive care unit. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
5. Discussion
This study provides evidence for the first time on the critical care nursing deficit created by pandemic surge models. Insufficient ICU skill mix was present on over 1 in 10 days during the recent pandemic wave December 2021–April 2022. There was a reduced ICU nursing ratio on many occasions, when there were insufficient numbers of nurses to care for patients in ICU according to the nurse to patient ratio standards and demonstrated an insufficient population of skilled CCRNs in Victoria to provide care as the population and acuity of ICU patients increased. The redeployed nurses filled an important gap in meeting patient care needs and minimising reduced ratios, however, ICU nurse staffing gaps remained during the study period.
Adapted models of care delivery in ICUs were common across the world during the COVID-19 pandemic.4 , 16 , 17 In countries that experienced a high COVID-19 disease burden, ICU capacity was rapidly doubled or even quadrupled.18 , 19 Whilst there are large numbers of published studies reporting on increasing ICU capacity in response to COVID-1918 , 19 and non-ICU staff education preparation and deployment,20 there are few on the critical care nursing deficit created by pandemic surge staffing models. A single paper reported the association with critical care staffing and patient mortality during the COVID-19 pandemic, demonstrating that ICU nurse and medical staffing were important determinants of mortality in ICU.21 This is consistent with pre-pandemic data that patient mortality is associated with staff resources and workload in the ICU.22 However, the nuances of what constitutes an “ICU nurse” when referring to ICU staffing and the implications for patient outcomes is poorly understood.23 The clinical relevance for patient outcomes resulting from a deficit of critical care registered nurses in ICU requires further exploration.
Direct ‘one-to-one’ (1:1) nursing care is required for ICU patients who receive invasive therapies such as mechanical ventilation, renal replacement therapy, high-dose vasoactive infusions, or extracorporeal membrane oxygenation.15 This is also required for other patients with complex or high-risk needs such as potential airway compromise or severe delirium. In Australia, the bedside ICU nurse titrates and manages all equipment and medication associated with patient care. Consequently, ICU nursing is a postgraduate specialty qualification, not replaceable by pandemic ‘upskilling’ education programs. ICU care delivered by clinicians without adequate expertise, qualifications, training, or support may result in adverse outcomes.4 , 24 Patients in ICU with COVID-19 require more nursing time than non-COVID-19 patients25 and pandemic staffing models have contributed to missed nursing care.26 Excess mortality for patients with COVID-19 admitted to Australian ICUs during the peak phases of the pandemic in late 2021 has been reported.27
There was wide variation of ICU capacity, with some operating with fewer ICU beds than usual and others well over their usual bed number. This likely reflects both the Victorian Department of Health's policy of ‘streaming’ COVID-19 patients to specified hospitals and also reductions in elective surgery particularly at private hospitals. Insufficient ICU skill mix occurred in over two-thirds of ICUs. Insufficient ICU skill mix was more likely to occur when there were more additional ICU beds open over the ‘business-as-usual’ number, when there was higher occupancy and with higher numbers of COVID-19 patients within the ICU. The increased demand for critical care support meant that patients with COVID-19 had to be admitted to the ICU and cared for with whatever resources were available. Redeployment of nursing staff with or without critical care experience from outside the ICU was required in response to this increased demand. The ability to match provision of critical care trained nursing staff to the increased demand was likely limited by a fixed available number of critical care–trained staff, organisational logistics of redeployment of staff both within and between hospitals and also by staff who were unavailable for work due to either having COVID-19 or being furloughed due to COVID-19 exposure.
Most ICUs experienced an occasion when they did not have enough nurses for recognised nurse to patient ratio standards.11 Notably, if redeployed staff members were not utilised during the study period, there would have been more occasions of reduced nurse to patient ratios. As a response to an extreme health system emergency, redeployed staff were an important strategy to meet patient care needs. Of note, other countries have reported chronic ICU nurse understaffing prior to the pandemic, which the pandemic has exacerbated.4 , 28 , 29 The ICU nurse vacancy rate across Australia prior to the pandemic was over 6%,27 so likewise, the Australian ICU nursing workforce was already depleted. Detailed information about the ICU nursing workforce has not been regularly captured before, and continued collection of such data has the potential to provide valuable information regarding the ICU nursing workforce during regular operations and during other extraordinary events, e.g., disasters.
There is a risk that pandemic-inspired new models of care will remain.30 However, these new models place unreasonable burden on experienced critical care nurses and may contribute to burnout, disengagement,31 and job dissatisfaction (intent to leave).13 Our findings also highlight that quantifying the gap in service provision (critical care nurses to ICU patients) is highly relevant when considering future demands on ICU services and sustainability of ICU nurse staffing.
There are multiple reports of poor staff wellbeing associated with working during the pandemic, including in Australia.32 As the pandemic surge demand peaks and troughs, there is a need for restorative care for staff whenever an opportunity arises. The Safer Care Victoria guidelines incorporate a ‘stand down and recovery’ phase, where healthcare services are expected to provide opportunities for staff to have personal leave and rest and access to psychological supports and counselling.10 Internationally, it is well recognised that nurses working to meet the pandemic surge require organisational support to assist their recovery.33 It is unclear how the negative impacts on nurses from delivering health care in response to the pandemic will be addressed in Victoria.24
6. Strengths and limitations
CHRIS had good capability to allow quick initiation and collection of additional nursing staff data items. Whilst data entry for nursing staff items was voluntary, familiarity with using CHRIS and with the defined surge workforce groupings, provided high-quality, consistent, generalisable and representative data across all care settings. However, although we report (Appendix Table 1 and 3) and also adjusted for different hospital characteristics (Table 3), our study includes data from 24 out of a possible 47 ICUs and thus may not be representative of all ICUs. There may be a bias related to capacity to provide data, for example, busier units may not have contributed data.
The ICU nursing staff data collection began after the pandemic surge associated with the October 2021 Delta wave, so it is possible that the worst of the ICU nursing deficit was not captured. Data gathered about nursing workforce were specific to nurses ‘directly involved in patient care’ only. CHRIS did not capture other nursing roles and resources like educators, managers, equipment nurses, and outreach team members who are usually supernumerary to the nurse to patient ratio numbers and who are a vital support resource each shift. Thus, deficits in ICU nursing staff reported in our study refer only to bedside nursing and not the whole ICU. Numbers of supernumerary staff supporting nursing skill mix or redeployed to replace bedside nursing shortages were unknown. Furthermore, we have no data on overtime worked. Anecdotally, we are aware that double shifts were common in ICUs during the study period to meet direct patient care needs. Additionally, as defined by the Safer Care Victoria guidelines, Group One critical care registered nurses included experienced ICU nurses who do not possess a postgraduate critical care nursing qualification. This limits our ability to interpret our findings as evidence suggests that a minimum proportion of postgraduate-qualified ICU nurses providing direct care is of relevance.11
Furthermore, the timing of data entry on nursing skill mix varied and the mean daily values may not account for variation over the day, e.g., unknown if staffing was worse at night than during the day. This also means some variation in interpretation for ICUs that have hybrid staffing models, e.g., both 12-hr shifts and 8/8/10-hr shift options. Due to the lack of data collection on supernumerary staff, we are unable to comment on how non-CCRNs were supported or supervised as they cared for ICU patients. We are also unable to report on the impact of pandemic staffing models on patient outcomes or nurse outcomes, e.g., burnout.
7. Future research
We have demonstrated that it is feasible to collect high-quality data regarding the ICU nursing workforce. Detailed information about the ICU nursing workforce has not been regularly captured before and has the potential to provide valuable information post-pandemic. Future studies should capture categories of nursing workforce as detailed in the ACCCN Workforce Standards,11 in addition to ICU medical and allied health workforce data.
The COVID pandemic put ICU staffing in the spotlight and exposed the critical dependence on having an available, highly skilled ICU nursing workforce. Routinely collected and access to detailed data on the ICU nursing workforce will be important as health services recover from the previous waves of the pandemic, manage COVID patients ongoing, and deal with a predicted increase in influenza presentations and increase elective/emergency surgery demands. The creation of an ICU staffing dashboard is feasible34 and would enable benchmarking across the sector. There is a pressing need to research the impact of ICU nursing skill mix on patient outcomes and ICU workforce factors on nurse outcomes. Furthermore, research on how to create and maintain a potential flexible redeployment workforce, and the implications for patient care and ICU staffing sustainability, is warranted, if redeployment of non-ICU staff is to become part of the health system response to extreme events.
8. Conclusion
This study has demonstrated that redeployment of workforce was required to ensure adequate patient care and accommodate the increased burden in Victorian ICUs during the COVID-19 pandemic. Despite this, at times, some ICUs had insufficient staff to cope with the number and acuity of patients. There is concern that the pandemic model of care is not sustainable in the long term because of the burden on staff, and further research is needed to examine the impact of ICU nursing models of care on patient outcomes and on nurse outcomes.
Conflict of interest
David Pilcher is the Chair of The ANZICS Centre for Outcome and Resource Evaluation and member of the management committee of the Critical Health Resources Information System (CHRIS).
Jason McClure is the Director of Adult Retrieval Victoria and member of the management committee of the Critical Health Resources Information System (CHRIS).
Melissa Rosenow is a member of the management committee of the Critical Health Resources Information System (CHRIS).
Wendy Pollock was Chair of the ACCCN Workforce Standards Working Party which generated the ACCCN Workforce Standards (2016).
Rose Jaspers is the current ACCCN Victoria President.
Michelle Topple and Jason Watterson are ICU NUMs and contributed data to CHRIS.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Credit authorship contribution statement
MT - Conceptualisation; Investigation; Methodology; Project administration; Validation; Data entry; Writing - original draft; Writing - review & editing.
RJ - Conceptualisation; Investigation; Methodology; Project administration; Validation; Writing - original draft; Writing - review & editing.
JW - Conceptualisation; Investigation; Methodology; Project administration; Validation; Data entry; Writing - original draft; Writing - review & editing.
JMcC - Data curation, Writing - review & editing.
MR - Data curation, Writing - review & editing.
WP - Conceptualisation; Investigation; Methodology; Project administration; Validation; Writing - original draft; Writing - review & editing.
DP - Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Project administration; Validation; Visualisation; Writing - original draft; Writing - review & editing.
Acknowledgements
The authors would like to thank all ICU staff members at the following hospitals who were included in this study: The Alfred Hospital, Angliss Hospital, The Austin Hospital, Ballarat Health Services, Bendigo Hospital, Dandenong Hospital, Epworth Freemasons, Epworth Geelong, Epworth Richmond, Frankston Hospital, University Hospital Geelong, Latrobe Regional Hospital, Maroondah Hospital, Mildura Base Hospital, Monash Children's Hospital, Monash Medical Centre Clayton, Northeast Health Wangaratta, The Northern Hospital, Peninsula Private Hospital, The Royal Children's Hospital, The Royal Melbourne Hospital, St John of God Geelong Hospital, St Vincent's Hospital, Sunshine Hospital.
The authors gratefully acknowledge the contribution and work of the following nurse unit managers without whom this study would not have been possible: Tania Birthisel, Clare Kitch, Michelle Topple, Courtney Rowe, Penny Spencer, Dacielle Johnson, Monique Sammut, Vanessa Sawyer, Stuart Shakespeare, Jason Watterson, Donna Robertson, Bec Wittmer, Carol McKenzie, Sue Hale, Diana Sarraj, Adrienne Pendry, Juliana Sheridan, Narkitaa Van Ekeren, Sarah Edwards, Ashley Doherty, Michelle Spence, Sharnie McAuliffe, Philippe Thomas, Sam Angiolella
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.aucc.2022.12.001.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
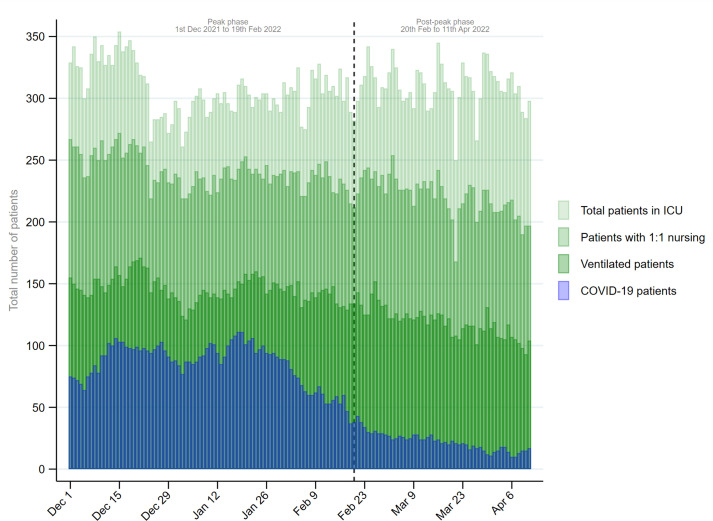
Appendix Fig. 1.
Daily number of total, 1:1 nursed, ventilated and COVID-19 patients in the 24 study hospital ICUs
Explanatory footnote: This shows the number of COVID-19 patients (blue) in study hospital ICUs plotted against the numbers of overall ventilated (dark green), not ventilated but 1:1 nursed (mid-green) and HDU 1:2 nursed patients (light green). As COVID-19 numbers declined in the later phase, the total number of patients requiring 1:1 ICU nursing care also declined and the number of HDU 1:2 patients increased as more ICU beds became available
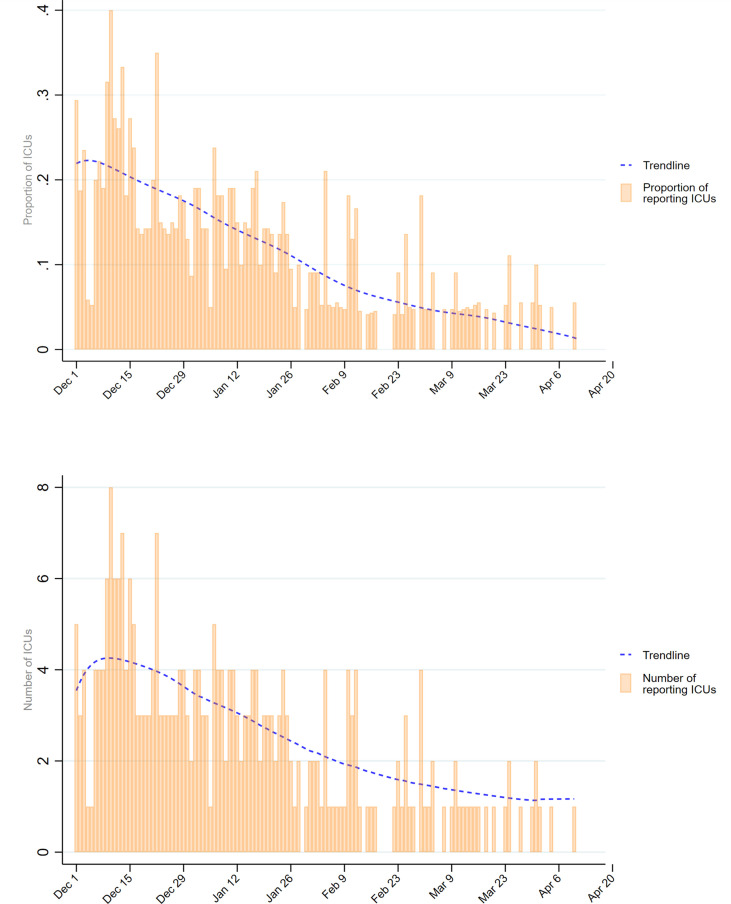
Appendix Fig. 2.
Daily proportion and number of intensive care units (ICUs) which reported more patients requiring 1:1 nursing than the number of critical care nursing staff working in the ICU
Explanatory footnote: The daily proportion and number of ICUs which reported having more patients receiving 1:1 nursing than they had critical care nursing staff declined progressively over the study period
References
- 1.Bhatla A., Ryskina K.L. Healthcare. Elsevier; 2020. Hospital and ICU patient volume per physician at peak of COVID pandemic: state-level estimates. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burau V, Falkenbach M., Neri S., Peckham S., Wallenburg I., Kuhlmann E., et al. Health system resilience and health workforce capacities: comparing health system responses during the COVID-19 pandemic in six European countries. Int J Health Plann Manag. 2022;37:2032–2048. doi: 10.1002/hpm.3446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doyle J, Smith E.M., Gough C.J., Haq A., Willis C., Stevenson T., et al. Mobilising a workforce to combat COVID-19: an account, reflections, and lessons learned. J Intens Care Soc. 2020 doi: 10.1177/1751143720971540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Endacott R., Pearce S., Rae P., Richardson A., Bench S., Pattison N., et al. How COVID-19 has affected staffing models in intensive care: a qualitative study examining alternative staffing models (SEISMIC) J Adv Nurs. 2022;78(4):1075–1088. doi: 10.1111/jan.15081. [DOI] [PubMed] [Google Scholar]
- 5.Goh K.J, Wong J., Tien J.C., Ng S.Y., Duu Wen S., Phua G.C., et al. Preparing your intensive care unit for the COVID-19 pandemic: practical considerations and strategies. Crit Care. 2020;24(1):1–12. doi: 10.1186/s13054-020-02916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta N., Balcom S.A., Gulliver A., Witherspoon R.L. Health workforce surge capacity during the COVID-19 pandemic and other global respiratory disease outbreaks: a systematic review of health system requirements and responses. Int J Health Plann Manag. 2021;36(S1):26–41. [Google Scholar]
- 7.Marshall A.P., Chamberlain D., Cree M., Fetterplace K., Freeman-Sanderson A., Fyfe R., et al. A critical care pandemic staffing framework in Australia. Aust Crit Care. 2021;34(2):123–131. doi: 10.1016/j.aucc.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Litton E., Bucci T., Chavan S., Ho Y.Y., Holley A., Howard G., et al. Surge capacity of intensive care units in case of acute increase in demand caused by COVID-19 in Australia. Med J Aust. 2020;212(10):463–467. doi: 10.5694/mja2.50596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pilcher D., Coatsworth N.R., Rosenow M., McClure J. A national system for monitoring intensive care unit demand and capacity: the Critical Health Resources Information System (CHRIS) Med J Aust. 2021;214(7):297. doi: 10.5694/mja2.50988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department of Health Victoria, Coronavirus (COVID-19) Intensive Care Unit surge workforce models of care delivery.
- 11.Chamberlain D., Pollock W., Fulbrook P. ACCCN workforce standards for intensive care nursing: systematic and evidence review, development, and appraisal. Aust Crit Care. 2018;31(5):292–302. doi: 10.1016/j.aucc.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 12.Rae P.J.L., Pearce S., Greaves P.J., Dall’Ora C., Griffiths P., Endacott R. Outcomes sensitive to critical care nurse staffing levels: a systematic review. Intensive Crit Care Nurs. 2021;67 doi: 10.1016/j.iccn.2021.103110. [DOI] [PubMed] [Google Scholar]
- 13.Bae S.H. Intensive care nurse staffing and nurse outcomes: a systematic review. Nurs Crit Care. 2021;26(6):457–466. doi: 10.1111/nicc.12588. [DOI] [PubMed] [Google Scholar]
- 14.Government of Victoria . 2022. Victorian COVID-19 data.https://www.coronavirus.vic.gov.au/victorian-coronavirus-covid-19-data 18 October 2022]; Available from: [Google Scholar]
- 15.Australian College of critical care nurses workforce standards for intensive care nursing. ACCCN Ltd; Melbourne: 2016. [Google Scholar]
- 16.Al Mutair A., Amr A., Ambani Z., AI Salman K., Schwebius D. Nursing surge capacity strategies for management of critically ill adults with COVID-19. Nursing Reports. 2020;10(1):23–32. doi: 10.3390/nursrep10010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kerlin M.P., Costa D.K., Davis B.S., Admon A.J., Vranas K.C., Kahn J.M., et al. Actions taken by US hospitals to prepare for increased demand for intensive care during the first wave of COVID-19: a national survey. Chest. 2021;160(2):519–528. doi: 10.1016/j.chest.2021.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carenzo L., Costantini E., Greco M., Barra F.L., Rendiniello M., Bui A., et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020;75(7):928–934. doi: 10.1111/anae.15072. [DOI] [PubMed] [Google Scholar]
- 19.Chew M.S., Kattainen S., Haase N., Buanes E.A., Kristinsdottir L.B., Hofso K., et al. A descriptive study of the surge response and outcomes of ICU patients with COVID-19 during first wave in Nordic countries. Acta Anaesthesiol Scand. 2022;66(1):56–64. doi: 10.1111/aas.13983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Camilleri M., Zhang X., Corner E. Covid-19 ICU remote-learning course (CIRLC): rapid ICU remote training for frontline health professionals during the COVID-19 pandemic in the UK. J Intense Care Soc. 2020 doi: 10.1177/1751143720972630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xi J, Zeng L., Li S., Ai Y., He X., Kang Y., et al. COVID-19 mortality in ICUs associated with critical care staffing. vol. 9. Burns & Trauma; 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neuraz A, Claude G., Payet C., Polazzie S., Aubrun F., Dailler F., et al. Patient mortality is associated with staff resources and workload in the ICU: a multicenter observational study. Crit Care Med. 2015;43(8):1587–1594. doi: 10.1097/CCM.0000000000001015. [DOI] [PubMed] [Google Scholar]
- 23.Pattison N. Wiley Online Library; 2021. An ever-thorny issue: defining key elements of critical care& nursing and its relation to staffing; pp. 421–424. [DOI] [PubMed] [Google Scholar]
- 24.Riddell K, Bignell L., Bourne D., Boyd L., Crowe S., Cucanic S., et al. The context, contribution and consequences of addressing the COVID-19 pandemic: a qualitative exploration of executive nurses’ perspectives. J Adv Nurs. 2022;78:2214–2231. doi: 10.1111/jan.15186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lucchini A, Giani M., Elli S., Villa S., Rona R., Foti G. Nursing Activities Score is increased in COVID-19 patients. Intensive Crit Care Nurs. 2020;59 doi: 10.1016/j.iccn.2020.102876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bergman L, Falk A.C., Wolf A., Larsson I.M. Registered nurses’ experiences of working in the intensive care unit during the COVID-19 pandemic. Nurs Crit Care. 2021;26(6):467–475. doi: 10.1111/nicc.12649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Australian and New Zealand intensive care society Centre for outcome and resource evaluation, report on COVID-19 admissions to intensive care in Australia 01 january 2021 - 31 december 2021. 2022, The Australian and New Zealand Intensive Care Society (ANZICS).
- 28.Endacott R, Pattison N., Dall’Ora C., Griffiths P., Richardson A., Pearce S., et al. The organisation of nurse staffing in intensive care units: a qualitative study. J Nurs Manag. 2022;30:1283–1294. doi: 10.1111/jonm.13611. [DOI] [PubMed] [Google Scholar]
- 29.Lasater K.B, Aiken L.H., Sloane D.M., French R., Martin B., Reneau K., et al. Chronic hospital nurse understaffing meets COVID-19: an observational study. BMJ Qual Saf. 2021;30(8):639–647. doi: 10.1136/bmjqs-2020-011512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arabi Y.M, Azoulay E., AI-Dorzi H.M., Phua J., Salluh J., Binnie A., et al. How the COVID-19 pandemic will change the future of critical care. Intensive Care Med. 2021;47(3):282–291. doi: 10.1007/s00134-021-06352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baez-Leon C., Palacios-Cena D., Fernandez-de-las-Penas C., Verlade-Garcia J.F., Rodriguez-Martinez A., Arribas-Cobo P. A qualitative study on a novel peer collaboration care programme during the first COVID-19 outbreak: a SWOT analysis. Nursing Open. 2022;9(1):765–774. doi: 10.1002/nop2.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hammond N.E, Crowe L., Abbenbroek B., Elliot R., Tian D.H., Donaldson L.H., et al. Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers’ depression, anxiety, and stress levels. Aust Crit Care. 2021;34(2):146–154. doi: 10.1016/j.aucc.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clark S.E., Chisnall G., Vindrola-Padros C. A systematic review of de-escalation strategies for redeployed staff and repurposed facilities in COVID-19 intensive care units (ICUs) during the pandemic. EClinicalMedicine. 2022;44 doi: 10.1016/j.eclinm.2022.101286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davidson B, Portillo K.M.F., Wac M., McWilliams C., Bourdeaux C., Craddock I. Requirements for a bespoke intensive care unit dashboard in response to the COVID-19 pandemic: semistructured interview study. JMIR Human Factors. 2022;9(2) doi: 10.2196/30523. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.