Abstract
Background:
Social determinants of health (SDOH) are associated with cardiovascular disease, but little is known about mechanisms underlying those relationships. We hypothesized that SDOH would be associated with uncontrolled hypertension (HTN) in adults with Medicaid.
Methods:
This was a retrospective analysis of adults in a Medicaid accountable care organization who had HTN diagnoses, received regular care at community health centers, and enrolled in a cohort study between December 2019 and December 2020. Baseline surveys collected demographics and SDOH, including food insecurity, unstable housing, cost-related medication underuse, and financial stress. Blood pressure (BP) measurements over 12 months after survey completion were obtained from the electronic health record. Participants were categorized as: uncontrolled HTN (mean systolic BP ≥ 140 mm Hg and/or mean diastolic BP ≥ 90 mm Hg), controlled HTN, or unknown HTN control (no BP documented). We examined the association of individual and cumulative (count, 0-4) SDOH with uncontrolled HTN and unknown HTN control using multivariable logistic regression adjusting for demographics, smoking, diabetes, and HTN medication.
Results:
Participants (n = 245) were mean (SD) age 51.3 (8.6) years, 66.1% female, 43.7% Hispanic, 34.3% White, and 18.0% Black. Overall, 58.0% had food insecurity, 38.0% had unstable housing, 29.4% had financial stress, and 20.0% reported cost-related medication underuse. BP was documented for 180 participants; 44 (24.4%) had uncontrolled HTN. In multivariable models, neither individual nor cumulative SDOH were associated with uncontrolled HTN or unknown HTN control.
Conclusions:
In a Medicaid-insured population receiving care at community health centers, adverse SDOH were prevalent but were not associated with HTN control.
Keywords: hypertension control, Medicaid, social determinants of health, adults
Introduction
Poorly controlled blood pressure (BP) is the leading modifiable risk factor for cardiovascular events like stroke and myocardial infarction.1 In 2018, about 60% of adults with hypertension (HTN) had uncontrolled BP.1 Some studies have shown that low income and adverse social determinants of health (SDOH), such as food insecurity and unstable housing, are associated with HTN2,3 and cardiovascular disease events. A study of more than 25 000 adults over the age of 45 demonstrated that the presence of each additional adverse SDOH was associated with higher risk of stroke.4 A United Kingdom-based study with over 40 000 adult participants found higher incidence and prevalence of 12 cardiovascular diseases in individuals experiencing homelessness.5 In the Jackson Heart Study, financial stress was associated with incident coronary heart disease in over 2000 mostly Black, non-Hispanic adults after accounting for socioeconomic status.6
One potential pathway between adverse SDOH and cardiovascular disease may be poorly controlled BP.4 Adverse SDOH are associated with psychological stress, poor dietary quality, and lack of time and resources for self-care.7 To date, there have been few studies examining the relationship between adverse SDOH and control of BP among people with a diagnosis of HTN. Data from the National Health and Nutrition Examination Survey (NHANES) from 2011 to 2018 showed that individuals without consistent access to a health care provider had higher rates of uncontrolled HTN,2 but a recent meta-analysis found no difference in the rates of antihypertensive medication underuse in participants with uncontrolled versus controlled HTN.8
Addressing SDOH could be especially important for lower-income populations with HTN, such as those covered by Medicaid. A number of Medicaid programs are implementing accountable care organization (ACO) models that include substantial focus on addressing SDOH,9 so it could be particularly instructive to study the relationship between SDOH and HTN control among those with Medicaid. In previous studies, individuals with health insurance had lower cost-related medication underuse and lower uncontrolled HTN than those without health insurance.2,10 However, the impact of SDOH on HTN control in lower-income individuals who are insured and have access to care is unknown.
The objective of this study was to examine whether food insecurity, unstable housing, cost-related medication underuse, and financial stress were associated with HTN control in adults participating in a Medicaid ACO. We hypothesized that in this population of low-income adults with public health insurance, adverse SDOH would be associated with worse HTN control over 12 months.
Methods
This was a retrospective analysis of data from the LiveWell study, an observational cohort study evaluating the implementation and health impact of a new state Medicaid program that provides funding to ACOs to pay for and connect participants with food and housing resources. The LiveWell study was approved by the Mass General Brigham Institutional Review Board in 2019. A total of 1056 participants provided informed consent and were enrolled from 5 community health centers near Boston, Massachusetts. To be eligible for the LiveWell study, participants had to be between 21 and 62 years old, have had at least 1 visit at their primary care practice in the previous 2 years, speak English or Spanish, and be participating in the Mass General Brigham Medicaid ACO or a commercial ACO insurance plan. The present study focused on the 846 participants who were in the Medicaid ACO, of whom 245 (28.9%) had a diagnosis of HTN documented in the electronic health record by an ICD-10 code or in the problem list during the 2 years before enrollment. The corresponding author had full access to all data in the study.
Survey Measures
Baseline survey data were collected in person, over the phone, and by email between December 2019 and December 2020 and included questions about demographics and SDOH. Participants self-reported their age, sex, race, ethnicity, marital status, children at home, smoking status, and participation in food assistance programs. Self-reported educational attainment was dichotomized as high school or less versus more than high school.
Food security was measured with the 10-item United States Department of Agriculture’s Adult Food Security Survey Module 11; scores range from 0 to 10. We dichotomized responses so that participants with scores 0 to 2 (ie, high or marginal food security) were considered food secure, and those with scores ≥3 were food insecure.
Housing stability was measured with a 3-item screening scale that included not renting or owning a house or apartment, moving 2 or more times in the past 12 months, and worrying about having housing in next 2 months. Participants were considered to have housing instability if they answered yes to at least 1 item on the scale.
Cost-related medication underuse was measured with 2 items that have been used in prior research10; the items assessed whether participants had delayed filling or reduced their use of a prescription medication because of financial concerns. Participants with an affirmative response to either item were categorized as positive for cost-related medication underuse.
Financial stress was measured with a subscale from the Weekly Stress Inventory that was previously shown to be associated with incident cardiovascular disease.6 Participants were asked whether they had experienced any of 5 financial problems over the previous week. For any item endorsed, participants were prompted to rate its stressfulness on a 7-point Likert-type scale on which higher ratings reflected higher stressfulness. A mean score greater than 4 indicated moderate to severe financial stress.
Measures from the Electronic Health Record (EHR)
Mean systolic and diastolic blood pressure (BP) were calculated for each participant who had at least 1 BP recorded in an outpatient setting (either a primary care or a specialty clinic) in the 12 months after enrollment. Blood pressure measures from hospitalizations or emergency department visits were excluded. To be conservative in our estimate of uncontrolled HTN, only the lowest recorded BP was included if a participant had more than 1 BP recorded on a single day. Uncontrolled HTN was defined as mean systolic BP ≥ 140 mm Hg or mean diastolic BP ≥ 90 mm Hg. Participants with no BP recorded in the 12-month window were considered to have unknown HTN control.
Participants’ BMI during the study period was defined as the BMI recorded closest to the date of enrollment within 3 months before or 3 months after the day of enrollment. A participant was considered to have a diagnosis of type 2 diabetes if it was documented in the EHR by an ICD-10 code or in the problem list during the 2 years prior to the date of enrollment. Hypertension medications were obtained from the EHR, and participants were dichotomized as having any versus no HTN medication prescription on their records in the year after enrollment.
Statistical Analysis
Differences in characteristics of participants with controlled, uncontrolled, and unknown HTN control were examined using t-tests or chi-squared tests. We analyzed associations of individual SDOH (food insecurity, unstable housing, cost-related medication underuse, and financial stress) with HTN control in logistic regression models that assessed the odds of uncontrolled vs. controlled HTN and of unknown control vs. controlled HTN. Both models adjusted for age, gender, race/ethnicity, diabetes diagnosis, smoking status, time of study enrollment (by quarter of year), and use of any HTN medication. In a secondary analysis, we examined the association of total measured number of adverse SDOH (0, 1, 2, or 3+) with HTN control. All outcomes were considered statistically significant at P ≤ .05. Analyses were performed using STATA (version 16, 2019, StataCorp, College Station, TX, USA).
Results
Among 245 participants with a diagnosis of HTN, 180 (73.5%) had at least 1 BP measurement documented in the EHR in the 12 months following enrollment; 66.5% of BP measurements were documented at primary care visits and 33.5% at specialty visits. Only 4 participants had multiple BP readings in 1 day. Of the 180 with a BP measurement, 44 (24.4%) had uncontrolled HTN. Overall, 109 (44.5%) participants had either uncontrolled HTN or unknown HTN control. Table 1 shows participant characteristics by category of HTN control.The mean (SD) age of all participants was 51.3 (8.6) years; 66.1% were female; 43.7% were Hispanic, non-Black; 34.3% were White, non-Hispanic; and 18.0% were Black. The education level of most participants (57.1%) was high school or less.
Table 1.
Participant Characteristics for Those with Controlled Hypertension, Uncontrolled Hypertension, and Unknown Hypertension Control.
| Controlled HTN (N = 136) | Uncontrolled HTN (N = 44) | Unknown HTN control (N = 65) | |
|---|---|---|---|
| Age, mean [SD] | 51.7 [8.6] | 50.8 [8.4] | 50.7 [8.7] |
| Female sex, N (%) | 96 (70.6) | 32 (72.7) | 34 (52.3)** |
| Race/ethnicity, N (%) | |||
| Hispanic | 61 (44.9) | 22 (50.0) | 24 (36.9) |
| White, non-Hispanic | 44 (32.4) | 13 (29.6) | 27 (41.5) |
| Black | 25 (18.4) | 7 (15.9) | 12 (18.5) |
| Other races, non-Hispanic† | 6 (4.4) | 2 (4.6) | 2 (3.1) |
| Married/living with significant other, N (%) | 49 (36.0) | 11 (25.0) | 23 (35.4) |
| Children <18 years old in household, N (%) | 58 (42.7) | 17 (38.6) | 20 (30.8) |
| Employed full/part-time, N (%) | 40 (29.4) | 12 (27.3) | 15 (23.1) |
| Education, N (%) | |||
| High school degree or less | 75 (55.2) | 28 (63.6) | 37 (56.9) |
| Some education past high school | 60 (44.1) | 16 (36.4) | 28 (43.1) |
| Household income <$30 000, N (%) | 101 (74.3) | 38 (86.4) | 51 (78.5) |
| Language preference: Spanish | 50 (36.8) | 11 (25.0) | 11 (16.9)** |
| Enrolled in SNAP, N (%) | 95 (69.9) | 30 (68.2) | 44 (67.7) |
| Current smoking, N (%) | 33 (24.3) | 13 (29.6) | 23 (35.4) |
| BMI, kg/m2, mean [SD] | 32.3 [7.3] | 33.7 [7.1] | 34.3 [8.7] |
| Diabetes, N (%) | 59 (43.4) | 16 (36.4) | 16 (24.6)* |
| Any HTN medications before enrollment | 116 (85.3) | 39 (88.6) | 44 (67.7)** |
| Days with BP measurement over 12 months, mean [SD]# | 3.0 [2.6] | 2.5 [2.4] | 0 |
Abbreviations: BMI, body mass index; BP, blood pressure; HTN, hypertension; SNAP, supplemental nutrition assistance program.
P < .05 for comparison with controlled HTN group.
P < .01 for comparison with controlled HTN group. All other comparisons between uncontrolled HTN group or unknown HTN group and the controlled HTN group were P > .05.
Other races, non-Hispanic includes Asian/Native American and Mixed/Alaskan Native.
By definition, participants in the unknown HTN control group had 0 day with a BP measurement in the year after enrollment.
4 participants had 2 or more BP readings in 1 day; only the lowest BP was included.
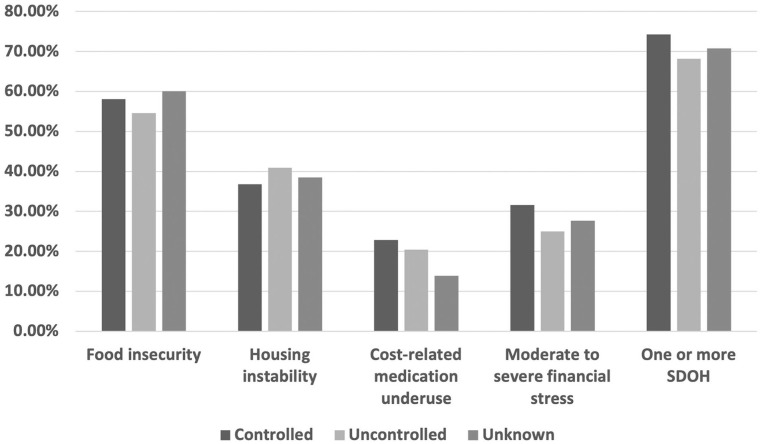
Figure 1 shows the prevalence of having each adverse SDOH and having any adverse SDOH by HTN group. Overall, 72.2% of participants experienced at least 1 adverse SDOH; 58.0% of participants had food insecurity, 38.0% had housing instability, 29.4% had moderate-severe financial stress, and 20.0% reported cost-related medication underuse. The mean (SD) number of adverse SDOH for each participant was 1.5 (1.2), and the mean (SD) number of SDOH was similar for each category of HTN control: 1.5 (1.2) for controlled HTN, 1.4 (1.3) for uncontrolled HTN, and 1.4 (1.1) for unknown HTN control.
Figure 1.
Prevalence of select social determinants of health among those with controlled and uncontrolled hypertension and unknown hypertension control. Abbreviations: SDOH, social determinants of health. All differences in rates of SDOH among hypertension groups were not statistically significant.
In multivariable analyses, there were no differences in the odds of having uncontrolled HTN over 12 months for participants reporting food insecurity, unstable housing, cost-related medication underuse, or financial stress compared to those who did not report those SDOH (Table 2). Participants who reported cost-related medication underuse had lower odds of having unknown HTN control over 12 months.
Table 2.
Social Determinants of Health and Odds of Uncontrolled Hypertension Over 12 months.
| SDOH | Uncontrolled vs controlled HTN OR (95% CI)* | Unknown control vs controlled HTN OR (95% CI)* |
|---|---|---|
| Food insecurity | 0.92 (0.41, 3.60) | 1.82 (0.82, 4.00) |
| Housing insecurity | 1.45 (0.61, 3.46) | 0.87 (0.39, 1.91) |
| Cost-related medication underuse | 1.28 (0.47, 3.52) | 0.33 (0.12, 0.93)** |
| Moderate/severe financial stress | 0.47 (0.18, 1.27) | 0.82 (0.35, 1.88) |
Abbreviations: HTN, hypertension; SDOH, social determinants of health.
Odds ratio adjusted for age, gender, race/ethnicity, diabetes, smoking, education, quarter of enrollment, and any hypertension medication.
P = .04.
We conducted secondary analyses to assess whether participants’ total number of SDOH was associated with HTN control (Table 3). There were no significant associations between the number of SDOH reported by a participant and having uncontrolled HTN or unknown HTN.
Table 3.
Adjusted Odds Ratios for Uncontrolled and Unknown Versus Controlled Hypertension as a Function of Total Number of Adverse Social Determinants of Health.
| Number of SDOH* | Uncontrolled vs controlled HTN OR (95% CI)** | Unknown control vs controlled HTN OR (95% CI)** |
|---|---|---|
| 0 | Reference | Reference |
| 1 | 0.62 (0.24, 1.60) | 0.75 (0.30, 1.87) |
| 2 | 0.79 (0.29, 2.19) | 1.57 (0.64, 3.86) |
| 3 or more | 0.52 (0.18, 1.54) | 0.45 (0.15, 1.33) |
Abbreviations: HTN, hypertension; SDOH, social determinants of health.
The individual SDOH were food insecurity, housing instability, cost-related medication underuse, and moderate to severe financial stress.
Odds ratio adjusted for age, gender, race/ethnicity, diabetes, smoking, quarter of enrollment, and any (versus no) HTN medication.
Discussion
In this sample of adults with HTN participating in a Medicaid ACO, adverse SDOH were prevalent, with almost three quarters of study participants experiencing at least 1. Contrary to our hypothesis, we found no evidence that participants reporting food insecurity, unstable housing, financial stress, or cost-related medication underuse were more likely to have uncontrolled HTN than participants who did not report these SDOH.
Unlike previous studies that included participants with a range of income levels and health insurance coverage,6,12 our study only included adults with low income who had Medicaid health insurance and were connected to a primary care clinic. More than 75% of our study participants reported annual household incomes below $30 000. There is some evidence that US trends in HTN control might differ by income level. From 1999 to 2014, the mean systolic blood pressure of both high- and middle-income American adults dropped by more than 3 mm Hg, while no significant difference was observed among low-income adults.13
Prior research has not demonstrated a clear association between SDOH and HTN control; a recent systematic review found that food insecurity was linked to higher rates of self-reported HTN diagnosis but not to worse HTN control.12 Despite having low income, 55.5% of all participants in our study and 75.6% of participants with a documented BP were categorized as having controlled HTN. These estimates are higher than national estimates from 2017 in which only 43.7% of US adults with HTN had controlled HTN.1 Other research has shown that people with health insurance have lower rates of uncontrolled blood pressure.2 All participants in our study belonged to the Medicaid ACO and were connected to primary care providers; those factors might have contributed to better HTN control, despite experiencing many adverse SDOH. However, it is possible that among individuals who are uninsured or disconnected from health care, adverse SDOH may negatively affect HTN control.
In this study, over a quarter of the study sample had no outpatient health care visit with a documented BP during the 12-month follow-up period and were considered to have unknown HTN control. The most recent American College of Cardiology/American Heart Association guidelines for HTN management recommend that patients with HTN have their BP checked professionally every 3 to 6 months.14 Although it is possible that some of the participants with unknown HTN control either received care outside the ACO or did not come in for a visit because their BP was controlled and they were monitoring it at home, it is likely that many in this group delayed necessary health care due to the COVID-19 pandemic or other factors. While rates of adverse SDOH did not differ much among this study’s 3 HTN groups, the unknown HTN control group was less likely to have any antihypertensive medications recorded in the EHR, which might have contributed to this group having lower cost-related medication underuse.
This study has limitations. There was a relatively small sample size with SDOH measured at one time point, and this may have affected the power to detect statistical differences. The study was a secondary analysis of baseline data collected for the larger LiveWell study. However, the rates of adverse SDOH were not meaningfully different between the groups with uncontrolled and controlled HTN (Figure 1). Participants in this study were enrolled from December 2019 to December 2020, which included the early months of the COVID-19 pandemic when people may have had changes in their health behaviors, health care utilization, and social needs, such as food insecurity.15,16 It is possible that the prevalence of SDOH among study participants may have been higher at the time of enrollment than before the pandemic, and it is likely that participants had fewer BP measurements than usual due to reduced in-person health care visits because of pandemic-related restrictions. Although we assessed 4 important adverse SDOH in this study, other SDOH that were not included, such as transportation and community-level factors, could have been associated with HTN control. We evaluated cost-related medication underuse, but we did not measure other factors associated with medication nonadherence, such as side effects and risk perception, that may have influenced HTN control.17 All participants in this study had Medicaid insurance, were younger than 64 years old, and resided in eastern Massachusetts; results may not generalize to non-Medicaid and older populations or to individuals living in other states.
In conclusion, adverse SDOH were prevalent in this sample of community health center patients with Medicaid insurance and a diagnosis of HTN, and approximately 1 in 4 participants did not have a BP measured within the health care system over the course of a year. Neither individual nor cumulative SDOH were associated with uncontrolled HTN. Future research should continue to explore mechanisms of how SDOH may contribute to cardiovascular disease, including how SDOH influence health behaviors, psychological stress, and other cardiometabolic risk factors.
Acknowledgments
The authors would like to thank Peyton Williams and Oldy Bejarano who were instrumental in collecting data for this study.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is funded by the grant NIDDK R01 DK124145.
ORCID iD: Anne N. Thorndike  https://orcid.org/0000-0003-1096-9221
https://orcid.org/0000-0003-1096-9221
References
- 1. Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324(12):1190-1200. doi: 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Commodore-Mensah Y, Turkson-Ocran RA, Foti K, Cooper LA, Himmelfarb CD. Associations between social determinants and hypertension, stage 2 hypertension, and controlled blood pressure among men and women in the United States. Am J Hypertens. 2021;34(7):707-717. doi: 10.1093/ajh/hpab011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Te Vazquez J, Feng SN, Orr CJ, Berkowitz SA. Food insecurity and cardiometabolic conditions: a review of recent research. Curr Nutr Rep. 2021;10(4):243-254. doi: 10.1007/s13668-021-00364-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reshetnyak E, Ntamatungiro M, Pinheiro LC, et al. Impact of multiple social determinants of health on incident stroke. Stroke. 2020;51(8):2445-2453. doi: 10.1161/STROKEAHA.120.028530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nanjo A, Evans H, Direk K, Hayward AC, Story A, Banerjee A. Prevalence, incidence, and outcomes across cardiovascular diseases in homeless individuals using national linked electronic health records. Eur Heart J. 2020;41(41):4011-4020. doi: 10.1093/eurheartj/ehaa795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moran KE, Ommerborn MJ, Blackshear CT, Sims M, Clark CR. Financial stress and risk of coronary heart disease in the Jackson Heart Study. Am J Prev Med. 2019;56(2):224-231. doi: 10.1016/j.amepre.2018.09.022 [DOI] [PubMed] [Google Scholar]
- 7. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. New Engl J Med. 2010;363(1):6-9. doi: 10.1056/NEJMp1000072 [DOI] [PubMed] [Google Scholar]
- 8. Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Medicine. 2017;96(4):e5641. doi: 10.1097/MD.0000000000005641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rutledge RI, Romaire MA, Hersey CL, Parish WJ, Kissam SM, Lloyd JT. Medicaid accountable care organizations in four states: implementation and early impacts. Milbank Q. 2019;97(2):583-619. doi: 10.1111/1468-0009.12386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127(4):303-310.e3. doi: 10.1016/j.amjmed.2014.01.002 [DOI] [PubMed] [Google Scholar]
- 11. United States Department of Agriculture. U.S. adult food security survey module. Survey tools. September 2012. Updated April 22, 2022. Accessed August 17, 2022. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/survey-tools/#adult
- 12. Beltrán S, Pharel M, Montgomery CT, López-Hinojosa IJ, Arenas DJ, DeLisser HM. Food insecurity and hypertension: a systematic review and meta-analysis. PLoS One. 2020;15(11):e0241628. doi: 10.1371/journal.pone.0241628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Odutayo A, Gill P, Shepherd S, et al. Income disparities in absolute cardiovascular risk and cardiovascular risk factors in the United States, 1999-2014. JAMA Cardiol. 2017;2(7):782-790. doi: 10.1001/jamacardio.2017.1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30(3):160-164. doi: 10.1016/j.tcm.2019.05.003 [DOI] [PubMed] [Google Scholar]
- 15. Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021;174(1):129-131. doi: 10.7326/M20-3026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wolfson JA, Leung CW. Food insecurity during COVID-19: an acute crisis with long-term health implications. Am J Public Health. 2020;110(12):1763-1765. doi: 10.2105/AJPH.2020.305953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028-3035. doi: 10.1161/CIRCULATIONAHA.108.768986 [DOI] [PubMed] [Google Scholar]