Abstract
Background/aim:
Given the current severe acute respiratory syndrome coronavirus 2 pandemic, coughing at the time of extubation is at risk of creating aerosolisation. This may place health care workers at risk of nosocomial infection during the perioperative period. This study aims to summarise the current pharmacologic methods to minimise cough at the time of extubation, and to determine whether some strategies could be more beneficial than others.
Methods:
This is a summary of systematic reviews. A comprehensive search through MEDLINE was performed. Thirty-three publications were screened for eligibility. Only the manuscripts discussing pharmacologic methods to minimise coughing on extubation were included in this review.
Findings:
Many pharmacological agents have been proposed to decrease the incidence of cough at the time of extubation. Of these, intravenous administration of dexmedetomidine (relative risk 0.4; 95% CI: 0.4–0.5) or remifentanil (RR 0.4; 95% CI: 0.4–0.5) seems to have the largest effect to reduce cough on extubation.
Conclusion:
The available data in the current literature is sparse. Yet, dexmedetomidine and remifentanil seem to be the most efficient agents to decrease the incidence of emergence coughing.
Keywords: Aerosol-generating procedures, Airway management, COVID-19, Tracheal intubation, Anaesthesia
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in December 2019 and has claimed over six million lives (John Hopkins University 2020, Yang et al 2020a). Its transmission occurs mostly through respiratory droplets (>5µm) and aerosol (<5µm particles) that can remain suspended in the air for prolonged periods (Meyerowitz et al 2021). Clinicians who perform airway procedures, such as tracheal intubation and extubation, are particularly at risk of contracting severe respiratory viral infections such as SARS-CoV-2, as these procedures are considered aerosol-generating procedures (odds ratio [OR] 6.6; 95% confidence interval [CI]: 2.3–18.9) (Jackson et al 2020, Tran et al 2012, Zayas et al 2012). More examples of aerosol-generating airway procedures include airway suctioning, tracheostomy and cardiopulmonary resuscitation (Schimmel & Berkowitz 2022).
A recent publication suggests that 1 in 10 health care workers involved in airway management of suspected or confirmed COVID-19 patients subsequently reported infection (El-Boghdadly et al 2020). Coughing is commonly seen during extubation of a surgical patient; in fact, coughing occurs up to 15 times more common during extubation than during intubation and may contribute to additional aerosolisation (Asai et al 1998, Brown et al 2021). Therefore, minimising coughing during extubation is essential to mitigate the risk of nosocomial transmission (Wilson et al 2020). Clinicians have explored various innovative barrier methods to minimise the dispersion of aerosols during emergence from general anaesthesia. Some examples of these methods include the use of plastic sheets (Matava et al 2020) or a protection box (Yang et al 2020c). Although a barrier method may appear to be effective, they add an additional level of complexity to airway management and may delay the time of intubation (Begley et al 2020). Compared with barrier methods, a pharmacologic strategy offers the advantage of minimising disruption from a routine anaesthetic practice. We aim to summarise the current perioperative pharmacologic methods to minimise cough at the time of extubation, which is particularly beneficial given the current pandemic. We also aim to determine which strategy would be the most beneficial.
Method
For this summary of systematic reviews, we performed a comprehensive search through MEDLINE using the following search strategy: (intubation[tiab] OR extubation[tiab]) AND (cough*[tiab]) AND (systematic review[tiab]) from inception to 1 November 2021. A total of 33 publications resulted from this search strategy and were screened for eligibility. Publications were considered eligible for review if they were systematic reviews, including adult patients undergoing surgery under general anaesthesia with tracheal intubation. Only the manuscripts discussing pharmacologic methods to minimise coughing on extubation were included in this review. Exclusion criteria also include (1) study limited to the paediatric population, (2) study not performed in a perioperative setting, (3) no discussion of tracheal intubation and (4) coughing on intubation only. There were no language limits.
Results
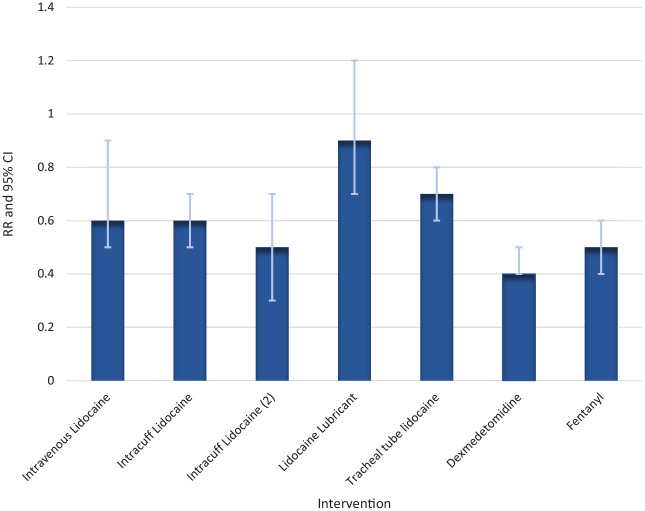
Thirty-three articles were eligible based on the initial search. After title and abstract screening, five full-text articles were reviewed. One article was excluded because the outcome of interest was coughing on intubation only (Clivio et al 2019). Four systematic reviews were included for analysis (Figure 1). Many pharmacological interventions have been proposed to decrease the incidence of cough at the time of extubation. These include the use of lidocaine (either intravenous (IV), intracuff or topical), IV opioids and dexmedetomidine (Table 1). In a population of 1516 patients, the use of IV lidocaine demonstrated a decrease in the incidence of cough at extubation (relative risk (RR) 0.6; 95% CI: 0.5–0.9) (Yang et al 2020b). Similarly, the use of intracuff lidocaine (n = 963) (RR 0.6; 95% CI: 0.5–0.7) and tracheal tube lidocaine (n = 495) (RR 0.7; 95% CI: 0.6–0.8) also had similar effects to reduce cough (Tung et al 2020). In another systematic review of 868 patients, the use of intracuff lidocaine resulted in a significant decrease in the incidence of cough at the time of extubation (RR 0.5; 95% CI 0.3–0.7) (Peng et al 2020). In a large systematic review of 2146 patients, the use of lidocaine lubricants did not result in a statistical difference in the incidence of cough at the time of extubation (RR 0.9; 95% CI: 0.7–1.2) (Liao et al 2019). The use of dexmedetomidine (n = 857) (RR 0.4; 95% CI: 0.4–0.5), fentanyl (n = 126) (RR 0.5; 95% CI: 0.4–0.6) and remifentanil (n = 571) (RR 0.4; 95% CI: 0.4–0.5) all had large effect size to minimise coughing at extubation (Figure 2) (Tung et al 2020). There were no reported adverse events in any of the systematic reviews, although the use of dexmedetomidine was associated with bradycardia. An increase in time to extubation was seen in IV lidocaine (mean difference (MD) 1.9 min; 95% CI: 0.8–3.0 min), and intracuff lidocaine (MD 5.3 min; 95% CI: 1.9–8.8 min) (Tung et al 2020, Yang et al 2020b). The other strategies did not result in a statistically significant difference in time to extubation (Liao et al 2019, Tung et al 2020).
Figure 1.
Flow diagram of systematic review selection
Table 1.
Summary of pharmacologic methods to minimise cough during extubation
| Authors (year) | Surgical population | Number of participants | Intervention | Doses | Cough prevention RR (95% CI) |
|---|---|---|---|---|---|
| Yang et al (2020b) | GS, GYN, Neuro, Oph, Ortho, OTL, Uro. | 1516 | IV Lidocaine | 1–2mg kg–1 | 0.6 (0.5–0.9) |
| Tung et al (2020) a | Any elective | 963 | Intracuff lidocaine | Lidocaine 2% × 2–6mL Lidocaine 4% × 5mL |
0.6 (0.5–0.7) |
| Peng et al (2020) | GYN, OTL, Dental, Opth, Spine, Plastic, Ortho, Uro | 868 | Intracuff lidocaine | Lidocaine 1%–10% ± sodium bicarbonate | 0.5 (0.3–0.7) |
| Liao et al (2019) | GS, GYN, Ortho, OTL | 2146 | Lidocaine lubricants | Not reported | 0.9 (0.7–1.2) |
| Tung et al (2020) a | Any elective | 495 | TT lidocaine | 1–2mg kg −1 | 0.7 (0.6–0.8) |
| Tung et al (2020) a | Any elective | 857 | IV dexmedetomidine | 0.25–1.2μg kg−1 | 0.4 (0.4–0.5) |
| Tung et al (2020) a | Any elective | 126 | IV fentanyl | 1–2μg kg−1 | 0.5 (0.4–0.6) |
| Tung et al (2020) a | Any elective | 571 | IV remifentanil | Bolus: 0.1–1.0μg kg−1 Inf: 0.001–0.3μg kg −1 min−1 |
0.4 (0.4–0.5) |
CI: confidence interval; GS: general surgery; GYN: gynaecology; Neuro: neurosurgery; OTL: otorhinolaryngology; Oph: ophthalmology; PS: plastic surgery; RR: relative risk versus placebo; TT: tracheal tube; Uro: urology.
Transformed data from absolute effects.
Figure 2.
Pharmacologic interventions to reduce cough during extubation. Data are relative risks (RR) of coughing on extubation and 95% confidence intervals (CI), compared with placebo. Intracuff lidocaine = Tung et al. Intracuff lidocaine (2) = Peng et al
Discussion
The COVID-19 pandemic has raised awareness of the increased risk of viral transmission to health care workers when performing aerosol-generating procedures, especially tracheal extubation (Jackson et al 2020). This review aimed to summarise the current pharmacologic methods available to minimise cough at the time of extubation and to determine whether some strategies could be more beneficial than others. Based on the available data from various systematic reviews, dexmedetomidine and remifentanil seem to have the largest effect to reduce cough on extubation. Alternatively, the use of intracuff lidocaine is also an option to consider.
The antitussive actions of opioids such as remifentanil are well known; opioids exert coughing suppression centrally by their effect on medullary cough centres. On the contrary, the mechanism(s) by which alpha-2 agonists, such as dexmedetomidine, exhibit cough suppressant effects remain unclear. One possible hypothesis may be related to the attenuation of C-fibre-mediated airway smooth muscle contraction (Mikami et al 2017). When we compare the RR of each medication (and their respective 95% CI), it seems like remifentanil and dexmedetomidine would be the optimal choice to decrease the incidence of coughing on extubation. However, the use of these medications would come with the caveat of adverse effects on respiratory drive, neuromuscular function and haemodynamics. Some concerns regarding prolongation of the extubation time when using medication to prevent coughing may also be raised. Although no statistical difference was seen in the systematic reviews included in this article, this may be due to an underpowered analysis.
One could consider a combination of multiple strategies to prevent coughing on extubation would be even more effective and could minimise the side effects of each respective pharmacological agent. However, to the best of our knowledge, multimodal cough-prevention strategies have not yet been explored in randomised controlled trials. In addition, no retrospective study has been published to assess the strategies employed by health care workers who reported infection by SARS-CoV-2 after performing tracheal intubation or extubating of a patient with suspected or confirmed COVID-19.
This summary of systematic reviews is limited by the sparse available data in the current literature. The generalisability of the effect size for each pharmacologic agent should be made with caution, as these systematic reviews may not include the same population of interest. Moreover, the systematic reviews performed by Liao et al 2019, Peng et al 2020 and Yang et al 2020b focused specifically on lidocaine lubricants and IV solutions, respectively, and did not examine the efficacy of alpha2-agonists and opioids on coughing prevention. On the contrary, Tung et al 2020 examined the efficacies of every pharmacologic agent included in this summary (lidocaine IV, intracuff, topical or tracheal application, dexmedetomidine, remifentanil and fentanyl). In other words, the only systematic review that assessed the effect of dexmedetomidine and remifentanil on cough prevention was that of Tung et al 2020. The authors concluded that all the medications studied (ie: lidocaine, dexmedetomidine, opioids) had the potential to decrease the incidence of coughing on extubation in comparison with either placebo or no medication. Yet, a post hoc ranking curve analysis (SUCRA) demonstrated that despite a lower number of participants to whom it was administered (857 participants versus 1458 having received lidocaine), dexmedetomidine had the highest likelihood of ranking first with regard to decreasing the incidence of emergence coughing, followed by remifentanil, which is consistent with our conclusion.
Conclusion
The results of this summary of systematic reviews are hypothesis-generating and emphasise the lack of available data at the present time. According to currently available systematic reviews, perioperative IV administration of dexmedetomidine and remifentanil, or intracuff injection of lidocaine, seem to have the largest effect on cough prevention at the time of tracheal extubation. Despite providing promising results, these pharmacologic agents should be further explored in a network meta-analysis to determine the granularity of the data. Furthermore, the relative efficacy for cough prevention and safety data for each medication should be determined with prospective randomised controlled trials.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Provenance and Peer review: Unsolicited contribution; Peer reviewed; Accepted for publication 19 September 2022.
ORCID iD: Stephen Su Yang  https://orcid.org/0000-0003-3859-5110
https://orcid.org/0000-0003-3859-5110
References
- Asai T, Koga K, Vaughan RS.1998Respiratory complications associated with tracheal intubation and extubation British Journal of Anaesthesia 80767–775 [DOI] [PubMed] [Google Scholar]
- Begley JL, Lavery KE, Nickson CP, Brewster DJ.2020The aerosol box for intubation in coronavirus disease 2019 patients: An in-situ simulation crossover study Anaesthesia 751014–1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown J, Gregson FKA, Shrimpton A, Cook TM, Bzdek BR, Reid JP, Pickering AE.2021A quantitative evaluation of aerosol generation during tracheal intubation and extubation Anaesthesia 76174–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clivio S, Putzu A, Tramèr MR.2019Intravenous lidocaine for the prevention of cough: Systematic review and meta-analysis of randomized controlled trials Anesthesia & Analgesia 1291249–1255 [DOI] [PubMed] [Google Scholar]
- El-Boghdadly K, Wong DJN, Owen R, et al. 2020Risks to healthcare workers following tracheal intubation of patients with COVID-19: A prospective international multicentre cohort study Anaesthesia 751437–1447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson T, Deibert D, Wyatt G, et al. 2020Classification of aerosol-generating procedures: A rapid systematic review BMJ Open Respiratory Research 7 e000730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John Hopkins University 2020Worldometer. COVID-19 Coronavirus Pandemic Available at https://www.worldometers.info/coronavirus
- Liao AH, Yeoh SR, Lin YC, Lam F, Chen T-L, Chen C-Y.2019Lidocaine lubricants for intubation-related complications: A systematic review and meta-analysis Can J Anaesth 661221–1239 [DOI] [PubMed] [Google Scholar]
- Matava CT, Yu J, Denning S.2020Clear plastic drapes may be effective at limiting aerosolization and droplet spray during extubation: Implications for COVID-19 Can J Anaesth 67902–904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerowitz EA, Richterman A, Gandhi RT, Sax PE.2021Transmission of SARS-CoV-2: A review of viral, host, and environmental factors Annals of Internal Medicine 17469–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikami M, Zhang Y, Kim B, Worgall TS, Groeben H, Emala CW. Dexmedetomidine’s inhibitory effects on acetylcholine release from cholinergic nerves in guinea pig trachea: A mechanism that accounts for its clinical benefit during airway irritation BMC Anesthesiology. 2017;17:52. doi: 10.1186/s12871-017-0345-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng F, Wang M, Yang H, Yang X, Long M.2020Efficacy of intracuff lidocaine in reducing coughing on tube: a systematic review and meta-analysis Journal of International Medical Research 48(2) DOI: 10.1177/0300060520901872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schimmel M, Berkowitz DM.2022Pulmonary procedures in the COVID-19 era Current Pulmonology Reports 1139–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J.2012Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review PLoS ONE 7 e35797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung A, Fergusson NA, Ng N, Hu V, Dormuth C, Griesdale DEG.2020Medications to reduce emergence coughing after general anaesthesia with tracheal intubation: A systematic review and network meta-analysis British Journal of Anaesthesia Epub ahead of print 22February DOI 10.1016/j.bja.2019.12.041 [DOI] [PubMed] [Google Scholar]
- Wilson NM, Norton A, Young FP, Collins DW.2020Airborne transmission of severe acute respiratory syndrome coronavirus-2 to healthcare workers: A narrative review Anaesthesia 751086–1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang SS, Lipes J, Dial S, et al. 2020. a Outcomes and clinical practice in patients with COVID-19 admitted to the intensive care unit in Montréal, Canada: A descriptive analysis CMAJ Open 8 E788–E795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang SS, Wang NN, Postonogova T, et al. 2020. b Intravenous lidocaine to prevent postoperative airway complications in adults: A systematic review and meta-analysis British Journal of Anaesthesia 124314–323 [DOI] [PubMed] [Google Scholar]
- Yang SS, Zhang M, Chong JJR.2020. c Comparison of three tracheal intubation methods for reducing droplet spread for use in COVID-19 patients British Journal of Anaesthesia 125 e190–e191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas G, Chiang MC, Wong E, MacDonald F, Lange CF, Senthilselvan A, King M. Cough aerosol in healthy participants: Fundamental knowledge to optimize droplet-spread infectious respiratory disease management BMC Pulmonary Medicine. 2012;12:11. doi: 10.1186/1471-2466-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]