Abstract
Objectives:
Early in the COVID-19 pandemic, several outbreaks were linked with facilities employing essential workers, such as long-term care facilities and meat and poultry processing facilities. However, timely national data on which workplace settings were experiencing COVID-19 outbreaks were unavailable through routine surveillance systems. We estimated the number of US workplace outbreaks of COVID-19 and identified the types of workplace settings in which they occurred during August–October 2021.
Methods:
The Centers for Disease Control and Prevention collected data from health departments on workplace COVID-19 outbreaks from August through October 2021: the number of workplace outbreaks, by workplace setting, and the total number of cases among workers linked to these outbreaks. Health departments also reported the number of workplaces they assisted for outbreak response, COVID-19 testing, vaccine distribution, or consultation on mitigation strategies.
Results:
Twenty-three health departments reported a total of 12 660 workplace COVID-19 outbreaks. Among the 12 470 workplace types that were documented, 35.9% (n = 4474) of outbreaks occurred in health care settings, 33.4% (n = 4170) in educational settings, and 30.7% (n = 3826) in other work settings, including non–food manufacturing, correctional facilities, social services, retail trade, and food and beverage stores. Eleven health departments that reported 3859 workplace outbreaks provided information about workplace assistance: 3090 (80.1%) instances of assistance involved consultation on COVID-19 mitigation strategies, 1912 (49.5%) involved outbreak response, 436 (11.3%) involved COVID-19 testing, and 185 (4.8%) involved COVID-19 vaccine distribution.
Conclusions:
These findings underscore the continued impact of COVID-19 among workers, the potential for work-related transmission, and the need to apply layered prevention strategies recommended by public health officials.
Keywords: COVID-19, workplace, disease outbreaks
Workplace transmission of SARS-CoV-2 has been recognized since the start of the COVID-19 pandemic, and several outbreaks have been linked with workplaces such as long-term care facilities, 1 meat and poultry processing plants, 2 and correctional facilities. 3 Recommendations for operation of businesses and other facilities and stay-at-home measures to mitigate the spread of COVID-19 have evolved during the pandemic. COVID-19 vaccines became available in December 2020 in phases, with health care personnel and long-term care residents prioritized first 4 ; availability and implementation of vaccines varied across the country. With the emergence of the Delta variant in summer 2021, 5 workplaces continued to be important settings for mitigation efforts to reduce the risk of transmission. To help understand how much workplace transmission may have been occurring during August through October 2021 and in what settings, the Centers for Disease Control and Prevention (CDC) invited the health departments from all 50 states, 8 US territories and freely associated states, and the District of Columbia to report aggregate surveillance data for COVID-19 outbreaks occurring in public or private work settings from August 1 through October 31, 2021. Some states passed the request on to health departments representing individual cities or counties.
Methods
CDC requested information reported to the health department by workplace establishments on the number of workplace COVID-19 outbreaks, by workplace setting, and the total number of cases among workers linked to these outbreaks. We categorized workplaces according to categories based on the 2017 North American Industry Classification System. 6 For this study, CDC asked health departments to apply the case definition of a workplace outbreak provided by the Council of State and Territorial Epidemiologists (CSTE), which is based on ≥2 COVID-19 cases among workers, 7 to all workplaces. CSTE defines an outbreak in a nonresidential, non–health care workplace setting as the following: “Two or more laboratory-confirmed COVID-19 cases among workers at a facility with onset of illness within a 14-day period, who are epidemiologically linked, do not share a household, and are not listed as a close contact of each other outside of the workplace during standard case investigation or contact tracing.” 7
CDC asked health departments to include only cases among workers associated with each outbreak. Health departments followed this guidance to the extent that they were able, given that many of them recorded workplace outbreaks based on different local passive reporting requirements (eg, California defined outbreaks in non–health care settings as ≥3 probable or confirmed cases 8 rather than ≥2). CDC also asked health departments to report the total numbers of confirmed working-age cases 9 (aged 18-64 years, including outbreak related and non–outbreak related) during the study period and the number of workplaces that they assisted for outbreak response, COVID-19 testing, vaccine distribution, or consultation on mitigation strategies. CDC reviewed this activity and conducted it consistent with applicable federal law and CDC policy (eg, 45 CFR part 46.102[I][2], 21 CFR part 56; 42 USC §241[d]; 5 USC §552a; 44 USC §3501 et seq).
We estimated counts of workplace establishments and quarterly employment for the various workplace types by aggregating industry-specific second quarter 2021 Quarterly Census of Employment and Wages (QCEW) data for each jurisdiction covered by participating health departments into categories approximating those used by the health departments for reporting. The QCEW is a quarterly count of the number of business establishments, monthly employment, and quarterly wages for workers covered by state unemployment insurance laws and federal workers covered by the Unemployment Compensation for Federal Employees program compiled by the Bureau of Labor Statistics. 10 Establishment counts are derived from administrative data from state and federal unemployment insurance programs. Employment and wage data are reported by employers. We calculated quarterly employment as the average monthly employment for the 3 months of the quarter. We conducted all analyses in SAS version 9.4 (SAS Institute Inc).
Results
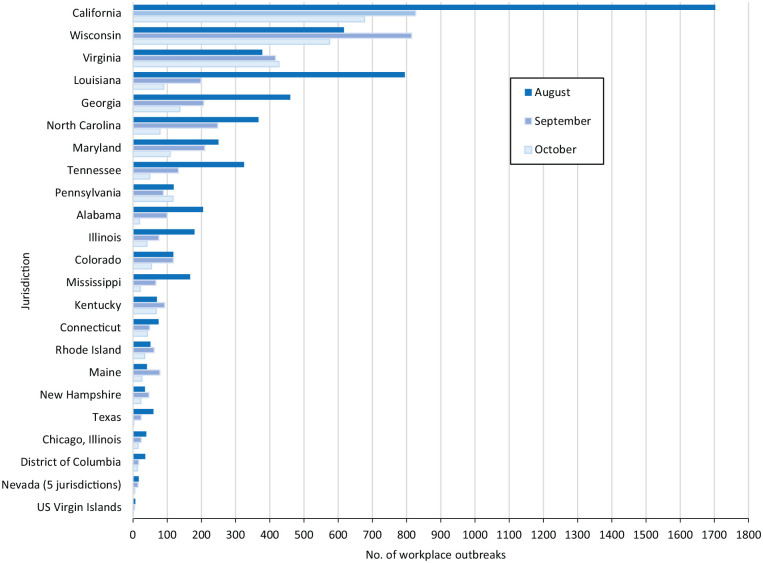
Twenty-three health departments reported a total of 12 660 workplace COVID-19 outbreaks during August–October 2021 (Table 1, Figure 1). These outbreaks included at least 52 635 cases among workers, an average of 4.2 confirmed cases per outbreak. We found an average of 1.85 workplace outbreak–associated cases per 100 working-age cases in the participating jurisdictions. In 16 of 23 jurisdictions, the highest number of workplace outbreaks was reported in August.
Table 1.
Number of workplace COVID-19 outbreaks, a outbreak-associated cases, and total cases among working-age adults by jurisdiction, 23 US jurisdictions, August–October 2021 b
| No. of workplace outbreaks | August–October, no. | |||||||
|---|---|---|---|---|---|---|---|---|
| Jurisdiction | August | September | October | August–October | Outbreak-associated cases among workers | Average cases per outbreak | Total cases among working-age adults c | Workplace outbreak-associated cases per 100 working-age cases d |
| Alabama | 205 | 100 | 19 | 324 | 3820 | 11.8 | 154 977 | 2.5 |
| California e | 1703 | 827 | 677 | 3207 | 7812f,g,h | 2.4 | 523 459 | 1.5 |
| Colorado i | 118 | 118 | 54 | 290 | 1324 | 4.6 | 102 243 | 1.3 |
| Connecticut j | 75 | 49 | 42 | 166 | 563 | 3.4 | 27 194 | 2.1 |
| District of Columbia | 36 | 17 | 13 | 66 | 296 | 4.5 | 9006 | 3.3 |
| Georgia | 460 | 207 | 137 | 804 | 3117f,g | 3.9 | 218 042 | 1.4 |
| Illinois, excluding Chicago | 180 | 76 | 41 | 297 | 1317 | 4.4 | 173 079 | 0.8 |
| Chicago k | 39 | 24 | 15 | 78 | 316 | 4.1 | 23 409 | 1.4 |
| Kentucky l | 70 | 93 | 68 | 231 | 1848 m | 8.0 | 110 630 | 1.7 |
| Louisiana n | 795 | 199 | 90 | 1084 | 5002 | 4.6 | 96 301 | 5.2 |
| Maine o | 41 | 79 | 26 | 146 | 894 | 6.1 | 14 340 | 6.2 |
| Maryland | 250 | 210 | 109 | 569 | 2748 | 4.8 | 58 934 | 4.7 |
| Mississippi | 167 | 67 | 21 | 255 | 1328 | 5.2 | 95 637 | 1.4 |
| Nevada p | 17 | 15 | 5 | 37 | 120 | 3.2 | 4986 | 2.4 |
| New Hampshirei,o | 35 | 47 | 23 | 105 | 468 | 4.5 | 10 458 | 4.5 |
| North Carolina | 367 | 248 | 79 | 694 | 4740 | 6.8 | 230 226 | 2.1 |
| Pennsylvania q | 119 | 89 | 117 | 325 | 1119 f | 3.4 | 162 352 | 0.7 |
| Rhode Island | 51 | 62 | 34 | 147 | 447 | 3.0 | 17 229 | 2.6 |
| Tennessee | 325 | 133 | 49 | 507 | 3103 | 6.1 | 169 841 | 1.8 |
| Texas | 60 | 24 | 2 | 86 | 358 | 4.2 | 387 545 | 0.1 |
| US Virgin Islands | 7 | 5 | 1 | 13 | 78 | 6.0 | 1751 | 4.5 |
| Virginia | 378 | 417 | 427 | 1222 | 5985 g | 4.9 | 143 394 | 4.2 |
| Wisconsin | 617 | 815 | 575 | 2007 | 5832 g | 2.9 | 108 699 | 5.4 |
| Total | 6115 | 3921 | 2624 | 12 660 | 52 635 | 4.2 | 2 843 732 | 1.9 |
The Centers for Disease Control and Prevention invited the health departments from all 50 states, 8 US territories and freely associated states, and the District of Columbia to report aggregate surveillance data for COVID-19 outbreaks occurring in public or private work settings from August 1 through October 31, 2021. Some states passed the request on to health departments representing individual cities or counties.
Except where otherwise noted, “workplace outbreak” was defined for this study according to the Council of State and Territorial Epidemiologists’ surveillance definition for an outbreak in a nonresidential, non–health care workplace setting: “Two or more laboratory-confirmed COVID-19 cases among workers at a facility with onset of illness within a 14-day period, who are epidemiologically linked, do not share a household, and are not listed as a close contact of each other outside of the workplace during standard case investigation or contact tracing.” 7
Total cases among adults aged 18-64 years, including both outbreak-related and non–outbreak-related cases.
Workplace outbreak-associated cases per 100 working-age cases was calculated according to the following formula: number of outbreak-associated cases among workers (August–October 2021) divided by the total number of cases among working-age adults × 100.
California defines outbreaks in non–health care settings as ≥3 cases, rather than ≥2 cases.
Case counts include probable cases.
Case counts may include nonworker adults associated with the outbreaks.
Limited to people aged 18-64 years. Age only available for 67% of outbreak-associated cases reported by California; outbreak-associated cases without available age information were excluded from outbreak-associated case numbers.
Excluded outbreaks still active at the time of reporting.
Connecticut did not consistently track college/university or correctional facility outbreaks.
Chicago definition of school outbreak changed on October 4 (from 2 cases to 3).
Kentucky data exclude correctional facilities, hospitals, and skilled nursing facilities.
Kentucky definition of health care setting outbreaks and non–health care setting (except for education) outbreaks requires ≥5 cases.
Louisiana reporting in September was likely reduced because of Hurricane Ida.
Outbreak definition based on ≥3 confirmed cases (2 of which are staff).
Includes only Carson City, Churchill County, Douglas County, Lyon County, and Storey County.
Pennsylvania excluded Philadelphia County in all counts except for hospital outbreaks. Only daycares/preschools were included for educational settings. First response does not include any health care services (eg, emergency medical services).
Figure 1.
Workplace outbreaks reported to the Centers for Disease Control and Prevention by 23 US jurisdictions, August–October 2021. Data for Nevada were reported by these jurisdictions only: Churchill County, Carson City, Douglas County, Lyon County, and Storey County.
Health departments documented workplace type for 12 470 (98.5%) outbreaks involving 49 938 (94.9%) workers; we grouped these workplace outbreaks into 3 broad settings: 4474 (35.9%) outbreaks involving 18 046 (36.1%) workers in health care settings, 4170 (33.4%) outbreaks involving 13 097 (26.2%) workers in educational settings, and 3826 (30.7%) outbreaks involving 18 795 (37.6%) workers in other work settings (Table 2). Of the >5 million workplace establishments in the 23 participating jurisdictions, 7.5% were categorized as health care, 2.6% as educational, and 89.9% as other non–health care settings; the corresponding proportions of all employed workers in these jurisdictions were 12.0%, 9.5%, and 78.5%. Most outbreaks in health care settings (81.7%; 3655 of 4474) occurred in nursing and residential care facilities, and most in educational settings (73.2%; 3051 of 4170) occurred in K-12 schools (kindergarten through 12th grade). Other settings included non–food manufacturing facilities (11.0%; 419 of 3826), correctional facilities (10.7%; n = 410), social services (6.7%; n = 258), retail trade (6.7%; n = 256), and food and beverage stores (5.9%; n = 226).
Table 2.
Workplace COVID-19 outbreaks, a by work setting category and specific work setting, 23 US jurisdictions, August–October 2021 b
| No. (%) | |||||
|---|---|---|---|---|---|
| Work setting (approximate NAICS code) c | No. of jurisdictions reporting | Workplace outbreaks (n = 12 470) d | Establishments e f (n = 5 660 735) | Outbreak-associated cases among workers (n = 49 938) | Employed population (n = 71 758 633)e,f |
| Any health care setting | 23 | 4474 (35.9) | 422 744 (7.5) | 18 046 (36.1) | 8 616 484 (12.0) |
| Hospital (622) | 17 | 404 (9.0) | 7442 (1.8) | 1625 (9.0) | 2 741 842 (31.8) |
| Nursing and residential health care facility (623) | 20 | 3655 (81.7) | 41 040 (9.7) | 15 603 (86.5) | 1 474 930 (17.1) |
| Pharmacy (446110) | 2 | 8 (0.2) | 32 358 (7.7) | 14 (0.1) | 346 436 (4.0) |
| Ambulatory health care (621) | 14 | 175 (3.9) | 341 904 (80.9) | 795 (4.4) | 4 053 276 (47.0) |
| Health care setting–type not specified | — | 232 (5.2) | — | — | — |
| Any educational setting | 23 | 4170 (33.4) | 149 682 (2.6) | 13 097 (26.2) | 6 805 267 (9.5) |
| Preschool or daycare (62441) | 20 | 905 (21.7) | 38 622 (25.8) | 2264 (17.3) | 412 461 (6.1) |
| K-12 school (61111) | 20 | 3051 (73.2) | 43 562 (29.1) | 9974 (76.2) | 4 105 781 (60.3) |
| Other schools and instructional settings (other 611) | 13 | 168 (4.0) | 67 498 (45.1) | 2763 (21.1) | 2 287 025 (33.6) |
| Educational setting–type not specified | — | 46 (1.1) | — | — | — |
| Other setting | 23 | 3826 (30.7) | 5 088 309 (89.9) | 18 795 (37.6) | 56 336 882 (78.5) |
| Correctional facility (92214) | 19 | 410 (10.7) | 2834 (0.1) | 4420 (23.5) | 248 867 (0.4) |
| Non–food manufacturing facility (other 31-33) | 16 | 419 (11.0) | 169 403 (3.3) | 2346 (12.5) | 4 948 068 (8.8) |
| Social service (624) | 13 | 258 (6.7) | 692 565 (13.6) | 981 (5.2) | 1 796 662 (3.2) |
| Retail trade (44-45, excluding 446110 and 445) | 10 | 256 (6.7) | 417 278 (8.2) | 1074 (5.7) | 5 268 617 (9.4) |
| Food and beverage store (445) | 15 | 226 (5.9) | 72 913 (1.4) | 861 (4.6) | 1 607 812 (2.9) |
| Accommodation and food services (72) | 7 | 192 (5.0) | 380 006 (7.5) | 592 (3.1) | 6 244 896 (11.1) |
| Other services (except public administration) (81 excluding 8122) | 9 | 127 (3.3) | 427 001 (8.4) | 539 (2.9) | 2 078 507 (3.7) |
| Food manufacturing facility (311) | 14 | 104 (2.7) | 18 121 (0.4) | 1098 (5.8) | 729 479 (1.3) |
| Construction (23) | 7 | 140 (3.7) | 413 839 (8.1) | 349 (1.9) | 3 897 096 (6.9) |
| Professional, scientific, technical, management, administrative, and waste management services (54, 55, 56) | 8 | 89 (2.3) | 1 067 264 (21.0) | 282 (1.5) | 11 427 517 (20.3) |
| Transportation and warehousing (48-49, excluding 485 and 491) | 5 | 81 (2.1) | 140 128 (2.8) | 394 (2.1) | 2 935 327 (5.2) |
| Finance, insurance, real estate, rental, and leasing (52, 53) | 7 | 83 (2.2) | 495 138 (9.7) | 211 (1.1) | 4 120 430 (7.3) |
| Arts, entertainment, and recreation (71) | 7 | 73 (1.9) | 88 658 (1.7) | 245 (1.3) | 1 109 333 (2.0) |
| Public administration (except first responders and correctional facilities) (92, excluding 922) | 13 | 112 (2.9) | 54 365 (1.1) | 669 (3.6) | 2 905 067 (5.2) |
| First response (92212, 92216, 92219) | 11 | 58 (1.5) | 6945 (0.1) | 252 (1.3) | 548 963 (1.0) |
| Utilities (22) | 7 | 58 (1.5) | 14 080 (0.3) | 198 (1.1) | 275 998 (0.5) |
| Agriculture, forestry, fishing, or hunting (11) | 10 | 41 (1.1) | 52 785 (1.0) | 272 (1.4) | 690 889 (1.2) |
| Public transit (485) | 9 | 41 (1.1) | 10 364 (0.2) | 203 (1.1) | 217 677 (0.4) |
| Wholesale trade (42) | 4 | 32 (0.8) | 313 101 (6.2) | 148 (0.8) | 2 978 484 (5.3) |
| US Postal Service (491) | 5 | 24 (0.6) | 13 629 (0.3) | 109 (0.6) | 306 932 (0.5) |
| Information (51) | 4 | 17 (0.4) | 112 813 (2.2) | 37 (0.2) | 1 554 359 (2.8) |
| Death care (8122) | 5 | 12 (0.3) | 9167 (0.2) | 57 (0.3) | 69 235 (0.1) |
| Mining, quarrying, and oil and gas extraction (21) | 3 | 9 (0.2) | 16 865 (0.3) | 37 (0.2) | 291 930 (0.5) |
| Other or unknown | 20 | 396 (10.4) | 99 047 (2.0) | 1870 (9.9) | 84 738 (0.2) |
Abbreviations: —, does not apply; K-12, kindergarten through 12th grade; NAICS, North American Industry Classification System.
The Centers for Disease Control and Prevention invited the health departments from all 50 states, 8 US territories and freely associated states, and the District of Columbia to report aggregate surveillance data for COVID-19 outbreaks occurring in public or private work settings from August 1 through October 31, 2021. Some states passed the request on to health departments representing individual cities or counties.
Except where otherwise noted, “workplace outbreak” was defined for this study according to the Council of State and Territorial Epidemiologists’ surveillance definition for an outbreak in a nonresidential, non–health care workplace setting: “Two or more laboratory-confirmed COVID-19 cases among workers at a facility with onset of illness within a 14-day period, who are epidemiologically linked, do not share a household, and are not listed as a close contact of each other outside of the workplace during standard case investigation or contact tracing.” 7
Data source: US Census Bureau. 6
During August–October 2021, there were 12 660 workplace COVID-19 outbreaks reported overall; however, setting was unknown or undocumented for 190 workplace outbreaks.
Based on the second quarter 2021 Quarterly Census of Employment and Wages (QCEW). The QCEW is a quarterly count of the number of business establishments and monthly employment and quarterly wages for workers covered by state unemployment insurance laws and federal workers covered by the Unemployment Compensation for Federal Employees program compiled by the Bureau of Labor Statistics. Establishment counts are derived from administrative data from state and federal unemployment insurance programs. Employment and wage data are reported by employers. The QCEW covers >95% of all US jobs. 9
For major categories (ie, any health care setting, any educational setting, any other non–health care setting), column percentage denominators are based on the total number of establishments or employment across all work settings; for subcategories, column percentage denominators are based on the applicable major category.
Among 11 health departments that reported 3859 workplace outbreaks during August–October 2021 and provided information about workplace assistance from health departments, 3090 (80.1%) instances of assistance involved consultation on COVID-19 mitigation strategies, 1912 (49.5%) involved outbreak response, 436 (11.3%) involved COVID-19 testing, and 185 (4.8%) involved COVID-19 vaccine distribution.
Discussion
Preventing and tracking COVID-19 workplace outbreaks is important because workers have little control over their work environment, workplace outbreaks can drive community transmission, and understanding the types of settings affected by COVID-19 can help inform interventions. A study of early COVID-19 cases in Colorado found that 47 of 99 (47%) cases with known infected contacts reported workplace exposure. 11 Most workplace types reporting outbreaks in this study (ie, nursing and residential care facilities, K-12 schools, manufacturing facilities, correctional facilities) were previously identified as being at increased risk for COVID-19 spread. However, to our knowledge, our study is one of the first multistate reports to confirm that outbreaks continued to be common in non–health care, noneducational workplaces during a period dominated by the Delta variant, after COVID-19 vaccines and other mitigation measures became widely promoted by public health officials. Consultation on COVID-19 mitigation strategies was the most frequently requested assistance. We found a high ratio of reported outbreaks in health care and educational settings relative to the proportions of these settings among all workplaces. This high ratio may reflect a combination of a high risk of spread and increased testing and reporting in these settings compared with other workplaces.
CDC published COVID-19 guidance for health care settings, 12 educational settings, 13 correctional and detention facilities, 14 other industries, and general businesses. 15 The Occupational Safety and Health Administration has also published guidance for workplaces. 16 Both agencies emphasize that preventing workplace transmission of SARS-CoV-2 requires layering multiple mitigation strategies that include vaccination, improved building ventilation, the wearing of well-fitting face masks, physical distancing, handwashing, cleaning and disinfection, screening tests, isolation of cases, and quarantine of unvaccinated close contacts.
Both CDC and Occupational Safety and Health Administration guidance recommend that employers report outbreaks to local health departments as required and support their contact tracing efforts; reporting is required by law in some jurisdictions. CSTE developed definitions of COVID-19 outbreaks in specific settings and provided guidance for documenting individual cases as outbreak associated. CSTE published separate outbreak definitions for nonresidential, non–health care workplace, educational, and health care settings. 17 Many jurisdictions adapted the CSTE definitions to meet their local needs, as evidenced in the range in cases per outbreak and outbreak-associated cases per 100 cases reported by various jurisdictions. Health departments also developed various strategies for prioritizing workplace outbreak investigations. 18 We applied the CSTE case definition of an outbreak in a nonresidential, non–health care workplace setting to all workplaces, including health care and educational settings. Using this definition, jurisdictions identified the highest number of workplace outbreaks during the study period in health care settings, followed by educational settings. Most other reported workplace settings were those in which workers interact with large numbers of the public (eg, retail trade, food and beverage stores) or work in close proximity to one another (eg, manufacturing facilities).
Limitations
Our study had several limitations. First, because data on workplace COVID-19 outbreaks are not consistently collected across health departments, our study was based on a passively collected convenience sample that depended on state-specific requirements. Second, reporting biases made comparisons among work settings challenging. Regular COVID-19 screening programs and public health emphasis in some work settings (eg, long-term care) meant that we compared settings that conducted active surveillance with those conducting passive surveillance. Third, difficulty in linking cases to workplaces, especially during widespread community transmission, may have resulted in under- or overcounting workplace COVID-19 outbreaks and associated cases. Fourth, use of the CSTE workplace outbreak case definition, which requires ≥2 cases among workers, could have resulted in an underestimation of outbreaks with an occupational component because of patient-, student-, or customer-to-worker transmission. Fifth, undercounts may also have resulted from a lack of reporting requirements, data lags, and other reporting challenges. Sixth, overcounts may have resulted from duplicate reporting caused by overlap among jurisdictions, ongoing cases from July outbreaks that were counted in August, transmission outside the workplace among workers, or data collection that does not distinguish between workers and nonworkers. However, CDC’s requirement that health departments report only the number of confirmed working-age cases (aged 18-64 years) minimized overcounts caused by counting nonworkers.
Seventh, some limitations applied to the comparisons made between the distribution of workplace types and workers involved in the reported outbreaks and the underlying distribution of workplace types and workers in the participating jurisdictions based on QCEW data. Industry categories used in QCEW data differ slightly from industry categories used for outbreak reporting. We also note a slight mismatch between the geographic areas represented in the outbreak data and those available in the reference data. Eighth, data collection on workplace requests for assistance varied by jurisdiction: some jurisdictions included only workplace-initiated requests, and other jurisdictions included active outreach from health departments to workplaces. Follow-up data were not available to determine the extent to which the technical assistance and guidance were implemented and enforced. Ninth, data were also unavailable on the vaccination status of workers involved in outbreaks and on the prevalence of remote work in different work settings.
Conclusion
Our study illustrates that COVID-19 outbreaks linked to workplaces, as defined here, were commonly reported to health departments during August–October 2021, when the Delta variant was predominant in the United States. It also highlights the workplace demand for assistance that health departments experienced, particularly for consultations on COVID-19 mitigation strategies. These findings underscore the continued impact of COVID-19 among workers, the potential for work-related transmission, and the need to apply layered prevention strategies recommended by public health officials, especially as new variants of concern arise. Vaccination with the primary series and recommended boosters remain the leading public health prevention strategy to lessen economic impacts and to help end the COVID-19 pandemic by reducing transmission and risk of severe disease, hospitalization, and death.
Acknowledgments
We acknowledge the following people for assistance in coordinating data collection and compilation: Namita Agravat, Caroline Bennett, Lauren Billick, Charles Braxton, Alicia Dunajcik, Laura Hill, Otto Ike, Geremy Lloyd, Veneranda Ngulefac, Francisco Palomeque, Neela Persad, Jessica Ricaldi, Laird Ruth, Rebecca Sabo, Fija Scipio, Denise Sheriff, and Christina Winfield, Centers for Disease Control and Prevention COVID-19 Response Team; Jade Angulo, Churchill County Department of Health; Katrina Hansen and Jonathan Stewart, New Hampshire Department of Public Health; Uche Ekwomadu, Salwa-Haque Mefruz, Will Still, and Christina Willut, District of Columbia Department of Health; Jaime Cassidy Comella, Monika Drogosz, Alison Green, Morgan Hargraves, Amanda Jain, Mukiio Hannah Kimanthi, Anna Makaretz, Theodore Marak, Dwayne Mitchell, Victoria Novotny, Shannon O’Rourke, and James C. Rajotte, Rhode Island Department of Health; and Elena Chan, Matt Frederick, Kathryn Gibb, Andrea Rodriguez, and Jessie Wong, California Department of Public Health.
Footnotes
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Sara E. Luckhaupt, MD  https://orcid.org/0000-0002-3000-8818
https://orcid.org/0000-0002-3000-8818
Cheryl L. Robbins, PhD  https://orcid.org/0000-0003-1320-2739
https://orcid.org/0000-0003-1320-2739
Isabel Thomas, MPH  https://orcid.org/0000-0001-6878-9704
https://orcid.org/0000-0001-6878-9704
Diana Valencia, MS  https://orcid.org/0000-0002-9578-3751
https://orcid.org/0000-0002-9578-3751
Katharine A. Owers Bonner, PhD  https://orcid.org/0000-0002-5323-5079
https://orcid.org/0000-0002-5323-5079
Kim Angelon-Gaetz, PhD  https://orcid.org/0000-0002-8530-0066
https://orcid.org/0000-0002-8530-0066
References
- 1. McMichael TM, Clark S, Pogosjans S, et al. COVID-19 in a long-term care facility—King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):339-342. doi: 10.15585/mmwr.mm6912e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Waltenburg MA, Rose CE, Victoroff T, et al. Coronavirus disease among workers in food processing, food manufacturing, and agriculture workplaces. Emerg Infect Dis. 2021;27(1):243-249. doi: 10.3201/eid2701.203821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lewis NM, Salmanson AP, Price A, et al. Community-associated outbreak of COVID-19 in a correctional facility—Utah, September 2020–January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(13):467-472. doi: 10.15585/mmwr.mm7013a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dooling K, McClung N, Chamberland M, et al. The Advisory Committee on Immunization Practices’ interim recommendation for allocating initial supplies of COVID-19 vaccine—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(49):1857-1859. doi: 10.15585/mmwr.mm6949e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. SARS-CoV-2 variant classifications and definitions. Updated April 26, 2022. Accessed September 15, 2022. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html
- 6. US Census Bureau. North American Industry Classification System. Last revised September 15, 2022. Accessed September 15, 2022. https://www.census.gov/naics
- 7. Council of State and Territorial Epidemiologists. Proposed investigation criteria and outbreak definition for COVID-19 in non-residential, non-healthcare workplace settings. July 14, 2020. Accessed September 15, 2022. https://preparedness.cste.org/wp-content/uploads/2020/08/OH-Outbreak-Definition.pdf
- 8. California Department of Public Health. Non-healthcare congregate facilities COVID-19 outbreak definitions and reporting guidance for local health departments. May 18, 2020. Accessed September 15, 2022. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/OutbreakDefinitionandReportingGuidance-10-13-2020.aspx
- 9. Centers for Disease Control and Prevention. National Notifiable Disease Surveillance System (NNDSS): coronavirus disease 2019 (COVID-19) 2021 case definition. Page last reviewed August 24, 2021. Accessed September 15, 2022. https://ndc.services.cdc.gov/case-definitions/coronavirus-disease-2019-2021
- 10. US Bureau of Labor Statistics. Quarterly census of employment and wages. Accessed September 15, 2022. https://www.bls.gov/cew
- 11. Marshall K, Vahey GM, McDonald E, et al. Exposures before issuance of stay-at-home orders among persons with laboratory-confirmed COVID-19—Colorado, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(26):847-849. doi: 10.15585/mmwr.mm6926e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. Updated February 2, 2022. Accessed September 15, 2022. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
- 13. Centers for Disease Control and Prevention. Operational guidance for K-12 schools and early care and education programs to support safe in-person learning. Updated August 11, 2022. Accessed September 15, 2022. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-childcare-guidance.html
- 14. Centers for Disease Control and Prevention. Guidance on prevention and management of coronavirus disease 2019 (COVID-19) in correctional and detention facilities. Updated May 3, 2022. Accessed September 15, 2022. https://www.cdc.gov/coronavirus/2019-ncov/community/correction-detention/guidance-correctional-detention.html
- 15. Centers for Disease Control and Prevention. COVID-19 information for the workplace. Page last reviewed October 5, 2021. Accessed September 15, 2022. https://www.cdc.gov/niosh/emres/2019_ncov_default.html
- 16. Occupational Safety and Health Administration. Protecting workers: guidance on mitigating and preventing the spread of COVID-19 in the workplace. Updated June 10, 2021. Accessed September 15, 2022. https://www.osha.gov/coronavirus/safework
- 17. Council of State and Territorial Epidemiologists. COVID-19 outbreak investigations and reporting. Accessed September 15, 2022. https://preparedness.cste.org/?page_id=211
- 18. Bonwitt J, Deya RW, Currie DW, et al. COVID-19 surveillance and investigations in workplaces—Seattle and King County, Washington, June 15–November 15, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(25):916-921. doi: 10.15585/mmwr.mm7025a3 [DOI] [PMC free article] [PubMed] [Google Scholar]