Short abstract
Content available: Audio Recording
Listen to an audio presentation of this article.

Edward Richard Howard
Amyloidosis is a general term for the extracellular infiltration of insoluble fibrils 1 , 2 (Fig. 1) of a variety of proteins that are produced in the bone marrow and found in the circulation as constituents of plasma. The wide spectrum of clinical phenotypes that result from this infiltration depends on the location and extent of the accumulation of the amyloid material. 4 , 6 , 7
FIG 1.

Amyloid fibrils. (A) Transmission electron. microscopy (TEM) of a typical amyloid nodule, in which amyloid bundles are seen arranged in a radial fashion in the vicinity of the Kupffer cell (×12,000). Reproduced with permission from 3 Acta Pathologica Japonica 1977; 27: 809‐822. (B) Schematic representation of amyloid fibril (above left) consisting of up of 4‐6 protofilaments – each made up of contiguous ß‐sheet polypeptide chains – wound around one another to form a 7.5‐10 nm structure seen on TEM (×100,000 – below left). The ultrastructure of the fibril allows the regular intercalation of Congo red dye (above right), which confers a diagnostic optical property to amyloid such as apple‐green birefringence under polarised light microscopy (below right). Reproduced with permission from 4 The New England Journal of Medicine 2003; 349: 583‐596. (C) Electron microscopy of platinum‐palladium shadowed amyloid fibrils that were sucrose gradient‐separated from homogenates of liver or spleen, obtained at autopsy of patients with primary, secondary, or myeloma‐associated amyloidosis (×70,000). Reproduced with permission from 5 Journal of Cell Biology 1967; 33:679‐708.
As with a majority of diseases, the etiology of amyloidosis remained something of a mystery in the 18th and 19th centuries. Early investigations were focused on patients who presented with gross hepatomegaly. The post‐mortem macroscopic appearances of the enlarged livers were variously described as pituitous (mucoid), waxy, lardaceous (i.e., greasy, oily, bacony, or bacon‐like) or scrofulous. 8 , 9 Srofulous amyloid was associated with chronic tuberculous infection of the cervical lymph glands, otherwise known as Scrofula. This term, which was familiar to the Hippocratic school, was subsequently encountered in 16th century medical literature from Salerno, Italy, as the diminutive of scrofa, which is Latin for a breeding sow. Apparently, the propensity to lymphadenopathy among scrofae was recorded by Aristotle 10 some 23 centuries before the German Nobel Laureate, Heinrich Hermann Robert Koch (Fig. 2A), discovered his eponymous tubercle bacillus, 11 which he demonstrated in scrofulous lymph nodes. Pre‐Koch, however, scrofula simply denoted “ … an inflammatory tumor…”, commonly in the neck, 12 of unknown transmissibility and an uncertain connection with tuberculosis in other parts of the body. 13
FIG 2.

(A) Robert Koch. Credit: Robert Koch Institute, Berlin, Germany. (B) Portrait of Sir Samuel Wilks Bt, by artist and caricaturist Sir Matthew Leslie Ward (aka SPY, 1851‐1922), which was painted first as a watercolor and then turned into a chromolithograph for publication in Vanity Fair in 1892 ©National Portrait Gallery, London. (C) Portrait of Rudolf Ludwig Karl Virchow by SPY, published in Vanity Fair in 1893 ©National Portrait Gallery, London. (D) Heinrich Meckel von Hemsbach. Reproduced with permission from 20 Neurosurgery 2010; 66:758‐771. (E) John Abercrombie, Credit: The Royal College Of Physicians Edinburgh. (F) Baron Karl Freiherr von Rokitansky. Credit: Wellcome Collection, London.
The more colorful historic name for tuberculous lymphadenopathy of the neck, “The King’s Evil,” began in the reigns of Clovis of France (481‐511) and Edward the Confessor in England (1042‐1066) and derived from the belief that that these Royal Houses had a supernatural gift to cure scrofula by touching the sufferers. The formal practice in which the monarch touched the diseased subject. – as vividly described by Shakespeare in Macbeth (Act IV Scene 3), which included awarding the medallion touch‐piece as a talisman for the supplicant – began with Louis IX of France (1226‐1270) and Edward III in England (1327‐1377). 14
There was a prolonged debate in earlier times as to whether the extracellular deposition of material responsible for the hepatomegaly was a carbohydrate or a protein derivative. Although initial reports were mostly concerned with its hepatic infiltration, renal involvement was eventually documented, and was then followed by descriptions in other organs by Sir Samuel Wilks Bt* (Fig. 2B), 15 collaborator and biographer of his “Three Great” contemporaries at Guy’s Hospital, Thomas Addison, Richard Bright and Thomas Hodgkin. Arguably, one of the most eminent physicians of the Victorian era, Wilks (1824‐1911) – whom The Times once called ‘‘the most philosophical of English physicians…’, and “who thought that the most wonderful thing in the world is a woman’s nervous system.” 16 – was a Fellow of the Royal Society, onetime President of the Pathological Society, President of the Neurological Society, Member of the Senate of the University of London and of the General Medicine Council, President of the Royal College of Physicians (1896‐1899) and Physician Extraordinary to Queen Victoria.
The term amyloid was suggested, nay decreed, in 1854 by the great German pathologist and outspoken reform‐minded political activist, Rudolph Ludwig Karl Virchow (Fig. 2C, 1821‐1902), whose alleged choice of weapons in response to Prussian Chancellor Otto Eduard Leopold von Bismark’s challenge to a duel, was a Trichinella‐infected pork sausage for one and a non‐tainted sausage for the other, masked and randomly assigned. Virchow’s proposal was declined by his would‐be combatant, and a duel did not materialize. (This is the stuff that myths are made of, and here the colorful legend is almost certainly apocryphal). Virchow was a champion of the Theodor Schwann’s and Matthias Schleiden’s Cell Theory – omnis cellula e cellula (“all cells come from cells”) – and his eponyms include cells in the bone and the cornea, a law about the origin of cells, a metastatic cancerous supraclavicular node, and the triad of factors that predispose to vascular thrombosis. Yet he rejected the Germ Theory of Disease and Darwin’s Theory of Evolution. It is generally considered that Virchow believed that the color change of macroscopic human tissue from brown to violaceous blue‐black after the application of iodine and sulphuric acid indicated either cellulose or starch. 17 Thus, when he observed that small round deposits in the nervous system reacted to the sequential application of iodine and sulphuric acid with this color change, he named the deposits “corpora amylacea”, derived from the Latin word amylum – amylon, , in Greek. – meaning starch or fine meal. But, nowadays, it is almost impossible to know exactly whether Virchow thought that the material in question that stained blue‐black in the human brain, was cellulose‐like or starch‐like because nomenclature and chemical connotations have changed since Schleiden’s and Virchow’s time, and a precise literal translation into English of passages in German are impossible. 18 The word amyloid was originally used by the botanist Matthias Schleiden in 1838 to describe the amylaceous, or starch‐like, constituent of plants 19 that turned out to be cellulose. Johann Heinrich Meckel von Hemsbach (Fig. 2D), the last scientist in the renowned Meckel dynasty (Fig. 3), 20 and Virchow’s successor as Prosector at Charité Hospital in Berlin and predecessor as Chair of Pathological Anatomy at the University of Berlin, preferred the designation cholesterin. Von Hemsbach’s terminology only adds to the confusion that results from the proliferation of amyloid aliases in the literature, which we have already briefly noted (and will expound further), that comprise lardaceous, bacony, waxy, pituitous, starch, cellulose, and scrofulous.
FIG 3.

The Meckel family tree with the 5 anatomist/pathologists and their spouses. Reproduced with permission from 20 Neurosurgery 2010; 66:758‐771.
The current essay will commence with a brief review of selected publications from the 18th and 19th centuries in which were reported clinical cases of hepatomegaly secondary to an infiltration, and the attempts to define the nature of the infiltrating material. These early reports will be followed by a description of the work of George Budd (Fig. 4), who gave perhaps the clearest descriptions and analysis of the condition in the first half of the 19th century, in successive editions 21 , 22 , 23 of his comprehensive textbook of liver disease (Fig. 5). Section III, that dealt with “Scrofulous enlargement of the liver, and other kindred states,” increased from 10 pages in the 1845 1st edition, 21 to 25 pages by 1857 when the 3rd edition 23 was published. Summaries of the clinical histories and presentations of Budd’s cases are included below with references to his accurate analyses of the proteinaceous and not fatty nature of the infiltration, in which assays he was assisted by a certain Mr. Beale. George Budd’s older brother William – the esteemed pioneer epidemiologist who had discovered the water‐borne transmission of typhoid fever that he also distinguished from typhus – and a nephew, the notoriously sociopathic George Turnavine Budd, nemesis of Arthur Conan Doyle, creator of Sherlock Holmes – were also involved in the amyloid story.
FIG 4.

George Budd. (A) Age 40‐years, at the time of his appointment to King’s College and Hospital, Lithograph by TH Maguire, courtesy of the Wellcome Trustees. (B) Writing at his desk – date unknown – © Royal College of Physicians.
FIG 5.

Title page of the first edition of George Budd’s “On diseases of the liver”, John Churchill, London, 1845.
Early Reports of Amyloidosis
Jeremiah Wainewright
Jeremiah Wainewright (1673‐?1722), a physician and Member of the College of Physicians in London gave perhaps the first detailed description of amyloid infiltration of the liver in his 1722 treatise on the liver 24 (Fig. 6). He wrote: “The liver as it is a glandulous body, is a proper seat for schirrous tumours, which here, as in other parts of the body, are hard tumours, resisting any impression made upon them; and when exquisite, are without pain, tho’at their beginning, before they are confirmed, they will have pain. These tumours frequently arise from the matter of them, being insensibly, and in process of time, accumulated in the liver; tho’ they are likewise the consequences of inflammations, where the thinner parts of the circulating humours being evaporated, the remaining thicker matter became the original cause of a scirrhous tumour; and this, it may be, in the very glands of the Liver.” Wainewright went on to describe a case reported by Francis Glisson (Fig. 7), a physician and Professor of Physics at Cambridge University (1597‐1677). The patient died after suffering with strumous (scrofulous or tuberculous), cervical glands for several years and post‐mortem examination revealed a liver enlarged by “swellings of a clay‐coloured pituitous (mucoid) substance.” To the renowned anatomist, physician and historian of French Medicine, Baron Antoine Portal (1742‐1832) Knight of the Empire and post‐revolutionary physician of kings† (Fig. 8), the substance was reminiscent of bacon and therefore became designated lardaceous. It is believed, however, that Wainewright’s account may be the first clear report of a case of amyloid liver associated with long standing cervical tuberculosis. Although Wainewright undoubtedly deserves his due for having been the first to describe amyloid liver, it seems likely that in 1639 Nicolaus Fontanus (Nicolaes Fonteyn, Nicolao Fontano), a Dutch physician and poet living in Amsterdam, was the first to describe systemic amyloidosis in the autopsy of a young man (with ascites, jaundice, epistaxis and a liver abscess), epitomized by amyloid spleen, 26 known then as white stone‐containing or Sago spleen (sagomilz), because the white nodules in the spleen were reminiscent of sago seeds or pearls, the starchy food that is extracted from the spongy pith of various tropical palms, especially those of Metroxylon sagu, and is a staple foodstuff in New Guinea and the Moluccas. Thomas Bartholin, discoverer of the lymphatic system, likened the sound of incising a wood hard amyloid spleen like cutting through spongy timbers. 27
FIG 6.

Front cover of 2018 paperback version of Jeremiah Wainewright’s 1722 “Anatomical Treatise of the Liver, with the diseases incident to it,” 24 printed by the Gale publishing company from an original a high‐quality copy of a manuscript in the Eighteenth Century Collections Online (ECCO) digital collection of books published in Great Britain in the 18th century.
FIG 7.
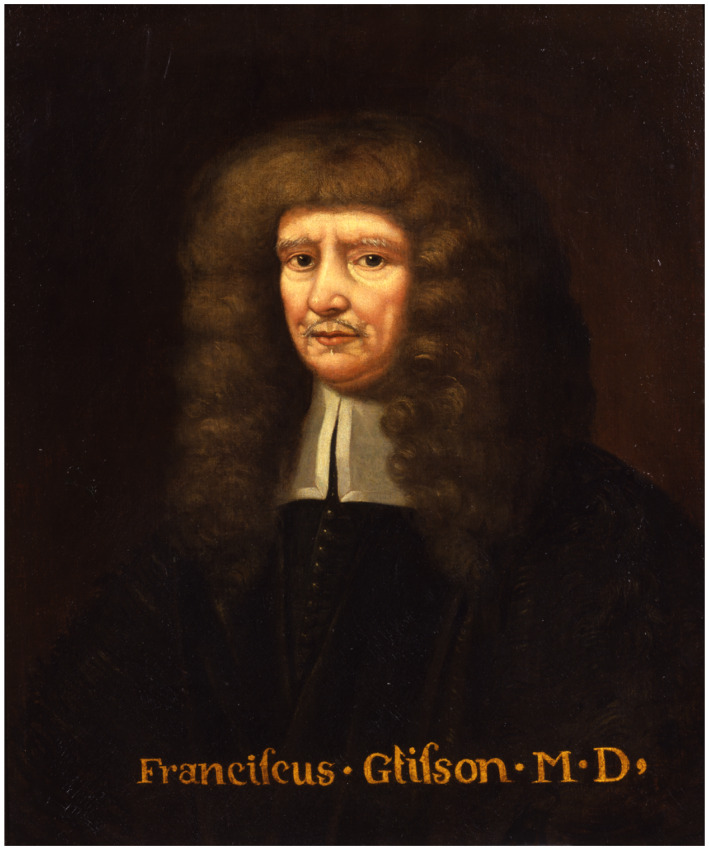
Portrait of Francis Glisson located in the Museum of the Royal College of Physicians. © Royal College of Physicians. It is arguable that this portrait was painted by William Faithorne (c1620‐c1691), who was the artist responsible for the line drawing engraving that is found in the National Portrait Gallery and the Wellcome Institute, because Faithorne was not accustomed to paint in oils.
FIG 8.

Baron Antoine Portal, depicted in a line engraving by J.P. Dupin, Jr., 1782, after A. Pujos 1781. Credit: Wellcome Collection, London.
John Abercrombie
Abercrombie (Fig. 2e), an Edinburgh physician (1780‐1844), was “First Physician to his Majesty in Scotland (William 1V)” and a close friend and medical advisor to Sir Walter Scott. He described the case of a boy aged 11 years who presented with severe tuberculous enlargement of cervical nodes and who died 1 year later with a severe chest infection. Post‐mortem examination confirmed tuberculous infection of the lungs and enlarged lymph nodes in the chest and abdomen. The liver was pale and severely enlarged to fill the whole of the upper half of the abdomen. Abercrombie wrote – “I think this is most frequently observed in young persons of a scrofulous habit, but is occasionally met with at a more advanced age.” He also referred to cases of “pale degeneration of the liver” with a uniform dull yellow colour “closely resembling the colour of impure bees’ wax….., they are chiefly observed when the patient has died of some other affection.” 28
While Abercrombie in Edinburgh was musing on the nature of pale bulky livers, Robert Carswell, Professor of Pathological Anatomy in University College in London, was wrestling with the nature of the pallid hepatomegaly that he observed chiefly in women who had died of the progressive wasting disease that was pulmonary tuberculosis. 29 The prevailing prejudice among pathologists to explain lardaceous disease, was that there was superadded fatty material rather than fatty transformation of the involved organs. But, somehow, the consistency of the affected organ to the probing finger seemed unlike fat. 29
Karl Rokitansky
Baron Karl Freiherr von Rokitansky (1804‐1878), pathologist and philosopher (Fig. 2F), was the Professor of Pathological Anatomy in Vienna. In agreement with his French near‐contemporary Antoine Portal, 30 the renowned Bohemian Viennese pathologist referred to amyloid of the liver as a lardaceous (like bacon‡) infiltration and confirmed its relationship with tuberculosis (scrofula), rickets, syphilis, and medication with mercury. 32 , 33 He described an affected liver, Die speckige leber, as being considerably enlarged, of a doughy consistency – that Carswell had remarked upon 29 – and colored a grayish‐white or greyish red. He noted that the spleen is commonly affected and described concomitant renal disease as Bright’s disease (acute or chronic nephritis).
George Budd
In his highly regarded book, On Diseases of the Liver, 21 , 22 , 23 George Budd (1808‐1882) began his section on Scrofulous enlargement of the liver, and other kindred states, with the two earlier reports by Abercrombie 28 and Portal, 30 respectively, of children who had died with extensive tuberculosis and severe hepatomegaly Accordingly, this section of Budd’s books commences with a statement that enlargement of the liver may occur in association with scrofulous disease of the glands or of the bones, i.e., chronic tuberculous infection, and that the enlargement resembles fatty infiltration in many respects but differs from it in the character of the matter deposited.
Budd notes that Portal gave a detailed description of a post‐mortem of an 8‐year old boy who had died of chronic tuberculous disease with a “liver of prodigious size,” which had a whitish appearance. Sections of the liver exposed to heat, boiling water, or alcohol were “hardened like albumen.” 30
A third, personal case, a child referred by George Budd’s younger brother William, had suffered for several years with tuberculosis of the hip and an “immensely enlarged liver.” Post‐mortem examination showed a pale red colour “mottled by white lines and spots having much the look of bacon rind.” Budd commented that the patient had no fever and no jaundice.
A fourth case, also referred by William Budd, was a woman aged thirty who had a long history of tuberculous disease of the metatarsals of both feet and one ankle joint, and who died from the mechanical effects of massive enlargement of the liver that filled the abdomen and part of the chest and was described at post‐mortem as having the appearance of yellow wax. Chemical analysis of the liver confirmed that the liver was infiltrated with an albuminous material.
Three further cases can be summarised as follows:‐
Case 5 – A male 21 years of age died after a long history of tuberculous bone infection of the left arm, the great toe, the 7th rib, and left lung. His liver was “enormously enlarged” and showed a “waxy appearance” at post‐mortem examination caused by the deposit of a large amount of whitish material shown on analysis to be albuminous. A similar substance was observed in the kidneys.
Case 6 – A male 15 years of age died after a 4‐year history of tuberculous infection of the right hip, “enormous enlargement of the liver and spleen,” and renal failure. At post‐mortem the liver was infiltrated with a greyish material which was albuminous on analysis. Similar material was present in the kidneys.
Budd summarised the hepatic features of the last four personal cases in a very clear manner. All were associated with tuberculosis. The infiltration of the liver by an albuminous substance was whitish and although tough it was not hard, and the cut surface had the appearance of “compact bacon.” Microscopically the foreign material was between and not within the liver cells which continued to function and jaundice‖ was not a feature of the disease.
Case 7 – A male 40 years of age died after a 4‐year history of severe infection of the left kidney and a perinephric abscess. His liver was “enormously enlarged” and post‐mortem examination revealed changes of “precisely the same kind as in the preceding cases.” There was no evidence of tuberculous infection in this case, only chronic infection in the left kidney.
Budd concludes this section of his book with a review of other possible causes of severe hepatic enlargement. He highlights the similarity of the features of scrofulous enlargement with those found in enlarged livers of patients with syphilitic bone disease, particularly those who had been treated with mercury.
In summary, Budd described very clearly the progressive enlargement of the liver associated with chronic infection with tuberculosis, syphilis, or renal infection. He attributed the absence of liver tenderness and pain to the slow pace of hepatic enlargement; he also noted the infrequency of fever and the variable presentation with jaundice and ascites. Budd described the gross and microscopic features of the hepatic infiltration with an albuminous substance now known as amyloid, and he stated that the patients died from a similar infiltration of the kidneys.
Friedrich Theodore von Frerichs
In 1861, Frerichs (1819‐1885), Director and Professor of Medicine (Fig. 9) at the Charité Hospital in Berlin, who gave the first description of familial hepatolenticular degeneration (now known as Wilson disease), summarized the early knowledge and understanding of amyloidosis in a comprehensive chapter headed Waxy, Lardaceous or Amyloid Degeneration of the Liver in the second volume of his book A Clinical Treatise on Diseases of the Liver 34 (Fig. 9), in the frontispiece of which were line drawings of hepatocytes in various stages of waxy or amyloid degeneration (Fig. 10). In the preface, Frerichs apologizes that the second volume of this treatise on liver diseases appeared later than intended, which he attributed to his move from Breslau to Berlin. Furthermore, he expresses the hope that when he has more leisure than his new position in Berlin affords, he will furnish remarks on the general pathology and treatment of the liver.
FIG 9.

Friedrich Theodor von Frerichs. Lithography by P. Rohrbach, 1859, from a photograph by G. Schaue and the title page from the second volume of his Clinical Treatise on Diseases of the Liver, in an English translation by Charles Murchison MD, FRCP, published by the New Sydenham Society in 1861.
FIG 10.

Line drawings of hepatocytes in various stages of waxy or amyloid degeneration, selected from the frontispiece of Frerichs’s 1861 Clinical Treatise on Diseases of the Liver, Volume 2 (see Figure 9). 34 Drawing 3: A group of hepatocytes in which the different stages of the deposit of amyloid matter may be traced – (A) A cell with a distended nucleus; (B) An enlarged cell, uniformly filled in which the nucleus is no longer visible; (C) crushed debris of cells. Drawing 4: Change of color in the cells produced by the addition of solution of iodine. Drawing 5: The same after the addition of solution of iodine and sulphuric acid. Drawing 6: A firm aggregation of hepatic cells covered by solution of iodine.
In the chapter on amyloid of the liver, Frerichs credited Georg Ernst Stahl (1659‐1734), the scientifically controversial and antagonistic German chemist and physician, and Herman Boerhaave (1668‐1738), a Dutch botanist, chemist, Christian humanist and physician – best remembered for his eponymous description of rupture of the esophagus caused by violent vomiting – with early descriptions of hepatic amyloid and suggestions that the cause of the condition was thickened blood leading to infarction and engorgement of the liver. Like Budd, he also credited Antoine Portal, with an early case report, and with the classification of amyloid into “albuminous, gelatinous and mucus varieties.”
Frerichs stated that Rokitansky gave “the first clear account of the essential features of lardaceous degeneration 32 , 33 that Budd 22 had described as “Scrofulous Enlargement of the Liver,” and that Friedreich and Kekulé had reported in 1859 35 that amyloid consisted of deposits of albuminoid proteinaceous material and neither fat nor carbohydrate nor cellulose, as had been previously suggested. Budd, however, had already arrived at the same conclusion in 1852 22 when he deduced after chemical analyses in three cases that “The foreign matter, to which the liver owes its large size is albuminous, and, when not stained by bile is whitish and somewhat glistening.” Moreover, Budd noted that “The matter infiltrating the liver when treated with a solution of iodine, it acquires, like starch, an intense reddish‐yellow color, turning on the addition of sulphuric acid, to a beautiful violet and blue,” and he endorsed Virchow’s point of view concerning nomenclature, namely that the so‐called lardaceous or waxy condition of the liver be recognized as “amyloid degeneration.” However, neither the amyloid appellation nor the interpretation of the violet/blue reaction with iodine and sulphuric acid nor the demise of the term lardaceous, were universally accepted lightly, and especially not by Samuel Wilks Bt (Fig. 2B), who led a rear‐guard lardaceous or bacony counterattack.
William Howship Dickinson (Fig. 11) (1832‐1913), physician at St. George’s Hospital and the Hospital for Sick Children at Great Ormond Street, London, focused his attention on what he alluded to as Waxy, Amyloid or Depurative, i.e., connected with suppuration, Disease affecting the kidneys, 34 , 37 which he described with great clarity in print, and in person at a meeting of The Pathological Society of London in 1869 when he appealed for the creation of a committee of pathologists to decide upon the most suitable name for the condition and to recognize that the substance deposited in organs was proteinaceous material derived from the blood. 38 The Committee on Lardaceous Disease duly met, debated, reported and upheld the term Lardaceous, 39 against which decision Dickinson subsequently railed, 40 and despite the finding that “the waxy liver is unusually poor in oil.” 41 Virchow’s label 17 , 42 eventually prevailed, such was his standing among pathologists.
FIG 11.

William Howship Dickinson. Photograph from his obituary in the British Medical Journal. Reproduced with permission from 36 British Medical Journal 1913;1:141.
The violet blue‐black staining reaction of starch with iodine and sulphuric acid that was discovered by Jean Jaques Colin and Henri‐François Gaultier de Claubry in Gay‐Lussac’s laboratory in Paris, 43 used by Schleiden to detect starches in plants 18 and interpreted by Virchow as detecting a starch‐like (or was it cellulose‐like?) substance, i.e., amyloid, initially in the human brain 17 and later in the liver and other organs afflicted with scrofulous enlargement, turned out to be highly complex and exquisitely dependent on experimental conditions, such as the concentration of the sulphuric acid. Anyway, interpretation of the results with respect to the composition and nature of the target tissues was far from unequivocal.’ 44
The introduction of the metachromatic aniline dyes with their tantalizing property of metachromasia, turned out to be a boon to the discipline of histopathology and to the field of amyloid studies, and for the textile and fashion enterprises. Metachromasia, refers to the phenomenon in which certain tissue constituents reacting with a single dye show different colors from that of the dye solution; apparently, the binding of dye molecules by certain substances in the tissues, so‐called chromotropes, brings dye molecules close enough together to form dimeric and polymeric aggregates that have different light absorption spectra from the parent monomeric dye molecules. 45 In 1856, in a failed attempt to synthesize quinine for the treatment of malaria, 18‐year‐old William Henry Perkin, in an apartment of his London East End home, 46 serendipitously synthesized the world’s first aniline dye that he called aniline purple (on account of its intense purple color), which was later changed to mauve (Mauvine) after the name of French flower, Following the runaway commercial success of Mauveine, a veritable rainbow of aniline dyes followed produced from cheap synthetic aniline by the emerging massive German dye industry, which the Allies broke down after the Second World War because of the use of slave labor in Auschwitz and other Nazi concentration camps.
Meanwhile, in 1875, three eminent European pathologists, André‐Victor Cornil in Paris, Richard Heschl in Vienna, and Rudolf Jürgens in Berlin, almost simultaneously published novel staining methods for amyloid, using the new aniline dyes: methyl violet, violet ink (aniline violet), and iodine violet (a compound of methyl iodine and aniline, known as dahlia), respectively. 45 The publication in 1874 by J. André, of the use of aniline red and aniline blue to stain the outer segments of retinal rods yellow or green, respectively 47 that predicted the breakthrough revolutionary durable and non‐destructive amyloid staining, was seemingly overlooked. Notwithstanding. the stunning success of the new staining methods for amyloid sounded the death knell for the time‐honored iodine‐sulphuric acid technique. However, before the advent of structural techniques (illustrated in Fig. 1A and C) to identify and characterize amyloid, one last, even more colorful development occurred in the amyloid story that endures to this day, namely Congo Red staining. 48
In 1883, an obscure young chemist working in the dyestuff chemical laboratory of Friedrich Bayer in Elberfeld, Germany, Paul Böttiger, discovered a brilliant red dye that could stain textiles directly without the usual need for a separate permanent fixative to the fabric. Yet Bayer was disinterested; so Böttiger eventually sold his patent elsewhere. The Berlin manufacturer, Actiengesellschaft für Anilinfarbenfabrikation (AGFA), began selling the dye in 1885. Their exotic tradermark, Congo red was seemingly inspired by a newsworthy current geopolitical diplomatic trade conference in Berlin concerning the Congo River basin. The term “Congo” in the trademark was solely a marketing ploy, there being no Central African connection.
As with the myriad aniline dyes, Congo red was used as soon as 1886 to stain tissue, 48 but it was only in 1922 that the avidity for amyloid fibrils was appreciated (Fig. 1B, above right), and especially the characteristic apple‐green birefringence under polarized light (Fig. 1B, below right). Congo red remains the dye of choice for amyloid diagnosis.
George Budd and Family
Cook and others have published detailed histories of George Budd’s remarkable family (Fig. 12) and its academic achievements. 49 , 50 , 51 , 52 , 53
FIG 12.

Coat of Arms of the Budd family.
Budd was born in England in 1808, in the southwest County of Devon, in North Tawton, a town that dates from Roman times, at or near the site of an ancient Celtic Druidic sanctuary. George’s father, Samuel (1772‐1841), was a local surgeon and general practitioner, whose family of 9 sons and one daughter were all home‐schooled. George and four of his brothers studied at Cambridge University, where all were Wranglers, an arcane term that indicates having obtained first‐class honors in the Mathematics Tripos bachelor examination. In addition, six of George’s siblings also became physicians. George was a remarkably gifted mathematician and achieved “Third Wrangler” status (third position) in the Cambridge mathematical tripos examination in 1831. This achievement can be measured against the attainments of people like William Bragg (3rd), Bertrand Russell (7th), and John Maynard Keynes (12th). Bachelor examinations at Cambridge University took the name Tripos, allegedly from the three‐legged stool on which a candidate sat for cross‐examination and to deliver a satirical speech at the degree ceremony.
George’s younger brother William, who was born in 1811, and who studied in Paris, London, and Edinburgh, is perhaps the most widely recognized member of the family for his outstanding work on typhoid fever and cholera and for his fundamental work in improving sewers and water supplies. Many people have recognized him as the founder of public health and preventive medicine.
George Budd is now recognized as perhaps the leading hepatologist of the 19th century, and he is chiefly remembered for the first description of what he described as an “extremely rare” adhesive inflammation and obstruction of the hepatic veins in a man of 52 years of age, which he attributed to the drinking of large quantities of gin. 22 In 1898, Hans Chiari (1851‐1916), an Austrian pathologist and colleague of Rokitansky in Vienna, published the first comprehensive patient series of the condition, 54 which later became known by the eponym Budd‐Chiari syndrome.
Notably both George, who studied in Paris and at the Middlesex Hospital, London, and William, were elected as Fellows of the Royal Society in 1836 and 1871, respectively. Both were appointed as visiting physicians to the floating Dreadnought Seaman’s Hospital (Fig. 13), at Greenwich on the River Thames, between 1837 and 1840. George resigned after his appointment as Professor of Medicine at the recently opened King’s College Hospital in Portugal Street,¶ Holborn, and William also resigned after a severe illness with the Rickettsial infection typhus. He transferred to the Bristol Royal Infirmary. The two brothers continued to correspond on clinical matters, and William would send complex patients to George for diagnosis and treatment.
FIG 13.

Woodcut showing the Dreadnought hospital ship on which Budd served as visiting physician from 1837 to 1840. Reproduced with permission of the Seafarers’s Hospital Society.
George Budd’s work in Greenwich included a detailed study of cholera in collaboration with the polymath, Mr. George Busk,§ – surgeon, parasitologist, zoologist, and paleontologist. 55 Most important, Budd explored the reasons for a rise in the incidence of scurvy during the 19th century, almost a 100 years after results of James Lind’s conclusive prospective randomized trial on HMS Salisbury showed the anti‐scorbutic benefits of fresh citrus fruit. Budd’s study resulted in clear rules for the prevention of the disease, resulting in a document (Fig. 14) that was circulated to all ship owners and captains of merchant ships. His interests were very wide ranging. Not only did he publish his clinical experience in two major books – On diseases of the liver 21 , 22 , 23 and On the organic diseases and functional disorders of the stomach 56 but also a series of remarkable papers in the London Medical Gazette, which gave much evidence for the presence of “obligatory” micronutrient substances in normal diet the absence of which would lead to well defined deficiency diseases. 57 , 58 These papers were published at a time when studies of the physiology of nutrition were mostly concerned with detailed nutritional aspects of proteins, carbohydrates and fats and Budd’s revolutionary observations on other possible important substances in normal diets were virtually ignored. More than 50 years before their recognition as vitamins A, C, and D, Budd concluded from his studies on patients with corneal ulceration, scurvy, and rickets that their etiology might be related to the dietary deficiency of ‘essential micronutrient’ factors in the diet.
FIG 14.

Poster published by the Dreadnought Seaman’s Hospital Society about 1840 – contain advice for prevention of scurvy in seafarers; this was almost certainly derived from George Budd’s researches, from. 52
In summary, George Budd deserves special recognition for his wide‐ranging work on nutrition, liver disease and gastrointestinal disease. The clarity of the publications of his studies on amyloid disease is typical of his work which was so highly praised in his obituaries. For his book On Diseases of the Liver, for example, he was described as “….the first writer who, for nearly half a century, had systematised the practical knowledge of liver diseases, and he for the first time gave this knowledge the form which it has retained for nearly forty years.” 50 Similar sentiments were expressed in the Proceedings of the Royal Society of London. 59
There is a final curious history relating to amyloid disease and the Budd family. William Budd had two sons and five daughters. Both sons became medical practitioners, Arthur James Budd (1853‐1899 ) at St Bartholomew’s hospital in London, and George Turnavine Budd (1856 – 1889) at Edinburgh University. Both young men were renowned rugby football players (Fig. 15), and Arthur won five caps playing for England. G. Turnavine Budd was born at 22 Park Street in Bristol, now numbered 89, later the site of the now defunct Jaimie Oliver’s Italian Restaurant, and Blackwell’s Bookshop.
FIG 15.

Edinburgh Wanderers Rugby Team of 1876‐1877, with George Turnavine Budd (2nd from the right, back row), who became captain 1879‐1880. 70
George Turnavine Budd befriended Arthur Conan Doyle and the two men both gained medical qualification in Edinburgh in 1880. Conan Doyle later commented on Budd’s rugby prowess but stated that he was”… rather handicapped by the berserk fury with which he would play.” 49 After working together for a short time in general practice (Fig. 16) the relationship between the two men ended in 1882 following the onset of George T. Budd’s unprovoked hostility to Doyle; this was one of the factors responsible for Conan Doyle giving up his medical practice in favor of a literary career and is well documented in two of his biographical books. (George Turnavine Budd’s name is given as ‘Cullingworth’ in these biographies.) 60 , 61
FIG 16.

Blue wall plaque in Plymouth, England, marking the site at which George Turnavine Budd and Arthur Conan Doyle were partners in a brief and unhappy medical practice. This is a photograph of a plaque on a wall in Plymouth, UK.
George T. Budd later published two papers on amyloid disease using the name ‘George Budd Jun.’ instead of his full name George Turnavine Budd 62 , 63 In these papers, he concluded that amyloid might be glycogen, a starchy substance “concerned commonly with nutrition in the body” and that through some undefined process it might become exceedingly stable and remain in the tissues blocking the nutrient arteries and “packing in its substance the remains of attenuated tissues”, i.e., protein. With this improbable hypothesis., he explains why the amyloid material turns blue‐black with iodine and sulphuric acid like starch and yet analysis shows nitrogen typical of protein.
The use of the name George Budd Jun. and the complete lack of reference to his uncle’s work on the protein nature of amyloid is unexplained. It is, however, noteworthy that George Turnavine Budd died at the young age of 34‐years (1855‐1889) having suffered possible dementia for some months before his death. Pearce has suggested from his study of GTB’s erratic behaviour, dementia, and early death a possible diagnosis of neurosyphilis. 64 Perhaps George T’s behavior earned the Illustrious and Industrious Budd family the questionable epithet Notorious. 51
In summary George Budd was a member of an outstanding medical family. His practice was wide‐ranging and his academic ability of a very high standard. The clarity of his observations on amyloid disease was a typical example of his work in many fields.
Series Editor’s Postscript
It is a pleasure and a privilege to publish this essay on Amyloidosis by the distinguished Emeritus Professor of Surgery at King’s College Hospital (KCH) London, and dear friend, Ted Howard.
The topic of amyloidosis is still something of a riddle wrapped in a mystery inside an enigma, despite the enormous advances that have been made in the molecular and cellular pathobiology of this protean entity of protein misfolding. 2 , 4 , 6 , 7 Amyloid protein is evident in such diverse conditions as plaques in the brain of Alzheimer sufferers – which incidentally were the first lesions to be recognized as exhibiting pathognomonic apple‐green birefringence when viewed under polarized light, 65 various syndromes associated with chronic hemodialysis, 66 and the now relatively uncommon secondary cases resulting from chronic infections, especially tuberculosis (and other chronic inflammatory states) that introduce the history with which Ted’s essay begins. The bewildering and burgeoning array of primary amyloidoses that result from inherited and acquired genetic aberrations, 2 as well as from plasma cell dyscrasias, myelomas, and other malignancies, round off the amyloid catalog; and include explanations for the pathogenesis of this tantalizing complex multiorgan disease. 4
The history of amyloid is a perfect topic for the current series, as it intrigued and challenged a host of famous physicians, anatomists, pathologists and medical scientists through the ages, provoking controversy and semantic dissent. 8 , 67 This current presentation also highlights the invention of chemicals that transformed life in the 19th and 20th centuries in advanced nations, and the invention of novel laboratory techniques. Who would have guessed that the vast aniline dye industry and its myriad spin‐offs (too numerous to discuss here), resulted from the serendipitous discovery by an English teenager tinkering in his East London apartment as he tried to synthesize quinine for the treatment of malaria? And, of course, this essay is the perfect vehicle for its author to indulge his fascination with George Budd, whose contributions to the understanding of amyloidosis were paramount, 49 , 50 who wrote the first modern textbook of hepatology in English, 21 , 22 , 23 and whose family’s biography 51 , 52 could rival Downton Abbey and other television series or movie melodramas.
At first sight, it might seem surprising that a renowned professor of surgery should be attracted to an obscure medical condition and a mid‐19th century physician from Devon. Yet, somehow, it seems axiomatic that academic surgeons are devotees of medical history especially pertaining to the evolution of surgical techniques, as exemplified by the essay in this series on the surgery of portal hypertension by Mississippi surgeons Michael Henderson, MD, and Christopher D Anderson, MD (Clinical Liver Disease 2020; 15; S52‐S63).
Ted Howard graduated in Medicine in 1960 from KCH Medical School and obtained the postgraduate qualifications of Master of Surgery and Fellow of the Royal College of Surgeons. An Honorary Fellowship of the Royal College of Surgeons in Edinburgh was awarded in recognition of his achievements in surgery and research, as well as two Hunterian Fellowships at the Royal College of Surgeons and a Fellowship of the Royal College of Physicians. Ted was appointed at KCH as a General and Pediatric Surgeon with a special interest in liver disease, where he was instrumental in the introduction of Kasai’s porto‐enterostomy into the United Kingdom, with comparable survival patterns to those in Japan. 68 In this context, Ted gave invaluable advice for the writing of an earlier historic essay on the surgery of biliary atresia. 69 (See also the contribution about the timing of the Kasai operation by pediatric hepatologists Mary Tessier and Ben Shneider [Clinical Liver Disease 2020; 15: S3‐S7].)
Ted’s appetite for medical history was whetted as he explored the historical background to his surgical thesis. A detailed interest in the life and work of George Budd began later, during the preparation of a lecture on the history of KCH. Among the biographical details available of many of the staff from the time of the opening of the first building in 1839, in a converted London workhouse in Portugal Street (that is now part LSE), were those of George Budd, including the discovery, in the archives, of a photograph of this remarkable Professor of Hepatology. Finally, among several other related coincidences, a member of a school governor committee of which Ted was the Chairman, asked if he knew of a physician named Budd because, it turned out, he was descended from Diana, one of William Budd’s four daughters.
Footnotes
Baronet.
Resulting from his close relationship with Emperor Louis XVIII, not only was Portal named le premier médecin du roi but additionally l’Académie Nationale de Médecine was created, of which he was the lifelong president. 25
In characteristic outspoken fashion, Virchow rejected the term “lardaceous,” on gastronomic grounds, because he felt that those who favored it could not be true epicures of good bacon. 31
Which Budd encountered on occasion, and it had been observed by others.
Where the London School of Economics (LSE) was subsequently located.
In Great Britain, surgeons are traditionally known by the title “Mister” and not “Doctor”, even though they are medically qualified practitioners.
References
- 1. Cohen AS, Calkins E. Electron microscopic observations on a fibrous component in amyloid of diverse origins. Nature 1959;183:1202‐1203. [DOI] [PubMed] [Google Scholar]
- 2. Benson MD, Buxbaum JN, Eisenberg DS, et al. Amyloid nomenclature 2020: update and recommendations by the International Society of Amyloidosis (ISA) nomenclature committee. Amyloid 2020;27:217‐222. [DOI] [PubMed] [Google Scholar]
- 3. Takahashi M. Pathological study on amyloidosis. Scanning electron microscopic observation of amyloid‐laden mouse liver. Acta Path Jap 1977;27:809‐822. [DOI] [PubMed] [Google Scholar]
- 4. Merlini G, Bellott V. Molecular mechanisms of amyloidosis. New Engl J Med 2003;349:583‐596. [DOI] [PubMed] [Google Scholar]
- 5. Shirahama T, Cohen AS. High resolution electron microscopic analysis of the amyloid fibril. J Cell Biol 1967;33:679‐708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. New Engl J Med 1997;337:898‐909. [DOI] [PubMed] [Google Scholar]
- 7. Hazenberg BPC. Amyloidosis: a clinical overview. Rheum Dis Clin N Am 2013;39:323‐345. [DOI] [PubMed] [Google Scholar]
- 8. Kyle RA. Amyloidosis: a convoluted story. Br J Haematol 2001;114:529‐538. [DOI] [PubMed] [Google Scholar]
- 9. Reuben A. The legend of the lardaceous liver. Hepatology 2004;40:763‐766. [DOI] [PubMed] [Google Scholar]
- 10. Keers RY. Pulmonary Tuberculosis: A Journey Down the Centuries. London: Balliière Tyndall; 1978:6‐19. [Google Scholar]
- 11. Koch HHR. Die Aetiologie der Tuberculose. Berliner Klinische Wochenschrift 1882;19:221‐230. [Google Scholar]
- 12. Hirsch A. A Handbook of Geographical and Historical Pathology (translated from the 2nd German edition by Creighton C). London: The New Sydenham Society; 1885:2: 604‐641. [Google Scholar]
- 13. Osler W. The Principles and Practice of Medicine. New York: D. Appleton and Company; 1892:184‐256. [Google Scholar]
- 14. Grzybowski S, Allen EA. History and importance of scrofula. Lancet 1995;346:1472‐1474. [DOI] [PubMed] [Google Scholar]
- 15. Wilks S. Cases of lardaceous disease and some allied affections. With Remarks. Guy’s Hospital Rep 1856;2:103‐132. [Google Scholar]
- 16. Pearce JMS. Sir Samuel Wilks (1824‐1911): ‘The Most Philosophical of English Physicians’. Eur Neurol 2009;61:119‐112. [DOI] [PubMed] [Google Scholar]
- 17. Virchow R. Über eine in Gehirn und Ruckenmark des Menschen aufgefundene Substanz mit der chemischen Reaction der Cellulose. In Virchow’s Archiv für Pathologische Anatomie und Physiologie und für klinische Medicin, Berlin 6; 1854:354‐368. [Google Scholar]
- 18. Puchtler H, Sweast F. A review of early concepts of amyloid in context with contemporary chemical literature from 1839 to 1859. J Histochem Cytochem 1966;14:123‐134. [DOI] [PubMed] [Google Scholar]
- 19. Schleiden MJ. Einige Bermerkungen über den vegetabilischen Faserstoff und sein Verhältnis zum Stärkemehl. Series 2. Ann. Physik 1838;43:391‐397. [Google Scholar]
- 20. Janjua RM, Schultka R, Goebbel L, Pait TG, Shields CB. The Legacy of Johann Friedrich Meckel the Elder. (1724‐1774): a 4‐generation dynasty of anatomists. Neurosurgery 2010;66: 758‐771. [DOI] [PubMed] [Google Scholar]
- 21. Budd G. On Diseases of the Liver. London: John Churchill; 1845. 246‐255. [Google Scholar]
- 22. Budd G. On Diseases of the Liver. 2nd ed. London: John Churchill; 1852:304‐329. [Google Scholar]
- 23. Budd G. On Diseases of the Liver. 3rd ed. London: John Churchill; 1857:312‐316. [Google Scholar]
- 24. Wainewright J. An Anatomical Treatise of the Liver with the Diseases Incident to It. London: James Lacy and John Clarke; 1722:28‐30. [Google Scholar]
- 25. Ganière P. Baron antoine portal, perpetual president of the académie royale de médecine. Bull Acad Natl Med 1966;150:539‐545. [PubMed] [Google Scholar]
- 26. Fontano N. Responsionum & Curationum Medicinalium. Book One. Amsterdam, The Netherlands: Joannis Janssonii; 1639. [Google Scholar]
- 27. Bartholini T. Historarium Anatomicarum Rariorum. Centuria I et II. Copenhagen, Denmark: Typis Academicis Martzani sumptibus Petri Hauboldt; 1654. [Google Scholar]
- 28. Abercrombie J. Researches on Diseases of the Stomach, the Intestinal Canal, the Liver and Other Viscera of the Abdomen. 3rd ed. Albemarle Street, London: John Murray; 1837. Simple enlargement of the liver without change of texture. 333‐334. [Google Scholar]
- 29. Carswell R. Pathological Anatomy: Illustrations of the Elementary Forms of Disease. Fasciculus 11. London: Longman, Orme, Brown, Green and Longman; 1837. [Google Scholar]
- 30. Portal A. Observations sur La Nature et le Traitement des Maladies du Foie. Paris: Caille et Ravier; 1813: 93‐94. [Google Scholar]
- 31. Virchow R. Lecture XVII. Amyloid degeneration delivered in the Pathological Institute of Berlin on April 17, 1858. In: John Churchill Chance F. (trans). Cellular Pathology as Based Upon Physiological and Pathological Histology. London, UK; 1860. [Google Scholar]
- 32. Rokitansky C. Handbuch der speciellin pathologischen. Vienna Braumuller und Seidel 1842;311‐312. [Google Scholar]
- 33. Rokitansky C. A Manual of Pathological Anatomy. London: Printed for the Sydenham Society; 1849; Vol. 2:121‐122. [Google Scholar]
- 34. Frerichs FT. A Clinical Treatise on Diseases of the Liver. London: The New Sydenham Society; 1861; Vol. 2:167‐206. [Google Scholar]
- 35. Friedreich N, Kekule A. Zur Amyloidfrage. Arch Pathol Anat Physiol Klin Med 1859;16:50‐65. [Google Scholar]
- 36. Obituary: William Howship Dickinson, M.D.Cantab., F.R.C.P.Lond. Br Med J 1913;1:141. [Google Scholar]
- 37. Dickinson WH. Illustrations of the waxy, amyloid or depurative disease as affecting the kidneys. Trans Path Soc Lond 1868;19:273‐274. [Google Scholar]
- 38. Dickinson WH. Lardaceous disease of the kidney consequent upon abscess of the ovary. Trans Path Soc Lond 1869;20:435‐439. [Google Scholar]
- 39. Report of the committee on lardaceous diseases. Trans Path Soc Lond 1871;22:1‐12. [Google Scholar]
- 40. Dickinson WH. Address on lardaceous disease. Trans Path Soc London 1879;30:511‐512. [Google Scholar]
- 41. Gairdner WT. On some points in the pathology of the liver: with seven analyses by Dr James Drummond. Mon J Med 1854;18:393‐399. [Google Scholar]
- 42. Virchow R. Cellular Pathology (translated from German into English by Chance F). London: John Churchill; 1860:368. [Google Scholar]
- 43. Colin JJ, Gaultier de Claubry HF. Sur les combinaisons de l'iode avec les substances végétales et animales. Ann Chimie 1814;90:87‐100. [Google Scholar]
- 44. Aterman K. A historical notes on the iodine‐sulphuric acid reaction of amyloid. Histochemistry 1976;49:131‐143. [DOI] [PubMed] [Google Scholar]
- 45. Aterman K. A pretty a vista reaction for tissues with amyloid degeneration. J Hist Med Allied Sci 1976;31:431‐447. [DOI] [PubMed] [Google Scholar]
- 46. Mauve GS. How One Man Invented a Color that Changed the World. New York: WW Norton and Company; 2001. [Google Scholar]
- 47. André J. L'emploi de l'hydrate de chloral en histologie. J Anat Physiol Paris 1874;10:96‐97. [Google Scholar]
- 48. Steensma DP. “Congo Red”. Out of Africa? Arch Pathol Lab Med 2001;125:250‐252. [DOI] [PubMed] [Google Scholar]
- 49. Cook GC. George Budd FRS (1808‐1882): pioneer gastroenterologist and hepatologist. J Med Biogr 1998;6:152‐159. [PubMed] [Google Scholar]
- 50. Budd SJA. Budd, George (1808‐1882). Dictionary of National Biography 1885‐1900, 1886; 7:219. London. Oxford University Press; 1886. [Google Scholar]
- 51. Crisp B. The Budd family of Devon. Hist Med 1970;2:13‐16. [Google Scholar]
- 52. Oswald NC. The Budds of North Tawton. A medical family of the 19th Century. Rep Trans Devon Assoc Advancement Sci Literature Art 1985;117:139‐150. [PubMed] [Google Scholar]
- 53. Reuben A. illustrious, industrious, and perhaps notorious. Hepatology 2003;38:1065‐1069. [DOI] [PubMed] [Google Scholar]
- 54. Chiari H. Erfahrungen über Infarktbildungen in der Leber des Menschen. Zeitschrift für Heilkunde, Prague 1898;19:475–512. [Google Scholar]
- 55. Cook GC. George Busk FRS (21807‐1886), 19th‐century: surgeon, parasitologist, zoologist and paleontologist. J Med Biography 1997;5:88‐101. [DOI] [PubMed] [Google Scholar]
- 56. Budd G. On the Organic Diseases and Functional Disorders of the Stomach. London: John Churchill; 1855. [Google Scholar]
- 57. Hughes RE. George Budd (1808‐1882) and nutritional deficiency diseases. Med Hist 1973;17:127‐135. 10.1017/S002572730001841X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Budd G. Lectures on the Disorders Resulting From Defective Nutriment. London Medical Gazette; 1842;2:632‐636; 712‐716; 743‐749; 825‐831; 906‐915.23. [Google Scholar]
- 59. Paget JD. George Budd. Proc R Soc London 1882;34:i‐iii. [Google Scholar]
- 60. Doyle AC. The Stark Munro Letters; reprinted by 1st World Library – Literary Society, 2004, PO Box 2211, Fairfield, IA 52556. 1895. [Google Scholar]
- 61. Doyle AC. In Memories and Adventures and Western Wanderings. Newcastle upon Tyne: Cambridge Scholars Publishing Classic Texts; 2009:39‐43. 1924. [Google Scholar]
- 62. Budd G. Amyloid degeneration. Br Med J 1879;1:659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Budd G. Amyloid degeneration. Lancet 1880;115:322‐324, 487. [Google Scholar]
- 64. Pearce DN. The illness of Dr George Turnavine Budd and its influence on the literary career of Sir Arthur Conan Doyle. J Med Biogr 1995;3:236‐238. [DOI] [PubMed] [Google Scholar]
- 65. Divry P, Florkin M. Sur les proprietés optiques de l'amyloïde. CR Société de Biologie (Paris) 1927;97:1808‐1810. [Google Scholar]
- 66. Kleinman KS, Coburn JW. Amyloid syndromes associated with hemodialysis. Kidney Int 1989;35:567‐575. [DOI] [PubMed] [Google Scholar]
- 67. Doyle L. Lardaceous disease: some early reports by British authors (1722‐1879). J Roy Soc Med 1988;981:729‐731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Howard ER, MacLean G, Nio M, Donaldson N, Singer J, Ohi R. Survival patterns in biliary atresia and comparison of Quality‐of‐Life of long‐term survivors in Japan and England. J Pediatr Surg 2001;36:892‐897. [DOI] [PubMed] [Google Scholar]
- 69. Reuben A. The sensei of Sendai: correcting the uncorrectable. Hepatology 2003;37:952‐955. [DOI] [PubMed] [Google Scholar]
- 70. http://www.cliftonrfchistory.co.uk/other/gtbudd/gtbudd.htm


