Short abstract
Content available: Audio Recording
Listen to an audio presentation of this article.

Toni Herta

Ulrich Beuers
To quote* * Johann Wolfgang von Goethe (1749 [Frankfurt a.M.]‐1832 [Weimar]; Figure 1).
FIGURE 1.

Statue of Johann Wolfgang von Goethe, by sculptor Fritz Schaper (1841–1919), located in the Grosse Tiergarten, Ebertstraße 18, Berlin, Germany. Johann Wolfgang von Goethe was a poet, playwright, novelist, scientist, statesman, theater director, and critic. His works include plays, poetry, literature, and aesthetic criticism, as well as treatises on botany, anatomy, and color. Photograph credit: René & Peter van der Krogt, Available at: https://statues.vanderkrogt.net. Accessed March 24, 2022.
Geschichte schreiben ist immer eine bedenkliche Sache. Denn bei dem redlichen Vorsatz kommt man in die Gefahr, unredlich zu sein, ja, wer eine solche Darstellung unternimmt, erklärt im Voraus, dass er manches ins Licht, manches in den Schatten rücken wird. (“Writing history is always a questionable thing. Despite best intentions one runs the risk of being unbalanced; indeed, whoever undertakes such a venture declares in advance that he will cast some in the light and some in the shadow.”) Goethe, author and polymath, was considered by many to be the most important writer in the German language and one of the most important thinkers in Western culture.
Jaundice (“Icterus“) has attracted the attention of physicians and researchers for more than 2500 years, as documented on clay tablets from Bronze Age Mesopotamia 1 and repeatedly in the Old Testament. 2 The ancients related jaundice, the yellow discoloration of eyes and skin (Figure 2), 3 to impaired drainage of bile—an entity termed constipation (émpraxis, ἔμφραξις) of the liver or liver obstruction, by the Byzantine physician Alexander Trallianus (525–605 CE) and others, 4 even though little was known about the underlying fundamental pathophysiological mechanisms until the beginning of the 20th century. At any rate, because bile is a “hidden” secretion and sampling would require access to the abdominal cavity and its contents, knowledge about bile and its yellow pigment, bilirubin, lagged behind our understanding of other body fluids, such as urine and saliva, and their components. 5 This article reviews historical sources and studies of jaundice, from the observations and myths of the ancient world to the experimental findings of the 20th and early 21st centuries. Considering the mountain of outstanding contributions to this topic over the centuries, this overview will inevitably be incomplete with respect to accreditation. At the outset, we therefore apologize to those esteemed authors if we have not cited (m)any of the excellent reports of their discoveries.
FIGURE 2.
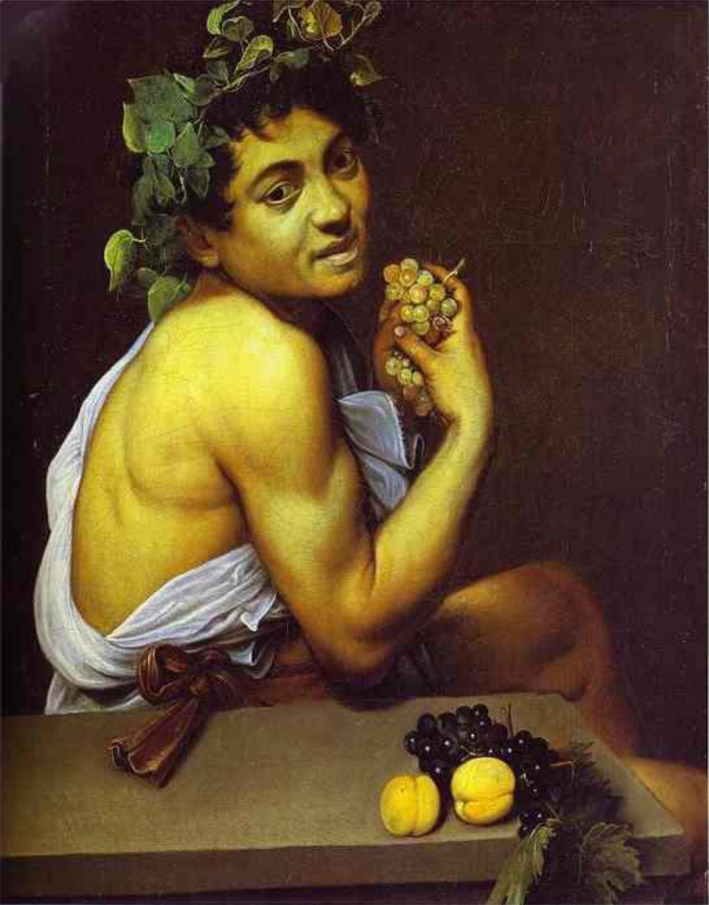
Self‐portrait as sick Bacchus (Bacchino Malato), oil on canvas, painted by Michelangelo Merisi Caravaggio, 1594 (Galleria Borghese, Rome, Italy). Bacchus, the god of agriculture and wine, depicted with jaundice, a yellow tint of skin and sclera, which matches those of the fruits on the table in front of him. In 1592, Caravaggio spent 6 months in the hospital, most likely with acute viral hepatitis from which he finally recovered. During his time in the hospital he had seen chronic alcoholics, jaundiced and dying of liver failure as a result of cirrhosis or alcoholic hepatitis, an impression that he processed with this portrait of a jaundiced Bacchus. Reproduced with permission from Journal of the Royal Society of Medicine. 3 Copyright 2007, Royal Society of Medicine.
THE EURASIAN GOLDEN ORIOLE
The word icterus is a Latinized form of the Greek ίκτερος ikteros, which to the ancient Greeks signified both the yellow discoloration of the jaundiced patient and a small bird with golden‐yellow plumage, the colorful Old World passerine (i.e., perching) Eurasian golden oriole 6 , 7 (Figure 3). Oriolus oriolus, the binomial nomenclature for Old World golden orioles, is derived phonetically from the Latin aureolus for gold. In medieval England, the oriole was called a woodwele, a name derived onomatopoeically from its song. † †
FIGURE 3.

Oriolus oriolus (Eurasian golden oriole). Drawing by Magnus von Wright, 1929. To hear the song of the golden oriole, go online to https://m.youtube.com/watch?v=_oJZ_BhZB48. Reproduced with permission from Svenska faglar efter naturen och pa sten ritade. 7 Copyright 1929, Förlaget Svenska Fåglar.
The term jaundice has evolved from the Old French jaunisse (modern jaunise)—which itself comes from jaune, meaning “yellow”—by the subconscious insertion of the sound “d” to facilitate pronunciation. It was thought that jaundice, described as “when the body is yellow, yellow the face, and the flesh is trembling” 8 (Figure 2), could be cured by having the icteric patient gaze at a golden oriole. The often deadly disease underlying the jaundice would then mysteriously be transferred from the patient to the hapless bird. 6 This article explains why the golden oriole is not threatened with extinction anymore, and its fluting birdsong, a pleasurable weela‐wee‐ooo or or‐iii‐ole (contrasted with its screeching call), can still be enjoyed nowadays. ‡ ‡ Whereas the Greeks were quite unambiguous when describing icterus and its avian cure, not so were the authors of the Old Testament and the (Babylonian) Talmud. § § Here too, however, the most well‐known cure was avian, but instead of telemedicine, that is, gazing at the bird from afar, one (or more, as needed) of the ill‐fated Columbidae family in this pigeon ¶ ¶ remedy (or segula) was placed on the patient's umbilicus to draw out the yellowness, 9 invariably leading to the demise of the bird and one hopes the survival of the patient, although this was not always assured. 9 Moreover, it is not clear whether ירקון Yerakon, the Biblical Hebrew word usually taken to mean “yellow,” in fact denoted a greenish pallor, 2 as in the anemia of young women called the “Disease of Virgins” by the 16th‐century German physician Johannes Lange. This same pale affliction was coined in 1615 as chlorosis (the “green sickness”) by Montpellier Professor of Medicine Jean Varandal, from the Greek χλωρός chloros, meaning greenish yellow. The renowned English physician Thomas Sydenham (1624–1689) considered chlorosis to be a hysterical disease, yet it became fashionably common among Victorian young women.
Other unpalatable Talmudic treatments for jaundice included drinking ass's urine, eating the flesh of a donkey, drinking water of palm trees or a potion of roots, and even swallowing eight lice taken from one's own head 9 —all of which served well the conservation of the Columbidae.
CORPUS HIPPOCRATICUM
Jaundice was described in detail and related to the choleric humor, yellow bile (ξανθη χολή xanthe chole), in the Corpus Hippocraticum, a collection of Ancient Greek textbooks, research notes, and philosophical reflections on medical topics, gathered between the 5th and 4th century BCE. 10 At that time, jaundice was regarded not as a symptom or sign but as an independent disease entity arising from imbalance (dyscrasia) of the four humors, with yellow bile, the lightest fluid, rising to the skin. 8 , 11 Based on precise observations comprising color of skin, urine, feces, and other factors, such as the season of the year during which the disease first appeared, five types of jaundice were discerned and known as the Hippocratic types of jaundice. 11 It is remarkable that although dissections and laboratory tests were not yet performed, yellow bile was believed to originate from the liver, as Malpighi 12 had later opined. Several authors speculated on a connection between the appearance of jaundice and liver malfunction. 8 , 13 Despite the striking precision of the ancient descriptions that can be linked to modern diseases, some of the proposed treatments, such as the daily consumption of a pint of very old dry white wine before going to bed, 11 are no longer regarded as beneficial for patients with liver disease.
ANCIENT CHINA
An ancient medical anthology written on silk fragments and bamboo cuttings was unearthed from a tomb in the South of China in 1973. It dated back to about 300 BCE during the Warring States period, an era of rivalry and fierce battles among different states in ancient China. 14 , 15 These manuscripts provide reflections on the origin of diseases (such as jaundice) and their treatment in ancient Chinese medicine. It was believed that man ** ** was the mirror of the universe. The structure of the body would reflect the physical design of the world. Its function would follow natural and social orders, all animated by the life force qi, that is, the vital air. 16 , 17 Jaundice was ascribed to a moist, hot blockade of the qi in the liver, spleen, and stomach, mainly caused by an improper diet. 16 Based on the therapeutic principle Yi Du Gong Du, that is, combatting poison with poison, the use of animal bile was advocated for treating jaundice in patients. Bear bile was considered the “king” of animal biles. 18 The harvest of bear bile is a testimony to the adventurousness and knowledge of anatomy of ancient Chinese physicians and pharmacists, let alone their biochemical intuition. Bears were captured and held in small wooden cages and were usually killed with axe‐like tools (Figure 4) to obtain about 50 g of bile from the gallbladder of one sacrificed bear. 18 , 19 , 20 In the Tang Materia Medica, the first state pharmacopoeia worldwide, collected during the Tang dynasty (618–907 CE), a Golden Age of Chinese poetry, it was stated that “bear bile which tastes bitter can be used to treat jaundice, intractable diarrhea in summer and cardialgia.” Bear bile contains high levels of mainly taurine‐conjugated ursodeoxycholic acid (UDCA), a tertiary bile acid in humans, but a primary bile acid in bears, which is formed from cholesterol in the liver. UDCA may constitute up to 60% of Chinese black bears’ total biliary bile acids. 21 In the early 20th century, UDCA was first isolated and described in the bile of polar bears 22 and was later discovered to be highly efficient in treating patients with chronic cholestatic liver diseases, 23 , 24 , 25 , 26 having previously been used to dissolve cholesterol gallstones within the gallbladder. 27 , †† †† There is another ancient application of animal bile that did not find its way into modern medical textbooks, namely, the oral administration of an animal bile tincture to dislodge fishbones stuck in the throat and esophagus. 18 It is probable that the bones were softened by calcium chelation and although prolonged therapy was not enjoyable, it was surprisingly successful. 18
FIGURE 4.

Woodcuts showing how to catch a bear and harvest bear bile: capturing a bear in a cave (top panel), seizing a bear (middle panel), and killing a bear with an axe‐like tool (bottom panel). 18 , 19 Illustrated by Shitomi Kangetsu, 1799. Reproduced with permission from Nihon Sankai meisan zue. 20 Copyright 1799.
HELLENISTIC PERIOD
The first detailed anatomic description of the bile duct system from different animal species was provided by the Greek philosopher and polymath Aristotle (384–322 BCE). His student, Diocles of Carystus, an ancient polis on the Greek island of Euboea, was actually the first physician‐anatomist to conclude that jaundice was the consequence of obstruction of the bile ducts, 13 that is, the so‐called émpraxis, (constipation) of the liver, which the itinerant Trallanius championed 800 years later. 4 Whoever deserves precedence, Diocles or Alexander of Tralles, this was undoubtedly a milestone in the understanding of jaundice.
The first dissections of the human body were performed in Alexandria, the center of medical and biological research of the Hellenistic period, which spanned the years between the death of Alexander the Great in 323 BCE and the rise of the Roman Empire. 28 A celebrity among ancient anatomists was Erasistratus (304–250 BCE), notoriously known as the Butcher of Alexandria. Rumors were propagated that he, along with other colleagues, was performing vivisections on condemned criminals “while they were yet breathing.” 29 Erasistratus coined the term parenchyma (meaning “poured out beside”) for liver tissue, based on the belief that this “structure” was formed of coagulated blood released from hepatic vessels. In Erasistratus’ view, bile was separated from blood in the liver by the different viscosities of the two fluids, and thence conducted to the intestines via a small tube that he named the choledochus. 30 When bile flow in the choledochus is interrupted, jaundice follows. Thereafter, the observations of Diocles were confirmed in various animal species. 30 , 31
ROMAN EMPIRE AND MIDDLE AGES
Aulus Cornelius Celsus (25 BCE to 50 CE) was an outstanding medical encyclopedist who lived when the Roman Empire flourished, an era that saw major progress in politics, architecture, and urban development but negligible growth in medical knowledge. 8 Celsus compiled opinions of ancient Greek and Alexandrian physicians mingled with new reflections in his treatise De Medicina (Figure 5), which currently is housed in the Laurentian Library, in Florence, Italy. Celsus ascribed jaundice to an inflammation or affliction of the liver, the “royal organ,” and named jaundice “Morbus Regius,” the Regal Disease, not to be confused with the Royal Maladies, that is, the hereditary conditions porphyria and hemophilia that tormented the personal and political lives of the European Royal Families, ‡‡ ‡‡ or with the King's Evil (tuberculous lymphadenitis, i.e., scrofula). Pliny held that jaundice was so called because those who visit the courts of kings are most liable to it, because of the voluptuous habits of such societies. As Celsus explained facetiously, the therapy prescribed for jaundiced patients was so costly that only royalty could afford it 32 : “One should have a good bed in a tasteful room, seek relaxation and good humor, and take heart from the comforting pleasure, §§ §§ which will relieve the soul.” 33 A rather progressive idea was conceived by another physician of that time, Rufus of Ephesus (80–150 CE), who, although he followed the theory of the humors, started to depart from Hippocrates’ teachings. Ephesus distinguished obstructive jaundice from a hematogenous form, whereby blood was converted into bile. 13 , 29 This can be seen as the first description of prehepatic or hemolytic jaundice. The distinction was soon adopted by Galen of Pergamon (129–216 CE), the single most productive physician and investigator of late antiquity. More economically than Hippocrates, Galen recognized jaundice as (1) resulting from inflammation or hardening or compression of the choledochus; (2) occurring during the course of a feverish illness (i.e., cholestasis of sepsis); and (3) caused by the transformation of blood into bile, for example after the bite of a poisonous snake. 13 , 30 Galen's teachings were accepted unchanged for more than 1500 years during the Middle Ages, a period dominated by a dogmatic Christian church that opposed creative thinking in its sphere of influence. 8 , 13
FIGURE 5.

Facsimile of Celsus's 1st century Encyclopedia, De Medicina, published in 1989 by The Classics of Medicine Library of the Internet Archive Open Library collection, San Francisco, CA.
ANCIENT MUSLIM WORLD
Baghdad soon emerged as the new capital of the scientific world, although Arab‐Muslim physicians did not substantially challenge the concepts of Galen on the origin of jaundice. Patients with jaundice were mainly treated with dietary therapies, such as drinking chicory water or camel's milk. 34 , 35 The Persian physician Haly Abbas (c.930–c.994 CE) observed that a pale stool only occurs in patients with biliary obstruction and not in other forms of jaundice, 36 a criterion that was included a millennium later in the definition of obstructive or posthepatic jaundice by the Swiss wunderkind anatomist, physiologist, naturalist, encyclopedist, bibliographer, physician, and poet, Albrecht von Haller (1708–1777), in his Elementa physiologiae corporis humani (published in 1764).
17TH TO 19TH CENTURY
The 17th to 19th century period can undoubtedly be seen as the dawn of modern hepatology. Scientists started to study the yellow pigment visible as jaundice. Marcello Malpighi (1628–1694), Johannes Bohn (1640–1718), and Herman Boerhaave (1668–1738) refuted the doctrine of Erasistratus that bile was a product of filtration from the blood and demonstrated that bile was formed in the liver. 13 , 30 , ¶¶ ¶¶ Antoine François de Fourcroy (1755–1809), a French physician and chemist, Jacobite supporter, and confidant of Robespierre during the French Revolution, first mentioned a yellow pigment as one of several components of bile in his Système des connaissances chimiques (published in 1801). But it was Louis‐Jacques Thénard (1777–1857, Figure 6) who first extracted unconjugated bilirubin from the inspissated common duct bile of an elephant that had died at the Paris Zoo, and published the method in a late edition of his celebrated chemistry treatise. 37 Thénard, a French chemist of humble origins, a farmworker's son in the Champagne district, had studied under Fourcroy and Louis Nicolas Vauquelin. Six years after Fourcroy's death, and with Vauquelin's influence, Thénard was elected to the chairs of chemistry at the École Polytechnique and the Faculté des Sciences (Figure 6A) and soon he succeeded Fourcroy as a member of the French Academy of Sciences. In 1825, he received the title of Baron from Charles X (Figure 6B), and in 1832 Louis Philippe made him a peer of France.
FIGURE 6.

(A) Louis‐Jacques Thénard. (B) Baron Thénard. Reproduced from (A) the English and (B) the French versions of Wikipedia, respectively.
The chemists Leopold Gmelin (1788–1853) and Friedrich Tiedemann (1781–1861) introduced a chemical test to detect the bile pigment in various body fluids such as urine, known as Gmelin's test or Gmelin's reaction. 38 The fluids were mixed with equal amounts of nitric acid in a test tube. When bile pigments were present, they were oxidized, and several chemical products became visible as blue, green, and violet rings. Gmelin observed a change in color from yellow‐brown to green when bile was exposed to oxygen, and he concluded that the bile pigment exists in a reduced, yellow‐brown form (later called bilirubin) and an oxidized, green form (later called biliverdin). 38 The structural chemist Wilhelm Heinrich Heintz (1817–1880) succeeded in isolating the yellow bile pigment and its green oxidation product from bile; in 1863, Georg Städeler (1821–1871) named the yellow bile pigment bilirubin (from the Latin bilis bile and ruber = red). 13 , 39 As scientists in the 19th century often had a rather sublime view of their work, possibly influenced by the Romantic era that peaked around 1850, the epithet Pigments of Life emerged, a term favored a century later by no less than Sir Alan R. Battersby 40 (1925–2018), international authority on the chemistry of living systems. And so now we have the red pigment of blood (now known as hemoglobin), the yellow pigment of bile (bilirubin), and the green pigment of plants (chlorophyll). 41 The riddle concerning the reason why blood is red and grass is green was posed almost coincidentally early in the 17th century by John Donne, 42 renowned love poet and Dean of St. Paul's Cathedral, and Sir Walter Raleigh, 43 who was imprisoned in the Tower of London for treason. But that conundrum was not solved for nigh on 30 years.
The site of bilirubin formation, the yellow pigment of life, was a matter of controversy. ††† ††† Johannes Peter Müller's (1801–1858) localization of the synthesis of bilirubin to the liver 44 was endorsed by Oskar Minkowski (1858–1931) and Bernhard Naunyn (1839–1925), who treated animals with arsenic to induce severe jaundice, which was not observed when the liver was first removed (“Ohne Leber kein Ikterus” [“Without the liver no ikterus”]). 45 , 46 Rudolf Virchow (1821–1902) opposed this concept and emphasized that hemolytic jaundice occurs in patients in the absence of liver disease, as described 2000 years earlier by Rufus and Galen. Virchow 47 observed a striking similarity between bilirubin and a pigment that he found in old blood extravasations, which he reasoned might be a metabolite of the red blood pigment and formed outside the liver.
20TH CENTURY
The 20th century was characterized by the development of an extensive arsenal of techniques and laboratory procedures. In 1911, the Nobel laureate Hans Fischer (1881–1945, Figure 7) supported Virchow's view that bilirubin was a breakdown product of heme by his brilliant chemical analysis of bilirubin and its metabolites. 49 , 50 , 51 Fischer and his student Hans Plieninger (1914–1984) were the first to synthesize the bilirubin molecule containing four pyrrole rings linked by three carbon bridges in an open chain structure, 52 and finally the identity of the yellow pigment of jaundice was brought to light, so to speak.
FIGURE 7.

Nobel prize winner Hans Fischer. (A) Portrait by J.F. Lehmann in 1930 at age 50 years old. Reproduced with permission from Perspectives in Biology and Medicine. 48 Copyright 1965, Johns Hopkins University Press. (B) Laboratory photograph. In 1921, Fischer became professor of organic chemistry at the Technical University of Munich, where he stayed and worked until his untimely demise. After the total destruction of his institute during the last days of World War II, he committed suicide in despair in 1945. The lunar crater Fischer shared the last names of Hans and another Nobel laureate in Chemistry (1902), Hermann Emil Louis Fischer (1852–1919). Coincidentally, Emil (as he was always known) also committed suicide, in despair at the loss of his sons in World War I. Reproduced with permission from Alamy.com.
Moritz Löwit (1851–1918) and the German pathologist Ludwig Aschoff (1866–1942) highlighted the role of the reticuloendothelial system in bilirubin formation, 53 , 54 but they focused only on its (admittedly large) hepatic component, the Kupffer cells. American physiologist Frank Charles Mann (1887–1962) finally disproved the liver's exclusivity in bilirubin formation by showing, in hepatectomized dogs, that bilirubin could also be formed in extrahepatic tissue such as the bone marrow or spleen, 55 a discovery crucial for the understanding of prehepatic jaundice. The concepts on the origin of jaundice were expanded by Abraham Albert Hijmans van den Bergh (1869–1943), Professor of Internal Medicine in Groningen and Utrecht and member of the Royal Netherlands Academy of Arts and Sciences, who developed a sensitive colorimetric assay for the determination of bilirubin in serum, known as the Van den Bergh reaction. 56 , 57 Based on the findings of Paul Ehrlich, 58 he observed that serum bilirubin in obstructive jaundice gives an immediate color reaction with the diazo reagent (“direct reacting”), whereas bilirubin found in patients with hemolytic jaundice would react only after prior extraction with alcohol (“indirect reacting”), 56 , 57 which he reasoned indicated that only the direct‐reacting bilirubin had passed through the polygonal hepatocytes. 56 , 57 His presumption that albumin binding restricted the indirect form to the bloodstream was contradicted by Grant Henry Lathe 59 (1913–2007, Figure 8), 60 who separated two protein‐free bilirubin fractions from cholestatic serum, one of which gave a direct and the other one an indirect Van den Bergh reaction. Protein binding could not account for the chemical difference. Four years later, Rudi Schmid (1922–2007), 61 Barbara Heap Billing (1920–2017), 62 and Edmund Talafant (1914–1986) 63 all independently showed that bilirubin was secreted into bile as monoglucuronide and diglucuronide esters after conjugation by the liver. The responsible enzyme was identified to be a single isoform of a uridine diphosphate‐glucuronyltransferase, UGT1A1, located mainly in the endoplasmic reticulum (ER) of hepatocytes. 64 , 65 The East‐West USA splenetic public dispute over the mechanism of bilirubin diglucuronide formation in vivo, which has been ironically described as a “particularly piquant pyrrolic polemic,” 66 was resolved by Canadian Ellen Ruth Gordon, PhD (1923–2010), while at Yale University, using clean microsomes, highly purified canalicular membranes prepared from rat liver, stringent experimental conditions, and impeccable technique. 67 Rather than the second conjugation of bilirubin monoglucuronide being affected by a postulated transglucuronidase (also known as dismutase) in the canalicular membrane immediately before secretion into bile, diglucuronidation simply took place in the ER mediated by the same UGT1A1.
FIGURE 8.

Grant Henry Lathe (b. 1913, Grand Forks, British Columbia, Canada) in his laboratory in London, around 1955. As a child he was considered “backward”; his parents bought him a birdlife guide to stimulate his intellect. Later he became one of the most outstanding scientists of his time. Reproduced with permission from Biochemistry. 60 Copyright 2007, American Chemical Society.
Conjugated bilirubin corresponds to the direct‐reacting Van den Bergh form and unconjugated to the indirect‐reacting form, respectively, both of which can reversibly bind to serum proteins such as albumin. Liver cell damage reduces the liver's ability to glucuronidate bilirubin, leading to a buildup of unconjugated bilirubin in the blood. Impaired secretion of conjugated bilirubin into bile causes an increase of conjugated serum bilirubin. 68 The third form of jaundice, termed intrahepatic or hepatocellular jaundice, was understood to be due to some combination of impaired hepatic uptake, intracellular metabolism, transport, and biliary secretion, resulting from dysfunction as a result of liver injury. Subsequent discoveries deepened the understanding of the three forms of jaundice, as explained in today's medical textbooks. Charles H. Gray (1911–1997) and Irving M. London (1918–2018) recognized that about 20% of total bilirubin derives from the degradation of nonhemoglobin heme, mostly of hepatic and renal origin, thereby showing that the occurrence of prehepatic jaundice is not restricted to hemolysis. 69 , 70 A collaborative group from Yale Laboratory Medicine and Hepatology 71 identified a third fraction of bilirubin, which having undergone conjugation becomes tightly (covalently) bound to serum albumin (termed albumin‐bound bilirubin). This form of bilirubin accounts for the slow resolution of long‐term jaundice in some patients with conjugated hyperbilirubinemia whose hepatobiliary function would otherwise have appeared to return to normal. 71 Remarkable studies by investigators such as Carl Arthur Goresky (1932–1996) in Montreal, Jonathan Levi (1933–1999) in London, and Allan W. Wolkoff (b. 1948) in New York, among others, uncovered the molecular mechanisms of hepatic bilirubin uptake, intracellular transport, and bilirubin excretion into bile, paving the way for the cloning and molecular characterization of transporter gene mutations for the different syndromes of hereditary hyperbilirubinemia. 72 , 73 , 74 Meanwhile, disease‐causing mutations and variants have been identified for (1) the unconjugated hyperbilirubinemia of the Crigler‐Najjar syndrome, by Ida S. Owens and Namita Roy‐Chowdhury and colleagues 75 , 76 ; (2) Gilbert syndrome, in the human UGT1A1 gene, by Piter Bosma and colleagues 77 ; (3) the conjugated hyperbilirubinemia of the Dubin‐Johnson syndrome, by Coen Paulusma, Ronald Oude Elferink, and colleagues 78 ; (4) the ABCC2 gene, by Dietrich Keppler's group 79 ; and (5) the conjugated hyperbilirubinemia of the Rotor syndrome, by the groups of Alfred Schinkel and Milan Jirsa, 80 in the OATP1B1 and OATP1B3 genes. These crucial contributions of the recent decades have largely unraveled the handling of bilirubin by the human liver.
CONCLUDING REMARKS
In the past 2500 years our perceptions of jaundice/icterus underwent a fundamental metamorphosis from that of a disease per se to a sign of liver disorder refined into the different clinical presentations of hyperbilirubinemia according to various prehepatic, hepatic, and posthepatic etiologies. Today's challenge is to devise treatments for the underlying diseases. Therapeutic options include anticholestatic medications, such as the tertiary bile acid UDCA, 81 , 82 the farnesoid X receptor agonist obeticholic acid 83 , 84 (which may even prove effective in treating fatty liver disease 85 ), and the peroxisomal proliferator‐associated receptor agonist bezafibrate, 86 in disorders such as primary biliary cholangitis,*** *** the pregnane X receptor agonist rifampicin in persistent hepatocellular secretory failure, 87 enzyme induction therapy with the constitutive androstane receptor agonist phenobarbital, phototherapy, or liver‐directed gene therapy in rare forms of hereditary hyperbilirubinemia—not forgetting liver transplantation for end‐stage liver disease. Much more research effort will have to be made to further improve the outcomes in patients with jaundice of different origins. Nonetheless, it is thanks to advances in knowledge about the pathogenesis of jaundice, over scores of centuries by scores of dedicated physician‐scientists, that the delightful call of the Eurasian golden oriole can still be enjoyed today.
SERIES EDITOR'S POSTSCRIPT
We are indebted to Toni Herta and his esteemed mentor, Ulrich Beuers, for their animated chronological hurtle through the history of jaundice, from the astute observations of the ancients to the elegant molecular mechanisms of the current millennium. And yet, even these intrepid cognoscenti dare not try to explain why in US medicine, even today, 88 jaundice in the eyes is termed icterus and icterus of the body is jaundice; it has been observed 66 that, whether derived from French or Greek, both terms denote yellow (dis)coloration of the body parts being scrutinized. In keeping with the genre of this series of essays, there are anecdotes and serendipity aplenty, which, so to speak, color the narrative of the discourse. Who might have expected that one of the foremost chemists in this history, who solved the structure of bilirubin, Nobel laureate Hans Fischer, would share the eponym of a lunar crater with a fellow German Nobelist, both of whom committed suicide brought on by a personal calamity of World Wars II and I, respectively.
Toni Herta, a native of Dresden, graduated in Medicine at Charité‐University Hospital of Berlin, after studies in Dresden and Paris, which included electives in Nepal and Uganda. Following residency in Leipzig, he completed a research fellowship in Dr. Beuers's laboratory in Amsterdam, whither he was drawn by the attractive reputation of his mentor‐to‐be and intrigued by the concept of the biliary bicarbonate umbrella. 89 His not unexpected professional aspiration is for basic science–based clinical excellence in his current appointment as a clinical scientist and physician back in Leipzig. However, despite his brief sojourn in Kathmandu in 2010, he readily admits that his passion for percussion—he plays drums in a jazz band—does not extend to proficiency playing the Madal (Nepali: मादल), which we all know is a musical instrument used mainly for rhythm‐keeping in Nepalese folk music.
And now it is my pleasure to acquaint the reader with the senior author, Prof. Ulrich Beuers, with whom I have happily been personally acquainted since his research fellowship at Yale University (1991–1993) in Jim Boyer's laboratory. I am reminded of much productive time spent together, in my laboratory at Yale, when he was writing a book chapter (“Bile: A historical review of its form and function”) 8 ; by coincidence, his role then vis‐a‐vis me was occupied recently by Toni Herta vis‐a‐vis him.
Ulrich has been a Full Professor and Head of Hepatology in the Department of Gastroenterology & Hepatology, Tytgat Institute for Liver and Intestinal Research, Academic Medical Center of the University of Amsterdam and later Amsterdam University Medical Centers since 2010. Ulrich migrated there in 2007 from Munich (Department of Medicine II–Grosshadern, Ludwig Maximilians University). A native of Hagen in North Rhine‐Westphalia, Germany, where he attended the Albrecht Dürer Gymnasium, Prof. Beuers began his peripatetic career with medical studies in Ghent, Berlin, and Freiburg, clerkships in Indonesia and Brasil, a dissertation in neuropharmacology (1983) in Freiburg, postdoctoral training in biochemistry at the University of Göttingen (1984–1986), and extensive clinical grounding in internal medicine, gastroenterology, and hepatology (1986–1991 and 1993–1996) in Munich, under the watchful eye of the venerable Prof. Gustave Pargartner, who is venerated still for his time‐honored wisdom, character, and now longevity. 90 In 1994, Ulrich completed his Habilitation (from Medieval Latin habilitare, “to make suitable or fit”), a postdoctoral qualification of excellence in research and teaching, dating from 17th‐century Germany; habilitation is still extant in scores of countries globally (except England and the United States), but it is widely threatened with extinction. Aside from an intensive research program, clinical responsibilities, and authorship of upward of 500 publications, Ulrich is a glutton for professional punishment, in journal editorial duties, chairing guideline committees, membership of numerous societal boards, and administrative activities in several liver study associations. In his spare time, he indulges his love of sports, music, literature, and gardening. It remains to be seen whether these myriad pursuits have cured his wanderlust.
CONFLICT OF INTEREST
Nothing to report.
Herta T, Beuers U. A historical review of jaundice: May the golden oriole live forever. Clin Liver Dis. 2022;20:45–56. 10.1002/cld.1267
Footnotes
Johann Wolfgang Goethe. Gedenkausgabe der Werke, Briefe und Gespräche. Band 1–24 und Erg.‐Bände 1–3, Band 16, Zürich 1948 ff, S. 7–9767. Erstdruck. In: Zur Farbenlehre, 1. Bd., Stuttgart; 1808.
Future essays in this series will focus on the liver in Judaism, Islam, Christianity, and Hinduism (editor's note).
Or dove or turtledove remedy.
Admittedly, the phraseology in these ancient texts may not be considered politically correct nowadays.
Bile acid therapy for gallstone dissolution and cholestatic liver disease is discussed more fully by Frank Lammert and Serge Erlinger, respectively, in their essays in this series.
These are well documented in Alan R. Rushton's account “Royal Maladies: Inherited Diseases in the Ruling Houses of Europe,” Bloomington, IN: Trafford Publishing; 2008.
“Its cure, says he, is to be attempted by exertions of every kind, ‘lusu, joco, ludis, lacivia, per quae mens exhilaretur: ob quae regius morbus dictus videtur,’” exertions that are variously translated to refer to sport, merriment, games, and playfulness (or wantonness or petulance or impudence). 32
Reviewed comprehensively by Serge Erlinger in this series.
See Reuben A. Seeing purple. Hepatology 2006; 43: 1403‐1409
Formerly primary biliary cirrhosis.
REFERENCES
- 1. Küchler F. Beiträge zur Kenninis der Assyrisch‐Babylonischen Medizin. Texte mit Umschrift, Übersetzung und Kommentar. Leipzig: JC Hinrichs; 1904. [Google Scholar]
- 2. Rosner F. Yerakon in the Bible and Talmud: jaundice or anemia? Am J Clin Nutr. 1972;25:626–8. [DOI] [PubMed] [Google Scholar]
- 3. Aronson JK, Ramachandran M. The diagnosis of art: Caravaggio's jaundiced Bacchus. J R Soc Med. 2007;100:429–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leven KH. Antike Medizin. Ein Lexikon. München: C.H. Beck; 2005. p. 322–3. [Google Scholar]
- 5. Boyer JL. Bile formation and secretion. Compr Physiol. 2013;3:1035–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Haubrich WS. Medical meanings: a glossary of word origins. 2nd ed. Philadelphia: American College of Physicians; 2003. [Google Scholar]
- 7. Wright M, von Wright F. Svenska faglar efter naturen och pa sten ritade. Stockholm: Förlaget Svenska Fåglar; 1929. [Google Scholar]
- 8. Beuers U, Boyer JL. Bile: a historical review of studies on its form and function. In: Kirsner JB, editor. The growth of gastroenterologic knowledge during the twentteeth century. Philadelphia: Lea & Febiger; 1994. p. 267–88. [Google Scholar]
- 9. Rosner F. Pigeons as a remedy (segulah) for jaundice. NY State J Med. 1992;92:189–92. [PubMed] [Google Scholar]
- 10. Cantor D. Reinventing hippocrates (the history of medicine in context). 1st ed. London: Routledge; 2001. [Google Scholar]
- 11. Papavramidou N, Fee E, Christopoulou‐Aletra H. Jaundice in the hippocratic corpus. J Gastrointest Surg. 2007;11:1728–31. [DOI] [PubMed] [Google Scholar]
- 12. Malpighi M. De viscerum structura exercitatio anatomica. Bologna: Giacomo Monti; 1666. [Google Scholar]
- 13. Mani N. Die historischen Grundlagen der Leberforschung. Basel: Benno Schwabe & Co; 1967. [Google Scholar]
- 14. Research Group for Collating Mawangdui Medical Books (RGCMMB) . A transcription of some of the medical texts contained in the silk manuscripts and unearthed at the No. 3 Han tomb at Mawangdui. Wen Wu; 1975. 6:1–5, 9:35–48. [Google Scholar]
- 15. Sun Q. Infering the date of writing of the Recipes for 52 kinds of disease by the archaic linguistics of the Book of Song (Chi). Zhonghua Yi Shi Za Zhi. 1986;16:243–6. [PubMed] [Google Scholar]
- 16. Chen TS, Chen PS. The liver in traditional Chinese medicine. J Gastroenterol Hepatol. 1998;13:437–42. [DOI] [PubMed] [Google Scholar]
- 17. Wisemann N, Ellis A. Fundamentals of Chinese medicine: Zhong Yi Xue Ji Chu. 2nd ed. Boulder, CO: Paradigm Publications; 1995. [Google Scholar]
- 18. Wang DQ, Carey MC. Therapeutic uses of animal biles in traditional Chinese medicine: an ethnopharmacological, biophysical chemical and medicinal review. World J Gastroenterol. 2014;20:9952–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang YL, Li XH. Progress in the studies of the drained bear bile. Zhongguo Zhongyao Zazhi. 1991;16:592–4. [Google Scholar]
- 20. Kimura K, Kangetsu S. Nihon Sankai meisan zue (Famous products of mountains and sea). Osaka: Shioya Chobei, 11th year of Kansei; 1799. p. 5. [Google Scholar]
- 21. Hagey LR, Crombie DL, Espinosa E, Carey MC, Igimi H, Hofmann AF. Ursodeoxycholic acid in the Ursidae: biliary bile acids of bears, pandas, and related carnivores. J Lipid Res. 1993;34:1911–7. [PubMed] [Google Scholar]
- 22. Hammarsten O. Untersuchungen über die Gallen einiger Polarthiere. Hoppe Seylers Z Physiol Chem. 1901;32:435–66. [Google Scholar]
- 23. Poupon RE, Balkau B, Eschwège E, Poupon R. A multicenter, controlled trial of ursodiol for the treatment of primary biliary cirrhosis. UDCA‐PBC Study Group. N Engl J Med. 1991;324:1548–54. [DOI] [PubMed] [Google Scholar]
- 24. Leuschner U, Fischer H, Kurtz W, Güldütuna S, Hübner K, Hellstern A, et al. Ursodeoxycholic acid in primary biliary cirrhosis: results of a controlled double‐blind trial. Gastroenterology. 1989;97:1268–74. [DOI] [PubMed] [Google Scholar]
- 25. Beuers U, Boyer JL, Paumgartner G. Ursodeoxycholic acid in cholestasis: potential mechanisms of action and therapeutic applications. Hepatology. 1998;28:1449–53. [DOI] [PubMed] [Google Scholar]
- 26. Paumgartner G, Beuers U. Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited. Hepatology. 2002;36:525–31. [DOI] [PubMed] [Google Scholar]
- 27. Hofmann AF. Medical dissolution of gallstones by oral bile acid therapy. Am J Surg. 1989;158:198–204. [DOI] [PubMed] [Google Scholar]
- 28. Serageldin I. Ancient Alexandria and the dawn of medical science. Glob Cardiol Sci Pract. 2013;2013:395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Magner LN. A history of medicine. 2nd ed. Philadelphia: Taylor & Francis; 2005. [Google Scholar]
- 30. Kuntz E, Kuntz HD. Hepatology textbook and atlas. 3rd ed. New York: Springer; 2008. [Google Scholar]
- 31. Garofalo I, Fuchs B. Anonymi Medici: De Morbis Acutis et Chroniis (studies in ancient medicine). Leiden, The Netherlands: Brill; 1997. [Google Scholar]
- 32. Chapman N. Thoughts on the pathology and treatment of lcterus, or jaundice. Lond Med Phys J. 1828;4:478–90. [PMC free article] [PubMed] [Google Scholar]
- 33. Celsus AC, Spencer WG. Celsus De Medicina. Cambridge, MA: Harvard University Press; 1935. [Google Scholar]
- 34. Alvarez Millan C. The case history in medieval Islamic medical literature: Tajarib and Mujarrabat as source. Med Hist. 2010;54:195–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Saad B, JadAllah R, Daraghmeh H, Said O. Medicines and method of therapy in the Arab and Islamic medicine. Biosci Biotech Res Comm. 2009;2:123–32. [Google Scholar]
- 36. Heydari M, Dalfardi B, Golzari SEJ, Mosavat SH. Haly abbas and the early description of obstructive jaundice. Iran J Public Health. 2014;43:1161–2. [PMC free article] [PubMed] [Google Scholar]
- 37. Thenard LJ. Traite de chemie elementaire theorique et pratique. 5th ed. Paris: Corchard Libraire‐Editeurs des Ann. Clinic Physique; 1827. p. 602. [Google Scholar]
- 38. Tiedemann F, Gmelin L. Die Verdauung nach Versuchen. Heidelberg, Leipzig: Karl Gross; 1826–27. [Google Scholar]
- 39. Städeler G. Ueber die Farbstoffe der Galle. Justus Liebigs Ann Chem. 1864;132:323–54. [Google Scholar]
- 40. Battersby AR, Fookes CJR, Matcham GWJ, McDonald E. Biosynthesis of the pigments of life: formation of the macrocycle. Nature. 1980;285:17–20. [DOI] [PubMed] [Google Scholar]
- 41. Lightner DA. Bilirubin: Jekyll and Hyde pigment of life; pursuit of its structure through two world wars to the new millenium. Prog Chem Org Nat Prod. 2013;98:1–776. [DOI] [PubMed] [Google Scholar]
- 42. Donne J. Of the progresse of the soule—the second anniversary. In: Coffin CM, editor. Modern library. The complete poetry and selected prose of John Dunne. New York: The Random House Publishing Group; 1994. [Google Scholar]
- 43. Whitehead C. The life and times of Sir Walter Raleigh with copious extracts from his History of the World. Whitefish, MT: Kessinger Publishing LLC; 2005. [Google Scholar]
- 44. Müller JP. Handbuch der Physiologie des Menschen. Coblenz: Hölscher; 1837. [Google Scholar]
- 45. Minkowski O. Über den Einfluss der Leberexstirpation auf den Stoffwechsel. Beiträge zur Pathologie der Leber und des Ikterus. Arch F Exp Pathol. 1886;21:41–87. [Google Scholar]
- 46. Minkowski O, Naunyn B. Über den Ikterus durch Polycholie und die Vorgänge in der Leber bei demselben. Beiträge zur Pathologie der Leber und des Ikterus. Arch F Exp Pathol. 1886;21:1–33. [Google Scholar]
- 47. Virchow R. Die pathologischen Pigmente. Archiv für pathologische Anatomie und Physiologie und für klinische Medicin. 1847;1:379–404. [Google Scholar]
- 48. Watson CJ. Reminiscences of Hans Fischer and his laboratory. Perspect Biol Med. 1965;8:418–35. [DOI] [PubMed] [Google Scholar]
- 49. Fischer H, Reindel F. Über Hämatoidin. Z Physiol Chem. 1923;127:299–316. [Google Scholar]
- 50. Fischer H. Zur Kenntnis der Gallenfarbstoffe. Z Physiol Chem. 1911;73:204–39. [Google Scholar]
- 51. Seidel W, Fischer H. Über die Konstitution des Bilirubins, Synthesen der Neo‐ und der Iso‐Neoxanthobilirubinsäure. Z Physiol Chem. 1933;214:145–72. [Google Scholar]
- 52. Fischer H, Plieninger H. Synthese des Biliverdins (Uteroverdins) und Bilirubins, der Biliverdine XIIIa und IIIa sowie der Vinylneoxanthosäure. Z Physiol Chem. 1942;274:231–60. [Google Scholar]
- 53. Löwit M. Ueber die Bildung des Gallenfarbstoffes in der Froschleber. Beiträge zur Lehre vom Icterus, Beitr z path Anat u z allg Path. 1888;9:223–64. [Google Scholar]
- 54. Aschoff L, Kiyono K. Ein Beitrag zur Lehre von den Makrophagen. Verh d dtsch Path Ges. 1913;16:107. [Google Scholar]
- 55. Mann FC, Bollman JL, Magath TB. Studies on the physiology of the liver: IX. The formation of bile pigment after total removal of the liver. Am J Physiol. 1924;692:393–409. [Google Scholar]
- 56. Van den Bergh AAH, Snapper I. Die Farbstoffe des Blutserums. Eine quantitative Bestimmung des Bilirubins im Blutserum. Dtsch Arch Klin Med. 1913;110:540–61. [Google Scholar]
- 57. Van den Bergh AAH, Snapper I, Müller F. Die Gallenfarbstoffe im Blute. 1st ed. Leiden, The Netherlands: SC van Doesburgh; 1918. [Google Scholar]
- 58. Ehrlich P. Sulfodiazobenzol als reagens auf bilirubin. Fresenius, Zeitschrift f Anal Chemie. 1884;23:275–6. [Google Scholar]
- 59. Cole PG, Lathe GH. The separation of serum pigments giving the direct and indirect van den Bergh reaction. J Clin Pathol. 1953;6:99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lathe R. Grant Henry Lathe (1913–2007). Biochemist. 2007;2007:43–4. [Google Scholar]
- 61. Schmid R. Direct‐reacting bilirubin, bilirubin glucuronide, in serum, bile and urine. Science. 1956;124:76–7. [DOI] [PubMed] [Google Scholar]
- 62. Billing BH, Cole PG, Lathe GH. The excretion of bilirubin as a diglucuronide giving the direct van den Bergh reaction. Biochem J. 1957;65:774–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Talafant E. Properties and composition of the bile pigment giving a direct diazo reaction. Nature. 1956;178:312. [DOI] [PubMed] [Google Scholar]
- 64. Lathe GH, Walker M. The synthesis of bilirubin glucuronide in animal and human liver. Biochem J. 1958;70:705–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Roy Chowdhury J, Roy Chowdhury N, Falany CN, Tephly TR, Arias IM. Isolation and characterization of multiple forms of rat liver UDP‐glucuronate glucuronosyltransferase. Biochem J. 1986;233:827–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Reuben A. By indirections find directions out. Hepatology. 2002;35:1287–90. [DOI] [PubMed] [Google Scholar]
- 67. Gordon ER, Meier PJ, Goresky CA, Boyer JL. Mechanism and subcellular site of bilirubin diglucuronide formation in rat liver. J Biol Chem. 1984;259:5500–6. [PubMed] [Google Scholar]
- 68. Hall JE, Guyton AC. Textbook of medical physiology. 13th ed. New York: Elsevier; 2015. [Google Scholar]
- 69. Gray CH, Neuberger A, Sneath PH. Studies in congenital porphyria. 2. Incorporation of 15N in the stercobilin in the normal and in the porphyric. Biochem J. 1950;47:87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. London IM, West R, Shemin D, Rittenberg D. On the origin of bile pigment in normal man. J Biol Chem. 1950;184:351–8. [PubMed] [Google Scholar]
- 71. Weiss JS, Gautam A, Lauff JJ, Sundberg MW, Jatlow P, Boyer JL, et al. The clinical importance of a protein‐bound fraction of serum bilirubin in patients with hyperbilirubinemia. N Engl J Med. 1983;309:147–50. [DOI] [PubMed] [Google Scholar]
- 72. Goresky CA. The hepatic uptake process: its implications for bilirubin transport. Jaundice. New York: Springer; 1975. [Google Scholar]
- 73. Levi AJ, Gatmaitan Z, Arias IM. Two hepatic cytoplasmic protein fractions, Y and Z, and their possible role in the hepatic uptake of bilirubin, sulfobromophthalein, and other anions. J Clin Invest. 1969;48:2156–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Wolkoff AW, Wolpert E, Pascasio FN, Arias IM. Rotor's syndrome. A distinct inheritable pathophysiologic entity. Am J Med. 1976;60:173–9. [DOI] [PubMed] [Google Scholar]
- 75. Ritter JK, Yeatman MT, Ferreira P, Owens IS. Identification of a genetic alteration in the code for bilirubin UDP‐glucuronosyltransferase in the UGT1 gene complex of a Crigler‐Najjar type I patient. J Clin Invest. 1992;90:150–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bosma PJ, Chowdhury NR, Goldhoorn BG, Hofker MH, Oude Elferink RP, Jansen PL, et al. Sequence of exons and the flanking regions of human bilirubin‐UDP‐glucuronosyltransferase gene complex and identification of a genetic mutation in a patient with Crigler‐Najjar syndrome, type I. Hepatology. 1992;15:941–7. [DOI] [PubMed] [Google Scholar]
- 77. Bosma PJ, Chowdhury JR, Bakker C, Gantla S, de Boer A, Oostra BA, et al. The genetic basis of the reduced expression of bilirubin UDP‐glucuronosyltransferase 1 in Gilbert's syndrome. N Engl J Med. 1995;333:1171–5. [DOI] [PubMed] [Google Scholar]
- 78. Paulusma CC, Kool M, Bosma PJ, Scheffel GL, ter Borg F, Scheper RJ, et al. A mutation in the human canalicular multispecific organic anion transporter gene causes the Dubin‐Johnson syndrome. Hepatology. 1997;25:1539–42. [DOI] [PubMed] [Google Scholar]
- 79. Tsujii H, König J, Rost D, Stöckel B, Leuschner U, Keppler D. Exon‐intron organization of the human multidrug‐resistance protein 2 (MRP2) gene mutated in Dubin‐Johnson syndrome. Gastroenterology. 1999;117:653–60. [DOI] [PubMed] [Google Scholar]
- 80. van de Steeg E, Stránecký V, Hartmannová H, Nosková L, Hřebíček M, Wagenaar E, et al. Complete OATP1B1 and OATP1B3 deficiency causes human Rotor syndrome by interrupting conjugated bilirubin reuptake into the liver. J Clin Invest. 2012;122:519–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Poupon R, Chrétien Y, Poupon RE, Ballet F, Calmus Y, Darnis F. Is ursodeoxycholic acid an effective treatment for primary biliary cirrhosis? Lancet. 1987;1:834–6. [DOI] [PubMed] [Google Scholar]
- 82. European Association for the Study of the Liver . EASL clinical practice guidelines in primary biliary cholangitis. J Hepatol. 2017;67:145–72. [DOI] [PubMed] [Google Scholar]
- 83. Nevens F, Andreone P, Mazzella G, Strasser SI, Bowlus C, Invernizzi P, et al. A placebo‐controlled trial of obeticholic acid in primary biliary cholangitis. N Engl J Med. 2016;375:631–43. [DOI] [PubMed] [Google Scholar]
- 84. Trauner M, Nevens F, Shiffman ML, Drenth JPH, Bowlus CL, Vargas V, et al. Long‐term efficacy and safety of obeticholic acid for patients with primary biliary cholangitis: 3‐year results of an international open‐label extension study. Lancet Gastroenterol Hepatol. 2019;4:445–53. [DOI] [PubMed] [Google Scholar]
- 85. Younossi ZM, Ratziu V, Loomba R, Rinella M, Anstee QM, Goodman Z, et al. Obeticholic acid for the treatment of non‐alcoholic steatohepatitis: interim analysis from a multicentre, randomised, placebo‐controlled phase 3 trial. Lancet. 2019;394:2184–96. [DOI] [PubMed] [Google Scholar]
- 86. Corpechot C, Chazouillères O, Rousseau A, le Gruyer A, Habersetzer F, Mathurin P, et al. A placebo‐controlled trial of bezafibrate in primary biliary cholangitis. N Engl J Med. 2018;378:2171–81. [DOI] [PubMed] [Google Scholar]
- 87. van Dijk R, Kremer AE, Schmit W, van den Elzen B, van Gulik T, Gouma D, et al. Characterization and treatment of persistent hepatocellular secretory failure. Liver Int. 2015;35:1478–88. [DOI] [PubMed] [Google Scholar]
- 88. Fung BM, Perumpail M, Patel YA, Tabibian JH. Telemedicine in hepatology: current applications and future directions. Liver Transpl. 2021;28:294–303. [DOI] [PubMed] [Google Scholar]
- 89. Beuers U, Maroni L, Elferink RO. The biliary HCO3 − umbrella: experimental evidence revisited. Curr Opin Gastroenterol. 2012;28:253–7. [DOI] [PubMed] [Google Scholar]
- 90. Reuben A. Never say dye. Hepatology. 2004;39:259–64. [DOI] [PubMed] [Google Scholar]


