Abstract
Background:
Gender disparities in surgical care exist but have been minimally studied, particularly in low- and middle-income countries. This study explored perceptions and gender differences in health-seeking behavior and attitudes toward surgical care in Malawi among community members.
Methods:
A survey tool was administered to adults ≥18 years old at a central hospital, district hospital, and two marketplaces in Malawi from June 2018 to December 2018. Responses from men and women were compared using chi-squared tests.
Results:
Four hundred eighty-five adults participated in the survey, 244 (50.3%) men and 241 (49.7%) women. Women were more likely to state that fear of surgery might prevent them from seeking surgical care (29.1% of men, 43.6% of women, P = .0009). Both genders reported long wait times, medicine/physician shortages, and lack of information about when surgery is needed as potential barriers to seeking surgical care. More men stated that medical preference should be given to sons (17.1% of men, 9.3% of women, P = .01). Men were more likely to report that men should have the final word about household decisions (28.7% of men vs 19.5% of women, P < .0001) and were more likely to spend money independently (68.7% of married men, 37.5% of married women, P < .0001). Few participants reported believing gender equality had been achieved (61% of men and 66.8% of women).
Conclusions:
A multi-pronged approach is needed to reduce gender disparities in surgical care in Malawi, including addressing paternalistic societal norms, education, and improving health infrastructure.
Keywords: gender disparities, Malawi, surgical care, survey
Introduction
Gender inequality in health care is prevalent among a wide variety of specialties, particularly in Africa. A key finding in the World Health Organization’s (WHO) recent report on African women’s health was that “women bear an unacceptably huge burden of disease and death.”1 Women are often marginalized, putting them at risk for unequal care and poorer health outcomes.2-4 In Malawi, a previous study demonstrated that among general surgery patients presenting with peritonitis, 68.8% were men compared to 31.2% of women, even when excluding cesarean sections, operative trauma, and other gender-skewed cases like inguinal hernias. Of these patients, only 54% of women underwent an operation within 24 h of presentation compared to 70% of men (P = .01). Women had significantly more delays in presentation, delays to operation, and longer lengths of stay (LOS).5 While not a direct comparison, in the United States, 46% of emergency general surgery cases are performed on men, while 54% are performed on women.6
No prior studies have evaluated potential causes of gender disparities in surgical care in Malawi. We hypothesized that the reasons for these disparities are likely multi-factorial, including cultural norms, socioeconomic issues, gender biases, health literacy, and perceptions of the health care system. While biological sex differences and biases of health care workers may play a role as well, this study assessed the perceptions of the general Malawian population on gender biases and barriers in access to surgical care via a survey tool.
Methods
This study, approved by the Malawi Institute of Health and the UNC Institutional Review Board (IRB#18-0165), was a verbal survey (Supplemental Figure 1) conducted with a convenience sample of persons ≥18 years from June 2018 to December 2018. Community members were recruited from Kamuzu Central Hospital (KCH), the capital city Lilongwe’s marketplace, Salima District Hospital, and Salima’s marketplace. Kamuzu Central Hospital is a 1000-bed tertiary hospital with a catchment of five million and is the referral center for eight district hospitals, including Salima Hospital. Respondents at KCH and Salima Hospital were selected by requesting participation of every 10th adult male visitor and 10th adult female visitor to the surgical/medical wards. The marketplaces were randomly sampled to reduce selection bias. Market respondents were randomly selected by requesting participation of every 20th man and 20th woman who accessed the two main marketplace entrances. In clusters of people, survey administrators counted to the best of their ability. During the interview, tallying and recruitment of new entrants was paused. Respondents provided information on demographics, health-seeking behavior, barriers to care, gender equity attitudes, decision-making power, and social prioritization.
Surveys were constructed from validated surveys, including the Demographic and Health Surveys Woman’s Questionnaire DH-S7 (questions on demographics, health-seeking behavior, barriers to care, and decision-making power) and the International Men and Gender Equality (IMAGES) Survey (questions on gender equity attitudes).7,8 Questions on social prioritization were adopted from a non-validated survey on gender inequality in West Bengal.9 Two questions on health knowledge were discarded as they were not validated and confusingly worded. The surveys were 20 min, with 43 mixed closed- and open-ended questions, with open-ended responses directly transcribed by clerks. The surveys were in English, translated into local Chichewa, and administered by two trained Malawian clerks in a private area separated from the flow of traffic. Verbal informed consent was obtained. Surveys were beta-tested with 15 participants before implementation. Participants received standard incentives of packs of flour or sugar.
Demographic information was collected, as well as rural or urban (within city limits) domicile, surgical history (emergency vs elective and anatomic location), and income (converted from Kwacha to USD$). The surveys asked about distance to nearest clinic and hospital (in kilometers and minutes traveled), use of traditional healers, transportation methods, perceived barriers to care, reasons for not presenting for general or surgical care, and questions to determine if people are dying at home without seeking medical attention. Additional questions included perceptions on differences in access between men and women and gender equality. Two open-ended questions were asked about health topics participants would like to learn more about and opinions on ways to improve access to surgical care for women.
We used descriptive statistics to characterize the study sample. Open-ended questions were categorized via constant comparative method by two team members and reported as quantitative data. We summarized categorical variables with frequencies/percentages and continuous variables with median and interquartile range. Association between variables was assessed using chi-squared tests. Analyses were conducted using SAS, version 9.4 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Demographics
A total of 485 community members completed the survey (97% response rate), with 244 (50.3%) men and 241 (49.7%) women. Median age was 36 (IQR 28-44.5) for men and 38 (IQR 29.5-45) for women. Overall, women lived farther from hospitals, had lower education levels, made less money, and were more likely to be married. (Table 1)
Table 1.
Baseline Interviewee Characteristics, Stratified by Gender (N = 485).
| Male |
Female |
||
|---|---|---|---|
| N = 244a | N = 241a | P-Value | |
| Age, median (IQR) | 36 (28-44.5) | 38 (29.5-45) | .47 |
| Residence, n (%) | .12 | ||
| Rural | 145 (59.7) | 159 (66.5) | |
| Urban | 98 (40.3) | 80 (33.5) | |
| Closest district hospital, in minutes, median (IQR) | 30 (15-60) | 40 (20-100) | .0006 |
| Highest education, n (%) | .0003 | ||
| No school | 17 (7.3) | 25 (10.5) | |
| Primary | 81 (34.8) | 122 (51.3) | |
| Secondary | 123 (52.8) | 82 (34.5) | |
| University | 12 (5.2) | 7 (2.9) | |
| Graduate school | 0 (0) | 2 (.8) | |
| Occupation, n (%) | <.0001 | ||
| Farmer | 79 (32.4) | 113 (47.1) | |
| White collar (business) | 52 (21.3) | 69 (28.8) | |
| Part-time employed | 27 (11.1) | 8 (3.3) | |
| Student | 14 (5.7) | 8 (3.3) | |
| Housewife/stay at home | 0 (0) | 12 (5.0) | |
| Unemployed | 10 (4.1) | 14 (5.8) | |
| Other | 62 (25.4) | 16 (6.7) | |
| Annual income, USD$, median (IQR) | 550 (275-894) | 275 (138-619) | <.0001 |
| Religion, n (%) | .25 | ||
| Christian | 175 (72.0) | 185 (76.8) | |
| Muslim/Islam | 49 (20.2) | 45 (18.7) | |
| Traditional/local religion | 7 (2.9) | 7 (2.9) | |
| No religion | 9 (3.7) | 4 (1.7) | |
| Other | 3 (1.2) | 0 (0) | |
| Marital status, n (%) | .006 | ||
| Married | 183 (75.0) | 192 (79.7) | |
| Single | 46 (18.9) | 28 (11.6) | |
| Divorced | 13 (5.3) | 9 (3.7) | |
| Widowed | 2 (.8) | 12 (5.0) | |
| Number of children, median (IQR) | 3 (2-5) | 4 (3-5) | .13 |
| Spouse’s highest educationb, n (%) | .004 | ||
| No school | 20 (10.9) | 7 (3.7) | |
| Primary | 93 (50.8) | 84 (43.8) | |
| Secondary | 64 (35.0) | 85 (44.3) | |
| University | 6 (3.3) | 12 (6.3) | |
| Graduate school | 0 (0) | 4 (2.1) | |
| Spouse occupationb, n (%) | .04 | ||
| Farmer | 68 (37.1) | 91 (47.4) | |
| White collar (business) | 52 (28.4) | 69 (35.9) | |
| Part-time employed | 5 (2.7) | 22 (11.5) | |
| Student | 2 (1.1) | 1 (.5) | |
| Housewife/stay at home | 46 (25.1) | 0 (0) | |
| Unemployed | 8 (4.4) | 5 (2.6) | |
| Other | 2 (1.1) | 4 (2.1) | |
| Spouse annual incomeb, USD$, median (IQR) | 206 (41-468) | 550 (275-894) | <.0001 |
IQR, interquartile range; USD$, United States dollars.
Participants were able to skip questions or refuse to answer, so not all categories will sum to total
Among individuals who reported being married; n = 375 total, 183 men and 192 women.
Health-Seeking Behaviors
Both genders reported similar health-seeking behaviors for general medical problems (eg, fever and chest pain) and one quarter of patients reported having had a prior operation. (Table 2) Men were more likely to report having visited a hospital for trauma/burns (27.5% men, 19.9% women, P = .05). Among participants who reported having had surgery and knew if the procedure was an emergency, the percentage of emergent surgery was higher for men (30/54, 55.6%) than women (20/59, 33.9%, P = .02).
Table 2.
Health-Seeking Behaviors, Stratified by Gender.
| Male |
Female |
||
|---|---|---|---|
| N (%) | N (%) | P-Value | |
| Total, Na | 244 | 241 | |
| Any hospital visit | 242 (99.2) | 239 (99.2) | NA |
| Mode of travel to district hospital | |||
| Walk | 53 (22.0) | 55 (23.0) | .79 |
| Bicycle | 88 (36.5) | 76 (31.8) | .28 |
| Car/motorbike | 37 (15.4) | 31 (13.0) | .45 |
| Other (minibus, oxcart, and ambulance) | 63 (26.1) | 77 (32.2) | .14 |
| What type of issues have you visited a hospital for? (ever)b | |||
| Malaria | 110 (45.1) | 119 (49.4) | .34 |
| Edema | 21 (8.6) | 17 (7.1) | .52 |
| Chest pain | 39 (16.0) | 54 (22.4) | .07 |
| HIV-related illness | 11 (4.5) | 7 (2.9) | .35 |
| Dyspnea | 29 (11.9) | 31 (12.9) | .74 |
| Gastrointestinal bleeding | 10 (4.1) | 18 (7.5) | .11 |
| Cancer | 9 (3.7) | 8 (3.3) | .83 |
| Diarrhea | 88 (36.1) | 94 (39.0) | .50 |
| Trauma or burn | 67 (27.5) | 48 (19.9) | .05 |
| Other | 17 (7.0) | 6 (2.5) | .02 |
| Had an operation (ever) among the 127 who had an operation | 61 (25.0) | 66 (27.4) | .55 |
| Emergencyb | 30 (55.6) | 20 (33.9) | .02 |
| Non-emergencyb | 24 (44.4) | 39 (66.1) | .02 |
| Do not know | 7 | 7 | – |
| Of the 127 who had an operation, body part operated onb | |||
| Head/neck | 3 (4.9) | 2 (3.0) | NA |
| Chest/abdomen | 24 (39.3) | 46 (69.7) | .0006 |
| Pelvis/back | 10 (16.4) | 10 (15.2) | .85 |
| Extremity | 28 (45.9) | 16 (24.2) | .01 |
| Unknown | 1 (1.6) | 1 (1.5) | NA |
| Where do you go if you have a fever? | |||
| Stay at home | 38 (15.6) | 35 (14.6) | .75 |
| Health center | 91 (37.5) | 94 (39.2) | .70 |
| Hospital | 104 (42.8) | 105 (43.8) | .83 |
| Traditional healer | 10 (4.1) | 6 (2.5) | .32 |
| Where did you go the last time you had abdominal pain? | |||
| Stay at home | 50 (20.5) | 47 (19.5) | .79 |
| Health center | 71 (29.1) | 82 (34.0) | .24 |
| Hospital | 105 (43.0) | 97 (40.3) | .53 |
| Traditional healer/other | 5 (2.1) | 5 (2.1) | NA |
| Never had abdominal pain | 13 (5.3) | 10 (4.2) | .54 |
| Experienced a burn | 51 (20.9) | 44 (18.3) | .46 |
| Mechanism of burn among those who were burnedb | |||
| Cooking fire | 13 (25.5) | 3 (6.8) | NA |
| Stove | 9 (17.7) | 4 (9.1) | NA |
| Hot water/food | 10 (19.6) | 18 (40.9) | .02 |
| Hot oil | 9 (17.7) | 15 (34.1) | .07 |
| Chemical | 4 (7.8) | 1 (2.3) | NA |
| House fire | 3 (5.9) | 0 (0) | NA |
| Other | 2 (3.9) | 2 (4.6) | NA |
| Among those who were burned, went to a health center/hospital for burn | 27 (55.1) | 20 (45.5) | .35 |
NA, not analyzable due to low response.
Participants were able to skip questions or refuse to answer, so not all categories will sum to total.
Participants were allowed to select multiple responses.
Approximately 20% reported having been burned. Only half of those with burns reported seeking care at a hospital/health center, citing reasons such as “I could handle it on my own” (9/22, 40.9% men; 16/24, 66.7% women), the burn was small (7/22, 31.8% men; 5/24, 20.8% women), and use of local healers (4/22, 18.2% men; 2/24, 8.3% women).
Approximately 95% of both genders reported having had abdominal pain in their lifetime, with almost 75% of them seeking health care at a health center or hospital during the last episode. The most common reasons for not visiting a hospital included travel distance (13/55, 23.6% men; 24/53, 45.3% women), “I could handle it on my own” (16/55, 29.1% men; 11/53, 20.8% women), wait times (10/55, 18.2% men; 6/53, 11.3% women), and medicine/physician shortages (9/55, 16.4% men; 6/53, 11.3% women).
Of the 28% who had a household member die within the last five years, 77 (40.3%) were female. Deaths occurred at home for 34 (17.8%) and in the hospital for 157 (79.1%). Of those who died, 83% visited a health center or hospital prior to dying and 18.3% had surgery within one week before death.
Barriers to Access to Surgical Care
Most participants lived within 30-40 min (<50 km) of a district hospital and traveled to the hospital by bicycle or foot. When asked why men might have more emergency surgeries, participants believed that men have more surgical conditions (42.6% men, 50.6% women, P = .08). (Figure 1) Additional common answers among both genders included: men do not actually have more surgeries (17.2% men, 19.1% women, P = .59), a lack of understanding about illness (12.7% men, 13.3% women, P = .85), and that women have to take care of children (14.3% men, 9.1% women, P = .07). Men were more likely to think that the husband/father had not given women permission to visit the hospital (8.2% men, 3.3% women, P = .02).
Figure 1.
Barriers to access to care: Responses as to why men have more emergency surgery, by gendera. aRespondents could select more than one reason; thus, percentages add up to >100%.
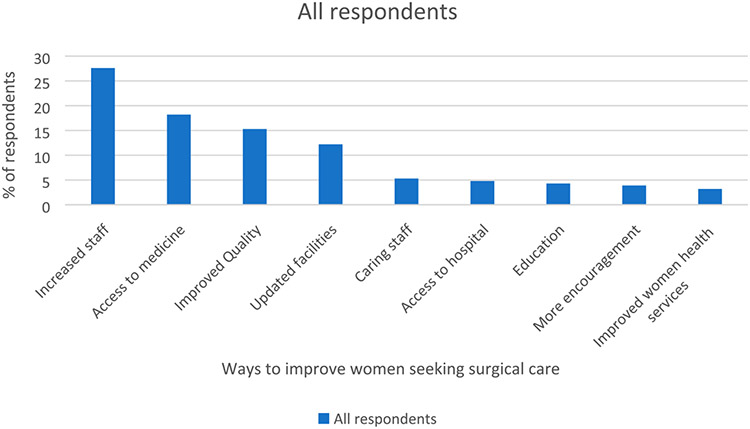
Participants believed that ways to improve women seeking surgical care could include systems-based access issues, such as increased staff (n = 224, 27.6%), access to medicine (n = 148, 18.2%), improved quality of the hospital system (n = 124, 15.3%), and updated facilities (n = 99, 12.2%). (Figure 2) Women were more likely to state that fear of surgery might prevent them from seeking care (29.1% men, 43.6% women, P = .0009). Long wait times (14.3% men, 18.7% women, P = .1991), medicine/physician shortages (7.8% men, 6.6% women, P = .63), and lack of information about when surgery is needed (8.2% men, 6.2% women, P = .40) were also mentioned.
Figure 2.
Barriers to access to care: ways to improve women seeking surgical carea. aRespondents could select more than one reason; thus, percentages add up to >100%.
Gender Equity Attitudes, Decision-Making Power, and Social Prioritization
Cultural gender norms may also play a role. Although men and women agreed that both genders share domestic responsibility, gender biases were noted. Men were more likely to agree/strongly agree that men should have the final word about household decisions (28.7% men, 19.5% women, P < .0001. (Figure 3) The majority of both genders believed that gender equality has not been achieved (61% men, 66.8% women, P = .19).
Figure 3.
Gender equity attitudes, stratified by gender.*responses to “men should have the final decision in the home” was significantly different among men and women, P < .0001.
Among married participants, men were more likely to make solo decisions about household purchases (59/182, 32.4% married men; 18/192, 9.4% married women, P < .0001) and were less likely to need to ask permission before spending money (57/182, 31.3% men; 120/192, 62.5% women, P < .0001). (Table 3) Men were more likely to think sons should be given medical preference over daughters (17.1% men and 9.3% women), while women were more likely to show preference for daughters (9.2% men, 15.6% women, P = .009).
Table 3.
Decision-Making Power, Stratified by Gender.
| Male |
Female |
||
|---|---|---|---|
| N (%) | N (%) | P-Value | |
| Total, Na | 244 | 241 | – |
| Do you ask permission from spouse before you go to a health center or hospital?b | |||
| Yes | 67 (36.6) | 67 (34.9) | .73 |
| No | 116 (63.4) | 125 (65.1) | .73 |
| Who makes decisions about health care for you?b | |||
| You | 113 (62.1) | 107 (55.7) | .21 |
| Your spouse/partner | 21 (11.5) | 17 (8.9) | .39 |
| You and your spouse together | 47 (25.8) | 65 (33.9) | .09 |
| Parents | 1 (.6) | 3 (1.6) | NA |
| Who makes decisions about major household purchases?b | |||
| You | 59 (32.4) | 18 (9.4) | <.0001 |
| Your spouse/partner | 15 (8.2) | 25 (13.0) | .14 |
| You and your spouse together | 108 (59.3) | 148 (77.1) | .0002 |
| Other | 0 (0) | 1 (.5) | NA |
| Do you have to ask permission from your spouse before spending money?b | |||
| Yes | 57 (31.3) | 120 (62.5) | <.0001 |
| No | 125 (68.7) | 72 (37.5) | <.0001 |
| Have you ever put your spouse’s health needs above your own?b | |||
| Always | 34 (18.7) | 32 (16.7) | .61 |
| Sometimes | 119 (65.4) | 134 (69.8) | .36 |
| Never, my health needs come first | 7 (3.9) | 9 (4.7) | .69 |
| Never had to | 22 (12.1) | 17 (8.9) | .31 |
| Reasons for placing spouse’s health needs above your ownc,d | |||
| I had to take care of children | 14 (9.2) | 31 (18.7) | .01 |
| I had to work | 18 (11.8) | 6 (3.6) | .01 |
| Religious reasons | 1 (.7) | 0 (0) | NA |
| My spouse was more ill than I was | 51 (33.3) | 44 (26.5) | .18 |
| My spouse’s health is more important than mine | 9 (5.9) | 7 (4.2) | .50 |
| My spouse makes the decisions about how we treat our health problems | 4 (2.6) | 6 (3.6) | NA |
| Problems with transportation | 10 (6.5) | 11 (6.6) | .97 |
| I didn’t think anything was wrong with me | 6 (3.9) | 2 (1.2) | NA |
| Money reasons | 39 (25.5) | 26 (15.7) | .03 |
| My spouse is the bread-winner | 11 (7.2) | 41 (24.7) | <.0001 |
| Other | 3 (2.0) | 1 (.6) | NA |
NA, not analyzable due to low response.
Participants were able to skip questions or refuse to answer, so not all categories will sum to total.
Among married participants, n = 375 total, 183 men and 192 women.
Among married participants that said always or sometimes for “Have you ever put your spouse’s health needs above your own?“, n = 319, 153 men and 166 women.
Participants were allowed to select multiple responses.
Discussion
This investigation provides insight into community perceptions of gender biases and reasons that women might have for not seeking surgical care in Malawi. The study is unique because the few studies that delve into surgical disparities in Africa based on gender are mostly limited to cataract surgery and do not examine why these surgical disparities might exist.10,11 One study in the Republic of Congo showed that 96% of patients experienced a barrier to surgical care, with cost, female sex, and lack of surgeon associated with increased odds of post-operative complication, highlighting some similar issues around gender and infrastructure that may be prevalent in Malawi.12
Health-Seeking Behavior
Our prior study at KCH showed that among patients with peritonitis, women were operated on less frequently.4 As to why this difference was noted, the majority of survey participants in this study thought that men simply have more surgical conditions. This may be true, and certainly diagnosis of peritonitis in women may be more challenging; however, the original study excluded trauma, obstetric and gynecological conditions, and hernias, and women also experienced delays in presentation, delays to operation, and longer LOS. Some survey participants believed that women may lack understanding or have more childcare responsibilities. These answers uncover some inherent biases. If sociocultural norms dictate that women are the caregivers, women may be expected to prioritize child-rearing and may be less likely to seek care. Men were also more likely to think that a male figure had not given the women permission to go to the hospital. This perception highlights some paternalistic views that mirror findings from the United Nations State of the World Population report that reveals only 48% of sub-Saharan African and 53% of Malawian women feel they have the power to make choices regarding their own sexual activity, contraception, and general health care.13
Barriers to Access to Surgical Care
In our study, women were more likely to express fear of surgery as a possible barrier. It is important to note that these are perceptions and may not reflect actual practice. That being said, some of this fear might stem from women feeling less in control of surgical options and decision-making. The fear may also be couched in real experiences with an under-resourced health care system. The majority of participants who had family die reported that the deceased had died in the hospital or recently visited a hospital, and many had had surgery. Even if the surgery itself did not directly cause death, this association could erode trust, especially for individuals with limited health literacy. Of those who died at home, we do not know how many died from surgical diseases. One Rwandan survey showed that 30% of household deaths might have been surgically preventable but how this might translate to the Malawian population has not been studied.14
Lack of infrastructure is perceived as a large barrier and seems to further diminish trust, but unfortunately may be one of the more difficult obstacles to overcome. The WHO report discusses how often women in Africa do not seek care because it is both poor quality and not gender sensitive, citing examples of women being forced to deliver in the dorsal position rather than traditional squatting position, inability to be examined by female providers, and lack of family planning services.1 Women may feel that the system does not provide the resources they need and thus they avoid hospitals. Also of note, women had lower incomes and education levels and lived farther from the hospital, which might play into their ability to seek care.
Gender Equity Attitudes, Decision-Making Power, and Social Prioritization
Social prioritization and the belief of both genders that gender equality has not been achieved may further compound the problem. Our findings of men prioritizing sons differ slightly from those of a recent smaller study on gender roles in Malawi, in which women also prioritized sons over daughters for medical care.15 That study also demonstrated that women were more likely to underutilize health care. The responses underscore subtle societal norms in which men may have more independence and give preferential treatment to sons. If these views are pervasive enough, they could lead to fewer women independently seeking care, or the prioritization of men who come to the hospital by health care personnel. Two issues that were not evaluated in this study are the biases of health care personnel and the potential increased difficulty in diagnosing surgical diseases in women. If inherent biases are present in the community, they may exist in the health care system as well.
Study limitations include the systematic sampling; relying on clerks to choose the nth person from a cluster could cause selection bias. Participants from the hospital would not necessarily represent community members who choose not to visit hospitals and may not represent those who live in small villages, although sampling the marketplace reduces some of this bias. Results may not be generalizable, although the demographics of the rural and urban participants were similar enough to be combined and were reasonably representative of Malawians based on age, income, employment, religion, and education.16 Participants may not have been able to recall events exactly or may have responded to questions to appease the interviewers. While there were several open-ended questions, the queries may not have covered all potential causes of gender disparities.
In conclusion, this survey of Malawian perceptions of gender-based access to surgical care highlighted certain themes, including gender equity attitudes, social determinants, and issues in health care infrastructure, quality, and availability. If these perceptions are driving health-seeking behaviors, identifying these problems is the first step. Changes in education and health infrastructure could empower women to seek care but may be difficult to enact given poor resources. The health care system needs more workers, but specifically it needs more females holding positions of authority to give women the power and voice to direct change.1 At KCH, UNC has partnered with the hospital to support a local surgery residency program, which has now trained four female general surgeons and one female orthopedic surgeon. One of these women is on staff at KCH and the others work in Blantyre and Mzuzu. Changing local infrastructure and empowering women to take over their own care are steps in the right direction, but there is still a long way to go. Future plans include surveying health care personnel to identify any provider biases that might be addressed with education, and layperson education sessions about surgical problems.
Supplementary Material
Key Takeaways.
In Malawi, perceptions of gender-based access to surgical care may be influenced by gender equity attitudes, social determinants, and issues in the health care system infrastructure quality and availability.
Both genders reported long wait times, medicine/physician shortages, and lack of information about when surgery is needed as potential barriers to seeking surgical care.
Few Malawians surveyed felt that gender equality has been achieved, and men were more likely to state that medical preference should be given to sons and that men should have the final word about household decisions and expenditures.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Dr. Paula Strassle is supported by the Division of Intramural Research, National Institute of Minority Health and Health Disparities, and National Institutes of Health.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Disclaimer
The contents and views in this manuscript are those of the authors and should not be construed to represent the views of the National Institutes of Health.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.World Health Organization. Addressing the challenge of women’s health in Africa. Report of the commission on women’s health in the African region. Republic of Congo: WHO Regional Office for Africa. 2012:6. [Google Scholar]
- 2.UNICEF. Annual Results Report Gender Equality. NY: UNICEF. 2017. https://www.unicef.org/media/47776/file/Annual_Results_Report_2017_Gender_Equality.pdf. Accessed April, 2018. [Google Scholar]
- 3.Whitehead M The concepts and principles of equity and health. Int J Health Serv. 1992;22(3):429–445. [DOI] [PubMed] [Google Scholar]
- 4.The Agency for Healthcare Research and Quality. Healthcare Quality and Disparities in Women. Rockville, MD: Agency for Healthcare Research and Quality. 2010. https://archive.ahrq.gov/research/findings/nhqrdr/nhqrdr10/women.html. Accessed April 2018. [Google Scholar]
- 5.Reid TD, Wren SM, Grudziak J, Maine R, Kajombo C, Charles AG. Sex disparities in access to surgical care at a single institution in Malawi. World J Surg. 2019;43(1):60–66. [DOI] [PubMed] [Google Scholar]
- 6.Gale SC, Shafi S, Dombrovskiy VY, et al. The public health burden of emergency general surgery in the United States: A 10-year analysis of the Nationwide Inpatient Sample: 2001 to 2010. J Trauma Acute Care Surg. 2014; 77(2):202–208. [DOI] [PubMed] [Google Scholar]
- 7.The DHS Program. Demographic and Health Surveys Methodology Questionnaire- Phase 7, Household Woman’s and Man’s. Rockville, MD: ICF International. 2015. https://dhsprogram.com/publications/publication-dhsq7-dhs-questionnaires-and-manuals.cfm. Accessed April 2018. [Google Scholar]
- 8.Barker GCJ, Contreras JM, Heilman B, et al. Evolving Men: Initial Results from the International Men and Gender Equality Survey (IMAGES). Washington DC: International Center for Research on Women. 2011. https://promundoglobal.org/programs/international-men-and-gender-equality-survey-images/. Accessed April 2018. [Google Scholar]
- 9.Tisdell C Gender inequality in India: evidence from a survey in rural West Bengal. Int J Soc Econ. 2002;29(9): 706–721. [Google Scholar]
- 10.Dean WH, Patel D, Sherwin JC, Metcalfe NH. Follow-up survey of cataract surgical coverage and barriers to cataract surgery at Nkhoma, Malawi. Ophthalmic Epidemiol. 2011; 18(4):171–178. [DOI] [PubMed] [Google Scholar]
- 11.Nkomazana O Disparity in access to cataract surgical services leads to higher prevalence of blindness in women as compared with men: results of a national survey of visual impairment. Health Care Women Int. 2009;30(3):228–229. [DOI] [PubMed] [Google Scholar]
- 12.Lin BM, White M, Glover A, et al. Barriers to surgical care and health outcomes: a prospective study on the relation between wealth, sex, and postoperative complications in the Republic of Congo. World J Surg. 2017;41(1):14–23. [DOI] [PubMed] [Google Scholar]
- 13.United Nations Population Fund. State of the World Population, 2021. New York, NY: UNFPA; 2021:19–21. [Google Scholar]
- 14.Petroze RT, Joharifard S, Groen RS, et al. Injury, disability and access to care in Rwanda: results of a nationwide cross-sectional population study. World J Surg. 2015;39(1):62–69. [DOI] [PubMed] [Google Scholar]
- 15.Azad AD, Charles AG, Ding Q, Trickey AW, Wren SM. The gender gap and healthcare: Associations between gender roles and factors affecting healthcare access in central Malawi, June-August 2017. Arch Publ Health. 2020;78(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Central Intelligence Agency. The World Factbook- Malawi. 2018. https://www.cia.gov/the-world-factbook/countries/malawi/. Accessed August 9, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.