Since the start of the SARS-CoV-2 pandemic, numerous planned surgeries have been postponed or canceled up until now. Previous research showed that hospitals discriminately managed postponements and cancellations of surgeries primarily based on urgency and regional infection incidence (1). Operations in patients who postoperatively require intensive care treatment do constitute a special case. On the one hand, these cases are typically urgent, so preferential treatment of such patients could have been expected even during the pandemic. On the other hand, these cases competed with COVID-19 cases in terms of intensive care unit (ICU) resources.
A recently published study on the impact of lockdowns in 61 countries on postponement or cancellation of cancer surgery showed that the risk of postponement was increased especially in cases requiring complex cancer surgery (2). Rather than limited surgical capacity, limited intensive care resources appear to have contributed to the postponement of these operations or a change in management regime to the detriment of the affected patients.
The aim of this study was to evaluate the impact of regional ICU occupancy on the number of cases undergoing surgery usually requiring postoperative ICU treatment.
Footnotes
Conflict of interest statement
Olga Karaca, MPH, and Dr. Bialas are employees of digmed.
Dr. Rüggeberg is a member of the Professional Society of German Surgeons (BDC), Prof. Schuster is member of the Professional Association of German Anesthesiologists (BDA). Both are members of the Advisory Board of the OR Benchmarking Program of the BDA, BDC and Professional Association of OR Management (VOPM). The OR Benchmarking Program is technically implemented by digmed.
Methods
The case number analysis is based on surgical process data of hospitals participating in the Benchmarking Program of the Professional Association of German Anesthesiologists (BDA, Berufsverband Deutscher Anästhesisten), Professional Society of German Surgeons (BDC, Berufsverband der Deutschen Chirurgen) and the Professional Association of OR Management (VOPM, Verband für OP-Management). We analyzed the changes over time in case numbers per month and case numbers per hospital during the second and third wave (1 September 2020 to 31 August 2021) of the SARS-CoV-2 pandemic. For comparison on the hospital level, the mean number of cases of the corresponding months for the period 2017–2019 were used; weekends and holidays were not taken into account. Hospitals were split into two equally sized groups based on the proportion of COVID 19 patients with ICU treatment in their respective districts or cities with district status during the peak of the second wave (mean of December 2020 and January 2021): hospitals with higher COVID-19 load and hospitals with lower COVID-19 load in their districts or cities.
Data were analyzed on a district level to take regional clusters into account (3). Calculation of ICU occupancy was based on the data reported by hospitals to the DIVI Intensive Care Registry of the German Interdisciplinary Association of Intensive Care Medicine and Emergency Medicine (DIVI, Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin) during the study period.
From the 500 most frequently coded Operation and Procedure codes (OPS) of all participating hospitals, we selected those that we considered to be frequently or usually associated with a postoperative ICU stay. Only hospitals that submitted an OPS for at least 80% of surgical procedures across all years and performed at least three procedures of the included OPS per month in the period 2017–2019 were considered for analysis of these procedures. Using the Mann-Whitney test, each month of the analyzed period was examined as to whether the mean percentage change in case numbers differed between the two groups (assumed p value <0.05). Calculations were performed using Stata version 14.2 (StataCorp LLC College Station, Texas, USA).
Results
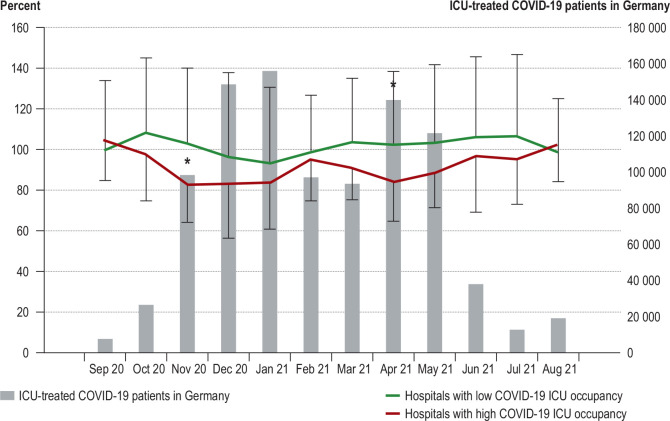
A total of 113 445 surgical procedures usually associated with postoperative ICU admission from 52 hospitals (24 secondary care hospitals, 15 tertiary care hospitals and 13 university hospitals) were analyzed. The Figure shows the changes over time in the number of these cases as a percentage compared to the previous three years for each group of 26 hospitals with either a higher or lower ICU occupancy by COVID-19 patients. Cut-off between the two groups was a proportion of COVID-19 patients of 18.29% of all ICU patients. In addition, the Figure shows the changes in the total number of COVID-19 cases with ICU treatment in Germany during the analysis period. The hospitals more affected by COVID-19, but not the hospitals less affected by COVID-19 showed continuously reduced case numbers for critical surgeries. Statistical differences between the two groups were found for November 2020 (p = 0.0386) and April 2021 (p = 0.0281). The Table shows the reduction in the number of cases by specialty.
Figure.
Changes over time in the number of cases with surgical procedures usually associated with postoperative ICU treatment (in percent compared to the previous years) in relation to COVID-19 ICU occupancy;
*Differences (p<0.05) between the groups
Table. Number of included surgeries usually associated with postoperative ICU treatment by specialty and extent of reduction during the peak of the second SARS-CoV-2 wave.
| Specialty | Surgeries | Hospital case number changes over time (Nov 20–Jan 21) | |
| High COVID-19 ICU occupancy | Low COVID-19 ICU occupancy | ||
| Vascular surgery | 31 304 | −22 % | −5 % |
| Cardiac surgery | 30 824 | −20 % | −22 % |
| Neurosurgery | 22 722 | −13 % | 2 % |
| Thoracic surgery | 10 186 | −22 % | 2 % |
| Urology | 12 135 | −22 % | −13 % |
| Visceral surgery | 6 274 | 2 % | −9 % |
Discussion
In hospitals from districts with higher COVID-19 ICU load, the numbers of cases of the considered surgical procedures declined significantly throughout the analysis period.
The consequences of postponement of surgery for the patient were not the subject of this study. The COVIDSurg Collaborative study performed a cumulatively analysis of data from 61 countries, including Germany, and found that one of seven cancer patients did not receive potentially life-saving surgery due to the pandemic-related lockdowns (2). In the data evaluated here, no catch-up effect was observed in hospitals with high COVID-19 ICU occupancy. Consequently, there are concerns that the pandemic not only resulted in a high mortality rate due to the pandemic disease itself, but also increased the mortality rates for other diseases due to limitations in the provision of surgical care and due to reduced ICU capacities (4). Thus, it would seem necessary to develop strategic concepts to mitigate such effects (5).
In order to prevent excessive demands on local and regional structures, so-called cluster and cloverleaf concepts have been developed for the care of COVID-19 patients requiring ICU treatment (3). A similar cross-border, nationwide cooperation may be necessary in Germany to ensure that patients in need of elective but critical surgery receive treatment even in situations of prolonged strain on ICU resources.
References
- 1.Karaca O, Rüggeberg JA, Schuster M. Zweite Pandemiewelle: Rückgang der Operationen variiert. Dtsch Arztebl. 2021;118:A824–A825. [Google Scholar]
- 2.COVIDSurg Collaborative. Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol. 2021;22:1507–1517. doi: 10.1016/S1470-2045(21)00493-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pfenninger EG, Naser J, Träger K, et al. Die Pandemie bewältigen - Verlegungskonzept von COVID-19-Intensivpatienten und Non-COVID-19-Intensivpatienten in Baden-Württemberg. Anaesthesist. 2021;70:951–961. doi: 10.1007/s00101-021-00961-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Søreide K, Hallet J, Matthews JB, et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020;107:1250–1261. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bennett S, Søreide K, Gholami S, et al. Strategies for the delay of surgery in the management of resectable hepatobiliary malignancies during the COVID-19 pandemic. Curr Oncol. 2020;27:e501–e511. doi: 10.3747/co.27.6785. [DOI] [PMC free article] [PubMed] [Google Scholar]