Abstract
Endothelial dysfunction (ED) has a substantial role in the pathogenesis of atherosclerosis and other vascular diseases. Multiple risk factors, including smoking, hyperlipiadaemia and diabetes, can have associated ED, which is correlated with cardiac events. Measurement of coronary artery endothelial function requires the use of invasive techniques to assess both epicardial coronary artery and microvascular beds. Peripheral vascular techniques and endothelial biomarkers can be used to indirectly assess coronary ED. In this review of coronary artery ED, we discuss the current state of the field, the techniques used to measure ED and its clinical implications.
Keywords: Microvascular Angina, RISK FACTORS, CORONARY ARTERY DISEASE, Atherosclerosis
Introduction
The accumulation of atherosclerosis over many years leads to the coronary artery disease (CAD), which presents clinically as stable angina or acute coronary syndrome. Stable CAD consists of a broad range of coronary pathophysiology, including obstructive CAD and non-obstructive CAD, resulting in angina and inducible ischaemia. The conductive and resistance vessels of the coronary arterial circulation play a key role in matching the delivery of blood to the metabolic demands of the myocardium.1 The sole mechanism of increasing blood flow to meet increased myocardial metabolic demand is the dilation of small coronary arterioles. In endothelial dysfunction (ED), the small arterioles lose their ability to dilate when needed, and this is a principal determinant of myocardial ischaemia. In addition, in the large epicardial coronary arteries, ED is the earliest measurable deterioration of the vessel wall in atherogenesis and precedes the development of morphological changes.2 3
The vessel lumen is lined with endothelium, the main regulator of vascular homeostasis.3 The endothelium serves as a selective barrier and is the source of multiple vasoactive substances which help to maintain vascular tone and regulate haemostasis and inflammation. Altered vascular function alters coronary blood flow and contributes to atherosclerosis lesion development and progression. ED is an early marker of atherosclerosis, and many risk factors for CAD are associated with altered ED.2 3 Thus, ED not only affects epicardial and microvascular coronary blood flow but also plays an important role in the development of atherosclerosis.
Epidemiology and risk factors
The prevalence of coronary ED is not fully known, and its position in both macrovascular atherogenesis and microvascular disease makes it difficult to differentiate from related disease processes. However, observational studies have demonstrated that 65%–90% of patients with chest pain and non-obstructive CAD have coronary microvascular abnormalities,4 5 with 50%–70% reported having endothelium-dependent vascular dysfunction.5 Given its role in coronary macrovascular and microvascular dysfunction, the prevalence of coronary ED may be in the millions in the USA alone.
Risk factors for coronary ED tend to correlate with those of macrovascular and microvascular disease. ED has been demonstrated in patients with risk factors such as hypercholesterolaemia, hypertension, smoking, diabetes, autoimmune disease and ageing, and in patients with preclinical or clinical atherosclerotic disease.2 3 Smoking, for example, has a dose-dependent association with ED, which is reversible with smoking cessation. Several of these associations are related to metabolic processes. Elevated low-density lipoprotei and triglycerides with reduced high-density lipoprotein predispose to ED.3 6 In addition, type 2 diabetes and obese patients even in the absence of CAD have higher rates of ED,7 and hyperglycaemia alone can induce ED in otherwise healthy individuals.8 Obstructive sleep apnoea and atrial fibrillation also correlate positively with ED, and even mental stress is a risk factor.9 ED progression appears to be related to the intensity and duration of risk factors of individual patients. Although it is difficult to ascertain causation, these factors all appear to be prospectively associated with ED.
Pathophysiology
Endothelium serves as a selective barrier to control permeability, and it releases many vasoactive substances to regulate vascular tone and remodelling. The release of nitric oxide (NO), prostacyclin and endothelium-derived hyperpolarising factor result in vasodilation, whereas endothelin-1 and thromboxane release result in vasoconstriction.10 Cardiovascular (CV) risk factors impair vascular function such as vasomotor tone and increase vessel thrombosis, smooth muscle cell proliferation and leucocyte adhesion and migration. Both epicardial and microvascular coronary ED are predictors of CV events, irrespective of the presence or absence of angiographically detectable lesions.11
Increased coronary blood flow is necessary to meet increased metabolic demand. Among the effects of ED is the loss of small arterioles’ ability to dilate, which is a primary mechanism of regulating blood flow. ED in epicardial vessels not only affects coronary blood flow, but a loss of NO bioavailability contributes to the initiation and progression of atherosclerosis through alterations in endothelial permeability, inflammatory activation and increased thrombosis.12 Microvessel ED contributes to ischaemia in the absence of occlusive CAD but has also been implicated in contributing to impaired left ventricular relaxation and cardiomyopathy.12 Further, vascular smooth muscle cell hyperreactivity appears to be connected to ED, which is involved in coronary vasospasm.13
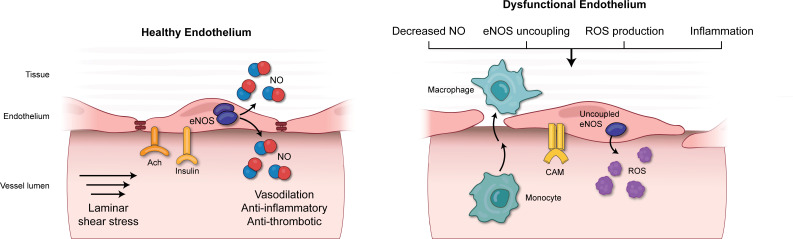
NO produced by the enzyme endothelial NO synthase (eNOS or Nos3) plays a critical role in maintaining endothelial function (EF). Laminar shear stress, insulin and acetylcholine (Ach) are known agonists for eNOS (figure 1) and induce the production of NO. Animal studies have shown that NO inhibits inflammation (reducing NF-κB signalling), reduces vascular smooth muscle proliferation, and reduces platelet aggregation.14 A reduction in NO bioavailability, either by decreased production or increased destruction, results in ED.
Figure 1.
An overview of nitric oxide (NO) signalling in both healthy (left) and dysfunctional (right) endothelium. Healthy endothelium maintains physiological vascular function through the beneficial effects of NO. The endothelium maintains tight junctions and has an anti-inflammatory and antithrombotic phenotype. Laminar shear stress, insulin and acetylcholine stimulate eNOS to produce NO. The dysfunctional endothelium is characterised by decreased NO production, an inflammatory phenotype shown by increased expression of cell adhesion molecules (CAMs), increased permeability shown by increased migration of vascular monocytes and increased leucocyte infiltration. Instead of forming a dimer, eNOS becomes uncoupled, resulting in the production of reactive oxygen species (ROS) instead of NO. The reduced level of NO and increased ROS lead to the initiation and progression of atherosclerosis.
A variety of factors may damage endothelial cells, resulting in ED. Physical injury such as alterations in fluid shear stress and metabolic stress can result in reduced NO production. Immune-related damage initiated by infection or systemic inflammatory diseases can also reduce NO bioavailability. Oxidative stress plays an important role in increasing the production of reactive oxygen species (ROS) through several mechanisms. These include uncoupling eNOS, increasing mitochondrial ROS production, and increasing nicotinamide adenine dinucleotide phosphate-oxidase activity in the vessel wall. All of these interacting pathologies contribute to the initiation and progression of atherosclerosis.15 The pathophysiology of ED is illustrated in figure 1.
Evaluation of coronary artery EF
Direct measurements
Intracoronary infusion of agonists and quantitative angiography to assess vasomotion is considered the gold standard method for direct quantification of coronary EF. Direct invasive testing evaluates endothelium-independent function by the use of adenosine and endothelium-dependent circulatory components by infusion of Ach.16 Infused Ach dilates healthy epicardial coronary arteries, but patients with ED exhibit reduced dilation or even coronary vascular constriction when exposed to intracoronary Ach. This response can be associated with angina and ischaemia. Thus, the concept that atherosclerosis is simply a structural disease has expanded to include functional outcomes such as paradoxical vasoconstriction from ED.
Direct observation of changes in blood vessel diameter in the cardiac microcirculation is not possible, however, changes in coronary blood flow can be measured by use of the thermodilution technique or an intracoronary Doppler ultrasound wire. These invasive coronary physiology techniques have been a valuable addition in evaluating patients with angina that have non-obstructive CAD by diagnostic angiogram. Many of these patients are diagnosed with angina with no obstructive CAD (ANOCA), a term which includes patients with coronary microvascular disease, coronary artery ED (both macrovascular and microvascular) and epicardial vasospasm. Normal responses to Ach include vasodilation and an increase in coronary blood flow of at least 50% above baseline. Adenosine largely tests the non-endothelial component and vasodilatory reserve of the microcirculation. Although coronary flow reserve combines both epicardial and microcirculatory flow, in patients with ANOCA, coronary flow reserve primarily represents microcirculatory function.2 Efforts to standardise the invasive assessment of ANOCA patients have been proposed. These include standard coronary angiogram, assessment of coronary microvascular function by intravenous adenosine, coronary artery EF by IV Ach and coronary vasospasm assessment by high-dose intracoronary AcH.17 18
Indirect measurements
Invasive techniques may be suitable for patients undergoing angiography but are not suitable for the assessment of asymptomatic patients or for use in large clinical studies. Non-invasive measures of EF have been used with the assumption that systemic EF reflects coronary artery EF. However, these non-invasive systemic measures of EF cannot fully recapitulate coronary EF assessment, because they are not influenced by localised coronary shear stress.
Flow-mediated dilation (FMD) uses ultrasound of the brachial artery to measure peripheral macrovascular EF under physiological reactive hyperaemia, a surrogate for coronary EF.19 The maximal artery diameter and the preocclusion and postocclusion maximal diameters are measured, often with the inclusion of flow velocity. Early research showed a weak relationship between forearm FMD and direct measurements of coronary EF. However, improved methodology and technology have greatly improved the reliability and clinical utility of FMD. For example, in patients referred for cardiac catheterisation who underwent FMD using current guidelines, FMD was strongly correlated with AcH-induced coronary artery dilation (r=0.77).20
FMD-induced and AcH-induced coronary artery responses are the most widely used assessments of NO-mediated vascular function in both systemic and coronary vasculature. Early research showed that inhibition of eNOS abolished brachial FMD responses. However, investigators using up-to-date FMD protocols found that NO may contribute less than 20% of the FMD response.21 Similarly, evidence suggests that AcH-induced coronary artery vasodilation is not always NO mediated.22 With increased CV risk factors, NO may have a lesser role in FMD and coronary vasodilation. Mechanistically, endothelin and oxidative stress, which are increased with known vascular disease, may play a greater role than NO.
Peripheral artery tonometry (PAT) assesses microvascular EF via changes in a digital pulse waveform (peripheral arterial tone) in response to reactive hyperaemia. A probe on the index finger measures the waveform preocclusion and postocclusion of the brachial artery. These values are quantified by the reactive hyperaemia–PAT index.23 The reactive hyperaemia index (RHI) estimates peripheral microvascular function and is a combined measure of endothelium-dependent and endothelium-independent function. With a focus on microvasculature, RHI is distinct from FMD and there is little correlation between them. RHI is lower in patients with diabetes, hypertension, obesity and smoking.24 Studies looking at the relationship between coronary microcirculation and peripheral microvascular function by RHI have had variable results,25 possibly as a result of differing methodologies. The link between RHI and coronary microcirculation is now an area of active research.
ED biomarkers
Blood endothelial biomarkers (table 1) have the potential to greatly aid ED diagnosis and are important alternatives to traditional methods for diagnosing and stratifying the CV risk of diseases in their earliest stages. A growing body of evidence supports their measurement as the easiest and most informative way to evaluate EF.26 Biomarkers of ED are generally derived from pathways involved in NO production, coagulation and inflammation, and interest in them has increased as alternatives to direct measures of ED.
Table 1.
Biomarkers of ED
| Biomarker class | Biomarkers |
| Blood laboratory values | Thyroid function |
| Uric acid level | |
| Lipoprotein-associated phospholipase A2 | |
| C reactive protein | |
| White cell count | |
| N-terminal brain natriuretic peptide | |
| Endothelial activation | Cell adhesion molecules: |
| Soluble products of E-selectin | |
| Intercellular adhesion molecule 1 | |
| Vascular adhesion molecule 1 | |
| Coagulation cascade: | |
| von Willebrand factor | |
| Soluble thrombomodulin | |
| Endothelial microparticles | Fluorescence-activated cell sorting (FACS) based on CD31, CD105, (endoglin) and CD142 expression. |
| Multiple potential component biomarkers | |
| Endothelial-specific and associated with endothelial inflammation and ED | Endothelial cell-specific molecule-1 (endocan) Endoglin |
ED, endothelial dysfunction.
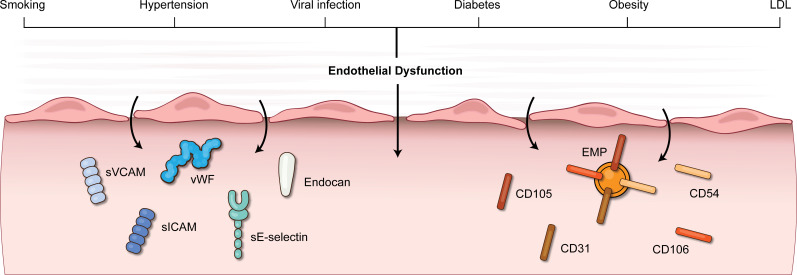
Factors released on endothelial injury can be detected and potentially used as more specific, circulating markers of ED. Endothelium activation in the context of CV risk factors or host defence and inflammatory activation causes important signalling changes that can be used as biomarkers. Numerous CV risk factors (figure 2) are associated with altered endothelial signalling from NO-mediated anti-inflammatory activity, NO-mediated silencing of redox signalling and vasoconstriction.2 3
Figure 2.
Risk factors leading to endothelial dysfunction, and possible biomarkers found in circulation. EMP, endothelial microparticles. sICAM, soluble intercellular adhesion molecule. sVCAM, soluble vascular cell adhesion molecule. vWF, von Willebrand factor.
Endothelial microparticles (EMPs), complex vesicular structures shed from activated, injured or apoptotic endothelial cells,26 are potentially highly specific biomarkers for ED. They are enriched in endothelial cell proteins and can be measured in plasma. Significant increases in these particles are associated with CV risk factors associated with ED, but the requirement for their preparation byfluorescence-activated cell sorting (FACS) and differing methodologies have largely confined these techniques to clinical research.26
Two candidate biomarkers that would avoid the necessity for flow sorting and are highly specific to endothelium and ED are endothelial cell-specific molecule-1 (endocan) and endoglin.
Endocan is a soluble proteoglycan mainly secreted by endothelial cells from both the systemic and coronary vasculature. Inflammatory factors increase the expression and release of endocan, resulting in increased expression of adhesion molecules. Changes in plasma levels of endocan reflect endothelial activation. High endocan levels may represent an increased risk for the onset of CV disease,27 increased risk for adverse events following ACS28 or increased adverse events following MI.29 Alterations in endocan levels have been associated with hypertension and diabetes. Although endocan is not specific to the coronary circulation, its specificity for ED approaches that of EMP, reflects EF and has the characteristics necessary for clinical use.
Endoglin, also called CD105, is found primarily in the plasma membrane of proliferating endothelial cells and is part of the TGF-β receptor complex.30 Cleavage of this receptor results in the release of soluble endoglin (sEng). Although its physiological function opposes that of its parent receptor, sEng may be a useful marker of endothelial damage. Risk factors for ED, such as hyperlipidaemia, hypertension and diabetes, are associated with sEng levels.31 However, there is variable consistency across studies and it has been hypothesised that sEng is an early marker of ED but that levels then decrease as the disease progresses.32 Overall, sEng has yet to show the same level of sensitivity and specificity as endocan for ED.
Due to the complexity of EF, many of the current biomarkers do not provide consistent information about coronary EF. Additional clinical investigations with these newer biomarkers may provide more insight. Using multiple biomarkers or using them in combination with non-invasive measures of EF has also been proposed to increase the utility of these biomarkers.
Clinical use and implications
Clinical associations
The association of ED with epicardial CAD as well as disease of other large vessels is well documented. Considering that ED may be an early component of atherogenesis, this has raised the question of whether ED is an independent predictor of future CV events. Studies using various techniques to assess ED and its association with prognosis are presented in table 2. For asymptomatic CV patients, ED testing seems to add little to prognosis compared with traditional risk-factor assessment; however, for symptomatic CV patients, ED may play a role in prognosis. Coronary ED has been associated with coronary plaque progression,33 vulnerable plaque features,34 increased risk of major adverse CV events,35 cerebrovascular events,36 thrombotic events37 and congestive heart failure.38 Finally, the value of ED measurement may be further increased if restoration of normal EF by lifestyle interventions or drugs is found to reduce CV risk.
Table 2.
Examples of clinical studies utilising endothelial function for prognosis
| Clinical study | Study subjects | Author, year | N | Endo measure | Predictive? |
| Cardiovascular health study | Older adults, asymptomatic | Yeboah, J, 2007 Circulation |
2792 | FMD | +/- Predictive, but adds little to prognostic accuracy of traditional risk factors |
| Multiethnic study of atherosclerosis | Avg age 61, white, Chinese, Black, Hispanic, asymptomatic | Yeboah J, 2009 Circulation |
3026 | FMD | + |
| Firefighters and their endothelium | Healthy firefighters | Anderson TJ, 2011 Circulation |
1574 | FMD | – |
| Patients with chest pain | Patients with CAD and without CAD on coronary angiogram | Halcox, J PJ, 2002 Circulation |
308 | Intracoronary AcH | + (for patients with CAD and without) |
| Patients with vascular disease | Patients undergoing vascular surgery | Gocke, N, 2003 JACC |
199 | Brachial FMD | + |
| Symptomatic outpatients with chest pain | Patients with low-risk findings on stress study or absence of obstructive lesions on angiogram | Rubinshtein R, 2010 European Heart Journal |
329 | Endo pat | + |
| Patients with stable CAD | Patients with CAD proven angiographically | Sinning, J-M, 2010 European Heart Journal |
200 | CD31+/annexin V+microparticles | + |
AcH, acetylcholine; CAD, coronary artery disease; FMD, flow-mediated dilation.
Additional studies have revealed multiple cardiac conditions with a higher incidence in the setting of ED. Typical angina, even in the absence of CAD, correlates with more severe coronary ED,39 highlighting a potential role in microvascular angina. More controversially related to angina, myocardial bridging is closely associated with ED.40
ANOCA is an inclusive term for chest pain syndrome without obstructive CAD. Large retrospective studies demonstrate a prevalence of nonobstructive CAD of 40%–60% of all referrals.41 Up to two-thirds of patients with non-obstructive CAD have coronary ED represented by microvascular dysfunction or epicardial artery spasm following AcH.42 In addition, coronary ED in both epicardial and microvascular vessels is a significant contributor of chest pain. In patients with nonobstructive CAD, both epicardial and microvascular ED were found to be independent predictors of acute CV events (stroke, MI and CV death).43
Coronary ED showed a 5.8-fold increase in relative risk of development of atrial fibrillation among patients with chest pain and non-obstructive CAD.44 ED is associated with cardiac amyloidosis, possibly reflecting the vascular changes that occur with this disease. Impressively, 81% of patients with heart failure with preserved ejection fraction (HFpEF) have coronary microvascular dysfunction,45 of which a large fraction is driven by ED and is exercise associated,46 suggesting a plausible role for ED in the pathophysiology of HFpEF. Furthermore, in orthotopic heart transplant patients, ED is associated with the incidence and progression of coronary allograft vasculopathy, as well as cardiac death.47
COVID-19 is an additional cause of ED that undoubtedly influences cardiac processes. The specific relationship between SARS-CoV-2 infection and coronary EF is currently unknown, but ED as measured by FMD was present with an OR of 3.6 2 months after infection.48 Similar results have been shown by PAT.49 The virus is known to directly infect endothelium, and systemic cytokine activation can also cause ED. Further, COVID-19-induced ED has been associated with inflammation, vasoconstriction and coagulation,50 which would provide a plausible relationship between this viral disease and the known higher rates of coronary events.
Overall, the wide breadth of clinical associations indicates the high potential impact of an ED-targeted therapeutic or intervention.
Future directions
ED is associated with the initiation and progression of CAD and predicts poor CV outcomes.
The ability to measure EF has increased our understanding of one aspect of vascular disease progression. A comprehensive approach would incorporate EF, traditional risk factors, genetic predisposition and clinical assessment.
The development of validated, clinically usable biomarkers is vital to expanding clinical EF assessment and will enable testing of larger populations and serial measures. For the assessment of preclinical disease or interventions, methods should be non-invasive, easy to use, low cost and reproducible. The development of biomarkers with the necessary sensitivity and specificity for ED is an essential step toward more widespread clinical use. Although many non-invasive assessment techniques are available and easy to use, standardised protocols are required for accurate and reproducible results. The combined use of biomarkers and non-invasive EF measures for prognosis and clinical studies of asymptomatic at-risk patients warrants future studies.
Patients suffering from ANOCA with ED represent a large population of undertreated patients. Patients undergoing diagnostic angiography would likely benefit from endothelial provocation with AcH and adenosine testing if protocols become more standardised and available. The development of non-invasive measures would allow testing in ANOCA patients who are not undergoing invasive angiography and would be useful in assessing potential therapies for this subgroup of patients.
Footnotes
Twitter: @obtusediagonal
Contributors: LB: paper writing. FK: editing, paper writing.
Funding: This study was funded by R01 DK106703, R01 HL139555, John L. Locke Jr. Charitable Trust and from Kenneth H. Cooper Endowed Professorship in Preventative Cardiology.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Goodwill AG, Dick GM, Kiel AM, et al. Regulation of coronary blood flow. Compr Physiol 2017;7:321–82. 10.1002/cphy.c160016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexander Y, Osto E, Schmidt-Trucksäss A, et al. Endothelial function in cardiovascular medicine: a consensus paper of the European Society of cardiology working groups on atherosclerosis and vascular biology, aorta and peripheral vascular diseases, coronary pathophysiology and microcirculation, and thrombosis. Cardiovasc Res 2021;117:29–42. 10.1093/cvr/cvaa085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poredos P, Poredos AV, Gregoric I. Endothelial dysfunction and its clinical implications. Angiology 2021;72:604–15. 10.1177/0003319720987752 [DOI] [PubMed] [Google Scholar]
- 4.Sara JD, Widmer RJ, Matsuzawa Y, et al. Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. JACC Cardiovasc Interv 2015;8:1445–53. 10.1016/j.jcin.2015.06.017 [DOI] [PubMed] [Google Scholar]
- 5.Kumar S, Mehta PK, Eshtehardi P, et al. Functional coronary angiography in symptomatic patients with no obstructive coronary artery disease. Catheter Cardiovasc Interv 2021;98:827–35. 10.1002/ccd.29237 [DOI] [PubMed] [Google Scholar]
- 6.Hermida N, Balligand J-L. Low-density lipoprotein-cholesterol-induced endothelial dysfunction and oxidative stress: the role of statins. Antioxid Redox Signal 2014;20:1216–37. 10.1089/ars.2013.5537 [DOI] [PubMed] [Google Scholar]
- 7.Shi Y, Vanhoutte PM. Macro- and microvascular endothelial dysfunction in diabetes. J Diabetes 2017;9:434–49. 10.1111/1753-0407.12521 [DOI] [PubMed] [Google Scholar]
- 8.Loader J, Montero D, Lorenzen C, et al. Acute hyperglycemia impairs vascular function in healthy and cardiometabolic diseased subjects: systematic review and meta-analysis. Arterioscler Thromb Vasc Biol 2015;35:2060–72. 10.1161/ATVBAHA.115.305530 [DOI] [PubMed] [Google Scholar]
- 9.Lima BB, Hammadah M, Kim JH, et al. Association of transient endothelial dysfunction induced by mental stress with major adverse cardiovascular events in men and women with coronary artery disease. JAMA Cardiol 2019;4:988–96. 10.1001/jamacardio.2019.3252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandoo A, van Zanten JJCSV, Metsios GS, et al. The endothelium and its role in regulating vascular tone. Open Cardiovasc Med J 2010;4:302–12. 10.2174/1874192401004010302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Little PJ, Askew CD, Xu S, et al. Endothelial dysfunction and cardiovascular disease: history and analysis of the clinical utility of the relationship. Biomedicines 2021;9. 10.3390/biomedicines9060699. [Epub ahead of print: 20 06 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Godo S, Takahashi J, Yasuda S, et al. Endothelium in coronary macrovascular and microvascular diseases. J Cardiovasc Pharmacol 2021;78:S19–29. 10.1097/FJC.0000000000001089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hubert A, Seitz A, Pereyra VM, et al. Coronary artery spasm: the interplay between endothelial dysfunction and vascular smooth muscle cell hyperreactivity. Eur Cardiol 2020;15:e12. 10.15420/ecr.2019.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lei J, Vodovotz Y, Tzeng E, et al. Nitric oxide, a protective molecule in the cardiovascular system. Nitric Oxide 2013;35:175–85. 10.1016/j.niox.2013.09.004 [DOI] [PubMed] [Google Scholar]
- 15.Förstermann U, Xia N, Li H. Roles of vascular oxidative stress and nitric oxide in the pathogenesis of atherosclerosis. Circ Res 2017;120:713–35. 10.1161/CIRCRESAHA.116.309326 [DOI] [PubMed] [Google Scholar]
- 16.Widmer RJ, Samuels B, Samady H, et al. The functional assessment of patients with non-obstructive coronary artery disease: expert review from an international microcirculation working group. EuroIntervention 2019;14:1694–702. 10.4244/EIJ-D-18-00982 [DOI] [PubMed] [Google Scholar]
- 17.Perera D, Berry C, Hoole SP, et al. Invasive coronary physiology in patients with angina and non-obstructive coronary artery disease: a consensus document from the coronary microvascular dysfunction workstream of the British Heart Foundation/National Institute for health research partnership. Heart 2022. 10.1136/heartjnl-2021-320718. [Epub ahead of print: 22 Mar 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feenstra RGT, Seitz A, Boerhout CKM, et al. Principles and pitfalls in coronary vasomotor function testing. EuroIntervention 2022;17:1271–80. 10.4244/EIJ-D-21-00402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thijssen DHJ, Black MA, Pyke KE, et al. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol 2011;300:H2–12. 10.1152/ajpheart.00471.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Broxterman RM, Witman MA, Trinity JD, et al. Strong relationship between vascular function in the coronary and brachial arteries. Hypertension 2019;74:208–15. 10.1161/HYPERTENSIONAHA.119.12881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Green DJ, Dawson EA, Groenewoud HMM, et al. Is flow-mediated dilation nitric oxide mediated?: a meta-analysis. Hypertension 2014;63:376–82. 10.1161/HYPERTENSIONAHA.113.02044 [DOI] [PubMed] [Google Scholar]
- 22.Ming Z, Parent R, Lavallée M. Nitric oxide-independent dilation of conductance coronary arteries to acetylcholine in conscious dogs. Circ Res 1997;81:977–87. 10.1161/01.RES.81.6.977 [DOI] [PubMed] [Google Scholar]
- 23.Bonetti PO, Pumper GM, Higano ST, et al. Noninvasive identification of patients with early coronary atherosclerosis by assessment of digital reactive hyperemia. J Am Coll Cardiol 2004;44:2137–41. 10.1016/j.jacc.2004.08.062 [DOI] [PubMed] [Google Scholar]
- 24.Konttinen J, Lindholm H, Sinisalo J, et al. Association between lowered endothelial function measured by peripheral arterial tonometry and cardio-metabolic risk factors - a cross-sectional study of Finnish municipal workers at risk of diabetes and cardiovascular disease. BMC Cardiovasc Disord 2013;13:83. 10.1186/1471-2261-13-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Motozato K, Suematsu Y, Norimatsu K, et al. Reactive hyperemia index associated with atherosclerotic cardiovascular disease under treatment for lifestyle diseases. J Clin Med Res 2020;12:293–9. 10.14740/jocmr4100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leite AR, Borges-Canha M, Cardoso R, et al. Novel biomarkers for evaluation of endothelial dysfunction. Angiology 2020;71:397–410. 10.1177/0003319720903586 [DOI] [PubMed] [Google Scholar]
- 27.Zhao T, Kecheng Y, Zhao X, et al. The higher serum endocan levels may be a risk factor for the onset of cardiovascular disease: a meta-analysis. Medicine 2018;97:e13407. 10.1097/MD.0000000000013407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ziaee M, Mashayekhi S, Ghaffari S, et al. Predictive value of Endocan based on TIMI risk score on major adverse cardiovascular events after acute coronary syndrome. Angiology 2019;70:952–9. 10.1177/0003319718815241 [DOI] [PubMed] [Google Scholar]
- 29.Qiu C-R, Fu Q, Sui J, et al. Serum endothelial cell-specific molecule 1 (Endocan) levels in patients with acute myocardial infarction and its clinical significance. Angiology 2017;68:354–9. 10.1177/0003319716651349 [DOI] [PubMed] [Google Scholar]
- 30.Cheifetz S, Bellón T, Calés C, et al. Endoglin is a component of the transforming growth factor-beta receptor system in human endothelial cells. J Biol Chem 1992;267:19027–30. 10.1016/S0021-9258(18)41732-2 [DOI] [PubMed] [Google Scholar]
- 31.Blázquez-Medela AM, García-Ortiz L, Gómez-Marcos MA, et al. Increased plasma soluble endoglin levels as an indicator of cardiovascular alterations in hypertensive and diabetic patients. BMC Med 2010;8:86. 10.1186/1741-7015-8-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li CG, Bethell H, Wilson PB, et al. The significance of CD105, TGFbeta and CD105/TGFbeta complexes in coronary artery disease. Atherosclerosis 2000;152:249–56. 10.1016/s0021-9150(99)00476-1 [DOI] [PubMed] [Google Scholar]
- 33.Yoon MH, Reriani M, Mario G, et al. Long-term endothelin receptor antagonism attenuates coronary plaque progression in patients with early atherosclerosis. Int J Cardiol 2013;168:1316–21. 10.1016/j.ijcard.2012.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lavi S, Bae J-H, Rihal CS, et al. Segmental coronary endothelial dysfunction in patients with minimal atherosclerosis is associated with necrotic core plaques. Heart 2009;95:1525–30. 10.1136/hrt.2009.166017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bonetti PO, Lerman LO, Lerman A. Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler Thromb Vasc Biol 2003;23:168–75. 10.1161/01.atv.0000051384.43104.fc [DOI] [PubMed] [Google Scholar]
- 36.Targonski PV, Bonetti PO, Pumper GM, et al. Coronary endothelial dysfunction is associated with an increased risk of cerebrovascular events. Circulation 2003;107:2805–9. 10.1161/01.CIR.0000072765.93106.EE [DOI] [PubMed] [Google Scholar]
- 37.Prasad M, McBane R, Reriani M, et al. Coronary endothelial dysfunction is associated with increased risk of venous thromboembolism. Thromb Res 2016;139:17–21. 10.1016/j.thromres.2015.12.024 [DOI] [PubMed] [Google Scholar]
- 38.Zuchi C, Tritto I, Carluccio E, et al. Role of endothelial dysfunction in heart failure. Heart Fail Rev 2020;25:21–30. 10.1007/s10741-019-09881-3 [DOI] [PubMed] [Google Scholar]
- 39.AlBadri A, Leong D, Bairey Merz CN, et al. Typical angina is associated with greater coronary endothelial dysfunction but not abnormal vasodilatory reserve. Clin Cardiol 2017;40:886–91. 10.1002/clc.22740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Javadzadegan A, Moshfegh A, Qian Y, et al. Myocardial bridging and endothelial dysfunction - Computational fluid dynamics study. J Biomech 2019;85:92–100. 10.1016/j.jbiomech.2019.01.021 [DOI] [PubMed] [Google Scholar]
- 41.Wang ZJ, Zhang LL, Elmariah S, et al. Prevalence and prognosis of nonobstructive coronary artery disease in patients undergoing coronary angiography or coronary computed tomography angiography: a meta-analysis. Mayo Clin Proc 2017;92:329–46. 10.1016/j.mayocp.2016.11.016 [DOI] [PubMed] [Google Scholar]
- 42.Shaw J, Anderson T. Coronary endothelial dysfunction in non-obstructive coronary artery disease: risk, pathogenesis, diagnosis and therapy. Vasc Med 2016;21:146–55. 10.1177/1358863X15618268 [DOI] [PubMed] [Google Scholar]
- 43.Gutiérrez E, Flammer AJ, Lerman LO, et al. Endothelial dysfunction over the course of coronary artery disease. Eur Heart J 2013;34:3175–81. 10.1093/eurheartj/eht351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Corban MT, Godo S, Burczak DR, et al. Coronary endothelial dysfunction is associated with increased risk of incident atrial fibrillation. J Am Heart Assoc 2020;9:e014850. 10.1161/JAHA.119.014850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rush CJ, Berry C, Oldroyd KG, et al. Prevalence of coronary artery disease and coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. JAMA Cardiol 2021;6:1130–43. 10.1001/jamacardio.2021.1825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Borlaug BA, Olson TP, Lam CSP, et al. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J Am Coll Cardiol 2010;56:845–54. 10.1016/j.jacc.2010.03.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hollenberg SM, Klein LW, Parrillo JE, et al. Coronary endothelial dysfunction after heart transplantation predicts allograft vasculopathy and cardiac death. Circulation 2001;104:3091–6. 10.1161/hc5001.100796 [DOI] [PubMed] [Google Scholar]
- 48.Ergül E, Yılmaz AS, Öğütveren MM, et al. COVID 19 disease independently predicted endothelial dysfunction measured by flow-mediated dilatation. Int J Cardiovasc Imaging 2022;38:25–32. 10.1007/s10554-021-02356-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mejia-Renteria H, Travieso A, Sagir A, et al. In-vivo evidence of systemic endothelial vascular dysfunction in COVID-19. Int J Cardiol 2021;345:153–5. 10.1016/j.ijcard.2021.10.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nägele MP, Haubner B, Tanner FC, et al. Endothelial dysfunction in COVID-19: current findings and therapeutic implications. Atherosclerosis 2020;314:58–62. 10.1016/j.atherosclerosis.2020.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study.