Abstract
Ferrets which had been orally dosed with 5 mg of Staphylococcal enterotoxin B (SEB) responded with an increase in subcutaneous temperature. At 75 min, the subcutaneous temperature was significantly higher (+ 0.9°C ± 0.38°C, P < 0.007) than in control animals. Animals dosed with 1 or 2 mg of SEB responded with a small, but not significant, increase in subcutaneous temperature. All of the animals dosed with 5 mg of SEB retched and vomited. The mean latency for the onset of retching was 105 ± 36 min, and the mean latency for the onset of vomiting was 106 ± 34 min. The mean number of retches was 17.8 ± 19.6, and the mean number of vomits was 2.0 ± 1.5. These findings indicate that ferrets can be used as alternatives to primates for the study of the biological activities of SEB.
The enterotoxins produced by coagulase-positive strains of Staphylococcus aureus are a major cause of symptoms of food poisoning in humans (15, 20). It is the second most common cause of food poisoning in the United States (5). The genes encoding a number of Staphylococcal enterotoxins (SE) have been cloned and sequenced: A (SEA), B, C123, D, E, G, H, I, and J (11, 13, 15, 24). The toxins can be divided into two groups with SEA and SEB representing each group. Despite this body of molecular information, relatively little is known of the mechanisms by which the toxins can produce the symptoms of food poisoning, which in turn hampers the design of protective measures and antitoxic drugs. A major factor contributing to this lack of progress has been the lack of a small-animal model which mimics the clinical features of SE intoxication, including nausea, vomiting, abdominal cramping, and diarrhea. Low-grade fever can occur in severe cases, but hypotension and prostration are rare (10). The commonly used animal models for studies of infection such as the mouse, rat, and rabbit are excluded as suitable models, since they do not display an emetic reflex. Previous animal studies have focused on the emetic and related effects of the SEB group, although there is less information on the SEA group. This study confined itself to the SEB group. In the rhesus monkey, vomiting can be induced by intravenous or intragastric (3, 17, 18) administration of SEB. In the cynomologous monkey, emesis and diarrhea have been reported following the intraduodenal administration of SEB (12). Intravenous administration of SEB induced emesis in the cat, but intragastric administration curiously did not (19), although pyrexia was induced via both routes (19). Whilst nonhuman primates would appear to be the most appropriate model, such studies are severely restricted by the availability of animals and ethical considerations. In the past 20 years there has been a general resurgence of interest in emetic mechanisms because of the clinical requirement for drugs to block the severe emetic effects of the drugs and radiation used to treat cancer. These studies, which led to the identification of selective 5-hydroxytryptamine-3 receptor antagonists now widely used to treat emesis induced by anticancer therapy, used the ferret as the emetic model (1). This species has now become widely accepted for the study of emetic mechanisms. The ferret is a small carnivore which responds to the full spectrum of agents known to induce emesis in humans (8). A preliminary study reported that the ferret had an emetic response to SEB when given intravenously, but the oral route was not investigated (14) nor were other effects of SEB monitored. A further advantage of the ferret for the study of food poisoning is that the morphology and physiology of the ferret gastrointestinal tract have many features in common with the human gastrointestinal tract (23). The aim of the present study was to investigate whether orally administered SEB induced emesis, diarrhea, or pyrexia in the ferret and to assess its potential as a model for studying the mechanism of action of SEB-induced food poisoning.
Experiments were performed with adult female ferrets (Mustela putorius furo L.; Marshall Farms, Inc., New York, N.Y.) with a mean body weight of 735 g (standard error of the mean [SEM], 41 g; n = 24). They were not in estrus. SEB, which had been purified from culture supernatant of S. aureus S6 (Centre for Applied Microbiology and Research, Porton Down, Wiltshire, United Kingdom) and which was greater than 95% pure by sodium dodecyl sulfate-polyacrylamide gel electrophoresis was used in these studies. Prior to dosing with SEB, animals were deprived of food for 24 h but were allowed free access to water. SEB was given to groups of five animals at doses of 1, 2, or 5 mg into the stomach via an oral dosing tube. The SEB was given in 10 ml of sterile 154 mM NaCl which was also used for control experiments. Following dosing with either saline or SEB in saline, changes in subcutaneous body temperature and activity and the incidence of retching, vomiting, and defecation were monitored over a period of 3 h by trained observers. All values are expressed as means ± SEMs. Statistical comparisons were made by using unpaired sample t tests.
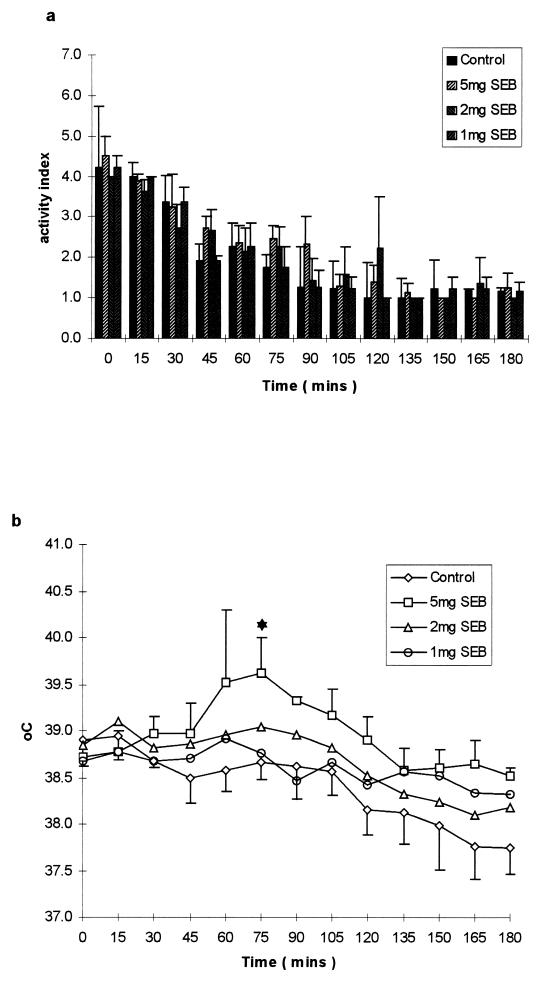
Activity was assessed every 5 min and was scored by using a truncated scale of 1 to 5 (1, inactive or apparently sleeping; 2, grooming; 3, low-level of intermittent activity; 4, medium level of continuous activity; and 5, high level of intense continuous activity). The scale was derived from observation of animals under identical conditions a week prior to experimentation. In the saline-dosed animals, there was a progressive decline in activity over the first 90 min, after which it plateaued (Fig. 1a). Although at individual times the SEB-treated animals appeared to have elevated levels of activity, overall this was not statistically significant, and the overall decline in activity during the course of the experiment was similar to that seen in control animals (Fig. 1a).
FIG. 1.
(a) Change in activity, on a scale from 1 to 5, in ferrets dosed with 1, 2, or 5 mg of SEB in comparison with control animals. The temperature of control animals or animals dosed with 1, 2, or 5 mg of SEB is recorded in panel b. ★, P < .01 compared to control.
Fourteen days prior to experimentation, each experimental animal was anesthetized with halothane-oxygen and a DAS5002 identity and temperature transponder (Plexx BV, Elst, The Netherlands) was implanted under the dorsal skin at the junction between the thorax and the abdomen. During experiments, the subcutaneous interscapular temperature was measured every 15 min by using an external receiver. The ambient temperature for the experiments was 20°C. The subcutaneous interscapular temperature showed a progressive decline over the observation period in animals dosed with saline alone (Fig. 1b). This appeared to mirror the progressive decrease in the activity score (see above and Fig. 1a). Following administration of 5 mg of SEB, the subcutaneous temperature began to increase after 45 min, reaching a peak between 60 and 75 min. At 75 min, the temperature in animals treated with 5 mg of SEB was significantly higher (+ 0.9°C ± 0.38°C, P < 0.007) than in control animals. Animals dosed with 1 or 2 mg of SEB showed a small, but not significant, increase in temperature over the course of the experiment in comparison with control animals.
Retching and vomiting were quantified separately. Retching was defined as the number of forceful rhythmic abdominal contractions occurring with the animal in a chracteristic posture not resulting in expulsion of upper gastrointestinal tract contents (22). Vomiting was defined as the forceful oral expulsion of upper gastrointestinal contents (22). The time of occurrence of each episode of retching and vomiting was noted (Table 1). Retching and vomiting were not induced by saline in any animal. Two out of five animals dosed with 1 mg of SEB retched, and one of the five animals vomited. The latency of retching was 120 and 143 min, and the mean number of retches in the group was 8.8 ± 10.6. A 2-mg dose of SEB induced retching and vomiting in one animal which vomited eight times and retched 50 times beginning at 160 min after dosing. Retching and vomiting was induced in all four animals tested by using a 5-mg dose of SEB. The mean latency was 105 ± 36 min for the onset of retching and was 106 ± 34 min for the onset of vomiting (n = 4), and the mean number of retches was 17.8 ± 19.6 and the mean number of vomits was 2.0 ± 1.5 (n = 4).
TABLE 1.
Emetic, retching, and diarrheal responses of ferrets orally dosed with SEB
| Dose of SEB (mg) | No. of animals per group | Retching
|
Vomiting
|
Defecation
|
|||||
|---|---|---|---|---|---|---|---|---|---|
| No.a | Meanb | Latencyc | No.a | Meanb | Latencyc | No.a | Appearanced | ||
| None | 5 | 0 | NAe | NA | 0 | NA | NA | 2 | 1.5 |
| 1 | 5 | 2 | 8.8 ± 10.6 | 132 | 1 | 4 | 150 | 4 | 1 |
| 2 | 5 | 1 | 10 | 160 | 1 | 8 | 160 | 2 | 1 |
| 5 | 4 | 4 | 17.8 ± 19.6 | 105 ± 36 | 4 | 2 ± 1.5 | 106 ± 34 | 10 | 2.5 |
Number of animals in each group showing this response.
Mean number of episodes (± SEM).
Mean time (min) for response (± SEM).
Mean score from 1 (normal) to 3 (fully mucoid).
NA, not applicable.
Ferrets usually defecate in one corner of their cage, and this facilitated monitoring. As episodes of defecation are relatively rare (see below), attention focused on the nature of the feces. Each stool was scored as follows: 1, normal consistency and color; 2, semisolid/partially mucoid; and 3, fully mucoid. In the control, animals that received 1 or 2 mg of SEB and defecated had only single episodes of defecation (Table 1), and out of nine episodes in 15 animals, eight episodes scored 1 and the remaining episode scored 2. In contrast, in the four animals of the group that received 5 mg of SEB there were 10 episodes of defecation with one scoring 1, three scoring 2, and six scoring 3. Thus, the highest dose of SEB dramatically changed the nature of the feces produced from the normal firm type to almost purely mucoid feces which closer inspection revealed were either transparent or yellow/orange stained, probably indicating the presence of bile. Similar mucoid feces have been reported in ferrets exposed to total body radiation (7).
The dose of SEB required to cause emesis in monkeys after intragastric dosing has been reported to be in the range of 5 to 1,000 μg/kg (2–4, 18), although most reports suggest the emetic dose is between 5 and 50 μg/kg. In the ferret, the dose of SEB required to elicit emesis is higher than that required to elicit it in primates. The reason for the apparent reduced susceptibility of ferrets to SEB is not clear. Sagrada et al. (14) have reported that doses of 30 μg of SEB per kg given by the intravenous route to ferrets reproducibly caused retching and emesis in ferrets 45 min after administration. Taken together with our results, this suggests that ferrets are more susceptible to SEB given by the intravenous route. Receptors for SEB in the gut have not been identified, but it seems likely that such receptors do exist and that differences in the density of these receptors might explain the different sensitivities to SEB. Alternatively, it is possible that SEB is degraded more efficiently in the ferret gut than in the gut of humans or other primates. The degradation of SEB in the ferret gut might explain why a 5-mg/kg dose appeared to reach critical threshold for the induction of emesis in all tested animals. Further studies with SEB codosed with protease inhibitors or inhibitors of gastric acid secretion, or in foodstuffs, might allow this question to be addressed.
Previous workers have shown a febrile response (an increase in core temperature of >0.9°C) develops after the intravenous administration of 0.1 μg of SEA per kg into rabbits (6, 9) within 5 h. It was suggested that the pyrexia was due to the release of interferons, tumor necrosis factor, and interleukin-2 (6). Similarly, the intravenous administration of SE in cats (9) or in goats (21) resulted in a pyrexic response. In murine models of disease, the effects of SE on body temperature appear to be more variable. Huang et al. (6) reported that the intravenous administration of 0.3 μg of SEA per kg into C3H/HeJ strain (endotoxin-resistant) mice resulted in a 1.15°C temperature increase, whereas Stiles et al. (16) have reported that the intraperitoneal administration of a mixture of endotoxin and up to 10 μg of SEA, SEB, or SEC3 into BALB/c or C57BL/6 mice resulted in a decline in body temperature over a period of 12 h (16). In the latter study, the oral administration of endotoxin/enterotoxin did not elicit any change in body temperature. To our knowledge, the experiments in ferrets that we have reported here are the first describing a pyrexic effect after the oral delivery of an SE.
The quantities of SEB which reliably elicit emetic, thermoregulatory, and diarrheal responses in the ferret are small enough to allow the use of this model to explore the molecular basis of SEB activity without the use of primates. Previous studies with site-directed mutated forms of SEB in primates have suggested that the emetic activity of SEB may not be related to the ability of SEB to cause T-cell mitogenicity (4). However, the low numbers of animals used in this study makes it difficult to draw firm conclusions. The finding that the ferret responds to orally delivered SEB will also permit work to elucidate the site and mode of action of SEB.
REFERENCES
- 1.Andrews P L R, Davies C J. Physiology of emesis induced by anti-cancer therapy. In: Reynolds D J M, Andrews P L R, Davis C J, editors. Serotonin and the scientific basis of anti-emetic therapy. Clinical Communications Oxford, United Kingdom: Oxford; 1995. pp. 25–49. [Google Scholar]
- 2.Bergdoll M S. Monkey feeding test for staphylococcal enterotoxin. Methods Enzymol. 1988;165:324–333. doi: 10.1016/s0076-6879(88)65048-8. [DOI] [PubMed] [Google Scholar]
- 3.Elwell M R, Liu C T, Spertzel R O, Beisel W R. Mechanisms of oral staphylococcal enterotoxin B-induced emesis in the monkey. Proc Soc Exp Biol Med. 1975;148:424–427. doi: 10.3181/00379727-148-38553. [DOI] [PubMed] [Google Scholar]
- 4.Harris T O, Grossman D, Kappler J W, Marrack P, Rich R R, Betley M J. Lack of complete correlation between emetic and T-cell-stimulating activities of staphylococcal enterotoxins. Infect Immun. 1993;61:3175–3183. doi: 10.1128/iai.61.8.3175-3183.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holmberg S D, Blake P A. Staphylococcal food poisoning in the United States. New facts and old misconceptions. JAMA. 1984;251:487–489. [PubMed] [Google Scholar]
- 6.Huang W T, Lin M T, Won S J. Staphylococcal enterotoxin A-induced fever is associated with increasing circulating levels of cytokines in rabbits. Infect Immun. 1997;65:2656–2662. doi: 10.1128/iai.65.7.2656-2662.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King G L. Characterization of radiation-induced emesis in the ferret. Radiat Res. 1988;114:599–612. [PubMed] [Google Scholar]
- 8.King G L. Animal models in the study of vomiting. Can J Physiol Pharmacol. 1990;68:260–268. doi: 10.1139/y90-040. [DOI] [PubMed] [Google Scholar]
- 9.Martin W J, Marcus S. Relation of pyrogenic and emetic properties of enterobacterial endotoxin and of staphylococcal enterotoxin. J Bacteriol. 1964;87:1019–1026. doi: 10.1128/jb.87.5.1019-1026.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monday S R, Bohach G A. Properties of Staphylococcus aureus enterotoxins and toxic shock syndrome toxin-1. In: Alouf J E, Freer J H, editors. The comprehensive sourcebook of bacterial protein toxins. London, England: Academic Press; 1999. pp. 589–610. [Google Scholar]
- 11.Munson S H, Tremaine M T, Betley M J, Welch R A. Identification and characterization of staphylococcal enterotoxin types G and I from Staphylococcus aureus. Infect Immun. 1998;66:3337–3348. doi: 10.1128/iai.66.7.3337-3348.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reck B, Scheuber P H, Londong W, Sailer-Kramer B, Bartsch K, Hammer D K. Protection against the staphylococcal enterotoxin-induced intestinal disorder in the monkey by anti-idiotypic antibodies. Proc Natl Acad Sci USA. 1988;85:3170–3174. doi: 10.1073/pnas.85.9.3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ren K, Bannan J D, Panchli V, Cheung A L, Robbins J C, Fischetti V A, Zabriskie J B. Characterisation and biological properties of a new staphylococcal exotoxin. J Exp Med. 1994;180:1675–1683. doi: 10.1084/jem.180.5.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sagrada A, Rizzi C, Bonali P, Donetti A. 5-HT3 receptor antagonists inhibit enterotoxin B-induced emesis in the ferret. In: Reynolds D J M, Andrews P L R, Davis C J, editors. Serotonin and the scientific basis of anti-emetic therapy. Oxford, United Kingdom: Oxford Clinical Communications; 1995. pp. 256–257. [Google Scholar]
- 15.Spero L, Johnson-Winegar A, Schmidt J. Enterotoxins of staphylococci. In: Hardegree M C, Tu A T, editors. Handbook of natural toxins. Vol. 4. New York, N.Y: Marcel Dekker, Inc.; 1988. pp. 131–163. [Google Scholar]
- 16.Stiles B G, Campbell Y G, Castle R M, Grove S A. Correlation of temperature and toxicity in murine studies of Staphylococcal enterotoxins and toxic shock syndrome toxin 1. Infect Immun. 1999;67:1521–1525. doi: 10.1128/iai.67.3.1521-1525.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sugiyama H, Chow K L, Dragstedt L R., III Study of emetic receptor sites for staphylococcal enterotoxin in monkeys. Proc Soc Exp Biol Med. 1961;108:92–95. doi: 10.3181/00379727-108-26855. [DOI] [PubMed] [Google Scholar]
- 18.Sugiyama H, Hayama T. Comparative resistance of vagotomized monkeys to intravenous vs. intragastric staphylococcal enterotoxin B. Proc Soc Exp Biol Med. 1964;115:243–246. doi: 10.3181/00379727-115-28881. [DOI] [PubMed] [Google Scholar]
- 19.Sugiyama H, Hayama T, Yagasaki O. Emetic action of bacterial endotoxin in the cat. Proc Soc Exp Biol Med. 1966;121:278–281. doi: 10.3181/00379727-121-30758. [DOI] [PubMed] [Google Scholar]
- 20.Tranter H S. Foodborne staphylococcal illness. Lancet. 1990;336:1044–1046. doi: 10.1016/0140-6736(90)92500-h. [DOI] [PubMed] [Google Scholar]
- 21.Van Miert A S, Van Duin C T, Schotman A J. Comparative observations of fever and associated clinical hematological and blood biochemical changes after intravenous administration of staphylococcal enterotoxins B and F (toxic shock syndrome toxin-1) in goats. Infect Immun. 1984;46:354–460. doi: 10.1128/iai.46.2.354-360.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watson J W, Gonsalves S F, Fossa A J, McLean S, Seeger T, Obach S, Andrews P L R. The anti-emetic effects of CP-99,994 in the ferret and the dog: role of the NK1 receptor. Br J Pharmacol. 1995;115:84–94. doi: 10.1111/j.1476-5381.1995.tb16324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Whary M T, Andrews P L R. Physiology of the ferret. In: Fox J G, editor. Biology and diseases of the ferret. Baltimore, Md: Williams and Wilkins; 1998. pp. 103–148. [Google Scholar]
- 24.Zhang S, Iandolo J J, Stewart G C. The enterotoxin D plasmid of Staphylococcus aureus encodes a second enterotoxin determinant (sej) FEMS Microbiol Lett. 1998;168:227–233. doi: 10.1111/j.1574-6968.1998.tb13278.x. [DOI] [PubMed] [Google Scholar]