Abstract
Background
Bifurcation percutaneous coronary intervention (PCI) is associated with higher risk of clinical events.
Objectives
This study aimed to determine clinical and lesion features that predict adverse outcomes, and to evaluate the differential prognostic impact of these features in patients undergoing PCI for bifurcation lesions.
Methods
We analyzed 5,537 patients from the BIFURCAT (comBined Insights From the Unified RAIN and COBIS bifurcAtion regisTries) registry. The primary outcome was major adverse cardiac events (MACE) at 2-year follow-up; secondary outcomes included hard endpoints (all-cause death, myocardial infarction) and lesion-oriented clinical outcomes (LOCO) (target-vessel myocardial infarction, target lesion revascularization). The least absolute shrinkage and selection operator (LASSO) model was used for feature selection.
Results
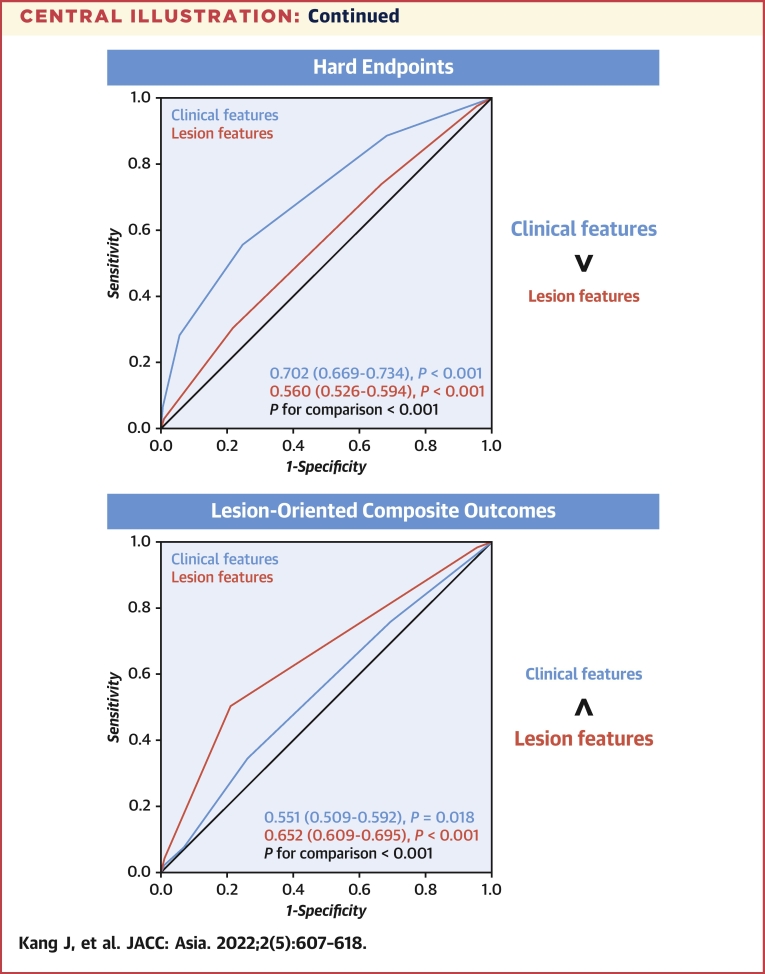
During the 2-year follow-up period, MACE occurred in 492 patients (8.9%). The LASSO model identified 5 clinical features (old age, chronic renal disease, diabetes mellitus, current smoking, and left ventricular dysfunction) and 4 lesion features (left main disease, proximal main branch disease, side branch disease, and a small main branch diameter) as significant features that predict MACE. A combination of all 9 features improved the predictive value for MACE compared with clinical and lesion features (area under the receiver-operating characteristics curve: 0.657 vs 0.636 vs 0.581; P < 0.001). For secondary endpoints, the clinical features had a higher impact than lesion features on hard endpoints, whereas lesion features had a higher impact than clinical features on LOCO.
Conclusions
In bifurcation PCI, 9 features were associated with MACE. Clinical features were predominant predictors for hard endpoints, and lesion features were predominant for predicting LOCO. Clinical and lesion features have distinct values, and both should be considered in bifurcation PCI.
Key Words: bifurcation, clinical feature, feature selection, lesion feature, percutaneous coronary intervention
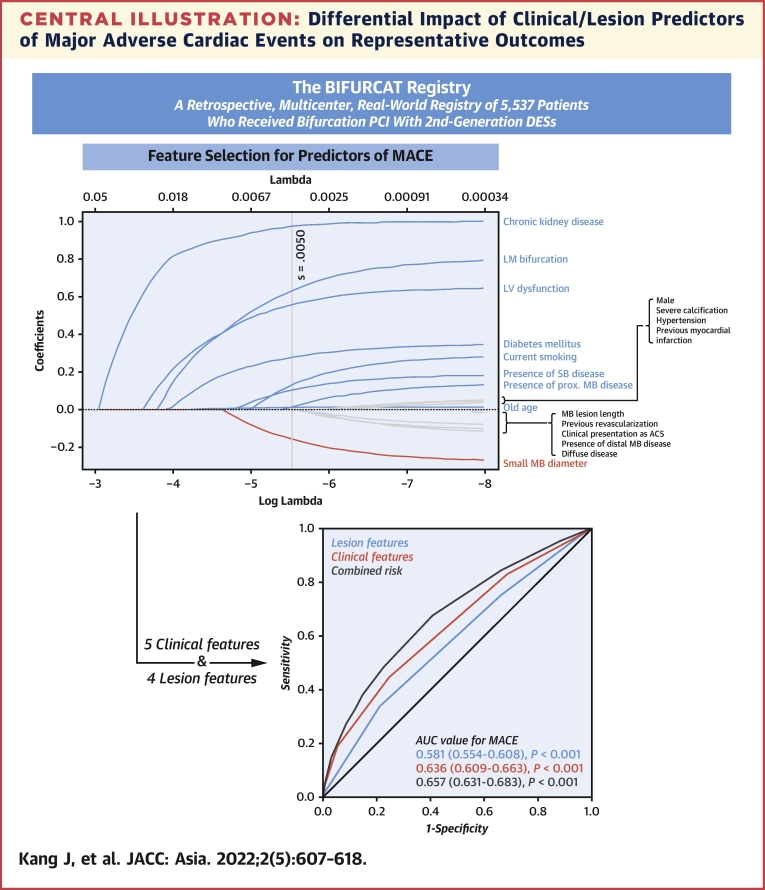
Central Illustration
In the field of percutaneous coronary intervention (PCI), numerous improvements have been made in terms of devices, procedural techniques, and adjunctive medical therapy. These improvements have led to an expansion of potential PCI candidates, including complex bifurcation lesions. Despite these advances, bifurcation PCI is still associated with a lower procedural success rate and worse clinical outcome, compared with nonbifurcation PCI.1 Various factors have been studied for their influence on clinical outcomes, and risk scores that include these factors have been created as a tool to guide clinical practice and improve patient outcomes. Traditionally, a hiatus originated between risk scores predicting mortality mainly focus on clinical factors,2 whereas risk scores incorporate lesion and procedural factors to predict adverse clinical outcomes in bifurcation PCI. Specifically, the RESOLVE (Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion) score was established to evaluate the risk of side branch occlusion,3 and the DEFINITION (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts) criteria were designed to establish a stratification system that could guide optimal stenting strategy.4 These risk scores mainly focused on lesion-related factors and the procedural techniques that determine the clinical outcome; however, it is not difficult to appreciate the fact that clinical factors may also have a significant impact on clinical outcomes in patients after bifurcation PCI.
In the present study, we sought to define clinical and lesion features that can influence clinical outcomes after bifurcation PCI from the large-scale bifurcation-dedicated registry. In addition, the distinct discriminative value for clinical and lesion features on various outcomes was compared to investigate the importance of considering both clinical and lesion features in patients undergoing bifurcation PCI.
Methods
Study population
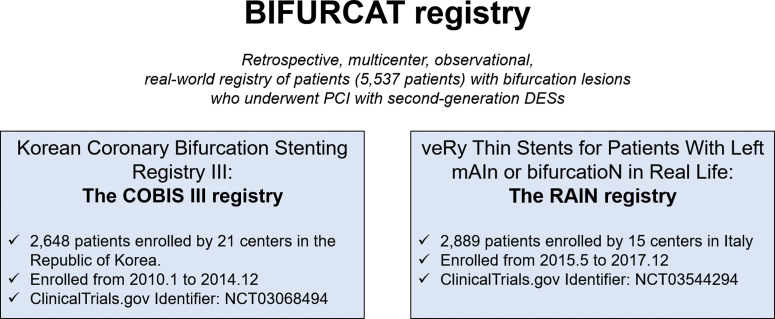
This study was based on the BIFURCAT (comBined Insights From the Unified RAIN and COBIS bifurcAtion regisTries) (Figure 1) registry, which is a merged registry of 2 data sets, the COBIS III (Coronary Bifurcation Stenting Registry III; NCT01642992) and the RAIN (VeRy Thin Stents for Patients With Left mAIn or bifurcatioN in Real Life; NCT03544294). Both studies complied with the provisions of the Declaration of Helsinki and were approved by the institutional review board at each center. The requirement for written informed consent was waived caused by the retrospective nature of the study.
Figure 1.
Overview of the BIFURCAT Registry
A total of 5,537 patient were included (2,648 from the COBIS III registry and 2,889 from the RAIN registry) in the current analysis. All patients underwent percutaneous coronary intervention for bifurcation lesions with second-generation drug-eluting stents. BIFURCAT = comBined Insights From the Unified RAIN and COBIS bifurcAtion regisTries; COBIS = Coronary Bifurcation Stenting Registry; RAIN = VeRy Thin Stents for Patients With Left mAIn or bifurcatioN in Real Life.
PCI for bifurcation lesions
PCI and adjunctive treatment after PCI were performed according to the practice guidelines established by the Korean Society of Interventional Cardiology and the European Society of Cardiology. Stenting technique (provisional vs 2 stents), along with the type of drug-eluting stent implanted, and the use of ancillary techniques, such as intravascular ultrasound, optical coherence tomography, and fractional flow reserve, were performed according to the operating physician’s discretion.
Clinical endpoints
Clinical follow-up data were collected at 2 years after index PCI. The primary analysis outcome of the present study was the occurrence of major adverse cardiac events (MACE), defined as a composite endpoint of all-cause death, myocardial infarction (MI), and target lesion revascularization (TLR) at 2-year follow-up. Secondary endpoints included hard endpoints (defined as all-cause death and MI), and the lesion-oriented composite outcome (LOCO, defined as TLR and target-vessel MI), along with the individual components of the primary endpoint.
Feature selection and statistical analysis
The BIFURCAT registry included 18 variables: 10 clinical variables (age, sex, diabetes, hypertension, hyperlipidemia, peripheral artery disease, estimated glomerular filtration rate, previous MI, previous PCI, left ventricular ejection fraction) and 8 lesion variables (location of the bifurcation lesion, presence of side branch disease, presence of proximal main branch disease, presence of distal main branch disease, main branch lesion length, main branch lesion diameter, severe calcification in the bifurcation lesion, diffuse lesion in the bifurcation lesion). Lesion variables were defined by the Qualitative comparative analysis and the Medina classification. We performed feature selection using the least absolute shrinkage and selection operator (LASSO) Cox regression model, with a training set and testing set of a ratio of 1:1.5,6 All 18 features with non-zero coefficients were enrolled in the regression model. By introducing a tuning parameter (λ) to penalize the coefficient of variables entered into the regression model, LASSO aimed to reduce the possibility of overfitting. A 10-fold cross-validation procedure was performed, first to get the lambda sequence, and then the remainders to compute the fit with each of the folds omitted.7 With the increase in the tuning parameter, the absolute values of variable coefficients were reduced toward zero, and fewer variables were then selected. The area under the curve (AUC) of the receiver-operating characteristic (ROC) curve was used as the criterion of model performance, and the model with the maximum AUC and minimum mean square error was selected.
Data are presented as numbers and frequencies for categorical variables and as mean ± SD for continuous variables. For comparison among groups, the chi-square test for categorical variables and unpaired Student’s t-test or 1-way analysis of variance for continuous variables were applied. To compare the discriminative ability of 2 different risk scores, the net reclassification improvement and integrated discrimination improvement statistics were calculated.8 Event rates were calculated based on Kaplan-Meier censoring estimates and compared with the log-rank test. All probability values were 2-sided and P values <0.05 were considered statistically significant. Statistical tests were performed using R (version 3.0.2, R Foundation for Statistical Computing) and SPSS (version 24.0, SPSS Inc).
Results
The baseline clinical and lesion characteristics of the BIFURCAT registry are shown in Table 1. Among the total population, 29.7% had left main (LM) bifurcation lesions, 64.7% had true bifurcations defined by the Medina classification. During the 2-year follow-up period, MACE occurred in 492 patients (8.9%). For the secondary outcomes, all-cause death occurred in 217 patients (3.9%), MI in 134 patients (2.4%), and TLR in 150 patients (2.7%) (Supplemental Table 1).
Table 1.
Baseline Clinical and Lesion Features of the Total Population
| Clinical features | |
| Age (y) | 66.2 ± 11.3 |
| Male | 4,228 (76.4) |
| Hypertension | 3,657 (66.0) |
| Hyperlipidemia | 2,736 (49.4) |
| Diabetes mellitus | 1,834 (33.1) |
| Current smoker | 1,408 (25.4) |
| Chronic kidney disease | 718 (13.0) |
| Previous PCI | 1,244 (22.5) |
| Previous CABG | 157 (2.8) |
| Previous MI | 944 (17.0) |
| Left ventricular ejection fraction, % | 57.7 ± 9.5 |
| Clinical diagnosis at presentation | |
| ST-segment elevation MI | 803 (14.5) |
| Non-ST-segment elevation MI | 1,163 (21.0) |
| Unstable angina | 1,265 (22.8) |
| Stable angina | 1,758 (31.8) |
| Other | 548 (9.9) |
| Lesion features | |
| Location of bifurcation | |
| Left main | 1,647 (29.7) |
| LAD/Dg | 2,466 (44.5) |
| LCX/OM | 859 (15.5) |
| RCA | 343 (6.2) |
| Other | 222 (4.0) |
| Severe calcification | 966 (17.4) |
| Diffuse disease | 2045 (36.9) |
| Medina classification | |
| 0,0,1 | 231 (4.2) |
| 0,1,0 | 751 (13.6) |
| 0,1,1 | 429 (7.7) |
| 1,0,0 | 544 (9.8) |
| 1,0,1 | 436 (7.9) |
| 1,1,0 | 1,366 (24.7) |
| 1,1,1 | 1,780 (32.1) |
| True bifurcation | 3,582 (64.7) |
Values are mean ± SD or n (%).
CABG = coronary artery bypass surgery; Dg = diagonal branch; LAD = left anterior descending coronary artery; LCX = left circumflex coronary artery; MI = myocardial infarction; OM = obtuse marginal; PCI = percutaneous coronary intervention; RCA = right coronary artery.
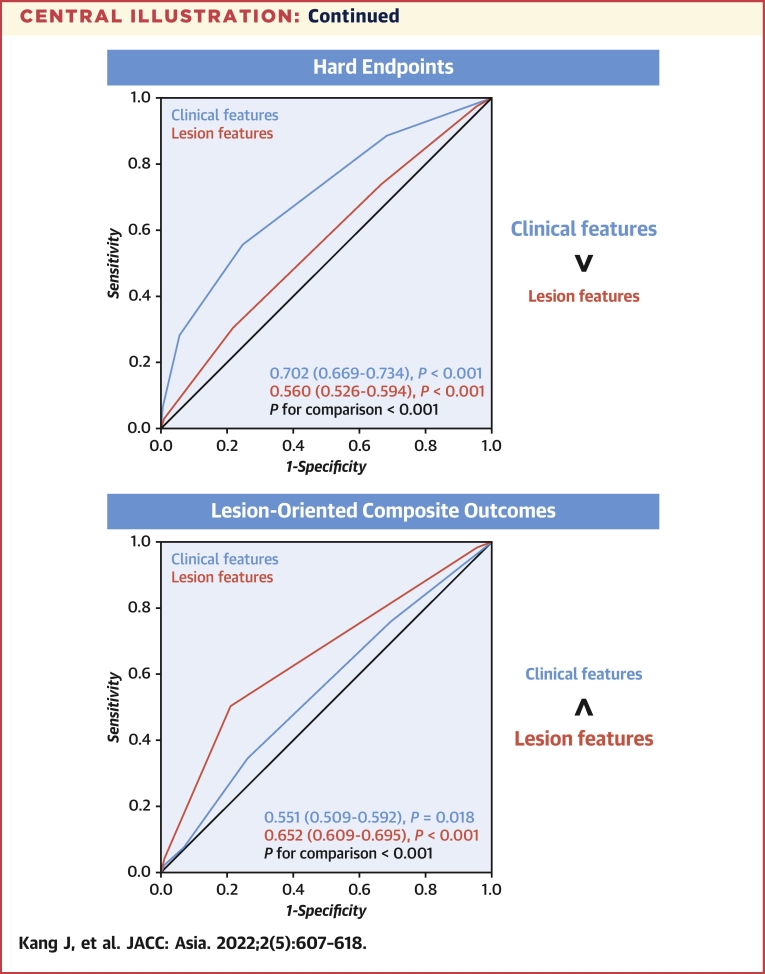
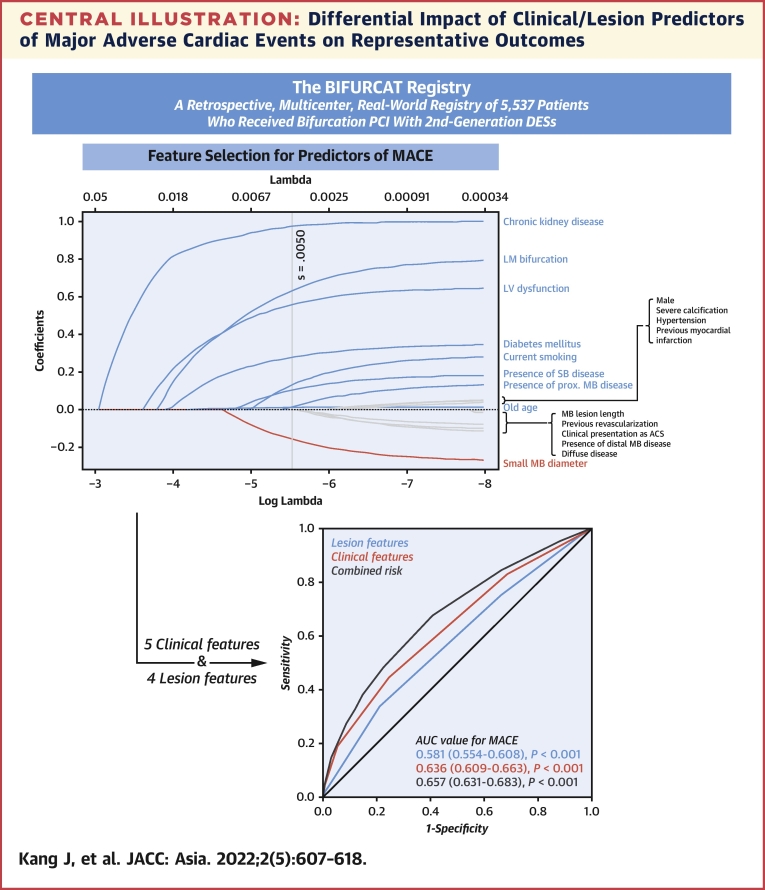
The machine learning-based LASSO regression model demonstrated the best predictive performance for MACE by selecting 9 features from a total of 18 clinical and lesion features. As shown in Figure 2, 5 clinical features (age, left ventricular dysfunction, chronic kidney disease, diabetes mellitus, and current smoking) and 4 lesion features (LM bifurcation, presence of significant proximal main branch disease, presence of significant side branch disease, diameter of the main branch) could derive the maximum AUC and minimum mean square error (Supplemental Figure 1). Using the best cutoff value for age (75 years) and diameter of the main branch (3 mm), the distribution of the number of clinical and lesion features is shown in Supplemental Figure 2, and the impact of each individual feature on MACE is shown in Supplemental Table 2. Among the 9 features, chronic kidney disease was the most important clinical feature to affect MACE, and LM bifurcation was the most important lesion feature to affect MACE, according to the log lambda value from the LASSO algorithm. By including one additional clinical or lesion feature in the reverse order of importance, a gradual increase of the predictive value of MACE was observed (Supplemental Figure 3).
Figure 2.
Feature Selection Using the LASSO Cox Regression Model
From a total of 18 clinical and lesion features, 5 clinical features (old age, chronic renal disease, diabetes mellitus, current smoking, and LV dysfunction) and 4 lesion features (LM disease, proximal MB disease, SB disease, and a small MB diameter), which could derive the maximum AUC and minimum MSE were selected. ACS = acute coronary syndrome; AUC = area under the curve; LASSO = least absolute shrinkage and selection operator; LM = left main; LV = left ventricular; MB = main branch; MSE = mean square error; SB = side branch.
Risk model for MACE
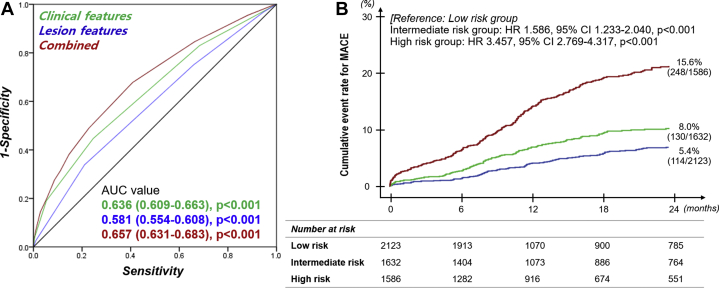
The combined risk was calculated by the total number of clinical and lesion features per patient. The distribution of the combined risk is shown in Supplemental Figure 4, along with the HR of MACE according to the number of features. By combining clinical and lesion features, the discriminative performance for MACE, expressed by the ROC curves, was improved compared with clinical and lesion features (Figure 3A). Clinical features had a significantly higher predictive value than lesion features (AUC values: clinical features: 0.636; 95% CI: 0.609-0.663; P < 0.001; lesion features: 0.581; 95% CI: 0.554-0.608; P < 0.001; P for comparison of AUC values <0.001), and the combined score significantly improved the predictive value (C-statistic: 0.657; 95% CI: 0.631-0.683; P < 0.001; P for comparison of AUC values: 0.001 for clinical features and <0.001 for lesion features). The net reclassification improvement and integrated discrimination improvement statistics also showed consistent results (Supplemental Table 3). For sensitivity analysis, the predictive value of the combined risk features was also validated in each individual registry (the RAIN and COBIS registry), and in patients receiving different stenting strategies (1-stenting and 2-stenting), showing a similar trend with the total population (Supplemental Table 4).
Figure 3.
Predictive Value of the Combined Clinical and Lesion Risk
(A) Comparison of the predictive value of the combined risk, clinical risk, and lesion risk using the AUC value for MACE. (B) The population was divided into tertiles based on the number of risk features (low-risk group [number of risk features ≤2], moderate-risk group [number of risk features = 3], high-risk group [number of risk features ≥4]), and the Kaplan-Meier survival curve presented that patients in a higher-risk group had a significantly higher risk of MACE. AUC = area under the curve; MACE = major adverse cardiac events.
The population was divided into tertiles based on the number of risk features (low-risk group [number of risk features ≤2]: n = 2,213 [40.0%], intermediate-risk group [number of risk features = 3]: n = 1,685 [30.4%], the high-risk group [number of risk features ≥4]: n = 1,639 [29.6%]). As shown in Figure 3B, MACE significantly increased along with the risk groups (MACE: 5.4% vs 8.0% vs 15.6%, long rank P < 0.001). The high-risk group showed a 3.46-fold increased risk of 2-year MACE, compared with the low-risk group.
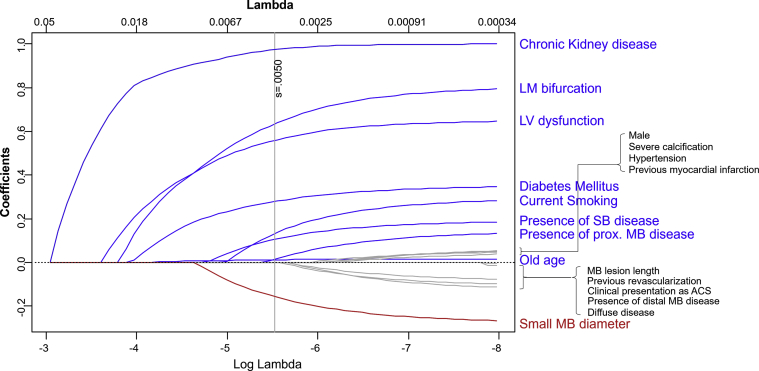
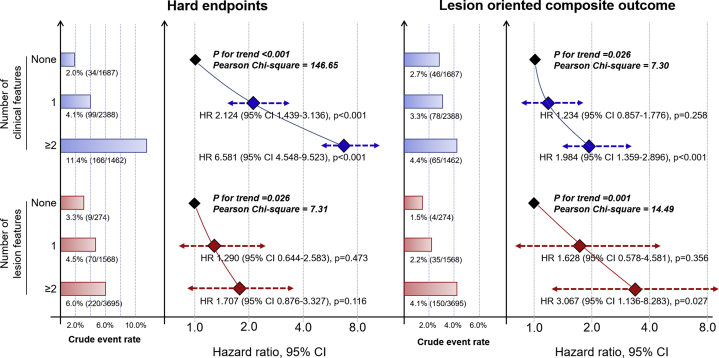
Differential impact of clinical and lesion features
For additional analysis, the impact of clinical and lesion features on each secondary outcome was assessed. The crude event rates increased along with the increase in both clinical and lesion risk features (Figure 4). However, when comparing the relative impact of clinical and lesion features, clinical features had a higher impact for hard endpoint (Pearson’s chi-square test: 146.65 vs 7.31, for clinical and lesion features), and the lesion features had a higher impact for LOCO (Pearson’s chi-square test: 7.30 vs 14.49, for clinical and lesion features). The ROC analysis also showed that the clinical features had superior predictive value for hard endpoints, while the lesion features had superior value for LOCO (Supplemental Figure 5).
Figure 4.
Number of Clinical/Lesion Features and the Risk for Adverse Outcomes
The risk for hard endpoints and lesion-oriented composite outcome increased along with the number of clinical and lesion features.
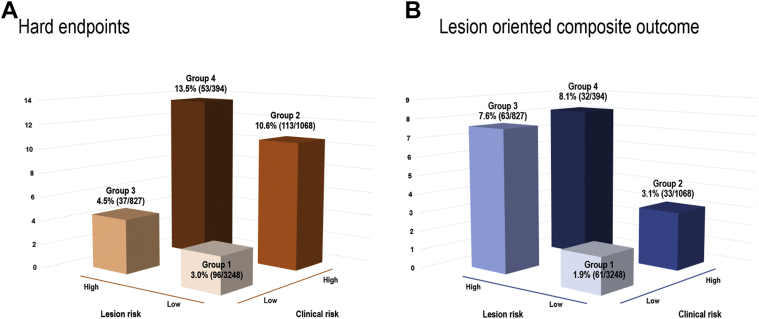
The total population was stratified into high and low clinical and lesion risk feature groups, according to the number of risk factors. MACE and other secondary outcomes occurred more frequently in the high-risk groups for both clinical and lesion risk (Table 2). The HR for hard endpoint was larger for clinical risk compared with lesion risk, whereas that for LOCO was larger for lesion risk compared with clinical risk. Then, by a 2 by 2 combination of high/low clinical and lesion risk, the population was categorized into 4 groups (Group 1: low clinical risk and low lesion risk; Group 2: high clinical risk and low lesion risk; Group 3: low clinical risk and high lesion risk; Group 4: high clinical risk and high lesion risk). The crude rates of secondary endpoints are shown in Figure 5. Compared with group 1, group 4 had a higher risk for both hard endpoints and LOCO (Table 3). However, when comparing the hard endpoints and LOCO risk between groups 2 and 3, the risk for hard endpoints was higher for group 2 (group 3 vs group 2: HR: 0.378; 95% CI: 0.261-0.549; P < 0.001), whereas the LOCO risk was higher for group 3 (group 3 vs group 2: HR: 2.108; 95% CI: 1.383-3.213; P = 0.001), implying the significant impact of clinical features on hard endpoints and that of lesion features on LOCO.
Table 2.
Clinical Events According to the Clinical and Angiographic Risk Features
| Clinical Risk Feature |
Lesion Risk Feature |
|||||
|---|---|---|---|---|---|---|
| Low Risk | High Risk | P Value | Low Risk | High Risk | P Value | |
| MACE | 275 (6.7) | 217 (14.8) | <0.001 | 328 (7.6) | 164 (13.4) | <0.001 |
| HR: 2.512 (95% CI: 2.101-3.003); P < 0.001 | HR: 1.757 (95% CI: 1.456-2.121); P < 0.001 | |||||
| Hard endpoints | 124 (3.0) | 65 (4.4) | 0.011 | 94 (2.2) | 95 (7.8) | <0.001 |
| HR: 1.650 (95% CI: 1.221-2.230); P = 0.001 | HR: 3.710 (95% CI: 2.787-4.938); P < 0.001 | |||||
| LOCO | 133 (3.3) | 166 (11.4) | <0.001 | 209 (4.8) | 90 (7.4) | 0.001 |
| HR: 3.963 (95% CI: 3.152-4.982); P < 0.001 | HR: 1.452 (95% CI: 1.133-01.860); P = 0.003 | |||||
| All-cause death | 84 (2.1) | 133 (9.1) | <0.001 | 152 (3.5) | 65 (5.3) | 0.004 |
| Myocardial infarction | 68 (1.7) | 66 (4.5) | <0.001 | 95 (2.2) | 39 (3.2) | 0.046 |
| Target lesion revascularization | 96 (2.4) | 54 (3.7) | 0.007 | 87 (2.0) | 63 (5.2) | <0.001 |
| Target-vessel revascularization | 176 (4.3) | 77 (5.3) | 0.137 | 161 (3.7) | 92 (7.5) | <0.001 |
Values are n (%) unless otherwise indicated.
MACE = major adverse cardiac events, defined as a composite endpoint of all-cause death, myocardial infarction, target lesion revascularization; Hard endpoints = defined as all-cause death and myocardial infarction; LOCO = lesion-oriented composite outcome, defined as target lesion revascularization, target-vessel myocardial infarction.
Figure 5.
Adverse Outcomes by 2-by-2 Combination of High/Low Clinical/Lesion Risk
Adverse outcome rate for (A) hard endpoints and (B) lesion-oriented composite outcome in 4 groups (group 1: low clinical risk and low lesion risk; group 2: low clinical risk and high lesion risk; group 3: high clinical risk and low lesion risk; group 4: high clinical risk and high lesion risk).
Table 3.
Risk of Hard Endpoints and Lesion-Oriented Composite Outcome Across the 4-Group Categories
| Group 2 | Group 3 | Group 4 | |
|---|---|---|---|
| Hard endpoints | HR (95% CI); P value | ||
| vs Group 1 | 4.093 (3.118-5.374); P < 0.001 | 1.547 (1.059-2.261); P = 0.024 | 5.673 (4.054-7.938); P < 0.001 |
| vs Group 2 | 0.378 (0.261-0.549); P < 0.001 | 1.387 (1.001-1.923); P = 0.050 | |
| vs Group 3 | 3.592 (2.358-5.473); P < 0.001 | ||
| LOCO | HR (95% CI); P value | ||
| vs Group 1 | 1.980 (1.296-3.025); P = 0.002 | 4.194 (2.949-5.963); P < 0.001 | 5.811 (3.786-8.921); P < 0.001 |
| vs Group 2 | 2.108 (1.383-3.213); P = 0.001 | 2.953 (1.815-4.803); P < 0.001 | |
| vs Group 3 | 1.409 (0.92-2.159); P = 0.115 | ||
Hard endpoints = defined as all-cause death and myocardial infarction; LOCO = lesion-oriented composite outcome, defined as target lesion revascularization, target-vessel myocardial infarction.
Discussion
In this study, we identified the clinical and lesion features that determine clinical outcomes after PCI for bifurcation lesions. The main findings can be summarized as follows. 1) Based on our large bifurcation PCI population, 9 features (including 5 clinical features and 4 lesion features) were selected as significant features associated with clinical outcomes. 2) Both clinical features and lesion features had predictive value for MACE, whereas the combination of risk features had superior predictive value compared with either clinical or lesion features. 3) Regarding secondary endpoints, the impact of clinical features was greater than lesion features for hard endpoints, whereas the lesion features had greater impact than clinical features for LOCO (Central Illustration). Collectively, we could identify 9 significant clinical and lesion features associated with clinical outcomes in bifurcation PCI. Both clinical and lesion features should be considered in treating patients with bifurcation PCI.
Central Illustration.
Differential Impact of Clinical/Lesion Predictors of Major Adverse Cardiac Events on Representative Outcomes
The BIFURCAT registry, which included 5,537 patients who received percutaneous coronary intervention for bifurcation lesions with second-generation drug-eluting stent, was analyzed. The LASSO Cox regression model derived 5 clinical features and 4 lesion features as important features that determine major adverse cardiac events. Clinical features had a higher impact on the hard endpoint (all-cause death, myocardial infarction), and lesion features had a higher impact on lesion-oriented clinical outcomes (target-vessel myocardial infarction, target lesion revascularization). AUC = area under the curve; BIFURCAT = comBined Insights From the Unified RAIN and COBIS bifurcAtion regisTries; DES = drug-eluting stent; LASSO = least absolute shrinkage and selection operator; LM = left main; LV = left ventricular; MACE = major adverse cardiac events; MB = main branch; PCI = percutaneous coronary intervention; SB = side branch.
Risk models in bifurcation PCI
Because of the complexity of the procedure, and the relatively higher risk for clinical events after PCI, there have been growing efforts to identify the optimal method of PCI in bifurcation lesions.9 Despite this effort, the clinical outcomes of patients receiving PCI for bifurcation are still below expectation. This can be explained by 2 aspects. First, the procedure itself is complex, leaving a higher risk for adverse outcomes.10 Second, patients who receive bifurcation PCI tend to have a higher clinical risk profile.5,11 For these reasons, defining lesions and patients vulnerable to adverse outcomes and performing risk stratification, which may lead to a more meticulous follow-up, is essential in this patient population.
Accordingly, previous studies have proposed tools to estimate the risk of adverse clinical outcomes after bifurcation PCI. A previous study included 6 variables (plaque distribution, main vessel thrombolysis in MI flow grade before stenting, pre-procedural diameter stenosis of bifurcation core, bifurcation angle, diameter stenosis of side branch before stenting, and the diameter ratio between main vessel and side branch: the RESOLVE score) to estimate the risk of side branch occlusion.4 Also, recent criteria included 8 angiographic factors (side branch diameter stenosis, side branch lesion length, main vessel reference vessel diameter, main vessel lesion length, presence of calcification, presence of multiple lesions, bifurcation angle, and presence of a thrombus: the DEFINITION score) to differentiate simple vs complex coronary bifurcation lesions.4 In a following clinical trial, these criteria were validated to select bifurcation lesions suitable for a systematic 2-stent approach.12 However, a common limitation of these 2 scoring systems is that they are fully lesion-based scores evaluated by angiography and quantitative coronary analysis. Meanwhile, it is well known that clinical risk factors have a significant impact on clinical outcomes, whereas the impact size is more prominent in the long run.13,14 Therefore, clinical factors also should be included in a risk stratification system for patients with bifurcation lesions.
Clinical and lesion features for prognosis after bifurcation PCI
From our analysis, a total 9 features, which included clinical and lesion features, were identified as significant predictors of MACE. All 5 clinical features (old age, left ventricular dysfunction, chronic kidney disease, diabetes mellitus, and current smoking) were well-known traditional clinical risk factors that have been verified to affect clinical outcomes in patients who receive PCI.15 Also, all 4 lesion features (LM bifurcation, presence of a significant proximal main branch disease, presence of a significant side branch disease, small reference diameter of the main branch) were important angiographic factors that are associated with adverse events after PCI in previous studies.13,16,17 Although each may be a well-known feature that is associated with clinical outcomes, we could identify 9 key factors that are important in bifurcation PCI. The finding that other clinical features (eg, hypertension, previous revascularization) and other lesion features (eg, severe calcification, lesion length of the main branch) were not included in the 9 key features denotes that these features may have collinearity with the selected 9 factors, and that these features may have a minimal independent value for predicting clinical outcomes in bifurcation PCI. Even after considering the interaction between risk features via the LASSO model, chronic kidney disease and LM disease were the most important features among clinical and lesion features, respectively, which are classical significant features that determine MACE.18,19
Distinctive impact of clinical and lesion features on different outcomes
From our study, we could verify the distinctive importance of clinical and lesion features for 2 different categories of outcomes: the clinical outcome (hard endpoint) and lesion outcome (LOCO). It should be noted that, although both clinical and lesion features had discriminative value for both secondary endpoints, a significant dominancy of the major determinant was observed. First, clinical features had a larger impact for predicting adverse clinical hard outcomes, and was confirmed by the Cox regression analysis, AUC analysis, and the 4-group categorization analysis. This denotes the significance of clinical factors even in bifurcation PCI, which is a typical disease entity in which the treatment results largely depend on the optimal procedural technique. Second, lesion features had a more superior predictive value than clinical features for LOCO. LOCO was a defined as a lesion- or procedure-specific outcome, and considering the clinical significance of a procedure-specific success in lesions that require complex procedures, as in bifurcation PCI, we should set great store to the high predictability of lesion features for LOCO. Collectively, our analysis could provide the distinct value of clinical and lesion features in predicting outcomes, while stressing that both clinical and lesion features should be taken into account for risk stratification in patients receiving bifurcation PCI.
Study limitations
First, this was an observational analysis of a large retrospective registry, which may have hidden confounding factors or allocation biases that could affect the results. Second, procedural features, including the coronary bifurcation angle, length of lesion in side branch, various adjunctive treatments, such as final kissing balloon technique and the proximal optimization techniques, or the specific stenting techniques were not included in the analysis. The lack of sufficient details regarding bifurcation PCI strategy and technique may limit the interpretation of our study, but the purpose of our study was to evaluate the intrinsic risk of a bifurcation lesion that was independent of the physician’s performance. Third, the C-statistic of the combined risk features was between 0.6 and 0.7, implying a modest discrimination for clinical event prediction. However, previous scores estimating clinical events after PCI have also shown similar C-statistic values, reflecting the difficulty in predicting clinical events by a simplified scoring system. Fourth, our study lacks an external validation of the significant features that were selected.
Conclusions
In the present study, we determined 9 clinical and lesion features that were associated with a higher risk of clinical events in patients with coronary bifurcation receiving PCI. The clinical and lesion features both had a significant additive value in predicting MACE. For secondary endpoints, clinical features were the major determinant for hard endpoints, and lesion features were that for LOCO. Considering the clinical implication of both hard endpoints and LOCO, clinical and lesion features should be considered in risk stratification for patients receiving bifurcation PCI.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: We confirmed clinical and lesion features that are associated with adverse clinical outcomes after PCI for coronary bifurcation lesions. Both clinical and lesion features should be considered for optimal patient care, while clinical features have a larger impact on clinical adverse outcomes and lesion features have a larger impact on lesion-oriented adverse outcomes.
TRANSLATIONAL OUTLOOK: Procedure-related features that are highly determined by the physician’s performance and preference also affect the adverse clinical outcomes after PCI for coronary bifurcation lesions. Further research may elucidate the relative impact of procedure-related features over clinical and lesion features on clinical adverse outcomes and lesion-oriented adverse outcomes.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental tables and figures, please see the online version of this paper.
Appendix
References
- 1.Sawaya F.J., Lefevre T., Chevalier B., et al. Contemporary approach to coronary bifurcation lesion treatment. J Am Coll Cardiol Intv. 2016;9(18):1861–1878. doi: 10.1016/j.jcin.2016.06.056. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones D.M., Braun L.T., Ndumele C.E., et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology. Circulation. 2019;139(25):e1162–e1177. doi: 10.1161/CIR.0000000000000638. [DOI] [PubMed] [Google Scholar]
- 3.Dou K., Zhang D., Xu B., et al. An angiographic tool for risk prediction of side branch occlusion in coronary bifurcation intervention: the RESOLVE score system (Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion) J Am Coll Cardiol Intv. 2015;8(1 Pt A):39–46. doi: 10.1016/j.jcin.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Chen S.L., Sheiban I., Xu B., et al. Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts) J Am Coll Cardiol Intv. 2014;7(11):1266–1276. doi: 10.1016/j.jcin.2014.04.026. [DOI] [PubMed] [Google Scholar]
- 5.Tibshirani R. The lasso method for variable selection in the Cox model. Stat Med. 1997;16(4):385–395. doi: 10.1002/(sici)1097-0258(19970228)16:4<385::aid-sim380>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 6.Sauerbrei W., Royston P., Binder H. Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med. 2007;26(30):5512–5528. doi: 10.1002/sim.3148. [DOI] [PubMed] [Google Scholar]
- 7.Simon N., Friedman J., Hastie T., Tibshirani R. Regularization Paths for Cox's Proportional Hazards Model via Coordinate Descent. J Stat Softw. 2011;39(5):1–13. doi: 10.18637/jss.v039.i05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pencina M.J., D'Agostino R.B., Sr., D'Agostino R.B., Jr., Vasan R.S. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–172. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 9.Di Gioia G., Sonck J., Ferenc M., et al. Clinical outcomes following coronary bifurcation PCI techniques: a systematic review and network meta-analysis comprising 5,711 patients. J Am Coll Cardiol Intv. 2020;13(12):1432–1444. doi: 10.1016/j.jcin.2020.03.054. [DOI] [PubMed] [Google Scholar]
- 10.Nakazawa G., Yazdani S.K., Finn A.V., Vorpahl M., Kolodgie F.D., Virmani R. Pathological findings at bifurcation lesions: the impact of flow distribution on atherosclerosis and arterial healing after stent implantation. J Am Coll Cardiol. 2010;55(16):1679–1687. doi: 10.1016/j.jacc.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 11.Genereux P., Giustino G., Redfors B., et al. Impact of percutaneous coronary intervention extent, complexity and platelet reactivity on outcomes after drug-eluting stent implantation. Int J Cardiol. 2018;268:61–67. doi: 10.1016/j.ijcard.2018.03.103. [DOI] [PubMed] [Google Scholar]
- 12.Zhang J.J., Ye F., Xu K., et al. Multicentre, randomized comparison of two-stent and provisional stenting techniques in patients with complex coronary bifurcation lesions: the DEFINITION II trial. Eur Heart J. 2020;41(27):2523–2536. doi: 10.1093/eurheartj/ehaa543. [DOI] [PubMed] [Google Scholar]
- 13.Kang J., Park K.W., Lee H.S., et al. relative impact of clinical risk versus procedural risk on clinical outcomes after percutaneous coronary intervention. Circ Cardiovasc Interv. 2021;14(2) doi: 10.1161/CIRCINTERVENTIONS.120.009642. [DOI] [PubMed] [Google Scholar]
- 14.Schwietz T., Spyridopoulos I., Pfeiffer S., et al. Risk stratification following complex PCI: clinical versus anatomical risk stratification including "post PCI residual SYNTAX-score" as quantification of incomplete revascularization. J Interv Cardiol. 2013;26(1):29–37. doi: 10.1111/j.1540-8183.2013.12014.x. [DOI] [PubMed] [Google Scholar]
- 15.Bohula E.A., Bonaca M.P., Braunwald E., et al. Atherothrombotic risk stratification and the efficacy and safety of vorapaxar in patients with stable ischemic heart disease and previous myocardial infarction. Circulation. 2016;134(4):304–313. doi: 10.1161/CIRCULATIONAHA.115.019861. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe Y., Mitomo S., Naganuma T., et al. impact of chronic kidney disease in patients with diabetes mellitus after percutaneous coronary intervention for left main distal bifurcation (from the Milan and New-Tokyo (MITO) Registry) Am J Cardiol. 2021;138:33–39. doi: 10.1016/j.amjcard.2020.10.021. [DOI] [PubMed] [Google Scholar]
- 17.Cha J.J., Hong S.J., Joo H.J., et al. Differential factors for predicting outcomes in left main versus non-left main coronary bifurcation stenting. J Clin Med. 2021;10(14):3024. doi: 10.3390/jcm10143024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi K.H., Song Y.B., Lee J.M., et al. Prognostic effects of treatment strategies for left main versus non-left main bifurcation percutaneous coronary intervention with current-generation drug-eluting stent. Circ Cardiovasc Interv. 2020;13(2) doi: 10.1161/CIRCINTERVENTIONS.119.008543. [DOI] [PubMed] [Google Scholar]
- 19.Sarnak M.J., Amann K., Bangalore S., et al. Chronic kidney disease and coronary artery disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;74(14):1823–1838. doi: 10.1016/j.jacc.2019.08.1017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.