Abstract
Extracellular vesicles (EVs) are small bilipid layer-enclosed vesicles that can be secreted by all tested types of brain cells. Being a key intercellular communicator, EVs have emerged as a key contributor to the pathogenesis of various neurodegenerative diseases (NDs) including Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, and Huntington’s disease through delivery of bioactive cargos within the central nervous system (CNS). Importantly, CNS cell-derived EVs can be purified via immunoprecipitation, and EV cargos with altered levels have been identified as potential biomarkers for the diagnosis and prognosis of NDs. Given the essential impact of EVs on the pathogenesis of NDs, pathological EVs have been considered as therapeutic targets and EVs with therapeutic effects have been utilized as potential therapeutic agents or drug delivery platforms for the treatment of NDs. In this review, we focus on recent research progress on the pathological roles of EVs released from CNS cells in the pathogenesis of NDs, summarize findings that identify CNS-derived EV cargos as potential biomarkers to diagnose NDs, and comprehensively discuss promising potential of EVs as therapeutic targets, agents, and drug delivery systems in treating NDs, together with current concerns and challenges for basic research and clinical applications of EVs regarding NDs.
Keywords: Extracellular vesicle, Exosome, Neurodegenerative disease, Therapeutics, Biomarker
Introduction
Neurodegenerative diseases (NDs) are a group of disorders characterized by progressive neuronal loss associated with deposition of pathological proteins/peptides in the central and peripheral nervous systems [1]. Examples of NDs include Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), amyotrophic lateral sclerosis (ALS), and many other NDs. The pathogeneses of NDs are complicated and far from being fully understood. However, the delivery of pathogenic molecules among diverse cellular populations and the establishment of disease-associated microenvironment have emerged as key contributors [2, 3]. Although cells can interact with surrounding and distant cells through various pathways, extracellular vesicles (EVs) are one of the most powerful tools for intercellular communication [2, 4, 5].
The discovery of EVs is one of the most groundbreaking discoveries in cell biology over the past few decades [2, 4, 6, 7]. EVs are the nanoscale bilipid layer-enclosed vesicles that are released from most eukaryotic cells and can be found in tissues and biological fluids [8–11]. They are a heterogeneous group of cell-derived membranous structures that mainly comprise exosomes and ectosomes/microvesicles (MVs) [2, 4, 8–12]. Other types of EVs include mitovesicles [12], apoptotic bodies, and retrovirus-like vesicles [13], which are not included in this review. In the central nervous system (CNS), EVs are widely involved in brain development and regeneration by regulating cell fate commitment and neural plasticity [14, 15], in the pathogenesis of NDs via transferring disease-associated molecules (e.g., amyloid precursor protein [APP], Tau, cytokines) [10, 16], and in the neuroregeneration/repair in NDs and acute brain damage [17]. Therefore, EVs have been considered as important pathological factors, potential therapeutic targets, and promising therapeutic agents of NDs. In this review, we summarize the pathological roles of EVs in NDs, and comprehensively discuss current progress of basic research and clinical investigations that utilize EVs as potential therapeutics and drug delivery systems for treating NDs.
EVs: biogenesis, composition, and secretion
Biogenesis of EVs
The mechanism of biogenesis is a major difference between exosomes and MVs. Exosomes are one of the smallest EVs that are also known as endosome-derived vesicles. The biogenesis of exosomes starts with the inward budding of the plasma membrane (Fig. 1). The fusion of primary endocytic vesicles forms early endosome (EE) in clathrin- or caveolin-dependent or -independent pathways [18]. EEs mature into late endosomes, also known as multivesicular bodies (MVBs). The formation and maturation of MVBs is under the regulation of various pathways including Rab5/Rab7 [19] and integral membrane protein of the lysosome/late endosome (SIMPLE) [20]. For instance, Rab5 forms a complex with Rabaptin-5 and Rabex-5, causing rapid recruitment of Rab5 effectors including the VPS34/p150 complex [19]. Rab5 is then removed from MVB membrane by the Mon1/SAND-1/Ccz1 complex, which promotes the recruitment and activation of Rab7 and of the HOPS complex (e.g., Vps11, Vps16, and Vps18) for membrane tethering and fusion [21]. In this process, intraluminal vesicles (ILVs) are formed via inward membrane budding in Rab5- and endosomal sorting complex required for transport (ESCRT)-dependent and -independent manners [19, 22–25]. In the ESCRT-dependent machinery, ESCRT-0, ESCRT-I, ESCRT-II, and ESCRT-III constitute the crossroad for recognition of proteins and membrane budding [22–25]. The ESCRT-independent mechanism has been reported in the formation of melanosomes, where Pmel17 [26] and Tetraspanin CD63 [27] contribute to ILV formation. After that, one part of MVBs (degradative MVBs) are degraded by lysosomes, and the remaining MVBs (secretory MVBs) are guided to the plasma membrane [28, 29]. Triggered by Ca2+ influx, MVBs fuse with the plasma membrane mainly through the exocytic pathway that requires a fusion machinery (SNARE [soluble N-ethylmaleimide-sensitive factor attachment protein receptor] and tethering factors), molecular switches (small Rab GTPases), cytoskeleton and its motor proteins (actin, microtubules, kinesins, myosins), and other supporting factors [4, 30]. Moreover, recent evidence suggests that only certain subpopulations of MVBs fuse with plasma membrane due to the selective binding of supporting factors for plasma fusion [4, 31, 32]. After MVB fusion with the plasma membrane, ILVs are released into extracellular space, which are defined as exosomes.
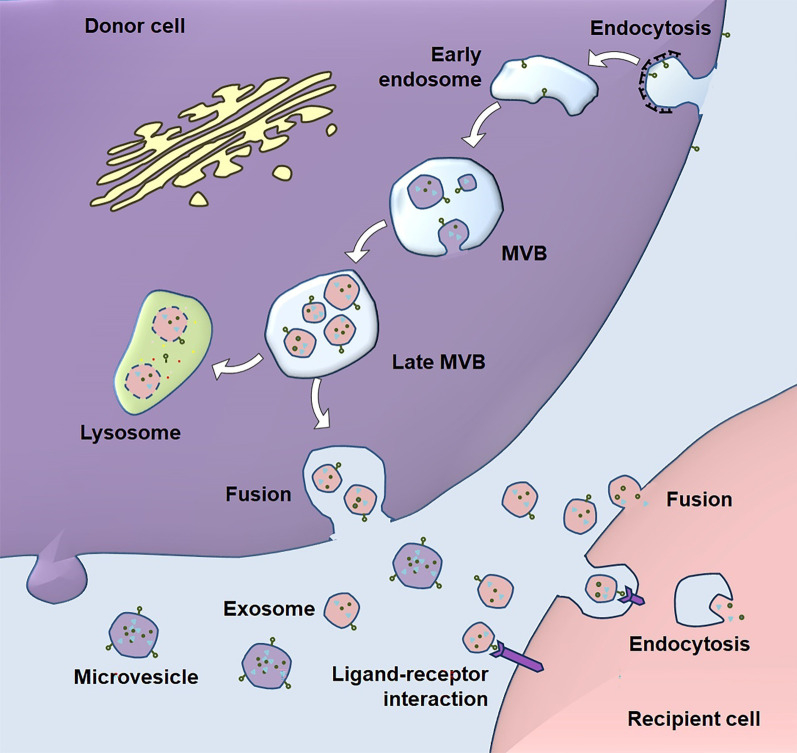
Fig. 1.
The biogenesis and uptake of EVs. Exosome biogenesis pathway starts with the formation of early endosome by endocytosis at the plasma membrane. ILVs are generated by inward budding of the multivesicular body (MVB, also known as late endosome) lipid bilayer membrane. MVB can fuse with the plasma membrane under the regulation of multistep processes including MVB trafficking along microtubules and docking at the plasma membrane for exosome secretion. Alternatively, MVBs fuse with lysosomes for degradation. Unlike exosomes, microvesicles are released directly by budding from the plasma membrane. EVs in extracellular space bind to the surface of recipient cells through protein-protein or receptor-ligand interactions, leading to the internalization of EVs by recipient cells through fusion or endocytosis. EV contents are then released into the recipient cells to manipulate various biological processes
Unlike exosomes, MVs are generated through direct outward budding and fission of the plasma membrane. MVs tend to be larger in size (50–2000 nm) compared with exosomes, despite an overlap of the size range. The release of MVs relies on the dynamic interplay between phospholipid redistribution and cytoskeletal protein contraction [13]. In this process, ADP-ribosylation factor 6 activates phospholipase D, leading to the recruitment of extracellular signal-regulated kinase (ERK) to the plasma membrane. ERK phosphorylates and activates myosin light-chain kinase, which triggers the release of MVs.
Notably, although exosomes and MVs utilize distinct pathways for biogenesis, there are many technical challenges for isolating EVs and specific types of EVs due to the small size of EVs and enrichment of contaminants with similar size and/or density as EVs in biological fluids [33, 34]. Several techniques have been developed for isolating EVs (e.g., ultracentrifugation, density-gradient centrifugation, filtration, size-exclusion chromatography, modified polymer co-precipitation, and commercially available commercial kits) and separating exosomes (e.g., immunoaffinity chromatography) [35]. These techniques have their disadvantages such as low purity, high cost, insufficient homogeneity, and high labor intensity [34, 36, 37]. Besides, the characterization of EVs also faces many technical issues. Methodologies that characterize the sizes of EVs like the dynamic light scattering and nanoparticle tracking analyses cannot distinguish nanoscale contaminants from EVs, and bulk methods like western blotting requires a great number of EVs [34]. Inspiringly, single EV-based high-throughput analysis has been developed recently, which opens a window to fully understand the heterogeneity and complex functions of EVs [38, 39].
Contents of EVs
EVs contain a broad spectrum of proteins, lipids, and nucleic acids. Based on the database ExoCarta (http://www.exocarta.org), there are more than 9700 proteins, 3400 mRNA, and 2800 miRNAs that have been identified in exosomes. Among all identified proteins, exosomes are abundantly loaded with endosome-associated membrane proteins including annexins, flotillin, and Tetraspanins (e.g., CD63, CD81, and CD9) [40, 41]. Exosomes also carry biologically active soluble proteins (e.g., growth factors [42] and transcription factors [43]) and transmembrane proteins (e.g., APP [10]). Furthermore, exosomes contain multiple types of nucleic acids including DNA, mRNAs, and non-coding RNAs like miRNAs and long non-coding RNAs (lncRNAs) [2, 44–46]. These nucleic acids are highly likely to be located within exosomes in a soluble form [47], although recent studies indicated that miRNAs bind to membrane proteins [48]. Besides, exosomes also carry various lipids including sphingomyelin, phosphatidylserine, cholesterol, and ceramide [41, 49], and these lipids are mainly located on the exosomal surface to regulate the biogenesis and release of exosomes [49, 50].
Similar to exosomes, MVs also contain various proteins, lipids, and nucleic acids. Interestingly, MVs have been found to contain certain proteins different from exosomes. For example, MVs express CD40, selectins, integrins, and highly likely cytoskeletal proteins due to their plasma membrane origin [51]. Recent studies reported that small MVs also express CD63-like exosomes, but the expression levels of CD81 and CD9 are significantly lower in MVs versus exosomes [52]. Thus, these surface proteins have been widely utilized to distinguish between exosomes and MVs. Besides, the membranes of MVs are highly enriched in cholesterol, phosphatidylserine, and diacylglycerol [51].
Content sorting mechanisms of EVs
Molecules in the cytosol are sequestrated into ILVs through various machineries. Proteins can be passively loaded and actively transferred into exosomes. ESCRT-related molecules syndecans and syntenin bind to CD63 and Alix through the LYPX9(n)L motif, therefore enhancing EV accumulation of syntenin, clathrin, Alix, CD63, heat shock proteins, and ubiquitinated proteins [53–56]. Protein sorting into exosomes is mediated by tetraspanins [57], Nedd4 family-interacting protein 1 (Ndfip1) [58], SIMPLE [20], and lipid (raft)-related mechanism in an ESCRT-independent manner [59]. For example, exosomal surface proteins CD9 and CD63 bind to CD10, premelanosome protein (PMEL), Epstein Barr virus (EBV) protein, and the latent membrane protein 1 (LMP1) to facilitate the loading of the latter into ILVs/exosomes [27, 57, 60]. Similar to the situation of protein loading, exosomes are loaded with nucleic acids, especially miRNAs, through passive packaging and selective sorting mechanisms [61, 62]. Growing studies have identified multiple soluble/membrane-bound RNA-binding proteins that function as “chaperones” to transfer miRNAs into exosomes [48, 62, 63]. hnRNPA2B1 specifically binds to certain miRNAs with GGAG and CCCU motifs and selectively loads these miRNAs into exosomes [62]. Similarly, SYNCRIP enhances the sorting of miRNAs into exosomes by the same motif-binding mechanism as hnRNPA2B1 [63]. Ago2, a key component of the RNA-induced silencing complex (RISC), loads miRNAs into exosomes with high miRNA-binding affinity via interacting with endosomal CD63 [48]. Together, exosomes contain various bioactive cargos that are passively packaged or selectively loaded. By delivery of cargos, exosomes exert their biological functions under physiological and pathological conditions.
To date, little is known about how cargos in MVs are loaded. It is highly likely that both passive packaging and selective sorting (e.g., endogenous RNA-modulated miRNA sorting [61] and CD63-mediated protein sorting [60]) act in concert to load cargos into MVs. More studies are needed to advance our knowledge on the content-sorting mechanisms of MVs.
Uptake of EVs
Generally, EVs deliver their cargos to target cells mainly through two ways, endocytosis and fusion with target cell membrane. Endocytosis is the dynamic internalization of cargos by cells for signaling transduction and nutrient uptake. There are at least five types or pathways of endocytosis, namely, caveolae-dependent endocytosis, clathrin-dependent endocytosis, clathrin and caveolin-independent endocytosis, micropinocytosis, and phagocytosis [64]. Accumulating evidence has demonstrated the relevance of these pathways to EV uptake [65, 66]. Rat pheochromocytoma PC12 cells have been found to utilize both clathrin-dependent endocytosis and macropinocytosis for EV uptake [66]. In another type of tumor cells, colon carcinoma COLO205 cells exploit both caveolae- and clathrin-dependent endocytosis for EV uptake [67]. Moreover, EVs can be internalized into macrophages by phagocytosis, and phagocytosis is a much more efficient way for EV uptake than endocytosis [68]. Importantly, many proteins that are involved in recognition and uptake of viruses, liposomes, and nanoparticles are expressed on EVs [69]. Following studies further demonstrated that endocytosis of EVs is facilitated by receptor-ligand complexes consisting of CD9, CD33, CD62, CD81, CD106, and many other molecules [65]. It is worth noting that although ligand-receptor interaction plays an important role in the endocytosis of EVs, whether this interaction confers targeting specificity to EVs remains inconclusive, with literature providing support for both possibilities.
EVs can also release their cargos in the cytosol of the recipient cells through fusion or hemi-fusion of EV and recipient cell membranes [2, 4]. The fusion of EV hydrophobic lipid bilayers and recipient cell plasma membrane has been found to be mediated by fusogenic SNARE proteins, Rab family, lipid raft-like domains, integrins, and adhesion molecules [70]. However, opposite viewpoints are raised that SNARE proteins should not mediate the fusion of EVs with recipient cells as the cytosolic sides of these two membranes are in opposite orientations. Therefore, the mechanisms that mediate EV-to-recipient cell fusion remain largely unknown, and evidence has implicated EV-to-recipient cell fusion as a minor mechanism for EV uptake in physiological conditions. Interestingly, the plasma membrane of tumor cells exhibit great potential to fuse with EVs in the low-pH tumor microenvironment conditions due to the enhanced rigidity of plasma membrane and increased sphingomyelin [71]. Moreover, once activated, platelets display higher fusion capacity with EV membrane, suggesting the relevance of EV-to-recipient cell fusion to the pathogenesis of diseases [72].
Besides, EVs can modulate intracellular signaling through directly binding to the surface receptors on the recipient cell [70]. For instance, dendritic cell-derived EVs activate T lymphocytes via CD40-CD40L interaction [73] and enhance immune responses of bystander dendritic cells through binding to Toll-like receptor ligands on bacterial surface [74]. However, whether these EVs are internalized by the recipient cells through ligand-receptor interaction-mediated endocytosis remains to be clarified.
Pathological roles of EVs in NDs
To date, mounting literature has reported roles of EVs in the occurrence and progression of different NDs including AD, PD, ALS, and HD. Here, we discuss the contributions of EVs derived from different types of brain cells to the pathogenesis of NDs (Table 1; Fig. 2).
Table 1.
Summary of pathological functions of EVs in NDs
| Cell origin | Disease | Up-regulated cargos | Down-regulate cargos | Outcome of EV cargo alteration | References |
|---|---|---|---|---|---|
| Neuron | AD | P-T181-tau, Aβ1−42, cathepsin D | – | Promoting Aβ deposition and NFT formation | [84] |
| AD | APP mRNA & protein | – | Facilitating the production of Aβ | [10] | |
| AD | miR-124, miR-155, miR-146a, miR-21, miR-125b | – | Inducing microglial activation and pro-inflammatory cytokine release | [87] | |
| AD | – | miR-185 | Elevating APP expression levels | [10] | |
| PD | α-syn | – | Inducing neurotoxicity and α-syn-rich Lewy bodies formation | [272] | |
| PD | Rab8b, Rab31 | – | Contributing to non-motor symptoms in PD pathology including hearing loss | [123] | |
| PD | 20 S Proteasome complex, PARK7, Gelsolin, Amyloid P component, Clusterin | – | Participating in PD onset and progression | [124] | |
| PD | miR-19a-3p, miR-155 | – | Mediating α-syn-induced inflammatory responses | [121] | |
| ALS | mutant SOD1 | – | Inducing mitochondrial toxicity | [138] | |
| ALS | DPRs, TDP-43 | – | Inducing astrocyte toxicity and neurodegeneration | [139] | |
| ALS | miR-4736, miR-4700-5p, miR-1207-5p, miR-4739, miR-4505, miR-24-3p, miR-149-3p, etc. | miR-1268a, miR-2861, miR-4508, miR-4507, miR-3176, miR-3911, miR-150-3p, etc. | Disturbing neuroplasticity and enhancing neural damage | [141] | |
| HD | mutant HTT | – | Inducing neurodegeneration | [156] | |
| Astrocyte | AD | p-Tau | – | Enhancing the formation of NFT | [95] |
| AD | BACE1, complement proteins | – | Promoting Aβ cleavage and neuronal damage | [99, 100] | |
| PD | – | miR-200a-3p | Inhibiting c-Jun N-terminal kinase cell death pathway | [129] | |
| ALS | mutant SOD1 | – | Inducing selective motor neuron death | [146] | |
| ALS | – | miR-494-3p | Unlocking SEMA3A-induced motor neuron degeneration | [147] | |
| ALS | IL-6 | – | Exacerbating pro-inflammatory responses of neuroglial cells | [148] | |
| HD | – | CRYAB | Suppressing EV secretion | [273] | |
| Microglia | AD | Human tau | – | Spreading of tau protein | [80] |
| AD | TREM2 | – | Changing environment around Aβ and promoting microglia to phagocytose Aβ | [114] | |
| AD | APP/Aβ, P2RY12, TMEM119, FTH1, TREM2 | – | Stimulating microglial activation and contributing to Aβ deposition | [111, 112] | |
| AD | Cholesterol, BMP, MhCer lipid species | DHA-containing polyunsaturated lipids | Inducing defect in acyl-chain remodeling | [112] | |
| AD | miR-28-5p, miR-381-3p, miR-651-5p, miR-188-5p | – | Enhancing neuroinflammation and cellular senescence | [112] | |
| PD | α-syn | – | Spreading α-syn oligomers through microglia-neuron α-syn transmission | [130] | |
| PD | MHC class II molecules, TNF-α | – | Triggering neuroinflammation and dopaminergic neurodegeneration | [131, 132] | |
| ALS | mutant SOD1 | – | Inducing neurotoxicity and motor neuron death | [150] | |
| ALS | HMGB1, miR-155, miR-146a | – | Activating microglia and impairing mitophagy | [151] | |
| Oligodendrocyte | PD | α-syn | – | Inducing neurotoxicity and formation of α-syn-rich Lewy bodies | [136] |
BMP, bis(monoacylglycerol)phosphate; MhCer, monohexosylceramide; DHA, docosahexaenoic acid
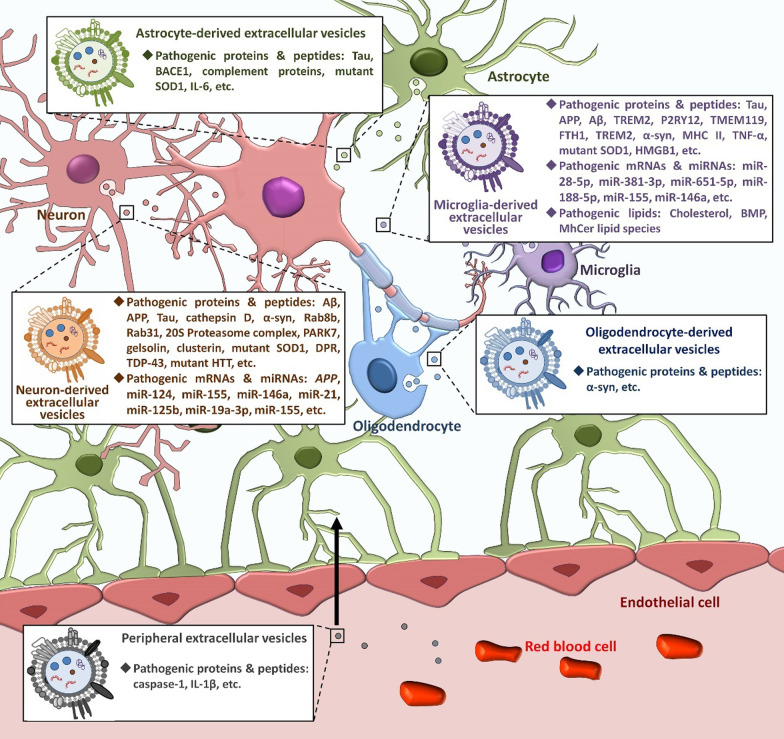
Fig. 2.
The pathological effects of EVs on NDs. In the brain, there are EVs released from brain cells (e.g., neurons, astrocytes, microglia, and oligodendrocytes) and peripheral EVs that enter the brain through the BBB. Under pathological conditions, these EVs carry pathogenic factors including proteins/peptides, coding and non-coding RNAs, and lipids that contribute to the onset and progression of NDs through facilitating the spreading and aggregation of pathogenic molecules, enhancing cell death, stimulating inflammatory responses, and disrupting the BBB
Pathological roles of EVs in AD
AD is the most common neurodegenerative disease and most common cause of dementia in the elderly [75]. The etiology of AD is not clear, which is mainly related to genetic and environmental factors like phosphorylated Tau protein (p-Tau) and amyloid-beta (Aβ) [75]. Other hypotheses/theories including neuroinflammation, gut-brain axis disorder, and metabolic dysfunction have also been proposed [75–78]. Interestingly, growing evidence has shown altered secretion and functions of EVs during the progression of AD [79], and that blocking EV release significantly mitigates AD phenotype [80], revealing the non-ignorable contributions of EVs to the pathogenesis of AD [81].
Pathological roles of neuron-derived EVs (NDEVs) in AD
Neurons are electrically excitable cells that communicate with other cells via neurotransmission, and are the main component of the CNS [4]. Neurons release a great number of EVs to modulate synaptic activities and regulate cell homeostasis in physiological conditions [4, 82]. The pathological roles of NDEVs in AD are receiving much attention from the scientific community. Recently, an immunoabsorption-based strategy using anti-human L1CAM antibody has been developed to purify NDEVs from blood samples [83]. NDEVs isolated from blood of AD patients demonstrate significantly increased levels of Aβ1−42 and p-Tau, and altered lysosomal proteins, when compared with healthy donors [83, 84]. However, recent studies have questioned the utility of L1CAM as a marker of NDEVs [85, 86]. L1CAM is not specifically expressed in neurons, but also in oligodendrocytes in the CNS, immune cells (e.g., T cells, B cells, and monocytes), and endothelial cells. Besides, Norman et al. demonstrated that L1CAM is not associated with EVs in human CSF or plasma. Instead, ND-related proteins (e.g., soluble α-synuclein [α-syn]) in plasma can nonspecifically bind to the anti-L1CAM antibody and are isolated by L1CAM-immunocapture experiment [85]. Hence, advanced methodology is required to purify NDEVs from blood samples without contamination. In addition, altered levels of AD-related miRNAs have been found in EVs derived from human neuroblastoma SH-SY5Y cells stably expressing APP695 Swedish mutation (SHSwe) and mouse neuroblastoma N2a cells expressing human APP, compared to the responding controls [10, 87]. These observations suggest that NDEVs facilitate the pathological spread of AD-related factors among brain cells and drive Aβ to form amyloid fibrils in the CNS [88, 89].
The altered profiles of cargos also influence the biological functions of NDEVs. Compared with NDEVs isolated from the plasma of healthy individuals, NDEVs isolated from blood of AD patients exhibit significant neurotoxic effects on cultured E18 rat cortical neurons, ascertained by the reduced cell viability determined by MTT assay [90]. The NDEV-induced neuronal damage is likely mediated by the transition of pathogenic molecules of AD such as APP and toxic Aβ oligomers [10, 88]. The complement system, especially the membrane attack complex (MAC), also mediates the pathological effects of NDEVs isolated from blood of AD patients, since CD59, a GPI-anchored cell membrane glycoprotein that inhibits MAC assembly, significantly reduces NDEV-induced neuronal loss [90]. In an in vitro AD model, EVs derived from SHSwe cells can be internalized by microglia, and induce acute and delayed microglial up-regulation of tumor necrosis factor-alpha (TNF-α) and other pro-inflammatory factors that cause neuroinflammation, through delivery of miR-155, miR-146a, miR-124, miR-21 and miR-125b to the microglia [87]. However, we recently found that N2a cells release miR-185-enriched EVs to suppress the expression of APP in recipient N2a cells in vitro, which implies an anti-Aβ deposition role of NDEVs [10]. Therefore, NDEVs exhibit both pathological and beneficial effects, suggesting dynamic changes of NDEVs during the progression of AD.
Pathological roles of astrocyte-derived EVs (ADEVs) in AD
Astrocytes are the most abundant glial cells in the CNS and are associated with many functions vital to CNS physiology, including blood-brain barrier (BBB) formation and maintenance, neuroplasticity, neurotransmission, and metabolic regulation [91]. Astrocytes have high capacity for EV release and ADEVs have been shown to be an important contributor to ND pathogenesis [9, 92].
In AD, astrocytes respond to both p-Tau and Aβ, leading to the accumulation of Aβ42 protofibrils within astrocytes. The excessive Aβ up-regulates the expression of p-Tau, prostate apoptosis response 4 and ceramide to form giant endosomes for ADEV release in a co-culture system [93]. In contrast, Abdullah et al. reported that Aβ1−42 inhibits ADEV release via stimulation of the JNK signal pathway in vitro [94]. Although conflicting results have been obtained regarding the effects of Aβ on ADEV secretion, ADEVs have been found to promote Aβ aggregation and interfere with Aβ uptake by neuroglia [95], leading to neuronal loss in AD cells and animal models [96, 97]. Inhibition of Aβ formation in astrocytes by the calcium-sensing receptor signaling antagonist calcilytic NPS 2143 or blockade of exosome secretion by GW4869, a neutral sphingomyelinase2 (nSMase2) inhibitor [98], has been shown to dramatically repress the release of p-Tau-loaded ADEVs or Aβ aggregation, respectively [95]. Moreover, enzyme-linked immunosorbent assay (ELISA) has identified significantly increased levels of BACE1 and complement proteins (e.g., C3b, and C5b-C9 terminal complex) in both plasma- and CSF-isolated ADEVs [99, 100]. BACE1 is a beta-secretase involved in the cleavage of APP to form Aβ peptides, and C3b and C5b-C9 complex may injure neurons directly or indirectly via enhancing microglial neurotoxicity [100, 101]. These results suggest that ADEVs regulate Aβ deposition and exert neurotoxicity through transferring Aβ processing enzymes and pro-inflammatory factors in addition to p-Tau. Interestingly, ADEVs may also function as a negative regulator of AD progression since ultrasound-mediated ADEV release alleviates Aβ-induced neurotoxicity in vitro. Whether ADEVs exert beneficial effects on AD in vivo remains to be investigated.
Pathological roles of microglia-derived EVs (MDEVs) in AD
Microglia are resident immune-competent cells of the brain, which respond to exogenous and endogenous CNS insults and regulate brain development, neuronal network maintenance, and injury repair. Under pathological conditions, microglia polarize into different phenotypes to exert neurotoxic or neuroprotective functions and the simplest model defines microglial polarization into two main phenotypes: classic M1 activation (pro-inflammatory) and alternative M2 activation (anti-inflammatory) [102]. Transcriptome studies at the single-cell level further indicate that the M1/M2 paradigm is inadequate to summarize microglial phenotypes, since microglia rarely exhibit a significant bias toward either M1 or M2 phenotype in vivo [103]. Instead, distinct microglia subtypes have been identified in physiological and pathological conditions, which reflect the innate dynamic nature of tissue monocytes [104–106]. Thus, microglial polarization is multidimensional with extensive overlap in gene expression rather than a simplified linear spectrum [105]. The activation of microglia, irrespective of the particular polarized state, has emerged as the driving force of neuroinflammation in NDs [107–109]. In this process, microglia release a great number of EVs to mediate delivery of pathogenic molecules, to regulate the functions and viability of brain cells, and to facilitate the establishment of disease-related microenvironment, suggesting an important role of MDEVs in the pathogenesis of NDs [110].
In AD, MDEVs have been found to directly transfer classic AD pathogenic factors including Aβ and tau among cells. Extracellular Aβ42 protofibrils can be internalized by microglia and then trafficked into MDEVs [111–113]. Moreover, MDEVs have been reported to strongly increase Aβ neurotoxicity through promoting Aβ1–42 extracellular aggregates to form small soluble neurotoxic species via lipid components of EVs. Microglia also phagocytose and load human tau into MDEVs [80]. MDEVs thus deliver tau to neurons through non-synaptic pathways and trigger abnormal aggregation of tau, demonstrating a synergy between microglia and EVs in the spread of tau pathology in human brains [80].
Besides Aβ and p-Tau, shotgun proteomics studies have demonstrated a significant decrease in the abundance of homeostatic microglia markers P2RY12 and TMEM119, and increased levels of AD-associated factors FTH1 and TREM2 in CD11b+ MDEVs isolated from cryopreserved human brain tissues of AD patients, compared with age-matched normal/low pathology cases [112]. Lipidomic analysis also showed increases in levels of cholesterol, major bis(monoacylglycerol)phosphate, and monohexosylceramide lipid species, and a significant decline in levels of docosahexaenoic acid-containing polyunsaturated lipids in AD patient brain-derived MDEVs versus controls, indicating potentially defective acyl-chain remodeling [112]. Inflammation and cellular senescence-related miRNAs, namely miR-28-5p, miR-381-3p, miR-651-5p, and miR-188-5p, have also been found to be enriched in AD patient brain-derived MDEVs, further suggesting the complicated mechanisms of MDEV-mediated neuroinflammation and neurotoxicity in AD [112].
Importantly, Li et al. utilized IL-4 to induce the M2 phenotype of microglia and found that EVs derived from M2 microglia restored viability and mitochondrial dysfunction of neuronal cells in vitro, and reduced Aβ deposition in vivo, suggesting the beneficial effects of MDEVs on AD. Moreover, Huang et al. reported that TREM2 on the surface of MDEVs binds to Aβ, thus changing the inflammatory environment around Aβ and facilitating Aβ phagocytosis by microglia, which suggests a MDEV-mediated mechanism of microglia–Aβ crosstalk that accelerates Aβ elimination [114].
Overall, EVs have been identified as a key component of pathological microenvironment in AD as deregulation of EV release and cargo sorting significantly influences the onset and progression of AD. Inspiringly, a great number of studies has been performed and more pathological functions of EVs are highly likely to be announced shortly, making EVs and their contents a potential biomarker and therapeutic target of AD.
Pathological roles of EVs in PD
PD is another common ND among the elderly with the impairment of voluntary motor control evolving over time. The main pathological change of PD is the degeneration of dopaminergic neurons in substantia nigra of midbrain, resulting in significant decrease of dopamine content in the striatum [115]. Although the exact etiology and natural course of PD have yet to be fully clarified, the spreading of neuronal cytoplasmic protein α-syn with the polymorphous and fibrillar conformation by EVs has emerged as a key pathogenic factor that mediates the degeneration of dopaminergic neurons [115].
Pathological roles of NDEVs in PD
Multiple groups have reported the existence of α-syn in NDEVs in an in vitro PD model, SH-SY5Y human neuronal cells with α-syn expression [116, 117]. Afterwards, α-syn has been identified in L1CAM+ NDEVs isolated from human blood, and NDEVs collected from the plasma samples of PD patients have significantly higher levels of α-syn compared with healthy controls [118, 119]. Although anti-L1CAM-capture of NDEVs may be problematic, these findings implicate the involvement of NDEVs in the transmission of α-syn. This premise is confirmed by Danzer et al., who demonstrated efficient neuron-to-neuron transportation of α-syn oligomers to induce α-syn oligomerization in normal neurons, therefore inducing neuronal death, promoting the spreading of pathological synuclein, and enhancing the disease process [116, 120]. NDEVs also transfer α-syn to microglia and impair microglial autophagy [121]. A following study showed that the sorting of α-syn into EVs is regulated by sumoylation-mediated membrane binding [122].
In addition, FGF2-triggered hippocampal NDEVs are specifically enriched in Rab8b and Rab31 that may contribute to non-motor symptoms in PD pathology including hearing loss [123]. Other PD-related proteins including the 20 S Proteasome complex (PSMA1-3, PSMA5-7, PSMB1, PSMB3, and PSMB5-6), Parkinson’s disease protein 7 (PARK7), Gelsolin, Amyloid P component, Clusterin, and Stromal cell-derived factor 1 (SDF-1) are also identified in PD patient plasma-derived NDEVs [124]. The enrichment of these pathogenic proteins in NDEVs may also participate in the onset and progression of PD directly or indirectly, which requires further investigations. Moreover, multiple miRNAs including miR-19a-3p and miR-155 have been found to be overloaded into NDEVs collected from in vitro PD models and blood samples of PD patients [121, 124]. miR-19a-3p and its family members in NDEVs target various transcripts including those that translate phosphatase and tensin homolog/AKT/mTOR signaling pathway components to suppress autophagy in recipient cells, and miR-155 is a key mediator of α-syn-induced inflammatory responses [121, 124–126]. Therefore, NDEVs facilitate α-syn aggregation and neuroinflammation via delivering PD-associated miRNAs to microglia, hence contributing to the onset and progression of PD.
Meanwhile, the beneficial effects of NDEVs on PD have also been found. EVs isolated during dopaminergic neuron differentiation reduce protein levels of interleukin (IL)-6, IL-1β, TNF-α, and reactive oxygen species (ROS) in the substantia nigra of a rodent model of PD, highly likely through wnt5a-mediated neuroinflammation modulation [127]. Hence, similar to the situation in the pathogenesis of AD, NDEVs are also double-edged in the pathogenesis of PD.
Pathological roles of ADEVs in PD
In PD, astrocytes and microglia remove extracellular α-syn via endocytosis to avoid α-syn accumulation in neurons [48, 49]. Meanwhile, α-syn uptake induces inflammatory response of astrocytes, which causes excessive release of ADEVs. Although there is evidence supporting glia-glia and glia-neuron transfer of α-syn through EVs [128], whether ADEVs contain α-syn and directly mediate the spreading of α-syn remain unknown. Moreover, although astrocytes carrying PD-related mutant LRRK2 G2019S release comparable numbers of EVs versus normal astrocytes, the LRRK2 G2019S-ADEVs fail to provide full neurotrophic support after being internalized by dopaminergic neurons, indicating that alterations of the enrichment of ADEV cargos directly contribute to the progression of PD. miRNAs in ADEVs are a convincing example. Shakespear et al. reported that ADEVs contain high levels of miR-200a-3p which targets the 3’-untranslated region (UTR) of Map2k4 and MKK4 mRNA, therefore inhibiting the c-Jun N-terminal kinase cell death pathway in an in vitro model of PD [129]. EVs derived from MPP (a PD-related neurotoxin)-stimulated astrocytes contain reduced levels of miR-200a-3p, resulting in absence of caspase-3 signaling inhibition and enhancement of dopaminergic neuron degeneration.
Pathological roles of MDEVs in PD
Investigations on the pathological effects of MDEVs on PD initiated from identification of α-syn oligomers in MDEVs. EVs obtained from microglia treated with preformed fibrils (PFF) (PFF-MDEVs) contain high levels of α-syn oligomers [130]. More importantly, α-syn oligomers have been detected in CD11b+ MDEVs derived from CSF of PD patients, confirming the in vitro findings [130]. MDEVs then spread α-syn oligomers through microglia–neuron α-syn transmission, leading to dopaminergic neuron degeneration and behavioral changes of mice that received stereotaxic injection of PFF-MDEVs into the striatum [130]. Moreover, α-syn induces an increase of exosomal secretion by microglia, forming a vicious cycle to exacerbate MDEV-mediated pathological spread of α-syn [131]. Besides, EVs derived from microglia stimulated by α-syn/interferon-γ (IFN-γ)/lipopolysaccharide (LPS) to mimic PD inflammatory conditions also contain high levels of MHC class II molecules and TNF-α that trigger dopaminergic neurodegeneration, indicating the complex mechanisms of MDEV-mediated onset and progression of PD [131, 132].
Pathological roles of oligodendrocyte-derived EVs (ODEVs) in PD
Besides the aforementioned cell types, other types of brain cells also perform vital physiological and pathological functions in the brain, particularly oligodendrocytes, glial cells that generate myelin sheaths to promote rapid neurotransmission in the CNS. Triggered by neuronal signals, myelinating oligodendrocytes secrete EVs into the extracellular space [133]. These ODEVs can be internalized by neurons, supporting axonal transport and maintenance [134]. Given the great impact of ODEVs on the homeostasis of the CNS, studies on the pathological contributions of ODEVs in PD have been carried out recently.
The most recent study using a modified ELISA assay for brain-derived EVs, has demonstrated that the plasma levels of ODEVs are significantly higher in PD patients, compared with healthy controls and patients with multiple system atrophy (MSA), a synucleinopathy whose symptoms largely overlap with that of PD [135]. Similar to the cell type-specific EV immunoprecipitation approach for NDEV and ADEV isolation from human blood and CSF, Dutta et al. utilized an antibody for myelin oligodendrocyte glycoprotein (MOG) to collect ODEVs from the blood of PD patients [136]. The collected EVs contain significantly higher levels of α-syn than healthy controls, indicating ODEVs as a platform for α-syn spreading in the CNS [136]. However, our knowledge on the pathological contributions of ODEVs in PD remains seriously lacking, and extensive investigations are needed in the future.
Together, numerous studies have suggested exosomes as a double-edged sword in PD. More comprehensive studies are needed to clarify the pathological and beneficial effects of exosomes on PD.
Pathological roles of EVs in ALS
ALS is a fatal, adult-onset neurodegenerative disease characterized by a progressive loss of motor neurons in the brain, brainstem, and spinal cord, rapidly leading to atrophy of bulbar, limb, or respiratory muscles. Although the majority of clinical ALS cases are sporadic, mutations in human copper-zinc superoxide dismutase (SOD1) and other genes have been identified in inherited cases of ALS. As a key component of pathological microenvironment, EVs have been found to play a significant role in the pathogenesis of ALS.
Pathological roles of NDEVs in ALS
One important contribution of NDEVs to the pathogenesis of ALS is the delivery of pathogenic factors to neuroglial cells. A recent study reported that EVs positive for SNAP25 (a synaptic marker) harvested from the brain and spinal cord tissues of an ALS mouse model contain misfolded neurotoxic SOD1 [137]. Microglial uptake of mutant SOD1-containing NDEVs induces inflammatory responses and reduces the phagocytic ability of microglia [138]. Moreover, other pathogenic factors of ALS, dipeptide repeat proteins (DPRs) and TAR DNA-binding protein-43 (TDP-43), have also been found in EVs released from spinal motor neurons derived from induced pluripotent stem cells from C9orf72-ALS patients [139]. DPR-containing NDEVs can be internalized by astrocytes and induce astrocyte toxicity, therefore causing neurodegeneration [139, 140]. These observations suggest a tight association of NDEVs with progressive propagation of ALS-related pathology spreading from the CNS foci. The miRNA profiles are also significantly altered in NDEVs in plasma of ALS patients [141]. In ALS patient plasma-isolated NDEVs, 13 miRNAs were significantly up-regulated (e.g., miR-24-3p) and 17 miRNAs were significantly down-regulated (e.g., miR-150-3p), compared with controls. miR-24-3p has been identified as a neurodegeneration-related miRNA by disturbing neuroplasticity and enhancing neural damage presumably through regulating BOK and CHD5 [142, 143]. In contrast, miR-150-3p has neuroprotective effects by targeting CASP2 [144]. The up-regulated neurotoxic miRNAs and down-regulated neuroprotective ones in NDEVs imply another potential mechanism of NDEV-mediated pathogenesis of ALS. Moreover, the expression levels of proteins that are involved in the regulation of synaptic membrane and axoneme are also significantly reduced in EVs collected from the cerebrospinal fluid (CSF) of ALS patients [145]. However, whether these observations are mediated by NDEVs remains unknown since the cellular origins of these exosomes are unclarified.
Pathological roles of ADEVs in ALS
Under ALS pathological conditions, astrocytes exhibit distinct EV secretion capacity. For example, in ALS models in vitro, astrocytes with SOD1 mutation release more EVs compared with controls [146], leading to increased effect of ADEVs on the brain microenvironment in ALS. More importantly, the content profiles of ADEVs are also significantly altered in ALS. Basso et al. reported that mutant SOD1 is packaged into ADEVs [146]. The delivery of mutant SOD1 from astrocytes to neurons via ADEVs induces selective motor neuron death in vitro. Moreover, human induced astrocytes from ALS patients carrying C9orf72 mutations release EVs lacking miR-494-3p, a negative regulator of axonal maintenance-related gene semaphorin 3 A (SEMA3A) [147]. The depletion of miR-494-3p in ADEVs therefore unlocks SEMA3A-induced motor neuron degeneration in ALS. Similar to the situation in vitro, Chen et al. showed a significant increase of IL-6 in ADEVs isolated from the plasma of sporadic ALS patients, suggesting alterations of ADEV cargos in ALS patients [148]. This finding implies an important role of the ADEV-mediated pathological spread of pro-inflammatory factors in the initiation and exacerbation of neuroinflammation, a key pathological feature of ALS.
Pathological roles of MDEVs in ALS
The involvement of microglia in the onset and progression of ALS is being increasingly recognized. In ALS animal models, the overexpression of mutant SOD1 drives microglial activation, autophagy impairment, and hyperexpression of pro-inflammatory factors (e.g., MFG-E8, RAGE, IL-1β, TNF-α, and iNOS), therefore reducing the capacity for mutant SOD1 elimination [149]. Consequently, microglia release excessive mutant SOD1 via MDEVs [150]. When motor neurons internalize MDEVs, the intracellular accumulation of mutant SOD1 then induces neurotoxicity and neuronal damage [149, 150]. Furthermore, the levels of HMGB1, miR-155 and miR-146a are significantly increased in EVs derived from mutant SOD1-overexpressing microglia [151]. The HMGB1/RAGE axis has been reported to mediate neuroinflammation via impairing the mitophagy flux in microglia [152], and miR-155 and miR-146a have been identified as pro-inflammatory miRNAs that regulate microglial activation [153, 154]. Thus, MDEVs enriched in these pro-inflammatory molecules also contribute to neuroinflammation, leading to aggravation of ALS phenotypes.
Pathological roles of EVs in HD
HD is a rare, progressive, and fatal hereditary ND caused by CAG expansion in the first coding exon of the HTT gene [155]. It is characterized by progressive movement dysfunction and cognitive decline, ending in death within 15–20 years after diagnosis. Elevated levels of total HTT and mutant HTT (mHTT) fragments have been reported in EVs from plasma of both pig models and HD patients compared to controls, implying the involvement of EVs in the pathogenesis of HD [156].
Pathological roles of NDEVs in HD
Neurons express excessive HTT in the brains of HD patients [155, 157]. EVs have been found to inherit the mRNA with an expanded CAG-repeat element from their parent cells with excessive HTT expression, although total HTT and mutant HTT fragments have not been detected in NDEVs [157]. These observations implicate that NDEVs participate in the spreading of pathogenic HTT within the brain, although conclusive evidence remains lacking. Besides, an in vitro study also suggests a role for NDEVs against HTT spreading [158]. NDEVs can transfer HTT-targeting miRNAs to HD patient-derived neurons, which leads to the inhibition HTT mRNA expression in the latter, providing evidence for NDEV-dependent HTT suppression mechanisms [158]. Despite these preliminary studies in vitro, more studies are required to further clarify the pathological/beneficial roles of NDEVs in HD.
Pathological roles of ADEVs in HD
To date, studies that focus on the involvement of ADEVs in the pathogenesis of HD remain limited. Deep sequencing analysis of genes highly expressed in ADEVs reveals that ADEVs are responsible for promoting HD [159]. In the HD 140Q knock-in mouse model of HD, although mHTT is not identified in ADEVs, it inhibits ADEV release through suppressing the expression of αB-Crystallin (CRYAB), a heat shock protein that mediates EV secretion [160]. Furthermore, the sorting of CRYAB into ADEVs is also inhibited by mHTT, leading to neuroglial activation and neuroinflammation that cause neurodegeneration in HD.
Pathological/beneficial roles of peripheral EVs in NDs
Interestingly, growing evidence has implicated the involvement of peripheral EVs in the pathogenesis of neurological diseases with the discovery of crosstalk between brain and other organ systems in a “bottom-up” manner including gut-brain, lung-brain, and bone-brain axes [161, 162]. Intestinal epithelial cells have been reported to release EVs to induce IL-1β-mediated neuronal injury in sepsis-associated encephalopathy, which launches long-term cognitive deficits and neurodegeneration [163]. Moreover, ventilation-induced lung injury causes lung inflammation, leading to selective loading of caspase-1 into lung-derived EVs [164]. Caspase-1-enriched peripheral EVs induce microglial activation and cell pyroptosis in the brain, revealing circulating EVs as a pathogenic factor of NDs [164].
Besides, peripheral EVs have been reported with potential beneficial effects on NDs. For instance, young osteocytes, the most abundant cells in bone, secrete neuroprotective EVs to enhance cognitive function and ameliorate pathological changes in AD mice [161]. Another example is mesenchymal stem cells (MSCs) that have been widely used for production of EVs with therapeutic effects on NDs (details in this field summarized in a later section) [165–167]. These observations imply that endogenous MSCs may release EVs to decrease the risk of NDs or delay the progression of NDs, which is an interesting topic for future investigations.
It is worth noting that there are also hints for the involvement of EVs in the pathogenesis of multiple sclerosis (MS), an autoimmune ND [168]. However, they are not discussed in this review due to the limited literature support. Besides, although out of the scope of our review, EVs also participate in acute neural damage by modulating the activation of neurotoxic microglia and astrocytes [165, 169]. Overall, current evidence indicates both pathological and beneficial roles of EVs in the pathogenesis of NDs. More studies, especially in vivo ones, are urgently needed to clarify the involvement of EVs in NDs, and develop novel EV-based diagnostic and therapeutic strategies for NDs.
EVs as novel biomarkers for the diagnosis of NDs
Identification of biomarkers for NDs in the blood is challenging since the BBB prevents free passage of molecules between the CNS and blood compartments. Furthermore, several potential biomarkers related to the pathology of NDs are expressed in non-CNS tissues, significantly confounding their measurement in the blood. Given the pathological roles of EVs in NDs and their BBB penetration capacity, the brain-derived EVs natively possess the potential to serve as biomarkers for diagnosis of NDs. In this section, we summarize recent studies that provide evidence for utilizing EVs and their cargos as potential biomarkers for disease diagnosis (Table 2).
Table 2.
Summary of differentially expressed EV contents and their potential diagnostic values in NDs
| Disease | Down-regulated | Up-regulated | AUC | Sensitivity (%) | Specificity (%) | Specimens | Species | References |
|---|---|---|---|---|---|---|---|---|
| AD | APOC3, APOH, C4BPα, CO3, KV230 | AACT, CO9, IGHM, K2C6A | – | – | – | Serum EVs | Human | [172] |
| AD | miR-342-3p, miR-23b-3p, miR-24-3p, miR-125b-5p | miR-141-3p, miR-342-5p | 0.919 | 81.7 | – | Serum EVs | Human | [174] |
| AD | BACE-1-AS-LncRNA (in Pre-AD) | BACE-1-AS-LncRNA (in late AD) | – |
75 (pre-AD) 68 (late-AD) |
100 100 |
Plasma EVs | Human | [177] |
| AD | miR-135a, miR-384 | miR-193b | – | 99 | 95 | Plasma EVs | Human | [175] |
| AD | miR-138-5p, miR-342-3p | miR-29c-5p, miR-143-3p, miR-335-5p, miR-485-5p | 0.880 | – | – | Serum EVs | Human | [176] |
| AD | – |
Aβ42/40 miR-384 |
0.973 0.909 |
– | – | Blood NCAM+ NDEVs | Human | [178] |
| AD | – | miR-29c-3p | 0.927 | Blood NCAM+ NDEVs | Human | [179] | ||
| AD |
miR-212 miR-132 |
– |
0.84 0.77 |
92.2 | 69 | Blood L1CAM+ NDEVs | Human | [180] |
| AD | – |
tau, p-T181-tau, p-S396-tau, Aβ1−42 |
0.99 | 96 | Blood L1CAM+ NDEVs | Human | [181] | |
| PD | – | α-synuclein | 0.724 | 76.8 | 53.5 | Plasma EVs | Mouse | [183] |
| PD | Prp | – | – | – | – | Plasma EVs | Human | [184] |
| PD |
miR-1 miR-19b-3p |
miR-153, miR-409-3p miR-10a-5p let-7 g-3p |
0.920 0.705 0.990 0.900 |
– | – | CSF EVs | Human | [185] |
| PD | – | α-synuclein, clusterin | 0.98 (PD VS. atypical PD) | – | – | Serum EVs | Human | [119] |
| PD | α-synuclein (in PD VS. MSA) | 0.902 PD VS. MSA) | – | – | Blood MOG+ ODEVs, L1CAM+ NDEVs | Human | [136] | |
| ALS | – | CORO1A | – | – | – | Plasma EVs | Human | [186] |
| ALS | – | TDP-43, NFL | – | – | – | Plasma EVs | Human | [187] |
| ALS | miR-146a-5p | – | – | – | – | CSF EVs | Human | [189] |
| ALS | – |
miR-15a-5p miR-193a-5p |
0.976 0.844 |
92.9 80.0 |
91.7 88.9 |
Plasma EVs | Human | [190] |
| ALS |
miR-10b-5p miR-29b-3p |
miR-146-5p miR-199a-3p, miR-199a-5p miR-151a-3p, miR-151a-5p |
– | – | – | Plasma L1CAM+ NDEVs | Human | [191] |
AACT, alpha-1-antichymotrypsin; CO9, complement component 9; IGHM, immunoglobulin heavy constant mu; K2C6A, keratin, type II cytoskeletal 6 A; APOC3, apolipoprotein C-III; APOH, beta-2-glycoprotein 1; C4BPα, C4b-binding protein alpha chain; CO3, Complement C3; KV230 immunoglobulin kappa variable 2–30
EVs as novel biomarkers for the diagnosis of AD
As accumulation of Aβ deposits and formation of neurofibrillary tangles composed of p-Tau in the brain are major pathological hallmarks of AD, neuroimaging approaches including magnetic resonance imaging (MRI) and positron emission tomography (PET), and CSF examinations that detect Aβ (Aβ1–42 and Aβ1–40) and p-Tau, are used as the gold-standard for AD diagnosis [170]. However, the invasive nature of procedures, the associated risks, and the relatively high costs have limited their practicability. Blood-based diagnostics can overcome these disadvantages due to their non-invasiveness, lower cost, and capability of multiple sampling in large cohorts. The correlation between blood-based AD biomarkers and pathological changes in the brain has been widely investigated [171].
Scientists have isolated EVs from sera of healthy controls and AD patients, and characterized their contents via proteomic analyses [172]. They identified that four circulating EV proteins, including alpha-1-antichymotrypsin (AACT) isoform 1, complement component 9, immunoglobulin heavy constant mu Isoform 2, and keratin, type II cytoskeletal 6 A, are significantly up-regulated in AD patients compared with control individuals. Furthermore, five circulating EV proteins, including apolipoprotein C-III, beta-2-glycoprotein 1, C4b-binding protein alpha chain (C4BPα), complement C3, and immunoglobulin kappa variable 2–30 are significantly down-regulated in AD patients compared with control individuals, implying these proteins as putative biomarker candidates. The altered expression levels of two Aβ-binding proteins AACT and C4BPα, in AD patient serum-isolated EVs, were further validated in individuals from independent cohorts [172]. Besides, non-coding RNAs in peripheral EVs were found to have diagnostic potentials for AD [173]. Lugli et al. identified seven miRNAs (e.g., miR-342-3p, miR-141-3p, miR-342-5p, miR-23b-3p, miR-24-3p, miR-125b-5p, and miR-152-3p) in plasma EVs as significant predictors of AD in a machine learning model [174]. The receiver operating characteristic (ROC) curve analysis, which identifies optimal cut-off values for these miRNAs by the area under the curve (AUC), suggested excellent sensitivity of these miRNAs in plasma EV for discriminating AD patients from healthy controls (sensitivity, 81.7%). In addition, Yang et al. reported that miR-135a and miR-384 were up-regulated, while miR-193b was down-regulated in EVs isolated from AD patient sera. The combination of miR-135a, miR-193b, and miR-384 in serum-derived EVs performs better in AD diagnosis than each individual miRNA (sensitivity, 99%; specificity, 95%) [175]. Moreover, miRNAs in blood-derived EVs have been demonstrated to be predictors of AD at the asymptomatic stage (pre-AD). A multicenter study has identified a panel of miRNAs that are changed (up-regulated: miR-29c-5p, miR-143-3p, miR-335-5p, and miR-485-5p; down-regulated: miR-138-5p and miR-342-3p) in AD patients and predicted that this panel can detect pre-AD 5 to 7 years before the onset of cognitive decline (AUC = 0.88) [176]. Fotuhi et al. also found that the level of BACE1-AS lncRNA in plasma-derived EVs significantly differs between AD patients and healthy controls, and that the plasma-derived EV lncRNA BACE1-AS exhibited great diagnostic power for pre-AD (sensitivity, 75%; specificity, 100%) [177]. These findings show the possibility of utilizing circulating EV contents as a biomarker for AD before the occurrence of clinical symptoms.
To further enhance the sensitivity and specificity of EV-based diagnosis, scientists have made a great effort to identify potential AD biomarkers in NDEVs, ADEV, and MDEVs isolated from plasma or serum. They demonstrated that Aβ42/40 (AUC = 0.973) and miR-384 (AUC = 0.909) in NDEVs co-labeled with neural cell adhesion molecule (NCAM) and ATP-binding cassette transporter A1 have potential advantages in AD diagnosis [178]. In another study, miR-29c-3p in plasma NCAM/amphiphysin 1 dual-labeled NDEVs showed a good diagnostic performance for subjective cognitive decline (AUC = 0.789) and AD (AUC = 0.927) [179]. Combination of Aβ42, Aβ42/40, Tau, p-T181-tau, and miR-29c-3p in plasma-isolated NDEVs displays even better diagnostic efficiency than each individual biomarker. More importantly, the levels of these AD biomarkers in plasma-isolated NDEVs are strongly correlated to those in the CSF, and the AD biomarkers of the two sources have comparable diagnostic power (plasma-isolated NDEVs, AUC = 0.911; CSF-isolated NDEVs, AUC = 0.901). Cha et al. showed that miR-212 and miR-132 were down-regulated in AD patient plasma-derived NDEVs and could be used as potential AD biomarkers (AUC = 0.84, sensitivity = 92.2%, specificity = 69.0% for miR-212; AUC = 0.77 for miR-132) [180]. Importantly, isolation of NDEVs from plasma significantly increases the sensitivity for diagnosing AD at pre-AD stage, compared with raw plasma-isolated EVs. Fiandaca et al. found that the mean levels of total Tau, p-T181-tau, p-S396-tau, and Aβ1−42 in NDEVs isolated from plasma or serum of AD patients were significantly higher than that of healthy donors even 1 to 10 years before they were diagnosed with AD [181]. Combination of these biomarkers in blood-isolated NDEVs displays promising potential for pre-AD diagnosis (AUC = 0.999, sensitivity = 96%), indicating the ability of NDEVs to predict AD onset and development. In addition, accumulating evidence suggests that mitochondrial dysfunction is associated with the contribution of diabetes to AD progression and may serve as a potential biomarker to diagnose AD among diabetic patients. Scientists have reported that the levels of NADH ubiquinone oxidoreductase core subunit S3 (NDUFS3) and succinate dehydrogenase complex subunit B (SDHB) are significantly lower in L1CAM+ NDEVs isolated from the plasma of type 2 diabetes mellitus (T2DM) patients with AD dementia and progressive mild cognitive impairment (MCI) patients than in cognitively healthy individuals [182]. They also found that the levels of NDUFS3 and SDHB in plasma-isolated NDEV are lower in progressive MCI patients than in stable MCI patients [182]. These results indicate the promise of mitochondrial proteins in plasma-isolated NDEVs as potential diagnostic biomarkers at the earliest symptomatic stage of AD in participants with diabetes, although further studies separating NDEVs from blood samples using more reliable neuronal markers are required to validate these results [182].
Apart from the potential NDEV biomarkers, MDEV may also contain AD biomarkers. Fernandes et al. found that microglia internalize SHSwe cell-released EVs, which are enriched in miR-155, miR-146a, miR-124, miR-21 and miR-125b, and recapitulate the cells of origin [87]. Their data revealed that miR-21 is a consistent biomarker that is found not only in SHSwe cells and SHSwe-released EVs, but also in the recipient microglia and MDEVs. This study highlights miR-21 in EVs as a potential biomarker for AD [87].
EVs as novel biomarkers for the diagnosis of PD
EVs and their contents have also been studied for their potential as biomarkers of PD. The plasma levels of different types of brain-derived EVs are increased in PD compared to control and MSA [135]. AUC values of the ROC curve for plasma-isolated SNAP25+ NDEVs, EAAT1+ ADEVs, and OMG+ ODEVs were 0.82, 0.75, and 0.78, respectively, indicating the capability of the plasma levels of brain-derived EVs as diagnostic biomarkers for PD.
Besides EVs per se, the level of α-syn in EVs remains stably increased with PD progression and is positively correlated with the severity of PD, displaying a moderate diagnostic value (AUC = 0.724, sensitivity = 76.8%, specificity = 53.5%) [183]. Moreover, the level of prion protein (PrP), a protein contributing to cognitive decline in PD patients, in plasma-derived EVs, negatively correlates with the cognitive performance of PD patients, suggesting that PrP in circulating EVs might be a potential biomarker for PD patients at risk of cognitive impairment [184]. In addition to EV proteins, Gui et al. identified down-regulated (e.g., miR-1 and miR-19b-3p) and up-regulated miRNAs (e.g., let-7 g-3p, miR-153, miR-409-3p, and miR-10a-5p) in EVs isolated from CSF of PD patients versus controls [185]. Each of the differentially expressed miRNAs in CSF-derived EVs exhibits excellent to moderate diagnostic power for PD (AUC: 0.780–0.920), and a combination of miR-153 and miR-409-3p achieves an AUC of 0.990 [185].
The differential diagnosis between PD and atypical parkinsonian syndromes is difficult due to the lack of reliable, easily accessible biomarkers. Contents in serum EVs have been shown to be capable of predicting and distinguishing PD from atypical parkinsonian. Jiang et al. showed that α-syn in combination with clusterin in serum-derived NDEVs predictes and differentiates PD from atypical parkinsonism with a promising diagnostic value (AUC = 0.98) [119]. Similarly, Dutta et al. analyzed α-syn levels in serum- or plasma-derived EVs of PD patients, MSA patients, and healthy individuals. They found that α-syn levels are significantly lower in the control group and significantly higher in the MSA group compared with that in the PD group. The ratio of α-syn level in putative ODEVs to that in putative NDEVs is a particularly sensitive biomarker for distinguishing between PD and MSA (AUC = 0.902, sensitivity = 89.8%, specificity = 86.0%). Their data demonstrated that a minimally invasive blood test measuring α-syn level in circulating EVs that can be immunoprecipitated using CNS markers can distinguish between PD patients and MSA patients with high sensitivity and specificity [136].
EVs as novel biomarkers for the diagnosis of ALS
To date, no definite ALS biomarkers are available. To discover efficient and accessible biomarkers for ALS, studies have been carried out to examine differentially expressed proteins in EVs between ALS and control groups utilizing blood samples from ALS patients. Among them, the level of coronin-1a (CORO1A) is 5.3-fold higher in EVs isolated from plasma of ALS patients than that in the controls [186]. CORO1A level increases with disease progression at a certain proportion in plasma of ALS patients and in the spinal cord of ALS mice. As CORO1A significantly affects ALS pathogenesis, it may be a potential biomarker for ALS [186]. Moreover, in a longitudinal study, plasma-derived EV samples collected from 18 ALS patients aged between 20 and 65 years were analyzed at baseline, and at 1, 3, 6 and 12 months of follow-up [187]. The ratio of neurofilament light chain (NFL) and phosphorylated neurofilament heavy chain (pNFH) was measured by ELISA, and that of TDP-43 was determined by flow cytometry. The ratio of TDP-43 in plasma-derived EVs significantly increased at 3-month and 6-month follow-up. When subclassifying patients into rapid- and slow-progression groups, EV NFL but not pNFH was significantly higher in the rapid-progression group at baseline and at 3-month follow-up [187], indicating NFL in plasma-derived EVs as a biomarker for disease progression. However, further studies are needed to demonstrate the diagnostic power of the aforementioned proteins.
ALS-associated miRNA profiles in EVs from CSF or peripheral blood of patients have also been tested. miR-146a-5p, a miRNA involved in the regulation of synaptic plasticity and inflammatory response through inhibition of synaptotagmin1 and neuroligin1 [188], shows decreased expression in EVs from CSF of ALS patients [189]. However, its diagnostic power remains unknown. Saucier et al. sequenced miRNAs in EVs from plasma of ALS patients, and found differential expression of 22 miRNAs between ALS and controls [190]. Among these miRNAs, miR-15a-5p (AUC = 0.976, sensitivity = 92.9%, specificity = 91.7%) and miR-193a-5p (AUC = 0.844, sensitivity = 80.0%, specificity = 88.9%) show promising diagnostic value for ALS [190]. Similarly, miRNA analysis of L1CAM+ NDEVs from ALS patient plasma showed deregulation of 30 miRNAs compared with healthy controls [141]. The deregulated miRNAs are involved in synaptic vesicle-related pathways, four of which are also deregulated in motor cortex tissues of ALS patients [141]. Another study using the same approach identified a potential miRNA fingerprint in L1CAM+ NDEVs from plasma of ALS patients (containing miR-146a-5p, miR-199a-3p, miR-151a-3p, miR-151a-5p, and miR-199a-5p) that showed up-regulation in ALS patients compared with healthy controls, while 3 miRNAs (miR-4454, miR-10b-5p, and miR-29b-3p) were down-regulated in ALS [191]. However, the authors did not further validate L1CAM+ NDEVs or determine the sensitivity and specificity of these miRNAs regarding the diagnosis of HD.
EVs as novel biomarkers for the diagnosis of HD
Misfolded proteins or protein aggregates are pathological hallmarks of HD as well, thus studying misfolded proteins or their regulators might be a crucial part in developing biomarkers for HD [192]. Numerous studies have shown that EVs contain mHTT, its fragments, and many other molecules to reflect disease state, which may be potential biomarkers of HD. However, till date, only few studies have analyzed EVs or their contents in seeking for HD biomarkers.
Ananbeh and colleagues reported elevated total HTT levels in plasma-derived EVs of HD patients compared with control donors, as well as in HD pig models compared with control pigs, representing an important initial step towards characterization of EV contents in seeking for HD biomarkers [156]. Afterwards, EVs derived from platelets, a cell type that contains the highest level of mHTT among blood cells [193], were investigated as probable HD biomarker carriers [194]. However, no differences were found in the number of platelet-released EVs between HD patients and healthy controls, and no correlations were found for the number of platelet-released EVs with the age, CAG repeat number, or disease stage of patients [194]. More importantly, mHTT protein is undetectable in EVs released from platelets [194], indicating that platelet-derived EVs might not be able to serve as HD biomarkers. On the other hand, while EV nonprotein contents, such as miRNAs, have been frequently studied for their potential as biomarkers for AD, PD, and ALS, little is known in HD due to the scarcity of relevant studies [192]. Hence, no significant advance has been made in utilizing EVs as potential ALS biomarkers.
Together, the findings discussed above represent important contributions to the identification of EV biomarker candidates for AD, PD, ALS, and HD. More importantly, although isolation of brain cell-derived EVs can be costly, time-consuming, and labor-intensive, a large number of studies have demonstrated that contents (e.g., miRNAs) of brain cell-derived EVs isolated from blood are much more sensitive and specific, compared with blood molecules [2, 195, 196]. However, there are challenges that restrict the application of EVs and their cargos on the diagnosis of NDs. First, advanced technologies are required to minimize contaminants, especially in the plasma, and to clearly validate the key biological/pathological components in EVs. Second, it remains challenging to isolate circulating EVs derived from the brain and identify specific types of brain cells [85, 86], which can be overcome by discovery of more specific markers and development of more innovative separation methodologies. Third, it is important to distinguish between different subtypes of EVs, since reduction of the heterogeneity of EV samples will greatly strengthen diagnostic interpretations. Fourth, as alterations of contents of circulating EVs reflect systemic host responses, studies in large patient cohorts are necessary to clarify the power, sensitivity, and specificity of certain EV contents in the diagnosis of NDs. Therefore, further studies are needed to overcome current challenges and provide a clearer and more comprehensive picture of the utilization of EVs or their contents as standard, routine diagnostic tools for NDs in the clinic.
EV-based therapeutic strategies in the treatment of NDs
Cells are able to manipulate the molecular composition and function of extracellular matrix via secreting EVs to extracellular matrix [197]. EVs transmit signaling molecules through local or distal pathways [198]. Given that EVs can contain and transport toxic molecules and the relatively long-lasting stability of EV contents, EV-based therapeutic strategies are proposed in NDs treatment. As EV-mediated responses can be either disease-promoting or -restraining depending on its contents and states, EVs have been proposed as potential therapeutic targets or agents for ND treatment. Engineered EVs can deliver diverse therapeutic cargos, including short interfering RNAs, antisense oligonucleotides, chemotherapeutic agents, and immune modulators [199]. Importantly, because EVs are components of the native cellular transport system, they would not induce activation of immunogenic responses as external bioactive medications may probably do. Given these properties, engineered EVs are proposed as a potential drug delivery platform for ND therapeutics. Here we summarize recent studies that demonstrate the usage of EVs as therapeutic targets, agents, or drug delivery platforms for ND treatment in cellular and animal studies.
Pathogenic EVs as targets for the treatment of NDs
Due to the identification of EVs as carriers of pathological molecules during disease progression, pharmacological modification on the release of EVs that contain pathogenic cargos of ND-associated proteins is a common approach for EV-based therapy development. For instance, EVs derived from neurons and activated glial cells were found to carry Aβ, tau, and pathogenically altered miRNAs in AD [10, 83, 84, 87, 111–113]. One study using a transgenic AD mouse model (5×FAD mouse) showed that reducing exosome release by GW4869 decreased total Aβ1−42 and the number of plaques in mouse brains, suggesting that reducing exosome release might have therapeutic benefit for AD treatment [95]. Similar results were obtained in an AD in vitro model that blockage of exosome release via siRNA for sphingomyelin synthase 2 enhanced Aβ uptake by microglia and significantly suppressed Aβ deposition [89]. However, indiscriminately modifying EV release in the brain may exert undesirable side effects, thus fine-tuning on EVs derived from specific cell types or EVs altered in distinct signaling pathways is in urgent need.
EVs have also been found to carry PD pathogenic cargos such as α-syn and altered miRNAs that mediate disease progression [116, 117, 130, 131]. Studies targeting EVs in PD have revealed promising directions. Indirect modulation of EV release through restoration of the autophagy flux by inhibiting Drp1, the key regulator of mitochondria fission and fusion, attenuates α-syn propagation and aggregation [200]. This study demonstrates that limiting EV release by modulating Drp1 has therapeutic potentials to mitigate α-syn transmission and aggregation in PD, with efficacy shown in both NDEVs and MDEVs [201].
Although many studies have shown promising potential of blocking EV release in animal models of NDs, this strategy remains far from clinical practice. Due to the lack of knowledge on EV biogenesis, it is impossible to manipulate EV secretion without interrupting other biological processes in the cells. The generally accepted approach to blocking EV release is to inhibit the activity of nSMase2 by GW4869, PDDC, and other chemicals [202, 203]. In addition to controlling exosome secretion, nSMase2 and its product ceramide are widely associated with other biological processes, including synaptic vesicle recycling [204], cell death regulation [205], and cell metabolic homeostasis maintenance [206]. Hence, inhibition of nSMase2 activity may inevitably cause many adverse effects. Moreover, GW4869 has been found to reduce exosome release while enhancing MV generation [98]. Without fully dissecting the heterogeneity of EVs under pathological conditions, it would be impossible and meaningless to target key subtypes of EVs with pathogenic potential for treatment of NDs.
Stem cell-derived EVs as potential therapeutic agents for the treatment of NDs
Utilizing EVs as potential therapeutic agents for disease treatment is another area of interest in the field. Recent studies have revealed that, after transplantation, stem cells exert their therapeutic effects by secreting EVs and other factors into the microenvironment via a paracrine mechanism. Due to the fact that crossing the BBB is a critical challenge for stem cell therapy, stem cell-derived EV-based therapeutic strategy might be particularly useful for the treatment of NDs (Table 3; Fig. 3).
Table 3.
Summary of stem cell-derived EVs as potential therapeutic agents for NDs
| Cell origin | Disease | Therapeutic cargos | Targets | Administration mode | Models | Outcomes | References |
|---|---|---|---|---|---|---|---|
| MSC | AD | miR-29 | HDAC4 | Weekly intravenous injection for 4 weeks | hAPP-J20 mice | Improve cognitive function, decrease Aβ levels, inhibit astrocyte activation. | [208] |
| MSC | AD | NEP | Aβ | Co-culture | N2a cells | Promote Aβ degradation | [209] |
| MSC | AD | miR-223 | PTEN | Co-culture | Aβ-treated SH-SY5Y cells | Inhibit neuronal cell apoptosis, enhance cell migration | [213] |
| MSC | AD | – | – | Co-culture | TG2576 mouse-derived neurons | Reduces Aβ levels, attenuates apoptosis, increases neurite outgrowth | [214] |
| MSC | AD | – | – | Intracerebroventricle injection once per 2 days for 2 weeks | APP/PS1 mice | Mitigate neuroinflammation and neural impairment | [221] |
| MSC | PD | – | – | SNpc and striatum injection | 6-OHDA-injected rats | Attenuate fine motor deficits, protects against TH damage | [216, 218] |
| MSC | PD | – | – | Diluted in inactivated OP50 | Two C. elegans models | Reduce α-syn levels | [211] |
| MSC | PD | – | – | Intravenous injection every 3 days for 8 weeks | 6-OHDA-injected rats | Improve the behavioral deficits, reduce dopaminergic neuron loss | [215] |
| MSC | PD | – | SMAD3, p38 MAPK | Subcutaneous injection into the right forelimb | MPTP-injected mice | Promote angiogenesis | [217] |
| MSC | PD | – | – | Co-culture | 6-OHDA-treated SH-SY5Y cells | Protect neuronal cells from oxidative damage | [223] |
| MSC | ALS | – | – | Co-culture | Mutant SOD1-NSC-34 cells | Promote cell survival, inhibit apoptotic genes | [219] |
| MSC | ALS | – | – | Intravenous and intranasal injection | SOD1(G93A) mice | Improve motor performance, inhibit neurodegeneration | [220] |
| MSC | ALS | – | – | Co-culture | Mutant SOD1-overexpressing NSC-34 cells | Protect NSC-34 cells from oxidative damage and apoptosis | [224] |
| NSC | AD | – | – | Single retro-orbital vein injection | 5×FAD mice | Reduce Aβ deposition, rescue the cognitive defects | [228] |
| NSC | AD | – | – | Bilateral injection into the lateral ventricles | APP/PS1 mice | Rescue the cognitive defects | [229] |
| NSC | PD | – | – | Injection into the SN region | 6-OHDA-induced mice | Reduce ROS levels and 6-OHDA-induced dopaminergic neuronal loss | [230] |
| NBC | AD | GSLs | Aβ | Brain infusion for 2 weeks | APPSweInd mice | Decrease Aβ pathologies | [239] |
| SHED | PD | – | – | Co-culture | 6-OHDA-treated neuron | Suppress 6-OHDA-induced apoptosis | [238] |
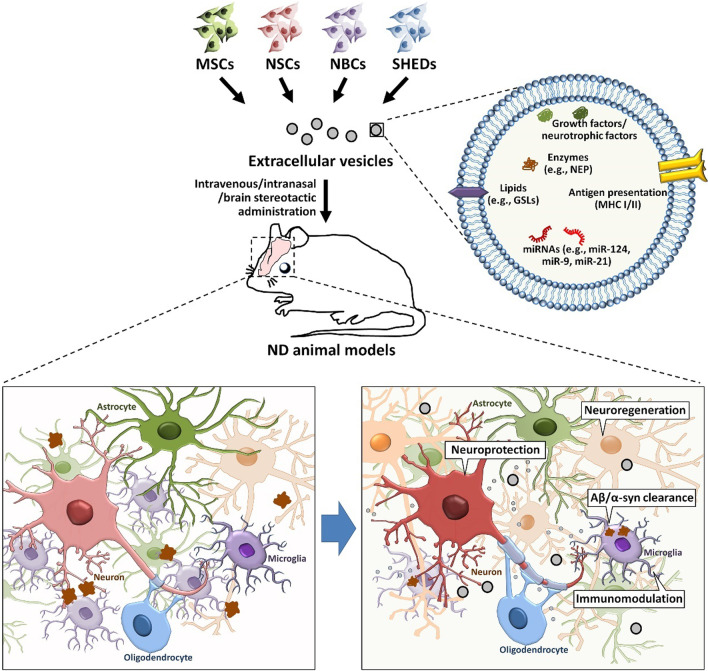
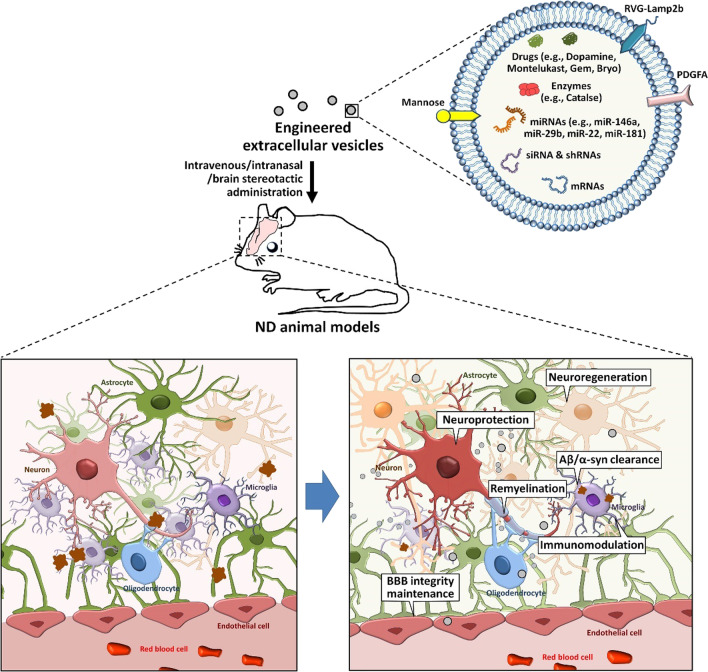
Fig. 3.
The therapeutic effects of stem cell-derived EVs on NDs.
To date, the therapeutic effects of EVs derived from MSCs, NSCs, NBCs, and SHEDs have been reported in various animal models of NDs. These stem cell-derived EVs carry Aβ degradation-related enzyme (e.g., NEP) and lipids (e.g., GSLs), growth factors, neurotrophic factors, therapeutic miRNAs. The administration of stem cell-derived EVs therefore improves cognitive/motor function, facilitates Aβ/α-syn clearance, enhances neuroprotection, suppresses neuroinflammation, promotes neuroregeneration of ND animal models
Mesenchymal stem cell-derived EVs as potential therapeutic agents for the treatment of NDs
MSCs are the most commonly investigated stem cells for therapies due to their ability of damage repair and inflammation modulation. Mounting in vitro and in vivo studies have demonstrated promising effects of MSCs on neurological recovery, immunomodulation, and neo-angiogenesis in various NDs [207]. In recent years, MSC-derived EVs have attracted much attention since they exhibit similar therapeutic effects as their parental cells in treating NDs and have multiple advantages including negligible immunogenicity, more flexible administration strategies, and convenient content and surface modifications [166]. Emerging evidence has suggested that the MSC-derived EVs achieve their therapeutic effects via multiple mechanisms.
MSC-derived EVs facilitate the degradation of pathogenic proteins, and have been shown to attenuate Aβ expression while increasing expression of genes related with memory and neural synaptic function in both cell and animal models of AD [208]. These alterations, in turn, elevate brain glucose metabolism and reverse cognitive dysfunctions in AD transgenic mice [208]. Katsuda and colleagues reported the existence of neprilysin (NEP), one of the most pivotal Aβ-degrading enzymes, in adipose MSC-derived EVs [209]. In cultured cells, NEP-loaded EVs reduce levels of both released and intracellular Aβ in neuroblastoma cells (NBCs), demonstrating the beneficial significance of adipose MSC-derived EVs for AD [210]. Likewise, bone marrow MSC-derived EVs largely reverse dopaminergic neurodegeneration in a C. elegans model of PD through decreasing α-syn aggregates, suggesting that the MSC-derived EVs facilitate degradation of pathogenic proteins in PD [211].
MSC-derived EVs also exert anti-apoptosis and pro-survival effects [212–216]. Wei et al. demonstrated that miR-223-enriched MSC-derived EVs inhibit neuronal cell apoptosis and enhance cell migration in an AD cell model via PTEN and PI3K-Akt pathways [213]. Lee et al. also demonstrated that EVs secreted by adipose MSCs reduce β-amyloidosis and neuronal apoptosis in AD transgenic mice and enhance axonal growth in the brains of AD patients [214]. Decreased expression of p53, Bax, pro-caspase-3 and cleaved-caspase-3, and increased expression of Bcl-2 have been found following treatment with adipose MSC-derived EVs in AD transgenic mice [214]. This study reflects the pro-survival effects of MSC-derived EVs against Aβ-triggered neuronal dysfunction and neural loss [214]. In addition, recent studies have shown that pretreatment with MSC-derived EVs dampened 6-OHDA-stimulated SH-SY5Y cell apoptosis through boosting autophagy for neural protection [215, 216]. In 6-OHDA-injected rats, transplanted EVs cross the BBB, diminish apoptosis of dopaminergic neurons, and meanwhile enhance dopamine levels in the striatum [215]. In MPTP-treated mice, Xue et al. found that MSC-derived EVs stimulate angiogenesis of human brain microvascular endothelial cells (HBMECs) following enhancing the expression of intercellular adhesion molecule-1 (ICAM-1) and restoring the 1-methyl-4-phenylpyridinium (MPP+)-induced damage to endothelial cells [217]. Indeed, MSC-derived EVs trigger HBMEC angiogenesis through up-regulation of ICAM1 by provoking the SMAD3 and P38MAPK signaling pathways [217]. Moreover, intraperitoneal injection of EVs notably increases TH+ dopaminergic neurons in substantia nigra (SN) and up-regulates CD31 expression in the corpus striatum of treated mice, leading to recovery of these animals [217]. Reports also showed that the desired pro-survival effects of MSC-derived EVs are, to a large extent, mediated by various biologic molecules in MSC-derived secretomes, including SDF-1, growth factors (BDNF, VEGF and GDNF), MMP2, heat shock protein 27, and semaphorin 7a in 6-OHDA-injected rats [218]. Moreover, scientists demonstrated that adipose MSC-derived EVs play a neuroprotective role in ALS models in vitro [219]. They discovered 189 proteins in adipose MSC-derived EVs that contribute to cell adhesion and negative modification of the apoptotic pathways. Further analysis revealed that the EV therapy suppresses the expression of pro-apoptotic proteins Bax and cleaved caspase-3 and conversely increases the expression of anti-apoptotic protein Bcl-2 in ALS in vitro models [219]. Intravenous and intranasal administration of adipose MSC-derived EVs in the SOD1G93A mouse model of ALS protects lumbar spinal cord motor neurons from neurodegeneration presumably through suppressing glial cell functions up to 17 weeks post-transplantation [220].
MSC-derived EVs exert neuroprotective effects through reversing brain inflammation. Wang et al. found improved cognitive behaviors / synaptic transmission and suppression of expression of pro-inflammatory iNOS after MSC-derived EV administration in AD mice, and that down-regulation of iNOS expression indeed rescues neural function impairment in vivo [221]. In addition, MSC-derived EVs up-regulate the expression of anti-inflammatory factors such as IL-10 and tissue inhibitor matrix metalloproteinase 1 in activated microglia, implying an important role of MSC-derived EVs in initiating anti-inflammatory responses in AD mice [222].
Moreover, MSC-derived EVs show promising antioxidant effects in various ND models. For example, Chierchia et al. found that MSC-derived EVs elicit antioxidant effects by elevating Sirt3 expression in 6-OHDA-treated SH-SY5Y cells, which led to further neuroprotective effects in vivo [223]. Furthermore, a recent in vitro study revealed that adipose MSC-derived EVs protect NSC-34 cells that overexpress human SOD1(G93A) from oxidative stress and rescue NSC-34 cells from apoptosis, suggesting that MSC-derived EVs function as potential antioxidants in treating ALS [224].
Taken together, MSC-derived EVs have been shown to alleviate disease phenotypes in various cell and animal models through various mechanisms. However, the therapeutic effects of MSC-derived EVs have to be confirmed in clinical studies, which is currently under investigation in China and many other countries (ClinicalTrials.gov Identifier: NCT04388982).
Neural stem cell (NSC)-derived EVs as potential therapeutic agents for the treatment of NDs
Unlike MSCs, NSCs are a population of endogenous stem cells in the CNS that play a crucial role in the neural development and repair as they differentiate into both neurons and neurogliocytes [225]. To date, the therapeutic roles of NSC-derived EVs have been studied in various models of NDs and acute neural injury, and encouraging results have been obtained [17, 226]. Importantly, studies have demonstrated that NSC-derived EVs have better effects in improving neural function recovery than MSC-derived EVs [227]. These findings suggest that the NSC-derived EVs inherit the great neurogenic/neuroregenerative potential from their parent cells, making them potential therapeutics for NDs.
Till now, investigations on the therapeutic effects of NSC-derived EVs on NDs mainly focus on AD. Multiple independent groups have reported that NSC-derived EVs rescue cognitive defects in different AD animal models including 5×FAD and APP/PS1 transgenic mice [228, 229]. Different pathological and molecular mechanisms of neurofunction restoration by NSC-derived EVs in NDs have been unveiled. Similar to MSC-derived EVs, NSC-derived EVs may also reduce the burdens of key pathological molecules in NDs. A single injection of human NSC-derived EVs in the retro-orbital vein significantly reduces Aβ deposition in the brains of 5×FAD transgenic mice [228]. However, conflict results have been reported that the lateral ventricle injection of NSC-derived EVs does not alter Aβ burden in APP/PS1 transgenic mice [229]. Thus, the effects of therapies based on NSC-derived EVs on Aβ deposition remain an open question. NSC-derived EVs also achieve their therapeutic effects through immunomodulation and neuroprotection. After intravenous injection, NSC-derived EVs inhibit activation of microglia and excessive expression of pro-inflammatory cytokines in AD mouse brains highly likely through the delivery of miR-124 and other inflammation-regulatory miRNAs [228]. Meanwhile, NSC-derived EVs also restore the levels of memory-related synaptic proteins and improve synaptic morphology in the cortex of AD mice by promoting mitochondrial function and decreasing oxidative damage, suggesting promising neuroprotective effects of NSC-derived EVs [229]. Similar results have been obtained in 6-OHDA-induced PD model that administration of NSC-derived EVs down-regulates pro-inflammatory signals and decreases the 6-OHDA-induced dopaminergic neuronal loss in vivo [230]. NSC-derived EVs also enhance neuroregeneration in 5×FAD mouse brains including increasing the NSC pool and facilitating NSC differentiation into neuronal lineage, presumably through transferring miRNAs (e.g., miR-9, and miR-21) and proteins (e.g., growth factors) to endogenous NSCs [17]. Moreover, NSC-derived EVs reverse AD-caused BBB disruption in vitro and in vivo [231]. Together with the finding that NSC-derived EVs promote angiogenesis in CNS injury [232], cerebrovascular regulation could be an important therapeutic effect of NSC-derived EVs.
Notably, although NSC-derived EVs exhibit outstanding therapeutic effects, NSCs also have disadvantages including ethical/religious concerns and problematic logistics of acquiring fetal tissues, restricting mass production of EVs [233]. Our recent studies have generated NSC-like cells using cell reprogramming approach [234]. In this approach, somatic cells like fibroblasts and astrocytes are directly reprogrammed into induced NSCs (iNSCs) that exhibit comparable proliferation/renewal and multipotent differentiation capacities [235]. The iNSC-derived EVs exhibit comparable or even better performance in enhancing the proliferation, migration, and differentiation of NSCs in vitro via transferring growth factors including EGF, FGF2, and IGF [236]. The iNSC-derived EVs also significantly inhibit apoptosis of NSCs induced by oxidative stress or starvation [237]. More importantly, intravenous administration of iNSC-derived EVs promotes recovery of neurofunction and neural tissue regeneration, and suppresses neuroinflammation and neuronal injury in a stroke model [17] and an AD mouse model (unpublished data), presumably through activation of the MEK/ERK signaling pathway. Therefore, both NSC- and iNSC-derived EVs display great therapeutic effects in cell and animal models of NDs, implicating the equal necessity to evaluate the potential of NSC- and iNSC-derived EVs for clinical application, compared to MSC-derived EVs.
Potential therapeutic effects of EVs derived from other stem cell types on NDs
Besides the aforementioned two types of stem cells, there are other types of stem cells that have been utilized as EV producer for ND treatment [238]. For instance, NBC-derived EVs have been reported to trap Aβ and facilitate Aβ internalization into brain-resident phagocyte microglia [239]. This finding demonstrates that intracerebrally administered EVs utilize membrane glycosphingolipids (GSLs) to act as Aβ scavengers and suggests a role for NBC-derived EVs in Aβ clearance in the brain [239]. Furthermore, scientists have found that EVs derived from the microcarrier-cultured stem cells from the dental pulp of human exfoliated deciduous teeth (SHEDs) suppress the 6-OHDA-induced apoptosis of dopaminergic neurons [238], probably through reducing the sensitivity of dopaminergic neurons to the 6-OHDA-induced oxidative stress [240]. Notably, EVs derived from SHEDs under standard culture conditions do not exert similar anti-apoptotic effect, indicating that culture conditions have a crucial influence on EV function.
Hence, although multiple types of stem cells have been utilized to generate EVs as potential therapeutics of NDs, much more investigations are urgently required to investigate the therapeutic effects of EVs derived from more types of stem cells, to fully unravel the underlying mechanisms of alleviation of ND phenotypes by stem cell-derived EVs, and to develop a standard for preparing pharmaceutical-grade EVs in order to accelerate clinical applications of these EVs in ND treatment.
Engineered EVs as a potential drug delivery platform for treatment of NDs
Mounting studies have demonstrated that engineered EVs can be an effective platform for delivery of drugs [241, 242]. As described previously in this review, EVs can permeate membranes including the BBB, indicating them as an effective platform for the delivery of drugs to the CNS [243, 244]. Moreover, engineered EVs may also be able to target specific recipient cells for site-specific delivery [201, 245], suggesting feasibility of intravenous or intranasal delivery approaches that avoid neurosurgery (Table 4; Fig. 4).
Table 4.
Summary of EVs with drug delivery capacity for the treatment of NDs
| Cell/tissue origin | Disease | Surface modification | Loaded cargos | Therapeutic Targets | Administration mode | Models | Outcomes | References |
|---|---|---|---|---|---|---|---|---|
| Dendritic cell | PD | RVG | α-syn-siRNA | α-syn | Intravenous injection | α-Syn Tg mice | Reduce intraneuronal α-syn aggregates | [247] |
| Dendritic cell | PD | RVG | α-syn-shRNA | α-syn | Intravenous injection | Syn PFFs-injected mice | Reduce α-syn aggregation, decrease neuronal death, alleviate PD symptoms | [249] |
| U87 cell | HD | – | Htt siRNA | Htt | Infusion into the striatum for 7 days | Wild type mice | Reduce Htt expression | [248] |
| MSC | AD | RVG | miR-146a | NF-κB pathways | Intracerebroventricular injection for 2 times | APP/PS1 mice | Inhibit pro-inflammatory responses of astrocytes and microglia | [167] |
| MSC & 293T cell | AD | – | miR-29b | BACE1, BIM | Bilateral injection into hippocampal CA1 region | Aβ-treated model rats | Enhance spatial learning and memory | [251] |
| MSC | AD | – | miR-22 | GSDMD | Intravenous injection every 7 days | APP/PS1 mice | Enhance behavioral performance, repress neuroinflammation | [252] |
| MSC | PD | – | miR-188-3p | CDK5, NLRP3 | Intravenous injection for 5 days | MPTP-induced PD mice | Suppress autophagy and pyroptosis | [253] |
| 293T cell | PD | – | Catalase mRNA | ROS | Implantation of EV producers into the brains | 6-OHDA-injected mice | Protect neurons against neurotoxicity, inhibit neuroinflammation | [246] |
| Macrophage | PD | – | Redox catalase | ROS | Intranasal injection for 10 times every other day | 6-OHDA-injected mice | Eliminate ROS and display neuroprotective effects | [254] |
| Macrophage | AD | Mannose | Gemfibrozil | Aβ | Intraperitoneal injection for 7 consecutive days | Aβ-injected mice | Promote Aβ clearance by microglia, improve learning and memory ability | [267] |
| Blood | PD | – | Dopamine | Dopamine receptors | Intravenous injection | 6-OHDA-injected mice | Improve dopaminergic neurons, ameliorate PD phenotype | [255] |
| NSC | MS | PDGFA | Montelukast | GPR17 | Intranasal injection every day for 2 weeks | Cuprizone-treated mice | Promote myelin regeneration | [257] |
| NSC | MS | – | Bryostatin-1 | GPR17 | Intravenous injection | Cuprizone-treated mice | Promote myelin regeneration | [256] |
Fig. 4.
The therapeutic effects of engineered EVs on NDs.
EVs have been utilized as a drug delivery platform for the treatment of NDs. Therapeutic cargos including shRNA/siRNA/miRNAs that target ND-related genes, mRNAs that express Aβ degradation enzymes, and therapeutic drugs can be specifically loaded into EVs via transfection or physical strategies. Moreover, through being decorated with RVG, mannose, or PDGFA on the surface, EVs are further conferred targeting capacity to the CNS, microglia, and OPCs, respectively. These engineered EVs reach their target cells to facilitate Aβ clearance, mitigate oxidative stress, protect neuronal cells, inhibit neuroglial activation, promote remyelination, and restore BBB integrity, thus alleviating behavioral phenotypes of ND animal models
Engineered EVs with modified cargos for the treatment of NDs
To date, EVs have been successfully used for the delivery of therapeutically active molecules, including RNAs, proteins, and pharmaceutical compounds to the brain [241, 242]. For instance, therapeutic genetic materials that could regulate gene expression have been transported to the brain by EVs to alter ND progression. Scientists have reported that therapeutic catalase mRNAs delivered by engineered EVs alleviate neurotoxicity and neuroinflammation in both cell and animal models of PD, indicating the potential value of EVs for delivery of genetic materials in therapeutic applications [246]. The therapeutic potential of EV-based siRNA delivery for NDs has also been reported. One research group systemically injected modified EVs containing α-syn siRNA into the S129D α-syn transgenic mice and found reduced mRNA and protein levels of α-syn in mouse brain [247]. Another group reported that EVs carrying hydrophobically modified siRNA to the CNS efficiently targeted mHtt mRNA in a HD mouse model [248]. Though therapeutic siRNAs can be efficiently transported by EVs to the CNS [245], their effectiveness is limited in ND treatment due to short time of efficacy and poor bioavailability in systemic circulation. Therefore, scientists investigated the efficacy of EV-delivered shRNAs. They found that α-syn shRNAs delivered by EVs reduce α-syn aggregation, decrease dopaminergic neuronal death, and alleviate PD symptoms in mice [249]. These studies again support the potential of EVs as a drug delivery platform for genetic modulators, such as siRNAs and shRNAs, into the CNS for therapeutic benefits. On the other hand, EV delivery has been demonstrated to increase the stability of various RNA-based therapies for NDs, as they protect RNAs from degradation [250]. Besides siRNAs and shRNAs, miRNAs with therapeutic effects have also been loaded into EVs to treat NDs. In a rat model of AD, bilateral hippocampal injection of miR-29-enriched MSC-derived EVs alleviates the pathological impacts of Aβ peptide and improves spatial learning and memory by suppressing the expression of BACE1, suggesting an inhibitory effect of MSC-derived EVs on Aβ formation [251]. Similarly, miR-146a has been packaged into bone marrow MSC-derived EVs, which down-regulates NF-κB pathways in astrocytes and restores astrocytic activation, ultimately leading to improved synaptogenesis and amelioration of cognitive deficits in AD mice [167]. Adipose MSC-derived EVs specifically loaded with miR-22 enhance the motor and memory capability of AD mice by inhibiting inflammatory factors, down-regulating pyroptosis, and improving neural survival [252]. Further studies demonstrated that MSC-derived EVs loaded with miR-188-3p exhibit anti-inflammatory and anti-apoptotic effects in PD animal models through inhibiting NLRP3-induced inflammation and cyclin-dependent kinase 5-induced autophagy [253].
Besides, EVs have been modified to package natural enzymes for the clearance of pathogenic molecules in NDs. After being transfected with catalase-encoded plasmid DNA, mouse macrophages release EVs preloaded with redox catalase [254]. These EVs significantly increase the viability of 6-OHDA-pretreated PC12 cells as they decrease ROS levels in activated macrophages, suggesting that they reduce neuroinflammation by decreasing ROS in activated microglia [254]. Indeed, in vivo experiments confirmed that catalase-preloaded EVs reduce microglial activation and increase survival of dopaminergic neurons in 6-OHDA-intoxicated mice [254].
Apart from transporting genetic materials or modulators, various in vitro and in vivo studies have suggested EVs as promising vehicles for direct delivery of therapeutic agents for ND treatment. One study reported that EVs isolated from human blood and preloaded with saturated dopamine solution are able to cross the BBB for dopamine delivery into the CNS via interactions with transferrin and the transferrin receptor [255]. Another in vivo study showed that dopamine-preloaded EVs display greater therapeutic efficacy and lower toxicity than intravenously delivered free dopamine [201]. Furthermore, NSC-derived EVs have been utilized to package montelukast and bryostatin-1, two drugs for MS [256, 257]. Results showed that the EV-based delivery of drugs to lesion areas in cuprizone-treated mice, an animal model of MS, protects the myelin sheath and promotes remyelination, suggesting EVs as a novel drug delivery platform with great potential for treatment of NDs [256, 257].
Engineered EVs with modified surface for targeted therapy of NDs
Although stem cell-derived EVs are proposed as potential treatment tools that have demonstrated beneficial efficacy in a number of NDs [258, 259], further investigations and clinical trials are required to confirm the benefits of therapeutic application of EVs in NDs. Until now, mounting evidence supports that modification of EVs in order for specific targeting may hold substantial therapeutic benefits for NDs [245, 260–264].
Currently, the most commonly used strategy to confer brain-targeting capacity to exosomes is to conjugate the CNS-specific rabies viral glycoprotein (RVG) peptide (YTIWMPENPRPGTPCDIFTNSRGKRASNG) with an exosomal membrane protein Lamp2b [245]. Through transfection of plasmids encoding the RVG-Lamp2b constructs, cells release RVG-expressing exosomes that could be used to deliver desired molecules into the CNS. Multiple studies have utilized this approach to deliver siRNAs, shRNAs, and miRNAs into the brain through dendritic cell- and MSC-derived exosomes, and obtained outstanding outcomes in alleviating AD and PD phenotypes in vivo [167, 247, 249]. It is noteworthy that RVG may not help exosomes to cross the BBB directly and target the CNS through retrograde transport from peripheral nerves [261, 265]. Instead, RVG may confer the BBB penetration capacity to exosomes through direct interaction with nicotinic acetylcholine receptors expressed on endothelial cells [261, 266]. A similar strategy that expresses the cyclo(Arg-Gly-Asp-D-Tyr-Lys) peptide [c(RGDyK)] on exosomal surface, which has high affinity to the integrin αvβ3 in reactive cerebral vascular endothelial cells, successfully facilitates accumulation of modified exosomes in brain lesions compared to the undamaged tissue on the contralateral side of the brain in an in vivo ischemic model [262].
Moreover, scientists have bioengineered EVs to target specific types of cells in the CNS. For instance, to address the inefficient clearance of Aβ caused by abnormal lysosomal function in microglia in AD, EVs are bioengineered to target microglia by adding mannose on EV surface [267]. Mannose-expressing EVs specifically bind to mannose receptor (CD206), a microglial enriched protein, therefore enhancing the uptake of EVs by microglia. Through this approach, EVs deliver gemfibrozil to restore the lysosomal activity of microglia, accelerate lysosome-mediated clearance of Aβ in microglia, and successfully improve the learning and memory ability of AD mice [267]. Similarly, PDGFA can be expressed on engineered EVs that exhibit excellent affinity to oligodendrocyte progenitor cell (OPC) surface receptor PDGFRα [257]. PDGFA-expressing EVs therefore transfer montelukast to OPCs to promote oligodendrocyte generation and myelin regeneration, resulting in mitigation of MS-like phenotypes in a cuprizone-induced demyelination animal model [257].
To summarize, EVs orchestrate various events that facilitate recovery and regeneration in neurodegenerative conditions. Many efforts have been made to improve the homing property of EVs to convey therapeutic agents to brain sites and potentiate recovery. Merging the intrinsic attributes of EVs with a targeted medicine is proposed as a novel therapeutic strategy that may exert a profound influence on the future of ND treatment. However, in view of translation into clinic, some technical challenges still need to be solved. One important challenge is how to enhance BBB penetration and targeting potential of EVs. To date, the mechanisms underlying EV crossing the BBB remain controversy and multiple theoretical routes have been proposed [268]. Based on these theories, EVs can be macropinocytosed or transcytosed into the MVBs of endothelial cells through the endocytic pathway, and then traffick from the MVB to the plasma membrane as neoformed exosomes [268, 269]. EVs may also cross the BBB through the paracellular pathway when BBB integrity is disturbed under pathological conditions [269]. Thus, more studies that sort out the BBB penetration mechanisms will dramatically increase the number of EVs that reach the CNS after intravenous or even oral administration. Moreover, the cargo loading efficiency of EVs remains limited. Intrinsically packed natural molecules (e.g., proteins and nucleic acids) significantly increase the difficulty of desired cargo loading, resulting in a much lower cargo loading efficiency for these EVs than unpacked synthetic liposomes [270, 271]. Besides, other technical issues like quality control due to the high heterogeneity of EVs, hard expedition towards industrial manufacturing, high cost of production and storage also impede the application of EVs for drug delivery [270].
Conclusions and future perspectives
In summary, numerous studies have demonstrated a tight association of EVs with NDs including but not limited to the direct delivery of pathogenic molecules, the modulation of inflammatory responses of immune cells, the regulation of neuronal cell function and viability, and manipulation of BBB integrity. Inspiringly, the aforementioned findings have suggested great values in translational medicine. With the help of newly developed immunoprecipitation approaches, EVs derived from specific types of brain cells could be purified and certain cargos within these EVs have been reported to be outstanding biomarkers for the diagnosis and prognosis of NDs, providing novel perspectives to realize early diagnosis, a key step for effective prevention of irreversible neurodegeneration. Moreover, drugs targeting pathogenic EVs as well as EVs with therapeutic effects or drug delivery capacity have demonstrated promising therapeutic potential in cellular and animal models of NDs, including mitigating neurofunction impairment, alleviating neuroinflammation and neurotoxicity, and mitigating neurodegeneration and neuronal loss. With extensive investigations, more pathological/beneficial roles of EVs in ND pathogenesis and the underlying mechanisms could be unveiled, dramatically expanding our understanding of EVs within the CNS and shedding light on the development of EV-based therapeutic strategies for more precise diagnosis and more effective treatment of NDs.
Acknowledgements
We thank Dr. Xinrui Qi, Jie Zhu, Yanyan Zhang for proofreading the manuscript.
Abbreviations
- α-syn
α-synuclein
- Aβ
Amyloid-beta
- AD
Alzheimer’s disease
- ADEV
Astrocyte-derived extracellular vesicle
- ALS
Amyotrophic Lateral Sclerosis
- AUC
Area under the curve
- BBB
Blood-brain barrier
- CNS
Central nervous system
- CORO1A
Coronin-1a
- CSF
Cerebral spinal fluid
- DPRs
Dipeptide repeat proteins
- EBV
Epstein Barr virus
- ELISA
Enzyme-linked immunosorbent assay
- EV
Extracellular vesicle
- GSLs
Glycosphingolipids
- GST
Glutathione S-transferase
- GWAS
Genome-wide association studies
- HBMEC
Human brain microvascular endothelial cell
- HD
Huntington’s Disease
- HIV
Human immunodeficiency virus
- HPV
Human papilloma virus
- ICAM-1
Intercellular adhesion molecule-1
- IL
Interleukin
- ILV
Intraluminal vesicle
- iNSC
Induced neural stem cell
- LMP1
Latent membrane protein 1
- MAC
Membrane attack complex
- MCI
Mild cognitive impairment
- MDEV
Microglia-derived extracellular vesicle
- MPP
1-methyl-4-phenylpyridinium
- MSA
Multiple system atrophy
- MSC
Mesenchymal stem cells
- MS
Multiple sclerosis
- MV
Microvesicle
- MVBs
Multivesicular bodies
- NBC
Neuroblastoma cell
- NCAM
Neural cell adhesion molecule
- ND
Neurodegenerative disease
- NDEV
Neuron-derived extracellular vesicle
- NDUFS3
NADH ubiquinone oxidoreductase core subunit S3
- NEP
Neprilysin
- NFL
Neurofilament light chain
- NSC
Neural stem cell
- nSMase2
Neutral sphingomyelinase2
- ODE
Oligodendrocyte-derived extracellular vesicle
- OPC
Oligodendrocyte progenitor cells
- p-Tau
Phosphorylated Tau protein
- PD
Parkinson’s disease
- PMEL
Premelanosome protein
- pNFH
phosphorylated neurofilament heavy chain
- PrP
Prion protein
- RISC
RNA-induced silencing complex
- ROC
Receiver operating characteristic
- ROS
Reactive oxygen species
- RVG
Rabies viral glycoprotein
- scFvs
Single-chain fragment variable antibodies
- SDF-1
Stromal cell-derived factor-1
- SDHB
Succinate dehydrogenase complex subunit B
- SEMA3A
Semaphorin 3 A
- SN
Substantia nigra
- SOD
Superoxide dismutase
- T2DM
Type 2 diabetes mellitus
- TDP-43
TAR DNA-binding protein-43
- TNF-α
Tumor necrosis factor-alpha
- UTR
Untranslated region
Author contributions
XX, JCZ conceived the manuscript. XX, YW collected references. XX, YW wrote the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported in part by research grants from the National Natural Science Foundation of China (No. 81971145 and No. 82271477 to X.X., No. 91949204 and 81830037 to J.C.Z.).
Availability of aata and materials
Not applicable.
Declarations
Ethical approval and Consent to participate
The authors approved the final manuscript.
Consent for publication
The authors approved the final manuscript.
Competing interests
The authors declare no competing interests regarding the publication of this paper.
Footnotes
Xiaohuan Xia and Jialin C. Zheng this two author only shared the equal contributions
Contributor Information
Xiaohuan Xia, Email: xiaohuan_xia1@163.com.
Jialin C. Zheng, Email: jialinzheng@tongji.edu.cn
References
- 1.Dugger BN, Dickson DW. Pathology of neurodegenerative diseases. Cold Spring Harb Perspect Biol. 2017;9(7). [DOI] [PMC free article] [PubMed]
- 2.Xia X, Wang Y, Huang Y, Zhang H, Lu H, Zheng JC. Exosomal miRNAs in central nervous system diseases: biomarkers, pathological mediators, protective factors and therapeutic agents. Prog Neurobiol. 2019;183:101694. doi: 10.1016/j.pneurobio.2019.101694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hill AF. Extracellular vesicles and neurodegenerative diseases. J Neurosci. 2019;39(47):9269–73. doi: 10.1523/JNEUROSCI.0147-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xia X, Wang Y, Qin Y, Zhao S, Zheng JC. Exosome: a novel neurotransmission modulator or non-canonical neurotransmitter? Ageing Res Rev. 2022;74:101558. doi: 10.1016/j.arr.2021.101558. [DOI] [PubMed] [Google Scholar]
- 5.Mathieu M, Martin-Jaular L, Lavieu G, Thery C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell-to-cell communication. Nat Cell Biol. 2019;21(1):9–17. doi: 10.1038/s41556-018-0250-9. [DOI] [PubMed] [Google Scholar]
- 6.Harding C, Stahl P. Transferrin recycling in reticulocytes: pH and iron are important determinants of ligand binding and processing. Biochem Biophys Res Commun. 1983;113(2):650–8. doi: 10.1016/0006-291X(83)91776-X. [DOI] [PubMed] [Google Scholar]
- 7.Pan BT, Johnstone RM. Fate of the transferrin receptor during maturation of sheep reticulocytes in vitro: selective externalization of the receptor. Cell. 1983;33(3):967–78. doi: 10.1016/0092-8674(83)90040-5. [DOI] [PubMed] [Google Scholar]
- 8.Xia X, Yuan P, Liu Y, Wang Y, Cao W, Zheng JC. Emerging roles of extracellular vesicles in COVID-19, a double-edged sword? Immunology. 2021;163(4):416–30. doi: 10.1111/imm.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao S, Sheng S, Wang Y, Ding L, Xu X, Xia X, et al. Astrocyte-derived extracellular vesicles: a double-edged sword in central nervous system disorders. Neurosci Biobehav Rev. 2021;125:148–59. doi: 10.1016/j.neubiorev.2021.02.027. [DOI] [PubMed] [Google Scholar]
- 10.Ding L, Yang X, Xia X, Li Y, Wang Y, Li C, et al. Exosomes mediate APP dysregulation via APP-miR-185-5p axis. Front Cell Dev Biol. 2022;10:793388. doi: 10.3389/fcell.2022.793388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xia X, Wang Y, Zheng JC. Emerging roles of extracellular vesicles in mediating RNA virus infection. Fundamental Res. 2021;1(2):7. doi: 10.1016/j.fmre.2021.02.005. [DOI] [Google Scholar]
- 12.D’Acunzo P, Perez-Gonzalez R, Kim Y, Hargash T, Miller C, Alldred MJ, et al Mitovesicles are a novel population of extracellular vesicles of mitochondrial origin altered in Down syndrome. Sci Adv. 2021;7(7). [DOI] [PMC free article] [PubMed]
- 13.Akers JC, Gonda D, Kim R, Carter BS, Chen CC. Biogenesis of extracellular vesicles (EV): exosomes, microvesicles, retrovirus-like vesicles, and apoptotic bodies. J Neurooncol. 2013;113(1):1–11. doi: 10.1007/s11060-013-1084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morton MC, Neckles VN, Seluzicki CM, Holmberg JC, Feliciano DM. Neonatal subventricular zone neural stem cells release extracellular vesicles that act as a microglial morphogen. Cell Rep. 2018;23(1):78–89. doi: 10.1016/j.celrep.2018.03.037. [DOI] [PubMed] [Google Scholar]
- 15.Sharma P, Mesci P, Carromeu C, McClatchy DR, Schiapparelli L, Yates JR 3. Exosomes regulate neurogenesis and circuit assembly. Proc Natl Acad Sci U S A. 2019;116(32):16086–94. rd, et al. [DOI] [PMC free article] [PubMed]
- 16.Selmaj I, Mycko MP, Raine CS, Selmaj KW. The role of exosomes in CNS inflammation and their involvement in multiple sclerosis. J Neuroimmunol. 2017;306:1–10. doi: 10.1016/j.jneuroim.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Gao G, Li C, Zhu J, Sheng S, Liang Z, Fu S, et al. Induced neural stem/progenitor cell-derived extracellular vesicles promote recovery post-stroke. Clin Transl Med. 2022;12(6):e936. doi: 10.1002/ctm2.936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mayor S, Pagano RE. Pathways of clathrin-independent endocytosis. Nat Rev Mol Cell Biol. 2007;8(8):603–12. doi: 10.1038/nrm2216. [DOI] [PubMed] [Google Scholar]
- 19.Huotari J, Helenius A. Endosome maturation. EMBO J. 2011;30(17):3481–500. doi: 10.1038/emboj.2011.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhu H, Guariglia S, Yu RY, Li W, Brancho D, Peinado H, et al. Mutation of SIMPLE in Charcot-Marie-Tooth 1 C alters production of exosomes. Mol Biol Cell. 2013;24(11):1619–37. doi: 10.1091/mbc.e12-07-0544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cabrera M, Ungermann C. Guiding endosomal maturation. Cell. 2010;141(3):404–6. doi: 10.1016/j.cell.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 22.Colombo M, Moita C, van Niel G, Kowal J, Vigneron J, Benaroch P, et al. Analysis of ESCRT functions in exosome biogenesis, composition and secretion highlights the heterogeneity of extracellular vesicles. J Cell Sci. 2013;126(Pt 24):5553–65. doi: 10.1242/jcs.128868. [DOI] [PubMed] [Google Scholar]
- 23.McGough IJ, Vincent JP. Exosomes in developmental signalling. Development. 2016;143(14):2482–93. doi: 10.1242/dev.126516. [DOI] [PubMed] [Google Scholar]
- 24.van Niel G, Porto-Carreiro I, Simoes S, Raposo G. Exosomes: a common pathway for a specialized function. J Biochem. 2006;140(1):13–21. doi: 10.1093/jb/mvj128. [DOI] [PubMed] [Google Scholar]
- 25.Wollert T, Wunder C, Lippincott-Schwartz J, Hurley JH. Membrane scission by the ESCRT-III complex. Nature. 2009;458(7235):172–7. doi: 10.1038/nature07836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Babst M. MVB vesicle formation: ESCRT-dependent, ESCRT-independent and everything in between. Curr Opin Cell Biol. 2011;23(4):452–7. doi: 10.1016/j.ceb.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Niel G, Charrin S, Simoes S, Romao M, Rochin L, Saftig P, et al. The tetraspanin CD63 regulates ESCRT-independent and -dependent endosomal sorting during melanogenesis. Dev Cell. 2011;21(4):708–21. doi: 10.1016/j.devcel.2011.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mathivanan S, Ji H, Simpson RJ. Exosomes: extracellular organelles important in intercellular communication. J Proteom. 2010;73(10):1907–20. doi: 10.1016/j.jprot.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 29.Grant BD, Donaldson JG. Pathways and mechanisms of endocytic recycling. Nat Rev Mol Cell Biol. 2009;10(9):597–608. doi: 10.1038/nrm2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cocucci E, Meldolesi J. Ectosomes and exosomes: shedding the confusion between extracellular vesicles. Trends Cell Biol. 2015;25(6):364–72. doi: 10.1016/j.tcb.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 31.Kobayashi T, Startchev K, Whitney AJ, Gruenber J. Localization of lysobisphosphatidic acid-rich membrane domains in late endosomes. Biol Chem. 2001;382(3):483–5. doi: 10.1515/BC.2001.059. [DOI] [PubMed] [Google Scholar]
- 32.Tauro BJ, Greening DW, Mathias RA, Mathivanan S, Ji H, Simpson RJ. Two distinct populations of exosomes are released from LIM1863 colon carcinoma cell-derived organoids. Mol Cell Proteomics. 2013;12(3):587–98. doi: 10.1074/mcp.M112.021303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramirez MI, Amorim MG, Gadelha C, Milic I, Welsh JA, Freitas VM, et al. Technical challenges of working with extracellular vesicles. Nanoscale. 2018;10(3):881–906. doi: 10.1039/C7NR08360B. [DOI] [PubMed] [Google Scholar]
- 34.Couch Y, Buzas EI, Di Vizio D, Gho YS, Harrison P, Hill AF, et al. A brief history of nearly EV-erything - the rise and rise of extracellular vesicles. J Extracell Vesicles. 2021;10(14):e12144. doi: 10.1002/jev2.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gardiner C, Di Vizio D, Sahoo S, Thery C, Witwer KW, Wauben M, et al. Techniques used for the isolation and characterization of extracellular vesicles: results of a worldwide survey. J Extracell Vesicles. 2016;5:32945. doi: 10.3402/jev.v5.32945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang J, Huang X, Xie J, Han Y, Huang Y, Zhang H. Exosomal analysis: advances in biosensor technology. Clin Chim Acta. 2021;518:142–50. doi: 10.1016/j.cca.2021.03.026. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y, Bi J, Huang J, Tang Y, Du S, Li P, Exosome A review of its classification, isolation techniques, storage, diagnostic and targeted therapy applications. Int J Nanomedicine. 2020;15:6917–34. doi: 10.2147/IJN.S264498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Luo T, Chen SY, Qiu ZX, Miao YR, Ding Y, Pan XY, et al Transcriptomic features in a single extracellular vesicle via single-cell RNA sequencing. Small Methods. 2022:e2200881. [DOI] [PubMed]
- 39.Ferguson S, Yang KS, Weissleder R. Single extracellular vesicle analysis for early cancer detection. Trends Mol Med. 2022;28(8):681–92. doi: 10.1016/j.molmed.2022.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thery C. Exosomes: secreted vesicles and intercellular communications. F1000 Biol Rep. 2011;3:15. doi: 10.3410/B3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200(4):373–83. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ma Y, Wang K, Pan J, Fan Z, Tian C, Deng X, et al. Induced neural progenitor cells abundantly secrete extracellular vesicles and promote the proliferation of neural progenitors via extracellular signal-regulated kinase pathways. Neurobiol Dis. 2019;124:322–34. doi: 10.1016/j.nbd.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Park JE, Tan HS, Datta A, Lai RC, Zhang H, Meng W, et al. Hypoxic tumor cell modulates its microenvironment to enhance angiogenic and metastatic potential by secretion of proteins and exosomes. Mol Cell Proteomics. 2010;9(6):1085–99. doi: 10.1074/mcp.M900381-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crescitelli R, Lasser C, Szabo TG, Kittel A, Eldh M, Dianzani I, et al Distinct RNA profiles in subpopulations of extracellular vesicles: apoptotic bodies, microvesicles and exosomes. J Extracell Vesicles. 2013;2. [DOI] [PMC free article] [PubMed]
- 45.Guescini M, Genedani S, Stocchi V, Agnati LF. Astrocytes and glioblastoma cells release exosomes carrying mtDNA. J Neural Transm (Vienna) 2010;117(1):1–4. doi: 10.1007/s00702-009-0288-8. [DOI] [PubMed] [Google Scholar]
- 46.Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9(6):654–9. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 47.Matarredona ER, Pastor AM. Extracellular vesicle-mediated communication between the glioblastoma and its microenvironment. Cells. 2019;9(1). [DOI] [PMC free article] [PubMed]
- 48.McKenzie AJ, Hoshino D, Hong NH, Cha DJ, Franklin JL, Coffey RJ, et al. KRAS-MEK signaling controls Ago2 sorting into exosomes. Cell Rep. 2016;15(5):978–87. doi: 10.1016/j.celrep.2016.03.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Skotland T, Sandvig K, Llorente A. Lipids in exosomes: current knowledge and the way forward. Prog Lipid Res. 2017;66:30–41. doi: 10.1016/j.plipres.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 50.Llorente A, Skotland T, Sylvanne T, Kauhanen D, Rog T, Orlowski A, et al. Molecular lipidomics of exosomes released by PC-3 prostate cancer cells. Biochim Biophys Acta. 2013;1831(7):1302–9. doi: 10.1016/j.bbalip.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 51.Ratajczak MZ, Ratajczak J. Extracellular microvesicles/exosomes: discovery, disbelief, acceptance, and the future? Leukemia. 2020;34(12):3126–3135. [DOI] [PMC free article] [PubMed]
- 52.Mathieu M, Nevo N, Jouve M, Valenzuela JI, Maurin M, Verweij FJ, et al. Specificities of exosome versus small ectosome secretion revealed by live intracellular tracking of CD63 and CD9. Nat Commun. 2021;12(1):4389. doi: 10.1038/s41467-021-24384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baietti MF, Zhang Z, Mortier E, Melchior A, Degeest G, Geeraerts A, et al. Syndecan-syntenin-ALIX regulates the biogenesis of exosomes. Nat Cell Biol. 2012;14(7):677–85. doi: 10.1038/ncb2502. [DOI] [PubMed] [Google Scholar]
- 54.Thompson CA, Purushothaman A, Ramani VC, Vlodavsky I, Sanderson RD. Heparanase regulates secretion, composition, and function of tumor cell-derived exosomes. J Biol Chem. 2013;288(14):10093–9. doi: 10.1074/jbc.C112.444562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Henne WM, Buchkovich NJ, Emr SD. The ESCRT pathway. Dev Cell. 2011;21(1):77–91. doi: 10.1016/j.devcel.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 56.Villarroya-Beltri C, Baixauli F, Gutierrez-Vazquez C, Sanchez-Madrid F, Mittelbrunn M. Sorting it out: regulation of exosome loading. Semin Cancer Biol. 2014;28:3–13. doi: 10.1016/j.semcancer.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mazurov D, Barbashova L, Filatov A. Tetraspanin protein CD9 interacts with metalloprotease CD10 and enhances its release via exosomes. FEBS J. 2013;280(5):1200–13. doi: 10.1111/febs.12110. [DOI] [PubMed] [Google Scholar]
- 58.Putz U, Howitt J, Lackovic J, Foot N, Kumar S, Silke J, et al. Nedd4 family-interacting protein 1 (Ndfip1) is required for the exosomal secretion of Nedd4 family proteins. J Biol Chem. 2008;283(47):32621–7. doi: 10.1074/jbc.M804120200. [DOI] [PubMed] [Google Scholar]
- 59.de Gassart A, Geminard C, Fevrier B, Raposo G, Vidal M. Lipid raft-associated protein sorting in exosomes. Blood. 2003;102(13):4336–44. doi: 10.1182/blood-2003-03-0871. [DOI] [PubMed] [Google Scholar]
- 60.Verweij FJ, van Eijndhoven MA, Hopmans ES, Vendrig T, Wurdinger T, Cahir-McFarland E, et al. LMP1 association with CD63 in endosomes and secretion via exosomes limits constitutive NF-kappaB activation. EMBO J. 2011;30(11):2115–29. doi: 10.1038/emboj.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Squadrito ML, Baer C, Burdet F, Maderna C, Gilfillan GD, Lyle R, et al. Endogenous RNAs modulate microRNA sorting to exosomes and transfer to acceptor cells. Cell Rep. 2014;8(5):1432–46. doi: 10.1016/j.celrep.2014.07.035. [DOI] [PubMed] [Google Scholar]
- 62.Villarroya-Beltri C, Gutierrez-Vazquez C, Sanchez-Cabo F, Perez-Hernandez D, Vazquez J, Martin-Cofreces N, et al. Sumoylated hnRNPA2B1 controls the sorting of miRNAs into exosomes through binding to specific motifs. Nat Commun. 2013;4:2980. doi: 10.1038/ncomms3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Santangelo L, Giurato G, Cicchini C, Montaldo C, Mancone C, Tarallo R, et al. The RNA-binding protein SYNCRIP is a component of the hepatocyte exosomal machinery controlling microRNA sorting. Cell Rep. 2016;17(3):799–808. doi: 10.1016/j.celrep.2016.09.031. [DOI] [PubMed] [Google Scholar]
- 64.Doherty GJ, McMahon HT. Mechanisms of endocytosis. Annu Rev Biochem. 2009;78:857–902. doi: 10.1146/annurev.biochem.78.081307.110540. [DOI] [PubMed] [Google Scholar]
- 65.Gonda A, Kabagwira J, Senthil GN, Wall NR. Internalization of ‘sis. Mol Cancer Res. 2019;17(2):337–47. doi: 10.1158/1541-7786.MCR-18-0891. [DOI] [PubMed] [Google Scholar]
- 66.Tian T, Zhu YL, Zhou YY, Liang GF, Wang YY, Hu FH, et al. Exosome uptake through clathrin-mediated endocytosis and macropinocytosis and mediating miR-21 delivery. J Biol Chem. 2014;289(32):22258–67. doi: 10.1074/jbc.M114.588046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Horibe S, Tanahashi T, Kawauchi S, Murakami Y, Rikitake Y. Mechanism of recipient cell-dependent differences in exosome uptake. BMC Cancer. 2018;18(1):47. doi: 10.1186/s12885-017-3958-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Feng D, Zhao WL, Ye YY, Bai XC, Liu RQ, Chang LF, et al. Cellular internalization of exosomes occurs through phagocytosis. Traffic. 2010;11(5):675–87. doi: 10.1111/j.1600-0854.2010.01041.x. [DOI] [PubMed] [Google Scholar]
- 69.Guitart K, Loers G, Buck F, Bork U, Schachner M, Kleene R. Improvement of neuronal cell survival by astrocyte-derived exosomes under hypoxic and ischemic conditions depends on prion protein. Glia. 2016;64(6):896–910. doi: 10.1002/glia.22963. [DOI] [PubMed] [Google Scholar]
- 70.Gurung S, Perocheau D, Touramanidou L, Baruteau J. The exosome journey: from biogenesis to uptake and intracellular signalling. Cell Commun Signal. 2021;19(1):47. doi: 10.1186/s12964-021-00730-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Parolini I, Federici C, Raggi C, Lugini L, Palleschi S, De Milito A, et al. Microenvironmental pH is a key factor for exosome traffic in tumor cells. J Biol Chem. 2009;284(49):34211–22. doi: 10.1074/jbc.M109.041152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Del Conde I, Shrimpton CN, Thiagarajan P, Lopez JA. Tissue-factor-bearing microvesicles arise from lipid rafts and fuse with activated platelets to initiate coagulation. Blood. 2005;106(5):1604–11. doi: 10.1182/blood-2004-03-1095. [DOI] [PubMed] [Google Scholar]
- 73.Tkach M, Kowal J, Zucchetti AE, Enserink L, Jouve M, Lankar D, et al. Qualitative differences in T-cell activation by dendritic cell-derived extracellular vesicle subtypes. EMBO J. 2017;36(20):3012–28. doi: 10.15252/embj.201696003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sobo-Vujanovic A, Munich S, Vujanovic NL. Dendritic-cell exosomes cross-present toll-like receptor-ligands and activate bystander dendritic cells. Cell Immunol. 2014;289(1–2):119–27. doi: 10.1016/j.cellimm.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Soria Lopez JA, Gonzalez HM, Leger GC. Alzheimer’s disease. Handb Clin Neurol. 2019;167:231–55. doi: 10.1016/B978-0-12-804766-8.00013-3. [DOI] [PubMed] [Google Scholar]
- 76.Leng F, Edison P. Neuroinflammation and microglial activation in Alzheimer disease: where do we go from here? Nat Rev Neurol. 2021;17(3):157–72. doi: 10.1038/s41582-020-00435-y. [DOI] [PubMed] [Google Scholar]
- 77.Cryan JF, O’Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, et al. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019;99(4):1877–2013. doi: 10.1152/physrev.00018.2018. [DOI] [PubMed] [Google Scholar]
- 78.Butterfield DA, Halliwell B. Oxidative stress, dysfunctional glucose metabolism and Alzheimer disease. Nat Rev Neurosci. 2019;20(3):148–60. doi: 10.1038/s41583-019-0132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gallart-Palau X, Guo X, Serra A, Sze SK. Alzheimer’s disease progression characterized by alterations in the molecular profiles and biogenesis of brain extracellular vesicles. Alzheimers Res Ther. 2020;12(1):54. doi: 10.1186/s13195-020-00623-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Asai H, Ikezu S, Tsunoda S, Medalla M, Luebke J, Haydar T, et al. Depletion of microglia and inhibition of exosome synthesis halt tau propagation. Nat Neurosci. 2015;18(11):1584–93. doi: 10.1038/nn.4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Su H, Rustam YH, Masters CL, Makalic E, McLean CA, Hill AF, et al. Characterization of brain-derived extracellular vesicle lipids in Alzheimer’s disease. J Extracell Vesicles. 2021;10(7):e12089. doi: 10.1002/jev2.12089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Men Y, Yelick J, Jin S, Tian Y, Chiang MSR, Higashimori H, et al. Exosome reporter mice reveal the involvement of exosomes in mediating neuron to astroglia communication in the CNS. Nat Commun. 2019;10(1):4136. doi: 10.1038/s41467-019-11534-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Goetzl EJ, Boxer A, Schwartz JB, Abner EL, Petersen RC, Miller BL, et al. Altered lysosomal proteins in neural-derived plasma exosomes in preclinical Alzheimer disease. Neurology. 2015;85(1):40–7. doi: 10.1212/WNL.0000000000001702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Abner EL, Jicha GA, Shaw LM, Trojanowski JQ, Goetzl EJ. Plasma neuronal exosomal levels of Alzheimer’s disease biomarkers in normal aging. Ann Clin Transl Neurol. 2016;3(5):399–403. doi: 10.1002/acn3.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Norman M, Ter-Ovanesyan D, Trieu W, Lazarovits R, Kowal EJK, Lee JH, et al. L1CAM is not associated with extracellular vesicles in human cerebrospinal fluid or plasma. Nat Methods. 2021;18(6):631–4. doi: 10.1038/s41592-021-01174-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gomes DE, Witwer KW. L1CAM-associated extracellular vesicles: a systematic review of nomenclature, sources, separation, and characterization. J Extracell Biol. 2022;1(3). [DOI] [PMC free article] [PubMed]
- 87.Fernandes A, Ribeiro AR, Monteiro M, Garcia G, Vaz AR, Brites D. Secretome from SH-SY5Y APPSwe cells trigger time-dependent CHME3 microglia activation phenotypes, ultimately leading to miR-21 exosome shuttling. Biochimie. 2018;155:67–82. doi: 10.1016/j.biochi.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 88.Sardar Sinha M, Ansell-Schultz A, Civitelli L, Hildesjo C, Larsson M, Lannfelt L, et al. Alzheimer’s disease pathology propagation by exosomes containing toxic amyloid-beta oligomers. Acta Neuropathol. 2018;136(1):41–56. doi: 10.1007/s00401-018-1868-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yuyama K, Sun H, Mitsutake S, Igarashi Y. Sphingolipid-modulated exosome secretion promotes clearance of amyloid-beta by microglia. J Biol Chem. 2012;287(14):10977–89. doi: 10.1074/jbc.M111.324616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nogueras-Ortiz CJ, Mahairaki V, Delgado-Peraza F, Das D, Avgerinos K, Eren E, et al Astrocyte- and neuron-derived extracellular vesicles from Alzheimer’s disease patients effect complement-mediated neurotoxicity. Cells. 2020;9(7). [DOI] [PMC free article] [PubMed]
- 91.Sofroniew MV. Astrocyte reactivity: subtypes, states, and functions in CNS innate immunity. Trends Immunol. 2020;41(9):758–70. doi: 10.1016/j.it.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Upadhya R, Zingg W, Shetty S, Shetty AK. Astrocyte-derived extracellular vesicles: neuroreparative properties and role in the pathogenesis of neurodegenerative disorders. J Control Release. 2020;323:225–39. doi: 10.1016/j.jconrel.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sollvander S, Nikitidou E, Brolin R, Soderberg L, Sehlin D, Lannfelt L, et al. Accumulation of amyloid-beta by astrocytes result in enlarged endosomes and microvesicle-induced apoptosis of neurons. Mol Neurodegener. 2016;11(1):38. doi: 10.1186/s13024-016-0098-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Abdullah M, Takase H, Nunome M, Enomoto H, Ito J, Gong JS, et al. Amyloid-beta reduces exosome release from astrocytes by enhancing JNK phosphorylation. J Alzheimers Dis. 2016;53(4):1433–41. doi: 10.3233/JAD-160292. [DOI] [PubMed] [Google Scholar]
- 95.Dinkins MB, Dasgupta S, Wang G, Zhu G, Bieberich E. Exosome reduction in vivo is associated with lower amyloid plaque load in the 5XFAD mouse model of Alzheimer’s disease. Neurobiol Aging. 2014;35(8):1792–800. doi: 10.1016/j.neurobiolaging.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang G, Dinkins M, He Q, Zhu G, Poirier C, Campbell A, et al. Astrocytes secrete exosomes enriched with proapoptotic ceramide and prostate apoptosis response 4 (PAR-4): potential mechanism of apoptosis induction in Alzheimer disease (AD) J Biol Chem. 2012;287(25):21384–95. doi: 10.1074/jbc.M112.340513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chiarini A, Armato U, Gardenal E, Gui L, Dal Pra I. Amyloid beta-exposed human astrocytes overproduce phospho-tau and overrelease it within exosomes, effects suppressed by calcilytic NPS 2143-further implications for Alzheimer’s therapy. Front Neurosci. 2017;11:217. doi: 10.3389/fnins.2017.00217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Menck K, Sonmezer C, Worst TS, Schulz M, Dihazi GH, Streit F, et al. Neutral sphingomyelinases control extracellular vesicles budding from the plasma membrane. J Extracell Vesicles. 2017;6(1):1378056. doi: 10.1080/20013078.2017.1378056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Goetzl EJ, Mustapic M, Kapogiannis D, Eitan E, Lobach IV, Goetzl L, et al. Cargo proteins of plasma astrocyte-derived exosomes in Alzheimer’s disease. FASEB J. 2016;30(11):3853–9. doi: 10.1096/fj.201600756R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Goetzl EJ, Schwartz JB, Abner EL, Jicha GA, Kapogiannis D. High complement levels in astrocyte-derived exosomes of Alzheimer disease. Ann Neurol. 2018;83(3):544–52. doi: 10.1002/ana.25172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Winston CN, Goetzl EJ, Schwartz JB, Elahi FM, Rissman RA. Complement protein levels in plasma astrocyte-derived exosomes are abnormal in conversion from mild cognitive impairment to Alzheimer’s disease dementia. Alzheimers Dement (Amst) 2019;11:61–6. doi: 10.1016/j.dadm.2018.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hu X, Leak RK, Shi Y, Suenaga J, Gao Y, Zheng P, et al. Microglial and macrophage polarization-new prospects for brain repair. Nat Rev Neurol. 2015;11(1):56–64. doi: 10.1038/nrneurol.2014.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Colonna M, Butovsky O. Microglia function in the central nervous system during health and neurodegeneration. Annu Rev Immunol. 2017;35:441–68. doi: 10.1146/annurev-immunol-051116-052358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wright-Jin EC, Gutmann DH. Microglia as dynamic cellular mediators of brain function. Trends Mol Med. 2019;25(11):967–79. doi: 10.1016/j.molmed.2019.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Li Q, Barres BA. Microglia and macrophages in brain homeostasis and disease. Nat Rev Immunol. 2018;18(4):225–42. doi: 10.1038/nri.2017.125. [DOI] [PubMed] [Google Scholar]
- 106.Menassa DA, Muntslag TAO, Martin-Estebane M, Barry-Carroll L, Chapman MA, Adorjan I, et al. The spatiotemporal dynamics of microglia across the human lifespan. Dev Cell. 2022;57(17):2127–39 e2126. doi: 10.1016/j.devcel.2022.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Li Y, Xia X, Wang Y, Zheng JC. Mitochondrial dysfunction in microglia: a novel perspective for pathogenesis of Alzheimer’s disease. J Neuroinflammation. 2022;19(1):248. doi: 10.1186/s12974-022-02613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Deczkowska A, Keren-Shaul H, Weiner A, Colonna M, Schwartz M, Amit I. Disease-associated microglia: a universal immune sensor of neurodegeneration. Cell. 2018;173(5):1073–81. doi: 10.1016/j.cell.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 109.Hickman S, Izzy S, Sen P, Morsett L, El Khoury J. Microglia in neurodegeneration. Nat Neurosci. 2018;21(10):1359–69. doi: 10.1038/s41593-018-0242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Guo M, Hao Y, Feng Y, Li H, Mao Y, Dong Q, et al. Microglial exosomes in neurodegenerative disease. Front Mol Neurosci. 2021;14:630808. doi: 10.3389/fnmol.2021.630808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gouwens LK, Ismail MS, Rogers VA, Zeller NT, Garrad EC, Amtashar FS, et al. Abeta42 protofibrils interact with and are trafficked through microglial-derived microvesicles. ACS Chem Neurosci. 2018;9(6):1416–25. doi: 10.1021/acschemneuro.8b00029. [DOI] [PubMed] [Google Scholar]
- 112.Cohn W, Melnik M, Huang C, Teter B, Chandra S, Zhu C, et al. Multi-omics analysis of microglial extracellular vesicles from human Alzheimer’s disease brain tissue reveals disease-associated signatures. Front Pharmacol. 2021;12:766082. doi: 10.3389/fphar.2021.766082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mager SELA, Breakefield I, Wood XO. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov. 2013;12(5):347–57. doi: 10.1038/nrd3978. [DOI] [PubMed] [Google Scholar]
- 114.Huang S, Liao X, Wu J, Zhang X, Li Y, Xiang D, et al. The microglial membrane receptor TREM2 mediates exosome secretion to promote phagocytosis of amyloid-beta by microglia. FEBS Lett. 2022;596(8):1059–71. doi: 10.1002/1873-3468.14336. [DOI] [PubMed] [Google Scholar]
- 115.Chistiakov DA, Chistiakov AA. Alpha-synuclein-carrying extracellular vesicles in Parkinson’s disease: deadly transmitters. Acta Neurol Belg. 2017;117(1):43–51. doi: 10.1007/s13760-016-0679-1. [DOI] [PubMed] [Google Scholar]
- 116.Emmanouilidou E, Melachroinou K, Roumeliotis T, Garbis SD, Ntzouni M, Margaritis LH, et al. Cell-produced alpha-synuclein is secreted in a calcium-dependent manner by exosomes and impacts neuronal survival. J Neurosci. 2010;30(20):6838–51. doi: 10.1523/JNEUROSCI.5699-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Alvarez-Erviti L, Seow Y, Schapira AH, Gardiner C, Sargent IL, Wood MJ, et al. Lysosomal dysfunction increases exosome-mediated alpha-synuclein release and transmission. Neurobiol Dis. 2011;42(3):360–7. doi: 10.1016/j.nbd.2011.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Niu M, Li Y, Li G, Zhou L, Luo N, Yao M, et al. A longitudinal study on alpha-synuclein in plasma neuronal exosomes as a biomarker for Parkinson’s disease development and progression. Eur J Neurol. 2020;27(6):967–74. doi: 10.1111/ene.14208. [DOI] [PubMed] [Google Scholar]
- 119.Jiang C, Hopfner F, Katsikoudi A, Hein R, Catli C, Evetts S, et al. Serum neuronal exosomes predict and differentiate Parkinson’s disease from atypical parkinsonism. J Neurol Neurosurg Psychiatry. 2020;91(7):720–9. doi: 10.1136/jnnp-2019-322588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Danzer KM, Kranich LR, Ruf WP, Cagsal-Getkin O, Winslow AR, Zhu L, et al. Exosomal cell-to-cell transmission of alpha synuclein oligomers. Mol neurodegeneration. 2012;7:42. doi: 10.1186/1750-1326-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhou T, Lin D, Chen Y, Peng S, Jing X, Lei M, et al. Alpha-synuclein accumulation in SH-SY5Y cell impairs autophagy in microglia by exosomes overloading miR-19a-3p. Epigenomics. 2019;11(15):1661–77. doi: 10.2217/epi-2019-0222. [DOI] [PubMed] [Google Scholar]
- 122.Kunadt M, Eckermann K, Stuendl A, Gong J, Russo B, Strauss K, et al. Extracellular vesicle sorting of alpha-synuclein is regulated by sumoylation. Acta Neuropathol. 2015;129(5):695–713. doi: 10.1007/s00401-015-1408-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kumar R, Donakonda S, Muller SA, Botzel K, Hoglinger GU, Koeglsperger T. FGF2 affects Parkinson’s Disease-Associated Molecular Networks through Exosomal Rab8b/Rab31. Front Genet. 2020;11:572058. doi: 10.3389/fgene.2020.572058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Anastasi F, Masciandaro SM, Carratore RD, Dell’Anno MT, Signore G, Falleni A, et al Proteomics profiling of neuron-derived small extracellular vesicles from human plasma: enabling single-subject analysis. International journal of molecular sciences. 2021;22(6). [DOI] [PMC free article] [PubMed]
- 125.Xia X, Wang Y, Zheng JC. The microRNA-17 ~ 92 family as a key regulator of neurogenesis and potential regenerative therapeutics of neurological disorders. Stem Cell Rev Rep. 2022;18(2):401–11. doi: 10.1007/s12015-020-10050-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Xia X, Lu H, Li C, Huang Y, Wang Y, Yang X, et al. miR-106b regulates the proliferation and differentiation of neural stem/progenitor cells through Tp53inp1-Tp53-Cdkn1a axis. Stem Cell Res Ther. 2019;10(1):282. doi: 10.1186/s13287-019-1387-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Li Y, Li Z, Gu J, Xu X, Chen H, Gui Y. Exosomes isolated during dopaminergic neuron differentiation suppressed neuronal inflammation in a rodent model of Parkinson’s disease. Neurosci Lett. 2022;771:136414. doi: 10.1016/j.neulet.2021.136414. [DOI] [PubMed] [Google Scholar]
- 128.Valdinocci D, Radford RA, Siow SM, Chung RS, Pountney DL. Potential modes of intercellular alpha-synuclein transmission. Int J Mol Sci. 2017;18(2). [DOI] [PMC free article] [PubMed]
- 129.Norshalena Shakespear M, Ogura, Yamaki J, Homma Y. Astrocyte-derived exosomal microRNA miR-200a-3p prevents MPP(+)-induced apoptotic cell death through down-regulation of MKK4. Neurochem Res. 2020;45(5):1020–33. doi: 10.1007/s11064-020-02977-5. [DOI] [PubMed] [Google Scholar]
- 130.Guo M, Wang J, Zhao Y, Feng Y, Han S, Dong Q, et al. Microglial exosomes facilitate alpha-synuclein transmission in Parkinson’s disease. Brain. 2020;143(5):1476–97. doi: 10.1093/brain/awaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chang C, Lang H, Geng N, Wang J, Li N, Wang X. Exosomes of BV-2 cells induced by alpha-synuclein: important mediator of neurodegeneration in PD. Neurosci Lett. 2013;548:190–5. doi: 10.1016/j.neulet.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 132.Tsutsumi R, Hori Y, Seki T, Kurauchi Y, Sato M, Oshima M, et al. Involvement of exosomes in dopaminergic neurodegeneration by microglial activation in midbrain slice cultures. Biochem Biophys Res Commun. 2019;511(2):427–33. doi: 10.1016/j.bbrc.2019.02.076. [DOI] [PubMed] [Google Scholar]
- 133.Fruhbeis C, Frohlich D, Kuo WP, Amphornrat J, Thilemann S, Saab AS, et al. Neurotransmitter-triggered transfer of exosomes mediates oligodendrocyte-neuron communication. PLoS Biol. 2013;11(7):e1001604. doi: 10.1371/journal.pbio.1001604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Fruhbeis C, Kuo-Elsner WP, Muller C, Barth K, Peris L, Tenzer S, et al. Oligodendrocytes support axonal transport and maintenance via exosome secretion. PLoS Biol. 2020;18(12):e3000621. doi: 10.1371/journal.pbio.3000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ohmichi T, Mitsuhashi M, Tatebe H, Kasai T, Ali El-Agnaf OM, Tokuda T. Quantification of brain-derived extracellular vesicles in plasma as a biomarker to diagnose Parkinson’s and related diseases. Parkinsonism Relat Disord. 2019;61:82–7. doi: 10.1016/j.parkreldis.2018.11.021. [DOI] [PubMed] [Google Scholar]
- 136.Dutta S, Hornung S, Kruayatidee A, Maina KN, Del Rosario I, Paul KC, et al. Alpha-synuclein in blood exosomes immunoprecipitated using neuronal and oligodendroglial markers distinguishes Parkinson’s disease from multiple system atrophy. Acta Neuropathol. 2021;142(3):495–511. doi: 10.1007/s00401-021-02324-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Silverman JM, Christy D, Shyu CC, Moon KM, Fernando S, Gidden Z, et al. CNS-derived extracellular vesicles from superoxide dismutase 1 (SOD1)(G93A) ALS mice originate from astrocytes and neurons and carry misfolded SOD1. J Biol Chem. 2019;294(10):3744–59. doi: 10.1074/jbc.RA118.004825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Pinto S, Cunha C, Barbosa M, Vaz AR, Brites D. Exosomes from NSC-34 cells transfected with hSOD1-G93A are enriched in miR-124 and drive alterations in microglia phenotype. Front Neurosci. 2017;11:273. doi: 10.3389/fnins.2017.00273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Westergard T, Jensen BK, Wen X, Cai J, Kropf E, Iacovitti L, et al. Cell-to-cell transmission of dipeptide repeat proteins linked to C9orf72-ALS/FTD. Cell Rep. 2016;17(3):645–52. doi: 10.1016/j.celrep.2016.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kok JR, Palminha NM, Dos Santos Souza C, El-Khamisy SF, Ferraiuolo L. DNA damage as a mechanism of neurodegeneration in ALS and a contributor to astrocyte toxicity. Cell Mol Life Sci. 2021;78(15):5707–29. doi: 10.1007/s00018-021-03872-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Katsu M, Hama Y, Utsumi J, Takashina K, Yasumatsu H, Mori F, et al. MicroRNA expression profiles of neuron-derived extracellular vesicles in plasma from patients with amyotrophic lateral sclerosis. Neurosci Lett. 2019;708:134176. doi: 10.1016/j.neulet.2019.03.048. [DOI] [PubMed] [Google Scholar]
- 142.Qi Y, Ma N, Chen X, Wang Y, Zhang W, Wan J. CircRtn4 acts as the sponge of mir-24-3p to promote neurite growth by regulating CHD5. Front Mol Neurosci. 2021;14:660429. doi: 10.3389/fnmol.2021.660429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Di G, Yang X, Cheng F, Liu H, Xu M. CEBPA-AS1 knockdown alleviates oxygen-glucose deprivation/reperfusion-induced neuron cell damage by the microRNA 24-3p/BOK axis. Mol Cell Biol. 2021;41(8):e0006521. doi: 10.1128/MCB.00065-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Luo H, Ye G, Liu Y, Huang D, Luo Q, Chen W, et al. Mir-150-3p enhances neuroprotective effects of neural stem cell exosomes after hypoxic-ischemic brain injury by targeting CASP2. Neurosci Lett. 2022;779:136635. doi: 10.1016/j.neulet.2022.136635. [DOI] [PubMed] [Google Scholar]
- 145.Thompson AG, Gray E, Mager I, Thezenas ML, Charles PD, Talbot K, et al. CSF extracellular vesicle proteomics demonstrates altered protein homeostasis in amyotrophic lateral sclerosis. Clin Proteom. 2020;17:31. doi: 10.1186/s12014-020-09294-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Basso M, Pozzi S, Tortarolo M, Fiordaliso F, Bisighini C, Pasetto L, et al. Mutant copper-zinc superoxide dismutase (SOD1) induces protein secretion pathway alterations and exosome release in astrocytes: implications for disease spreading and motor neuron pathology in amyotrophic lateral sclerosis. J Biol Chem. 2013;288(22):15699–711. doi: 10.1074/jbc.M112.425066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Varcianna A, Myszczynska MA, Castelli LM, O’Neill B, Kim Y, Talbot J, et al. Micro-RNAs secreted through astrocyte-derived extracellular vesicles cause neuronal network degeneration in C9orf72 ALS. EBioMedicine. 2019;40:626–35. doi: 10.1016/j.ebiom.2018.11.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Chen Y, Xia K, Chen L, Fan D. Increased interleukin-6 levels in the astrocyte-derived exosomes of sporadic amyotrophic lateral sclerosis patients. Front Neurosci. 2019;13:574. doi: 10.3389/fnins.2019.00574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Boillee S, Yamanaka K, Lobsiger CS, Copeland NG, Jenkins NA, Kassiotis G, et al. Onset and progression in inherited ALS determined by motor neurons and microglia. Science. 2006;312(5778):1389–92. doi: 10.1126/science.1123511. [DOI] [PubMed] [Google Scholar]
- 150.Massenzio F, Pena-Altamira E, Petralla S, Virgili M, Zuccheri G, Miti A, et al. Microglial overexpression of fALS-linked mutant SOD1 induces SOD1 processing impairment, activation and neurotoxicity and is counteracted by the autophagy inducer trehalose. Biochim Biophys Acta Mol Basis Dis. 2018;1864(12):3771–85. doi: 10.1016/j.bbadis.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 151.Vaz AR, Pinto S, Ezequiel C, Cunha C, Carvalho LA, Moreira R, et al. Phenotypic effects of wild-type and mutant SOD1 expression in N9 murine microglia at steady state, inflammatory and immunomodulatory conditions. Front Cell Neurosci. 2019;13:109. doi: 10.3389/fncel.2019.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhang S, Hu L, Jiang J, Li H, Wu Q, Ooi K, et al. HMGB1/RAGE axis mediates stress-induced RVLM neuroinflammation in mice via impairing mitophagy flux in microglia. J Neuroinflammation. 2020;17(1):15. doi: 10.1186/s12974-019-1673-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Aloi MS, Prater KE, Sopher B, Davidson S, Jayadev S, Garden GA. The pro-inflammatory microRNA miR-155 influences fibrillar beta-Amyloid1 -42 catabolism by microglia. Glia. 2021;69(7):1736–48. doi: 10.1002/glia.23988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Yang B, Yang R, Xu B, Fu J, Qu X, Li L, et al. miR-155 and miR-146a collectively regulate meningitic Escherichia coli infection-mediated neuroinflammatory responses. J Neuroinflammation. 2021;18(1):114. doi: 10.1186/s12974-021-02165-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wanker EE, Ast A, Schindler F, Trepte P, Schnoegl S. The pathobiology of perturbed mutant huntingtin protein-protein interactions in Huntington’s disease. J Neurochem. 2019;151(4):507–19. doi: 10.1111/jnc.14853. [DOI] [PubMed] [Google Scholar]
- 156.Ananbeh H, Novak J, Juhas S, Juhasova J, Klempir J, Doleckova K, et al Huntingtin co-isolates with small extracellular vesicles from blood plasma of TgHD and KI-HD pig models of Huntington’s disease and human blood plasma. International journal of molecular sciences. 2022;23(10). [DOI] [PMC free article] [PubMed]
- 157.Zhang X, Abels ER, Redzic JS, Margulis J, Finkbeiner S, Breakefield XO. Potential transfer of polyglutamine and CAG-repeat RNA in extracellular vesicles in Huntington’s disease: background and evaluation in cell culture. Cell Mol Neurobiol. 2016;36(3):459–70. doi: 10.1007/s10571-016-0350-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Morais R, Sogorb-Gonzalez M, Bar C, Timmer NC, Van der Bent ML, Wartel M, et al Functional intercellular transmission of miHTT via extracellular vesicles: an in Vitro Proof-of-mechanism study. Cells. 2022;11(17). [DOI] [PMC free article] [PubMed]
- 159.Xie HM, Su X, Zhang FY, Dai CL, Wu RH, Li Y, et al. Profile of the RNA in exosomes from astrocytes and microglia using deep sequencing: implications for neurodegeneration mechanisms. Neural Regen Res. 2022;17(3):608–17. doi: 10.4103/1673-5374.320999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hong Y, Zhao T, Li XJ, Li S. Mutant huntingtin inhibits αB-Crystallin expression and impairs exosome secretion from astrocytes. J Neurosci. 2017;37(39):9550–63. doi: 10.1523/JNEUROSCI.1418-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Jiang YL, Wang ZX, Liu XX, Wan MD, Liu YW, Jiao B, et al. The protective effects of osteocyte-derived extracellular vesicles against Alzheimer’s disease diminished with aging. Adv Sci (Weinh) 2022;9(17):e2105316. doi: 10.1002/advs.202105316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zhao L, Ye Y, Gu L, Jian Z, Stary CM, Xiong X. Extracellular vesicle-derived miRNA as a novel regulatory system for bi-directional communication in gut-brain-microbiota axis. J Transl Med. 2021;19(1):202. doi: 10.1186/s12967-021-02861-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Xi S, Wang Y, Wu C, Peng W, Zhu Y, Hu W. Intestinal epithelial cell exosome launches IL-1beta-mediated neuron injury in sepsis-associated encephalopathy. Front Cell Infect Microbiol. 2021;11:783049. doi: 10.3389/fcimb.2021.783049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Chavez L, Meguro J, Chen S, de Paiva VN, Zambrano R, Eterno JM, et al. Circulating extracellular vesicles activate the pyroptosis pathway in the brain following ventilation-induced lung injury. J Neuroinflammation. 2021;18(1):310. doi: 10.1186/s12974-021-02364-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Gao G, Li C, Zhu J, Wang Y, Huang Y, Zhao S, et al Glutaminase 1 regulates neuroinflammation after cerebral ischemia through enhancing microglial activation and pro-inflammatory exosome release. Frontiers Immunol. 2020;11. [DOI] [PMC free article] [PubMed]
- 166.Guo M, Yin Z, Chen F, Lei P. Mesenchymal stem cell-derived exosome: a promising alternative in the therapy of Alzheimer’s disease. Alzheimers Res Ther. 2020;12(1):109. doi: 10.1186/s13195-020-00670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Nakano M, Kubota K, Kobayashi E, Chikenji TS, Saito Y, Konari N, et al. Bone marrow-derived mesenchymal stem cells improve cognitive impairment in an Alzheimer’s disease model by increasing the expression of microRNA-146a in hippocampus. Sci Rep. 2020;10(1):10772. doi: 10.1038/s41598-020-67460-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Casella G, Rasouli J, Boehm A, Zhang W, Xiao D, Ishikawa LLW, et al Oligodendrocyte-derived extracellular vesicles as antigen-specific therapy for autoimmune neuroinflammation in mice. Sci Transl Med. 2020;12(568). [DOI] [PMC free article] [PubMed]
- 169.Jiang D, Gong F, Ge X, Lv C, Huang C, Feng S, et al. Neuron-derived exosomes-transmitted mir-124-3p protect traumatically injured spinal cord by suppressing the activation of neurotoxic microglia and astrocytes. J Nanobiotechnol. 2020;18(1):105. doi: 10.1186/s12951-020-00665-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Frisoni GB, Boccardi M, Barkhof F, Blennow K, Cappa S, Chiotis K, et al. Strategic roadmap for an early diagnosis of Alzheimer’s disease based on biomarkers. Lancet Neurol. 2017;16(8):661–76. doi: 10.1016/S1474-4422(17)30159-X. [DOI] [PubMed] [Google Scholar]
- 171.Cheng L, Doecke JD, Sharples RA, Villemagne VL, Fowler CJ, Rembach A, et al. Prognostic serum miRNA biomarkers associated with Alzheimer’s disease shows concordance with neuropsychological and neuroimaging assessment. Mol Psychiatry. 2015;20(10):1188–96. doi: 10.1038/mp.2014.127. [DOI] [PubMed] [Google Scholar]
- 172.Soares Martins T, Marcalo R, da Cruz ESCB, Trindade D, Catita J, Amado F, et al. Novel exosome biomarker candidates for Alzheimer’s disease unravelled through mass spectrometry analysis. Mol Neurobiol. 2022;59(5):2838–54. doi: 10.1007/s12035-022-02762-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wang Y, Yuan P, Ding L, Zhu J, Qi X, Zhang Y, et al Circulating extracellular vesicle-containing microRNAs reveal potential pathogenesis of Alzheimer’s disease. Frontiers in cellular neuroscience. 2022;16. [DOI] [PMC free article] [PubMed]
- 174.Lugli G, Cohen AM, Bennett DA, Shah RC, Fields CJ, Hernandez AG, et al. Plasma exosomal miRNAs in persons with and without Alzheimer Disease: altered expression and prospects for biomarkers. PLoS ONE. 2015;10(10):e0139233. doi: 10.1371/journal.pone.0139233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yang TT, Liu CG, Gao SC, Zhang Y, Wang PC. The serum exosome derived microRNA-135a, -193b, and – 384 were potential Alzheimer’s disease biomarkers. Biomed Environ Sci. 2018;31(2):87–96. doi: 10.3967/bes2018.011. [DOI] [PubMed] [Google Scholar]
- 176.Jia L, Zhu M, Yang J, Pang Y, Wang Q, Li T, et al. Exosomal microRNA-based predictive model for preclinical Alzheimer’s disease: a multicenter study. Biol Psychiatry. 2022;92(1):44–53. doi: 10.1016/j.biopsych.2021.12.015. [DOI] [PubMed] [Google Scholar]
- 177.Fotuhi SN, Khalaj-Kondori M, Hoseinpour Feizi MA, Talebi M. Long non-coding RNA BACE1-AS may serve as an Alzheimer’s disease blood-based biomarker. J Mol Neurosci. 2019;69(3):351–9. doi: 10.1007/s12031-019-01364-2. [DOI] [PubMed] [Google Scholar]
- 178.Li Y, Meng S, Di W, Xia M, Dong L, Zhao Y, et al. Amyloid-beta protein and MicroRNA-384 in NCAM-Labeled exosomes from peripheral blood are potential diagnostic markers for Alzheimer’s disease. CNS Neurosci Ther. 2022;28(7):1093–107. doi: 10.1111/cns.13846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li Y, Xia M, Meng S, Wu D, Ling S, Chen X, et al. MicroRNA-29c-3p in dual-labeled exosome is a potential diagnostic marker of subjective cognitive decline. Neurobiol Dis. 2022;171:105800. doi: 10.1016/j.nbd.2022.105800. [DOI] [PubMed] [Google Scholar]
- 180.Cha DJ, Mengel D, Mustapic M, Liu W, Selkoe DJ, Kapogiannis D, et al. miR-212 and miR-132 are downregulated in neurally derived plasma exosomes of Alzheimer’s patients. Front Neurosci. 2019;13:1208. doi: 10.3389/fnins.2019.01208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Fiandaca MS, Kapogiannis D, Mapstone M, Boxer A, Eitan E, Schwartz JB, et al. Identification of preclinical Alzheimer’s disease by a profile of pathogenic proteins in neurally derived blood exosomes: a case-control study. Alzheimers Dement. 2015;11(6):600–7 e601. doi: 10.1016/j.jalz.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Chi H, Yao R, Sun C, Leng B, Shen T, Wang T, et al. Blood neuroexosomal mitochondrial proteins predict Alzheimer disease in diabetes. Diabetes. 2022;71(6):1313–23. doi: 10.2337/db21-0969. [DOI] [PubMed] [Google Scholar]
- 183.Shi M, Liu C, Cook TJ, Bullock KM, Zhao Y, Ginghina C, et al. Plasma exosomal alpha-synuclein is likely CNS-derived and increased in Parkinson’s disease. Acta Neuropathol. 2014;128(5):639–50. doi: 10.1007/s00401-014-1314-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Leng B, Sun H, Zhao J, Liu Y, Shen T, Liu W, et al. Plasma exosomal prion protein levels are correlated with cognitive decline in PD patients. Neurosci Lett. 2020;723:134866. doi: 10.1016/j.neulet.2020.134866. [DOI] [PubMed] [Google Scholar]
- 185.Gui Y, Liu H, Zhang L, Lv W, Hu X. Altered microRNA profiles in cerebrospinal fluid exosome in Parkinson disease and Alzheimer disease. Oncotarget. 2015;6(35):37043–53. doi: 10.18632/oncotarget.6158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Zhou Q, He L, Hu J, Gao Y, Shen D, Ni Y, et al Increased expression of coronin-1a in amyotrophic lateral sclerosis: a potential diagnostic biomarker and therapeutic target. Front Med. 2022. [DOI] [PubMed]
- 187.Chen PC, Wu D, Hu CJ, Chen HY, Hsieh YC, Huang CC. Exosomal TAR DNA-binding protein-43 and neurofilaments in plasma of amyotrophic lateral sclerosis patients: a longitudinal follow-up study. J Neurol Sci. 2020;418:117070. doi: 10.1016/j.jns.2020.117070. [DOI] [PubMed] [Google Scholar]
- 188.Prada I, Gabrielli M, Turola E, Iorio A, D’Arrigo G, Parolisi R, et al. Glia-to-neuron transfer of miRNAs via extracellular vesicles: a new mechanism underlying inflammation-induced synaptic alterations. Acta Neuropathol. 2018;135(4):529–50. doi: 10.1007/s00401-017-1803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Waller R, Wyles M, Heath PR, Kazoka M, Wollff H, Shaw PJ, et al. Small RNA sequencing of sporadic amyotrophic lateral sclerosis cerebrospinal fluid reveals differentially expressed miRNAs related to neural and glial activity. Front Neurosci. 2017;11:731. doi: 10.3389/fnins.2017.00731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Saucier D, Wajnberg G, Roy J, Beauregard AP, Chacko S, Crapoulet N, et al. Identification of a circulating miRNA signature in extracellular vesicles collected from amyotrophic lateral sclerosis patients. Brain Res. 2019;1708:100–8. doi: 10.1016/j.brainres.2018.12.016. [DOI] [PubMed] [Google Scholar]
- 191.Banack SA, Dunlop RA, Cox PA. An miRNA fingerprint using neural-enriched extracellular vesicles from blood plasma: towards a biomarker for amyotrophic lateral sclerosis/motor neuron disease. Open Biol. 2020;10(6):200116. doi: 10.1098/rsob.200116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Ananbeh H, Vodicka P, Kupcova Skalnikova H. Emerging roles of exosomes in Huntington’s disease. Int J Mol Sci. 2021;22(8). [DOI] [PMC free article] [PubMed]
- 193.Denis HL, Lamontagne-Proulx J, St-Amour I, Mason SL, Rowley JW, Cloutier N, et al. Platelet abnormalities in Huntington’s disease. J Neurol Neurosurg Psychiatry. 2019;90(3):272–83. doi: 10.1136/jnnp-2018-318854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Denis HL, Lamontagne-Proulx J, St-Amour I, Mason SL, Weiss A, Chouinard S, et al. Platelet-derived extracellular vesicles in Huntington’s disease. J Neurol. 2018;265(11):2704–12. doi: 10.1007/s00415-018-9022-5. [DOI] [PubMed] [Google Scholar]
- 195.Riancho J, Vazquez-Higuera JL, Pozueta A, Lage C, Kazimierczak M, Bravo M, et al. MicroRNA profile in patients with Alzheimer’s disease: analysis of mir-9-5p and miR-598 in raw and exosome enriched cerebrospinal fluid samples. J Alzheimers Dis. 2017;57(2):483–91. doi: 10.3233/JAD-161179. [DOI] [PubMed] [Google Scholar]
- 196.Kumar S, Reddy PH. Are circulating microRNAs peripheral biomarkers for Alzheimer’s disease? Biochim Biophys Acta. 2016;1862(9):1617–27. doi: 10.1016/j.bbadis.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Pegtel DM, Gould SJ, Exosomes Annu Rev Biochem. 2019;88:487–514. doi: 10.1146/annurev-biochem-013118-111902. [DOI] [PubMed] [Google Scholar]
- 198.Isaac R, Reis FCG, Ying W, Olefsky JM. Exosomes as mediators of intercellular crosstalk in metabolism. Cell Metab. 2021;33(9):1744–62. doi: 10.1016/j.cmet.2021.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478). [DOI] [PMC free article] [PubMed]
- 200.Fan RZ, Guo M, Luo S, Cui M, Tieu K. Exosome release and neuropathology induced by alpha-synuclein: new insights into protective mechanisms of Drp1 inhibition. Acta Neuropathol Commun. 2019;7(1):184. doi: 10.1186/s40478-019-0821-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Pinnell JR, Cui M, Tieu K. Exosomes in Parkinson disease. J Neurochem. 2021;157(3):413–28. doi: 10.1111/jnc.15288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Sala M, Hollinger KR, Thomas AG, Dash RP, Tallon C, Veeravalli V, et al. Novel human neutral sphingomyelinase 2 inhibitors as potential therapeutics for Alzheimer’s disease. J Med Chem. 2020;63(11):6028–56. doi: 10.1021/acs.jmedchem.0c00278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Trajkovic K, Hsu C, Chiantia S, Rajendran L, Wenzel D, Wieland F, et al. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science. 2008;319(5867):1244–7. doi: 10.1126/science.1153124. [DOI] [PubMed] [Google Scholar]
- 204.Rohrbough J, Rushton E, Palanker L, Woodruff E, Matthies HJ, Acharya U, et al. Ceramidase regulates synaptic vesicle exocytosis and trafficking. J Neurosci. 2004;24(36):7789–803. doi: 10.1523/JNEUROSCI.1146-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Abdel Shakor AB, Atia M, Alshehri AS, Sobota A, Kwiatkowska K. Ceramide generation during curcumin-induced apoptosis is controlled by crosstalk among Bcl-2, Bcl-xL, caspases and glutathione. Cell Signal. 2015;27(11):2220–30. doi: 10.1016/j.cellsig.2015.07.022. [DOI] [PubMed] [Google Scholar]
- 206.Heras V, Castellano JM, Fernandois D, Velasco I, Rodriguez-Vazquez E, Roa J, et al. Central ceramide signaling mediates obesity-induced precocious puberty. Cell Metab. 2020;32(6):951–66 e958. doi: 10.1016/j.cmet.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 207.Chen X, Wang S, Cao W. Mesenchymal stem cell-mediated immunomodulation in cell therapy of neurodegenerative diseases. Cell Immunol. 2018;326:8–14. doi: 10.1016/j.cellimm.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 208.Chen YA, Lu CH, Ke CC, Chiu SJ, Jeng FS, Chang CW, et al Mesenchymal stem cell-derived exosomes ameliorate Alzheimer’s disease pathology and improve cognitive deficits. Biomedicines. 2021;9(6). [DOI] [PMC free article] [PubMed]
- 209.Katsuda T, Oki K, Ochiya T. Potential application of extracellular vesicles of human adipose tissue-derived mesenchymal stem cells in Alzheimer’s disease therapeutics. Methods Mol Biol. 2015;1212:171–81. doi: 10.1007/7651_2014_98. [DOI] [PubMed] [Google Scholar]
- 210.Katsuda T, Tsuchiya R, Kosaka N, Yoshioka Y, Takagaki K, Oki K, et al. Human adipose tissue-derived mesenchymal stem cells secrete functional neprilysin-bound exosomes. Sci Rep. 2013;3:1197. doi: 10.1038/srep01197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Marques CR, Pereira-Sousa J, Teixeira FG, Sousa RA, Teixeira-Castro A, Salgado AJ. Mesenchymal stem cell secretome protects against alpha-synuclein-induced neurodegeneration in a Caenorhabditis elegans model of Parkinson’s disease. Cytotherapy. 2021;23(10):894–901. doi: 10.1016/j.jcyt.2021.04.002. [DOI] [PubMed] [Google Scholar]
- 212.Kang X, Jiang L, Chen X, Wang X, Gu S, Wang J, et al. Exosomes derived from hypoxic bone marrow mesenchymal stem cells rescue OGD-induced injury in neural cells by suppressing NLRP3 inflammasome-mediated pyroptosis. Exp Cell Res. 2021;405(1):112635. doi: 10.1016/j.yexcr.2021.112635. [DOI] [PubMed] [Google Scholar]
- 213.Wei H, Xu Y, Chen Q, Chen H, Zhu X, Li Y. Mesenchymal stem cell-derived exosomal miR-223 regulates neuronal cell apoptosis. Cell Death Dis. 2020;11(4):290. doi: 10.1038/s41419-020-2490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Lee M, Ban JJ, Yang S, Im W, Kim M. The exosome of adipose-derived stem cells reduces beta-amyloid pathology and apoptosis of neuronal cells derived from the transgenic mouse model of Alzheimer’s disease. Brain Res. 2018;1691:87–93. doi: 10.1016/j.brainres.2018.03.034. [DOI] [PubMed] [Google Scholar]
- 215.Chen HX, Liang FC, Gu P, Xu BL, Xu HJ, Wang WT, et al. Exosomes derived from mesenchymal stem cells repair a Parkinson’s disease model by inducing autophagy. Cell Death Dis. 2020;11(4):288. doi: 10.1038/s41419-020-2473-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Mendes-Pinheiro B, Anjo SI, Manadas B, Da Silva JD, Marote A, Behie LA, et al. Bone marrow mesenchymal stem cells’ secretome exerts neuroprotective effects in a Parkinson’s disease rat model. Front Bioeng Biotechnol. 2019;7:294. doi: 10.3389/fbioe.2019.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Xue C, Li X, Ba L, Zhang M, Yang Y, Gao Y, et al. MSC-derived exosomes can enhance the angiogenesis of human brain MECs and show therapeutic potential in a mouse model of Parkinson’s disease. Aging Dis. 2021;12(5):1211–22. doi: 10.14336/AD.2020.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Teixeira FG, Vilaca-Faria H, Domingues AV, Campos J, Salgado AJ. Preclinical comparison of stem cells secretome and levodopa application in a 6-hydroxydopamine rat model of Parkinson’s disease. Cells. 2020;9(2). [DOI] [PMC free article] [PubMed]
- 219.Bonafede R, Brandi J, Manfredi M, Scambi I, Schiaffino L, Merigo F, et al The anti-apoptotic effect of ASC-exosomes in an in vitro ALS model and their proteomic analysis. Cells. 2019;8(9). [DOI] [PMC free article] [PubMed]
- 220.Bonafede R, Turano E, Scambi I, Busato A, Bontempi P, Virla F, et al ASC-exosomes ameliorate the disease progression in SOD1(G93A) murine model underlining their potential therapeutic use in human ALS. Int J Mol Sci. 2020;21(10). [DOI] [PMC free article] [PubMed]
- 221.Wang SS, Jia J, Wang Z. Mesenchymal stem cell-derived extracellular vesicles suppresses iNOS expression and ameliorates neural impairment in Alzheimer’s disease mice. J Alzheimers Dis. 2018;61(3):1005–13. doi: 10.3233/JAD-170848. [DOI] [PubMed] [Google Scholar]
- 222.Garcia-Contreras M, Thakor AS. Human adipose tissue-derived mesenchymal stem cells and their extracellular vesicles modulate lipopolysaccharide activated human microglia. Cell Death Discov. 2021;7(1):98. doi: 10.1038/s41420-021-00471-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Chierchia A, Chirico N, Boeri L, Raimondi I, Riva GA, Raimondi MT, et al. Secretome released from hydrogel-embedded adipose mesenchymal stem cells protects against the Parkinson’s disease related toxin 6-hydroxydopamine. Eur J Pharm Biopharm. 2017;121:113–20. doi: 10.1016/j.ejpb.2017.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Bonafede R, Scambi I, Peroni D, Potrich V, Boschi F, Benati D, et al. Exosome derived from murine adipose-derived stromal cells: neuroprotective effect on in vitro model of amyotrophic lateral sclerosis. Exp Cell Res. 2016;340(1):150–8. doi: 10.1016/j.yexcr.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 225.Bond AM, Ming GL, Song H. Adult mammalian neural stem cells and neurogenesis: five decades later. Cell Stem Cell. 2015;17(4):385–95. doi: 10.1016/j.stem.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Vogel A, Upadhya R, Shetty AK. Neural stem cell derived extracellular vesicles: attributes and prospects for treating neurodegenerative disorders. EBioMedicine. 2018;38:273–82. doi: 10.1016/j.ebiom.2018.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Webb RL, Kaiser EE, Scoville SL, Thompson TA, Fatima S, Pandya C, et al. Human neural stem cell extracellular vesicles improve tissue and functional recovery in the murine thromboembolic stroke model. Transl Stroke Res. 2018;9(5):530–9. doi: 10.1007/s12975-017-0599-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Apodaca LA, Baddour AAD, Garcia C, Jr, Alikhani L, Giedzinski E, Ru N, et al. Human neural stem cell-derived extracellular vesicles mitigate hallmarks of Alzheimer’s disease. Alzheimers Res Ther. 2021;13(1):57. doi: 10.1186/s13195-021-00791-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Li B, Liu J, Gu G, Han X, Zhang Q, Zhang W. Impact of neural stem cell-derived extracellular vesicles on mitochondrial dysfunction, sirtuin 1 level, and synaptic deficits in Alzheimer’s disease. J Neurochem. 2020;154(5):502–18. doi: 10.1111/jnc.15001. [DOI] [PubMed] [Google Scholar]
- 230.Lee EJ, Choi Y, Lee HJ, Hwang DW, Lee DS. Human neural stem cell-derived extracellular vesicles protect against Parkinson’s disease pathologies. J Nanobiotechnol. 2022;20(1):198. doi: 10.1186/s12951-022-01356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Liu Y, Huber CC, Wang H. Disrupted blood-brain barrier in 5xFAD mouse model of Alzheimer’s disease can be mimicked and repaired in vitro with neural stem cell-derived exosomes. Biochemical and biophysical research communications; 2020. [DOI] [PubMed]
- 232.Zhong D, Cao Y, Li CJ, Li M, Rong ZJ, Jiang L, et al. Neural stem cell-derived exosomes facilitate spinal cord functional recovery after injury by promoting angiogenesis. Exp Biol Med (Maywood) 2020;245(1):54–65. doi: 10.1177/1535370219895491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Henningson CT Jr, Stanislaus MA, Gewirtz AM. 28. Embryonic and adult stem cell therapy. J Allergy Clin Immunol. 2003;111(2 Suppl):S745-753. [DOI] [PubMed]
- 234.Ma K, Deng X, Xia X, Fan Z, Qi X, Wang Y, et al. Direct conversion of mouse astrocytes into neural progenitor cells and specific lineages of neurons. Transl Neurodegener. 2018;7:29. doi: 10.1186/s40035-018-0132-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Xia X, Li C, Wang Y, Deng X, Ma Y, Ding L, et al. Reprogrammed astrocytes display higher neurogenic competence, migration ability and cell death resistance than reprogrammed fibroblasts. Transl Neurodegener. 2020;9:6. doi: 10.1186/s40035-020-0184-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Ma Y, Li C, Huang Y, Wang Y, Xia X, Zheng JC. Exosomes released from neural progenitor cells and induced neural progenitor cells regulate neurogenesis through miR-21a. Cell Commun Signal. 2019;17(1):96. doi: 10.1186/s12964-019-0418-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Ma Y, Xu X, Li C, Wang Y, Zhu J, Xia X, et al Induced neural progenitor cell-derived extracellular vesicles promote neural progenitor cell survival via extracellular signal-regulated kinase pathway. CNS Neurosci Ther. 2021. [DOI] [PMC free article] [PubMed]
- 238.Jarmalaviciute A, Tunaitis V, Pivoraite U, Venalis A, Pivoriunas A. Exosomes from dental pulp stem cells rescue human dopaminergic neurons from 6-hydroxy-dopamine-induced apoptosis. Cytotherapy. 2015;17(7):932–9. doi: 10.1016/j.jcyt.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 239.Yuyama K, Sun H, Sakai S, Mitsutake S, Okada M, Tahara H, et al. Decreased amyloid-beta pathologies by intracerebral loading of glycosphingolipid-enriched exosomes in Alzheimer model mice. J Biol Chem. 2014;289(35):24488–98. doi: 10.1074/jbc.M114.577213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Jarmalaviciute A, Pivoriunas A. Exosomes as a potential novel therapeutic tools against neurodegenerative diseases. Pharmacol Res. 2016;113(Pt B):816–22. doi: 10.1016/j.phrs.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 241.Pardridge WM, Boado RJ. Reengineering biopharmaceuticals for targeted delivery across the blood-brain barrier. Methods Enzymol. 2012;503:269–92. doi: 10.1016/B978-0-12-396962-0.00011-2. [DOI] [PubMed] [Google Scholar]
- 242.Ha D, Yang N, Nadithe V. Exosomes as therapeutic drug carriers and delivery vehicles across biological membranes: current perspectives and future challenges. Acta Pharm Sin B. 2016;6(4):287–96. doi: 10.1016/j.apsb.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Lai CP, Breakefield XO. Role of exosomes/microvesicles in the nervous system and use in emerging therapies. Front Physiol. 2012;3:228. doi: 10.3389/fphys.2012.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Zhuang X, Xiang X, Grizzle W, Sun D, Zhang S, Axtell RC, et al. Treatment of brain inflammatory diseases by delivering exosome encapsulated anti-inflammatory drugs from the nasal region to the brain. Mol Ther. 2011;19(10):1769–79. doi: 10.1038/mt.2011.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29(4):341–5. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 246.Kojima R, Bojar D, Rizzi G, Hamri GC, El-Baba MD, Saxena P, et al. Designer exosomes produced by implanted cells intracerebrally deliver therapeutic cargo for Parkinson’s disease treatment. Nat Commun. 2018;9(1):1305. doi: 10.1038/s41467-018-03733-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Cooper JM, Wiklander PB, Nordin JZ, Al-Shawi R, Wood MJ, Vithlani M, et al. Systemic exosomal siRNA delivery reduced alpha-synuclein aggregates in brains of transgenic mice. Mov Disord. 2014;29(12):1476–85. doi: 10.1002/mds.25978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Didiot MC, Hall LM, Coles AH, Haraszti RA, Godinho BM, Chase K, et al. Exosome-mediated delivery of hydrophobically modified siRNA for huntingtin mRNA silencing. Mol Ther. 2016;24(10):1836–47. doi: 10.1038/mt.2016.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Izco M, Blesa J, Schleef M, Schmeer M, Porcari R, Al-Shawi R, et al. Systemic exosomal delivery of shRNA minicircles prevents parkinsonian pathology. Mol Ther. 2019;27(12):2111–22. doi: 10.1016/j.ymthe.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Maheshwari R, Tekade M, Gondaliya P, Kalia K, D’Emanuele A, Tekade RK. Recent advances in exosome-based nanovehicles as RNA interference therapeutic carriers. Nanomed (Lond) 2017;12(21):2653–75. doi: 10.2217/nnm-2017-0210. [DOI] [PubMed] [Google Scholar]
- 251.Jahangard Y, Monfared H, Moradi A, Zare M, Mirnajafi-Zadeh J, Mowla SJ. Therapeutic effects of transplanted exosomes containing miR-29b to a rat model of Alzheimer’s disease. Front Neurosci. 2020;14:564. doi: 10.3389/fnins.2020.00564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Zhai L, Shen H, Sheng Y, Guan Q. ADMSC Exo-MicroRNA-22 improve neurological function and neuroinflammation in mice with Alzheimer’s disease. J Cell Mol Med. 2021;25(15):7513–23. doi: 10.1111/jcmm.16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Li Q, Wang Z, Xing H, Wang Y, Guo Y. Exosomes derived from mir-188-3p-modified adipose-derived mesenchymal stem cells protect Parkinson’s disease. Mol Ther Nucleic Acids. 2021;23:1334–44. doi: 10.1016/j.omtn.2021.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Haney MJ, Klyachko NL, Zhao Y, Gupta R, Plotnikova EG, He Z, et al. Exosomes as drug delivery vehicles for Parkinson’s disease therapy. J Control Release. 2015;207:18–30. doi: 10.1016/j.jconrel.2015.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Qu M, Lin Q, Huang L, Fu Y, Wang L, He S, et al. Dopamine-loaded blood exosomes targeted to brain for better treatment of Parkinson’s disease. J Control Release. 2018;287:156–66. doi: 10.1016/j.jconrel.2018.08.035. [DOI] [PubMed] [Google Scholar]
- 256.Wu XY, Liao BY, Xiao D, Wu WC, Xiao Y, Alexander T, et al. Encapsulation of bryostatin-1 by targeted exosomes enhances remyelination and neuroprotection effects in the cuprizone-induced demyelinating animal model of multiple sclerosis. Biomater Sci. 2022;10(3):714–27. doi: 10.1039/D1BM01142A. [DOI] [PubMed] [Google Scholar]
- 257.Xiao Y, Zhang Y, Gao YH, Zhao ZH, He J, Gao R, et al. A targeted extracellular vesicles loaded with montelukast in the treatment of demyelinating diseases. Biochem Biophys Res Commun. 2022;594:31–7. doi: 10.1016/j.bbrc.2022.01.051. [DOI] [PubMed] [Google Scholar]
- 258.Li Z, Liu F, He X, Yang X, Shan F, Feng J. Exosomes derived from mesenchymal stem cells attenuate inflammation and demyelination of the central nervous system in EAE rats by regulating the polarization of microglia. Int Immunopharmacol. 2019;67:268–80. doi: 10.1016/j.intimp.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 259.Mianehsaz E, Mirzaei HR, Mahjoubin-Tehran M, Rezaee A, Sahebnasagh R, Pourhanifeh MH, et al. Mesenchymal stem cell-derived exosomes: a new therapeutic approach to osteoarthritis? Stem Cell Res Ther. 2019;10(1):340. doi: 10.1186/s13287-019-1445-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Batrakova EV, Kim MS. Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release. 2015;219:396–405. doi: 10.1016/j.jconrel.2015.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Terstappen GC, Meyer AH, Bell RD, Zhang W. Strategies for delivering therapeutics across the blood-brain barrier. Nat Rev Drug Discov. 2021;20(5):362–83. doi: 10.1038/s41573-021-00139-y. [DOI] [PubMed] [Google Scholar]
- 262.Tian T, Zhang HX, He CP, Fan S, Zhu YL, Qi C, et al. Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials. 2018;150:137–49. doi: 10.1016/j.biomaterials.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 263.Lorca C, Laparra M, Cespedes MV, Casani L, Florit S, Jove M, et al Industrial By-products as a novel circular source of biocompatible extracellular vesicles. Adv Funct Mater. 2022;32(29).
- 264.Ding S, Khan AI, Cai X, Song Y, Lyu Z, Du D, et al. Overcoming blood-brain barrier transport: advances in nanoparticle-based drug delivery strategies. Mater Today (Kidlington) 2020;37:112–25. doi: 10.1016/j.mattod.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Salinas S, Schiavo G, Kremer EJ. A hitchhiker’s guide to the nervous system: the complex journey of viruses and toxins. Nat Rev Microbiol. 2010;8(9):645–55. doi: 10.1038/nrmicro2395. [DOI] [PubMed] [Google Scholar]
- 266.Kumar P, Wu H, McBride JL, Jung KE, Kim MH, Davidson BL, et al. Transvascular delivery of small interfering RNA to the central nervous system. Nature. 2007;448(7149):39–43. doi: 10.1038/nature05901. [DOI] [PubMed] [Google Scholar]
- 267.Hao Y, Su C, Liu X, Sui H, Shi Y, Zhao L. Bioengineered microglia-targeted exosomes facilitate Abeta clearance via enhancing activity of microglial lysosome for promoting cognitive recovery in Alzheimer’s disease. Biomater Adv. 2022;136:212770. doi: 10.1016/j.bioadv.2022.212770. [DOI] [PubMed] [Google Scholar]
- 268.Saint-Pol J, Gosselet F, Duban-Deweer S, Pottiez G, Karamanos Y. Targeting and crossing the blood-brain barrier with Extracellular vesicles. Cells. 2020;9(4). [DOI] [PMC free article] [PubMed]
- 269.Chen CC, Liu L, Ma F, Wong CW, Guo XE, Chacko JV, et al. Elucidation of exosome migration across the blood-brain barrier model in vitro. Cell Mol Bioeng. 2016;9(4):509–29. doi: 10.1007/s12195-016-0458-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Fu SY, Wang Y, Xia XH, Zheng JLC. Exosome engineering: current progress in cargo loading and targeted delivery. Nanoimpact. 2020;20.
- 271.Das CK, Jena BC, Banerjee I, Das S, Parekh A, Bhutia SK, Mandal M. Exosome as a novel shuttle for delivery of therapeutics across biological barriers. Mol Pharm. 2019;16(1):24–40. doi: 10.1021/acs.molpharmaceut.8b00901. [DOI] [PubMed] [Google Scholar]
- 272.Alvarez-Erviti L, Seow Y, Schapira AH, Rodriguez-Oroz MC, Obeso JA, Cooper JM. Influence of microRNA deregulation on chaperone-mediated autophagy and alpha-synuclein pathology in Parkinson’s disease. Cell Death Dis. 2013;4:e545. doi: 10.1038/cddis.2013.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Hong Y, Zhao T, Li XJ, Li S. Mutant huntingtin inhibits alphab-crystallin expression and impairs exosome secretion from astrocytes. J Neurosci. 2017;37(39):9550–63. doi: 10.1523/JNEUROSCI.1418-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.