Abstract
Cardiovascular disease is a leading cause of morbidity and mortality. Oral health is associated with smoking and cardiovascular outcomes, but there are gaps in knowledge of many mechanisms connecting smoking to cardiovascular risk. Therefore, the aim of this review is to synthesize literature on smoking and the oral microbiome, and smoking and cardiovascular risk/disease, respectively. A secondary aim is to identify common associations between the oral microbiome and cardiovascular risk/disease to smoking, respectively, to identify potential shared oral microbiome-associated mechanisms. We identified several oral bacteria across varying studies that were associated with smoking. Atopobium, Gemella, Megasphaera, Mycoplasma, Porphyromonas, Prevotella, Rothia, Treponema, and Veillonella were increased, while Bergeyella, Haemophilus, Lautropia, and Neisseria were decreased in the oral microbiome of smokers versus non-smokers. Several bacteria that were increased in the oral microbiome of smokers were also positively associated with cardiovascular outcomes including Porphyromonas, Prevotella, Treponema, and Veillonella. We review possible mechanisms that may link the oral microbiome to smoking and cardiovascular risk including inflammation, modulation of amino acids and lipids, and nitric oxide modulation. Our hope is this review will inform future research targeting the microbiome and smoking-related cardiovascular disease so possible microbial targets for cardiovascular risk reduction can be identified.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12967-022-03785-x.
Keywords: Oral microbiome, Microbiota, Oral health, Genetics, Smoking, Cardiovascular risk, Cardiovascular disease
Cardiovascular disease (CVD) greatly increases morbidity and mortality, and contributed to approximately 18.6 million global deaths in 2019 [1]. Data from epidemiological studies show strong links between smoking and CVD, and smoking is directly associated with nearly 20 percent of deaths from CVD [2]. It has been established that smoking is a main modifiable risk factor in developing early atherosclerosis, CVD, and death. Smoking leads to increased systemic inflammation, platelet activation, and dysregulation of vascular smooth muscle control, thus affecting the cardiovascular system [3]. The paired endothelial and vascular dysfunction and platelet/clotting abnormalities create a pro-atherogenic environment in which stable and unstable plaques can develop. The development of atherosclerotic plaque leads to various types of CVD-related morbidity, including myocardial infarction, stroke, and congestive heart failure. Periodontitis, a condition associated with cardiovascular risk and CVD [4–6], occurs at significantly higher rates in subjects who smoke cigarettes [7]. Periodontitis is associated with characteristic bacterial alterations and local inflammatory responses [8], but the documented connection of periodontitis to systemic inflammation suggests local disruptions in oral bacteria may have implications that reach beyond the oral environment [9, 10].
The human microbiome is defined as the collection of bacteria (and their genes) that inhabit and coexist within humans. These bacteria play an integral role in vital physiologic processes such as metabolite production through fermentation of complex carbohydrates, modulation of host immune responses, and regulation of lipid metabolism [11, 12]. Since the development of the Human Microbiome Project, the role of the human microbiome in the maintenance of health and several physiological processes has been of great interest [13], including those associated with cardiovascular health [14]. Several internal and external factors, including diet and smoking, influence the structure and function of these microbial communities [15, 16]. Alteration in bacterial composition of microbiome communities across body sites have been associated with several diseases, including hypertension, obesity, hyperlipidemia and alcohol use disorder [17–20]. There are mechanisms linking the microbiome to CVD, although most of this research focuses on the gut microbiome and researchers understand less about the interaction between bacterial communities of the oral environment and host physiology [20, 21].
The oral cavity is a highly complex, open ecosystem with several microenvironments [22]. Bacterial species colonize the mouth in organized communities called biofilms that are in continual interface with the external environment and host immune system through the oral mucosal epithelium [23]. These biofilms pose advantages to bacteria of the oral microbiome by increasing bacteria-specific nutrient availability and providing protection from environmental or physiologic stressors [24]. Importantly, the structure and composition of oral microbiome biofilms varies across oral sampling sites [25]. Mucosal oral surfaces with high cellular turnover have largely different characteristics versus non-mucosal surfaces (e.g. teeth), despite their close proximity within the oral cavity. Furthermore, the mucosal and non-mucosal microenvironments of the mouth have significant differences in oxygen exposure, pH, and temperature, creating favorable growing conditions for different species of bacteria. Each oral microenvironment, i.e., the subgingival sulcus, tongue dorsum, buccal mucosa and saliva, has distinct but temporally stable bacterial populations that may have disparate responses to smoking exposure.
Importantly, the oral cavity is exposed to different chemicals and substances when e-cigarette vapor versus tobacco smoke is inhaled. For example, cigarette smoking exposes the oral environment to irritants, chemicals, and carcinogens through incomplete combustion byproducts, including polycyclic aromatic hydrocarbons and nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone, along with carbon monoxide [26]. Electronic-cigarette (e-cigarette) use, originally proposed as a safer alternative to cigarette smoking, results in oral exposure to nicotine dissolved in solvents including alcohols, glycerin, propylene glycol, and propylene oxide through the inhalation of aerosols [27]. In e-cigarettes, levels of volatile organic compounds, nitrosamines, aldehydes, and metals vary considerably across different brands making understanding the link between aerosol inhalation and oral chemical exposure difficult [28]. Both cigarette and e-cigarette smoking have been shown to alter the oral environment by decreasing saliva volumes, increasing saliva viscosity, destroying protective salivary macromolecules and triggering inflammatory responses and chronic inflammation [29–31].
Potential mechanisms between oral microbes, smoking, and cardiovascular conditions are largely unexplored. The physiologic implications of many of the chemicals present in cigarette smoke are historically understudied, and even less is known about how the oral microbiome may modulate interactions between cigarette smoke versus e-cigarette vapor and human physiology. The circulatory system provides a route where the bacteria of the oral microbiome may influence CVD risk. Each tooth has a blood supply, and byproducts of oral bacterial metabolism can produce metabolites or endotoxins that migrate into the bloodstream, causing systemic inflammation that affects other parts of the body [32]. This is a potential mechanism, but the specific pathways linking smoking to CVD through the oral microbiome are still unknown. As the oral cavity and its associated microbial communities are the first contact with inhaled cigarette smoke, responses of the oral microbial taxa to smoke products and subsequent implications for health are important to elucidate. Therefore, this manuscript reviews associations between the oral microbiome and smoking, and the oral microbiome and CVD, focusing on shared associations and potential oral microbial-mediated mechanisms linking smoking to CVD risk.
In collaboration with our institutional biomedical librarian, PubMed was searched for primary literature to yield sources focused on smoking and the oral microbiome, and smoking and cardiovascular risk or disease, respectively. Please see Additional file 1 for search terms, combinations and strategy used in the PubMed searches for primary literature source data acquisition.
Cigarette smoking and oral microbiome compositional changes
As the oral microbial communities exist in an intricate and coordinated ecosystem, changes in the oral environment result in adaptation and shifts in which bacteria thrive based on their phenotypic and colony characteristics. Several factors are known to modify the oral environment and influence the composition of the oral microbiome as a result. Factors (both internal and external) such as diet, certain medications, smoking, moisture of the environment, and periodontal disease status alter the amount and composition of saliva, which impacts the surrounding epithelial tissues and oral cavity [33]. As previously mentioned, cigarette smoking exposes the oral environment to irritants, chemicals, and carcinogens [26], and alters the oral environment promoting inflammatory responses [29–31]. Since niche-specific colonization exists in the oral cavity, we will review the associations between smoking and the oral microbiome across different sites: whole mouth, saliva, tongue dorsum, supragingival plaque, and subgingival plaque (see Table 1 for a list of studies that evaluated associations between smoking and the oral microbiome). The relationship between smoking and alpha diversity was greatly heterogenous across studies. Alpha diversity is defined as microbial diversity within an individual sample, and is often used as a global indicator of the bacterial characteristics within a microbiome sampling site [22]. Smoking was associated with an increased alpha diversity of whole mouth [34], buccal mucosa [35], and saliva [36, 37] samples in some research, while other studies reported decreased alpha diversity in whole mouth [38], saliva [39, 40] and tongue dorsum [41] samples in smokers versus non-smokers. Additionally, smoking was associated with decreased alpha diversity of subgingival samples of patients with and without chronic periodontal disease [42]. Other groups reported no differences in alpha diversity of whole mouth (via mouthwash) [43], buccal [44], tongue dorsum [45] and saliva [45, 46] samples of smokers, compared to non-smokers.
Table 1.
Included studies examining the association between smoking and the oral microbiome
| Author, year | Oral sample site | Aim | Population studied | Sequencing | Region if 16S | Citation |
|---|---|---|---|---|---|---|
| Cigarette smokers | ||||||
| Al-Zyoud et al., 2019 | Saliva | Investigate the shift in the salivary microbiota between smokers and non-smokers in Jordan | Nonsmoking subjects (n = 51), subjects who smoke (n = 49), total sample (n = 100) | 16S | V3–V4 | [37] |
| Beghini et al., 2019 | Oral rinse | To evaluate the effect of tobacco exposure on the oral microbiome from oral rinse samples in the 2013–14 New York City Health and Nutrition Examination Study | Total sample (n = 259) | 16S | V4 | [43] |
| Coretti et al., 2017 | Subgingival | Assess the subgingival microbiota in smoker patients with chronic periodontitis, non‑smoker patients with chronic periodontitis and healthy controls | Subjects with chronic periodontitis who smoke (n = 6), non‑smoker patients with chronic periodontitis (n = 6), nonsmoking subjects without periodontitis (n = 8), total sample (n = 20) | 16S | V3–V4 | [42] |
| Duan et al., 2017 | Saliva | Studied the impact of smoking on the salivary microbiome and its further influence on marginal bone loss around an implant during a 3-month bone-healing period | Smokers (n = 10) and non-smokers (n = 10) presenting for single-tooth replacement, total sample (n = 20) | 16S | V4 | [39] |
| Gaetti-Jardim, 2018 | Supra- and sub-gingival plaque | Aimed to evaluate the effects of conventional radiotherapy on the prevalence and populations of oral microorganisms in head and neck cancer patients who did not receive adequate preventive dental care | Subjects with head and neck cancer (n = 28) | Culture dependent | N/A | [56] |
| Ganesan et al., 2017 | Subgingival plaque | Analyzed 16S sequences from non-smoking normoglycemic individuals (controls), smokers, diabetics and diabetic smokers with periodontitis, as well as periodontally healthy controls, smokers and diabetics to assess subgingival bacterial biodiversity and co-occurrence patterns | Normoglycemic non-smokers with periodontitis (n = 14), hyperglycemic non-smokers with periodontitis (n = 9), normoglycemic smokers with periodontitis (n = 16), and hyperglycemic smokers with periodontitis (n = 8), normoglycemic non-smokers without periodontitis (n = 14), hyperglycemic non-smokers without periodontitis (n = 12), normoglycemic smokers without periodontitis (n = 12), total sample (n = 175) | 16S | V1–V3; V7–V9 | [58] |
| Gopinath et al., 2022 | Buccal swab | Investigate the compositional and functional attributes of the oral bacteriome of smokeless tobacco users and smokers relative to controls by 16S rRNA metagenomic sequencing in an Indian population | Smokers (n = 17), smokeless tobacco users (n = 14), age-matched non-smokers (n = 13), total sample (n = 44) | 16S | V3–V4 | [35] |
| Hsiao et al., 2018 | Saliva | Investigated the association between oral bacterial profile and oral squamous cell carcinoma risk in a case–control study | Subjects with oral squamous cell carcinoma (n = 138), controls (n = 151), total sample (n = 289) | 16S | V3–V5 | [54] |
| Jia et al., 2021 | Saliva | Improve our understanding of the impact of cigarette smoking on the oral microbiota in the Chinese population | Subjects from Guangdong Providence (n = 150), subjects from Yangquan city (n = 81), subjects from Mishan city (n = 85), total sample (n = 316) | 16S | V4 | [36] |
| Karabudak et al., 2019 | Buccal swab | Investigate the effect of smoking on the buccal microbiome and to analyze the descriptive ability of each of the seven hypervariable regions in their 16S rRNA genes | Smokers (n = 20), non-smokers (n = 20), total sample (n = 40) | 16S | V2, V3, V4, V6–7, V8, V9 | [44] |
| Karasneh et al., 2017 | Subgingival plaque | Investigate the impact of smoking on the subgingival bacterial profile in both healthy adults and chronic periodontitis patients | Subjects with chronic periodontitis (n = 37 non-smokers and n = 18 smokers), subjects without periodontitis (37 non-smokers and 18 smokers), total sample (n = 94) | 16S | V1–V9 | [59] |
| Lin et al., 2019 | Saliva | Leveraged next generation sequencing for microbiome and functional neuroimaging to enable the delineation of microbiome-brain network links as well as their relationship to cigarette smoking | Smokers (n = 30), non-smokers (n = 30), total sample (n = 60) | 16S | V4 | [52] |
| Mukherjee et al., 2018 | Oral rinse | Assessed the relationship of microbial dysbiosis with smoking and markers of human immunodeficiency virus disease | HIV-infected smokers (n = 48), HIV-infected non-smokers (n = 24), HIV-uninfected smokers (n = 24), total sample (n = 96) | 16S | V4 | [50] |
| Murugesan et al., 2020 | Saliva | Characterize the salivary microbiome composition in the Qatari population, and to explore specific microbial signatures that can be associated with various lifestyles and different oral conditions | Total sample (n = 997) | 16S | V1–V3 | [40] |
| Pushalkar et al., 2020* | Saliva | Evaluate the effects of e-cigarette aerosol and its influence on human salivary microbiome and immune health. Additionally, the authors evaluate the influence of e-cigarette aerosols on infection efficiency of oral pathogens in pre-cancerous and cancer cell lines using a novel e-cigarette aerosol-generating machine and pro-inflammatory immune mediators | Smokers (n = 40), never smokers (n = 39), e-cigarette users (n = 40), total sample (n = 119) | 16S | V3–V4 | [46] |
| Renson et al., 2019 | Oral rinse | Describe sociodemographic variation of oral microbiomes in a subsample of the 2013–14 population-based New York City Health and Nutrition Examination Study | Total sample (n = 282) | 16S | V4 | [47] |
| Rodríguez- Rabassa et al., 2018 | Saliva | Investigated the effects of cigarette smoking on bacterial diversity and host responses compared to non-smokers | Non-smokers (n = 16), current smokers (n = 18), total sample (n = 34) | 16S | V3–V4 | [51] |
| Sato et al., 2020a | Tongue dorsum | Investigated the bacterial species composition in the tongue microbiome, as well as single-nucleotide variant profiles and gene content of these species, in never and current smokers by utilizing metagenomic sequences | Never smokers (n = 234), current smokers (n = 52), total sample (n = 286) | Shotgun metagenomic sequencing | N/A | [55] |
| Sato et al., 2020b | Tongue dorsum | Used 16S rRNA amplicon sequencing of tongue-coating samples obtained from East Asian subjects who were current, former, or never smokers to identify differences in their tongue microbiomes and related metagenomic functions | Never smokers (n = 384), former smokers (n = 129), current smokers (n = 144), total sample (n = 657) | 16S | V3–V4 | [41] |
| Shay et al., 2020 | Oral rinse | Characterize the bacteriome, mycobiome and mycobiome-bacteriome interactions of oral wash samples in head and neck squamous cell carcinoma patients and to determine if they are distinct from those of the oral wash of matched non-head and neck squamous cell carcinoma patients | Subjects with head and neck squamous cell carcinoma (n = 46), subjects without cancer (n = 46), total sample (n = 92) | 16S | V1–V2 | [49] |
| Suzuki et al., 2022 | Saliva and tongue dorsum | Investigated the differences in the microbial composition of the tongue directly exposed to cigarette smoke in smokers with that of nonsmokers | Saliva (n = 47) and tongue dorsum (n = 50) samples of healthy volunteers, total sample (n = 50) | 16S | V3–V4 | [45] |
| Thomas et al., 2014 | Oral biofilm/whole mouth swab | Investigate the effects of the chronic use of alcohol and tobacco over the oral microbiome, in terms of diversity and composition, using 16S rRNA gene sequencing | Subjects with no alcohol or tobacco consumption (n = 9); subjects with heavy alcohol and tobacco consumption (n = 7), subjects who smoke but do not consume alcohol (n = 6), total sample (n = 22) | 16S | V1 | [38] |
| Vallès et al., 2018 | Oral rinse | Compared the effects of cigarette, dokha and shisha use on community composition of the oral microbiome by high-throughput sequencing of the bacterial 16S rRNA gene in 330 participants from the “UAE Healthy Future” pilot study | Subjects who smoke (n = 105), subjects who do not smoke (n = 225), total sample (n = 330) | 16S | V4 | [34] |
| Wolff et al., 2019 | Supragingival plaque | Study patterns in pathogenic biofilm composition to characterize the oral microbiome present in tooth surfaces with and without caries. Smoking and socio-economic status were studied as exploratory variables | Total sample (n = 56) | 16S | V4 | [57] |
| Yeo et al., 2019 | Saliva | Address the gap in knowledge by reporting on the anthropometrics and cardiometabolic health of a resettled Temiar community and investigated their saliva microbiome in association with their health | Total sample (n = 72) | 16S | V3–V4 | [53] |
| Yeoh et al., 2019 | Oral rinse | Collected oral rinse samples from patients showing symptoms of acute tonsillitis and compared their oral cavity microbial community composition to healthy individuals without oral disease | Healthy (n = 165), tonsillitis (n = 43), total sample (n = 208) | 16S | V3–V4 | [48] |
| E-cigarette smokers | ||||||
| Ganesan et al., 2020 | Subgingival plaque | Investigate the effects of e-cigarettes on the subgingival microbiome using complementary approaches to achieve comprehensive insights into community assembly, dynamics, and function, as well as the impact of this community on the host’s immunoinflammatory response | Smokers (n = 25), non-smokers (n = 25), e-cigarette users (n = 20), former smokers currently using e-cigarettes (n = 25), concomitant cigarette and e-cigarette users (n = 28), total sample (n = 123) | Shotgun metagenomic sequencing | N/A | [15] |
| Pushalkar, 2020* | Saliva | Study the in vivo effects of e-cigarette aerosol and its influence Additionally, the authors evaluated the influence of e-cigarette aerosols on infection efficiency of oral pathogens in pre-cancerous and cancer cell lines using a novel e-cigarette aerosol-generating machine and pro-inflammatory immune mediators | Smokers (n = 40), never smokers (n = 39), e-cigarette users (n = 40), total sample (n = 119) | 16S | V3–V4 | [46] |
16S 16S ribosomal ribonucleic acid sequencing, HIV human immunodeficiency virus, V variable region of the 16S ribosomal ribonucleic acid gene
*Denotes study included comparisons with both cigarette and e-cigarette smokers
Whole mouth, saliva and buccal mucosa
Researchers collected whole mouth samples by swabbing multiple surfaces of the mouth [38] or collecting an alcohol- [43, 47–50] or saline-based [34] mouthwash to analyze microbial populations across multiple oral microenvironments. Similar to whole mouth samples, saliva microbiome composition may be influenced by other oral microbial niches, but sample collection occurred through spontaneous passive [36, 37, 39, 40, 45, 51–54] or stimulated [46] salivary fluid collection in the reviewed studies. In saliva or buccal mucosa samples of cigarette smokers, the majority of studies demonstrated an increased relative abundance (RA) of Actinomyces [36, 37, 48], Actinomyces species [46, 52], Aggregatibacter [53], Bacteroides [52], and Lachnoanaerobaculum [39] versus non-smokers. Cigarette smoking also increased the RA of Alloprevotella species [39], Campylobacter [36, 43, 53], Dialister [34], Eubacterium [52] and Eubacterium species [39, 52] in saliva and whole mouth samples versus subjects who did not smoke. Conversely, several studies reported a decreased RA of Acinetobacter species [39], Bifidobacterium [47], Catonella [39], Capnocytophaga [40, 45], Cardiobacterium [36, 45], Granulicatella [38, 48, 51], Lactococcus [40, 47], Leptotrichia [34, 48, 49, 51], Pseudomonas orientalis [39], Selenomonas [39, 52], and Selenomonas species [39] in saliva and whole mouth samples of cigarette smokers versus non-smokers. The RA of Actinobacillus had different associations with cigarette smoking, where the RA of Actinobacillus was increased in saliva samples [51] but decreased in whole mouth samples [34, 47] in cigarette smokers (versus non-smokers). There were also conflicting results on the influence of cigarette smoking on the RA of Fusobacterium and Fusobacterium species in the whole mouth, buccal mucosa and saliva samples. For example, several studies reported both an increased RA of genus-level Fusobacterium and Fusobacterium species (specifically F. nucleatum; [35, 46, 48, 52, 54]) and decreased RA of Fusobacterium and Fusobacterium species (specifically F. periodonticum; [34, 37, 46, 49, 51]) in cigarette smokers versus non-smokers (see Additional file 2: Table S1 for all smoking-associated oral bacteria responses in the reviewed studies).
Tongue dorsum
Two studies by the same group [41, 55] explored the impact of smoking on the oral microbiome using tongue dorsum samples. These studies reported that cigarette smoking was associated with a decrease in the RA of Alloprevotella, Campylobacter, Cardiobacterium, Capnocytophaga, Fusobacterium, Eubacterium, and Lachnoanaerobaculum versus non-smoking subjects [41]. Two independent groups reported that smoking was associated with a decrease in Peptostreptococcus and Catonella in tongue dorsum samples, compared to non-smokers [41, 45]. Cigarette smoking was also associated with an increased RA of species-level Eubacterium brachy, Eubacterium nodatum, Eubacterium saphenum, Filifactor alocis, Fusobacterium nucleatum, and Mogibacterium timidum in tongue dorsum samples compared to non-smokers [41, 55].
Supragingival and subgingival plaque
Supragingival and subgingival plaque samples were collected by soft tissue removal [42] or by biofilm [56, 57] and direct plaque [58, 59] collection using sterilized paper points in patients with and without periodontal disease, depending on the study design (Table 1). Cigarette smoking was associated with an increased RA of Bifidobacterium [42, 58] and Campylobacter rectus [59], Eikenella corrodens [59], Fusobacterium [42], Granulicatella [42], and Selenomonas sputigena [59] in subgingival plaque samples and an increased RA of Haemophilus parainfluenzae [57] in supragingival samples versus non-smoking subjects. Conversely, the RA of Capnocytophaga ochracea [59] and Pseudomonas [42] in subgingival plaque samples were decreased in cigarette smokers versus non-smokers.
Similar bacterial associations across multiple sites
Specific bacterial taxa had similar associations with cigarette smoking in multiple oral microbiome sampling sites (i.e. a shared increase or decrease in RA in response to cigarette smoking in more than one oral microbiome site; Table 2 and Fig. 1A). For example, cigarette smoking was associated with an increased RA of Atopobium and Atopobium species [34, 36, 37, 41, 45, 55, 58], Rothia and Rothia species [36, 38, 41, 44, 46, 52, 55], Lactobacillus [50, 58], Mycoplasma and Mycoplasma hyosynoviae [34, 41, 52], Megasphaera and Megasphaera micronuciformis [34, 36, 37, 39, 41, 43, 46, 55], Tannerella and Tannerella forsythia [39, 41, 52], Corynebacterium and Corynebacterium species [41, 57], Prevotella and Prevotella species [34, 36–40, 44, 46, 52, 55], Streptococcus and Streptococcus species [41, 44, 55, 58], Porphyromonas and Porphyromonas species [34, 46, 55], Treponema and Treponema species [34, 42, 45, 48, 52, 55, 59], and Veillonella or Veillonella species [36–38, 43, 44, 46, 48, 50, 55, 58], compared to non-smokers. Interestingly, the RA of Lactobacillus and Rothia were also increased in subjects exposed to secondhand smoke [47]. Cigarette smoking was associated with a decreased RA of Gemella [37, 38, 40, 41, 43, 45, 47], Haemophilus and H. haemolyticus [34, 37, 41, 43, 45, 47, 55], Neisseria and Neisseria species [34, 36–38, 41, 43, 47, 50, 52, 53, 55, 58], Bergeyella [37, 43, 47, 48], Oribacterium and Oribacterium species [39, 41, 46, 52], Lautropia and L. mirabilis [34, 36, 37, 41–43, 47, 52, 55, 58] in most oral sites versus subjects who did not smoke. An exception to the previous inverse association between bacterial RA and cigarette or e-cigarette smoking was an increased RA of L. mirabilis in supragingival [57] samples and increased Oribacterium in the whole mouth [48] and subgingival plaque [42] samples in smokers compared to non-smokers. Additionally, in cigarette smokers (versus non-smokers), the RA of Actinobacillus was increased in saliva samples [51] but decreased in whole mouth samples [34, 47]. Not all taxa had agreement across studies when reporting the association between RA and cigarette smoking. For example, in the whole mouth and saliva samples, there were almost an equal number of studies reporting a decreased [40, 43, 49, 51] and increased [37–39, 46, 49] RA of Streptococcus or Streptococcus species, and the association between smoking and Prevotella RA was equivocal in subgingival plaque samples, with one study reporting an increase [58] and the other a decrease [59] in RA versus non-smoking subjects. Current cigarette use was associated with a decreased RA of Bergeyella, Haemophilus, Lautropia, and Neisseria compared to former smokers in whole mouth samples [47], indicating that abstinence from smoking might reverse the smoking-associated decrease in RA of these taxa.
Table 2.
Bacteria of the oral microbiome with similar responses to smoking across multiple sites
| Bacteria | Whole mouth | Saliva | Tongue dorsum | Subgingival plaquea | Buccal | References |
|---|---|---|---|---|---|---|
| Atopobium and Atopobium species | ↑ | ↑ | ↑ | ↑ | [34, 36, 37, 41, 45, 55, 58] | |
| Bergeyella | ↓ | ↓ | [37, 43, 47, 48] | |||
| Corynebacterium and Corynebacterium species | ↑ | ↑ | [41, 57] | |||
| Gemella | ↑ | ↑ | ↑ | [37, 38, 40, 41, 43, 45, 47] | ||
| Haemophilus and H. haemolyticus | ↓ | ↓ | ↓ | [34, 37, 41, 43, 45, 47, 55] | ||
| Lactobacillus | ↑ | ↑ | [50, 58] | |||
| Lautropia and Lautropia mirabilis | ↓ | ↓ | ↓ | ↓↑b | [34, 36, 37, 41–43, 47, 52, 55, 57, 58] | |
| Megasphaera and Megasphaera micronuciformis | ↑ | ↑ | ↑ | [34, 36, 37, 39, 41, 43, 46, 55] | ||
| Mycoplasma and Mycoplasma hyosynoviae | ↑ | ↑ | ↑ | [34, 41, 52] | ||
| Neisseria and Neisseria species | ↓ | ↓ | ↓ | ↓ | [34, 36–38, 41, 43, 47, 50, 52, 53, 55, 58] | |
| Oribacterium and Oribacterium species | ↑ | ↓ | ↓ | ↑ | [39, 41, 42, 46, 48, 52] | |
| Peptococcus | ↓ | ↓ | [36, 41] | |||
| Porphyromonas and Porphyromonas species | ↑ | ↑ | ↑ | [34, 46, 55] | ||
| Prevotella and Prevotella species | ↑ | ↑ | ↑ | ↑↓b | ↑ | [34, 36–40, 44, 46, 52, 55, 58, 59] |
| Rothia and Rothia species | ↑ | ↑ | ↑ | ↑ | [36, 38, 41, 44, 46, 52, 55] | |
| Streptococcus and Streptococcus species | ↑↓b | ↑↓b | ↑ | ↑ | ↑ | [37–41, 43, 44, 46, 49, 51, 55, 58] |
| Tannerella and Tannerella forsythia | ↑ | ↑ | [39, 41, 52] | |||
| Treponema and Treponema species | ↑ | ↑ | ↑ | ↑ | [34, 42, 45, 48, 52, 55, 59] | |
| Veillonella and Veillonella species | ↑ | ↑ | ↑ | ↑ | ↑ | [15, 36–38, 43, 44, 46, 48, 50, 55, 58] |
aSubgingival and/or supragingival plaque
bEqual number of studies reporting an increased or decreased relative abundance of bacterial taxa in association with smoking
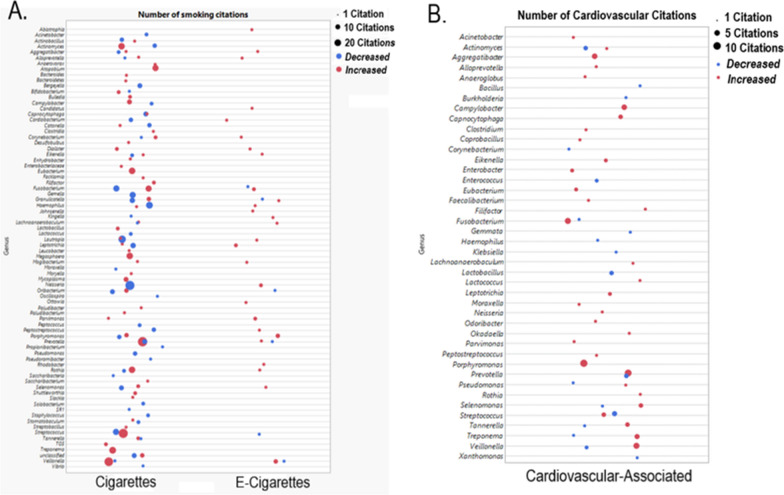
Fig. 1.
A sub-section of the genera that were cited in manuscripts that studied associations of oral bacteria with cigarette smoking, electronic cigarette smoking, and cardiovascular risk/disease, respectively. Red circles indicate a significant increase of the corresponding oral microbiome taxon to cigarette smoking, e-cigarette smoking or cardiovascular variables, while blue indicate a significantly decreased relative abundance. These figures were generated in JMP™ Version 14 Data Discovery Statistical Software. Data is shown across all oral sites and larger circles indicate more references to an increase or decrease in the specified genus. Species-level features were collapsed to the genus level for illustrative purposes. Taxa at the species and genus level used to make this figure, and the corresponding citations, can be found in Additional file 2: Table S1 (oral microbiome and smoking) and Additional file 3: Table S2 (oral microbiome and cardiovascular risk/disease). E-cigarette electronic cigarette
Cigarette smoking and oral microbiome-associated metabolite pathway and inflammatory biomarker changes
Glycine, serine, and threonine metabolism pathways, amino acid enzyme and phenylalanine, tyrosine, and tryptophan biosynthesis pathways were upregulated in smokers’ saliva, tongue dorsum and buccal mucosa samples [35, 36, 52]. In studies that documented the presence or absence of periodontal disease, smoking subjects without periodontal disease had higher levels of protein/amino acid biosynthesis and metabolism pathway genes in saliva and buccal mucosa samples compared to non-smokers without periodontal disease [35, 52]. Interestingly, the same pathways (glycine, serine, and threonine metabolism and phenylalanine, tyrosine, and tryptophan biosynthesis pathways) were downregulated in subgingival plaque samples of subjects who smoked and also carried a diagnosis of periodontal disease, suggesting that sampling site and/or associated periodontal disease may influence metabolic responses to smoking [42]. The galactose metabolism pathway was downregulated [55], while lipopolysaccharide biosynthesis pathways were upregulated in tongue dorsum samples of smokers compared to non-smokers [52]. In saliva samples, smoking was associated with a decreased abundance of general lipid metabolism pathways, but increased polyketide metabolism pathways compared to non-smokers [52]. The relationship between smoking and salivary cytokine levels had conflicting results. In one study, saliva levels of pro-inflammatory cytokines tumor necrosis factor (TNF)-α, INF-ɣ, and interleukin (IL)-4 were significantly increased in non-smokers compared to cigarette smokers [46]. In another study, smoking was associated with increased levels of pro-inflammatory IL-2 and IL-4 and decreased levels of anti-inflammatory IL-10 versus non-smokers [51]. Finally, after adjusting for multiple factors, both cigarette smoking and detectible Porphyromonas gingivalis bacteria in subgingival plaque samples were associated with plasma high-sensitivity C-reactive protein (CRP) levels [60].
Electronic-cigarette smoking and oral microbiome compositional changes
The studies reporting associations between the oral microbiome and e-cigarette smoking are limited, but the two studies reported in this review present a comprehensive evaluation of e-cigarette exposure on the saliva and subgingival microbiome communities in addition to the metabolic pathway and cytokine alterations [15, 46]. E-cigarette smoking was associated with an increased RA of Abiotrophia, Aggregatibacter, Cardiobacterium, Eikenella, Granulicatella, Haemophilus, Johnsenella, Kingella, Lachnoanaerobaculum, Leptotrichia, Mogibacterium, Parvimonas, Peptostreptococcus, and Selenomonas in subgingival plaque samples of e-cigarette smokers versus non-smokers [15]. In saliva samples, there was an increased RA of species-level Alloprevotella tannerae, Corynebacterium durum, Dialister invisus, Leptotrichia wadei, Parvimonas micra, Prevotella oris, and Veillonella dispar in e-cigarette smokers versus non-smokers [46].
Conversely, the RA of Granulicatella adiacens, Oribacterium parvum, Prevotella sp. HMT 317, Streptococcus oralis subsp. tigurinus clade 071, and Veillonella rogosae were decreased in saliva samples of e-cigarette smokers versus non-smokers [46]. The RA of genus-level Fusobacterium and Neisseria were also increased in saliva samples compared to both cigarette smokers and non-smokers [46]. Fusobacterium species, specifically F. nucleatum and F. periodonticum, were increased and decreased, respectively, in saliva samples of e-cigarette smokers versus non-smokers [46]. Additionally, Porphyromonas species, specifically P. gingivalis, P. endodontalis and P. pasteri, were all increased in saliva samples of e-cigarette smokers versus non-smokers [46].
Electronic-cigarette smoking and oral microbiome-associated metabolite pathway and inflammatory biomarker changes
Several carbohydrate metabolism pathways were elevated in subgingival plaque samples of e-cigarette users, including the central carbohydrate metabolism, one carbon metabolism, fructose kinase, and the monosaccharide, disaccharide and oligosaccharide metabolism pathways compared to non-smokers [15]. Additionally, in subgingival plaque samples of e-cigarette users, lipid A biosynthesis, glycerol kinase, glycerate kinase lipid metabolism pathways, and general protein/amino acid metabolism genes were all upregulated in e-cigarette users [15]. Lysine fermentation, alanine biosynthesis, and arginine biosynthesis pathways were also upregulated in subgingival plaque samples of e-cigarette users [15]. Lipopolysaccharide biosynthesis pathways were upregulated in both subgingival plaque samples of e-cigarette users and tongue dorsum samples of e-cig smokers compared to non-smokers [15, 52]. In e-cigarette users, general protein/amino acid metabolism genes were upregulated in plaque samples compared to non-smokers [15].
E-cigarette smokers had significantly higher levels of the pro-inflammatory cytokines IL-2, IL-6, TNF-ɑ, and INF-ɣ, and lower levels of the anti-inflammatory cytokine IL-10 present in the gingival crevicular fluid compared to non-smokers [15]. Additionally, gingival crevicular fluid levels of the pro-inflammatory cytokine GM-CSF was higher in e-cigarette users versus cigarette smokers and non-smokers [15]. In another study, salivary levels of the pro-inflammatory cytokine IL-2 were elevated in e-cigarette smokers versus non-smokers [46]. Salivary IL-6 and IL-1ß were also elevated in e-cigarette users versus cigarette smokers and non-smokers in this study, although these differences were not significant [46]. Conversely, the pro-inflammatory cytokine TNF-α had the highest saliva concentrations in non-smokers, followed by cigarette smokers, and finally e-cigarette smokers [46]. Finally, FaDu and Leuk-1 cell lines exposed to e-cigarette aerosol and individually co-infected with the bacterial taxa P. gingivalis and F. nucleatum, respectively, displayed higher mRNA levels of the pro-inflammatory cytokines IL-1ß, TNF-α, IFN-ɣ, IL-6, and IL-8, when compared to the same co-infected cells exposed to air [46].
Cardiovascular disease/risk and oral microbiome compositional changes
Alterations in the oral microbiome and clinical periodontitis have been thought to mediate CVD and CVD risk by promoting systemic low-grade inflammation through pathogenic bacteria and their byproducts [61]. Importantly, many current reviews on the link between oral bacteria and CVD have focused on specific bacteria associated with periodontitis [6, 62], and not how changes in other bacterial members of the oral microbiome community may contribute to CVD through cardiovascular migration or endotoxemia. Across most studies analyzed in this review, the number of smokers reported ranged from 11 to 80% in the CVD group (Table 3).
Table 3.
Included studies examining the association between cardiovascular risk/disease and the oral microbiome
| Author, year | Oral sample site(s) | Aim | Population studied | % Smokers | Sequencing | Region if 16S | Citation |
|---|---|---|---|---|---|---|---|
| Boaden, 2017 | Saliva, buccal mucosa, tongue, gingiva and hard palate | Describe the bacterial profile of the oral flora during the first two weeks following a stroke, examining changes in the condition of the oral cavity and infections | Patients with stroke (n = 50) | 20% current, 30% prior-smokers | 16S | V1–V9 | [75] |
| Fåk et al., 2015 | Whole mouth swab | Elucidate whether the oral microbiota composition differed between patients with asymptomatic and symptomatic atherosclerosis | Asymptomatic atherosclerosis (n = 35), symptomatic atherosclerosis (n = 27), control (n = 30), total (n = 92) | Current smokers: 9% asymptomatic atherosclerosis, 23% symptomatic atherosclerosis, 21% control | 16S | V1–V2 | [70] |
| Gordon et al., 2019 | Subgingival plaque | Characterize and compare the oral microbiome between four study groups based on BP status in postmenopausal women | Normal BP (n = 179), stage I hypertension (n = 106), Stage II hypertension (n = 42), patients on hypertension medications, irregardless of BP (n = 119), total (n = 446) | Current 4.5%, former 39.7% normal BP; current 2.8%, former 47.2% stage I; current 2.4%, former 40.5% Stage II, current 2.5%, former 45.4% patients on hypertension medications | 16S | V3–V4 | [69] |
| Leskelä et al., 2020 | Saliva | Investigate associations of specific oral bacteria and LPS neutralizing capacity in a case–control study of ischemic stroke | Controls (n = 100), Patients with stroke (n = 98), total (n = 198) | Current smokers: 12% controls, 28% patients with stroke | Targeted qPCR sequencing | N/A | [63] |
| Liljestrand et al., 2018 | Subgingival plaque | Study the association between periodontal pathogen burden, saliva and serum LPS activity and how periodontitis and coronary artery disease interrelate with them | Control (n = 123), stable CAD (n = 184), ACS (n = 169), ACS-like, no CAD (n = 29); total (n = 505) | Ever smokers: 46.3% control, stable CAD, ACS, ACS-like, no CAD; 52.9% total | DNA hybridization | N/A | [64] |
| Kannosh et al., 2018 | Subgingival plaque | Assess temporal changes in the frequency of periodontal bacteria in the subgingival plaque and in atherosclerotic blood vessels of patients with atherosclerosis | Patients with atherosclerosis (n = 100) | Smokers: 55% of total sample | Targeted 16S sequencing | N/A | [67] |
| Koren et al., 2011 | Oral cavity swab | Aimed to address: Is there a core atherosclerotic plaque microbiota? Are bacteria present in the plaque also detectable in the oral cavities or guts of the same individuals? Is an altered oral or fecal microbiota associated with atherosclerosis? | Controls (n = 15), patients with atherosclerosis (n = 15); total (n = 30) | Current smoker: 0%, controls, 40% patients with atherosclerosis | 16S | V1–V2 | [74] |
| Mahalakshmi et al., 2017 | Subgingival plaque | Determine the incidence of anaerobic periodontopathic bacterial co-occurrences in periodontitis and atherosclerosis | Control patients without periodontitis or systemic disease (n = 100), patients with atherosclerosis (n = 65); patients with periodontitis but no systemic disease (n = 59); total (n = 224) | Current or past smokers were excluded from the study | Targeted 16S sequencing | N/A | [71] |
| Nikolaeva et al., 2019 | Subgingival plaque | Characterize composition of subgingival biofilm with periodontopathogenic bacteria species and endothelium-dependent vasodilation in patients with chest pain and concomitant periodontitis | Patients with angina pectoris (n = 15); patients with acute myocardial infarction (n = 15); Patients with chest pain but no coronary artery disease (n = 15); total (n = 45) | Current smokers: 80% patients with angina pectoris; 60% patients with acute myocardial infarction; 47% patients with chest pain but no coronary artery disease | Targeted 16S sequencing | N/A | [72] |
| Perry et al., 2020 | Saliva | Establish how oral bacteria are related to cough sensitivity and pneumonia in a clinical stroke population | Patients with atherosclerosis (n = 100) | Not reported | Targeted qPCR | N/A | [76] |
| Serra e Silva Filho et al., 2014) | Subgingival plaque | Assess microbial diversity of the subgingival environment and atheroma plaques of patients with periodontitis and obstructive coronary artery atherosclerosis | Patients with periodontitis and atherosclerosis (n = 18) | Smokers: 55.6% of total sample | 16S | V1–V9 (27f/ 1492r primers) | [68] |
| Su et al., 2019 | Tongue dorsum | Study the association between oral bacteria on the tongue dorsum and factors associated with oral health and systemic disease in middle-aged and elderly patients | Total sample (n = 70) | Smokers: 11% of total sample | Targeted PCR sequencing | N/A | [73] |
| Ziebolz, Jahn, et al., 2018 | Subgingival plaque | Detect periodontal pathogens DNA in atrial and myocardial tissue, and to investigate periodontal status and their connection to cardiac tissue inflammation | Patients undergoing surgery for aortic valve stenosis (n = 30) | Smoking history was present in only 8 patients: average of 27.2 ± 21.8 pack/years in that subset | Targeted PCR sequencing | N/A | [66] |
| Ziebolz, Rost, et al., 2018 | Subgingival plaque | Detect correlations of microbiological DNA, inflammatory proteins, and infection parameters in patients with periodontal disease and valvular heart disease | Patients undergoing surgery for aortic valve stenosis (n = 10) | Smokers: 30% of total sample | Targeted PCR sequencing | N/A | [65] |
16S 16S ribosomal ribonucleic acid sequencing, ACS Acute Coronary Syndrome, BP blood pressure, CAD Coronary Artery Disease, DNA deoxyribonucleic acid, LPS lipopolysaccharide, PCR polymerase chain reaction, qPCR quantitative polymerase chain reaction, V variable region of the 16S ribosomal ribonucleic acid gene
The RA of Aggregatibacter, Campylobacter, Fusobacterium, and Porphyromonas were associated with CVD in several studies (Fig. 1B). For example, increased RA of A. actinomycetemcomitans in saliva samples was seen in patients with ischemic stroke [63], increased RA of A. actinomycetemcomitans in periodontal pocket/subgingival samples occurred in patients with coronary artery disease [64], acute coronary symptom [64], and valvular heart disease [65, 66], and A. actinomycetemcomitans was present in both subgingival plaque and samples of coronary artery atherosclerotic samples [67]. Increased RA of Campylobacter rectus in periodontal pocket/subgingival samples also occurred in patients with coronary artery disease [64], acute coronary symptom [64], and valvular heart disease [65–67], and C. rectus was present in both subgingival plaque and samples of coronary artery atherosclerotic samples [68]. Campylobacter concisus was an additional species that was found in both subgingival biofilm samples and coronary artery plaques of patients with coronary artery disease [68]. Increased RA of Fusobacterium in subgingival samples occurred in patients with increased blood pressure [69], valvular heart disease [65, 66], and several Fusobacterium species were present in both subgingival plaque and samples of coronary artery atherosclerotic plaques [68]. Increased RA of Porphyromonas in whole mouth samples of patients with coronary artery disease [70], Porphyromonas gingivalis was also elevated in subgingival samples of patients with coronary heart disease [67, 68, 71, 72], valvular heart disease [65], and in smokers with a history of CVD [73]. Porphyromonas gingivalis was found in both subgingival and coronary artery atherosclerotic plaque samples alone and in combination with several species, including Tannerella forsythia, Tannerella denticola, Eikenella corrodens, and Campylobacter rectus [68, 71].
The association between the RA of Prevotella in the oral microbiome and cardiovascular risk/CVD had conflicting results in the literature. There was an inverse association of the RA of Prevotella, P. scopos, and P. intermedia in subgingival plaque samples in patients with increased blood pressure [69] and acute myocardial infarction [72] in two studies. Other research reported a positive association of Prevotella, P. shahii, and P. nigrescens in whole mouth samples in patients with coronary artery disease [70], and subgingival samples in patients with increased blood pressure [69], diagnosed with hypertension [69], coronary artery disease [68, 71], valvular heart disease [65, 66], and both subgingival and coronary artery plaque samples had P. nigrescens, P. intermedia, and P. loescheii present. The RA of Treponema and Veillonella were increased in whole mouth samples in patients with coronary artery disease [70], and subgingival plaque samples in patients with coronary artery disease [71] and diagnosed hypertension [69]. Veillonella was additionally identified in both whole mouth samples and in carotid artery atherosclerotic plaque samples [74].
Increased blood pressure was associated with a reduced RA of Actinomyces and increased RA of Selenomonas in subgingival plaque samples [69], respectively, and both Actinomyces and Selenomonas were preset both in subgingival, and coronary artery atherosclerotic plaque samples [68]. Capnocytophaga leadbetteri and Eikenella corrodens were found in both subgingival plaque and coronary artery atherosclerotic plaque samples [68], and an increased RA of these bacteria in subgingival biofilm samples occurred in patients with valvular heart disease [65, 66]. The RA of Streptococcus and several Streptococcus species were decreased in saliva and oral samples of patients with elevated blood pressure and ischemic stroke compared to patients without CVD [69, 75, 76]. Finally, species-level Filifactor alocis and Treponema denticola were seen in both subgingival and coronary artery plaque samples in patients with coronary artery disease [67, 68, 71]. See Additional file 3: Table S2 for all cardiovascular-associated oral bacteria responses in the reviewed studies.
Oral microbiome as an intersection between smoking and CVD: potential/plausible mechanisms
Smoking remains a significant risk factor for CVD development, and differences in the bacterial community of different oral niches have been associated with both smoking and CVD in the studies outlined in this review. The association between smoking and alpha diversity differed across studies, with some studies reporting an increase in alpha diversity, others reporting a decrease and others reporting no association of alpha diversity with smoking. Furthermore, many research studies did not report alpha diversity associations and focused solely on differential abundance differences in specific bacteria of the oral microbiome. Nevertheless, differences in alpha diversity associations with cigarette smoking may be related to different oral microbiome sampling sites, studies not powered to evaluate smokers versus non-smokers or different confounders present that may influence the overall bacterial community. Future research studies using consistent alpha diversity metrics will allow continued cross-study comparison across oral microbiome sampling sites and will inform the relationships between smoking and alpha diversity.
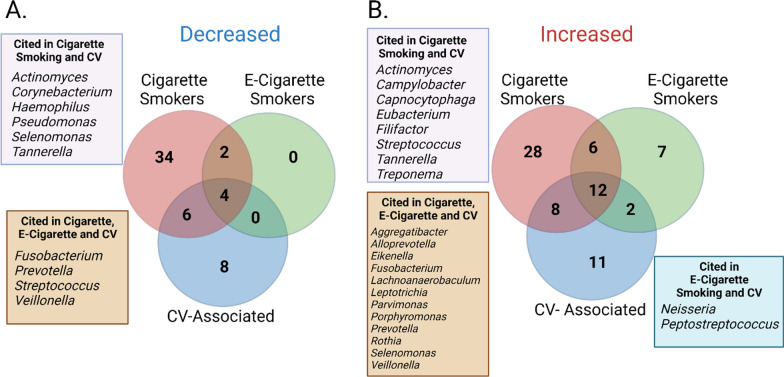
Through comparing the associations between oral microbial taxa and smoking (Additional file 2: Table S1) and cardiovascular disease/risk (Additional file 3: Table S2), respectively, we found oral bacteria that had shared negative (Fig. 2A) and positive (Fig. 2B) associations with smoking (both cigarette and e-cigarette) and CVD. Additionally, there were several oral microbiome-associated bacteria that were present in both subgingival samples and atherosclerotic plaques that also had positive RA associations with cigarette and e-cigarette smoking (versus non-smokers). The bacteria sequenced from atherosclerotic plaques that were also associated with smoking included Aggregatibacter actinomycetemcomitans, Campylobacter rectus, Filifactor alocis, Fusobacterium, Leptotrichia, Porphyromonas, Prevotella, Selenomonas, Treponema/Treponema denticola, and Veillonella. As these bacteria have shared associations between smoking and CVD and/or cardiovascular risk, these may be important for future studies directly examining the oral microbiome as a mediator between smoking and elevated risk of CVD. Although identifying the oral microbiome compositional changes related to smoking and CVD is important in exploratory and preliminary studies, understanding the functional roles of oral microbiome shifts will provide deeper insight into the role oral bacteria has on human pathophysiology. From our extensive review of the literature, we have identified several mechanisms in which smoking can increase CVD risk through the oral microbiome, those include (1) inflammatory mechanisms, (2) lipid and amino acid modulation, and (3) production of vasoactive metabolites (Fig. 3).
Fig. 2.
A Shared and unique oral bacterial taxa that are decreased in association with cigarette smoking, e-cigarette smoking and CV-associated risk or disease. B Shared and unique oral bacterial taxa that are increased in association with cigarette smoking, e-cigarette smoking and CV-associated risk or disease. Bacteria summary tables from Additional file 2: Table S1 (oral microbiome and smoking) and Additional file 3: Table S2 (oral microbiome and cardiovascular risk/disease) were imported into JMP™ Version 14 Data Discovery Statistical Software, and species-level bacteria was collapsed to the genus level. If a genus-level bacterium was mentioned as increased or decreased in association with cigarette smoking, e-cigarette smoking or CVD, it was binned in the respective category. See Additional file 4: Table S3 for a summary of shared and unique bacteria. CV cardiovascular, e-cigarette electronic cigarette. Figure created with BioRender.com
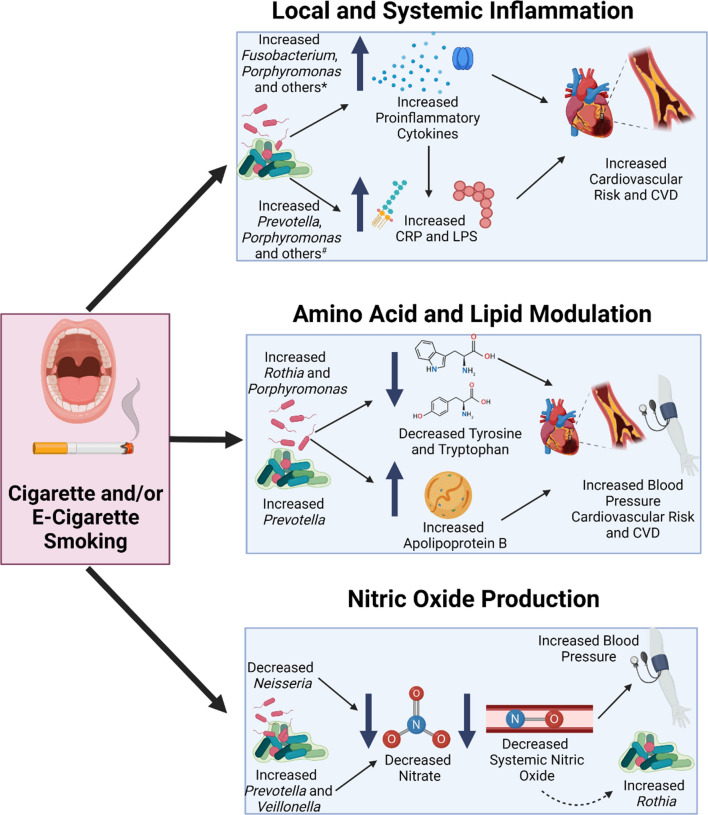
Fig. 3.
Schematic summarizing hypothesized pathways where the oral microbiome mediates cardiovascular risk and disease in response to smoking. A An increased RA of multiple bacteria associated with smoking including Fusobacterium, Porphyromonas, Lachnoanaerobaculum Parvimonas, Mogibacterium Streptococcus, Selenomonas, and Rothia in the oral microbiome have been positively associated with increased proinflammatory cytokine levels. A smoking-associated increase in the RA of Alloprevotella, Filifactor, Fusobacterium, Porphyromonas, Veillonella, Treponema, and Parvimonas was associated with LPS levels or biosynthesis genes, while Parvimonas was associated with CRP. Increases in local and systemic cytokines, along with elevated CRP and LPS are associated with an increased risk of CVD. B Increased RA of Rothia and Porphyromonas, both elevated in the oral cavities of smokers versus non-smokers, are potentially associated with decreased tyrosine and tryptophan levels through different hypothesized mechanisms. Prevotella RA was increased in smokers, which is positively associated with increased Apolipoprotein B levels. Both decreases in tyrosine/tryptophan and increased Apolipoprotein B is associated with increased cardiovascular risk. C An increase in the oral RA of Prevotella and Veillonella, and a decrease in the RA of Neisseria that was documented in smokers versus non-smokers is associated with decrease nitrate levels that ultimately lead to decreased nitric oxide levels. Decreased nitic oxide levels are associated with alterations in blood pressure and CVD, and may lead to a compensatory increase in oral Rothia abundance in association with smoking. Figure created with BioRender.com
Inflammatory mechanisms
Evidence has demonstrated that periodontal disease creates an inflammatory oral environment in which mediators may transmit to the systemic circulation. Systemic diseases such as diabetes mellitus [77, 78] and CVD [79] have also been associated with increases in oral inflammation and periodontal pathology through disease mechanisms and treatment modalities [79], suggesting a bidirectional relationship between local (oral) and systemic inflammatory processes and health. The RA of bacterial taxa associated with periodontal disease, including Porphyromonas, Treponema, Tannerella, Campylobacter, and Prevotella spp. were positively associated with cigarette and e-cigarette smoking in many studies (Table 3). Additionally, in studies evaluating shared oral and coronary artery plaques, atherosclerotic plaques were found to contain DNA from periodontal pathogens, indicating transmission of bacteria from the oral cavity to the heart [68, 71]. The potential link between the periodontal disease pathogens and increased cardiovascular risk or CVD has been studied extensively [32, 60, 62, 80]. Evidence has demonstrated that periodontal disease creates an inflammatory oral environment in which mediators may transmit to the systemic circulation [60].
Lipopolysaccharide (LPS): LPS, an endotoxin that is commonly found in the cell wall of gram-negative bacteria, has been demonstrated to trigger the inflammatory cascade resulting in the systemic inflammation that increases cardiovascular risk and CVD [81, 82]. There is a strong connection of periodontitis to cardiometabolic disorders, mediated by LPS, that has been reviewed in detail [83]. In the reviewed studies, LPS biosynthesis pathway genes were upregulated in subgingival plaque sample of e-cigarette smokers and tongue dorsum samples of cigarette smokers [15, 55]. Additionally, many bacteria that had positive associations with LPS biosynthesis genes had increased RA levels in the oral microbiome of cigarette and e-cigarette smokers [81, 84]. For example, Alloprevotella tannerae was increased in saliva samples of e-cigarette smokers [46], Filifactor was increased in tongue dorsum samples of cigarette smokers [41, 55], Fusobacterium nucleatum was increased in saliva samples of e-cigarette and cigarette smokers [46, 52, 54]; and Prevotella was increased in saliva, whole mouth, buccal, and tongue dorsum samples of cigarette and e-cigarette smokers [34, 38–40, 44, 46, 55, 58]. Other bacteria associated with LPS biosynthesis that were increased in smokers included Porphyromonas endodontalis in tongue dorsum and saliva samples of cigarette and e-cigarette smokers [46, 55], Veillonella in saliva, whole mouth, buccal, tongue dorsum, and subgingival plaque samples of cigarette and e-cigarette smokers [15, 38, 43, 44, 46, 48, 50, 55, 58], Treponema in saliva, whole mouth and subgingival plaque samples of cigarette smokers [34, 48, 52, 55, 59], and Parvimonas in saliva and subgingival plaque samples of cigarette and e-cigarette smokers [15, 46]. The RA of genus-level Parvimonas was also positively correlated with LPS biosynthesis genes in the oral microbiome [70]. Additionally, in one study, the LPS gene in commensal biofilm samples was upregulated 22.8-fold with nicotine-free vapor and 10.1-fold in nicotine-containing vapor in e-cigarette users versus non-smokers [15].
C-Reactive Protein, CRP: CRP is another biomarker associated with inflammation and cardiovascular risk [85]. Plasma CRP levels can reliably predict the prognosis of atherosclerosis, heart failure, and other CVD, even in otherwise asymptomatic individuals [86]. Plasma CRP levels have shown to be higher in cigarette smokers versus non-smokers in studies with [60] and without [87] inclusion of oral bacteria measures. Increased CRP transcription in the liver have been associated with increased levels of pro-inflammatory cytokines IL-6, IL-1, and TNF-α, suggesting another cardiovascular risk mechanism linked to inflammation and mediated by smoking-associated changes in the oral microbiome and elevated cytokine levels [86]. As there has been a longstanding connection between oral infection and septicemia, especially in immunocompromised patients [88, 89], oral bacterial translocation to the liver and systemic circulation through the gut is another potential mechanism that deserves future research. CRP can also indirectly activate TNF-α, reactive oxygen species, and IL-1ß in apoptotic pathways leading to a persistent systemic inflammatory state [86, 90]. Parvimonas was positively correlated with plasma CRP in subjects with asymptomatic and symptomatic atherosclerosis in previous research [70]. In the reviewed studies of smoking and the oral microbiome, both cigarette and e-cigarette smoking were associated with an increased RA of Parvimonas in subgingival plaque and saliva samples [15, 46]. Collectively, these associations provide evidence that cardiovascular risk may be mediated through cigarette and e-cigarette smoking-associated oral microbiome changes that promote a systemic inflammation driven by LPS and CRP. Future mechanistic research will elucidate the pathways underlying oral microbiome-associated LPS and CRP responses to cigarette smoking so interventional research studies can be designed to lower cardiovascular risk and CVD in these patients.
Cytokines: Oral bacteria that had significant positive associations with cigarette and e-cigarette smoking were also associated with several salivary pro-inflammatory cytokines. For example Porphyromonas correlated positively with proinflammatory cytokines such as IL-2, IL-13, IL-8, and IL-1ß; Lachnoanaerobaculum with IL-2, IL-4, IL-8, IL-13, IL-10, IL-12p70, and IFN-ɣ; Parvimonas and Mogibacterium with IL-8 and IL-1ß; and Fusobacterium with IL-1ß [46]. Streptococcus and Rothia (increased in several oral sites of cigarette smokers) and Selenomonas (increased in subgingival plaque samples of cigarette smokers) also had positive associations with pro-inflammatory cytokines IL-1ß, IL-2, IL-4, IL-6, IL-7, IL-9, IL-12 and IL-17 [91]. The RA of Johnsonella (increased RA in e-cigarette smokers) was positively associated with IL-1ß levels [46]. Conversely, Peptostreptococcus (decreased in the whole mouth and tongue dorsum samples of cigarette smokers versus non-smokers [38, 41]) was negatively associated with salivary IL-8 and IL-1ß [46]. Finally, two bacteria (Porphyromonas gingivalis and Fusobacterium nucleatum) that play pivotal roles in periodontal disease and act on macrophages, neutrophils, and monocytes to induce TNF-α, IL-6, and IL-8 production [92] were increased in smokers’ tongue dorsum [55] and saliva samples [46, 52, 54], suggesting another link between smoking, periodontal disease and inflammation-mediated cardiovascular risk. It is important to note that some of the bacteria that were positively associated with smoking and LPS biosynthesis were not periodontal pathogens but genera that are common to the healthy oral microbiome habitat (i.e. Streptococcus and Veillonella). This suggests that an imbalance of “healthy” oral-associated bacteria as a result of smoking may also contribute to increased inflammation in addition to an increased RA of periodontal pathogens. Overall, upregulation of common and unique inflammatory cytokines in salivary and gingival crevicular fluids in both e-cigarette cigarette smokers suggests that smoking alters the oral microbiome in a manner associated with increased inflammation that plausibly contributes to the increased CVD risk in this population.
Amino acids
Increases or decreases in local (i.e. oral) and systemic amino acid levels through modulation of amino acid metabolism and biosynthesis pathways is another possible mechanism in which smoking may influence cardiovascular risk through oral microbiome-associated bacteria. Amino acids are the foundational molecules for protein catabolism and are involved in the biosynthesis of important molecules including hormones, neurotransmitters, and coenzymes. Gut microbial metabolites have been strongly associated with amino acid and lipid metabolism [93], but relationships between similar oral bacteria and associated amino acid or lipid metabolic functions is not as well known.
Tyrosine is derived from phenylalanine and is a nonessential amino acid involved in protein synthesis and signal transduction, while tryptophan is an essential amino acid also involved in the production and maintenance of enzymes and neurotransmitters [94]. In many of the evaluated studies, smoking was associated with an increase in the RA of Rothia in saliva, whole mouth, tongue dorsum, and buccal samples [38, 41, 44, 46, 52, 55]. Associational analyses demonstrated that oral microbiome communities with higher levels of Rothia were more likely to display greater utilization of tyrosine and tryptophan [55], which could lead to lower levels of these amino acids. Salivary composition changes and increased incidence of periodontitis, both associated with smoking, contribute to an oral environment where gram-positive facultative anaerobes and amino-acid degrading bacteria like Prevotella proliferate [95]. Similarly, smoking was associated with an increased RA of Prevotella across all of the oral sampling sites (Table 2). Therefore, reductions in oral amino acid levels via smoking-associated bacterial changes may occur through known mechanisms such as changes in oral environment or from other mechanisms that will be identified as more work is performed on the functional implications of oral bacteria alterations in response to e-cigarette and cigarette smoking.
It is not known if smoking-associated changes in oral amino acid levels are directly associated with plasma levels, but connections between oral disorders and decreased plasma amino acid levels have been reported [96, 97]. This topic will be of great interest to establishing connections between the oral microbiome and systemic disease as many plasma amino acids are associated with cardiovascular risk and CVD. For example, tryptophan has been thought to be inversely associated with cardiovascular risk, as serum tryptophan levels have predicted lower risk of CVD events and death related to CVD in observational studies [98, 99]. Decreased serum tyrosine levels were also reported in patients with stroke [100] and hypertension [101], and increased tyrosine intake was associated with lower peripheral and central blood pressure [102]. Low plasma serum tryptophan concentrations are associated with increased CRP and other pro-inflammatory cytokines previously discussed, subsequently increasing risk for CVD [99, 103]. Therefore, an increased understanding of pathways linking smoking to the modulation of amino acid-associated oral microbiota and the influence these bacteria have on host-microbial protein–protein interactions and systemic cardioprotective amino acids such as tyrosine or tryptophan is an exciting avenue for future research.
Lipids
Bacteria of the oral microbiome that are impacted by smoking may also modulate cardiovascular risk through associations with lipids implicated in CVD. For example, the RA of Streptococcus salivarius was increased in saliva and tongue dorsum samples of cigarette smokers versus non-smokers [39, 46, 55], and was also positively associated with oleic acid biosynthesis pathways in a separate in-vitro study of cultured S. salivarius and metabolites [104]. Circulating levels of oleic acid, a fatty acid, are not indicative of dietary intake, and may involve hepatic synthesis by the enzyme Stearoyl-CoA desaturase-1. Interestingly, circulating levels of oleic acid were independently associated with increased rates of CVD and all-cause mortality in a large Multi-Ethnic Study of Atherosclerosis [105], and oleic acid was also positively associated with diastolic blood pressure in other research [106]. The RA of Lactobacillus, which was increased in whole mouth and subgingival plaque samples of cigarette smokers [50, 58], was positively associated with plasma Apolipoprotein B levels in a separate study using linear regression analysis [70]. Apolipoprotein B is being increasingly acknowledged as a main contributor to atherosclerotic CVD [107], and large cohorts studies of have found oxidized lipids like Apolipoprotein B to be associated with coronary artery disease [108]. Finally, platelet activating factor, a potent phospholipid activator, has been reported to increase in both tobacco and e-cigarette smokers through the release of free radicals, creating oxidative stress to the intercellular environment [109, 110]. The RA of Prevotella was found to be positively associated with platelet activating factor in an in vitro experiment in mice [111], and the RA of Prevotella was also increased in saliva, whole mouth, and subgingival plaque samples of cigarette smokers versus non-smokers [34, 37, 38, 40, 46, 58], suggesting a potential link between smoking, Prevotella and platelet activating factor. Platelet activating factor has been associated with worse stroke outcomes through its thrombotic and platelet aggregation properties in addition to promoting oxidative stress and systemic inflammation [112]. While all of these relationships point to a possibility that smoking may contribute to CVD through modulation of specific oral microbiome-associated bacteria that have relationships with amino acid and lipid levels, these studies are associational in nature. Future research confirming the above relationships and testing associations with plasma amino acid and lipid levels will inform mechanisms and pathways potentially underlying the relationship between smoking and the oral microbiome and their combined impact on cardiovascular risk.
Nitric oxide production
Nitric oxide is a known vasodilator that decreases cardiovascular risk through reduction of blood pressure and inhibition of oxidative stress, platelet aggregation and leukocyte adhesion [113, 114]. Nitric oxide is produced endogenously by nitric oxide synthases from the amino acid l-arginine and molecular oxygen. Since human cells lack nitrate (NO3) reducing capability, commensal oral bacteria have been identified for their role in converting dietary NO3 to nitrite (NO2), which can be further reduced to nitric oxide [113, 115]. This alternate nitric oxide production mechanism is important for maintenance of cardiovascular integrity during periods of hypoxia. This NO3–NO2-nitric oxide entero-salivary pathway is an important pathway in which the oral cavity influences systemic physiological processes and could prove to be a potential therapeutic target. Alterations in oral bacterial communities induced by antibacterial mouthwash use, had been documented to decrease nitric oxide levels and was associated with alterations in blood pressure [116, 117]. Furthermore, studies have shown that dietary nitrate supplementation using nitrate rich foods (such as green leafy vegetables) could enhance nitric oxide production. Similar to nitric oxide, carbon monoxide is a gas that possesses vasodilatory properties, has documented interactions with the microbiome (particularly the gut microbiome), and its levels are potentially influenced by dietary consumption including fiber, leafy greens, carbohydrates and proteins [118–120]. Periodontal disease-associated alterations in oral bacteria and consequential impacts of nitric oxide and cardiovascular risk through blood pressure modulation have also been previously reviewed in the literature [17]. Nevertheless, these relationships have not been as thoroughly explored for smoking-associated modulation of oral bacteria or if other small gas production (like carbon monoxide) is modulated by smoking and/or the oral microbiome and how these associations might impact subsequent cardiovascular risk. Multidirectional interactions between vasodilatory gas and associated signaling pathways with the microbiome and host are exciting avenues for future research that potentially holds promising therapeutic benefits for cardiovascular risk and disease.
In the reviewed studies, there were significant associations between smoking and nitrate-reducing bacteria (i.e., Rothia and Neisseria [24, 121]) and bacteria that are inversely associated with nitrate and nitric oxide (Prevotella and Veillonella [24, 121]). Interestingly, the two major nitrate-reducing bacteria in the oral microbiome had disparate RA associations with smoking. For example, there was agreement across several studies that the RA of Neisseria was decreased in saliva, whole mouth, tongue dorsum, and subgingival plaque samples [34, 36–38, 41, 43, 47, 50, 52, 53, 55, 58], while the RA of Rothia increased in whole mouth, saliva, tongue dorsum and subgingival plaque samples of cigarette and e-cigarette smokers versus non-smokers [36, 38, 41, 44, 46, 52, 55, 58]. Whether the smoking-associated increase in Rothia RA is a compensatory mechanism in response to smoking-induced decreased nitric oxide levels resulting from oral environment changes (acidity, salivary production etc.) and reduced Neisseria levels or is a completely separate mechanism is unknown. Future research with direct nitric oxide measures in response to smoking-associated changes in oral microbiome RA of nitrate-reducing bacteria will continue to inform these mechanisms and pathways. Unlike associations between nitrate-reducing bacteria and smoking, there was equally as strong but consistent evidence that smoking was associated with an increased RA of bacteria that possess negative relationships with nitric oxide production and availability. For example, the RA of Prevotella was increased in saliva, whole mouth, tongue dorsum and buccal samples [34, 36–40, 44, 46, 52, 58], and Veillonella increased in saliva, whole mouth, tongue dorsum, buccal, and subgingival plaque samples of e-cigarette and cigarette smokers versus non-smokers [15, 36–38, 41, 43, 44, 46, 48, 50, 55, 58]. A previous study evaluating the RA of Prevotella and Veillonella after nitrate administration reported a decrease in both Prevotella and Veillonella after 10 days of dietary supplementation with nitrate-rich beetroot juice [122]. Nitrate supplementation also lowered blood pressure in two studies using dietary nitrate interventions [113, 123], and the one study that measured oral microbiome responses to nitrate supplementation reported greater plasma NO2 levels were associated with higher RA of Rothia and Neisseria and lower RA of Prevotella and Veillonella [113]. Taken together, this evidence indicates smoking-mediated responses of nitric oxide-associated oral bacteria plausibly impact cardiovascular risk, and dietary nitrate supplementation may be a way to mitigate progression of CVD through modulation of oral bacteria.
Conclusions and future directions
This review synthesized the literature on bacteria associated with smoking and the oral microbiome, and the oral microbiome and cardiovascular risk and disease. The goal of this review was to find shared bacterial taxa between smoking and CVD, respectively, to inform future research on the role of the oral microbiome in smoking-associated cardiovascular risk and disease. We identified several shared bacteria in the oral microbiome that are associated with both smoking and cardiovascular risk, and discussed potential mechanisms that may underlie these correlations including inflammation, amino acid and lipid metabolism modulation and influence on nitric oxide production and availability. Nevertheless, some limitations of this review must be discussed. The metabolites and metabolic genes identified in the reviewed manuscripts were only measured directly or indirectly in the oral cavity. Future research studying associations between oral and plasma metabolite or cytokine levels in response to cigarette and e-cigarette smoking will continue to inform how smoking-mediated alterations in the compositional and functional profiles of the microbial environment can impact systemic physiologic processes and cardiovascular risk. Studies in our review did not provide dietary data for us to determine if diet-related byproducts or metabolites directly or indirectly impacted by smoking affect the structure and function of the oral microbiome.
Many of the studies reviewed in this manuscript used different methods for DNA extraction and sequencing, which have been known to impact microbiome results [124], and may account for some of the variability in oral microbiome bacteria association with cigarette or e-cigarette smoking in the synthesized literature. Additionally, many of the studies listed in Tables 1 and 3 used different V regions for amplicon sequencing, which may also impact annotation accuracy and the RA of oral microbiome-associated taxa [125]. Therefore, consideration of the extraction and sequencing methodology is important in the interpretation of the studies reviewed in this manuscript. Smoking was not the main outcome measure in all of the reviewed studies, and therefore not all studies may have been powered to evaluate smoking-associated oral microbiome changes. Furthermore, the percentage of current and past smokers were not reported in all of the studies that evaluated relationships between the oral microbiome and cardiovascular-associated diseases. Adequately powered studies evaluating oral microbiome and smoking associations, while controlling for previous or current smoking status in studies exploring the relationship of the oral microbiome to CVD will further identify mechanisms in which the oral microbiome mediates associations between smoking and CVD. Only two published papers included e-cigarettes in studies evaluating the impact of smoking on the oral microbiome. Although both presented a clear synopsis of multiple pathways in associations between e-cigarette smoking and both bacterial and functional responses of the oral microbiome community, they surveyed different oral microbiome habitats and therefore results could not be accurately synthesized. Future work to confirm these findings and test mechanisms and pathways will be of benefit to future advancement in the field.
Multi-modal studies linking metagenomics, metatranscriptomics and metabolomics will allow a comprehensive survey of the metabolic and functional cardiovascular implications of smoking on the oral microbiome, and will be of great interest in future research. Additionally, research integrating the multi-modal oral metagenomics data with salivary and plasma biomarkers (e.g. cytokines or cortisol) will inform some of the hypothesized inflammatory mechanisms connecting smoking-associated oral microbiome changes to CVD. Specific pathways underlying metabolite production, inflammation and communication with the host have been reported in the gut microbiome. Nevertheless, the oral environment is very different from the gut microbiome and therefore putative mechanisms surrounding gut microbiome bacteria may not necessarily replicate in the oral cavity. Therefore, future work sampling both oral and gut microbiome bacterial communities can identify shared and unique mechanistic responses to smoking and CVD, and potential implications for human health. As multiple species belong to the same taxonomic level of genus can have disparate functions in the oral microbiome, sequencing methodologies that have the ability to annotate bacteria to the species level will provide more granular taxonomic annotation and precise functional assignment.
Another important consideration in future research investigating relationships between smoking, the oral microbiome and CVD is to incorporate biobehavioral methodologies that consider environmental, health behavior and physiologic/biologic markers of health in addition to smoking such as nutritional intake, exercise, or heart rate variability. Incorporating factors that quantify health disparities and socioeconomic indicators are also needed in addition to recruiting individuals from diverse ethnicities and backgrounds in oral microbiome research, as this data is limited. An exciting potential biomarker that is emerging in the quantification of environmental and smoking-associated exposure is using epigenetic markers, such as methylation levels. For example, low methylation in the aryl-hydrocarbon receptor repressor gene at cg05575921 is strongly associated with smoking [126, 127], and may be a novel way to quantify smoking exposure and smoking-associated risk in addition to traditional measures such as subjective pack-years or cotinine levels. As the environment is a known contributor to oral microbiome composition, omitting these biobehavioral measures will prevent the field from truly advancing in the understanding of how the oral microbiome influences human disease in response to insults such as smoking across populations. Therefore, interdisciplinary teams with expertise in clinical/periodontology, microbial, nutritional and biobehavioral factors will catalyze studies powered to evaluate these relevant moderating factors, which will accelerate the field’s mechanistic understanding of relationships between smoking, the oral microbiome and CVD. Our hope is that by presenting a synthesis of shared associations between smoking and the oral microbiome, and the oral microbiome and CVD, we will stimulate future high-quality research evaluating these relationships. In the future, the potential for disease risk characterization using personalized oral microbiome strategies is feasible with increased understanding of how differences in oral microbiome communities can impact both local and systemic body systems. Interdisciplinary research incorporating cutting edge technology, paired with consideration of patient-centric factors will not only advance the current understanding of pathways linking the oral microbiome to human physiology, but also stimulate the development of non-pharmacological interventions that will mitigate or prevent the progression of cardiovascular risk to CVD and benefit human health.
Supplementary Information
Additional file 1: PubMed search strategy and search terms.
Additional file 2: Oral microbiome bacteria, bacteria response in association with smoking, oral sampling site location and citations from reviewed studies.
Additional file 3: Oral microbiome bacteria, bacteria response in association with cardiovascular-associated risk measure or disease, oral sampling site location and citations from reviewed studies.
Additional file 4: Shared and unique responses to cigarette smoking, e-cigarette smoking and cardiovascular risk/disease stratified by increased and decreased bacterial relative abundance associations.
Acknowledgements
We would like to acknowledge Nancy Terry, clinical informationist NIH Library, for her assistance with the literature search.
Abbreviations
- CRP
C-reactive protein
- CVD
Cardiovascular disease
- E-cigarette
Electronic cigarette
- LPS
Lipopolysaccharide
- IL
Interleukin
- NO2
Nitrite
- NO3
Nitrate
- PAF
Platelet activating factor
- RA
Relative abundance
- TNF
Tumor necrosis factor
Author contributions
KAM, BM and GRW conceptualized the review. KAM and BM performed the literature review, screened manuscript sources, and performed data extraction and synthesis. KAM and BM drafted the main manuscript text. SMG, BM, NF, NK, JJB, PVG and GRW provided edits and feedback. All authors reviewed the manuscript. All authors read and approved the final manuscript.
Authors’ information
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. BM completed this work as an intramural fellow at the National Institutes of Health, Clinical Center.
Funding
Open Access funding provided by the National Institutes of Health (NIH). This research is supported by intramural research funds from the National Institutes of Health, Clinical Center.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and the Additional files.
Declarations
Ethics approval and consent to participate
All methods were carried out in accordance with institution-specific regulations. This review synthesized previously published, publicly available, and de-identified data.
Competing interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Katherine A. Maki, Email: Katherine.Maki@nih.gov
Sukirth M. Ganesan, Email: Sukirth-Ganesan@uiowa.edu
Brianna Meeks, Email: Bkmeeks@gmail.com.
Nicole Farmer, Email: Nicole.Farmer@nih.gov.
Narjis Kazmi, Email: Narjis.Kazmi@nih.gov.
Jennifer J. Barb, Email: BarbJ@mail.nih.gov
Paule V. Joseph, Email: Paule.Joseph@nih.gov
Gwenyth R. Wallen, Email: Gwallen@cc.nih.gov
References
- 1.Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.(USDHHS). USDoHaHS. Let’s make the next generation tobacco-free: your guide to the 50th anniversary surgeon general’s report on smoking and health. 2014.
- 3.Reilly MP. Tobacco-related cardiovascular diseases in the 21st century. Arterioscler Thromb Vasc Biol. 2013;33(7):1458–1459. doi: 10.1161/ATVBAHA.113.301632. [DOI] [PubMed] [Google Scholar]
- 4.Pirih FQ, Monajemzadeh S, Singh N, Sinacola RS, Shin JM, Chen T, et al. Association between metabolic syndrome and periodontitis: the role of lipids, inflammatory cytokines, altered host response, and the microbiome. Periodontol 2000. 2021;87(1):50–75. doi: 10.1111/prd.12379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lundmark A, Hu YOO, Huss M, Johannsen G, Andersson AF, Yucel-Lindberg T. Identification of salivary microbiota and its association with host inflammatory mediators in periodontitis. Front Cell Infect Microbiol. 2019;9:216. doi: 10.3389/fcimb.2019.00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanz M, Marco Del Castillo A, Jepsen S, Gonzalez-Juanatey JR, D'Aiuto F, Bouchard P, et al. Periodontitis and cardiovascular diseases: consensus report. J Clin Periodontol. 2020;47(3):268–288. doi: 10.1111/jcpe.13189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leite FRM, Nascimento GG, Scheutz F, López R. Effect of smoking on periodontitis: a systematic review and meta-regression. Am J Prev Med. 2018;54(6):831–841. doi: 10.1016/j.amepre.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Holt SC, Ebersole JL. Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia: the “red complex”, a prototype polybacterial pathogenic consortium in periodontitis. Periodontol 2000. 2005;38:72–122. doi: 10.1111/j.1600-0757.2005.00113.x. [DOI] [PubMed] [Google Scholar]
- 9.Preshaw PM, Taylor JJ, Jaedicke KM, De Jager M, Bikker JW, Selten W, et al. Treatment of periodontitis reduces systemic inflammation in type 2 diabetes. J Clin Periodontol. 2020;47(6):737–746. doi: 10.1111/jcpe.13274. [DOI] [PubMed] [Google Scholar]
- 10.Martínez-García M, Hernández-Lemus E. Periodontal inflammation and systemic diseases: an overview. Front Physiol. 2021;12:709438. doi: 10.3389/fphys.2021.709438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schoeler M, Caesar R. Dietary lipids, gut microbiota and lipid metabolism. Rev Endocr Metab Disord. 2019;20(4):461–472. doi: 10.1007/s11154-019-09512-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belkaid Y, Harrison OJ. Homeostatic Immunity and the microbiota. Immunity. 2017;46(4):562–576. doi: 10.1016/j.immuni.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lloyd-Price J, Mahurkar A, Rahnavard G, Crabtree J, Orvis J, Hall AB, et al. Strains, functions and dynamics in the expanded human microbiome project. Nature. 2017;550(7674):61–66. doi: 10.1038/nature23889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med. 2016;375(24):2369–2379. doi: 10.1056/NEJMra1600266. [DOI] [PubMed] [Google Scholar]
- 15.Ganesan SM, Dabdoub SM, Nagaraja HN, Scott ML, Pamulapati S, Berman ML, et al. Adverse effects of electronic cigarettes on the disease-naive oral microbiome. Sci Adv. 2020;6(22):eaaz0108. doi: 10.1126/sciadv.aaz0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34(3):509–515. doi: 10.1161/ATVBAHA.113.300156. [DOI] [PubMed] [Google Scholar]
- 17.Pignatelli P, Fabietti G, Ricci A, Piattelli A, Curia MC. How periodontal disease and presence of nitric oxide reducing oral bacteria can affect blood pressure. Int J Mol Sci. 2020;21(20):7538. doi: 10.3390/ijms21207538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hills RD, Jr, Pontefract BA, Mishcon HR, Black CA, Sutton SC, Theberge CR. Gut microbiome: profound implications for diet and disease. Nutrients. 2019;11(7):1613. doi: 10.3390/nu11071613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barb JJ, Maki KA, Kazmi N, Meeks BK, Krumlauf M, Tuason RT, et al. The oral microbiome in alcohol use disorder: a longitudinal analysis during inpatient treatment. J Oral Microbiol. 2022;14(1):2004790. doi: 10.1080/20002297.2021.2004790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maki KA, Burke LA, Calik MW, Watanabe-Chailland M, Sweeney D, Romick-Rosendale LE, et al. Sleep fragmentation increases blood pressure and is associated with alterations in the gut microbiome and fecal metabolome in rats. Physiol Genom. 2020;52(7):280–292. doi: 10.1152/physiolgenomics.00039.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Durgan DJ, Ganesh BP, Cope JL, Ajami NJ, Phillips SC, Petrosino JF, et al. Role of the gut microbiome in obstructive sleep apnea-induced hypertension. Hypertension. 2016;67(2):469–474. doi: 10.1161/HYPERTENSIONAHA.115.06672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maki KA, Kazmi N, Barb JJ, Ames N. The oral and gut bacterial microbiomes: similarities, differences, and connections. Biol Res Nurs. 2021;23(1):7–20. doi: 10.1177/1099800420941606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilbert SA, Mark Welch JL, Borisy GG. Spatial ecology of the human tongue dorsum microbiome. Cell Rep. 2020;30(12):4003–15.e3. doi: 10.1016/j.celrep.2020.02.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Radaic A, Kapila YL. The oralome and its dysbiosis: new insights into oral microbiome-host interactions. Comput Struct Biotechnol J. 2021;19:1335–1360. doi: 10.1016/j.csbj.2021.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eren AM, Borisy GG, Huse SM, Mark Welch JL. Oligotyping analysis of the human oral microbiome. Proc Natl Acad Sci USA. 2014;111(28):E2875–E2884. doi: 10.1073/pnas.1409644111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hecht SS. Tobacco smoke carcinogens and lung cancer. J Natl Cancer Inst. 1999;91(14):1194–1210. doi: 10.1093/jnci/91.14.1194. [DOI] [PubMed] [Google Scholar]
- 27.Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972–1986. doi: 10.1161/CIRCULATIONAHA.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cheng T. Chemical evaluation of electronic cigarettes. Tob Control. 2014;23(Suppl 2):ii11–ii17. doi: 10.1136/tobaccocontrol-2013-051482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Javed F, Kellesarian SV, Sundar IK, Romanos GE, Rahman I. Recent updates on electronic cigarette aerosol and inhaled nicotine effects on periodontal and pulmonary tissues. Oral Dis. 2017;23(8):1052–1057. doi: 10.1111/odi.12652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagler R, Dayan D. The dual role of saliva in oral carcinogenesis. Oncology. 2006;71(1–2):10–17. doi: 10.1159/000100445. [DOI] [PubMed] [Google Scholar]
- 31.Petrušić N, Posavac M, Sabol I, Mravak-Stipetić M. The effect of tobacco smoking on salivation. Acta Stomatol Croat. 2015;49(4):309–315. doi: 10.15644/asc49/4/6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bui FQ, Almeida-da-Silva CLC, Huynh B, Trinh A, Liu J, Woodward J, et al. Association between periodontal pathogens and systemic disease. Biomed J. 2019;42(1):27–35. doi: 10.1016/j.bj.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cornejo Ulloa P, van der Veen MH, Krom BP. Review: modulation of the oral microbiome by the host to promote ecological balance. Odontology. 2019;107(4):437–448. doi: 10.1007/s10266-019-00413-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vallès Y, Inman CK, Peters BA, Ali R, Wareth LA, Abdulle A, et al. Types of tobacco consumption and the oral microbiome in the United Arab Emirates Healthy Future (UAEHFS) Pilot Study. Sci Rep. 2018;8(1):11327. doi: 10.1038/s41598-018-29730-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gopinath D, Wie CC, Banerjee M, Thangavelu L, Kumar RP, Nallaswamy D, et al. Compositional profile of mucosal bacteriome of smokers and smokeless tobacco users. Clin Oral Investig. 2022;26(2):1647–1656. doi: 10.1007/s00784-021-04137-7. [DOI] [PubMed] [Google Scholar]
- 36.Jia Y-J, Liao Y, He Y-Q, Zheng M-Q, Tong X-T, Xue W-Q, et al. Association between oral microbiota and cigarette smoking in the Chinese population. Front Cell Infect Microbiol. 2021;11:658203. doi: 10.3389/fcimb.2021.658203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Al-Zyoud W, Hajjo R, Abu-Siniyeh A, Hajjaj S. Salivary microbiome and cigarette smoking: a first of its kind investigation in Jordan. Int J Environ Res Public Health. 2019;17(1):256. doi: 10.3390/ijerph17010256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thomas AM, Gleber-Netto FO, Fernandes GR, Amorim M, Barbosa LF, Francisco AL, et al. Alcohol and tobacco consumption affects bacterial richness in oral cavity mucosa biofilms. BMC Microbiol. 2014;14:250. doi: 10.1186/s12866-014-0250-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duan X, Wu T, Xu X, Chen D, Mo A, Lei Y, et al. Smoking may lead to marginal bone loss around non-submerged implants during bone healing by altering salivary microbiome: a prospective study. J Periodontol. 2017;88(12):1297–1308. doi: 10.1902/jop.2017.160808. [DOI] [PubMed] [Google Scholar]
- 40.Murugesan S, Al Ahmad SF, Singh P, Saadaoui M, Kumar M, Al KS. Profiling the Salivary microbiome of the Qatari population. J Transl Med. 2020;18(1):127. doi: 10.1186/s12967-020-02291-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sato N, Kakuta M, Uchino E, Hasegawa T, Kojima R, Kobayashi W, et al. The relationship between cigarette smoking and the tongue microbiome in an East Asian population. J Oral Microbiol. 2020;12(1):1742527. doi: 10.1080/20002297.2020.1742527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Coretti L, Cuomo M, Florio E, Palumbo D, Keller S, Pero R, et al. Subgingival dysbiosis in smoker and non-smoker patients with chronic periodontitis. Mol Med Rep. 2017;15(4):2007–2014. doi: 10.3892/mmr.2017.6269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beghini F, Renson A, Zolnik CP, Geistlinger L, Usyk M, Moody TU, et al. Tobacco exposure associated with oral microbiota oxygen utilization in the New York City health and nutrition examination study. Ann Epidemiol. 2019;34:18–25.e3. doi: 10.1016/j.annepidem.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karabudak S, Ari O, Durmaz B, Dal T, Basyigit T, Kalcioglu MT, et al. Analysis of the effect of smoking on the buccal microbiome using next-generation sequencing technology. J Med Microbiol. 2019;68(8):1148–1158. doi: 10.1099/jmm.0.001003. [DOI] [PubMed] [Google Scholar]
- 45.Suzuki N, Nakano Y, Yoneda M, Hirofuji T, Hanioka T. The effects of cigarette smoking on the salivary and tongue microbiome. Clin Exp Dent Res. 2022;8(1):449–456. doi: 10.1002/cre2.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pushalkar S, Paul B, Li Q, Yang J, Vasconcelos R, Makwana S, et al. Electronic cigarette aerosol modulates the oral microbiome and increases risk of infection. iScience. 2020;23(3):100884. doi: 10.1016/j.isci.2020.100884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Renson A, Jones HE, Beghini F, Segata N, Zolnik CP, Usyk M, et al. Sociodemographic variation in the oral microbiome. Ann Epidemiol. 2019;35:73–80.e2. doi: 10.1016/j.annepidem.2019.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yeoh YK, Chan MH, Chen Z, Lam EWH, Wong PY, Ngai CM, et al. The human oral cavity microbiota composition during acute tonsillitis: a cross-sectional survey. BMC Oral Health. 2019;19(1):275. doi: 10.1186/s12903-019-0956-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shay E, Sangwan N, Padmanabhan R, Lundy S, Burkey B, Eng C. Bacteriome and mycobiome and bacteriome-mycobiome interactions in head and neck squamous cell carcinoma. Oncotarget. 2020;11(25):2375–2386. doi: 10.18632/oncotarget.27629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mukherjee PK, Chandra J, Retuerto M, Tatsuoka C, Ghannoum MA, McComsey GA. Dysbiosis in the oral bacterial and fungal microbiome of HIV-infected subjects is associated with clinical and immunologic variables of HIV infection. PLoS ONE. 2018;13(7):e0200285. doi: 10.1371/journal.pone.0200285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rodríguez-Rabassa M, López P, Rodríguez-Santiago RE, Cases A, Felici M, Sánchez R, et al. Cigarette smoking modulation of saliva microbial composition and cytokine levels. Int J Environ Res Public Health. 2018;15(11):2479. doi: 10.3390/ijerph15112479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lin D, Hutchison KE, Portillo S, Vegara V, Ellingson JM, Liu J, et al. Association between the oral microbiome and brain resting state connectivity in smokers. Neuroimage. 2019;200:121–131. doi: 10.1016/j.neuroimage.2019.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yeo LF, Aghakhanian FF, Tan JSY, Gan HM, Phipps ME. Health and saliva microbiomes of a semi-urbanized indigenous tribe in Peninsular Malaysia. F1000Res. 2019;8:175. doi: 10.12688/f1000research.17706.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hsiao JR, Chang CC, Lee WT, Huang CC, Ou CY, Tsai ST, et al. The interplay between oral microbiome, lifestyle factors and genetic polymorphisms in the risk of oral squamous cell carcinoma. Carcinogenesis. 2018;39(6):778–787. doi: 10.1093/carcin/bgy053. [DOI] [PubMed] [Google Scholar]
- 55.Sato N, Kakuta M, Hasegawa T, Yamaguchi R, Uchino E, Kobayashi W, et al. Metagenomic analysis of bacterial species in tongue microbiome of current and never smokers. NPJ Biofilms Microbiomes. 2020;6(1):11. doi: 10.1038/s41522-020-0121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gaetti-Jardim E, Jr, Jardim ECG, Schweitzer CM, da Silva JCL, Oliveira MM, Masocatto DC, et al. Supragingival and subgingival microbiota from patients with poor oral hygiene submitted to radiotherapy for head and neck cancer treatment. Arch Oral Biol. 2018;90:45–52. doi: 10.1016/j.archoralbio.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 57.Wolff D, Frese C, Schoilew K, Dalpke A, Wolff B, Boutin S. Amplicon-based microbiome study highlights the loss of diversity and the establishment of a set of species in patients with dentin caries. PLoS ONE. 2019;14(7):e0219714. doi: 10.1371/journal.pone.0219714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ganesan SM, Joshi V, Fellows M, Dabdoub SM, Nagaraja HN, O'Donnell B, et al. A tale of two risks: smoking, diabetes and the subgingival microbiome. ISME J. 2017;11(9):2075–2089. doi: 10.1038/ismej.2017.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Karasneh JA, Al Habashneh RA, Marzouka NA, Thornhill MH. Effect of cigarette smoking on subgingival bacteria in healthy subjects and patients with chronic periodontitis. BMC Oral Health. 2017;17(1):64. doi: 10.1186/s12903-017-0359-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Winning L, Patterson CC, Cullen KM, Stevenson KA, Lundy FT, Kee F, et al. The association between subgingival periodontal pathogens and systemic inflammation. J Clin Periodontol. 2015;42(9):799–806. doi: 10.1111/jcpe.12450. [DOI] [PubMed] [Google Scholar]
- 61.Pietiäinen M, Liljestrand JM, Kopra E, Pussinen PJ. Mediators between oral dysbiosis and cardiovascular diseases. Eur J Oral Sci. 2018;126(Suppl 1):26–36. doi: 10.1111/eos.12423. [DOI] [PubMed] [Google Scholar]
- 62.Priyamvara A, Dey AK, Bandyopadhyay D, Katikineni V, Zaghlol R, Basyal B, et al. Periodontal inflammation and the risk of cardiovascular disease. Curr Atheroscler Rep. 2020;22(7):28. doi: 10.1007/s11883-020-00848-6. [DOI] [PubMed] [Google Scholar]
- 63.Leskelä J, Pietiäinen M, Safer A, Lehto M, Metso J, Malle E, et al. Serum lipopolysaccharide neutralizing capacity in ischemic stroke. PLoS ONE. 2020;15(2):e0228806. doi: 10.1371/journal.pone.0228806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liljestrand JM, Paju S, Pietiäinen M, Buhlin K, Persson GR, Nieminen MS, et al. Immunologic burden links periodontitis to acute coronary syndrome. Atherosclerosis. 2018;268:177–184. doi: 10.1016/j.atherosclerosis.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 65.Ziebolz D, Rost C, Schmidt J, Waldmann-Beushausen R, Schöndube FA, Mausberg RF, et al. Periodontal bacterial DNA and their link to human cardiac tissue: findings of a pilot study. Thorac Cardiovasc Surg. 2018;66(1):83–90. doi: 10.1055/s-0035-1564689. [DOI] [PubMed] [Google Scholar]
- 66.Ziebolz D, Jahn C, Pegel J, Semper-Pinnecke E, Mausberg RF, Waldmann-Beushausen R, et al. Periodontal bacteria DNA findings in human cardiac tissue—is there a link of periodontitis to heart valve disease? Int J Cardiol. 2018;251:74–79. doi: 10.1016/j.ijcard.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 67.Kannosh I, Staletovic D, Toljic B, Radunovic M, Pucar A, Matic Petrovic S, et al. The presence of periopathogenic bacteria in subgingival and atherosclerotic plaques—an age related comparative analysis. J Infect Dev Ctries. 2018;12(12):1088–1095. doi: 10.3855/jidc.10980. [DOI] [PubMed] [Google Scholar]
- 68.Serra e Silva Filho W, Casarin RC, Nicolela EL, Jr, Passos HM, Sallum AW, Gonçalves RB. Microbial diversity similarities in periodontal pockets and atheromatous plaques of cardiovascular disease patients. PLoS ONE. 2014;9(10):e109761. doi: 10.1371/journal.pone.0109761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gordon JH, LaMonte MJ, Genco RJ, Zhao J, Li L, Hovey KM, et al. Is the oral microbiome associated with blood pressure in older women? High Blood Press Cardiovasc Prev. 2019;26(3):217–225. doi: 10.1007/s40292-019-00322-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fåk F, Tremaroli V, Bergström G, Bäckhed F. Oral microbiota in patients with atherosclerosis. Atherosclerosis. 2015;243(2):573–578. doi: 10.1016/j.atherosclerosis.2015.10.097. [DOI] [PubMed] [Google Scholar]
- 71.Mahalakshmi K, Krishnan P, Arumugam SB. “Association of periodontopathic anaerobic bacterial co-occurrence to atherosclerosis”—a cross-sectional study. Anaerobe. 2017;44:66–72. doi: 10.1016/j.anaerobe.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 72.Nikolaeva EN, Tsarev VN, Tsareva TV, Ippolitov EV, Arutyunov SD. Interrelation of cardiovascular diseases with anaerobic bacteria of subgingival biofilm. Contemp Clin Dent. 2019;10(4):637. doi: 10.4103/ccd.ccd_84_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Su CY, Shigeishi H, Nishimura R, Ohta K, Sugiyama M. Detection of oral bacteria on the tongue dorsum using PCR amplification of 16S ribosomal RNA and its association with systemic disease in middle-aged and elderly patients. Biomed Rep. 2019;10(1):70–76. doi: 10.3892/br.2018.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Koren O, Spor A, Felin J, Fåk F, Stombaugh J, Tremaroli V, et al. Human oral, gut, and plaque microbiota in patients with atherosclerosis. Proc Natl Acad Sci USA. 2011;108(Suppl 1):4592–4598. doi: 10.1073/pnas.1011383107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boaden E, Lyons M, Singhrao SK, Dickinson H, Leathley M, Lightbody CE, et al. Oral flora in acute stroke patients: a prospective exploratory observational study. Gerodontology. 2017;34(3):343–356. doi: 10.1111/ger.12271. [DOI] [PubMed] [Google Scholar]
- 76.Perry SE, Huckabee ML, Tompkins G, Milne T. The association between oral bacteria, the cough reflex and pneumonia in patients with acute stroke and suspected dysphagia. J Oral Rehabil. 2020;47(3):386–394. doi: 10.1111/joor.12903. [DOI] [PubMed] [Google Scholar]
- 77.Stöhr J, Barbaresko J, Neuenschwander M, Schlesinger S. Bidirectional association between periodontal disease and diabetes mellitus: a systematic review and meta-analysis of cohort studies. Sci Rep. 2021;11(1):13686. doi: 10.1038/s41598-021-93062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kudiyirickal MG, Pappachan JM. Diabetes mellitus and oral health. Endocrine. 2015;49(1):27–34. doi: 10.1007/s12020-014-0496-3. [DOI] [PubMed] [Google Scholar]
- 79.Tavares M, Lindefjeld Calabi KA, San ML. Systemic diseases and oral health. Dent Clin N Am. 2014;58(4):797–814. doi: 10.1016/j.cden.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 80.Carrizales-Sepúlveda EF, Ordaz-Farías A, Vera-Pineda R, Flores-Ramírez R. Periodontal disease, systemic inflammation and the risk of cardiovascular disease. Heart Lung Circ. 2018;27(11):1327–1334. doi: 10.1016/j.hlc.2018.05.102. [DOI] [PubMed] [Google Scholar]
- 81.Liljestrand JM, Paju S, Buhlin K, Persson GR, Sarna S, Nieminen MS, et al. Lipopolysaccharide, a possible molecular mediator between periodontitis and coronary artery disease. J Clin Periodontol. 2017;44(8):784–792. doi: 10.1111/jcpe.12751. [DOI] [PubMed] [Google Scholar]
- 82.Zhang B, Wang X, Xia R, Li C. Gut microbiota in coronary artery disease: a friend or foe? Biosci Rep. 2020;40(5):BSR20200454. doi: 10.1042/BSR20200454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pussinen PJ, Kopra E, Pietiäinen M, Lehto M, Zaric S, Paju S, et al. Periodontitis and cardiometabolic disorders: the role of lipopolysaccharide and endotoxemia. Periodontol 2000. 2022;89(1):19–40. doi: 10.1111/prd.12433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hoffman KL, Hutchinson DS, Fowler J, Smith DP, Ajami NJ, Zhao H, et al. Oral microbiota reveals signs of acculturation in Mexican American women. PLoS ONE. 2018;13(4):e0194100. doi: 10.1371/journal.pone.0194100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Della Corte V, Tuttolomondo A, Pecoraro R, Di Raimondo D, Vassallo V, Pinto A. Inflammation, endothelial dysfunction and arterial stiffness as therapeutic targets in cardiovascular medicine. Curr Pharm Des. 2016;22(30):4658–4668. doi: 10.2174/1381612822666160510124801. [DOI] [PubMed] [Google Scholar]
- 86.Sproston NR, Ashworth JJ. Role of C-reactive protein at sites of inflammation and infection. Front Immunol. 2018;9:754. doi: 10.3389/fimmu.2018.00754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gallus S, Lugo A, Suatoni P, Taverna F, Bertocchi E, Boffi R, et al. Effect of tobacco smoking cessation on C-reactive protein levels in a cohort of low-dose computed tomography screening participants. Sci Rep. 2018;8(1):12908. doi: 10.1038/s41598-018-29867-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bergmann OJ. Oral infections and septicemia in immunocompromised patients with hematologic malignancies. J Clin Microbiol. 1988;26(10):2105–2109. doi: 10.1128/jcm.26.10.2105-2109.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Greenberg MS, Cohen SG, McKitrick JC, Cassileth PA. The oral flora as a source of septicemia in patients with acute leukemia. Oral Surg Oral Med Oral Pathol. 1982;53(1):32–36. doi: 10.1016/0030-4220(82)90483-2. [DOI] [PubMed] [Google Scholar]
- 90.Del Giudice M, Gangestad SW. Rethinking IL-6 and CRP: why they are more than inflammatory biomarkers, and why it matters. Brain Behav Immun. 2018;70:61–75. doi: 10.1016/j.bbi.2018.02.013. [DOI] [PubMed] [Google Scholar]
- 91.Joshi V, Matthews C, Aspiras M, de Jager M, Ward M, Kumar P. Smoking decreases structural and functional resilience in the subgingival ecosystem. J Clin Periodontol. 2014;41(11):1037–1047. doi: 10.1111/jcpe.12300. [DOI] [PubMed] [Google Scholar]
- 92.Petković AB, Matić SM, Stamatović NV, Vojvodić DV, Todorović TM, Lazić ZR, et al. Proinflammatory cytokines (IL-1beta and TNF-alpha) and chemokines (IL-8 and MIP-1alpha) as markers of peri-implant tissue condition. Int J Oral Maxillofac Surg. 2010;39(5):478–485. doi: 10.1016/j.ijom.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 93.Tang ZZ, Chen G, Hong Q, Huang S, Smith HM, Shah RD, et al. Multi-omic analysis of the microbiome and metabolome in healthy subjects reveals microbiome-dependent relationships between diet and metabolites. Front Genet. 2019;10:454. doi: 10.3389/fgene.2019.00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Waløen K, Kleppe R, Martinez A, Haavik J. Tyrosine and tryptophan hydroxylases as therapeutic targets in human disease. Expert Opin Ther Targets. 2017;21(2):167–180. doi: 10.1080/14728222.2017.1272581. [DOI] [PubMed] [Google Scholar]
- 95.Takahashi N. Oral microbiome metabolism: from “who are they?” to “what are they doing?”. J Dent Res. 2015;94(12):1628–1637. doi: 10.1177/0022034515606045. [DOI] [PubMed] [Google Scholar]
- 96.Musharraf SG, Shahid N, Naqvi SMA, Saleem M, Siddiqui AJ, Ali A. Metabolite profiling of preneoplastic and neoplastic lesions of oral cavity tissue samples revealed a biomarker pattern. Sci Rep. 2016;6:38985. doi: 10.1038/srep38985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Goel R, Gheena S, Chandrasekhar T, Ramani P, Sherlin HJ, Natesan A, et al. Amino acid profile in oral submucous fibrosis: a high performance liquid chromatography (HPLC) study. J Clin Diagn Res. 2014;8(12):ZC44–ZC48. doi: 10.7860/JCDR/2014/10201.5290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yu G, Phillips S, Gail MH, Goedert JJ, Humphrys MS, Ravel J, et al. The effect of cigarette smoking on the oral and nasal microbiota. Microbiome. 2017;5(1):3. doi: 10.1186/s40168-016-0226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Murr C, Grammer TB, Kleber ME, Meinitzer A, März W, Fuchs D. Low serum tryptophan predicts higher mortality in cardiovascular disease. Eur J Clin Invest. 2015;45(3):247–254. doi: 10.1111/eci.12402. [DOI] [PubMed] [Google Scholar]
- 100.Wang H, Funchain P, Bebek G, Altemus J, Zhang H, Niazi F, et al. Microbiomic differences in tumor and paired-normal tissue in head and neck squamous cell carcinomas. Genome Med. 2017;9(1):14. doi: 10.1186/s13073-017-0405-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hao Y, Wang Y, Xi L, Li G, Zhao F, Qi Y, et al. A nested case–control study of association between metabolome and hypertension risk. Biomed Res Int. 2016;2016:7646979. doi: 10.1155/2016/7646979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jennings A, MacGregor A, Welch A, Chowienczyk P, Spector T, Cassidy A. Amino acid intakes are inversely associated with arterial stiffness and central blood pressure in women. J Nutr. 2015;145(9):2130–2138. doi: 10.3945/jn.115.214700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ormstad H, Verkerk R, Aass HC, Amthor KF, Sandvik L. Inflammation-induced catabolism of tryptophan and tyrosine in acute ischemic stroke. J Mol Neurosci. 2013;51(3):893–902. doi: 10.1007/s12031-013-0097-2. [DOI] [PubMed] [Google Scholar]
- 104.Whiteson K, Agrawal S, Agrawal A. Differential responses of human dendritic cells to metabolites from the oral/airway microbiome. Clin Exp Immunol. 2017;188(3):371–379. doi: 10.1111/cei.12943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Steffen BT, Duprez D, Szklo M, Guan W, Tsai MY. Circulating oleic acid levels are related to greater risks of cardiovascular events and all-cause mortality: the multi-ethnic study of atherosclerosis. J Clin Lipidol. 2018;12(6):1404–1412. doi: 10.1016/j.jacl.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lin YT, Salihovic S, Fall T, Hammar U, Ingelsson E, Ärnlöv J, et al. Global plasma metabolomics to identify potential biomarkers of blood pressure progression. Arterioscler Thromb Vasc Biol. 2020;40(8):e227–e237. doi: 10.1161/ATVBAHA.120.314356. [DOI] [PubMed] [Google Scholar]
- 107.Sniderman AD, Thanassoulis G, Glavinovic T, Navar AM, Pencina M, Catapano A, et al. Apolipoprotein B particles and cardiovascular disease: a narrative review. JAMA Cardiol. 2019;4(12):1287–1295. doi: 10.1001/jamacardio.2019.3780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Paynter NP, Balasubramanian R, Giulianini F, Wang DD, Tinker LF, Gopal S, et al. Metabolic predictors of incident coronary heart disease in women. Circulation. 2018;137(8):841–853. doi: 10.1161/CIRCULATIONAHA.117.029468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kispert S, Marentette J, McHowat J. Cigarette smoking promotes bladder cancer via increased platelet-activating factor. Physiol Rep. 2019;7(3):e13981. doi: 10.14814/phy2.13981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Miyashita L, Suri R, Dearing E, Mudway I, Dove RE, Neill DR, et al. E-cigarette vapour enhances pneumococcal adherence to airway epithelial cells. Eur Respir J. 2018;51(2):1701592. doi: 10.1183/13993003.01592-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nagaoka K, Yanagihara K, Morinaga Y, Nakamura S, Harada T, Hasegawa H, et al. Prevotella intermedia induces severe bacteremic pneumococcal pneumonia in mice with upregulated platelet-activating factor receptor expression. Infect Immun. 2014;82(2):587–593. doi: 10.1128/IAI.00943-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chi NF, Chang TH, Lee CY, Wu YW, Shen TA, Chan L, et al. Untargeted metabolomics predicts the functional outcome of ischemic stroke. J Formos Med Assoc. 2021;120(1 Pt 1):234–241. doi: 10.1016/j.jfma.2020.04.026. [DOI] [PubMed] [Google Scholar]
- 113.Vanhatalo A, Blackwell JR, L'Heureux JE, Williams DW, Smith A, van der Giezen M, et al. Nitrate-responsive oral microbiome modulates nitric oxide homeostasis and blood pressure in humans. Free Radic Biol Med. 2018;124:21–30. doi: 10.1016/j.freeradbiomed.2018.05.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Förstermann U, Xia N, Li H. Roles of vascular oxidative stress and nitric oxide in the pathogenesis of atherosclerosis. Circ Res. 2017;120(4):713–735. doi: 10.1161/CIRCRESAHA.116.309326. [DOI] [PubMed] [Google Scholar]
- 115.Hyde ER, Andrade F, Vaksman Z, Parthasarathy K, Jiang H, Parthasarathy DK, et al. Metagenomic analysis of nitrate-reducing bacteria in the oral cavity: implications for nitric oxide homeostasis. PLoS ONE. 2014;9(3):e88645. doi: 10.1371/journal.pone.0088645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Morou-Bermúdez E, Torres-Colón JE, Bermúdez NS, Patel RP, Joshipura KJ. Pathways linking oral bacteria, nitric oxide metabolism, and health. J Dent Res. 2022 doi: 10.1177/00220345211064571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kapil V, Haydar SM, Pearl V, Lundberg JO, Weitzberg E, Ahluwalia A. Physiological role for nitrate-reducing oral bacteria in blood pressure control. Free Radic Biol Med. 2013;55:93–100. doi: 10.1016/j.freeradbiomed.2012.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hopper CP, De La Cruz LK, Lyles KV, Wareham LK, Gilbert JA, Eichenbaum Z, et al. Role of carbon monoxide in host–gut microbiome communication. Chem Rev. 2020;120(24):13273–13311. doi: 10.1021/acs.chemrev.0c00586. [DOI] [PubMed] [Google Scholar]
- 119.Hopper CP, Zambrana PN, Goebel U, Wollborn J. A brief history of carbon monoxide and its therapeutic origins. Nitric Oxide. 2021;111–112:45–63. doi: 10.1016/j.niox.2021.04.001. [DOI] [PubMed] [Google Scholar]
- 120.Naito Y, Takagi T, Uchiyama K, Katada K, Yoshikawa T. Multiple targets of carbon monoxide gas in the intestinal inflammation. Arch Biochem Biophys. 2016;595:147–152. doi: 10.1016/j.abb.2015.06.020. [DOI] [PubMed] [Google Scholar]
- 121.Rosier BT, Takahashi N, Zaura E, Krom BP, MartÍnez-Espinosa RM, van Breda SGJ, et al. The importance of nitrate reduction for oral health. J Dent Res. 2022 doi: 10.1177/00220345221080982. [DOI] [PubMed] [Google Scholar]
- 122.Vanhatalo A, L'Heureux JE, Kelly J, Blackwell JR, Wylie LJ, Fulford J, et al. Network analysis of nitrate-sensitive oral microbiome reveals interactions with cognitive function and cardiovascular health across dietary interventions. Redox Biol. 2021;41:101933. doi: 10.1016/j.redox.2021.101933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dewhurst-Trigg R, Yeates T, Blackwell JR, Thompson C, Linoby A, Morgan PT, et al. Lowering of blood pressure after nitrate-rich vegetable consumption is abolished with the co-ingestion of thiocyanate-rich vegetables in healthy normotensive males. Nitric Oxide. 2018;74:39–46. doi: 10.1016/j.niox.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 124.Maki KA, Diallo AF, Lockwood MB, Franks AT, Green SJ, Joseph PV. Considerations when designing a microbiome study: implications for nursing science. Biol Res Nurs. 2019;21(2):125–141. doi: 10.1177/1099800418811639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Green SJ, Venkatramanan R, Naqib A. Deconstructing the polymerase chain reaction: understanding and correcting bias associated with primer degeneracies and primer-template mismatches. PLoS ONE. 2015;10(5):e0128122. doi: 10.1371/journal.pone.0128122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Grieshober L, Graw S, Barnett MJ, Thornquist MD, Goodman GE, Chen C, et al. AHRR methylation in heavy smokers: associations with smoking, lung cancer risk, and lung cancer mortality. BMC Cancer. 2020;20(1):905. doi: 10.1186/s12885-020-07407-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bojesen SE, Timpson N, Relton C, Davey Smith G, Nordestgaard BG. AHRR (cg05575921) hypomethylation marks smoking behaviour, morbidity and mortality. Thorax. 2017;72(7):646–653. doi: 10.1136/thoraxjnl-2016-208789. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: PubMed search strategy and search terms.
Additional file 2: Oral microbiome bacteria, bacteria response in association with smoking, oral sampling site location and citations from reviewed studies.
Additional file 3: Oral microbiome bacteria, bacteria response in association with cardiovascular-associated risk measure or disease, oral sampling site location and citations from reviewed studies.
Additional file 4: Shared and unique responses to cigarette smoking, e-cigarette smoking and cardiovascular risk/disease stratified by increased and decreased bacterial relative abundance associations.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and the Additional files.