Abstract
Background
Healthy diet, exercise, and sleep practices may mitigate stress and prevent illness. However, lifestyle behaviors of acute care nurses working during stressful COVID-19 surges are unclear.
Purpose
To quantify sleep, diet, and exercise practices of 12-hour acute care nurses working day or night shift during COVID-19-related surges.
Methods
Nurses across 10 hospitals in the United States wore wrist actigraphs and pedometers to quantify sleep and steps and completed electronic diaries documenting diet over 7-days.
Findings
Participant average sleep quantity did not meet national recommendations; night shift nurses (n = 23) slept significantly less before on-duty days when compared to day shift nurses (n = 34). Proportionally more night shift nurses did not meet daily step recommendations. Diet quality was low on average among participants.
Discussion
Nurses, especially those on night shift, may require resources to support healthy sleep hygiene, physical activity practices, and diet quality to mitigate stressful work environments.
Keywords: Diet, Sleep, Exercise, Nurses, Shift-workers, COVID-19
1. Introduction
Nurses represent a critical and essential component of the health care team. Support of both short and long-term health of nurses is imperative to ensure an adequate workforce is available to provide vital healthcare services to community members across the spectrum of wellbeing and illness. Studies have demonstrated an inherent connection between self-care activities of physical activity (PA), diet quality, sleep hygiene, and physical/mental health in the nursing workforce (Berent et al., 2021; Jiang et al., 2021; Mazurek Melnyk et al., 2022). For example, high-quality sleep, healthy eating habits, and regular physical activity are associated with a reduced risk of psychological conditions such as stress and burnout (Fitzpatrick & Valentine, 2021) and lower risk for all-cause mortality (Saeidifard et al., 2019; Sotos-Prieto et al., 2017; Yin et al., 2017). Despite advanced health knowledge and the professional expectation to provide healthy diet, physical activity, and sleep education to patients, nurses do not always follow national recommendations for health-promoting behaviors (Priano et al., 2018), increasing risk for negative physical and emotional conditions.
According to Orem's theory of self-care (Denyes et al., 2001), individual patterns of engaging in self-care activities such as adequate sleep, diet and exercise, are influenced by personal attributes (i.e. age, gender), environmental situations such as occupational stress, self-efficacy, and ability to act on self-care needs. The COVID-19 pandemic has caused lasting emotional strain on nurses working in hospitals and, according to Orem's theory of self-care, nursing ability to engage in self-care activities may have suffered as a result. Reasons creating increased stress on nurses included fear of at-work COVID-19 exposure, personal illness with the virus, and infecting family members and friends (Cui et al., 2020; Kellogg et al., 2021). Inadequate personal protective equipment supply was also reported as an emotional stressor (Kellogg et al., 2021), along with critical short staffing situations that continue today (Galanis et al., 2021). Witnessing unprecedented, sudden clinical deterioration and death (Cui et al., 2020) in the context of extreme visitor limitations leaving patients isolated and dying alone (Kellogg et al., 2021) also created emotional turmoil. Finally, public misperceptions of the lived experience of working during the COVID-19 pandemic as a direct patient care nurse (Cui et al., 2020) is cited as a reason that the acute care nursing workforce has reported a disproportionate amount of stress since the COVID-19 pandemic (Al Maqbali et al., 2021; Sriharan et al., 2021). Individuals experiencing high levels of stress and fatigue may report worsened sleep quantity and quality (Al Maqbali et al., 2021; Cui et al., 2020; Neculicioiu et al., 2022), diet quality (Khubchandani et al., 2020), and physical activity (Is et al., 2021), threatening overall wellbeing.
There is an urgent call to action to mitigate nursing fatigue to support nursing and patient safety and wellbeing (Caruso et al., 2019). Measuring changes to sleep, diet, and physical activity during times of high stress such as the COVID-19 pandemic is warranted as a first step to inform targeted wellness strategies. Wearable fitness trackers and smartphones allow for objective, valid, and reliable collection of lifestyle behaviors data including sleep duration, quality, and efficiency (Fuller et al., 2020), diet quality and composition (Zhang et al., 2021), and number of steps walked per day (Guillodo et al., 2020; Jin et al., 2022). Mobile applications empower individuals to self-report sleep, diet, and physical activity habits daily into electronic repositories (Jin et al., 2022). Despite the relative abundance of wearable devices and smartphone applications for documenting self-care activities, few studies reported using technology to remotely measure the self-care activities of registered nurses during COVID-19 (Vigoureux et al., 2022). The purpose of this observational research was to use Orem's theory of self-care as a lens to describe sleep, diet, and physical activity habits of registered nurses working 12-h shifts in hospitals following the onset of the COVID-19 pandemic using wearable devices and validated smartphone applications. Secondary aims included 1) determine if differences in socio-demographics, lifestyle behaviors or stress were noted between nurses working night versus day shifts, and 2) test for correlations between lifestyle behaviors and stress.
2. Methods
2.1. Study design and settings
Nurses were recruited remotely to participate in this observational, week-long study between November 2020 and September 2021 from ten hospitals in three states: Washington, California, and Texas. Registered nurses provided sleep, diet, and physical activity data using smartphone applications and wearable tracking devices for one week, and completed surveys capturing demographics, stress, and sleep metrics.
2.2. Participants
RNs working full-time (totaling six shifts and 72 h every 14 days), 12-hour day or night shifts (not alternating) in the hospital who were not pregnant, breastfeeding, or reporting a chronic illness and owned a smartphone were eligible to participate.
2.3. Procedures
Registered Nurse study sponsors at 10 urban hospitals within a large health system posted approved recruitment flyers containing a brief study description and a quick response (QR) code that led to an electronic screening form. Recruitment across sites was phased. Three hospitals in Washington began recruitment first followed by five hospitals in California and finally the two hospitals in Texas advertised the study. Flyers were removed from all sites by the end of September 2021 once enough participants consented. Eligible, self-screened RNs were emailed a link to an electronic consent form. After e-consenting, participants were assigned a study identification (ID) number and were emailed a document detailing how to track their personal health habits per study protocol. Additional instructions on protocol adherence were provided via an interactive, online module, and each participant received a phone call from researchers to describe the protocol, clarify questions, and coordinate mailing of study supplies. Supplies needed for this study included actigraphs, pedometers, and measuring tape, including a prepaid return shipping package for those RNs who did not already have monitoring devices.
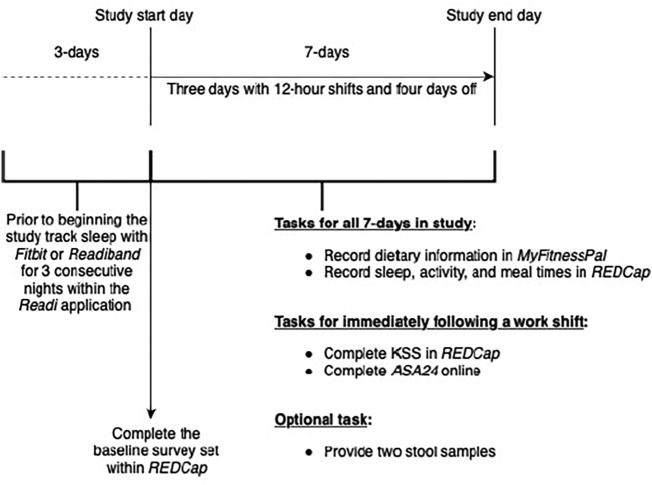
Participants completed four tasks during the study protocol. The first task was entering demographics, sleep quality measures, self-reported physical activity, stress measures, and items measuring COVID-19's impact on lifestyle behaviors into REDCap. The second task involved wearing a wrist actigraph daily for 10 days (three control nights, then seven days coinciding with three on-duty and four off-duty time periods). The third task required participants to record three completed post-shift ASA24 diet recalls. The final task was to input seven consecutive days of sleep timing (onset and wake), meal timing, shift condition (on-duty versus off-duty) and total steps walked into log sheets within REDCap (Fig. 1 ).
Fig. 1.
Study tasks and timing for participants.
2.4. Measurements
Study variables of interest included: 1. demographics, including the perceived impact of COVID-19 on self-care activities, 2. sleep, 3. diet quality, 4. physical activity, and 5. perceived stress.
2.4.1. Socio-demographic characteristics
Baseline and daily data logs were entered into Research Electronic Data Capture (REDCap) by the participant (Harris et al., 2009). Demographics (age range, gender, education, shift worked, waist circumference, height and weight) were collected during the baseline survey. Body Mass Index (BMI) was calculated using participant reported height and weight.
The impact of COVID-19 on self-care activities was assessed through author-created items asking whether diet quality, sleep quantity, sleep quality, and physical activity (respectively) worsened, stayed the same, or improved since the onset of COVID-19.
2.4.2. Sleep
Objective sleep data were collected via a wrist actigraph (either a researcher-supplied ReadiBand or participant-owned wearable device compatible with the ReadiOne system which measured sleep quality, sleep quantity, and sleep efficiency). Data were downloaded from the wrist actigraph into the ReadiOne smartphone application (Fatigue Sciences). The sleep data provided by the Fatigue Science Corporation have been shown to be valid (Russell et al., 2000) and reliable (Driller et al., 2016). Subjective sleep data included the Revised Morningness-Eveningness Questionnaire (rMEQ) which is a 5-item valid and reliable survey that measures one's preference to rise early in the morning, later in the day, or to report no affinity for when to wake up (Chelminski et al., 2000). In our study, this measure had a Cronbach's alpha of 0.73, demonstrating strong reliability.
2.4.3. Diet
Dietary intake was measured using the valid and reliable Automated Self-Administered Recall System (ASA24) 24-hour diet recall daily during on-duty time periods (Thompson et al., 2015). Detailed dietary intake was calculated in this platform which researchers used to quantify a diet quality scored called the Healthy Eating Index (HEI) (Reedy et al., 2018).
2.4.4. Physical activity
Physical activity was self-reported during the baseline survey using the International Physical Activity Questionnaire (IPAQ). Participants monitored their steps daily during the study period using a researcher-supplied pedometer or participant-owned wrist pedometer by entering total daily steps into a REDCap survey, a valid and reliable method for collecting step data (Prince et al., 2008).
2.4.5. Stress
Stress was measured using the valid and reliable Perceived Stress Scale (PSS-4) during the baseline survey (Abdulameer et al., 2019). In our study, this scale demonstrated a strong Cronbach's alpha of 0.78.
2.5. Data analysis
Data were collected between November 2020 and September 2021 and were reviewed to ensure participant completion of each study task. Due to data being collected from multiple sources, all data exports were concatenated using participant ID as the key identifier. The concatenation process started with the export of data files from all sources (REDCap, ReadiOne, and ASA24) after completion of the data collection portion of the study. Once the uniformity of participant ID was completed, exports were uploaded into a local project server in the database management tool PostgreSQL via pgAdmin. Exports of the cleaned, complete dataset were then used for the analysis process.
Analyses were conducted within SPSS Statistics by IBM Corp version 27 (2020). Categorical variables were described with counts and percentages while numeric variables were described with means and standard deviations. Chi-square tests were completed to assess any significant differences in completing the study for categorical variables; effect size (phi) was also calculated and reported. Independent t-tests were conducted for continuous data with Cohen's d for effect size reporting among normally distributed continuous variables. All tests were conducted as two-tailed to remain conservative, with a p-value of 0.05 or less regarded as a significant finding.
To quantify the number of days the goals were reached, endpoints for sleep (minutes asleep), diet (HEI score), and physical activity (step count and IPAQ score) were categorized into “met goal” or “did not meet goal.” The goal for daily sleep was set at a lower limit of 450 min (7.5 h) due to the National Sleep Foundation's (2020) current recommendation. The HEI goal was set at a score of over 80 per recommendations, while scores between 51 and 79 indicated “needs improvement,” and anything 50 or lower was considered a “very poor” diet (Reedy et al., 2018). The researchers dichotomized reaching the daily step goal as a step value of >7000 steps versus less than this goal (Paluch et al., 2021). Furthermore, nurses were categorized as meeting national physical activity guidelines if reporting 150 min of moderate intensity, 75 min of vigorous intensity, or 150 min of combined intensities on the IPAQ (U.S. Department of Health and Human Services, 2018). Finally, the proportion of nurses who reported that self-care behaviors had worsened since COVID-19 were categorized as having a negative lifestyle change due to the pandemic.
Last, correlations were run between continuous, numeric variables via the Pearson's Correlation Coefficient (PCC). Significant correlations with sleep (minutes asleep or rMEQ score), diet (HEI score), or physical activity (step count) were reported with the PCC, also known as “r”, and a p-value.
2.6. Ethical review
The study received institutional review board (IRB) approval from the Principal Investigator's healthcare institutional system. All participants provided electronic informed consent prior to initiating the protocol and received a gift card ($50) upon completion.
3. Results
3.1. Participant socio-demographic characteristics
A total of 57 nurses participated (Table 1 ). Most of the nurses were female (82.5 %), had a bachelor's degree (77.2 %), had been working their current shift over four years (M = 4.16; SD = 5.22), and reported a stress score of 5.98 on the 16-point scale (SD = 2.79). Most responders indicated that the COVID-19 pandemic did not have an impact on the amount or quality of sleep they were getting each day (70.2 % and 71.9 % reporting no differences, respectively), with no difference in responses between day shift and night shift nurses. Nearly half of responding nurses (47.4 %) reported they were exercising less when compared to pre-pandemic times with no between-shift differences in answers. Finally, many participating nurses (42.1 %) reported their diet had worsened since the start of the COVID-19 pandemic compared to staying the same or improving. Significantly more night shift nurses reported having their diet negatively impacted than those working the day shift (X 2 = 5.88; p = 0.05).
Table 1.
Study participant characteristics.
| All nurses (N = 57) |
Day shift nurses (n = 34) |
Night shift nurses (n = 23) |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Age Range 21 to 30 years 31 to 40 years 41 to 50 years 51 to 60 years |
18 25 8 6 |
31.6 43.9 14 10.5 |
7 17 5 5 |
20.6 50 14.7 14.7 |
11 8 3 1 |
47.8 34.8 13 4.3 |
| Gender Female Male |
47 10 |
82.5 17.5 |
24 6 |
70.6 29.4 |
19 4 |
82.6 17.4 |
| Highest RN Degree Associates Bachelors Masters |
9 44 4 |
15.8 77.2 7 |
7 24 3 |
20.6 70.6 8.8 |
2 20 1 |
8.7 87 4.3 |
| Met PA Guidelines Yes No Missing |
32 21 4 |
60.4 39.6 7 |
20 13 1 |
60.6 39.4 2.9 |
12 8 3 |
60 40 13 |
| M ± SD | M ± SD | M ± SD | ||||
| Months Working Current Shift | 49.91 ± 62.67 | 40.21 ± 39.25 | 64.26 ± 85.59 | |||
| Body Mass Index in kg/m2 | 26.22 ± 5.83 | 25.4 ± 5.08 | 27.43 ± 6.72 | |||
| Waist Circumference in inches | 33.75 ± 6.13 | 33.61 ± 6.31 | 33.95 ± 6.02 | |||
| Perceived Stress Scale Score | 5.98 ± 2.79 | 5.91 ± 2.73 | 6.09 ± 2.94 | |||
| Reduced Morningness-Eveningness Questionnaire Score | 14.75 ± 4.24 | 15.74 ± 3.93⁎ | 13.3 ± 4.34⁎ | |||
| Recorded Minutes of Daily Sleep† | 410.75 ± 125.04 | 409.24 ± 106.98 | 412.54 ± 144.1 | |||
| Recorded Daily Step Count‡ | 8429.01 ± 5240.47 | 8732.09 ± 5178.46 | 8016.4 ± 5324.68 | |||
| Healthy Eating Index Score during Workdays§ | 58.54 ± 10.91 | 59.51 ± 11.26 | 56.73 ± 10.34 | |||
p < 0.05; Abbreviations: Mean plus or minus Standard Deviation (M ± SD); p-value (p).
Forty-one participants provided sleep data over an average of 5.88 days (SD: 1.81).
Fifty-four participants provided step data over an average of 6.83 days (SD: 0.47).
Forty-six participants provided diet data over an average of 2.41 on-duty days (SD: 0.83).
3.2. Sleep findings
On the baseline survey, participant self-reported daily sleep quantity averaged 417 min (7.0 h; SD = 74.4) with day shift (m = 409.2 min; 6.8 h; SD = 72.6) and night shift (m = 429 min; 7.15 h; SD = 77.4) estimations being similar. According to sleep actigraphy data (see Table 1) mean daily sleep totaled 410.75 min (6.8 h; SD = 125.04) across the sample while no difference was found between day shift (m = 409.24 min; SD = 106.98) and night shift (m = 412.54; SD = 144.1) nurses. On the rMEQ sleep measurement, day shift nurses (n = 34) scored significantly higher (m = 15.74) than night shift (n = 23; m = 13.3) nurses (p = 0.032), indicating a preference to rise earlier in the day.
Day shift nurses attained similar amounts of sleep during both on-duty and off-duty time periods, while night shift nurses did not (see Table 2 ). Individuals working the day shift averaged 406.33 min (6.8 h) of sleep daily (SD = 96.2) during on-duty time periods and 411.43 min (6.9 h) of sleep (SD = 115.08) during off-duty time periods (p = 0.796). Nurses working the night shift averaged only 366.44 min (6.1 h) of sleep (SD = 151.29) during on-duty time periods while sleeping significantly more (448.93 min; 7.5 h; SD = 128.11) during off-duty time periods (p = 0.004). The proportion of day shift nurses who reached recommended sleep quantity between on-duty and off-duty time periods did not differ; however, night shift nurses were significantly less likely to meet the goal during on-duty time periods compared to off-duty time periods (X 2 = 14.27; p < 0.001). During off-duty time periods, significantly more RNs working nights reached the sleep goal compared to those working days (X 2 = 7.39; p = 0.007) (see Table 3 ).
Table 2.
Differences in sleep quantity between on and off-duty days for day and night shift nurses.
| On-duty days (M ± SD) |
Off-duty days (M ± SD) |
On-duty – off-duty between group differences |
|||
|---|---|---|---|---|---|
| Mean difference | p-Value | Cohen's d | |||
| Average daily minutes of sleep | |||||
| Day shift nurses (n = 23) | 406.33 ± 96.2 | 411.43 ± 115.08 | 5.11 | 0.796 | 0.048 |
| Night shift nurses (n = 18) | 366.44 ± 151.29 | 448.93 ± 128.11 | 82.49 | 0.004⁎ | 0.594 |
Abbreviations: Mean plus or minus Standard Deviation (M ± SD).
p < 0.05.
Table 3.
Nightly sleep quantity goals met for day and night shift nurses over study.
| Day shift nurses (n = 23) |
Night shift nurses (n = 18) |
Day shift – night shift between group differences |
|||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | X2 | p-Value | Phi | |
| Met daily sleep goal (7.5 h) | |||||||
| All study days | |||||||
| Yes | 35 | 28.9 | 39 | 38.2 | 2.16 | 0.141 | 0.098 |
| No | 86 | 71.1 | 63 | 61.8 | |||
| On-duty day observations | |||||||
| Yes | 14 | 26.9 | 8 | 17.8 | 1.15 | 0.283 | 0.109 |
| No | 38 | 73.1 | 37 | 82.2 | |||
| Off-duty day observations | |||||||
| Yes | 21 | 30.4 | 31 | 54.4 | 7.39 | 0.007⁎ | 0.242 |
| No | 48 | 69.6 | 26 | 45.6 | |||
| On-duty – off-duty between group differences | |||||||
| X2 | 0.18 | 14.27 | |||||
| p-Value | 0.673 | <0.001⁎ | |||||
| Phi | 0.038 | 0.374 | |||||
Abbreviations: Percent (%); Chi-square (X2).
p < 0.05.
3.3. Diet findings
Nurses had an average Healthy Eating Index score of 58.54 (SD = 10.91) during on-duty time periods (see Table 1) with no significant differences between day shift and night shift nurses. During the study period, a score of >80 (the cut-off for an optimal diet) was only recorded twice (1.75 %) while a score lower than 50 was recorded 33 times (28.9 %). Nearly one-quarter (23.9 %) of participating nurses averaged a Healthy Eating Index score below 50.
3.4. Physical activity (step) findings
Nurses in the sample averaged 8429.01 steps per day (SD = 5240.47) with no difference between day shift (m = 8732.09; SD = 5178.46) and night shift (m = 8016.4; SD = 5324) (see Table 1). All participants averaged 10,587.84 steps daily (SD = 5441.52) during on-duty time periods and 6756.88 steps (SD = 4419.82) during off-duty time periods (p < 0.001). Both groups of nurses averaged significantly more steps during on-duty than off-duty time periods (see Table 4 ). Day shift nurses averaged greater step counts during both on-duty and off-duty time periods compared to night shift nurses, although not statistically significant (see Table 4). A similar relationship was noted when using a cut-off of 7000-steps daily, with a greater percentage of day shift nurses reaching the step goal across all study time periods (see Table 5 ). A significantly smaller proportion of night shift nurses met the step goal during on-duty time periods when compared to day shift nurses. Using the IPAQ, 39.4 % of day shift nurses (n = 13) and 40 % of night shift nurses (n = 8) reported engaging in insufficient minutes of physical activity in the prior 7 days according to national recommendations (p > 0.05).
Table 4.
Differences in average daily step count between on and off-duty days for day and night shift nurses.
| On-duty days (M ± SD) |
Off-duty days (M ± SD) | On-duty – off-duty between group differences |
|||
|---|---|---|---|---|---|
| Mean difference | p-Value | Cohen's d | |||
| Average daily step count | |||||
| Day shift nurses (n = 33) | 11,296.53 ± 4816.65 | 6828.79 ± 4597.16 | 4467.74 | <0.001⁎ | 0.952 |
| Night shift nurses (n = 21) | 9701.37 ± 6091.14 | 6655.74 ± 4180.13 | 3045.64 | <0.001⁎ | 0.594 |
Abbreviations: Mean plus or minus Standard Deviation (M ± SD).
p < 0.05.
Table 5.
Step quantity goals met for day and night shift nurses over study.
| Day shift nurses |
Night shift nurses |
Day shift – night shift between group differences |
|||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | X2 | p-value | Phi | |
| Reached daily step quantity goal | |||||||
| All overserved study days | |||||||
| Yes | 134 | 60.1 | 87 | 52.1 | 2.49 | 0.115 | 0.078 |
| No | 89 | 39.9 | 80 | 47.9 | |||
| On-duty observations | |||||||
| Yes | 83 | 87.4 | 54 | 72 | 6.33 | 0.012⁎ | 0.193 |
| No | 12 | 12.6 | 21 | 28 | |||
| Off-duty observations | |||||||
| Yes | 51 | 39.8 | 33 | 36.3 | 0.29 | 0.591 | 0.036 |
| No | 77 | 60.2 | 58 | 63.7 | |||
| On-duty – off-duty between group differences | |||||||
| X2 | 51.4 | 21.1 | |||||
| p-Value | <0.001⁎ | <0.001⁎ | |||||
| Phi | 0.48 | 0.356 | |||||
Abbreviations: Percent (%); Chi-square (X2).
p < 0.05.
3.5. Correlations between sleep, diet, physical activity, and stress
Few significant correlations were observed. Participants self-reported sleep was inversely related to the length of time they have been in the current shift (r = −0.306; p = 0.039) indicating individuals reported less sleep the longer they have been working their shift. Step counts were found to be inversely correlated with PSS-4 score (r = −0.363; p = 0.013) showing nurses taking more steps had lower PSS-4 scores (indicating less perceived stress) and vice-versa. Finally, Healthy Eating Index scores were directly related with rMEQ scores (r = 0.384; p = 0.008) meaning those with higher Healthy Eating Index scores also had higher rMEQ scores, indicating a preference to rise earlier in the day (Danielsson et al., 2019).
4. Discussion
In all, 57 acute care nurses across 10 hospitals participated in this technology-based study conducted after the onset of the COVID-19 pandemic. On average, nurses did not sleep per general recommendations for at least 7.5 h per 24 h (National Sleep Foundation, 2020), on-duty diet quality did not reach high-quality scores (Reedy et al., 2018), and nurses did not meet physical activity standards for number of steps taken (Paluch et al., 2021) during off-duty time periods. Few significant differences emerged between night and day shift nurses; notably, night shift nurses were more likely to report a worsened diet quality since the onset of the COVID-19 pandemic, prefer to rise later in the day, and sleep less time during on-duty time periods compared to day shift counterparts. Viewed through the lens of Orem's theory of self-care, it appears that during times of heightened occupational stress, self-care activities among full-time nurses may suffer.
Sleep findings from our study indicate significant differences in the sleep attained between day and night shift nurses. This was especially evident when considering the difference between sleep attained by nurses during on-duty versus off-duty periods. Day shift nurses received roughly equivalent sleep regardless of duty, whereas night shift nurses received almost an hour and a half more sleep per 24-hour period when off-duty, suggesting compensating for sleep debt accumulated during the work week. This finding is supported by previous research, including from our own work funded by the Agency for Health Research and Quality (AHRQ) where we found significant differences between sleep attained by day and night shift nurses (James et al., 2020). We found a steady decline in the sleep attained by night shift nurses over the work week (three consecutive 12-hour shifts), leading to accumulation of sleep debt that is partially recovered through longer periods of sleep during days off. The reduction in sleep associated with night shift work is driven by circadian factors which make it difficult for people to sleep during the day to attain sufficient sleep, hence the need to “catch up” (Boivin & Boudreau, 2014). This pattern has repeated itself in prior studies by our team that also indicate night shift nurses revert to nighttime sleep patterns on their off-duty time periods and report worse sleep quality on average than their day shift counterparts (Riedy et al., 2017).
Analysis of the Healthy Eating Index (HEI) scores indicated that nurses had a poor diet quality during on-duty time periods. A multitude of individual and social factors can influence eating patterns, particularly among night shift workers (Gupta et al., 2019). It is possible that nurses were under more stress during their workday due to the COVID-19 pandemic, leading to a preference for foods of lower dietary quality that may help temporarily boost mood (van Galen et al., 2021). Essential care workers such as nurses also experienced restricted access to healthy foods amid the COVID-19 pandemic compared to prior availability (Clay & Rogus, 2021). Occupational factors such as availability of on-the-job food choices or break timing may also influence diet quality. In the recruitment sites for this study, on-site cafeterias were closed, leaving foods sold in vending machines, traditionally low in nutritional value, as the only option for food to purchase in the workplace during the duration of the study. Participants were also frequently the recipients of community outpouring and were provided meals both high and low in nutritional value by various vendors while working which could have influenced diet quality. Aside from COVID-19, night shift nurses traditionally have restricted access to the cafeteria due to limited hours open during the night which could impact diet quality during on-duty time periods. Previous work by our team found that nurses report inconsistencies in access to break time (Landis et al., 2021) and lack of resources such as a quiet place to rest (Wilson et al., 2018) which may contribute to poorer eating habits while at work.
Sleep disruptions may affect hunger cues which could drive unhealthy eating choices, particularly for night shift nurses. Feelings of hunger as well as plasma ghrelin and leptin levels [the hormones that regulate hunger and appetite] have been shown to be altered when sleep duration is restricted (McHill et al., 2022; Spiegel et al., 2004) which could also explain mechanisms behind our nurses' dietary choices. Our findings displayed a trend toward night shift nurses reporting poorer diet quality while on-duty than day shift nurses, but this finding was not significant. Yet, night shift nurses in our study were more likely to report a worsened diet quality since the onset of the COVID-19 pandemic, indicating these nurses may need more support to follow a healthy diet under times of increased stress. Furthermore, our work suggested higher HEI scores were correlated with a higher rMEQ score, indicating a preference to rise earlier in the day (Danielsson et al., 2019) and aligning with prior studies suggesting that nurses working day shift hours may follow a healthier diet (Yoshizaki et al., 2018). Future research should continue to investigate the connection between diet quality on off-duty versus on-duty time periods and how workplace attributes, sleep patterns, and individual variables contribute to or detract from healthy eating behaviors employed by nurses.
On average, nurses in this study met the commonly recommended step goal of 7000 steps daily over the course of a 7-day period (Paluch et al., 2021) although significantly fewer night shift nurses attained this metric compared to day shift nurses. Yet, most nurses were not meeting this step goal during their off-duty time periods. Inadequate physical activity measured by step count may have clinical consequences including increased risk for cardiovascular disease and all-cause mortality which may be mitigated by increased physical activity, even among those walking 7000 steps daily (Sheng et al., 2021). Furthermore, a large proportion of nurses reported their physical activity decreased since the onset of the COVID-19 pandemic. This may have contributed to the relatively low reported physical activity and steps taken during off-duty time periods and aligns with evidence demonstrating fewer steps were taken following lockdown measures aimed at reducing the spread of COVID-19 (Sun et al., 2020). Additionally, a higher number of steps walked significantly correlated with a lower perceived stress score in our study. Given that the overall stress score was higher than norms estimated by prior research (Vallejo et al., 2018), and literature supporting emotional and occupational health benefits of increased physical activity among nurses (Stanulewicz et al., 2019), our study suggests that nurses may reduce stress through increased PA. Further research to enhance nursing engagement in physical activity, even when off-duty and particularly during times of increased occupational stress, are warranted.
Our study may have suffered selection bias, given that studies involving applications and devices to document diet (Zhang et al., 2021) or steps (Chaudhry et al., 2020) usually attract participants who are interested in healthy lifestyles. Yet, given our sample size and diverse recruitment strategy, we mitigated this risk and are confident in representativeness of our findings. It is possible that diet may have been incorrectly documented in the ASA24 platform, potentially skewing findings, yet studies support validity of mobile applications to collect diet data (Zhang et al., 2021), and our team opted to use a valid and reliable diet instrument, increasing our confidence in findings. Our pilot study was not adequately powered to detect differences for variables with small effect sizes (<0.1); most effect sizes were moderate or larger, suggesting an adequate sample size to support validity of results.
Night shift nurses were unable to accurately submit step data as most wearable pedometers time steps from midnight to midnight, and on-duty time periods likely only reflected steps taken during the first half of the worked shift. However, between-group differences for day and night shift nurses in terms of steps walked when on versus off-duty varied in the same direction, suggesting the variation may not have been clinically significant and increasing confidence in physical activity results. Nurses were not asked about specialty area of practice which could have influenced stress levels as certain specialties were more impacted by COVID-19 than others, yet a strength of study design was standardizing shift length and number of hours worked during the study period among participants. Stress was only measured at baseline and while it encompassed perceived stress in the prior month, more transient changes in stress could not be ascertained. Finally, despite the protocol requiring nurses to work three, 12-h shifts during the seven days of observation, one nurse reported working only two shifts due to illness while others (n = 7) picked up an extra shift due to high incentives to work overtime during short staffing conditions. While a small percentage of the total sample, such variability in work hours should be considered for future health research in this population, especially in the context of a global pandemic.
5. Conclusions
While nurses are responsible to provide high-quality care for their patients, environmental conditions such as workforce shortages, increased patient workloads and augmented personal stress can lead to poor self-care strategies and worsened physical and emotional outcomes. According to Orem's self-care theory, when external demands overpower the ability to engage in self-care practices, a self-care deficit is the result. Our findings urge organizations to put resources in place to support nursing self-care practices during on-duty time periods, particularly for those working night shift. Innovative strategies may include providing space for napping when nurses (particularly during night shift) are on break to promote healthy sleep, ensuring access to healthy eating options in the workplace, and providing safe indoor spaces for physical activity such as walking while nurses are working. Promoting healthy self-care practices of nurses, especially during times of heightened occupational stress, can support overall nursing wellbeing and may contribute to improved occupational outcomes such as less missed days of work, less worker's compensation claims, and lower levels of turnover (Salvagioni et al., 2017). The implications for improved patient care and occupational savings can be far-reaching when a healthier nursing workforce is in place.
Funding
This study received funding from the Selinger Shone Foundation and the Providence Inland Northwest Washington Foundation. The sponsors had no role in the conduct of the study.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the conduct of research, authorship, or publication of this article.
Acknowledgments
Our study team would like to thank Washington State University collaborators and researchers for donating several wearable devices to make this work feasible. We would also like to acknowledge all Providence and Washington State University students and research assistants who made data entry, cleaning, and analysis possible. We finally acknowledge the Selinger Shone Foundation (2493-3930) and Providence Inland Northwest Washington Foundation (P20-11-23) for generously funding our work.
Footnotes
This study was reviewed by the Providence St. Joseph Health Institutional Review Board and received expedited approval on September 8, 2020 (STUDY2020000434).
References
- Abdulameer S.A., Al-Jewari W.M., Sahib M.N. Psychological health status and salivary IgA among pharmacy students in Iraq: Validation of PSS-4 and WHO-5 wellbeing (Arabic version) Pharmacy Education. 2019;19:10–18. [Google Scholar]
- Al Maqbali M., Al Sinani M., Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Psychosomatic Research. 2021;141 doi: 10.1016/j.jpsychores.2020.110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boivin D.B., Boudreau P. Impacts of shift work on sleep and circadian rhythms. Pathologie Biologie. 2014;62(5):292–301. doi: 10.1016/j.patbio.2014.08.001. [DOI] [PubMed] [Google Scholar]
- Caruso C.C., Baldwin C.M., Berger A., Chasens E.R., Edmonson J.C., Gobel B.H., Tucker S.… Policy brief: Nurse fatigue, sleep, and health, and ensuring patient and public safety. Nursing Outlook. 2019;67(5):615–619. doi: 10.1016/j.outlook.2019.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhry U.R., Wahlich C., Fortescue R., Cook D.G., Knightly R., Harris T. The effects of step-count monitoring interventions on physical activity: Systematic review and meta-analysis of community-based randomised controlled trials in adults. International Journal of Behavioral Nutrition and Physical Activity. 2020;17(1):129. doi: 10.1186/s12966-020-01020-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chelminski I., Petros T.V., Plaud J.J., Ferraro F.R. Psychometric properties of the reduced Horne and Ostberg questionnaire. Personality and Individual Differences. 2000;29(3):469–478. doi: 10.1016/S0191-8869(99)00208-1. [DOI] [Google Scholar]
- Clay L.A., Rogus S. Impact of employment, essential work, and risk factors on food access during the COVID-19 pandemic in New York state. International Journal of Environmental Research and Public Health. 2021;18(4):1451. doi: 10.3390/ijerph18041451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui S., Zhang L., Yan H., Shi Q., Jiang Y., Wang Q., Chu J. Experiences and psychological adjustments of nurses who voluntarily supported COVID-19 patients in Hubei Province, China. Psychology Research and Behavior Management. 2020;13:1135–1145. doi: 10.2147/prbm.s283876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielsson K., Sakarya A., Jansson-Fröjmark M. The reduced morningness-eveningness questionnaire: Psychometric properties and related factors in a young Swedish population. Chronobiology International. 2019;36(4):530–540. doi: 10.1080/07420528.2018.1564322. [DOI] [PubMed] [Google Scholar]
- Denyes M.J., Orem D.E., Bekel G. Self-care: A foundational science. Nursing Science Quarterly. 2001;14(1):48–54. doi: 10.1177/089431840101400113. [DOI] [PubMed] [Google Scholar]
- Berent D., Skoneczny M., Macander M., Wojnar M. The association among health behaviors, shift work and chronic morbidity: A cross-sectional study on nurses working in full-time positions. Journal of Public Health Research. 2021 doi: 10.4081/jphr.2021.2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driller M., McQuillan J., O’Donnell S. Inter-device reliability of an automatic-scoring actigraph for measuring sleep in healthy adults. Sleep Science. 2016;9(3):198–201. doi: 10.1016/j.slsci.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick T.A., Valentine N.M. Dealing with COVID-19 post-traumatic stress: Strategies for preserving the nursing workforce and supporting all vital frontline personnel. Nursing Economics. 2021;39(5):225–250. http://www.nursingeconomics.net/necfiles/2021/SO21/225.pdf http://www.nursingeconomics.net/necfiles/2021/SO21/225.pdf. [Google Scholar]
- Fuller D., Colwell E., Low J., Orychock K., Tobin M., Simango B., Buote R., Van Heerden D., Luan H., Cullen K., Slade L., Taylor N.A. Reliability and validity of commercially available wearable devices for measuring steps, energy expenditure, and heart rate: Systematic review. Journal of Medical Internet Research mHealth and uHealth. 2020;8(9) doi: 10.2196/18694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses' burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Advanced Nursing. 2021;77(8):3286–3302. doi: 10.1111/jan.14839. (John Wiley & Sons, Inc.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillodo E., Lemey C., Simonnet M., Walter M., Baca-García E., Masetti V., Moga S., Larsen M., Ropars J., Berrouiguet S. Clinical applications of mobile health wearable–based sleep monitoring: Systematic review. Journal of Medical Internet Research mHealth and uHealth. 2020;8(4) doi: 10.2196/10733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta C.C., Coates A.M., Dorrian J., Banks S. The factors influencing the eating behaviour of shiftworkers: What, when, where, and why. Industrial Health. 2019;57(4):419–453. doi: 10.2486/indhealth.2018-0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H., Huang N., Jiang X., Jianghong Y., Zhou Y., Hengping P. Factors related to job burnout among older nurses in Guizhou province,China. PeerJ. 2021;1–16 doi: 10.7717/peerj.12333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp . IBM Corp; Armonk, NY: 2020. IBM SPSS statistics for Windows, version 27.0. Released. [Google Scholar]
- Is E.E., Sahillioglu A., Demirel S., Kuran B., Ozdemir H.M. Effect of COVID-19 pandemic on physical activity habits, musculoskeletal pain, and mood of healthcare workers. Medical Bulletin of Sisli Etfal Hospital. 2021;55(4):462–468. doi: 10.14744/SEMB.2021.87523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James L., James S., Wilson M., Brown N., Dotson E., Edwards C., Butterfield P. Sleep health and predicted cognitive effectiveness of nurses working 12-hour shifts: An observational study. International Journal of Nursing Studies. 2020 doi: 10.1016/j.ijnurstu.2020.103667. [DOI] [PubMed] [Google Scholar]
- Jin D., Halvari H., Maehle N., Olafsen A.H. Self-tracking behaviour in physical activity: A systematic review of drivers and outcomes of fitness tracking. Behaviour & Information Technology. 2022;41(2):242–261. doi: 10.1080/0144929X.2020.1801840. [DOI] [Google Scholar]
- Kellogg M.B., Schierberl Scherr A.E., Ayotte B.J. “All of this was awful:” Exploring the experience of nurses caring for patients with COVID-19 in the United States. Nursing Forum. 2021;56(4):869–877. doi: 10.1111/nuf.12633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khubchandani J., Kandiah J., Saiki D. The COVID-19 pandemic, stress, and eating practices in the United States. European Journal of Investigation in Health, Psychology and Education. 2020;10(4):950–956. doi: 10.3390/ejihpe10040067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis T.T., Wilson M., Bigand T., Cason M. Registered nurses' experiences taking breaks on night shift: A qualitative analysis. Workplace Health and Safety. 2021;69(6):252–256. doi: 10.1177/2165079920983018. [DOI] [PubMed] [Google Scholar]
- Mazurek Melnyk B., Pavan Hsieh A., Tan A., Teall A.M., Weberg D., Jun J., Gawlik K., Hoying J. Associations among nurses' mental/physical health, lifestyle behaviors, shift length, and workplace wellness support during COVID-19: Important implications for health care systems. Nursing Administration Quarterly. 2022;46(1):5–18. doi: 10.1097/NAQ.0000000000000499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHill A.W., Hull J.T., Klerman E.B. Chronic circadian disruption and sleep restriction influence subjective hunger, appetite, and food preference. Nutrients. 2022;14(9):1800. doi: 10.3390/nu14091800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Sleep Foundation How much sleep do you really need? 2020. https://www.thensf.org/how-many-hours-of-sleep-do-you-really-need/ Retrieved from.
- Neculicioiu V.S., Colosi I.A., Costache C., Sevastre-Berghian A., Clichici S. Time to sleep? A review of the impact of the COVID-19 pandemic on sleep and mental health. International Journal of Environmental Research and Public Health. 2022;19(6) doi: 10.3390/ijerph19063497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paluch A.E., Gabriel K.P., Fulton J.E., Lewis C.E., Schreiner P.J., Sternfeld B., Sidney S., Siddique J., Whitaker K.M., Carnethon M.R. Steps per day and all-cause mortality in middle-aged adults in the coronary artery risk development in young adults study. JAMA Network Open. 2021;4(9) doi: 10.1001/jamanetworkopen.2021.24516. e2124516-e2124516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priano S.M., Hong O., Chen J.L. Lifestyles and health-related outcomes of U. S. hospital nurses: A systematic review. Nursing Outlook. 2018;66(1):66–76. doi: 10.1016/j.outlook.2017.08.013. [DOI] [PubMed] [Google Scholar]
- Prince S.A., Adamo K.B., Hamel M.E., Hardt J., Gorber S.C., Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2008;5(1):1–24. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reedy, Lerman, Krebs-Smith, Subar, Kahle, Tooze Evaluation of the healthy eating index-2015. Journal of the Academy of Nutrition and Dietetics. 2018;118(9):1622–1633. doi: 10.1016/j.jand.2018.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedy S.M., English A., Albritton S., Burton J., Himmel M., Morgan P., Kadel K., Van Dongen H., Wilson M. 0169 sleep patterns during duty periods and during off-days between duty cycles in hospital employees working 12-hour night shifts. Sleep. 2017;40(suppl_1) doi: 10.1093/sleepj/zsx050.168. A63-A63. [DOI] [Google Scholar]
- Russell C., Caldwell J.A., Arand D., Myers L., Wubbels P., Downs H. Arch LLC; 2000. Validation of the fatigue science readiband actigraph and associated sleep/wake classification algorithms. [Google Scholar]
- Saeidifard F., Medina-Inojosa J.R., West C.P., Olson T.P., Somers V.K., Bonikowske A.R., Prokop L.J., Vinciguerra M., Lopez-Jimenez F. The association of resistance training with mortality: A systematic review and meta-analysis. European Journal of Preventive Cardiology. 2019;26(15):1647–1665. doi: 10.1177/2047487319850718. [DOI] [PubMed] [Google Scholar]
- Salvagioni D.A.J., Melanda F.N., Mesas A.E., González A.D., Gabani F.L., Andrade S.M.D. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PloS one. 2017;12(10) doi: 10.1371/journal.pone.0185781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheng M., Yang J., Bao M., Chen T., Cai R., Zhang N., Chen H., Liu M., Wu X., Zhang B., Liu Y., Chao J. The relationships between step count and all-cause mortality and cardiovascular events: A dose-response meta-analysis. Journal of Sport and Health Science. 2021;10(6):620–628. doi: 10.1016/j.jshs.2021.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotos-Prieto M., Bhupathiraju S.N., Mattei J., Fung T.T., Li Y., Pan A., Willett W.C., Rimm E.B., Hu F.B. Association of changes in diet quality with total and cause-specific mortality. New England Journal of Medicine. 2017;377(2):143–153. doi: 10.1056/NEJMoa1613502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel K., Tasali E., Penev P., Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- Sriharan A., Ratnapalan S., Tricco A.C., Lupea D. Women in healthcare experiencing occupational stress and burnout during COVID-19: A rapid review. British Medical Journal Open. 2021;11(4) doi: 10.1136/bmjopen-2021-048861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanulewicz N., Knox E., Narayanasamy M., Shivji N., Khunti K., Blake H. Effectiveness of lifestyle health promotion interventions for nurses: A systematic review. International Journal of Environmental Research and Public Health. 2019;17(01):17. doi: 10.3390/ijerph17010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S., Folarin A.A., Ranjan Y., Rashid Z., Conde P., Stewart C., Cummins N., Matcham F., Dalla Costa G., Simblett S., Leocani L., Lamers F., Sørensen P., Buron M., Zabalza A., Guerrero Pérez A., Penninx B., Siddi S., Haro J., Dobson R.… Using smartphones and wearable devices to monitor behavioral changes during COVID-19. Journal of Medical Internet Research. 2020;22(9) doi: 10.2196/19992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson F.E., Dixit-Joshi S., Potischman N., Dodd K.W., Kirkpatrick S.I., Kushi L.H., Subar A.F.… Comparison of interviewer-administered and automated self-administered 24-hour dietary recalls in 3 diverse integrated health systems. American Journal of Epidemiology. 2015;181(12):970–978. doi: 10.1093/aje/kwu467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . 2nd ed. U.S Department of Health and Human Services; 2018. Physical activity guidelines for Americans. [Google Scholar]
- Vallejo M.A., Vallejo-Slocker L., Fernández-Abascal E.G., Mañanes G. Determining factors for stress perception assessed with the Perceived Stress Scale (PSS-4) in Spanish and other European samples. Frontiers in Psychology. 2018;9(37) doi: 10.3389/fpsyg.2018.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Galen K.A., Ter Horst K.W., Serlie M.J. Serotonin, food intake, and obesity. Obesity Reviews. 2021;22(7) doi: 10.1123/jpah.2013-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigoureux T.F., Mu C.X., Mason T.M., Gonzalez B.D., Lee S. Adapting research to a global pandemic: A fully remote actigraphy and ecological momentary assessment study. Nursing Research. 2022;71(2):119–127. doi: 10.1097/NNR.0000000000000561. [DOI] [PubMed] [Google Scholar]
- Wilson M., Reidy S., Himmel M., English A., Burton J., Albritton S., Johnson K., Morgan P., Van Dongen H.P.A. Sleep quality, sleepiness and the influence of workplace breaks: A cross-sectional survey of health-care workers in two US hospitals. Chronobiology International. 2018;35(6):849–852. doi: 10.1080/07420528.2018.1466791. Epub ahead of print March 8, 2018. [DOI] [PubMed] [Google Scholar]
- Yin J., Jin X., Shan Z., Li S., Huang H., Li P., Peng X., Peng Z., Yu K., Bao W., Yang W., Chen X., Liu L. Relationship of sleep duration with all-cause mortality and cardiovascular events: A systematic review and dose-response meta-analysis of prospective cohort studies. Journal of the American Heart Association. 2017;6(9) doi: 10.1161/JAHA.117.005947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshizaki T., Komatsu T., Tada Y., Hida A., Kawano Y., Togo F. Association of habitual dietary intake with morningness-eveningness and rotating shift work in Japanese female nurses. Chronobiology International. 2018;35(3):392–404. doi: 10.1080/07420528.2017.1410169. [DOI] [PubMed] [Google Scholar]
- Zhang L., Misir A., Boshuizen H., Ocké M. A systematic review and meta-analysis of validation studies performed on dietary record apps. Advances in Nutrition. 2021;12(6):2321–2332. doi: 10.1093/advances/nmab058. [DOI] [PMC free article] [PubMed] [Google Scholar]