Abstract
Background
The World Health Organization declared monkeypox as a Public Health Emergency of International Concern. A cross-sectional online survey was conducted to understand beliefs, attitudes, perceived preventive measures, and vaccination acceptance related to monkeypox in the public in China.
Methods
Between August 30 and September 15, 2022, we recruited adults through an online survey platform. Demographic characteristics, perceptions, common knowledge, concerns, attitudes, willingness to adopt preventive measures (including hygiene practices, social distancing, and travel avoidance), and vaccination acceptance related to monkeypox were collected. Logistic regression was used to assess correlates of concerns about monkeypox, willingness to adopt preventive measures, and vaccination acceptance.
Results
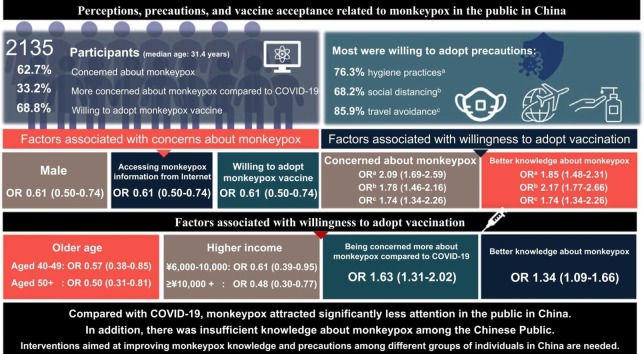
2135 participants were recruited (median age: 31.4 years). 62.7% were concerned about monkeypox. 33.2% were more concerned about monkeypox compared to COVID-19. Males (aOR 0.61, 95%CI 0.50–0.74), accessing monkeypox information from the Internet (0.77, 0.61–0.98), and willingness to adopt monkeypox vaccine (2.9, 2.38–3.53) were associated with concerns about monkeypox. Most participants were willing to adopt precautions (76.3% hygiene practices, 68.2% social distancing, 85.9% travel avoidance). Individuals who were concerned about monkeypox (hygiene practices: 2.09, 1.69–2.59; social distancing: 1.78, 1.46–2.16; travel avoidance: 1.74, 1.34–2.26) and had better knowledge about monkeypox (hygiene practices: 1.85, 1.48–2.31; social distancing: 2.17, 1.77–2.66; travel avoidance: 1.74, 1.34–2.26) were more likely to adopt precautions. 68.8% were willing to adopt monkeypox vaccine. Participants with older age (aged 40–49: 0.57, 0.38–0.85; aged 50 +: 0.50, 0.31–0.81), and higher income (¥6000–10,000: 0.61, 0.39–0.95; ≥¥10,000: 0.48, 0.30–0.77) were less likely to adopt the monkeypox vaccine. Being concerned more about monkeypox compared to COVID-19 (1.63, 1.31–2.02), and having better knowledge about monkeypox (1.34, 1.09–1.66) were associated with willingness to adopt vaccination.
Conclusions
Compared with COVID-19, monkeypox attracted significantly less attention in the public in China, who currently have insufficient monkeypox knowledge. Interventions aimed at improving monkeypox knowledge and precautions among different groups of individuals in China are needed.
Keywords: Monkeypox, Vaccine, The public, Prevention, China
Graphical Abstract
Background
Monkeypox virus is a zoonotic orthopox DNA virus related to the virus that causes smallpox-like disease [1], [2], [3], [4]. According to the latest data report from the US Centers for Disease Control and Prevention [5], as of November 24, 2022, a total of 80,850 cases of monkeypox have been reported in 102 countries around the world. To date, no specific treatment for monkeypox has been offered [6], [7], [8]. The conventional treatment methods remain the main recommendations, including supportive care, symptomatic management, and treatment of secondary bacterial infections [6]. The monkeypox virus is transmitted through large respiratory droplets, close or direct contact with skin lesions, and possibly through contaminated fomites [9]. Therefore, preventive behaviors by the public are fundamental and effective in preventing monkeypox and controlling its spread.
Although the world remains challenged by the coronavirus disease 2019 (COVID-19) pandemic, the emergence of a new outbreak caused by the monkeypox virus has raised concerns among public health authorities as to whether it constitutes a new threat [2], [9]. Since monkeypox was declared a public health emergency of international concerns by the Director-General of WHO on July 23, 2022, health policy planning and pandemic preparedness have become priorities for public health agencies at all levels. The governments and relevant departments need to consider the implementation phase when formulating applicable health policies. However, policy implementation is usually affected by group behaviors [10]. The public's response to an epidemic depends partly on each person's perceptions of the disease and their ability to adjust their behaviors as circumstances change [11]. The experience of the COVID-19 epidemic has taught us that public perceptions, concerns, and attitudes are crucial for developing response measures during an emerging pandemic. In other words, a prerequisite for effective emergency preparedness and response is a comprehensive understanding of how the public perceives and responds to the threat of a pandemic and developing risk communication strategies that may promote appropriate public preventive behaviors [12].
In China, there is limited research on how people perceive risk from previous infectious disease outbreaks [13]. Most of these studies focus on specific populations, such as older adults [14], medical staff [15], college students [16], or assess perceptions and attitudes in specific periods, such as quarantine [17]. By understanding public perceptions, concerns, and attitudes, it will be possible to develop tailored interventions to encourage preventive measures. To date, the number of “netizens” (citizens of the Internet) in China has reached 989 million, with an Internet penetration rate of 70.4% [18], which lays a good foundation for potentially representative samples recruited from the Internet. Compared with traditional surveys, one of the most significant advantages of online surveys is the ability to recruit a large number of participants nationwide to collect the needed information in a short time, especially during infectious disease outbreaks. Therefore, we conducted a cross-sectional online survey to understand perceived beliefs, attitudes, preventive behaviors, and vaccine acceptance related to monkeypox. Our findings may help identify populations with low-risk perceptions by exploring the understanding of monkeypox-related knowledge, concerns about the monkeypox epidemic, and its influencing factors in the public in China.
Methods
Study design and participants
This is a cross-sectional online study of the public conducted from August 30 to September 15, 2022. The self-administered electronic questionnaire (published on Wenjuanxing, an online survey platform) was distributed online through social networking platforms such as QQ and WeChat. The questionnaire is shown in Appendix. Before delivering the questionnaire, 30 participants were recruited for a pilot study to ensure clarity.
Participants who could read and understand electronic questionnaires and ≥ 18 years or older were eligible to participate in this study. Participants who refused to complete the questionnaire after understanding the purpose of the study were excluded.
Ethical consideration
All participants were provided with online informed consent. The study was approved and was performed in accordance with the Helsinki Declaration.
Measures
Demographic characteristics
Participants were asked to provide socio-demographic information as following items: age (in years), gender (Male/Female), educated level (Below undergraduate, Undergraduate, Postgraduates), steady marital status (No/Yes), residential area (Rural/Urban), employment status (Students/Unemployed or retired/Employed) and monthly income (No fixed,<¥5000, ¥5000–9999, ≥ ¥10000).
Depressive symptoms
In addition, we assessed participants' depressive symptoms in the past two weeks using a two-item Patient Health Questionnaire (PHQ-2). Probable depressive symptoms were defined with a summed score ≥ 3 [19], [20], [21]. The PHQ-2 has been previously used in Chinese populations and was found to have good reliability (Cronbach α = 0.83) [22]. The current study also shows high internal consistency for the scale (Cronbach α = 0.80).
Perceptions of monkeypox
The perceptions of monkeypox were assessed through two questions with a logical connection. Briefly, participants were asked “Did you learn about monkeypox/monkeypox virus before this survey?” (Yes/No). Only who selected “Yes” were asked to recall the way they learned about monkeypox.
Common knowledge of monkeypox
The common knowledge of monkeypox was evaluated by seven knowledge items, as follows:
-
1.
Monkeypox is a dangerous and rapidly transmitted disease.
-
2.
Monkeypox is a zoonotic disease.
-
3.
Monkeypox prevention calls for respiratory and contact precautions.
-
4.
Monkeypox can be transmitted before symptoms appear, especially skin blisters.
-
5.
The smallpox vaccine (that generally was given before 1980) is effective against monkeypox?
-
6.
The chickenpox vaccine is effective against monkeypox.
-
7.
There are currently specific treatments for monkeypox infections.
These knowledge items are some basic knowledge extracted from Walter and Malani's article [23]. Participants were presented with three options (Yes/No/Don't know) for each question. The answer “don’t know” was considered wrong. A high level of common knowledge about monkeypox was defined as answering more than four questions correctly.
Concerns about monkeypox
The question with two responses, “Are you concerned about the monkeypox epidemic? (Yes/No)”, was provided to assess concerns about monkeypox [24]. Participants who selected “Yes” were additionally asked to choose at least one of the reasons listed. All participants were asked a validated question with two responses “Compared to COVID-19, how much were you concerned nowadays about Monkeypox?” (More concerned about COVID-19/More concerned about Monkeypox) to measure levels of concern about Monkeypox compared to COVID-19 [24].
Attitudes toward monkeypox
Participants were asked, “Will there be a pandemic of monkeypox in China” to evaluate their attitudes toward monkeypox. Regardless of which option the participant chooses, they will jump to the corresponding question and be asked to select at least one reason.
Willingness to adopt preventive measures
Willingness to adopt preventive measures was defined as taking measures to protect themselves and/or others. Referring to the previous study in Saudi Arabia [25], the preventive measures were categorized into three groups, including hygiene practices, social distancing, and travel avoidance.
Willingness to adopt monkeypox vaccine
The willingness to adopt monkeypox vaccine was measured by a five-point Likert scale (“Would you like to be vaccinated against monkeypox?”) ranging from 1 (strongly disagree) to 5 (strongly agree) [26]. For this study, vaccine acceptance was re-categorized as willingness (4−5) and unwillingness (1−3). Participants who were unwilling to be vaccinated were additionally asked to indicate the main reasons for their unwillingness [27].
Statistical analyses
As the electronic questionnaire was set up to be fully answered before submission, there was no missing data in the final dataset. Descriptive analyses, including percentage, mean, and standard deviation, were presented to characterize the study sample. The Chi-square test was used to compare the proportions of characteristics between groups. The variables associated with outcomes were analyzed by logistic regression models. Only variables judged relevant from professional knowledge or statistically significantly correlated with outcomes were introduced into multivariable logistic regression models. Python version 3.8 was used to analyze the survey data. The statistical significance was set as P < 0.05. Adjusted odds ratio (aOR) and the 95% confidence interval (95% CI) were estimated.
Results
As shown in Table 1, the majority of the 2135 participants who completed the online survey were male (73%) and residents of the urban area (68.4%). More than half of the participants (61.0%) were in the younger age group (i.e., between 18 and 29 years old). 45.7% of the participants had no fixed monthly income. Most participants were undergraduates (47.4%) and employed (45.8%). Most respondents (86.3%) had no depressive symptoms.
Table 1.
Basic characteristics of participants (N = 2135).
| Characteristics | N (%) |
|---|---|
| All | 2135 |
| Gender | |
| Female | 1337 (62.6) |
| Male | 798 (37.4) |
| Age | |
| 18–29 | 1303 (61.0) |
| 30–39 | 450 (21.1) |
| 40–49 | 233 (10.9) |
| 50+ | 149 (7.0) |
| Living area | |
| Rural | 282 (13.2) |
| Urban | 1853 (86.8) |
| Educational level | |
| Below undergraduate | 407 (19.1) |
| Undergraduate | 1012 (47.4) |
| Postgraduate | 716 (33.5) |
| Steady marital status | |
| No | 1398 (65.5) |
| Yes | 737 (34.5) |
| Employment status | |
| Current student | 986 (46.2) |
| Unemployed | 172 (8.1) |
| Employed | 977 (45.8) |
| Monthly income (¥) | |
| No fixed | 975 (45.7) |
| < 6000 | 494 (23.1) |
| 6000–10,000 | 341 (16.0) |
| > 10,000 | 325 (15.2) |
| Depressive symptoms | |
| No | 1842 (86.3) |
| Yes | 293 (13.7) |
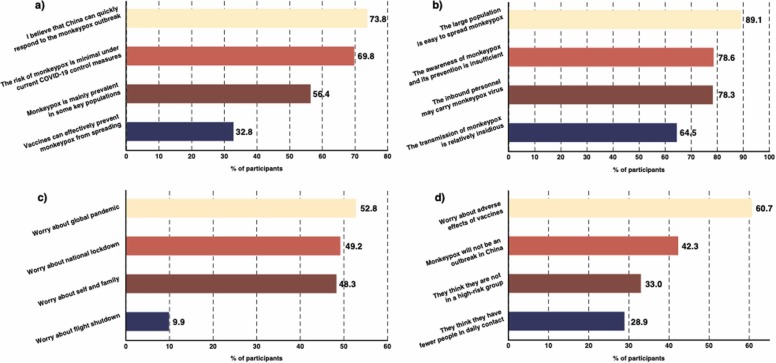
Table 2 displayed participants’ attitudes, perceptions, and beliefs about monkeypox. Over half of the respondents (54.5%) had previously gotten monkeypox information before the survey, and the Internet was the main information source (50.1%). During this survey, only 14.2% of participants perceived that monkeypox would become a pandemic in China. 85.8% of dissenting participants believed that China could quickly respond to the monkeypox outbreak (73.8%) or felt the minimal risk of monkeypox infection under current COVID-19 control measures (69.8%) ( Fig. 1a). Contrary, the main reason why participants perceived that “monkeypox will become a pandemic in China” was that the large population was easy to spread (89.1%), followed by insufficient awareness of monkeypox and its prevention (78.6%), inbound personnel could carry monkeypox virus (78.3), and the transmission of monkeypox was relatively insidious (64.5%) (Fig. 1b).
Table 2.
Participants’ perceived beliefs, attitudes, willingness to adopt precautions, and vaccine acceptance related to monkeypox.
| Characteristics | N (%) |
|---|---|
| Had got monkeypox information before the survey | |
| No | 971 (45.5) |
| Yes | 1164 (54.5) |
| Getting monkeypox information from Internet sources | |
| No | 1065 (49.9) |
| Yes | 1070 (50.1) |
| Getting monkeypox information from traditional media | |
| No | 1639 (76.8) |
| Yes | 496 (23.2) |
| Perceived that monkeypox will become a pandemic in China | |
| No | 1831 (85.8) |
| Yes | 304 (14.2) |
| Concerned about monkeypox outbreak | |
| No | 796 (37.3) |
| Yes | 1339 (62.7) |
| Concerned more about monkeypox compared to COVID-19 | |
| No | 1427 (66.8) |
| Yes | 708 (33.2) |
| Common knowledge of monkeypox | |
| Low level | 649 (30.4) |
| High level | 1486 (69.6) |
| Willingness to adopt preventive behaviors | |
| Hygiene practices | 1630 (76.3) |
| Social distancing | 1457 (68.2) |
| Travel avoidance | 1834 (85.9) |
| Willingness to adopt monkeypox vaccine | |
| No | 667 (31.2) |
| Yes | 1468 (68.8) |
Fig. 1.
Reasons for disagreeing (a) or agreeing (b) with the idea that monkeypox will be a pandemic in China, worries about monkeypox (c), and unwillingness to get monkeypox vaccine (d).
The majority of participants (62.7%) were concerned about the monkeypox outbreak. Most participants (52.8%) were worried about monkeypox turning into a global pandemic, followed by the national lockdown (49.2%), themselves and their families infected (48.3%), and flight shutdowns (9.9%), as Fig. 1c shown. About one-third of participants (33.2%) were more concerned about monkeypox compared to COVID-19 (Table 2). More than half of participants (69.6%) had a high level of common knowledge about monkeypox.
For willingness to adopt preventive measures against monkeypox, most participants choose travel avoidance (85.9%), followed by hygiene practices (76.3%) and social distancing (68.2%).
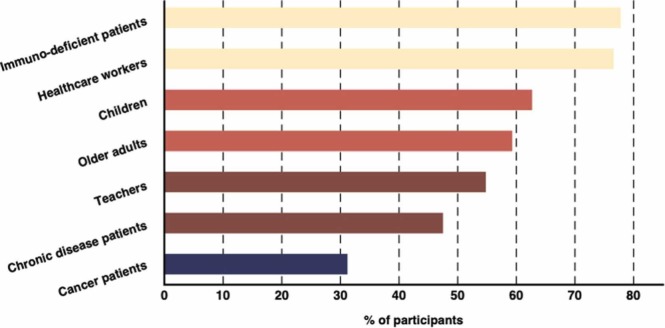
About the monkeypox vaccination, over half of the participants (68.8%) were willing to adopt monkeypox vaccine. In response to those who were unwilling to be vaccinated, most participants (60.7%) were worried about the adverse effects of vaccines, followed by felt monkeypox would not be an outbreak in China (42.3%), and they were not in a high-risk group (33.0%), or they had fewer people in daily contact (28.9%). Over three-quarters of participants (77.7%) felt that immunodeficient patients should be vaccinated, followed by healthcare workers (76.6%), children (62.7%), older adults (59.3%), teachers (54.8%), chronically disease patients (47.5%), and cancer patients (31.2%) ( Fig. 2).
Fig. 2.
The perceptions of monkeypox vaccine candidates.
Table 3 presented factors associated with being concerned about monkeypox. Compared to female participants, males (aOR 0.61, 95%CI 0.50–0.74) were less likely to worry about monkeypox. Getting monkeypox information from Internet sources (0.77, 0.61–0.98) was negatively associated with being concerned about monkeypox. Compared to students, non-student participants (unemployed: 1.98, 1.27–3.07; employed: 1.46, 1.12–1.90) were likely to be concerned about monkeypox. Willingness to adopt monkeypox vaccine (2.9, 2.38–3.53) was positively associated with being concerned about monkeypox.
Table 3.
Multivariable logistic regression estimates of factors associated with concerned about monkeypox.
| Variables | Concerned about monkeypox |
P† | Adjusted OR | P‡ | |
|---|---|---|---|---|---|
| No | Yes | ||||
| All | 796 (37.3) | 1339 (62.7) | |||
| Gender | |||||
| Female | 446 (56.0) | 891 (66.5) | <0.001 | 1.00 | |
| Male | 350 (44.0) | 448 (33.5) | 0.61 (0.50–0.74) | <0.001 | |
| Age | |||||
| 18–29 | 525 (66.0) | 778 (58.1) | 0.003 | 1.00 | |
| 30–39 | 142 (17.8) | 308 (23.0) | 1.08 (0.77–1.50) | 0.664 | |
| 40–49 | 75 (9.4) | 158 (11.8) | 1.13 (0.76–1.69) | 0.54 | |
| 50+ | 54 (6.8) | 95 (7.1) | 0.87 (0.55–1.39) | 0.569 | |
| Living area | |||||
| Rural | 91 (11.4) | 191 (14.3) | 0.071 | 1.00 | |
| Urban | 705 (88.6) | 1148 (85.7) | 0.78 (0.59–1.03) | 0.077 | |
| Steady marital status | |||||
| No | 567 (71.2) | 831 (62.1) | <0.001 | 1.00 | |
| Yes | 229 (28.8) | 508 (37.9) | 1.27 (0.95–1.71) | 0.111 | |
| Employment status | |||||
| Current student | 421 (52.9) | 565 (42.2) | <0.001 | 1.00 | |
| Unemployed | 46 (5.8) | 126 (9.4) | 1.98 (1.27–3.07) | 0.002 | |
| Employed | 329 (41.3) | 648 (48.4) | 1.46 (1.12–1.90) | 0.005 | |
| Common knowledge of monkeypox | |||||
| Low level | 265 (33.3) | 384 (28.7) | 0.028 | 1.00 | |
| High level | 531 (66.7) | 955 (71.3) | 1.15 (0.94–1.42) | 0.169 | |
| Depressive symptoms | |||||
| No | 682 (85.7) | 1160 (86.6) | 0.580 | 1.00 | |
| Yes | 114 (14.3) | 179 (13.4) | 0.88 (0.67–1.15) | 0.341 | |
| Getting monkeypox information from Internet sources | |||||
| No | 404 (50.8) | 661 (49.4) | 0.565 | 1.00 | |
| Yes | 392 (49.2) | 678 (50.6) | 0.77 (0.61–0.98) | 0.034 | |
| Getting monkeypox information from traditional media | |||||
| No | 599 (75.3) | 1040 (77.7) | 0.220 | 1.00 | |
| Yes | 197 (24.7) | 299 (22.3) | 1.11 (0.90–1.37) | 0.322 | |
| Willingness to adopt monkeypox vaccine | |||||
| No | 358 (45.0) | 309 (23.1) | <0.001 | 1.00 | |
| Yes | 438 (55.0) | 1030 (76.9) | 2.9 (2.38–3.53) | <0.001 | |
† The P-value is from the Chi-square test. ‡ The P-value is for the OR. * The statistical significance was set as P < 0.05.
As shown in Table 4, the logistic regression identified variables associated with the willingness to adopt preventive behaviors. Concerned about monkeypox was associated with the willingness to adopt preventive behaviors, including hygiene practices (2.09, 1.69–2.59), social distancing (1.78, 1.46–2.16), and travel avoidance (1.74, 1.34–2.26). Participants with a high level of common knowledge about monkeypox were likely to adopt preventive behaviors (hygiene practices: 2.09, 1.69–2.59; social distancing: 2.17, 1.77–2.66; travel avoidance: 2.78, 2.14–3.61). Compared to female participants, males were less likely to adopt social distancing (0.74, 0.61–0.90) and travel avoidance (0.71, 0.55–0.92). Getting monkeypox information from traditional media (1.29, 1.01–1.66) was associated with the willingness to adopt social distancing. Participants with depressive symptoms were less likely (0.68, 0.49–0.96) to adopt travel avoidance as a preventive measure.
Table 4.
Multivariable logistic regression estimates of factors associated with willingness to adopt preventive behaviors.
| Variables | Willingness to adopt preventive behaviors |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Hygiene practices |
Social distancing |
Travel avoidance |
|||||||
| N (%) | Adjusted OR | P† | N (%) | Adjusted OR | P† | N (%) | Adjusted OR | P† | |
| All | 1630 (76.3) | 1457 (68.2) | 1834 (85.9) | ||||||
| Gender | |||||||||
| Female | 1049 (64.4) | 1.00 | 954 (65.5) | 1.00 | 1179 (64.3) | 1.00 | |||
| Male | 581 (35.6) | 0.82 (0.66–1.02) | 0.081 | 503 (34.5) | 0.74 (0.61–0.90) | 0.003 | 655 (35.7) | 0.71 (0.55–0.92) | 0.011 |
| Age | |||||||||
| 18–29 | 1019 (62.5) | 1.00 | 914 (62.7) | 1.00 | 1138 (62.1) | 1.00 | |||
| 30–39 | 323 (19.8) | 0.76 (0.53–1.09) | 0.136 | 295 (20.2) | 0.69 (0.49–0.96) | 0.029 | 382 (20.8) | 0.82 (0.52–1.27) | 0.371 |
| 40–49 | 166 (10.2) | 0.80 (0.52–1.23) | 0.311 | 151 (10.4) | 0.74 (0.49–1.10) | 0.136 | 190 (10.4) | 0.70 (0.42–1.17) | 0.171 |
| 50+ | 122 (7.5) | 1.53 (0.89–2.64) | 0.126 | 97 (6.7) | 0.73 (0.46–1.18) | 0.201 | 124 (6.8) | 0.85 (0.46–1.58) | 0.614 |
| Living area | |||||||||
| Rural | 221 (13.6) | 1.00 | 189 (13.0) | 1.00 | 234 (12.8) | 1.00 | |||
| Urban | 1409 (86.4) | 0.90 (0.65–1.23) | 0.502 | 1268 (87.0) | 1.08 (0.82–1.43) | 0.593 | 1600 (87.2) | 1.29 (0.90–1.85) | 0.166 |
| Steady marital status | |||||||||
| No | 1084 (66.5) | 1.00 | 970 (66.6) | 1.00 | 1209 (65.9) | 1.00 | |||
| Yes | 546 (33.5) | 0.90 (0.66–1.24) | 0.521 | 487 (33.4) | 0.89 (0.66–1.20) | 0.453 | 625 (34.1) | 1.17 (0.80–1.72) | 0.421 |
| Monthly income (¥) | |||||||||
| No fixed | 765 (46.9) | 1.00 | 671 (46.1) | 1.00 | 855 (46.6) | 1.00 | |||
| < 6000 | 381 (23.4) | 1.05 (0.68–1.60) | 0.835 | 352 (24.2) | 1.14 (0.77–1.68) | 0.52 | 423 (23.1) | 1.01 (0.60–1.66) | 0.996 |
| 6000–10,000 | 263 (16.1) | 1.21 (0.74–1.95) | 0.447 | 233 (16.0) | 1.09 (0.70–1.68) | 0.714 | 293 (16.0) | 1.06 (0.59–1.89) | 0.849 |
| > 10,000 | 221 (13.6) | 0.82 (0.50–1.33) | 0.422 | 201 (13.8) | 0.88 (0.56–1.38) | 0.57 | 263 (14.3) | 0.76 (0.42–1.36) | 0.353 |
| Employment status | |||||||||
| Current student | 775 (47.5) | 1.00 | 678 (46.5) | 1.00 | 867 (47.3) | 1.00 | |||
| Unemployed | 129 (7.9) | 0.85 (0.50–1.42) | 0.529 | 116 (8.0) | 1.27 (0.78–2.05) | 0.331 | 138 (7.5) | 0.65 (0.35–1.19) | 0.163 |
| Employed | 726 (44.5) | 0.86 (0.55–1.34) | 0.496 | 663 (45.5) | 1.18 (0.79–1.79) | 0.419 | 829 (45.2) | 0.81 (0.47–1.40) | 0.455 |
| Concerning about monkeypox | |||||||||
| No | 540 (33.1) | 1.00 | 476 (32.7) | 1.00 | 648 (35.3) | 1.00 | |||
| Yes | 1090 (66.9) | 2.09 (1.69–2.59) | <0.001 | 981 (67.3) | 1.78 (1.46–2.16) | <0.001 | 1186 (64.7) | 1.74 (1.34–2.26) | <0.001 |
| Common knowledge of monkeypox | |||||||||
| Low level | 444 (27.2) | 1.00 | 366 (25.1) | 1.00 | 492 (26.8) | 1.00 | |||
| High level | 1186 (72.8) | 1.85 (1.48–2.31) | <0.001 | 1091 (74.9) | 2.17 (1.77–2.66) | <0.001 | 1342 (73.2) | 2.78 (2.14–3.61) | <0.001 |
| Depressive symptoms | |||||||||
| No | 1416 (86.9) | 1.00 | 1259 (86.4) | 1.00 | 1596 (87.0) | 1.00 | |||
| Yes | 214 (13.1) | 0.82 (0.62–1.10) | 0.189 | 198 (13.6) | 0.95 (0.72–1.25) | 0.699 | 238 (13.0) | 0.68 (0.49–0.96) | 0.027 |
| Getting monkeypox information from Internet sources | |||||||||
| No | 803 (49.3) | 1.00 | 720 (49.4) | 1.00 | 888 (48.4) | 1.00 | |||
| Yes | 827 (50.7) | 0.90 (0.71–1.13) | 0.362 | 737 (50.6) | 0.81 (0.66–1.00) | 0.052 | 946 (51.6) | 1.10 (0.82–1.46) | 0.529 |
| Getting monkeypox information from traditional media | |||||||||
| No | 1234 (75.7) | 1.00 | 1102 (75.6) | 1.00 | 1391 (75.8) | 1.00 | |||
| Yes | 396 (24.3) | 1.30 (0.99–1.72) | 0.063 | 355 (24.4) | 1.29 (1.01–1.66) | 0.046 | 443 (24.2) | 1.26 (0.88–1.79) | 0.211 |
† The P-value is from the Chi-square test. * The statistical significance was set as P < 0.05.
Table 5 shown multivariable logistic regression estimates of factors associated with willingness to adopt the monkeypox vaccine. Participants in the 18–29 age group were more likely to adopt the vaccine than participants in older age groups (40–49 age group: 0.57, 0.38–0.85, 50 + age group: 0.50, 0.31–0.81). Participants with post-graduate degrees were less likely (0.41, 0.29–0.58) to adopt the vaccine than those who had below undergraduate degrees. Similarly, participants in higher-income groups (¥6000–10,000 group: 0.61, 0.39–0.95;>¥10,000 group: 0.48, 0.30–0.77) were less likely to adopt the monkeypox vaccine. Besides, getting monkeypox information from traditional media (1.29, 1.01–1.66) and being concerned more about monkeypox compared to COVID-19 (1.63, 1.31–2.02) were associated with the willingness to adopt the vaccine. Participants with a high level of common knowledge about monkeypox (1.34, 1.09–1.66) were likely to adopt preventive behaviors.
Table 5.
Multivariable logistic regression estimates of factors associated with willingness to adopt monkeypox vaccine.
| Variables | Willingness to adopt monkeypox vaccine |
P | Adjusted OR | P | |
|---|---|---|---|---|---|
| No | Yes | ||||
| All | 667 (31.2) | 1468 (68.8) | |||
| Gender | |||||
| Female | 405 (60.7) | 932 (63.5) | 0.239 | 1.00 | |
| Male | 262 (39.3) | 536 (36.5) | 0.93 (0.76–1.14) | 0.511 | |
| Age | |||||
| 18–29 | 365 (54.7) | 938 (63.9) | <0.001 | 1.00 | |
| 30–39 | 148 (22.2) | 302 (20.6) | 0.83 (0.59–1.17) | 0.283 | |
| 40–49 | 95 (14.2) | 138 (9.4) | 0.57 (0.38–0.85) | 0.006 | |
| 50+ | 59 (8.8) | 90 (6.1) | 0.50 (0.31–0.81) | 0.004 | |
| Living area | |||||
| Rural | 66 (9.9) | 216 (14.7) | 0.003 | 1.00 | |
| Urban | 601 (90.1) | 1252 (85.3) | 0.78 (0.57–1.06) | 0.109 | |
| Educational level | |||||
| Below undergraduate | 108 (16.2) | 299 (20.4) | <0.001 | 1.00 | |
| Undergraduate | 267 (40.0) | 745 (50.7) | 0.80 (0.58–1.08) | 0.146 | |
| Postgraduate | 292 (43.8) | 424 (28.9) | 0.41 (0.29–0.58) | <0.001 | |
| Steady marital status | |||||
| No | 402 (60.3) | 996 (67.8) | 0.001 | 1.00 | |
| Yes | 265 (39.7) | 472 (32.2) | 0.90 (0.67–1.21) | 0.482 | |
| Employment status | |||||
| Current student | 282 (42.3) | 704 (48.0) | 0.020 | 1.00 | |
| Unemployed | 50 (7.5) | 122 (8.3) | 1.34 (0.79–2.26) | 0.279 | |
| Employed | 335 (50.2) | 642 (43.7) | 1.21 (0.79–1.86) | 0.373 | |
| Monthly income (¥) | |||||
| No fixed | 264 (39.6) | 711 (48.4) | <0.001 | 1.00 | |
| < 6000 | 136 (20.4) | 358 (24.4) | 0.73 (0.49–1.09) | 0.129 | |
| 6000–10,000 | 121 (18.1) | 220 (15.0) | 0.61 (0.39–0.95) | 0.031 | |
| > 10,000 | 146 (21.9) | 179 (12.2) | 0.48 (0.30–0.77) | 0.002 | |
| Common knowledge of monkeypox | |||||
| Low level | 234 (35.1) | 415 (28.3) | 0.002 | 1.00 | |
| High level | 433 (64.9) | 1053 (71.7) | 1.34 (1.09–1.66) | 0.006 | |
| Depressive symptoms | |||||
| No | 577 (86.5) | 1265 (86.2) | 0.888 | 1.00 | |
| Yes | 90 (13.5) | 203 (13.8) | 0.93 (0.71–1.24) | 0.633 | |
| Getting monkeypox information from Internet sources | |||||
| No | 355 (53.2) | 710 (48.4) | 0.042 | 1.00 | |
| Yes | 312 (46.8) | 758 (51.6) | 0.98 (0.80–1.22) | 0.888 | |
| Getting monkeypox information from traditional media | |||||
| No | 550 (82.5) | 1089 (74.2) | <0.001 | 1.00 | |
| Yes | 117 (17.5) | 379 (25.8) | 1.80 (1.38–2.34) | <0.001 | |
| Concerned more about monkeypox compared to COVID-19 | |||||
| No | 493 (73.9) | 934 (63.6) | <0.001 | 1.00 | |
| Yes | 174 (26.1) | 534 (36.4) | 1.63 (1.31–2.02) | <0.001 | |
† The P-value is from the Chi-square test. ‡ The P-value is for the OR. * The statistical significance was set as P < 0.05.
Discussion
This study analyzed the public's perceptions, concerns, and attitudes toward monkeypox. Unlike previous studies [14], [15], [16], our study assessed public awareness and knowledge of monkeypox and was not limited to a specific population. The individuals' perceived protective behaviors were affected by their perception of infection risk, especially in the early stages of 2022 multi-country outbreak. Under this hypothesis, our study identified factors influencing concerned about monkeypox, perception of preventive behaviors, and acceptance of monkeypox vaccine. These findings could be a reference for health policies promoting the adoption of preventive behaviors, strengthening health education about monkeypox, and encouraging vaccination in the future.
We found that 62.7% of participants were concerned about monkeypox outbreak, even over half of participants were worried that it would become a global pandemic. However, only 33.2% of participants were more concerned about monkeypox than COVID-19. It means that compared with COVID-19, monkeypox failed to get much attention. Besides, getting information and common knowledge levels about monkeypox before the survey were insufficient. These findings suggest that knowledge about monkeypox or other smallpox-like infectious diseases, including common knowledge and preventive measures, should become an essential aspect of health education about infectious diseases.
We found several factors associated with being concerned about monkeypox, including gender, employment status, and the sources which access monkeypox information. Correlates of sociodemographic variables suggested a greater focus on health education for both student and male groups. The Internet was a candidate medium for health education.
The monkeypox virus is mainly transmitted through large respiratory droplets, close or direct contact with skin lesions, and possibly through contaminated fomites [9]. Therefore, adopting effective preventive behaviors was crucial to contain the spread of monkeypox. In this study, we found participants with a high level of common knowledge about monkeypox were more willing to adopt preventive behaviors, including hygiene practices, social distancing, and travel avoidance. It again highlighted the importance of health education about infectious diseases in the general population. In addition, females tend to percept hygiene practices and travel avoidance as preventing measures compared to men. Similar findings about gender differences in adopting preventive behaviors had been reported in previous studies [28], [29]. Furthermore, the results suggest that access to monkeypox-related news through traditional media was associated with perception of social distancing. During the COVID-19 pandemic, the government generally released official information through traditional media. The finding suggested that recommendations about preventive measures, especially social distancing, published through traditional media were more likely to be adopted by the public. Similar results were found in a previous study in Saudi Arabia on public beliefs about COVID-19 [30].
A previous study about vaccination acceptance among the general population in Saudi Arabia indicated that the public is divided into vaccine acceptance and refusal whenever available [31]. Vaccine hesitancy was one of the great challenges in adopting vaccinations to fight epidemics. Therefore, public acceptance of the monkeypox vaccine deserves research at this stage. We found several sociodemographic variables are associated with the acceptance of vaccination, including age, educational level, and monthly income. Younger participants tended to be more accepting of vaccination. One possible explanation is that the young population may trust modern medical techniques more than older adults [31]. Similar to previous research [32], [33], [34], we also found that vaccine hesitancy was more likely to occur among participants with higher income and educational levels. Differences in vaccine acceptance between high- and low-income groups may be due to the former's more accessible access to accurate/reliable sources of information [31], [34]. This difference between the low- and high-educational level groups was attributed to the latter having more background knowledge [31], [33]. In either case, they would need time for further research to confirm the effectiveness and safety of vaccination before they are willing to vaccinate. Similar to the findings about preventive measures in our study, traditional media may be ideal for promoting vaccination.
The current study has certain limitations. First, our study is limited by cross-sectional surveys such as convenience sampling and possible recall bias. Second, this online survey potentially introduced selection bias, as participants were limited to those who could access the Internet only. Therefore, the generalizability of the findings needs to be interpreted with caution. Future studies could be implemented through a combination of online and offline approaches to increase sample representativeness. Furthermore, the public's acceptance and beliefs may change over time. Therefore, cohort studies may be considered to observe this dynamic change in the future.
Conclusions
Understanding the public's perceived beliefs, attitudes, willingness to adopt preventive behaviors, and vaccine acceptance were crucial for developing response measures during an emerging pandemic. Compared with COVID-19, monkeypox attracted significantly less attention in the public in China. In addition, there was insufficient knowledge about monkeypox among the Chinese public. In response to the possible pandemic, health education about monkeypox or other smallpox-like infectious diseases should be strengthened in the general population. Targeting specific groups by providing appropriate resources or directing tailored interventions for the public’s behaviors can help promote the adoption of preventive measures and vaccination against monkeypox.
Ethics approval and consent to participate
All procedures contributing to this work comply with the ethical standards of relevant national and institutional committees on human experimentation and with the Helsinki Declaration. Online informed consent will be obtained from all participants before any procedure of this Study. The Study (including online informed consent) was approved by the Human Research Ethics Committee of the School of Public Health (Shenzhen), Sun Yat-sen University (approval number SYSU-PHS[2022]051).
Funding
This study was supported by the Natural Science Foundation of China International/Regional Research Collaboration Project [72061137001], Natural Science Foundation of China Excellent Young Scientists Fund [82022064], Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences [2020-JKCS-030], Natural Science Foundation of China Young Scientist Fund [81703278], the National Science and Technology Major Project of China [2018ZX10721102], the Sanming Project of Medicine in Shenzhen [SZSM201811071], the High Level Project of Medicine in Longhua, Shenzhen [HLPM201907020105], the National Key Research and Development Program of China [2020YFC0840900], the Shenzhen Science and Technology Innovation Commission Basic Research Program [JCYJ20190807155409373], Special Support Plan for High-Level Talents of Guangdong Province [2019TQ05Y230], and the Fundamental Research Funds for the Central Universities [58000-31620005]. All funding parties did not have any role in the study design or data explanation.
Authors’ contributions
HZ conceived the study. BW and XP conducted this study. BW, XP, YL, and LF drafted the manuscript. TT, SY, YC, WX, QL, YL, XM, and HZ revised the manuscript. All authors have read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
We thank our partners, including Wuxi CDC and Chongqing CDC, Guangdong Association of STD & AIDS Prevention and Control, and Guangdong Youth Sexual Health Union. We thank Yatao Wang, Zhilu Yao, Huifang Xu from Guangdong Association of STD & AIDS Prevention and Control, Chengjia Xu, and Zhenwei Liang from Guangdong Youth Sexual Health Union for their help in recruiting participants. We thank Yu Jie from School of Sociology and Anthropology, Xiamen University for his comments in the preparation of this manuscript. We thank all participants who made this research possible.
Consent to publish
Not applicable.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jiph.2022.12.010.
Appendix A. Supplementary material
Supplementary material
.
Data availability
The data collected and questionnaire in this study will not be publicly available. However, the corresponding author can be contacted for de-identified data and questionnaire upon reasonable request.
References
- 1.Thornhill J.P., Barkati S., Walmsley S., Rockstroh J., Antinori A., Harrison L.B., et al. Monkeypox virus infection in humans across 16 countries - April-June 2022. N Engl J Med. 2022 doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 2.Bunge E.M., Hoet B., Chen L., Lienert F., Weidenthaler H., Baer L.R., et al. The changing epidemiology of human monkeypox—a potential threat? A systematic review. PLoS Negl Trop Dis. 2022;16:1–20. doi: 10.1371/journal.pntd.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilson M.E., Hughes J.M., McCollum A.M., Damon I.K. Human monkeypox. Clin Infect Dis. 2014;58:260–267. doi: 10.1093/cid/cit703. [DOI] [PubMed] [Google Scholar]
- 4.Heymann D.L., Simpson K. The evolving epidemiology of human monkeypox: questions still to be answered. J Infect Dis. 2021;223:1839–1841. doi: 10.1093/infdis/jiab135. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. 2022 Monkeypox Outbreak Cases & Data 2022. 〈https://www.cdc.gov/poxvirus/monkeypox/response/2022/〉.
- 6.Petersen E., Kantele A., Koopmans M., Asogun D., Yinka-Ogunleye A., Ihekweazu C., et al. Human monkeypox: epidemiologic and clinical characteristics, diagnosis, and prevention. Infect Dis Clin N Am. 2019;33:1027–1043. doi: 10.1016/j.idc.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adalja A., Inglesby T. A novel international monkeypox outbreak. Ann Intern Med. 2022;175:1175–1176. doi: 10.7326/M22-1581. [DOI] [PubMed] [Google Scholar]
- 8.Kumar N., Acharya A., Gendelman H.E., Byrareddy S.N. The 2022 outbreak and the pathobiology of the monkeypox virus. J Autoimmun. 2022;131 doi: 10.1016/j.jaut.2022.102855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Z. Monkeypox: a potential global threat. J Med Virol. 2022;94:4034–4036. doi: 10.1002/jmv.27884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiu X., Wang A., Qian Q., Wu S. The US public’s perception of the threat of COVID-19 during the rapid spread of the COVID-19 outbreak: cross-sectional survey study. J Med Internet Res. 2021;23:1–20. doi: 10.2196/23400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu J., Peng Z. People at risk of influenza pandemics: the evolution of perception and behavior. PLoS One. 2015;10:1–14. doi: 10.1371/journal.pone.0144868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim Y., Zhong W., Jehn M., Walsh L. Public risk perceptions and preventive behaviors during the 2009 H1N1 influenza pandemic. Disaster Med Public Health Prep. 2015;9:145–154. doi: 10.1017/dmp.2014.87. [DOI] [PubMed] [Google Scholar]
- 13.Yu F., Geldsetzer P., Meierkord A., Yang J., Chen Q., Jiao L., et al. Knowledge about COVID-19 among adults in China: cross-sectional online survey. J Med Internet Res. 2021:23. doi: 10.2196/26940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y., Zhou R., Chen B., Chen H., Li Y., Chen Z., et al. Knowledge, perceived beliefs, and preventive behaviors related to covid-19 among Chinese older adults: cross-sectional web-based survey. J Med Internet Res. 2020:22. doi: 10.2196/23729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yin Q., Chen A., Song X., Deng G., Dong W. Risk perception and PTSD symptoms of medical staff combating against COVID-19: a PLS structural equation model. Front Psychiatry. 2021;12:1–10. doi: 10.3389/fpsyt.2021.607612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Y., Liu R.De, Ding Y., Wang J., Hong W., Wu Y. The influence of communication on college students’ self–other risk perceptions of covid-19: a comparative study of china and the united states. Int J Environ Res Public Health. 2021:18. doi: 10.3390/ijerph182312491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ding Y., Du X., Li Q., Zhang M., Zhang Q., Tan X., et al. Risk perception of coronavirus disease 2019 (COVID-19) and its related factors among college students in China during quarantine. PLoS One. 2020;15:1–13. doi: 10.1371/journal.pone.0237626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cyberspace Administration of China. The 47th China statistical report on Internet development. n.d.
- 19.Questionnaire- PH. The PHQ-2 in Dermatology — Standardized Screening for Depression and Suicidal Ideation 2022;154:15–7. [DOI] [PubMed]
- 20.Ransing R., Deshpande S.N., Shete S.R., Patil I., Kukreti P., Raghuveer P., et al. Assessing antenatal depression in primary care with the PHQ-2 and PHQ-9: can it be carried out by auxiliary nurse midwife (ANM)? Asian J Psychiatry. 2020:53. doi: 10.1016/j.ajp.2020.102109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schuler M., Strohmayer M., Mühlig S., Schwaighofer B., Wittmann M., Faller H., et al. Assessment of depression before and after inpatient rehabilitation in COPD patients: psychometric properties of the German version of the Patient Health Questionnaire (PHQ-9/PHQ-2) J Affect Disord. 2018;232:268–275. doi: 10.1016/j.jad.2018.02.037. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y.L., Liang W., Chen Z.M., Zhang H.M., Zhang J.H., Weng X.Q., et al. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia-Pac Psychiatry. 2013;5:268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 23.KristinWalter P.M. What is monkeypox. JAMA J Am Med Assoc. 2022;327:2278–2279. doi: 10.1001/jama.2022.9499. [DOI] [Google Scholar]
- 24.Temsah M.H., Aljamaan F., Alenezi S., Alhasan K., Saddik B., Al-Barag A., et al. Monkeypox caused less worry than COVID-19 among the general population during the first month of the WHO Monkeypox alert: experience from Saudi Arabia. Travel Med Infect Dis. 2022;49 doi: 10.1016/j.tmaid.2022.102426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alkhaldi G., Aljuraiban G.S., Alhurishi S., De Souza R., Lamahewa K., Lau R., et al. Perceptions towards COVID-19 and adoption of preventive measures among the public in Saudi Arabia: a cross sectional study. BMC Public Health. 2021;21:1251. doi: 10.1186/s12889-021-11223-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Humer E., Jesser A., Plener P.L., Probst T., Pieh C. Education level and COVID-19 vaccination willingness in adolescents. Eur Child Adolesc Psychiatry. 2021:4–6. doi: 10.1007/s00787-021-01878-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Othman S.S., Alsuwaidi A., Aseel R., Alotaibi R., Bablgoom R., alsulami G., et al. Association between social media use and the acceptance of COVID-19 vaccination among the general population in Saudi Arabia – a cross-sectional study. BMC Public Health. 2022;22:1–11. doi: 10.1186/s12889-022-12757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eastwood K., Durrheim D., Francis J.L., D’Espaignet E.T., Duncan S., Islam F., et al. Knowledge about pandemic influenza and compliance with containment measures among Australians. Bull World Health Organ. 2009;87:588–594. doi: 10.2471/BLT.08.060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seale H., Heywood A.E., Leask J., Sheel M., Thomas S., Durrheim D.N., et al. COVID-19 is rapidly changing: examining public perceptions and behaviors in response to this evolving pandemic. PLoS One. 2020;15:1–13. doi: 10.1371/journal.pone.0235112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Almutairi A.F., Mustafa A.B., Alessa Y.M., Almutairi S.B., Almaleh Y. Public trust and compliance with the precautionary measures against COVID-19 employed by authorities in Saudi Arabia. Risk Manag Healthc Policy. 2020;13:753–760. doi: 10.2147/RMHP.S257287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Magadmi R.M., Kamel F.O. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health. 2021;21:1–8. doi: 10.1186/s12889-021-11501-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cata-Preta B., de O., Wehrmeister F.C., Santos T.M., Barros A.J.D., Victora C.G. Patterns in wealth-related inequalities in 86 low- and middle-income countries: global evidence on the emergence of vaccine hesitancy. Am J Prev Med. 2021;60:S24–S33. doi: 10.1016/j.amepre.2020.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phadke V.K., Bednarczyk R.A., Salmon D.A., Omer S.B. Association between vaccine refusal and vaccine-preventable diseases in the United States a review of measles and pertussis. JAMA J Am Med Assoc. 2016;315:1149–1158. doi: 10.1001/jama.2016.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moola S., Gudi N., Nambiar D., Dumka N., Ahmed T., Sonawane I.R., et al. A rapid review of evidence on the determinants of and strategies for COVID-19 vaccine acceptance in low- and middle-income countries. J Glob Health. 2021:11. doi: 10.7189/JOGH.11.05027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The data collected and questionnaire in this study will not be publicly available. However, the corresponding author can be contacted for de-identified data and questionnaire upon reasonable request.