Abstract
Background
Peripheral intravenous cannulation is one of the most fundamental and common procedures in medicine. Securing a peripheral line is occasionally difficult with the landmark method. Ultrasound guidance has become a standard procedure for central venous cannulation, but its efficacy in achieving peripheral venous cannulation is unclear.
Objectives
To evaluate the effectiveness and safety of ultrasound guidance compared to the landmark method for peripheral intravenous cannulation in adults.
Search methods
We used standard, extensive Cochrane search methods. The latest search date was 29 November 2021.
Selection criteria
We included randomised controlled trials (RCTs) and quasi‐RCTs (RCTs in which participants are systematically allocated based on data such as date of birth or recruitment) comparing the effects of ultrasound guidance to the landmark method for peripheral intravenous cannulation in adults.
Data collection and analysis
We used standard Cochrane methods. Our primary outcomes were first‐pass success of cannulation, overall success of cannulation, and pain. Our secondary outcomes were procedure time for first‐pass cannulation, procedure time for overall cannulation, number of attempts, patient satisfaction, and overall complications. We used GRADE to assess the certainty of the evidence.
Placing a peripheral intravenous line in individuals can be classed as ‘difficult’, ‘moderate’, or ‘easy’. We use the terms ‘difficult participants’, ‘moderate/moderately difficult participants’ and ‘easy participants’ as shorthand to characterise the difficulty level in placing a peripheral line using the landmark method. We used the original studies’ definitions of difficulty levels of peripheral intravenous cannulation with the landmark method. We analysed the results in these subgroups: ‘difficult participants’, ‘moderate participants’, and ‘easy participants’. We did this because we expected the effect of ultrasound‐guided peripheral venous cannulation to be largest in participants classed as ‘difficult’ and smaller in participants classed as ‘moderate’ and ‘easy’.
Main results
We included 14 RCTs and two quasi‐RCTs involving 2267 participants undergoing peripheral intravenous cannulation. Participants were classed as 'difficult' in 12 studies (880 participants), 'moderate' in one study (401 participants), and 'easy' in one study (596 participants). Two studies (390 participants) did not restrict by landmark method difficulty level. The overall risk of bias assessments ranged from low to high. We judged studies to be at high risk of bias mainly because of concerns about blinding for subjective outcomes.
In difficult participants, ultrasound guidance increased the first‐pass success of cannulation (risk ratio (RR) 1.50, 95% confidence interval (95% CI) 1.15 to 1.95; 10 studies, 815 participants; low‐certainty evidence), and the overall success of cannulation (RR 1.40, 95% CI 1.10 to 1.77; 10 studies, 670 participants; very low‐certainty evidence). There was no clear difference in pain (mean difference (MD) ‐0.20, 95% CI ‐1.13 to 0.72; 4 studies, 323 participants; very low‐certainty evidence; numerical rating scale (NRS) 0 to 10 where 10 is maximum pain). Ultrasound guidance increased the procedure time for first‐pass cannulation (MD 119.9 seconds, 95% CI 88.6 to 151.1; 2 studies, 219 participants; low‐certainty evidence), and patient satisfaction (standardised mean difference (SMD) 0.49, 95% CI 0.07 to 0.92; 5 studies, 333 participants; very low‐certainty evidence; NRS 0 to 10 where 10 is maximum satisfaction). Ultrasound guidance decreased the number of cannulation attempts (MD ‐0.33, 95% CI ‐0.64 to ‐0.02; 9 studies, 568 participants; very low‐certainty evidence). Ultrasound guidance showed no clear difference in the procedure time for overall cannulation (MD ‐24.9 seconds, 95% CI ‐323.1 to 273.3; 8 studies, 413 participants; very low‐certainty evidence) and overall complications (RR 0.64, 95% CI 0.37 to 1.10; 5 studies, 431 participants; low‐certainty evidence).
In moderate participants, ultrasound guidance increased the first‐pass success of cannulation (RR 1.14, 95% CI 1.02 to 1.27; 1 study, 401 participants; moderate‐certainty evidence). No studies assessed the overall success of cannulation. There was no clear difference in pain (MD 0.10, 95% CI ‐0.47 to 0.67; 1 study, 401 participants; low‐certainty evidence; NRS 0 to 10 where 10 is maximum pain). Ultrasound guidance increased the procedure time for first‐pass cannulation (MD 95.2 seconds, 95% CI 72.8 to 117.6; 1 study, 401 participants; high‐certainty evidence). Ultrasound guidance showed no clear difference in overall complications (RR 0.83, 95% CI 0.38 to 1.82; 1 study, 401 participants; moderate‐certainty evidence). No studies assessed the procedure time for overall cannulation, number of cannulation attempts, or patient satisfaction.
In easy participants, ultrasound guidance decreased the first‐pass success of cannulation (RR 0.89, 95% CI 0.85 to 0.94; 1 study, 596 participants; high‐certainty evidence). No studies assessed the overall success of cannulation. Ultrasound guidance increased pain (MD 0.60, 95% CI 0.17 to 1.03; 1 study, 596 participants; moderate‐certainty evidence; NRS 0 to 10 where 10 is maximum pain). Ultrasound guidance increased the procedure time for first‐pass cannulation (MD 94.8 seconds, 95% CI 81.2 to 108.5; 1 study, 596 participants; high‐certainty evidence). Ultrasound guidance showed no clear difference in overall complications (RR 2.48, 95% CI 0.90 to 6.87; 1 study, 596 participants; moderate‐certainty evidence). No studies assessed the procedure time for overall cannulation, number of cannulation attempts, or patient satisfaction.
Authors' conclusions
There is very low‐ and low‐certainty evidence that, compared to the landmark method, ultrasound guidance may benefit difficult participants for increased first‐pass and overall success of cannulation, with no difference detected in pain. There is moderate‐ and low‐certainty evidence that, compared to the landmark method, ultrasound guidance may benefit moderately difficult participants due to a small increased first‐pass success of cannulation with no difference detected in pain. There is moderate‐ and high‐certainty evidence that, compared to the landmark method, ultrasound guidance does not benefit easy participants: ultrasound guidance decreased the first‐pass success of cannulation with no difference detected in overall success of cannulation and increased pain.
Keywords: Adult; Humans; Catheterization, Central Venous; Catheterization, Central Venous/methods; Catheterization, Peripheral; Catheterization, Peripheral/adverse effects; Pain; Randomized Controlled Trials as Topic
Plain language summary
Is ultrasound guidance a good option for peripheral intravenous cannulation in adults?
What is peripheral intravenous cannulation?
Placing a peripheral intravenous line is one of the most essential procedures in medicine. It involves putting a thin, flexible tube (known as a catheter or cannula) into a vein using a needle. This process is known as 'cannulation'. It is necessary when administering fluids, drugs, and drawing blood samples.
Peripheral intravenous cannulation is usually carried out by seeing and touching a target vein in the hand or arm. This is known as the landmark method. Placing a peripheral intravenous line is sometimes difficult, requiring multiple needle punctures if healthcare providers cannot find a suitable vein. If peripheral intravenous cannulation fails with the landmark method, a central venous line in the neck or chest is often the next step. However, central venous line placement can have serious complications, such as infection, thrombosis (blood clots), and pneumothorax (collapsed lung). It is also more time‐consuming and costly. Therefore, the insertion of a central venous line should be a last resort.
How can ultrasound guidance (USG) help?
Ultrasound can find target veins invisible to the eye. Ultrasound also allows healthcare providers to see the needle and important surrounding structures that should not be damaged when inserting the tube. Ultrasound guidance is often used to help central venous cannulation, but the usefulness for peripheral venous cannulation remains unclear.
What did we want to find out?
We wanted to find out if ultrasound guidance was useful and safe compared to the landmark method for peripheral intravenous cannulation in adults. We also wanted to find out if using ultrasound guidance was different in people when cannulation was classed as difficult, moderately difficult, or easy.
What did we do?
We systematically searched for studies comparing the effects of ultrasound guidance to the landmark method on peripheral intravenous cannulation in adults. We combined the studies' results, and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found 16 studies with 2267 participants comparing peripheral intravenous cannulation using ultrasound guidance to the landmark method. The effect of ultrasound guidance was dependent on the difficulty levels of cannulating people using the landmark method. The largest effect was seen in people classed as 'difficult' to cannulate, and the effect became smaller as the difficulty decreased.
‐ In 'difficult' patients, ultrasound guidance may increase the first‐pass success of cannulation (that is, successful insertion of the tube on the first attempt), overall success of cannulation, and did not have a clear effect on people's pain.
‐ In 'moderately difficult' patients, ultrasound guidance probably increased the first‐pass success of cannulation, and there was no clear effect on people's pain. No studies assessed the overall success of cannulation.
‐ In 'easy' patients, ultrasound guidance decreased the first‐pass success of cannulation and probably increased people's pain. No studies assessed the overall success of cannulation.
What are the limitations of the evidence?
We are not very confident in this evidence because studies did not always measure outcomes in reliable ways. In addition, the studies varied in how they defined difficulty levels with the landmark method and 'puncture failure'.
How up to date is this evidence?
This evidence is up to date to November 2021. We identified six ongoing studies. We will include results from these studies in future updates.
Key messages
In people where peripheral intravenous cannulation using the landmark method is difficult, ultrasound guidance may increase the first‐pass and overall success of cannulation and has no clear effect on pain. In moderately difficult patients, ultrasound guidance probably increases the first‐pass success of cannulation slightly and may have no clear effect on pain. In easy patients, ultrasound guidance reduces the first‐pass success of cannulation and probably increases pain slightly.
The lack of common definitions amongst the included studies for difficulty levels with the landmark method and puncture failure undermined the results. Future studies should use common definitions.
Summary of findings
Summary of findings 1. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults classed as difficult.
|
Patient or population: adults undergoing peripheral venous cannulation classed as difficulta Settings: emergency department, ICU, operating room Intervention: USG Comparison: LM | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with LM | Risk with USG | |||||
|
First‐pass success of cannulation Follow‐up: immediately after the procedure |
358 per 1000 | 537 per 1000 (421 to 698) | RR 1.50 (1.15 to 1.95) | 815 (10 RCTs) | ⊕⊕⊝⊝
Lowb |
|
|
Overall success of cannulation Follow‐up: immediately after the procedure |
575 per 1000 | 806 per 1000 (633 to 1000) | RR 1.40 (1.10 to 1.77) | 670 (10 RCTs) | ⊕⊝⊝⊝
Very lowc |
|
|
Pain NRS: from 0 to 10, where 10 is maximum pain Follow‐up: immediately after the procedure |
The mean pain score was 3.97 | MD 0.20 lower (1.13 lower to 0.72 higher) | ‐ | 323 (4 RCTs) | ⊕⊝⊝⊝ Very lowd | |
|
Procedure time for first‐pass cannulation (seconds) Follow‐up: immediately after the procedure |
The mean procedure time for first‐pass cannulation was 130.5 seconds | MD 119.9 seconds longer (88.6 longer to 151.1 longer) | ‐ | 219 (2 RCTs) | ⊕⊕⊝⊝
Lowe |
|
|
Number of cannulation attempts Follow‐up: immediately after the procedure |
The mean number of cannulation attempts was 2.15 | MD 0.33 lower (0.64 lower to 0.02 lower) | ‐ | 568 (9 RCTs) | ⊕⊝⊝⊝ Very lowf | |
|
Patient satisfaction NRS from 0 to 10 or 4‐step Likert scale The higher the score, the higher the level of satisfaction Follow‐up: immediately after the procedure |
The mean patient satisfaction score was 5.61 | SMD 0.49 higher (0.07 higher to 0.92 higher) | ‐ | 333 (5 RCTs) | ⊕⊝⊝⊝ Very lowg | |
|
Overall complications Follow‐up: immediately after the procedure |
121 per 1000 |
78 per 1000 (45 to 133) |
RR 0.64 (0.37 to 1.10) |
431 (5 RCTs) | ⊕⊕⊝⊝ Lowh | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; ICU: intensive care unit; LM: landmark method; MD: mean difference; NRS: numeric rating scale; RCTs: randomised controlled trials; RR: risk ratio; SMD: standardised mean difference; USG: ultrasound guidance | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aParticipants were classified according to the original studies' definitions. bWe downgraded by a total of two levels to low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors) and substantial inconsistency. There was minimal risk of publication bias (one small study was asymmetrical but would have had little impact). cWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors) and serious inconsistency due to the lack of a standardised definition of failure. There was minimal risk of publication bias (two quasi‐randomised trials were asymmetrical). dWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors, and incomplete outcome data), substantial inconsistency, and imprecision. eWe downgraded by a total of two levels to low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors), and imprecision. fWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors, and incomplete outcome data) and inconsistency due to heterogeneity and the lack of a standardised definition of failure. gWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors, and incomplete outcome data), substantial inconsistency, and imprecision. hWe downgraded by a total of two levels to low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors), and imprecision.
Summary of findings 2. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults classed as moderately difficult.
|
Patient or population: adults undergoing peripheral venous cannulation classed as moderately difficulta Settings: emergency department Intervention: USG Comparison: LM | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with LM | Risk with USG | |||||
|
First‐pass success of cannulation Follow‐up: immediately after the procedure |
714 per 1000 | 813 per 1000 (728 to 906) | RR 1.14 (1.02 to 1.27) | 401 (1 RCT) | ⊕⊕⊕⊝ Moderateb | |
|
Overall success of cannulation Follow‐up: immediately after the procedure |
See comment | ‐ | ‐ | ‐ | ‐ | None of the studies included moderately difficult participants |
|
Pain NRS: from 0 to 10, where 10 is maximum pain Follow‐up: immediately after the procedure |
The mean pain score was 3.20 | MD 0.10 higher (0.47 lower to 0.67 higher) | 401 (1 RCT) |
⊕⊕⊝⊝
Lowc |
||
|
Procedure time for first‐pass cannulation (seconds) Follow‐up: immediately after the procedure |
The mean procedure time for first‐pass cannulation was 122.6 seconds | MD 95.2 seconds longer (72.8 longer to 117.6 longer) | 401 (1 RCT) |
⊕⊕⊕⊕ High | ||
|
Number of cannulation attempts Follow‐up: immediately after the procedure |
See comment | ‐ | ‐ | ‐ | ‐ | None of the studies included moderately difficult participants |
|
Patient satisfaction NRS from 0 to 10 or 4‐step Likert scale The higher the score the higher the level of satisfaction Follow‐up: immediately after the procedure |
See comment | ‐ | ‐ | ‐ | ‐ | None of the studies included moderately difficult participants |
|
Overall complications Follow‐up: immediately after the procedure |
65 per 1000 | 54 per 1000 (25 to 119) | RR 0.83 (0.38 to 1.82) | 401 (1 RCT) | ⊕⊕⊕⊝ Moderated | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; LM: landmark; MD: mean difference; NRS: numeric rating scale; RCTs: randomised controlled trials; RR: risk ratio; USG: ultrasound guidance | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aParticipants were classified according to the original studies' definitions. bWe downgraded by one level to moderate certainty due to imprecision. cWe downgraded by a total of two levels to low certainty due to risk of bias concerns (lack of blinding of the outcome assessors) and imprecision. dWe downgraded by one level to moderate certainty due to imprecision.
Summary of findings 3. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults classed as easy.
|
Patient or population: adults undergoing peripheral venous cannulation classed as easya Settings: emergency department Intervention: USG Comparison: LM | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with LM | Risk with USG | |||||
|
First‐pass success of cannulation Follow‐up: immediately after the procedure |
966 per 1000 | 859 per 1000 (821 to 908) | RR 0.89 (0.85 to 0.94) | 596 (1 RCT) |
⊕⊕⊕⊕ High | |
|
Overall success of cannulation Follow‐up: immediately after the procedure |
See comment | ‐ | ‐ | ‐ | ‐ | None of the studies included easy participants |
|
Pain NRS: from 0 to 10, where 10 is maximum pain Follow‐up: immediately after the procedure |
The mean pain score was 2.30 | MD 0.60 higher (0.17 higher to 1.03 higher) | 596 (1 RCT) |
⊕⊕⊕⊝
Moderateb |
||
|
Procedure time for first‐pass cannulation (seconds) Follow‐up: immediately after the procedure |
The mean procedure time for first‐pass cannulation was 89.7 seconds | MD 94.8 seconds longer (81.2 longer to 108.5 longer) | 596 (1 RCT) |
⊕⊕⊕⊕ High | ||
|
Number of cannulation attempts Follow‐up: immediately after the procedure |
See comment | ‐ | ‐ | ‐ | ‐ | None of the studies included easy participants |
|
Patient satisfaction NRS from 0 to 10 or 4‐step Likert scale The higher the score, the higher the level of satisfaction Follow‐up: immediately after the procedure |
See comment | ‐ | ‐ | ‐ | ‐ | None of the studies included easy participants |
|
Overall complications Follow‐up: immediately after the procedure |
17 per 1000 | 43 per 1000 (15 to 118) | RR 2.48 (0.90 to 6.87) | 596 (1 RCT) | ⊕⊕⊕⊝ Moderatec | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; LM: landmark; NRS: numeric rating scale; RCTs: randomised controlled trials; RR: risk ratio; USG: ultrasound guidance | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aParticipants were classified according to the original studies' definitions. bWe downgraded by one level to moderate certainty due to risk of bias concerns (lack of blinding of the outcome assessors). cWe downgraded by one level to moderate certainty due to imprecision.
Background
Description of the condition
Placing a peripheral intravenous line is one of the most essential procedures in hospitals. It is necessary when administering fluids and drugs, and drawing blood. It is usually performed using the landmark method, comprising visualisation and palpation of the veins (Moureau 2019; Sadud 2019; Troianos 2012). Placing a peripheral intravenous line is occasionally difficult. The first attempt is unsuccessful in as many as 14% to 21% of adults in the emergency department (Carr 2016; Sebbane 2013), and in 9% to 26% of adults in the prehospital setting (Jones 1989; Lapostolle 2007; Minville 2006). About 10% of surgical patients or those in emergency departments require three or more attempts (Civetta 2019; Davis 2021; Fields 2012). This is mainly due to factors including obesity, chronic illness, intravenous drug use, dehydration, and shock (Mills 2007; Ortega 2008; Sebbane 2013). The failure rate at the first attempt is much higher in people with difficult intravenous access, reported as being between 34% and 93% (McCarthy 2016; Sebbane 2013; Van Loon 2016). Multiple punctures lead to discomfort, anxiety, delay in subsequent interventions, and return of test results (Davis 2021). If a peripheral intravenous line cannot be placed with the landmark method, a central venous line is often the next step in those with difficult intravenous access. However, central venous line placement is costly, time‐consuming, and exposes people to more pain and discomfort. In addition, central venous line placement can cause serious complications, such as infection, thrombosis, and pneumothorax, which are reported to occur in more than 15% of people (McGee 2003). Hence, the insertion of a central venous line should be considered as a last resort. Placing a peripheral intravenous line with ultrasound guidance may be an alternative for people with difficult intravenous cannulation.
Description of the intervention
Ullmann and Stoelting first reported the use of ultrasound for intravenous cannulation in 1978 (Ullman 1978). Since then, ultrasound guidance has been widely used for cannulation of central veins, and it has become the standard of care in recent years. Keyes and colleagues first reported ultrasound‐guided peripheral intravenous cannulation in 1999 (Keyes 1999). There are two techniques for ultrasound guidance: short‐axis (out‐of‐plane) and long‐axis (in‐plane). The short‐axis technique uses the short‐axis image of a targeted vein and has two methods: a static method and a dynamic method. In the static method, ultrasound is used to determine the location and the diameter of the vein and to evaluate important surrounding structures, such as arteries and nerves. Because cannulation is attempted without real‐time ultrasound guidance, the location of the targeted vein can be missed. In the dynamic method, the entire procedure is performed under real‐time ultrasound guidance, enabling operators to visualise both the vein and the important surrounding structures. However, there is a risk of puncturing the posterior wall because it is occasionally difficult to identify and visualise the needle tip throughout the procedure. The long‐axis technique uses a long‐axis image of the targeted vein and needle. Because it can visualise the entire length of the needle, the risk of puncturing the posterior wall is theoretically low. However, it is difficult for operators to maintain the needle and targeted vein within the narrow width of the ultrasound beam, and they cannot visualise important surrounding structures. Two randomised controlled trials (RCTs) compared short‐ and long‐axis techniques, and in neither trial was there a significant overall difference in success between the two techniques (Mahler 2011; Privitera 2021).
Although evidence about the longevity of functional catheters placed with ultrasound guidance versus the landmark methods is mixed, the target vein's depth and the appropriate needle length are probably important factors. Using 4.8 cm or 6.35 cm catheters, 53% to 75% of catheters placed under ultrasound guidance were still functional at 24 hours, compared with 74% to 99% of catheters placed by the landmark method. (Dargin 2010; Dillon 2008). However, another study showed a similar proportion of functional catheters for ultrasound guidance and the landmark method at 72 hours: 73% and 78%, respectively (Shokoohi 2019). Of note, long needles were used more often in the ultrasound guidance group than in the landmark method group (40% versus 1%) (Shokoohi 2019). Furthermore, using a 4.8 cm catheter, the proportion of functional catheters placed with ultrasound guidance at 48 hours was 100% for veins at less than 0.4 cm depth, 62% for veins that were at 0.41 cm to 1.19 cm depth, and 29% for veins at 1.2 cm depth or greater (Fields 2012). Therefore, ultrasound guidance requires a longer needle appropriate for the vein's depth because ultrasound guidance targets deeper veins than the landmark method.
The length of the catheter in the vein is also important for the longevity of functional catheters. At 72 hours, 100% of intravenous lines failed if the length of the catheter in the vein was less than 30% of the total catheter length, 32% failed if it was between 30% and 64%, and none failed if it was greater than 65% (Pandurangadu 2018). It is occasionally difficult to visualise the needle tip or needle when the subcutaneous tissue between the skin surface and the target vein is thin. The ideal depth of the target vein could be at least 0.5 cm, using a 4.57 cm catheter (Avila 2019). Therefore, when using a usual intravenous catheter of up to about 5 cm, it may be desirable to select a vein with a depth of approximately 0.5 cm to 1 cm and place a catheter roughly half the length into the vein. Longer catheters (approximately 6 cm to 20 cm), such as midline catheters, may be a better option, especially for veins that are at a subcutaneous depth of approximately 1 cm or more because long catheters survive longer and have a similar success of cannulation compared to usual catheters (Bahl 2019; Bahl 2020; Elia 2012). However, the Seldinger technique is used for midline catheters, which are more costly (Adams 2016; Seldinger 1953). The usefulness of longer catheters is beyond the scope of this review. The Michigan Appropriateness Guide for Intravenous Catheters offers a method for selecting catheters (Chopra 2015).
How the intervention might work
If the targeted peripheral vein is visible or palpable, cannulation is usually straightforward with the landmark method and will be successful at the first attempt in over 95% of cases (McCarthy 2016). However, the location and diameter of peripheral veins differ substantially between people. It is often difficult to cannulate deep peripheral veins that are not visible and palpable from the skin surface. Ultrasound can help the operator to: visualise the local anatomy of interest; identify the size and direction of veins and important surrounding structures, such as arteries and nerves; and clarify the diameter and route of these important structures. Furthermore, in the dynamic method, where the needle is visualised with ultrasound, the operator can see the spatial relationships between the vein, surrounding structures, and the needle. Thus, ultrasound guidance may facilitate successful cannulation and prevent complications, especially in people with difficult intravenous access who would otherwise be candidates for central venous line placement. Shokoohi and colleagues reported data from a cohort study, where the number of central venous lines placed decreased by 80% during the six years after the introduction of ultrasound‐guided peripheral intravenous cannulation (Shokoohi 2013).
Why it is important to do this review
The efficacy of ultrasound guidance for central venous cannulation has been established (Brass 2015a; Brass 2015b; Wu 2013). The National Institute for Health and Care Excellence and the American Society of Anesthesiologists recommend using ultrasound guidance for central venous cannulation (ASA Task Force 2012; NICE 2002), and it is currently the standard of care. However, the efficacy of ultrasound guidance for peripheral intravenous cannulation has not been well established. Several meta‐analyses have been conducted (Egan 2013; Heinrichs 2013; Liu 2014; Stolz 2015; Van Loon 2018; Tran 2021), and the results have shown a fairly consistent increase in the overall success with ultrasound guidance in people with difficult intravenous cannulation. However, there are several weaknesses in the synthesised evidence on this topic to date. Most of the included studies had fewer than 60 participants and larger studies (1189 participants) have since been published (McCarthy 2016). Older studies did not always use appropriate methodology and seldom evaluated the first‐pass success (successful cannulation at first attempt), reporting the overall success instead. Even if the overall success improves, it may not be beneficial if it subjects individuals to more skin punctures. Furthermore, because peripheral intravenous cannulation with the landmark method is usually straightforward for people with easy intravenous access, the efficacy of ultrasound guidance for peripheral intravenous cannulation varies according to the difficulty of intravenous access. However, previous studies were unclear in their definition of the difficulty or did not take into account the impact of the difficulty. This methodologically rigorous meta‐analysis assesses the influence of intravenous access difficulty, reports the current evidence for patient‐relevant outcomes, and hopes to aid decision‐making for placing peripheral intravenous cannulation.
Objectives
To evaluate the effectiveness and safety of ultrasound guidance compared to the landmark method for peripheral intravenous cannulation in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), including cluster‐randomised controlled trials, cross‐over trials, and quasi‐RCTs (RCTs in which participants are allocated based on data such as date of birth, date of recruitment, or medical record number).
Types of participants
We included all adult participants (≥ 18 years old) with any clinical characteristics, in any setting, who required a peripheral intravenous line, irrespective of the difficulty of cannulation. We defined a peripheral intravenous line as a catheter placed in a peripheral vein. We excluded central lines, intraosseous lines, and peripherally inserted central lines. We excluded children because the effect of ultrasound guidance would be different for them, due to smaller veins and extremities, and a possible lack of cooperation.
Placing a peripheral intravenous line in individuals can be classed as ‘difficult’, ‘moderate’, or ‘easy’. We use the terms ‘difficult participants’, ‘moderate/moderately difficult participants’ and ‘easy participants’ as shorthand to characterise the difficulty level in placing a peripheral line using the landmark method. We used the original studies’ definitions of difficulty levels of peripheral intravenous cannulation with the landmark method. We analysed the results in these subgroups: ‘all participants’, ‘difficult participants’, ‘moderate participants’, and ‘easy participants'. We did this because we expected the effect of ultrasound‐guided peripheral venous cannulation to be the largest in participants classed as 'difficult' and smaller in participants classed as 'moderate' and 'easy' (see Subgroup analysis and investigation of heterogeneity).
Types of interventions
We included studies comparing ultrasound‐guided peripheral intravenous cannulation with the landmark method, irrespective of the profession of the operators, number of operators (one‐ or two‐person method), methods (short‐axis or long‐axis, static or dynamic), or the sites of the peripheral veins, and all studies using ultrasonography, irrespective of the manufacturer or generation of the ultrasound machine. We excluded studies on peripherally inserted central catheters.
Types of outcome measures
We did not use outcome measures as a criterion for excluding studies. All outcome measures below would be reported at the time of cannulation.
Primary outcomes
First‐pass success of cannulation
Overall success of cannulation
Pain
We defined the overall success of cannulation as the success of cannulation irrespective of the number of attempts and procedure time. We defined successful cannulation as stated by the study authors. A cutaneous puncture was counted as one attempt, irrespective of the duration of subcutaneous exploration. We anticipated that studies would use different pain intensity scales, with most studies using standard subjective scales, such as a numerical rating scale (NRS) or a visual analogue scale (VAS).
Secondary outcomes
Procedure time for first‐pass cannulation
Procedure time for overall cannulation
Number of cannulation attempts
Patient satisfaction
Overall complications (including arterial puncture, haematoma, and nerve injury)
Studies could report patient satisfaction results as either continuous or dichotomous data. Scales of patient satisfaction included Likert scales and validated instruments, such as the Client Satisfaction Questionnaire‐18 (Attkisson 1982).
Search methods for identification of studies
Electronic searches
The Cochrane Vascular Information Specialist conducted systematic searches of the following databases for RCTs and controlled clinical trials without language, publication year, or publication status restrictions:
the Cochrane Vascular Specialised Register via the Cochrane Register of Studies (CRS‐Web);
the Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Register of Studies Online (CRSO);
MEDLINE (Ovid MEDLINE Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE);
Embase Ovid;
CINAHL (Cumulative Index to Nursing and Allied Health Literature) EBSCO;
LILACS (Latin American and Caribbean Health Science Information) Bireme.
We developed search strategies for other databases from the search strategy designed for MEDLINE. Where appropriate, they were combined with adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials (as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 4, Lefebvre 2021). Search strategies for major databases are provided in Appendix 1.
We searched the following trials registries:
the World Health Organization International Clinical Trials Registry Platform (who.int/trialsearch);
ClinicalTrials.gov (clinicaltrials.gov).
The most recent searches were carried out on 29 November 2021.
Searching other resources
Four review authors (MT, TM, CT, NY) checked the reference lists of all identified studies and review articles to find additional studies. We contacted trial authors, experts in this field, and manufacturers of ultrasound machines to identify unpublished studies.
Data collection and analysis
Selection of studies
We used the reference management software Mendeley to collate the results of searches and to remove duplicates (Mendeley). We used Rayyan software to screen the results of the search (Ouzzani 2016). Four review authors (MT, TM, CT, NY) independently and in duplicate checked titles and abstracts of the results of the search and identified potentially relevant studies. We obtained full texts of all potentially relevant studies if any of the authors judged them to be relevant or potentially relevant. We excluded only the clearly irrelevant articles at this stage. Four review authors (MT, TM, CT, NY) independently and in duplicate assessed the full papers for eligibility using a pre‐designed checklist. We compared the results and resolved disagreements through discussion. If we were unable to reach a consensus, we consulted the sixth review author (NW). We recorded the number of papers retrieved at each stage and reported this information using a PRISMA flowchart.
Data extraction and management
We used a Microsoft Excel data extraction sheet that we designed specifically for this study (Microsoft Excel 2020). Four review authors (MT, TM, CT, NY) independently and in duplicate extracted the data using the extraction form. We resolved disagreements through discussions. If we could not reach a consensus, we consulted the sixth review author (NW). If additional information was necessary, one review author (MT) contacted the corresponding author of the relevant studies. When we completed data extraction, one review author (MT) entered the data into Review Manager software and another review author (NY) checked the data (RevMan Web 2020).
Assessment of risk of bias in included studies
Four review authors (MT, TM, CT, NY) independently assessed the methodological quality of each included study using the Cochrane risk of bias 1 tool (Higgins 2011). We evaluated the following domains and rated them as at low, unclear, or high risk of bias:
random sequence generation (selection bias);
allocation concealment (selection bias);
blinding (performance bias and detection bias);
incomplete outcome data (attrition bias);
selective outcome reporting (outcome reporting bias);
other potential sources of bias;
overall risk.
Due to the nature of the intervention, blinding the operators was not possible. This might have caused some performance bias, but it was unavoidable and not expected to be serious. It was also not possible to blind the participants, but this should not have affected objective outcomes, such as the success of cannulation. For this reason, we assessed performance and detection bias as one domain and assessed blinding separately for each outcome. We evaluated objective outcomes as low risk when a third person assessed the outcome. For subjective outcomes, such as pain and satisfaction, we evaluated them as high risk regardless of the outcome assessor. We also assessed incomplete outcome data and overall risk separately for each outcome.
We defined the overall risk of bias for each outcome as follows:
low risk of bias: all domains rated as low risk;
moderate risk of bias: one or more domains rated as being at unclear risk;
high risk of bias: one or more domains rated as being at high risk.
We reviewed the assessments and resolved any disagreements through discussion. If needed, we consulted the sixth review author (NW).
Measures of treatment effect
We calculated dichotomous data as risk ratios (RR) with 95% confidence intervals (CIs). We calculated continuous data as mean differences (MDs) with 95% CIs when the outcomes of all studies used the same scale. We used a standardised mean difference (SMD) with 95% CIs if different scales were used.
Unit of analysis issues
The unit of analysis was the individual participant. If we included any cluster‐randomised trials, we planned to adjust the sample size by the trial's intracluster correlation coefficient, using the method described in the Cochrane Handbook for Systematic Reviews of Intervention (Higgins 2021a). We excluded any cluster‐randomised trials which did not report the intracluster correlation coefficient.
Dealing with missing data
We contacted the study authors when possible to obtain missing data. We performed an intention‐to‐treat analysis when possible. We planned to impute data for binary outcomes using various scenarios, such as "best‐case" and "worst‐case" scenarios. For continuous outcomes, we used available case analysis. We calculated the standard deviation from P values, standard errors, or CIs according to the instructions given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021a). Otherwise, we imputed them from other studies in the meta‐analysis according to the validated method (Furukawa 2006).
Assessment of heterogeneity
We assessed heterogeneity by inspecting forest plots visually and examined statistical heterogeneity by Chi2 and I2 statistics. We used P = 0.10 as the predefined significance level of heterogeneity for the Chi2 test. We considered I2 statistics of 25% or lower to indicate low heterogeneity, between 25% and 50% to indicate moderate heterogeneity, and 50% or more to indicate substantial heterogeneity. However, we interpreted this value in light of the size and direction of effect and the strength of the evidence for heterogeneity, based on the P value from the Chi2 test (Higgins 2021a). If we identified substantial heterogeneity, we investigated and reported potential reasons for this.
Assessment of reporting biases
We tried to minimise the effect of publication bias by performing well‐designed, comprehensive literature searches, by using trial registries, such as ClinicalTrials.gov, and by contacting the manufacturers of ultrasound machines. If we included a sufficient number of studies in a meta‐analysis (that is, more than 10 studies; Higgins 2021a), we visually inspected funnel plots to evaluate small study effects and used contour‐enhanced funnel plots to evaluate publication bias. We evaluated reporting bias by checking the protocol of the study if we could identify one from trial registries.
Data synthesis
We reviewed the data from the included studies and, if possible, synthesised and analysed data using Review Manager software (RevMan Web 2020). We used the random‐effects model to pool data because we expected the definitions of participants and operators to vary to some extent amongst studies, and also because the random‐effects model is more conservative than the fixed‐effect model. If it was not possible to pool data, we provided clear reasons for this and reported results narratively.
Subgroup analysis and investigation of heterogeneity
We performed subgroup analyses of the following parameters for the primary outcomes if we found sufficient data from the included studies. For conditions other than the definition of the difficulty of intravenous access with the landmark method, we performed subgroup analyses using the original studies' definitions of the difficulty.
The difficulty of obtaining intravenous access: 'difficult' versus 'moderately difficult' versus 'easy'
Because the effect of ultrasound guidance varied depending on the difficulty of obtaining intravenous access in each participant, we evaluated participants separately for each difficulty level, according to the following criteria:
we used the definition of the difficulty of peripheral intravenous cannulation adopted by original studies;
we defined the difficulty based on the first‐pass success or the overall success of cannulation using the landmark method.
Because we expected the definition of the difficulty of peripheral intravenous cannulation to differ between studies (Egan 2013; Liu 2014), we also defined the difficulty based on the first‐pass success and, where the first‐pass success was not assessed, on the overall success of cannulation using the landmark method. As in previous studies, we classified success rates of lower than 60%, 60% to 80%, and higher than 80% as "difficult", "moderately difficult", and "easy", respectively (McCarthy 2016; Sebbane 2013; Van Loon 2016). For example, Aponte 2007 moves from 'difficult' venous access participants, based on the original study's definition, to 'easy' participants, based on the definition of the success rate with the landmark method. We performed a post hoc meta‐regression analysis to assess the effect of the difficulty level on the primary outcomes if the test for subgroup difference was significant, and there were three or more subgroups and 10 or more studies in total. We performed the following post hoc subgroup analyses on difficult participants only, except for the type of ultrasound guidance, due to the small number of studies for moderately difficult and easy participants. We used the original studies' definitions of the difficulty for the subgroup analyses. We performed the meta‐regression analyses with R (version 4.0.3) (R 2020).
Practical difficulties of obtaining intravenous access
We analysed participants separately where they satisfied the definition of a difficult case. A difficult case was defined as any of the following:
the operator could not see and palpate the targeted vein;
the operator identified a participant as a difficult case;
the participant had a history of difficult intravenous access;
the participant had multiple failed attempts.
Operators' skill and study setting
We analysed separately according to the following criteria:
finished any kind of training programme for ultrasound‐guided peripheral intravenous cannulation;
had any clinical experience with ultrasound‐guided peripheral intravenous cannulation;
finished any kind of training programme for ultrasound‐guided peripheral intravenous cannulation and had any clinical experience with ultrasound‐guided peripheral intravenous cannulation;
types of operators;
study settings: emergency departments or intensive care units (ICUs) versus operating rooms.
Compared to participants in operating rooms, those in emergency departments or ICUs would be more likely to be in shock or dehydrated. Since these factors are associated with difficult intravenous cannulation, ultrasound guidance might be more effective in the setting of emergency departments or ICUs than in operating rooms.
Date of publication: 1999 to 2008 versus 2009 to 2019
Advances in machine technology have led to improved ultrasound image quality, improving the effectiveness of ultrasound guidance. Therefore, we stratified the studies by publication year into two groups: 1999 to 2008, and 2009 to 2019. If we included more than 10 studies, we also performed univariate meta‐regression with R software, using publication year as a continuous covariate (R 2020).
Types of ultrasound guidance
We planned to analyse studies separately according to the type of ultrasound guidance:
short‐axis technique versus long‐axis technique;
dynamic method versus static method.
Sensitivity analysis
We performed sensitivity analyses for the following factors, using the original studies' definitions of the difficulty, if applicable.
We limited the analysis to studies with a low overall risk of bias. We defined the low overall risk of bias as satisfying all the following domains: adequate allocation concealment, blinding of outcome assessment, and data analysis performed according to the intention‐to‐treat principle.
We limited the analysis to RCTs only.
Summary of findings and assessment of the certainty of the evidence
We summarised the main findings of each relevant outcome, recording the magnitude of effect, total number of participants, and the number of relevant studies. We assessed the certainty of the evidence using the GRADE approach (GRADE 2004). We used the GRADEpro software to assist in the preparation of the summary of findings tables (GRADEpro GDT). We created one table each for each class of difficulty using the original studies' definitions of the difficulty. See Table 1; Table 2; Table 3. We included the following outcomes:
first‐pass success of cannulation;
overall success of cannulation;
pain;
procedure time for first‐pass cannulation;
number of attempts before successful cannulation;
patient satisfaction;
overall complications (arterial punctures, haematoma formations, and nerve injuries).
We presented the results of the subgroup analyses in additional summary of findings tables where sufficient data were available. We considered the following subgroup analyses to be sufficiently clinically relevant to present as additional summary of findings tables:
Operators had any clinical experience with ultrasound‐guided peripheral intravenous cannulation (see Appendix 2);
Setting (see Appendix 3).
Results
Description of studies
Results of the search
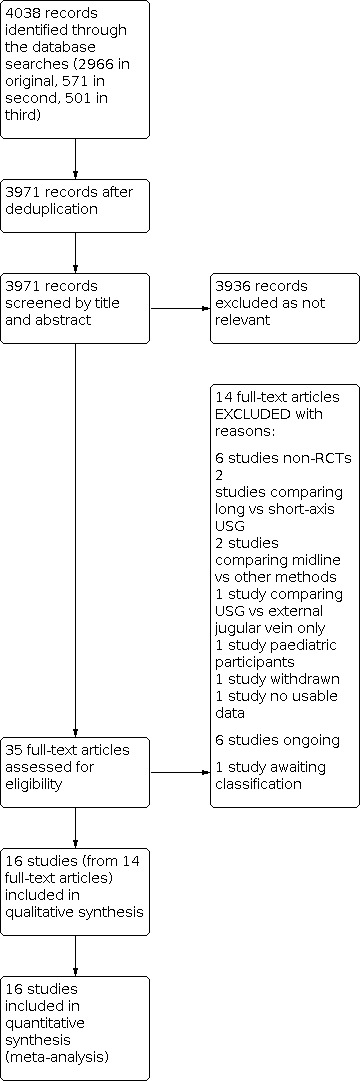
The first search in October 2019 identified 2966 articles; the second update search in November 2020 identified 571 articles; the third update search in November 2021 identified a further 501 articles. We removed 67 duplicate articles and screened the remaining 3971 articles. We removed 3936 articles after title and abstract screening, and assessed the remaining 35 articles in full text. We included 16 studies (from 14 full‐text articles) in the quantitative analysis and excluded 14 articles at full‐text review. We identified six ongoing studies and listed one study as 'awaiting classification'. The inter‐rater agreement for the full‐text screening stage was substantial (ĸ = 0.82). See Figure 1 for the flow diagram and exclusion reasons.
1.
Study flow diagram
Included studies
See Characteristics of included studies.
We identified 14 articles (2267 participants) that compared the efficacy of ultrasound guidance and the landmark method for peripheral intravenous cannulation (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; Glasin 2020; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016; Nishizawa 2020; Pappas 2006; River 2009; Skulec 2019; Stein 2009; Weiner 2013). McCarthy 2016 randomised participants separately according to the difficulty of the landmark method (easy, moderate, and difficult). Because it is only possible to analyse two comparisons from any study in Review Manager at one time, we split the study according to the difficulty level and added the details for each level as a separate study, indicated by the study ID 'McCarthy 2016' plus A, B, or C (McCarthy 2016A; McCarthy 2016B; McCarthy 2016C). Therefore, in effect, we included 16 studies. Kerforne 2012 and River 2009 were conference reports, and Pappas 2006 was a report from the United States Air Force. Glasin 2020 has not been published yet, but the data were available owing to the courtesy of the study author. All other studies were published in peer‐reviewed journals. Amongst the 16 studies, 14 were RCTs, and two were quasi‐RCTs (Costantino 2005; İsmailoğlu 2015). Costantino 2005 allocated participants according to the day of presentation to the emergency department (odd day: ultrasound guidance, even day: landmark method), and İsmailoğlu 2015 allocated participants to each group alternately, in the order in which they were seen. Ten studies were conducted in the emergency department (Bahl 2016; Costantino 2005; Glasin 2020; İsmailoğlu 2015; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; River 2009; Stein 2009; Weiner 2013), three in the ICU (Bridey 2018; Kerforne 2012; Nishizawa 2020), two in the operating room (Aponte 2007; Pappas 2006), and one in the prehospital setting (Skulec 2019).
Most studies targeted participants with difficult intravenous cannulation with the landmark method (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; Nishizawa 2020; Pappas 2006; River 2009; Stein 2009; Weiner 2013). The studies varied in how they defined 'difficulty', but all definitions were clinically valid. Three studies defined it as failing at least two or three times with the landmark method (Pappas 2006; River 2009; Stein 2009); three studies as no apparent or palpable veins (Bridey 2018; Kerforne 2012; McCarthy 2016A); and one study as a history of difficult intravenous cannulation (Bahl 2016). Aponte 2007 defined 'difficulty' as either a history of difficult intravenous cannulation or an operator's decision that a participant was difficult. Costantino 2005 defined it as a history of difficult cannulation and failing at least three times. İsmailoğlu 2015 defined it as a history or suspicion of difficult cannulation, and no apparent or palpable veins. Nishizawa 2020 defined it as either failing two times with the landmark method or an operator's decision based on the absence of palpable veins or a history of difficult intravenous cannulation. Weiner 2013 defined it as either failing two times with the landmark method or having a history of difficult intravenous cannulation.
One study defined 'moderately difficult' participants as those in whom the operators could visualise or palpate at least one vein but were expected to have difficulty with the landmark method (McCarthy 2016B). One study defined 'easy' participants as those in whom the operator could see or palpate at least one vein and thought intravenous access would be easy with the landmark method (McCarthy 2016C). Two studies did not limit by the landmark method difficulty (Glasin 2020; Skulec 2019). Glasin 2020 recruited participants with obesity (body mass index > 25 kg/m2), and Skulec 2019 included all participants irrespective of the difficulty.
We expected that the varying definitions of 'difficulty' would cause heterogeneity. Therefore, we also redefined the difficulty by the first‐pass success or the overall success of cannulation with the landmark method as planned in the protocol, with a success rate of lower than 60% defined as difficult, 60% to 80% as moderate, and higher than 80% as easy. As a result, nine studies were classified as difficult (Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; Nishizawa 2020; Stein 2009; Weiner 2013), four were classified as moderate (Glasin 2020; McCarthy 2016B; River 2009; Skulec 2019), and two were classified as easy (Aponte 2007; McCarthy 2016C). Pappas 2006 was unclassifiable because there were no success rate results.
Twelve studies employed dynamic ultrasound guidance (Aponte 2007; Costantino 2005; Glasin 2020; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Nishizawa 2020; Pappas 2006; Stein 2009; Weiner 2013), and one study had three arms comparing dynamic ultrasound guidance, static ultrasound guidance, and the landmark method (Skulec 2019). Three studies did not specify if they employed dynamic or static guidance (Bahl 2016; Bridey 2018; River 2009). Amongst the 13 studies employing dynamic guidance, five studies used short‐axis ultrasound guidance (Costantino 2005; Glasin 2020; Nishizawa 2020; Skulec 2019; Weiner 2013), and eight studies did not specify if they used short‐ or long‐axis ultrasound guidance (Aponte 2007; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Pappas 2006; Stein 2009). No study used only long‐axis ultrasound guidance. A variety of ultrasound machines were used, with the oldest being Site‐Rite 3 (Aponte 2007; Pappas 2006), and the newest being x‐Porte (Glasin 2020). Five studies used M‐turbo (Bahl 2016; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Weiner 2013); this machine was the most commonly used amongst the included studies.
In 10 studies, the operators were nurses (Aponte 2007; Bahl 2016; Bridey 2018; Glasin 2020; İsmailoğlu 2015; Kerforne 2012; Nishizawa 2020; Pappas 2006; River 2009; Weiner 2013); in two studies, the operators were physicians (Costantino 2005; Stein 2009); in three studies, the operators were technicians (McCarthy 2016A; McCarthy 2016B; McCarthy 2016C); and in one study, they were paramedics and physicians (Skulec 2019). The number of operators ranged from two to 33 (median 20). Five studies did not report the number of operators (Bridey 2018; İsmailoğlu 2015; Kerforne 2012; River 2009; Weiner 2013). The operators performed both ultrasound guidance and the landmark method in most studies, but Glasin 2020 had 17 operators, and only one operator performed ultrasound guidance. The operators had clinical experience (any) with ultrasound guidance before the trials in 10 studies (Aponte 2007; Bridey 2018; Costantino 2005; Glasin 2020; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Pappas 2006; River 2009; Stein 2009), but not in three studies (Bahl 2016; Nishizawa 2020; Weiner 2013). In Skulec 2019, physicians had clinical experience (any), but paramedics did not. In 14 studies, the operators had finished a training programme for ultrasound guidance (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; Glasin 2020; İsmailoğlu 2015; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Nishizawa 2020; River 2009; Skulec 2019; Stein 2009; Weiner 2013); the training consisted mainly of lectures and hands‐on practice. Kerforne 2012 and Pappas 2006 did not specify whether they provided a training programme. Seven studies reported the number of ultrasound guidance cases or experiences before the studies started, ranging from three cases in Nishizawa 2020 to more than 200 cases in Skulec 2019 (median five). Three studies reported on the frequency of ultrasound guidance during the study period, with 39% of operators performing five or more ultrasound‐guided procedures per day (McCarthy 2016A; McCarthy 2016B; McCarthy 2016C).
All studies used usual intravenous catheters. McCarthy 2016A, McCarthy 2016B, McCarthy 2016C, Nishizawa 2020, and Skulec 2019 used both short (approximately 30 mm) and long needles (approximately 45 mm), while Bridey 2018 and Costantino 2005 used only short needles. The other studies did not specify the length of the needles used.
Excluded studies
We excluded 14 studies for the following reasons: six were not randomised controlled trials (Bauman 2009; DRKS00013797; Evans 2013; Galen 2018; NCT01602133; Raio 2018); two compared long‐ and short‐axis ultrasound guidance (Hill 2017; NCT04234347); two compared midline and other methods (NCT03440944; NCT03457259); one compared ultrasound guidance with external jugular vein only (Costantino 2010); one study was in children (Curtis 2015); one study was withdrawn (NCT02360163); and one study had no usable data (Troisi 2013). See Characteristics of excluded studies.
Ongoing studies
We identified six ongoing studies (NCT03745209; NCT03841864; NCT04218643; NCT04853290; NCT04856826; NCT05119985). See Characteristics of ongoing studies.
Studies awaiting classification
One study is awaiting classification (IRCT201408097751N4). It was registered in 2015, but its status is unknown. See Characteristics of studies awaiting classification.
Risk of bias in included studies
To assess risk of bias, we considered each outcome separately for blinding (performance and detection bias), incomplete outcome data, and for overall bias. See Figure 2 and Figure 3. Of the high‐risk assessments across the 16 studies, 78% were from the blinding domain, 15% were from the incomplete outcome data domain, and 7% were from the random sequence and allocation domain.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
We assessed most of the studies (10/16) to be at low risk of selection bias (Bahl 2016; Bridey 2018; Glasin 2020; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Nishizawa 2020; Skulec 2019; Stein 2009; Weiner 2013). One study allocated participants according to whether the emergency department visit was on an even or odd date (Costantino 2005). Another study allocated participants alternately to ultrasound guidance or the landmark method in the order in which they were seen (İsmailoğlu 2015). Therefore, we evaluated both random sequence generation and allocation concealment as high risk for both these studies. Four studies did not report the details on randomisation methods or allocation concealment, so we judged these to have an unclear risk of selection bias (Aponte 2007; Kerforne 2012; Pappas 2006; River 2009).
Blinding
Due to the nature of the intervention, it was impossible to blind participants and operators, so the main source of bias was performance and detection bias. We assessed each outcome for bias. Amongst the blinding domain risk assessments, 39% were low risk, and 61% were high risk. In six studies, a third person acted as the outcome assessor for all outcomes; we evaluated these as low risk for objective outcomes (successful cannulation, procedure time, number of attempts, and complications), and as high risk for subjective outcomes (pain and satisfaction) (Bahl 2016; Glasin 2020; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Stein 2009). In four studies, the outcome assessors were operators themselves for all outcomes (Aponte 2007; Bridey 2018; Costantino 2005; Pappas 2006), and investigators in three studies (İsmailoğlu 2015; Nishizawa 2020; Weiner 2013). Therefore, we evaluated these as high risk for all outcomes. One study did not report who assessed the outcomes, and we evaluated it as high risk for all outcomes (River 2009). In Kerforne 2012, the operators assessed successful cannulation (we evaluated as high risk), but a third person assessed procedure time (we evaluated as low risk) (Kerforne 2012). In Skulec 2019, operators assessed the overall success of cannulation and complications (we evaluated as high risk), but a third person assessed the other outcomes (we evaluated as low risk).
Incomplete outcome data
Eighty‐seven per cent of the risk of bias assessments in this domain were low risk, and 13% were high risk. All studies that reported on first‐pass success and overall success of cannulation were at low risk for attrition bias. One study reported results only for participants with successful cannulation in all its outcomes, and we evaluated all the outcomes of this study as high risk (Pappas 2006). The procedure time for first‐pass cannulation in Aponte 2007 and Skulec 2019, and the procedure time for overall cannulation in Kerforne 2012, Pappas 2006, and Stein 2009 were reported only for participants with successful cannulation, and so we evaluated these as high risk. River 2009 did not specify whether the procedure time was reported for all participants or not, so we considered it at unclear risk. Bridey 2018 had 10 dropouts amongst 114 total participants (five in the ultrasound guidance group and five in the landmark method group; i.e. an 8.8% dropout rate), and Stein 2009 had seven dropouts amongst 59 participants (four in the ultrasound guidance group and three in the landmark method group; i.e. a 12% dropout rate) from the assessment of patient satisfaction. Although the numbers of dropouts were balanced between the two arms, the total numbers were substantial, and we considered these studies at high risk of attrition bias.
Selective reporting
Seven studies did not publish their protocols or register the studies (Aponte 2007; Bahl 2016; Costantino 2005; İsmailoğlu 2015; Kerforne 2012; Pappas 2006; River 2009). Thus, we could not exclude selective reporting and evaluated them as at unclear risk of bias. The remaining nine studies were at low risk of selective reporting (Bridey 2018; Glasin 2020; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Nishizawa 2020; Skulec 2019; Stein 2009; Weiner 2013).
Other potential sources of bias
There were no other potential sources of bias in any included study.
Overall bias
The percentage of studies with low overall risk was 43% (6/14) for first‐pass success of cannulation, 17% (2/12) for overall success of cannulation, zero (0/7) for pain, 67% (4/6) for procedure time for first‐pass cannulation, 20% (2/10) for procedure time for overall cannulation, 27% (3/11) for number of attempts, zero (0/6) for patient satisfaction, and 56% (5/9) for complications.
The percentage of studies with unclear overall risk was 7% (1/14) for first‐pass success of cannulation, 8% (1/12) for overall success of cannulation, zero (0/7) for pain, zero (0/6) for procedure time for first‐pass cannulation, 10% (1/10) for procedure time for overall cannulation, 9% (1/11) for number of attempts, zero (0/6) for patient satisfaction, and zero (0/9) for complications.
The percentage of studies with high overall risk was 50% (7/14) for first‐pass success of cannulation, 75% (9/12) for overall success of cannulation, 100% (7/7) for pain, 33% (2/6) for procedure time for first‐pass cannulation, 70% (7/10) for procedure time for overall cannulation, 64% (7/11) for number of attempts, 100% (6/6) for patient satisfaction, and 44% (4/9) for complications.
Effects of interventions
See: Table 1; Table 2; Table 3
We have reported the results of our meta‐analyses subgrouped by level of difficulty as we expected the effect of ultrasound‐guided peripheral venous cannulation to be largest in participants classed as ‘difficult’ and smaller in participants classed as ‘moderate’ and ‘easy’. We have presented results using the original studies' definition of difficulty and also when defined by success rate with the landmark method. We have presented the main findings by level of difficulty defined by the original studies in Table 1, Table 2, and Table 3. We have presented the main findings by level of difficulty defined by success rate with the landmark method in additional Summary of findings tables in Appendix 4, Appendix 5, and Appendix 6.
Primary outcomes
First‐pass success of cannulation
All participants
Fourteen studies (2202 participants) evaluated first‐pass success of cannulation (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; Glasin 2020; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Nishizawa 2020; Skulec 2019; Stein 2009; Weiner 2013). Ultrasound guidance increased the first‐pass success of cannulation by 31% (RR 1.31, 95% CI 1.08 to 1.59; I2 = 90%; low‐certainty evidence; Analysis 1.1). The heterogeneity was considerable and the test for subgroup difference indicated a difference (P < 0.001). The effect sizes of ultrasound guidance varied: the effect size was the largest in difficult participants and became smaller with decreasing difficulty according to the original studies' definitions. Meta‐regression analysis for the effect of the difficulty level indicated a difference (P = 0.009). This difficulty‐dependent trend of the effect sizes was similar when we defined the studies’ difficulty by their success rate with the landmark method. Both the test for subgroup difference and the meta‐regression analysis for the effect of the difficulty level also indicated a difference using the definition of success rate with the landmark method (P < 0.001) (Analysis 1.2).
1.1. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 1: Difficulty levels defined by original studies
1.2. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 2: Difficulty levels defined by the success rate with landmark method
Difficult participants
Ultrasound guidance improved the first‐pass success of cannulation in difficult participants. According to the original studies' definitions, we classified ten studies (815 participants) as having difficult participants (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; Nishizawa 2020; Stein 2009; Weiner 2013). Ultrasound guidance increased the first‐pass success of cannulation by 50% (RR 1.50, 95% CI 1.15 to 1.95; I2 = 62%; low‐certainty evidence; Analysis 1.1). When we categorised studies based on their success rate with the landmark method, we classified nine studies (780 participants) as having difficult participants (Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; Nishizawa 2020; Stein 2009; Weiner 2013). With this definition, ultrasound guidance increased the first‐pass success of cannulation by 62%, and the heterogeneity was lower than that defined by the original studies' definitions (RR 1.62, 95% CI 1.28 to 2.06; I2 = 43%; moderate‐certainty evidence; Analysis 1.2).
Moderate participants
Ultrasound guidance improved the first‐pass success of cannulation in moderately difficult participants, but to a lesser extent than that in the difficult participants. According to the original studies' definitions, we classified one study (401 participants) as having moderately difficult participants (McCarthy 2016B). Ultrasound guidance increased the first‐pass success of cannulation by 14% (RR 1.14, 95% CI 1.02 to 1.27; moderate‐certainty evidence; Analysis 1.1). When we categorised studies based on their success rate with the landmark method, we classified three studies (791 participants) as having moderately difficult participants (Glasin 2020; McCarthy 2016B; Skulec 2019), and ultrasound guidance increased the first‐pass success of cannulation by 17% (RR 1.17, 95% CI 1.09 to 1.26; I2 = 0%; high‐certainty evidence; Analysis 1.2).
Easy participants
Ultrasound guidance was less effective than the landmark method in easy participants. According to the original studies' definitions, we classified one study (596 participants) as having easy participants (McCarthy 2016C). Ultrasound guidance decreased the first‐pass success of cannulation by 11% (RR 0.89, 95% CI 0.85 to 0.94; high‐certainty evidence; Analysis 1.1). When we categorised studies based on their success rate with the landmark method, we classified two studies (631 participants) as having easy participants (Aponte 2007; McCarthy 2016C), and ultrasound guidance decreased the first‐pass success of cannulation by 11% (RR 0.89, 95% CI 0.85 to 0.94; I2 = 0%; moderate‐certainty evidence; Analysis 1.2).
No restriction by intravenous access difficulty level
According to the original studies' definitions, there were no restrictions in terms of difficulty levels in two studies (390 participants) (Glasin 2020; Skulec 2019). Ultrasound guidance increased the first‐pass success of cannulation by 20% (RR 1.20, 95% CI 1.09 to 1.33; I2 = 0%; moderate‐certainty evidence; Analysis 1.1).
Overall success of cannulation
All participants
Twelve studies (1059 participants) evaluated overall success of cannulation (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; Glasin 2020; İsmailoğlu 2015; Kerforne 2012; Nishizawa 2020; River 2009; Skulec 2019; Stein 2009; Weiner 2013). Ultrasound guidance increased the overall success of cannulation by 27% (RR 1.27, 95% CI 1.08 to 1.49; I2 = 92%; very low‐certainty evidence; Analysis 2.1). The majority of studies focused on difficult participants, there were no studies with moderate and easy participants, and two studies were classified as having no restrictions of difficulty with the original studies' definition. Heterogeneity was considerable and the test for subgroup difference indicated a difference (P = 0.04). The effect size of ultrasound guidance was larger in studies with difficult participants than in studies without restrictions of difficulty. When we categorised studies based on their success rate with the landmark method, we classified eight studies as having difficult participants and three studies as moderate and one as easy. The test for subgroup difference indicated a difference (P = 0.04). The effect of ultrasound guidance visually showed the difficulty‐dependent trend, and the meta‐regression analysis for the effect of the difficulty level indicated a difference (P = 0.032) (Analysis 2.2).
2.1. Analysis.

Comparison 2: Overall success of cannulation, Outcome 1: Difficulty levels defined by original studies
2.2. Analysis.

Comparison 2: Overall success of cannulation, Outcome 2: Difficulty levels defined by the success rate with landmark method
Difficult participants
Ultrasound guidance improved the overall success of cannulation in difficult participants. According to the original studies' definitions, we classified ten studies (670 participants) as having difficult participants (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Kerforne 2012; Nishizawa 2020; River 2009; Stein 2009; Weiner 2013). Ultrasound guidance increased the overall success of cannulation by 40% (RR 1.40, 95% CI 1.10 to 1.77; I2 = 88%; very low‐certainty evidence; Analysis 2.1). When we categorised studies based on their success rate with the landmark method, we classified eight studies (588 participants) as having difficult participants (Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Kerforne 2012; Nishizawa 2020; Stein 2009; Weiner 2013). Ultrasound guidance increased the overall success of cannulation by 53% (RR 1.53, 95% CI 1.12 to 2.08; I2 = 86%; very low‐certainty evidence; Analysis 2.2).
Moderate participants
According to the original studies' definitions, none of the studies included participants with moderate difficulty. When we categorised studies based on their success rate with the landmark method, we classified three studies (436 participants) as having moderately difficult participants (Glasin 2020; River 2009; Skulec 2019). We found no clear difference between the ultrasound guidance and landmark method groups in the overall success of cannulation (RR 1.07, 95% CI 0.94 to 1.23; I2 = 87%; very low‐certainty evidence; Analysis 2.2).
Easy participants
According to the original studies' definitions, none of the studies included easy participants. When we categorised studies based on their success rate with the landmark method, we classified one study (35 participants) as having easy participants (Aponte 2007). We found no evidence of a difference in overall success in cannulation (RR 1.00, 95% CI 0.90 to 1.11; low‐certainty evidence; Analysis 2.2).
No restriction by intravenous access difficulty level
According to the original studies' definitions, there were no restrictions in terms of difficulty levels in two studies (389 participants) (Glasin 2020; Skulec 2019). We found no clear difference in overall success in cannulation (RR 1.05, 95% CI 0.92 to 1.19; I2 = 91%; very low‐certainty evidence; Analysis 2.1). No studies remained in this subgroup when we categorised studies based on their success rate with the landmark method.
Pain
All participants
Seven studies (1410 participants) evaluated pain (Glasin 2020; İsmailoğlu 2015; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Pappas 2006; Weiner 2013). All studies used a numerical rating scale (NRS), with scores ranging from 0 to 10, with 0 indicating no pain and 10 indicating maximum pain. We found no clear difference (MD 0.05, 95% CI ‐0.42 to 0.51; I2 = 58%; very low‐certainty evidence; Analysis 3.1). The effect of ultrasound guidance visually showed the difficulty‐dependent trend with both definitions of the difficulty, but the tests for subgroup differences did not indicate a difference for both definitions of difficulty (P = 0.20 for the original studies' and P = 0.09 for the success rate definition) (Analysis 3.2).
3.1. Analysis.

Comparison 3: Pain, Outcome 1: Difficulty levels defined by original studies
3.2. Analysis.

Comparison 3: Pain, Outcome 2: Difficulty levels defined by the success rate with landmark method
Difficult participants
According to the original studies' definitions, we classified four studies (323 participants) as having difficult participants (Pappas 2006; McCarthy 2016A; Weiner 2013). We found no clear difference in pain (MD ‐0.20, 95% CI ‐1.13 to 0.72; I2 = 62%; very low‐certainty evidence; Analysis 3.1). When we categorised studies based on their success rate with the landmark method, we classified three studies (305 participants) as having difficult participants (İsmailoğlu 2015; McCarthy 2016A; Weiner 2013). We found no clear difference in pain (MD ‐0.49, 95% CI ‐1.48 to 0.49; I2 = 60%; very low‐certainty evidence; Analysis 3.2).
Moderate participants
According to the original studies' definitions, we classified one study (401 participants) as having moderately difficult participants (McCarthy 2016B), and we found no clear difference in pain (MD 0.10, 95% CI ‐0.47 to 0.67; low‐certainty evidence; Analysis 3.1). When we categorised studies based on their success rate with the landmark method, we classified two studies (491 participants) as having moderately difficult participants (Glasin 2020; McCarthy 2016B). We found no clear difference in pain (MD 0.03, 95% CI ‐0.43 to 0.48; I2 = 0%; low‐certainty evidence; Analysis 3.2).
Easy participants
According to the original studies' definitions, we classified one study (596 participants) as having easy participants (McCarthy 2016C), and ultrasound guidance increased pain (MD 0.60, 95% CI 0.17 to 1.03; moderate‐certainty evidence; Analysis 3.1). When we categorised studies based on their success rate with the landmark method, we found the same study and the same result (Analysis 3.2).
No restriction by intravenous access difficulty level
According to the original studies' definitions, there were no restrictions in terms of difficulty levels in one study (Glasin 2020). We found no clear difference in pain (MD ‐0.10, 95% CI ‐0.85 to 0.65; low‐certainty evidence; Analysis 3.1). No studies remained in this subgroup when we categorised studies based on their success rate with the landmark method.
Secondary outcomes
Procedure time for first‐pass cannulation
All participants
Six studies (1564 participants) evaluated procedure time for first‐pass cannulation (Aponte 2007; Glasin 2020; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Skulec 2019). Two studies reported the outcome only for participants in whom cannulation was successful (Aponte 2007; Skulec 2019). Ultrasound guidance increased the procedure time for first‐pass cannulation by 61.4 seconds (MD 61.4, 95% CI 10.4 to 112.5; I2 = 98%; low‐certainty evidence; Analysis 4.1). Although the difficulty‐dependent trend was visually unclear, the test for subgroup differences indicated a difference for both definitions of the difficulty due to two studies where ultrasound guidance did not have as much effect as that in other studies (P < 0.001 for the original studies' definition and P = 0.02 for the success rate definition) (Glasin 2020; Skulec 2019) (Analysis 4.2).
4.1. Analysis.

Comparison 4: Procedure time for first‐pass cannulation, Outcome 1: Difficulty levels defined by original studies
4.2. Analysis.

Comparison 4: Procedure time for first‐pass cannulation, Outcome 2: Difficulty levels defined by the success rate with the landmark method
Difficult participants
Ultrasound guidance increased the procedure time for first‐pass cannulation in difficult participants. According to the original studies' definitions, we classified two studies (219 participants) as having difficult participants (Aponte 2007; McCarthy 2016A). Ultrasound guidance increased the procedure time for first‐pass cannulation by 119.9 seconds (MD 119.9, 95% CI 88.6 to 151.1; I2 = 0%; low‐certainty evidence; Analysis 4.1). When we categorised studies based on their success rate with the landmark method, we classified one study as having difficult participants (192 participants) (McCarthy 2016A), and ultrasound guidance increased the procedure time for first‐pass cannulation by 120.6 seconds (MD 120.6, 95% CI 88.3 to 152.9; moderate‐certainty evidence; Analysis 4.2).
Moderate participants
Ultrasound guidance increased the procedure time for first‐pass cannulation in moderately difficult participants. According to the original studies' definitions, we classified one study (401 participants) as having moderately difficult participants (McCarthy 2016B). Ultrasound guidance increased the procedure time for first‐pass cannulation by 95.2 seconds (MD 95.2, 95% CI 72.8 to 117.6; high‐certainty evidence; Analysis 4.1). When we categorised studies based on their success rate with the landmark method, we classified three studies (749 participants) as having moderately difficult participants (Glasin 2020; McCarthy 2016B; Skulec 2019). Ultrasound guidance did not clearly increase the procedure time for first‐pass cannulation (MD 23.0, 95% CI ‐39.9 to 85.9; I2 = 97%; very low‐certainty evidence; Analysis 4.2).
Easy participants
Ultrasound guidance increased the procedure time for first‐pass cannulation in easy participants. According to the original studies' definitions, we classified one study (596 participants) as having easy participants (McCarthy 2016C). Ultrasound guidance increased the procedure time for first‐pass cannulation by 94.8 seconds (MD 94.8, 95% CI 81.2 to 108.5; high‐certainty evidence; Analysis 4.1). When we categorised studies based on their success rate with the landmark method, we classified two studies (623 participants) as having easy participants (Aponte 2007; McCarthy 2016C). Ultrasound guidance increased the procedure time for first‐pass cannulation by 95.0 seconds (MD 95.0, 95% CI 81.4 to 108.6; I2 = 0%; moderate‐certainty evidence; Analysis 4.2).
No restriction by intravenous access difficulty level
According to the original studies' definitions, there were no restrictions in terms of difficulty levels in two studies (348 participants) (Glasin 2020; Skulec 2019). We found no clear difference in procedure time for first‐pass cannulation (MD ‐11.3, 95% CI ‐58.4 to 35.7; I2 = 85%; low‐certainty evidence; Analysis 4.1). No studies remained in this subgroup when we categorised studies based on their success rate with the landmark method.
Procedure time for overall cannulation
All participants
Ten studies (803 participants) evaluated the procedure time for overall cannulation (Aponte 2007; Bahl 2016; Costantino 2005; Glasin 2020; Kerforne 2012; Pappas 2006; River 2009; Skulec 2019; Stein 2009; Weiner 2013). Three studies reported the outcome only for participants in whom cannulation was successful (Kerforne 2012; Pappas 2006; Stein 2009). River 2009 was unclear for which participants they assessed the outcome; therefore, we assumed they assessed only participants with successful cannulation, as in a study by the same research team (Stein 2009). We found no clear difference in the procedure time for overall cannulation (MD ‐61.1 seconds, 95% CI ‐161.3 to 39.1; I2 = 86%; very low‐certainty evidence; Analysis 5.1). The tests for subgroup differences did not indicate a difference by either definition of the difficulty (P = 0.75 for the original studies' definition and P = 0.23 for the success rate definition) (Analysis 5.1; Analysis 5.2).
5.1. Analysis.

Comparison 5: Procedure time for overall cannulation, Outcome 1: Difficulty levels defined by original studies
5.2. Analysis.

Comparison 5: Procedure time for overall cannulation, Outcome 2: Difficulty levels defined by the success rate with the landmark method
Difficult participants
According to the original studies' definitions, we classified eight studies (413 participants) as having difficult participants (Aponte 2007; Bahl 2016; Costantino 2005; Kerforne 2012; Pappas 2006; River 2009; Stein 2009; Weiner 2013). We found no clear difference in the procedure time for overall cannulation (MD ‐24.9 seconds, 95% CI ‐323.1 to 273.3; I2 = 77%; very low‐certainty evidence; Analysis 5.1). When we categorised studies based on their success rate with the landmark method, we classified five studies (322 participants) as having difficult participants (Bahl 2016; Costantino 2005; Kerforne 2012; Stein 2009; Weiner 2013). We found no clear difference in the procedure time for overall cannulation (MD ‐117.0 seconds, 95% CI ‐662.8 to 428.8; I2 = 83%; very low‐certainty evidence; Analysis 5.2).
Moderate participants
According to the original studies' definitions, none of the studies included moderately difficult participants. When we categorised studies based on their success rate with the landmark method, we classified three studies (428 participants) as having moderately difficult participants (Glasin 2020; River 2009; Skulec 2019). We found no clear difference in the procedure time for overall cannulation (MD ‐69.8 seconds, 95% CI ‐176.2 to 36.6; I2 = 94%; very low‐certainty evidence; Analysis 5.2).
Easy participants
According to the original studies' definitions, none of the studies included easy participants. When we categorised studies based on their success rate with the landmark method, we classified one study (35 participants) as having easy participants (Aponte 2007). Ultrasound guidance tended to increase the procedure time for overall cannulation, but there was no clear difference (MD 131.6 seconds, 95% CI ‐39.8 to 303.0; low‐certainty evidence; Analysis 5.2).
No restriction by intravenous access difficulty level
According to the original studies' definitions, there were no restrictions in terms of difficulty levels in two studies (390 participants) (Glasin 2020; Skulec 2019). We found no clear difference in the procedure time for overall cannulation (MD ‐77.4, 95% CI ‐185.7 to 30.9; I2 = 97%; very low‐certainty evidence; Analysis 5.1).
No data on the success of cannulation
Pappas 2006 (18 participants) did not report data on the success rate of cannulation with either ultrasound guidance or the landmark method. Thus, we could not classify this study according to its success rate with the landmark method. We found no clear difference in the procedure time for overall cannulation (MD 156.0 seconds, 95% CI ‐450.1 to 762.1; low‐certainty evidence; Analysis 5.2).
Number of cannulation attempts
All participants
Eleven studies (958 participants) evaluated the number of cannulation attempts (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; Glasin 2020; İsmailoğlu 2015; Pappas 2006; River 2009; Skulec 2019; Stein 2009; Weiner 2013). Ultrasound guidance may slightly decrease the number of cannulation attempts (MD ‐0.29, 95% CI ‐0.49 to ‐0.09; I2 = 61%; very low‐certainty evidence; Analysis 6.1). The tests for subgroup differences did not indicate a difference by either definition of the difficulty (P = 0.87 for the original studies' definition and P = 0.31 for the success rate definition) (Analysis 6.2).
6.1. Analysis.

Comparison 6: Number of cannulation attempts, Outcome 1: Difficulty levels defined by original studies
6.2. Analysis.

Comparison 6: Number of cannulation attempts, Outcome 2: Difficulty levels defined by the success rate with the landmark method
Difficult participants
According to the original studies' definitions, we classified nine studies (568 participants) as having difficult participants (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Pappas 2006; River 2009; Stein 2009; Weiner 2013). Ultrasound guidance may slightly decrease the number of cannulation attempts (MD ‐0.33, 95% CI ‐0.64 to ‐0.02; I2 = 64%; very low‐certainty evidence; Analysis 6.1). When we categorised studies based on their success rate with the landmark method, we classified six studies (468 participants) as having difficult participants (Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Stein 2009; Weiner 2013). Ultrasound guidance tended to decrease the number of cannulation attempts, but there was no clear difference (MD ‐0.36, 95% CI ‐0.75 to 0.03; I2 = 73%; very low‐certainty evidence; Analysis 6.2).
Moderate participants
According to the original studies' definitions, none of the studies included moderately difficult participants. When we categorised studies based on their success rate with the landmark method, we classified three studies (437 participants) as having moderately difficult participants (Glasin 2020; River 2009; Skulec 2019). Ultrasound guidance probably decreased the number of cannulation attempts (MD ‐0.32, 95% CI ‐0.47 to ‐0.16; I2 = 20%; moderate‐certainty evidence; Analysis 6.2).
Easy participants
According to the original studies' definitions, none of the studies included easy participants. When we categorised studies based on their success rate with the landmark method, we classified one study (35 participants) as having easy participants (Aponte 2007). We found no clear difference in the number of cannulation attempts (MD 0.10, 95% CI ‐0.44 to 0.64; low‐certainty evidence; Analysis 6.2).
No restriction by intravenous access difficulty level
According to the original studies' definitions, there were no restrictions in terms of difficulty levels in two studies (390 participants) (Glasin 2020; Skulec 2019). Ultrasound guidance probably decreased the number of cannulation attempts (MD ‐0.30, 95% CI ‐0.50 to ‐0.11; I2 = 52%; moderate‐certainty evidence; Analysis 6.1). No studies remained in this subgroup when we categorised studies based on their success rate with the landmark method.
No data on the success rate
Pappas 2006 (18 participants) did not report data on the success rate of cannulation with either ultrasound guidance or the landmark method. Thus, we could not classify this study according to its success rate with the landmark method. We found no clear difference in the number of cannulation attempts (MD ‐1.50, 95% CI ‐3.50 to 0.50; low‐certainty evidence; Analysis 6.2).
Patient satisfaction
All participants
Six studies (423 participants) evaluated patient satisfaction using an NRS of 0 to 10 or a 4‐step Likert scale. (Bridey 2018; Costantino 2005; Glasin 2020; River 2009; Stein 2009; Weiner 2013). Ultrasound guidance tended to increase patient satisfaction, but there was no clear difference (standardised mean difference (SMD) 0.37, 95% CI ‐0.03 to 0.77; I2 = 75%; very low‐certainty evidence; Analysis 7.1). Satisfaction was higher in studies including difficult participants than in studies with no restriction in terms of difficulty levels according to the original studies' definitions (test for subgroup differences: P = 0.02). We found no clear difference between studies including difficult participants and those including moderately difficult participants according to the definition of the success rate with the landmark method (P = 0.27).
7.1. Analysis.

Comparison 7: Patient satisfaction, Outcome 1: Difficulty levels defined by original studies
Difficult participants
According to the original studies' definitions, we classified five studies (333 participants) as having difficult participants (Bridey 2018; Costantino 2005; River 2009; Stein 2009; Weiner 2013). Ultrasound guidance increased patient satisfaction (SMD 0.49, 95% CI 0.07 to 0.92; I2 = 71%; very low‐certainty evidence; Analysis 7.1). When we categorised studies based on their success rate with the landmark method, we classified four studies (286 participants) as having difficult participants (Bridey 2018; Costantino 2005; Stein 2009; Weiner 2013). Ultrasound guidance tended to increase patient satisfaction, but there was no clear difference (SMD 0.52, 95% CI ‐0.01 to 1.05; I2 = 78%; very low‐certainty evidence; Analysis 7.2).
7.2. Analysis.

Comparison 7: Patient satisfaction, Outcome 2: Difficulty levels defined by the success rate with the landmark method
Moderate participants
According to the original studies' definitions, none of the studies included moderately difficult participants. When we categorised studies based on their success rate with the landmark method, we classified two studies (137 participants) as having moderately difficult participants (Glasin 2020; River 2009). We found no clear difference in patient satisfaction (SMD 0.08, 95% CI ‐0.51 to 0.66; I2 = 63%; very low‐certainty evidence; Analysis 7.2).
No restriction by intravenous access difficulty level
According to the original studies' definitions, there were no restrictions in terms of difficulty levels in one study (90 participants) (Glasin 2020). We found no clear difference in patient satisfaction (SMD ‐0.19, 95% CI ‐0.60 to 0.23; low‐certainty evidence; Analysis 7.1). No studies remained in this subgroup when we categorised studies based on their success rate with the landmark method.
Overall complications
All participants
Nine studies (1818 participants) evaluated overall complications (Costantino 2005; Glasin 2020; İsmailoğlu 2015; Nishizawa 2020; McCarthy 2016A; McCarthy 2016B; McCarthy 2016C; Skulec 2019; Stein 2009). The most frequent complication was swelling or haematoma. The details of the complications are given in Table 4. We found no clear difference in overall complications for all participants (RR 0.72, 95% CI 0.46 to 1.14; I2 = 44%; low‐certainty evidence; Analysis 8.1). Ultrasound guidance tended to have more complications in easy participants than in difficult and moderately difficult participants according to both definitions of difficulty. The test for subgroup differences did not indicate a difference amongst difficulty levels with the original studies' definitions (P = 0.06), but indicated a difference when we categorised studies based on their success rate with the landmark method (P = 0.04) (Analysis 8.2). This was due to a study of easy participants (McCarthy 2016C), and the subgroup difference disappeared when this study was excluded.
1. Complications.
| Level |
Number of participants |
Overall complications |
Swelling or haematoma |
Pain |
Nerve injury |
Arterial puncture |
Catheter dislocation |
||||||||||||||
| USG | LM | USG | LM | USG | LM | USG | LM | USG | LM | USG | LM | USG | LM | ||||||||
| Difficult | |||||||||||||||||||||
| Costantino 2005 | 39 | 21 | 0 | 2 (9.5) | 0 | 2 (9.5) | NS | NS | NS | NS | NS | NS | NS | NS | |||||||
| Stein 2009 | 28 | 31 | 0 | 0 | 0 | 0 | NS | NS | 0 | 0 | 0 | 0 | NS | NS | |||||||
| İsmailoğlu 2015 | 30 | 30 | 9 (30.0) | 14 (46.7) | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | |||||||
| McCarthy 2016A | 98 | 94 | 4 (4.1) | 5 (5.3) | 2 (2.0) | 3 (3.2) | NS | NS | 1 (1.0) | 1 (1.1) | 1 (1.0) | 1 (1.1) | NS | NS | |||||||
| Nishizawa 2020 | 30 | 30 | 3 (10.0) | 4 (13.3) | 3 (10.0) | 4 (13.3) | NS | NS | NS | NS | NS | NS | NS | NS | |||||||
| Moderate | |||||||||||||||||||||
| McCarthy 2016B | 202 | 199 | 11 (5.4) | 13* (6.5) | 8 (4.0) | 13 (6.5) | NS | NS | 2 (1.0) | 2 (1.0) | 1 (0.5) | 0 | NS | NS | |||||||
| Easy | |||||||||||||||||||||
| McCarthy 2016C | 305 | 291 | 13 (4.3) | 5 (1.7) | 12 (3.9) | 5 (1.7) | NS | NS | 1 (0.3) | 0 | 0 | 0 | NS | NS | |||||||
| No restriction of difficulty | |||||||||||||||||||||
| Glasin 2020 | 45 | 45 | 5 (11.1) | 6† (13.3) | 0 | 1 (2.2) | 5 (11.1) | 6 (13.3) | NS | NS | NS | NS | NS | NS | |||||||
| Skulec 2019 | D | S | 100 | D | S | 26 (26.0) | D | S | 10 (10.0) | D | S | 16 (16.0) | D | S | NS | D | S | 0 | D | S | 0 |
| 100 | 100 | 13 (13.0) |
7 (7.0) |
8 (8.0) | 3 (3.0) | 4 (4.0) | 3 (3.0) | NS | NS | 0 | 1 (1.0) |
1 (1.0) |
0 | ||||||||
| Total | |||||||||||||||||||||
| 977 | 841 | 65 | 75 | 36 | 38 | 12 | 22 | 4 | 3 | 3 | 1 | 1 | 0 | ||||||||
Values are n (%)
USG: ultrasound guidance, LM: landmark method, NS: not specified, D: dynamic guidance, S: static guidance
*Two participants had complications of both swelling and nerve injury. †One participant had complications of both swelling and pain.
8.1. Analysis.

Comparison 8: Overall complications, Outcome 1: Difficulty levels defined by original studies
8.2. Analysis.

Comparison 8: Overall complications, Outcome 2: Difficulty levels defined by the success rate with the landmark method
Difficult participants
According to the original studies' definitions, we classified five studies (431 participants) as having difficult participants (Costantino 2005; İsmailoğlu 2015; McCarthy 2016A; Nishizawa 2020; Stein 2009). Ultrasound guidance tended to decrease overall complications, but there was no clear difference (RR 0.64, 95% CI 0.37 to 1.10; I2 = 0%; low‐certainty evidence; Analysis 8.1). When we categorised studies based on their success rate with the landmark method, we got the same five studies and results (Analysis 8.2).
Moderate participants
According to the original studies' definitions, we classified one study as having moderately difficult participants (401 participants) (McCarthy 2016B). We found no clear difference in overall complications (RR 0.83, 95% CI 0.38 to 1.82; moderate‐certainty evidence; Analysis 8.1). When we categorised studies based on their success rate with the landmark method, we classified three studies (791 participants) as having moderately difficult participants (Glasin 2020; McCarthy 2016B; Skulec 2019). Ultrasound guidance tended to decrease overall complications, but there was no clear difference (RR 0.58, 95% CI 0.33 to 1.02; I2 = 40%; low‐certainty evidence; Analysis 8.2).
Easy participants
According to the original studies' definitions, we classified one study (596 participants) as having easy participants (McCarthy 2016C). Ultrasound guidance tended to increase overall complications, but there was no clear difference (RR 2.48, 95% CI 0.90 to 6.87; moderate‐certainty evidence; Analysis 8.1). When we categorised studies based on their success rate with the landmark method, we got the same study and result (Analysis 8.2).
No restriction by intravenous access difficulty level
According to the original studies' definitions, there were no restrictions in terms of difficulty levels in two studies (390 participants) (Glasin 2020; Skulec 2019). Ultrasound guidance decreased the overall complications (RR 0.48, 95% CI 0.24 to 0.96; I2 = 34%; low‐certainty evidence; Analysis 8.1). No studies remained in this subgroup when we categorised studies based on their success rate with the landmark method.
Additional subgroup analysis
We conducted additional subgroup analyses only for the three primary outcomes: first‐pass success of cannulation; overall success of cannulation; and pain. Due to the small number of studies with moderate and easy participants, we conducted the subgroup analyses only for studies including difficult participants, except for the type of ultrasound guidance. Only two studies defined the difficulty at the discretion of operators, and we did not perform subgroup analyses with this definition of the difficulty. Because none of the studies used only long‐axis ultrasound guidance, we did not conduct a subgroup analysis for short‐ and long‐axis ultrasound guidance. See Appendix 2 and Appendix 3.
First‐pass success of cannulation
Difficulty of obtaining access:
Difficult: operator could not see and palpate a target vein
When we defined a difficult case as "an operator could not see and palpate a target vein", we included five studies (486 participants) (Bridey 2018; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; Nishizawa 2020). Ultrasound guidance increased the first‐pass success of cannulation by 94% (RR 1.94, 95% CI 1.53 to 2.45; I2 = 12%; low‐certainty evidence; Analysis 1.3).
1.3. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 3: Operators could not see and palpate a target vein
Difficult: participants had a history of difficult intravenous cannulation
When we defined a difficult case as "participants had a history of difficult intravenous cannulation", we included six studies (390 participants) (Aponte 2007; Bahl 2016; Costantino 2005; İsmailoğlu 2015; Nishizawa 2020; Weiner 2013). Ultrasound guidance tended to increase the first‐pass success of cannulation, but there was no clear difference (RR 1.28, 95% CI 0.97 to 1.70; I2 = 38%; very low‐certainty evidence; Analysis 1.4).
1.4. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 4: Participants had a history of difficult intravenous access
Difficult: participants had multiple failed attempts
When we defined a difficult case as "participants had multiple failed attempts", we included four studies (232 participants) (Costantino 2005; Nishizawa 2020; Stein 2009; Weiner 2013). Ultrasound guidance increased the first‐pass success of cannulation by 60% (RR 1.60, 95% CI 1.15 to 2.21; I2 = 0%; low‐certainty evidence; Analysis 1.5).
1.5. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 5: Participants had multiple failed attempts
Operator's skill and study setting:
Operators finished any training programme for ultrasound guidance
When we divided the RCTs according to whether operators had finished any training programme for ultrasound guidance, nine studies had had any training programme (755 participants) (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; McCarthy 2016A; Nishizawa 2020; Stein 2009; Weiner 2013), and one study (60 participants) did not specify whether operators had finished a training programme (Kerforne 2012). Because all studies had had any training programme, we could not compare studies with and without any training programme (Analysis 1.6).
1.6. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 6: Operators finished any training program for ultrasound‐guided peripheral venous cannulation
Operators had any clinical experience with ultrasound guidance
Operators had had any clinical experience with ultrasound guidance before study initiation in five studies (460 participants) (Aponte 2007; Bridey 2018; Costantino 2005; McCarthy 2016A; Stein 2009). Ultrasound guidance tended to increase the first‐pass success of cannulation, but there was no clear difference (RR 1.44, 95% CI 0.91 to 2.27; I2 = 78%; very low‐certainty evidence; Analysis 1.7). Operators did not have any clinical experience with ultrasound guidance in three studies (235 participants) (Bahl 2016; Nishizawa 2020; Weiner 2013). Ultrasound guidance tended to increase the first‐pass success of cannulation, but there was no clear difference (RR 1.33, 95% CI 0.99 to 1.79; I2 = 19%; low‐certainty evidence). Two studies did not specify whether operators had had any clinical experience (120 participants) (İsmailoğlu 2015; Kerforne 2012). The test for subgroup difference did not indicate a difference (P = 0.33), and it was similar even when we excluded the two studies without the specification.
1.7. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 7: Operators had any clinical experience with ultrasound‐guided peripheral intravenous cannulation
Operators finished any kind of training programme for ultrasound guidance and had any clinical experience of ultrasound guidance
We had the same results as for the definition "operators had any clinical experience of ultrasound guidance" (Analysis 1.8).
1.8. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 8: Operators finished any training program for ultrasound‐guided peripheral venous cannulation plus any clinical experience
Types of operators
Operators were nurses in seven studies (504 participants) (Aponte 2007; Bahl 2016; Bridey 2018; İsmailoğlu 2015; Kerforne 2012; Nishizawa 2020; Weiner 2013). Ultrasound guidance increased the first‐pass success of cannulation by 32% (RR 1.32, 95% CI 1.03 to 1.71; I2 = 40%; low‐certainty evidence; Analysis 1.9). Operators were physicians in two studies (119 participants) (Costantino 2005; Stein 2009). Ultrasound guidance tended to increase the first‐pass success of cannulation, but there was no clear difference (RR 1.47, 95% CI 0.86 to 2.50; I2 = 0%; low‐certainty evidence). Operators were technicians in one study (192 participants) (McCarthy 2016A). Ultrasound guidance increased the first‐pass success of cannulation by 133% (RR 2.33, 95% CI 1.74 to 3.11; moderate‐certainty evidence). The test for subgroup difference indicated a difference (P = 0.01) and was considered to originate from McCarthy 2016A.
1.9. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 9: Types of operators
Study setting
Six studies were conducted in the emergency department (546 participants) (Bahl 2016; Costantino 2005; İsmailoğlu 2015; McCarthy 2016A; Stein 2009; Weiner 2013). Ultrasound guidance increased the first‐pass success of cannulation by 60% (RR 1.60, 95% CI 1.12 to 2.28; I2 = 59%; very low‐certainty evidence, Analysis 1.10). Three studies were in the intensive care unit (ICU) (234 participants) (Bridey 2018; Kerforne 2012; Nishizawa 2020). Ultrasound guidance increased the first‐pass success of cannulation by 64% (RR 1.64, 95% CI 1.20 to 2.23; I2 = 0%; low‐certainty evidence). One study was in the operating room (35 participants) (Aponte 2007). We found no clear difference in the first‐pass success of cannulation (RR 0.91, 95% CI 0.63 to 1.30; low‐certainty evidence). Although the test for subgroup difference indicated there was a difference (P = 0.03), it disappeared when Aponte 2007 was excluded.
1.10. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 10: Setting
Year of publication
Two studies were published between 1999 and 2008 in two studies (95 participants) (Aponte 2007; Costantino 2005). We found no clear difference in the first‐pass success of cannulation (RR 1.24, 95% CI 0.51 to 3.02; I2 = 75%; very low‐certainty evidence; Analysis 1.11). Eight studies were published in 2009 or later (720 participants) (Bahl 2016; Bridey 2018; İsmailoğlu 2015; Kerforne 2012; McCarthy 2016A; Nishizawa 2020; Stein 2009; Weiner 2013). Ultrasound guidance increased the first‐pass success of cannulation by 60% (RR 1.60, 95% CI 1.24 to 2.07; I2 = 50%; low‐certainty evidence). The test for subgroup differences did not indicate a difference (P = 0.59).
1.11. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 11: Year of publication
Type of ultrasound guidance
One study evaluated both dynamic and static ultrasound guidance (300 participants) (Skulec 2019). Dynamic ultrasound guidance did not clearly increase the first‐pass success of cannulation (RR 1.16, 95% CI 0.98 to 1.37; moderate‐certainty evidence; Analysis 1.12). Static ultrasound guidance increased the first‐pass success of cannulation by 24% (RR 1.24, 95% CI 1.05 to 1.46; moderate‐certainty evidence). The test for subgroup differences did not indicate a difference (P = 0.59).
1.12. Analysis.

Comparison 1: First‐pass success of cannulation, Outcome 12: Dynamic guidance or static guidance
Overall success of cannulation
Difficulty of obtaining access:
Difficult: operator could not see and palpate a target vein
When we defined a difficult case as "an operator could not see and palpate a target vein", we included four studies (294 participants) (Bridey 2018; İsmailoğlu 2015; Kerforne 2012; Nishizawa 2020). Ultrasound guidance tended to increase the overall success of cannulation, but there was no clear difference (RR 1.53, 95% CI 0.98 to 2.41; I2 = 77%; very low‐certainty evidence; Analysis 2.3).
2.3. Analysis.

Comparison 2: Overall success of cannulation, Outcome 3: Operators could not see and palpate a target vein
Difficult: participants had a history of difficult intravenous cannulation
When we defined a difficult case as "participants had a history of difficult intravenous cannulation", we included six studies (390 participants) (Aponte 2007; Bahl 2016; Costantino 2005; İsmailoğlu 2015; Nishizawa 2020; Weiner 2013). Ultrasound guidance tended to increase the overall success of cannulation, but there was no clear difference (RR 1.66, 95% CI 0.97 to 2.86; I2 = 94%; very low‐certainty evidence; Analysis 2.4).
2.4. Analysis.

Comparison 2: Overall success of cannulation, Outcome 4: Participants had a history of difficult intravenous access
Difficult: participants had multiple failed attempts
When we defined a difficult case as "participants had multiple failed attempts", we included five studies (279 participants) (Costantino 2005; Nishizawa 2020; River 2009; Stein 2009; Weiner 2013). Ultrasound guidance tended to increase the overall success of cannulation, but there was no clear difference (RR 1.53, 95% CI 0.93 to 2.51; I2 = 91%; very low‐certainty evidence; Analysis 2.5).
2.5. Analysis.

Comparison 2: Overall success of cannulation, Outcome 5: Participants had multiple failed attempts
Operator's skill and study setting:
Operators finished any training programme for ultrasound guidance
When we divided the RCTs according to whether operators had finished any training programme for ultrasound guidance, nine studies had had any training programme (610 participants) (Aponte 2007; Bahl 2016; Bridey 2018; Costantino 2005; İsmailoğlu 2015; Nishizawa 2020; River 2009; Stein 2009; Weiner 2013), and one study (60 participants) did not specify whether operators had finished a training programme (Kerforne 2012). Because all studies had had any training programme, we could not compare studies with and without any training programme (Analysis 2.6).
2.6. Analysis.

Comparison 2: Overall success of cannulation, Outcome 6: Operators finished any training program for ultrasound‐guided peripheral venous cannulation
Operators had any clinical experience with ultrasound guidance
Operators had had any clinical experience with ultrasound guidance before study initiation in five studies (315 participants) (Aponte 2007; Bridey 2018; Costantino 2005; River 2009; Stein 2009). We found no clear difference (RR 1.15, 95% CI 0.91 to 1.44; I2 = 85%; very low‐certainty evidence; Analysis 2.7). Operators did not have any clinical experience with ultrasound guidance in three studies (235 participants) (Bahl 2016; Nishizawa 2020; Weiner 2013). Ultrasound guidance increased the overall success of cannulation by 46% (RR 1.46, 95% CI 1.18 to 1.79; I2 = 0%; low‐certainty evidence). Two studies (120 participants) did not specify whether operators had had any clinical experience (İsmailoğlu 2015; Kerforne 2012). Although the test for subgroup difference indicated a difference (P = 0.03), this was lost when we excluded the two studies without the specification.
2.7. Analysis.

Comparison 2: Overall success of cannulation, Outcome 7: Operators had any clinical experience with ultrasound‐guided peripheral intravenous cannulation
Operators finished any kind of training programme for ultrasound guidance and had any clinical experience of ultrasound guidance
We had the same results as for the definition "operators had any clinical experience of ultrasound guidance" (Analysis 2.8).
2.8. Analysis.

Comparison 2: Overall success of cannulation, Outcome 8: Operators finished any training program for ultrasound‐guided peripheral venous cannulation and had any clinical experience
Types of operators
Operators were nurses in eight studies (551 participants) (Aponte 2007; Bahl 2016; Bridey 2018; İsmailoğlu 2015; Kerforne 2012; Nishizawa 2020; River 2009; Weiner 2013). Ultrasound guidance increased the overall success of cannulation by 37% (RR 1.37, 95% CI 1.05 to 1.78; I2 = 83%; very low‐certainty evidence; Analysis 2.9). Operators were physicians in two studies (119 participants) (Costantino 2005; Stein 2009). Ultrasound guidance did not clearly increase the overall success of cannulation (RR 1.72, 95% CI 0.22 to 13.47; I2 = 98%; very low‐certainty evidence). The test for subgroup difference did not indicate a difference (P = 0.83).
2.9. Analysis.

Comparison 2: Overall success of cannulation, Outcome 9: Types of operators
Study setting
Six studies (401 participants) were conducted in the emergency department (Bahl 2016; Costantino 2005; İsmailoğlu 2015; River 2009; Stein 2009; Weiner 2013). Ultrasound guidance increased the overall success of cannulation by 57% (RR 1.57, 95% CI 1.05 to 2.36; I2 = 90%; very low‐certainty evidence). Three studies (234 participants) were in the ICU (Bridey 2018; Kerforne 2012; Nishizawa 2020). Ultrasound guidance did not clearly increase the overall success of cannulation (RR 1.36, 95% CI 0.86 to 2.15; I2 = 75%; very low‐certainty evidence). One study (35 participants) was in the operating room (Aponte 2007), and we found no evidence of a difference (RR 1.00, 95% CI 0.90 to 1.11; low‐certainty evidence; Analysis 2.10). The test for subgroup difference did not indicate a difference between settings (P = 0.06).
2.10. Analysis.

Comparison 2: Overall success of cannulation, Outcome 10: Setting
Year of publication
Two studies (95 participants) were published between 1999 and 2008 (Aponte 2007; Costantino 2005). We found no clear difference (RR 1.70, 95% CI 0.10 to 29.24; I2 = 99%; very low‐certainty evidence; Analysis 2.11). Eight studies (575 participants) were published in 2009 or later (Bahl 2016; Bridey 2018; İsmailoğlu 2015; Kerforne 2012; Nishizawa 2020; River 2009; Stein 2009; Weiner 2013). Ultrasound guidance increased the overall success of cannulation by 36% (RR 1.36, 95% CI 1.08 to 1.71; I2 = 78%; very low‐certainty evidence). The test for subgroup difference did not indicate a difference (P = 0.88).
2.11. Analysis.

Comparison 2: Overall success of cannulation, Outcome 11: Year of publication
Type of ultrasound guidance
One study (300 participants) evaluated both dynamic and static ultrasound guidance (Skulec 2019). The overall success of cannulation for dynamic and static ultrasound guidance was the same; ultrasound guidance did not clearly increase the success of cannulation and the 95% CI included no effect (RR 1.10, 95% CI 1.00 to 1.21; low‐certainty evidence; Analysis 2.12). The test for subgroup difference did not indicate a difference (P = 1.00).
2.12. Analysis.

Comparison 2: Overall success of cannulation, Outcome 12: Dynamic guidance or static guidance
Pain
We conducted subgroup analyses only for the following four parameters for this outcome, and not for the other parameters owing to the small number of studies.
Operator's skill and study setting:
Operators finished any training programme for ultrasound guidance
When we divided the RCTs by whether operators had finished any training programme for ultrasound guidance, three studies (305 participants) had had any training programme (İsmailoğlu 2015; McCarthy 2016A; Weiner 2013). One study (18 participants) did not specify whether operators had finished a training programme (Pappas 2006). Because all studies had had any training programme, we could not compare studies with and without any training programme (Analysis 3.3).
3.3. Analysis.

Comparison 3: Pain, Outcome 3: Operators finished any training program for ultrasound‐guided peripheral venous cannulation
Types of operators
Operators were nurses in three studies (131 participants) (İsmailoğlu 2015; Pappas 2006; Weiner 2013). We found no clear difference in pain between the ultrasound guidance and landmark method groups in these studies (MD ‐0.36, 95% CI ‐1.68 to 0.95; I2 = 66%; very low‐certainty evidence; Analysis 3.4). Operators were technicians in one study (192 participants) (McCarthy 2016A). We found no clear difference in pain between the two groups in this study (MD 0.20, 95% CI ‐0.61 to 1.01; low‐certainty evidence). The test for subgroup difference did not indicate a difference (p = 0.48).
3.4. Analysis.

Comparison 3: Pain, Outcome 4: Types of operators
Study setting
Four studies (323 participants) were conducted in the emergency department (İsmailoğlu 2015; McCarthy 2016A; Pappas 2006; Weiner 2013). Because there were no studies in other settings, we could not compare them (Analysis 3.5).
3.5. Analysis.

Comparison 3: Pain, Outcome 5: Setting
Year of publication
One study (18 participants) was published between 1999 and 2008 (Pappas 2006). We found no clear difference in pain (MD 0.90, 95% CI ‐0.52 to 2.32; low‐certainty evidence; Analysis 3.6). Three studies (305 participants) were published in 2009 or later (İsmailoğlu 2015; McCarthy 2016A; Weiner 2013). We found no clear difference (MD ‐0.49, 95% CI ‐1.48 to 0.49; I2 = 60%; very low‐certainty evidence). The test for subgroup difference did not indicate a difference (P = 0.11).
3.6. Analysis.

Comparison 3: Pain, Outcome 6: Year of publication
Sensitivity analysis
We limited the studies to RCTs only or studies with a low overall risk of bias (see Sensitivity analysis), and all the results were comparable to the original results and not qualitatively different (Analysis 9.1 to Analysis 9.8; Analysis 10.1 to Analysis 10.7; Table 5; Table 6; Table 7).
9.1. Analysis.

Comparison 9: Sensitivity analyses 1 (RCTs only), Outcome 1: First‐pass success of cannulation
9.8. Analysis.

Comparison 9: Sensitivity analyses 1 (RCTs only), Outcome 8: Overall complications
10.1. Analysis.

Comparison 10: Sensitivity analysis 2 (low risk of bias studies only), Outcome 1: First‐pass success of cannulation
10.7. Analysis.

Comparison 10: Sensitivity analysis 2 (low risk of bias studies only), Outcome 7: Overall complications
2. Sensitivity analysis for difficult participants.
| Outcomes | Original results | RCTs only | Low ROB studies only | |
| First‐pass success of cannulation | ES | 1.50 (1.15, 1.95) | 1.50 (1.15, 1.96) | 1.82 (0.98, 3.37) |
| I2 | 62% | 66% | 65% | |
| Overall success of cannulation | ES | 1.40 (1.10, 1.77) | 1.19 (0.98, 1.45) | 1.03 (0.92, 1.16) |
| I2 | 88% | 79% | NA *1 | |
| Pain | ES | ‐0.20 (‐1.13, 0.72) | 0.23 (‐0.42, 0.88) | 0.20 (‐0.61, 1.01) |
| I2 | 62% | 0% | NA *1 | |
| Procedure time for first‐pass cannulation | ES | 119.9 (88.6, 151.1) | 119.9 (88.6, 151.1) | 120.6 (88.3, 152.9) |
| I2 | 0% | 0% | NA *1 | |
| Procedure time for overall cannulation | ES | ‐24.9 (‐323.1, 273.3) | 97.5 (‐17.6, 212.5) | NA *2 |
| I2 | 77% | 0% | NA *2 | |
| Number of cannulation attempts | ES | ‐0.33 (‐0.64, ‐0.02) | ‐0.17 (‐0.36, 0.03) | ‐0.60 (‐1.51, 0.31) |
| I2 | 64% | 0% | NA *1 | |
| Patient satisfaction | ES | 0.49 (0.07, 0.92) | 0.25 (0.01, 0.50) | NA *2 |
| I2 | 71% | 5% | NA *2 | |
| Overall complications | ES | 0.64 (0.37, 1.10) | 0.76 (0.29, 1.96) | 0.77 (0.21, 2.77) |
| I2 | 0% | 0% | NA | |
Dichotomous outcomes shown as RR (95% CI), continuous outcomes as MD or SMD (95% CI) ES: effect size; MD: mean difference; NA: not applicable; RCT: randomised controlled trial; ROB: risk of bias; RR: risk ratio; SMD: standardised mean difference *1: only one study; *2: no study
3. Sensitivity analysis for moderate participants.
| Outcomes | Original results | RCTs only | Low ROB studies only | |
| First‐pass success of cannulation | ES | 1.14 (1.02, 1.27) | 1.14 (1.02, 1.27) | 1.14 (1.02, 1.27) |
| I2 | NA *1 | NA*1 | NA*1 | |
| Overall success of cannulation | ES | NA *2 | NA *2 | NA *2 |
| I2 | NA *2 | NA *2 | NA *2 | |
| Pain | ES | 0.10 (‐0.47, 0.67) | 0.10 (‐0.47, 0.67) | 0.10 (‐0.47, 0.67) |
| I2 | NA *1 | NA *1 | NA *1 | |
| Procedure time for first‐pass cannulation | ES | 95.2 (72.8, 117.6) | 95.2 (72.8, 117.6) | 95.2 (72.8, 117.6) |
| I2 | NA *1 | NA *1 | NA *1 | |
| Procedure time for overall cannulation | ES | NA *2 | NA *2 | NA *2 |
| I2 | NA *2 | NA *2 | NA *2 | |
| Number of cannulation attempts | ES | NA *2 | NA *2 | NA *2 |
| I2 | NA *2 | NA *2 | NA *2 | |
| Patient satisfaction | ES | NA *2 | NA *2 | NA *2 |
| I2 | NA *2 | NA *2 | NA *2 | |
| Overall complications | ES | 0.83 (0.38, 1.82) | 0.83 (0.38, 1.82) | 0.83 (0.38, 1.82) |
| I2 | NA *1 | NA *1 | NA *1 | |
Dichotomous outcomes shown as RR (95% CI), continuous outcomes as MD or SMD (95% CI) ES: effect size; MD: mean difference; NA: not applicable; RCT: randomised controlled trial; ROB: risk of bias; RR: risk ratio; SMD: standardised mean difference *1: only one study; *2: no study
4. Sensitivity analysis for easy participants.
| Outcomes | Original results | RCTs only | Low ROB studies only | |
| First‐pass success of cannulation | ES | 0.89 (0.85, 0.94) | 0.89 (0.85, 0.94) | 0.89 (0.85, 0.94) |
| I2 | NA *1 | NA*1 | NA*1 | |
| Overall success of cannulation | ES | NA *2 | NA *2 | NA *2 |
| I2 | NA *2 | NA *2 | NA *2 | |
| Pain | ES | 0.60 (0.17, 1.03) | 0.60 (0.17, 1.03) | 0.60 (0.17, 1.03) |
| I2 | NA *1 | NA *1 | NA *1 | |
| Procedure time for first‐pass cannulation | ES | 94.8 (81.2, 108.5) | 94.8 (81.2, 108.5) | 94.8 (81.2, 108.5) |
| I2 | NA *1 | NA *1 | NA *1 | |
| Procedure time for overall cannulation | ES | NA *2 | NA *2 | NA *2 |
| I2 | NA *2 | NA *2 | NA *2 | |
| Number of cannulation attempts | ES | NA *2 | NA *2 | NA *2 |
| I2 | NA *2 | NA *2 | NA *2 | |
| Patient satisfaction | ES | NA *2 | NA *2 | NA *2 |
| I2 | NA *2 | NA *2 | NA *2 | |
| Overall complications | ES | 2.48 (0.90, 6.87) | 2.48 (0.90, 6.87) | 2.48 (0.90, 6.87) |
| I2 | NA *1 | NA *1 | NA *1 | |
Dichotomous outcomes shown as RR (95% CI), continuous outcomes as MD or SMD (95% CI) ES: effect size; MD: mean difference; NA: not applicable; RCT: randomised controlled trial; ROB: risk of bias; RR: risk ratio; SMD: standardised mean difference *1: only one study; *2: no study
Discussion
Summary of main results
We included 16 studies that compared ultrasound guidance with the landmark guidance method for peripheral venous cannulation in adults. The effect of ultrasound guidance on achieving peripheral venous cannulation depends on the difficulty level and the included studies used varying definitions of difficulty. We described the results by the difficulty levels used by the studies, and we also defined the difficulty by the success rate of the landmark method to evaluate consistency.
Difficult participants
Ultrasound guidance was probably helpful for difficult participants. Ultrasound guidance probably increased the primary outcome first‐pass success of cannulation (low‐certainty evidence) and may increase the overall success of cannulation (very low‐certainty evidence), but not pain (very low‐certainty evidence). The results were consistent across the two definitions of the difficulty, but the certainty of the evidence was moderate when we defined the difficulty levels based on the success rate with the landmark method. For secondary outcomes, ultrasound guidance may decrease the number of cannulation attempts (very low‐certainty evidence) and may improve patient satisfaction (very low‐certainty evidence) with the original studies' definitions. Ultrasound guidance did not show a clear benefit to the number of cannulation attempts or patient satisfaction using the definition based on the success rate with the landmark method. In contrast, ultrasound guidance probably increased the procedure time for first‐pass cannulation with both definitions (low‐certainty evidence), but the difference was less than three minutes, which is clinically small unless the patient has a very urgent condition. The certainty of the evidence was moderate when we defined the difficulty levels based on the success rate with the landmark method. We found no clear difference in the procedure time for overall cannulation (very low‐certainty evidence) and overall complications with both definitions (low‐certainty evidence).
Moderate participants
Ultrasound guidance might be helpful for moderately difficult participants. Ultrasound guidance probably increased the first‐pass success of cannulation to a lesser extent than in the difficult participants (moderate‐certainty evidence), but not pain (low‐certainty evidence). Results were consistent across both definitions of the difficulty, but the certainty of the evidence was high for first‐pass success of cannulation when we defined the difficulty levels based on the success rate with the landmark method. For the overall success of cannulation, no relevant studies involved moderately difficult participants with the original definition, and there was no apparent effect of ultrasound guidance based on the definition of the success rate with the landmark method (very low‐certainty evidence). For secondary outcomes, ultrasound guidance increased the procedure time for first‐pass cannulation with the original studies' definitions (high‐certainty evidence), but not with the definition based on the success rate (very low‐certainty evidence). For the procedure time for overall cannulation, number of cannulation attempts, and patient satisfaction, no relevant studies involved moderately difficult participants with the original definition. Based on the definition of the success rate with the landmark method, ultrasound guidance decreased the number of cannulation attempts (moderate‐certainty evidence), and there was no apparent effect of ultrasound guidance on the procedure time for overall cannulation (very low‐certainty evidence), and patient satisfaction (very low‐certainty evidence). Regardless of the definition used, we found no clear difference in overall complications (low‐ to moderate‐certainty evidence).
Easy participants
Ultrasound guidance was likely not beneficial in easy participants. Ultrasound guidance probably decreased the first‐pass success of cannulation (high‐certainty evidence) and slightly increased pain (moderate‐certainty evidence). The results were consistent across both definitions of the difficulty. For the overall success of cannulation, no relevant studies involved easy participants with the original definition, and there was no apparent effect of ultrasound guidance based on the definition of the success rate with the landmark method (low‐certainty evidence). For secondary outcomes, ultrasound guidance increased the procedure time for first‐pass cannulation with both definitions (moderate‐ to high‐certainty evidence). For the procedure time for overall cannulation, and number of cannulation attempts, no relevant studies involved easy participants with the original definition. Based on the definition of the success rate with the landmark method, there was no apparent effect of ultrasound guidance on the procedure time for overall cannulation (low‐certainty evidence), and number of cannulation attempts (low‐certainty evidence). For patient satisfaction, there were no studies with easy participants for both definitions of the difficulty. Regardless of the definition used, we found no clear difference in overall complications (moderate‐certainty evidence).
Subgroup analyses
In the subgroup analyses, the effect of ultrasound guidance was qualitatively similar for each original study's definition of difficulty, although the number of studies was very small to perform meta‐analysis for some outcomes. There was no consistent definition of difficulty which showed low heterogeneity across the outcomes. Because all studies had had any training programme, we could not compare studies with and without any training programme. The clinical experience of operators, study settings, and year of publication did not affect the effects of ultrasound guidance. There were three types of operators, and the first‐pass success of cannulation was higher for technicians than for nurses or physicians. We found no differences amongst types of operators in the overall success of cannulation or pain. Only one study compared dynamic and static ultrasound guidance, so we could not perform the meta‐analysis. Static ultrasound guidance had a shorter procedure time for first‐pass and overall cannulation and fewer overall complications for participants without restriction by difficulty level than dynamic ultrasound guidance. The other outcomes were similar for both types of guidance.
Overall completeness and applicability of evidence
We conducted a thorough search and contacted study authors directly to obtain unpublished data and studies, and also to confirm the details of the studies. Nine study authors provided us with unpublished data, making our meta‐analysis the most comprehensive to date (Bahl 2016; Bridey 2018; Costantino 2005; Glasin 2020; Kerforne 2012; McCarthy 2016; Nishizawa 2020; Skulec 2019; Weiner 2013). The 16 included studies had various participant backgrounds, operators, and settings, and the effect of ultrasound guidance was similar amongst the various situations, except for the difficulty level. Therefore, we believe that ultrasound guidance is applicable in many situations, regardless of the operator's ultrasound experience if a training programme is available, and in settings including the emergency department, ICU, operating room, and prehospital setting. However, these results must be interpreted carefully in some respects.
As the effects of ultrasound guidance depend on the difficulty level with the landmark method, it is necessary to assess the difficulty when performing ultrasound guidance. However, as we expected, the definition of difficulty varied between studies. There were four types of original studies' definitions of difficulty, and we could not find any consistent difference across the outcomes amongst the four definitions. An accurate assessment was difficult because some outcomes were only evaluated in a few studies, and some studies combined multiple definitions of difficulty. Stratification by factors after randomisation should usually be avoided, but the landmark method is a widely used procedure, and the success rate of the landmark method would reflect the difficulty level (McCarthy 2016; Sebbane 2013; Van Loon 2016). The effect sizes and difficulty‐dependent trends were similar for both definitions of difficulty, which made the results more certain. Clinically, each of the four definitions of difficulty seemed reasonable, but they might not be enough to stand alone, and there is also the issue of reproducibility. A promising way to assess the difficulty level is to use a prediction score. The modified Adult Difficult IntraVenous Access (A‐DIVA) scale consists of five items, such as visibility or palpability of the target vein and a history of difficult intravenous access. The first‐pass success of cannulation was 6% in the high‐risk group, 63% in the moderate‐risk group, and 96% in the low‐risk group (Van Loon 2019). High‐risk and probably moderate‐risk patients are good candidates for ultrasound guidance on this scale. Another Enhanced Adult DIVA (EA‐DIVA) score, consisting of eight items, predicted patients who required four or more cannulation attempts with a positive predictive value of 56% and a negative predictive value of 97.5% (Civetta 2019). However, both prediction models have methodological limitations because univariate regression analysis was used to select predictors, and have not been validated externally to date.
Regarding the characteristics of operators, we could not compare the presence and absence of any training programme on ultrasound guidance, and previous experience with ultrasound guidance had no apparent benefit. However, from a clinical standpoint, proficiency in ultrasound guidance is essential, and an appropriate training programme and sufficient clinical experience are necessary. The first‐pass success of ultrasound guidance cannulation varied widely amongst the included studies, ranging from approximately 20% to 80% (average 57%), and operators' proficiency was likely one major factor. İsmailoğlu 2015 had the lowest first‐pass success of cannulation at 20% with ultrasound guidance, which according to the authors, was due to the low proficiency of the operators. In the three studies that showed high first‐pass success of cannulation with ultrasound guidance (80% to 85%), the operators were technicians specialising in peripheral intravenous cannulation, with 39% of the operators performing five or more ultrasound guidance cases per day (McCarthy 2016A; McCarthy 2016B; McCarthy 2016C). Performing five ultrasound guidance cases per day was highly frequent, suggesting a high proficiency in these operators. In one study, a dedicated peripheral venous cannulation team of nurses was trained in ultrasound guidance and performed up to six ultrasound guidance cases per day, achieving a high first‐pass success rate of 93% (Sou 2017). Therefore, increasing the frequency and proficiency of ultrasound guidance seems important, and having a dedicated team could be one way to achieve this. Monitoring operators' proficiency level, such as their success rates, would be preferable in the clinical application of ultrasound guidance. It would also allow an appropriate assessment by the operators of the difficulty levels of the patients eligible for ultrasound guidance. This is because, in studies classified as moderately difficult cases, the first‐pass success of cannulation was as high as 80% or more, and the effectiveness of ultrasound guidance for moderately difficult cases can be expected in highly skilled operators (Glasin 2020; McCarthy 2016B; Skulec 2019). We did not aim to assess the content of training programmes or conduct a quantitative assessment of previous clinical ultrasound guidance experience in this review.
Complications varied widely, from 0% to 22% in the included studies and 1% to 60% in previous studies (Bauman 2009; Duran 2016; Oliveira 2016; Schoenfeld 2011). This large difference was probably due to operators' proficiency, patient characteristics, the definition of complications, and small sample sizes. İsmailoğlu 2015 had the most complications in the included studies; it also had the lowest successful cannulation rate. Low successful cannulation leads to more cannulation attempts and increased complications. Therefore, operators' proficiency may also be important in complications.
Three occupational groups were included in the subgroup analysis, with technicians having higher first‐pass success of cannulation than nurses and physicians. However, this result was derived only from McCarthy 2016A, where technicians in this study performed a high frequency of ultrasound‐guided cannulations and appeared to be more skilled. Previous studies have suggested that ultrasound guidance is similarly effective regardless of operator occupation (Duran‐Gehring 2016; Oliveira 2016; Schoenfeld 2011). Therefore, we consider that proficiency is more likely to be a factor than occupational differences.
We could not find any consistent difference across the outcomes amongst the four settings—the emergency department, ICU, operating room, and prehospital setting. Only two studies were conducted in the operating room and the total number of participants was very small (53 combined). Only one study was conducted in a prehospital setting. Given the nature of the intervention, we believe that it is likely ultrasound guidance will be similarly effective irrespective of the setting.
Because quantitative evaluation was expected to be difficult and there are many models of ultrasound machines, we did not conduct an analysis of the effect of the quality of the ultrasound machines. Instead, we divided the studies by year of publication. Although we could not find any meaningful results, it is likely that the visibility of the needle could affect the effect of ultrasound guidance. Additional data in future updates may allow detection of differences due to the use of newer machines.
Another issue was whether the appropriate length of needle was used according to the depth of the vein. Because no studies reported the depth of the targeted vein, it was not possible to determine the extent of this effect. However, in two studies that used only short needles, the first‐pass success of ultrasound guidance cannulation was low (40% to 50%), suggesting that the needles may have been too short (Bridey 2018; Costantino 2005).
This meta‐analysis did not evaluate the longevity of functional catheters placed under ultrasound guidance and the landmark method. According to earlier studies, and as mentioned in the Methods section, it is crucial to use needles of the appropriate length according to the depth of the target vein (Avila 2019; Bahl 2019; Bahl 2020; Elia 2012; Pandurangadu 2018). We will consider including this issue in future updates.
Certainty of the evidence
See Table 1; Table 2; Table 3; Appendix 4; Appendix 5; and Appendix 6.
First‐pass success of cannulation
We downgraded to low‐certainty evidence due to the serious risk of bias and heterogeneity in the difficult participants according to the original studies' definition. However, using the definition based on the success rate with the landmark method reduced heterogeneity, so we assessed it as moderate‐certainty evidence. Although the risk of bias was high in seven of the 14 studies, the results of sensitivity analyses, which excluded quasi‐RCTs or studies with high risk of bias, were similar to the overall results (Analysis 9.1; Analysis 10.1). We found no obvious publication bias (Figure 4).
4.

Funnel plot of analysis 1.1: First‐pass success of cannulation ‐ difficulty levels defined by original studies
The certainty of the evidence for the moderately difficult participants was moderate, downgraded by one level for imprecision. When using the definition based on the success rate, the certainty of the evidence was high.
The certainty of the evidence for the easy participants was high according to the original studies' definitions, and it was moderate using the definition based on the success rate, downgraded for lack of blinding of the outcome assessors. The difficulty‐dependent effect size was similar for both definitions of the difficulty.
Overall success of cannulation
The certainty of the evidence for the overall success of cannulation was very low for difficult participants. We downgraded by one level as the risk of bias was high in nine of 12 studies due to quasi‐randomisation and non‐blinding of the outcome assessors. We downgraded by two levels due to serious heterogeneity, mainly due to the lack of a standardised definition of failure. Two studies defined a failure as unsuccessful cannulation after three punctures (Bridey 2018; Costantino 2005), three studies defined failure as unsuccessful cannulation after two punctures (Bahl 2016; Kerforne 2012; Nishizawa 2020), and the remaining seven studies did not give a definition. Some participants in one study had as many as eight punctures, which would have been affected by the ceiling effect (Stein 2009). Furthermore, the threshold for judging failure could differ between the two arms. The funnel plot was asymmetric, but since this was due to two quasi‐RCTs, we did not downgrade further due to publication bias (Figure 5).
5.

Funnel plot of analysis 2.1: Overall success of cannulation ‐ difficulty levels defined by original studies
Pain
We downgraded to very low‐certainty evidence in the difficult participants, according to both definitions of the difficulty, because of the serious risk of bias mainly due to non‐blinding, inconsistency, and imprecision. The certainty of the evidence for moderately difficult participants was low due to risk of bias concerns and imprecision. We downgraded the certainty of the evidence for easy participants to moderate due to risk of bias concerns.
Although we assessed the blinding domain as high risk in all studies because all participants were not blinded and this outcome is subjective, it seemed unlikely that participants would have had a strong preference for either of the intervention methods. The outcome assessors were not neutral third parties in three studies in difficult participants (İsmailoğlu 2015; Pappas 2006; Weiner 2013); excluding these three studies did not affect the results (data not shown). The outcome assessors were third parties in the studies including easy and moderately difficult participants (McCarthy 2016B; McCarthy 2016C).
To our knowledge, no studies have assessed the minimum clinically important difference (MCID) for pain in peripheral intravenous cannulation, but a meta‐analysis examining the MCID for acute pain found it to be 1.7 for pain relief and 1.1 for worsening pain on an NRS of 0 to 10 (Olsen 2017). The mean differences and their upper limits of the 95% CI for all difficulty levels were less than the MCID in the overall analysis and all sensitivity analyses; hence, there was no clinically meaningful difference detected. However, the lower success of ultrasound guidance cannulation in easy participants can explain the increased pain, and therefore, it is reasonably certain that ultrasound guidance increased pain in easy participants. However, the upper limit of the 95% CI did not exceed the MCID, and the degree of increase in pain was considered small. Finally, excluding the quasi‐RCT İsmailoğlu 2015 improved the heterogeneity to zero in difficult participants with both definitions, and the results were similar to the overall results.
Procedure time for first‐pass cannulation
We downgraded to low certainty‐evidence in difficult participants due to risk of bias concerns and imprecision. The certainty of the evidence for moderate and easy participants was high. There were important differences amongst the studies in the definitions of the outcome and study participants. First, the definitions of start and stop times were similar in all studies, except one (Aponte 2007), and included two steps: searching for a target vein and puncturing it. In Aponte 2007, the ultrasound guidance group started measuring time after the target vein was identified, but the landmark method group started measuring when searching for the target vein. However, this study was small, and excluding it from the meta‐analysis did not change the results. Second, ultrasound guidance increased the procedure time in all studies, except for two with different characteristics (Glasin 2020; Skulec 2019). In Skulec 2019, ultrasound guidance had a slightly longer procedure time than the landmark method (approximately 10 seconds), but to a lesser degree than in the other studies (90 to 120 seconds). The main reason is that the result was based only on successful cases. Another reason was that it was the only study that had a static ultrasound guidance arm in addition to dynamic ultrasound guidance, and the static ultrasound guidance was significantly faster than dynamic ultrasound guidance. Glasin 2020 was the only study to show a shorter procedure time in the ultrasound guidance arm. We believe that the reason for this was the difference in the time it took to search for a target vein. This study included only participants with obesity irrespective of the difficulty level. In participants with obesity, it is often more difficult to see and palpate veins (Sebbane 2013), and ultrasound guidance would help to find a target vein more quickly. However, puncturing with ultrasound guidance is more complicated than with the landmark method, and the puncture itself would take longer. Therefore, in cases where a target vein is easy to find with the landmark method, the procedure time as a whole will be longer with ultrasound guidance, especially dynamic ultrasound guidance. Of note, this outcome relies largely on a single article, McCarthy 2016. The three studies in it defined difficulty as an inability to see and palpate a target vein, but did not define how much to look for a vein. The difference in procedure time for first‐pass cannulation with the landmark method between difficult and easy participants in the study was under one minute; in other words, even in difficult participants, the extra time to find a target vein was less than a minute. Therefore, the operators did not necessarily have difficulty finding a target vein in the difficult participants in this study. If ultrasound guidance is used in people in whom a target vein is more difficult to find, the benefit of the procedure time would probably increase.
Procedure time for overall cannulation
The certainty of the evidence for the procedure time for overall cannulation was very low in difficult participants. No participants were classed as moderate or easy for this outcome using the original studies' definitions. We downgraded by one level due to risk of bias concerns. One reason for this was incomplete outcome data, with three studies excluding failure cases from the analysis (Kerforne 2012; Pappas 2006; Stein 2009). We also downgraded by two levels for serious heterogeneity, because there was no standardised definition of failure, as with the overall success of cannulation outcome. In addition, another three studies included the time taken when the assigned intervention failed and a different method was used (Bahl 2016; Costantino 2005; Weiner 2013).
Number of cannulation attempts
The certainty of the evidence for the number of cannulation attempts was very low in difficult participants. No participants were classed as moderate or easy for this outcome using the original studies' definitions. We downgraded by one level due to risk of bias concerns. We downgraded one level each for considerable heterogeneity and inconsistency (lack of the same definition of failure or the outcome amongst studies). One study excluded failure cases from the analysis (Pappas 2006). Three studies included the number of cannulation attempts taken when the assigned intervention failed and a different method was used (Bahl 2016; Costantino 2005; Weiner 2013), six studies only analysed the allocated interventions (Aponte 2007; Bridey 2018; Glasin 2020; Pappas 2006; Skulec 2019; Stein 2009), and two studies did not specify details on this (İsmailoğlu 2015; River 2009). However, because ultrasound guidance tended to improve success rates, it is natural that the number of cannulation attempts also decreased. Although River 2009 did not specify a definition, Glasin 2020 and Skulec 2019 used the same definitions of the population and outcome in the moderately difficult participants using the definition of success rate, and ultrasound guidance reduced the number of cannulation attempts with moderate‐certainty evidence (Analysis 6.2). Considering the difficulty‐dependent effect, ultrasound guidance can potentially reduce the number of cannulation attempts even in difficult participants.
Patient satisfaction
The certainty of the evidence for patient satisfaction was very low for difficult participants. No participants were classed as moderate or easy for this outcome using the original studies' definitions. We downgraded by one level each for risk of bias concerns, inconsistency, and imprecision. The risk of bias was high in all the studies, and two studies only included successful cases, with weights accounting for a total of 35% of the results (Bridey 2018; Stein 2009). A quasi‐RCT was the main source of heterogeneity, and when we excluded this study (Costantino 2005), the effect sizes decreased. The number of participants was small for all difficulty levels, and their CIs were wide.
Overall complications
The certainty of the evidence for overall complications was low for difficult participants, and we downgraded by one level each for risk of bias and imprecision. However, the risk of bias was low in five of the nine studies, and the results were similar when studies with a high risk of bias were excluded. The effect sizes in difficult and moderately difficult participants were reasonably consistent, except for Skulec 2019, in which ultrasound guidance reduced complications. The study included pain as a complication, and when we excluded pain, there was no apparent difference, consistent with other studies. The certainty of the evidence for moderately difficult and easy participants was moderate: we downgraded by one level due to imprecision.
Potential biases in the review process
We made every effort to identify and include all eligible studies and to assess them appropriately. The Cochrane Vascular Information Specialist conducted a thorough search to identify eligible studies for the review. Eight studies were potentially eligible, but their results had not been published at the time of the searches. We contacted the investigators and were able to obtain unpublished results owing to the courtesy of the investigators for Glasin 2020. Amongst the seven remaining studies, one was registered in 2014, and it is unclear if it was actually conducted (IRCT201408097751N4). The other six were registered between 2019 and 2021, and results may be available in the future (NCT03745209; NCT03841864; NCT04218643; NCT04853290; NCT04856826; NCT05119985). We will monitor the progress of these studies and include them, if possible, in an update of this review.
We contacted the investigators of the included studies and were able to obtain unpublished outcome results and design details from nine of the 14 articles. Therefore, we believe we managed to conduct comprehensive analyses and clarify the risk of bias assessments.
We analysed data for the number of cannulation attempts using mean values, because seven of the 11 included studies reported mean values, and only one reported median value (Costantino 2005). Following guidance in the Cochrane Handbook for Systematic Reviews of Interventions, we treated the median as the mean (Higgins 2021b). In the remaining three studies, we calculated means from tables and figures (Bridey 2018; Glasin 2020; Stein 2009). We used SMD as an outcome measure of satisfaction because two different measures were used, and four out of six studies reported an NRS of 0 to 10.
Agreements and disagreements with other studies or reviews
The results of this review differed from those of previous reviews in several ways (Egan 2013; Heinrichs 2013; Liu 2014; Stolz 2015; Van Loon 2018). First, the previous reviews included six to eight articles (involving 240 to 1660 participants), and our review included 14 articles (2267 participants). In addition, with the help of the investigators of the studies, we obtained some unpublished results and included them in this current review. Second, in the earlier reviews, three studies included children who were analysed together with adults (Egan 2013; Liu 2014; Stolz 2015). Children should be analysed separately because adults and children have different characteristics, such as the size and depth of a target vein, and adherence during the procedure.
The review by Van Loon 2018 included the largest trial (McCarthy 2016) and was the largest amongst previous meta‐analyses. However, it did not distinguish the difficulty levels of the participants and analysed them together. It is necessary to analyse the effects of ultrasound guidance separately for each difficulty level because ultrasound guidance effects depend on the difficulty level. We separated the difficulty levels of participants in McCarthy 2016 and reported it as three different studies (McCarthy 2016A; McCarthy 2016B; McCarthy 2016C). This issue is important not only for the heterogeneity but also for the selection of appropriate patients for ultrasound guidance. Heinrichs 2013 included only adult difficult participants and the results were similar to those of this review. It included six studies with 242 participants. Each outcome included only one to three studies because Heinrichs and colleagues analysed settings, such as the emergency department, ICU, and operating room, separately. However, the differences in the settings did not have a substantial impact on the effect of ultrasound guidance, and separate analyses may have unnecessarily reduced the sample size.
Authors' conclusions
Implications for practice.
There is very low‐ and low‐certainty evidence that ultrasound guidance may benefit difficult participants compared to the landmark method because of increased first‐pass success and overall cannulation with no difference detected in pain. With the exception of the procedure time for first‐pass cannulation, all the primary and secondary outcomes favoured ultrasound guidance or showed no evidence of a difference, and the results were consistent with both definitions of the difficulty. We believe that the benefits of ultrasound guidance, especially the improvement in the first‐pass success of cannulation, are clinically meaningful. In addition, ultrasound guidance did not clearly increase complications. The difference in the procedure time for first‐pass cannulation was small, less than three minutes. This difference is unlikely to be clinically important unless the patient is in a very urgent condition. Therefore, we are certain that ultrasound guidance had some benefit but no apparent harm to difficult patients except in cases of urgency.
There is low‐ and moderate‐certainty evidence that ultrasound guidance may benefit moderately difficult participants compared to the landmark method because of increased first‐pass success of cannulation with no difference detected in pain. The results were consistent with both definitions of the difficulty. The direction of the effect of ultrasound guidance was similar to that of the difficult participants but to a lesser extent. As in the difficult participants, ultrasound guidance slightly increased the procedure time for first‐pass cannulation, but this is of little clinical significance as discussed above. There were no clear differences in other outcomes, including complications. Therefore, in the absence of obvious harm, ultrasound guidance may be useful in moderately difficult patients.
There is moderate‐ and high‐certainty evidence that ultrasound guidance does not benefit easy participants compared to the landmark method because ultrasound guidance decreased the first‐pass success of cannulation and increased pain. All the outcomes, including the procedure time for first‐pass cannulation and complications, consistently favoured the landmark method or showed no apparent difference with reasonable certainty with both definitions of the difficulty. Therefore, we believe ultrasound guidance should not be used in easy patients.
Although we were unable to demonstrate any apparent effect on training or previous experience in ultrasound guidance, both are clinically important. We consider attempts to maintain and monitor operators' proficiency essential in the clinical application of ultrasound guidance. Combined with a proper scale to assess the difficulty, ultrasound guidance could be used more appropriately.
Implications for research.
The effectiveness of ultrasound guidance depended on the level of participants' difficulty, but the definition of difficulty varied, and this problem undermined the certainty of our results. A reproducible method of difficulty stratification will make the evidence more robust and allow for more appropriate selection of patients for ultrasound guidance.
Because the definition of failure and outcomes were not the same, the results of the overall success of cannulation, procedure time for overall cannulation, and number of cannulation attempts were uncertain. Future studies should use a common, standardised definition of failure for ultrasound guidance and the landmark method. Also, if an allocated intervention fails and another method is used, it is better to prioritise the results of only the allocated intervention. This is because the alternative methods are expected to vary and could be a source of further heterogeneity.
Because of the lack of detailed descriptions, the effect of operators' training and experience on ultrasound guidance was unclear. However, it is clearly a clinically important factor. We will include this issue in a future update if studies which randomise by training programmes or operators' occupation or experience levels are conducted.
Although not included in this review, devices such as midline catheters could be a new option. In a future update, we will evaluate these devices, especially for the duration of functional catheters and cost, if data are available. Differences in needle visibility due to features of ultrasound machines and their effects will also be an important issue to consider.
History
Protocol first published: Issue 9, 2019
Notes
Parts of the Methods section of this review are based on a standard template produced by Cochrane Vascular.
Acknowledgements
We sincerely thank Cochrane Vascular for their support and guidance in the preparation of this review. We are also deeply grateful to the investigators, Amit Bahl, Antoine Kimmoun, Daniel Wilhelms, Hamid Shokoohi, Melissa L McCarthy, Takuya Nishizawa, Thomas G Costantino, Thomas Kerforne, Roman Skulec, and Scott G Weiner, who provided us with unpublished, additional data. Without their generosity, this review would not have been possible.
The review authors, and the Cochrane Vascular Editorial base, are grateful to the following peer reviewers for their time and comments:
Evan Alexandrou RN MPH PhD, Western Sydney University and Liverpool Hospital Australia; Fredericus HJ van Loon PhD CRNA, Fontys University of Applied Sciences and Catharina Hospital, the Netherlands; Prof Dr Caren Randon, Ghent University Hospital, Belgium; Partha Shah MBBS, India.
Appendices
Appendix 1. Sources searched and search strategies
| Source | Search strategy | Hits retrieved |
| 1. VASCULAR REGISTER IN CRSW (Date of most recent search: 29 November 2021) |
#1 Catheterization, Peripheral OR peripheral vein OR peripheral venous OR peripheral intravenous AND INREGISTER #2 ULTRASONOGRAPHY OR Ultrasound AND INREGISTER #3 #1 AND #2 |
Oct 2019: 81 NOV 2020: 33 Nov 2021: 5 |
| 2. CENTRAL via CRSO (Date of most recent search: 29 November 2021) |
#1 MESH DESCRIPTOR Catheterization, Peripheral EXPLODE ALL TREES #2 Cathlon:TI,AB,KY #3 (intravenous cannul*):TI,AB,KY #4 (peripheral intravenous):TI,AB,KY #5 (peripheral vein*):TI,AB,KY #6 (peripheral venous):TI,AB,KY #7 Venflon:TI,AB,KY #8 ((Catheter* or cannula* or puncture* or line or access) near3 (peripher* or intravenous)):TI,AB,KY #9 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 #10 MESH DESCRIPTOR ULTRASONOGRAPHY, INTERVENTIONAL EXPLODE ALL TREES #11 ultrasonograph*:TI,AB,KY #12 Ultrasound*:TI,AB,KY #13 #10 OR #11 OR #12 #14 #9 AND #13 |
Oct 2019: 323 NOV 2020: 77 Nov 2021: 43 |
| 3. Clinicaltrials.gov (Date of most recent search: 29 November 2021) |
Catheterization, Peripheral OR peripheral vein OR peripheral venous OR peripheral intravenous | ULTRASONOGRAPHY OR Ultrasound | Oct 2019: 198 NOV 2020: 43 Nov 2021: 16 |
| 4. ICTRP Search Portal (Date of most recent search: 29 November 2021) |
Catheterization, Peripheral OR peripheral vein OR peripheral venous OR peripheral intravenous | ULTRASONOGRAPHY OR Ultrasound | Oct 2019: 17 NOV 2020: 0 Nov 2021: 2 |
| 5. MEDLINE (Ovid MEDLINE Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE) 1946 to present Date of most recent search: 29 November 2021) | 1 Catheterization, Peripheral/ 2 Cathlon.ti,ab. 3 "intravenous cannul*".ti,ab. 4 "peripheral intravenous".ti,ab. 5 "peripheral vein*".ti,ab. 6 "peripheral venous".ti,ab. 7 Venflon.ti,ab. 8 ((Catheter* or cannula* or puncture* or line or access) adj3 (peripher* or intravenous)).ti,ab. 9 or/1‐8 10 exp ULTRASONOGRAPHY, INTERVENTIONAL/ 11 ultrasonograph*.ti,ab. 12 Ultrasound*.ti,ab. 13 or/10‐12 14 9 and 13 15 randomized controlled trial.pt. 16 controlled clinical trial.pt. 17 randomized.ab. 18 placebo.ab. 19 drug therapy.fs. 20 randomly.ab. 21 trial.ab. 22 groups.ab. 23 or/15‐22 24 exp animals/ not humans.sh. 25 23 not 24 26 14 and 25 |
Oct 2019: 432 NOV 2020: 90 Nov 2021: 96 |
| 6. Embase via OVID (Date of most recent search: 29 November 2021) |
1 exp catheterization/ 2 Cathlon.ti,ab. 3 "intravenous cannul*".ti,ab. 4 "peripheral intravenous".ti,ab. 5 "peripheral vein*".ti,ab. 6 "peripheral venous".ti,ab. 7 Venflon.ti,ab. 8 ((Catheter* or cannula* or puncture* or line or access) adj3 (peripher* or intravenous)).ti,ab. 9 or/1‐8 10 exp interventional ultrasonography/ 11 ultrasonograph*.ti,ab. 12 Ultrasound*.ti,ab. 13 or/10‐12 14 9 and 13 15 randomized controlled trial/ 16 controlled clinical trial/ 17 random$.ti,ab. 18 randomization/ 19 intermethod comparison/ 20 placebo.ti,ab. 21 (compare or compared or comparison).ti. 22 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 23 (open adj label).ti,ab. 24 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 25 double blind procedure/ 26 parallel group$1.ti,ab. 27 (crossover or cross over).ti,ab. 28 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 29 (assigned or allocated).ti,ab. 30 (controlled adj7 (study or design or trial)).ti,ab. 31 (volunteer or volunteers).ti,ab. 32 trial.ti. 33 or/15‐32 34 14 and 33 35 from 34 keep 2001‐2371 |
Oct 2019: 2371 NOV 2020: 406 Nov 2021: 398 |
| 7. CINAHL via EBSCO (Date of most recent search: 29 November 2021) |
S30 S14 AND S29 S29 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 S28 MH "Random Assignment" S27 MH "Triple‐Blind Studies" S26 MH "Double‐Blind Studies" S25 MH "Single‐Blind Studies" S24 MH "Crossover Design" S23 MH "Factorial Design" S22 MH "Placebos" S21 MH "Clinical Trials" S20 TX "multi‐centre study" OR "multi‐center study" OR "multicentre study" OR "multicenter study" OR "multi‐site study" S19 TX crossover OR "cross‐over" S18 AB placebo* S17 TX random* S16 TX trial* S15 TX "latin square" S14 S9 AND S13 S13 S10 OR S11 OR S12 S12 TX Ultrasound* S11 TX ultrasonograph* S10 (MH "Ultrasonography+") S9 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 S8 TX (Catheter* or cannula* or puncture* or line or access) N3 (peripher* or intravenous) S7 TX Venflon S6 TX peripheral venous S5 TX peripheral vein* S4 TX peripheral intravenous S3 TX intravenous cannul* S2 TX Cathlon S1 (MH "Catheterization, Peripheral+") |
Oct 2019: 163 NOV 2020: 48 Nov 2021: 42 |
| 8. LILACS (Date of most recent search: 29 November 2021) |
Catheterization, Peripheral OR peripheral vein OR peripheral venous OR peripheral intravenous OR Cateterización [Palavras] and ULTRASONOGRAPHY OR Ultrasound or Sonografía OR Ultrasonido [Palavras] | Oct 2019: 53 NOV 2020: 5 Nov 2021: 1 |
| TOTAL before de‐duplication | Oct 2019: 3638 Nov 2020: 702 Nov 2021: 603 |
|
| TOTAL after de‐duplication | Oct 2019: 2966 Nov 2020: 571 Nov 2021: 501 |
|
Appendix 2. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults classed as difficult – subgrouped by operators' experience
|
Patient or population: adults undergoing peripheral venous cannulation classed as difficulta Settings: emergency department, ICU, operating room Intervention: USG Comparison: LM | |||||||
| Outcomes | Subgroups | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with LM | Risk with USG | ||||||
|
First‐pass success of cannulation Follow‐up: immediately after the procedure |
Operators had any clinical experience | 361 per 1000 | 519 per 1000 (328 to 819) | RR 1.44 (0.91 to 2.27) | 460 (5 RCTs) |
⊕⊝⊝⊝ Very lowb | |
| Operators did not have any clinical experience | 446 per 1000 |
594 per 1000 (442 to 799) |
RR 1.33 (0.99 to 1.79) | 235 (3 RCTs) |
⊕⊕⊝⊝ Lowc | ||
| Operators experience was not specified | 183 per 1000 |
403 per 1000 (224 to 726) |
RR 2.20 (1.22 to 3.96) | 120 (2 RCTs) |
⊕⊕⊝⊝ Lowd | ||
|
Overall success of cannulation Follow‐up: immediately after the procedure |
Operators had any clinical experience | 726 per 1000 | 835 per 1000 (661 to 1000) | RR 1.15 (0.91 to 1.44) | 315 (5 RCTs) |
⊕⊝⊝⊝ Very lowe | |
| Operators did not have any clinical experience | 509 per 1000 | 743 per 1000 (601 to 911) | RR 1.46 (1.18 to 1.79) | 235 (3 RCTs) |
⊕⊝⊝⊝ Very lowf | ||
| Operators experience was not specified | 333 per 1000 | 693 per 1000 (470 to 1000) | RR 2.08 (1.41 to 3.09) | 120 (2 RCTs) |
⊕⊝⊝⊝ Very lowg | ||
|
Pain NRS: from 0, no pain to 10, maximum pain Follow‐up: immediately after the procedure |
Operators had any clinical experience | Not performed due to insufficient number of studies | |||||
| Operators did not have any clinical experience | Not performed due to insufficient number of studies | ||||||
| Operators experience was not specified | Not performed due to insufficient number of studies | ||||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; ICU: intensive care unit; LM: landmark method; MD: mean difference; NRS: numerical rating scale; RCTs: randomised controlled trials; RR: risk ratio; USG: ultrasound guidance | |||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aParticipants were classified according to the original study's definition. bWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors), considerable inconsistency, and imprecision. cWe downgraded by a total of two levels to low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), and imprecision. dWe downgraded by a total of two levels to low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors), and imprecision. eWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors), considerable inconsistency, and imprecision. fWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), considerable inconsistency, and imprecision. gWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors), considerable inconsistency, and imprecision.
Appendix 3. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults classed as difficult – subgrouped by settings
|
Patient or population: adults undergoing peripheral venous cannulation classed as difficulta Settings: emergency department, ICU, operating room Intervention: USG Comparison: LM | |||||||
| Outcomes | Subgroups | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with LM | Risk with USG | ||||||
|
First‐pass success of cannulation Follow‐up: immediately after the procedure |
Emergency department | 345 per 1000 | 552 per 1000 (386 to 787) | RR 1.60 (1.12 to 2.28) | 546 (6 RCTs) |
⊕⊝⊝⊝ Very lowb | |
| ICU | 325 per 1000 | 533 per 1000 (390 to 724) | RR 1.64 (1.20 to 2.23) | 234 (3 RCTs) |
⊕⊕⊝⊝ Lowc | ||
| Operating room | 813 per 1000 | 739 per 1000 (512 to 1000) | RR 0.91 (0.63 to 1.30) | 35 (1 RCT) |
⊕⊕⊝⊝ Lowc | ||
|
Overall success of cannulation Follow‐up: immediately after the procedure |
Emergency department | 557 per 1000 | 874 per 1000 (585 to 1000) | RR 1.57 (1.05 to 2.36) | 401 (6 RCTs) |
⊕⊝⊝⊝ Very lowd | |
| ICU | 547 per 1000 | 744 per 1000 (470 to 1000) | RR 1.36 (0.86 to 2.15) | 234 (3 RCTs) |
⊕⊝⊝⊝ Very lowe | ||
| Operating room | 1000 per 1000 | 1000 per 1000 (900 to 1000) | RR 1.00 (0.90 to 1.11) | 35 (1 RCT) |
⊕⊕⊝⊝ Lowc | ||
|
Pain NRS: from 0, no pain to 10, maximum pain Follow‐up: immediately after the procedure |
Emergency department | The mean pain score was 4.0 | MD 0.2 lower (1.13 lower to 0.72 higher) | ‐ | 323 (4 RCTs) | ⊕⊝⊝⊝ Very lowf | |
| ICU | No eligible studies | ||||||
| Operating room | No eligible studies | ||||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; ICU: intensive care unit; LM: landmark method; MD: mean difference; NRS: numerical rating scale; RCTs: randomised controlled trials; RR: risk ratio; USG: ultrasound guidance | |||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aParticipants were classified according to the original study's definition. bWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors), substantial inconsistency, and imprecision. cWe downgraded by a total of two levels to low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), and imprecision. dWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors), serious inconsistency, and imprecision. eWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), serious inconsistency, and imprecision. fWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (a quasi‐randomised trial, lack of blinding of the outcome assessors, incomplete outcome data), substantial inconsistency, and imprecision.
Appendix 4. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults classed as difficult – classified according to the success rate with landmark method
|
Patient or population: adults undergoing peripheral venous cannulation classed as difficulta Settings: emergency department, ICU Intervention: USG Comparison: LM | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with LM | Risk with USG | |||||
|
First‐pass success of cannulation Follow‐up: immediately after the procedure |
339 per 1000 | 549 per 1000 (433 to 698) | RR 1.62 (1.28 to 2.06) | 780 (9 RCTs) | ⊕⊕⊕⊝
Moderateb |
|
|
Overall success of cannulation Follow‐up: immediately after the procedure |
541 per 1000 | 828 per 1000 (606 to 1000) | RR 1.53 (1.12 to 2.08) | 588 (8 RCTs) | ⊕⊝⊝⊝
Very lowc |
|
|
Pain NRS: from 0, no pain to 10, maximum pain Follow‐up: immediately after the procedure |
The mean pain score was 4.07 | MD 0.49 lower (1.48 lower to 0.49 higher) | ‐ | 305 (3 RCTs) | ⊕⊝⊝⊝ Very lowd | |
|
Procedure time for first‐pass cannulation (seconds) Follow‐up: immediately after the procedure |
The mean procedure time for first‐pass cannulation was 137.8 seconds | MD 120.6 seconds longer (88.3 longer to 152.9 longer) | ‐ | 192 (1 RCT) | ⊕⊕⊕⊝
Moderatee |
|
|
Number of cannulation attempts Follow‐up: immediately after the procedure |
The mean number of cannulation attempts was 2.20 | MD 0.36 lower (0.75 lower to 0.03 higher) | ‐ | 468 (6 RCTs) | ⊕⊝⊝⊝ Very lowf | |
|
Patient satisfaction NRS from 0 to 10 or 4‐step Likert scale The higher the score, the higher the level of satisfaction Follow‐up: immediately after the procedure |
The mean patient satisfaction score was 5.96 | SMD 0.52 higher (0.01 lower to 1.05 higher) | ‐ | 286 (4 RCTs) | ⊕⊝⊝⊝ Very lowg | |
|
Overall complications Follow‐up: immediately after the procedure |
121 per 1000 | 78 per 1000 (45 to 133) | RR 0.64 (0.37 to 1.10) | 431 (5 RCTs) | ⊕⊕⊝⊝ Lowh | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; ICU: intensive care unit; LM: landmark method; MD: mean difference; NRS: numeric rating scale; RCTs: randomised controlled trials; RR: risk ratio; SMD: standardised mean difference; USG: ultrasound guidance | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aParticipants were classified according to the success rate with LM. bWe downgraded one level to moderate certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors). cWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors), serious inconsistency due to the lack of standardised definition of failure, and imprecision. dWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors), inconsistency, and imprecision. eWe downgraded one level to moderate certainty due to imprecision. fWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors), serious inconsistency due to the lack of standardised definition of failure, and imprecision. gWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors, incomplete outcome data), inconsistency, and imprecision. hWe downgraded by a total of two levels to low certainty due to risk of bias concerns (quasi‐randomised trials, lack of blinding of the outcome assessors), and imprecision.
Appendix 5. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults classed as moderately difficult – classified according to the success rate with landmark method
|
Patient or population: adults undergoing peripheral venous cannulation classed as moderately difficulta Settings: emergency department, prehospital setting Intervention: USG Comparison: LM | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with LM | Risk with USG | |||||
|
First‐pass success of cannulation Follow‐up: immediately after the procedure |
733 per 1000 | 857 per 1000 (798 to 923) | RR 1.17 (1.09 to 1.26) | 791 (3 RCTs) | ⊕⊕⊕⊕
High |
|
|
Overall success of cannulation Follow‐up: immediately after the procedure |
904 per 1000 | 967 per 1000 (849 to 1000) | RR 1.07 (0.94 to 1.23) | 436 (3 RCTs) | ⊕⊝⊝⊝
Very lowb |
|
|
Pain NRS: from 0, no pain, to 10, maximum pain Follow‐up: immediately after the procedure |
The mean pain score was 2.96 | MD 0.03 higher (0.43 lower to 0.48 higher) | ‐ | 491 (2 RCTs) | ⊕⊕⊝⊝ Lowc | |
|
Procedure time for first‐pass cannulation (seconds) Follow‐up: immediately after the procedure |
The mean procedure time for first‐pass cannulation was 100.6 seconds | MD 23.0 seconds longer (39.9 shorter to 85.9 longer) | ‐ | 749 (3 RCTs) | ⊕⊝⊝⊝
Very lowd |
|
|
Number of cannulation attempts Follow‐up: immediately after the procedure |
The mean number of cannulation attempts was 1.51 | MD 0.32 lower (0.47 lower to 0.16 lower) | ‐ | 437 (3 RCTs) | ⊕⊕⊕⊝ Moderatee | |
|
Patient satisfaction NRS from 0 to 10 or 4‐step Likert scale The higher the score the higher the level of satisfaction Follow‐up: immediately after the procedure |
The mean patient satisfaction score was 7.63 | SMD 0.08 higher (0.51 lower to 0.66 higher) | ‐ | 137 (2 RCTs) | ⊕⊝⊝⊝ Very lowf | |
|
Overall complications Follow‐up: immediately after the procedure |
131 per 1000 | 76 per 1000 (43 to 133) | RR 0.58 (0.33 to 1.02) | 791 (3 RCTs) | ⊕⊕⊝⊝ Lowg | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; LM: landmark method; MD: mean difference; NRS: numeric rating scale; RCTs: randomised controlled trials; RR: risk ratio; USG: ultrasound guidance | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aParticipants were classified according to the success rate with LM. bWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), serious inconsistency due to the lack of standardised definition of failure, and imprecision. cWe downgraded by a total of two levels to low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), and imprecision. dWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (incomplete outcome data), inconsistency, and imprecision. eWe downgraded one level to moderate certainty due to risk of bias concerns (lack of blinding of the outcome assessors). fWe downgraded by a total of three levels to very low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), inconsistency, and imprecision. gWe downgraded by a total of two levels to low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), and imprecision.
Appendix 6. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults classed as easy – classified according to the success rate with landmark method
|
Patient or population: adults undergoing peripheral venous cannulation classed as easya Settings: emergency department, operating room Intervention: USG Comparison: LM | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with LM | Risk with USG | |||||
|
First‐pass success of cannulation Follow‐up: immediately after the procedure |
958 per 1000 | 852 per 1000 (814 to 900) | RR 0.89 (0.85 to 0.94) | 631 (2 RCTs) | ⊕⊕⊕⊝ Moderateb |
|
|
Overall success of cannulation Follow‐up: immediately after the procedure |
1000 per 1000 | 1000 per 1000 (900 to 1000) | RR 1.00 (0.90 to 1.11) | 35 (1 RCT) | ⊕⊕⊝⊝ Lowc |
|
|
Pain NRS: from 0, no pain, to 10, maximum pain Follow‐up: immediately after the procedure |
The mean pain score was 2.30 | MD 0.60 higher (0.17 higher to 1.03 higher) | ‐ | 596 (1 RCT) | ⊕⊕⊕⊝ Moderated | |
|
Procedure time for first‐pass cannulation (seconds) Follow‐up: immediately after the procedure |
The mean procedure time for first‐pass cannulation was 89.2 seconds | MD 95.0 seconds longer (81.4 longer to 108.6 longer) | ‐ | 623 (2 RCTs) | ⊕⊕⊕⊝
Moderatee |
|
|
Number of cannulation attempts Follow‐up: immediately after the procedure |
The mean number of cannulation attempts was 1.30 | MD 0.10 higher (0.44 lower to 0.64 higher) | ‐ | 35 (1 RCT) | ⊕⊕⊝⊝ Lowf | |
|
Patient satisfaction NRS from 0 to 10 or 4‐step Likert scale The higher the score, the higher the level of satisfaction Follow‐up: immediately after the procedure |
See comment | ‐ | ‐ | ‐ | ‐ | None of the studies included easy participants |
|
Overall complications Follow‐up: immediately after the procedure |
17 per 1000 | 43 per 1000 (15 to 118) | RR 2.48 (0.90 to 6.87) | 596 (1 RCT) | ⊕⊕⊕⊝ Moderateg | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; LM: landmark method; NRS: numeric rating scale; RCTs: randomised controlled trials; RR: risk ratio; USG: ultrasound guidance | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aParticipants were classified according to the success rate with LM. bWe downgraded one level to moderate certainty due to risk of bias concerns (lack of blinding of the outcome assessors). cWe downgraded by a total of two levels to low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), and imprecision. dWe downgraded one level to moderate certainty due to risk of bias concerns (lack of blinding of the outcome assessors). eWe downgraded by a total of one level to moderate certainty due to risk of bias concerns (lack of blinding of the outcome assessors, incomplete outcome data). fWe downgraded by a total of two levels to low certainty due to risk of bias concerns (lack of blinding of the outcome assessors), and imprecision. gWe downgraded one level to moderate certainty due to imprecision.
Data and analyses
Comparison 1. First‐pass success of cannulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Difficulty levels defined by original studies | 14 | 2202 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.08, 1.59] |
| 1.1.1 Difficult | 10 | 815 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [1.15, 1.95] |
| 1.1.2 Moderate | 1 | 401 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.02, 1.27] |
| 1.1.3 Easy | 1 | 596 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.85, 0.94] |
| 1.1.4 No restriction by intravenous access difficulty level | 2 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.09, 1.33] |
| 1.2 Difficulty levels defined by the success rate with landmark method | 14 | 2202 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.08, 1.59] |
| 1.2.1 Difficult | 9 | 780 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [1.28, 2.06] |
| 1.2.2 Moderate | 3 | 791 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.09, 1.26] |
| 1.2.3 Easy | 2 | 631 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.85, 0.94] |
| 1.3 Operators could not see and palpate a target vein | 5 | 486 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.53, 2.45] |
| 1.4 Participants had a history of difficult intravenous access | 6 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.97, 1.70] |
| 1.5 Participants had multiple failed attempts | 4 | 232 | Risk Ratio (M‐H, Random, 95% CI) | 1.60 [1.15, 2.21] |
| 1.6 Operators finished any training program for ultrasound‐guided peripheral venous cannulation | 10 | 815 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [1.15, 1.95] |
| 1.6.1 Finished | 9 | 755 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [1.09, 1.91] |
| 1.6.2 Not specified | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 2.25 [1.16, 4.36] |
| 1.7 Operators had any clinical experience with ultrasound‐guided peripheral intravenous cannulation | 10 | 815 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [1.15, 1.95] |
| 1.7.1 Had any clinical experience | 5 | 460 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.91, 2.27] |
| 1.7.2 Did not have any clinical experience | 3 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.99, 1.79] |
| 1.7.3 Not specified | 2 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 2.20 [1.22, 3.96] |
| 1.8 Operators finished any training program for ultrasound‐guided peripheral venous cannulation plus any clinical experience | 10 | 815 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [1.15, 1.95] |
| 1.8.1 Finished any training program for ultrasound‐guided peripheral venous cannulation plus any clinical experience | 5 | 460 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.91, 2.27] |
| 1.8.2 Not finished any training program for ultrasound‐guided peripheral venous cannulation or no clinical experience | 3 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.99, 1.79] |
| 1.8.3 Not specified | 2 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 2.20 [1.22, 3.96] |
| 1.9 Types of operators | 10 | 815 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [1.15, 1.95] |
| 1.9.1 Nurses | 7 | 504 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.03, 1.71] |
| 1.9.2 Physicians | 2 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [0.86, 2.50] |
| 1.9.3 Technicians | 1 | 192 | Risk Ratio (M‐H, Random, 95% CI) | 2.33 [1.74, 3.11] |
| 1.10 Setting | 10 | 815 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [1.15, 1.95] |
| 1.10.1 Emergency department | 6 | 546 | Risk Ratio (M‐H, Random, 95% CI) | 1.60 [1.12, 2.28] |
| 1.10.2 ICU | 3 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [1.20, 2.23] |
| 1.10.3 Operating room | 1 | 35 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.63, 1.30] |
| 1.11 Year of publication | 10 | 815 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [1.15, 1.95] |
| 1.11.1 Publication year: 1999 ~ 2008 | 2 | 95 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.51, 3.02] |
| 1.11.2 Publication year: 2009 ~ | 8 | 720 | Risk Ratio (M‐H, Random, 95% CI) | 1.60 [1.24, 2.07] |
| 1.12 Dynamic guidance or static guidance | 1 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.06, 1.35] |
| 1.12.1 Dynamic | 1 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.98, 1.37] |
| 1.12.2 Static | 1 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.05, 1.46] |
Comparison 2. Overall success of cannulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Difficulty levels defined by original studies | 12 | 1059 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [1.08, 1.49] |
| 2.1.1 Difficult | 10 | 670 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.10, 1.77] |
| 2.1.2 No restriction by intravenous access difficulty level | 2 | 389 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.92, 1.19] |
| 2.2 Difficulty levels defined by the success rate with landmark method | 12 | 1059 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [1.08, 1.49] |
| 2.2.1 Difficult | 8 | 588 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [1.12, 2.08] |
| 2.2.2 Moderate | 3 | 436 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.94, 1.23] |
| 2.2.3 Easy | 1 | 35 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.90, 1.11] |
| 2.3 Operators could not see and palpate a target vein | 4 | 294 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [0.98, 2.41] |
| 2.4 Participants had a history of difficult intravenous access | 6 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 1.66 [0.97, 2.86] |
| 2.5 Participants had multiple failed attempts | 5 | 279 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [0.93, 2.51] |
| 2.6 Operators finished any training program for ultrasound‐guided peripheral venous cannulation | 10 | 670 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.10, 1.77] |
| 2.6.1 Finished | 9 | 610 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [1.06, 1.71] |
| 2.6.2 Not specified | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [1.13, 3.23] |
| 2.7 Operators had any clinical experience with ultrasound‐guided peripheral intravenous cannulation | 10 | 670 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.10, 1.77] |
| 2.7.1 Had any clinical experience | 5 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.91, 1.44] |
| 2.7.2 Did not have any clinical experience | 3 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [1.18, 1.79] |
| 2.7.3 Not specified | 2 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [1.41, 3.09] |
| 2.8 Operators finished any training program for ultrasound‐guided peripheral venous cannulation and had any clinical experience | 10 | 670 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.10, 1.77] |
| 2.8.1 Finished any training program for ultrasound‐guided peripheral venous cannulation and had any clinical experience | 5 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.91, 1.44] |
| 2.8.2 Not finished any training program for ultrasound‐guided peripheral venous cannulation or no clinical experience | 3 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [1.18, 1.79] |
| 2.8.3 Not specified | 2 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [1.41, 3.09] |
| 2.9 Types of operators | 10 | 670 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.10, 1.77] |
| 2.9.1 Nurses | 8 | 551 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [1.05, 1.78] |
| 2.9.2 Physicians | 2 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 1.72 [0.22, 13.47] |
| 2.10 Setting | 10 | 670 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.10, 1.77] |
| 2.10.1 Emergency department | 6 | 401 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [1.05, 2.36] |
| 2.10.2 ICU | 3 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.86, 2.15] |
| 2.10.3 Operating room | 1 | 35 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.90, 1.11] |
| 2.11 Year of publication | 10 | 670 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.10, 1.77] |
| 2.11.1 Publication year: 1999 ~ 2008 | 2 | 95 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [0.10, 29.24] |
| 2.11.2 Publication year: 2009 ~ | 8 | 575 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [1.08, 1.71] |
| 2.12 Dynamic guidance or static guidance | 1 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.03, 1.18] |
| 2.12.1 Dynamic | 1 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.00, 1.21] |
| 2.12.2 Static | 1 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.00, 1.21] |
Comparison 3. Pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Difficulty levels defined by original studies | 7 | 1410 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.42, 0.51] |
| 3.1.1 Difficult | 4 | 323 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.13, 0.72] |
| 3.1.2 Moderate | 1 | 401 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.47, 0.67] |
| 3.1.3 Easy | 1 | 596 | Mean Difference (IV, Random, 95% CI) | 0.60 [0.17, 1.03] |
| 3.1.4 No restriction by intravenous access difficulty level | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.85, 0.65] |
| 3.2 Difficulty levels defined by the success rate with landmark method | 7 | 1410 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.42, 0.51] |
| 3.2.1 Difficult | 3 | 305 | Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.48, 0.49] |
| 3.2.2 Moderate | 2 | 491 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.43, 0.48] |
| 3.2.3 Easy | 1 | 596 | Mean Difference (IV, Random, 95% CI) | 0.60 [0.17, 1.03] |
| 3.2.4 No results on both first‐pass and overall success of cannulation | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐0.52, 2.32] |
| 3.3 Operators finished any training program for ultrasound‐guided peripheral venous cannulation | 4 | 323 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.13, 0.72] |
| 3.3.1 Finished | 3 | 305 | Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.48, 0.49] |
| 3.3.2 Not specified | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐0.52, 2.32] |
| 3.4 Types of operators | 4 | 323 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.13, 0.72] |
| 3.4.1 Nurses | 3 | 131 | Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐1.68, 0.95] |
| 3.4.2 Technicians | 1 | 192 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.61, 1.01] |
| 3.5 Setting | 4 | 323 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.13, 0.72] |
| 3.5.1 Emergency department | 4 | 323 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.13, 0.72] |
| 3.6 Year of publication | 4 | 323 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.13, 0.72] |
| 3.6.1 Publication year: 1999 ~ 2008 | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐0.52, 2.32] |
| 3.6.2 Publication year: 2009 ~ | 3 | 305 | Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.48, 0.49] |
Comparison 4. Procedure time for first‐pass cannulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Difficulty levels defined by original studies | 6 | 1564 | Mean Difference (IV, Random, 95% CI) | 61.44 [10.40, 112.49] |
| 4.1.1 Difficult | 2 | 219 | Mean Difference (IV, Random, 95% CI) | 119.85 [88.64, 151.05] |
| 4.1.2 Moderate | 1 | 401 | Mean Difference (IV, Random, 95% CI) | 95.20 [72.77, 117.63] |
| 4.1.3 Easy | 1 | 596 | Mean Difference (IV, Random, 95% CI) | 94.80 [81.15, 108.45] |
| 4.1.4 No restriction by intravenous access difficulty level | 2 | 348 | Mean Difference (IV, Random, 95% CI) | ‐11.31 [‐58.36, 35.74] |
| 4.2 Difficulty levels defined by the success rate with the landmark method | 6 | 1564 | Mean Difference (IV, Random, 95% CI) | 61.44 [10.40, 112.49] |
| 4.2.1 Difficult | 1 | 192 | Mean Difference (IV, Random, 95% CI) | 120.60 [88.30, 152.90] |
| 4.2.2 Moderate | 3 | 749 | Mean Difference (IV, Random, 95% CI) | 23.01 [‐39.89, 85.92] |
| 4.2.3 Easy | 2 | 623 | Mean Difference (IV, Random, 95% CI) | 94.98 [81.42, 108.55] |
Comparison 5. Procedure time for overall cannulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Difficulty levels defined by original studies | 10 | 803 | Mean Difference (IV, Random, 95% CI) | ‐61.14 [‐161.33, 39.06] |
| 5.1.1 Difficult | 8 | 413 | Mean Difference (IV, Random, 95% CI) | ‐24.92 [‐323.09, 273.25] |
| 5.1.2 No restriction by intravenous access difficulty level | 2 | 390 | Mean Difference (IV, Random, 95% CI) | ‐77.42 [‐185.70, 30.86] |
| 5.2 Difficulty levels defined by the success rate with the landmark method | 10 | 803 | Mean Difference (IV, Random, 95% CI) | ‐61.14 [‐161.33, 39.06] |
| 5.2.1 Difficult | 5 | 322 | Mean Difference (IV, Random, 95% CI) | ‐116.99 [‐662.82, 428.83] |
| 5.2.2 Moderate | 3 | 428 | Mean Difference (IV, Random, 95% CI) | ‐69.79 [‐176.18, 36.61] |
| 5.2.3 Easy | 1 | 35 | Mean Difference (IV, Random, 95% CI) | 131.60 [‐39.84, 303.04] |
| 5.2.4 No data of the success rate | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 156.00 [‐450.08, 762.08] |
Comparison 6. Number of cannulation attempts.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Difficulty levels defined by original studies | 11 | 958 | Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.49, ‐0.09] |
| 6.1.1 Difficult | 9 | 568 | Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.64, ‐0.02] |
| 6.1.2 No restriction by intravenous access difficulty level | 2 | 390 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.50, ‐0.11] |
| 6.2 Difficulty levels defined by the success rate with the landmark method | 11 | 958 | Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.49, ‐0.09] |
| 6.2.1 Difficult | 6 | 468 | Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.75, 0.03] |
| 6.2.2 Moderate | 3 | 437 | Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.47, ‐0.16] |
| 6.2.3 Easy | 1 | 35 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.44, 0.64] |
| 6.2.4 No data of the success rate | 1 | 18 | Mean Difference (IV, Random, 95% CI) | ‐1.50 [‐3.50, 0.50] |
Comparison 7. Patient satisfaction.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Difficulty levels defined by original studies | 6 | 423 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.03, 0.77] |
| 7.1.1 Difficult | 5 | 333 | Std. Mean Difference (IV, Random, 95% CI) | 0.49 [0.07, 0.92] |
| 7.1.2 No restriction by intravenous access difficulty level | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.60, 0.23] |
| 7.2 Difficulty levels defined by the success rate with the landmark method | 6 | 423 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.03, 0.77] |
| 7.2.1 Difficult | 4 | 286 | Std. Mean Difference (IV, Random, 95% CI) | 0.52 [‐0.01, 1.05] |
| 7.2.2 Moderate | 2 | 137 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.51, 0.66] |
Comparison 8. Overall complications.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Difficulty levels defined by original studies | 9 | 1818 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.46, 1.14] |
| 8.1.1 Difficult | 5 | 431 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.37, 1.10] |
| 8.1.2 Moderate | 1 | 401 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.38, 1.82] |
| 8.1.3 Easy | 1 | 596 | Risk Ratio (M‐H, Random, 95% CI) | 2.48 [0.90, 6.87] |
| 8.1.4 No restriction by intravenous access difficulty level | 2 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.24, 0.96] |
| 8.2 Difficulty levels defined by the success rate with the landmark method | 9 | 1818 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.46, 1.14] |
| 8.2.1 Difficult | 5 | 431 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.37, 1.10] |
| 8.2.2 Moderate | 3 | 791 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.33, 1.02] |
| 8.2.3 Easy | 1 | 596 | Risk Ratio (M‐H, Random, 95% CI) | 2.48 [0.90, 6.87] |
Comparison 9. Sensitivity analyses 1 (RCTs only).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 First‐pass success of cannulation | 12 | 2082 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.07, 1.59] |
| 9.1.1 Difficult | 8 | 695 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [1.15, 1.96] |
| 9.1.2 Moderate | 1 | 401 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.02, 1.27] |
| 9.1.3 Easy | 1 | 596 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.85, 0.94] |
| 9.1.4 No restriction by intravenous access difficulty level | 2 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.09, 1.33] |
| 9.2 Overall success of cannulation | 8 | 728 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [1.00, 1.27] |
| 9.2.1 Difficult | 7 | 428 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.98, 1.45] |
| 9.2.2 No restriction by intravenous access difficulty level | 1 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.03, 1.18] |
| 9.3 Pain | 5 | 1260 | Mean Difference (IV, Random, 95% CI) | 0.38 [0.08, 0.68] |
| 9.3.1 Difficult | 3 | 263 | Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.42, 0.88] |
| 9.3.2 Moderate | 1 | 401 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.47, 0.67] |
| 9.3.3 Easy | 1 | 596 | Mean Difference (IV, Random, 95% CI) | 0.60 [0.17, 1.03] |
| 9.4 Procedure time for first‐pass cannulation | 6 | 1564 | Mean Difference (IV, Random, 95% CI) | 61.44 [10.40, 112.49] |
| 9.4.1 Difficult | 2 | 219 | Mean Difference (IV, Random, 95% CI) | 119.85 [88.64, 151.05] |
| 9.4.2 Moderate | 1 | 401 | Mean Difference (IV, Random, 95% CI) | 95.20 [72.77, 117.63] |
| 9.4.3 Easy | 1 | 596 | Mean Difference (IV, Random, 95% CI) | 94.80 [81.15, 108.45] |
| 9.4.4 No restriction by intravenous access difficulty level | 2 | 348 | Mean Difference (IV, Random, 95% CI) | ‐11.31 [‐58.36, 35.74] |
| 9.5 Procedure time for overall cannulation | 9 | 743 | Mean Difference (IV, Random, 95% CI) | ‐14.82 [‐100.35, 70.72] |
| 9.5.1 Difficult | 7 | 353 | Mean Difference (IV, Random, 95% CI) | 97.47 [‐17.58, 212.52] |
| 9.5.2 No restriction by intravenous access difficulty level | 2 | 390 | Mean Difference (IV, Random, 95% CI) | ‐77.42 [‐185.70, 30.86] |
| 9.6 Number of cannulation attempts | 8 | 748 | Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.43, ‐0.15] |
| 9.6.1 Difficult | 7 | 448 | Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.36, 0.03] |
| 9.6.2 No restriction by intravenous access difficulty level | 1 | 300 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.59, ‐0.21] |
| 9.7 Patient satisfaction | 5 | 363 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.10, 0.44] |
| 9.7.1 Difficult | 4 | 273 | Std. Mean Difference (IV, Random, 95% CI) | 0.25 [0.01, 0.50] |
| 9.7.2 No restriction by intravenous access difficulty level | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.60, 0.23] |
| 9.8 Overall complications | 7 | 1698 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.45, 1.43] |
| 9.8.1 Difficult | 3 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.29, 1.96] |
| 9.8.2 Moderate | 1 | 401 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.38, 1.82] |
| 9.8.3 Easy | 1 | 596 | Risk Ratio (M‐H, Random, 95% CI) | 2.48 [0.90, 6.87] |
| 9.8.4 No restriction by intravenous access difficulty level | 2 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.24, 0.96] |
9.2. Analysis.

Comparison 9: Sensitivity analyses 1 (RCTs only), Outcome 2: Overall success of cannulation
9.3. Analysis.

Comparison 9: Sensitivity analyses 1 (RCTs only), Outcome 3: Pain
9.4. Analysis.

Comparison 9: Sensitivity analyses 1 (RCTs only), Outcome 4: Procedure time for first‐pass cannulation
9.5. Analysis.

Comparison 9: Sensitivity analyses 1 (RCTs only), Outcome 5: Procedure time for overall cannulation
9.6. Analysis.

Comparison 9: Sensitivity analyses 1 (RCTs only), Outcome 6: Number of cannulation attempts
9.7. Analysis.

Comparison 9: Sensitivity analyses 1 (RCTs only), Outcome 7: Patient satisfaction
Comparison 10. Sensitivity analysis 2 (low risk of bias studies only).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 First‐pass success of cannulation | 6 | 1638 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.97, 1.59] |
| 10.1.1 Difficult | 2 | 251 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.98, 3.37] |
| 10.1.2 Moderate | 1 | 401 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.02, 1.27] |
| 10.1.3 Easy | 1 | 596 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.85, 0.94] |
| 10.1.4 No restriction by intravenous access difficulty level | 2 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.09, 1.33] |
| 10.2 Overall success of cannulation | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.96, 1.05] |
| 10.2.1 Difficult | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.92, 1.16] |
| 10.2.2 No restriction by intravenous access difficulty level | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.96, 1.04] |
| 10.3 Pain | 4 | 1279 | Mean Difference (IV, Random, 95% CI) | 0.29 [‐0.03, 0.61] |
| 10.3.1 Difficult | 1 | 192 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.61, 1.01] |
| 10.3.2 Moderate | 1 | 401 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.47, 0.67] |
| 10.3.3 Easy | 1 | 596 | Mean Difference (IV, Random, 95% CI) | 0.60 [0.17, 1.03] |
| 10.3.4 No restriction by intravenous access difficulty level | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.85, 0.65] |
| 10.4 Procedure time for first‐pass cannulation | 4 | 1279 | Mean Difference (IV, Random, 95% CI) | 69.47 [19.15, 119.78] |
| 10.4.1 Difficult | 1 | 192 | Mean Difference (IV, Random, 95% CI) | 120.60 [88.30, 152.90] |
| 10.4.2 Moderate | 1 | 401 | Mean Difference (IV, Random, 95% CI) | 95.20 [72.77, 117.63] |
| 10.4.3 Easy | 1 | 596 | Mean Difference (IV, Random, 95% CI) | 94.80 [81.15, 108.45] |
| 10.4.4 No restriction by intravenous access difficulty level | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐39.00 [‐75.04, ‐2.96] |
| 10.5 Procedure time for overall cannulation | 2 | 390 | Mean Difference (IV, Random, 95% CI) | ‐77.42 [‐185.70, 30.86] |
| 10.5.1 No restriction by intravenous access difficulty level | 2 | 390 | Mean Difference (IV, Random, 95% CI) | ‐77.42 [‐185.70, 30.86] |
| 10.6 Number of cannulation attempts | 3 | 449 | Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.47, ‐0.15] |
| 10.6.1 Difficult | 1 | 59 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.51, 0.31] |
| 10.6.2 No restriction by intravenous access difficulty level | 2 | 390 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.50, ‐0.11] |
| 10.7 Overall complications | 5 | 1338 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.62, 1.85] |
| 10.7.1 Difficult | 2 | 251 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.21, 2.77] |
| 10.7.2 Moderate | 1 | 401 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.38, 1.82] |
| 10.7.3 Easy | 1 | 596 | Risk Ratio (M‐H, Random, 95% CI) | 2.48 [0.90, 6.87] |
| 10.7.4 No restriction by intravenous access difficulty level | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.27, 2.54] |
10.2. Analysis.

Comparison 10: Sensitivity analysis 2 (low risk of bias studies only), Outcome 2: Overall success of cannulation
10.3. Analysis.

Comparison 10: Sensitivity analysis 2 (low risk of bias studies only), Outcome 3: Pain
10.4. Analysis.

Comparison 10: Sensitivity analysis 2 (low risk of bias studies only), Outcome 4: Procedure time for first‐pass cannulation
10.5. Analysis.

Comparison 10: Sensitivity analysis 2 (low risk of bias studies only), Outcome 5: Procedure time for overall cannulation
10.6. Analysis.

Comparison 10: Sensitivity analysis 2 (low risk of bias studies only), Outcome 6: Number of cannulation attempts
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aponte 2007.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: operating room Number of participants: 35 (USG 19, LM 16) Age, mean (SD) years: USG 55.5 (15.7), LM 57.3 (18.9) Difficulty: difficult (participants reported past difficulties or anaesthesia providers identified them as having the potential for difficulty) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Site‐Rite 3 Ultrasound Unit (Bard Access Systems) with a 9.0 MHz probe
Axis: not specified
Guidance: dynamic Operator Profession: certified registered nurse anaesthetist Number of operators: two Experience of USG before the study: yes Length of experience with USG before the study: not specified A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: 5 Needle Length: not specified Gauge: 18 ‐ 22 |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, procedure time for first‐pass cannulation, procedure time for overall cannulation, number of attempts Definition of successful cannulation: blood return from a catheter Definition of start and end of time measurement Start:
End: successful intravenous cannulation |
|
| Funding | Not specified | |
| Declarations of interest | Not specified | |
| Notes | We attempted to contact the authors to obtain additional information but were unable to reach them. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of randomisation process |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment process |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Procedure time for first‐pass cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Number of attempts | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Procedure time for first‐pass cannulation | High risk | The outcome was evaluated only for participants with successful cannulation |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Unclear risk | No study register or protocol was available |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Procedure time for first‐pass cannulation | High risk | At least one domain was at high risk |
| Overall risk Procedure time for overall cannulation | High risk | At least one domain was at high risk |
| Overall risk Number of attempts | High risk | At least one domain was at high risk |
Bahl 2016.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ED Number of participants: 122 (USG 63, LM 59) Age, mean (SD) years: USG 61 (not specified), LM 62 (not specified) Difficulty: difficult (participants reported past difficulties or experienced at least one previous episode where at least 2 attempts were required to obtain a peripheral IV) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Sonosite M‐turbo (Sonosite) with a high‐frequency linear transducer
Axis: not specified
Guidance: not specified Operator Profession: ED registered nurses Number of operators: 20 Experience of USG before the study: no Length of experience with USG before the study: none A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: 10 Needle Length: not specified Gauge: not specified |
|
| Outcomes | First‐pass success of cannulation, time for overall cannulation, number of attempts Definition of successful cannulation: blood return from a catheter, smooth normal saline flush, and no signs of extravasation Definition of start and end of time measurement Start: a study nurse placed a tourniquet on a participant End: functional intravenous cannulation was obtained and a tegaderm was positioned over the catheter |
|
| Funding | Blue Cross Blue Shield of Michigan Physician Investigator Award Number 2069 | |
| Declarations of interest | None declared | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation scheme was created by a biostatistician using a computer‐generated program |
| Allocation concealment (selection bias) | Low risk | Randomisation with varying block sizes, sealed envelopes |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome (this was not stated in the article, but obtained through the communication with an author (AB)) |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome (this was not stated in the article, but obtained through the communication with an author (AB)) |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome (this was not stated in the article, but obtained through the communication with an author (AB)) |
| Blinding (performance bias and detection bias) Number of attempts | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome (this was not stated in the article, but obtained through the communication with an author (AB)) |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Unclear risk | No study register or protocol was available |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | Unclear risk | At least one domain was unclear |
| Overall risk Overall success of cannulation | Unclear risk | At least one domain was unclear |
| Overall risk Procedure time for overall cannulation | Unclear risk | At least one domain was unclear |
| Overall risk Number of attempts | Unclear risk | At least one domain was unclear |
Bridey 2018.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ICU Number of participants: 114 (USG 57, LM 57) Age, mean (SD) years: USG 65.5 (17.6), LM 64 (17) Difficulty: difficult (could not see and palpate a vein) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Sonosite M‐turbo (Sonosite) with a high‐frequency linear transducer
Axis: not specified
Guidance: not specified Operator Profession: ED registered nurse Number of operators: 20 Experience of USG before the study: 70% of the operators had previous experience Length of experience with USG before the study: not specified A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: 10 Needle Length: 29 mm Gauge: not specified |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, number of attempts, patient satisfaction Definition of successful cannulation: smooth normal saline flush, and no signs of extravasation |
|
| Funding | The French Intensive Care Society, ‘Bourse Recherche Paramédicale 2016’ | |
| Declarations of interest | None declared | |
| Notes | Although IV cannulation was attempted for four days in this study, we used results from day one to align with the conditions in other studies | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation list was computer‐generated (this was not stated in the article, but obtained through communication with an author (AK)) |
| Allocation concealment (selection bias) | Low risk | Randomisation with varying block sizes, sealed and opaque envelopes (this was not stated in the article, but obtained through communication with an author (AK)) |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves (this was not stated in the article, but obtained through communication with an author (AK)) |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves (this was not stated in the article, but obtained through communication with an author (AK)) |
| Blinding (performance bias and detection bias) Number of attempts | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves (this was not stated in the article, but obtained through communication with an author (AK)) |
| Blinding (performance bias and detection bias) Patient satisfaction | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | There were only three dropouts (USG 1, LM 2), and the reasons were detailed |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | There were only two dropouts (USG 1, LM 1), and the reasons were detailed |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | There were only three dropouts (USG 1, LM 2), and the reasons were detailed |
| Incomplete outcome data (attrition bias) Patient satisfaction | High risk | There were 10 dropouts from the assessment (USG 5, LM 5), and the reasons were not detailed |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial registry (NCT02285712) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Number of attempts | High risk | At least one domain was at high risk |
| Overall risk Patient satisfaction | High risk | At least one domain was at high risk |
Costantino 2005.
| Study characteristics | ||
| Methods | Quasi‐randomised (participants' presentation on an odd or even day), open‐label trial | |
| Participants | Setting: ED Number of participants: 60 (USG 39, LM 21) Age, mean (SD) years: not specified Difficulty: difficult (at least 3 failed attempts and a history of difficult IV cannulation) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Versapro (Siemens) with a 7.5 MHz probe or Sonosite 180 plus (Sonosite) with an 8.0 MHz probe
Axis: short
Guidance: dynamic Operator Profession: emergency physicians (resident and attending) Number of operators: 20 Experience of USG before the study: yes Length of experience with USG before the study: not specified A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: 32 mm Gauge: 18 |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, procedure time for overall cannulation, number of attempts, patient satisfaction, complications Definition of successful cannulation: blood return from a catheter Definition of start and end of time measurement Start: first percutaneous puncture End: successful cannulation |
|
| Funding | None | |
| Declarations of interest | Not specified | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Systematically allocated based on the day of presentation to the ED (odd day: USG, even day: LM) |
| Allocation concealment (selection bias) | High risk | Concealment is impossible due to method of allocation |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Number of attempts | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Patient satisfaction | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Overall complications | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Patient satisfaction | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Unclear risk | No study register or protocol was available |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Procedure time for overall cannulation | High risk | At least one domain was at high risk |
| Overall risk Number of attempts | High risk | At least one domain was at high risk |
| Overall risk Patient satisfaction | High risk | At least one domain was at high risk |
| Overall risk Overall complications | High risk | At least one domain was at high risk |
Glasin 2020.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ED Number of participants: 90 (USG 45, LM 45) Age, mean (SD) years: USG 61.7 (16), LM 60.8 (18.6) Difficulty: not restricted, but obese (BMI ≥ 25) Sites of peripheral veins: not specified | |
| Interventions |
Technique
LM vs USG:
Machine: x‐Porte (Fujifilm Sonosite) with a high‐frequency linear transducer
Axis: short
Guidance: dynamic Operator Profession: nurse Number of operators: 17 (16 nurses performed LM, 1 nurse performed USG) Experience of USG before the study: yes Length of experience with USG before the study: 1 year A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: 50 Needle Length: not specified Gauge: 12 ‐ 18 |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, pain, procedure time for first‐pass cannulation, procedure time for overall cannulation, number of attempts, patient satisfaction, overall complications Definition of successful cannulation: smooth normal saline flush Definition of start and end of time measurement Start: applying stasis with either a tourniquet or a blood pressure cuff End: blood entered a catheter flashback chamber |
|
| Funding | DW obtained research funding, but the source was not specified | |
| Declarations of interest | None declared | |
| Notes | The study had not yet been published as of December 2020. We received an unpublished manuscript courtesy of the author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation list was computer‐generated |
| Allocation concealment (selection bias) | Low risk | Used sequentially numbered, sealed and opaque envelopes (this was not stated in the article, but obtained through communication with an author (DW)) |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Pain | High risk | Although a third person assessed the outcome, participants were not blinded and the outcome could be influenced by subjectivity |
| Blinding (performance bias and detection bias) Procedure time for first‐pass cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Number of attempts | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Patient satisfaction | High risk | Although a third person assessed the outcome, participants were not blinded and the outcome could be influenced by subjectivity |
| Blinding (performance bias and detection bias) Overall complications | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | There was only one dropout (USG 1), and the reason was detailed |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | There was only one dropout (USG 1), and the reason was detailed |
| Incomplete outcome data (attrition bias) Pain | Low risk | There was only one dropout (USG 1), and the reason was detailed |
| Incomplete outcome data (attrition bias) Procedure time for first‐pass cannulation | Low risk | There was only one dropout (USG 1), and the reason was detailed |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | Low risk | There was only one dropout (USG 1), and the reason was detailed |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | There was only one dropout (USG 1), and the reason was detailed |
| Incomplete outcome data (attrition bias) Patient satisfaction | Low risk | There was only one dropout (USG 1), and the reason was detailed |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | There was only one dropout (USG 1), and the reason was detailed |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial registry (NCT04412967) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | Low risk | All domains were at low risk |
| Overall risk Overall success of cannulation | Low risk | All domains were at low risk |
| Overall risk Pain | High risk | At least one domain was at high risk |
| Overall risk Procedure time for first‐pass cannulation | Low risk | All domains were at low risk |
| Overall risk Procedure time for overall cannulation | Low risk | All domains were at low risk |
| Overall risk Number of attempts | Low risk | All domains were at low risk |
| Overall risk Patient satisfaction | High risk | At least one domain was at high risk |
| Overall risk Overall complications | Low risk | All domains were at low risk |
İsmailoğlu 2015.
| Study characteristics | ||
| Methods | Quasi‐randomised, open‐label trial Participants were allocated to each group alternately, in the order in which they were seen |
|
| Participants | Setting: ED Number of participants: 60 (USG 30, LM 30) Age, mean (SD) years: not specified Difficulty: difficult (a history or suspicion of difficult cannulation, and could not see or palplate a target vein) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Sonosite Micromaxx (Sonosite) with a high‐frequency linear transducer
Axis: not specified
Guidance: dynamic Operator Profession: ED nurses Number of operators: not specified Experience of USG before the study: no Length of experience with USG before the study: not specified A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: not specified Gauge: 20 |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, number of attempts, pain, overall complications Definition of successful cannulation: blood return from a catheter, smooth normal saline flush, and no signs of extravasation |
|
| Funding | None | |
| Declarations of interest | Not specified | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants were assigned alternately to USG and LM in the order in which they were seen. Not consecutive cases |
| Allocation concealment (selection bias) | High risk | This was a systematically allocated trial |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Pain | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Number of attempts | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Overall complications | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | No dropouts from the analysis |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | No dropouts from the analysis |
| Incomplete outcome data (attrition bias) Pain | Low risk | No dropouts from the analysis |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | No dropouts from the analysis |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | No dropouts from the analysis |
| Selective reporting (reporting bias) | Unclear risk | No study register or protocol was available |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Pain | High risk | At least one domain was at high risk |
| Overall risk Number of attempts | High risk | At least one domain was at high risk |
| Overall risk Overall complications | High risk | At least one domain was at high risk |
Kerforne 2012.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ICU Number of participants: 60 (USG 30, LM 30) Age, mean (SD) years: USG 61 (17), LM 56 (15) Difficulty: difficult (an operator could not see and palpate the targeted vein) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Vivid e (General Electric) with a 10 MHz probe
Axis: not specified
Guidance: dynamic Operator Profession: nurse Number of operators: not specified Experience of USG before the study: not specified Length of experience with USG before the study: not specified A training programme of USG for the study: not specified Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: not specified Gauge: not specified |
|
| Outcomes | First‐pass success of cannulation, overall successful of cannulation, procedure time for overall cannulation Definition of successful cannulation: not specified Definition of start and end of time measurement
|
|
| Funding | University Hospital of Poitiers | |
| Declarations of interest | None declared | |
| Notes | Data for first‐pass success of cannulation were unpublished and obtained through communication with an author (TK). We attempted to contact the authors to obtain additional information for the risk of bias (ROB) assessment but did not receive a response. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of randomisation process |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves (this was not stated in the article, but obtained through communication with an author (TK)) |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves (this was not stated in the article, but obtained through communication with an author (TK)) |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome (this was not stated in the article, but obtained through communication with an author (TK)) |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | High risk | The outcome was evaluated only for participants with successful cannulation |
| Selective reporting (reporting bias) | Unclear risk | No study register or protocol was available |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Procedure time for overall cannulation | High risk | At least one domain was at high risk |
McCarthy 2016A.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ED Number of participants: 192 (USG 98, LM 94) Age, mean (SD) years: not specified Difficulty: difficult (could not see or palpate a vein) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Sonosite M‐Turbo (Sonosite) or Zonare ultra (Zonare)
Axis: not specified
Guidance: dynamic Operator Profession: technician Number of operators: 33 Experience of USG before the study: yes Length of experience with USG before the study: 82% of the operators had more than one year of experience A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: 32 or 48 mm Gauge: 18 ‐ 22 |
|
| Outcomes | First‐pass success of cannulation, procedure time for first‐pass cannulation, pain, complications Definition of successful cannulation: smooth normal saline flush, and no signs of extravasation Definition of start and end of time measurement
|
|
| Funding | Award K01HS017957 from the Agency for Healthcare Research and Quality | |
| Declarations of interest | None declared | |
| Notes | McCarthy 2016 randomised participants separately according to the difficulty of the LM (easy, moderate, and difficult), and we split them according to the difficulty level (McCarthy 2016A; McCarthy 2016B; McCarthy 2016C) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation scheme was created by SAS software (version 9.3; SAS Institute Inc, Cary, NC) |
| Allocation concealment (selection bias) | Low risk | Centrally randomised with REDCap (version 6.5.12; Nashville, TN) |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Pain | High risk | Although a third person assessed the outcome, participants were not blinded and the outcome could be influenced by subjectivity |
| Blinding (performance bias and detection bias) Procedure time for first‐pass cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Overall complications | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | There were only two dropouts (USG 1, LM 1) |
| Incomplete outcome data (attrition bias) Pain | Low risk | There were only 4 dropouts out of 1189 participants across the whole study |
| Incomplete outcome data (attrition bias) Procedure time for first‐pass cannulation | Low risk | There were only 7 dropouts out of 1189 participants across the whole study |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial registry (NCT01859559) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | Low risk | All domains were at low risk |
| Overall risk Pain | High risk | At least one domain was at high risk |
| Overall risk Procedure time for first‐pass cannulation | Low risk | All domains were at low risk |
| Overall risk Overall complications | Low risk | All domains were at low risk |
McCarthy 2016B.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ED Number of participants: 401 (USG 202, LM 199) Age, mean (SD) years: not specified Difficulty: moderate (could see or palpate at least 1 vein but anticipated difficulty using LM) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Sonosite M‐Turbo (Sonosite) or Zonare ultra (Zonare)
Axis: not specified
Guidance: dynamic Operator Profession: technician Number of operators: 33 Experience of USG before the study: yes Length of experience with USG before the study: 82% of the operators had more than one year of experience A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: 32 or 48 mm Gauge: 18 ‐ 22 |
|
| Outcomes | First‐pass success of cannulation, procedure time for first‐pass cannulation, pain, complications Definition of successful cannulation: smooth normal saline flush, and no signs of extravasation Definition of start and end of time measurement
|
|
| Funding | Award K01HS017957 from the Agency for Healthcare Research and Quality | |
| Declarations of interest | None declared | |
| Notes | McCarthy 2016 randomised participants separately according to the difficulty of the LM (easy, moderate, and difficult), and we split them according to the difficulty level (McCarthy 2016A; McCarthy 2016B; McCarthy 2016C) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation scheme was created by SAS software (version 9.3; SAS Institute Inc., Cary, NC) |
| Allocation concealment (selection bias) | Low risk | Centrally randomised with REDCap (version 6.5.12; Nashville, TN) |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Pain | High risk | Although a third person assessed the outcome, patients were not blinded and the outcome could be influenced by subjectivity |
| Blinding (performance bias and detection bias) Procedure time for first‐pass cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Overall complications | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Pain | Low risk | There were only 4 dropouts out of 1189 participants across the whole study |
| Incomplete outcome data (attrition bias) Procedure time for first‐pass cannulation | Low risk | There were only 7 dropouts out of 1189 participants across the whole study |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial registry (NCT01859559) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | Low risk | All domains were at low risk |
| Overall risk Pain | High risk | At least one domain was at high risk |
| Overall risk Procedure time for first‐pass cannulation | Low risk | All domains were at low risk |
| Overall risk Overall complications | Low risk | All domains were at low risk |
McCarthy 2016C.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ED Number of participants: 596 (USG 305, LM 291) Age, mean (SD) years: not specified Difficulty: easy (could see or palpate at least 1 vein and thought IV access would be easy with LM) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Sonosite M‐Turbo (Sonosite) or Zonare ultra (Zonare)
Axis: not specified
Guidance: dynamic Operator Profession: technician Number of operators: 33 Experience of USG before the study: yes Length of experience with USG before the study: 82% of the operators had more than one year of experience A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: 32 or 48 mm Gauge: 18 ‐ 22 |
|
| Outcomes | First‐pass success of cannulation, procedure time for first‐pass cannulation, pain, complications Definition of successful cannulation: smooth normal saline flush, and no signs of extravasation Definition of start and end of time measurement
|
|
| Funding | Award K01HS017957 from the Agency for Healthcare Research and Quality | |
| Declarations of interest | None declared | |
| Notes | McCarthy 2016 randomised participants separately according to the difficulty of the LM (easy, moderate, and difficult), and we split them according to the difficulty level (McCarthy 2016A; McCarthy 2016B; McCarthy 2016C) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation scheme was created by SAS software (version 9.3; SAS Institute Inc., Cary, NC) |
| Allocation concealment (selection bias) | Low risk | Centrally randomised with REDCap (version 6.5.12; Nashville, TN) |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Pain | High risk | Although a third person assessed the outcome, participants were not blinded and the outcome could be influenced by subjectivity |
| Blinding (performance bias and detection bias) Procedure time for first‐pass cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Blinding (performance bias and detection bias) Overall complications | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third person assessed the outcome |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | There were only 5 dropouts (USG 5) out of 305 participants |
| Incomplete outcome data (attrition bias) Pain | Low risk | There were only 4 dropouts out of 1189 participants across the whole study |
| Incomplete outcome data (attrition bias) Procedure time for first‐pass cannulation | Low risk | There were only 7 dropouts out of 1189 participants across the whole study |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial registry (NCT01859559) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | Low risk | All domains were at low risk |
| Overall risk Pain | High risk | At least one domain was at high risk |
| Overall risk Procedure time for first‐pass cannulation | Low risk | All domains were at low risk |
| Overall risk Overall complications | Low risk | All domains were at low risk |
Nishizawa 2020.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ICU Number of participants: 60 (USG 30, LM 30) Age, mean (SD) years: USG 74.2 (14.7), LM 79.4 (10.8) Difficulty: difficult (at least 2 failed attempts with LM, or at least 2 experienced nurses anticipated difficulty with LM based on the absence of a palpable vein or a history of difficult IV cannulation) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Noblus (Hitachi) with a 10‐5 MHz
probe
Axis: short
Guidance: dynamic Operator Profession: nurse Number of operators: 30 Experience of USG before the study: no Length of experience with USG before the study: none A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: 3 Needle Length: 31 or 51 mm Gauge: 20 |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, complications Definition of successful cannulation: blood return from a catheter, saline flush without signs of extravasation |
|
| Funding | None | |
| Declarations of interest | None declared | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence was created by a computer |
| Allocation concealment (selection bias) | Low risk | Concealed using opaque, sealed envelopes |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Overall complications | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial protocol (obtained through communication with an author (TN)) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Overall complications | High risk | At least one domain was at high risk |
Pappas 2006.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: operating room Number of participants: 18 (USG 12, LM 6) Age, mean (SD) years: not specified Difficulty: at least 2 failed attempts with LM Sites of peripheral veins: upper extremity (forearm) | |
| Interventions |
Technique
LM vs USG:
Machine: Site‐Rite3 Ultrasound Unit (Bard Access Systems) with a 9.0 MHz probe
Axis: not specified
Guidance: dynamic Operator Profession: anaesthesia provider Number of operators: 3 Experience of USG before the study: yes Length of experience with USG before the study: not specified A training programme of USG for the study: not specified Number of clinical cases with USG required or experienced before the study intervention started: 5 Needle Length: not specified Gauge: 18 or 20 |
|
| Outcomes | Procedure time for overall cannulation, number of attempts, pain Definition of successful cannulation: blood return from a catheter Definition of start and end of time measurement:
|
|
| Funding | None | |
| Declarations of interest | Not specified | |
| Notes | Although original sample size was 46, they actually randomised only 22 participants, and did not mention the reason. Of the 22 participants, 2 were excluded due to broken randomisation and another 2 were excluded due to unsuccessful cannulation. We attempted to contact the authors to obtain additional information but were unable to reach them. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Packets, including consent and data collection tool with operational definitions, were shuffled and then numbered consecutively |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment |
| Blinding (performance bias and detection bias) Pain | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Blinding (performance bias and detection bias) Number of attempts | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves |
| Incomplete outcome data (attrition bias) Pain | High risk | 22 participants were initially randomised, but two participants were excluded due to broken randomisation, and another two participants were excluded from analysis due to unsuccessful cannulation |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | High risk | 22 participants were initially randomised, but two participants were excluded due to broken randomisation, and another two participants were excluded from analysis due to unsuccessful cannulation |
| Incomplete outcome data (attrition bias) Number of attempts | High risk | 22 participants were initially randomised, but two participants were excluded due to broken randomisation, and another two participants were excluded from analysis due to unsuccessful cannulation |
| Selective reporting (reporting bias) | Unclear risk | No study register or protocol was available |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk Pain | High risk | At least one domain was at high risk |
| Overall risk Procedure time for overall cannulation | High risk | At least one domain was at high risk |
| Overall risk Number of attempts | High risk | At least one domain was at high risk |
River 2009.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ED Number of participants: 47 (USG 26, LM 21) Age, mean (SD) years: not specified Difficulty: difficult (2 prior unsuccessful attempts with LM) Sites of peripheral veins: not specified | |
| Interventions |
Technique
LM vs USG:
Machine: not specified
Axis: not specified
Guidance: not specified Operator Profession: nurse Number of operators: not specified Experience of USG before the study: yes Length of experience with USG before the study: several months A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: not specified Gauge: not specified |
|
| Outcomes | Overall success of cannulation, procedure time for overall cannulation, number of attempts, patient satisfaction Definition of successful cannulation: not specified Definition of start and end of time measurement: not specified |
|
| Funding | Not specified | |
| Declarations of interest | Not specified | |
| Notes | We attempted to contact the authors to obtain additional information but were unable to reach them. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of randomisation process |
| Allocation concealment (selection bias) | Unclear risk | No description of randomisation process |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Who assessed the outcome was not specified |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Who assessed the outcome was not specified |
| Blinding (performance bias and detection bias) Number of attempts | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Who assessed the outcome was not specified |
| Blinding (performance bias and detection bias) Patient satisfaction | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Who assessed the outcome was not specified |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | Unclear risk | No mention of which participants were assessed |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Patient satisfaction | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Unclear risk | No study register or protocol was available |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Procedure time for overall cannulation | High risk | At least one domain was at high risk |
| Overall risk Number of attempts | High risk | At least one domain was at high risk |
| Overall risk Patient satisfaction | High risk | At least one domain was at high risk |
Skulec 2019.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: prehospital Number of participants: 300 (dynamic USG 100, static USG 100, LM 100) Age, mean (SD) years: dynamic USG 66.6 (17.4), static USG 65.3 (21.2), LM 64.5 (18.8) Difficulty: not restricted (all participants irrespective of difficulty) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs Dynamic USG vs Static USG
Machine: Vscan dual probe (General Electric)
Axis: short Operator Profession: paramedic, emergency physician Number of operators: 7 (5 paramedics, 2 emergency physicians) Experience of USG before the study: paramedics no; emergency physicians yes Length of experience with USG before the study: paramedics none, emergency physicians not specified A training programme of USG for the study: paramedics yes; emergency physicians no Number of clinical cases with USG required or experienced before the study intervention started:
Needle Length: 32 or 45 mm Gauge: 20 or more |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, procedure time for first‐pass cannulation, procedure time for overall cannulation, number of attempts, complications Definition of successful cannulation: blood return from a catheter, smooth normal saline flush, and no signs of extravasation Definition of start and end of time measurement
|
|
| Funding | None | |
| Declarations of interest | The author received a temporary loan of ultrasound machines from GE Medical Systems Ceska republika for study purposes, but no financial support | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation scheme was created by computer (this was not stated in the article, but obtained through communication with an author (RS)) |
| Allocation concealment (selection bias) | Low risk | Each random allocation was conducted by a person independent of the study, and used opaque, sealed envelopes (this was not stated in the article, but obtained through communication with an author (RS)) |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome (this was not stated in the article, but obtained through communication with an author (RS)) |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves (this was not stated in the article, but obtained through communication with an author (RS)) |
| Blinding (performance bias and detection bias) Procedure time for first‐pass cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome (this was not stated in the article, but obtained through communication with an author (RS)) |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome (this was not stated in the article, but obtained through communication with an author (RS)) |
| Blinding (performance bias and detection bias) Number of attempts | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome (this was not stated in the article, but obtained through communication with an author (RS)) |
| Blinding (performance bias and detection bias) Overall complications | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. Operators assessed the outcome themselves (this was not stated in the article, but obtained through the communication with an author (RS)) |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Procedure time for first‐pass cannulation | High risk | The outcome was evaluated only for participants with successful cannulation |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | The outcome was available for all participants |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial registry (NCT03709394) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | Low risk | All domains were at low risk |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Procedure time for first‐pass cannulation | High risk | At least one domain was at high risk |
| Overall risk Procedure time for overall cannulation | Low risk | All domains were at low risk |
| Overall risk Number of attempts | Low risk | All domains were at low risk |
| Overall risk Overall complications | High risk | At least one domain was at high risk |
Stein 2009.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ED Number of participants: 59 (USG 28, LM 31) Age, mean (SD) years: USG 58.1 (15.6), LM 54.8 (17.8) Difficulty: difficult (at least 2 failed attempts with LM) Sites of peripheral veins: upper extremity and jugular vein | |
| Interventions |
Technique
LM vs USG:
Machine: Sonosite Titan (Sonosite) with a 10 MHz probe
Axis: not specified
Guidance: dynamic Operator Profession: emergency physician (attending: USG and LM, resident: LM) Number of operators: 20 Experience of USG before the study: yes Length of experience with USG before the study: more than 6 months A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: not specified Gauge: not specified |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, procedure time for overall cannulation, number of attempts, patient satisfaction, complications Definition of successful cannulation: blood return from a catheter, smooth normal saline flush, and no signs of extravasation Definition of start and end of time measurement:
|
|
| Funding | None | |
| Declarations of interest | None declared | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by a research computer |
| Allocation concealment (selection bias) | Low risk | Research staff randomised participants with a research computer |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome |
| Blinding (performance bias and detection bias) Number of attempts | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome |
| Blinding (performance bias and detection bias) Patient satisfaction | High risk | Blinding of participants and operators is impossible due to the nature of the intervention |
| Blinding (performance bias and detection bias) Overall complications | Low risk | Although blinding of participants and operators is impossible due to the nature of the intervention, a third‐person assessed the outcome |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | The outcome was available for all participants |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | There were only 2 dropouts (USG 1, LM 1), and the reasons were detailed |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | High risk | It seems likely that only participants with successful cannulation were analysed |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | There were only 2 dropouts (USG 1, LM 1), and the reasons were detailed |
| Incomplete outcome data (attrition bias) Patient satisfaction | High risk | There were 7 dropouts (USG 4, LM 3), and the reasons were not specified |
| Incomplete outcome data (attrition bias) Overall complications | Low risk | There were only 2 dropouts (USG 1, LM 1), and the reasons were detailed |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial registry (NCT00692549) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | Low risk | All domains were at low risk |
| Overall risk Overall success of cannulation | Low risk | All domains were at low risk |
| Overall risk Procedure time for overall cannulation | High risk | At least one domain was at high risk |
| Overall risk Number of attempts | Low risk | All domains were at low risk |
| Overall risk Patient satisfaction | High risk | At least one domain was at high risk |
| Overall risk Overall complications | Low risk | All domains were at low risk |
Weiner 2013.
| Study characteristics | ||
| Methods | Randomised, open‐label trial | |
| Participants | Setting: ED Number of participants: 53 (USG 30, LM 23) Age, mean (SD) years: USG 46.2 (14.6), LM 53 (14.2) Difficulty: difficult (had a history of difficult IV cannulation, or at least 2 failed attempts with LM) Sites of peripheral veins: upper extremity | |
| Interventions |
Technique
LM vs USG:
Machine: Zonare z.one ultra Convertible Ultrasound System (Zonare) with a 8‐3 MHz probe, or Sonosite M‐turbo (Sonosite) with a 13‐6 MHz probe
Axis: short
Guidance: dynamic Operator Profession: nurse Number of operators: not specified Experience of USG before the study: no Length of experience with USG before the study: not specified A training programme of USG for the study: yes Number of clinical cases with USG required or experienced before the study intervention started: not specified Needle Length: up to operators' discretion Gauge: 18 ‐ 20 |
|
| Outcomes | First‐pass success of cannulation, overall success of cannulation, procedure time for overall cannulation, number of attempts, pain, patient satisfaction Definition of successful cannulation: blood return from a catheter, and no signs of extravasation Definition of start and end of time measurement:
|
|
| Funding | Not specified | |
| Declarations of interest | Not specified | |
| Notes | Data for first‐pass success of cannulation and patient satisfaction were unpublished and obtained through communication with an author (SW) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Initially a computerised coin‐toss, later randomised by shuffling sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Initially a computerised coin‐toss, later randomised by shuffling sealed envelopes |
| Blinding (performance bias and detection bias) First‐pass success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Overall‐success of cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Pain | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Procedure time for overall cannulation | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Number of attempts | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Blinding (performance bias and detection bias) Patient satisfaction | High risk | Blinding of participants and operators is impossible due to the nature of the intervention. One of the co‐authors assessed the outcome |
| Incomplete outcome data (attrition bias) First‐pass success of cannulation | Low risk | There were only 3 dropouts (USG 1, LM 2) |
| Incomplete outcome data (attrition bias) Overall success of cannulation | Low risk | There were only 3 dropouts (USG 1, LM 2) |
| Incomplete outcome data (attrition bias) Pain | Low risk | There were only 3 dropouts (USG 1, LM 2) |
| Incomplete outcome data (attrition bias) Procedure time for overall cannulation | Low risk | There were only 3 dropouts (USG 1, LM 2) |
| Incomplete outcome data (attrition bias) Number of attempts | Low risk | There were only 3 dropouts (USG 1, LM 2) |
| Incomplete outcome data (attrition bias) Patient satisfaction | Low risk | There were only 3 dropouts (USG 1, LM 2) |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the article were consistent with the trial registry (NCT01439113) |
| Other bias | Low risk | No concerns about other sources of bias |
| Overall risk First‐pass success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Overall success of cannulation | High risk | At least one domain was at high risk |
| Overall risk Pain | High risk | At least one domain was at high risk |
| Overall risk Procedure time for overall cannulation | High risk | At least one domain was at high risk |
| Overall risk Number of attempts | High risk | At least one domain was at high risk |
| Overall risk Patient satisfaction | High risk | At least one domain was at high risk |
BMI: body mass index ED: emergency department ICU: intensive care unit IV: intravenous LM: landmark method SD: standard deviation USG: ultrasound guidance
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bauman 2009 | Not a randomised controlled trial |
| Costantino 2010 | This trial compared ultrasound guidance and external jugular vein |
| Curtis 2015 | The participants in this study were children |
| DRKS00013797 | Not a randomised controlled trial |
| Evans 2013 | Not a randomised controlled trial |
| Galen 2018 | Not a randomised controlled trial |
| Hill 2017 | Not a comparison of USG peripheral intravenous cannulation and landmark method (long‐axis vs short‐axis USG) |
| NCT01602133 | Not a randomised controlled trial |
| NCT02360163 | This study was withdrawn (no enrolment was achieved) |
| NCT03440944 | Not a comparison of ultrasound‐guided peripheral intravenous cannulation and landmark method (midline vs USG) |
| NCT03457259 | Not a comparison of ultrasound‐guided peripheral intravenous cannulation and landmark method (midline vs peripheral, central, or peripherally inserted central lines) |
| NCT04234347 | Not a comparison of ultrasound‐guided peripheral intravenous cannulation and landmark method |
| Raio 2018 | Not a randomised controlled trial |
| Troisi 2013 | We contacted the author for further information but received no response |
USG: ultrasound guidance
Characteristics of studies awaiting classification [ordered by study ID]
IRCT201408097751N4.
| Methods | Randomised, controlled, multicentre trial |
| Participants | ED patients with difficult intravenous cannulation |
| Interventions | USG vs LM |
| Outcomes | Duration of USG and LM procedures Reason for using USG |
| Notes | This trial was registered in 2015, but the results have not been published and its status is unknown. |
ED: emergency department LM: landmark method USG: ultrasound guidance
Characteristics of ongoing studies [ordered by study ID]
NCT03745209.
| Study name | Ultrasound‐guided peripheral IV vs standard technique in difficult vascular access patients by ICU nurses |
| Methods | Randomised, controlled, single‐center trial |
| Participants | ICU patients with difficult cannulation |
| Interventions | USG vs LM |
| Outcomes | Overall success rate of IV cannulation Number of attempts 24 hours catheter survival Complications Subsequent need for PICC or central line |
| Starting date | 21 January 2019 |
| Contact information | Kingston General Hospital, Kingston, Ontario, Canada, K7L 2V7 Contact: Mohammed R Alshamsi, MD, 17mras@queensu.ca Contact: Gordon Boyd, MD, boydj@kgh.kari.net |
| Notes | We asked about the status of this trial but received no response. |
NCT03841864.
| Study name | Ultrasound guided peripheral IV insertion (USGPIV) |
| Methods | Randomised, controlled, single‐center trial |
| Participants | Adult elective pre‐operative patients Grade 1: visual vein classification grade described as excellent visualisation Grade 2a: veins that don't fit grade 1 or 2b classification Grade 2b: only faint vein shadow appearance described as poor visualisation Grade 3: no vein visualisation |
| Interventions | USG vs LM |
| Outcomes | IV insertion success rate |
| Starting date | 21 January 2019 |
| Contact information | Roya Yumul, MD, PhD, Roya.Yumul@cshs.org Ofelia Loani Elvir Lazo, MD, loanidoc@yahoo.com |
| Notes | We asked about the status of this trial but received no response. |
NCT04218643.
| Study name | Ultrasound‐guided peripheral intravenous catheter insertion technique (PIVC) |
| Methods | Randomised, controlled trial |
| Participants | Adult patients requiring a peripheral intravenous catheter |
| Interventions | USG vs LM |
| Outcomes | Post insertion failure rates Overall dwell time of the catheter Post removal complication rates Catheter to vein ratio |
| Starting date | 11 February 2020 |
| Contact information | Principal Investigator: Scott Leroux, BS NRP Reading Hospital |
| Notes |
NCT04853290.
| Study name | Patient experience in peripheral venipuncture with and without ultrasound (PERCEPT) |
| Methods | Randomised, controlled trial |
| Participants | Patients admitted to clinical inpatient units |
| Interventions | USG vs LM |
| Outcomes | Pain Patient satisfaction Overall success rate of IV cannulation Sleep quality Functional life of the catheter Complications |
| Starting date | 23 June 2021 |
| Contact information | Universidade Federal do Rio Grande do Sul ‐ Post Graduated Program Porto Alegre, Rio Grande Do Sul, Brazil Principal Investigator: Eneida R Rabelo da Silva, RN, ScD, eneidarabelo@gmail.com |
| Notes |
NCT04856826.
| Study name | Placement of peripheral venous catheters under echo guidance in a post‐emergency medical service (KatECHO) |
| Methods | Randomised, controlled trial |
| Participants | Patients hospitalised in a post‐emergency unit |
| Interventions | USG vs LM |
| Outcomes | First‐pass success rate of IV placement Pain Patients satisfaction Number of attempts Overall success of cannulation Location of the final placement site Calibre of the catheter placed Infectious or thromboembolic events Duration of catheter placement Functional life of the catheter Satisfaction of nursing staff |
| Starting date | 5 March 2021 |
| Contact information | CHU Grenoble Alpes La Tronche, France, 38700 Contact: Julie Duhoo, jduhoo@chu‐grenoble.fr |
| Notes |
NCT05119985.
| Study name | Ultrasound guided peripheral venous cannulation in patient undergoing elective surgery under general anesthesia |
| Methods | Randomised, controlled trial |
| Participants | Patients undergoing elective surgery under general anesthesia |
| Interventions | USG vs LM |
| Outcomes | First‐pass success of cannulation Number of attempts Complications Procedure time |
| Starting date | 1 October 2021 |
| Contact information | Masarykova Nemocnice v Ústí nad Labem, Krajská Zdravotní a.s. Ústí Nad Labem, Ústí Nad Labem Region, Czechia, 40001 Contact: Michal Kalina, michal.kalina@kzcr.eu |
| Notes |
ICU: intensive care unit IV: intravenous LM: landmark method PICC: peripheral intravenous central catheter USG: ultrasound guidance vs: versus
Differences between protocol and review
We initially intended to report the procedure time for peripheral venous cannulation. Due to different clinical significance, we reported two outcomes in the final review ‐ first‐pass and overall cannulation procedure times. For clarity, the secondary outcome 'number of attempts' was rephrased as 'number of cannulation atempts'.
We initially planned to evaluate performance bias and detection bias separately, but due to the nature of the intervention, we combined these. We assessed the blinding domain, incomplete outcome domain, and overall risk separately for each outcome.
We removed "difficult versus not difficult" and "experience of ultrasound‐guided cannulation: training versus clinical experience versus training plus clinical experience" from the Subgroup analysis and investigation of heterogeneity section because they were unnecessary.
We have rephrased the planned subgroup analysis relating to the operators' skills and setting to clarify our intentions in the Subgroup analysis and investigation of heterogeneity section.
We changed some subgroup analyses to match the difficulty with the landmark method and added explanations about the post hoc analysis in the Subgroup analysis and investigation of heterogeneity section.
We performed a meta‐regression analysis to assess the effect of difficulty levels in the primary outcomes and added an explanation for it.
Because the analysis showed clear heterogeneity between the difficulty levels, we regarded the results for all participants considered together to be less meaningful and only reported the results separately according to the difficulty levels in the abstract and summary of findings tables.
We added subgroup analyses on types of operators.
Contributions of authors
MT: clinical expertise, study selection, data extraction and bias assessment, conception and writing of the manuscript NY: clinical expertise, study selection, data extraction and bias assessment, and writing of the manuscript TM: clinical expertise, study selection, data extraction and bias assessment, conception and writing of the manuscript CT: clinical expertise, study selection, data extraction and bias assessment, and writing of the manuscript TF: methodological expertise and advice, critical revising for important intellectual content, final approval of the manuscript NW: methodological expertise and advice, conception and writing of the manuscript
Sources of support
Internal sources
-
No sources of support supplied, Other
No sources of support supplied
External sources
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK
The Cochrane Vascular editorial base is supported by the Chief Scientist Office.
Declarations of interest
MT: declared that his institute received research grants from Nakatani Foundation (ongoing multicentre prospective cohort study for myocardial infarction in the emergency department) and Radiometer America, Inc. (ongoing multicentre prospective cohort study of myocardial infarction in the emergency department). MT declared that he has received royalties from Japan Medical Journal as he co‐authored a textbook about ultrasound‐guided peripheral intravenous cannulation in emergency medicine. The textbook is about the technical issues of the review intervention. It explains the review intervention as one of various options and is not intended to promote the review intervention. Japan Medical Journal has no role in this Cochrane Review and meta‐analysis. NY: none known TM: none known CT: none known TF: has received financial payment for speaker's fees (Mitsubishi Tanabe Pharma Corporation), clinical trial consultancy (Mitsubishi Tanabe Pharma Corporation, Sony Electronics), scientific advisory board (Kyoto University Original), grant (Shionogi) and declares intellectual properties and patent‐pending (2020‐548587) for smartphone CBT apps (Mitsubishi Tanabe Pharma Corporation). NW: his institution has received research funds from the Japanese Ministry of Health Labor and Welfare and the Japanese Ministry of Education, Science, and Technology. He has also received royalties from Sogensha and Akatsuki for writing a book and developing software about interventions for insomnia. This review is completely independent from the intention of these grants.
New
References
References to studies included in this review
Aponte 2007 {published data only}
- Aponte H, Acosta S, Rigamonti D, Sylvia B, Austin P, Samolitis MT. The use of ultrasound for placement of intravenous catheters. American Association of Nurse Anesthesiology Journal 2007;75(3):212-6. [PubMed] [Google Scholar]
Bahl 2016 {published and unpublished data}
- Bahl A, Pandurangadu AV, Tucker J, Bagan M. A randomized controlled trial assessing the use of ultrasound for nurse-performed IV placement in difficult access ED patients. American Journal of Emergency Medicine 2016;34(10):1950-4. [DOI] [PubMed] [Google Scholar]
Bridey 2018 {published and unpublished data}
- Bridey C, Thilly N, Lefevre T, Maire-Richard A, Morel M, Levy B, et al. Ultrasound-guided versus landmark approach for peripheral intravenous access by critical care nurses: a randomised controlled study. BMJ Open 2018;8:e020220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Costantino 2005 {published and unpublished data}
- Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Annals of Emergency Medicine 2005;46(5):456-61. [DOI] [PubMed] [Google Scholar]
Glasin 2020 {unpublished data only}
- Glasin J, Henricson J, Wilhelms D. A randomized, controlled comparison of nurse-led peripheral venous catheter placement in overweight emergency patients using standard or dynamic ultrasound-guided technique. Data on file.
İsmailoğlu 2015 {published data only}
- İsmailoğlu EG, Zaybak A, Akarca FK, Kıyan S. The effect of the use of ultrasound in the success of peripheral venous catheterisation. International Emergency Nursing 2015;23:89-93. [DOI] [PubMed] [Google Scholar]
Kerforne 2012 {published and unpublished data}
- Kerforne T, Petitpas F, Frasca D, Goudet V, Robert R, Mimoz O. Ultrasound-guided peripheral venous access in severely ill patients with suspected difficult vascular puncture. Chest 2012;141(1):279-80. [DOI] [PubMed] [Google Scholar]
McCarthy 2016A {published and unpublished data}
- McCarthy M, Shokoohi H, Boniface KS, Eggelton R, Lowey A, Lim K, et al. Ultrasonography versus landmark for peripheral intravenous cannulation: a randomized controlled trial. Annals of Emergency Medicine 2016;68(1):10-8. [DOI] [PubMed] [Google Scholar]
McCarthy 2016B {published and unpublished data}
- McCarthy M, Shokoohi H, Boniface KS, Eggelton R, Lowey A, Lim K, et al. Ultrasonography versus landmark for peripheral intravenous cannulation: a randomized controlled trial. Annals of Emergency Medicine 2016;68(1):10-8. [DOI] [PubMed] [Google Scholar]
McCarthy 2016C {published and unpublished data}
- McCarthy M, Shokoohi H, Boniface KS, Eggelton R, Lowey A, Lim K, et al. Ultrasonography versus landmark for peripheral intravenous cannulation: a randomized controlled trial. Annals of Emergency Medicine 2016;68(1):10-8. [DOI] [PubMed] [Google Scholar]
Nishizawa 2020 {published and unpublished data}
- Nishizawa T, Matsumoto T, Todaka T, Sasano M, Kitagawa H, Shimabuku A. Nurse-performed ultrasound-guided technique for difficult peripheral intravenous access in critically ill patients: a randomized controlled trial. Journal of the Association for Vascular Access 2020;25(2):34-9. [Google Scholar]
Pappas 2006 {published data only}
- Pappas NL, Michaud TE, Wolbers RM, Steward JC, Fevurly TA, Samolitis TJ, et al. Ultrasound guidance as a rescue technique for peripheral intravenous cannulation; September 2006. www.researchgate.net/publication/235055786_Ultrasound_Guidance_as_a_Rescue_Technique_for_Peripheral_Intravenous_Cannulation [accessed 13 Oct 2020] (accessed 13 October 2020).
River 2009 {published data only}
- River G, Hebig A, McAlpine I, Stein J. Nurse-operated ultrasound for difficult intravenous access: a randomized trial. Annals of Emergency Medicine 2009;1:S87. [DOI] [PubMed] [Google Scholar]
Skulec 2019 {published and unpublished data}
- Skulec R, Callerova J, Vojtisek P, Cerny V. Two different techniques of ultrasound-guided peripheral venous catheter placement versus the traditional approach in the pre-hospital emergency setting: a randomized study. Internal and Emergency Medicine 2020;15(2):303-10. [DOI] [PubMed] [Google Scholar]
Stein 2009 {published data only}
- Stein J, George B, River G, Hebig A, McDermott D. Ultrasonographically guided peripheral intravenous cannulation in emergency department patients with difficult intravenous access: a randomized trial. Annals of Emergency Medicine 2009;54(1):33-40. [DOI] [PubMed] [Google Scholar]
Weiner 2013 {published and unpublished data}
- Weiner SG, Sarff AR, Esener DE, Shroff SD, Budhram GR, Switkowski KM, et al. Single-operator ultrasound-guided intravenous line placement by emergency nurses reduces the need for physician intervention in patients with difficult-to-establish intravenous access. Journal of Emergency Medicine 2013;44(3):653-60. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bauman 2009 {published data only}
- Bauman M, Braude D, Crandall C. Ultrasound-guidance vs standard technique in difficult vascular access patients by ED technicians. American Journal of Emergency Medicine 2009;27(2):135-40. [DOI] [PubMed] [Google Scholar]
Costantino 2010 {published and unpublished data}
- Costantino TG, Kirtz JF, Satz WA. Ultrasound-guided peripheral venous access vs. the external jugular vein as the initial approach to the patient with difficult vascular access. Journal of Emergency Medicine 2010;39(4):462-7. [DOI] [PubMed] [Google Scholar]
Curtis 2015 {published data only}
- Curtis S, Craig WR, Logue E, Vandermeer B, Hanson A, Klassen T. Ultrasound or near-infrared vascular imaging to guide peripheral intravenous catheterization in children: a pragmatic randomized controlled trial. Canadian Medical Association Journal 2015;19(187):563-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
DRKS00013797 {published data only}DRKS00013797
- DRKS00013797. Ultrasound-guided peripheral venous access [Sonographisch gesteuerte Anlage und Platzierung von peripher venösen Verweilkathetern]. drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00013797 (first received 17 January 2018).
Evans 2013 {published data only}
- Evans DP. Comparison of standard peripheral intravenous cannulation versus ultrasound guided peripheral intravenous cannulation in a novice study group. Academic Emergency Medicine 2013;20(Suppl 1):S80. [DOI] [PubMed] [Google Scholar]
Galen 2018 {published data only}
- Galen BT, Southern WN. Ultrasound-guided peripheral intravenous catheters to reduce central venous catheter use on the inpatient medical ward. Quality Management in Health Care 2018;27(1):30-2. [DOI] [PubMed] [Google Scholar]
Hill 2017 {published data only}
- Hill P, Ankiel S, Milam L. Evaluation of methods for ultrasound guided peripheral intravenous catheter insertion; August 2017. researchgate.net/publication/325105862_Evaluation_of_Methods_for_Ultrasound_Guided_Peripheral_Intravenous_Catheter_Insertion_Evaluation_of_Methods_for_Ultrasound_Guided_Peripheral_Intravenous_Catheter_Insertion_Background (accessed prior to 31 October 2022). [DOI: 10.13140/RG.2.2.21351.55202] [DOI]
NCT01602133 {published data only}
- NCT01602133. Assessment of ultrasound-guided inserted peripheral intravenous catheter (ECLIPSE). clinicaltrials.gov/ct2/show/results/NCT01602133?view=results (first received 18 May 2012).
NCT02360163 {published data only}
- NCT02360163. The "Peripheral Access Utilizing Sonographic Evaluation" Study (PAUSE). clinicaltrials.gov/ct2/show/NCT02360163 (first received 10 February 2015).
NCT03440944 {published data only}
- NCT03440944. Superior venous access, midline vs ultrasound IVs. clinicaltrials.gov/ct2/show/NCT03440944 (first received 22 February 2018).
NCT03457259 {published data only}
- NCT03457259. The clinical efficacy of midline catheters. clinicaltrials.gov/ct2/show/NCT03457259 (first received 7 March 2018).
NCT04234347 {published data only}
- NCT04234347. Long versus short axis approach for ultrasound guided peripheral intravenous access. clinicaltrials.gov/ct2/show/NCT04234347 (first received 21 January 2020).
Raio 2018 {published data only}
- Raio C, Elspermann R, Kittisarapong N, Stankard B, Bajaj T, Modayil V, et al. A prospective feasibility trial of a novel intravascular catheter system with retractable coiled tip guidewire placed in difficult intravascular access (DIVA) patients in the emergency department. Internal and Emergency Medicine 2018;13(5):757-4. [DOI: ] [DOI] [PubMed] [Google Scholar]
Troisi 2013 {published data only}
- Troisi F, Carelli S, Antonini F, Ranieri G, Rucci F, Galassi A, et al. Patients with difficult peripheral intravenous access in preference surgery: ultrasound guided technique. Regional Anesthesia and Pain Medicine 2013;38:E222. [Google Scholar]
References to studies awaiting assessment
IRCT201408097751N4 {published data only}https://en.irct.ir/trial/8201
- IRCT201408097751N4. Ultrasound-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access in the emergency room. en.irct.ir/trial/8201 (first received 17 March 2015).
References to ongoing studies
NCT03745209 {published data only}
- NCT03745209. Ultrasound-guided peripheral IV vs. standard technique in difficult vascular access patients by ICU nurses. clinicaltrials.gov/ct2/show/NCT03745209 (first received 19 November 2018).
NCT03841864 {published data only}
- NCT03841864. Ultrasound guided peripheral IV insertion (USGPIV). clinicaltrials.gov/ct2/show/NCT03841864 (first received 15 February 2019).
NCT04218643 {published data only}
- NCT04218643. Ultrasound-guided peripheral intravenous catheter insertion technique (PIVC). clinicaltrials.gov/ct2/show/NCT04218643 (first received 6 January 2020).
NCT04853290 {published data only}
- NCT04853290. Patient experience in peripheral venipuncture with and without ultrasound (PERCEPT). clinicaltrials.gov/ct2/show/NCT04853290 (first received 21 April 2021).
NCT04856826 {published data only}
- Placement of peripheral venous catheters under echo guidance in a post-emergency medical service (KatECHO). clinicaltrials.gov/ct2/show/NCT04856826 (first received 23 April 2021).
NCT05119985 {published data only}
- NCT05119985. Ultrasound guided peripheral venous cannulation in patient undergoing elective surgery under general anesthesia. clinicaltrials.gov/ct2/show/NCT05119985 (first received 15 November 2021).
Additional references
Adams 2016
- Adams DZ, Little A, Vinsant C, Khandelwal S. The midline catheter: a clinical review. Journal of Emergency Medicine 2016;51(3):252-8. [DOI] [PubMed] [Google Scholar]
ASA Task Force 2012
- American Society of Anesthesiologists Task Force on Central Venous Access, Rupp SM, Apfelbaum JL, Blitt C, Caplan RA, Connis RT, et al. Practice guidelines for central venous access: a report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology 2012;116(3):539-73. [DOI] [PubMed]
Attkisson 1982
- Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning 1982;5(3):233-7. [DOI] [PubMed] [Google Scholar]
Avila 2019
- Avila J. REBELCast Ep62 – US Guided PIVs with Jacob Avila, MD. rebelem.com/rebelcast-ep62-us-guided-pivs-with-jacob-avila-md/ Accessed 6 September 2019.
Bahl 2019
Bahl 2020
- Bahl A, Hijazi M, Chen NW, Clavette LL, Price J. Ultralong versus standard long peripheral intravenous catheters: a randomized controlled trial of ultrasonographically guided catheter survival. Annals of Emergency Medicine 202;76(2):134-42. [DOI] [PubMed] [Google Scholar]
Bauman 2009
- Bauman M, Braude D, Crandall C. Ultrasound-guidance vs. standard technique in difficult vascular access patients by ED technicians. American Journal of Emergency Medicine 2009;27:135-40. [DOI] [PubMed] [Google Scholar]
Brass 2015a
- Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database of Systematic Reviews 2015, Issue 1. Art. No: CD006962. [DOI: 10.1002/14651858.CD006962.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brass 2015b
- Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database of Systematic Reviews 2015, Issue 1. Art. No: CD011447. [DOI: 10.1002/14651858.CD011447] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carr 2016
- Carr PJ, Rippey JC, Budgeon CA, Cooke ML, Higgins N, Rickard CM. Insertion of peripheral intravenous cannulae in the emergency department: factors associated with first-time insertion success. Journal of Vascular Access 2016;17(2):182-90. [DOI] [PubMed] [Google Scholar]
Chopra 2015
- Chopra V, Flanders SA, Saint S, Woller SC, O'Grady NP, Safdar N, et al. The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC): results from a multispecialty panel using the RAND/UCLA appropriateness method. Annals of Internal Medicine 2015;163:S1-39. [DOI] [PubMed] [Google Scholar]
Civetta 2019
- Civetta G, Cortesi S, Mancardi M, Pirro AD, Vischio M, Mazzocchi M, et al. EA-DIVA score (Enhanced Adult DIVA score): a new scale to predict difficult preoperative venous cannulation in adult surgical patients. Journal of Vascular Access 2019;20(3):281-9. [DOI] [PubMed] [Google Scholar]
Dargin 2010
- Dargin JM, Rebholz CM, Lowenstein RA, Mitchell PM, Feldman JA. Ultrasonography-guided peripheral intravenous catheter survival in ED patients with difficult access. American Journal of Emergency Medicine 2010;28(1):1-7. [DOI] [PubMed] [Google Scholar]
Davis 2021
- Davis EM, Feinsmith S, Amick AE, Sell J, McDonald V, Trinquero P, et al. Difficult intravenous access in the emergency department: performance and impact of ultrasound-guided IV insertion performed by nurses. American Journal of Emergency Medicine 2021;46:539-44. [DOI] [PubMed] [Google Scholar]
Dillon 2008
- Dillon MF, Curran J, Martos R, Walsh C, Walsh J, Al-Azawi D, et al. Factors that affect longevity of intravenous cannulas: a prospective study. QJM: Monthly Journal of the Association of Physicians 2008;101(9):731-5. [DOI] [PubMed] [Google Scholar]
Duran 2016
- Duran LS, Pumarola CF, Borras NB, Font XP, Granes FXS. Ultrasound-guided peripheral venous catheterization in emergency services. Journal of Emergency Nursing 2016;42(4):338-43. [DOI] [PubMed] [Google Scholar]
Duran‐Gehring 2016
- Duran-Gehring P, Bryant L, Reynolds J, Aldridge P, Kalynych C, Guirgis F. Ultrasound-guided peripheral intravenous catheter training results in physician-level success for emergency department technicians. Journal of Ultrasound in Medicine 2016;35:2343-52. [DOI] [PubMed] [Google Scholar]
Egan 2013
- Egan G, Healy D, O'Neill H, Clarke-Moloney M, Grace PA, Walsh SR. Ultrasound guidance for difficult peripheral venous access: systematic review and meta-analysis. Emergency Medicine Journal 2013;30(7):521-6. [DOI] [PubMed] [Google Scholar]
Elia 2012
- Elia F, Ferrari G, Molino P, Converso M, De Filippi G, Milan A, et al. Standard-length catheters vs long catheters in ultrasound-guided peripheral vein cannulation. American Journal of Emergency Medicine 2012;30(5):712-6. [DOI] [PubMed] [Google Scholar]
Fields 2012
- Fields JM, Dean AJ, Todman RW, Au AK, Anderson KL, Ku BS, et al. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. American Journal of Emergency Medicine 2012;30(7):1134-40. [DOI] [PubMed] [Google Scholar]
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59(1):7-10. [DOI] [PubMed] [Google Scholar]
GRADE 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al, GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 6 September 2019. Hamilton (ON): McMaster University (developed by Evidence Prime), 2019. Available at gradepro.org.
Heinrichs 2013
- Heinrichs J, Fritze Z, Vandermeer B, Klassen T, Curtis S. Ultrasonographically guided peripheral intravenous cannulation of children and adults: a systematic review and meta-analysis. Annals of Emergency Medicine 2013;61(4):444-54 e1. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1.
Higgins 2021a
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Higgins 2021b
- Higgins JP, Li T, Deeks JJ, editor(s). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
Jones 1989
- Jones SE, Nesper TP, Alcouloumre E. Prehospital intravenous line placement: a prospective study. Annals of Emergency Medicine 1989;18(3):244-6. [DOI] [PubMed] [Google Scholar]
Keyes 1999
- Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Annals of Emergency Medicine 1999;34(6):711-4. [DOI] [PubMed] [Google Scholar]
Lapostolle 2007
- Lapostolle F, Catineau J, Garrigue B, Monmarteau V, Houssaye T, Vecci I, et al. Prospective evaluation of peripheral venous access difficulty in emergency care. Intensive Care Medicine 2007;33(8):1452-7. [DOI] [PubMed] [Google Scholar]
Lefebvre 2021
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Liu 2014
- Liu YT, Alsaawi A, Bjornsson HM. Ultrasound-guided peripheral venous access: a systematic review of randomized controlled trials. European Journal of Emergency Medicine 2014;21:18-23. [DOI] [PubMed] [Google Scholar]
Mahler 2011
- Mahler SA, Wang H, Lester C, Skinner J, Arnold TC, Conrad SA. Short- vs long-axis approach to ultrasound-guided peripheral intravenous access: a prospective randomized study. American Journal of Emergency Medicine 2011;29(9):1194-7. [DOI] [PubMed] [Google Scholar]
McCarthy 2016
- McCarthy ML, Shokoohi H, Boniface KS, Eggelton R, Lowey A, Lim K, et al. Ultrasonography versus landmark for peripheral intravenous cannulation: a randomized controlled trial. Annals of Emergency Medicine 2016;68(1):10-8. [DOI] [PubMed] [Google Scholar]
McGee 2003
- McGee DC, Gould MK. Preventing complications of central venous catheterization. New England Journal of Medicine 2003;348(12):1123-33. [DOI] [PubMed] [Google Scholar]
Mendeley [Computer program]
- Mendeley. Amsterdam, NL: Elsevier, accessed 6 September 2019. Available at mendeley.com/reference-management/reference-manager.
Microsoft Excel 2020 [Computer program]
- Microsoft Excel. Microsoft Corporation. Microsoft, 2020. www.microsoft.com/ja-jp/microsoft-365/excel/?rtc=1.
Mills 2007
- Mills CN, Liebmann O, Stone MB, Frazee BW. Ultrasonographically guided insertion of a 15-cm catheter into the deep brachial or basilic vein in patients with difficult intravenous access. Annals of Emergency Medicine 2007;50(1):68-72. [DOI] [PubMed] [Google Scholar]
Minville 2006
- Minville V, Pianezza A, Asehnoune K, Cabardis S, Smail N. Prehospital intravenous line placement assessment in the French emergency system: a prospective study. European Journal of Anaesthesiology 2006;23(7):594-7. [DOI] [PubMed] [Google Scholar]
Moureau 2019
- Moureau NL. Vessel Health and Preservation: The Right Approach for Vascular Access. Springer Cham, 2019. [DOI: 10.1007/978-3-030-03149-7] [DOI] [Google Scholar]
NICE 2002
- National Institute for Health and Care Excellence (NICE). Guidance on the use of ultrasound locating devices for placing central venous catheters. Technology appraisal guidance; October 2002 (TA49). www.nice.org.uk/guidance/ta49 (accessed 14 August 2018).
Oliveira 2016
- Oliveira L, Lawrence M. Ultrasound-guided peripheral intravenous access program for emergency physicians, nurses, and corpsmen (technicians) at a military hospital. Military Medicine 2016;181:272-6. [DOI] [PubMed] [Google Scholar]
Olsen 2017
- Olsen MF, Bjerre E, Hansen MD, Hilden J, Landler NE, Tendal B, et al. Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Medicine 2017;15:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ortega 2008
- Ortega R, Sekhar P, Sing M, Hansen CJ, Peterson L. Peripheral intravenous cannulation. New England Journal of Medicine 2008;359(21):e26. [DOI] [PubMed] [Google Scholar]
Ouzzani 2016
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan - a web and mobile app for systematic reviews. Systematic Reviews 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pandurangadu 2018
- Pandurangadu AV, Tucker J, Brackney AR, Bahl A. Ultrasound-guided intravenous catheter survival impacted by amount of catheter residing in the vein. Emergency Medicine Journal 2018;35:550-5. [DOI] [PubMed] [Google Scholar]
Privitera 2021
- Privitera D, Mazzone A, Pierotti F, Airoldi C, Galazzi A, Geraneo A, et al. Ultrasound-guided peripheral intravenous catheters insertion in patient with difficult vascular access: short axis/out-of-plane versus long axis/in-plane, a randomized controlled trial. Journal of Vascular Access 2021;4:1-9. [DOI: 10.1177/11297298211006996] [DOI] [PubMed] [Google Scholar]
R 2020 [Computer program]
- R: A language and environment for statistical computing. Version 4.0.3. Vienna, Austria: R Foundation for Statistical Computing, 2020. Available at www.R-project.org.
RevMan Web 2020 [Computer program]
- Review Manager Web (RevMan Web). Version 4.1.0. The Cochrane Collaboration, 2020. Available at revman.cochrane.org.
Sadud 2019
- Sadud RF, Schnobrich D, Mathews BK, Candotti C, Abdel-Ghani S, Perez MG, et al. Recommendations on the use of ultrasound guidance for central and peripheral vascular access in adults: a position statement of the Society of Hospital Medicine. Journal of Hospital Medicine 2019;14:E1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schoenfeld 2011
- Schoenfeld E, Boniface K, Shokoohi H. ED technicians can successfully place ultrasound-guided intravenous catheters in patients with poor vascular access. American Journal of Emergency Medicine 2011;29:496-501. [DOI] [PubMed] [Google Scholar]
Sebbane 2013
- Sebbane M, Claret PG, Lefebvre S, Mercier G, Rubenovitch J Jreige R, et al. Predicting peripheral venous access difficulty in the emergency department using body mass index and a clinical evaluation of venous accessibility. Journal of Emergency Medicine 2013;44(2):299-305. [DOI] [PubMed] [Google Scholar]
Seldinger 1953
- Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiologica 1953;39(5):368-76. [DOI: 10.3109/00016925309136722] [DOI] [PubMed] [Google Scholar]
Shokoohi 2013
- Shokoohi H, Boniface K, McCarthy M, Khedir Al-tiae T, Sattarian M, Ding R, et al. Ultrasound-guided peripheral intravenous access program is associated with a marked reduction in central venous catheter use in non-critically ill emergency department patients. Annals of Emergency Medicine 2013;61:198-203. [DOI] [PubMed] [Google Scholar]
Shokoohi 2019
- Shokoohi H, Boniface KS, Kulie P, Long A, McCarthy M. The utility and survivorship of peripheral intravenous catheters inserted in the emergency department. Annals of Emergency Medicine 2019;74:381-90. [DOI] [PubMed] [Google Scholar]
Sou 2017
- Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nursing 2017;16:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stolz 2015
- Stolz LA, Stolz U, Howe C, Farrell IJ, Adhikari S. Ultrasound-guided peripheral venous access: a meta-analysis and systematic review. Journal of Vascular Access 2015;16(4):321-6. [DOI] [PubMed] [Google Scholar]
Tran 2021
- Tran QK, Fairchild M, Yardi I, Mirda D, Markin K, Pourmand A. Efficacy of ultrasound-guided peripheral intravenous cannulation versus standard of care: a systematic review and meta-analysis. Ultrasound in Medicine and Biology 2021;47(11):3068-78. [DOI] [PubMed] [Google Scholar]
Troianos 2012
- Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, et al. Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesthesia and Analgesia 2012;114(1):46-72. [DOI] [PubMed] [Google Scholar]
Ullman 1978
- Ullman JI, Stoelting RK. Internal jugular vein location with the ultrasound Doppler blood flow detector. Anesthesia and Analgesia 1978;57(1):118. [DOI] [PubMed] [Google Scholar]
Van Loon 2016
- Van Loon FH, Puijn LA, Houterman S, Bouwman AR. Development of the A-DIVA Scale: a clinical predictive scale to identify difficult intravenous access in adult patients based on clinical observations. Medicine (Baltimore) 2016;95(16):e3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Loon 2018
- Van Loon FH, Buise MP, Claassen JJ, Dierick-van Daele AT, Bouwman AR. Comparison of ultrasound guidance with palpation and direct visualisation for peripheral vein cannulation in adult patients: a systematic review and meta-analysis. British Journal of Anaesthesia 2018;121(2):358-66. [DOI] [PubMed] [Google Scholar]
Van Loon 2019
- Van Loon FH, Van Hooff LW, De Boer HD, Koopman SS, Buise MP, Korsten HH, et al. The modified A-DIVA scale as a predictive tool for prospective identification of adult patients at risk of a difficult intravenous access: a multicenter validation study. Journal of Clinical Medicine 2019;8(2):144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2013
- Wu SY, Ling Q, Cao LH, Wang J, Xu MX, Zeng WA. Real-time two-dimensional ultrasound guidance for central venous cannulation: a meta-analysis. Anesthesiology 2013;118(2):361-75. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Tada 2019
- Tada M, Matsumoto T, Takeda C, Yamada N, Furukawa TA, Watanabe N. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults. Cochrane Database of Systematic Reviews 2019, Issue 9. Art. No: CD013434. [DOI: 10.1002/14651858.CD013434] [DOI] [PMC free article] [PubMed] [Google Scholar]


