Abstract
Background
Hepatocellular carcinoma lacks ideal diagnostic biomarkers. There is a lack of scientific evaluation of relevant promising biomarkers as well. Therefore this study reanalyzes the related studies of 11 blood biomarkers of HCC, and compares the diagnostic value of these biomarkers for HCC systematically.
Methods
The relevant literatures on the diagnostic value in HCC of 11 blood indexes in recent 5 years were searched in PubMed, Embase, and Cochrane libraries. Data were extracted and analyzed.
Results
Finally, 83 literature studies were brought into meta-analysis. The pooled sensitivity and specificity of AFP were 0.61 and 0.87, respectively. The AUC of AFP were 0.78. The AUC and sum of sensitivity and specificity of the combination of AFP and other biomarkers were all significantly higher than that of AFP, including AFP + AFP-L3 + DCP, AFP + DCP, AFP/DCP, AFP + GPC3. Among other biomarkers, the AUC and sum of sensitivity and specificity of biomarkers including DCP, GPC3, GP73, Hsp90alpha, midkine, and OPN were significantly higher than that of AFP. In this study, GP73 had the highest sum of sensitivity and specificity (1.78) and AUC (0.95).
Conclusions
The pooled sensitivity and specificity of AFP were 0.61 and 0.87, respectively. The AUC of AFP were 0.78. The combination of AFP and other biomarkers improved the diagnostic efficiency. The diagnostic value of biomarkers including DCP, GPC3, GP73, Hsp90alpha, midkine, and OPN was higher than that of AFP. GP73 had the best diagnostic value for HCC with the highest sum of sensitivity and specificity (1.78) and AUC (0.95).
KEY MESSAGES
The pooled sensitivity and specificity of AFP were 0.61 and 0.87, respectively. The AUC of AFP were 0.78. The combination of AFP and other biomarkers improved the diagnostic efficiency of HCC.
The diagnostic value of biomarkers including DCP, GPC3, GP73, Hsp90alpha, midkine, and OPN was higher than that of AFP.
GP73 had the best diagnostic value for HCC.
Keywords: Biomarkers, HCC, the diagnostic value, meta-analysis
1. Introduction
Hepatocellular carcinoma(HCC) has become an important public health problem worldwide because of its high mortality [1]. In Asia, HCC secondary to hepatitis B virus is more common. HCC secondary to alcoholic liver disease is also increasing in western developed countries. Due to the symptoms of HCC are not obvious in the early stage, many patients are in the advanced stage when diagnosed, missing the best opportunity for treatment. The early diagnosis of HCC can not only improve the survival time and quality of life of patients but also save the cost of treatment. Therefore, the early diagnosis is the breakthrough focus of HCC treatment.
Alpha fetoprotein (AFP) is the most commonly used biomarker for the diagnosis of HCC, but the diagnostic value of AFP is gradually being doubted because of its low sensitivity, especially for early HCC [2]. Many studies were devoted to finding biomarkers with better diagnostic value in HCC [3].
Recently, many new biomarkers attracted public attention, such as AFP-L3, DCP, DKKI, GP73, and so on. Alpha-fetoprotein-L3(AFP-L3), as a heterogeneous body of AFP, mainly comes from HCC cells. Des-γ-carboxyprothrombin (DCP), also known as protein induced by vitamin K absence or antagonist II (PIVKAII), can appear in the serum of patients with vitamin K absence or HCC [4]. Dickkopf-1 (DKK1) is a secretory glycoprotein that inhibits Wnt signalling pathway by binding to Wnt receptor LRP5/6 [5]. Wnt signalling pathway is an important mechanism for the occurrence and development of HCC and other tumours. Golgi protein 73 (GP73), a type II transmembrane glycoprotein resident in golgi apparatus, is expressed in a small amount in normal liver while it can be specifically expressed, especially around connective tissue and cirrhotic nodules, when liver diseases, such as HCC occur [6]. Glypican-3 (GPC3) is a heparan sulphate glycoprotein on the surface of cell membrane, which is a specific antigen related to HCC [7]. Osteopontin (OPN) is a kind of protein, widely distributed in a variety of tissues and cells. It can participate in tissue repair, self-metabolism, and other functions. The expression level of OPN is closely related to the clinicopathological features of HCC, such as envelope infiltration, vascular invasion, lymph node metastasis, and clinical stage [8,9]. A-L-fucosidase (AFU) is an acidic hydrolase, which is mainly involved in the catabolism of macromolecular substances containing fucosyl, such as glycolipids, glycoproteins, mucopolysaccharides. Junna reported the over expression of AFU in the serum of patients with primary HCC, suggesting that AFU might be a potential marker for the early diagnosis of HCC [10]. Carbohydrate antigen199 (CA199), glycolipid on cell membrane is a kind of glycoprotein antigen that can recognize tumour specific macromolecules [11,12]. Heat shock protein 90alpha (Hsp90alpha) is a multifunctional molecular chaperone, which is widely involved in physiological activities, such as cell signal transduction, hormone response, and transcriptional regulation, maintaining the normal physiological function of cells [13]. Hsp90alpha keeps silent in normal cells while active in tumour cells. Midkine (MDK) is a secretory cytokine, which can participate in the occurrence and development of malignant tumours by promoting division, promoting angiogenesis, and antiapoptosis [14,15]. In recent years, there were more and more studies on the diagnostic value of the above biomarkers for HCC, so which biomarker had a better diagnostic value?
In this study, the meta-analysis was used to reanalyze the related studies of 11 biomarkers, so as to analyze and compare the diagnostic value of biomarkers for HCC more systematically and scientifically.
2. Materials and methods
2.1. Literature search
This meta-analysis followed Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) Guidelines. The relevant literatures on the diagnostic value of 11 blood indexes, such as AFP, AFP-L3, and DCP in HCC in recent 5 years were comprehensively and systematically searched in PubMed, Embase, and Cochrane libraries. The keywords used for retrieval included three parts: (1) (AFP OR alpha-fetoprotein) OR (AFP-L3 OR alpha-fetoprotein-L3 OR lens culinaris-agglutinin-reactive fraction of AFP) OR (PIVKA-II OR DCP OR des-γ-carboxyprothrombin) OR (dickkopf-1 OR DKK1) OR (GP73 OR golgi protein 73) OR (glypican-3 OR GPC3) OR (osteopontin OR OPN) OR (α-L-fucosidase OR AFU) OR (carbohydrate antigen199 OR CA199) OR (heat shock protein 90alpha OR Hsp90alpha) OR (midkine OR MDK) (2) HCC OR hepatocellular carcinoma OR liver cancer OR hepatocellular OR hepatoma (3) sensitivity OR specificity. The above three parts were connected by ‘and’. The retrieved literature was published from January 2017 to January 2022.
2.2. Inclusion and exclusion criteria
The inclusion criteria of literature were as follows:
The diagnostic value of at least one of the 11 biomarkers was described to ensure that we could extract and calculate key indicators directly or indirectly, including sensitivity, specificity, true positive (TP), false positive (FP), false negative (FN) and true negative (TN);
The diagnosis of HCC was based on recognized guidelines, such as histopathology or other appropriate diagnostic criteria;
The specimen type was serum;
The control group was consisted of patients with chronic liver disease, such as liver cirrhosis or hepatitis, or patients with benign liver disease like liver cyst or healthy people.
The exclusion criteria were defined as follows:
The article provided incomplete diagnostic information;
Meta analysis, systematic review, case review, case report, letter;
The control group involved other malignant tumours, especially gastrointestinal tumours;
The article from non-human research;
The article with <20 research samples;
2.3. Data extraction
Two authors screened each record retrieved and extracted data independently. Any differences were resolved through discussion until a consensus was reached or a third author was consulted. Following information was extracted from qualified Literature: author, year of publication, patient country, comprehensive sensitivity and specificity of biomarkers, TP, FP, FN, and TN, type, and number of cases. Finally, the pooled sensitivity and specificity, diagnostic odds ratio, area under the curve, positive likelihood ratio, and negative likelihood ratio were evaluated.
2.4. Statistical analysis
The stata software (midas) was used for meta-analysis. Meta-disc software was used to calculate Spearman’s correlation coefficient values to evaluate the threshold effect. p < 0.05 was considered as a significant manifestation of threshold effect. At the same time, the Cochran Q test and I-squared test were performed to estimate the existence and severity of heterogeneity. p < 0.1, and I2 > 50% were considered significant manifestations of heterogeneity. The Deeks’ funnel plot was used for publication bias analysis. p < 0.05 was considered to have potential publication bias.
3. Results
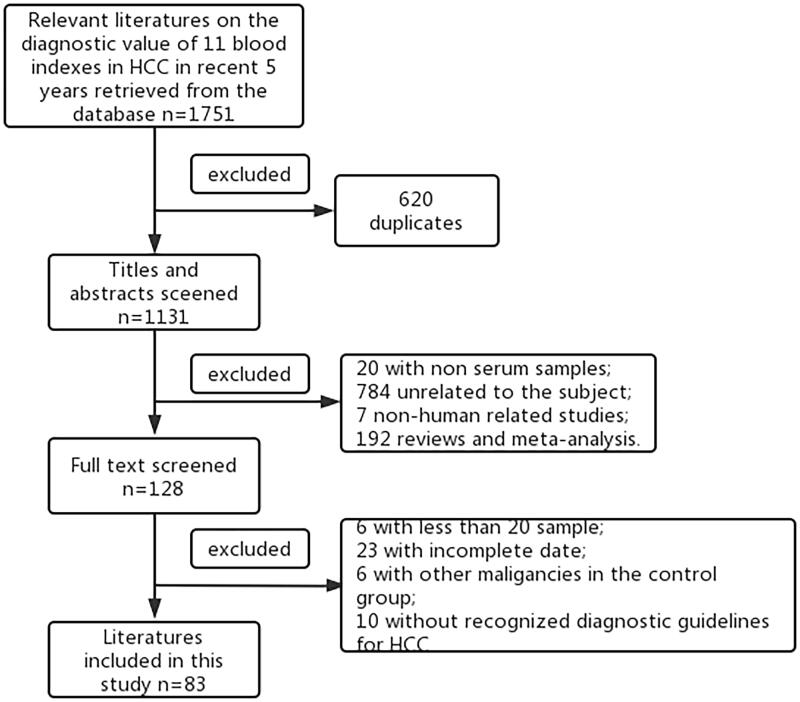
The flow chart of the inclusion and exclusion of studies in the review is shown in Figure 1. As shown in the figure, a total of 1751 documents were retrieved from three databases, of which 620 duplicates were eliminated and 1131 were left. Among the leaving documents, there were 784 unrelated to the subject, 192 reviews or meta-analysis, seven non-human related studies, 20 non serum samples, 23 with incomplete date, six with other malignancies in the control group, 10 without recognized diagnostic guidelines for HCC, and six studies with <20 samples. Finally, 83 studies were included in the meta-analysis.
Figure 1.
Flow chart of research.
3.1. AFP and AFP combined with other biomarkers
Among the 83 literature studies, 43 were related to the diagnostic value of AFP, six were related to AFP + AFP-L3, six were related to AFP + AFP-L3 + DCP, 10 were related to AFP + DCP, six were related to AFP/DCP, and eight were related to AFP + GPC3. In the above multi-biomarker combination types, ‘A + B’ represents series diagnosis, which can be diagnosed as positive if they are all positive, while ‘A/B’ is parallel diagnosis, and one positive item can be diagnosed as positive. The study ID, region, and other research characteristics were summarized in Table 1.
Table 1.
Main characteristics of the included literature related to AFP and AFP combined with other biomarkers in this study.
| Markers | Study id [Ref] | Region | Case/control | Sample size (case/control) | TP | FP | FN | TN | Se (%) | Sp (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| AFP | Mashaly, A. H. 2018 [14] | Egypt | HCC/CLD | 44/31 | 23 | 1 | 21 | 30 | 52.27 | 96.77 |
| Qian, Y. 2020 [16] | China | HCC/CLD | 118/75 | 68 | 27 | 50 | 48 | 57.63 | 64.00 | |
| Lee, J. 2021 [17] | Korea | HCC/CLD | 184/134 | 83 | 11 | 101 | 123 | 45.00 | 91.80 | |
| Sultanik, P. 2017 [18] | France | HCC/CLD | 46/116 | 29 | 21 | 17 | 95 | 63.00 | 82.00 | |
| Kim, M. N. 2019 [19] | Korea | HCC/CLD | 64/328 | 42 | 22 | 22 | 306 | 65.60 | 93.30 | |
| Park, S. J. 2017 [20] | Korea | HCC/CLD | 79/77 | 49 | 6 | 30 | 71 | 62.03 | 92.21 | |
| Xu, F. 2021 [21] | China | HCC/CLD | 308/60 | 212 | 10 | 96 | 50 | 68.80 | 83.30 | |
| Loglio, A. 2020 [22] | Italy | HCC/CLD | 64/148 | 36 | 9 | 28 | 139 | 56.00 | 94.00 | |
| Ye, F. 2021 [23] | China | HCC/CLD | 133/101 | 80 | 9 | 53 | 92 | 60.15 | 91.09 | |
| Wang, F. 2021 [24] | China | HCC/CLD | 186/235 | 118 | 58 | 68 | 177 | 63.40 | 75.30 | |
| Omran, M. M. 2021 [25] | Egypt | HCC/CLD | 155/60 | 42 | 0 | 113 | 60 | 27.00 | 100.00 | |
| Malov, S. I. 2021 [26] | Russia | HCC/CLD | 55/55 | 25 | 3 | 30 | 52 | 45.50 | 94.50 | |
| Lambrecht, J. 2021 [27] | Germany | HCC/CLD | 122/145 | 97 | 31 | 25 | 114 | 79.17 | 78.87 | |
| Zhou, P. C. 2020 [28] | China | HCC/CLD | 20/20 | 6 | 0 | 14 | 20 | 30.00 | 100.00 | |
| Zhang, X. 2020 [29] | China | HCC/CLD | 288/286 | 210 | 53 | 78 | 233 | 72.90 | 81.50 | |
| Hendy, O. M. 2020 [30] | Egypt | HCC/CLD | 40/30 | 25 | 2 | 15 | 28 | 62.50 | 93.33 | |
| Mao, L. 2017 [31] | China | HCC/CLD | 82/29 | 37 | 10 | 45 | 19 | 45.12 | 65.52 | |
| Jasirwan, C. O. 2020 [32] | Indonesia | HCC/CLD | 132/198 | 109 | 57 | 23 | 141 | 82.60 | 71.20 | |
| Lee, H. A. 2021 [33] | Korea | HCC/CLD | 160/462 | 126 | 181 | 34 | 281 | 78.80 | 61.00 | |
| Yang, M. Y. 2021 [34] | China | HCC/CLD | 314/300 | 194 | 114 | 120 | 186 | 61.80 | 62.00 | |
| Schotten, C. 2021 [35] | Germany | HCC/CLD | 196/377 | 119 | 15 | 77 | 362 | 60.70 | 96.00 | |
| Liu, D. 2021 [36] | China | HCC/CLD | 123/143 | 65 | 9 | 58 | 134 | 52.80 | 93.70 | |
| Omran, M. M. 2020 [37] | Egypt | HCC/CLD | 104/92 | 30 | 0 | 74 | 92 | 29.00 | 100.00 | |
| Li, B. 2020 [38] | China | HCC/CLD | 104/95 | 60 | 13 | 44 | 82 | 57.70 | 86.30 | |
| Yang, T. 2019 [39] | China | HCC/CLD | 289/211 | 193 | 44 | 96 | 167 | 66.80 | 79.20 | |
| Wang, Q. 2019 [40] | China | HCC/CLD | 176/359 | 114 | 82 | 62 | 277 | 64.80 | 77.20 | |
| Shimagaki, T. 2019 [41] | Japan | HCC/CLD | 185/108 | 93 | 16 | 92 | 92 | 50.30 | 85.20 | |
| Hu, J. 2018 [42] | China | HCC/CLD | 369/176 | 213 | 26 | 156 | 150 | 57.70 | 85.20 | |
| Guo, W. 2018 [43] | China | HCC/CLD | 200/101 | 114 | 20 | 86 | 81 | 57.00 | 80.00 | |
| Chuaypen, N. 2018 [44] | Thailand | HCC/CLD | 150/150 | 97 | 4 | 53 | 146 | 64.70 | 97.30 | |
| Tian, M. M. 2017 [45] | China | HCC/CLD | 120/146 | 66 | 56 | 54 | 90 | 55.00 | 61.60 | |
| Shaker, M. K. 2017 [46] | Egypt | HCC/CLD | 50/25 | 35 | 1 | 15 | 24 | 70.00 | 96.00 | |
| Ismail, M. M. 2017 [47] | Saudi Arabia | HCC/CLD | 66/99 | 45 | 12 | 21 | 87 | 68.20 | 87.90 | |
| Hu, N. 2017 [48] | China | HCC/CLD | 80/80 | 47 | 20 | 33 | 60 | 58.75 | 75.00 | |
| Fu, Y. 2017 [49] | China | HCC/CLD | 531/171 | 408 | 29 | 123 | 142 | 76.82 | 83.01 | |
| Liu, H. H. 2020 [50] | China | HCC/CLD | 105/54 | 38 | 5 | 67 | 49 | 36.19 | 90.74 | |
| Tang, X. Q. 2017 [51] | China | HCC/CLD | 176/190 | 130 | 32 | 46 | 158 | 73.90 | 82.90 | |
| Ali, O. M. 2020 [52] | Egypt | HCC/CLD | 30/30 | 22 | 4 | 8 | 26 | 72.20 | 86.20 | |
| Sai, W. L. 2021 [53] | China | HCC/CLD | 126/96 | 93 | 21 | 33 | 75 | 73.81 | 78.13 | |
| Alzamzamy, A. 2021 [54] | Egypt | HCC/CLD | 40/60 | 26 | 10 | 14 | 50 | 65.00 | 83.30 | |
| Ricco G. 2018 [55] | Italy | HCC/CLD | 258/130 | 135 | 32 | 123 | 98 | 52.50 | 75.20 | |
| Caviglia GP. 2021 [56] | Italy | HCC/CLD | 72/119 | 55 | 37 | 17 | 82 | 76.40 | 68.90 | |
| Caviglia GP. 2020 [57] | Italy | HCC/CLD | 149/200 | 107 | 68 | 42 | 132 | 72.00 | 66.00 | |
| AFP + AFP-L3 | Song, T. 2020 [58] | China | HCC/CLD | 100/67 | 54 | 7 | 46 | 60 | 53.50 | 89.60 |
| Pan, Y. 2019 [59] | China | HCC/CLD, HC | 125/280 | 72 | 23 | 53 | 257 | 57.60 | 91.80 | |
| Hu, R. Z. 2019 [60] | China | HCC/CLD | 56/91 | 36 | 8 | 20 | 83 | 64.28 | 90.90 | |
| Park, S. J. 2017 [20] | Korea | HCC/CLD | 79/77 | 35 | 2 | 44 | 75 | 44.30 | 97.40 | |
| Choi, J. 2019 [61] | Korea | HCC/CLD | 42/168 | 33 | 22 | 9 | 146 | 79.00 | 87.00 | |
| Chen, H. 2018 [62] | China | HCC/CLD | 202/441 | 83 | 44 | 119 | 397 | 40.90 | 90.00 | |
| AFP + AFP-L3 + DCP | Song, T. 2020 [58] | China | HCC/CLD | 100/67 | 67 | 11 | 33 | 56 | 66.70 | 83.10 |
| Pan, Y. 2019 [59] | China | HCC/CLD, HC | 125/280 | 65 | 18 | 60 | 262 | 52.00 | 93.60 | |
| Hu, R. Z. 2019 [60] | China | HCC/CLD | 56/91 | 31 | 2 | 25 | 89 | 55.35 | 98.48 | |
| Park, S. J. 2017 [20] | Korea | HCC/CLD | 79/77 | 30 | 0 | 49 | 77 | 37.97 | 100.00 | |
| Choi, J. 2019 [61] | Korea | HCC/CLD | 42/168 | 35 | 42 | 7 | 126 | 83.00 | 75.00 | |
| Chen, H. 2018 [62] | China | HCC/CLD, HC | 202/644 | 149 | 64 | 53 | 580 | 73.70 | 90.00 | |
| AFP + DCP | Park, S. J. 2017 [20] | Korea | HCC/CLD | 79/77 | 40 | 0 | 39 | 77 | 51.00 | 100.00 |
| Xu, F. 2021 [21] | China | HCC/CLD, BLD | 308/120 | 293 | 20 | 15 | 100 | 95.10 | 83.30 | |
| Yang, T. 2019 [39] | China | HCC/CLD | 289/211 | 254 | 40 | 35 | 171 | 87.80 | 81.00 | |
| Wang, Q. 2019 [40] | China | HCC/CLD | 176/359 | 129 | 22 | 47 | 337 | 73.30 | 93.90 | |
| Tang, X. Q. 2017 [51] | China | HCC/CLD | 176/190 | 154 | 25 | 22 | 165 | 87.50 | 87.00 | |
| Pan, Y. 2019 [59] | China | HCC/CLD, HC | 125/280 | 78 | 21 | 47 | 259 | 62.00 | 92.50 | |
| Wu, M. 2020 [63] | China | HCC/CLD, HC | 198/176 | 160 | 52 | 38 | 124 | 80.80 | 70.60 | |
| Maeda, T. 2019 [64] | Japan | HCC/CLD, HC | 304/152 | 224 | 13 | 80 | 139 | 73.70 | 91.70 | |
| Wu, J. 2018 [65] | China | HCC/CLD, HC | 143/131 | 126 | 44 | 17 | 87 | 88.10 | 66.41 | |
| Ricco G. 2018 [55] | Italy | HCC/CLD | 258/130 | 225 | 62 | 33 | 68 | 87.40 | 52.20 | |
| AFP/DCP | Park, S. J. 2017 [20] | Korea | HCC/CLD | 79/77 | 65 | 29 | 14 | 48 | 82.28 | 62.34 |
| Lee, Q. 2021 [66] | China | HCC/CLD | 158/62 | 114 | 2 | 44 | 60 | 72.20 | 96.80 | |
| Loglio, A. 2020 [22] | Italy | HCC/CLD | 64/148 | 51 | 21 | 13 | 127 | 80.00 | 86.00 | |
| Sultanik, P. 2017 [18] | France | HCC/CLD | 46/116 | 40 | 28 | 6 | 88 | 87.00 | 76.00 | |
| Wu, J. 2018 [65] | China | HCC/CLD, HC | 143/131 | 76 | 9 | 67 | 122 | 53.02 | 93.13 | |
| Pan, Y. 2019 [59] | China | HCC/CLD, HC | 125/280 | 114 | 53 | 11 | 227 | 91.20 | 81.10 | |
| AFP + GPC3 | Wu, M. 2020 [63] | China | HCC/CLD, HC | 198/176 | 172 | 50 | 26 | 126 | 86.90 | 71.70 |
| Zhu, X. 2019 [67] | China | HCC/CLD | 47/89 | 40 | 16 | 7 | 73 | 85.01 | 81.62 | |
| Taketomi, A. 2020 [68] | Egypt | HCC/CLD, HC | 25/125 | 23 | 0 | 2 | 125 | 92.00 | 100.00 | |
| Tang, X. Y. 2020 [69] | China | HCC/HC, BLD | 166/144 | 146 | 32 | 20 | 112 | 87.82 | 77.86 | |
| Shimizu, Y. 2020 [70] | Japan | HCC/CLD | 105/95 | 72 | 10 | 33 | 85 | 68.30 | 89.40 | |
| Liu, S. 2020 [71] | China | HCC/HC | 210/127 | 185 | 22 | 25 | 105 | 88.10 | 82.68 | |
| Sun, B. 2017 [7] | China | HCC/CLD, HC | 76/100 | 65 | 4 | 11 | 96 | 85.50 | 96.00 | |
| Ali, O. M. 2020 [52] | Egypt | HCC/CLD | 30/30 | 27 | 4 | 3 | 26 | 91.00 | 86.00 |
CLD: chronic liver disease; BLD: benign liver disease; HC: healthy control; CH: cirrhosis; TP: true positive; FP: false positive; FN: false negative; TN: true negative; Se: sensitivity; Sp: specificity; Ref: reference.
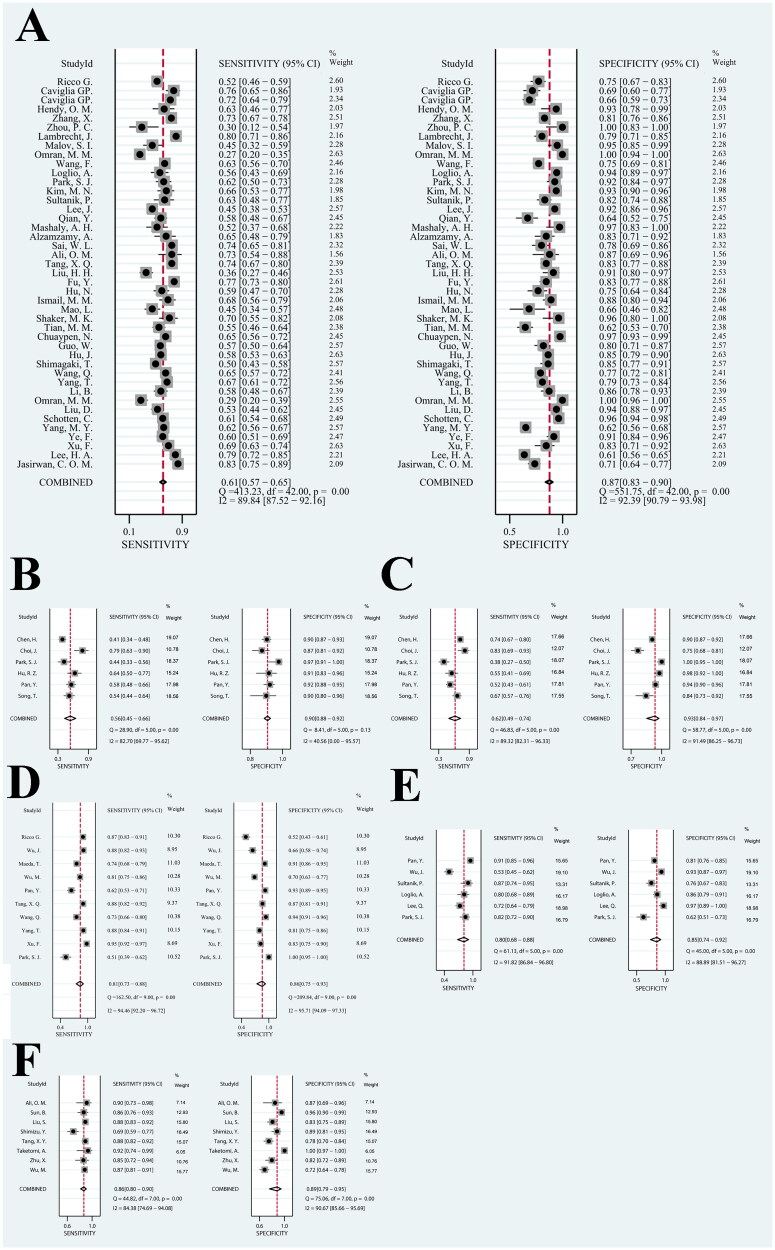
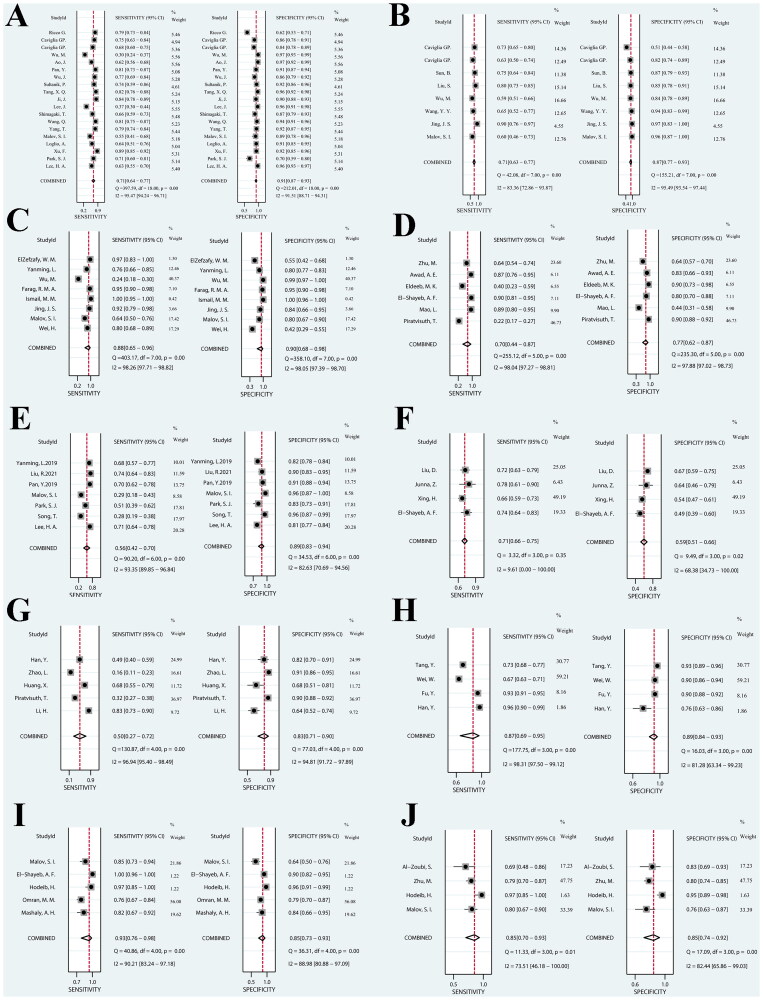
We combined the data from individual diagnostic tests for AFP and data from the study on combined analysis of AFP and other biomarkers. The sensitivity and specificity after combination are shown in Figure 2, and the SROC curve is shown in Figure 3. Forty-three literatures related to AFP in recent 5 years were included in the study. The pooled sensitivity and specificity of AFP were 0.61 and 0.87, respectively. The AUC of AFP were 0.78. To better compare the diagnostic value, we compared the sum of sensitivity and specificity.
Figure 2.
The sensitivity and specificity of AFP and its combined with other biomarkers (A, AFP; B, AFP + AFP-L3; C, AFP + AFP-L3 + DCP; D, AFP + DCP; E, AFP/DCP; F, AFP + GPC3).
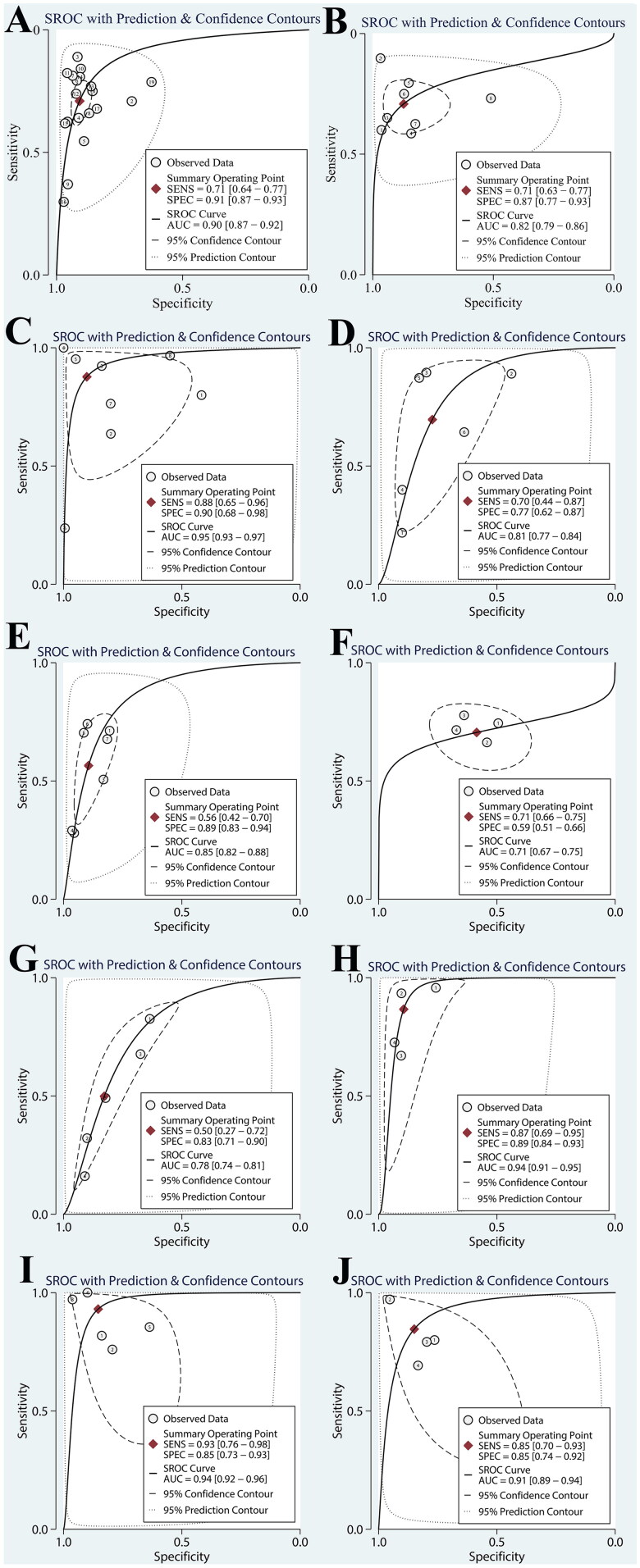
Figure 3.
The SROC curve of AFP and its combined with other biomarkers (A, AFP; B, AFP + AFP-L3; C, AFP + AFP-L3 + DCP; D, AFP + DCP; E, AFP/DCP; F, AFP + GP73).
Among studies on combined analysis of AFP and other biomarkers, the sum of sensitivity and specificity of AFP + AFP-L3 + DCP was significantly higher than that of AFP, as were AFP + DCP, AFP/DCP, and AFP + GPC3. The AUC of AFP + AFP-L3, AFP + AFP-L3 + DCP, AFP + DCP, AFP/DCP, and AFP + GPC3 were higher than that of AFP. The combination of AFP and other biomarkers improved the diagnostic efficiency. AFP + GPC3 had the highest sum of sensitivity and specificity (1.75) and AUC (0.91). The pooled sensitivity, specificity, diagnostic odds ratio, area under the curve, positive likelihood ratio, and negative likelihood ratio are shown in Table 2.
Table 2.
The pooled sensitivity, specificity, diagnostic odds ratio, area under the curve, positive likelihood ratio, and negative likelihood ratio of AFP and AFP combined with other biomarkers.
| Markers | Sensitivity (95% CI) | Specificity (95% CI) | PLR (95% CI) | NLR (95% CI) | DOR (95% CI) | AUC |
|---|---|---|---|---|---|---|
| AFP | 0.61 [0.57, 0.65] | 0.87 [0.83, 0.90] | 4.50 [3.60, 5.80] | 0.45 [0.41, 0.49] | 10.00 [8.00, 13.00] | 0.78 |
| AFP + AFP-L3 | 0.56 [0.45, 0.66] | 0.90 [0.88, 0.92] | 5.80 [4.70, 7.31] | 0.49 [0.39, 0.61] | 12.00 [8.00, 18.00] | 0.90 |
| AFP + AFP-L3 + DCP | 0.62 [0.49, 0.74] | 0.93 [0.84, 0.97] | 9.00 [4.50, 17.90] | 0.40 [0.30, 0.54] | 22.00 [13.00, 38.00] | 0.85 |
| AFP + DCP | 0.81 [0.73, 0.88] | 0.86 [0.75, 0.93] | 6.00 [3.40, 10.60] | 0.21 [0.15, 0.30] | 28.00 [17.00, 47.00] | 0.90 |
| AFP/DCP | 0.80 [0.68, 0.88] | 0.85 [0.74, 0.92] | 5.30 [3.20, 8.90] | 0.24 [0.16, 0.36] | 22.00 [13.00, 38.00] | 0.89 |
| AFP + GPC3 | 0.86 [0.80, 0.90] | 0.89 [0.79, 0.95] | 8.10 [3.80, 17.20] | 0.16 [0.12, 0.22] | 50.00 [20.00, 127.00] | 0.91 |
PLR: positive likelihood ratio; NLR: negative likelihood ratio; DOR: diagnostic odds ratio; CI: confidence interval; AUC: area under the curve.
We used meta-disc software to calculate Spearman’s correlation coefficient values to evaluate the threshold effect. Spearman’s relevance coefficient value was 0.407 (p = 0.154) in AFP, 0.371 (p = 0.468) in AFP + AFP-L3, 0.886 (p = 0.089) in AFP + AFP-L3 + DCP, 0.717 (p = 0.224) in AFP + DCP, 0.714 (p = 0.111) in AFP/DCP, −0.190 (p = 0.651) in AFP + GPC3. There was no threshold effect in the analysis of each group.
Cochran Q test and I-squared test were performed to estimate the existence and severity of heterogeneity. p < 0.1, and I2 > 50% were considered significant manifestations of heterogeneity. It was found that AFP + AFP-L3 + DCP, AFP, AFP + AFP-L3, AFP + DCP, AFP/DCP, and AFP + GPC3 was heterogeneous.
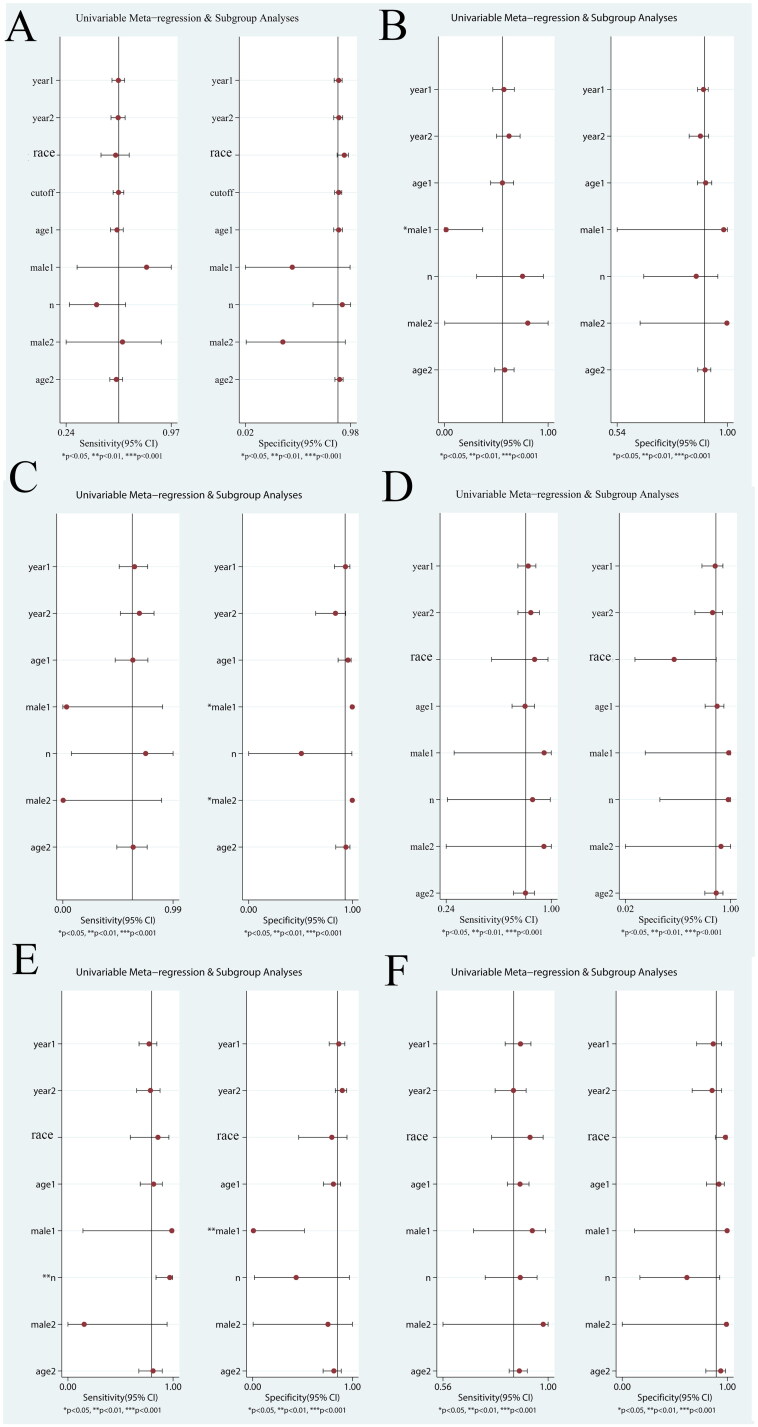
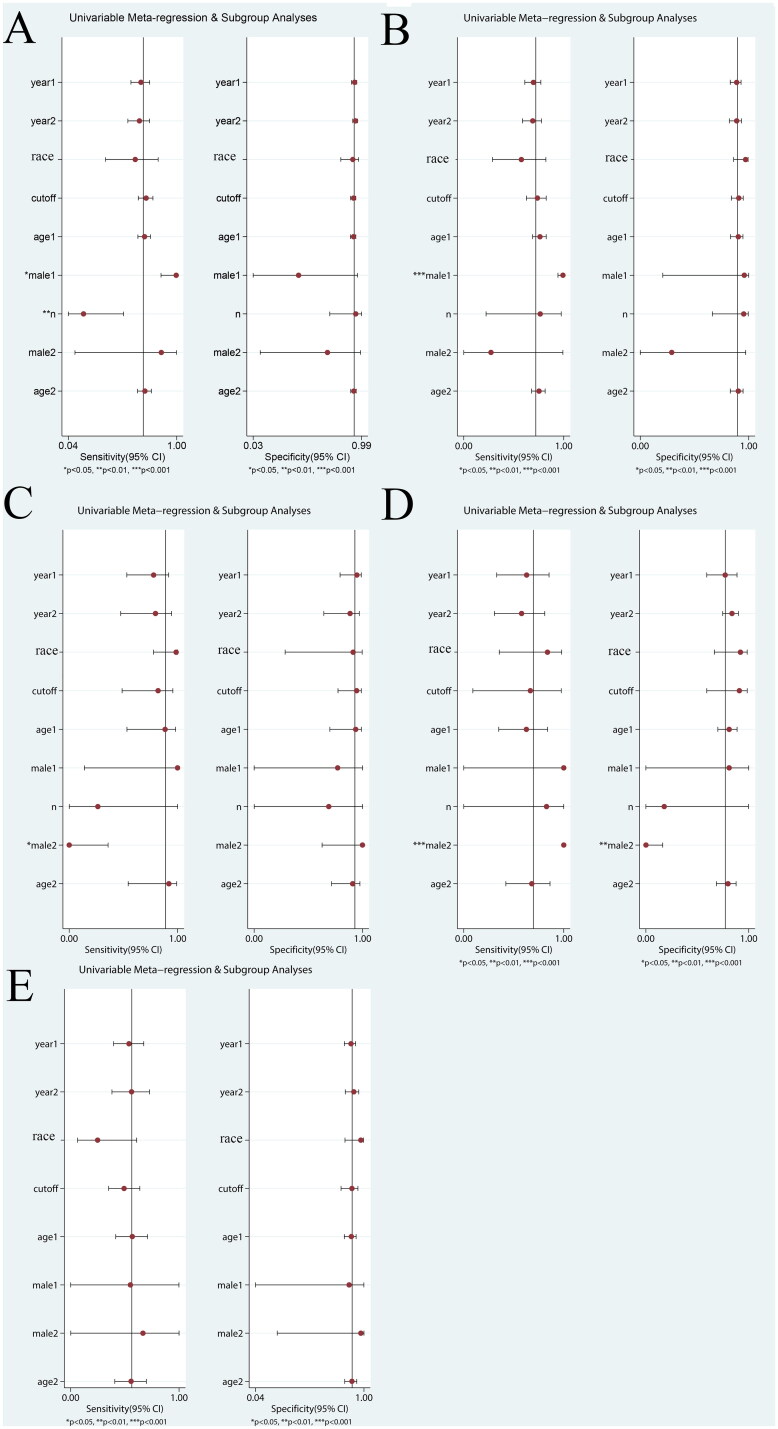
Meta-regression analysis was performed to analyze the sources of heterogeneity. Potential sources of heterogeneity included research time, publication time, race, average age of HCC group, male proportion of HCC group, proportion of early HCC, male proportion of control group, and average age of control group. The source of heterogeneity of AFP also included cut-off values. The inclusion studies of AFP + AFP-L3, and AFP + AFP-L3 + DCP were all from the same race. The results were shown in Figure 4.
Figure 4.
The univariable meta-regression and subgroup analysis of AFP and its combined with other biomarkers (A, AFP; B, AFP + AFP-L3; C, AFP + AFP-L3 + DCP; D, AFP + DCP; E, AFP/DCP; F, AFP + GPC3) (year1, research time; year2, publication time; age1, average age of HCC group; male1, male proportion of HCC group; n, proportion of early HCC; male2, male proportion of control group; age2, average age of control group).
As shown in Figure 4, the meta-regression results of AFP + AFP-L3 showed that the heterogeneity of AFP + AFP-L3 sensitivity may be derived from the male proportion of HCC group, the heterogeneity of AFP + AFP-L3 + DCP specificity may be derived from the male proportion of HCC group and control group, the heterogeneity of AFP/DCP sensitivity may be derived from the early HCC proportion of HCC group, and the heterogeneity of specificity may be derived from the male proportion of HCC group. The source of heterogeneity in other groups was not found.
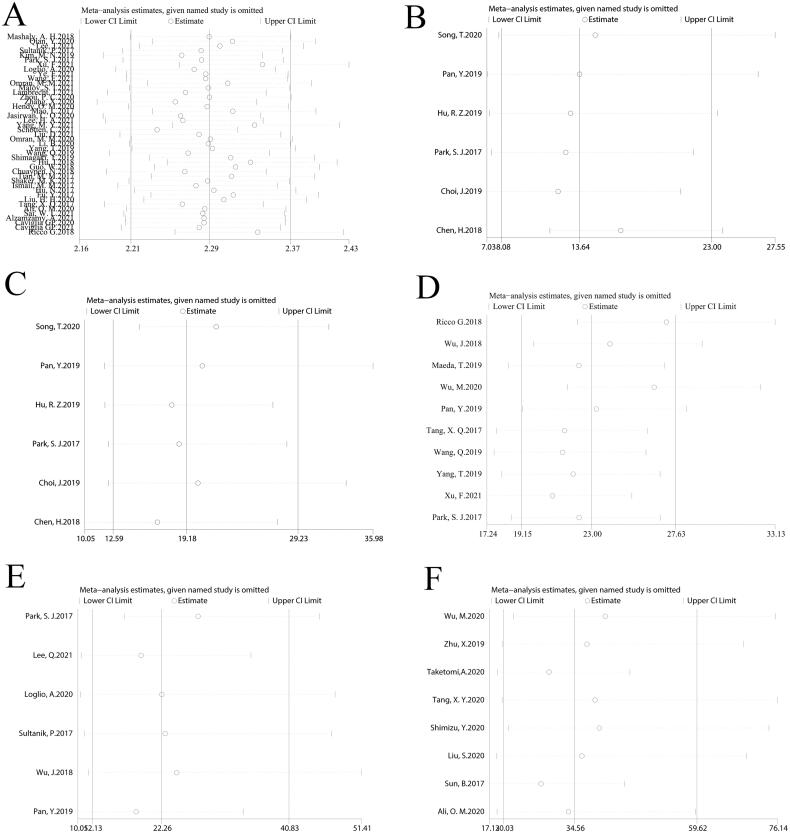
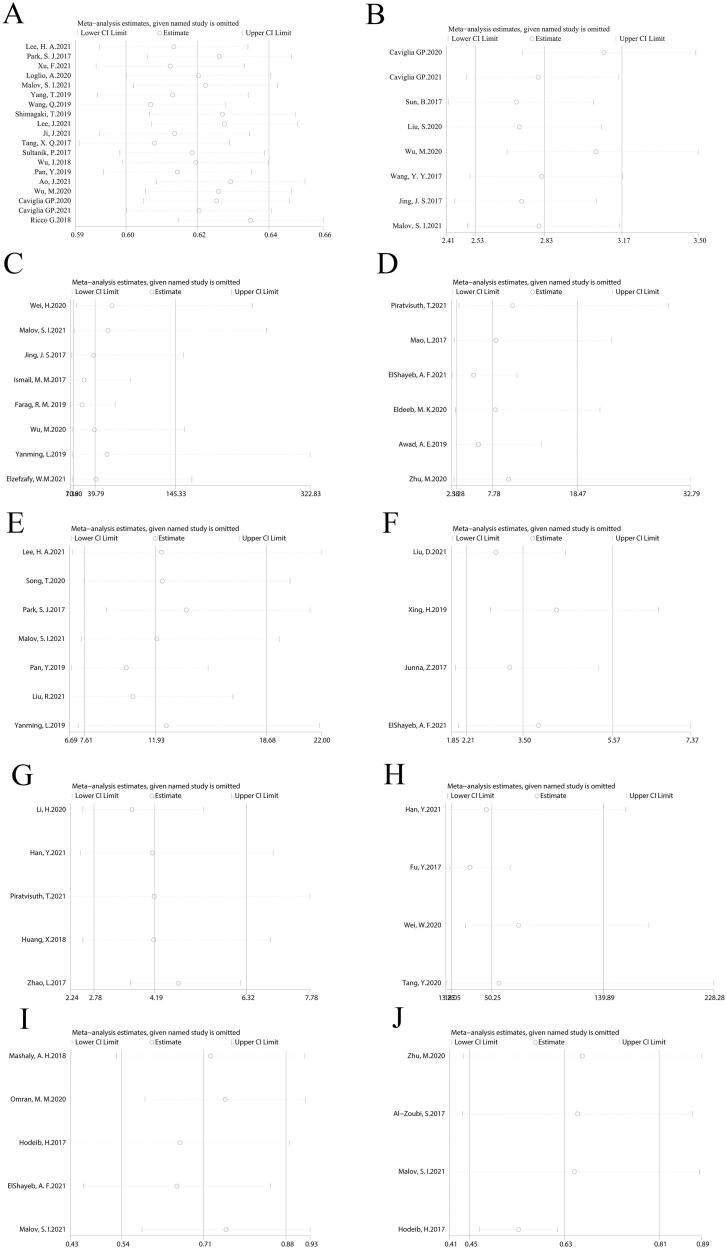
The sensitivity analysis results were shown in Figure 5. It could be seen from the figure that the meta-analysis results of all markers were relatively stable.
Figure 5.
The sensitivity analysis of AFP and its combined with other biomarkers (A, AFP; B, AFP + AFP-L3; C, AFP + AFP-L3 + DCP; D, AFP + DCP; E, AFP/DCP; F, AFP + GPC3).
We used stata software to analyze the potential publication bias of each group. There was no potential publication bias in each group.
3.2. Other biomarkers
Among the 83 literature studies, four were related to AFU, seven were related to AFP-L3, five were related to CA199, 19 were related to DCP, six were related to DKK1, nine were related to GP73, eight were related to GPC3, four were related to Hsp90alpha, five were related to midkine, four were related to OPN, The study ID, region and other research characteristics were summarized in Table 3.
Table 3.
Main characteristics of the included literature related to other biomarkers in this study.
| Markers | Study id [Ref] | Region | Case/control | Sample size (case/control) | TP | FP | FN | TN | Se (%) | Sp (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| DCP | Lee, H. A. 2021 [33] | Korea | HCC/CLD | 160/462 | 100 | 20 | 60 | 442 | 62.50 | 96.00 |
| Park, S. J. 2017 [20] | Korea | HCC/CLD | 79/77 | 56 | 23 | 23 | 54 | 70.89 | 70.13 | |
| Xu, F. 2021 [21] | China | HCC/CLD, BLD | 308/120 | 274 | 10 | 34 | 110 | 89.00 | 91.70 | |
| Loglio, A. 2020 [22] | Italy | HCC/CLD | 64/148 | 41 | 13 | 23 | 135 | 64.00 | 91.00 | |
| Malov, S. I. 2021 [26] | Russia | HCC/CLD | 55/55 | 30 | 6 | 25 | 49 | 54.60 | 88.60 | |
| Yang, T. 2019 [39] | China | HCC/CLD | 289/211 | 229 | 17 | 60 | 194 | 79.00 | 91.90 | |
| Wang, Q. 2019 [40] | China | HCC/CLD | 176/359 | 143 | 23 | 33 | 336 | 81.30 | 93.60 | |
| Shimagaki, T. 2019 [41] | Japan | HCC/CLD | 185/108 | 122 | 14 | 63 | 94 | 66.00 | 87.00 | |
| Lee, J. 2021 [17] | Korea | HCC/CLD | 184/134 | 68 | 6 | 116 | 128 | 37.00 | 95.50 | |
| Ji, J. 2021 [72] | China | HCC/CLD | 183/601 | 154 | 58 | 29 | 543 | 84.08 | 90.43 | |
| Tang, X. Q. 2017 [51] | China | HCC/CLD | 176/190 | 145 | 8 | 31 | 182 | 82.40 | 95.90 | |
| Sultanik, P. 2017 [18] | France | HCC/CLD | 46/116 | 34 | 9 | 12 | 107 | 74.00 | 92.00 | |
| Wu, J. 2018 [65] | China | HCC/CLD, HC | 143/131 | 110 | 18 | 33 | 113 | 76.92 | 86.26 | |
| Pan, Y. 2019 [59] | China | HCC/CLD, HC | 125/280 | 101 | 26 | 24 | 254 | 80.80 | 90.70 | |
| Ao, J. 2021 [73] | Japan | HCC/CLD, HC | 275/118 | 170 | 4 | 105 | 114 | 61.80 | 96.90 | |
| Wu, M. 2020 [63] | China | HCC/CLD, HC | 198/176 | 59 | 5 | 139 | 171 | 29.80 | 97.20 | |
| Caviglia GP. 2020 [57] | Italy | HCC/HC | 149/200 | 101 | 32 | 48 | 168 | 68.00 | 84.00 | |
| Caviglia GP. 2021 [56] | Italy | HCC/CLD | 72/119 | 54 | 17 | 18 | 102 | 75.00 | 85.70 | |
| Ricco G. 2018 [55] | Italy | HCC/CLD | 258/130 | 203 | 49 | 55 | 81 | 78.70 | 62.50 | |
| GPC3 | Malov, S. I. 2021 [26] | Russia | HCC/CLD | 55/55 | 33 | 2 | 22 | 53 | 60.00 | 96.40 |
| Jing, J. S. 2017 [74] | China | HCC/CLD | 39/31 | 35 | 1 | 4 | 30 | 89.70 | 96.77 | |
| Wang, Y. Y. 2017 [75] | China | HCC/CLD | 60/50 | 39 | 3 | 21 | 47 | 65.00 | 94.00 | |
| Wu, M. 2020 [63] | China | HCC/CLD, HC | 198/176 | 116 | 28 | 82 | 148 | 58.60 | 84.40 | |
| Liu, S. 2020 [71] | China | HCC/HC | 210/134 | 167 | 20 | 43 | 114 | 79.52 | 85.07 | |
| Sun, B. 2017 [7] | China | HCC/CLD, HC | 76/100 | 57 | 13 | 19 | 87 | 75.00 | 87.00 | |
| Caviglia GP. 2020 [57] | Italy | HCC/HC | 149/200 | 109 | 98 | 40 | 102 | 73.00 | 51.00 | |
| Caviglia GP. 2021 [56] | Italy | HCC/CLD | 72/119 | 45 | 21 | 27 | 98 | 62.50 | 82.40 | |
| GP73 | Wei, H. 2020 [76] | China | HCC/CLD | 60/60 | 48 | 35 | 12 | 25 | 80.00 | 41.70 |
| Malov, S. I. 2021 [26] | Russia | HCC/CLD | 55/55 | 35 | 11 | 20 | 44 | 63.60 | 80.00 | |
| Jing, J. S. 2017 [74] | China | HCC/CLD | 39/31 | 36 | 5 | 3 | 26 | 92.31 | 83.87 | |
| Ismail, M. M. 2017 [47] | Saudi Arabia | HCC/CLD | 66/99 | 66 | 0 | 0 | 99 | 100.00 | 100.00 | |
| Farag, R. M. 2019 [77] | Saudi Arabia | HCC/CLD, HC | 145/155 | 138 | 8 | 7 | 147 | 95.00 | 95.00 | |
| Wu, M. 2020 [63] | China | HCC/CLD, HC | 198/176 | 47 | 1 | 151 | 175 | 23.70 | 99.40 | |
| Yanming, L. 2019 [78] | China | HCC/CLD, HC | 93/628 | 71 | 125 | 22 | 503 | 76.34 | 80.09 | |
| Elzefzafy, W.M. 2021 [79] | Egypt | HCC/CLD, HC | 30/60 | 29 | 27 | 1 | 33 | 95.00 | 55.00 | |
| DKK1 | Piratvisuth, T. 2022 [80] | Thailand | HCC/CLD | 308/773 | 67 | 77 | 241 | 696 | 21.60 | 90.00 |
| Mao, L. 2017 [31] | China | HCC/CLD | 82/57 | 73 | 32 | 9 | 25 | 89.02 | 43.86 | |
| ElShayeb, A. F. 2021 [81] | Egypt | HCC/CLD | 86/89 | 77 | 18 | 9 | 71 | 89.00 | 80.00 | |
| Eldeeb, M. K. 2020 [82] | Egypt | HCC/CLD | 30/30 | 12 | 3 | 18 | 27 | 40.00 | 90.00 | |
| Awad, A. E. 2019 [83] | Egypt | HCC/CLD, HC | 55/35 | 48 | 6 | 7 | 29 | 87.30 | 82.90 | |
| Zhu, M. 2020 [8] | China | HCC/CLD | 101/221 | 65 | 80 | 36 | 141 | 64.36 | 63.80 | |
| AFP-L3 | Lee, H. A. 2021 [33] | Korea | HCC/CLD | 160/462 | 114 | 90 | 46 | 372 | 71.30 | 81.00 |
| Song, T. 2020 [58] | China | HCC/CLD | 100/67 | 28 | 3 | 72 | 64 | 28.30 | 95.50 | |
| Park, S. J. 2017 [20] | Korea | HCC/CLD | 79/77 | 40 | 13 | 39 | 64 | 50.63 | 83.12 | |
| Malov, S. I. 2021 [26] | Russia | HCC/CLD | 55/55 | 16 | 2 | 39 | 53 | 29.10 | 96.40 | |
| Pan, Y. 2019 [59] | China | HCC/CLD, HC | 125/280 | 88 | 24 | 37 | 256 | 70.40 | 91.40 | |
| Liu, R. 2021 [84] | China | HCC/CLD, HC | 89/119 | 66 | 12 | 23 | 107 | 74.20 | 89.90 | |
| Yanming, L. 2019 [78] | China | HCC/CLD, HC | 93/628 | 63 | 116 | 30 | 512 | 67.74 | 81.52 | |
| AFU | Liu, D. 2021 [36] | China | HCC/CLD | 123/143 | 88 | 47 | 35 | 96 | 71.50 | 67.10 |
| Xing, H. 2019 [85] | China | HCC/CLD | 187/214 | 124 | 98 | 63 | 116 | 66.31 | 54.21 | |
| Junna, Z. 2017 [10] | China | HCC/HC | 36/36 | 28 | 13 | 8 | 23 | 78.00 | 64.00 | |
| ElShayeb, A. F. 2021 [81] | Egypt | HCC/CLD | 86/89 | 64 | 45 | 22 | 44 | 74.00 | 50.00 | |
| CA199 | Li, H. 2020 [11] | China | HCC/CLD | 86/85 | 71 | 31 | 15 | 54 | 82.94 | 63.95 |
| Han, Y. 2021 [86] | China | HCC/CH, BLD | 118/62 | 58 | 11 | 60 | 51 | 48.90 | 81.50 | |
| Piratvisuth, T. 2022 [80] | Thailand | HCC/CLD | 308/773 | 99 | 77 | 209 | 696 | 32.00 | 90.00 | |
| Huang, X. 2018 [87] | China | HCC/CH | 62/40 | 42 | 13 | 20 | 27 | 68.43 | 68.36 | |
| Zhao, L. 2017 [88] | China | HCC/CH, BLD | 149/178 | 24 | 16 | 125 | 162 | 16.10 | 90.80 | |
| Hsp90alpha | Han, Y. 2021 [86] | China | HCC/CH, BLD | 118/62 | 113 | 15 | 5 | 47 | 95.70 | 75.00 |
| Fu, Y. 2017 [49] | China | HCC/CLD, HC | 531/743 | 496 | 72 | 35 | 671 | 93.32 | 90.27 | |
| Wei, W. 2020 [13] | China | HCC/HC | 659/230 | 442 | 22 | 217 | 208 | 67.07 | 90.43 | |
| Tang, Y. 2020 [89] | China | HCC/CH, BLD | 409/179 | 297 | 12 | 112 | 167 | 72.60 | 93.30 | |
| Midkine | Mashaly, A. H. 2018 [14] | Egypt | HCC/CLD | 44/31 | 36 | 5 | 8 | 26 | 81.82 | 83.87 |
| Omran, M. M. 2020 [37] | Egypt | HCC/CLD | 104/92 | 79 | 19 | 25 | 73 | 76.00 | 79.00 | |
| Hodeib, H. 2017 [90] | Egypt | HCC/CLD, HC | 35/105 | 34 | 4 | 1 | 101 | 98.40 | 96.20 | |
| ElShayeb, A. F. 2021 [81] | Egypt | HCC/CLD | 86/89 | 86 | 9 | 0 | 80 | 100.00 | 90.00 | |
| Malov, S. I. 2021 [26] | Russia | HCC/CLD | 55/55 | 47 | 20 | 8 | 35 | 85.50 | 63.60 | |
| OPN | Zhu, M. 2020 [8] | China | HCC/CLD | 101/221 | 80 | 45 | 21 | 176 | 79.21 | 79.64 |
| Al-Zoubi, S. 2017 [91] | Syria | HCC/CLD, HC | 26/42 | 18 | 7 | 8 | 35 | 69.00 | 84.00 | |
| Malov, S. I. 2021 [26] | Russia | HCC/CLD | 55/55 | 44 | 13 | 11 | 42 | 80.00 | 76.60 | |
| Hodeib, H. 2017 [90] | Egypt | HCC/CLD, HC | 35/105 | 34 | 5 | 1 | 100 | 97.10 | 95.30 |
CLD: chronic liver disease; BLD: benign liver disease; HC: healthy control; CH: cirrhosis; TP: true positive; FP: false positive; FN: false negative; TN: true negative; Se: sensitivity; Sp: specificity; Ref: reference.
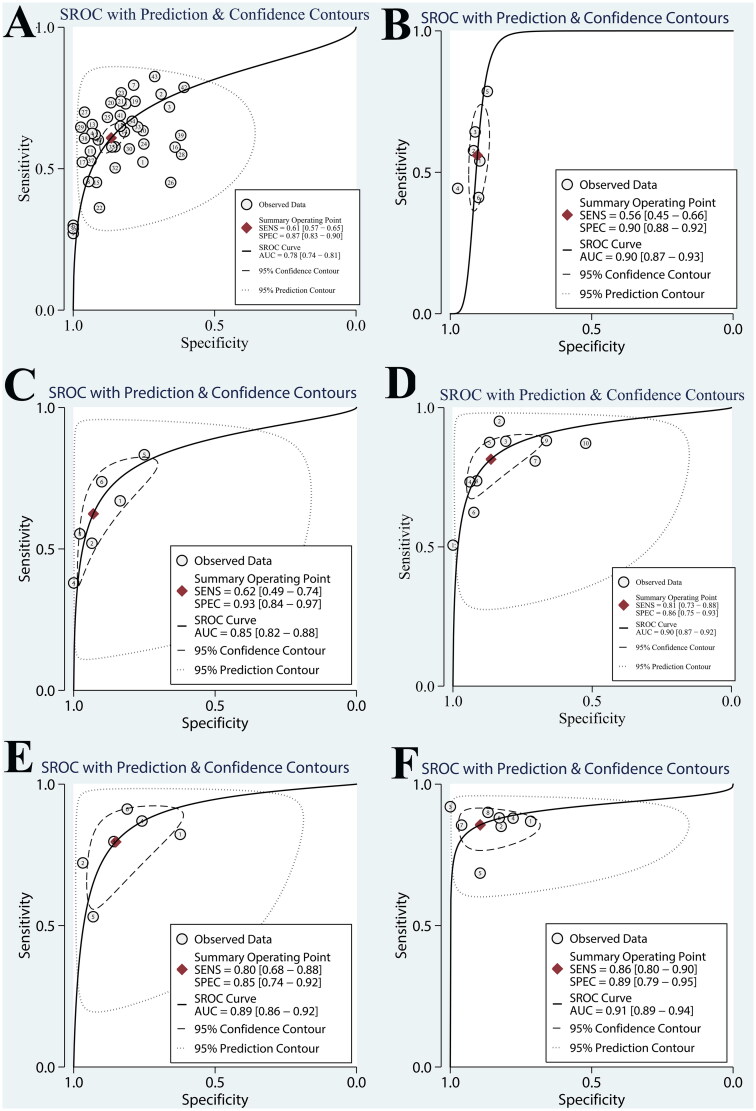
We combined the data from individual diagnostic tests for 10 biomarkers. The sensitivity and specificity after combination are shown in Figure 6, and the SROC curve is shown in Figure 7. Compared to AFP, the sum of sensitivity and specificity of DCP was significantly higher, as were GPC3, GP73, Hsp90alpha, midkine, and OPN. In addition, Midkine and GP73 had the highest sum of sensitivity and specificity (1.78).
Figure 6.
The sensitivity and specificity of other biomarkers (A, DCP; B, GPC3; C, GP73; D, DK-K1; E, AFP-L3; F, AFU; G, CA199; H, Hsp90alpha; I, Midkine, J, OPN).
Figure 7.
The SROC curve of other biomarkers (A, DCP; B, GPC3; C, GP73; D, DK-K1; E, AFP-L3; F, AFU; G, CA199; H, Hsp90alpha; I, Midkine, J, OPN).
Taking AFP as the reference, the results showed that the AUC of DCP, GPC3, GP73, DKK1, AFP-L3, Hsp90alpha, Midkine, and OPN were significantly higher than that of AFP. The AUC of GP73 (0.95) was the highest. The pooled sensitivity, specificity, diagnostic odds ratio, area under the curve, positive likelihood ratio, and negative likelihood ratio are shown in Table 4.
Table 4.
The pooled sensitivity, specificity, diagnostic odds ratio, area under the curve, positive likelihood ratio, and negative likelihood ratio of other biomarkers.
| Markers | Sensitivity (95% CI) | Specificity (95% CI) | PLR (95% CI) | NLR (95% CI) | DOR (95% CI) | AUC |
|---|---|---|---|---|---|---|
| DCP | 0.71 [0.64, 0.77] | 0.91 [0.87, 0.93] | 7.8 [5.70, 10.50] | 0.32 [0.26, 0.40] | 24.00 [16.00, 36.00] | 0.90 |
| GPC3 | 0.71 [0.63, 0.77] | 0.87 [0.77, 0.93] | 5.50 [2.90, 10.40] | 0.33 [0.26, 0.43] | 17.00 [7.00, 37.00] | 0.82 |
| GP73 | 0.88 [0.65, 0.96] | 0.90 [0.68, 0.98] | 8.90 [2.30, 33.90] | 0.14 [0.04, 0.45] | 66.00 [9.00, 502.00] | 0.95 |
| DKK1 | 0.70 [0.44, 0.87] | 0.77 [0.62, 0.87] | 3.10 [2.00, 4.80] | 0.39 [0.20, 0.77] | 8.00 [3.00, 18.00] | 0.81 |
| AFP-L3 | 0.56 [0.42, 0.70] | 0.89 [0.83, 0.94] | 5.40 [3.70, 7.70] | 0.49 [0.36, 0.66] | 11.00 [7.00, 18.00] | 0.85 |
| AFU | 0.71 [0.66, 0.75] | 0.59 [0.51, 0.66] | 1.70 [1.40, 2.10] | 0.50 [0.40, 0.63] | 3.00 [2.00, 5.00] | 0.71 |
| CA199 | 0.50 [0.27, 0.72] | 0.83 [0.71, 0.90] | 2.90 [2.40, 3.50] | 0.61 [0.42, 0.88] | 5.00 [3.00, 7.00] | 0.78 |
| Hsp90alpha | 0.87 [0.69, 0.95] | 0.89 [0.84, 0.93] | 8.20 [5.60, 11.90] | 0.15 [0.06, 0.37] | 55.00 [24.00, 126.00] | 0.94 |
| Midkine | 0.93 [0.76, 0.98] | 0.85 [0.73, 0.93] | 6.40 [3.10, 13.30] | 0.08 [0.02, 0.33] | 78.00 [11.00, 582.00] | 0.94 |
| OPN | 0.85 [0.70, 0.93] | 0.85 [0.74, 0.92] | 5.60 [2.80, 11.40] | 0.18 [0.08, 0.41] | 31.00 [7.00, 137.00] | 0.91 |
PLR: positive likelihood ratio; NLR: negative likelihood ratio; DOR: diagnostic odds ratio; CI: confidence interval; AUC: area under the curve.
Spearman’s relevance coefficient value was 0.000 (p = 1.000) in AFU, 0.571 (p = 0.180) in AFP-L3, 1.220 (p = 0.230) in CA199, 0.207 (p = 0.395) in DCP, 0.714 (p = 0.111) in DKK1, −0.143 (p = 0.736) in GP73, −0.286 (p = 0.493) in GPC3, 0.800 (p = 0.200) in Hsp90alpha, −0.600 (p = 0.285) in Midkine, −0.200 (p = 0.800) in OPN. There was no threshold effect in the analysis of each group.
Cochran Q test and I-squared test were performed to estimate the existence and severity of heterogeneity. It was found that AFU, AFP-L3, CA199, DCP, DKK1, GP73, GPC3, Hsp90alpha, Midkine, OPN was heterogeneous.
Meta-regression analysis was performed to analyze the sources of heterogeneity of meta-analysis involving more than five articles. Potential sources of heterogeneity included research time, publication time, race, cut-off values, average age of HCC group, male proportion of HCC group, proportion of early HCC, male proportion of control group, and average age of control group.
As shown in Figure 8, the meta-regression results showed that the heterogeneity of DCP sensitivity may be derived from the male proportion of HCC group and the early HCC proportion of HCC group, the heterogeneity of GPC3 sensitivity may be derived from the male proportion of HCC group, the heterogeneity of GP73 sensitivity may be derived from the male proportion of control group, the heterogeneity of DKK1 sensitivity and specificity may be derived from the male proportion of control group. The source of heterogeneity in other groups was not found.
Figure 8.
The univariable meta-regression and subgroup analysis of other biomarkers (A, DCP; B, GPC3; C, GP73; D, DKK1; E, AFP-L3) (year1, research time; year2, publication time; age1, average age of HCC group; male1, male proportion of HCC group; n, proportion of early HCC; male2, male proportion of control group; age2, average age of control group).
The sensitivity analysis results are shown in Figure 9. It could be seen from the figure that the meta-analysis results of all markers were relatively stable.
Figure 9.
The sensitivity analysis of other biomarkers (A, DCP; B, GPC3; C, GP73; D, DK-K1; E, AFP-L3; F, AFU; G, CA199; H, Hsp90alpha; I, Midkine, J, OPN).
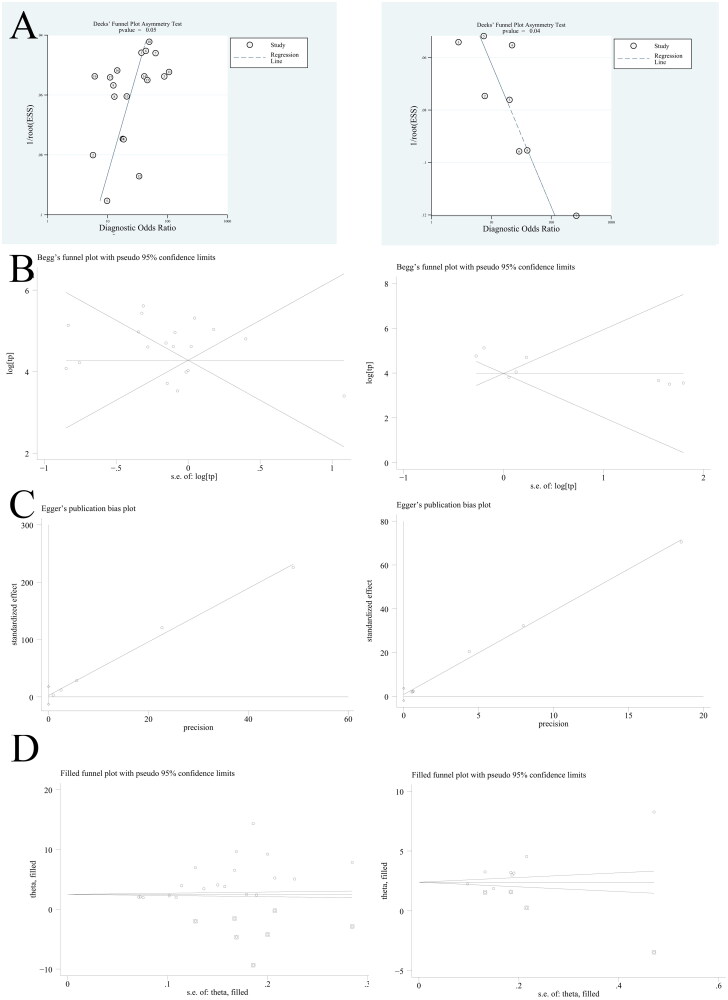
We used Deeks’ funnel plot to analyze the potential publication bias of each group. Among the analysis of each group, DCP (p = 0.05) and GPC3 (p = 0.04) have potential publication bias. For the publication bias test results of DCP and GPC3, we further tested the publication bias by using Egger’ funnel plot, Begger’ funnel plot, trim and fill methods. The results are shown in Figure 10.
Figure 10.
Publication bias analysis of DCP and GPC3 (A, Deeks’ funnel plot; B, Beggs’ funnel plot; C, Egger’ funnel plot; D, filled funnel plot) (Left, DCP; Right, GPC3).
As shown in Figure 10, the Egger test result of DCP is p = 0.50, and the Egger test result of GPC3 is p = 0.286. We analyzed the analysis results of DCP and GPC3 by the trim and fill method. Seven studies were added to DCP. The combined RR value and 95% effect interval before repair were 5.003 (3.766, 6.240), and the combined RR value and 95% effect interval after repair were 14.885 (3.523, 62.893). Four studies were added to GPC3. The combined RR value and 95% effect interval before repair were 3.606 (2.864, 4.348), and the combined RR value and 95% effect interval after repair were 11.676 (5.443, 25.047). The combined RR value before and after repair showed no significant impact on the study.
4. Discussion
The early diagnosis is the key to the treatment of HCC. AFP, as the most commonly used clinical biomarker of HCC, has been questioned for its diagnostic value. However, there is no ideal recognized biomarker of HCC at present [92]. There are more and more studies on new biomarkers with better diagnostic value for HCC, lack of scientific evaluation yet. In view of this, we tried to use meta-analysis to compare 11 biomarkers of HCC which were played more attention by public. According to our investigation, there are few such studies to conduct such a wide range of literature research, screen and evaluate so many biomarkers at the same time.
The pooled sensitivity and specificity of AFP were 0.61 and 0.87, respectively, which were consistent with the results of previous studies. It was found that the combination of AFP and other biomarkers improved the diagnostic efficiency. The sum of sensitivity and specificity of AFP + GP73 was the highest (1.75), and AUC was the highest (0.91) as well.
The sum of sensitivity and specificity of DCP was significantly higher than that of AFP, as were GPC3, GP73, Hsp90alpha, midkine, and OPN. Midkine and GP73 had the highest sum of sensitivity and specificity (1.78), higher than AFP + GP73 in the combination diagnosis of AFP and other biomarkers of HCC. The AUC of DCP, GPC3, GP73, DKK1, AFP-L3, Hsp90alpha, midkine, and OPN were significantly higher than that of AFP and GP73’s (0.95) was the highest. It indicated the above biomarkers had higher diagnostic value for HCC, and expected to become ideal biomarkers for HCC diagnosis, worthy of further research.
GP73 was a type II transmembrane glycoprotein that existed in Golgi apparatus. It was generally believed that GP73 was mainly expressed in bile duct epithelial cells in normal liver, with no or only a small amount of expression in hepatocytes and low serum GP73 level; However, hepatocytes in patients with liver cancer produced a large amount of GP73 and further release it into serum, resulting in a significant increase in serum GP73 level [90].
As a potential biomarker of tumour diagnosis and prognosis, GP73 had become a research hotspot. Previous studies had shown that in the diagnosis of early HCC, the sensitivity of GP73 was 62%, which was much higher than that of AFP (sensitivity was 25%), indicating that GP73 was better than AFP in the diagnosis of early HCC [89]. In a study on the population of China, it was found that the serum GP73 level of liver cancer patients infected with hepatitis B virus was the highest in all detection groups [93]. According to this study, it was shown that in the study, GP73 had the highest AUC (0.95), and sum of sensitivity and specificity (1.78). The data of this study shows that GP73 has the best diagnostic value. but the number of relevant research cases was small, which still needed a lot of clinical data for further support.
The diagnostic value of individual biomarker may not be significantly different from that of multi-biomarker combined assays. Perhaps we can find enough good biomarkers from an individual biomarker instead of focusing on multi-biomarker combined assays.
A large number of case–control studies investigated the diagnostic accuracy of serologic biomarkers; However, only few studies investigated the predictiveness of these biomarkers. Serologic biomarkers that monitor the risk stratification of HCC development in patients are crucial to personalize surveillance strategies and thus to improve early HCC detection by optimizing resource allocation.
Loglio et al. reported that in Caucasian patients with HBV compensatory cirrhosis who received long-term NUC treatment, AFP higher than 7 ng/mL showed excellent specificity (99.6%), indicating the occurrence of HCC within a year [94]. El-Derany MO reported HCC development in NASH was associated with higher serum AFP, IL-13 levels [95]. Choi et al. found that the level of DCP in HCC patients began to increase half a year before diagnosis, and the level of AFP-L3 began to increase one year before diagnosis, but there was no significant change in the control group [61]. Li et al. found that the AFP, AFP-L3, ALT, and AFP-L3/AFP increased significantly in patients with HCC 3 years before the diagnosis of HCC [96]. Shakado suggested that the elevation of AFP and DCP levels at 24 weeks after the completion of IFN and ribavirin therapy were strongly associated with the incidence of HCC irrespective of virological response among Japanese hepatitis C virus-related liver cirrhosis patients [97]. Gatselis et al. reported that the combination of GP73 and the cartilage oligomeric matrix protein (COMP) seems efficient to detect the development of HCC in patients with chronic liver diseases [98].
5. Conclusions
The pooled sensitivity and specificity of AFP were 0.61 and 0.87, respectively. The AUC of AFP were 0.78. The combination of AFP and other biomarkers improved the diagnostic efficiency. The diagnostic value of biomarkers including DCP, GPC3, GP73, Hsp90alpha, midkine, OPN was higher than that of AFP. GP73 had the best diagnostic value for HCC with the highest sum of sensitivity and specificity (1.78) and AUC (0.95).
Funding Statement
This study was funded by The National Key R&D Program of China (2017YFC1700305).
Author contributions
All authors provided substantial intellectual contribution to the study to qualify for authorship. Bingyao Pang, Yan Leng, and Lihong Jiang conceived the study design. Bingyao Pang, Xiaoli Wang, and Yiqiang Wang collected and processed the data. Bingyao Pang and Yan Leng prepared the manuscript. Bingyao Pang, Yan Leng, and Lihong Jiang edited the manuscript and provided valuable comments. Bingyao Pang, Yan Leng, and Lihong Jiang approved the final version to be published. All authors read and approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article.
References
- 1.Liu J, Kuang S, Zheng Y, et al. Prognostic and predictive significance of the tumor microenvironment in hepatocellular carcinoma. Cancer Biomark. 2021;32(1):99–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Debes JD, Romagnoli PA, Prieto J, et al. Serum biomarkers for the prediction of hepatocellular carcinoma. Cancers. 2021;13(7):1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campion D, Tucci A, Ponzo P, et al. Non-invasive biomarkers for the detection of hepatocellular carcinoma. Minerva Biotecnol. 2019;31(1):43–44. [Google Scholar]
- 4.Guarneri V, Loggi E, Serra C, et al. Diagnostic performance of PIVKA-II in patients with hepatocellular carcinoma. J Hepatol. 2020;73:S631–S632. [Google Scholar]
- 5.Mohamed AA, Ghanem HM, Kamal MM, et al. Dickkopf-1 and β-catenin as biomarkers for early diagnosis of hepato-cellular carcinoma. CCTR. 2020;16(2):136–144. [Google Scholar]
- 6.Shaker MK, Attia FM, Hassan AA, et al. Evaluation of golgi protein 73 (GP73) as a potential biomarkers for hepatocellular carcinoma. Clin Lab. 2020;66(8). [DOI] [PubMed] [Google Scholar]
- 7.Sun B, Huang Z, Wang B, et al. Significance of glypican-3 (GPC3) expression in hepatocellular cancer diagnosis. Med Sci Monit. 2017;23:850–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu M, Zheng J, Wu F, et al. OPN is a promising serological biomarker for hepatocellular carcinoma diagnosis. J Med Virol. 2020;92(12):3596–3603. [DOI] [PubMed] [Google Scholar]
- 9.Unić A, Derek L, Duvnjak M, et al. Diagnostic specificity and sensitivity of PIVKAII, GP3, CSTB, SCCA1 and HGF for the diagnosis of hepatocellular carcinoma in patients with alcoholic liver cirrhosis. Ann Clin Biochem. 2018;55(3):355–362. [DOI] [PubMed] [Google Scholar]
- 10.Junna Z, Gongde C, Jinying X, et al. Serum AFU, 5′-NT and AFP as biomarkers for primary hepatocellular carcinoma diagnosis. Open Med. 2017;12:354–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li H, Liu Z, Han C.. Role of AFP, AFP-L3, PIVKA-II, and CA199 in diagnosis and prognosis evaluation of liver cancer. Int J Clin Exp Med. 2020;13:9778–9785. [Google Scholar]
- 12.Topolcan O, Kucera R, Karlikova M, et al. Biomarkers and liver cancer process. Tumor Biol. 2019;41:22. [Google Scholar]
- 13.Wei W, Liu M, Ning S, et al. Diagnostic value of plasma HSP90α levels for detection of hepatocellular carcinoma. BMC Cancer. 2020;20(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mashaly AH, Anwar R, Ebrahim MA, et al. Diagnostic and prognostic value of Talin-1 and Midkine as tumor markers in hepatocellular carcinoma in Egyptian patients. Asian Pac J Cancer Prev. 2018;19:1503–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Song X, Wu A, Ding Z, et al. Soluble Axl is a novel diagnostic biomarker of hepatocellular carcinoma in Chinese patients with chronic hepatitis B virus infection. Cancer Res Treat. 2020;52(3):789–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qian Y, Wang JW, Yu F, et al. Measurement of cyclin D2 (CCND2) gene promoter methylation in plasma and peripheral blood mononuclear cells and alpha-fetoprotein levels in patients with hepatitis B virus-associated hepatocellular carcinoma. Med Sci Monit. 2020;26:e927444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee J, Lim YS, Lee JH, et al. Inclusive quantification assay of serum des-γ-carboxyprothrombin proteoforms for hepatocellular carcinoma surveillance by targeted mass spectrometry. Hepatol Commun. 2021;5(10):1767–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sultanik P, Ginguay A, Vandame J, et al. Diagnostic accuracy of des-gamma-carboxy prothrombin for hepatocellular carcinoma in a French cohort using the Lumipulse® G600 analyzer. J Viral Hepat. 2017;24(1):80–85. [DOI] [PubMed] [Google Scholar]
- 19.Kim MN, Kim BK, Kim SU, et al. Longitudinal assessment of alpha-fetoprotein for early detection of hepatocellular carcinoma in patients with cirrhosis. Scand J Gastroenterol. 2019;54(10):1283–1290. [DOI] [PubMed] [Google Scholar]
- 20.Park SJ, Jang JY, Jeong SW, et al. Usefulness of AFP, AFP-L3, and PIVKA-II, and their combinations in diagnosing hepatocellular carcinoma. Medicine. 2017;96(11):e5811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu F, Zhang L, He W, et al. The diagnostic value of serum PIVKA-II alone or in combination with AFP in Chinese hepatocellular carcinoma patients. Dis Markers. 2021;2021:8868370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loglio A, Iavarone M, Facchetti F, et al. The combination of PIVKA-II and AFP improves the detection accuracy for HCC in HBV Caucasian cirrhotics on long-term oral therapy. Liver Int. 2020;40(8):1987–1996. [DOI] [PubMed] [Google Scholar]
- 23.Ye F, Huang W, Xue Y, et al. Serum levels of itgbl1 as an early diagnostic biomarker for hepatocellular carcinoma with hepatitis B virus infection. J Hepatocell Carcinoma. 2021;8:285–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang F, Liu H, Bai Y, et al. Performance of SPINK1 and SPINK1-based diagnostic model in detection of hepatocellular carcinoma. J Clin Lab Anal. 2021;35(11):e24025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Omran MM, Mosaad S, Emran TM, et al. A novel model based on interleukin 6 and insulin-like growth factor II for detection of hepatocellular carcinoma associated with hepatitis C virus. J Genet Eng Biotechnol. 2021;19(1):168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malov SI, Malov IV, Kuvshinov AG, et al. Search for effective serum tumor markers for early diagnosis of hepatocellular carcinoma associated with hepatitis. Sovrem Tekhnologii Med. 2021;13(1):27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lambrecht J, Porsch-Özçürümez M, Best J, et al. The Apac score: a novel and highly performant serological tool for early diagnosis of hepatocellular carcinoma in patients with liver cirrhosis. J Clin Med. 2021;10(15):3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou PC, Sun LQ, Shao L, et al. Establishment of a pattern recognition metabolomics model for the diagnosis of hepatocellular carcinoma. World J Gastroenterol. 2020;26(31):4607–4623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X, Wang T, Zhang KH, et al. Simple clinical metrics enhance AFP to effectively identify cirrhotic patients with complicating hepatocellular carcinoma at various AFP levels. Front Oncol. 2020;9:1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hendy OM, El-Aarag B, Abdel-Samiee M.. Latent transforming growth factor-beta binding protein 1: molecular diagnostic marker for hepatocellular carcinoma in Egyptian patients. Hepatol Int. 2020;14:S251–S252. [Google Scholar]
- 31.Mao L, Wang Y, Wang D, et al. TEMs but not DKK1 could serve as complementary biomarkers for AFP in diagnosing AFP-negative hepatocellular carcinoma. PLOS One. 2017;12(9):e0183880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jasirwan COM, Fahira A, Siregar L, et al. The alpha-fetoprotein serum is still reliable as a biomarker for the surveillance of hepatocellular carcinoma in Indonesia. BMC Gastroenterol. 2020;20(1):215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee HA, Lee YR, Lee YS, et al. Lens culinaris agglutinin-reactive fraction of alpha-fetoprotein improves diagnostic accuracy for hepatocellular carcinoma. World J Gastroenterol. 2021;27(28):4687–4696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang MY, Wu F, Fang F, et al. Serum epidermal growth factor-like domain 7 serves as a novel diagnostic marker for early hepatocellular carcinoma. BMC Cancer. 2021;21(1):772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schotten C, Ostertag B, Sowa JP, et al. Galad score detects early-stage hepatocellular carcinoma in a European cohort of chronic hepatitis B and C patients. Pharmaceuticals. 2021;14(8):735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu D, Luo Y, Chen L, et al. Diagnostic value of 5 serum biomarkers for hepatocellular carcinoma with different epidemiological backgrounds: a large-scale, retrospective study. Cancer Biol Med. 2021;18(1):256–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Omran MM, Farid K, Omar MA, et al. A combination of α-fetoprotein, midkine, thioredoxin and a metabolite for predicting hepatocellular carcinoma. Cells. 2020;19:179–185. [DOI] [PubMed] [Google Scholar]
- 38.Li B, Huang H, Huang R, et al. SEPT9 gene methylation as a noninvasive marker for hepatocellular carcinoma. Dis Markers. 2020;2020:6289063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang T, Xing H, Wang G, et al. A novel online calculator based on serum biomarkers to detect hepatocellular carcinoma among patients with hepatitis B. Clin Chem. 2019;65(12):1543–1553. [DOI] [PubMed] [Google Scholar]
- 40.Wang Q, Chen Q, Zhang X, et al. Diagnostic value of gamma-glutamyltransferase/aspartate aminotransferase ratio, protein induced by vitamin K absence or antagonist II, and alpha-fetoprotein in hepatitis B virus-related hepatocellular carcinoma. World J Gastroenterol. 2019;25(36):5515–5529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shimagaki T, Yoshio S, Kawai H, et al. Serum milk fat globule-EGF factor 8 (MFG-E8) as a diagnostic and prognostic biomarker in patients with hepatocellular carcinoma. Sci Rep. 2019;9(1):15788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hu J, Wang N, Yang Y, et al. Diagnostic value of alpha-fetoprotein combined with neutrophil-to-lymphocyte ratio for hepatocellular carcinoma. BMC Gastroenterol. 2018;18(1):186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guo W, Sun YF, Shen MN, et al. Circulating tumor cells with stem-like phenotypes for diagnosis, prognosis, and therapeutic response evaluation in hepatocellular carcinoma. Clin Cancer Res. 2018;24(9):2203–2213. [DOI] [PubMed] [Google Scholar]
- 44.Chuaypen N, Chittmittraprap S, Pinjaroen N, et al. Serum Wisteria floribunda agglutinin-positive Mac-2 binding protein level as a diagnostic marker of hepatitis B virus-related hepatocellular carcinoma. Hepatol Res. 2018;48(11):872–881. [DOI] [PubMed] [Google Scholar]
- 45.Tian MM, Fan YC, Zhao J, et al. Hepatocellular carcinoma suppressor 1 promoter hypermethylation in serum. A diagnostic and prognostic study in hepatitis B. Clin Res Hepatol Gastroenterol. 2017;41(2):171–180. [DOI] [PubMed] [Google Scholar]
- 46.Shaker MK, Abdel Fattah HI, Sabbour GS, et al. Annexin A2 as a biomarker for hepatocellular carcinoma in Egyptian patients. World J Hepatol. 2017;9(9):469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ismail MM, Morsi HK, Abdulateef NA, et al. Evaluation of prothrombin induced by vitamin K absence, macrophage migration inhibitory factor and golgi protein-73 versus alpha fetoprotein for hepatocellular carcinoma diagnosis and surveillance. Scand J Clin Lab Invest. 2017;77(3):175–183. [DOI] [PubMed] [Google Scholar]
- 48.Hu N, Fan XP, Fan YC, et al. Hypomethylated Ubiquitin-Conjugating Enzyme2 Q1 (UBE2Q1) gene promoter in the serum is a promising biomarker for hepatitis B virus-associated hepatocellular carcinoma. Tohoku J Exp Med. 2017;242(2):93–100. [DOI] [PubMed] [Google Scholar]
- 49.Fu Y, Xu X, Huang D, et al. Plasma heat shock protein 90alpha as a biomarker for the diagnosis of liver cancer: an official, large-scale, and multicenter clinical trial. EBioMedicine. 2017;24:56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu HH, Fang Y, Wang JW, et al. Hypomethylation of the cyclin D1 promoter in hepatitis B virus-associated hepatocellular carcinoma. Medicine. 2020;99(20):e20326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tang XQ, Li H, Yan LB, et al. Diagnostic value of PIVKA-II in detecting hepatocellular carcinoma. Future Virol. 2017;12(5):259–267. [Google Scholar]
- 52.Ali OM, El Amin HA, Sharkawy YL, et al. Golgi protein 73 versus alpha-fetoprotein as a new biomarker in early diagnosis of hepatocellular carcinoma. Int J Gen Med. 2020;13:193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sai WL, Wang L, Sun JY, et al. Value of abnormal expression of Krüppel-like zinc-finger protein transcription factor 5 in the diagnosis and prognosis of liver cancer. Zhonghua Gan Zang Bing Za Zhi. 2021;29(8):781–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alzamzamy A, Elsayed H, Abd Elraouf M, et al. Serum vascular endothelial growth factor as a tumor marker for hepatocellular carcinoma in hepatitis C virus-related cirrhotic patients. World J Gastrointest Oncol. 2021;13(6):600–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ricco G, Cavallone D, Cosma C, et al. Impact of etiology of chronic liver disease on hepatocellular carcinoma biomarkers. Cancer Biomark. 2018;21(3):603–612. [DOI] [PubMed] [Google Scholar]
- 56.Caviglia GP, Armandi A, Rosso C, et al. Biomarkers of oncogenesis, adipose tissue dysfunction and systemic inflammation for the detection of hepatocellular carcinoma in patients with nonalcoholic fatty liver disease. Cancers. 2021;13(10):2305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Caviglia GP, Ciruolo M, Abate ML, et al. Alpha-fetoprotein, protein induced by vitamin K absence or antagonist II and glypican-3 for the detection and prediction of hepatocellular carcinoma in patients with cirrhosis of viral etiology. Cancers. 2020;12(11):3218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Song T, Wang L, Su B, et al. Diagnostic value of alpha-fetoprotein, lens culinaris agglutinin-reactive alpha-fetoprotein, and des-gamma-carboxyprothrombin in hepatitis B virus-related hepatocellular carcinoma. J Int Med Res. 2020;48(3):300060519889270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pan Y, Dai J, Hua X, et al. The value of combined detection of Pivka-II, AFP and AFP-L3 in the diagnosis of hepatocellular carcinoma. Acta Med Mediterr. 2019;35:2793–2797. [Google Scholar]
- 60.Hu RZ, Zhao SQ, Shen B, et al. [Diagnostic value of serum alpha-fetoprotein, alpha-fetoprotein variant and abnormal prothrombin in primary hepatocellular carcinoma]. Zhonghua Gan Zang Bing Za Zhi. 2019;27(8):634–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Choi J, Kim GA, Han S, et al. Longitudinal assessment of three serum biomarkers to detect very early-stage hepatocellular carcinoma. Hepatology. 2019;69(5):1983–1994. [DOI] [PubMed] [Google Scholar]
- 62.Chen H, Zhang Y, Li S, et al. Direct comparison of five serum biomarkers in early diagnosis of hepatocellular carcinoma. Cancer Manag Res. 2018;10:1947–1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wu M, Liu Z, Li X, et al. Dynamic changes in serum markers and their utility in the early diagnosis of all stages of hepatitis B-associated hepatocellular carcinoma. Onco Targets Ther. 2020;13:827–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Maeda T, Kanzaki H, Chiba T, et al. Serum fibroblast growth factor 19 serves as a potential novel biomarker for hepatocellular carcinoma. BMC Cancer. 2019;19(1):1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wu J, Xiang Z, Bai L, et al. Diagnostic value of serum PIVKA-II levels for BCLC early hepatocellular carcinoma and correlation with HBV DNA. Cancer Biomark. 2018;23(2):235–242. [DOI] [PubMed] [Google Scholar]
- 66.Lee Q, Yu X, Yu W.. The value of PIVKA-II versus AFP for the diagnosis and detection of postoperative changes in hepatocellular carcinoma. J Interv Med. 2021;4(2):77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhu X, Li J, Qiyu S, et al. Improving the detection of hepatocellular carcinoma using serum AFP expression in combination with GPC3 and Micro-RNA MiR-122 expression. Biomater Sci. 2019;14:53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Taketomi A, Hanayama R, Yoshizumi T, et al. Clinical impact of circulated miR-1291 in plasma of patients with liver cirrhosis (LC) and hepatocellular carcinoma (HCC): implication on glypican-3 expression. Sci Rep. 2020;51:234–241. [DOI] [PubMed] [Google Scholar]
- 69.Tang XY, Wang YC, Lu RQ, et al. The value of serum glypican-3 level in aided diagnosis of patients with primary hepatocellular carcinoma. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(9):998–1002. [DOI] [PubMed] [Google Scholar]
- 70.Shimizu Y, Mizuno S, Fujinami N, et al. Plasma and tumoral glypican-3 levels are correlated in patients with hepatitis C virus-related hepatocellular carcinoma. Cancer Sci. 2020;111(2):334–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu S, Wang M, Zheng C, et al. Diagnostic value of serum glypican-3 alone and in combination with AFP as an aid in the diagnosis of liver cancer. Clin Biochem. 2020;79:54–60. [DOI] [PubMed] [Google Scholar]
- 72.Ji J, Liu L, Jiang F, et al. The clinical application of PIVKA-II in hepatocellular carcinoma and chronic liver diseases: a multi-center study in China. J Clin Lab Anal. 2021;35(11):e24013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ao J, Chiba T, Kanzaki H, et al. Serum angiopoietin 2 acts as a diagnostic and prognostic biomarker in hepatocellular carcinoma. J Cancer. 2021;12(9):2694–2701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jing JS, Ye W, Jiang YK, et al. The value of GPC3 and GP73 in clinical diagnosis of hepatocellular carcinoma. J Cell Physiol. 2017;63:1903–1909. [DOI] [PubMed] [Google Scholar]
- 75.Wang YY, Zhou CJ, Li J, et al. [Value of detection of serum glypican-3 level in diagnosis and therapeutic effect evaluation of primary hepatocellular carcinoma]. Nan Fang Yi Ke Da Xue Xue Bao. 2017;37(8):1060–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wei H, Shixing G, Xiaotong Z, et al. Application value of combined detection of biomarkers in diagnosis of early stage primary liver cancer. Cancer Res Clin. 2020;32:705–710. [Google Scholar]
- 77.Farag RMA, Al Ayobi D, Alsaleh KA, et al. Studying the impact of golgi protein 73 serving as a candidate biomarker in early diagnosis for hepatocellular carcinoma among Saudi patients. Asian Pac J Cancer Prev. 2019;20(1):215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yanming L, Yue C, Wencan C, et al. Combined detection of AFP-L3, GP73 and TIP30 enhances diagnostic accuracy for HBV-related cirrhosis and hepatocellular carcinoma. Biosensors. 2019;69:1279–1286. [PubMed] [Google Scholar]
- 79.ElZefzafy WM, Hussien M, Mohmmed ZAZ, et al. The diagnostic value of golgi protien-73 and DICKKOPF-1 in hepatocellular carcinoma. J Immunoassay Immunochem. 2021;42(2):174–187. [DOI] [PubMed] [Google Scholar]
- 80.Piratvisuth T, Tanwandee T, Thongsawat S, et al. Multimarker panels for detection of early stage hepatocellular carcinoma: a prospective, multicenter, case-control study. Hepatol Commun. 2022;6:679–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.El-Shayeb AF, El-Habachi NM, Mansour AR, et al. Serum midkine is a more sensitive predictor for hepatocellular carcinoma than dickkopf-1 and alpha-L-fucosidase in cirrhotic HCV patients. Medicine. 2021;100(17):e25112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Eldeeb MK, Magour GM, Bedair RN, et al. Study of dickkopf-1 (DKK-1) in patients with chronic viral hepatitis C-related liver cirrhosis with and without hepatocellular carcinoma. Clin Exp Hepatol. 2020;6(2):85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Awad AE, Ebrahim MA, Eissa LA, et al. Dickkopf-1 and amphiregulin as novel biomarkers and potential therapeutic targets in hepatocellular carcinoma. Int J Hematol Oncol Stem Cell Res. 2019;13(3):153–163. [PMC free article] [PubMed] [Google Scholar]
- 84.Liu R, Li Y, Wu A, et al. Identification of plasma hsa_circ_0005397 and combined with serum AFP, AFP-L3 as potential biomarkers for hepatocellular carcinoma. Front Pharmacol. 2021;12:639963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xing H, Qiu H, Ding X, et al. Clinical performance of α-L-fucosidase for early detection of hepatocellular carcinoma. PLOS One. 2019;13:545–555. [DOI] [PubMed] [Google Scholar]
- 86.Han Y, Zhang Y, Cui L, et al. Plasma heat shock protein 90alpha as a biomarker for the diagnosis of liver cancer: in patients with different clinicopathologic characteristics. Biomed Res Int. 2021;19:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang X, Li J, Wang F, et al. CT combined with tumor markers in the diagnosis and prognosis of hepatocellular carcinoma. J Buon. 2018;23(4):985–991. [PubMed] [Google Scholar]
- 88.Zhao L, Xie C, Liu D, et al. Early detection of hepatocellular carcinoma in patients with hepatocirrhosis by soluble B7-H3. J Gastrointest Surg. 2017;21(5):807–812. [DOI] [PubMed] [Google Scholar]
- 89.Tang Y, Li K, Cai Z, et al. HSP90α combined with AFP and TK1 improved the diagnostic value for hepatocellular carcinoma. Biomark Med. 2020;14(10):869–878. [DOI] [PubMed] [Google Scholar]
- 90.Hodeib H, O EL, Selim A, et al. Serum midkine and osteopontin levels as diagnostic biomarkers of hepatocellular carcinoma. Electron Physician. 2017;9(1):3492–3498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Al-Zoubi S, Wassouf A, Zetoune AB.. Measuring levels of osteopontin as potential biomarker for hepatocellular carcinoma in Syrian patients. Gastroenterol Hepatol Bed Bench. 2017;10(2):97–101. [PMC free article] [PubMed] [Google Scholar]
- 92.Wang T, Zhang KH.. New blood biomarkers for the diagnosis of AFP-negative hepatocellular carcinoma. Front Oncol. 2020;10:1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang D, Han G, Fu S, et al. Soluble Axl is an accurate biomarker of cirrhosis and hepatocellular carcinoma development: results from a large scale multicenter analysis. PLOS One. 2017;8:46234–46248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Loglio A, Iavarone M, Viganò M, et al. Minimal increases of serum alpha-foetoprotein herald HCC detection in caucasian HBV cirrhotic patients under long-term oral therapy. Liver Int. 2019;39(10):1964–1974. [DOI] [PubMed] [Google Scholar]
- 95.El-Derany MO. Polymorphisms in interleukin 13 signaling and interacting genes predict advanced fibrosis and hepatocellular carcinoma development in non-alcoholic steatohepatitis. Biology. 2020;9(4):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bo L, Boan L, Guo T, et al. The clinical values of serum markers in the early prediction of hepatocellular carcinoma. Biomed Res Int. 2017;2017:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shakado S, Sakisaka S, Chayama K, et al. Alpha-fetoprotein and des-gamma-carboxy-prothrombin at twenty-four weeks after interferon-based therapy predict hepatocellular carcinoma development. World J Hepatol. 2015;7(27):2757–2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gatselis NK, Zachou K, Giannoulis G, et al. Serum cartilage oligomeric matrix protein and golgi protein-73: new diagnostic and predictive tools for liver fibrosis and hepatocellular cancer? Cancers. 2021;13(14):3510. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.