Abstract
Background
Further investigation is needed to define the impact of long-term pandemic lockdown in children.
Objectives
To examine changes in body mass index z-score (zBMI), lifestyle, Health-Related Quality of Life and proportion of overweight or obesity (OW/OB) in 6- to 9-year-old children in Argentina.
Methods
Observational study with baseline measurements prior to lockdown and follow-up after eight months of strict restrictive measures (November 2020, first visit, n = 144) and after ten months of partial reopening (September 2021, second visit, n = 108). Anthropometric changes from baseline to first visit in lockdown group (LG) were compared with a historical control group (HCG, n = 134). Follow-up visits included anthropometric measures, lifestyle questionnaire and Pediatric Quality of Life Inventory.
Results
Change in zBMI was higher in LG [median, IQR: 0.46 (−0.00; 0.83)] vs HCG [median, IQR: 0.02 (−0.31; 0.27)]; p < 0.001, particularly in children with pre-existing OW/OB. In LG, zBMI was higher at first and second visit vs baseline (p < 0.001) and in second visit vs first visit for boys (p = 0.037) but not for girls. The proportion of children with OW/OB increased from baseline (43.5%) to first (56.5%) and second visit (58.3%) (p = 0.029). Unlike girls, the proportion of boys with OW/OB increased from baseline to first and second visit (p = 0.045). Change in zBMI was higher in children with less healthy habits (p < 0.001).
Conclusions
Weight gain continued to increase in boys when lockdown measurements were eased, although sedentary behaviors decreased and quality of life improved, indicating that the effects of pandemic lockdown could be difficult to reverse.
Subject terms: Obesity, Paediatrics
Introduction
To mitigate the spread of the coronavirus disease 2019 (COVID-19), in March 2020 the Argentinian Government decided for strict lockdown measurements that included suspension of in-person schooling and closure of playgrounds, recreational facilities, and non-essential services [1]. Strict lockdown measurements were not eased until November 2020; [2] Argentina suffered one of the most prolonged lockdown periods worldwide [3]. Throughout 2021, the restrictions were gradually reduced and schools reopened partially in March with a hybrid learning pattern that combined equally in-person and online learning, and in September full in-person classes were resumed. It has been suggested that this changing reality may have negative implications especially on children [4–6].
Prior research has indicated that lockdown measurements affected several aspects of lifestyle all over the world: changes in diet, lower physical activity, higher screen time and sleeping disorders were widely reported [7–13]. Besides, children faced a dramatic change in their routine due to school closure, which deprives children from contact with their peers and teachers. Lifestyle changes may also affect Health-Related Quality of Life (HRQoL), a multidimensional measure of health used to assess the individual’s perceptions of the impact of a given condition on health status [14]. A stressful situation such as pandemic lockdown may significantly impact HRQoL [15].
In Argentina, excess weight was already a main nutritional problem before the pandemic according to the last national nutrition survey, affecting 41.1% of 5- to 17-year-old children [16]. The aforementioned changes in lifestyle predict severe consequences with increasing obesity, especially in predisposed individuals. Pre-COVID-19 studies reported that children usually gain more weight during the summer holidays [17–19], and it has been proposed that the pandemic may have exerted a similar effect due to increased time out of school [6, 20]. Based on the weight trend pattern during school time and summer recess, a simulation study predicted an important increase in weight gain during pandemic-induced school closures [21].
Although different studies showed that during the pandemic weight gain and obesity rates increased in children and adolescents [22–26], further investigation is mandatory to define the impact of long-term restrictive measurements, the effect of the progressive relaxation of restrictions and the direct implication of lifestyle changes. Besides, the excess weight gained by children could be difficult to reverse and might contribute to overweight (OW) and obesity (OB) in adulthood [27]. To our knowledge, few prior studies examined the consequences of prolonged lockdown in body weight [28–30]. The objective of this longitudinal study was to examine changes in body weight, lifestyle and HRQoL in children for almost two years after the beginning of the COVID-19 pandemic lockdown in Argentina, where a very long period of strict lockdown was followed by almost one year of gradual opening.
Methods
Study design
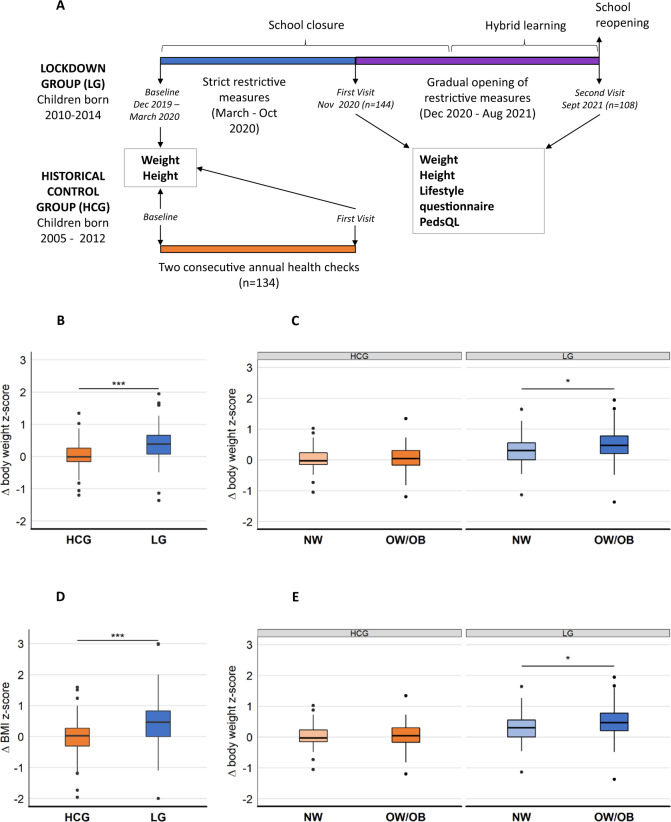
The study design can be seen in Fig. 1A. This observational follow-up study was conducted at Instituto de Desarrollo e Investigaciones Pediátricas (IDIP), HIAEP “Sor María Ludovica”, Healthy Children Outpatient Service, La Plata, Argentina. The database of the Institute was searched for children who were 6–to 9-year-old at the beginning of the pandemic. Included were children with available weight and height pre-pandemic (baseline) measurements recorded from December 1st, 2019 until March 10, 2020. Excluded were children who entered puberty and children undergoing chronic diseases that affect growth or weight gain or under pharmacological treatment. Parents of children who met the inclusion criteria were invited for follow-up visits in November 2020 (first visit) and in September 2021 (second visit). Visits included anthropometric measurements and completing a lifestyle questionnaire and the Pediatric Quality of Life Inventory (PedsQL). Anthropometric changes from baseline to 1st visit were compared with a historical control group (HCG) that included children born at least 2 years earlier than the lockdown-exposed children (LG, lockdown group), and did not experience lockdown. In LG, changes in anthropometric measurements were calculated from baseline and between visits. The timing of the 1st and 2nd visit was chosen according to the state of lockdown in Argentina. First visit was settled when strict restrictive measurements ended (November 2020) and 2nd visit occurred before school reopening (September 2021), therefore during this study children did not fully assist to daily in-person classes.
Fig. 1. Study design and changes in body weight and BMI z-scores in LG vs HCG.
A Study design. B Changes (Δ) in body weight z-score in LG and HCG analyzed by Mann-Whitney test. C Changes in body weight z-score in LG and HCG stratified by baseline weight status, analyzed by robust two-way ANOVA. D Changes in BMI z-score in LG and HCG analyzed by Mann-Whitney test. E Changes in BMI z-score in LG and HCG stratified by baseline weight status, analyzed by robust two-way ANOVA. In all cases ***p < 0.001, *p < 0.05. PedsQL Pediatric Quality of Life Inventory, LG Lockdown group, HCG Historical control group, NW Normoweight, OW/OB Overweight or obesity.
Data collection
Anthropometric measurements
Height was measured by a Harpenden stadiometer (Holtain Ltd., Crosswell, United Kingdom) and weight was measured wearing light clothing using a Systel scale (Argentina). Baseline measurements were retrieved from medical records. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Children´s height, weight, and BMI values were converted to sex- and age-specific standard deviation scores (z-scores) using WHO AnthroPlus software version 1.0.4 (World Health Organization). A BMI z-score (zBMI) greater than one was defined as OW, and a zBMI greater than two was defined as OB according to the World Health Organization [31].
Lifestyle questionnaire
In the 1st visit parents filled out a lifestyle questionnaire about their children´s changes in feeding behavior, sleep and physical activity vs baseline. The questionnaire included 8 closed questions. A lockdown healthy habits score (HHS) was calculated as the sum of the 8 questions using a 4-point scoring system. A cutoff value in the third quartile was chosen to discriminate low and high HHS. The items from the lifestyle questionnaire and the scoring criteria are presented in Suppl. Table 1. In the 2nd visit, parents filled out a similar questionnaire to evaluate changes with respect to 1st visit.
Health-Related Quality of Life - Pediatric Quality of Life Inventory (PedsQL)
In the 1st and 2nd visit parents and children completed the validated Spanish-Argentina version of PedsQLTM Generic Core Scales 4.0 [32], which includes the child self-report and parent proxy-report forms to assess HRQoL and comprises 4 domains (physical, emotional, social, and school functions) [14]. The items were measured using a 5-point Likert scale. The PedsQL total score was composed of the physical and psychosocial scores. The psychosocial score was composed of the emotional, social and school functioning scores.
Ethics
The study was approved by the Institutional Committee for the Revision of Research Protocols, IDIP, and conducted according to the Declaration of Helsinki guidelines. Parents or legal tutors signed a written informed consent, children above 8 years old signed a written informed assent.
Statistical analyses
Sample size was calculated assuming a standard deviation of 0.6 [33], a difference in zBMI between groups of 0.25, 80% statistical power and 5% significance level, leading to a minimal sample size of 91 children per group. Statistical analyses were performed using the R statistical software version 4.0.3. The Kolmogorov-Smirnov test was applied to test normal distribution. Continuous variables with normal distribution are presented as mean (standard deviation [SD]); non-normal variables are reported as median (interquartile range [IQR]) and categorical data are summarized as frequency counts and percentages. Baseline characteristics were compared by t-test or Mann-Whitney for quantitative data and using Chi-squared for qualitative data. Changes in z-scores between groups were assessed by Mann-Whitney and robust two-way mixed model ANOVA when stratified by baseline weight status. Changes over time for the LG group were analyzed by repeated measures ANOVA and 2-way mixed repeated-measures ANOVA when analyzed by sex. Pairwise comparisons were adjusted by Bonferroni method. Changes in proportion of OW/OB were analyzed by Chi-squared test for linear trend. Changes in lifestyle questionnaire were analyzed by Fisher exact test. Differences in PedsQL between 1st and 2nd visit were assessed by Wilcoxon signed rank test. All statistical tests were two-tailed and significance level was set at p < 0.05.
Results
Baseline characteristics
Baseline characteristics of the children can be seen in Table 1. Pre-pandemic data was retrieved from 205 medical records of children who met the inclusion criteria and parents were invited to participate. Of these, 144 agreed and were called for the 1st visit, conforming the LG. Besides, 134 medical records of children with similar characteristics to the LG in terms of sex, age, weight and height before the COVID-19 pandemic were selected for the HCG and data from 2 anthropometric measurements taken with time intervals similar to the LG were collected. Sex differences were not observed in baseline anthropometric characteristics (data not shown).
Table 1.
Baseline characteristics of the children.
| HCG (N = 134) | LG (N = 144) | p-value | |
|---|---|---|---|
| Male, n (%) | 58 (43.3%) | 72 (50%) | 0.281 |
| Female, n (%) | 76 (57.7%) | 72 (50%) | |
| Age (years) | 6.73 (6.06, 7.77) | 6.74 (5.97, 7.49) | 0.320 |
| Interval between baseline and 1st visit (years) | 0.92 (0.80, 1.01) | 0.91 (0.79, 0.97) | 0.246 |
| Height at baseline (cm) | 120 (114, 126) | 119 (113.3, 124) | 0.228 |
| Body weight at baseline (kg) | 23.50 (20.80, 28.85) | 24 (20.30, 26.92) | 0.535 |
| Body weight z-score at baseline | 0.47 (1.16) | 0.43 (1.10) | 0.431 |
| BMI at baseline (kg/m2) | 16.62 (15.55, 18.55) | 16.64 (15.49, 18.08) | 0.801 |
| BMI z-score at baseline | 0.78 (1.09) | 0.77 (1.07) | 0.814 |
| NW, n (%) | 79 (58.9%) | 84 (58.3%) | 0.999 |
| OW, n (%) | 36 (26.9%) | 39 (27.1%) | |
| OB, n (%) | 19 (14.2%) | 21 (14.6%) |
LG Lockdown group, HCG Historical control group, BMI Body Mass Index, NW Normoweight, OW Overweight, OB Obesity. Data are presented as mean (SD) for body weight and BMI z-scores at baseline. Age, interval between baseline and 1st visit and height, body weight and BMI at baseline are presented as median (IQR).
Changes in body weight z-score, zBMI and proportion of weight status in LG vs HCG
Figure 1 shows that changes (Δ) in body weight z-score (Fig. 1B) and zBMI (Fig. 1D) from baseline to 1st visit were significantly higher in LG vs HCG. Similar differences were observed in absolute weight gain [median, IQR: 3.9 (2.3; 6.4) kg in LG vs 2.5 (1.7; 4.2) kg in HCG, p < 0.001]. Δ-body weight z-score was significantly higher in children with OW or OB (OW/OB) at baseline vs normoweight (NW) children in the LG but not in the HCG (Fig. 1C), and a similar trend was observed in Δ-zBMI (Fig. 1E). No changes in Δ-height z-score were observed in LG vs HCG (p = 0.884). The proportion of children with OW/OB tended to increase from 41.7% at baseline to 52.8% at 1st visit in LG (p = 0.075) and remained unchanged in HCG (41.0% to 42.5%, p = 0.902). Furthermore, the proportion of children with OB increased from 14.6% at baseline to 27.8% at 1st visit in LG (p = 0.009) and remained unchanged in HCG (14.2% to 17.2%, p = 0.510).
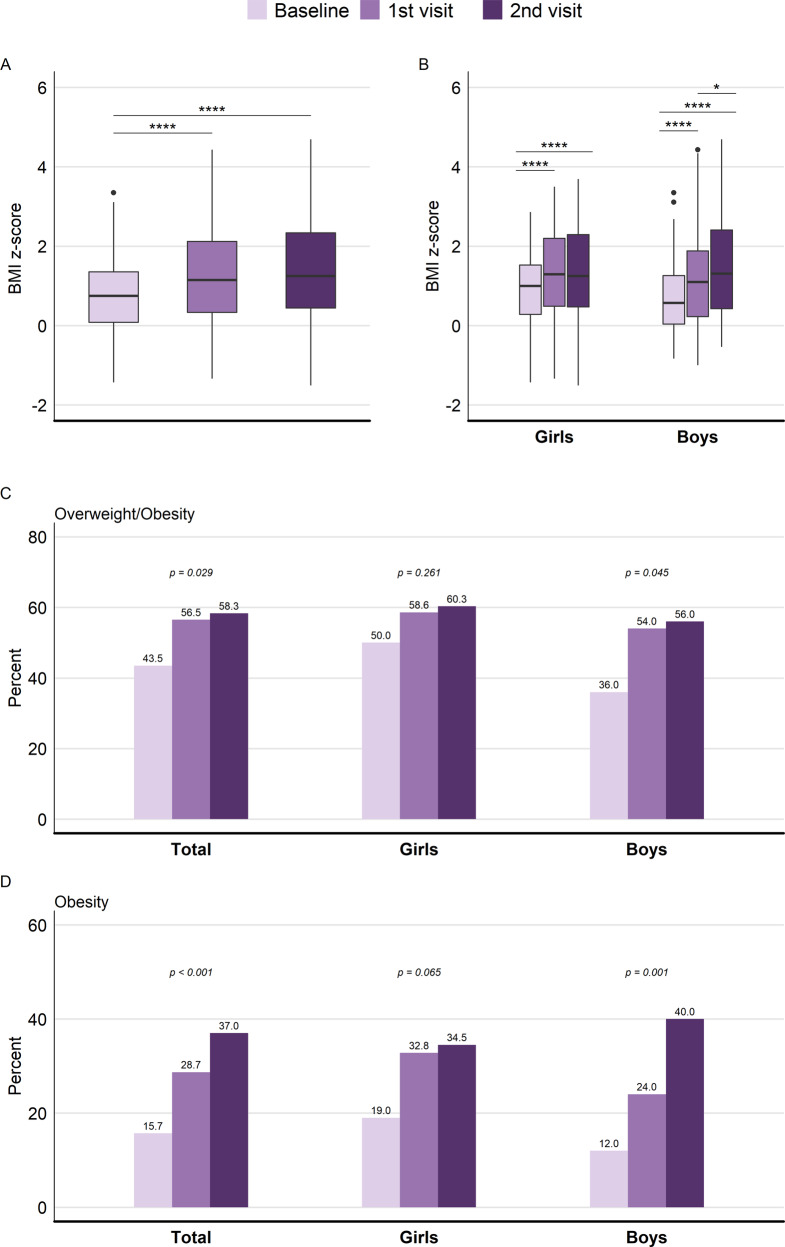
Longitudinal changes in zBMI and proportion of weight status in LG
Of the 144 children that attended the 1st visit, thirty-six did not follow up for the 2nd visit and were not included in this part of the analysis. zBMI was significantly higher at 1st and 2nd visit vs. baseline (Fig. 2A), and similar results were observed in children with OW/OB at baseline vs NW children (data not shown). zBMI was also analyzed considering sex and time as factors. Significant time effect (p < 0.001) and interaction were detected (F (1.87, 196.6) = 4.77, p = 0.011), and pairwise comparison showed that zBMI was significantly different at 1st and 2nd visit for boys and girls vs baseline, and in 2nd vs 1st visit only for boys (Fig. 2B). The proportion of children with OW/OB or OB increased from baseline to 1st and 2nd visit, significantly in boys but not in girls (Fig. 2C, D).
Fig. 2. Longitudinal changes in zBMI and proportion of weightstatus in LG.
A BMI z-score at baseline, 1st and 2nd visit in children exposed to lockdown in the total sample analyzed by repeated measures ANOVA, pairwise comparisons adjusted by Bonferroni method. B BMI z-score at baseline, 1st and 2nd visit in children exposed to lockdown in girls and boys analyzed by two-way mixed ANOVA, pairwise comparisons adjusted by Bonferroni method. C Proportion of children with overweight or obesity in the total sample and stratified by sex, analyzed by Chi-squared test for trend. D Proportion of children with obesity in the total sample and stratified by sex analyzed by Chi-squared test for trend. In all cases ****p < 0.001, *p < 0.05.
Lifestyle changes
Lifestyle changes from baseline to 1st visit and from 1st to 2nd visit are depicted in Table 2. At 1st visit most parents reported that their children reduced the intake of snacks, sweetened beverages and sweets, reduced their physical activity, slept more hours and increased leisure screen time. Some changes reversed at 2nd visit: vegetables consumption and physical activity increased, and intake of sweetened beverages, sleeping and leisure screen hours decreased. No sex differences were observed (data not shown). zBMI and its changes were also stratified by baseline weight status and HHS and analyzed by two-way robust ANOVA (Suppl. Table 2). zBMI at 1st and 2nd visit was higher in children with OW/OB at baseline (p < 0.001) and with low HHS (p < 0.01), and ΔzBMI from baseline to 1st visit was higher in children with low HHS (p < 0.001).
Table 2.
Lifestyle changes.
| 1st visit | 2nd visit | ||
|---|---|---|---|
| (vs baseline) | (vs 1st visit) | p-value | |
| Fruit intake | 0.074 | ||
| No | 3 (3%) | 0 (0%) | |
| Less | 18 (19%) | 9 (9%) | |
| The same | 40 (42%) | 47 (49%) | |
| More | 35 (36%) | 40 (42%) | |
| Vegetables intake | 0.005 | ||
| No | 8 (8%) | 2 (2%) | |
| Less | 25 (26%) | 12 (13%) | |
| The same | 41 (43%) | 43 (45%) | |
| More | 22 (23%) | 39 (41%) | |
| Snacks intake | 0.207 | ||
| More | 15 (16%) | 6 (6%) | |
| The same | 27 (28%) | 32 (33%) | |
| Less | 39 (41%) | 44 (46%) | |
| No | 15 (15%) | 14 (15%) | |
| Sweetened beverages intake | 0.019 | ||
| More | 20 (21%) | 6 (6%) | |
| The same | 27 (28%) | 27 (28%) | |
| Less | 35 (36%) | 41 (43%) | |
| No | 14 (15%) | 22 (23%) | |
| Sweets intake | 0.060 | ||
| More | 13 (14%) | 15 (16%) | |
| The same | 21 (22%) | 31 (33%) | |
| Less | 44 (46%) | 43 (45%) | |
| No | 17 (18%) | 6 (6%) | |
| Physical activity | <0.001 | ||
| Less | 56 (59%) | 13 (14%) | |
| The same | 13 (14%) | 23 (24%) | |
| More | 26 (27%) | 59 (62%) | |
| Sleeping | 0.003 | ||
| Less | 12 (13%) | 26 (27%) | |
| The same | 39 (41%) | 45 (47%) | |
| More | 44 (46%) | 24 (25%) | |
| Screen hours (leisure) | <0.001 | ||
| More | 55 (58%) | 20 (21%) | |
| The same | 20 (21%) | 24 (25%) | |
| Less | 20 (21%) | 51 (54%) |
Data are presented as frequency counts (percentages) (Fisher exact test).
Health-related quality of life
PedsQL scores at 1st and 2nd visit were stratified by weight status (Suppl. Table 3). Children with OW/OB at baseline had lower parent physical and total scores at 2nd visit. PedsQL scores were also stratified by HHS (Table 3). Children with high HHS showed greater self-reported scores and total parent score at 1st visit and higher self-reported physical and total self-reported scores at 2nd visit. All scores except the physical parent score improved from 1st to 2nd visit (Table 4).
Table 3.
PedsQL scores in children exposed to lockdown stratified by HHS.
| Low HHS (N = 80) | High HHS (N = 43) | p-value | |
|---|---|---|---|
| PedsQL Score - First visit | |||
| Child | |||
| Physical | 73.4 (62.5, 85.2) | 78.1 (68.8, 93.8) | 0.031 |
| Psychosocial | 72.7 (56.3, 86.4) | 81.8 (70.5, 88.6) | 0.043 |
| Total | 72.6 (59.2, 84.2) | 79.0 (71.7, 89.5) | 0.011 |
| Parent | |||
| Physical | 88.4 (75.0, 93.8) | 90.6 (84.4, 98.4) | 0.140 |
| Psychosocial | 81.8 (72.7, 90.9) | 86.4 (80.7, 93.2) | 0.065 |
| Total | 84.2 (74.4, 89.5) | 89.5 (80.3, 94.1) | 0.040 |
| PedsQL Score - Second visit | |||
| Child | |||
| Physical | 81.3 (75.0, 93.8) | 92.2 (81.3, 93.8) | 0.022 |
| Psychosocial | 87.5 (75.4, 96.7) | 93.3 (78.8, 96.7) | 0.172 |
| Total | 85.9 (76.1, 91.3) | 89.7 (82.9, 97.3) | 0.043 |
| Parent | |||
| Physical | 87.5 (78.1, 96.9) | 93.8 (82.8, 99.2) | 0.195 |
| Psychosocial | 90.0 (78.8, 97.9) | 94.2 (80.4, 96.7) | 0.597 |
| Total | 88.3 (80.4; 95.4) | 92.2 (83.2; 95.7) | 0.264 |
PedsQL Pediatric Quality of Life Inventory, HHS Healthy Habits Score. Data are presented as median (IQR). Statistical analysis was performed by Mann-Whitney test.
Table 4.
PedsQL scores in children exposed to lockdown at first and second visits.
| First visit (N = 91) | Second visit (N = 91) | p-value | |
|---|---|---|---|
| Child | |||
| Physical | 75.0 (62.5, 93.8) | 85.9 (77.3, 93.8) | <0.001 |
| Psychosocial | 79.6 (59.1, 86.4) | 90.0 (76.7, 96.7) | <0.001 |
| Total | 77.0 (63.2, 87.2) | 88.0 (78.3, 93.5) | <0.001 |
| Parent | |||
| Physical | 90.6 (77.3, 96.9) | 90.6 (80.6, 96.9) | 0.179 |
| Psychosocial | 84.1 (75.0, 90.9) | 90.0 (80.0, 96.7) | 0.001 |
| Total | 85.5 (77.6, 92.1) | 89.1 (82.6, 95.7) | 0.009 |
PedsQL Pediatric Quality of Life Inventory, HHS Healthy Habits Score. Data are presented as median (IQR). Statistical analysis was performed by Wilcoxon signed rank test.
Discussion
To our knowledge, this is the first longitudinal study showing that weight gain in children during lockdown continued to increase despite the progressive ease of restrictions, although sedentary behaviors decreased and HRQoL improved. Several authors have warned about the risks of greater overweight or obesity due to the change in habits resulting from lockdown [7–12], and several studies have shown that lockdown and school closure increased weight gain and obesity prevalence [11, 34–37]. The current study goes a step further and shows the consequences of long-term lockdown on children´s health.
One of the main findings of our study is that the body weight gain during strict COVID-19 lockdown in Argentina of 6- to 9 year-old children exceeded predictions [21] and reports from other populations [22, 24, 34, 38]. A Chinese study reported a yearly change in zBMI from 0.36 in 2019 to 0.55 in 2020 in 6 to 11 year-old children [22] and a Korean study reported a change of 0.219 in six months after school closure [34]. A study conducted in USA showed an absolute weight gain of 2.37 kg between 2019 and 2020 [24] and a recent meta-analysis reported a similar value [38]. Our study shows an absolute weight gain of 4 kg during strict lockdown and a change in zBMI of 0.46, values higher than reports and predictions by a microsimulation model which calculated an increase in zBMI by 0.141 in 6 months of school closure [21]. The long duration of strict lockdown in Argentina (almost 9 months, time elapsed between baseline and 1st visit) could be related to the greater weight gain, since most studies report the effects of 2-to-5 months of lockdown [38]. An important aspect of our study is the comparison with a HCG, which shows that lockdown-exposed children gained significantly more weight than those who did not go through a situation of social isolation. For this purpose, other studies have used data from several years prior to the pandemic [22–24], reaching similar conclusions. Our results also show that weight gain was more prominent in children with pre-existing obesity, who were already affected and vulnerable to excess weight gain, as observed in USA [23, 25] and Germany [39]. The longitudinal evaluation as lockdown measurements were eased and schools partially reopened (10 months between 1st and 2nd visit) revealed that relaxation of restrictive measures were not enough to influence the effects of the lockdown on weight gain. Few studies evaluated the effects of long-term lockdown: a recent study also reported sustained and significant weight gain for one year in Korean children, although schools were fully open for the last six months; [28] another study showed an important weight gain increase the first year of the pandemic followed by a period of stabilization [29] and a retrospective chart review study reported that excessive weight gain in 2020 did not reverse by 2021 [30]. We also observed that boys, unlike girls, continued gaining weight although lockdown measurements were eased. Boys also were more susceptible to weight gain during lockdown in studies in Austrian [40] and Chinese children [22, 41] and Italian adolescents with obesity [35].
The increase in the proportion of children with obesity as a consequence of strict lockdown was significantly high, similar to other reports [22, 24, 26, 42]. When lockdown measurements were eased, the proportion of children with OB continued to increase, particularly boys, in agreement with observations in Chinese adolescents [43]. Clearly, our results exceeded the projections about the impact of the pandemic on childhood obesity [18, 20, 21].
During strict lockdown, children´s screen time increased and physical activity decreased, as shown by our group [7] and others [8–11]. When lockdown measurements were eased, sedentary behaviors decreased. An interesting finding is that children with healthy habits during strict confinement, reflected by the HHS, gained less weight, irrespective of pre-existing OW/OB. Our results also show a reduction in the intake of unhealthy foods such as sweets, sweetened beverages and snacks, while other studies report an increase [8, 13, 37]. Discrepancies could be related to the limitations of the questionnaire, answered by parents, and to limited access related to food insecurity [44]. Our results highlight the importance of a healthy lifestyle for mitigating the consequences of lockdown in children, not only for individuals with obesity.
The COVID-19 pandemic lockdown also affected HRQoL, reflected by PedsQL scores. Children with healthy habits had a better quality of life, especially under strict restrictive measures. It was reported that more physical activity and less sedentary time [45], especially screen use [46], are associated with increased HRQoL in children and adolescents. Parents of children with pre-existing OW/OB reported a reduced quality of life, that was not self-perceived by the children. Although we could not assess HRQoL at baseline, physical and psychosocial scores improved as lockdown measurements were eased.
Weight gain is closely related to habits such as exercise and diet. During strict lockdown, increased weight gain was concomitant to sedentary behaviors, as reported by others [9–11], and not to consumption of unhealthy foods. When lockdown measurements were eased, weight gain continued to increase in boys, although sedentary behaviors decreased and HRQoL improved, indicating the long-lasting effects of lockdown on body weight. Although no differences were observed in lifestyle changes between boys and girls, previous results from our group show that during lockdown boys spent more time playing screen and online games (p < 0.001 vs girls) [7], in line with reports in Spanish children of greater risk of inadequate physical activity frequency and use of TV and electronic devices in boys [9].
Besides, school exerts a protective influence on children’s sedentary behaviors and weight status [17–19], as children engage in behaviors that lead to increased weight gain when they are not in school [47]. Therefore, school closure for such an extended time may have negative impact on children’s behaviors and consequently weight gain. Prolonged weight gain was previously observed in children after natural disasters: in Japan, elevated BMI was reported 1.5 years after the Great East Japan Earthquake [33, 48]. Besides, the reversion of childhood obesity needs a long follow-up period: multidisciplinary treatment programs can take up to five years to reach a significant weight loss [49].
This study has several limitations. It was conducted on a small sample and only 6- to 9-year-old children were included, who were likely most impacted by school closures and vulnerable to weight changes [22, 23]. Hence, caution must be exercised when interpreting evidence from other populations. Besides, lifestyle changes were parent-reported, and may provide less information than child reports, and changes in the long term could be difficult to remember. Also, lifestyle aspects were reported as changes vs. before lockdown, which limits data collection about time dedicated to physical activity and screen use. Despite these limitations, our work adds knowledge to previous studies about short-term consequences of lockdown.
We can conclude that pandemic lockdown increased weight gain and proportion of obesity in children, especially in boys and in those with pre-existing OW/OB. Weight gain continued to increase in boys when lockdown measurements were eased, although sedentary behaviors decreased and HRQoL improved, indicating that the effects of pandemic lockdown could be difficult to reverse. Tackling childhood obesity after the pandemic will not be easy and might require decades to fully reverse current trends. Governments, schools, and families should be encouraged to make efforts not only to prevent childhood obesity but also to ameliorate the effects of pandemic lockdown supporting healthy lifestyle choices.
Supplementary information
Acknowledgements
We thank the families, both children and parents and mothers, for their participation and collaboration in the study, even more in these complicated circumstances. We also thank the staff of the Institute of Development and Pediatric Research (IDIP), Sor Maria Ludovica Children´s Hospital, Healthy Children Outpatient Service for their help recruiting volunteers and collecting participant data.
Author contributions
Acquisition, analysis, or interpretation of data: MAA, AJA, MS, MP, AM, MFA. Organization of data: ALK, CC. Drafting of the manuscript: MFA, MVF. Statistical analysis: MVF. Obtained funding: MAA and MFA. All authors were involved in writing the paper and had final approval of the submitted and published versions.
Funding
This study (and MAA) was supported by Ministerio de Salud de la Nación, Dirección de Investigación en Salud, Becas Salud Investiga.
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: María Ángeles Azrak, María Victoria Fasano.
Supplementary information
The online version contains supplementary material available at 10.1038/s41430-022-01252-w.
References
- 1.Decreto Nro. 260/20 AISLAMIENTO SOCIAL PREVENTIVO Y OBLIGATORIO. 2020. Presidencia de la Nación. Argentina. http://servicios.infoleg.gob.ar/infolegInternet/anexos/335000-339999/335741/norma.htm. Accessed 17 June 2022.
- 2.Decreto Nro. 875/20 AISLAMIENTO SOCIAL PREVENTIVO Y OBLIGATORIO. 2020. Presidencia de la Nación. Argentina. http://servicios.infoleg.gob.ar/infolegInternet/verNorma.do?id=344033. Accessed 17 June 2022.
- 3.Ise A, Villalba S, Clementi L, Carrizo S. Extra long Argentinian lockdown: Revising the energy regime. Glob Transit. 2021;3:43–54. doi: 10.1016/j.glt.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golberstein E, Wen H, Miller BF. Coronavirus Disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174:819–20. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 5.Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–7. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-related school closings and risk of weight gain among children. Obes (Silver Spring) 2020;28:1008–9. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fasano MV, Padula M, Azrak MA, Avico AJ, Sala M, Andreoli MF. Consequences of lockdown during COVID-19 pandemic in lifestyle and emotional state of children in Argentina. Front Pediatr. 2021;9:660033. doi: 10.3389/fped.2021.660033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neshteruk CD, Zizzi A, Suarez L, Erickson E, Kraus WE, Li JS, et al. Weight-related behaviors of children with obesity during the COVID-19 pandemic. Child Obes. 2021;17:371–8. doi: 10.1089/chi.2021.0038. [DOI] [PubMed] [Google Scholar]
- 9.Ventura PS, Ortigoza AF, Castillo Y, Bosch Z, Casals S, Girbau C, et al. Children’s Health Habits and COVID-19 Lockdown in Catalonia: Implications for obesity and non-communicable diseases. Nutrients. 2021;13. [DOI] [PMC free article] [PubMed]
- 10.Ten Velde G, Lubrecht J, Arayess L, van Loo C, Hesselink M, Reijnders D, et al. Physical activity behaviour and screen time in Dutch children during the COVID-19 pandemic: Pre-, during- and post-school closures. Pediatr Obes. 2021;16:e12779. doi: 10.1111/ijpo.12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. BMI status and associations between affect, physical activity and anxiety among U.S. children during COVID-19. Pediatr Obes. 2021;16:e12786. doi: 10.1111/ijpo.12786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lopez-Bueno R, Lopez-Sanchez GF, Casajus JA, Calatayud J, Gil-Salmeron A, Grabovac I, et al. Health-related behaviors among school-aged children and adolescents during the Spanish Covid-19 confinement. Front Pediatr. 2020;8:573. doi: 10.3389/fped.2020.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obes (Silver Spring) 2020;28:1382–5. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–12. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Nobari H, Fashi M, Eskandari A, Villafaina S, Murillo-Garcia A, Perez-Gomez J. Effect of COVID-19 on health-related quality of life in adolescents and children: A Systematic Review. Int J Environ Res Public Health. 2021;18. [DOI] [PMC free article] [PubMed]
- 16.2° Encuesta Nacional de Nutrición y Salud. ENNyS2. Resumen Ejecutivo. 2019. Presidencia de la Nación. Argentina. http://www.msal.gob.ar/images/stories/bes/graficos/0000001565cntennys2_resumen-ejecutivo-2019.pdf. Accessed 17 June 2022.
- 17.Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014;11:E101. doi: 10.5888/pcd11.130355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.von Hippel PT, Workman J. From kindergarten through second grade, U.S. children’s obesity prevalence grows only during summer vacations. Obes (Silver Spring) 2016;24:2296–2300. doi: 10.1002/oby.21613. [DOI] [PubMed] [Google Scholar]
- 19.Wang YC, Vine S, Hsiao A, Rundle A, Goldsmith J. Weight-related behaviors when children are in school versus on summer breaks: does income matter? J Sch Health. 2015;85:458–66. doi: 10.1111/josh.12274. [DOI] [PubMed] [Google Scholar]
- 20.Workman J. How much may COVID-19 school closures increase childhood obesity? Obesity (Silver Spring). 2020;28:1787. [DOI] [PMC free article] [PubMed]
- 21.An R. Projecting the impact of the coronavirus disease-19 pandemic on childhood obesity in the United States: A microsimulation model. J Sport Health Sci. 2020;9:302–12. [DOI] [PMC free article] [PubMed]
- 22.Hu J, Liu J, Wang J, Shen M, Ge W, Shen H, et al. Unfavorable progression of obesity in children and adolescents due to COVID-19 pandemic: A school-based survey in China. Obesity (Silver Spring). 2021;29:1907–15. [DOI] [PMC free article] [PubMed]
- 23.Lange SJ, Kompaniyets L, Freedman DS, Kraus EM, Porter R, Blanck HM, et al. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2-19 Years - United States, 2018-2020. MMWR Morb Mortal Wkly Rep. 2021;70:1278–83. doi: 10.15585/mmwr.mm7037a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woolford SJ, Sidell M, Li X, Else V, Young DR, Resnicow K, et al. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA. 2021;326:1434–6. doi: 10.1001/jama.2021.15036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brooks CG, Spencer JR, Sprafka JM, Roehl KA, Ma J, Londhe AA, et al. Pediatric BMI changes during COVID-19 pandemic: An electronic health record-based retrospective cohort study. EClinicalMedicine. 2021;38:101026. doi: 10.1016/j.eclinm.2021.101026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wen J, Zhu L, Ji C. Changes in weight and height among Chinese preschool children during COVID-19 school closures. Int J Obes (Lond) 2021;45:2269–73. doi: 10.1038/s41366-021-00912-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl J Med. 2018;379:1303–12. doi: 10.1056/NEJMoa1803527. [DOI] [PubMed] [Google Scholar]
- 28.Gwag SH, Oh YR, Ha JW, Kang E, Nam HK, Lee Y, et al. Weight changes of children in 1 year during COVID-19 pandemic. J Pediatr Endocrinol Metab. 2022;35:297–302. doi: 10.1515/jpem-2021-0554. [DOI] [PubMed] [Google Scholar]
- 29.Jarnig G, Kerbl R, van Poppel MNM. Change in BMI and fitness among primary school children in Austria: A 24-Month follow-up study of 303 children measured before and during the ongoing COVID-19 Pandemic. Sports (Basel). 2022;10. [DOI] [PMC free article] [PubMed]
- 30.Miller A, Bochner R, Sohler N, Calixte R, Chan C, Umpaichitra V, et al. Modified body mass index z-scores in children in New York City during the COVID-19 pandemic. Pediatr Obes. 2022;17:e12958. [DOI] [PMC free article] [PubMed]
- 31.de Onis M, Lobstein T. Defining obesity risk status in the general childhood population: which cut-offs should we use? Int J Pediatr Obes. 2010;5:458–60. doi: 10.3109/17477161003615583. [DOI] [PubMed] [Google Scholar]
- 32.Roizen M, Rodriguez S, Bauer G, Medin G, Bevilacqua S, Varni JW, et al. Initial validation of the Argentinean Spanish version of the PedsQL 4.0 Generic Core Scales in children and adolescents with chronic diseases: acceptability and comprehensibility in low-income settings. Health Qual Life Outcomes. 2008;6:59. doi: 10.1186/1477-7525-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zheng W, Yokomichi H, Matsubara H, Ishikuro M, Kikuya M, Isojima T, et al. Longitudinal changes in body mass index of children affected by the Great East Japan Earthquake. Int J Obes (Lond) 2017;41:606–12. doi: 10.1038/ijo.2017.6. [DOI] [PubMed] [Google Scholar]
- 34.Kang HM, Jeong DC, Suh BK, Ahn MB. The impact of the Coronavirus Disease-2019 pandemic on childhood obesity and Vitamin D status. J Korean Med Sci. 2021;36:e21. doi: 10.3346/jkms.2021.36.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maltoni G, Zioutas M, Deiana G, Biserni GB, Pession A, Zucchini S. Gender differences in weight gain during lockdown due to COVID-19 pandemic in adolescents with obesity. Nutr Metab Cardiovasc Dis. 2021;31:2181–5. doi: 10.1016/j.numecd.2021.03.018. [DOI] [PubMed] [Google Scholar]
- 36.Androutsos O, Perperidi M, Georgiou C, Chouliaras G. Lifestyle Changes and Determinants of Children’s and Adolescents’ Body Weight Increase during the First COVID-19 Lockdown in Greece: The COV-EAT Study. Nutrients. 2021;13. [DOI] [PMC free article] [PubMed]
- 37.Ruiz-Roso MB, de Carvalho Padilha P, Mantilla-Escalante DC, Ulloa N, Brun P, Acevedo-Correa D, et al. Covid-19 confinement and changes of Adolescent’s dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020;12. [DOI] [PMC free article] [PubMed]
- 38.Chang TH, Chen YC, Chen WY, Chen CY, Hsu WY, Chou Y, et al. Weight Gain Associated with COVID-19 Lockdown in Children and Adolescents: A systematic review and meta-analysis. Nutrients. 2021;13. [DOI] [PMC free article] [PubMed]
- 39.Vogel M, Geserick M, Gausche R, Beger C, Poulain T, Meigen C, et al. Age- and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int J Obes (Lond) 2022;46:144–52. doi: 10.1038/s41366-021-00968-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jarnig G, Jaunig J, Kerbl R, Strenger V, Haeusler G, van Poppel MNM. Acceleration in BMI gain following COVID-19 restrictions. A longitudinal study with 7- to 10-year-old primary school children. Pediatr Obes. 2022;17:e12890. doi: 10.1111/ijpo.12890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ge W, Hu J, Xiao Y, Liang F, Yi L, Zhu R, et al. COVID-19 related childhood bmi increases in China: A health surveillancebased ambispective cohort analysis. Am J Prev Med. 2022;63:647–55. [DOI] [PMC free article] [PubMed]
- 42.Mulugeta W, Desalegn H, Solomon S. Impact of the COVID-19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin Obes. 2021;11:e12453. doi: 10.1111/cob.12453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang D, Luo C, Feng X, Qi W, Qu S, Zhou Y, et al. Changes in obesity and lifestyle behaviours during the COVID-19 pandemic in Chinese adolescents: A longitudinal analysis from 2019 to 2020. Pediatr Obes. 2022;17:e12874. doi: 10.1111/ijpo.12874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Adams EL, Caccavale LJ, Smith D, Bean MK. Food insecurity, the home food environment, and parent feeding practices in the Era of COVID-19. Obes (Silver Spring) 2020;28:2056–63. doi: 10.1002/oby.22996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu XY, Han LH, Zhang JH, Luo S, Hu JW, Sun K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS One. 2017;12:e0187668. doi: 10.1371/journal.pone.0187668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: A systematic review of reviews. BMJ Open. 2019;9:e023191. doi: 10.1136/bmjopen-2018-023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weaver RG, Hunt ET, Armstrong B, Beets MW, Brazendale K, Turner-McGrievy G, et al. COVID-19 leads to accelerated increases in children’s BMI z-Score Gain: An interrupted time-series study. Am J Prev Med. 2021;61:e161–e169. doi: 10.1016/j.amepre.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Isojima T, Yokoya S, Ono A, Kato N, Tanaka T, Yokomichi H, et al. Prolonged elevated body mass index in preschool children after the Great East Japan Earthquake. Pediatr Int. 2017;59:1002–9. doi: 10.1111/ped.13340. [DOI] [PubMed] [Google Scholar]
- 49.Danielsson P, Bohlin A, Bendito A, Svensson A, Klaesson S. Five-year outpatient programme that provided children with continuous behavioural obesity treatment enjoyed high success rate. Acta Paediatr. 2016;105:1181–90. doi: 10.1111/apa.13360. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.