Abstract
Background
To date, there has been very limited experimental research on the impact of Yoga on older adults’ mental health during the COVID-19 crisis. We aimed to explore the effect of a web-based Hatha yoga program on psychological and quality of sleep in older adults who self-isolated at home during the initial stage of the COVID-19 outbreak.
Methods
Two hundred volunteers of both sexes were split into experimental (Yoga group, YG) and control (Control group, CG) groups, in a web-based randomized controlled study. All participants were administered the Depression, Anxiety and Stress Scales (DASS-21) and the Pittsburgh sleep quality index (PSQI); at baseline and following an eight-week online Hatha yoga intervention.
Results
The YG showed significant reductions in depression (−56.1%; Z = 5.67, p < 0.01, r = 0.70) anxiety (−64.3%; Z = 5.27, p < 0.01, r = 0.65) and stress (−68.2%; Z = 5.86, r = 0.73) scores, while the CG showed a significant increase in depression. In addition, the total PSQI score of the YG was considerably lower during follow-up (3.38 ± 2.02, p < 0.05) than at baseline (4.8 ± 32, p < 0.05), which indicates an improvement of the quality of sleep. The proportion of individuals experiencing good sleep from the YG increased from 63% to 85% after the Hatha yoga intervention.
Conclusion
The use of a web-based Hatha Yoga intervention program was associated with a beneficial effect on the mental health and quality of sleep in older adults.
Keywords: COVID-19, Distress, Quality of sleep, Yoga, Older adults
1. Introduction
The study of psychological trauma in older adults is becoming a major field of research due to the current and projected growth of older adults' population worldwide. In most developing countries, globalization has resulted in rapid urbanization and out-migration of younger adults, which had a negative psychological impact on the well-being of older adults [1]. Many life and individual changes occur as people enter the old age period; which may, in turn, affect mental health and sleep quality. According to the World Health Organization, approximately 15% of older adults are likely to suffer from a mental health disorder (WHO, 2019). Also, older age is related to the likely occurrence of stressors that can significantly and negatively affect the course of aging [2]. Given these age-related issues, it is important to address older people's mental health needs and concerns. One of the major stressors that older adults have faced lately is the COVID-19 pandemic and the subsequent restrictions (social distancing and self-isolation measures) [3]. The older population has been the most vulnerable to COVID-19 morbidity and mortality [4], as well as social isolation and its harmful consequences on mental health [5]. Older adults showed a stronger emotional response to the COVID-19 crisis compared to people of other age groups [6], thus indicating a higher likelihood of psychological distress in this population [7]; Armitage, Nellums, 2020, [8]. For instance, one study showed that 37.1% of older adults had experienced depression and anxiety during the pandemic [9]. Therefore, actions to address the debilitating consequences of the pandemic need to be established and prioritized in older people.
A range of rehabilitative therapies may assist in dealing with the crisis, including yoga. In fact, various yoga organizations worldwide have recommended yoga to help persons remain mentally healthy during the COVID-19 pandemic (Ministry of AYUSH, 2020). Yoga is one of the widely accepted and structured lifestyle practices which promote the integration of the mind, body and soul (La Torre, 2020). This practice is known as an effective and safe intervention for individuals with depression or anxiety [10,11]. In the older population in particular, yoga has been found to promote both physical [12,13] and mental wellbeing [[12], [13], [14]].
We could find only a few experimental studies on the impact of Yoga on older adults’ health during the COVID-19 crisis. For instance, Yoga has been found to improve the immune system [15] and the well-being [16] of older adults. Interestingly, a study found that online delivery of a yoga program for older adults was as effective as face-to-face program for the majority of participants, and even more effective for some [17]. However, it is not known whether the practice of Hatha yoga is effective for improving mental health and sleep quality in older adults during the pandemic.
In the present study, we aimed to test the hypothesis that a web-based Hatha yoga program would improve psychological distress (i.e., depression, anxiety and stress) and sleep quality in a sample of Tunisian older adults who self-isolated at home during the initial stage of the COVID-19 outbreak, and could be used as a preventive measure against these mental health problems during life crises among older adults.
2. Methods
2.1. Data collection and participants
We adopted an online questionnaire designed in the English language. A link to the electronic survey was distributed by consortium colleagues via a range of methods: invitation via e-mails, shared in consortium's faculties official pages, ResearchGate, LinkedIn and other social media platforms such as Facebook, WhatsApp and Twitter. A snowball sampling strategy, focused on recruiting the general public living in Tunisia during the COVID-19 pandemic, was utilized. The online survey was first disseminated to the general public, and participants were encouraged to circulate it to older adults.
Survey participants were informed that their data will be solely utilized for research. In addition, as per Google's privacy policy (https://policies.google.com/privacy?hl=en), all responses are anonymous and private. Participants were also informed they could withdraw their consent at any time. By completing the survey, participants acknowledged the aforementioned approval form. This study was conducted in accordance with the Declaration of Helsinki (2013) and local regulations.
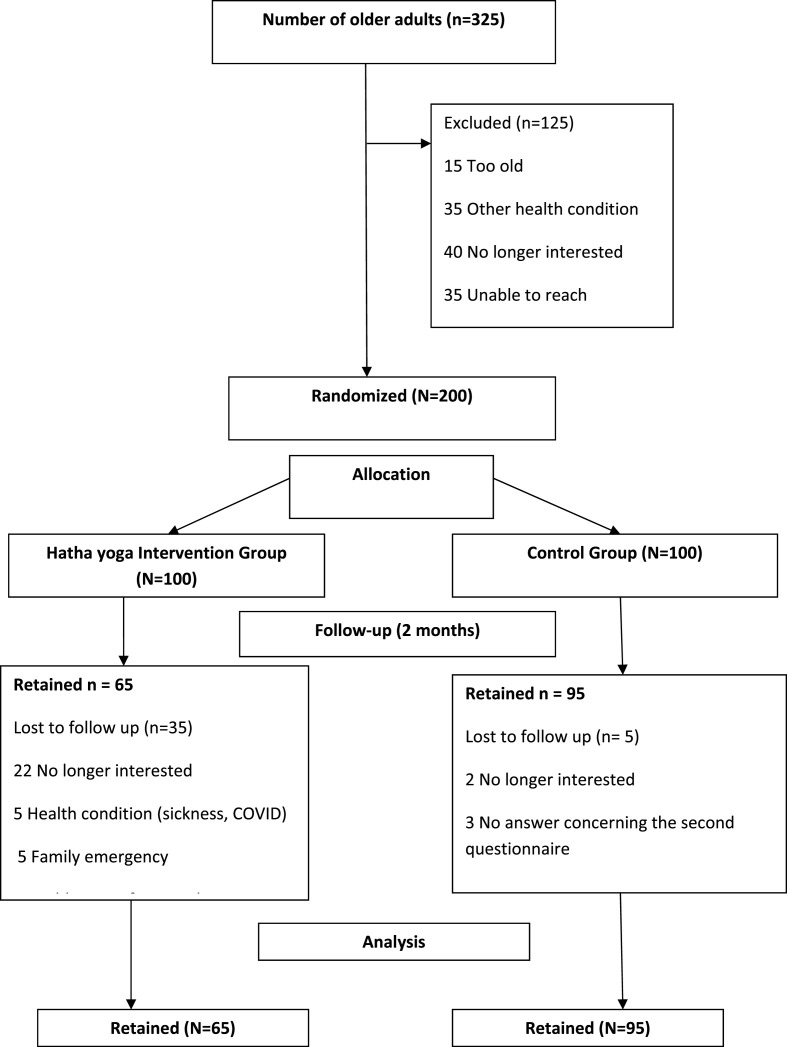
Individuals above the age of 65, of both genders, were eligible to participate. The sample size computation for the present randomized controlled study was performed using the sample size calculator G*Power version 3.1.9.6 (Franz Faul, University of Kiel, Kiel, Germany). The analysis displayed that a sample size 36 subjects would be sufficient to find significant differences (effect size = 0.6, p = 0.05, power [1-β] = 0.80) with an actual power of 80.94%. From March, 21st to June 25th, 2020, we collected data from 325 potential study participants via social media platforms. Based on survey's answers, the study excluded subjects who reported chronic diseases, orthopedic constraints, drug and alcohol use. Likewise, people with dementia, diagnosed mental illness, and inability to execute Hatha yoga were excluded. As shown in Fig. 1 , 200 individuals who met the inclusion criteria were randomly assigned to two groups. Only 160 subjects completed the study procedure due to dropouts and failure to complete the second questionnaire for the experimental group. The final sample included 160 participants (aged 65–80) who had given informed consent to participate: 65 and 95 subjects were assigned to the experimental (YG) and control (CG) groups respectively. During the research period, the wait-list CG received no intervention.
Fig. 1.
Flow diagram for study participants.
2.2. Procedure
An eight-week period of meeting via the Google meet videoconferencing technology was used to deliver the web-based Hatha yoga intervention to participants in the experiment group. The duration chosen relied on the confinement period to see the effect of the intervention during the early stage of the pandemic. It also allowed for comparison with other studies [[18], [19], [20]], in which intervention periods have lasted between 3 and 6 months. A trained Hatha yoga instructor created the yoga class. Before the start of the intervention, the objectives of Hatha yoga for balance and health for the physical, mental, emotional and spiritual dimensions were explained. Participants were given a pamphlet with illustrations of the positions for self-practice.
The experimental group had Hatha yoga sessions of 80 min twice a week, which involved a computer, a camera and video analyses as equipment. The intervention was taught to be progressively challenging over the 8 weeks, and each session was built on tasks introduced during prior sessions.
The control group received no treatment. They received the same questionnaire as other research participants to measure mental health and sleep quality. After the 8-week intervention for the Hatha yoga Group, all participants completed a follow-up online questionnaire.
2.3. Hatha yoga training program
The Hatha yoga classes had a duration of 80 min to help ensure a deep enough practice and produce expected effects. The Hatha yoga exercise program was implemented as the intervention. It is a branch of yoga which consisted of Asanas (physical postures), Praṇayama (breathing exercises), and Dhyana (meditation). Hatha yoga uses gentle and slow moving forms, incorporating a variety of poses that are ideal for elderly for stress relief, relaxation and enhanced mental health benefits [21]. It can be adopted as a recourse to provide mental health and quality of sleep benefits during the pandemic outbreak. Participants in the intervention group were led by a certified Hatha yoga instructor, two times a week for 2 months. The 3 components of Hatha yoga are linked, complement and integrated with each other.
Asana: Yogasanas are known to significantly reduce stress and anxiety (Smith, Hancock, Blake-Mortimer & Eckert, 2007). They are psychophysical practices to culture body and mind. Participants were encouraged to stretch as fully as possible while not exceeding the limits of their comfort and hold the pose for less time if necessary. Repetition was consistent from week to week and linked pose to pose. Each pose was held for approximately 20–30 s, with rest periods lasting 30 s to 1 min between poses. A mixture of standing and seated poses was introduced and practiced. Props such as blankets, blocks, and straps were used. The instruction was to concentrate on their breathing and try to be relaxed.
Pranayama: Diaphragmatic breathing techniques were chosen with special consideration for the physical abilities of older adults. During inspiration, the respiratory flow develops the abdominal area and stretches the ribs and the different parts of the chest. During exhalation, the air will deflate starting from the bottom of the lungs, the ribs, and finally the whole chest. The classes emphasized breathing throughout all postures.
Meditation: It is composed of meditative asana focusing on thoughts and breath. The meditation posture used in the Hatha yoga intervention was Siddhasana which is stable sitting posture, with cross-legged, enabling meditation, aiming at training the body in keeping motionless.
Before starting the training, 10 min were devoted to welcoming participants and checking the availability of participants' equipment. Each Hatha Yoga session took about 80 Minutes to complete, and included four phases:
-
1
Warm-up/Loosening exercises (10 min): This part contains postures to loosen up the body structure. Its objective is to increase range of motion and lubricate joints and also to avoid muscle soreness: ExpGreevasanchalana (Neck Mvt), Skandha chakra (Shoulder rotation), Katichakrasana (Hip exercise), Janu chakra (Knee Mvt).
-
2
Asanas (40 min): These are gentle stretching postures to increase range of motion and progressive muscle relaxation in older adults with special consideration for their physical abilities and tolerances: Standing Asanas: ExpTadasana, kati-cakrasana, Virabhadrasana I, II, and III; Prone Asanas: Exp Bhujangasana (cobra pose) and Dhanurasana (bow pose); Supine Asanas: ExpSetu Bandha Sarvangasana (bridge pose) and SuptaKapotasana (supine pigeon pose).
-
3
Pranayama (15 min): Three activities to rest the body, abdominal breathing is emphasized in each program phase.
-
4
Meditation (15 min): Two Poses (Savasana/Siddhasana) to facilitate a state of relaxation and meditation.
2.4. Survey questionnaire
The survey included an introductory page describing the background and the aims of the survey, the consortium and ethics information for participants. Then, a collection of validated and/or crisis-oriented brief questionnaires were included.
Sociodemographic and clinical data: Sociodemographic data were collected on gender (Male and Female), age (65–75 years; 76–85 years), level of education (High school graduate, diploma/equivalent or less; Bachelor's degree/; Master/Doctorate degree), family situation, (Single/Widowed/divorced; Married/Living as couple) current state of health (respondents were asked to rate their state of health physical condition and indicate any history of chronic illness) and employment status (Retired; Working).
Psychological assessment: Two measures were used, the Depression Anxiety and Stress Scales (DASS-21), and the Pittsburgh Sleep Quality Index (PSQI); in order to assess participants’ psychological distress and quality of sleep, respectively.
2.4.1. The DASS-21
We used the Arabic version of the DASS-21 [22]; Ali et al., 2017) that showed good reliability with a coefficient alpha = 0.883 [23]. This tool consists of 21 items, which comprise three sub-scales assessing the severity of depression, anxiety, and stress symptoms. Each sub-scale contains 7 questions and the answer for each question ranges from 0 (Did not apply to me at all) to 3 (Applied to me very much, or most of the time). Scores on each item of the DASS-21 will need to be multiplied by 2 to calculate the final score (See appendices, Table 1 ).
Table 2.
Shows the average scores and the Δ% differences for the two CG and YG groups before and after confinement.
|
Table 2. Means and standard deviations of study variables. | ||||||
|---|---|---|---|---|---|---|
| Variables | CG (N = 95) |
YG (N = 65) |
||||
| Before | After | Δ (Δ%) | Before | After | Δ (Δ%) | |
| Depression | 7.52 ± 5.49 | 10.95 ± 9.45# | 3.43 (45.7%) | 7.29 ± 5.28 | 3.2 ± 3.58#* | −4.09 (−56.1%)* |
| Anxiety | 5.71 ± 4.28 | 6.88 ± 7.47 | 1.18 (20.7%) | 5.6 ± 5.31 | 2 ± 2.85#* | −3.6 (−64.3%)* |
| Stress | 10.99 ± 6.57 | 11.58 ± 9.35 | 0.59 (5.4%) | 11.32 ± 8.91 | 3.6 ± 5.01#* | −7.72 (−68.2%)* |
| Sleep quality (PSQI global score) | 4.17 ± 2.55 | 5.59 ± 3.43# | 1.42 (34.1%) | 4.83 ± 2* | 3.38 ± 2.02#* | −1.45 (−29.9%)* |
Note. CG: Control group; YG: Yoga Group; PSQI: Pittsburgh Sleep Quality Index.
* Significantly different from CG at p < 0.05; # Significantly different from Before at p < 0.05.
Table 1.
Participants characteristics.
| Variables | CG (N = 95) |
YG (N = 65) |
||
|---|---|---|---|---|
| N | % | N | % | |
| Gender | ||||
| Male | 56 | 57.14% | 42 | 42.86% |
| Female | 39 | 62.90% | 23 | 37.10% |
| Age | ||||
| 65–75 years | 74 | 61.67% | 46 | 38.33% |
| 76–85 years | 21 | 52.50% | 19 | 47.50% |
| Marital status | ||||
| Single/Widowed/divorced | 17 | 94.44% | 1 | 5.56% |
| Married/Living as couple | 78 | 54.93% | 64 | 45.07% |
| Level of Education | ||||
| High school graduate/diploma/equivalent or less | 39 | 78.00% | 11 | 22.00% |
| Bachelor's degree | 34 | 61.82% | 21 | 38.18% |
| Master/Doctorate degree | 22 | 40.00% | 33 | 60.00% |
| Current employment status | ||||
| Retired | 46 | 65.71% | 24 | 34.29% |
| Working | 49 | 54.44% | 41 | 45.56% |
| Current state of health | ||||
| Healthy | 56 | 56.57% | 43 | 43.43% |
| With risk factors for cardiovascular diseases | 30 | 58.82% | 21 | 41.18% |
| With a cardiovascular disease | 9 | 90.00% | 1 | 10.00% |
| Practice of regular physical activity before confinement | ||||
| Yes | 21 | 37.50% | 35 | 62.50% |
| No | 74 | 71.15% | 30 | 28.85% |
| Need for psychosocial support before confinement | ||||
| Never | 76 | 64.41% | 42 | 35.59% |
| Rarely | 13 | 40.63% | 19 | 59.38% |
| Sometimes | 6 | 60.00% | 4 | 40.00% |
| Need for psychosocial support during confinement | ||||
| Never | 49 | 50.52% | 48 | 49.48% |
| Rarely | 18 | 56.25% | 14 | 43.75% |
| Sometimes | 28 | 90.32% | 3 | 9.68% |
Note. CG: Control group; YG: Yoga Group.
2.4.2. The PSQI
We used the Arabic version of the Pittsburgh Sleep Quality Index (PSQI; Suleiman et al., 2010). The scale is a 19 item self-report questionnaire that evaluates subjective sleep quality and different aspects of sleep over a 1-month interval (Buysse, 1989). The subdimensions of the index include subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication, and daytime dysfunction. The responses to the items are weighted on 7 components with a scoring scale between 0 and 3. The total score ranges from 0 to 21, with scores equal to or greater than 5 indicating a poor sleep quality. The Arabic PSQI has a good Cronbach's alpha of 0.77. The modified one-factor model had good discriminative validity, and first order confirmatory factor analysis fitted it well [24].
3. Statistical analysis
Statistical tests were performed using STATISTICA 12 software (StatSoft, France). Data are presented in the text and tables as means ± standard deviations and in the figures as means and standard errors. The assessment of normality by the Shapiro-Wilk test revealed that the distribution of the scales scores deviated from the normal distribution, which imposed the use of nonparametric tests. The Mann Whitney test was used to compare the means of the experimental group and the control group, and the Wilcoxon test was used to compare the means before and after the intervention. The magnitude of change was calculated with r = Z/√n formula. Values of 0.5, 0.3 and 0.1 are considered large; medium and small, respectively [25]. The change recorded between before and after the intervention (Δ = After – Before), as well as the percentage of change ([Δ/Before) *100]), were also calculated. A Mc Nemar Chi-square (χ2) analysis was used to assess the changes in the two experimental groups compared to before the intervention. All the differences observed were considered to be statistically significant for a probability threshold of less than 5% (p < 0.05).
4. Results
The comparison of socio-demographic and clinical variables between Hatha yoga and control group participants is displayed in Table 1.
These tests revealed statistically significant differences in the DASS-21 subscale scores. For the YG, the post-test subscale scores were considerably lower than the pre-test in Depression (Z = 5.67, p < 0.01, r = 0.70), Anxiety (Z = 5.27, p < 0.01, r = 0.65) and Stress (Z = 5.86, r = 0.73).
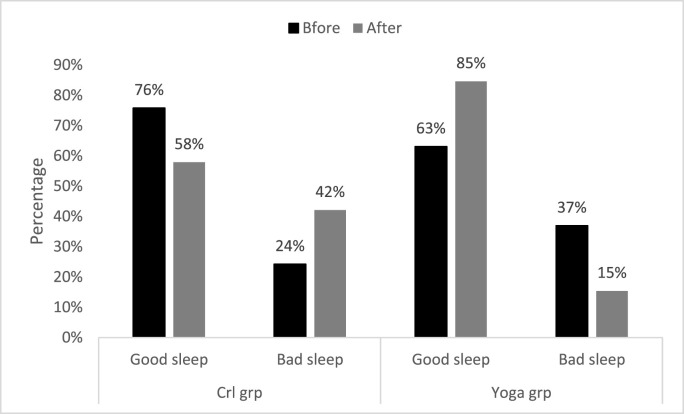
For the CG, DASS-21 scores did not change significantly between time points. Despite the lack of a statistically significant change, the scores on these two sub-scales were higher post-test than pre-test. However, the Depression subscale score was much lower before confinement than during confinement (Z = 2.65, p < 0.01, r = 0.27). In addition, the PSQI scores differed significantly between before and during confinement for CG (z = 5.50, p < 0.05, r = 0.56) with a delta increase Δ% of 34.1%, and for YG (z = 5.69, p < 0.05, r = 0.71) with a delta decrease of 29.9%. The total PSQI score in YG was 3.38 ± 2.02 after the intervention, as compared to 5.59 ± 3.43 in the CG throughout the same time of confinement. The total PSQI score in the YG was considerably lower in the post-test (3.38 ± 2.02, p < 0.05) than in the pre-test (4.8 ± 32, p < 0.05), which indicates an improvement in the quality of sleep. Fig. 2 depicts the frequency of respondents reporting good and poor sleep quality before and during confinement, as well as before and after the Hatha yoga intervention.
Fig. 2.
Frequency (%) of individuals experiencing good (PSQI score ≤ 5) and poor (PSQI score > 5) sleep before and after the intervention for the YG (before and during confinement).
After the Hatha yoga intervention, the frequency of individuals experiencing good sleep quality increased (85%), while the frequency of individuals experiencing poor sleep quality decreased (15%). For the CG, between pre-confinement and during confinement, the frequency of elderly people experiencing good sleep quality decreased from 76% to 58%; while the frequency of individuals experiencing poor sleep quality increased from 24% to 42%. On the other hand, the frequency of older adults experiencing good sleep quality increased from 63% (pre-intervention) to 85% (post-intervention) in the YG, while the frequency of individuals experiencing poor sleep quality decreased by 37%.
5Discussion
To our knowledge, this is one of the first studies to investigate the immediate impact of the Hatha yoga intervention on mental health and sleep quality in older adults in the initial stage of the COVID-19 outbreak. It aimed to investigate the effects of 2 months of web-based Hatha yoga intervention on mental health and quality of sleep-in elderly in Tunisia who self-isolated at home during this period. Findings indicated that the control group participants who received no intervention experienced significant depression, anxiety and stress as estimated using the DASS-21. This change among the control group participants is likely due to the negative effects of the Covid-19 pandemic and the restrictions in social life that were implemented during this period [26,27]; Wilson, Lee and Shook,2021). Furthermore, results showed that there were significant positive effects of the 2-month online Hatha yoga on mental health indicators in the experimental group. Older adults who received the Hatha yoga intervention reported lower scores of stress, anxiety, and depression and better sleep quality.
Our findings showed a substantial difference in the pre- and post-intervention DASS-21 scores for both the experimental and control groups. After a two-month intervention period, participants in the Hatha yoga group experienced a decrease in their levels of depression, anxiety, and stress (from 7.2 to 3.2; from 5.6 to 2; and 11.32 to 3.6 respectively), while the control group participants did not show any significant change in depression and stress. These findings indicate that Hatha yoga has a significant positive effect on all DASS-21 dimensions, thus confirming our hypothesis. These findings corroborate prior experiences with infectious diseases by indicating the increased presence of numerous psychological disorders such as stress, depression, irritability, insomnia, dread, bewilderment, and stigma during earlier periods of infection and quarantine [28,29]. In another studies [30,31], have confirmed that the practice of yoga can bring mental health benefits to older adults' population. Several studies have suggested yoga as a mechanism for reducing stress [[32], [33], [34], [35]], depression [36] and anxiety symptoms in older adults (Allen and Steinkohl, 1987). Yoga has been found to significantly reduce depressive symptoms (Krishnamurthy, Telles, 2007 [[37], [38], [39]]; and stress [40] in older adults. In fact, yoga has been found to aid in the development of resilience factors (Taylor, 2003). This may explain why the Hatha yoga group's DASS-21 scores significantly decreased. This is in line with previous findings suggesting that yoga dramatically lowers depressive symptoms and stress levels in older adults [[37], [38], [39],41].
Another finding of this study was that, after 2 months of Hatha yoga exercise, participants in the intervention group had significantly increased PSQI scores indicating a better sleep quality compared to controls. Particularly, sleep disturbances, use of sleep medication, sleep latency and daytime dysfunction significantly decreased, while sleep duration and habitual sleep efficiency showed no significant differences. Results found in this study further supported a previous study that applied the silver yoga exercise program in a community-dwelling elderly population [37,42], indicating that this exercise program could improve sleep quality of both community and institutionalized older adult populations. Similar findings were reported in that yoga improved different aspects of sleep (including less sleep disturbances and less daytime dysfunction) in a geriatric population after 6 months of practice [43]. The practice of yoga is based on stretching which massage blood vessels (Luskin et al., 2000), and on meditation that facilitate a state of relaxation [44], resulting in less sleep latency and fewer sleep disorders [37,42]. [37] reported that intervention group participants had shorter average duration of sleep but better habitual sleep efficiency than that of control group participants. Although WHO (2020) has proposed recommendations for older adults during confinement, there is a marked reduction in all physical activity, regardless of the level of intensity (vigorous, moderate etc.) during this period [45]. Findings of this study suggest that offering psychological first aid through telemedicine during major disasters such as a pandemic may be potentially beneficial for the management of psychological distress and poor sleep quality in older adults. Particularly, this study suggests that Hatha yoga delivered as a web-based intervention can be a useful, at least for the Tunisian older adult population.
5.1. Study limitations
There are a number of limitations to this study, which should be considered when interpreting its findings. Because there are many different kinds of Hatha yoga, the current findings cannot automatically be applied to other yoga forms. In addition, the majority of participants were in good health and had completed a degree beyond high school. There were considerable differences in sample sizes between the two groups. A larger sample size is required in future longitudinal study in order to replicate the findings.
6. Conclusion
Overall, the findings of this study showed that Hatha yoga training has the potential to improve mental health and sleep quality during major lifetime crises in older adults. Future studies should test the effects of other types of yoga interventions in more diverse populations, while including follow-ups at later time points to examine whether short-term effects are maintained over time.
Author statement
Author Noomen Guelmami contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript. Authors Souad Baklouti, Hana Baklouti, Asma Aloui, Liwa Masmoudi, Nizar Souissi, and Mohamed Jarraya helped to process the data and draft the manuscript. Authors Feten Fekih-Romdhane & Tore Bonsaksen helped write, review & edit the manuscript. All authors read and approved the final manuscript.
Appendices.
Table 1.
Score of depression, anxiety and stress according to the degree of severity
| Depression | Anxiety | Stress | |
|---|---|---|---|
| Normal | 0–9 | 0–7 | 0–14 |
| Mild | 10–13 | 8–9 | 15–18 |
| Moderate | 11–20 | 10–14 | 19–25 |
| Severe | 21–27 | 15–19 | 26–33 |
| Extremely severe | 28+ | 20+ | 34+ |
Table 2.
Hatha yoga training program
| Session/Procedure | Exercises | Duration |
|---|---|---|
| Sukṣmavyayama (Loosening exercises/warm up) | Greevasanchalana (Neck Mvt)/Skandha chakra (shoulder rotation)/KehuniNaman (Elbow Bending) | 15 Minutes |
| MushtikaBandhanan movement of fingers and hand)/Katichakrasana (Hip ex)/Janu chakra (Knee Mvt)/Goolf Naman (Ankle Bending, Rotation)/ | ||
| PadanguliNaman (Toe Bending) | ||
| (Same stretches completed in all sessions) | ||
| Yogasana (Physical postures) | Standing | 40 Minutes |
| Tadasana (Standing Mountain pose or seated, for those not comfortable standing) | ||
| Vrksasana (tree pose) (Can use chair for those not comfortable standing) | ||
| Virabhadrasana (warrior I) | ||
| PrasaritaPadottanasana (Wide-legged standing | ||
| forward bend) | ||
| Seated | ||
| Setu Bandha Sarvangasana (bridge pose) and SuptaKapotasana (supine pigeon pose) | ||
| Vakrsana (Twisted Pose) | ||
| Relaxation and breathing (repeated at the | ||
| completion of each session) | ||
| Praṇayama (Breathingexercises) | Diaphragmatic breathing | 15 Minutes |
| Sit and breathe, relaxation, emphasize exhale for relaxation | ||
| Talked about how to use breath to relax | ||
| Meditation | Pose:Siddhasana/Savasana | 15 Minutes |
References
- 1.Srivastava S., Purkayastha N., Chaurasia H., Muhammad T. Socioeconomic inequality in psychological distress among older adults in India: a decomposition analysis. BMC Psychiatr. 2021;21(1):1–15. doi: 10.1186/s12888-021-03192-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Infurna F.J., Luthar S.S. The multidimensional nature of resilience to spousal loss. J. Pers. Soc. Psychol. 2017;112(6):926–947. doi: 10.1037/pspp0000095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hossain M.M., Sultana A., Purohit N. 2020. Mental Health Outcomes of Quarantine and Isolation for Infection Prevention: A Systematic Umbrella Review of the Global Evidence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D'cruz M., Banerjee D. ‘An invisible human rights crisis’: the marginalization of older adults during the COVID-19 pandemic–An advocacy review. Psychiatr. Res. 2020;292 doi: 10.1016/j.psychres.2020.113369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vahia I.V., Jeste D.V., Reynolds C.F. Older adults and the mental health effects of COVID-19. JAMA. 2020;324(22):2253–2254. doi: 10.1001/jama.2020.21753. [DOI] [PubMed] [Google Scholar]
- 6.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reynolds K., Pietrzak R.H., El-Gabalawy R., Mackenzie C.S., Sareen J. Prevalence of psychiatric disorders in U.S. older adults: findings from a nationally representative survey. World Psychiatr. 2015;14:74–81. doi: 10.1002/wps.20193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatr. Clin. Neurosci. 2020;74(4):281–282. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meng H., Xu Y., Dai J., Zhang Y., Liu B., Yang H. Analyze the psychological impact of COVID-19 among older adults population in China and make corresponding suggestions. Psychiatr. Res. 2020;289 doi: 10.1016/j.psychres.2020.112983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cramer H., Lauche R., Anheyer D., Pilkington K., de Manincor M., Dobos G., Ward L. Yoga for anxiety: a systematic review and meta-analysis of randomized controlled trials. Depress. Anxiety. 2018;35(9):830–843. doi: 10.1002/da.22762. [DOI] [PubMed] [Google Scholar]
- 11.Wang F., Szabo A. Effects of yoga on stress among healthy adults: a systematic review. Alternative Ther. Health Med. 2020;26(4):AT6214. [PubMed] [Google Scholar]
- 12.Kraemer J.M., Marquez D.X. Psychosocial correlates and outcomes of yoga or walking among older adults. J. Psychol. 2009;143(4):390–404. doi: 10.3200/JRLP.143.4.390-404. [DOI] [PubMed] [Google Scholar]
- 13.Tulloch A., Bombell H., Dean C., Tiedemann A. Yoga-based exercise improves health-related quality of life and mental well-being in older people: a systematic review of randomised controlled trials. Age Ageing. 2018;47(4):537–544. doi: 10.1093/ageing/afy044. [DOI] [PubMed] [Google Scholar]
- 14.de Manincor M., Bensoussan A., Smith C., Fahey P., Bourchier S. Establishing key components of yoga interventions for reducing depression and anxiety, and improving well-being: a Delphi method study. BMC Compl. Alternative Med. 2015;15(1):1–10. doi: 10.1186/s12906-015-0614-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shahrbanian S., Alikhani S., Ahmadi Kakavandi M., Hackney A.C. Physical activity for improving the immune system of older adults during the COVID-19 pandemic. Alternative Ther. Health Med. 2020;26(S2):117–125. [PubMed] [Google Scholar]
- 16.Welford P., Östh J., Hoy S., Diwan V., Hallgren M. Effects of yoga and aerobic exercise on wellbeing in physically inactive older adults: randomized controlled trial (FitForAge) Compl. Ther. Med. 2022;66 doi: 10.1016/j.ctim.2022.102815. [DOI] [PubMed] [Google Scholar]
- 17.Haynes A., Gilchrist H., Oliveira J.S., et al. What helps older people persevere with yoga classes? A realist process evaluation of a COVID-19-affected yoga program for fall prevention. BMC Publ. Health. 2022;22:463. doi: 10.1186/s12889-022-12818-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bairy S., Rao M.R., Edla S.R., Manthena S.R., Tatavarti N.G.D. Effect of an integrated naturopathy and yoga program on long-term glycemic control in type 2 diabetes mellitus patients: a prospective cohort study. Int. J. Yoga. 2020;13(1):42. doi: 10.4103/ijoy.IJOY_32_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nosaka M., Okamura H. A single session of an integrated yoga program as a stress management tool for school employees: comparison of daily practice and nondaily practice of a yoga therapy program. J. Alternative Compl. Med. 2015;21(7):444–449. doi: 10.1089/acm.2014.0289. [DOI] [PubMed] [Google Scholar]
- 20.Cheema B.S., Marshall P.W., Chang D., Colagiuri B., Machliss B. Effect of an office worksite-based yoga program on heart rate variability: a randomized controlled trial. BMC Publ. Health. 2011;11(1):1–5. doi: 10.1186/1471-2458-11-578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith A., Greer T., Sheets T., Watson S. Is there more to yoga than exercise? Alternative Ther. Health Med. 2011;17:22–29. [PubMed] [Google Scholar]
- 22.Lovibond S.H., Lovibond P.F. second ed. DASS Publications; Sydney: 1995. Manual for the Depression Anxiety Stress Scales. [Google Scholar]
- 23.Ali A.M., Green J. Factor structure of the depression anxiety stress Scale-21 (DASS-21): unidimensionality of the Arabic version among Egyptian drug users. Subst. Abuse Treat. Prev. Pol. 2019;14(1):1–8. doi: 10.1186/s13011-019-0226-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Suleiman K.H., Yates B.C., Berger A.M., Pozehl B., Meza J. Translating the Pittsburgh sleep quality index into Arabic. West. J. Nurs. Res. 2010;32(2):250–268. doi: 10.1177/0193945909348230. [DOI] [PubMed] [Google Scholar]
- 25.Coolican H. 2009. Research Methods and Statistics in Psychology. (London) [Google Scholar]
- 26.Webb L.M., Chen C.Y. The COVID‐19 pandemic's impact on older adults' mental health: contributing factors, coping strategies, and opportunities for improvement. Int. J. Geriatr. Psychiatr. 2022;37(1) doi: 10.1002/gps.5647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grolli R.E., Mingoti M.E.D., Bertollo A.G., Luzardo A.R., Quevedo J., Réus G.Z., Ignácio Z.M. Impact of COVID-19 in the mental health in elderly: psychological and biological updates. Mol. Neurobiol. 2021;58(5):1905–1916. doi: 10.1007/s12035-020-02249-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharma A., Pillai D.R., Lu M., Doolan C., Leal J., Kim J., Hollis A. Impact of isolation precautions on quality of life: a meta-analysis. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.02.004. Available online 12 February. [DOI] [PubMed] [Google Scholar]
- 30.Pascoe M.C., Bauer I.E. A systematic review of randomised control trials on the effects of yoga on stress measures and mood. J. Psychiatr. Res. 2015;68:270–282. doi: 10.1016/j.jpsychires.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 31.Butterfield N., Schultz T., Rasmussen P., Proeve M. Yoga and mindfulness for anxiety and depression and the role of mental health professionals: a literature review. J. Ment. Health Train Educ. Pract. 2017 [Google Scholar]
- 32.Gura S.T. Yoga for stress reduction and injury prevention at work. Journal of Prevention, Assessment & Rehabilitation. 2002;19:3–7. [PubMed] [Google Scholar]
- 33.Carlson L.E., Speca M., Patel K.D., Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448–474. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- 34.Bower J.E., Woolery A., Sternlieb B., Garet D. Yoga for cancer patients andsurvivors. Cancer Control. 2005;12(3):165–171. doi: 10.1177/107327480501200304. [DOI] [PubMed] [Google Scholar]
- 35.Shapiro S., Astin J., Bishop S., Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int. J. Stress Manag. 2005;12:164–176. [Google Scholar]
- 36.Kaye V.G. An innovative treatment modality for elderly residents of a nursing home. Clin. Gerontol. 1985;3:45–51. [Google Scholar]
- 37.Chen K.M., Chen M.H., Lin M.H., Fan J.T., Lin H.S., Li C.H. Effects of yoga on sleep quality and depression in elders in assisted living facilities. J. Nurs. Res. 2010;18(1):53. doi: 10.1097/JNR.0b013e3181ce5189. WHO (2020). Stay physically active during self-quarantine, available at : http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov-technical-guidance-OLD. [DOI] [PubMed] [Google Scholar]
- 38.Wang Y.Y., Chang H.Y., Lin C.Y. Systematic review of yoga for depression and quality of sleep in older adults. J. Nurs. 2014;61:85–92. doi: 10.6224/JN.61.1.85. [DOI] [PubMed] [Google Scholar]
- 39.Ebrahimi Z., Esmaeilzadeh G., Mohamad R. Comparing the efficacy of yoga exercise and intergenerational interaction program on mental health of elderly. Journal of Research & Health. 2019;9:401–410. Epidemiol. Health, 42. e2020038. [Google Scholar]
- 40.Lindahl E., Tilton K., Eickholt N., Ferguson-Stegall L. Yoga reduces perceived stress and exhaustion levels in healthy elderly individuals. Compl. Ther. Clin. Pract. 2016;24:50–56. doi: 10.1016/j.ctcp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 41.Krishnamurthy M., Telles S. Assessing depression following two ancient Indian interventions: effects of yoga and ayurveda on older adults in a residential home. J. Gerontol. Nurs. 2007;33:17–23. doi: 10.3928/00989134-20070201-05. [DOI] [PubMed] [Google Scholar]
- 42.Chen K.M., Chen M.H., Chao H.C., Hung H.M., Lin H.S., Li C.H. Sleep quality, depression state, and health status of older adults after silver yoga exercises: cluster randomized trail. Int. J. Nurs. Stud. 2009;46(2):154–163. doi: 10.1016/j.ijnurstu.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 43.Manjunath N.K., Telles S. Influence of yoga and Ayurveda on self-rated sleep in a geriatric population. Indian J. Med. Res. 2005;121(5):683–690. [PubMed] [Google Scholar]
- 44.Chen K.M., Tseng W.S., Ting L.F., Huang G.F. Development and evaluation of a yoga exercise programme for older adults. J. Adv. Nurs. 2007;57:432–441. doi: 10.1111/j.1365-2648.2007.04115.x. [DOI] [PubMed] [Google Scholar]
- 45.Trabelsi K., Ammar A., Masmoudi L., et al. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol. Sport. 2021;38(4):495–506. doi: 10.5114/biolsport.2021.101605. [DOI] [PMC free article] [PubMed] [Google Scholar]