Abstract
Background:
The association between Helicobacter pylori infection and overweight, as one of the most common health issues, remains controversial. In this study, we systematically reviewed the effect of H. pylori infection and overweight to get a reliable answer.
Methods:
We used the Preferred Reporting Items for the Systematic Review and Meta-Analysis statement. We searched the association between H. pylori and overweight infection in international databases including Medline, Web of knowledge and Scopus, without any limitations of language, publication type, and publication status in search step of this systematic review from 2000 to 2020. We surveyed the title, abstract and full text of each research studies, and we used Newcastle-Ottawa quality for assessing the quality of each paper. A random effects model was used to calculate the pooled odd ratio with 95% confidence intervals.
Results:
Fifteen papers were eligible for this review. The selected studies reported different Odd Ratio between overweight and H. pylori infection but Odds Ratio (95% confidence interval) in our systematic and meta-analysis study was estimated at 1.42 (95% CI; 1.12, 1.81) and it was statistically significant (P: 0.003).
Conclusion:
H. pylori infection is significantly associated with overweight, therefore, the eradication of H. pylori infection is suggested because this infectious might be resulted in overweight.
Keywords: Helicobacter pylori, Overweight, Meta-analysis
Introduction
Overweight is one of the major health concerns. About two billion adults have overweight and 609 million adults are obese, approximately 39% of the world's adult population. The prevalence of obesity increased from 1975 to 2016 worldwide (1). Excessive caloric intake and decreased physical activity and totally industrialized life are the main reasons for the increasing prevalence of obesity (2).
Raised Body Mass Index (BMI) is a major risk factor for a number of diseases, including diabetes, cardiovascular diseases, musculoskeletal disorders and some cancers, such as endometrial, breast, ovarian, prostate, liver, gallbladder, kidney, and colon cancer (3) and also childhood asthma (4). Overall, obesity is responsible for significant morbidity and health care expenditure (5). Moreover, obesity is related to diabetes mellitus and hypertension (6). Recently researchers suggested a likely association between Helicobacter pylori and overweight. Because the results of the studies are inconsistent, therefore, the association remains still unclear.
Besides, H. pylori infection is one of the most important bacterial infections that could infect about half of the world population (7). Infection with this bacterium has been found to be associated with gastrointestinal disorders such as gastritis, non-ulcer disease, peptic ulcer disease, duodenal ulcer and gastric adenocarcinoma (8). A significant association was observed in H. pylori infection and other non-gastric diseases such as type 2 diabetes mellitus and insulin resistance (9, 10).
Specifically, high prevalence of H. pylori infection (88%) was reported among morbidly obese patients who underwent upper endoscopy prior to bariatric surgery (11). The prevalence of H. pylori infection was 57.2% among obese adults and 27.0% among non-obese adults (12). In spite of the information mentioned, in Taiwan, H. pylori prevalence among 414 morbidly obese and 683 control patients were 43.7% and 60.0%, respectively. There is an inverse relationship between H. pylori infection and overweight. H. pylori infection could down-regulate the obesity (13).
The association between H. pylori infection and overweight remains unclear and controversial. An ecological study reported an inverse correlation between H. pylori prevalence and the rate of overweight/obesity in developed countries of the world (14). In contrast, eradication of H. pylori was associated with significant weight gain as compared to untreated H. pylori patients (15). Another study has reported a linear relationship between H. pylori prevalence and obesity in developing countries (16). In another study, significantly successful eradication of H. pylori infection was observed in 55.0% of the overweight/obese patients and 85.4% in normal adult (17). While in a study, overweight/obese non-diabetic patients found a significantly lower rate of H. pylori eradication than control group (18). Therefore, over-weight may be independent risk factors for H. pylori eradication failure (17).
Due to the conflicting results of the literature about the H. pylori infection and overweight, we performed this systematic and meta-analysis study to find out the effect of H. pylori infection on overweight.
Methods
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (19) statement in this study.
The present study was approved by the Ethics Committee of Hamadan University of Medical Sciences, Hamadan, Iran. The protocol of this study has been registered for Hamadan University of Medical Science (No. 9712077464).
Search method
For this purpose, we searched the international databases such as Medline, Web of knowledge, Scopus, and Science Direct from 2000 to 2020. We used the MeSH keywords such as H. pylori, Overweight, Obesity, and Body Mass Index.
There are several overweight definitions according to the WHO Expert Consultation for Asians, European and American countries. Therefore, overweight patients were defined based on BMI≥25 and the comparison group with BMI<24.9 as control group to cover the most countries that included in this study (20). The outcome of interest was the relationship between H. pylori and overweight. Therefore, we used the related references of the papers to do a perfect search.
There were no limitations of language, date, publication type, and publication status in search step of this systematic review. Of course, some of the studies were excluded: any research had not enough information or were not consistent with our definitions or repetitive or have not a control group. The articles were searched until three months before meta-analysis.
Paper selection
First, we reviewed the title, abstract of the papers. Based on definitions explained in previous section, we selected studies investigated the association of H. pylori infection with overweight in all populations, regardless of age, sex, and race. After that, we used the Newcastle-Ottawa statement (NOS) (21) for assessing the quality of each study.
Data collection
The required data including the name of the first author, publication year, country, subjects source, sample size, mean age (year), H. pylori detected methods and Odds Ratio (OR) entered into a pre-designed excel file. The data of relevant papers were extracted.
Statistical analysis
Weighting averaging was used to combine odds ratio reported by different studies. Each study was given a weight equal to its inverse variance. Q and I2 tests were used for the evaluation of heterogeneity and the analysis was performed with a random-effects model.
Results
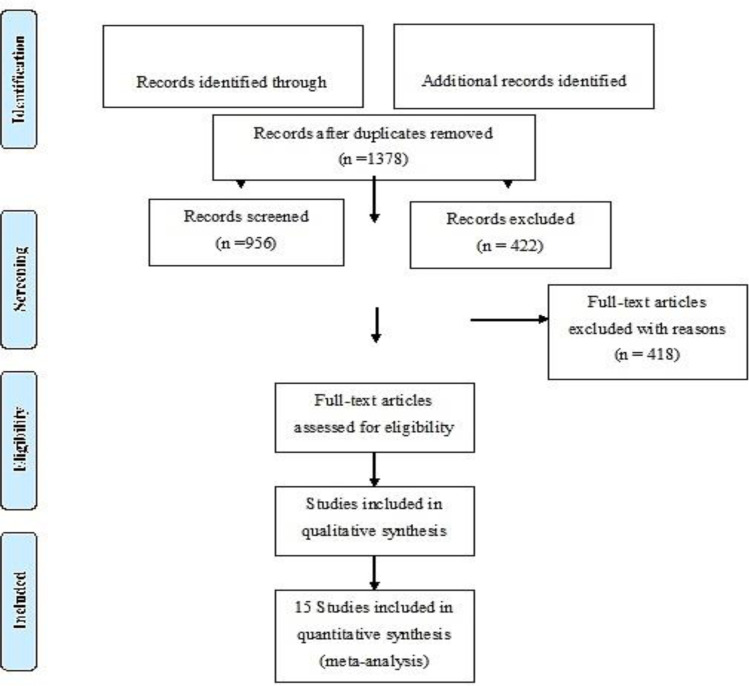
The article selection process in this study demonstrated in Fig. 1. Overall, 1987 papers were retrieved by related keywords. Out of these, 449 articles were published in Medline, 850 articles were published in Scopus, and 688 articles were published in Web of knowledge and finally among these articles, 15 studies were eligible for the review. The forest plot of the selected articles demonstrated in Fig. 2 and the funnels plot was given for the Meta-analyses in Fig. 3.
Fig. 1:
Flow diagram of the articles selection process
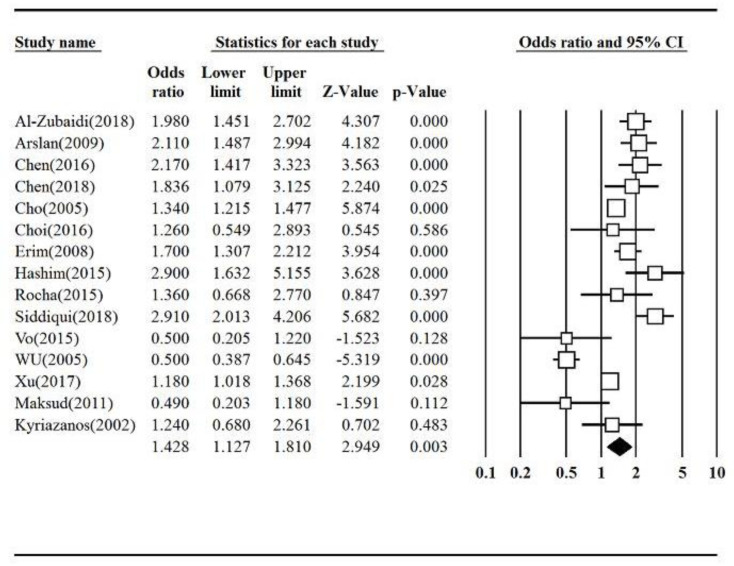
Fig. 2:
Forest plot of the selected articles
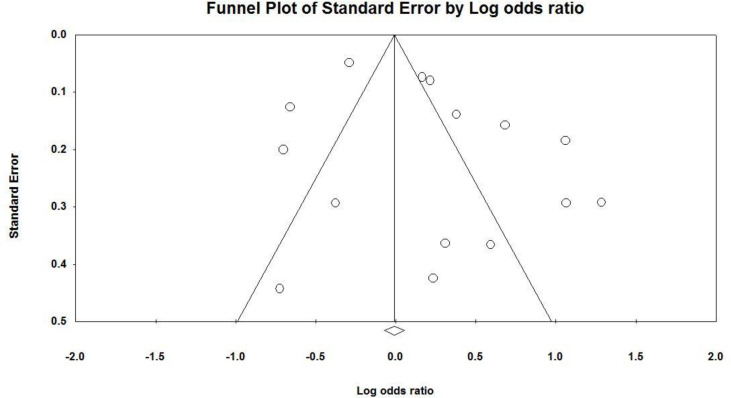
Fig. 3:
Funnel plot of the selected articles
All of the studies were carried out on both sexes and adults were the most dominant population of the studies. The serological methods that detect antibodies in serum or antigens in stool samples were the most common H. pylori diagnostic method among the selected articles (Table 1).
Table 1:
Characteristics and the quality score of the included studies
| Publication year | Nation | Subjects source | Sample size | Mean age (year) | H. pylori test | BMI (kg/m2) | Association (OR) | NOS* | Reference |
|---|---|---|---|---|---|---|---|---|---|
| 2018 | Saudi Arabia | General | 680 | 31.22 ± 8.10 | Histology | ≥30 | Yes (1.98) | 10 | [23] |
| 2018 | Pakistan | General | 662 | 44 ± 16 | Histology | >23 | Yes (2.91) | 9 | [28] |
| 2018 | Taiwan | General | 2604 | 58.7± 13.2 | UBT*1 | ≥24 | Yes (1.836) | 10 | [24] |
| 2017 | China | General | 2977 | 49 ± 19 | Serology | ≥24 | No (1.18) | 9 | [31] |
| 2016 | Taiwan | BE*2 | 736 | 53.8±13.7 | RUT*3 | ≥27 | No (2.17) | 9 | [35] |
| 2016 | Korea | Child | 164 | 9.89±3.28 | Serology | *4 | Yes (1.26) | 8 | [25] |
| 2015 | Bahrain | General | 200 | 38.6±11.06 | RUT*3 | >25 | Yes (2.9) | 9 | [27] |
| 2015 | Brazil | General | 137 | 39.7 ± 12.0 | Histology | ≥25 | No (1.36) | 9 | [33] |
| 2015 | USA | Child | 319 | 10.5 ± 4.7 | SAT*5 | *6 | No (2.0) | 8 | [32] |
| 2011 | Brazil | BP*7 | 100 | 35.4 | Histology | ≥25 | No (0.49) | 8 | [30] |
| 2009 | Turkey | General | 214 | 24.3±5.4 | Serology | ≥30 | Yes (2.11) | 8 | [12] |
| 2008 | Ohio | BP*7 | 2684 | 44 ± 13 | Serology | >30 | Yes (1.7) | 9 | [26] |
| 2005 | USA | General | 7003 | 45.2±0.45 | Serology | ≥25 | No (1.34) | 9 | [34] |
| 2005 | Taiwan | General | 1097 | 31.9 ± 9.2 | Serology | ≥25 | No (0.5) | 8 | [13] |
| 2002 | Salamis | General | 122 | 22.4 ± 2.4 | Serology | ≥25 | No (1.24) | 8 | [29] |
Newcastle-Ottawa quality assessment scale
Urea Breath Test
Barrett's esophagus
Rapid Urea Test
Body weight ≥90th percentile
Stool Antigen Test
Body weight ≥85th percentile
Bariatric patient
In addition, the selected articles were conducted in different geographical regions, in European, Asian and American countries and also among the developed and developing communities (Table 1).
Seven of the selected articles reported that the obesity can be a risk factor for H. pylori infection, because obese patients significantly had more H. pylori infection than non-obese patients. Whereas, eight of the selected articles had a lower risk in different ethnic population and reported that overweight is a protective factor for H. pylori infection (Table 1).
However, the selected studies reported different Odd Ratio ranged from 0.5 (22) to 2.91 (23), the pooled odds Ratio retrieved of these studies was 1.42 (95% CI; 1.12 to 1.81), that it is statistically significant (P=0.003).
Discussion
The association between H. pylori infection and overweight was mentioned from a decade ago (24). We retrieved the inconsistent studies (23, 31), both with and without adjustment for confounding factors (such as age and gender), we concluded that Odd Ratio (95% CI) is 1.42 that it is statistically significant (P: 0.003) and H. pylori infection might be resulted in overweight.
However, the epidemiological studies (23, 24, 28) showed an association between H. pylori infection and overweight, but the mechanisms of H. pylori infection and overweight were not invariably defined. H. pylori infection affects the gastric cells that lead to gastric secretion.
H. pylori infection induces an inflammatory response in many types of gastric cells, especially those responsible for leptin and ghrelin production, that it could affect the regulation of leptin and ghrelin expression. Leptin decreases appetite and food intake, in other words; it is a hormone for regulating energy balance by inhibiting hunger. In obesity, a decreased sensitivity to leptin occurs (similar to insulin resistance in type 2 diabetes), resulting in an inability to detect satiety despite high energy stores and high levels of leptin. Therefore, H. pylori infection could lead to overweight by decreasing the sensitivity to the leptin (25).
H. pylori eradication increases the gastric secretion of ghrelin, which leads to increased appetite and weight gain, means that ghrelin stimulates food intake and promotes weight gain. However, the eradication of H. pylori decreases gastric leptin expression, and this decrease was accompanied by overweight, but the precise effect of gastric secretion of ghrelin on circulating ghrelin levels is not straightforward (26–28). Meanwhile, eradication of H. pylori, resulted in a short-term weight gain that it is related to the eradication and their ulcer healing, so that, thereafter the effect did not last. That way, the decreasing incidence of this infection may be contributing to an increase in appetite and food intake (15).
In total, H. pylori infection causes gastritis or peptic ulcer in a likely mechanism that make an influence on immunological cytokines, leptin, and ghrelin production. Since, Gastric H. pylori colonization could reduce serum levels of leptin and ghrelin, by inhibiting their gastric production because ghrelin and leptin are present in gastric secretions. Moreover, H. pylori colonization may affect their levels in gastric juice. Therefore, H. pylori status affects leptin and ghrelin homeostasis, presumably via intra-gastric interactions (29).
Unfortunately, H. pylori was associated with metabolic disturbances. H. pylori infection also ameliorates glucose homeostasis that leads to over-weight. Eradication of H. pylori could improve carbohydrate metabolism possibly in relation to an increase in GLP-1 (Glucagon-like peptide-1) secretion. GLP-1 secretion may be related to alterations in intestinal microbiota, specifically Lachnobacterium genus, Bifidobacterium adolescentis and Coriobacteriaceae family (30).
Knowledge more about H. pylori infection could help us to inhibit infection (31–37). Obesity, by itself, is a cause of several diseases. The data in our study may be influencing the H. pylori infection eradication and obesity control and lifestyle strategy.
The results of the selected papers were different, because they were performed in various geographical areas and have different diagnosis methods and also different sample sizes. Due to the importance of dietary habits, especially in developing countries, the conclusion reported in this paper could be affected. However, we performed this retrospective study to explore the effect of H. pylori infection on overweight, but, we could not distinguished that the infection influences the overweight or vice versa and the exact mechanism that influence this process. They are the limitations of our study researched in the future.
Conclusion
The purpose of our research was to provide a plan to permit accurate assessment of the effect of H. pylori infection on overweight. H. pylori infection is associated with overweight and these data could be considered in the development of H. pylori eradication and overweight control strategies.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
The authors would like to thank the Research Council of Hamadan University of Medical Sciences, Hamadan, Iran. The study was funded by Vice-chancellor for Research and Technology, Hamadan University of Medical Sciences, Hamadan, Iran.
This study was supported by a grant from the Research deputy of Hamadan University of Medical Sciences, Hamadan University of Medical Sciences, Hamadan, Iran. (No. 9712077464) (IR.UMSHA.REC.1397.872).
Footnotes
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Chooi YC, Ding C, Magkos F. (2019). The epidemiology of obesity. Metabolism, 92:6–10. [DOI] [PubMed] [Google Scholar]
- 2.Damcott C. M. SP, Shuldiner AR. (2003). The genetics of obesity. Endocrinol Metab Clin North Am, 32: 761–786. [DOI] [PubMed] [Google Scholar]
- 3.Kyrou I, Randeva HS, Tsigos C, Kaltsas G, Weickert MO. (2018). Clinical problems caused by obesity. Endotext [Internet]: MDText. com, Inc. [Google Scholar]
- 4.Abreo A, Gebretsadik T, Stone CA, Hartert TV. (2018). The impact of modifiable risk factor reduction on childhood asthma development. Clin Transl Med, 7(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hruby A, Hu FB. (2015). The epidemiology of obesity: a big picture. Pharmacoeconomics, 33(7):673–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chu NF, Wang SC, Chang HY, Wu DM. (2010). Medical services utilization and expenditure of obesity-related disorders in Taiwanese adults. Value Health, 13(6):829–36. [DOI] [PubMed] [Google Scholar]
- 7.Hooi JK, Lai WY, Ng WK, et al. (2017). Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology, 153(2):420–9. [DOI] [PubMed] [Google Scholar]
- 8.Wotherspoon A, Ortiz-Hidalgo C, Falzon M, Isaacson P. (1991). Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet, 338(8776):1175–6. [DOI] [PubMed] [Google Scholar]
- 9.Aydemir S, Bayraktaroglu T, Sert M, et al. (2005). The effect of Helicobacter pylori on insulin resistance. Dig Dis Sci, 50(11):2090–3. [DOI] [PubMed] [Google Scholar]
- 10.Bener A, Micallef R, Afifi M, et al. (2007). Association between type 2 diabetes mellitus and Helicobacter pylori infection. Turk J Gastroenterol, 18(4):225–9. [PubMed] [Google Scholar]
- 11.Al-Akwaa AM. (2010). Prevalence of Helicobacter pylori infection in a group of morbidly obese Saudi patients undergoing bariatric surgery: a preliminary report. Saudi J Gastroenterol, 16(4):264–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arslan E, Atilgan H, Yavasoglu I. (2009). The prevalence of Helicobacter pylori in obese subjects. Eur J Intern Med, 20(7):695–7. [DOI] [PubMed] [Google Scholar]
- 13.Kamada T, Hata J, Kusunoki H, et al. (2005). Eradication of Helicobacter pylori increases the incidence of hyperlipidaemia and obesity in peptic ulcer patients. Dig Liver Dis, 37(1):39–43. [DOI] [PubMed] [Google Scholar]
- 14.Lender N, Talley NJ, Enck P, et al. (2014). Review article: Associations between Helicobacter pylori and obesity--an ecological study. Aliment Pharmacol Ther, 40(1):24–31. [DOI] [PubMed] [Google Scholar]
- 15.Imada T, Mizuno M, Take S, et al. (2016). Helicobacter pylori eradication may increase body mass index, but the effect may not last long. A 10-year observation. J Transl Med Res, 21(2):143–7. [Google Scholar]
- 16.Al-Zubaidi AM, Alzobydi AH, Alsareii SA, et al. (2018). Body Mass Index and Helicobacter pylori among Obese and Non-Obese Patients in Najran, Saudi Arabia: A Case-Control Study. Int J Environ Res Public Health, 15(11):2586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abdullahi M, Annibale B, Capoccia D, et al. (2008). The Eradication of Helicobacter pylori is Affected by Body Mass Index (BMI). Obes Surg, 18(11):1450–4. [DOI] [PubMed] [Google Scholar]
- 18.Peixoto A, Silva M, Gaspar R, et al. (2016). Loose ends in the eradication of Helicobacter pylori infection. J Transl Int Med, 4(4):178–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D LA, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med, 6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization (2000). Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser, 894:i–xii, 1–253. [PubMed] [Google Scholar]
- 21.Stang A. (2010). Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol, 25(9):603–5. [DOI] [PubMed] [Google Scholar]
- 22.Wu MS, Lee WJ, Wang HH, Huang SP, Lin JT. (2005). A case-control study of association of Helicobacter pylori infection with morbid obesity in Taiwan. Arch Intern Med, 165(13):1552–5. [DOI] [PubMed] [Google Scholar]
- 23.Siddiqui B, Yakoob J, Abbas Z, et al. (2018). Distribution of Helicobacter pylori infection and abnormal body-mass index (BMI) in a developing country. J Infect Dev Ctries, 12(5):342–6. [DOI] [PubMed] [Google Scholar]
- 24.Chen LW, Kuo SF, Chen CH, et al. (2018). A community-based study on the association between Helicobacter pylori Infection and obesity. Sci Rep, 8(1):10746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blaser MJ, Atherton JC. (2004). Helicobacter pylori persistence: biology and disease. J Clin Invest, 113(3):321–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Azuma T, Suto H, Ito Y, et al. (2001). Gastric leptin and Helicobacter pylori infection. Gut, 49(3):324–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thalmaier U, Lehn N, Pfeffer K, et al. (2002). Role of tumor necrosis factor alpha in Helicobacter pylori gastritis in tumor necrosis factor receptor 1-deficient mice. Infect Immun, 70(6):3149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pan H GJ, Su Z. (2014). Advances in understanding the interrelations between leptin resistance and obesity. Physiol Behav, 130: 157–69. [DOI] [PubMed] [Google Scholar]
- 29.Roper J, Francois F, Shue PL, et al. (2008). Leptin and ghrelin in relation to Helicobacter pylori status in adult males. J Clin Endocrinol Metab, 93(6):2350–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cornejo-Pareja I, Martín-Núñez GM, Roca-Rodríguez M, et al. (2019). H. pylori Eradication Treatment Alters Gut Microbiota and GLP-1 Secretion in Humans. J Clin Med, 8(4):451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salim MA, Eftekharian MM, Taheri M, Alikhani MY. (2017). Determining the IgM and IgG antibody titer against CMV and Helicobacter pylori in the serum of multiple sclerosis patients comparing to the control group in Hamadan. Hum Antibodies, 26(1):23–28. [DOI] [PubMed] [Google Scholar]
- 32.Nouri F, Kamarehei F, Asghari B, et al. (2022). Prevalence and drug resistance patterns of bacteria isolated from wound and bloodstream nosocomial infections in Hamadan, West of Iran. All Life, 15: 174–182. [Google Scholar]
- 33.Kamarehei F, Khabiri A, Saidijam M, et al. (2018). Designing a novel ELISA method based on CagA, NapA recombinant antigens to increase sensitivity and specificity of Helicobacter pylori whole cell antigen detection. Gastroenterol Hepatol Bed Bench, 11(4):333–342. [PMC free article] [PubMed] [Google Scholar]
- 34.Alikhani MY, Arebestani MR, Sayedin Khorasani M, Majlesi A, Jaefari M. (2014). Evaluation of Helicobacter pylori vacA and cagA Genotypes and Correlation With Clinical Outcome in Patients With Dyspepsia in Hamadan Province, Iran. Iran Red Crescent Med J, 16(11):e19173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kamarehei F, Taheri M, Mohammadi Y, et al. (2020). Prevalence of Helicobacter pylori virulence genes among Iranian infected patients: a systematic review and meta-analysis. Rev Med Microbiol, 31(4):191–200. [Google Scholar]
- 36.Bazmamoun H RZ, Esfahani H, Arefian (2014). Evaluation of Iron deficiency anemia and BMI in children suffering from Helicobacter pylori infection. Iran J Ped Hematol Oncol, 4(4):167–71. [PMC free article] [PubMed] [Google Scholar]
- 37.Ghasemi Basir HR, Ghobakhlou M, Akbari P, et al. (2017). Correlation between the Intensity of Helicobacter pylori Colonization and Severity of Gastritis. Gastroenterol Res Pract, 2017:8320496. [DOI] [PMC free article] [PubMed] [Google Scholar]