Abstract
Background
Home health monitoring shows promise in improving health outcomes; however, navigating the literature remains challenging given the breadth of evidence. There is a need to summarize the effectiveness of monitoring across health domains and identify gaps in the literature. In addition, ethical and user-centered frameworks are important to maximize the acceptability of health monitoring technologies.
Objective
This review aimed to summarize the clinical evidence on home-based health monitoring through a scoping review and outline ethical and user concerns and discuss the challenges of the current user-oriented conceptual frameworks.
Methods
A total of 2 literature reviews were conducted. We conducted a scoping review of systematic reviews in Scopus, MEDLINE, Embase, and CINAHL in July 2021. We included reviews examining the effectiveness of home-based health monitoring in older adults. The exclusion criteria included reviews with no clinical outcomes and lack of monitoring interventions (mobile health, telephone, video interventions, virtual reality, and robots). We conducted a quality assessment using the Assessment of Multiple Systematic Reviews (AMSTAR-2). We organized the outcomes by disease and summarized the type of outcomes as positive, inconclusive, or negative. Second, we conducted a literature review including both systematic reviews and original articles to identify ethical concerns and user-centered frameworks for smart home technology. The search was halted after saturation of the basic themes presented.
Results
The scoping review found 822 systematic reviews, of which 94 (11%) were included and of those, 23 (24%) were of medium or high quality. Of these 23 studies, monitoring for heart failure or chronic obstructive pulmonary disease reduced exacerbations (4/7, 57%) and hospitalizations (5/6, 83%); improved hemoglobin A1c (1/2, 50%); improved safety for older adults at home and detected changing cognitive status (2/3, 66%) reviews; and improved physical activity, motor control in stroke, and pain in arthritis in (3/3, 100%) rehabilitation studies. The second literature review on ethics and user-centered frameworks found 19 papers focused on ethical concerns, with privacy (12/19, 63%), autonomy (12/19, 63%), and control (10/19, 53%) being the most common. An additional 7 user-centered frameworks were studied.
Conclusions
Home health monitoring can improve health outcomes in heart failure, chronic obstructive pulmonary disease, and diabetes and increase physical activity, although review quality and consistency were limited. Long-term generalized monitoring has the least amount of evidence and requires further study. The concept of trade-offs between technology usefulness and acceptability is critical to consider, as older adults have a hierarchy of concerns. Implementing user-oriented frameworks can allow long-term and larger studies to be conducted to improve the evidence base for monitoring and increase the receptiveness of clinicians, policy makers, and end users.
Keywords: smart homes, concerns, user-centered frameworks, clinical evidence, home health monitoring, gerontechnology, telemonitoring, older adults
Introduction
Background
Current health care systems are being pushed to use the capabilities of modern technology outside the hospital to increase efficiency and effectiveness of health delivery [1]. Transforming care processes by using digital platforms and remote monitoring may help address our increasingly older population and higher life expectancies [2]. Smart home and health monitoring technologies have been touted as the future for managing chronic diseases and allowing people to age in place [3-6].
With the technological advancements in the Internet of Things and the widespread use of machine learning and artificial intelligence, the application of smart home technology for aging in place has become more realistic and feasible. Numerous studies on technology development [3,7-10], clinical applicability [11-14], and user considerations [15-17] have been conducted to demonstrate that the technology is ready for mainstream use. There is a plethora of clinically evaluated activity and health recording devices readily available in the market, including wearables (eg, wrist bands, chest bands, and textiles) and ambient sensors (eg, motion sensors, cameras, and pressure sensors) [18-21]. However, the widespread adoption and development of health monitoring platforms remain limited for 2 reasons.
First, the evidence remains siloed within disease-specific reviews or secondary prevention, whether in heart failure [22,23], chronic obstructive pulmonary disease (COPD) [24], diabetes [25], or cardiometabolic health [26], making it difficult to compare effective monitoring models, delineate the overall evidence for home monitoring, and identify where gaps remain [27-29]. There is also a need to differentiate automated monitoring from user-based monitoring, which involves patients texting or phoning in their results.
Second, user and ethical concerns related to monitoring technologies remain major barriers to user adoption, particularly in research [30-33]. Much of the smart home research is focused on the technical development of devices rather than the reliability and usability of smart home systems [34]. Although the feasibility of smart home technology is high in most studies, the acceptability is a critical factor [35]. The benefits of the technology are touted without considering if, how, and at what cost a user may be willing to integrate the technology in their lives [17,36]. In addition, concerns related to data privacy and control, autonomy, and social connectivity are sometimes neglected when designing such systems [37-39].
Objective
This review aimed to map out the literature on two major research questions: (1) what is the evidence for the effectiveness of home-based patient monitoring technologies for improving the health and well-being of older adults and (2) what are the ethical concerns that older adults have with home-based patient monitoring technologies, and what frameworks have been proposed to address these concerns? By addressing both questions, we aimed to provide a tool for researchers in this field to understand what needs to be studied and how to study them while keeping in mind ethical and user-centered practices.
In this study, we defined home health monitoring as the use of technology, omitting telecommunications, to monitor the health of users over time (ie, remotely) [40]. This could include using a variety of technologies, including wearables and ambient sensors, to track physiological parameters, activity levels, and routines or to facilitate rehabilitation and treatment [40].
The first part of this review outlined the clinical evidence for using home health monitoring through a scoping review of systematic reviews on home monitoring interventions. We highlighted the domains being researched; performed quality assessments; and determined whether the evidence is positive, neutral, or negative for home monitoring.
The second part of this review considered ethical concerns when researching and developing smart home monitoring technology and user-centered frameworks that address issues of acceptance and adoption. We outlined the ethical and user-centered frameworks that are available to improve these trials and described the current level of adoption of these frameworks in smart home monitoring.
Methods
To answer the first research question, we conducted a scoping review by searching for systematic reviews following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) methodology [41,42]. The PRISMA checklist can be found in Multimedia Appendix 1.
Data Sources and Search Strategy
Two researchers (AC and RC) conducted a probing search on MEDLINE for studies using smart homes related to older adults. We decided upon a summary of search terms with consultation with an interdisciplinary team of clinicians and engineers. We completed a systematic scoping search on Scopus, MEDLINE, Embase, and CINAHL in July 2021. The search focused on systematic reviews and meta-analyses using smart homes and remote monitoring of older adults (Table S1 in Multimedia Appendix 2).
Study Screening and Inclusion and Exclusion Criteria
Three researchers (AC, RC, and KR) completed abstract screening and full-text screening. Inclusion criteria included systematic reviews written in English with >80% articles focused on older participants (aged >65 years) and published from 2010 to 2021. We excluded studies that focused on assistive technology, mobile health interventions, telephone- or videoconferencing-based interventions, mobile phones and apps, virtual reality, and robots because we focused on automated sensing technologies with clinician intervention. We also excluded studies in which >80% of the articles involved users texting or phoning in the results, rather than using automated monitoring systems. Narrative reviews and technical articles outlining the implementation of these technologies were excluded. We excluded studies that were not journal articles because our focus was on identifying gaps rather than estimating effect sizes.
Data Extraction and Quality Assessment
We created an extraction table and completed extractions independently. The extracted items included population characteristics (number of articles, included diseases or disorders, and percentage of articles including older adults), study type (meta-analysis and quantitative or qualitative study inclusion), and monitoring methods (automated monitoring, mixed automated monitoring, and user-reported monitoring).
We extracted outcome measures, including physiological outcomes (vital signs and blood tests), symptoms or health events (falls, exacerbations, or mortality), health care use, cognitive decline, functional status, adherence to rehabilitation, and activity levels. Studies on human factors included user perspectives on the ethics of home monitoring, the acceptability and usability of devices, and changes in quality of life (QoL) or social connections through technology. We coded outcomes as positive, negative, mixed, or “not enough evidence” according to the author’s assessment and summarized in tables. Finally, we extracted the challenges that the author listed on health monitoring research, ranging from privacy and security concerns and technology acceptability to technical challenges and lack of clinical evidence. The challenges were coded based on what the authors reported. We developed a spreadsheet with a separate column for each challenge that each author would raise. If a new challenge was listed, it was added to a separate column. After we added all the articles and challenges, the 3 authors reduced the number of challenges by grouping together similar challenges by consensus.
Four authors (AC, RC, KR, and DB) conducted a quality appraisal using the AMSTAR-2 checklist and appraised independently after deciding upon critical, important, and unimportant categories. Categories rated as “Critical” included a comprehensive literature search strategy, describing included studies in adequate detail, and accounting for the risk of bias on evidence synthesis. Categories rated as “unimportant” in quality assessment included explaining the selection of study designs, providing a list of excluded studies, and reporting sources of funding for studies included in the review. All the other items were considered important. Studies with ≥2 “No” ratings on critical categories were considered critically low quality, whereas studies with one “No” rating were considered low quality. Moderate-quality studies had ≥2 “important” categories scored as “No,” whereas high-quality studies had <2 “important” categories scored as “No.” The entire list can be found in Multimedia Appendix 3.
Ethics and Stakeholder Participation Review
To answer the second research question, we conducted 2 searches. The first search focused on the ethical challenges and concerns related to smart home technology. We conducted a systematic search from April to May 2021 using Scopus, Web of Science, and Dimensions AI. The search terms are listed in Table S2 in Multimedia Appendix 2. Once we collected all the papers, we screened the titles and abstracts to select the papers to be used for this review. Studies published before 2015 were excluded.
The second search focused on studies involving stakeholder participation while developing health care services and apps. We used Google Scholar to gather related chapters, journals, and articles with keywords (Multimedia Appendix 2). We excluded studies with health care frameworks that did not focus on user centeredness (ie, stakeholder involvement).
Results
Study Characteristics for Question 1: Evidence for Smart Home Technologies
The search yielded 1022 articles, which was reduced to 822 after deduplication (Figure 1). Screening abstracts yielded 480 articles, whereas full-text and additional screening during extractions yielded 94 systematic reviews. Most articles were excluded because they did not focus on telemonitoring technologies (325/728, 44.6%), followed by articles that did not focus on older adult users (120/728, 16.5%) and that were not systematic reviews (104/728, 14.3%). The extraction procedures are presented in Multimedia Appendix 4.
Figure 1.
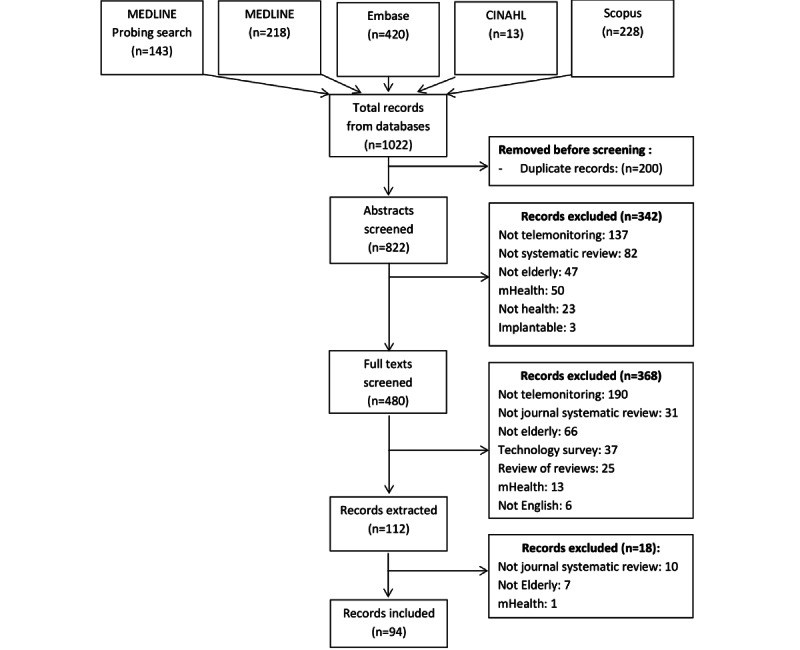
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram outlining the extraction process. mHealth: mobile health.
Figure 2 shows an increasing trend for systematic reviews on home-based patient monitoring technologies, particularly starting in 2018. Live and automonitoring has only become more commonly reviewed since 2018. The number of systematic reviews showed an upward trend starting in 2018.
Figure 2.
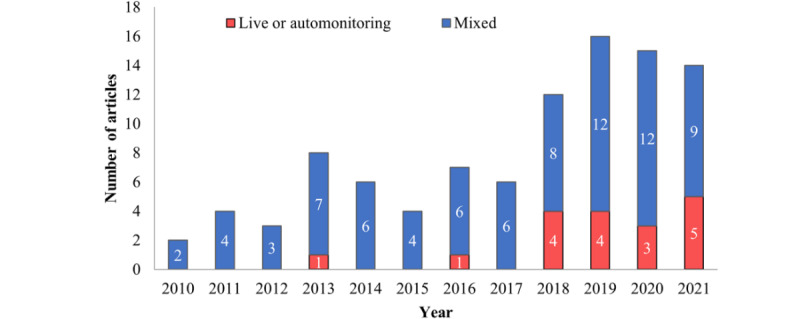
Number of systematic review articles published in each year which included only live or automated monitoring, or had mixed modes of monitoring.
Figure 3 displays the study designs used in each systematic review, organized according to the outcomes discussed. Many articles have presented >1 outcome category. Explanations of the outcomes are described in the methodology.
Figure 3.
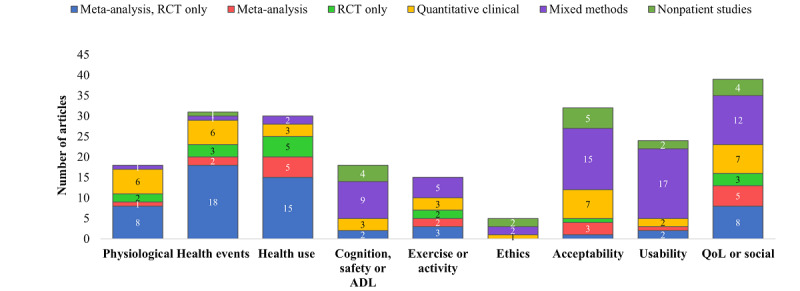
Number of articles according to outcome measures versus study design. ADL: activities of daily living; QoL: quality of life; RCT: randomized controlled trial.
Meta-analyses were most common when reporting physiological evidence, health events, and health use (9/18, 50.0% for physiological; 18/31, 58.1% for health events; and 20/30, 66.7% for health use). Studies focusing on cognition, safety, and activities of daily living (ADLs) were mostly mixed methods or nonpatient studies (13/18, 72.2%), whereas studies focusing on exercise were mostly meta-analyses or quantitative clinical studies (10/15, 66.7%). Most systematic reviews on ethics, acceptability, and usability used mixed methods or nonpatient studies (4/5, 80% for ethics; 20/32, 62.5% for acceptability; and 19/24, 79.2% for usability), and no single study design dominated QoL or social-focused studies.
Figure 4 displays the disease processes studied according to the category of disease monitoring. Acute prevention studies focused on reducing heart failure and COPD exacerbations and fall prevention (24/61, 39.3% reviews). Chronic management studies focused on blood pressure reduction, blood glucose control, and metabolic disease management (13/61, 21.3% reviews). Home monitoring studies focused on monitoring aging and status of patients with dementia (13/61, 21.3% reviews). Studies on physical activity monitoring focused on rehabilitation or increasing physical activity in the older population (11/61, 18.0% reviews).
Figure 4.
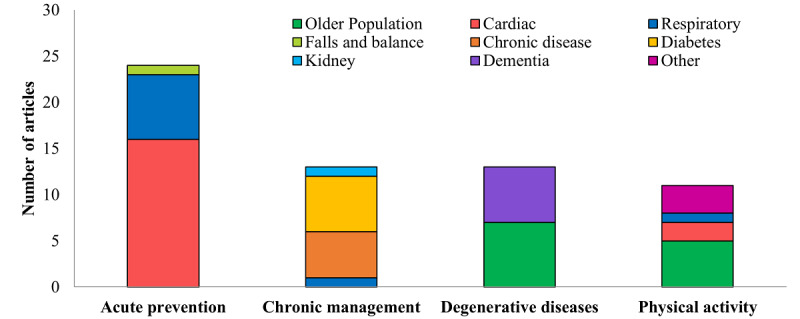
Disease processes organized according to the category of disease monitoring.
The challenges related to current evidence and implementation of home monitoring were also analyzed. Many studies listed multiple challenges, whereas 9.3% (9/94) studies listed no challenge. The most common challenges in the literature included a lack of strong clinical evidence for monitoring (510/94, 53.1%), poor descriptions of methodologies of how patients were monitored (27/94, 28.7%), and applicability to broader patient populations (10/94, 10.6%). On the implementation side related to human factors, the acceptance of technology (33/94, 35.1%), usability of devices (18/94, 19.1%), privacy concerns (17/94, 18%), cost-effectiveness (23/94, 24.2%), and safety concerns with devices (7/94, 7.6%) were listed. Technical challenges were not as commonly reported, although concerns with accuracy (10/94, 10.7%) and connectivity of devices (9/94, 9.7%) were more common than the others.
Figure 5 shows the AMSTAR-2 quality assessments organized according to the monitoring category. Most studies were either of critically low or low quality across all systematic reviews (36/94, 38.3%, and 35/94, 37.2%, respectively). Most studies did not discuss the impact of risk of bias on results (57/94, 60.6%), did not discuss heterogeneity (55/94, 58.5%), or did not include an explicit statement on following a protocol (50/94, 53.2%).
Figure 5.
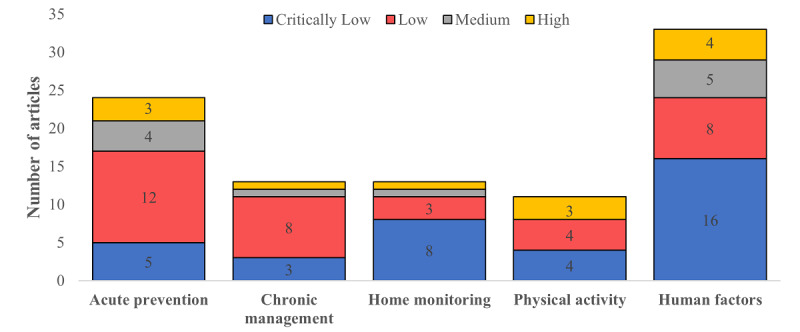
Number of articles listing challenges in smart home monitoring technology grouped by (top-to-bottom): evidence-based challenges, user-based challenges and technical challenges.
Summary of Systematic Reviews on Evidence for Remote Monitoring
Table 1 reports the outcomes from articles that focused on clinical outcomes, as shown in Figure 4. The disease-specific details are presented in Multimedia Appendix 5. In total, 51 of 64 (80%) or more systematic reviews reported positive results across all categories. Chronic disease management and physical activity were among the categories with the largest number of systematic reviews with positive evidence. Evidence was most limited in managing degenerative diseases, health events, and use in rehabilitation interventions.
Table 1.
Summary of evidence for home health monitoring according to category and outcome.
| Outcomes | Reviews | Positive evidence | Negative or inconclusive evidence | |
| Acute prevention | ||||
|
|
Health event (exacerbations, mortality, and falls) | 22/24, (91%) | ||
|
|
Health use (hospitalizations and ERa visits) | 21/24, (88%) | ||
| Chronic disease management | ||||
|
|
Physiological outcomes (blood pressure, HbA1cc, and blood lipids) | 10/14, (71%) | ||
|
|
Health events (mortality, medical events, and pain) | 4/14 (28%) |
|
|
|
|
Health use for chronic disease (hospitalizations and ER visits) | 5/14 (36%) |
|
|
| Degenerative disease monitoring | ||||
|
|
Function and independence | 8/13 (61%) |
|
|
|
|
Cognitive status | 5/13 (38%) | ||
|
|
Health use | 2/13 (15%) |
|
|
| Physical activity | ||||
|
|
Rehabilitation adherence or physical activity increase | 11/11 (100%) | —f | |
aER: emergency room.
bCOPD: chronic obstructive pulmonary disease.
cHbA1c: glycated hemoglobin.
dADLs: activities of daily living.
eQoL: quality of life.
fNot available.
The first theme involved detecting acute events including exacerbations of heart failure, COPD, or falls (Table 1 and Table S1 in Multimedia Appendix 5). Most reviews reported on exacerbations of heart failure and COPD. Monitoring reduced hospitalizations for patients with COPD (5/7, 71.4% studies) and for patients with heart failure (10/14, 71.4% studies). Mortality was unchanged for COPD in a few reviews (3/7, 42.8%) but for most reviews for heart failure (11/14, 78.6%). Only 1 study had reviewed fall interventions in an older population [46]. No clinical studies have focused on atrial fibrillation, although devices showed high specificity and sensitivity in detecting atrial fibrillation.
Management of chronic diseases included managing diabetes, blood pressure, kidney function, or multiple diseases simultaneously (Table 1 and Table S2 in Multimedia Appendix 5). In most studies, home health monitoring helped to reduce hemoglobin A1c (8/10, 80%) and blood pressure (5/9, 55.6%), although the results were more mixed when only considering high- or medium-quality studies. In total, (2/4 (50%) of studies reported reduced mortality, reduced health events, and fewer hospitalizations when monitoring chronic cardiovascular diseases.
Smart home monitoring for ensuring safety of older adults with dementia or cognitive impairment had scarce evidence (Table 1 and Table S3 in Multimedia Appendix 5). Only 1/2 (50%) of studies found no reduction in admission to care homes for monitored patients [87]. In addition, 2/5 (40%) of studies noted progress in the ability to detect cognitive decline [90] and aggression [91]. Most studies found that technologies were not mature enough to detect activity changes or improve independence [88,89,92,105]. For monitoring older adults in general, % (3/N) of studies noted weak evidence for detecting changes in ADLs [82-84], and 2 studies showed improved QoL [85,86].
The fourth theme, rehabilitation adherence and encouraging an active lifestyle at home, included 11 studies (Table 1 and Table S4 in Multimedia Appendix 5). All studies showed positive outcomes for both disease-specific rehabilitation programs and for monitoring older adults in general. Monitoring improved adherence to cardiac rehabilitation, increased activity levels in patients with COPD, and improved motor control in patients after stroke [94-96]. Monitoring increased physical activity in older adults in general in 4 studies, and telerehabilitation with monitoring was found to be as effective as traditional rehabilitation [104]. Wearables helped to increase activity in patients with cancer, improve functioning in patients with arthritis, and improve QoL in postoperative patients [97-99].
Summary of Systematic Reviews on Human Factors
As part of the scoping review, we included studies that focused on human factors such as acceptability of technology, ethical considerations, and costs. Although this was not the focus of question 1, we performed a basic analysis of the outcomes from these studies, recognizing the importance of human factors related to remote monitoring. Table 2 summarizes these 33 studies.
Table 2.
Summary of studies focused on human factors (N=33).
| Outcomes | Reviews, n (%) | Positive evidence | Negative or inconclusive evidence |
| Acceptability for managing chronic diseases | 9 (27) | 5 studies showing high acceptability of monitoring technology [106-110] | |
| Acceptability of telerehabilitation | 1 (3) | —a |
|
| Acceptability for home health monitoring | 14 (42) | 3 studies showing good acceptability of monitoring technologies [115-117] | |
| Costs | 3 (9) | 2 studies showed weak evidence that remote patient monitoring is cost-effective [127,128] |
|
| Ethics | 3 (9) | — | |
| QoLb | 3 (9) | 1 study showed improved QoL with monitoring, though not by validated measures [32] |
aNot available.
bQoL: quality of life.
Of the 24 studies on acceptability, 8/24 (33%) showed good acceptability of monitoring technologies in general. For chronic diseases, 5/9 (56%) showed good acceptability in monitoring for heart failure, COPD, and management of amyotrophic lateral sclerosis, whereas 2/9 (22%) studies on heart failure and COPD were inconclusive. Monitoring acceptability was less clear for generalized home health monitoring and rehabilitation for older adult patients with fatigue. Costs, ethical considerations, and QoL were inconclusive or were descriptive studies.
Although there appear to be positive results from specific diseases, there is a need to continue studying whether remote health monitoring is acceptable for the older adult population. Human factor considerations have been prominent in several studies and deserve closer inspection. Applying appropriate frameworks to the design and development of home health monitoring technology that address human factors such as users’ ethical concerns, like privacy and usability, need to be explored to ensure that users feel at ease while using and installing devices that monitor their lives. Therefore, the second part of our review focused on the ethical concerns that older adults have regarding home health monitoring technology and frameworks that have been suggested to address such concerns.
Study Characteristics for the Ethics and User-Centered Frameworks
The second research question in this study was “what frameworks have been proposed to address the ethical concerns that stakeholders, specifically older adults, have toward home health monitoring?” To learn which frameworks are available to address the ethical issues that arise with home health monitoring, the ethical issues themselves must be uncovered and discussed in more detail.
To explore the ethical issues, we conducted a literature review of ethical challenges. An initial search of 132 papers published since 2015 was conducted, focusing on the ethical challenges and concerns regarding smart home technology. After screening titles and abstracts, 19 papers discussing the ethical challenges and concerns regarding smart home technology were identified. The most discussed concerns are listed in Table 3. The papers were a mix of systematic reviews, literature reviews, qualitative research (including focus groups and interviews), and mixed methods research (qualitative and quantitative research, many using surveys to obtain results).
Table 3.
Summary of ethical concerns with smart home technology for the older population (N=19).
| Outcomes | Reviews, n (%) | Methods used | Reason for concern |
| Privacy [31,33,37,133-142] | 15 (79) | Literature review, mixed methods research, SRa, and qualitative research |
|
| Control [33,37,133-137,139,140,143] | 10 (53) | Literature review, mixed methods research, SR, and qualitative research |
|
| Social concerns [33,37,133,135,137,140-142,144] | 9 (47) | Literature review, mixed methods research, SR, and qualitative research |
|
| Autonomy [31,33,37,133-135,137,140,143] | 9 (47) | Literature review, mixed methods research, SR, and qualitative research |
|
| Stereotypes and stigmatization [31,33,37,134,138] | 5 (26) | Literature review, mixed methods research, and qualitative research |
|
aSR: systematic review.
Ethical Challenges and Concerns
Overview
The first half of this review made it apparent that home monitoring of older adults is a useful intervention. However, many studies have highlighted the ethical challenges and impacts on user acceptance and adoption that arise when using monitoring technology.
When home monitoring technology for aging in place is used appropriately, it can improve QoL, maintain health and wellness of older adults, and support other stakeholders [37]. Such technology may allow increased autonomy and independence in older adults while providing additional support for family members or health care professionals [133]. However, stakeholders and researchers have raised many ethical concerns regarding the design, development, and deployment of home monitoring technologies. This section expands on the most discussed ethical questions and concerns regarding home health monitoring technology, as outlined in Table 3. By understanding these concerns, solutions may be discovered to better design and implement home monitoring technology for older adults and other critical stakeholders [37].
Privacy
Privacy is one of the most critical factors affecting older adults’ willingness to participate in and use smart home technology [31,33,37,133-138,143]. Privacy can be classified into 2 types: physical and informational. Physical privacy relates to the degree to which a person or their personal space is physically accessible [136]. The home is a refuge for privacy and intimacy [139], so it is understandable that some users of home monitoring technology may feel discomfort or apprehension toward any device that can watch them, like an “invisible person” in the room [134,135,137,143]. Any technology that impinges on this refuge will have lower acceptance rates [31,33]. Informational privacy refers to the desire of a person to control the sharing of personal information with others [136]. Informational privacy can be violated when information is used against the wishes of the stakeholder [135]. As home monitoring devices may store and transmit intimate personal data, many older adults, their family members, and health care professionals have reservations about data collection policies including types of data collected, use of the data, and access levels [31,134,139]. Interestingly, the results of a study focused on designing home monitoring technology found that although information privacy was a priority for engineers and designers, physical privacy implications were not considered [143]. This highlighted the need to understand both the user’s and designer’s perspectives and to think broadly about privacy.
Control
Control has multiple meanings including controlling device data, settings, and who makes decisions about the device and the data it collects [31,37,134]. Older adults desire to maintain control of their lives and surroundings for as long as possible, with many seeing value in home monitoring, but more as a last resort or to be used later in life [31,134,138-140]. Older adults want to control whether and how to use the technology, when it is turned on or off, where it is placed, and with whom the collected data are shared [37,134]. From the designer’s perspective, Birchley et al [143] found that a common trend was to give end users the responsibility to decide what the technology did and how much control it had in their lives. However, it was pointed out that many of the ethical challenges regarding the design and implementation of technology, such as an opt-out feature for data sharing, were addressed in the early phases of design, which placed the responsibility of ethical design with the engineers and designers, not the end users [143].
Social Concerns
As shown in Table 3, social interaction is a growing ethical concern. Many older adults strongly indicate that technology should not replace human contact but should foster and promote human communication and support [140,141]. An increase in assistive technology could mean a decrease in human care and human contact for older adults [37,140,141,145]. Older adults, family members, and health care professionals insist that face-to-face interactions should not be systematized or replaced by technology [37,145]. For many older adults, visits from health care workers are often the only human contact they receive on a day-to-day basis, making this interaction critical to their health and well-being [37,140].
Stereotypes and Stigmatization
Stereotypes of “oldness” are often depicted as a time of ill health, dependency, and loneliness [31,33,37]. However, older adults want to be perceived as strong, capable, and independent individuals [31,134]. Any device that projects negative aging stereotypes is likely to be rejected by older adults, even if the device is helpful [31]. Of the older adults interviewed by Astell et al [31], many expressed fears of being judged or discriminated against if they used devices that would stigmatize them as being different, incompetent, or lonely. Participants were more likely to decline social events than to use devices that could incur judgment [31]. Home monitoring devices for older adults must not reflect stereotypes or stigmatizations but should augment how older adults view themselves as independent, competent, and self-reliant users.
Autonomy
Autonomy for smart home technology means “the assistive technology developed for elderly care must not interfere with the will of the person it is designed to care for” [133]. Older adults strive to maintain independence and personal autonomy to avoid burdening their loved ones or society [31,37,140,141]. Therefore, devices that enable or prolong independent performance in meaningful activities are met with great enthusiasm, although some still hold reservations regarding how home health monitoring could affect their autonomy and independence [31,37]. Some older adults expressed concerns about becoming overreliant on the devices [146], whereas others did not want technology to complete a task without them [140]. Nevertheless, older adults overwhelmingly agreed that if home health monitoring technologies could preserve their autonomy and accommodate their preferences, using the technology was preferable to moving into a nursing home [140]. Table 3 summarizes the most discussed ethical concerns along with how often they were mentioned in the collected papers.
Although many older adults admit that they see value in home health technology, they also have wide-ranging reservations about it. The ability to anticipate, address, and respond to ethical challenges and concerns is critical for future development and adoption for stakeholders. Communication between all involved stakeholders must occur to better understand the attitudes, concerns, and demands of those who are most impacted by the technology [31,134,147,148].
Impacts on User Acceptance and Adoption
Overview
In addition to the ethical concerns and challenges for home health monitoring technology discussed, many studies have also examined how ethical challenges and concerns impact user acceptance and adoption of smart home monitoring devices [31,33,37,134,138,142,149-155]. Table 4 highlights the most discussed user aspects found in the literature that influence user acceptance and adoption of home health monitoring technology.
Table 4.
Summary of older adult population’s user aspects concerning smart home technology (N=19).
| Concern | Papers, n (%) | Methods used | Feedback from users |
| User thoughts and feelings (eg, attitudes, preferences, and knowledge) [31,37,133,134,138,142,145,147-149] | 10 (53) | Literature review, mixed methods research, and qualitative research |
|
| User acceptance [31,33,37,134-137,142,143] | 9 (47) | Literature review, mixed methods approach, SRa, and qualitative research |
|
| Usability [37,134,142,144,145] | 6 (32) | Literature review, mixed methods research, and qualitative research |
|
| Usefulness [37,133,134,142,145,149] | 6 (32) | Literature review, mixed methods research, and qualitative research |
|
| User adoption or abandonment [31,33,37,142] | 4 (21) | Literature review, mixed methods research, and SR |
|
aSR: systematic review.
Often, health care tools are designed without considering the values and characteristics of the intended users and other key stakeholders, their literacy levels, or their information goals and preferences. This can result in the technology suffering “social failure modes” [156], ultimately leading to the abandonment of the technology and the need to redesign it [150]. Web-based medical platforms are one example, having low adoptability or acceptance rates [1], potentially because of inadequate user involvement, especially in the early development phases [151-153].
User Acceptance, Usefulness, and Usability
User acceptance is not only based on excitement with technology [31,37] but also on appearance, values and principles, situation, usability, opinions of other direct stakeholders [134], and especially attitude [31,37,134,142]. Older adults who have negative views on aging and associate it with traits such as “illness,” “loneliness,” or “dependency” tend to neglect assistive technology they believe reflects those ideals, whereas those who see aging as positive are more inclined to accept assistive technology and integrate it into their daily lives [31,134]. If end users see no benefit in using an assistive device, there is little chance of acceptance [37,149]. A device that is difficult to operate or understand can lead to frustration and lack of confidence [138,142,149]. Usefulness and usability also tie into developing technology that respects and accommodates end user’s values. If older adults believe that their values are being threatened without explanation, they will likely refuse to accept the technology, whereas they will be more likely to adopt it if those values are upheld [33,134]. All the factors discussed need to be weighed to determine the value of the technology. Tools should be tailored to the users to increase the usability and utility of the technology [154]. The transition from “doing for” users to “doing with” users requires considerable adjustments to be made in both attitude and practice [155].
User Adoption or Abandonment
Beyond the acceptability of technology is the adoption of these devices by end users. Chung et al [37] noted that for aging in place technology to be truly adopted by older adults, devices should address older adults’ values, self-perceptions, and ethical issues at the intersection of aging, technology, and the home environment. Device abandonment is a common reality, whether it is because the device impedes a user’s independence or because of the fear of judgment from their peers [31]. Careful decisions must be made throughout the development process to ensure that the final deliverable is something that is beneficial to the end user and aligns with how the end user sees themselves.
Frameworks for User-Centered Design
Health care tools are often designed without considering the intended users, their literacy levels, information goals, and preferences, which results in user dissatisfaction, leading to the abandonment of the technology and eventually the need to redesign it [150]. Despite constant advancements, web-based medical platforms have low adoptability or acceptance rates [1]. A reason for this is inadequate user involvement, especially in the early development phases [151-153]. We should aim to tailor the technology to the stakeholders’ needs and requirements to increase their usability and utility [154]. User-centered design (UCD) is a framework in which the requirements of stakeholders (including end users) are considered extensively at every stage of the product’s development and design [157]. Table 5 summarizes the various user-centered frameworks developed and adopted in various health care settings based on systematic reviews and individual articles. Moreover, the use of UCD-based evaluation instruments, such as the 11-item measure “UCD-11,” developed by Witteman et al [154] to quantitatively determine the user centeredness of the design and development of health care tools will ensure production of reliable and valid constructs.
Table 5.
User-centered frameworks in medical design.
| Framework | Description |
| 3-phase framework: narrative, metaphorical, and structured [2] |
|
| 3-phase iterative framework in repeated cycles [153] |
|
| Design thinking framework (5 modes executed iteratively, either sequentially or parallelly) [158] |
|
| Information systems research framework (3-phase framework) in combination with the 5 modes of the design thinking framework [158,159] |
|
| The website development model for consumers [150] |
|
| Wearable device design framework (3-level, top-down) [160] |
|
| The eHixa framework [161,162] |
|
aeHix: eHealth innovation matrix.
Discussion
This paper had 2 aims: to present the evidence for home health monitoring through a scoping review and to provide the ethical, user-centered considerations and potential frameworks that can be adopted for developing user-centered health care platforms and personalized support systems. The implementation of remote monitoring requires both a strong backing of the evidence for monitoring to demonstrate its benefits, while maintaining a focus on the ethical and user implications of remote monitoring.
Principal Findings
Evidence for Home Health Monitoring
The first half of this paper presented the evidence related to home health monitoring. We found numerous systematic reviews, with the majority showing positive evidence in monitoring for acute exacerbations of COPD and heart failure, improving blood pressure or diabetes markers, and increasing physical activity levels. When only high- or medium-quality articles were considered, monitoring for COPD and heart failure had the strongest evidence, diabetes had mixed results, and rehabilitation and physical activity had positive results.
Compared to a previous review of systematic reviews on telemedicine in 2010 [163], advancement can be seen in managing heart failure, COPD and for improving HbA1c levels. This result corresponds with the current literature, with a Cochrane review showing positive results in COPD and heart failure [164], another 2 showing improved diabetes management [165,166], and another showing equivalent outcomes comparing telerehabilitation with conventional rehabilitation, although monitoring was not the focus of this review [167].
Ethical Concerns and User-Centered Frameworks
Usability and ethical acceptability are critical for fostering adoption among older adults. The concept of a “trade-off” was key—where multiple factors cannot be attained at the same time, stemming from value tensions between older adults and technology [168]. The value tension between autonomy and privacy was common, where older adults were against being monitored by technology but were willing to relinquish some privacy if they could stay at home longer [37,134,136,139-141,143,149]. Other examples of trade-offs included safety and privacy [134,144], utility and privacy [33,139], and social interaction and privacy [149].
Moreover, end users find disparity between their requirements and the eHealth solutions provided to solve their problems [152]. Although developers may not approach the problem from the users’ perspective [150,152], UCD in eHealth comes with additional practical challenges, including ambiguity regarding the number of iterative cycles to be conducted, time and cost constraints associated with the process, difficulty in overcoming designer bias, and difficulties in establishing multidisciplinary collaboration [169]. To mitigate such challenges, researchers and developers are recommended to refer to established, flexible, reliable, and valid UCD frameworks with respect to the problem statement and the target population.
Limitations and Gaps in the Evidence
The literature on home monitoring is limited. First, the study quality was limited to secondary prevention in heart failure and COPD from 7 high- or medium-quality studies and encouraging rehabilitation and physical activity in 3 studies. Most systematic reviews were of low or critically low quality. We have presented the results of a subgroup analysis of only high- and medium-quality studies to mitigate our own risk of bias. Higher-quality systematic reviews are critical for chronic disease management and generalized monitoring.
Second, the older adult population is not always the focus of reviews. We found only 1 fall detection study in older adults using monitoring devices. A technology survey of fall detection systems found that only 4 out of 57 studies even included older adults in their study [170]. In the screening process, >120 reviews were excluded, as they did not focus on adults aged >65 years. It is important to differentiate these populations, as the acceptability of technology and challenges of multiple morbidities may change the effectiveness of monitoring.
Third, the evidence was sparse for monitoring older adults in general or patients, with most studies suggesting that the technology is not yet mature enough to detect ADLs or cognitive decline [89,92,93]. Most acceptability studies have focused on the domain of general home health monitoring, with the majority being descriptive or showing mixed acceptability. The question of whether it is worthwhile to monitor older adults in general or those with dementia remains unanswered. In addition, telemonitoring and telemedicine are often not differentiated, making it difficult to differentiate the benefits of clinician support from devices and technological support.
From an evidence-focused perspective, monitoring is effective for specific diseases, but challenges remain in researching generalized monitoring for older adults. Clinical outcomes are difficult to measure because objective physiological markers of aging and health utilization need to be measured across years to determine effectiveness. Second, technical obstacles remain in acquiring data from multiple sensors, synchronizing outputs in real time, storing the data, and performing data analytics to detect anomalies or track wellness, all of which can be time consuming and expensive. Finally, the drivers of long-term monitoring are older adults or families focused on the personal benefits of aging in place. Outcomes focused on improving function and independence and older adults’ sense of security and identity may not draw as much broad attention or funding compared with long-term clinical effectiveness and cost-effectiveness studies. Considering the promising results of remote monitoring in specific apps, it is worth researching broader generalized monitoring to improve clinical outcomes.
Limitations of This Review
The main limitation of our review was that we did not have a 2-person validation for screenings and extractions. This may have introduced a bias in the included studies and the information extracted. To mitigate the validation of screenings and extractions, we used common inclusion and exclusion criteria and communicated with team members regularly on questionable papers. In addition, our search was limited to clinical databases to focus on clinical effectiveness rather than technological developments; this may have biased our results related to human factors and monitoring. Moreover, it is possible that multiple studies were included in multiple reviews, which may have biased the results. However, this cannot be mitigated. Finally, we identified gaps in the data but were unable to quantify the effect sizes.
Regarding the ethics- and user-centered framework portion of the review, we did not follow a scoping review methodology, as we found that the qualitative nature of the findings could be summarized with a narrative review. However, we may have missed some trade-offs regarding the acceptability of monitoring technologies.
Future Work
An interesting area for future research is the extraction of what acceptability tools were used in each study. For the second half of this review, we did not provide an exhaustive list of the ethical concerns that end users have regarding home health monitoring technology. We also limited our study to older adults and did not consider family members; health care professionals; and other stakeholders such as engineers, computer scientists, and designers. More value tensions will arise and need to be addressed with the involvement of more stakeholders.
Conclusions
This scoping review provided a summary of the clinical evidence for monitoring older adults in their homes, ethical implications, and user-oriented frameworks found in the literature. Overall, there is promising evidence for monitoring specific diseases and for rehabilitation support, but generalized monitoring for older adults, including cognitive and physical decline, has not been well researched. More clinical research is required for the long-term monitoring of aging in place to provide evidence for its use. To conduct these future studies, we performed a review of important ethical and user considerations and existing user-centered frameworks that must be considered when conducting these monitoring studies. This study demonstrated the need to develop technology with stakeholders rather than for stakeholders to build the evidence for home health monitoring. User-centered frameworks allow stakeholders’ ethical concerns to be addressed and open iterative design opportunities to improve adoption. In developing a system that achieves ethical and UCD, researchers can collect long-term, meaningful data to demonstrate the efficacy of home health monitoring systems for aging in place.
Acknowledgments
This research was funded by the AGE-WELL Core Research Program (AW PP2019 PP3).
Abbreviations
- ADL
activity of daily living
- COPD
chronic obstructive pulmonary disease
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QoL
quality of life
- UCD
user-centered design
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist for evidence for remote monitoring.
Search strategy on evidence for remote monitoring.
Quality assessments for evidence on remote monitoring.
Extraction tables for evidence on remote monitoring.
Summary of evidence for remote monitoring.
Data Availability
We have included the search strings in Multimedia Appendix 2, quality assessments in Multimedia Appendix 3, the extracted articles in Multimedia Appendix 4, and more detailed summaries of the articles extracted in Multimedia Appendix 5 to provide transparency on extractions.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Christodoulakis C, Asgarian A, Easterbrook S. Barriers to adoption of information technology in healthcare. Proceedings of ACM CASCON conference; Proceedings of ACM CASCON conference; Nov, 2017; Toronto, Canada. 2017. [Google Scholar]
- 2.Islind AS, Lindroth T, Lundin J, Steineck G. Co-designing a digital platform with boundary objects: bringing together heterogeneous users in healthcare. Health Technol. 2019 May 20;9(4):425–38. doi: 10.1007/s12553-019-00332-5. [DOI] [Google Scholar]
- 3.Alam MR, Reaz MB, Ali MA. A review of smart homes—past, present, and future. IEEE Transactions Syst Man Cybernetics Part C (Applications and Reviews) 2012 Nov;42(6):1190–203. doi: 10.1109/TSMCC.2012.2189204. [DOI] [Google Scholar]
- 4.Mshali H, Lemlouma T, Moloney M, Magoni D. A survey on health monitoring systems for health smart homes. Int J Industrial Ergonomics. 2018 Jul;66:26–56. doi: 10.1016/j.ergon.2018.02.002. [DOI] [Google Scholar]
- 5.Linkous L, Zohrabi N, Abdelwahed S. Health monitoring in smart homes utilizing internet of things. Proceedings of the 2019 IEEE/ACM International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE); 2019 IEEE/ACM International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE); Sep 25-27, 2019; Arlington, VA, USA. 2019. [DOI] [Google Scholar]
- 6.Majumder S, Aghayi E, Noferesti M, Memarzadeh-Tehran H, Mondal T, Pang Z, Deen MJ. Smart homes for elderly healthcare-recent advances and research challenges. Sensors (Basel) 2017 Oct 31;17(11):2496. doi: 10.3390/s17112496. http://www.mdpi.com/resolver?pii=s17112496 .s17112496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Demiris G, Hensel BK. Technologies for an aging society: a systematic review of "smart home" applications. Yearb Med Inform. 2008:33–40.me08010033 [PubMed] [Google Scholar]
- 8.Chan M, Estève D, Escriba C, Campo E. A review of smart homes- present state and future challenges. Comput Methods Programs Biomed. 2008 Jul;91(1):55–81. doi: 10.1016/j.cmpb.2008.02.001.S0169-2607(08)00043-6 [DOI] [PubMed] [Google Scholar]
- 9.Alaa M, Zaidan A, Zaidan B, Talal M, Kiah M. A review of smart home applications based on Internet of Things. J Network Comput Appl. 2017 Nov;97:48–65. doi: 10.1016/j.jnca.2017.08.017. [DOI] [Google Scholar]
- 10.Talal M, Zaidan AA, Zaidan BB, Albahri AS, Alamoodi AH, Albahri OS, Alsalem MA, Lim CK, Tan KL, Shir WL, Mohammed KI. Smart home-based iot for real-time and secure remote health monitoring of triage and priority system using body sensors: multi-driven systematic review. J Med Syst. 2019 Jan 15;43(3):42. doi: 10.1007/s10916-019-1158-z.10.1007/s10916-019-1158-z [DOI] [PubMed] [Google Scholar]
- 11.Baig MM, Gholamhosseini H. Smart health monitoring systems: an overview of design and modeling. J Med Syst. 2013 Apr 15;37(2):9898. doi: 10.1007/s10916-012-9898-z. [DOI] [PubMed] [Google Scholar]
- 12.Deen MJ. Information and communications technologies for elderly ubiquitous healthcare in a smart home. Pers Ubiquit Comput. 2015 Jun 26;19(3-4):573–99. doi: 10.1007/s00779-015-0856-x. [DOI] [Google Scholar]
- 13.Queirós A, Alvarelhão J, Cerqueira M, Silva A, Santos M, Pacheco Rocha N. Remote care technology: a systematic review of reviews and meta-analyses. Technologies. 2018 Feb 10;6(1):22. doi: 10.3390/technologies6010022. [DOI] [Google Scholar]
- 14.Liu L, Stroulia E, Nikolaidis I, Miguel-Cruz A, Rios Rincon A. Smart homes and home health monitoring technologies for older adults: a systematic review. Int J Med Inform. 2016 Jul;91:44–59. doi: 10.1016/j.ijmedinf.2016.04.007.S1386-5056(16)30064-8 [DOI] [PubMed] [Google Scholar]
- 15.Solaimani S, Keijzer-Broers W, Bouwman H. What we do – and don’t – know about the Smart Home: an analysis of the Smart Home literature. Indoor Built Environ. 2013 Dec 30;24(3):370–83. doi: 10.1177/1420326x13516350. [DOI] [Google Scholar]
- 16.Gram-Hanssen K, Darby SJ. “Home is where the smart is”? Evaluating smart home research and approaches against the concept of home. Energy Res Social Sci. 2018 Mar;37:94–101. doi: 10.1016/j.erss.2017.09.037. [DOI] [Google Scholar]
- 17.Leonardsen AL, Hardeland C, Helgesen AK, Grøndahl VA. Patient experiences with technology enabled care across healthcare settings- a systematic review. BMC Health Serv Res. 2020 Aug 24;20(1):779. doi: 10.1186/s12913-020-05633-4. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-05633-4 .10.1186/s12913-020-05633-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soon S, Svavarsdottir H, Downey C, Jayne D. Wearable devices for remote vital signs monitoring in the outpatient setting: an overview of the field. BMJ Innov. 2020 Jan 14;6(2):55–71. doi: 10.1136/bmjinnov-2019-000354. [DOI] [Google Scholar]
- 19.Peetoom KK, Lexis MA, Joore M, Dirksen CD, De Witte LP. Literature review on monitoring technologies and their outcomes in independently living elderly people. Disabil Rehabil Assist Technol. 2015 Jul;10(4):271–94. doi: 10.3109/17483107.2014.961179. [DOI] [PubMed] [Google Scholar]
- 20.Evans J, Brown M, Coughlan T, Lawson G, Craven M. Human-Computer Interaction: Interaction Technologies. Cham: Springer; 2015. A systematic review of dementia focused assistive technology. [Google Scholar]
- 21.Wang J, Spicher N, Warnecke JM, Haghi M, Schwartze J, Deserno TM. Unobtrusive health monitoring in private spaces: the smart home. Sensors (Basel) 2021 Jan 28;21(3):864. doi: 10.3390/s21030864. https://www.mdpi.com/resolver?pii=s21030864 .s21030864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kitsiou S, Paré G, Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: an overview of systematic reviews. J Med Internet Res. 2015 Mar 12;17(3):e63. doi: 10.2196/jmir.4174. https://www.jmir.org/2015/3/e63/ v17i3e63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenhalgh T, A'Court C, Shaw S. Understanding heart failure; explaining telehealth - a hermeneutic systematic review. BMC Cardiovasc Disord. 2017 Jun 14;17(1):156. doi: 10.1186/s12872-017-0594-2. https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-017-0594-2 .10.1186/s12872-017-0594-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gaveikaite V, Grundstrom C, Winter S, Chouvarda I, Maglaveras N, Priori R. A systematic map and in-depth review of European telehealth interventions efficacy for chronic obstructive pulmonary disease. Respir Med. 2019 Oct;158:78–88. doi: 10.1016/j.rmed.2019.09.005. https://linkinghub.elsevier.com/retrieve/pii/S0954-6111(19)30285-9 .S0954-6111(19)30285-9 [DOI] [PubMed] [Google Scholar]
- 25.Eberle C, Stichling S. Clinical improvements by telemedicine interventions managing type 1 and type 2 diabetes: systematic meta-review. J Med Internet Res. 2021 Feb 19;23(2):e23244. doi: 10.2196/23244. https://www.jmir.org/2021/2/e23244/ v23i2e23244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Neil A, Cocker F, Rarau P, Baptista S, Cassimatis M, Barr Taylor C, Lau AY, Kanuri N, Oldenburg B. Using digital interventions to improve the cardiometabolic health of populations: a meta-review of reporting quality. J Am Med Inform Assoc. 2017 Jul 01;24(4):867–79. doi: 10.1093/jamia/ocw166. https://europepmc.org/abstract/MED/28339628 .2987422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ekeland AG, Bowes A, Flottorp S. Methodologies for assessing telemedicine: a systematic review of reviews. Int J Med Inform. 2012 Jan;81(1):1–11. doi: 10.1016/j.ijmedinf.2011.10.009.S1386-5056(11)00219-X [DOI] [PubMed] [Google Scholar]
- 28.Mallow J, Davis S, Herczyk J, Pauly N, Klos B, Jones A, Jaynes M, Theeke L. Dose of telehealth to improve community-based care for adults living with multiple chronic conditions: a systematic review. E Health Telecommun Syst Netw. 2021;10(01):20–39. doi: 10.4236/etsn.2021.101002. [DOI] [Google Scholar]
- 29.Vegesna A, Tran M, Angelaccio M, Arcona S. Remote patient monitoring via non-invasive digital technologies: a systematic review. Telemed J E Health. 2017 Jan;23(1):3–17. doi: 10.1089/tmj.2016.0051. https://europepmc.org/abstract/MED/27116181 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Courtney KL. Privacy and senior willingness to adopt smart home information technology in residential care facilities. Methods Inf Med. 2008 Jan 19;47(1):76–81. doi: 10.3414/me9104.08010076 [DOI] [PubMed] [Google Scholar]
- 31.Astell A, McGrath C, Dove E. ‘That's for old so and so's!’: does identity influence older adults’ technology adoption decisions? Ageing Soc. 2019 Mar 19;40(7):1550–76. doi: 10.1017/s0144686x19000230. [DOI] [Google Scholar]
- 32.Pal D, Triyason T, Funikul S. Smart homes and quality of life for the elderly: a systematic review. Proceedings of the 2017 IEEE International Symposium on Multimedia (ISM); 2017 IEEE International Symposium on Multimedia (ISM); Dec 11-13, 2017; Taichung, Taiwan. 2017. [DOI] [Google Scholar]
- 33.Curumsing M, Fernando N, Abdelrazek M, Vasa R, Mouzakis K, Grundy J. Emotion-oriented requirements engineering: a case study in developing a smart home system for the elderly. J Syst Softw. 2019 Jan;147:215–29. doi: 10.1016/j.jss.2018.06.077. [DOI] [Google Scholar]
- 34.Marikyan D, Papagiannidis S, Alamanos E. A systematic review of the smart home literature: a user perspective. Technol Forecast Social Change. 2019 Jan;138:139–54. doi: 10.1016/j.techfore.2018.08.015. [DOI] [Google Scholar]
- 35.Kimberly Miller AA. Smart-home technologies to assist older people to live well at home. J Aging Sci. 2013;01(01) doi: 10.4172/2329-8847.1000101. [DOI] [Google Scholar]
- 36.Kapadia V, Ariani A, Li J, Ray PK. Emerging ICT implementation issues in aged care. Int J Med Inform. 2015 Nov;84(11):892–900. doi: 10.1016/j.ijmedinf.2015.07.002.S1386-5056(15)30019-8 [DOI] [PubMed] [Google Scholar]
- 37.Chung J, Demiris G, Thompson HJ. Ethical considerations regarding the use of smart home technologies for older adults: an integrative review. Annu Rev Nurs Res. 2016;34:155–81. doi: 10.1891/0739-6686.34.155. [DOI] [PubMed] [Google Scholar]
- 38.Maher NA, Senders JT, Hulsbergen AF, Lamba N, Parker M, Onnela J, Bredenoord AL, Smith TR, Broekman ML. Passive data collection and use in healthcare: a systematic review of ethical issues. Int J Med Inform. 2019 Sep;129:242–7. doi: 10.1016/j.ijmedinf.2019.06.015.S1386-5056(19)30252-7 [DOI] [PubMed] [Google Scholar]
- 39.Zwijsen SA, Niemeijer AR, Hertogh CM. Ethics of using assistive technology in the care for community-dwelling elderly people: an overview of the literature. Aging Ment Health. 2011 May;15(4):419–27. doi: 10.1080/13607863.2010.543662.936414677 [DOI] [PubMed] [Google Scholar]
- 40.Ogawa M, Togawa T. The concept of the home health monitoring. Proceedings 5th International Workshop on Enterprise Networking and Computing in Healthcare Industry (HealthCom); Proceedings 5th International Workshop on Enterprise Networking and Computing in Healthcare Industry (HealthCom); Jun 7, 2003; Santa Monica, CA, USA. 2003. [DOI] [Google Scholar]
- 41.Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, McKenzie JE. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021 Mar 29;372:n160. doi: 10.1136/bmj.n160. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33781993 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010 Sep 20;5:69. doi: 10.1186/1748-5908-5-69. https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-5-69 .1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sul A, Lyu D, Park D. Effectiveness of telemonitoring versus usual care for chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Telemed Telecare. 2018 Dec 12;26(4):189–99. doi: 10.1177/1357633x18811757. [DOI] [PubMed] [Google Scholar]
- 44.Bolton C, Waters C, Peirce S, Elwyn G, EPSRCMRC Grand Challenge Team Insufficient evidence of benefit: a systematic review of home telemonitoring for COPD. J Eval Clin Pract. 2011 Dec;17(6):1216–22. doi: 10.1111/j.1365-2753.2010.01536.x. [DOI] [PubMed] [Google Scholar]
- 45.Jang J, Lin H, Chen Y, Hsieh M, Huang Y. Role of remote monitoring in detection of atrial arrhythmia, stroke reduction, and use of anticoagulation therapy ― a systematic review and meta-analysis ―. Circ J. 2020;84(11):1922–30. doi: 10.1253/circj.cj-20-0633. [DOI] [PubMed] [Google Scholar]
- 46.Chan JK, Klainin-Yobas P, Chi Y, Gan JK, Chow G, Wu XV. The effectiveness of e-interventions on fall, neuromuscular functions and quality of life in community-dwelling older adults: a systematic review and meta-analysis. Int J Nurs Stud. 2021 Jan;113:103784. doi: 10.1016/j.ijnurstu.2020.103784.S0020-7489(20)30270-4 [DOI] [PubMed] [Google Scholar]
- 47.Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D, Stewart S, Cleland JG. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010 Aug 04;(8):CD007228. doi: 10.1002/14651858.CD007228.pub2. [DOI] [PubMed] [Google Scholar]
- 48.Giamouzis G, Mastrogiannis D, Koutrakis K, Karayannis G, Parisis C, Rountas C, Adreanides E, Dafoulas GE, Stafylas PC, Skoularigis J, Giacomelli S, Olivari Z, Triposkiadis F. Telemonitoring in chronic heart failure: a systematic review. Cardiol Res Pract. 2012;2012:410820–7. doi: 10.1155/2012/410820. doi: 10.1155/2012/410820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Inglis SC, Conway A, Cleland JG, Clark RA. Is age a factor in the success or failure of remote monitoring in heart failure? Telemonitoring and structured telephone support in elderly heart failure patients. Eur J Cardiovasc Nurs. 2015 Jun 29;14(3):248–55. doi: 10.1177/1474515114530611.1474515114530611 [DOI] [PubMed] [Google Scholar]
- 50.Tse G, Chan C, Gong M, Meng L, Zhang J, Su XL, Ali-Hasan-Al-Saegh S, Sawant AC, Bazoukis G, Xia YL, Zhao JC, Lee AP, Roever L, Wong MC, Baranchuk A, Liu T, International Health Informatics Study (IHIS) Network Telemonitoring and hemodynamic monitoring to reduce hospitalization rates in heart failure: a systematic review and meta-analysis of randomized controlled trials and real-world studies. J Geriatr Cardiol. 2018 Apr;15(4):298–309. doi: 10.11909/j.issn.1671-5411.2018.04.008. https://europepmc.org/abstract/MED/29915620 .jgc-15-04-298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Conway A, Inglis SC, Clark RA. Effective technologies for noninvasive remote monitoring in heart failure. Telemed J E Health. 2014 Jun;20(6):531–8. doi: 10.1089/tmj.2013.0267. https://europepmc.org/abstract/MED/24731212 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ding H, Chen SH, Edwards I, Jayasena R, Doecke J, Layland J, Yang IA, Maiorana A. Effects of different telemonitoring strategies on chronic heart failure care: systematic review and subgroup meta-analysis. J Med Internet Res. 2020 Nov 13;22(11):e20032. doi: 10.2196/20032. https://www.jmir.org/2020/11/e20032/ v22i11e20032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Drews T, Laukkanen J, Nieminen T. Non-invasive home telemonitoring in patients with decompensated heart failure: a systematic review and meta-analysis. ESC Heart Fail. 2021 Oct;8(5):3696–3708. doi: 10.1002/ehf2.13475. doi: 10.1002/ehf2.13475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Inglis SC, Clark RA, McAlister FA, Stewart S, Cleland JG. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: abridged Cochrane review. Eur J Heart Fail. 2011 Sep 18;13(9):1028–40. doi: 10.1093/eurjhf/hfr039. doi: 10.1093/eurjhf/hfr039.hfr039 [DOI] [PubMed] [Google Scholar]
- 55.Lin M, Yuan W, Huang T, Zhang H, Mai J, Wang J. Clinical effectiveness of telemedicine for chronic heart failure: a systematic review and meta-analysis. J Investig Med. 2017 Jun;65(5):899–911. doi: 10.1136/jim-2016-000199.jim-2016-000199 [DOI] [PubMed] [Google Scholar]
- 56.Pandor A, Gomersall T, Stevens J, Wang J, Al-Mohammad A, Bakhai A, Cleland JG, Cowie MR, Wong R. Remote monitoring after recent hospital discharge in patients with heart failure: a systematic review and network meta-analysis. Heart. 2013 Dec;99(23):1717–26. doi: 10.1136/heartjnl-2013-303811.heartjnl-2013-303811 [DOI] [PubMed] [Google Scholar]
- 57.Yun JE, Park J, Park H, Lee H, Park D. Comparative effectiveness of telemonitoring versus usual care for heart failure: a systematic review and meta-analysis. J Card Fail. 2018 Jan;24(1):19–28. doi: 10.1016/j.cardfail.2017.09.006.S1071-9164(17)31211-3 [DOI] [PubMed] [Google Scholar]
- 58.Jang S, Kim Y, Cho WK. A systematic review and meta-analysis of telemonitoring interventions on severe COPD exacerbations. Int J Environ Res Public Health. 2021 Jun 23;18(13):6757. doi: 10.3390/ijerph18136757. https://www.mdpi.com/resolver?pii=ijerph18136757 .ijerph18136757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hong Y, Lee SH. Effectiveness of tele-monitoring by patient severity and intervention type in chronic obstructive pulmonary disease patients: a systematic review and meta-analysis. Int J Nurs Stud. 2019 Apr;92:1–15. doi: 10.1016/j.ijnurstu.2018.12.006.S0020-7489(18)30263-3 [DOI] [PubMed] [Google Scholar]
- 60.Pedone C, Lelli D. Systematic review of telemonitoring in COPD: an update. Pneumonol Alergol Pol. 2015;83(6):476–84. doi: 10.5603/PiAP.2015.0077. https://journals.viamedica.pl/pneumonologia_i_alergologia_pol/article/view/43870 .VM/OJS/J/43870 [DOI] [PubMed] [Google Scholar]
- 61.Yang F, Xiong Z, Yang C, Li L, Qiao G, Wang Y, Zheng T, He H, Hu H. Continuity of care to prevent readmissions for patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. COPD. 2017 Apr;14(2):251–61. doi: 10.1080/15412555.2016.1256384. [DOI] [PubMed] [Google Scholar]
- 62.Lelli D, Antonelli IR, Adiletta V, Pedone C. Is telemonitoring effective in older adults affected by heart failure? A meta-analysis focused on this population. J Gerontol Geriatr. 2019;67(2) [Google Scholar]
- 63.Pekmezaris R, Tortez L, Williams M, Patel V, Makaryus A, Zeltser R, Sinvani L, Wolf-Klein G, Lester J, Sison C, Lesser M, Kozikowski A. Home telemonitoring in heart failure: a systematic review and meta-analysis. Health Aff (Millwood) 2018 Dec;37(12):1983–9. doi: 10.1377/hlthaff.2018.05087. [DOI] [PubMed] [Google Scholar]
- 64.Yanicelli L, Goy C, Martínez EC, Herrera M. Heart failure non-invasive home telemonitoring systems: a systematic review. Comput Methods Programs Biomed. 2021 Apr;201:105950. doi: 10.1016/j.cmpb.2021.105950.S0169-2607(21)00024-9 [DOI] [PubMed] [Google Scholar]
- 65.Kamei T, Yamamoto Y, Kajii F, Nakayama Y, Kawakami C. Systematic review and meta-analysis of studies involving telehome monitoring-based telenursing for patients with chronic obstructive pulmonary disease. Jpn J Nurs Sci. 2013 Dec;10(2):180–92. doi: 10.1111/j.1742-7924.2012.00228.x. [DOI] [PubMed] [Google Scholar]
- 66.Taylor ML, Thomas EE, Snoswell CL, Smith AC, Caffery LJ. Does remote patient monitoring reduce acute care use? A systematic review. BMJ Open. 2021 Mar 02;11(3):e040232. doi: 10.1136/bmjopen-2020-040232. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=33653740 .bmjopen-2020-040232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Clark RA. Telehealth in the elderly with chronic heart failure: what is the evidence? Stud Health Technol Inform. 2018;246:18–23. [PubMed] [Google Scholar]
- 68.Yun JE, Park JE, Park J, Lee HY, Park DA. Comparative effectiveness of telemonitoring versus usual care for heart failure: a systematic review and meta-analysis. J Card Fail. 2018 Jan;24(1):19–28. doi: 10.1016/j.cardfail.2017.09.006.S1071-9164(17)31211-3 [DOI] [PubMed] [Google Scholar]
- 69.van den Berg N, Schumann M, Kraft K, Hoffmann W. Telemedicine and telecare for older patients--a systematic review. Maturitas. 2012 Oct;73(2):94–114. doi: 10.1016/j.maturitas.2012.06.010.S0378-5122(12)00227-7 [DOI] [PubMed] [Google Scholar]
- 70.Paré G, Moqadem K, Pineau G, St-Hilaire C. Clinical effects of home telemonitoring in the context of diabetes, asthma, heart failure and hypertension: a systematic review. J Med Internet Res. 2010 Jun 16;12(2):e21. doi: 10.2196/jmir.1357. https://www.jmir.org/2010/2/e21/ v12i2e21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wu C, Wu Z, Yang L, Zhu W, Zhang M, Zhu Q, Chen X, Pan Y. Evaluation of the clinical outcomes of telehealth for managing diabetes: a PRISMA-compliant meta-analysis. Medicine (Baltimore) 2018 Oct;97(43):e12962. doi: 10.1097/MD.0000000000012962. doi: 10.1097/MD.0000000000012962.00005792-201810260-00059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lee S, Chan CK, Chua SS, Chaiyakunapruk N. Comparative effectiveness of telemedicine strategies on type 2 diabetes management: a systematic review and network meta-analysis. Sci Rep. 2017 Oct 04;7(1):12680. doi: 10.1038/s41598-017-12987-z. doi: 10.1038/s41598-017-12987-z.10.1038/s41598-017-12987-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.De Groot J, Wu D, Flynn D, Robertson D, Grant G, Sun J. Efficacy of telemedicine on glycaemic control in patients with type 2 diabetes: a meta-analysis. World J Diabetes. 2021 Feb 15;12(2):170–97. doi: 10.4239/wjd.v12.i2.170. https://www.wjgnet.com/1948-9358/full/v12/i2/170.htm . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Greenwood DA, Young HM, Quinn CC. Telehealth remote monitoring systematic review: structured self-monitoring of blood glucose and impact on A1c. J Diabetes Sci Technol. 2014 Mar;8(2):378–89. doi: 10.1177/1932296813519311. https://europepmc.org/abstract/MED/24876591 .1932296813519311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Faruque LI, Wiebe N, Ehteshami-Afshar A, Liu Y, Dianati-Maleki N, Hemmelgarn BR, Manns BJ, Tonelli M, Alberta Kidney Disease Network Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. CMAJ. 2017 Mar 06;189(9):E341–64. doi: 10.1503/cmaj.150885. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=27799615 .cmaj.150885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Marcolino MS, Maia JX, Alkmim MB, Boersma E, Ribeiro AL. Telemedicine application in the care of diabetes patients: systematic review and meta-analysis. PLoS One. 2013;8(11):e79246. doi: 10.1371/journal.pone.0079246. https://dx.plos.org/10.1371/journal.pone.0079246 .PONE-D-13-21538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang W, Cheng B, Zhu W, Huang X, Shen C. Effect of telemedicine on quality of care in patients with coexisting hypertension and diabetes: a systematic review and meta-analysis. Telemed J E Health. 2021 Jun;27(6):603–14. doi: 10.1089/tmj.2020.0122. [DOI] [PubMed] [Google Scholar]
- 78.Luo L, Ye M, Tan J, Huang Q, Qin X, Peng S, Wang Y, Zou T, Jie X, Liu X, Wu Y. Telehealth for the management of blood pressure in patients with chronic kidney disease: a systematic review. J Telemed Telecare. 2017 Nov 27;25(2):80–92. doi: 10.1177/1357633x17743276. [DOI] [PubMed] [Google Scholar]
- 79.Miguel-Cruz A, Felipe Bohórquez A, Aya Parra PA. What does the literature say about using electronic pillboxes for older adults? A systematic literature review. Disabil Rehabil Assist Technol. 2019 Nov 19;14(8):776–87. doi: 10.1080/17483107.2018.1508514. [DOI] [PubMed] [Google Scholar]
- 80.Liu P, Li G, Jiang S, Liu Y, Leng M, Zhao J, Wang S, Meng X, Shang B, Chen L, Huang SH. The effect of smart homes on older adults with chronic conditions: a systematic review and meta-analysis. Geriatr Nurs. 2019;40(5):522–30. doi: 10.1016/j.gerinurse.2019.03.016.S0197-4572(18)30627-X [DOI] [PubMed] [Google Scholar]
- 81.Aardoom JJ, Loheide-Niesmann L, Ossebaard HC, Riper H. Effectiveness of eHealth interventions in improving treatment adherence for adults with obstructive sleep apnea: meta-analytic review. J Med Internet Res. 2020 Feb 18;22(2):e16972. doi: 10.2196/16972. https://www.jmir.org/2020/2/e16972/ v22i2e16972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lenouvel E, Novak L, Nef T, Klöppel S. Advances in sensor monitoring effectiveness and applicability: a systematic review and update. Gerontologist. 2020 May 15;60(4):e299–308. doi: 10.1093/geront/gnz049.5491622 [DOI] [PubMed] [Google Scholar]
- 83.Reeder B, Meyer E, Lazar A, Chaudhuri S, Thompson HJ, Demiris G. Framing the evidence for health smart homes and home-based consumer health technologies as a public health intervention for independent aging: a systematic review. Int J Med Inform. 2013 Jul;82(7):565–79. doi: 10.1016/j.ijmedinf.2013.03.007. https://europepmc.org/abstract/MED/23639263 .S1386-5056(13)00065-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang Y, D'Haeseleer I, Coelho J, Vanden Abeele V, Vanrumste B. Recognition of bathroom activities in older adults using wearable sensors: a systematic review and recommendations. Sensors (Basel) 2021 Mar 20;21(6):2176. doi: 10.3390/s21062176. https://www.mdpi.com/resolver?pii=s21062176 .s21062176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Turjamaa R, Pehkonen A, Kangasniemi M. How smart homes are used to support older people: an integrative review. Int J Older People Nurs. 2019 Dec 12;14(4):e12260. doi: 10.1111/opn.12260. [DOI] [PubMed] [Google Scholar]
- 86.Khosravi P, Ghapanchi AH. Investigating the effectiveness of technologies applied to assist seniors: a systematic literature review. Int J Med Inform. 2016 Jan;85(1):17–26. doi: 10.1016/j.ijmedinf.2015.05.014.S1386-5056(15)30003-4 [DOI] [PubMed] [Google Scholar]
- 87.Brims L, Oliver K. Effectiveness of assistive technology in improving the safety of people with dementia: a systematic review and meta-analysis. Aging Ment Health. 2019 Aug;23(8):942–51. doi: 10.1080/13607863.2018.1455805. [DOI] [PubMed] [Google Scholar]
- 88.Fleming R, Sum S. Empirical studies on the effectiveness of assistive technology in the care of people with dementia: a systematic review. J Assistive Technologies. 2014 Mar 12;8(1):14–34. doi: 10.1108/JAT-09-2012-0021. [DOI] [Google Scholar]
- 89.Pol MC, Poerbodipoero S, Robben S, Daams J, van Hartingsveldt M, de Vos R, de Rooij SE, Kröse B, Buurman BM. Sensor monitoring to measure and support daily functioning for independently living older people: a systematic review and road map for further development. J Am Geriatr Soc. 2013 Dec;61(12):2219–27. doi: 10.1111/jgs.12563. [DOI] [PubMed] [Google Scholar]
- 90.Lussier M, Lavoie M, Giroux S, Consel C, Guay M, Macoir J, Hudon C, Lorrain D, Talbot L, Langlois F, Pigot H, Bier N. Early detection of mild cognitive impairment with in-home monitoring sensor technologies using functional measures: a systematic review. IEEE J Biomed Health Inform. 2019 Mar;23(2):838–47. doi: 10.1109/jbhi.2018.2834317. [DOI] [PubMed] [Google Scholar]
- 91.Khan S, Ye B, Taati B, Mihailidis A. Detecting agitation and aggression in people with dementia using sensors-A systematic review. Alzheimers Dement. 2018 Jun;14(6):824–32. doi: 10.1016/j.jalz.2018.02.004. doi: 10.1016/j.jalz.2018.02.004.S1552-5260(18)30046-3 [DOI] [PubMed] [Google Scholar]
- 92.Piau A, Wild K, Mattek N, Kaye J. Current state of digital biomarker technologies for real-life, home-based monitoring of cognitive function for mild cognitive impairment to mild Alzheimer disease and implications for clinical care: systematic review. J Med Internet Res. 2019 Aug 30;21(8):e12785. doi: 10.2196/12785. https://www.jmir.org/2019/8/e12785/ v21i8e12785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Narasimhan R, McGlade C. Current state of non-wearable sensor technologies for monitoring activity patterns to detect symptoms of mild cognitive impairment to Alzheimer's disease. Int J Alzheimers Dis. 2021 Feb 10;2021:2679398–18. doi: 10.1155/2021/2679398. doi: 10.1155/2021/2679398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016 Aug 01;102(15):1183–92. doi: 10.1136/heartjnl-2015-308966.heartjnl-2015-308966 [DOI] [PubMed] [Google Scholar]
- 95.Bonnevie T, Smondack P, Elkins M, Gouel B, Medrinal C, Combret Y, Muir J, Cuvelier A, Prieur G, Gravier F. Advanced telehealth technology improves home-based exercise therapy for people with stable chronic obstructive pulmonary disease: a systematic review. J Physiother. 2021 Jan;67(1):27–40. doi: 10.1016/j.jphys.2020.12.006. https://linkinghub.elsevier.com/retrieve/pii/S1836-9553(20)30142-9 .S1836-9553(20)30142-9 [DOI] [PubMed] [Google Scholar]
- 96.Appleby E, Gill ST, Hayes LK, Walker TL, Walsh M, Kumar S. Effectiveness of telerehabilitation in the management of adults with stroke: a systematic review. PLoS One. 2019;14(11):e0225150. doi: 10.1371/journal.pone.0225150. https://dx.plos.org/10.1371/journal.pone.0225150 .PONE-D-19-15793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Blackwood J, Rybicki K. Outcomes of telehealth-delivered physical activity programs in adult cancer survivors: a systematic review. Rehab Oncol. 2021 Jul;39(3):128–36. doi: 10.1097/01.REO.0000000000000249. [DOI] [Google Scholar]
- 98.Schäfer AG, Zalpour C, von Piekartz H, Hall TM, Paelke V. The efficacy of electronic health-supported home exercise interventions for patients with osteoarthritis of the knee: systematic review. J Med Internet Res. 2018 Apr 26;20(4):e152. doi: 10.2196/jmir.9465. https://www.jmir.org/2018/4/e152/ v20i4e152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.van Egmond M, van der Schaaf M, Vredeveld T, Vollenbroek-Hutten M, van Berge Henegouwen M, Klinkenbijl J, Engelbert R. Effectiveness of physiotherapy with telerehabilitation in surgical patients: a systematic review and meta-analysis. Physiotherapy. 2018 Sep;104(3):277–98. doi: 10.1016/j.physio.2018.04.004.S0031-9406(18)30075-0 [DOI] [PubMed] [Google Scholar]
- 100.Muellmann S, Forberger S, Möllers T, Bröring E, Zeeb H, Pischke CR. Effectiveness of eHealth interventions for the promotion of physical activity in older adults: a systematic review. Prev Med. 2018 Mar;108:93–110. doi: 10.1016/j.ypmed.2017.12.026.S0091-7435(17)30514-5 [DOI] [PubMed] [Google Scholar]
- 101.Geraedts H, Zijlstra A, Bulstra S, Stevens M, Zijlstra W. Effects of remote feedback in home-based physical activity interventions for older adults: a systematic review. Patient Educ Couns. 2013 Apr;91(1):14–24. doi: 10.1016/j.pec.2012.10.018.S0738-3991(12)00425-9 [DOI] [PubMed] [Google Scholar]
- 102.Zhong R, Rau PP. Are cost-effective technologies feasible to measure gait in older adults? A systematic review of evidence-based literature. Arch Gerontol Geriatr. 2020 Mar;87:103970. doi: 10.1016/j.archger.2019.103970.S0167-4943(19)30213-4 [DOI] [PubMed] [Google Scholar]
- 103.Núñez de Arenas-Arroyo S, Cavero-Redondo I, Alvarez-Bueno C, Sequí-Domínguez I, Reina-Gutiérrez S, Martínez-Vizcaíno V. Effect of eHealth to increase physical activity in healthy adults over 55 years: a systematic review and meta-analysis. Scand J Med Sci Sports. 2021 Apr;31(4):776–89. doi: 10.1111/sms.13903. doi: 10.1111/sms.13903. [DOI] [PubMed] [Google Scholar]
- 104.Velayati F, Ayatollahi H, Hemmat M. A systematic review of the effectiveness of telerehabilitation interventions for therapeutic purposes in the elderly. Methods Inf Med. 2020 May 06;59(2-03):104–9. doi: 10.1055/s-0040-1713398. [DOI] [PubMed] [Google Scholar]
- 105.Narasimha S, Madathil KC, Agnisarman S, Rogers H, Welch B, Ashok A, Nair A, McElligott J. Designing telemedicine systems for geriatric patients: a review of the usability studies. Telemed J E Health. 2017 Jun;23(6):459–72. doi: 10.1089/tmj.2016.0178. [DOI] [PubMed] [Google Scholar]
- 106.Helleman J, Kruitwagen ET, van den Berg LH, Visser-Meily JM, Beelen A. The current use of telehealth in ALS care and the barriers to and facilitators of implementation: a systematic review. Amyotroph Lateral Scler Frontotemporal Degener. 2020 May;21(3-4):167–82. doi: 10.1080/21678421.2019.1706581. [DOI] [PubMed] [Google Scholar]
- 107.Cruz J, Brooks D, Marques A. Home telemonitoring in COPD: a systematic review of methodologies and patients' adherence. Int J Med Inform. 2014 Apr;83(4):249–63. doi: 10.1016/j.ijmedinf.2014.01.008. https://www.clinicalkey.es/playcontent/1-s2.0-S1386505614000215 .S1386-5056(14)00021-5 [DOI] [PubMed] [Google Scholar]
- 108.Li W, Liu S, Liu S, Li J, Wang W, Li K. Perceptions of patients with chronic obstructive pulmonary disease towards telemedicine: a qualitative systematic review. Heart Lung. 2021;50(5):675–84. doi: 10.1016/j.hrtlng.2021.03.081.S0147-9563(21)00190-4 [DOI] [PubMed] [Google Scholar]
- 109.Ciere Y, Cartwright M, Newman SP. A systematic review of the mediating role of knowledge, self-efficacy and self-care behaviour in telehealth patients with heart failure. J Telemed Telecare. 2012 Oct 27;18(7):384–91. doi: 10.1258/jtt.2012.111009.jtt.2012.111009 [DOI] [PubMed] [Google Scholar]
- 110.Nick J, Roberts L, Petersen A. Effectiveness of telemonitoring on self-care behaviors among community-dwelling adults with heart failure: a quantitative systematic review. JBI Evid Synth. 2021 Apr 26;19(10):2659–94. doi: 10.11124/JBIES-20-00329. https://europepmc.org/abstract/MED/33896907 .02174543-900000000-99685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gorst SL, Armitage CJ, Brownsell S, Hawley MS. Home telehealth uptake and continued use among heart failure and chronic obstructive pulmonary disease patients: a systematic review. Ann Behav Med. 2014 Dec 25;48(3):323–36. doi: 10.1007/s12160-014-9607-x. https://europepmc.org/abstract/MED/24763972 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Brunton L, Bower P, Sanders C. The contradictions of telehealth user experience in chronic obstructive pulmonary disease (COPD): a qualitative meta-synthesis. PLoS One. 2015;10(10):e0139561. doi: 10.1371/journal.pone.0139561. https://dx.plos.org/10.1371/journal.pone.0139561 .PONE-D-15-10853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Walker RC, Tong A, Howard K, Palmer SC. Patient expectations and experiences of remote monitoring for chronic diseases: systematic review and thematic synthesis of qualitative studies. Int J Med Inform. 2019 Apr;124:78–85. doi: 10.1016/j.ijmedinf.2019.01.013. https://linkinghub.elsevier.com/retrieve/pii/S1386-5056(18)30982-1 .S1386-5056(18)30982-1 [DOI] [PubMed] [Google Scholar]
- 114.Albergoni A, Hettinga F, La Torre A, Bonato M, Sartor F. The role of technology in adherence to physical activity programs in patients with chronic diseases experiencing fatigue: a systematic review. Sports Med Open. 2019 Sep 12;5(1):41. doi: 10.1186/s40798-019-0214-z. https://europepmc.org/abstract/MED/31512075 .10.1186/s40798-019-0214-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Vedel I, Akhlaghpour S, Vaghefi I, Bergman H, Lapointe L. Health information technologies in geriatrics and gerontology: a mixed systematic review. J Am Med Inform Assoc. 2013;20(6):1109–19. doi: 10.1136/amiajnl-2013-001705. https://europepmc.org/abstract/MED/23666776 .amiajnl-2013-001705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Song Y, van der Cammen TJ. Electronic assistive technology for community-dwelling solo-living older adults: a systematic review. Maturitas. 2019 Jul;125:50–6. doi: 10.1016/j.maturitas.2019.04.211.S0378-5122(19)30129-X [DOI] [PubMed] [Google Scholar]
- 117.Davies A, Rixon L, Newman S. Systematic review of the effects of telecare provided for a person with social care needs on outcomes for their informal carers. Health Soc Care Community. 2013 Nov 17;21(6):582–97. doi: 10.1111/hsc.12035. [DOI] [PubMed] [Google Scholar]
- 118.Sriram V, Jenkinson C, Peters M. Informal carers' experience of assistive technology use in dementia care at home: a systematic review. BMC Geriatr. 2019 Jun 14;19(1):160. doi: 10.1186/s12877-019-1169-0. https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-019-1169-0 .10.1186/s12877-019-1169-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yusif S, Soar J, Hafeez-Baig A. Older people, assistive technologies, and the barriers to adoption: a systematic review. Int J Med Inform. 2016 Oct;94:112–6. doi: 10.1016/j.ijmedinf.2016.07.004.S1386-5056(16)30155-1 [DOI] [PubMed] [Google Scholar]
- 120.Peek ST, Wouters EJ, van Hoof J, Luijkx KG, Boeije HR, Vrijhoef HJ. Factors influencing acceptance of technology for aging in place: a systematic review. Int J Med Inform. 2014 Apr;83(4):235–48. doi: 10.1016/j.ijmedinf.2014.01.004. https://linkinghub.elsevier.com/retrieve/pii/S1386-5056(14)00017-3 .S1386-5056(14)00017-3 [DOI] [PubMed] [Google Scholar]
- 121.Karlsen C, Ludvigsen MS, Moe CE, Haraldstad K, Thygesen E. Experiences of community-dwelling older adults with the use of telecare in home care services: a qualitative systematic review. JBI Database System Rev Implement Rep. 2017 Dec;15(12):2913–80. doi: 10.11124/JBISRIR-2017-003345.01938924-201712000-00012 [DOI] [PubMed] [Google Scholar]
- 122.Merkel S, Kucharski A. Participatory design in gerontechnology: a systematic literature review. Gerontologist. 2019 Jan 09;59(1):e16–25. doi: 10.1093/geront/gny034.4999719 [DOI] [PubMed] [Google Scholar]
- 123.Kruse C, Fohn J, Wilson N, Nunez Patlan E, Zipp S, Mileski M. Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: systematic review. JMIR Med Inform. 2020 Aug 12;8(8):e20359. doi: 10.2196/20359. https://medinform.jmir.org/2020/8/e20359/ v8i8e20359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.van Boekel LC, Wouters EJ, Grimberg BM, van der Meer NJ, Luijkx KG. Perspectives of stakeholders on technology use in the care of community-living older adults with dementia: a systematic literature review. Healthcare (Basel) 2019 May 28;7(2):73. doi: 10.3390/healthcare7020073. https://www.mdpi.com/resolver?pii=healthcare7020073 .healthcare7020073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Holthe T, Halvorsrud L, Karterud D, Hoel K, Lund A. Usability and acceptability of technology for community-dwelling older adults with mild cognitive impairment and dementia: a systematic literature review. Clin Interv Aging. 2018;13:863–86. doi: 10.2147/CIA.S154717. doi: 10.2147/CIA.S154717.cia-13-863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ollevier A, Aguiar G, Palomino M, Simpelaere IS. How can technology support ageing in place in healthy older adults? A systematic review. Public Health Rev. 2020 Nov 23;41(1):26. doi: 10.1186/s40985-020-00143-4. https://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-020-00143-4 .10.1186/s40985-020-00143-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Klersy C, De Silvestri A, Gabutti G, Raisaro A, Curti M, Regoli F, Auricchio A. Economic impact of remote patient monitoring: an integrated economic model derived from a meta-analysis of randomized controlled trials in heart failure. Eur J Heart Fail. 2011 Apr;13(4):450–9. doi: 10.1093/eurjhf/hfq232. doi: 10.1093/eurjhf/hfq232.hfq232 [DOI] [PubMed] [Google Scholar]
- 128.Sanyal C, Stolee P, Juzwishin D, Husereau D. Economic evaluations of eHealth technologies: a systematic review. PLoS One. 2018;13(6):e0198112. doi: 10.1371/journal.pone.0198112. https://dx.plos.org/10.1371/journal.pone.0198112 .PONE-D-17-32371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Peretz D, Arnaert A, Ponzoni NN. Determining the cost of implementing and operating a remote patient monitoring programme for the elderly with chronic conditions: a systematic review of economic evaluations. J Telemed Telecare. 2018 Jan;24(1):13–21. doi: 10.1177/1357633X16669239.1357633X16669239 [DOI] [PubMed] [Google Scholar]
- 130.Gochoo M, Alnajjar F, Tan T, Khalid S. Towards privacy-preserved aging in place: a systematic review. Sensors (Basel) 2021 Apr 28;21(9):A. doi: 10.3390/s21093082. https://www.mdpi.com/resolver?pii=s21093082 .s21093082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Baraković S, Baraković Husić J, van Hoof J, Krejcar O, Maresova P, Akhtar Z, Melero F. Quality of life framework for personalised ageing: a systematic review of ICT solutions. Int J Environ Res Public Health. 2020 Apr 24;17(8):2940. doi: 10.3390/ijerph17082940. https://www.mdpi.com/resolver?pii=ijerph17082940 .ijerph17082940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Choi HK, Lee SH. Trends and effectiveness of ICT interventions for the elderly to reduce loneliness: a systematic review. Healthcare (Basel) 2021 Mar 07;9(3):293. doi: 10.3390/healthcare9030293. https://www.mdpi.com/resolver?pii=healthcare9030293 .healthcare9030293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Panico F, Cordasco G, Vogel C, Trojano L, Esposito A. Ethical issues in assistive ambient living technologies for ageing well. Multimed Tools Appl. 2020 Jul 17;79(47-48):36077–89. doi: 10.1007/s11042-020-09313-7. [DOI] [Google Scholar]
- 134.Biermann H, Himmel S, Offermann-van Heek J, Ziefle M. Human Aspects of IT for the Aged Population. Cham: Springer; 2018. User-specific concepts of aging – a qualitative approach on AAL-acceptance regarding ultrasonic whistles. [Google Scholar]
- 135.Moraitou M, Pateli A, Fotiou S. Smart health caring home: a systematic review of smart home care for elders and chronic disease patients. Adv Exp Med Biol. 2017;989:255–64. doi: 10.1007/978-3-319-57348-9_22. [DOI] [PubMed] [Google Scholar]
- 136.O’Brolcháin F, Gordijn B. Privacy challenges in smart homes for people with dementia and people with intellectual disabilities. Ethics Inf Technol. 2019 Jul 12;21(3):253–65. doi: 10.1007/s10676-019-09507-0. [DOI] [Google Scholar]
- 137.Seymour W, Binns R, Slovak P, Van KM, Shadbolt N. Strangers in the room: unpacking perceptions of 'smartness' and related ethical concerns in the home. Proceedings of the 2020 ACM Designing Interactive Systems Conference; DIS '20: Designing Interactive Systems Conference 2020; Jul 6 - 10, 2020; Eindhoven Netherlands. 2020. [DOI] [Google Scholar]
- 138.Wang S, Bolling K, Mao W, Reichstadt J, Jeste D, Kim H, Nebeker C. Technology to support aging in place: older adults' perspectives. Healthcare (Basel) 2019 Apr 10;7(2):60. doi: 10.3390/healthcare7020060. https://www.mdpi.com/resolver?pii=healthcare7020060 .healthcare7020060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schomakers E, Ziefle M. Human Aspects of IT for the Aged Population. Cham: Springer; 2019. Privacy concerns and the acceptance of technologies for aging in place. [Google Scholar]
- 140.Sánchez VG, Anker-Hansen C, Taylor I, Eilertsen G. Older people's attitudes and perspectives of welfare technology in Norway. J Multidiscip Healthc. 2019;12:841–53. doi: 10.2147/JMDH.S219458. doi: 10.2147/JMDH.S219458.219458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Cesta A, Cortellessa G, Fracasso F, Orlandini A, Turno M. User needs and preferences on AAL systems that support older adults and their carers. J Ambient Intell Smart Environ. 2018 Jan 17;10(1):49–70. doi: 10.3233/ais-170471. [DOI] [Google Scholar]
- 142.Pal D, Funilkul S, Charoenkitkarn N, Kanthamanon P. Internet-of-things and smart homes for elderly healthcare: an end user perspective. IEEE Access. 2018;6:10483–96. doi: 10.1109/access.2018.2808472. [DOI] [Google Scholar]
- 143.Birchley G, Huxtable R, Murtagh M, Ter Meulen R, Flach P, Gooberman-Hill R. Smart homes, private homes? An empirical study of technology researchers' perceptions of ethical issues in developing smart-home health technologies. BMC Med Ethics. 2017 Apr 04;18(1):23. doi: 10.1186/s12910-017-0183-z. https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-017-0183-z .10.1186/s12910-017-0183-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Arthanat S, Chang H, Wilcox J. Determinants of information communication and smart home automation technology adoption for aging-in-place. J Enabling Technol. 2020 Jul 21;14(2):73–86. doi: 10.1108/jet-11-2019-0050. https://europepmc.org/abstract/MED/36196218 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Skär L, Söderberg S. The importance of ethical aspects when implementing eHealth services in healthcare: a discussion paper. J Adv Nurs. 2018 May 29;74(5):1043–50. doi: 10.1111/jan.13493. [DOI] [PubMed] [Google Scholar]
- 146.Ferati M, Babar A, Carine K, Hamidi A, Mortberg C. Universal Access in Human-Computer Interaction. Cham: Springer; 2018. Participatory design approach to internet of things: co-designing a smart shower for and with people with disabilities. [Google Scholar]
- 147.Borelli E, Paolini G, Antoniazzi F, Barbiroli M, Benassi F, Chesani F, Chiari L, Fantini M, Fuschini F, Galassi A, Giacobone G, Imbesi S, Licciardello M, Loreti D, Marchi M, Masotti D, Mello P, Mellone S, Mincolelli G, Raffaelli C, Roffia L, Salmon Cinotti T, Tacconi C, Tamburini P, Zoli M, Costanzo A. HABITAT: an IoT solution for independent elderly. Sensors (Basel) 2019 Mar 12;19(5):1258. doi: 10.3390/s19051258. https://www.mdpi.com/resolver?pii=s19051258 .s19051258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Grossi G, Lanzarotti R, Napoletano P, Noceti N, Odone F. Positive technology for elderly well-being: a review. Pattern Recognition Letters. 2020 Sep;137:61–70. doi: 10.1016/j.patrec.2019.03.016. [DOI] [Google Scholar]
- 149.Etemad-Sajadi R, Gomes Dos Santos G. Senior citizens’ acceptance of connected health technologies in their homes. IJHCQA. 2019 Oct 14;32(8):1162–74. doi: 10.1108/ijhcqa-10-2018-0240. [DOI] [PubMed] [Google Scholar]
- 150.Taylor HA, Sullivan D, Mullen C, Johnson CM. Implementation of a user-centered framework in the development of a web-based health information database and call center. J Biomed Inform. 2011 Oct;44(5):897–908. doi: 10.1016/j.jbi.2011.03.001. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(11)00041-4 .S1532-0464(11)00041-4 [DOI] [PubMed] [Google Scholar]
- 151.Bernhard G, Mahler C, Seidling HM, Stützle M, Ose D, Baudendistel I, Wensing M, Szecsenyi J. Developing a shared patient-centered, web-based medication platform for type 2 diabetes patients and their health care providers: qualitative study on user requirements. J Med Internet Res. 2018 Mar 27;20(3):e105. doi: 10.2196/jmir.8666. https://www.jmir.org/2018/3/e105/ v20i3e105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Calvillo-Arbizu J, Roa-Romero LM, Estudillo-Valderrama MA, Salgueira-Lazo M, Aresté-Fosalba N, Del-Castillo-Rodríguez NL, González-Cabrera F, Marrero-Robayna S, López-de-la-Manzana V, Román-Martínez I. User-centred design for developing e-Health system for renal patients at home (AppNephro) Int J Med Inform. 2019 May;125:47–54. doi: 10.1016/j.ijmedinf.2019.02.007.S1386-5056(19)30200-X [DOI] [PubMed] [Google Scholar]
- 153.Vaisson G, Provencher T, Dugas M, Trottier M, Chipenda Dansokho S, Colquhoun H, Fagerlin A, Giguere AM, Hakim H, Haslett L, Hoffman AS, Ivers NM, Julien A, Légaré F, Renaud J, Stacey D, Volk RJ, Witteman HO. User involvement in the design and development of patient decision aids and other personal health tools: a systematic review. Med Decis Making. 2021 Mar 03;41(3):261–74. doi: 10.1177/0272989x20984134. [DOI] [PubMed] [Google Scholar]
- 154.Witteman HO, Vaisson G, Provencher T, Chipenda Dansokho S, Colquhoun H, Dugas M, Fagerlin A, Giguere AM, Haslett L, Hoffman A, Ivers NM, Légaré F, Trottier M, Stacey D, Volk RJ, Renaud J. An 11-item measure of user- and human-centered design for personal health tools (UCD-11): development and validation. J Med Internet Res. 2021 Mar 16;23(3):e15032. doi: 10.2196/15032. https://www.jmir.org/2021/3/e15032/ v23i3e15032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Jokstad K, Skovdahl K, Landmark BT, Haukelien H. Ideal and reality; Community healthcare professionals' experiences of user-involvement in reablement. Health Soc Care Community. 2019 Jul 26;27(4):907–16. doi: 10.1111/hsc.12708. [DOI] [PubMed] [Google Scholar]
- 156.Millar J. The Oxford Handbook of Ethics of AI. Oxford, United Kingdom: Oxford Academic; 2020. Social failure modes in technology and the ethics of AI: an engineering perspective. [Google Scholar]
- 157.Willard S, Cremers G, Man YP, van Rossum E, Spreeuwenberg M, de Witte L. Development and testing of an online community care platform for frail older adults in the Netherlands: a user-centred design. BMC Geriatr. 2018 Apr 07;18(1):87. doi: 10.1186/s12877-018-0774-7. https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-018-0774-7 .10.1186/s12877-018-0774-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hou I, Lan M, Shen S, Tsai P, Chang K, Tai H, Tsai A, Chang P, Wang T-F, Sheu S-J, Dykes PC. The development of a mobile health app for breast cancer self-management support in Taiwan: design thinking approach. JMIR Mhealth Uhealth. 2020 Apr 30;8(4):e15780. doi: 10.2196/15780. https://mhealth.jmir.org/2020/4/e15780/ v8i4e15780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Farao J, Malila B, Conrad N, Mutsvangwa T, Rangaka MX, Douglas TS. A user-centred design framework for mHealth. PLoS One. 2020 Aug 19;15(8):e0237910. doi: 10.1371/journal.pone.0237910. https://dx.plos.org/10.1371/journal.pone.0237910 .PONE-D-20-01209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Francés-Morcillo L, Morer-Camo P, Rodríguez-Ferradas M, Cazón-Martín A. The role of user-centred design in smart wearable systems design process. Proceedings of the DESIGN 2018 15th International Design Conference; DS 92: Proceedings of the DESIGN 2018 15th International Design Conference; May 21-24, 2018; Dubrovnik, Croatia. 2018. [DOI] [Google Scholar]
- 161.Nauta J, Gyaltsen-Lohuis E, Hettinga M, Wink G, Braad A, van AG, de VK. Development of eHealth applications applying the eHix framework. Proceedings of the eTELEMED 2015 : The Seventh International Conference on eHealth, Telemedicine, and Social Medicine; eTELEMED 2015 : The Seventh International Conference on eHealth, Telemedicine, and Social Medicine; Fe, 2015; Lisbon, Portugal. 2015. [Google Scholar]
- 162.Gyaltsen-Lohuis E, Hettinga M, Janssen R, Nauta J, Visser S. Early stages of business modeling for open source home care technology lessons learned from an initial inventory. Int J Advances Life Sci. 2014;6(3 & 4) [Google Scholar]
- 163.Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010 Nov;79(11):736–71. doi: 10.1016/j.ijmedinf.2010.08.006.S1386-5056(10)00150-4 [DOI] [PubMed] [Google Scholar]
- 164.Flumignan C, Rocha AP, Pinto AC, Milby KM, Batista MR, Atallah AN, Saconato H. What do Cochrane systematic reviews say about telemedicine for healthcare? Sao Paulo Med J. 2019 Jul 15;137(2):184–92. doi: 10.1590/1516-3180.0177240419. https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-31802019000200184&lng=en&nrm=iso&tlng=en .S1516-31802019000200184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Honarvar B, Salehi F, Shaygani F, Hajebrahimi M, Homayounfar R, Dehghan S, Barahmand N, Bagheri Lankarani K. Opportunities and threats of electronic health in management of diabetes mellitus: an umbrella review of systematic review and meta-analysis studies. Shiraz E-Med J. 2018 Nov 11;In Press(In Press):e81794. doi: 10.5812/semj.81794. [DOI] [Google Scholar]
- 166.Eberle C, Stichling S. Effect of telemetric interventions on glycated hemoglobin A1c and management of type 2 diabetes mellitus: systematic meta-review. J Med Internet Res. 2021 Feb 17;23(2):e23252. doi: 10.2196/23252. https://www.jmir.org/2021/2/e23252/ v23i2e23252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Suso-Martí L, La Touche R, Herranz-Gómez A, Angulo-Díaz-Parreño S, Paris-Alemany A, Cuenca-Martínez F. Effectiveness of telerehabilitation in physical therapist practice: an umbrella and mapping review with meta-meta-analysis. Phys Ther. 2021 May 04;101(5):pzab075. doi: 10.1093/ptj/pzab075. https://europepmc.org/abstract/MED/33611598 .6145901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Definition of TRADE-OFF. Merriam Webster. [2021-07-13]. https://www.merriam-webster.com/dictionary/trade-off .
- 169.Cornet V, Toscos T, Bolchini D, Rohani Ghahari R, Ahmed R, Daley C, Mirro M, Holden R. Untold stories in user-centered design of mobile health: practical challenges and strategies learned from the design and evaluation of an app for older adults with heart failure. JMIR Mhealth Uhealth. 2020 Jul 21;8(7):e17703. doi: 10.2196/17703. https://mhealth.jmir.org/2020/7/e17703/ v8i7e17703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Chaudhuri S, Thompson H, Demiris G. Fall detection devices and their use with older adults: a systematic review. J Geriatr Phys Ther. 2014;37(4):178–96. doi: 10.1519/JPT.0b013e3182abe779. https://europepmc.org/abstract/MED/24406708 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist for evidence for remote monitoring.
Search strategy on evidence for remote monitoring.
Quality assessments for evidence on remote monitoring.
Extraction tables for evidence on remote monitoring.
Summary of evidence for remote monitoring.
Data Availability Statement
We have included the search strings in Multimedia Appendix 2, quality assessments in Multimedia Appendix 3, the extracted articles in Multimedia Appendix 4, and more detailed summaries of the articles extracted in Multimedia Appendix 5 to provide transparency on extractions.


