Abstract
BACKGROUND
To compare prevalence of hypertension and stage II hypertension assessed by 2 blood pressure (BP) observation protocols.
METHODS
Participants aged 18 years and older (n = 4,689) in the National Health and Nutrition Examination Survey (NHANES 2017–2018) had their BP measured following 2 protocols: the legacy auscultation protocol (AP) and oscillometric protocol (OP). The order of protocols was randomly assigned. Prevalence estimates for hypertension (BP ≥130/80 mm Hg or use of medication for hypertension) and stage II hypertension (BP ≥140/90 mm Hg) were determined overall, by demographics, and by risk factors for each protocol. Ratios (OP% ÷ AP%) and kappa statistics were calculated.
RESULTS
Age-adjusted hypertension prevalence was 44.5% (95% confidence interval [CI]: 41.1%–48.0%) using OP and 45.1% (95% CI: 41.5%–48.7%) using AP, prevalence ratio = 0.99 (95% CI = 0.94–1.04). Age-adjusted stage II hypertension prevalence was 15.8% (95% CI: 13.6%–18.2%) using AP and 17.1% (95% CI: 14.7%–19.7%) using OP, prevalence ratio = 0.92 (95% CI = 0.81–1.04). For both hypertension and stage II hypertension, the prevalence ratios by demographics and by risk factors all included unity in their 95% CI, except for stage II hypertension in adults 60+ years (ratio: 0.88 [95% CI: 0.78–0.98]). Kappa for agreement between protocols for hypertension and stage II hypertension was 0.75 (95% CI = 0.71–0.79) and 0.67 (95% CI = 0.61–0.72), respectively.
CONCLUSIONS
In adults and for nearly all subcategories there were no significant differences in prevalence of hypertension and stage II hypertension between protocols, indicating that protocol change may not affect the national prevalence estimates of hypertension and stage II hypertension.
Keywords: auscultation protocol, blood pressure, comparison, hypertension, hypertension stage II, NHANES, oscillometric protocol
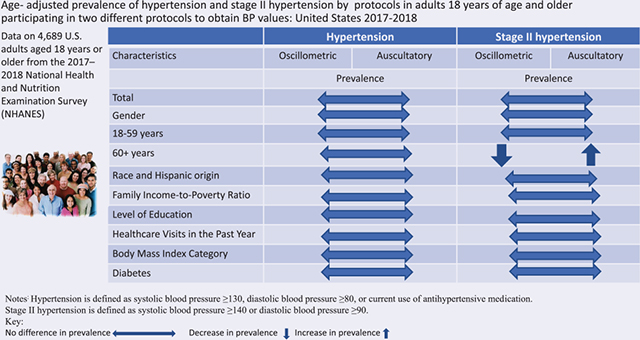
Graphical Abstract
Brachial upper-arm blood pressure (BP) measurements have traditionally been obtained in National Health and Nutrition Examination Survey (NHANES) following an auscultatory protocol (AP) using a stethoscope and wall-mounted mercury gravity sphygmomanometer.1 Mercury-contaminated devices have a risk of spills, and these devices have been phased out of clinical use.2 Alternative BP devices based on automatic oscillometric protocols (OPs) are increasingly used in clinical trials and epidemiological studies.3,4 During the 2017–2018 NHANES survey cycle, BP was obtained using both AP and OP for participants aged 8 years and older, however only adults aged 18 years and older results are presented in this report, with the protocol order randomly assigned. Previous analyses compared mean BP values obtained by these 2 protocols, a more recent analysis assessed the variation by protocol in prevalence ratios for stage I high BP (≥130/80 mm Hg), and although the mean systolic BP and diastolic BP obtained by AP and OP differed, the prevalence of stage 1 high BP did not differ.5–7 The current report compares hypertension categories (hypertension and stage II hypertension) using the 2017 American College of Cardiology/American Heart Association (ACC/AHA) hypertension guidelines to define high BP.8,9 The study had 2 overall objectives: (i) to compare the prevalence of hypertension and stage II hypertension assessed with the AP and OP protocols and (ii) to compare individual-level agreement between protocols for hypertension and stage II hypertension.
METHODS
Study population
NHANES is a cross-sectional national health and nutrition survey of the civilian, noninstitutionalized US population, conducted by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention. The survey operates continuously, and data are typically released in 2-year cycles. Descriptions of the sample design and data collection methods for NHANES are available on the survey website.10 Survey participants were interviewed in their homes and then examined in the NHANES mobile examination center (MEC). This methodology study was conducted as part of the NHANES MEC data collection in 2017–2018. The NCHS Research Ethics Review Board approved all survey protocols and consent was obtained from all MEC examined participants in this study.
Sample selection and item-level response rate
During the NHANES 2017–2018 cycle, 11,027 eligible participants aged 18 years and older from screened households were identified, of which 5,856 were interviewed, and 5,533 were examined in the MEC (50.2% MEC response rate out of the 11,027 eligible participants). Each participant was randomly assigned to a BP protocol order, and all BP measurements were obtained during a single MEC examination visit. The BP protocols were not done consecutively; instead, they were separated by other examination components conducted in the MEC. Of the 5,533 participants eligible to participate in the study, 166 were missing BP data obtained with both protocols, 561 had only AP values, and 117 had only OP values. These exclusions (n = 844) resulted in a final analytic sample of 4,689, reflecting 84.7% of the 5,533 eligible participants. The final analytic sample presented in this paper varies from the previous methodology study reported sample (n = 4,477), which restricted the sample to individuals with 3 BP determinations for both protocols.7 In contrast, in this study any individual with 1+ BP determination was included.
Equipment
Each protocol used a device and its corresponding cuffs to take BP measurements. The Omron HEM-907XL is a digital upper-arm electronic BP measurement device designed for clinical settings.6 The Omron device is validated by both the Association for the Advancement of Medical Instrumentation (AAMI) and the International Protocol of the European Society of Hypertension for taking BP measurements in populations aged 13 years and older.5,11,12 In addition, the device can accommodate various cuff sizes, including a child, adult, large adult, and extra-large adult.6 The clinical wall-mounted mercury gravity sphygmomanometer (Baumanometer) was used as the reference comparison device to the Omron HEM-907XL. Like the Omron device, the mercury device accommodated various cuff sizes, including a child, adult, large adult, and extra-large adult.13
Protocols
Participants were seated in a chair with back support for both protocols, with both feet resting comfortably on the floor and both forearms supported on a level surface at heart level. The appropriately sized BP cuff was selected based on the participant’s measured mid-arm circumference.13,14 Participants were asked to rest quietly in a seated position for 5 minutes before taking BP measurements. The AP was conducted exclusively by the physicians. The physician determined the maximum inflation level before taking the BP measurements, and then the physician obtained 3 consecutive BP measurements, waiting 30 seconds between the measurements.13 The OP was conducted exclusively by health technicians. After 5 minutes of rest, the device automatically obtained 3 consecutive BP measurements 60 seconds apart.14 The change from 30 seconds (AP) to 60 seconds (OP) aligned the OP with national and international standards of obtaining BP.15
The average of up to 3 brachial systolic and diastolic BP values was used in both protocols. However, if a participant only had one reading, the single reading was used (n = 29 for AP and n = 8 for OP).
Outcome variables
Hypertension was defined as a participant having at least one of the following: systolic BP of 130 mm Hg or greater, diastolic BP of 80 mm Hg or greater, or participant-reported current medication use for high BP.8,9 Stage II hypertension was defined as systolic BP of 140 mm Hg or greater or diastolic BP of 90 mm Hg or greater.8
Independent variables
Covariates included in both analyses were gender, age group (years), race and Hispanic origin, family income-to-poverty ratio, level of education, healthcare visits in the past year, body mass index category, and diabetes. Each covariate included is associated with hypertension. Moreover, many official publications include these stratifications so understanding the impact of the change in methods may inform future work.9,16–18
Demographics
Age was categorized as 18–39, 40–59, and 60 years and over. Self-reported data on race and Hispanic origin were classified as non-Hispanic (NH) White, NH Black, NH Asian, Hispanic, and other/multi-racial. Individuals reporting “other/multi-racial” were included in the overall analyses but not reported separately due to small numbers in this group.
Income
Family income-to-poverty ratio is the ratio of a family’s income to its appropriate poverty guidelines established by the US Department of Health and Human Services.19 Three categories of approximately equal number of participants in each category were used for these analyses: <1.30, 1.30 to <3.50, and 3.50+. Larger family income-to-poverty ratios indicate higher income, adjusted for the size of a family.
Education level
Education level was self-reported based on response to the question, “What is the highest grade or level of school you have completed or the highest degree you have received?”20 Response categories included: high school or less, more than high school or some college, and college graduate.
Healthcare utilization and health outcomes
The frequency of visits to a healthcare provider was self-reported based on the answer to the home interview question: “During the past 12 months, how many times have you seen a doctor or other health care professional about your health at a doctor’s office, a clinic, a hospital emergency room, at home, or some other place?”20 The frequency of visits was categorized as 0–1, 2–3, and 4 or more.
During the physical examination in the MEC, standardized measurements of weight and height were obtained.21 Body mass index was calculated as weight divided by height in meters squared (kg/m2) and was categorized using criteria established by the National Institutes of Health22 as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obesity (≥30.0 kg/m2). Underweight was included in the overall analysis but was not reported separately due to small numbers.
Diabetes was defined by participant self-report of ever having been told by a doctor or healthcare provider that he/she has diabetes or a glycated hemoglobin ≥6.5%.23
Analytic sample and statistical analysis
There was a difference between those included (n = 4,689) and excluded (n = 844) by race and Hispanic origin. Excluded participants tended to more likely to be Hispanic (20.4%, 95% confidence interval [CI]: 15.5–26.1) and less likely to be NH White (9.9%, 95% CI: 6.8–13.8) (P <0.001). Excluded participants also tended to be younger (18–39) and have a family income-to-poverty ratio less than 1.3 although these differences were near different (P = 0.05). See Supplementary Table S1 online for more details.
All statistical analyses were performed using survey procedures in SAS 9.4 for Windows (SAS Institute, Cary, NC) and SAS callable SUDAAN 11.0 software (Research Triangle Institute, Research Triangle Park, NC). All estimates were weighted using the MEC sample weights and incorporated sampling design information; the sample weights accounted for the unequal probabilities of selection resulting from the complex sample design, survey nonresponse, and the planned oversampling of selected population subgroups. Reweighting due to item nonresponse did not change any conclusions so the original MEC sample weights were used for all analyses. The calculated variance estimates accounted for the complex survey design by using Taylor series linearization.
A Satterthwaite-adjusted Wald chi-square test24 was used to examine the statistical difference in covariates. Prevalence estimates of hypertension and stage II hypertension were calculated overall and by selected covariates. The 95% CIs of prevalence estimates were calculated using the Korn and Graubard method.25 Effective sample size, absolute and relative 95% CI width, and degrees of freedom were evaluated to determine the reliability of prevalence estimates according to the NCHS Data Presentation Standards for Proportions.26 Prevalence estimates of hypertension and stage II hypertension were age adjusted by the direct method to the 2000 US census population, using age groups 18–39, 40–59, and 60 years and older.27
A weighted and age-adjusted ratio was computed with AP as the reference for each of the above prevalence estimates (hypertension and stage II hypertension). Established as the legacy protocol, the AP has historically been considered the gold standard and it is the gold standard for the sensitivity analyses. Ratios with a 95% CI not including one were considered statistically significant. The weighted individual-level agreement was determined using sensitivity and specificity. Sensitivity, or the “True Positive rate,” is the percent of predicted positive hypertensives and stage II hypertensives among actual positives. Specificity, or the “True Negative rate,” is the predicted percent negative among hypertensives and stage II hypertensives who are negative. Kappa statistics were also calculated to evaluate individual-level agreement; a kappa statistic between 60% and 80% was considered a good agreement.28
RESULTS
Randomization
Of the final analytic weighted sample, 49.1% had BP measurements obtained using the OP protocol first and 50.9% had BP measurements obtained using the AP protocol first (data not tabulated). The weighted distributions of gender, age (18–39, 40–59, 60+ years), self-reported race and Hispanic origin, family income-to-poverty ratio, level of education, healthcare visits, and diabetes were not associated with randomization order (data not tabulated). However, body mass index was associated with the randomization order (Supplementary Table S2 online), more persons in the underweight/normal weight were in OP first group and more persons with overweight categories and obesity were in AP first group (P < 0.01).
Sample characteristics
The mean age (±SE) was 47.6 (±0.66) years, and 51.1% (95% CI: 48.8–53.5) were female (Supplementary Table S3 online). For age categories, 37.1% (95% CI: 33.8–40.4), 34.1% (95% CI: 31.1–37.3), and 28.8% (95% CI: 24.9–33.0) were aged 18–39, 40–59, and 60 years and over, respectively. As for race and Hispanic origin, 63.9% (95% CI: 58.0–69.5), 11.0% (95% CI: 7.7–15.2), 5.5% (95% CI: 3.8–7.6), and 14.7% (95% CI: 10.9–19.2) were NH White, NH Black, NH Asian, and Hispanic. Also, 20.1% (95% CI: 18.4–21.9) had a family income-to-poverty ratio <1.3; 39.0 % (95% CI: 35.4–42.7) had less than a college education, 33% (95% CI: 30.4–35.8) had 0 to 1 healthcare visits in the past year, 43.1% (95% CI: 39.1–47.3) had obesity, and 13.6% (95% CI: 12.3–15.1) had diabetes.
Between-protocol agreement for hypertension and stage II hypertension
Table 1 shows the age-adjusted prevalence of hypertension for both protocols and the prevalence ratios (OP% ÷ AP%). Overall, the age-adjusted hypertension prevalence was 44.5% (95% CI: 41.1%–48.0%) using OP, 45.1% (95% CI: 41.5%–48.7%) using AP, and the prevalence ratio was 0.99 (95% CI: 0.94–1.04). Table 2 shows the age-adjusted prevalence of stage II hypertension for both protocols and the prevalence ratios (OP% ÷ AP%). Overall, the age-adjusted stage II hypertension prevalence was 15.8% (95% CI: 13.6%–18.2%) using OP, 17.1% (95% CI: 14.7%–19.7%) using AP, and the prevalence ratio was 0.92 (95% CI: 0.81–1.04). The prevalence ratios for overall hypertension and stage II hypertension were not different from 1 as the 95% CIs included unity.
Table 1.
Weighted and age-adjusted prevalence of hypertension by protocol and ratio (oscillometric protocol over auscultatory protocol) among adults 18 years of age and older participating in 2 different protocols to obtain BP values: United States 2017–2018
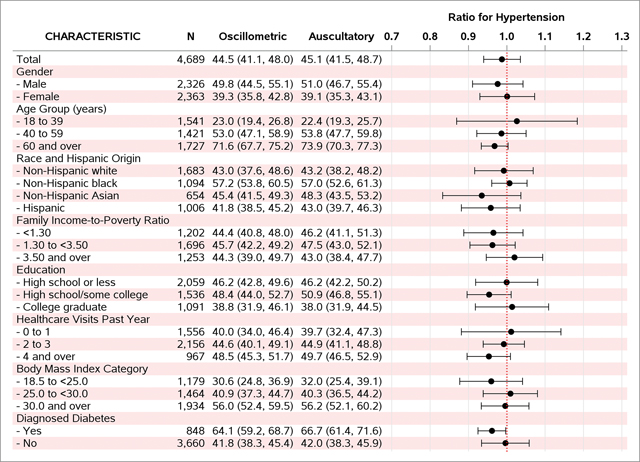
|
Notes: Hypertension is defined as systolic blood pressure ≥130, diastolic blood pressure ≥80, or current use of antihypertensive medication. Age adjusted to the US Census 2000 population using age groups 18–39, 40–59, 60, and older with weights 0.420263, 0.357202, and 0.222535. Diabetes defined as self-report or an HbA1c ≥6.5%.
Abbreviation: BP, blood pressure.
Source: 2017–2018 National Health and Nutrition Examination Survey.
Table 2.
Age-adjusted prevalence of stage II hypertension by protocol and ratios (oscillometric protocol over auscultatory protocol) among adults 18 years of age and older participating in 2 different protocols to obtain BP values: United States 2017–2018
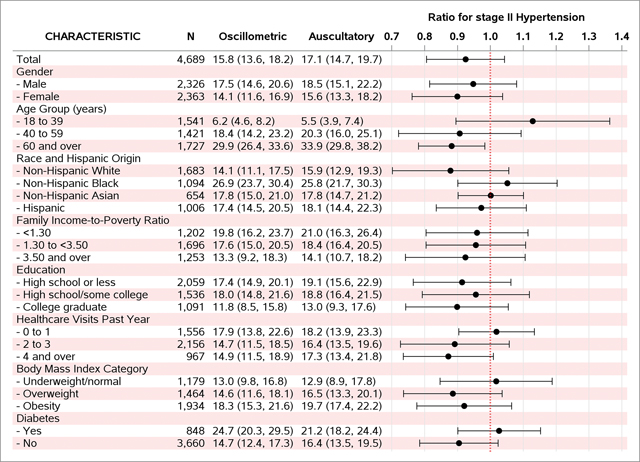
|
Notes: Stage II hypertension is defined as systolic blood pressure ≥140 or diastolic blood pressure ≥90. Age adjusted to the US Census 2000 population using age groups 18–39, 40–59, 60, and older with weights 0.420263, 0.357202, and 0.222535. Diabetes defined as self-report or an HbA1c ≥6.5%.
Abbreviation: BP, blood pressure.
Source: 2017–2018 National Health and Nutrition Examination Survey.
In the univariate analyses, the prevalence ratios for hypertension and stage II hypertension were not different from 1 (the 95% CIs included unity), except stage II hypertension for individuals aged 60+ years (prevalence ratio: 0.88 [95% CI: 0.78–0.98]). Lastly, although most of the CIs cross 1, the overall pattern of lower prevalence of for stage II hypertension by OP compared with AP was evident. The point estimate for the ratios and their 95% CIs are graphically presented in Tables 1 and 2 and tabulated values are in Supplementary Table S4 online.
Individual-level agreement
Weighted analyses of agreement between OP and AP on the prevalence of hypertension and stage II hypertension, with AP as the reference, are shown in Table 3. Among adults with hypertension, sensitivity values ranged from 70.2% (aged 18–39) to 93.1% (aged 60 years and over), and kappa statistics ranged from 0.60 (aged 18–39) to 0.80 (aged 60 and older). Among adults with stage II hypertension, sensitivity values ranged from 66.2% (aged 18–39) to 82.5% (underweight/normal weight) and kappa statistics ranged from 0.60 (aged 18–39) to 0.79 (underweight/normal weight).
Table 3.
Weighted individual-level agreement on hypertension, stage II hypertension, and hypertension control between auscultation (AP) and oscillometric (OP) protocols, United States 2017–2018 adults aged 18 and over
| Hypertension |
Stage II hypertension |
|||||
|---|---|---|---|---|---|---|
| Observations | Sensitivity % | Specificity % | Kappa (95% CI) | Sensitivity % | Specificity % | Kappa (95% CI) |
|
| ||||||
| Total | 86.3 | 88.8 | 0.75 (0.71–0.79) | 69.7 | 94.9 | 0.67 (0.61–0.72) |
| Gender | ||||||
| Men | 85.6 | 86.7 | 0.72 (0.66–0.78) | 68.4 | 93.8 | 0.64 (0.57–0.70) |
| Women | 87.1 | 90.4 | 0.78 (0.73–0.82) | 71.0 | 95.9 | 0.70 (0.63–0.77) |
| Age group | ||||||
| 18–39 years | 70.2 | 90.6 | 0.60 (0.54–0.67) | 66.2 | 97.3 | 0.60 (0.49–0.70) |
| 40–59 years | 85.7 | 85.0 | 0.71 (0.64–0.77) | 67.8 | 94.2 | 0.64 (0.55–0.74) |
| 60 years and over | 93.1 | 89.6 | 0.80 (0.75–0.86) | 71.8 | 91.6 | 0.65 (0.57–0.73) |
| Race and Hispanic origin | ||||||
| Non-Hispanic White | 86.8 | 88.7 | 0.76 (0.70–0.81) | 68.5 | 95.6 | 0.67 (0.58–0.76) |
| Non-Hispanic Black | 90.5 | 86.9 | 0.77 (0.74–0.81) | 78.1 | 90.9 | 0.68 (0.64–0.72) |
| Non-Hispanic Asian | 82.9 | 89.6 | 0.73 (0.68–0.77) | 68.5 | 93.1 | 0.62 (0.50–0.73) |
| Hispanic | 81.0 | 90.3 | 0.72 (0.64–0.80) | 68.4 | 94.7 | 0.64 (0.57–0.71) |
| Family income-to-poverty ratio | ||||||
| Less than 1.3 | 83.3 | 90.4 | 0.74 (0.69–0.79) | 73.5 | 95.1 | 0.70 (0.65–0.75) |
| 1.3 to less than 3.5 | 86.1 | 89.2 | 0.75 (0.68–0.82) | 70.9 | 93.7 | 0.66 (0.58–0.73) |
| 3.5 or more | 87.5 | 87.4 | 0.75 (0.67–0.82) | 68.1 | 95.4 | 0.66 (0.56–0.75) |
| Level of education | ||||||
| High school or less | 87.3 | 87.9 | 0.75 (0.70–0.80) | 69.6 | 94.4 | 0.66 (0.58–0.74) |
| More than high school/some college | 85.6 | 89.1 | 0.75 (0.68–0.81) | 70.2 | 93.7 | 0.65 (0.56–0.75) |
| College graduate | 85.7 | 89.4 | 0.75 (0.67–0.83) | 69.2 | 96.6 | 0.69 (0.62–0.76) |
| Healthcare visits in the past year | ||||||
| 0–1 | 78.7 | 87.0 | 0.66 (0.58–0.73) | 75.1 | 95.3 | 0.70 (0.63–0.78) |
| 2–3 | 89.4 | 90.1 | 0.79 (0.75–0.84) | 68.0 | 95.0 | 0.66 (0.58–0.73) |
| 4 or more | 87.9 | 89.4 | 0.76 (0.69–0.84) | 66.7 | 94.1 | 0.64 (0.55–0.72) |
| Body mass index category | ||||||
| Underweight/normal | 81.6 | 93.7 | 0.76 (0.71–0.81) | 82.5 | 97.3 | 0.79 (0.70–0.89) |
| Overweight | 86.8 | 88.3 | 0.75 (0.70–0.80) | 67.2 | 94.9 | 0.65 (0.57–0.74) |
| Obesity | 88.4 | 83.9 | 0.72 (0.65–0.79) | 66.5 | 93.3 | 0.62 (0.54–0.69) |
| Diabetes | ||||||
| Yes | 92.7 | 85.1 | 0.73 (0.63–0.84) | 79.9 | 90.6 | 0.70 (0.61–0.80) |
| No | 84.6 | 88.9 | 0.74 (0.69–0.78) | 67.0 | 95.3 | 0.65 (0.59–0.71) |
Notes: AP is the gold standard. Sensitivity (True Positive rate) = percent of predicted positive among actual positive. Specificity (True Negative rate) = percent of predicted negative among actual negative. Hypertension is defined as systolic blood pressure ≥130, diastolic blood pressure ≥80, or current use of antihypertensive medication. Stage II hypertension is defined as systolic blood pressure ≥140 or diastolic blood pressure ≥90. Diabetes = defined as self-report or an HbA1c ≥6.5%.
Abbreviation: CI, confidence interval.
Source: 2017–2018 National Health and Nutrition Examination Survey.
DISCUSSION
Overall, there were no significant differences in prevalence of hypertension and stage II hypertension between AP and OP. The overall agreement in hypertension and stage II hypertension between the 2 protocols was good (between 60% and 80%). This analysis compared US prevalence estimates for hypertension and stage II hypertension according to the use of the older AP to the newer OP, using the BP categories in the 2017 ACC/AHA hypertension guidelines.8 These findings indicate that the protocol change may not substantially affect the overall national BP prevalence estimates for US adults. Consequently, our findings may inform surveillance of hypertension in the United States when using the 2017 ACC/AHA hypertension definition with NHANES data, including in the American Heart Association’s annual Heart Disease and Stroke Statistics Update.29
The study had 2 objectives: (i) comparing the prevalence of hypertension and stage II hypertension using the 2 protocols and updated clinical guidelines (ii) comparing individual-level agreement for hypertension and stage II hypertension. For the first objective, there was no difference overall or by almost all demographics and hypertension risk factors analyzed. The prevalence of stage II hypertension in adults aged 60 and older, however, was significantly lower as measured by OP than by AP. One explanation for why adults aged 60 and older with stage II hypertension differ by protocol may be related to the auscultatory gap phenomenon. An auscultatory gap is more common among older individuals secondary to increased arterial stiffness.30 During the AP, a physician manually obtained the maximum inflation level to overcome the auscultatory gap phenomena and avoided falsely low estimates of systolic BP. In the OP, the oscillometric BP devices estimate systolic BP and diastolic BP from the mean arterial pressure using a device-specific algorithm.31 It is possible that the algorithm may not detect the auscultatory gap, explaining the difference by protocol in stage II hypertension among adults aged 60 and older (AP 33.9%) compared with OP 29.9%.
The individual agreements (OP and AP) for hypertension and stage II hypertension varied for the second objective. The percentage agreement for hypertension had a sensitivity of 86.3% (κ = 0.75), and the percentage agreement for stage II hypertension had a sensitivity of 69.7% (κ = 0.67). Overall, the findings suggest that individual-level protocol agreement where AP is the reference is stronger for hypertension than for stage II hypertension. One explanation for the lower individual agreement for stage II hypertension may be attributed to hypervigilance from physicians under the AP condition when observing BP values that are clinically important (i.e., 140 mm Hg systolic and 90 mm Hg diastolic, which was the previous, long-standing cutpoint to define hypertension).32 Indeed, in our earlier study, we reported that the end digit preference for zero was 43.8% for systolic ≤90 mm Hg but 19.3% for systolic of 134–142 mm Hg. Essentially, we suggest that the BP observer’s mental concentration lessens at the low extremes.33 This is not the case for oscillometric measurement of BP which is driven by device algorithm.31
The study’s strength is that it was conducted on a nationally representative sample of the US noninstitutionalized population aged 18 and over. This study had several limitations. First, the OP BP data were collected by 10 equally trained health technicians, with the percent of measurements per technician ranging from 1% to 17% of total OP data collected. Four equally trained physicians collected 99% of the AP BP data; the percent of measurements per physician ranged from 7% to 49% (similarly trained backup physicians collected the additional 1% of data). Accordingly, the variability in examiner (health technician vs. physician) may be a confounding variable. Second, there is a possibility that BP observers of either protocol were not always adhering to standardized data collection protocol, which could have introduced systemic or random bias to their readings. Third, among numerous validated oscillometric BP devices, the Omron 907XL was used in this study; therefore, the results of this study may not be generalized to other valid oscillometric BP devices because each BP device manufacturer has a unique algorithm to calculate systolic and diastolic BP values.31,34
This study compared 2 different standardized protocols for obtaining BP in a large, national sample of the US civilian noninstitutionalized population aged 18 and over. With one exception (participants aged 60 and older categorized stage II hypertension), the findings showed general agreement between protocols when following the 2017 ACC/AHA hypertension guidelines to obtain standardized BP readings.8 Lastly, the analysis is based on publicly released data which is open to further analysis using different BP values categories.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank Michele Chiappa, B.A., Peraton, for her editorial support. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the US Public Health Service.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
SUPPLEMENTARY MATERIAL
Supplementary data are available at American Journal of Hypertension online.
REFERENCES
- 1.Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National Health and Nutrition Examination Survey: plan and operations, 1999–2010. Vital Health Stat 1 2013;(56):1–37. [PubMed] [Google Scholar]
- 2.Messelbeck J, Sutherland L. Applying environmental product design to biomedical products research. Environ Health Perspect 2000; 108(Suppl 6):997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sorlie PD, Allison MA, Avilés-Santa ML, Cai J, Daviglus ML, Howard AG, Kaplan R, Lavange LM, Raij L, Schneiderman N, Wassertheil-Smoller S, Talavera GA. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens 2014; 27:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ostchega Y, Nwankwo T, Sorlie PD, Wolz M, Zipf G. Assessing the validity of the Omron HEM-907XL oscillometric blood pressure measurement device in a National Survey environment. J Clin Hypertens (Greenwich) 2010; 12:22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ostchega Y, Zhang G, Sorlie P, Hughes JP, Reed-Gillette DS, Nwankwo T, Yoon S. Blood pressure randomized methodology study comparing automatic oscillometric and mercury sphygmomanometer devices: National Health and Nutrition Examination Survey, 2009–2010. Natl Health Stat Rep 2012;(59):1–15. [PubMed] [Google Scholar]
- 7.Ostchega Y, Nwankwo T, Chiappa M, Wolz M, Graber J, Nguyen DT. Comparing blood pressure values obtained by two different protocols: National Health and Nutrition Examination Survey, 2017–2018. Vital Health Stat 2 2021;(87):1–26. [PubMed] [Google Scholar]
- 8.Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary. J Am Coll Cardiol 2018; 71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 9.Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension Prevalence Among Adults Aged 18 and Over: United States, 2017–2018. NCHS Data Brief, No. 364. National Center for Health Statistics: Hyattsville, MD, 2020. [PubMed] [Google Scholar]
- 10.NHANES Survey Methods and Analytic Guidelines. cdc.gov
- 11.White WB, Anwar YA. Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press Monit 2001; 6:107–110. [DOI] [PubMed] [Google Scholar]
- 12.El Assaad MA, Topouchian JA, Darné BM, Asmar RG. Validation of the Omron HEM-907 device for blood pressure measurement. Blood Press Monit 2002; 7:237–241. [DOI] [PubMed] [Google Scholar]
- 13.National Health and Nutrition Examination Survey (NHANES). Physician Examination Procedures Manual. https://wwwn.cdc.gov/nchs/data/nhanes/2017-2018/manuals/2018-Physician-Examination-Manual-508.pdf
- 14.National Health and Nutrition Examination Survey (NHANES). Blood Pressure Procedures Manual. https://wwwn.cdc.gov/nchs/data/nhanes/2019-2020/manuals/2019-Blood-Pressure-Procedures-Manual-508.pdf
- 15.Muntner P, Einhorn PT, Cushman WC, Whelton PK, Bello NA, Drawz PE, Green BB, Jones DW, Juraschek SP, Margolis KL, Miller ER III, Navar AM, Ostchega Y, Rakotz MK, Rosner B, Schwartz JE, Shimbo D, Stergiou GS, Townsend RR, Williamson JD, Wright JT Jr, Appel LJ; 2017 National Heart, Lung, and Blood Institute Working Group. Blood pressure assessment in adults in clinical practice and clinic-based research: JACC Scientific Expert Panel. J Am Coll Cardiol 2019; 73:317–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA 2020; 324:1190–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ostchega Y, Zhang G, Hughes JP, Nwankwo T. Factors associated with hypertension control in US adults using 2017 ACC/AHA Guidelines: National Health and Nutrition Examination Survey 1999–2016. Am J Hypertens 2018; 31:886–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Center for Health Statistics. Health, United States, 2019. U.S. Department Of Health And Human Services: Hyattsville, MD, 2021. [Google Scholar]
- 19.Department of Health and Human Services. Poverty Guidelines, Research, and Measurement. https://aspe.hhs.gov/poverty-research. Accessed 5 March 2021.
- 20.Centers for Disease Control and Prevention, National Center for Health Statistics, National Health and Nutrition Examination Survey (NHANES). NHANES Questionnaires, Datasets, and Related Documentation. cdc.gov. Accessed 5 March 2021.
- 21.National Health and Nutrition Examination Survey (NHANES). Anthropometry Procedures Manual. https://wwwn.cdc.gov/nchs/data/nhanes/2017-2018/manuals/2017_Anthropometry_Procedures_Manual.pdf. Accessed 5 March 2021.
- 22.National Heart, Lung, and Blood Institute. Managing Overweight and Obesity in Adults: Systematic Evidence Reviews from the Obesity Expert Panel. 2013. https://www.nhlbi.nih.gov/sites/default/files/media/docs/obesity-evidence-review.pdf. Accessed 5 March 2021.
- 23.American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes 2019. Diabetes Care 2019; 42(Suppl 1):S13–S28. [DOI] [PubMed] [Google Scholar]
- 24.Rao JNK, Scott AJ. The analysis of categorical data from complex sample surveys: chi-squared tests for goodness of fit and independence in two-way tables. J Am Stat Assoc 1981; 76:374, 221–230. [Google Scholar]
- 25.Korn EL, Graubard BI. Confidence intervals for proportions with the small expected number of positive counts estimated from survey data. Surv Methodol 1998; 23:193–201. [Google Scholar]
- 26.National Center for Health Statistics. National Center for Health Statistics Data Presentation Standards for Proportions. NCHS Vital and Health Statistics, Series 2, Number 175, August 2017. cdc.gov. Accessed 5 March 2021. [PubMed] [Google Scholar]
- 27.Klein RJ, Schoenborn CA. Age Adjustment Using the 2000 Projected US Population. Healthy People 2010 Statistical Notes, No. 20. National Center for Health Statistics: Hyattsville, MD, 2001. [PubMed] [Google Scholar]
- 28.Jekel JF, Katz DL, Elmore JF. Epidemiology, Biostatistics, and Preventive Medicine. W.B. Saunders: Philadelphia, PA, 2001. [Google Scholar]
- 29.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation 2021; 143:e254–e743. [DOI] [PubMed] [Google Scholar]
- 30.Cavallini MC, Roman MJ, Blank SG, Pini R, Pickering TG, Devereux RB. Association of the auscultatory gap with vascular disease in hypertensive patients. Ann Intern Med 1996; 124:877–888. [DOI] [PubMed] [Google Scholar]
- 31.Alpert BS, Quinn D, Gallick D. Oscillometric blood pressure: a review for clinicians. J Am Soc Hypertens 2014; 8:930–938. [DOI] [PubMed] [Google Scholar]
- 32.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003; 42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 33.Ostchega Y, Prineas RJ, Paulose-Ram R, Grim CM, Willard G, Collins D. National Health and Nutrition Examination Survey 1999–2000: effect of observer training and protocol standardization on reducing blood pressure measurement error. J Clin Epidemiol 2003; 56:768–774. [DOI] [PubMed] [Google Scholar]
- 34.Lewis PS; British and Irish Hypertension Society’s Blood Pressure Measurement Working Party. Oscillometric measurement of blood pressure: a simplified explanation. A technical note on behalf of the British and Irish Hypertension Society. J Hum Hypertens 2019; 33:349–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


