Abstract
The COVID-19 pandemic disproportionately affects females in the home and workplace. This study aimed to acquire information regarding the gender-specific effects of the COVID-19 lockdown on aspects of professional and personal lives of a subset of pediatric cardiologists. We sent an online multiple-choice survey to a listserv of Pediatric Cardiologists. Data collected included demographics, dependent care details, work hours, leave from work, salary cut, childcare hours before and after the COVID-19 peak lockdown/stay at home mandate and partner involvement. Two hundred forty-two pediatric cardiologists with dependent care responsibilities responded (response rate of 20.2%). A significantly higher proportion of females reported a salary cut (29.1% of females vs 17.6% of males, p = 0.04) and scaled back or discontinued work (14% vs 5.3%; p = 0.03). Prior to the COVID-19 lockdown phase, females provided more hours of dependent care. Females also reported a significantly greater increase in childcare hours overall per week (45 hours post/30 hours pre vs 30 hours post/20 hours pre for men; p < 0.001). Male cardiologists were much more likely to have partners who reduced work hours (67% vs 28%; p < 0.001) and reported that their partners took a salary cut compared with partners of female cardiologists (51% vs 22%; p < 0.001). In conclusion, gender disparity in caregiver responsibilities existed among highly skilled pediatric cardiologists even before the COVID-19 pandemic. The pandemic has disproportionately affected female pediatric cardiologists with respect to dependent care responsibilities, time at work, and financial compensation.
The COVID-19 pandemic continues to affect livelihoods around the world and its economic and social fallouts are disproportionately affecting women in the workplace and at home. Globally, the rate of job loss among women during this pandemic has exceeded 180% of the rate for men.1 Although women comprise 39% of the global work force, they have incurred 54% of all job losses.1 One reason for this disparity is that the virus has significantly increased the family burden of unpaid child and adult care, for which women carry a greater responsibility.1 Recent articles by Reza et al. and Brubaker highlight the need to retain and support female physicians during this pandemic.2 , 3 Although this study was limited to pediatric cardiologists, findings are likely to be similar among other highly skilled medical professionals.
Methods
We obtained approval from the University of Florida Institutional Review Board and conducted an online REDCap-based survey of a subset of current North American Pediatric Cardiologists in practice and training (subscribers to the ‘PediHeartNet’ listserv: PediHeartNet-http://pediheart.net is a private, unmoderated discussion group of predominantly North American Pediatric Cardiologists) who had child or adult dependent care responsibilities. Our 33-item survey (Supplemental File) collected demographic information including age, gender, work experience and details about dependent care. Questions addressed changes in work hours, work leave, and compensation that occurred as a consequence of COVID-19. The survey captured the average amount of time spent by the respondent and by the respondent's partner in providing care or supervision to child and adult dependents before and after many states issued COVID-19 stay-at-home mandates. Finally, the survey provided an opportunity for respondents to relate their most challenging experiences with changes in dependent care consequent to the COVID-19 pandemic. After obtaining permission from the moderators of the listserv, we emailed the survey in July 2020 to approximately 1,200 pediatric cardiologists and requested anonymous responses from pediatric cardiologist physicians in training or in practice whose household included child and/or adult dependents. We emailed a reminder 3, 7, and 14 days after the initial solicitation and closed data collection on day 16. As an incentive, we offered the opportunity to participate in a small online gift card drawing.
We performed descriptive and inferential statistical analyses using SAS v 9.4 and SPSS v 24. Categorical variables were expressed as frequencies and percentages and continuous variables were expressed as mean or median with standard deviation or ranges. The impact of COVID-19 was defined in terms of both categorical and continuous outcome variables. We analyzed categorical continuous variables using logistic regression with gender as the independent variable. Covariates that achieved a 0.15 level of significance were included in the model. We compared continuous variables between genders using t-test or Wilcoxon rank sum test. Significant covariates were included in a linear regression model. If the variable under consideration was not normally distributed then a log linear transformation was performed. p value <0.05 was considered significant.
The principal investigator and 2 other data analysts from the University of Florida with experience in qualitative research methodology (MAB and MF) reviewed all responses to the open-ended question that sought a narrative response to the dependent care challenges posed by COVID-19. Over a 3-week period, each member of the team sorted responses into 10 main topical areas and then all members organized the responses into 5 domains for analysis.
Results
A total of 256 respondents attempted the survey of which 242 respondents were actually eligible (response rate of 20.2%). Of these, 127 (52%) of respondents were female compared with 34% of all board certified pediatric cardiologists in the United States who are female.4 Demographics of respondents are outlined in Table 1 . The largest group of respondents were aged 30 to 39 and had been in practice for less than 5 years. Although there was no gender difference in the median age of surveyed trainees, female cardiologists in practice had a lower median age than male cardiologists. Interventional cardiac subspecialties accounted for 11.6% of overall respondents. Most (86.7%) cardiologists had childcare responsibilities and 12.8% cared for adults. Most single parents or adult caregivers tended to be female (p < 0.0001).
Table 1.
Study population baseline characteristics
| All | Male | Female | p Value | |
|---|---|---|---|---|
| Variable | ||||
| Age Group (years) | ||||
| 20 - 29 | 5 | 4 (3.5%) | 1 (0.8%) | 0.22† |
| 30 - 39 | 109 | 45 (39.8%) | 64 (50.4%) | |
| 40 - 49 | 85 | 44 (38.9%) | 41 (32.3%) | |
| 50 - 59 | 27 | 15 (13.3%) | 12 (9.4%) | |
| > 60 | 14 | 5 (4.4%) | 9 (7.1%) | |
| Gender | 240 | 113 (47.1%) | 127 (52.9%) | |
| Sexual Orientation | ||||
| Straight | 222 | 102 (90.3%) | 120 (94.5%) | 0.10† |
| Lesbian/Gay | 9 | 6 (5.3%) | 3 (2.4%) | |
| Bisexual | 6 | 5 (4.4%) | 1 (0.8%) | |
| Race | ||||
| Asian | 67 | 31 (27.7%) | 36 (28.3%) | 0.23* |
| Black/African American | 19 | 11 (9.8%) | 8 (6.3%) | |
| White | 132 | 59 (52.7%) | 73 (57.5%) | |
| Other | 15 | 9 (8%) | 6 (4.8%) | |
| Prefer not to answer | 6 | 2 (1.8%) | 4 (3.1%) | |
| Ethnicity | ||||
| Hispanic/Latino | 25 | 14 (12.7%) | 11 (8.8%) | 0.61† |
| Non-Hispanic/Latino | 201 | 92 (83.6%) | 109 (87.2%) | |
| Prefer not to answer | 9 | 4 (3.6%) | 5 (4%) | |
| Employment: | ||||
| Fellowship | 32 | 13 (11.5%) | 19 (15.1%) | 0.42* |
| Not in fellowship | 207 | 100 (88.5%) | 107 (84.9%) | |
| Years of fellowship | ||||
| 1 | 5 | 4 (30.8%) | 1 (6.7%) | 0.17† |
| 2 | 5 | 3 (23.1%) | 2 (13.3%) | |
| 3 | 9 | 2 (15.4%) | 7 (46.7%) | |
| 4 | 7 | 4 (30.8%) | 3 (20%) | |
| 5 | 2 | 0 (0%) | 2 (13.3%) | |
| Years of practice | ||||
| ≤ 5 | 86 | 35 (31.3%) | 51 (40.5%) | 0.02§ |
| 6 - 10 | 56 | 23 (20.5%) | 33 (26.2%) | |
| 11 - 15 | 47 | 28 (25%) | 19 (15.1%) | |
| 16 - 20 | 28 | 19 (17%) | 9 (7.1%) | |
| ≥ 21 | 21 | 7 (6.3%) | 14 (11.1%) | |
| Sub-specialty | ||||
| Interventional | 28 | 18 (15.9%) | 10 (7.9%) | |
| Non interventional | 212 | 95 (84.1%) | 117 (92.1%) | 0.05* |
| Time worked | ||||
| Full Time | 224 | 109 (96.5%) | 115 (91.3%) | 0.09* |
| Percentage Part Time | 15 | 4 (3.5%) | 11 (8.7%) | |
| 60 - 69 | 6 | 1 | 5 | |
| 70 - 79 | 6 | 2 | 4 | |
| 80 - 89 | 3 | 1 | 2 | |
| Dependent Care | ||||
| Children | 197 | 97 | 100 | |
| <7 years Mean (Range) | 1.53 (1-4) | 1.38 (1-3) | 1.67 (1-4) | 0.049‡ |
| 7-17 years: Mean (Range) | 1.63 (1-6) | 1.69 (1-6) | 1.57 (1-3) | 0.87‡ |
| Adult | 18 | 6 | 12 | 0.16* |
| Both Children and Adult | 13 | 6 | 7 | 0.78* |
| Single Parent or Adult Caregiver | 20 | 1 | 19 | <0.0001* |
Chi Square test.
Fisher's Exact test.
Wilcoxon Rank Sum test.
Trend test.
The lockdown phase significantly reduced work hours, with 56% of male and 53% of female cardiologists reporting some decrease in work hours. Most cardiologists reported less than a 20% decrease in work hours. However, despite a similar cut in work hours, a significantly higher proportion of females reported a salary cut and more females reported a salary cut greater than 20% (47% of females vs 25% of males, p = 0.2). More female cardiologists reduced or discontinued work compared with male cardiologists (Table 2 ).
Table 2.
Impact of lockdown on work distribution by gender
| All | Male | Female | p Value | |
|---|---|---|---|---|
| Work hours decreased | ||||
| Yes | 130 | 63 (55.8%) | 67 (52.8%) | 0.64* |
| No | 110 | 50 (44.2%) | 60 (47.2%) | |
| Percentage decrease in work hours | ||||
| < 20 | 104 | 54 (85.7%) | 50 (74.6%) | 0.37† |
| 21 - 40 | 16 | 5 (7.9%) | 11 (16.4%) | |
| 41 - 60 | 6 | 3 (4.7%) | 3 (4.5%) | |
| > 60 | 4 | 1(1.6%) | 3 (4.5%) | |
| Experienced Salary Cut | ||||
| Yes | 57 | 20 (17.7%) | 37 (29.1%) | 0.04* |
| No | 183 | 93 (82.3%) | 90 (70.9%) | |
| % Salary Cut: Median (Range) | 12.5 (5-50) | 15 (5-50) | ||
| Took Leave from Work or Quit Work | ||||
| Yes | 24 | 6 (5.3%) | 18 (14.2%) | 0.02* |
| No | 216 | 107 (94.7%) | 109 (85.8%) | |
| Are Genders Affected Disproportionately? | ||||
| Yes | 150 | 39 (35.5%) | 111 (89.5%) | <0.0001* |
| No | 70 | 65 (59.1%) | 5 (4.0%) | |
| Don't know | 14 | 6 (5.5%) | 8 (6.5%) | |
| Has Caring for Child Impacted Work Life Balance? | ||||
| Yes | 174 | 79 (79%) | 95 (89.6%) | 0.035* |
| No | 32 | 21 (21%) | 11 (10.4%) | |
| Has Caring for Adult Impacted Work Life Balance? | ||||
| Yes | 26 | 9 (81.8%) | 17 (89.5%) | 0.61† |
| No | 4 | 2 (18.2%) | 2 (10.5%) |
Chi Square test.
Fisher's Exact test.
COVID-19 had a pronounced gender-specific effect on spousal work hours during the peak lockdown. Male cardiologists were more likely to have partners who cut back on work hours and report that their partners took a salary cut compared with partners of female cardiologists (Table 3 ). Prior to the COVID-19 lockdown, females shouldered a greater burden of dependent care per week than males (30 hours vs 20 hours; p = 0.02). Females also reported spending significantly more time during the regular workweek (M-F, 9 A.M. to 6 P.M.) during which they provided dependent care. During the lockdown, the total number of childcare hours per week and during regular weekday work hours increased significantly for both females and males compared with their pre-COVID-19 baselines. However, when we compared the absolute increase in hours for males and females during lockdown to baseline, females reported a significantly greater increase in childcare hours overall per week (45 hours post/30 hours pre vs 30 hours post/20 hours pre; p < 0.001). Females also were responsible for a significantly greater number of hours of dependent care between 9 A.M. to 6 P.M. (M-F) compared with males (20 hours post/3 hours pre vs 4 hours post/1 hours pre; p < 0.001; Table 4 ).
Table 3.
Effect of COVID-19 on partner
| Partner work cut | All | Male | Female | p Value |
|---|---|---|---|---|
| Yes | 99 | 70 (66.7%) | 27 (28.4%) | <0.0001* |
| No | 103 | 35 (33.3%) | 68 (71.6%) | |
| % Decrease in Work Hours by Partner | ||||
| < 20 | 53 | 38 (54.3%) | 15 (55.6%) | 0.86† |
| 20 - 40 | 33 | 25 (35.7%) | 8 (29.6%) | |
| 41 - 60 | 8 | 5 (7.1%) | 3 (11.1%) | |
| > 60 | 3 | 2 (2.9%) | 1 (3.7%) | |
| Partner Salary Cut | ||||
| Yes | 75 | 54 (51.4%) | 21 (22.3%) | <0.0001* |
| No | 124 | 51 (48.6%) | 73 (77.7%) | |
| % Partner Salary Cut: Median (Range) | 20 (10-100) | 20 (10-100) |
Chi Square test.
Fisher exact test.
Table 4.
Distribution of dependent care responsibilities by gender
| Male |
Female |
|||||
|---|---|---|---|---|---|---|
| Median (Range) provided for all data | Pre COVID-19 | During COVID-19 lockdown | p Value | Pre COVID-19 | During COVID-19 Lockdown | p Value |
| Childcare Responsibility – All Hours | 20 (0-108) | 30 (0-120) | <0.0001 | 30 (0-118) | 45 (0-125) | <0.0001 |
| Childcare Responsibility – 9 AM – 6 PM | 1 (0-18) | 9 (0- 43) | <0.0001 | 3 (0-20) | 20 (1-45) | <0.0001 |
| Partner Childcare Responsibility – All Hours | 35 (0-118) | 60 (0-128) | 20 (0-118) | 30 (0-120) | ||
| Partner Childcare Responsibility – 9 AM – 6 PM | 5 (0-40) | 30 (0-45) | 2 (0-380) | 10 (0-40) | ||
| Adult Care Responsibility – All Hours | 13.5 (8-35) | 20 (15-50) | 0.008 | 20 (1-30) | 40 (1-70) | 0.002 |
| Adult Care Responsibility – 9 AM – 6 PM | 1 (0-5) | 5 (0-8) | 0.031 | 1 (0-5) | 20 (1-30) | 0.008 |
Values are denoted as median (range).
Wilcoxon sign rank test.
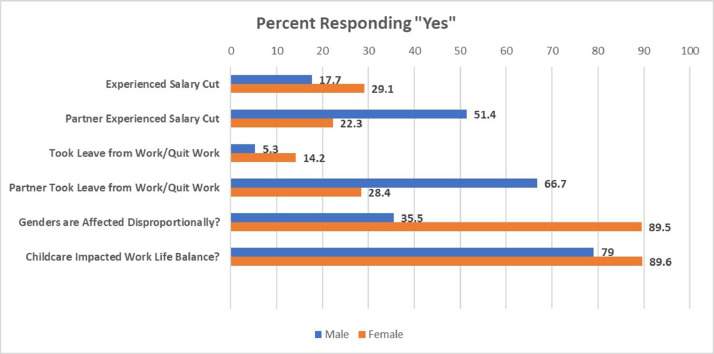
Female cardiologists reported a greater number of hours per week caring for adult dependents than did male cardiologists. During the lockdown phase, the overall number of adult care hours per week between (M-F, 9 A.M. to 6 P.M.) increased significantly for both males and females over their baseline preCOVID-19 hours. However, during the lockdown, females reported a significantly greater increase in adult care hours overall per week (40 hours post/20 hours pre vs 20 hours post/13.5 hours pre; p = 0.04). Females were also responsible for a significantly greater number of absolute hours of adult care between (M-F, 9 A.M. to 6 P.M.) compared with males (20 hours post/1 hours pre vs 5 hours post/1 hours pre; p = 0.01; Table 4). Figure 1 denotes gender distribution for significant binary outcomes. A univariate logistic regression was performed with gender as the independent variable. Covariates selected for the multivariate analysis included years in practice, subspecialty selection, sexual orientation and employment status (Table 5 ). Even when correcting for the imbalance in male and female respondents in the survey (1:1) and the distribution of board certified male and female pediatric cardiologists in practice (2:1) by attaching a weight of 2 for each male and 1 for each female, there were significant discrepancies between males and females with respect to dependent care responsibilities, loss of work and financial compensation. With respect to gender-specific perspectives, females more correctly perceived real disparities in the increased burden of dependent care (89.5% of females vs 35.5% of males; p < 0.0001; (Table 2). Both males and females agreed that caring for a child or adult dependent affected their work-life balance (90% of females vs 79% of males; p = 0.035).
Figure 1.
Gender distribution for significant binary outcomes.
Table 5.
Univariate and multivariate logistic regression
| Univariate |
Multivariate |
|||
|---|---|---|---|---|
| Outcome Variable | OR (95 % CI) | P | OR (95% CI) | P |
| Salary Cut | 1.91 (1.03-3.54) | 0.04 | 2.04 (1.09-1.58) | 0.03 |
| Leave /Quit work | 2.89 (1.10-7.56) | 0.03 | 3.15 (1.19-8.36) | 0.02 |
| Work life balance | 2.30 (1.04-5.05) | 0.04 | - | - |
| Perception on gender affection | 37.0 (13.89-98.59) | <0.0001 | 44.0(15.65- 123.57) | <0.0001 |
| Partner Salary Cut | 0.27 (0.15-0.50) | <0.0001 | - | - |
| Partner Work Cut | 0.20 (0.11-0.36) | <0.001 | - | - |
Responses to the open-ended question, "What is the most challenging aspect of dependent care you have faced during the COVID-19 lockdown?” were grouped into five domains: (1) Mental Health/Social isolation/Family tensions (2)Work-Home Balance (3) Caretaker (4) Family safety (5) Financial. A few responses crossed over domains, for instance, (1) “We have less money coming in, children who need supervision for school. Trying to work from home, with kids and my husband looking for a job means I am not only trying to do my job but also be a teacher, a cook, a housecleaner with a salary cut and a husband with no job.”(2)“No work life balance, no understanding from colleagues, super stressful, constant guilt and doubt (having to put children back in daycare, no family available etc.), worry about what to do if COVID-19 case at daycare or with online schooling”.
The researchers who designed the questionnaire and analyzed the qualitative responses acknowledged that their personal and work backgrounds might have influenced their qualitative interpretations. SF is a female electrophysiologist with 2 children under 5 whose husband works from home and assumes more than 50% of childcare responsibilities. She kept her 2 young children at home during the lockdown phase and worked from home 1 day a week to help with childcare. MAB is a female research coordinator, wife of an essential health care professional, and mother of 3 young adults who live separately. She and her children worked from home during the various mandated periods in the different states they live in. Her father passed away recently from complications related to hospital-acquired COVID-19. MF is a research administrator and single dad of a 6 year old daughter who along with support from family and friends were able to provide childcare for his daughter.
Discussion
Gender balance in the clinical workplace has been an important topic over the last decade. Pediatric cardiologists, like other healthcare providers, must balance work and family while facing choices that influence their selection of specialty, their choice of academic pursuit, and their employment status. Manifestations of solutions to achieving work-life balance differ between females and males, with female physicians more likely to make accommodations to restrict work time and duties to fulfill responsibilities at home. Family responsibilities may include providing care or supervision of children, aging parents, or both. The COVID-19 pandemic had the potential to exaggerate existing gender differences in the workplace because dually employed couples were no longer able to rely on another individual to care for or supervise their dependents.
Our study results demonstrated that the COVID-19 pandemic did disproportionately increase an already disparate burden of dependent care for both children and adults among female pediatric cardiologists. Our findings echo those of other studies. One study has shown that together, dual working parents devote six hours a day to dependent care with females absorbing two-thirds of this responsibility.5 Similarly, females are much more likely than males to be involved in the care of adult dependents.6 In other fields, both genders have assumed more home responsibilities during the COVID-19 lockdown, but previous disparities persist. Studies of nonmedical professionals have shown that even when males were initially unemployed and their female partners were the ones working full time, males continued to spend less time on household chores.7
Even though the results from this study clearly demonstrate that female cardiologists disproportionately assumed more caregiver hours during the COVID-19 lockdown, most males did not perceive this imbalance. This is consistent with the findings of a British Broadcasting Company survey that showed that perceptions of relative childcare responsibilities differ widely among males and females. Males tended to overestimate their share in domestic chores while females correctly identified their own greater contributions.8
Although the numbers were small, female cardiologists left the workplace at a rate three times greater than their male counterparts. On a global scale, females have been 1.8 times more likely to suffer job loss during the COVID-19 pandemic.1 Women comprise 39% of the global work force but have incurred 54% of all job losses.1 In the United States, for people with children under 12, unemployment increased by 11 absolute percentage points in women compared with 7.3 percentage points in men between February and April 2020.9
During the COVID-19 lockdown, both male and female pediatric cardiologists experienced similar loss of work hours, but females were twice as likely to sustain a decrease in salary. Furthermore, females in medicine have earned 26% less than their male colleagues10 so that the disproportionately larger salary reduction for women has exacerbated pre-existing disparities in compensation. This phenomenon has also played out on the global stage.11
In our study, spouses of male physicians were more likely to take leave from work or sustain a reduction in salary compared with spouses of female physicians. The spousal work differences by gender are in fact much more exaggerated than the reduced work and salary disparity between male and female cardiologists (Figure 1). Other studies during the pre-COVID-19 phase have shown that at baseline, spouses of female physicians on average work more hours and earn significantly more than spouses of male physicians. Therefore, for female physicians, a partner salary cut would impact the overall household income much more. These findings have been thought to place greater pressure on female physicians to trade professional for household responsibilities, highlighting yet another example of gender disparity even among high-earning professionals.12
This voluntary survey was launched using the PediHeartNet listserv and therefore targeted a select group of pediatric cardiologists. As with every survey, those who responded may have been particularly affected by the circumstances under inquiry or have had a particular interest in responding to questions about gender disparities. Our response rate of 20.2% exceeds the average 11% response rate for topical surveys but still does not capture the perspective of all pediatric cardiologists with dependent care responsibilities. Finally, not all respondents answered every question because participants were allowed to proceed to the next question even if they chose not to answer the prior one. The authors acknowledge that there were likely multiple factors influencing salary that were not elicited and controlled for in this study such as private versus academic practice, fixed vs incentive/volume-based salary models or discrepancies with some respondents being in less affected areas or receiving CARES Act funding.
Our study highlights that gender disparity in caregiver duties existed among pediatric cardiologists before the COVID-19 pandemic. The COVID-19 pandemic has disproportionately affected female pediatric cardiologists with respect to dependent care responsibilities, time at work, and financial compensation. Male pediatric cardiologists have not appreciated this gender disparity. The accentuation of gender disparity by the COVID-19 pandemic may continue to have an adverse effect on a woman's professional career long after its more acute effects resolve.
Author Contribution
Dr Ferns conceptualized and designed the study and data collection instruments, collected data, carried out the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript. Serves as guarantor. Dr Gautam co-designed the data collection instruments, carried out the initial analyses and reviewed and revised the manuscript. Dr Hudak contributed to conceptualization of the study, critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. The guarantor accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Acknowledgments
The authors acknowledge the efforts of Maria Abbey Bautista and Mark Fafard from the UF Research Affairs Office for assistance with REDCap survey design and qualitative analysis.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Footnotes
Funding: None.
References
- 1.Madgavkar A, White O, Krishnan M, Mahajan D, Azcue X. 2020. COVID-19 and Gender Equality: Countering the Regressive Effects. Mc Kinsey Global Institute. https://www.mckinsey.com/featured-insights/future-of-work/covid-19-and-gender-equality-countering-the-regressive-effects. Accessed Oct 20, 2020. [Google Scholar]
- 2.Reza N, DeFilippis EM, Michos ED. The cascading effects of COVID-19 on women in cardiology. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.049792. Epub ahead of print. PMID: 33016784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brubaker L. Women physicians and the COVID-19 pandemic. JAMA. 2020;324:835–836. doi: 10.1001/jama.2020.14797. [DOI] [PubMed] [Google Scholar]
- 4.American Board of Pediatrics . 2018. Workforce Database.https://www.abp.org/content/workforce Accessed October 20, 2020. [Google Scholar]
- 5.Miller CC. Nearly half of men say they do most of the home schooling. 3 percent of women agree. The New York Times. 2020 https://www.nytimes.com/2020/05/06/upshot/pandemic-chores-homeschooling-gender.html. Accessed Oct 2020. [Google Scholar]
- 6.Sharma N, Chakrabarti S, Grover S. Gender differences in caregiving among family - caregivers of people with mental illnesses. World J Psychiatry. 2016;6:7–17. doi: 10.5498/wjp.v6.i1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ortiz-Ospina E, Tzvetkova S. OurWorldInData.org; 2018. Women's Employment.https://ourworldindata.org/female-labor-supply Accessed Oct 20, 2020. [Google Scholar]
- 8.Savage M. BBC Worklife; June 2020. How COVID-19 is Changing Women's Lives. https://www.bbc.com/worklife/article/20200630-how-covid-19-is-changing-womens-lives. Accessed Oct 20, 2020. [Google Scholar]
- 9.Gupta S. How COVID-19 worsened gender inequality in the U.S. workforce. Science News. 2020 https://www.sciencenews.org/article/covid19-worsened-gender-inequality-us-workforce. Accessed Oct 20, 2020. [Google Scholar]
- 10.Doximity. “Second Annual Physician Compensation Report: March 2018.” https://www.doximity.com/careers/compensation_report?_csrf_ attempted=yes. Accessed Oct 20, 2020.
- 11.Boniol M, McIsaac M, Xu L, Wuliji T, Diallo K, Campbell J. 2019. Gender Equity in the Health Workforce: Analysis of 104 Countries Health Workforce Working Paper 1. https://www.who.int/hrh/resources/gender_equity-health_workforce_analysis/en/. Accessed Oct 20, 2020. [Google Scholar]
- 12.Ly DP, Seabury SA, Jena AB. Characteristics of U.S. physician marriages, 2000-2015: an analysis of data from a U.S. census survey. Ann Intern Med. 2018;168:375–376. doi: 10.7326/M17-1758. [DOI] [PubMed] [Google Scholar]