Abstract
Purpose
Prone positioning during the COVID-19 pandemic has become increasingly used as an adjunct to increase oxygenation in critical care patients. It is associated with an adverse event profile. This study sought to investigate the occurrence of ocular injuries reported in prone versus supine groups in adult critical care.
Design
Systematic review and meta-analysis.
Methods
A systematic review and meta-analysis were carried out in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. PubMed, SCOPUS, and the Cochrane Library were searched. The search period was January 1, 1990, to July 1, 2020.
Results
Eleven randomized controlled trials were included, with 2,247 patients. Twenty-eight events were recorded in 3 trials (174 patients) and no events in the other 8 trials (2,073 patients). The rates of eye injury were 5 events in 1,158 patients (1.30%) and 13 events in 1,089 patients (1.19%) in the prone and supine groups, respectively, which were reduced to 2 of 1,158 patients (0.17%) and 2 of 1,089 patients (0.18%), respectively, when reports of eye or eyelid edema were removed. Meta-analysis demonstrated no significant differences between groups with (an OR of 1.40 (95% CI: 0.37–5.27) and without (OR: 0.78; 95% CI: 0.11–5.73) reported edema.
Conclusions
This meta-analysis showed no significant difference in the rate of reported ocular injury between prone and supine critical care groups. These rates remain higher than the incidence reported during general anesthesia. There is a need for studies in critical care settings in which ocular injury is an end-point and which include extended patient follow-up.
During the first decade of the 21st century, multiple trials demonstrated an improvement in oxygenation in patients with acute respiratory distress syndrome receiving nurse attendance in the prone position.1, 2, 3, 4 In combination with lung protective ventilation, this improvement has subsequently been demonstrated to reduce mortality compared to conventional supine ventilation.5 However, this technique is not without risk. The Faculty of Intensive Care Medicine (FICM) released guidelines for the implementation of this technique in 2019 as there was concern that the increased use of prone positioning was contributing to the rise in critical safety incidents, including pressure injuries to anterior structures.6
One such structure was the eye. Vision loss and impairment due to optic nerve, corneal, and scleral injuries, along with extraocular muscle impingement had been reported previously following spinal and plastic surgery procedures performed with the patient in a prone position,7, 8, 9 with prone positioning having been reported to increase intraocular pressure.10 FICM prone position guidelines aimed to reduce both exposure and pressure, recommending several measures including taping patients’ eyes shut; ensuring there is no direct pressure on patients’ eyes; placing patients in a 30-degrees foot-down position (reverse Trendelenburg) while being nursed in this position (to limit dependent periocular swelling) and rotating patients’ heads from side-to-side at 2-hour intervals.6
Despite the increased use of prone positioning in critical care adults, as highlighted in both popular and scientific press during the recent COVID-19 pandemic, the complication profile of prone positioning is still emerging.11 A previous review of the complications associated with prone positioning revealed only studies in surgical patients.12 This is a different cohort from those in critical care, who should be considered separately. Due to longer cumulative time periods in the prone position, the need for increased repositioning and the easier access for nursing staff (no sterile field to avoid) in critical care patients form a distinct patient group and should be regarded as such. It may also be argued that, as a positive fluid balance may be more likely in critical care patients than in surgical patients, the risks of dependent edema and pressure injury are increased.
THE AIM OF THIS REVIEW
The purpose of this systematic review was to compare the incidence and types of ocular injury reported in randomized controlled trials of prone positioning versus supine positioning in adult critical care and, if possible, perform a meta-analysis. This investigation has not been conducted previously to the authors’ knowledge.
METHODS
This systematic review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.13 A review protocol was registered with the PROSPERO systematic review database (registration number: CRD42020196917).14
Study Eligibility Criteria
Studies in adult (18 years of age or older at the time of intervention) hospital inpatients in critical care (defined as patients requiring at least Level 2 care, as defined by the National Health Service Critical Care Service Framework) were eligible, regardless of patients’ sedation level, indication for prone positioning (eg, respiratory- or surgical site-related), or geographical location of care.15 Studies including any form of prone positioning adjuncts (where the patient is positioned face down on the bed) were included. Only randomized controlled trials (RCTs) that compared prone to supine positioning were included. Any variation of RCT design was eligible, including cluster or cross-over.
Primary outcome was the incidence of ocular injuries, presented as both crude rates and, after meta-analysis, odds ratios (OR). Only papers published in indexed medical journals (conference abstracts were excluded) were included, with English as the language of publication. The date of publication was restricted to the previous 3 decades (January 1, 1990 to July 1, 2020). This range was defined by the authors because prone positioning in critical care patients became increasingly common following a series of RCTs published during the year 2000. Allowing the search to include studies from between 1990 and 2000 would allow capturing any preceding studies within the same era of critical care.
Information Sources and Search
Four databases, PubMed (MeSH and Advanced), SCOPUS, and Cochrane Library were searched. For PubMed, the search was conducted using both MeSH terms and the advanced search option. MeSH terms (“Position,” “Prone’) were used. An advanced search was conducted using the terms “Prone” AND “Randomised.” Ovid, Embase, and SCOPUS were also searched using the same terms with automatic adjustment for Americanized spelling. The Cochrane Library was searched using the term “Prone.”
Study Selection and Data Collection Process
Two independent reviewers each reviewed all titles retrieved from the initial searches. Duplicates were eliminated, and if possible, using the available abstracts, each reviewer decided its inclusion. If the paper could not be included or excluded with certainty on the basis of the abstract, then the full text was read. Any disagreements between reviewers on papers’ eligibility were resolved by discussion or, if necessary, arbitration by a senior author. If an RCT had been reported by more than one publication, the last publication which reported the trial was used as the reference publication in this review.
Data Items
The following variables were recorded: study information (first author, publication year, and country of origin); participant information (total patients, sex, median/mean age); intervention information where available (prone positioning adjuncts, length of time spent in a prone position, head rotation frequency, eye care provided); and follow-up information (mean and median follow-up duration, planned follow-up period, and how many study participants completed follow-up).
The following outcome data were sought: whether ocular injury data were reported as present or absent; number or proportion of participants in each intervention arm with ocular injuries; injury type; laterality and any patient-reported outcomes available. If further information was required, then individual study authors were contacted with a return period of 30 days.
Risk of Bias in Individual Studies and Across Studies
Two authors independently assessed the potential bias using the Cochrane Collaboration bias tool.16
Summary Measurements and Synthesis of Results
The rates of ocular injury were shown as crude rates and, if appropriate, mean scores, for example, who diagnosed the ocular injury and how and when may vary in relevant ways between studies.
Meta-Analysis
Meta-analysis was performed for rates of injury overall and for each distinct injury type if there were 2 or more RCTs which examined the same injury type. The outcome groups were divided into supine positioning and prone positioning, with subdivisions into specific prone positioning pressure relief adjuncts if sufficient data were available (2 or more homologous studies).
Review Manager 5 software (Nordic Cochrane Center, Copenhagen, Denmark) was used for results synthesis.17 If the outcome data were presented in the form of dichotomous categorical variables, ORs would be reported with corresponding 95% confidence intervals (CI). Statistical heterogeneity between studies was checked and reported using the I2 measure of study heterogeneity. If low heterogeneity (I2: <50%) between studies was reported, then a fixed effect model was used. If higher heterogeneity was displayed, then a random effects model was used. If a meta-analysis displayed a heterogeneity of >75%, it was excluded from the results.18 , 19
The primary summary measurement (rate of ocular injuries) of the meta-analysis was given as an OR with 95% CI. If there was a zero-cell count for any given event, then Review Manager 5 software automatically added a 0.5 continuity correction. A sensitivity analysis was also undertaken. Only studies in which the majority of areas (4 or more) of potential bias were low risk would be analyzed and presented in this analysis.
RESULTS
Study Characteristics
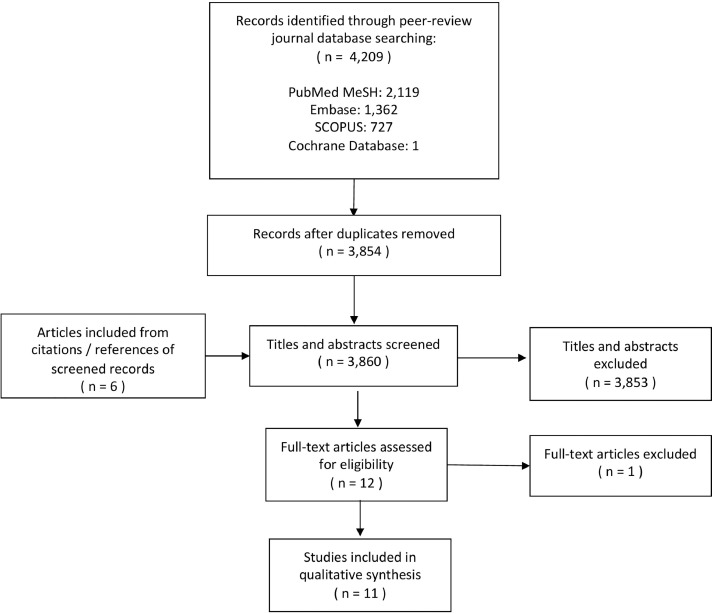
Twelve studies met inclusion criteria. Two studies had included the same participants, resulting in 11 studies with unique populations.1, 2, 3, 4, 5 , 20, 21, 22, 23, 24, 25 The PRISMA flow diagram of search results is presented in Figure 1 .
Figure 1.
PRISMA flow diagram of study selection. A total of 11 studies were included in the end quantitative synthesis. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
There were 2,247 randomly assigned patients included in this analysis (1,089 patients underwent supine positioning only, and 1,158 patients were randomized to receive prone positioning). Length of follow-up reporting heterogeneous. Study details are included in Table 1 .
TABLE 1.
Study and Patient Characteristics of Included Studies
| Study (ref), y | Location | Patient Group | Males/Females | Age Mean/Median ± SD, y | Number Prone | Number Supine | Mean Length of Follow-Up, Days Supine/Prone |
|---|---|---|---|---|---|---|---|
| Gattinoni (1), 2001 | Italy | ALI or ARDS | 214.0/90.0 | Prone: 57 ± 16 Supine: 59 ± 17 |
152.0 | 152.0 | 10/10 |
| Watanabe (20), 2002 | Japan | Post-esophagectomy | 14.0/2.0 | Prone: 66 ± 5.8 Supine: 63 ± 8.1 |
8.0 | 8.0 | Not available |
| Beuret (21), 2002 | France | Patients requiring intubation because of GCS <9.0 | 36.0/15.0 | Prone: 55 ± 19 Supine: 55 ± 20 |
25.0 | 26.0 | Not available |
| Guérin (2), 2004 | France | Acute respiratory failure | 593.0/198.0 | Prone: 62 ± 15.7 Supine: 62.5 ± 14.7 |
413.0 | 378.0 | 24.5/26.9 |
| Papazian (22), 2005 | France | ARDS | 23.0/16.0 | Prone: 51 ± 10.5 Supine: 55 ± 15 |
26.0 | 13.0 | Not available |
| Voggenreiter (23), 2005 | Germany | Trauma patients with ALI or ARDS | 33.0/7.0 | Prone: 40 ± 14 Supine: 43 ± 10 |
21.0 | 19.0 | Not available |
| Mancebo (3), 2006 | Spain | ARDS | 86.0/50.0 | Prone: 54 ± 17 Supine: 54 ± 16 |
76.0 | 60.0 | Not available |
| Chan (24), 2007 | Taiwan | CAP | 18.0/4.0 | Prone: 54.7 ± 21.8 Supine: 69 ± 15.5 |
11.0 | 11.0 | 3.0/3.0 |
| Fernandez (25), 2008 | Spain | ARDS | 25.0/15.0 | Prone: 53.9 ± 17.9 Supine: 55.3 ± 14.6 |
21.0 | 19.0 | 17.5/14.7 |
| Taccone (4), 2009 | Italy | ARDS | 246.0/96.0 | Population: 60 ± 16 |
168.0 | 174.0 | 28.0/28.0 |
| Guérin (5), 2013 | France | ARDS | 318.0/148.0 | Prone: 58 ± 16 Supine: 60 ± 16 |
237.0 | 229.0 | 26.0 (18.0 non-survivors)/ 24.0 (21.0 non-survivors) |
ALI = acute lung injury; ARDS = acute respiratory distress syndrome; CAP = community-acquired pneumonia; GCS = Glasgow coma scale.
Patient Characteristics
All studies reported patient sex. When the 11 studies were pooled, 641 patients (28.5%) were female patients. The mean ± SD ages of study participants were reported in all studies, ranging from 40 ± 14 to 66 ± 5.8 years in the prone group and 43 ± 10 to 69 ± 15.5 years in the supine group.
Risk of Bias Within Studies
An individual risk of bias analysis for each study is presented in Table 2 . In the case of Beuret and associates,21 although physiological endpoint data assessments were not blinded, as subjective as chest radiographs were, the authors still elected to place this study's blinding of outcome assessment in the negative category. The study by Guérin and associates2 was the only study to report full outcome assessment blinding. Allocation concealment and randomization methodology was unclear for most of the studies, with Chan and associates, 2007, appearing to have been quasi-randomized by the study author.24 Three studies reported adequate randomization and allocation concealment in full.2, 3, 4 The authors found those 3 studies had a minimal risk of bias in most areas so proceeded to a sensitivity analysis including those studies, as reported below.
TABLE 2.
Cochrane Risk of Biasa
| Study (ref), y | Random Sequence Generation (Selection Bias) | Allocation Concealment (Selection Bias) | Blinding of Participants and Personnel (Performance Bias) | Blinding of Outcome Assessment (Selection Bias) | Incomplete Outcome Data (Attrition Bias) | Selective Reporting (Reporting Bias) |
|---|---|---|---|---|---|---|
| Gattinoni (1), 2001 | + | ? | − | − | + | + |
| Watanabe (20), 2002 | ? | ? | − | − | + | + |
| Beuret (21), 2002 | ? | ? | − | − | + | + |
| Guérin (2), 2004 | + | + | − | + | + | + |
| Papazian (22), 2005 | ? | ? | − | − | + | + |
| Voggenreiter (23), 2005 | + | ? | − | − | + | + |
| Mancebo (3), 2006 | + | + | − | − | + | + |
| Chan (24), 2007 | ? | ? | − | − | + | + |
| Fernandez (25), 2008 | + | ? | − | − | + | + |
| Taccone (4), 2009 | + | ? | − | − | + | + |
| Guérin (5), 2013 | + | + | − | − | + | + |
All studies were found satisfactory in all areas of assessment.
+ = XXX; ? = XXX; − = XXX.
Ocular Injuries
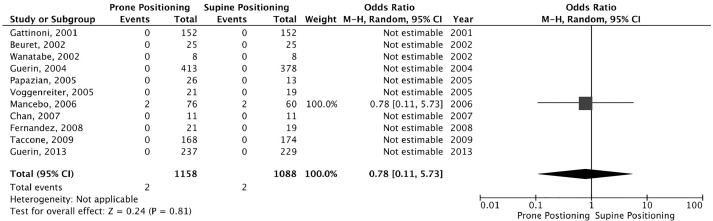
Three of the 11 studies reported ocular injuries, including 1 study reporting subconjunctival hemorrhage and 2 studies reporting eye (chemosis) or eyelid edema. Those occurrences of edema were included in an initial meta-analysis but were excluded from a subgroup analysis because transient dependent facial edema is anecdotally a common feature of prone positioning. Three studies reported ocular findings, with 8 of 11 studies reporting no events in either trial arm. The crude rate of eye injury across all 11 studies consisted of 15 events among 1,158 patients (1.30%) in the prone group and 13 of 1,089 patients (1.19%) in the supine group, which were reduced to 2 of 1,158 patients (0.17%) and 2 of 1,089 patients (0.18%), respectively, when reports of edema were removed. Meta-analysis demonstrated no significant differences between ORs in the supine group and ORs in the prone groups (OR: 1.40; 95% CI: 0.37–5.27) (Figure 2 ). Similarly, no differences were demonstrated when patients with reported edema were removed. An OR of 0.78 (95% CI: 0.11–5.73) (Figure 3 , Table 3 ) was the rate of ocular injuries reported in the included studies.
Figure 2.
Forest plot analysis of all ocular injuries recorded across the study populations. There were nonsignificant differences shown between groups. OR: 1.02 (95% CI: 0.82–1.26).
Figure 3.
Forest plot analysis of all ocular injuries, excluding eye and/or eyelid swelling, recorded across the study populations. There were non-significant difference shown between groups. OR: 0.79 (95% CI: 0.11–5.44).
TABLE 3.
Ocular Injuries Recorded in Each of the Included StudiesXXX
| Study (ref), y | Ocular Injury Recorded | Injury Type | Supine | Prone |
|---|---|---|---|---|
| Gattinoni (1), 2001 | None recorded | – | – | – |
| Watanabe (20), 2002 | Yes | Eyelid edema | 8 | 8 |
| Beuret (21), 2002 | None recorded | – | – | – |
| Guérin (2), 2004 | None recorded | – | – | – |
| Papazian (22), 2005 | None recorded | – | – | – |
| Voggenreiter (23), 2005 | None recorded | – | – | – |
| Mancebo (3), 2006 | Yes | Subconjunctival hemorrhage | 2 | 2 |
| Chan (24), 2007 | Yes | Chemosis “eye swelling” | 3 | 5 |
| Fernandez (25), 2008 | None recorded | – | – | – |
| Taccone (4), 2009 | None recorded | – | – | – |
| Guérin (5), 2013 | None recorded | – | – | – |
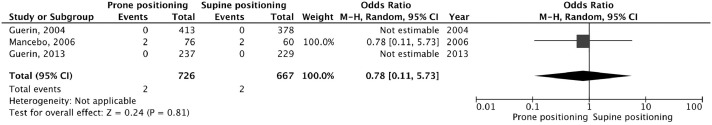
Following sensitivity analysis, no significant differences were found between the prone group, consisting of 2 of 726 patients (0.275%) or the supine group, consisting of 2 of 667 patients (0.300%; OR: 0.78; 95% CI: 0.11–5.73 for both groups) (Figure 4 ). Only 1 of the 3 studies in the sensitivity analysis reported ocular findings (Table 3).3
Figure 4.
Forest plot analysis of all ocular injuries recorded across studies assessed as having a low risk of bias. There were non-significant differences shown between groups. OR: 0.79 (95% CI: 0.11–44).
Each author was contacted and asked for additional information regarding ocular injuries if not reported; authors Guérin and Beuret kindly replied, with no additional information to add.
DISCUSSION
This systematic review and meta-analysis of ocular injury in supine versus prone patients contained 11 unique RCTs. Comparisons were made with all reported ocular injuries and with edema removed, as transient dependent facial edema is anecdotally expected on pronation. When prone versus supine positioning was reported, there was a nonsignificant difference between rates of ocular injuries between the groups. The crude rates of eye injury across all studies, including 15 of 1,158 patients (1.30%) in the prone group and 13 of 1,089 patients (1.19%) in the supine group, which were reduced to 2 of 1,158 patients (0.17%) and 2 of 1,089 patients (0.18%), respectively, when reports of edema were removed. Of note, only 3 studies reported ocular injury, which was reduced to 1 study following removal of eyelid edema and chemosis. The remaining ocular injuries were cases of subconjunctival hemorrhage.
Prior to this review, the risk profile of ocular injury during general anesthesia has been well characterized, with the largest single center study (75,120 non-ocular procedures) reporting a perioperative ocular injury incidence of 0.023% and 0.080% in the prone group, respectively, with patients having been operated on in the prone position at an increased risk of injury (OR: 10.8; 95% CI: 2.4–48.8).26 This poses a discrepancy with the results of the present study, in which incidence rates of 0.17% and 0.18% in prone and supine positions, respectively, were found in critical care patients. Speculatively, a higher incidence in a critical care settings compared to general anesthesia may be because of the prolonged corneal and/or conjunctival exposure time associated with critical care as opposed to procedural general anesthesia.
Previous studies specifically regarding ocular injury following prone positioning in critical care or general anesthesia, however, are limited. Population-based epidemiological studies of the rate of post-operative vision loss following prone spinal surgery showed an incidence of 0.094%, with risk factors, including hypotension, anemia, pre-existing peripheral vascular disease, and pediatric (<18 years old) and geriatric (>84 years old) age for development of vision loss.27 , 28 Loss of vision was not an outcome in this study of the incidence of ocular injury, nor was it reported by any of the included studies.
The present study was constrained by both the lack of ocular assessment for injury as a study endpoint and the limited follow-up period present in these critical care studies, as ocular structural injury may not be evident within the patients’ index hospital admission. Lack of personnel and observer blinding (with only 1 study reporting outcome assessment blinding) were highlighted by the Cochrane Risk of Bias tool; however, the authors acknowledge that pragmatically these would be difficult.2 The randomization process and allocation concealment for several studies was unclear. In addition, only 1 study reported full outcome assessor blinding. This prompted the authors to conduct a sensitivity analysis which included the 3 studies which displayed a minimal risk of bias in most (4 or greater) areas.2 , 3 , 5 This analysis again showed no significant differences between the prone and supine groups, with or without reports of eye or eyelid edema (RR: 0.79; 95% CI: 0.11–5.44) for both groups.
The authors highlight the fact that these results, although conducted to minimize bias, represent data from only 1 study, with the 2 other studies in the sensitivity analysis reporting no data in each study arm. The authors were also prompted to reflect that the study which reported ocular findings had a sample size of 136, whereas the additional 2 studies had a combined sample size of 1,257 participants without reported ocular events. This may indicate the underreporting of ocular injury as an adverse event. Although there is no indication of bias toward supine or prone positioning groups, this observation likely highlights the key deficiency of this study.
To advance this observation, when the studies included in this review were observed as a whole, it is notable that only 3 of 11 studies contained events.3 , 20 , 24 In these studies, the event rates for supine patients (3.33%–100%) and prone patients (3.33%–100%) were greater than those recorded by the review population as a whole. When the authors reviewed the outcome definitions for each of the included studies, they noted that 7 studies specifically mentioned pressure injuries either in the outcome sections of their methodology or results.1, 2, 3 , 20 , 21 Those which did not included the study by Taccone and associates,4 who stated that they would record adverse events relating to remaining in the prone position; Guérin and associates5; Fernandez and associates25; and Papazian and associates,22 who included “complications” as an outcome. None of the included studies included ocular injuries as a specific endpoint in their methodology. This observation highlights the need for ocular injuries as an endpoint in future critical care trials.
Further investigation of the longer-term effects of prone positioning is recommended, with an increased cohort of patients post-prone positioning expected following the COVID-19 pandemic. Clinical recommendations in critical care, beyond the implementation of recommendations of the FICM guidelines, are limited.6 However, the authors recommend that these observation that ocular injuries do occur in critical care, and at a higher rate than in cases of general anesthesia, guides the provision of critical follow-up and post-admission patient guidance.
This meta-analysis of RCTs showed that there was no differences in the rate of ocular injury between prone and supine patient groups in adult critical care. However, the rate of ocular injury was increased compared to general anesthesia, which was displayed. The authors acknowledge that this is a meta-analysis of studies which did not include ocular injury as an endpoint, so the rate of sustained ocular injury may be greater than reported by this study. The authors recommend that this study be used to guide future critical care follow-up services and to prompt further outcome studies and raise awareness of the need for meticulous ocular care in the critical care environment.
Acknowledgments
ALL AUTHORS HAVE COMPLETED AND SUBMITTED THE ICMJE FORM FOR DISCLOSURE OF POTENTIAL CONFLICTS OF INTEREST and none were reported.
Funding Support: None. Financial Disclosures: The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
(Ocular Injury Associated With Prone Positioning In Adult Critical Care: A Systematic Review And Meta-Analysis [CRD42020196917]; PROSPERO; University of York, York, UK)
References
- 1.Gattinoni L, Tognoni G, Pesenti A, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001;345(8):568–573. doi: 10.1056/NEJMoa010043. [DOI] [PubMed] [Google Scholar]
- 2.Geurin C, Gaillard S, Lemasson S. Effects of systematic prone positioning in hypoxaemic acute respiratory failure. JAMA. 2004;292(19):2379–2387. doi: 10.1001/jama.292.19.2379. [DOI] [PubMed] [Google Scholar]
- 3.Mancebo J, Fernández R, Blanch L., et al. A Multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;173(11):1233–1239. doi: 10.1164/rccm.200503-353OC. [DOI] [PubMed] [Google Scholar]
- 4.Taccone P, Pesenti A, Latini R, et al. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2009;302(18):1977–1984. doi: 10.1001/jama.2009.1614. [DOI] [PubMed] [Google Scholar]
- 5.Guérin C., Reignier J., Richard JC, et al. for the PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 6.Faculty of Intensive Care Medicine . 2019. Prone Position in Adult Critical Care.https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf Available at. Accessed June 4, 2020. [Google Scholar]
- 7.Grixti A, Sadri M, Datta AV. Uncommon ophthalmologic disorders in intensive care unit patients. J Crit Care. 2013;27(6) doi: 10.1016/j.jcrc.2012.07.013. 746.e9–22. [DOI] [PubMed] [Google Scholar]
- 8.Stambough JL, Dolan D, Werner R, Godfrey E. Ophthalmologic complications associated with prone positioning in spine surgery. J Am Acad Orthop Surg. 2007;15(3):156–165. doi: 10.5435/00124635-200703000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Woodruff C, English M, Zaouter C, et al. Postoperative visual loss after plastic surgery: case report and a novel continuous real-time video monitoring system for the eyes during prone surgery. Br J Anaesth. 2011;106(1):149–151. doi: 10.1093/bja/aeq349. [DOI] [PubMed] [Google Scholar]
- 10.Saran S, Gurjar M, Kanaujia V, et al. Effect of prone positioning on intraocular pressure in patients with acute respiratory distress syndrome. Crit Care Med. 2019;47(9):e761–e766. doi: 10.1097/CCM.0000000000003893. [DOI] [PubMed] [Google Scholar]
- 11.Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic's front line. N Engl J Med. 2020;382(20):1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 12.Kwee M, Ho Y-H, Rozen W. The prone position during surgery and its complications: a systematic review and evidence-based guidelines. Int Surg. 2015;100(2):292–303. doi: 10.9738/INTSURG-D-13-00256.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.PRISMA Statement and Checklist. 2009. Available at: http://www.prisma-statement.org/. Accessed June 4, 2020.
- 14.Prospero Systematic Review Database. 2020. Available at: https://www.crd.york.ac.uk/prospero/. Accessed June 4, 2020.
- 15.Inspection Framework: NHS Acute Hospitals. 2016. Available at: https://www.cqc.org.uk/sites/default/files/20160713_NHS_core_service_inspection_framework_critical_care.pdf. Accessed June 4, 2020.
- 16.Cochrane Risk of Bias Tool. Cochrane Collaboration. Available at: https://handbook-5-1.cochrane.org/chapter_8/8_assessing_risk_of_bias_in_included_studies.htm. Accessed June 4, 2020.
- 17.Review Manager 5. Cochrane Collaboration. Available at: https://community.cochrane.org/help/tools-and-software/revman-5. Accessed November 4, 2018.
- 18.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 19.Demets DL. Methods for combining randomized clinical trials: strengths and limitations. Stat Med. 1987;(3):341–350. doi: 10.1002/sim.4780060325. [DOI] [PubMed] [Google Scholar]
- 20.Watanabe I, Fujihara H, Sato K, et al. Beneficial effect of a prone position for patients with hypoxemia after transthoracic esophagectomy. Crit Care Med. 2002;30(8):1799–1802. doi: 10.1097/00003246-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Beuret P, Carton MJ, Nourdine K, Kaaki M, Tramoni G, Ducreux JC. Prone position as prevention of lung injury in comatose patients: a prospective, randomized, controlled study. Intensive Care Med. 2002;28(5):564–569. doi: 10.1007/s00134-002-1266-x. [DOI] [PubMed] [Google Scholar]
- 22.Papazian L, Gainnier M, Marin V, et al. Comparison of prone positioning and high-frequency oscillatory ventilation in patients with acute respiratory distress syndrome. Crit Care Med. 2005;33(10):2162–2171. doi: 10.1097/01.ccm.0000181298.05474.2b. [DOI] [PubMed] [Google Scholar]
- 23.Voggenreiter G, Aufmkolk M, Stiletto RJ, et al. Prone positioning improves oxygenation in post-traumatic lung injury—a prospective randomized trial. J Trauma. 2005;59(2):333–343. doi: 10.1097/01.ta.0000179952.95921.49. [DOI] [PubMed] [Google Scholar]
- 24.Chan MC, Hsu JY, Liu HH, et al. Effects of prone position on inflammatory markers in patients with ARDS due to community-acquired pneumonia. J Formos Med Assoc. 2007;106(9):708–716. doi: 10.1016/S0929-6646(08)60032-7. [DOI] [PubMed] [Google Scholar]
- 25.Fernandez R, Trenchs X, Klamburg J, et al. Prone positioning in acute respiratory distress syndrome: a multicenter randomized clinical trial. Intensive Care Med. 2008;34(8):1487–1491. doi: 10.1007/s00134-008-1119-3. [DOI] [PubMed] [Google Scholar]
- 26.Yu HD, Chou AH, Yang MW, Chang CJ. An analysis of perioperative eye injuries after nonocular surgery. Acta Anaesthesiol Taiwan. 2010;48(3):122–129. doi: 10.1016/S1875-4597(10)60043-4. [DOI] [PubMed] [Google Scholar]
- 27.Epstein N. Perioperative visual loss following prone spinal surgery: a review. Surg Neurol Int. 2016;7(13):347–360. doi: 10.4103/2152-7806.182550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patil CG, Lad EM, Lad SP, Ho C, Boakye M. Visual loss after spine surgery: a population-based study. Spine. 2008;33(13):1491–1496. doi: 10.1097/BRS.0b013e318175d1bf. [DOI] [PubMed] [Google Scholar]