ABSTRACT
Human Papillomavirus (HPV) causes almost all cervical cancers and many cancers of the anus, vagina, vulva, penis, and oropharynx. The HPV vaccine provides protection to all adolescents from a broad spectrum of cancers, yet HPV vaccination rates remain lower than those of other routine vaccines. Developing effective HPV vaccine interventions is particularly important in rural areas, whose residents have lower rates of HPV vaccination and higher cervical cancer incidence and mortality; however, interventional research in these populations is relatively limited. Furthermore, though rural areas are heterogeneous in many regards, few interventions engage stakeholders to develop community-specific solutions to overcome obstacles associated with HPV vaccination. Based on a review of existing literature, we recommend a multicomponent peer-based approach that includes school-based vaccination and awareness, parental involvement, and stakeholder engagement to increase HPV vaccination in rural areas, and we provide an example of such an intervention in rural Vermont.
KEYWORDS: HPV vaccine, rural health, vaccine intervention, peer education, school-based vaccination, parents, stakeholders
Introduction
Human Papillomavirus (HPV) causes most cervical and anal cancers and many cancers of the vagina, vulva, penis, and oropharynx. The HPV vaccine is the only vaccine that prevents multiple types of cancer, and yet, over a decade after its inclusion in the Advisory Committee on Immunization Practices (ACIP) recommendations for all adolescents, HPV vaccination rates in the United States remain lower than those of most other routine vaccines.
Developing effective and appropriate strategies to reach rural, often underserved, populations is particularly important to reducing overall morbidity and mortality associated with HPV. Compared with urban populations, rural communities have lower rates of adolescent HPV vaccination and higher rates of cervical cancer incidence and mortality, particularly in Black, Indigenous, and People of Color (BIPOC) women.1,2
This may in part be explained by unique barriers to HPV vaccination in rural communities, including parent or guardian characteristics. Older ages of caregivers in rural communities is associated with lower likelihood of initiating and completing HPV vaccination, perhaps due to differing attitudes about sexual health or knowledge of HPV vaccination among generations.3,4 Additionally, rural guardians may perceive that transportation issues will make multiple HPV vaccination appointments inaccessible, independent of intent to vaccinate.4
Lack of consistent and reliable access to broadband internet may also be a barrier to HPV vaccination in rural areas.5 This communication gap can prevent adolescents and their caregivers from learning about HPV or the HPV vaccine, since social media can increase HPV vaccine-related knowledge and awareness.6 Additionally, lack of broadband internet access can block or impede healthcare providers from accessing the state immunization registry, which many physicians use to monitor HPV vaccinations.5,7
Residents of rural areas also share wider challenges to HPV vaccination with their non-rural counterparts, including barriers associated with healthcare equity. In general, higher HPV vaccine uptake is associated with healthcare access metrics such as having health insurance, more healthcare utilization, receipt of childhood vaccines, and having a healthcare provider as a source of information.8 Adolescents (and adults) in rural areas have limited access to consistent healthcare appointments, both due to a shortage of providers and to long travel distances to care.
Rural healthcare inequities also extend to provider communication and clinical decision support, which may increase HPV vaccination.9,10 Many rural adolescents do not have “medical homes,” instead only seeing providers for sick visits or sports physicals.5 Thus, young people in rural areas may have fewer opportunities to be offered vaccination against HPV.11,12 Indeed, people who live in rural areas receive fewer recommendations about HPV vaccination, particularly if they are BIPOC, lower income, uninsured, or living in southern areas.13,14
Lack of HPV knowledge is a significant barrier to HPV vaccination, both within rural communities and without. Residents of rural areas are less likely to know about HPV or its association with cervical cancer compared to their non-rural counterparts.4,15,16 A pilot study conducted in rural Florida exploring parental knowledge and hesitancy of HPV vaccination found that low levels of knowledge about HPV vaccination was associated with low uptake of the vaccine.17
Stigma associated with HPV negatively impacts parents’ decisions about whether to vaccinate their children against HPV.18,19 Parents are often concerned that vaccination against an STI will result in disinhibition of sexual behavior.4,19,20 Worryingly, 80% of rural Floridian parents in the abovementioned study had a different fear: that HPV vaccination could leave their child sterile, a concern that, unsurprisingly, perpetuated HPV vaccine hesitancy.17
Though residents of rural areas bear a disproportionately high HPV disease burden, HPV interventional research in these communities is relatively limited, underscoring the need to identify appropriate strategies that address rural barriers to HPV vaccination.21 Additionally, most HPV interventions lack stakeholder engagement, which may result in failure to understand community-specific barriers to HPV vaccination.22 Rural communities are not uniform and present differing challenges such as geographic location, sociodemographic factors, and values, resulting in unique barriers to HPV vaccination and the need for locally appropriate solutions.4
Barriers to HPV vaccination in Lamoille County, Vermont
Lamoille County is a rural community in northern Vermont. A significant determinant of health in Lamoille County is healthcare access. The Vermont Department of Health (VDH) Behavioral Risk Factor Surveillance System (BRFSS) 2018 report found that among Vermonters, Lamoille County adults are the least likely to have had a doctor’s visit in the last year, as depicted in Figure 1.23s
Figure 1.
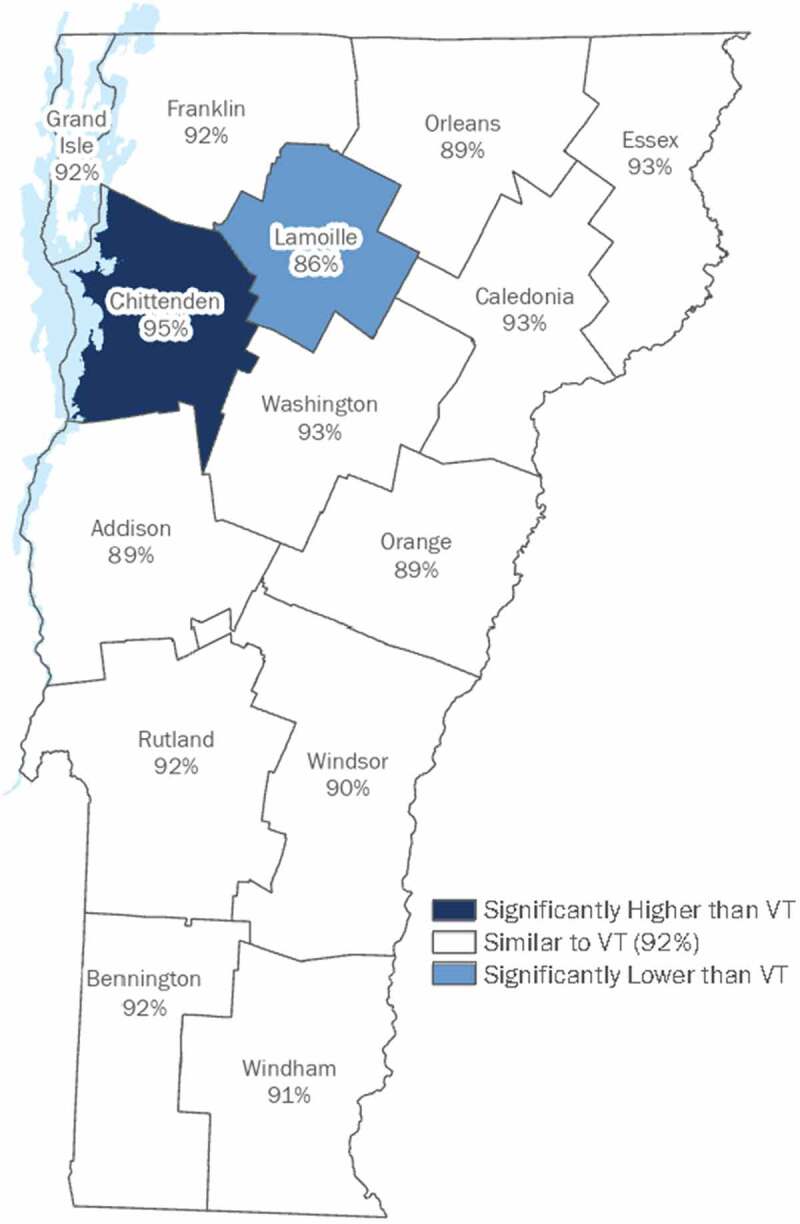
Vermont adults who had a routine doctor visit in the last year by County, 2017–2018. Figure from VDH, BRFSS, 2018 report23.
Lamoille County’s decreased healthcare access also extends to adolescent well-care and cancer prevention. Lamoille County has one of the lowest pediatrician-to-child ratios in Vermont, as shown in Figure 2.24s
Figure 2.
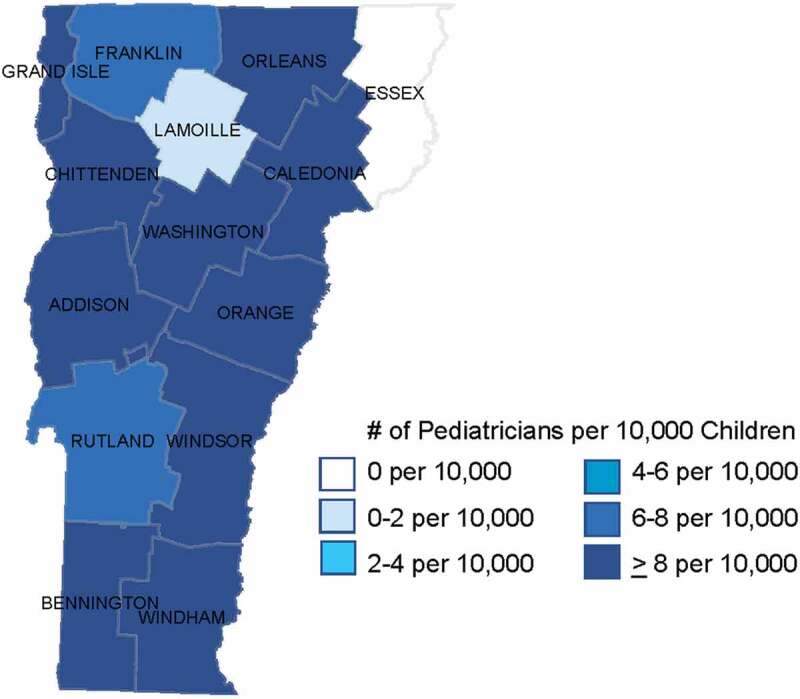
General pediatricians by county in Vermont. Figure adapted from American Board of Pediatrics, US Map of General Pediatricians by County24.
Furthermore, only 48.1% of Lamoille County youth aged 15 have completed their HPV vaccine series, compared with over 60% of 15-year-olds in other Vermont counties, depicted in Table 1.25 Notably, the five Vermont counties with the lowest rates of HPV vaccine series completion are all rural areas.
Table 1.
HPV vaccine series completion – Vermont teens born in 2005, by County. Data from Vermont IMR Annual Report, 202025.
| Vermont County | HPV Series Completion (% of youth aged 15) |
|---|---|
| Addison | 62.5 |
| Orange | 60.9 |
| Chittenden | 57.4 |
| Grand Isle | 55.9 |
| Washington | 55.7 |
| Franklin | 54.7 |
| Orleans | 53.6 |
| Statewide | 53.3 |
| Rutland | 51.7 |
| Windsor | 49.5 |
| Lamoille | 48.1 |
| Caledonia | 46.6 |
| Bennington | 45.9 |
| Windham | 45.1 |
| Essex | 29.9 |
Community stakeholder input
Lamoille County community stakeholders were engaged to provide input regarding local barriers to HPV vaccination and opportunities to overcome them. Stakeholders included school administrators, teachers, school nurses, local healthcare providers, members of community health organizations, high school coaches, and parents. Due to limitations presented by the COVID-19 pandemic, stakeholder meetings were held via telephone or video call. All stakeholder participation was entirely voluntary and self-directed.
Stakeholder input provided insight regarding Lamoille County identity including parental concerns, trusted local organizations, and values. Stakeholders also served as local partners, engendering community support and buy-in critical to creating an intervention centered on potentially sensitive topics including sexually transmitted infections (STIs) and vaccine hesitancy.
Initial stakeholder conversations were specifically focused on identifying local barriers to HPV vaccination in Lamoille County. The following is a list of community stakeholder-identified barriers to HPV vaccination and a select stakeholder quotation:
Lack of information about HPV
Insufficient sexual health education
Infrequent well-child visits
Limited access to primary care providers
Gender stereotypes (“in our community, the gender roles are very much in place”)
Lamoille County stakeholder perspectives on sexual health education
Another significant topic of stakeholder discussion involved determination of the extent to which sexual health should be emphasized in a local HPV vaccine intervention. Most literature and HPV prevention organizations suggest that presenting HPV as cancer prevention with minimal or no mention of HPV’s sexual transmission is the most effective strategy to improve vaccination, likely to mitigate parental concern that vaccination against an STI may increase sexual behaviors.26,27
However, Lamoille County community stakeholders identified that insufficient sexual health education was a significant barrier to HPV vaccination in their community, as listed above. Stakeholders were most concerned about STI prevention and curriculum inclusivity of lesbian, gay, bisexual, transgender, queer/questioning (LGBTQ) adolescents. When apprehension of parent receptivity was raised, stakeholders held steadfast in their belief that HPV vaccine intervention would not be effective in Lamoille County without also addressing inadequate sexual health education in the broader community.
The “Guard Your Health” intervention
Based on stakeholder-identified barriers to HPV vaccination in Lamoille County and a review of the literature, the primary author developed the “Guard Your Health” intervention, which contained the elements described herein.
The intervention centered around the Guard Your Health fair, named for Gardasil 9, the 9-valent HPV vaccine distributed in the United States. The fair was offered to three schools (a high school, a middle school, and a technical school for 10–12th grade students) that share a campus in Lamoille County. Select characteristics of the students at the high school (N = 486) and middle school (N = 283) are provided in Table 2; population data was not provided for the technical school.28
Table 2.
Student characteristics, provided as percentages of students, Data from State of Vermont Agency of Education, Vermont Education dashboard28.
| Lamoille County High School |
Lamoille County Middle School |
Vermont Schools | |
|---|---|---|---|
| Race/Ethnic Group | |||
| White | 96.91 | 95.41 | 88.74 |
| Hispanic | 1.65 | 1.06 | 2.63 |
| Black | 1.03 | 1.41 | 2.51 |
| Asian | 0.21 | 0.35 | 2.21 |
| Multi-Racial | 0.21 | 1.41 | 3.47 |
| Native Hawaiian/Pacific Islander | 0.13 | ||
| American Indian/Alaskan Native | 0.35 | 0.3 | |
| Family Income | |||
| Free or Reduced Lunch | 42.18 | 40.28 | 34.46 |
| Student Support Services | |||
| 504 Plan | 8.64 | 4.95 | 4.69 |
| Education Support Team | 15.23 | 20.14 | 6.4 |
Peer-based education
Peer-based education was the central educational strategy of the Guard Your Health intervention.
Based on conversations with stakeholders, it was determined that educational topics at the fair would include but extend beyond HPV in order to improve parental reception, particularly due to middle school student involvement. Thus, using student interests and community concerns identified by stakeholders, the following categories were selected for inclusion at the Guard Your Health fair:
Category 1: HPV and sexual health
Category 2: Disease prevention
Category 3: Healthcare and emergency response
Category 4: Vaping cessation
Three students identified by high school teachers (“youth stakeholders”) provided peer education related to Categories 1 and 2. Ten students from the technical school’s health program and one recent graduate of the program developed interactive booths related to Category 3, including airway management, splinting, wound dressing, taking vitals, disposable glove donning and doffing technique, using an automated external defibrillator (AED), abdominal thrust (Heimlich maneuver), and blood donation.
The only exception to peer teaching was in the case of one student who was not able to be at their booth for the entire duration of the Guard Your Health fair. This student was a youth member of Healthy Lamoille Valley, a local organization aimed at reducing substance misuse that was cited by stakeholders as a trusted healthcare organization by the community. Thus, it was determined that an adult representative from Healthy Lamoille Valley would support peer teaching at the fair in the context of Category 4, as youth vaping cessation was routinely cited by stakeholders as a significant community concern. The students who served as peer teachers at the Guard Your Health fair (hereafter referred to as the “Guard Your Health peer educators”) are summarized in Figure 3.
Figure 3.
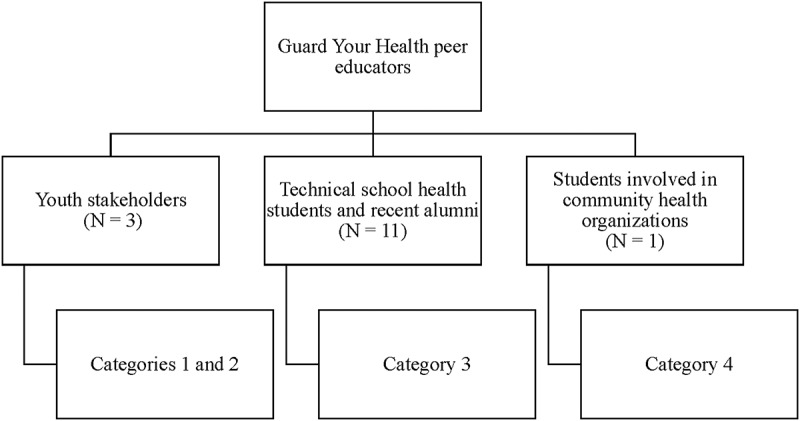
Description of Guard Your Health peer educators.
The fair featured a raffle, where, to enter a ticket, students had to correctly answer questions by learning from the Guard Your Health peer educators or posters made by students during the fair campaign (described below). Stakeholders and youth stakeholders helped identify raffle prizes that would be both motivating and health-promoting to the adolescents in Lamoille County, including an exercise bike, ski lift tickets, and a stand-up paddle board.
Each raffle ticket included four questions and a perforated edge to create a “ticket stub” with a QR code to UnhypedVT.com, a local vaping cessation resource. An example raffle ticket is provided in Figure 4. Guard Your Health peer educators helped develop raffle ticket questions and were encouraged to discuss – either with their peers, teachers, or the primary author – information they would be teaching prior to their fair to ensure their comfort and confidence. A complete list of raffle ticket questions is provided in Appendix A. There were ten sets of raffle tickets and each ticket contained one question from each of the four categories. Only raffle tickets with completely correct answers were eligible for a raffle prize and all students (including the Guard Your Health peer educators) were permitted one ticket each to enter the raffle.
Figure 4.
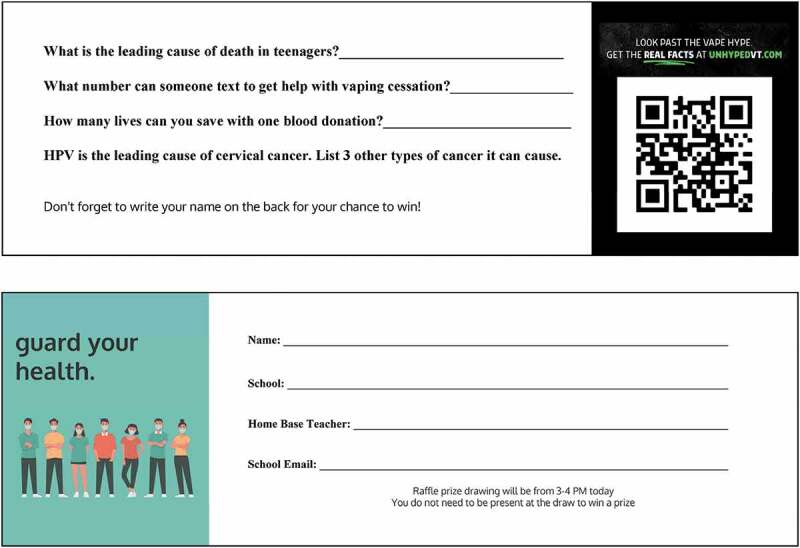
Guard Your Health fair sample raffle ticket.
The fair was held in an event space at the shared campus of the three schools over five hours during a typical school day. Due to capacity limitations of the event space and the COVID-19 pandemic, a sign-up sheet with nine 20- to 30-minute slots, each slot available to a maximum of three classes, was sent to teachers of the three schools prior to the Guard Your Health fair.
School-Based vaccination and awareness
The HPV awareness campaign began a month prior to the Guard Your Health fair with advertisement and promotion. Flyers were hung in hallways and in the school nurses’ office, and classrooms were visited to discuss HPV and the HPV vaccine.
One week before the event, the high school held a remote schoolwide assembly for the students to hear the story of a male teacher at their school who was a survivor of an HPV-associated oropharyngeal cancer.
In his story, the students’ teacher said he didn’t remember anything about his diagnosis, except for the beginning of the appointment, and the end. He remembered the beginning because when he walked in, his doctor was crying. The rest was a blur, he said, but at the end, his doctor told him that there was good news:
The good news was that a vaccine had just been approved for HPV, so no one ever has to go through this again.
School-based HPV vaccination was offered to students by the local Vermont Department of Health office during the Guard Your Health fair. Students with a signed permission slip had the opportunity to receive a single dose of the HPV vaccine series. A nurse practitioner from a Lamoille County healthcare office was present during vaccination to answer questions about vaccine dose scheduling or assuage parental concerns.
Parent or guardian involvement
Prior to the fair, the school nurse sent a letter home to the parents or guardians of the three schools. The letter provided HPV vaccine dosing and scheduling guidelines and recommended that adolescents who received a vaccine at the fair follow up with their primary care provider to ensure completion of the HPV vaccine series. The letter also included HPV educational materials and a consent form for HPV vaccination. Because parents view cancer prevention as the best reason to vaccinate their child against HPV, the letter presented the HPV vaccine as such with no mention of HPV’s sexual transmission.26
Sexual health education
The sexual health curriculum was delivered to four cohorts of 10th grade students at the high school over four 80-minute sessions, with the final day coinciding with the Guard Your Health fair. The sexual health curriculum was developed using materials from the Get Real High School curriculum and in accordance with Vermont’s sexual health guidelines and the Centers for Disease Prevention and Control (CDC) Health Education Curriculum Analysis Tool (HECAT). Based on stakeholders’ perceived limitations of the current health curriculum, highest emphasis was placed on STI prevention and de-stigmatization of sexual health, particularly in the context of gender stereotypes.
Local solutions to local problems
The multicomponent Guard Your Health intervention created solutions to address each of the local barriers to HPV vaccination identified by Lamoille County community stakeholders. A summary of barrier-specific solutions provided by the intervention is provided in Figure 5.
Figure 5.
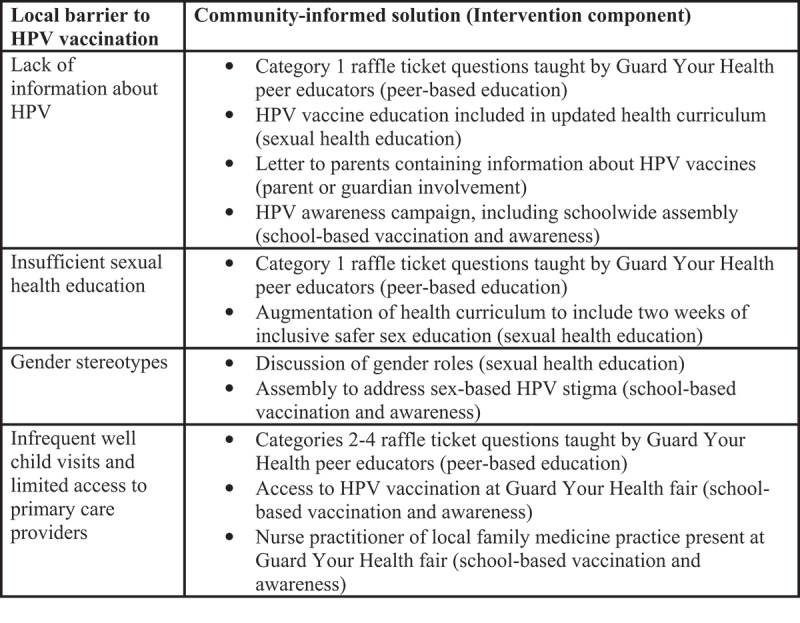
Guard Your Health intervention solutions to Lamoille County stakeholder perceived barriers to HPV vaccination.
The Guard Your Health intervention was very well-received by the Lamoille County community. Almost all Guard Your Health fair raffle prizes were donated by local businesses in support of the intervention. At the fair, over 120 raffle tickets were collected corresponding to nearly 500 questions, the vast majority of which were answered correctly.
Many elements of the Guard Your Health intervention will persist in Lamoille County to support HPV vaccination long-term. For example, the Guard Your Health fair is planned to be an annual event in Lamoille County. Additionally, two of the Guard Your Health peer educators have continued sexual health peer teaching a self-directed project without outside support from the authors. They have taught classes and developed a social media account to educate their peers and normalize discussions of sexual health on an ongoing basis.
Recommendations
Based on our experience with the Guard Your Health intervention, we recommend rural HPV vaccination interventions that include the following components:
Peer-based education
School-based vaccination and awareness
Parent or guardian involvement
Stakeholder engagement
A review of evidence supporting these recommendations and their applicability to rural settings is provided herein.
Peers are an important facilitator of HPV vaccination, particularly in rural areas.4,19 Peer-based education can improve sexual health knowledge, including knowledge regarding HPV and cervical cancer.29–31 Effective peer educators can normalize HPV vaccination while enabling frank and open discussion of stigmatized topics like sexual health. Peer teaching can also take many forms, lending itself to implementation in diverse settings. In a study in rural North Carolina, adolescents who received a peer-to-peer sexual health education program adapted from urban and suburban schools felt that that they learned better from peer education than from traditional health class.32
While peer-based education can result in behavior change related to human immunodeficiency virus (HIV), it might not be sufficient to change other sexual health behaviors.29,31,33 Thus, peer teaching may improve HPV vaccination more effectively if part of a multicomponent strategy.34,35
Providing vaccination is an important feature of many effective HPV interventions.36 Schools play a central role in small rural communities and are a trusted source of information.5 It is unsurprising, then, that school-based programs that offer vaccination are most successful, and those that also raise awareness facilitate HPV vaccination in rural areas.4,35,37 Kaul et al. conducted a study comparing HPV vaccine initiation and completion in rural Texas middle schools that received community-based HPV educational interventions with or without school-based vaccination; students who had access to on-site vaccination were over 3.6 times more likely to initiate and complete HPV vaccination than those who had only received community-based education.38
HPV interventions are particularly distinct from other sexual health programs in that the desired behavioral change (i.e., vaccination in 11- to 12-year-olds) requires consent from a parent or guardian; thus, HPV interventions aimed at increasing vaccination should include parent or guardian involvement. Indeed, interventions that actively engage parents, including education by a healthcare professional, more effectively increase HPV vaccination than those which only focus on adolescents.39
Rural areas are heterogeneous in terms of geographic location, sociodemographic factors, and values, leading to unique barriers to HPV vaccination and the need for locally appropriate interventions.4 Community identity may provide direction regarding certain elements of HPV interventions, including the extent to which sexual health should be emphasized as was the case for the Guard Your Health intervention. Similarly, religion or spirituality may influence parental decision-making regarding HPV vaccination in rural communities, suggesting some HPV interventions may benefit from faith-based interventions.40,41 Grass roots community engagement is particularly important for increasing HPV vaccination in BIPOC populations.39
While multicomponent peer-based approaches should include each of the elements discussed above, they need not be restricted to them. Based on barriers or specific qualities of the target population, interventions may also incorporate other facilitators of HPV vaccination, including providing incentives or creating opportunities for students or parents to personally connect with someone affected by HPV.42–44 Educational film interventions may provide a means for parent or guardian involvement in rural areas with limited access to primary care providers and clinics.45 Additionally, the student-directed sexual health peer teaching that began as a result of the Guard Your Health intervention indicates that social media may be a locally appropriate and effective tool to incorporate into HPV vaccine interventions, particularly as it is known to improve HPV and HPV vaccine knowledge.6
The multicomponent peer-based approach described in this review may prove beneficial beyond the scope of HPV vaccination, such as addressing hesitancy associated with other vaccines, or hesitancy to prioritize disease prevention and survivorship. Jarrett et al. found that multicomponent and dialogue-based interventions, particularly when developed in the context of specific target populations, were most effective at improving uptake of HPV, influenza, and childhood vaccines in vaccine hesitant populations.44 Thus, our approach may be useful for improving non-HPV related vaccine hesitancy, thus addressing an indispensable need in the rising anti-vaccine sentiment associated with the onset of the COVID-19 pandemic.
Summary and conclusion
More than ten years after its inclusion in the ACIP recommendations for all adolescents, HPV vaccination remains suboptimal. Identifying effective solutions to overcome these barriers is paramount to reducing incidence and mortality of cervical, anal, vaginal, vulvar, penile, and oropharyngeal cancers.
This is particularly important in rural areas, which have unique barriers to HPV vaccination and whose residents have lower rates of HPV vaccination and higher rates of cervical cancer incidence and mortality.1,2 Despite this, relatively limited interventional studies have been conducted in rural populations.21
Based on the Guard Your Health intervention in rural Vermont in conjunction with a review of the literature, we recommend a multicomponent peer-based approach that includes school-based vaccination and awareness, parent or guardian involvement, and stakeholder engagement to address barriers associated with HPV vaccination in rural areas.
More HPV interventional research is needed in rural areas. Future studies should aim to evaluate whether the multicomponent peer-based approach described in this review is associated with increased HPV vaccine uptake in rural communities. Ultimately, it is critical to continue to identify and implement effective solutions to address rural barriers to HPV vaccination to reduce morbidity and mortality associated with HPV.
Acknowledgements
We thank Albert Schweitzer Fellowship advisors Nancy Gabriel, Tim Lahey, MD, MMSc, and Molly Rideout, MD for their advice and support throughout the development of the Guard Your Health intervention in Lamoille County. We also thank Ellen Brennan, PhD, of the NNE-CTR Administrative Core for her assistance with manuscript preparation, structuring, and copy-editing. Finally, we especially thank the Lamoille County community stakeholders for their openness and collaboration, and for lending their limited time amid the COVID-19 pandemic.
Appendix.
Appendix A.
Guard Your Health fair raffle ticket questions.
| Category | Questions |
|---|---|
| Category 1: HPV and sexual health |
|
| Category 2: Disease prevention |
|
| Category 3: Healthcare and emergency response |
|
| Category 4: Vaping cessation |
|
*Questions were included on two separate sets of raffle tickets.
Funding Statement
The multicomponent peer-based approach in Lamoille County, Vermont was funded by the Albert Schweitzer Fellowship. The Vermont/New Hampshire Chapter of the Albert Schweitzer Fellowship awards $2,000 to medical and law students for the creation of projects aimed at addressing social determinants of health. Albert Schweitzer Fellowship funding enabled the purchase of educational materials (including Nearpod subscription and purchase of the Get Real High School curriculum), printing (Venngage subscription, banners, signs, and raffle tickets), and a few prizes for the Guard Your Health fair raffle. The majority of raffle prizes were donated as non-financial gifts by local businesses; one community member donated $500, used for the purchase of a raffle prize (an inflatable stand-up paddle board) of the same price. This manuscript was also supported by grant U54 GM115516 from the National Institutes of Health for the Northern New England Clinical and Translational Research (NNE-CTR) network.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Swiecki-Sikora AL, Henry KA, Kepka D.. HPV vaccination coverage among US teens across the rural-urban continuum. J Rural Health. 2019;35(4):1–10. doi: 10.1111/jrh.12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu L, Sabatino SA, White MC. Rural-urban and racial/ethnic disparities in invasive cervical cancer incidence in the United States, 2010-2014. Prev Chronic Dis. 2019;16:E70. doi: 10.5888/pcd16.180447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai D, Ding Q, Bodson J, Warner EL, Kepka D. Factors associated with increased HPV vaccine use in rural-frontier U.S. states. Public Health Nurs. 2016;33(4):283–94. doi: 10.1111/phn.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peterson CE, Silva A, Holt HK, Balanean A, Goben AH, Dykens JA. Barriers and facilitators to HPV vaccine uptake among US rural populations: a scoping review. Cancer Causes Control. 2020;31(9):801–14. doi: 10.1007/s10552-020-01323-y. [DOI] [PubMed] [Google Scholar]
- 5.Fish LJ, Harrison SE, McDonald JA, Yelverton V, Williams C, Walter EB, Vasudevan L. Key stakeholder perspectives on challenges and opportunities for rural HPV vaccination in North and South Carolina. Hum Vaccin Immunother. 2022;18(5):2058264. doi: 10.1080/21645515.2022.2058264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ortiz RR, Smith A, Coyne-Beasley T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum Vaccin Immunother. 2019;15(7–8):1465–75. doi: 10.1080/21645515.2019.1581543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsui J, Vincent A, Anuforo B, Btoush R, Crabtree BF. Understanding primary care physician perspectives on recommending HPV vaccination and addressing vaccine hesitancy. Hum Vaccin Immunother. 2021;17(7):1961–67. doi: 10.1080/21645515.2020.1854603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine. 2012;30(24):3546–56. doi: 10.1016/j.vaccine.2012.03.063. [DOI] [PubMed] [Google Scholar]
- 9.Oh NL, Biddell CB, Rhodes BE, Brewer NT. Provider communication and HPV vaccine uptake: a meta-analysis and systematic review. Prev Med. 2021;148:106554. doi: 10.1016/j.ypmed.2021.106554. [DOI] [PubMed] [Google Scholar]
- 10.Harry ML, Asche SE, Freitag LA, Sperl-Hillen JM, Saman DM, Ekstrom HL, Chrenka EA, Truitt AR, Allen CI, O’Connor PJ, et al. Human papillomavirus vaccination clinical decision support for young adults in an upper midwestern healthcare system: a clinic cluster-randomized control trial. Hum Vaccin Immunother. 2022;18(1):2040933. doi: 10.1080/21645515.2022.2040933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newcomer SR, Freeman RE, Albers AN, Murgel S, Thaker J, Rechlin A, Wehner BK. Missed opportunities for human papillomavirus vaccine series initiation in a large, rural U.S. state. Hum Vaccin Immunother. 2022;18(1):2016304. doi: 10.1080/21645515.2021.2016304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryan G, Ashida S, Gilbert PA, Scherer A, Charlton ME, Kahl A, Askelson N. The use of medical claims data for identifying missed opportunities for HPV immunization among privately insured adolescents in the state of Iowa. J Community Health. 2022. doi: 10.1007/s10900-022-01110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kong WY, Bustamante G, Pallotto IK, Margolis MA, Carlson R, McRee AL, Gilkey MB. Disparities in healthcare providers’ recommendation of HPV vaccination for U.S. adolescents: a systematic review. Cancer Epidemiol Biomarkers Prev. 2021;30(11):1981–92. doi: 10.1158/1055-9965.EPI-21-0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amboree TL, Darkoh C. Barriers to human papillomavirus vaccine uptake among racial/ethnic minorities: a systematic review. J Racial Ethn Health Disparities. 2021;8(5):1192–207. doi: 10.1007/s40615-020-00877-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohammed KA, Subramaniam DS, Geneus CJ, Henderson ER, Dean CA, Subramaniam DP, Burroughs TE. Rural-urban differences in human papillomavirus knowledge and awareness among US adults. Prev Med. 2018;109:39–43. doi: 10.1016/j.ypmed.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 16.Boyd ED, Phillips JM, Schoenberger YM, Simpson T. Barriers and facilitators to HPV vaccination among rural Alabama adolescents and their caregivers. Vaccine. 2018;36(28):4126–33. doi: 10.1016/j.vaccine.2018.04.085. [DOI] [PubMed] [Google Scholar]
- 17.Thomas TL, Caldera M, Maurer J. A short report: parents HPV vaccine knowledge in rural South Florida. Hum Vaccin Immunother. 2019;15(7–8):1666–71. doi: 10.1080/21645515.2019.1600986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zheng L, Wu J, Zheng M. Barriers to and facilitators of human papillomavirus vaccination among people aged 9 to 26 years: a systematic review. Sex Transm Dis. 2021;48(12):e255–62. doi: 10.1097/OLQ.0000000000001407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lacombe-Duncan A, Newman PA, Baiden P. Human papillomavirus vaccine acceptability and decision-making among adolescent boys and parents: a meta-ethnography of qualitative studies. Vaccine. 2018;36(19):2545–58. doi: 10.1016/j.vaccine.2018.02.079. [DOI] [PubMed] [Google Scholar]
- 20.Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14:700. doi: 10.1186/1471-2458-14-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brandt HM, Vanderpool RC, Pilar M, Zubizarreta M, Stradtman LR. A narrative review of HPV vaccination interventions in rural U.S. communities. Prev Med. 2021;145:106407. doi: 10.1016/j.ypmed.2020.106407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flood T, Wilson IM, Prue G, McLaughlin M, Hughes CM. Impact of school-based educational interventions in middle adolescent populations (15-17 yrs) on human papillomavirus (HPV) vaccination uptake and perceptions/knowledge of HPV and its associated cancers: a systematic review. Prev Med. 2020;139:106168. doi: 10.1016/j.ypmed.2020.106168. [DOI] [PubMed] [Google Scholar]
- 23.Vermont Department of Health . Vermont adults who had a routine doctor visit in the last year by county, 2017-2018: Behavioral Risk Factor Surveillance System; 2018 Report. [accessed 2022 Feb 24]. https://www.healthvermont.gov/sites/default/files/documents/pdf/HSVR_2018_BRFSSReport.pdf.
- 24.The American Board of Pediatrics . 2021 County distribution of US-based general pediatricians ever certified by the ABP, age 70 and under. [accessed 2022 Jul 9]. https://www.abp.org/content/us-map-general-pediatricians-county.
- 25.Vermont Department of Health . Human papilloma virus vaccine by age 15, by County. Vaccine coverage 2020: Vermont Immunization Registry Annual Report; 2021. [accessed forthcoming Feb 24].
- 26.Gilkey MB, Zhou M, McRee AL, Kornides ML, Bridges JFP. Parents’ views on the best and worst reasons for guideline-consistent HPV vaccination. Cancer Epidemiol Biomarkers Prev. 2018;27(7):762–67. doi: 10.1158/1055-9965.EPI-17-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perkins RB, Fisher-Borne M, Brewer NT. Engaging parents around vaccine confidence: proceedings from the National HPV Vaccination Roundtable meetings. Hum Vaccin Immunother. 2019;15(7–8):1639–40. doi: 10.1080/21645515.2018.1520592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.State of Vermont Agency of Education . Vermont education dashboard. [Accessed 11 Jul 2022]. https://education.vermont.gov/data-and-reporting/vermont-education-dashboard.
- 29.Sun WH, Miu HYH, Wong CKH, Tucker JD, Wong WCW. Assessing participation and effectiveness of the peer-led approach in youth sexual health education: systematic review and meta-analysis in more developed countries. J Sex Res. 2018;55(1):31–44. doi: 10.1080/00224499.2016.1247779. [DOI] [PubMed] [Google Scholar]
- 30.Sadoh AE, Okonkwobo C, Nwaneri DU, Ogboghodo BC, Eregiea C, Oviawe O, Famuyiwa O. Effect of peer education on knowledge of human papilloma virus and cervical cancer among female adolescent students in Benin City, Nigeria. Ann Glob Health. 2018;84(1):121–28. doi: 10.29024/aogh.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lazarus JV, Sihvonen-Riemenschneider H, Laukamm-Josten U, Wong F, Liljestrand J. Systematic review of interventions to prevent the spread of sexually transmitted infections, including HIV, among young people in Europe. Croat Med J. 2010;51(1):74–84. doi: 10.3325/cmj.2010.51.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Layzer C, Rosapep L, Barr S. A peer education program: delivering highly reliable sexual health promotion messages in schools. J Adolesc Health. 2014;54(3 Suppl):S70–77. doi: 10.1016/j.jadohealth.2013.12.023. [DOI] [PubMed] [Google Scholar]
- 33.He J, Wang Y, Du Z, Liao J, He N, Hao Y. Peer education for HIV prevention among high-risk groups: a systematic review and meta-analysis. BMC Infect Dis. 2020;20(1):338. doi: 10.1186/s12879-020-05003-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mavundza EJ, Iwu-Jaja CJ, Wiyeh AB, Gausi B, Abdullahi LH, Halle-Ekane G, Wiysonge CS. A systematic review of interventions to improve HPV vaccination coverage. Vaccines (Basel). 2021;9(7). doi: 10.3390/vaccines9070687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Acampora A, Grossi A, Barbara A, Colamesta V, Causio FA, Calabro GE, Boccia S, de Waure C. Increasing HPV vaccination uptake among adolescents: a systematic review. Int J Environ Res Public Health. 2020;17(21):7997. doi: 10.3390/ijerph17217997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walling EB, Benzoni N, Dornfeld J, Bhandari R, Sisk BA, Garbutt J, Colditz G. Interventions to improve HPV vaccine uptake: a systematic review. Pediatrics. 2016;138(1). doi: 10.1542/peds.2015-3863. [DOI] [PubMed] [Google Scholar]
- 37.Gallagher KE, Kadokura E, Eckert LO, Miyake S, Mounier-Jack S, Aldea M, Ross DA, Watson-Jones D. Factors influencing completion of multi-dose vaccine schedules in adolescents: a systematic review. BMC Public Health. 2016;16:172. doi: 10.1186/s12889-016-2845-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaul S, Do TQN, Hsu E, Schmeler KM, Montealegre JR, Rodriguez AM. School-based human papillomavirus vaccination program for increasing vaccine uptake in an underserved area in Texas. Papillomavirus Res. 2019;8:100189. doi: 10.1016/j.pvr.2019.100189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rani U, Darabaner E, Seserman M, Bednarczyk RA, Shaw J. Public education interventions and uptake of human papillomavirus vaccine: a systematic review. J Public Health Manag Pract. 2022;28(1):E307–15. doi: 10.1097/PHH.0000000000001253. [DOI] [PubMed] [Google Scholar]
- 40.Thomas T, Blumling A, Delaney A. The influence of religiosity and spirituality on rural parents’ health decision making and human papillomavirus vaccine choices. ANS Adv Nurs Sci. 2015;38(4):E1–E12. doi: 10.1097/ANS.0000000000000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lahijani AY, King AR, Gullatte MM, Hennink M, Bednarczyk RA. HPV vaccine promotion: the church as an agent of change. Soc Sci Med. 2021;268:113375. doi: 10.1016/j.socscimed.2020.113375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berenson AB, Brown VG, Fuchs EL, Hirth JM, Chang M. Relationship between maternal experiences and adolescent HPV vaccination. Hum Vaccin Immunother. 2017;13(9):2150–54. doi: 10.1080/21645515.2017.1332551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee HY, Kwon M, Vang S, DeWolfe J, Kim NK, Lee DK, Yeung M. Disparities in human papillomavirus vaccine literacy and vaccine completion among Asian American Pacific Islander undergraduates: implications for cancer health equity. J Am Coll Health. 2015;63(5):316–23. doi: 10.1080/07448481.2015.1031237. [DOI] [PubMed] [Google Scholar]
- 44.Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ, Hesitancy Swgo V. Strategies for addressing vaccine hesitancy - a systematic review. Vaccine. 2015;33(34):4180–90. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]
- 45.Panagides R, Voges N, Oliver J, Bridwell D, Mitchell E. Determining the impact of a community-based intervention on knowledge gained and attitudes towards the HPV vaccine in Virginia. J Cancer Educ. 2022. doi: 10.1007/s13187-022-02169-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


