ABSTRACT
Measles continues to result in focal outbreaks in India, despite over three decades of universal infant vaccination. The aims of this study were to examine measles immunity in the population of Chandigarh, India, and to compare immunity by vaccination vs. natural infection. In a cross-sectional study of individuals 1–60 years selected from 30 communities within Chandigarh during 2017–2018, measles immunity was assessed using serological surveys. Seropositivity was compared across demographic groups, and by prior history of vaccination and natural history of infection. Among those 1–20 years old, measles seropositivity, and histories of measles vaccination or prior measles diagnosis were separately assessed as outcomes in logistic regression models, with demographic factors as independent variables. Among 1690 participants, 94% were seropositive, and 6% had borderline or negative antibody levels. Of those positive, 30% had prior vaccination, 16% had a history of natural infection, and 54% had an unknown history. Over 50% of individuals among those >20 years old, had unknown history of immunity. In the multivariable regression models, vaccination was more common in younger ages (P < .0001), and in males compared to females (P = .0220), and in those with more education (P < .0001). The majority of the population was seropositive, and seropositivity increased with age. Older age groups were more likely to be protected because of previous natural infection, whereas younger age groups were protected by vaccination. There was inequity in vaccination coverage by gender, and maternal education status.
KEYWORDS: Measles vaccine, India, vaccination coverage, seroepidemiologic studies
Introduction
Measles is a highly contagious, but vaccine-preventable infectious disease. Development of effective vaccines and robust vaccination programs resulted in a significant decline in global measles burden. The global case load decreased from an estimated 9 of every 10 children being infected, to less than 20 cases per million people in 2016. However, there is considerable room for improvement, particularly in low- and middle-income countries which have not yet met measles elimination targets.1 In fact, between 2016 and 2019, the World Health Organization (WHO) South East Asian Region (SEAR) witnessed a 6% increase in measles cases.2 India has the third highest burden of cases globally.3
In 2019, prior to the COVID-19 pandemic, vaccination coverage with a single dose of measles vaccine exceeded 90% in the majority of WHO member states. Coverage with a second dose increased from 18% in 2000 to 71% during 2019.2 Despite considerable success in measles vaccination in the WHO SEAR, India has struggled with measles control. In addition to the high case load, it accounted for more than 50% of global measles-associated mortality, and ranked fifth among countries with children lacking even a single vaccine dose.2,4 In India, universal infant vaccination for measles was introduced in 1985, with a single dose administered at 9 months of age. In recent years, a second dose was introduced through the measles-mumps-rubella (MMR) vaccine administered at 15–18 months of age. Currently, the first dose is being administered as a combined measles-rubella (MR) vaccine. Introduction of a second dose of measles containing vaccine (MCV) along with implementation of the National Rural Health Mission, and additional supplementary district-level campaigns from 2005 onwards have resulted in reduction of annual measles-related mortality by nearly 40%, during 2005 to 2013, among children younger than 5 years of age.5 According to the National Family Health Survey (NFHS) and Demographic Health Survey (DHS), between 2005 and 2019, the proportion of children fully vaccinated in India increased from 43.2% to 62.3%.6 The government further intensified efforts through a measles-rubella vaccination campaign targeting over 400 million children as well as a nation-wide effort, the Intensified Mission Indradhanush 3.0, to improve overall vaccination coverage.7,8
The union territory of Chandigarh, a highly urbanized area, with a population of over 1 million, experienced a measles outbreak from July 1998 to February 1999.9 It witnessed a second outbreak in 2003 in a slum area with 58 cases.10 Thereafter, sporadic cases have been observed, suggesting that the population immunity is inadequate despite high infant vaccination coverage.
It is believed that community vaccination coverage in the range of 90 to 96% is required to establish herd immunity, and eliminate measles. The WHO also recommends a target of 95% vaccination and two doses of measles containing vaccines (MCV) for all countries.11,12 In addition, consistent, effective community-level surveillance is required to identify and target areas at increased risk of susceptibility. The COVID-19 pandemic resulted in disruption of childhood vaccination programs, reducing routine vaccination coverage globally.13
In India, there are few well-designed community-level studies exploring the status of population immunity against measles. This prospective study was undertaken to examine measles immunity across different age groups in Chandigarh, India. We also compared immunity acquired through vaccination vs. natural infection.
Methods
Study population
The study was conducted at the Postgraduate Institute of Medical Education and Research (PGIMER) in Chandigarh. We included individuals aged 1 through 60 years residing in 30 communities. These communities were selected through a stratified random sampling of 510 community-based units called ‘anganwadis.’ Anganwadis deliver the “Integrated Child Development Services” (ICDS) of the Government, and have a defined catchment population served by them. They are distributed throughout the city, and include the population residing in rural, urban, and resettlement colonies. We included participants in proportion to the population distribution, in these three designations.
Within each community, the first household was selected randomly from a list, followed by every tenth household. Within each household, only one participant was enrolled. Enrollment was stratified by age to achieve even distribution. In the event that an eligible participant declined, the study team moved on to the next eligible household. Vaccination status was ascertained by examining vaccination cards if available, or by recall. Natural history of measles was ascertained based on medical records (if available) or by recall.
We planned to recruit 1100 individuals above 1 year of age, and an additional 200 pairs of mothers and their newborn infants. The mothers in these pairs were included in this study. Due to substantial loss to follow up among mothers, we sampled more pairs of mothers and infants.14 The sample size chosen allowed us to calculate margins of error of <5% for different age bands (10 year increments from 1 to 60).
Laboratory work
Measles immunity was assessed by measuring anti-measles IgG antibodies in serum. Blood samples were collected from participants, serum separated, and antibody levels measured quantitatively by ELISA, using commercial ELISA kits (Immunolab, GmbH, Germany). Antibody levels were categorized as recommended in the product insert: <8 U/ml were considered negative (suggesting lack of immunity), levels from 8 to 12 U/ml were considered borderline, and levels above 12 U/ml were considered positive (suggesting measles immunity). All laboratory testing was performed at PGIMER by trained individuals in accordance with the National Accreditation Board for Testing and Calibration Laboratories (NABL) Standards, ISO 17025 for public health laboratories, and Manual for the laboratory diagnosis of measles and rubella, 2nd edition (WHO/IVB/07.01), WHO, Geneva, Switzerland. Quality system essential elements identified in CLSI GP26A3, that specifically apply to this project met these standards.
We analyzed measles seropositivity as a categorical variable (positive vs borderline or negative), and absolute antibody levels (among those who were seropositive) as a continuous variable.
Derived variables
Among those who were seropositive, measles exposure history was categorized as: any history of natural infection (regardless of vaccination history), measles vaccination history (regardless of natural infection), unknown, and neither natural history nor vaccination history. In additional analyses, categories were further specified as vaccination without natural history, vaccination with natural history, natural history without vaccination, and unknown or no natural history or vaccination history. In other analyses, vaccination without natural history was also divided into single-dose vaccination and double-dose vaccination.
We considered the following covariates: age, gender, maternal education level, income, and caste. Age was categorized as 1–5 years, 6–10 years, 11–15 years, 16–20 years, 21–30 years, 31–40 years, 41–50 years, and 51–60 years. Since measles vaccination was introduced in India only in 1985, it is unlikely that those older than 32 years would have received the vaccine. Gender was recorded as either male or female. Maternal education was divided into five categories: None, primary (up to 5 years), middle (up to 8 years), higher secondary (up to 12 years), and college or higher. Income was divided into three levels: Less than 10,000 rupees (Rs) per month, 10,000 to 25,000 Rs per month, and over 25,000 Rs per month. Caste was recorded as scheduled caste, scheduled tribe, other backward caste, or general (as designated by the Indian government).
Statistical analysis
We calculated the proportion of seropositive individuals in each age group, followed by seropositivity by source of immunity. Within each age group, we presented the percentages of participants with seronegative status, no or unknown history of measles, natural history only, natural history and vaccination, vaccination with one dose MCV only, and vaccination with two doses MCV). Pearson’s chi-square test was used to measure the statistical significance of results between positive and borderline or negative status as well as between reason for seropositivity by each demographic factor.
Among participants younger than 20 years, age, gender, maternal education level, income, and caste were included as independent variables in separate models of immune status, vaccination, and natural history of disease.
All analyses were completed using SAS version 9.4. P-values for logistic regression models were obtained via Wald tests in which p < .05 was considered statistically significant. Weights were developed via inverse probability weighting in each gender by age group to standardize the sample population to the national population.15 These weights were used in all analyses.
Ethical approval
This study was approved by both the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board, as well as the Institutional Ethics Committee of the Postgraduate Institute of Medical Education and Research, Chandigarh. Approval of the Government of India Health Ministry Screening Committee was also obtained. Participants were enrolled with written informed consent, signed by people older than 18 years themselves, and by a parent or legal guardian for children younger than 18 years old. Children older than 8 years old, provided an additional assent.
Results
We enrolled a total of 1690 participants. Table 1 describes the demographic characteristics of the participant group. Reflecting the weighted sample, a larger proportion of participants were male (52%), although the absolute number of females was higher due to the sampling scheme.
Table 1.
Demographics of study population, Chandigarh, India, 2017–2018.
| Count (weighted %) | |
|---|---|
| Overall | 1690 |
| Age (in years) | |
| 1–5 | 124 (10%) |
| 6–10 | 133 (10%) |
| 11–15 | 130 (10%) |
| 16–20 | 144 (10%) |
| 21–30 | 557 (19%) |
| 31–40 | 352 (17%) |
| 41–50 | 122 (14%) |
| 51–60 | 128 (10%) |
| Gender | |
| Male | 307 (52%) |
| Female | 1383 (48%) |
| Monthly income | |
| Rs <10,000 | 1067 (63%) |
| Rs 10,000–25,000 | 466 (30%) |
| Rs >25,000 | 157 (7%) |
| Education | |
| None | 282 (17%) |
| Primary | 283 (19%) |
| Middle school | 247 (17%) |
| High school | 455 (28%) |
| ≥College | 420 (19%) |
| Other/Unknown | 3 (<1%) |
| Caste | |
| SC/ST | 544 (31%) |
| OBC | 141 (9%) |
| Others | 1005 (60%) |
OBC, other backward caste; Rs, rupees; SC/ST, scheduled caste/scheduled tribe
The proportion of seropositive individuals was 94% overall. Seropositivity was 88% among 1–5 year old, 86% among 6–10 year old, 90% among 11–15 year old, 93% among 16–20 year old, 95% among 21–30 year old, 98% among 31–40 year old, 99% among 41–50 year old, and 99% among 51–60 year old. Figure 1 shows measles serostatus in each age group. In those younger than 20 years, there was a clear trend of immunity due (entirely or in part), to vaccination; and a more recent trend toward immunity with two dose vaccination and no natural history. Older age groups trended toward no history of measles or unknown history of both disease or vaccination, but also had higher overall immunity than younger age groups.
Figure 1.
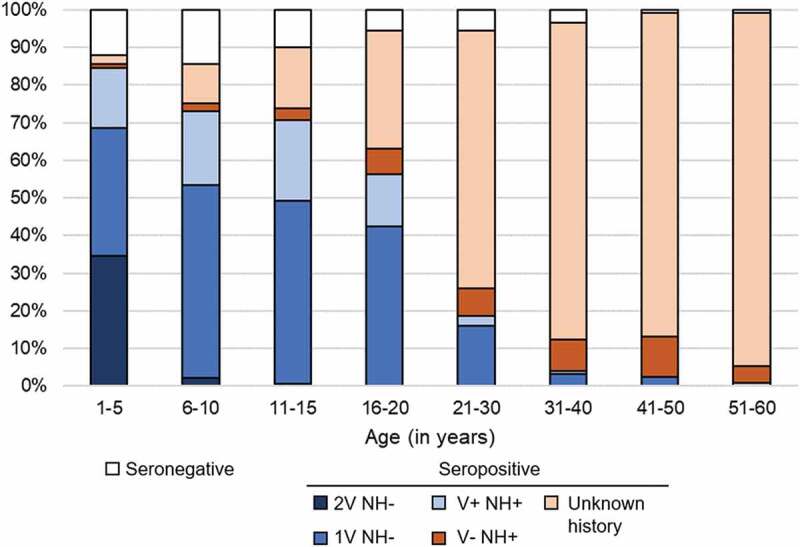
Measles immunity status by age group. NH = Natural History, V = Vaccination (any number of doses), 1 V = 1 dose of vaccine, 2 V = 2 doses of vaccine.
Table 2 summarizes measles serostatus by demographic factors. Among seropositive individuals, 54% reported no vaccination and unknown history of measles. This is especially common among those older than 20 years, which is understandable since measles vaccination was initiated in India only in 1985. Male participants were more likely to be seropositive from vaccination only (33%) than female participants (26%). Higher levels of maternal education were associated with considerably higher instance of vaccination without natural history, with the largest increase occurring between 5 (28%) and 8 (49%) year levels. Despite this trend, participants whose mothers had no formal education had considerably lower instance of non-immunity.
Table 2.
Measles immunity by source of immunity and demographic group, Chandigarh, India, 2017–2018.
| Measles antibody borderline or negative | P-value: positive vs borderline or negative | Antibody positive |
|||||
|---|---|---|---|---|---|---|---|
| Total | Vaccination | Natural History | No or unknown history | P-value | |||
| Overall | 100 (6%) | 1590 (94%) | 473 (30%) | 254 (16%) | 869 (54%) | ||
| Gender | .5708 | .0078 | |||||
| Male | 24 (5%) | 283 (95%) | 279 (33%) | 147 (18%) | 411 (49%) | ||
| Female | 76 (6%) | 1307 (94%) | 193 (26%) | 106 (14%) | 458 (60%) | ||
| Household income | .3661 | .2265 | |||||
| Rs <10,000 per month | 62 (6%) | 1005 (94%) | 296 (29%) | 151 (16%) | 555 (55%) | ||
| Rs 10,000–25,000 per month | 26 (4%) | 440 (96%) | 153 (32%) | 55 (18%) | 242 (50%) | ||
| Rs >25,000 per month | 12 (8%) | 145 (92%) | 24 (23%) | 9 (9%) | 71 (68%) | ||
| Maternal education | <.0001 | <.0001 | |||||
| None | 34 (3%) | 917 (97%) | 184 (20%) | 117 (13%) | 625 (67%) | ||
| Primary | 13 (10%) | 138 (90%) | 42 (28%) | 26 (17%) | 85 (55%) | ||
| Middle | 15 (7%) | 128 (93%) | 66 (49%) | 34 (26%) | 34 (25%) | ||
| Higher Secondary | 27 (15%) | 195 (85%) | 90 (55%) | 39 (24%) | 35 (21%) | ||
| College or Higher | 9 (7%) | 122 (93%) | 82 (62%) | 31 (23%) | 19 (15%) | ||
| Caste | .7847 | .0596 | |||||
| SC/ST | 30 (6%) | 514 (94%) | 159 (32%) | 94 (19%) | 244 (49%) | ||
| OBC | 9 (5%) | 132 (95%) | 34 (25%) | 10 (8%) | 92 (67%) | ||
| Others | 61 (5%) | 944 (95%) | 280 (29%) | 149 (15%) | 533 (56%) | ||
OBC, other backward caste; Rs, rupees; SC/ST, scheduled caste/scheduled tribe
Analysis of three regression models in participants younger than 20 years of age, for measles seropositivity, receipt of one or more doses of measles vaccine, and previous measles diagnosis (Table 3) showed a significant lower likelihood of vaccination in age groups over 5 years, although likelihood of seropositive status increased in older age groups. Males were significantly more likely to be vaccinated regardless of age than females (OR = 1.87, p = .0220), though rates of immunity and natural history were generally the same. Participants with mothers who had at least 8 years of formal education were over 6 times more likely to have been vaccinated and those whose mothers who had a college education were over 18 times more likely to be vaccinated (p < .0001) compared to those with no formal education. No significant trends were observed for income or caste for any of the three models.
Table 3.
Logistic regression models for measles immunity, vaccination, and natural history of disease among those 1–20 years old in Chandigarh, India, 2017–2018.
| Measles seropositive OR (95% CI)N = 523 | P-value | Received ≥1 dose of measles vaccine OR (95% CI)N = 523 | P-value | Previously diagnosed with measles OR (95% CI)N = 523 | P-value | |
|---|---|---|---|---|---|---|
| Age | .3740 | <.0001 | .2507 | |||
| 1–5 | Ref | Ref | Ref | |||
| 6–10 | 0.82 (0.38, 1.75) | 0.37 (0.14, 1.02) | 1.58 (0.86, 2.90) | |||
| 11–15 | 1.27 (0.53, 3.02) | 0.35 (0.13, 0.92) | 1.89 (1.01, 3.53) | |||
| 16–20 | 1.78 (0.68, 4.67) | 0.13 (0.05, 0.33) | 1.51 (0.78, 2.94) | |||
| Gender | .8962 | .0220 | .2419 | |||
| Female | Ref | Ref | Ref | |||
| Male | 0.96 (0.54, 1.71) | 1.87 (1.10, 3.18) | 1.28 (0.85, 1.93) | |||
| Maternal education | .3146 | <.0001 | .6864 | |||
| None | Ref | Ref | Ref | |||
| Primary | 0.63 (0.24, 1.66) | 1.18 (0.56, 2.47) | 1.29 (0.65, 2.55) | |||
| Middle | 0.99 (0.36, 2.69) | 6.62 (2.52, 17.38) | 1.52 (0.76, 3.04) | |||
| Higher Secondary | 0.52 (0.23, 1.16) | 6.24 (2.66, 14.66) | 1.47 (0.81, 2.67) | |||
| College or Higher | 1.38 (0.42, 4.50) | 18.14 (2.05, 160.43) | 1.25 (0.58, 2.70) | |||
| Income | .9882 | .3011 | .1761 | |||
| Rs <10,000 per month | Ref | Ref | Ref | |||
| Rs 10,000–25,000 per month | 1.06 (0.48, 2.39) | 2.04 (0.81, 5.19) | 0.56 (0.30, 1.03) | |||
| Rs >25,000 per month | 1.06 (0.12, 9.22) | 0.98 (0.21, 4.50) | 0.85 (0.24, 3.02) | |||
| Caste | .6385 | .7189 | .4261 | |||
| SC/ST | Ref | Ref | Ref | |||
| OBC | 0.92 (0.27, 3.19) | 1.61 (0.50, 5.13) | 0.50 (0.18, 1.42) | |||
| Others | 1.32 (0.70, 2.50) | 1.10 (0.64, 1.88) | 0.96 (0.60, 1.52) |
OBC, other backward caste; Rs, rupees; SC/ST, scheduled caste/scheduled tribe
Table 4 shows antibody titers among seropositive individuals. There were no significant differences across age groups and by reported source of immunity. Seropositivity itself also varied only slightly by source of immunity (Supplementary Table 1), with 92% being seropositive among those reporting no vaccine or natural history.
Table 4.
Mean antibody titer by age category and immune status, limited to those seropositive, Chandigarh, India, 2017–2018.
| Age (in years) |
||||||||
|---|---|---|---|---|---|---|---|---|
| 1–5 | 6–10 | 11–15 | 16–20 | 21–30 | 31–40 | 41–50 | 51–60 | |
| Overall | 85.53 | 116.28 | 112.86 | 115.46 | 119.78 | 121.61 | 119.90 | 120.25 |
| V- NH+ | 156.71 | 176.31 | 191.03 | 159.20 | 154.25 | 121.73 | 93.54 | 141.06 |
| V+ NH+ | 118.87 | 107.59 | 110.91 | 94.30 | 139.97 | 140.69 | N/A | 167.63 |
| 1 V NH- | 77.58 | 102.97 | 100.71 | 116.51 | 114.22 | 137.05 | 66.89 | N/A |
| 2 V NH- | 79.42 | 184.74 | 26.16 | N/A | N/A | N/A | N/A | N/A |
| Unknown | 38.34 | 169.55 | 141.15 | 113.73 | 116.52 | 121.17 | 124.68 | 118.81 |
NH = Natural History, V = Vaccination (any number of doses), 1 V = 1 dose of vaccine, 2 V = 2 doses of vaccine
Discussion
This study showed high overall population protection against measles in Chandigarh, India across various age groups. Older persons were protected through past natural infection, whereas the younger population was protected mostly by vaccination. However, the antibody levels generated by natural infection were higher than those generated by vaccination. Children in the age group 6–10 years who had received two doses showed higher antibody levels compared to those with a single dose, however this effect was not observed among 1–5 year old children. We also identified that maternal education was associated with immunity status.
This study provides valuable data for policymakers and program managers in India. Despite robust periodic national surveys on overall vaccination coverage, there is paucity of community-level serosurveillance to determine population susceptibility to measles.16 In this study, we found that 12% of 1–5 year-olds, 14% of 6–10 year-olds, and 10% of 11–15 year-olds, and 7% of 16–20 year-olds were seronegative, indicating a potential for substantial measles transmission in these groups. These data suggest that the government is justified in starting immunization campaigns to vaccinate all children 1–15 years old, regardless of prior immunization status.
Differences across age, map to changes over time in India’s focus on vaccination. The findings of this study illustrate that India’s vaccination coverage and outreach programs (e.g., Mission Indradhanush) have been very effective in generating increasingly high levels of single-dose measles vaccination coverage and since 2008, double dose coverage without natural disease in Chandigarh. Furthermore, antibody levels far above the level deemed to be protective have been maintained in populations without any non-vaccine exposure, indicating that the timing and quality of vaccine are sufficient for long-term protection. The sharp increase in known cause of immunity in younger age groups also indicates that medical recordkeeping has improved considerably in the past two decades, a factor that may be attributable to increased focus on, and successful implementation of several electronic medical recordkeeping programs implemented in different regions of the country including Chandigarh.17–19 The youngest age groups in Chandigarh have seen a considerable increase in single and, more recently, double-dose vaccination compared to their older counterparts. This trend also coincides with a decrease in immunity due to natural history of disease in these younger age groups. These findings indicate improved control of measles in the community largely driven by the increased focus on routine vaccination enacted by the Indian government in recent years. This improved control may also be responsible for the increase in individuals with no immunity in young age groups, as lower case load may result in less natural immunity. Understanding of the mechanisms behind this increase in nonimmune individuals would benefit from further research. Mean antibody titer in single and double vaccine dose groups was also comparable to overall mean titers in their respective age categories and remained well within the immune range in older groups (Table 4) indicating acceptable long-term effectiveness of current vaccine scheduling.
Additionally, maternal education appears to play a considerable role in likelihood of vaccination, with the most educated mothers being more than 18 times more likely to vaccinate their children compared to uneducated mothers. These findings are consistent with prior studies both globally and in India.20,21 This discrepancy indicates that pockets of low maternal education in Chandigarh are likely the most at-risk communities regardless of the presence of other risk factors included in this study. Given the consistent increase in maternal education levels nationally with each release of India’s National Health and Family Survey, this risk should trend downward over the next few decades.22 It will be important to implement proper strategies to reach lower educated families.
Despite the increase in vaccination coverage and decrease of rates of natural disease shown by this study, there are areas of concern presented by the data. Male participants were considerably more likely to have immunity from vaccination only than female participants (33% vs 26%, p = .0078) and also had higher odds of having received at least one dose of measles vaccine (OR = 1.87, p = .0220). Given that measles does not show increased infectivity in either males or females, this outcome may be explained by social, economic, or other non-biological factors.23,24 Additionally, younger age groups have a considerably higher rate of non-immunity, indicating that endemicity of measles in India is likely trending down as vaccination campaigns have successfully increased coverage. Given the highly infectious nature of measles and high levels of consistent vaccine coverage necessary for control, this elicits concerns regarding pockets of vulnerability in these groups. A previous serosurvey in Tianjin, China, found a high degree of correlation between the relative proportion of measles cases by age, and seronegativity in those age groups.25 Accordingly, it will be important to adjust coverage strategies to ensure adequate immunological protection through vaccination coverage in groups with low levels of immunity as determined in seroprevalence studies.
Findings of this study indicate that disparities in vaccination still exist within Chandigarh and steps should be taken to target those disparate groups, namely females and households with low maternal education, in future vaccine coverage strategy adjustments. Further research should be conducted regarding the demographics of the nonimmune population in order to better address coverage disparities. It may also be beneficial to conduct research regarding the considerable disparity between rates of immunity from vaccination only between males and females to uncover and address any potential factors of influence. Additionally, the results of this and other serosurveys in recent years warrant consideration for expansion in serosurvey usage in India. The insights provided regarding immunological profile and source of immunity for a number of diseases may be incredibly useful in ongoing development and deployment of vaccine coverage strategies as overall coverage improves and vulnerable pockets trend toward within-community levels.
An important limitation is that we could not ascertain the occurrence of subclinical or atyplical measles infection in participants, which often go undetected because of the lack of signs and symptoms of disease. Further, in the vaccine era, the disease itself may be milder or modified, making it difficult to identify without obtaining laboratory tests such as IgM antibody levels. These types of exposures could explain the large proportion of older participants reporting no history of natural infection, yet having seroprotection against measles. Antibodies acquired through natural infection generally result in a higher titer than vaccine-induced antibodies, and decline more slowly as well. In this study, we could not calculate the incidence rates of measles in the various age groups, as the participants lacked documents confirming physician diagnosed measles, or confirmatory laboratory tests for measles. We also do not make inferences about immunity from vaccination versus natural infection. The accepted paradigm is that immunity following natural disease is life-long, but after two doses of measles vaccine, immunity declines over time,26 which has been shown in a seroprevalence study.27 For those with a natural history of infection, any difference between antibody titer in those vaccinated and unvaccinated could be due to sampling error or to recency of infection.
While surveillance of diseases with high infectivity and low pathogenicity or clinical presentation stand to benefit more from serological measures, there is still considerable utility for diseases with higher pathogenicity such as measles including assessing immunity in countries or regions with rapidly changing immune profiles or vaccination programs.28,29 Furthermore, there may be additional benefit in countries with less reliable vaccination records.30 Given the most recent vaccination card availability data and the considerable lack of knowledge amongst older populations regarding history of measles or vaccine, there is reason to believe that this benefit is likely still applicable to many regions within India.31 Furthermore, improvements over the past decade in cold chain storage and health system infrastructure and outreach have made serological surveys much more feasible for a variety of diseases including rubella and, more recently, SARS-CoV-2.32,33
Strengths and limitations
The study group was both large, and derived from the local population via home visits. This likely helped to dispel response bias related to issues such as travel or survey response biases that may have otherwise existed. The study group also included individuals of all ages and residence types, ensuring that important subpopulations were not missed. Furthermore, collection of blood samples for serological testing allowed for insights not commonly seen in disease surveillance in India, particularly at the community level. This allowed us to generate insight from a perspective not often utilized in the country.
There are some limitations in the study as well. The most prominent of these is the oversampling of women in the population. 82% of the study group is female, considerably more than India’s actual female percentage (48%).34 This oversampling was in part purposeful, to obtain a larger proportion of mother-child dyads, which was another aim of this project, but it also could have been due to sampling of households during the day, during which time men would have been more likely to work outside of the home. While analyses were weighted to standardize the study population to India’s population, the raw data may not accurately capture trends that exist in the male population within the community and lower ability to generalize results. Additionally, scheduled castes and tribes are overrepresented compared to national and regional averages in this study.35 This may be due to differences in availability at home from differences in employment situations between castes. Furthermore, much of the vaccination data was collected via maternal recall due to lack of effective medical recordkeeping, which may not provide completely accurate data on true vaccination numbers. While our findings do not indicate any significant associations attributable to caste status, these differences still have the potential to generate bias and lessen generalizability.
An important limitation is that we could not ascertain the occurrence of subclinical measles infection in participants, which often go undetected. Further, in the vaccine era, the disease itself may be milder or modified, making it difficult to identify without laboratory tests such as IgM antibody levels. These types of exposure could explain the large proportion of older participants reporting no history of natural infection. It is also important to note that antibody levels are affected by repeated exposure. In this study, it was not possible to determine the number of episodes of exposure experienced by individual participants.
Conclusions
This study showed that, despite improving trends for vaccination coverage and endemicity, the lower overall immunity levels in younger age groups represents a risk for outbreaks that may become problematic if not addressed. Our findings also show that maternal education and gender could be related to vaccination status. Additional use of serosurveys may prove useful as India continues to identify vulnerable populations in their mission to improve measles coverage and overall vaccination coverage.
Acknowledgments
We appreciate the work of the community nurses and Anganwadi workers who participated in data collection.
Funding Statement
This work was funded by a gift to the University of Michigan from Ranvir Trehan and the Trehan Family Foundation to support public health research in India.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Hayman DTS. Measles vaccination in an increasingly immunized and developed world. Hum Vaccin Immunother. 2018;15(1):1–8. doi: 10.1080/21645515.2018.1517074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel MK, Goodson JL, Alexander JP, Kretsinger K, Sodha SV, Steulet C, Gacic-Dobo M, Rota PA, McFarland J, Menning L. Progress toward regional measles elimination — worldwide, 2000–2019. MMWR Morb Mortal Wkly Rep. 2020;69(45):1700–05. doi: 10.15585/MMWR.MM6945A6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention . Global measles outbreaks. 2022. [accessed 2022 Jun 9]. https://www.cdc.gov/globalhealth/measles/data/global-measles-outbreaks.html.
- 4.Shrivastava DSR, Shrivastava DPS, Ramasamy DJ. Measles in India: challenges & recent developments. Infect Ecol Epidemiol. 2015;5(1). doi: 10.3402/IEE.V5.27784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong BK, Fadel SA, Awasthi S, Khera A, Kumar R, Menon G, Jha P. The impact of measles immunization campaigns in India using a nationally representative sample of 27,000 child deaths. eLife. 2019;8. doi: 10.7554/ELIFE.43290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan N, Saggurti N. Socioeconomic inequality trends in childhood vaccination coverage in India: findings from multiple rounds of National Family Health Survey. Vaccine. 2020;38(25):4088–103. doi: 10.1016/j.vaccine.2020.04.023. [DOI] [PubMed] [Google Scholar]
- 7.Dhawan V, Singh P, Soni GK, Das A. Strengthening immunization systems to reach every child - operational guidelines. 2019. [accessed 2022 Feb 25]. https://imi3.nhp.gov.in/assets/document/Operational_Guidelines.pdf.
- 8.World Health Organization . India launches one of the world’s largest vaccination campaigns against measles and rubella syndrome with WHO support. 2017. [accessed 2022 Feb 25]. https://www.who.int/india/news/detail/11-07-2017-india-launches-one-of-the-world-s-largest-vaccination-campaigns-against-measles-and-rubella-syndrome-with-who-support.
- 9.Thakur JS, Ratho RK, Bhatia SPS, Grover R, Issaivanan M, Ahmed B, Parmar V, Swami HM. Measles outbreak in a periurban area of Chandigarh: need for improving vaccine coverage and strengthening surveillance. Indian J Pediatr. 2002;69(1):33–37. doi: 10.1007/BF02723774. [DOI] [PubMed] [Google Scholar]
- 10.Sharma MK, Bhatia V, Swami HM. Outbreak of measles amongst vaccinated children in a slum of Chandigarh. Indian J Med Sci. 2004;58(2):47–53. [PubMed] [Google Scholar]
- 11.Cutts FT, Dansereau E, Ferrari MJ, Hanson M, McCarthy KA, Metcalf CJE, Takahashi S, Tatem AJ, Thakkar N, Truelove S, et al. Using models to shape measles control and elimination strategies in low- and middle-income countries: a review of recent applications. Vaccine. 2020;38(5):979–92. doi: 10.1016/J.VACCINE.2019.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization . Measles vaccines: WHO position paper, April 2017 – recommendations. Vaccine. 2019;37(2):219–22. doi: 10.1016/j.vaccine.2017.07.066. [DOI] [PubMed] [Google Scholar]
- 13.Causey K, Fullman N, Sorensen RJD, Galles NC, Zheng P, Aravkin A, Danovaro-Holliday MC, Martinez-Piedra R, Sodha SV, Velandia-González MP, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398(10299):522–34. doi: 10.1016/S0140-6736(21)01337-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mathew JL, Patel PN, Wagner AL, Suri V, Bharti B, Carlson BF, Boulton ML. Analysis of reasons for loss to follow up in a prospective study in Chandigarh, India and impact from telecom changes. BMC Res Notes. 2021;14(1):419. doi: 10.1186/s13104-021-05837-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Population Pyramid . Population of India 2020. 2020. [accessed 2022 Jan 22]. https://www.populationpyramid.net/india/2020/.
- 16.World Health Organization, UNICEF . India: WHO and UNICEF estimates of immunization coverage: 2019 revision. 2020. [accessed 2022 Jun 17]. https://data.unicef.org/wp-content/uploads/country_profiles/India/Immunization-coverage-country-profiles-2019rev/Immunization-coverage-estimates-2019_ind.pdf.
- 17.Radhakrishna K, Goud BR, Kasthuri A, Waghmare A, Raj T. Electronic health records and information portability: a pilot study in a rural primary healthcare center in India. Perspect Health Inf Manag. 2014;11(Summer). [PMC free article] [PubMed] [Google Scholar]
- 18.Krishnan A, Nongkynrih B, Yadav K, Singh S, Gupta V. Evaluation of computerized health management information system for primary health care in rural India. BMC Health Serv Res. 2010;10:310. doi: 10.1186/1472-6963-10-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powell AC, Ludhar JK, Ostrovsky Y. Electronic health record use in an affluent region in India: findings from a survey of Chandigarh hospitals. Int J Med Inf. 2017;103:78–82. doi: 10.1016/J.IJMEDINF.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 20.Kumar A, Mohanty SK. Socio-economic differentials in childhood immunization in India, 1992–2006. J Popul Res. 2011;28(4):301–24. doi: 10.1007/s12546-011-9069-y. [DOI] [Google Scholar]
- 21.Forshaw J, Gerver SM, Gill M, Cooper E, Manikam L, Ward H. The global effect of maternal education on complete childhood vaccination: a systematic review and meta-analysis. BMC Infect Dis. 2017;17(1). doi: 10.1186/S12879-017-2890-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bettampadi D, Carlson BF, Mathew JL. Impact of multiple risk factors on vaccination inequities: analysis in Indian infants over 2 decades. Am J Prev Med. 2021;60(1):S34–S43. doi: 10.1016/J.AMEPRE.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Vlassoff C. Gender differences in determinants and consequences of health and illness. J Health Popul Nutr. 2007;25:47. [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization . Addressing sex and gender in epidemic-prone infectious diseases. 2007. [accessed 2022 Jun 17]. https://apps.who.int/iris/bitstream/handle/10665/43644/9789241595346_eng.pdf.
- 25.Boulton ML, Wang X, Zhang Y, Montgomery JP, Wagner AL, Carlson BF, Ding Y, Li X, Gillespie B, Su X, et al. A population profile of measles susceptibility in Tianjin, China. Vaccine. 2016;34(27):3037–43. doi: 10.1016/j.vaccine.2016.04.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bianchi FP, Mascipinto S, Stefanizzi P, De Nitto S, Germinario C, Tafuri S. Long-term immunogenicity after measles vaccine vs. wild infection: an Italian retrospective cohort study. Hum Vaccin Immunother. 2021;17(7):2078–84. doi: 10.1080/21645515.2020.1871296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anichini G, Gandolfo C, Fabrizi S, Miceli GB, Terrosi C, Gori Savellini G, Prathyumnan S, Orsi D, Battista G, Cusi MG, et al. Seroprevalence to measles virus after vaccination or natural infection in an adult population, in Italy. Vaccines. 2020;8(1):66. doi: 10.3390/vaccines8010066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cutts FT, Hanson M. Seroepidemiology: an underused tool for designing and monitoring vaccination programmes in low- and middle-income countries. Trop Med Int Health. 2016;21(9):1086–98. doi: 10.1111/TMI.12737. [DOI] [PubMed] [Google Scholar]
- 29.Wilson SE, Deeks SL, Hatchette TF, Crowcroft NS. The role of seroepidemiology in the comprehensive surveillance of vaccine-preventable diseases. CMAJ Can Med Assoc J. 2012;184(1):E70. doi: 10.1503/CMAJ.110506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO Regional Office for Europe . Guidance on conducting serosurveys in support of measles and rubella elimination in the WHO European region. 2013. [accessed 2022 Jun 17]. https://www.euro.who.int/__data/assets/pdf_file/0011/236648/Guidance-on-conducting-serosurveys-in-support-of-measles-and-rubella-elimination-in-the-WHO-European-Region.pdf.
- 31.Singh SK, Vishwakarma D. Spatial heterogeneity in the coverage of full immunization among children in India: exploring the contribution of immunization card. Child Youth Serv Rev. 2021;121:105701. doi: 10.1016/j.childyouth.2020.105701. [DOI] [Google Scholar]
- 32.Shanmugasundaram D, Awasthi S, Dwibedi B, Geetha S, Jain M, Malik S, Patel B, Singh H, Tripathi S, Viswanathan R, et al. Burden of congenital rubella syndrome (CRS) in India based on data from cross-sectional serosurveys, 2017 and 2019–20. PLoS Negl Trop Dis. 2021;15(7):e0009608. doi: 10.1371/JOURNAL.PNTD.0009608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prakash O, Solanki B, Sheth JK, Joshi B, Kadam M, Vyas S, Shukla A, Tiwari H, Rathod S, Rajput A, et al. Original research: assessing seropositivity for IgG antibodies against SARS-CoV-2 in Ahmedabad city of India: a cross-sectional study. BMJ Open. 2021;11(1):e044101. doi: 10.1136/BMJOPEN-2020-044101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Census of India . T 00-003: population by sex and sex ratio. [accessed 2021 Oct 29]. https://censusindia.gov.in/Tables_Published/A-Series/A-Series_links/t_00_003.aspx.
- 35.Census of India . T 00-005: total population, population of scheduled castes and scheduled tribes and their proportions to the total population. [accessed 2021 Oct 29]. https://censusindia.gov.in/tables_published/a-series/a-series_links/t_00_005.aspx.


