ABSTRACT
Vaccine hesitancy in healthcare workers (HCWs) has been studied for various contagious diseases, but there is still insufficient knowledge about this phenomenon for COVID-19. We developed and validated a knowledge, attitude, and practice survey of 39 questions to assess Italian HCWs’ hesitancy toward vaccination in general (general hesitancy), COVID-19 vaccination (COVID-19 hesitancy), and public health injunctive measures (refusal of obligations). The survey was administered through a web platform between July and November 2021. Three multivariable logistic regressions were performed to evaluate the association between the explored dimensions of hesitancy and the potential determinants investigated. Out of 2,132 respondents with complete answers, 17.0% showed to be generally hesitancy toward vaccination, 32.3% were hesitant on COVID-19 vaccination, while 18.8% were categorized as refusing obligations. A significant protective effect against all three dimensions of hesitancy was found for increasing fear of COVID-19, advising COVID-19 vaccination to relatives and patients, having received flu vaccination in the previous year and having higher levels of education. Better self-rated knowledge about COVID-19 vaccines and reading up institutional sources were significantly protective against general and COVID-19 hesitancy, while being a physician rather than another healthcare professional was protective only against COVID-19 hesitancy. Conversely, increasing age and referring to colleagues to expand knowledge about COVID-19 were positively associated with COVID-19 hesitancy. The determinants of general hesitancy, COVID-19 hesitancy and the refusal of obligations are mostly overlapping. Given the great influence they exert on patients and communities, it is pivotal to limit HCWs vaccine hesitancy through appropriate training activities.
KEYWORDS: COVID-19, Covid-19 vaccines, vaccination hesitancy, vaccination, health knowledge and attitudes, health personnel, physicians, surveys and questionnaires, Italy
Introduction
Vaccination is one of the most significant public health achievements and it was widely recognized as a key intervention to cope with the pandemic.1,2 Vaccines are an example of disruptive innovation of the contemporary era as demonstrated by their fundamental contribution to the control of the COVID-19 health emergency, and their benefits are recognized worldwide; however, many challenges still need to be addressed to increase vaccination coverage for different vaccine-preventable diseases, including COVID-19.3
As of April 2022, five COVID-19 vaccines have received conditional marketing authorization in the EU/EEA, following evaluation by European Medicines Agency (EMA), and are part of the EU Coronavirus Vaccines Strategy Portfolio: Comirnaty (BNT162b2) developed by BioNTech/Pfizer, Spikevax (mRNA-1273) produced by Moderna, Vaxzevria (previously COVID-19 Vaccine AstraZeneca) (AZD1222), COVID-19 Vaccine Janssen (Ad26.COV 2.5) and Nuvaxovid (NVX-CoV2373), developed by Novavax.4
Since the approval of the first COVID-19 vaccine in the EU/EEA in December 2020, the body of evidence regarding vaccine effectiveness and population impact has been increasing. Data from the real-world usage of COVID-19 vaccines have confirmed the clinical trial findings and showed high vaccine effectiveness against PCR-confirmed SARS-CoV-2 infection, significantly reducing viral load, especially toward the first virus variants.5 The five EU/EEA authorized COVID-19 vaccines all showed also a very good safety profile in clinical trials before receiving approval from the European Medicines Agency (EMA) and safety has always been continued to be monitored.4
Though the quality of evidence greatly varies depending on the vaccines considered, those authorized in the EU are safe and effective to prevent severe COVID-19, hospitalization, and death against all variants of concern currently known.6 However, questions remain open regarding booster doses and waning immunity, the immunity duration and heterologous vaccination.7,8
Even though COVID-19 vaccination could be recognized as one of the tools that has brought to a return to usual activities in most of countries, many people still show to be hesitant toward it. Vaccine hesitancy is a complex phenomenon, context specific, varies across time, place, and types of vaccines.9 In this study, we focus on vaccine hesitancy as a state of indecision and uncertainty that precedes the decision of being (or not being) vaccinated. In fact, whereas undergoing vaccination is a behavioral action that can be measured at the population level by retrieving vaccine coverage, vaccine hesitancy refers to an attitude or sentiment that, together with other factors (e.g. legal constraints), can influence this behavior.10 Thus, we consider hesitancy as a continuum between those that accept all vaccines with no doubts to complete refusal with no doubts, with vaccine hesitant individuals constituting the heterogeneous group between these two extremes.11,12
Evidently, the most-cited reason for general population hesitancy toward vaccination is safety concerns.13 Furthermore, a lack of awareness and a low perception of the severity of preventable illnesses, traits that are commonly reported also among adolescents,14 and a strong belief in alternative medicine have often been cited as elements associated with hesitancy.13 In addition to a segment of population that refuses vaccines, the novelty of the disease and concerns over safety and efficacy of the vaccine have generated a sizable proportion of people indicating reluctance to getting vaccinated against COVID-19, as shown in previous surveys conducted in the general population in different countries.15,16 Unfortunately, hesitant groups are found also among healthcare workers (HCWs). Since the emergence of SARS-CoV-2, HCWs have been on the front line in caring for COVID-19 patients, and consequently are at high risk of infection. According to the European center for disease prevention and control (ECDC), the proportion of HCWs among COVID-19 cases varied from 2.2% to 29% in countries with available data.17 Despite the unprecedented rates of mortality due to COVID-19 worldwide and hospitals close to collapse amid surge in COVID-19 patients, a large portion of HCWs were either uncertain or did not plan to receive the COVID-19 vaccine after the EMA emergency authorization in December 2020.18 At the time, reports suggested that less than half of HCW included in the studies were willing to get vaccinated.19,20 Considering also the educative role of HCWs among the society on vaccine acceptance, we should understand and prioritize such concerns and factors that can result in the COVID-19 vaccine acceptance. The rationale of this study consists in analyzing the knowledge, attitudes, and behaviors of different Italian HCWs regarding the COVID-19 vaccines, in order to investigate the main elements of the vaccine hesitancy phenomenon in this group.
Methods
Study design and participants
We conducted an online cross-sectional survey between 22 July 2021, and 20 November 2021, among HCWs aged 18 years and older residing and working in Italy. Based on a literature review,21–30 we developed a specific questionnaire that was pilot tested for validity on a group of 30 HCWs. The questionnaire was administered through the “Survey Monkey®” platform and the estimated time required for compilation was approximately 6 minutes. Before starting the survey, the study description and privacy policy were shown, and informed consent was required; to participate, people had to give their consent, otherwise access to the questionnaire was denied. Participation was voluntary and unpaid. Data collection was anonymous, and the recorded information cannot be linked to respondents. HCWs were enrolled in the study through the active collaboration of Professional Associations and research hospitals in Northern Italy (the Maugeri Clinical Scientific Institutes), which disseminated the link to the survey through their official communication channels, such as newsletters and social media profiles. In addition, the link was disseminated through flyers during the national congress of the Italian Society of Hygiene, Preventive Medicine and Public Health.
The protocol of the study was approved by the Ethics committee of the “Fondazione Policlinico Universitario A. Gemelli – IRCCS” (Prot. No. 0021609/21 ID 4104). The study was conducted according to the standards of Good Clinical Practice (GCP) and the requirements of the Declaration of Helsinki; collected data were processed according to EU Regulation No 2016/679 (GDPR), Legislative Decree No 196/2003 “Code for the Protection of Personal Data” and subsequent amendments, and all current legislation on data processing and protection.
Questionnaire structure
The online survey consisted of 39 closed-ended questions divided into five sections. Section 1 included questions about sociodemographic characteristics and work information (age, gender, resident region, marital status, education level, occupation and discipline, workplace, and impact of pandemic COVID-19 on work activity). Section 2 examined participants’ health conditions, investigating chronic diseases that result in susceptibility to severe forms of COVID-19 and former SARS-CoV-2 infection. The 11 questions of Section 3 investigated opinions and attitudes about COVID-19 vaccines and vaccination in general, using a 5-option Likert scale to assess degree of agreement or disagreement (Table 1). The questions of Section 3 were designed to explore three different, though partially overlapping, dimensions: safety and efficacy of vaccination in general (Q17, Q18, Q19, Q20); safety and efficacy of COVID-19 vaccination (Q21, Q22, Q23, Q24, Q25); and acceptability of injunctive measures to increase COVID-19 vaccination coverage (Q26, Q27).
Table 1.
5-option Likert scale used to evaluate agreement or disagreement for each specific item of the survey.
| Option | Score for questions in favor of vaccination | Score for questions against vaccination |
|---|---|---|
| Totally agree | 5 | 1 |
| Partially agree | 4 | 2 |
| Neither agree nor disagree | 3 | 3 |
| Partially disagree | 2 | 4 |
| Totally disagree | 1 | 5 |
For each question, the respondents had to choose one of 5 ordinal categories of agreeability, which was then translated into a numeric value between 1 and 5, with 1 expressing maximum disagreeability and 5 expressing maximum agreeability toward vaccination.
Section 4 investigated vaccination-related intentions, behaviors, and attitudes, examining factors influencing these behaviors; information regarding previous influenza vaccination, propensity to vaccinate against COVID-19 and willingness to recommend vaccines to their patients was collected. Finally, questions in Section 5 addressed participants’ knowledge related to COVID-19 vaccines and investigated information sources used, perceived level of preparedness, topics they would like to explore and desired communication channels.
Statistical analysis
Out of the 11 questions of Section 3, nine questions were selected as (dependent) outcome variables (Table 2), for their higher clearness and neutrality. Out of these nine questions, three summary scores were synthesized as follows: a score for hesitancy toward vaccination in general (“General hesitancy:” Q17, Q19, Q20), a score for hesitancy toward COVID-19 vaccination (“COVID-19 hesitancy:” Q21, Q22, Q23, Q25) and a score for refusal of obligations with regard to COVID-19-related injunctive measures (“Refusal of obligations:” Q26, Q27). Question 18 and Question 24 had to be excluded from our analysis, as they were found to reduce the internal consistency of the “General hesitancy” score and of the “COVID-19 hesitancy” score, respectively. As a matter of fact, these two questions explore beliefs concerning vaccination on which HCWs’ opinions are understandably less polarized, i.e. the existence of an even slim chance of vaccines causing serious adverse effects (Q17) and the presence of an absolute overlap in efficacy and safety of approved COVID-19 vaccines (Q24). The 5-option Likert scale for individual questions and summary scores was dichotomized as follows. For individual questions in favor of vaccination, the scale was divided between lack of explicit agreement (1, 2, 3 = 1) and presence of explicit agreement (4, 5 = 0). For individual questions against vaccination, the scale was divided between lack of explicit disagreement (1, 2, 3 = 1) and presence of explicit disagreement (4, 5 = 0). On the other hand, summary scores calculated for each respondent were dichotomized as 1 if at least one of the answers within the subset of questions was summarized as 1. Otherwise, they were set as 0.
Table 2.
Questions included in the statistical analysis as outcome variables.
| Please express your opinion regarding the following statements: | ||
|---|---|---|
| General hesitancy | Q17 | Vaccines are scientifically proven and are among the safest pharmaceutical products |
| Q19 | Vaccines represent an indispensable tool for the protection of individual and public health | |
| Q20 | Vaccines have a negligible impact on the spread of infectious diseases | |
| COVID-19 hesitancy | Q21 | The risk of complications from COVID-19 disease is greater than the risk of serious adverse effects from COVID-19 vaccine |
| Q22 | It is preferable to acquire immunity against SARS-CoV-2 by contracting the infection rather than by vaccination | |
| Q23 | There is insufficient evidence on the efficacy and safety of COVID-19 vaccines due to their rapid development | |
| Q25 | The COVID-19 vaccine is effective in preventing COVID-19 | |
| Refusal of obligations | Q26 | It is appropriate to provide for work restrictions for those who, although not presenting medical-health impediments, refuse to be vaccinated against COVID-19 |
| Q27 | The COVID-19 vaccine should be made mandatory for healthcare professionals | |
Multivariable logistic regressions were performed for each question and for each score, according to the previously described dichotomization of outcome variables. Dimensions measured by other questions of the survey have been included as independent variables based on their causal likelihood and on insights from the review of previous literature, after confirmation of their association with the outcome variables through univariable logistic regressions. The respondents who preferred not to specify their gender (n = 10, 0.5%) were excluded from the logistic regression analysis, as they constituted an excessively small sub-group.
Results have been reported in the form of odds ratio with 99% confidence intervals (Table 3) and graphically represented by means of forest plots (Figure 1). p-values below 0.01 were considered as statistically significant. All the statistical analyses were carried out using Stata software, version 15 (StataCorp LP, College Station, TX, USA).
Table 3.
Results of the multivariable logistic regression in form of odds ratio with 99% confidence intervals in brackets.
| General hesitancy | COVID-19 hesitancy | Refusal of obligations | ||
|---|---|---|---|---|
| Socio-demographic variables | ||||
| Gender | Female | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Male | 0.913 [0.623,1.337] |
0.827 [0.615,1.113] |
0.742 [0.507,1.088] |
|
| Age | 1.011 [0.996,1.026] |
1.018** [1.006,1.030] |
0.994 [0.979,1.008] |
|
| Professional category | Not physician | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Physician | 1.062 [0.627,1.796] |
0.708 [0.477,1.052] |
1.053 [0.622,1.782] |
|
| Education level | Primary or secondary | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Undergraduate | 0.715 [0.311,1.647] |
0.438* [0.200,0.962] |
0.767 [0.318,1.850] |
|
| Graduate | 0.408* [0.172,0.967] |
0.368** [0.170,0.800] |
0.404 [0.161,1.010] |
|
| Post-graduate | 0.308*** [0.132,0.718] |
0.361** [0.169,0.772] |
0.576 [0.240,1.385] |
|
| COVID-19-related variables | ||||
| Self-rated fear of COVID-19 | 0.945* [0.903,0.990] |
0.943** [0.909,0.979] |
0.883*** [0.844,0.924] |
|
| Advising COVID-19 vaccination to patients | No | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Yes | 0.300* [0.113,0.798] |
0.103** [0.0314,0.341] |
0.174** [0.0636,0.476] |
|
| Advising COVID-19 vaccination to relatives | No | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Yes | 0.150** [0.0561,0.400] |
0.241* [0.0771,0.756] |
0.102** [0.0356,0.293] |
|
| Self-rated knowledge about COVID-19 vaccines | 0.914 [0.812,1.029] |
0.828** [0.751,0.912] |
0.917 [0.814,1.033] |
|
| Information sources about COVID-19 vaccines | ||||
| Institutional sources | No | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Yes | 0.231** [0.107,0.499] |
0.481 [0.223,1.036] |
0.511 [0.211,1.240] |
|
| Social media | No | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Yes | 0.815 [0.278,2.389] |
1.209 [0.570,2.564] |
1.155 [0.443,3.006] |
|
| Colleagues | No | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Yes | 0.906 [0.615,1.335] |
1.366* [1.019,1.833] |
1.112 [0.760,1.626] |
|
| Health-related variables | ||||
| Previous flu vaccination | No | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Yes | 0.606* [0.402,0.914] |
0.579** [0.413,0.813] |
0.636* [0.420,0.963] |
|
| Previous SARS-CoV-2 infection | No | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Yes | 0.973 [0.575,1.649] |
1.004 [0.654,1.542] |
1.076 [0.644,1.796] |
|
| Presence of chronic diseases | No | 1 [1,1] |
1 [1,1] |
1 [1,1] |
| Yes | 1.022 [0.690,1.514] |
1.150 [0.850,1.557] |
1.259 [0.852,1.860] |
|
| N | 1998 | 1998 | 1998 | |
* p < .01, ** p < .001.
Figure 1.
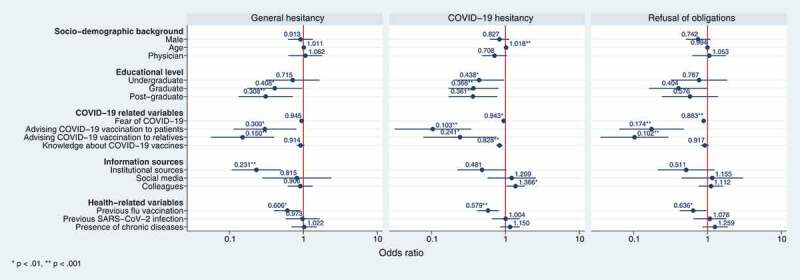
Results of the multivariable logistic regression in form of forest plots of odds ratios with 99% confidence intervals.
* p < 0.01, ** p < 0.001
Results
Among the HCWs to whom the questionnaire was sent, 2,142 HCWs consented to take part in the survey, of which 1,007 men (47.0%), 1,125 women (52.5%) and 10 who preferred not to specify their gender (0.5%), aged between 18 and 95. For what concerning the educational level, 4.2% of the participants had an upper secondary education or less, 10.0% had a Bachelor’s degree, 24.9% had a Master’s degree and 60.9% had a specialization or a PhD. For what concerning the category of HCWs, 71.8% of them were physicians, 8.0% dentists, 12.8% nurses and approximately 7.5% other healthcare professionals. They were mainly employed in hospitals (32.3%), teaching hospitals (12.2%), private activities (31.4%), local health districts (9.3%), general practice (8.0%) and specialist outpatient clinics (6.8%). Physicians were predominantly employed in medical departments (39.3%) with the remaining being distributed among surgical departments (12.6%), diagnostic and therapeutic departments (12.4%), public health district (11.2%), family medicine (9.7%) and other health services (18.4%). Nurses were mainly employed in medical departments (37.5%), with the remaining distributed among surgical departments (10.9%), emergency departments (17.5%), public health departments and primary care (8.0%), mental health departments (2.5%), and other health services (23.6%). For what concerning the health condition, 33.0% of the participants suffered from chronic diseases, among which the most frequent were arterial hypertension (52.4%), cardiovascular diseases (18.6%) and diabetes (13.4%). Finally, most of the HCWs had never tested positive for SARS-CoV-2 (87.6%) and those who tested positive, reported mild or moderate symptoms in most of the cases. Information about socio-demographic characteristics of the sample is reported in Table 5. For what concerning the score “General hesitancy,” 91.7% of HCWs believe that vaccines are scientifically studied and among the safest pharmaceutical products, 97.0% thinks that vaccines represent an indispensable tool for the protection of individual and public health, while 91.5% do not agree that vaccines have a negligible impact on the spread of infectious diseases. Overall, 17.0% of the sample showed a “General hesitancy” (Table 4). For what concerning the score “COVID-19 hesitancy,” 90.0% of the surveyed sample thinks the risk of complications from COVID-19 disease is greater than the risk of serious adverse effects from COVID-19 vaccine, 5.6% of them judge that it is preferable to acquire immunity against SARS-CoV-2 by contracting the infection rather than by vaccination, almost 10.9% is convinced that there is insufficient evidence on the efficacy and safety of COVID-19 vaccines due to their rapid development and 92.5% believes that the COVID-19 vaccine is effective in preventing COVID-19. In total, we can report a “COVID-19 hesitancy” in 32.3% of the sample analyzed. For what concerning the “Refusal of obligations,” only 83.6% of the interviewed agree that it is appropriate to provide for work restrictions for those who, although not presenting medical-health impediments, refuse to be vaccinated against COVID-19, while 89.5% reckons that the COVID-19 vaccine should be made mandatory for healthcare professionals. In general, hesitancy can be described in 18.7% of the HCWs for what concerning the score “Refusal of obligations.”
Table 5.
Descriptive analysis of the sample.
| Variable | Frequency | |
|---|---|---|
| Gender | M | 1,007 (47.0%) |
| F | 1,125 (52.5%) | |
| Not specified | 10 (0.5%) | |
| Age | 15-25 | 40 (1.9%) |
| 26-35 | 327 (15.3%) | |
| 36-45 | 299 (14.0%) | |
| 46-55 | 399 (18.6%) | |
| 56-65 | 601 (28.0%) | |
| 66-75 | 436 (20.3%) | |
| 76-85 | 36 (1.7%) | |
| 86-95 | 4 (0.2%) | |
| Level of education | Elementary diploma | 2 (0.1%) |
| Middle school diploma | 6 (0.3%) | |
| Upper secondary education diploma | 82 (3.8%) | |
| Bachelor’s degree | 214 (10.0%) | |
| Master’s degree | 534 (24.9%) | |
| Specialization or PhD | 1,304 (60.9%) | |
| Health profession | Physician | 1,538 (71.8%) |
| Dentist | 171 (8.0%) | |
| Nurse | 275 (12.8%) | |
| Chemist | 3 (0.1%) | |
| Healthcare assistants (OSS) | 19 (0.9%) | |
| Other | 136 (6.4%) | |
| Work setting | Hospital | 692 (32.3%) |
| Teaching hospital | 261 (12.2%) | |
| Specialist outpatient clinic | 146 (6.9%) | |
| Private activity | 673 (31.4%) | |
| General practice | 172 (8.0%) | |
| Public health district | 200 (9.3%) | |
| Extended care | 52 (2.4%) | |
| Home care | 44 (2.1%) | |
| Outpatient first aid | 22 (1.0%) | |
| Research institution | 84 (4.0%) | |
| Other | 266 (12.4%) | |
| Work department (physicians) | Medicine | 605 (39.3%) |
| Surgery | 194 (12.6%) | |
| Diagnosis and Therapy | 190 (12.4%) | |
| Public health | 173 (11.2%) | |
| General Practice | 149 (9.7%) | |
| Other | 228 (14.8%) | |
| Work department (nurses) | Medicine | 103 (37.5%) |
| Surgery | 30 (10.9%) | |
| Emergency unit | 48 (17.5%) | |
| Primary care and public health | 22 (8.0%) | |
| Mental Health | 7 (2.5%) | |
| Other | 65 (23.6%) | |
| Chronic diseases | Yes | 708 (33.0%) |
| No | 1,434 (67.0%) | |
| Previous SARS-CoV-2 infection | Yes, asymptomatic | 50 (2.3%) |
| Yes, mild-moderate symptoms | 197 (9.2%) | |
| Yes, severe symptoms and hospitalization | 20 (0.9%) | |
| No | 1,875 (87.6%) | |
Table 4.
Agreement or disagreement to single questions contributing to general scores.
| Score | Question | Partial or complete disagreement (percentage) | Partial or complete agreement (percentage) | Hesitancy Score |
|---|---|---|---|---|
| General hesitancy |
Q17 Vaccines are scientifically proven and are among the safest pharmaceutical products |
8.3 | 91.7 | 17.0% |
|
Q19 Vaccines represent an indispensable tool for the protection of individual and public health |
3.0 | 97.0 | ||
|
Q20 Vaccines have a negligible impact on the spread of infectious diseases |
91.5 | 8.5 | ||
| COVID-19 hesitancy |
Q21 The risk of complications from COVID-19 disease is greater than the risk of serious adverse effects from COVID-19 vaccine |
10.0 | 90.0 | 32.3% |
|
Q22 It is preferable to acquire immunity against SARS-CoV-2 by contracting the infection rather than by vaccination |
94.4 | 5.6 | ||
|
Q23 There is insufficient evidence on the efficacy and safety of COVID-19 vaccines due to their rapid development |
89.1 | 10.9 | ||
|
Q25 The COVID-19 vaccine is effective in preventing COVID-19 |
7.5 | 92.5 | ||
| Refusal ofobligations |
Q26 It is appropriate to provide for work restrictions for those who, although not presenting medical-health impediments, refuse to be vaccinated against COVID-19 |
16.4 | 83.6 | 18.7% |
|
Q27 The COVID-19 vaccine should be made mandatory for healthcare professionals |
10.5 | 89.5 | ||
| Not included in any score |
Q18 Vaccines can cause serious side effects |
49.3 | 50.7 | - |
|
Q24 COVID-19 vaccines approved in Italy to date are comparable in terms of efficacy and safety |
34.6 | 65.4 | - |
When the behavior of the participants was examined, 69.9% of them declared to have received influenza vaccination during 2020–2021 season, while 7.7% of them had vaccinated against flu only in the previous seasons. 98.1 of HCWs received anti-SARS-CoV-2 vaccine, motivated by social responsibility (63.0%), trust in COVID-19 vaccine as a preventive measure (79.0%), desire to protect one’s family (48.7%) and because of high risk of contracting SARS-CoV-2 infection because of their work (55.1%). Moreover, more than half of the participants (51.4%) declared that the fear of SARS-CoV-2 infection highly influenced their decision to get vaccinated (score 8–10 on a scale 1–10). Among those who did not vaccinate themselves against SARS-CoV-2 (1.5%), the majority believed that more proofs of efficacy and safety of the vaccine were needed (57.6%), most of them was afraid of possible side effects (54.6%) and some others did not consider themselves at high risk of developing severe disease (39.4%). Most of the surveyed HCWs advised the vaccine both to their patients (88.1%) and to their family (93.3%). However, 62.8% of respondents preferably recommended a COVID-19 vaccine developed in a specific country (Europe 47.9%, America 14.2%, Russia 0.4%, China 0,3%), against 37.2% who were indifferent to the country of development. The majority of the surveyed sample gathered information on this topic through institutional websites (84.1%), scientific literature or newsletters (almost 69.1%), webinars (almost 48.9%) and colleagues (32.9%), while 3.6% employed social networks. About 50.2% of HCWs declared their knowledge about COVID-19 vaccines to be good (score 8–10 on a scale 1–10), while 39.3% reported it as satisfactory (score 6–7 on a scale 1–10). Nevertheless, they claimed more information about COVID-19 vaccine side effects (66.1%), efficacy (48.1%) and types of vaccines (34.2%) particularly via institutional websites (71.2%), training courses (52.9%) and webinars (40.4%).
The multivariable logistic regression underlined, against “General hesitancy,” a weak protective effect of the increasing sense of fear of COVID-19 (OR 0.95 CI [0.90,0.99]) and the better self-rated knowledge about COVID-19 vaccines (OR 0.91 CI [0.84,1.00]). In addition, a moderate protective effect was shown for having received flu vaccination in the previous year (OR 0.61 CI [0.40,0.91]), as well as for advising COVID-19 vaccination to patients (OR 0.30 CI [0.11,0.80]). Similarly, being graduated (OR 0.41 CI [0.17,0.97]) and having a specialization or a PhD (OR 0.31 CI [0.13,0.72]) were found to be modestly protective. COVID Finally, there was a strong protective effect for reading up institutional sources (OR 0.23 CI [0.11,0.50]) and for advising COVID-19 vaccination to relatives (OR 0.15 CI [0.06,0.40]) (Table 3).
Increasing age (OR 1.02 CI [1.01,1.03]) and referring to colleagues to expand knowledge about COVID-19 (OR 1.37 CI [1.02,1.83]) were weakly associated with “COVID-19 hesitancy.” On the contrary, against “COVID-19 hesitancy,” we found a weak protective effect of the increasing fear of COVID-19 (OR 0.94 CI [0.90,0.99]) and the better self-rated knowledge about COVID-19 vaccines (OR 0.83 CI [0.75,0.91]). A modest protective effect against “COVID-19 hesitancy” was found also for having received flu vaccination in the previous year (OR 0.58 CI [0.41,0.81]), as well as for not being graduated (OR 0.44 CI [0.20,0.96]), for having a Bachelor’s degree (OR 0.37 CI [0.17,0.80]) and for having a Master’s degree, a specialization or a PhD (OR 0.36 CI [0.17,0.77]). Finally, a strong protective effect against “COVID-19 hesitancy” can be described for advising COVID-19 vaccination to relatives (OR 0.24 CI [0.07,0.76]) or to patients (OR 0.10 CI [0.03,0.34]). Conversely, the increasing sense of fear (OR 0.88 CI [0.83,0.94]) had a weak protective effect against the “Refusal of obligations,” whereas having received flu vaccination in the previous year has a modest protective effect (OR 0.64 CI [0.42,0.96]) against it. Finally, advising COVID-19 vaccination to patients (OR 0.17 CI [0.06,0.48]) and to relatives (OR 0.10 CI [0.04,0.29]) had a strong protective effect against the “Refusal of obligations.”
Discussion
In the present study, we analyzed the factors possibly associated with vaccine hesitancy, in particular related to the COVID-19 vaccination, in a large sample of Italian HCWs. Although clinical trials and real-world data have shown the efficacy of COVID-19 vaccination, in many countries coverage rates are still suboptimal, even among HCWs. This situation has led to the implementation of a number of measures to increase coverage, including mandatory vaccination for HCWs, as is the case of Italy, France, Greece, Hungary, Latvia, and Poland.31 Several studies have shown that many factors (socioeconomic, educational, informational) play an important role in vaccine hesitancy, both in the general population and in HCWs.32–36 In our study, we found that the level of education is an important factor that correlates with vaccination adherence: people with a higher degree of education (Master’s degree, specialization or PhD), in fact, appear to have confidence in vaccinations, resulting in a factor negatively associated with vaccine hesitancy. This finding is in line with other studies, which shows that in the overall population as well as among HCWs the educational level and, in general, the socio-economic conditions are important factors in determining vaccine hesitancy.35–40 Similarly, having received other previous vaccination (e.g., flu vaccination) proves to be an important factor in preventing vaccine hesitancy. This finding confirms previous results about how an aptitude for vaccination is a fundamental factor in favoring subsequent vaccinations.34,41–43
Having a higher educational level and being vaccinated for influenza both represent factors negatively associated with vaccine hesitancy, also considering specifically the COVID-19 vaccination. In addition, greater confidence in vaccination has been found in medical personnel than in other health professions, in line with similar recent studies.42,43 In the USA and UK, indeed, it has been observed that low socioeconomic conditions are more frequent in hesitant people hesitancy.44,45 A high rate of hesitancy (about 25%) was observed in France among HCWs, especially nurses and in general non-physicians.46,47 Also in Israel, a greater willingness to be vaccinated was observed among physicians compared to other professional categories, although in this case an important discriminating factor was the type of work (especially for those in contact with COVID-19 patients).24 As for Italy, a recent analysis of data from the Health Literacy Survey 2019 suggests that being trained in a healthcare profession is not a warranty of vaccine compliance per se, considering that the main predictor of vaccine literacy was found to be the financial background of respondents independently of their education or profession.48 Finally, an important factor to take into account for vaccine hesitancy is the source of information used for the vaccination topic, as also highlighted in a recent systematic review on COVID-19 vaccination hesitancy in Italian healthcare workers.49 The possibility of obtaining information from official sites was found in our study to be a predictor of non-hesitancy in our results. This observation is in line with the relationship between trust in the scientific community and vaccine acceptance previously described in literature for the general population50 and is particularly relevant, as it highlights the importance of a correct and clear information, especially among HCWs that might be one of the categories of the population more engaging about it with patients. Indeed, HCWs are a relevant source of information for them, therefore it is essential to understand their concerns and attitudes to prepare effective and evidence-based communication strategies. In this context, it is also important to highlight the ethical-social value of vaccination in this category. Considering other vaccinations, such as the one against influenza, it should be reminded that it is important that HCWs receive it not only for the direct benefits on their own’s health but also indirectly for patients’ health and wellness of the community,51,52 by reducing influenza cases, hospitalization and mortality in patients especially of healthcare facilities, thus showing an enhance of patient safety.53 At the same time, influenza in HCWs was associated with an increase of days loss due to illness with a substantial economic burden of sickness absenteeism, compared with the vaccinated HCWs.54,55 The same situation might be observed considering COVID-19 vaccination and, for this reason, further studies are required in order to enhance evidence about this important issue.
Our study has some limitations. As all web-surveys, it may be subject to self-selection bias and social desirability bias, the latter being even more likely given the particular nature of the reference population (HCWs). Furthermore, since the timeframe for the collection of data is quite wide (22 July 2021–20 November 2021), we have to consider that the attitudes about vaccine acceptance might have changed during the interval, for example due to new data about the real (or alleged) efficacy and safety of different COVID-19 vaccines. In addition, since the COVID-19 vaccination became compulsory for Italian HCWs on 1 April 2021, we could not evaluate the personal vaccination behavior of Italian HCWs with regard to COVID-19 vaccination, but had to rely purely on estimates of hesitancy for our analysis. With respect to this, we must acknowledge that our study might over-estimate HCW’s vaccine hesitancy, as we adopted a very strict approach to define lack of adherence toward vaccination in general (“General hesitancy”), toward Covid-19 vaccination specifically (“Covid-19 hesitancy”) and toward injunctive measures (“Refusal of obligations”). In fact, to dichotomize HCW’s answers to individual items, we considered unsure responses (i.e., responses corresponding to the central option of the 5-option Likert scale) as analogous to hesitant responses. Similarly, while computing the scores, we considered a respondent’s hesitant response to a single question of a score as sufficient to classify that respondent as hesitant for that specific score. However, in our study, we were interested in including as hesitant also those respondents with a lower level of hesitancy, to have a more complete view of the determinants underlying the development of this complex and multi-faceted phenomenon. For this reason, we wanted to minimize the risk of under-estimating hesitancy (type II error) more than the risk of over-estimating it (type I error), especially considering that our reference population are Italian HCWs, for whom not even a small “amount” of hesitancy (i.e., even answering to just one question like someone who is hesitant would answer) should be acceptable.
Conclusion
The results of the present survey show that almost a third of the HCWs involved were hesitant toward COVID-19 vaccination. This relevant finding, which is higher than the rates of hesitant HCWs found in previous studies in Italy,49 should be read in the light of many factors, among which the mandatory implications, the sociodemographic characteristics of the sample, their working setting, the geographical representativeness of the HCWs and the approach used to evaluate vaccine hesitancy.
COVID-19 vaccination is a critical tool to contain the pandemic, and vaccination of HCWs is essential to limit the spread in hospital settings with at-risk patients. However, more important is the need to convince people of the benefits of vaccination in general, and HCWs play a key role in this, also because mandatory vaccination is effective in reaching high coverage but, as other Authors underlined,49 cannot be considered a medium-long term successful strategy because of legal and ethical problems. Leaving aside the mandatory issue, HCWs are one of the main sources of information for users, thus it is essential for them to get vaccinated wholeheartedly and to adequately communicate how vaccination is effective and safe, as demonstrated by regulatory and well-conducted studies, besides being needful to get safely back to the everyday life with the pandemic still ongoing.
Acknowledgment
The authors would like to thank Dr. Gianfranco Damiani, Dr. Azzurra Massimi and Dr. Fidelia Cascini for their precious support in the dissemination of the survey.
Funding Statement
This study was funded by the National Center for Disease Prevention and Control (CCM) of the Ministero della Salute as part of the project “Survey of attitudes toward anti-SARS-CoV2 vaccination in the general population and among healthcare workers in the Italian territory”.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethical approval and consent to participate
The study was approved by the Ethics Committee of the “Fondazione Policlinico Universitario A. Gemelli – IRCCS” (Prot. No. 0021609/21, study ID 4104). Informed consent was obtained from all subjects involved in the study.
References
- 1.Centers for Disease Control and Prevention (CDC) . Ten great public health achievements — United States, 2001–2010 [Internet]. Morbidity and Mortality Weekly Report (MMWR); 2011. [accessed 2022 May 24]. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6019a5.htm [PubMed]
- 2.Greenwood B. The contribution of vaccination to global health: past, present and future. Philos Trans R Soc B: Biol Sci. 2014;369(1645):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Waure C, Calabrò GE, Ricciardi W. Recommendations to drive a value-based decision-making on vaccination. Expert Rev Vaccines. 2022;21(3):289–10. doi: 10.1080/14760584.2022.2021880. [DOI] [PubMed] [Google Scholar]
- 4.European Centre for Disease Prevention and Control (ECDC) . Vaccines [Internet]. ECDC; 2022 [accessed 2022 May 18]. https://www.ecdc.europa.eu/en/covid-19/latest-evidence/vaccines
- 5.European Centre for Disease Prevention and Control (ECDC) . Interim guidance on the benefits of full vaccination against COVID-19 for transmission risks and implications for non-pharmaceutical interventions [Internet]. Stockholm; 2021. [accessed 2022 May 18]. https://www.ecdc.europa.eu/en/publications-data/interim-guidance-benefits-full-vaccination-against-covid-19-transmission [Google Scholar]
- 6.European Medicines Agency (EMA) . COVID-19 vaccines: key facts [Internet]; [accessed 2022 May 18]. https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/vaccines-covid-19/covid-19-vaccines-key-facts
- 7.Fiolet T, Kherabi Y, MacDonald C-J, Ghosn J, Peiffer-Smadja N. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: a narrative review. Clin Microbiol Infect. 2022;28(2):202–221. doi: 10.1016/j.cmi.2021.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andrews N, Stowe J, Kirsebom F, Toffa S, Rickeard T, Gallagher E, Gower C, Kall M, Groves N, O’Connell A-M, et al. Covid-19 vaccine effectiveness against the Omicron (B.1.1.529) variant [Internet]. N Engl J Med. 2022. [accessed 2022 May 18];386(16):1532–1546. doi: 10.1056/NEJMoa2119451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.European Centre for Disease Prevention and Control (ECDC) . Vaccine hesitancy [Internet]. ECDC; [accessed 2022 May 18]. https://www.ecdc.europa.eu/en/immunisation-vaccines/vaccine-hesitancy
- 10.Larson HJ, Gakidou E, Murray CJL. The vaccine-hesitant moment. N Engl J Med [Internet]. 2022. [accessed 2022 Jul 28]. https://www.ncbi.nlm.nih.gov/pubmed/35767527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quinn S, Jamison A, Musa D, Hilyard K, Freimuth V. Exploring the continuum of vaccine hesitancy between African American and white adults: results of a qualitative study. PLoS Curr [Internet]. 2016. [accessed 2022 Jul 28];8. https://pmc/articles/PMC5309123/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dube E, Gellin B, Goldstein S, Larson H, Manzo ML, Reingold A, et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 13.Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med [Internet]. 2014. [accessed 2022 May 18];112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 14.Cadeddu C, Castagna C, Sapienza M, Lanza TE, Messina R, Chiavarini M, Ricciardi W, de Waure C. Understanding the determinants of vaccine hesitancy and vaccine confidence among adolescents: a systematic review. Hum Vaccin Immunother [Internet]. 2021. [accessed 2022 May 18];17(11):4470–4486. doi: 10.1080/21645515.2021.1961466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reno C, Maietti E, Fantini MP, Savoia E, Manzoli L, Montalti M, Gori D. Enhancing COVID-19 vaccines acceptance: results from a survey on vaccine hesitancy in Northern Italy. Vaccines [Internet]. 2021. [accessed 2022 May 18];9:378. https://www.mdpi.com/2076-393X/9/4/378/htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peretti-Watel P, Seror V, Cortaredona S, Launay O, Raude J, Verger P, Fressard L, Beck F, Legleye S, L’Haridon O, et al. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis [Internet]. 2020. [accessed 2022 May 18];20(7):769–770. doi: 10.1016/S1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burrer SL, de Perio MA, Hughes MM, Kuhar DT, Luckhaupt SE, McDaniel CJ, Porter RM, Silk B, Stuckey MJ, Walters M., et al. Characteristics of health care personnel with COVID-19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):477–481. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.European Medicines Agency (EMA) . COVID-19 vaccines: authorised [Internet]; [accessed 2022 May 18]. https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/vaccines-covid-19/covid-19-vaccines-authorised#authorised-covid-19-vaccines-section
- 19.Mena G, Blanco B, Casas I, Huertas A, Sánchez M-A, Auñón M, Viñas J, Esteve M., Tsuzuki, S.. Attitudes of Spanish hospital staff towards COVID-19 vaccination and vaccination rates. Plos One. 2021;16(9):e0257002. doi: 10.1371/journal.pone.0257002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fakonti G, Kyprianidou M, Toumbis G, Giannakou K.. Attitudes and acceptance of COVID-19 vaccination among nurses and midwives in cyprus: a cross-sectional survey. Front Public Health. 2021;9. doi: 10.3389/fpubh.2021.656138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Management and Healthcare Laboratory (MeS) of the Sant’Anna School of Advanced Studies and National Agency for Regional Health Services (AGENAS) . The vaccine and vaccination against COVID-19: the propensity of the Italian population to join the vaccination campaign [Internet]. 2021. [accessed 2022 May 18]. https://www.agenas.gov.it/images/agenas/In%20primo%20piano/2021/vaccini_indagine/ENG_AGENAS_MeS_Report_Vaccine_and_vaccination_against_COVID-19.pdf
- 22.World Health Organization (WHO) . SURVEY TOOL and GUIDANCE rapid, simple, flexible behavioural insights on COVID-19; 2020. [acccessed 2022 May 18]. https://www.euro.who.int/__data/assets/pdf_file/0007/436705/COVID-19-survey-tool-and-guidance.pdf
- 23.Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, Fang H.. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines (Basel) [Internet]. 2020. [accessed 2022 May 18];8:1–14. https://pubmed.ncbi.nlm.nih.gov/32867224/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E.. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol [Internet]. 2020. [accessed 2022 May 18];35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S.. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health [Internet]. 2021. [accessed 2022 May 18];6(4):e210–21. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reiter PL, Pennell ML, Katz ML.. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine [Internet]. 2020. [accessed 2022 May 18];38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verger P, Scronias D, Dauby N, Adedzi KA, Gobert C, Bergeat M, Gagneur A, Dubé E.. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Eurosurveillance [Internet]. 2021. [accessed 2022 May 18];26:2002047. https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2021.26.3.2002047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, Barrett E, Pal S.. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines (Basel) [Internet]. 2021. [accessed 2022 May 18];9:1–18. https://pubmed.ncbi.nlm.nih.gov/33546165/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paul E, Steptoe A, Fancourt D.. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Reg Health - Europe [Internet]. 2021. [accessed 2022 May 18]];1. https://www.thelancet.com/article/S2666776220300120/fulltext [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martin LR, Petrie KJ.. Understanding the dimensions of anti-vaccination attitudes: the Vaccination Attitudes Examination (VAX) scale; [accessed 2022 May 18]. https://academic.oup.com/abm/article/51/5/652/4648576 [DOI] [PubMed]
- 31.European Centre for Disease Prevention and Control (ECDC) . Overview of the implementation of COVID-19 vaccination strategies and vaccine deployment plans in the EU/EEA - Jan 2022 [Internet]; 2022. [accessed 2022 May 18]. https://www.ecdc.europa.eu/sites/default/files/documents/Overview-of-COVID-19-vaccination-strategies-deployment-plans-in-the-EU-EEA-Jan-2022_1.pdf
- 32.Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J.. Vaccine hesitancy: an overview. Hum Vaccin Immunother [Internet]. 2013. [accessed 2022 May 18];9(8):1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ.. Vaccine hesitancy and healthcare providers. Vaccine [Internet]. 2016. [accessed 2022 May 18];34(52):6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 34.Hollmeyer HG, Hayden F, Poland G, Buchholz U.. Influenza vaccination of health care workers in hospitals—a review of studies on attitudes and predictors. Vaccine [Internet]. 2009. [accessed 2022 May 18];27(30):3935–3944. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 35.Dubov A, Distelberg BJ, Abdul-Mutakabbir JC, Beeson WL, Loo LK, Montgomery SB, Oyoyo UE, Patel P, Peteet B, Shoptaw S, et al. Predictors of COVID-19 vaccine acceptance and hesitancy among healthcare workers in Southern California: not just “Anti” vs. “Pro” vaccine. Vaccines [Internet]. 2021. May [accessed 2022 18];9:1428. https://www.mdpi.com/2076-393X/9/12/1428/htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Biswas N, Mustapha T, Khubchandani J, Price JH.. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health [Internet]. 2021. [accessed 2022 May 18];46(6):1244–1251. doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bertoncello C, Ferro A, Fonzo M, Zanovello S, Napoletano G, Russo F, Baldo V, Cocchio, S. Socioeconomic determinants in vaccine hesitancy and vaccine refusal in Italy vaccines (Basel) [Internet]. 2020. [accessed 2020 May 18];8:1–9. https://pmc/articles/PMC7349972/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Danis K, Georgakopoulou T, Stavrou T, Laggas D, Panagiotopoulos T.. Socioeconomic factors play a more important role in childhood vaccination coverage than parental perceptions: a cross-sectional study in Greece. Vaccine [Internet]. 2010. [accessed 2022 May 18];28(7):1861–1869. doi: 10.1016/j.vaccine.2009.11.078. [DOI] [PubMed] [Google Scholar]
- 39.Anello P, Cestari L, Baldovin T, Simonato L, Frasca G, Caranci N, Grazia Pascucci M, Valent F, Canova C.. Socioeconomic factors influencing childhood vaccination in two northern Italian regions. Vaccine [Internet]. 2017. [accessed 2022 May 18];35(36):4673–4680. doi: 10.1016/j.vaccine.2017.07.058. [DOI] [PubMed] [Google Scholar]
- 40.Siddiqui M, Salmon DA, Omer SB.. Epidemiology of vaccine hesitancy in the United States. Hum Vaccin Immunother [Internet]. 2013. [accessed 2022 May 18];9(12):2643–2648. doi: 10.4161/hv.27243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Q, Yang L, Jin H, Lin L.. Vaccination against COVID-19: a systematic review and meta-analysis of acceptability and its predictors. Preventive Med [Internet]. 2021. [accessed 2022 May 18];150:106694. doi: 10.1016/j.ypmed.2021.106694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li M, Luo Y, Watson R, Zheng Y, Ren J, Tang J, Chen Y.. Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J [Internet]. 2021. [accessed 2022 May 18]. https://pubmed.ncbi.nlm.nih.gov/34193545 [DOI] [PubMed] [Google Scholar]
- 43.Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D.. Intention of healthcare workers to accept COVID-19 vaccination and related factors: a systematic review and meta-analysis. Asian Pac J Trop Med [Internet]. 2021. [accessed 2022 May 18];14(12):543. doi: 10.4103/1995-7645.332808. [DOI] [Google Scholar]
- 44.Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, Katikireddi SV, Benzeval MJ.. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun [Internet]. 2021. [accessed 2022 May 18];94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kricorian K, Civen R, Equils O.. COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin Immunother [Internet]. 2022. [accessed 2022 May 18]];18. https://pubmed.ncbi.nlm.nih.gov/34325612/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paris C, Bénézit F, Geslin M, Polard E, Baldeyrou M, Turmel V, É Tadié, Garlantezec R, Tattevin P.. COVID-19 vaccine hesitancy among healthcare workers. Infect Dis Now. 2021;51(5):484–487. doi: 10.1016/j.idnow.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gagneux-Brunon A, Detoc M, Bruel S, Tardy B, Rozaire O, Frappe P, Botelho-Nevers E.. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect [Internet]. 2021. [accessed 2022 May 18];108:168–173. https://pubmed.ncbi.nlm.nih.gov/33259883/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cadeddu C, Regazzi L, Bonaccorsi G, Rosano A, Unim B, Griebler R, Link T, de Castro P, D’Elia R, Mastrilli V, et al. The determinants of vaccine literacy in the Italian population: results from the health literacy survey 2019. Int J Environ Res Public Health [Internet]. 2022. [accessed 2022 May 18];19(8):4429. doi: 10.3390/ijerph19084429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bianchi FP, Stefanizzi P, Brescia N, Lattanzio S, Martinelli A, Tafuri S.. COVID-19 vaccination hesitancy in Italian healthcare workers: a systematic review and meta-analysis. Expert Rev Vaccines [Internet]. 2022. [accessed 2022 Jul 28];1–12. https://pubmed.ncbi.nlm.nih.gov/35757890/ [DOI] [PubMed] [Google Scholar]
- 50.Cadeddu C, Sapienza M, Castagna C, Regazzi L, Paladini A, Ricciardi W, Rosano A.. Vaccine hesitancy and trust in the scientific community in Italy: comparative analysis from two recent surveys. Vaccines (Basel) [Internet]. 2021. [accessed 2022 May 18];9. https://pubmed.ncbi.nlm.nih.gov/34696314/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van Delden JJM, Ashcroft R, Dawson A, Marckmann G, Upshur R, Verweij MF., van Delden, J.J.M.. The ethics of mandatory vaccination against influenza for health care workers. Vaccine [Internet]. 2008. [accessed 2022 May 18];26(44):5562–5566. doi: 10.1016/j.vaccine.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 52.Colamesta V, Tamburrano A, Barbara A, Gentili A, la Milia DI, Berloco F, Cicchetti A, Piacentini D, Galluzzi R, Mastrodonato SR, et al. Cost-consequence analysis of influenza vaccination among the staff of a large teaching hospital in Rome, Italy: a pilot study. Plos One. 2019;14(11):e0225326. doi: 10.1371/journal.pone.0225326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ahmed F, Lindley MC, Allred N, Weinbaum CM, Grohskopf L.. Effect of influenza vaccination of healthcare personnel on morbidity and mortality among patients: systematic review and grading of evidence. Clin Infect Dis [Internet]. 2014. [accessed 2022 May 18];58(1):50–57. doi: 10.1093/cid/cit580. [DOI] [PubMed] [Google Scholar]
- 54.Gianino MM, Politano G, Scarmozzino A, Stillo M, Amprino V, di Carlo S, Benso A, Zotti CM.. Cost of sickness absenteeism during seasonal influenza outbreaks of medium intensity among health care workers. Int J Environ Res Public Health [Internet]. 2019. [accessed 2022 May 18];16. https://pmc/articles/PMC6427598/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Antinolfi F, Battistella C, Brunelli L, Malacarne F, Bucci FG, Celotto D, Cocconi R, Brusaferro S.. Absences from work among healthcare workers: are they related to influenza shot adherence? BMC Health Serv Res [Internet]. 2020. [accessed 2022 May 18];20:1–8. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-05585-9 [DOI] [PMC free article] [PubMed] [Google Scholar]


