ABSTRACT
Vaccination for the novel coronavirus disease 2019 (COVID-19) provides an effective approach for the general improvement of social safety and individual health. To date, few studies have analyzed the adoption of COVID-19 vaccines from an entire impact process perspective. Using the health belief model (HBM) and the valence theory, this research evaluates the impact process of vaccine adoption for COVID-19. The respondents in this study were individuals who have been vaccinated in China. The effective sample included 595 individuals. Four valuable and novel findings are identified through this research. First, neither perceived susceptibility nor perceived severity has a statistically significant impact on the benefits from vaccination, threats from vaccination and self-efficacy. Second, benefits from vaccination produce a significant positive effect on self-efficacy and vaccine adoption. Third, threats from vaccination produce a significant negative effect on self-efficacy and vaccine adoption. Fourth, both self-efficacy and cues to adoption produce a significantly positive impact on vaccine adoption. Our theoretical model, which is the main contribution of this research, indicates that individual vaccine adoption is simply a process that leads from behavioral cognition to behavioral intention, rather than from psychological perception to behavioral cognition and then from behavioral cognition to behavioral intention.
KEYWORDS: Novel coronavirus disease 2019 (COVID-19), vaccine adoption, health belief model (HBM), valence theory, self-efficacy
Introduction
At the end of 2019, the novel coronavirus disease 2019 (COVID-19) broke out in the form of a pandemic, and the rapid onset of this disease has brought with it considerable challenges for many or all countries in the world (including challenges in political, economic, social, and security sectors).1 Follow this, national governments have been forced to adopt various methods and approaches to deal with this crisis.2 The technical means to provide COVID-19 vaccination has received extensive attention from relevant policy-makers. In particular, COVID-19 vaccination technology involves injecting a COVID-19 vaccine into the human body, such that the vaccinated individual has a demonstrably higher resistance to COVID-19.3 So far, several countries have developed COVID-19 vaccines and have begun to carry out vaccinations.4 For example, the United States of America started vaccinations on 15 December 2020. As of 16 October 2021, 65% of Americans are completely vaccinated.5 By the end of 2020, the 27 countries of the European Union had begun vaccinations. As of 16 October 2021, the vaccination rates in Spain and Portugal have exceeded 80%.6 China began implementing COVID-19 vaccinations at the end of 2020, so that by 16 October 2021, the proportion of Chinese completely vaccinated has reached 76%.7 As a consequence, the technology of COVID-19 has been recognized as effective, and vaccination has been rapidly deployed all over the world.
Although various countries are actively carrying out COVID-19 vaccinations, it is still the case that experts and interested individuals have concerns about the current technology involved in the vaccines. These questions include the side effects,8 the efficacy,9 and whether the testing of the COVID-19 vaccine has been rigorous,10 which has led a significant portion of the public to be unwilling to accept vaccination. How to encourage the public to adopt COVID-19 vaccines has become an urgent issue that many governments face. In response to this issue, we intend to analyze the impact process of COVID-19 vaccine adoption. At present, there are relatively few academic studies on the adoption of COVID-19 vaccines. In light of this finding, this study explores factors that theoretically affect the public’s vaccine adoption at every stage of implementation; this allows us to construct a theoretical model for vaccine adoption based on the health belief model (HBM) and the valence theory. Then, we empirically evaluated the direct and indirect effects of factors at every stage of the vaccine adoption process.
Until the current day, there are many studies on the adoption of COVID-19 vaccines.11–13 However, most of these studies evaluate the factors and effects of vaccine adoption. There are few researches to examine this issue from an entire impact process perspective. The purpose of this study is not only to explore the factors that affect vaccine adoption, but also to analyze the interactions and processes contained among these factors.
Theoretical background and research hypotheses
HBM
The HBM is a classic theoretical model that explores the formation of mechanism and influencing factors on individual health behavior from the perspective of the individual’s health care beliefs.14 The HBM was proposed by Hochbaum in 1958, and it has been revised and gradually improved, including in 1974 by Beck and other social psychologists.15 Grounded in the field of psychology, the HBM integrates value expectation theory, cognitive theory, and need motivation theory, so it can predict and explain individual behavior.16 The HBM consists of two major components: the first is perceived threat that indicates an individual’s self-perception of the severity of the disease and its consequences, and their judgment on the possibility of adverse outcomes (including perceived susceptibility and perceived severity),17 while the second is behavior cognition, including an individual’s perception of benefits and threats of vaccination. The latter component reflects an individual’s evaluation of the expected benefits and potential positive effects that a healthy behavior will bring, as well as the potential costs or difficulties encountered in implementing said behavior.17 Afterward, to further improve the explanatory power of this model, self-efficacy as an independent variable was introduced. According to the HBM, healthy behaviors are more likely to occur when individuals perceive the severity of the disease and the possibility of adverse outcomes, such that they believe that adopting healthy behaviors can bring more benefits and less costs.14
Valence theory
Valence theory was widely used in the fields of psychology and economics in the early days of those disciplines. Afterward, various scholars used this theory to explain and predict issues in the field of marketing.18 Valence theory is an individual decision-making theory based on rational cognition. According to this theory, the decision-making process of an individual is rational, and the behavior taken by an individual depends on his or her careful weighing of the pros and cons of their behavior; that is, the perceived positive valence and perceived negative valence are the basis of individual decision-making.19,20 With a variety of new technologies being applied in various fields of practice, studies on the initial adoption of these technologies have been attempted. Thus far, many scholars have used the valence theory to explain the initial adoption of technology by users.21,22
Impacts of perceived threat on behavior cognition
In this study, perceived threat describes an individual’s perception of the current or possible future threat brought about by COVID-19. The HBM holds that the greater the health threat that an individual perceives, the more likely the individual is to take action to avoid the actual occurrence of health issues.23 As far as the COVID-19 pandemic is concerned, individuals who believe that COVID-19 is a higher threat to their health have greater motivation to adopt health-oriented behavior, including preventive health behaviors such as vaccination.24 According to the cost-benefit paradigm, when decision-makers base their decision-making on subjective rather than objective standards, they need to evaluate the costs and benefits of decision-making.25
Furthermore, perceived susceptibility explains that if individuals think they are vulnerable to a negative outcome or health-threat, they will be more motivated to act in a way that promotes their health and well-being.26 Similar to the effect of perceived susceptibility, perceived severity implies that if individuals expect a negative threat to emerge that may cause serious health outcomes, then they will take action to prevent this threat.26 In this case as the public’s perceived threat of COVID-19 increases, they will be more likely to ascertain the benefits from vaccination. At the same time, it will reduce the threats from vaccination. In addition, according to the self-efficacy theory, individuals generally do not try new things. However, when individuals perceive threats from their environment, they will modify their lifestyles to ensure that this change can bring on satisfactory results.27 In reality, when perceiving the threat of COVID-19, the public will exert self-efficacy in order to affect their behaviors such as to ensure their own health outcomes are beneficial. From this perspective, perceived threat can stimulate individual self-efficacy. In this study, perceived susceptibility and perceived severity are two variables in the perceived threat stage. Therefore, based on the above argument, we propose the following hypotheses:
H1a:
Perceived susceptibility has a positive significant impact on benefits from vaccination.
H1b:
Perceived susceptibility has a positive significant impact on self-efficacy.
H1c:
Perceived susceptibility has a negative significant impact on threats from vaccination.
H2a:
Perceived severity has a positive significant impact on benefits from vaccination.
H2b:
Perceived severity has a positive significant impact on self-efficacy.
H2c:
Perceived severity has a negative significant impact on threats from vaccination.
Impacts of behavior cognition on behavior intention
In the HBM, perceived behavioral benefits and perceived behavioral threats are pre-factors for behavioral adoption.28 This conclusion has been supported in many studies.29,30 In addition, according to valence theory, an individual will maximize the positive valence of a product or service and minimize its negative valence.21 In other words, an individual expects to obtain the most value from the use of a product or service.31 In the context of COVID-19, vaccine adoption is an effective means to protect the public’s health. Thus, the positive impact of vaccination benefits on vaccine adoption is obvious. However, vaccination technology still has certain shortcomings, and to some extent, vaccination poses unknown threats to an individual’s health. In this sense, the negative valence of vaccination will have a negative impact on the public’s vaccine adoption.
In addition, the HBM indicates that if individuals are aware of current threats and believe in the benefits of changing behaviors, they will be more likely to change their behaviors in the long term. From this point of view, an individual will exert self-efficacy by evaluating the benefits and threats of behavior. The greater the benefit is, the easier it is to exert self-efficacy. In addition, social cognitive theory points out that behavior is a function of an individual’s ability to perform behavior (self-efficacy) and their belief that the behavior will achieve the desired results (reaction efficacy).32 Several recent studies have indicated that an individual’s self-efficacy can positively influence behavior adoption.32 FIn the context of COVID-19, the public’s self-efficacy will also be positively affected by the co-occurrence of their vaccination behavior. Therefore, on account of the above argument, we propose the following hypotheses:
H3:
Benefits from vaccination has a positive significant impact on vaccine adoption.
H4:
Threats from vaccination has a negative significant impact on vaccine adoption.
H5:
Benefits from vaccination has a positive significant impact on self-efficacy.
H6:
Threats from vaccination has a negative significant impact on self-efficacy.
H7:
Self-efficacy has a positive significant impact on vaccine adoption.
Impacts in the behavior intention stage
In the HBM, when an individual perceives a threat and realizes that a beneficial action can be taken in order to mitigate this threat, the action will occur as cues trigger this action.33 In other words, cues to action can stimulate individuals to take protective measures or behaviors.15,34 At present, several studies have demonstrated that cues to action have a significant positive impact on an individual’s behavioral intentions.35,36 In the context of COVID-19, the doctor’s recommendations, vaccination reports, and so on, are cues to vaccine adoption. In accordance with the conclusions of existing research, we argue that action cues can motivate the public to vaccinate and promote behavioral intention conducive to vaccination. Therefore, based on the above argument, we propose the following hypothesis:
H8:
Cues to adoption has a positive significant impact on vaccine adoption.
In view of the above hypotheses, we construct the theoretical model of this study in Figure 1.
Figure 1.
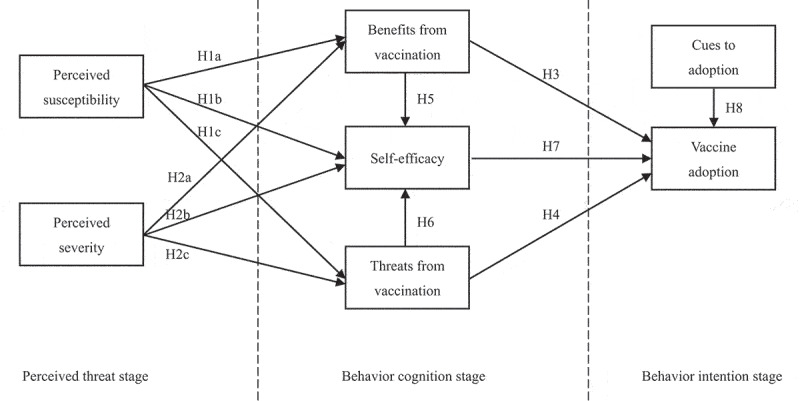
Theoretical model.
Methodology
In this study, our theoretical model illustrates the entire response process of individual vaccine adoption. In the perceived threat stage, we measure an individual’s psychological concerns and perceptions of threats related to COVID-19. This stage includes two variables: perceived susceptibility and perceived severity; these categories respectively denote an individual’s subjective feelings about the possibility and severity of the harm caused by COVID-19. The behavior cognition stage is used to analyze an individual’s evaluation of the benefits and costs of vaccination, including the benefits from vaccination, threats from vaccination, and self-efficacy. In particular, benefits from vaccination and threats from vaccination are designed according to the perceived benefits and perceived barriers in the HBM, respectively. They are an individual’s subjective evaluation of the potentialities of vaccination. In addition, self-efficacy denotes the evaluation-potential and judgment-ability of an individual’s own behavior and capacity to provide self-care during the epidemic. The third stage of the model is the behavioral intention stage, which is used to measure the intention of an individual’s vaccine-adoption behavior. This stage holds two variables: cues to adoption and vaccine adoption. Cues to adoption is designed according to cues to actions in the HBM. It represents factors that induce vaccine adoption. Vaccine adoption is the dependent variable of this study, which is designed according to the likelihood of behavior in the HBM and indicates the individual’s intention to pursue vaccination.
We selected citizens who have been vaccinated as subjects in China. This is mainly due to three reasons that we will subsequently describe. First, China has been studying the COVID-19 vaccine since March 2020. In June 2020, the country started the first clinical trial of the COVID-19 vaccine. In addition, China officially joined COVID-19 Vaccine Global Access in October 2020 and conducted COVID-19 vaccinations at the end of 2020.37 In this sense, China is one of the world’s leading countries in the development of the COVID-19 vaccine. Therefore, we expected to obtain high quality data from this country. Second, as of 21 April 2021, the number of COVID-19 vaccinations in China has exceeded 200 million doses.7 Therefore, data collection in this country is optimal for obtaining sufficient and effective samples. Third, the Chinese government adopted the principle of voluntary rather than compulsory vaccination during the process of COVID-19 vaccination. Each Chinese citizen can choose whether or not to vaccinate according to her or his preferences. In this respect, the policy environment of China meets the basic requirements for vaccine adoption as outlined in this research.
Measures
In this study, we designed 28 measurement items to measure the 7 variables in the theoretical model. The scale was designed as 7-point Likert scale. In this scale, “1” represented a measure of strongly disagreement, and “7” denoted strongly agreement. All items are shown in Table 1. The content of each item was designed with reference to prior valid measures. We refined the survey contents of the scale in order to obtain high-quality data. Throughout the investigation, all items were conducted in Chinese.
Table 1.
Specific measurement items of the scale.
| Variables | Items | References |
|---|---|---|
| Perceived susceptibility (PSU) | PSU1: I am concerned that I am at risk for the COVID-19. | Lee-Won et al.38; Lee & Aaker39 |
| PSU2: The extent to which I believed I am at risk for the COVID-19 is high. | ||
| PSU3: The likelihood that I might someday contract the COVID-19 is high. | ||
| Perceived severity (PSE) | PSE1: I think the COVID-19 is a very severe situation. | Fragkaki et al.40 |
| PSE2: The COVID-19 is a big problem in the area where I live. | ||
| PSE3: I think the COVID-19 is like the flu (reverse coded). | ||
| PSE4: I think the situation of the COVID-19 is exaggerated by the media (reverse coded). | ||
| Benefits from vaccination (BV) | BV1: I think vaccination can improve my physical health. | Wong et al.41 |
| BV2: I think vaccination can increase my positive emotion. | ||
| BV3: I think vaccination can strengthen my relationship with others. | ||
| Self-efficacy (SE) | SE1: I will be able to achieve most of the goals that I have set for myself during the outbreak. | Chen et al.42 |
| SE2: When facing difficult tasks during the outbreak, I am certain that I will accomplish them. | ||
| SE3: In general, I think that I can obtain outcomes that are important to me during the outbreak. | ||
| SE4: I believe I can succeed at most any endeavor to which I set my mind during the outbreak. | ||
| SE5: I will be able to successfully overcome many challenges during the outbreak. | ||
| SE6: I am confident that I can perform effectively on many different tasks during the outbreak. | ||
| SE7: Compared to other people, I can do most tasks very well during the outbreak. | ||
| SE8: Even when things are tough, I can perform quite well during the outbreak. | ||
| Threats from vaccination (TV) | TV1: I am concerned about the vaccine efficacy. | Al-Qerem, & Jarab10 |
| TV2: I am concerned about the vaccine side effects. | ||
| TV3: I am concerned about the vaccine rigor of testing. | ||
| TV4: I am concerned that I may be allergic to the vaccine. | ||
| Cues to adoption (CA) | CA1: I will get the vaccine when the doctor recommends it. | Al-Qerem, & Jarab10 |
| CA2: I will get the vaccine when vaccination becomes popular. | ||
| CA3: I will get the vaccine when I know enough about vaccinations. | ||
| Vaccine adoption (VA) | VA1: I intend to continue getting the vaccine in the future. | Su et al.43 |
| VA2: I will always try to get the vaccine in the future. | ||
| VA3: I plan to contribute to get the vaccine in the future. |
Data collection
A pilot survey was deployed in order to evaluate whether the scale was suitable for studying vaccine adoption. The results of the analysis showed that the scale was suitable for studying vaccine adoption. In addition, due to the effects of missing values, we used only “gender,” “age” and “education” as survey variables in our investigation of personal attribute information.
The formal investigation was based on Chinese samples. Given the feasibility and practical operability of surveys, we posted our questionnaires on the Sojump website (http://www.sojump.com/), a specialized online survey system in China similar to Qualtrics.com or SurveyMonkey.com in the United States. We selected registered members of Sojump as our target population. The website currently has over sixty million registered members that are located in various provinces across China. An advertisement for the survey was posted for one week on public forums. To improve the quality of our data, we charged five Chinese yuan for each respondent to participate. Participation was completely anonymous. Regardless of whether someone chose to participate, there was no risk of loss. To protect respondents’ privacy, “gender” was set as the nominal variable, while “age” and “education” were set as ordinal variables. The entire investigation period lasted half a month (from 25 April 2021 to 10 May 2021). We applied the following screening item: have you been vaccinated? Respondents who have not been vaccinated were not used as research samples. In addition, we deleted some samples of which responses were obviously unreasonable when screening the questionnaires. The answers to all questions in these samples were the same.Moreover, samples with a large number of missing values were also excluded. In total, 828 members participated in the study. The effective sample included 595 individuals after the data screening. Table 2 provides more detailed descriptive statistics.
Table 2.
Descriptive statistics of the respondents’ characteristics.
| Demographics | Category | Frequency | Percentage |
|---|---|---|---|
| Gender | Male | 317 | 53.3 |
| Female | 278 | 46.7 | |
| Age | ≤20 | 146 | 24.5 |
| 21–30 | 198 | 33.3 | |
| 31–40 | 152 | 25.6 | |
| 41–50 | 97 | 16.3 | |
| ≥50 | 2 | 0.3 | |
| Education | High school or below | 24 | 4.0 |
| Junior college | 78 | 13.1 | |
| University | 305 | 51.3 | |
| Master’s degree or higher | 188 | 31.6 |
Descriptive statistics
Using SPSS 17.0 software, we summarized the descriptive statistics of all items. Table 3 displays the results of the mean, standard deviation, skewness and kurtosis of all items.
Table 3.
Descriptive statistics of all measurement items.
| Variables | Items | Mean | Standard deviation | Skewness | Kurtosis |
|---|---|---|---|---|---|
| PSU | PSU1 | 3.65 | 1.95 | 0.08 | −1.06 |
| PSU2 | 2.49 | 1.54 | 0.91 | 0.23 | |
| PSU3 | 2.57 | 1.55 | 0.75 | −0.15 | |
| PSE | PSE1 | 3.99 | 1.89 | −0.05 | −0.99 |
| PSE2 | 2.25 | 1.45 | 1.17 | 0.76 | |
| PSE3 | 4.94 | 1.80 | −0.51 | −0.75 | |
| PSE4 | 5.50 | 1.44 | −0.80 | 0.12 | |
| BV | BV1 | 4.84 | 1.64 | −0.44 | −0.46 |
| BV2 | 4.96 | 1.59 | −0.52 | −0.30 | |
| BV3 | 4.59 | 1.69 | −0.29 | −0.55 | |
| TV | TV1 | 3.31 | 1.64 | 0.17 | −0.81 |
| TV2 | 3.68 | 1.71 | −0.06 | −0.91 | |
| TV3 | 3.37 | 1.72 | 0.21 | −0.87 | |
| TV4 | 3.63 | 1.71 | −0.01 | −0.90 | |
| SE | SE1 | 4.59 | 1.44 | −0.16 | −0.25 |
| SE2 | 4.93 | 1.38 | −0.35 | −0.11 | |
| SE3 | 4.94 | 1.34 | −0.24 | −0.05 | |
| SE4 | 4.86 | 1.45 | −0.35 | −0.18 | |
| SE5 | 5.05 | 1.35 | −0.44 | 0.06 | |
| SE6 | 5.02 | 1.34 | −0.38 | 0.04 | |
| SE7 | 4.92 | 1.35 | −0.30 | 0.04 | |
| SE8 | 5.04 | 1.31 | −0.38 | 0.17 | |
| CA | CA1 | 5.81 | 1.15 | −1.14 | 1.65 |
| CA2 | 5.85 | 1.16 | −1.29 | 2.25 | |
| CA3 | 5.84 | 1.17 | −1.26 | 2.09 | |
| VA | VA1 | 5.71 | 1.23 | −1.06 | 1.30 |
| VA2 | 5.38 | 1.38 | −0.57 | −0.12 | |
| VA3 | 5.43 | 1.28 | −0.51 | −0.09 |
PSU=perceived susceptibility; PSE=perceived severity; BV=benefits from vaccination; TV=threats from vaccination; SE=self-efficacy; CA=cues to adoption; VA=vaccine adoption.
Results
Reliability and validity test
Before hypothesis testing, the reliability and validity of the scale were tested. Using SPSS 17.0 and Lisrel 8.7 software, we conducted an exploratory factor analysis. In a series of analysis results, the KMO value was 0.92, which suggests that the sample data were suitable for factor analysis.44 Furthermore, this analysis extracted 7 factors that explained 89.07% of total variance, which indicates that these factors represent most of the information of the 28 items.45 In addition, the factor loadings of all 28 items exceeded 0.7, which demonstrates that these items can be analyzed for reliability and validity.38 The specific factor loading of each item was shown in Table 4.
Table 4.
Statistical results of some indicators.
| Factors | Items | Loadings | AVE | CR | Cronbach α |
|---|---|---|---|---|---|
| PSU | PSU1 | 0.73 | 0.72 | 0.88 | 0.86 |
| PSU2 | 0.91 | ||||
| PSU3 | 0.89 | ||||
| PSE | PSU1 | 0.81 | 0.62 | 0.86 | 0.84 |
| PSU2 | 0.74 | ||||
| PSU3 | 0.72 | ||||
| PSU4 | 0.86 | ||||
| BV | BV1 | 0.81 | 0.70 | 0.88 | 0.87 |
| BV2 | 0.85 | ||||
| BV3 | 0.85 | ||||
| TV | TV1 | 0.86 | 0.72 | 0.91 | 0.89 |
| TV2 | 0.89 | ||||
| TV3 | 0.87 | ||||
| TV4 | 0.76 | ||||
| SE | SE1 | 0.75 | 0.72 | 0.95 | 0.96 |
| SE2 | 0.83 | ||||
| SE3 | 0.82 | ||||
| SE4 | 0.85 | ||||
| SE5 | 0.88 | ||||
| SE6 | 0.89 | ||||
| SE7 | 0.88 | ||||
| SE8 | 0.88 | ||||
| CA | CA1 | 0.86 | 0.78 | 0.91 | 0.96 |
| CA2 | 0.90 | ||||
| CA3 | 0.89 | ||||
| VA | VA1 | 0.86 | 0.61 | 0.82 | 0.90 |
| VA2 | 0.76 | ||||
| VA3 | 0.71 |
PSU=perceived susceptibility; PSE=perceived severity; BV=benefits from vaccination; TV=threats from vaccination; SE=self-efficacy; CA=cues to adoption; VA=vaccine adoption.
The composite reliability (CR) values and Cronbach values were used to evaluate the reliability of the scale. Detailed analysis results are shown in Table 4. Based on this table, it can be seen that CR values and Cronbach values of all factors exceeded 0.7, which indicates that the scale had high reliability.46
In the validity test, we intended to test the convergent validity and discriminant validity of the scale respectively. The average variance extracted (AVE) was used to analyze the convergent validity. The analysis results were also shown in Table 4. We can see that all AVE values were greater than 0.5, which demonstrates that this scale had satisfactory convergent validity.47 In addition, the confirmatory factor analysis (CFA) was used to test the discriminant validity of the scale. After the CFA, we obtained the correlations between any two given factors. The specific results are shown in Table 5. We discovered that the square roots of AVE values were greater that these coefficients, which indicates that the discriminant validity of the scale meets the requirements for analysis.48
Table 5.
Statistical results of discriminant validity.
| Factors | PSU | PSE | BV | TV | SE | CA | VA |
|---|---|---|---|---|---|---|---|
| PSU | 0.85 | ||||||
| PSE | 0.06 | 0.79 | |||||
| BV | 0.09 | 0.40 | 0.84 | ||||
| TV | 0.40 | 0.61 | −0.11 | 0.85 | |||
| SE | −0.13 | −0.11 | 0.39 | −0.16 | 0.85 | ||
| CA | −0.09 | −0.25 | 0.44 | −0.21 | 0.52 | 0.88 | |
| VA | −0.09 | −0.21 | 0.52 | −0.27 | 0.58 | 0.71 | 0.78 |
PSU=perceived susceptibility; PSE=perceived severity; BV=benefits from vaccination; TV=threats from vaccination; SE=self-efficacy; CA=cues to adoption; VA=vaccine adoption.
Common method biases test and multiple collinearities test
By using Harman’s single factor test, we identified that the variance proportion explained by the factor with the largest eigenvalue was 36.08%; this suggests that the common method biases of this study were not serious.49 Furthermore, based on the correlation coefficients between any two factors shown in Table 5, we also understood that there were no serious multiple collinearities in the data.
Hypothesis tests
Using Lisrel 8.7 software, structural equation modeling was used to test our hypotheses. The analysis results of this model are shown in Table 6. We learned that all the fit indices results were acceptable, which demonstrates that our hypothesis tests that are used in this model were reasonable and effective.51
Table 6.
Fitting indices and evaluation criteria of research model.
| Fitting indices | Absolutely indices |
Parsimony indices |
Incremental indices |
||||||
|---|---|---|---|---|---|---|---|---|---|
| χ2/df | GFI | AGFI | RMSEA | PNFI | PGFI | CFI | NFI | IFI | |
| Values of fitting indices | 2.87 | 0.91 | 0.84 | 0.07 | 0.85 | 0.71 | 0.97 | 0.96 | 0.97 |
| Evaluation criteria values (Hoque & Sorwar)50 | <3 | >0.9 | >0.8 | <0.08 | >0.5 | >0.5 | >0.9 | >0.9 | >0.9 |
Figure 2 shows the model’s normalized path coefficients. From these data, we learned that perceived susceptibility had no significant influence on benefits from vac-cination (β=-0.02, p > .05), self-efficacy (β=-0.03, p > .05), and threats from vaccination (β = 0.04, p > .05), respectively. Therefore, H1a, H1b, and H1c were not supported. Similarly, the impact of perceived severity on benefits from vaccination (β = 0.02, p > .05), self-efficacy (β = 0.03, p > .05), and threats from vaccination (β=-0.02, p > .05) was not significant, respectively. Thus, H2a, H2b, and H2c were not supported. In addition, benefits from vaccination exerted a significantly positive impact on self-efficacy (β = 0.18, p < .05) and vaccine adoption (β = 0.23, p < .001), respectively, which supports H3 and H5. While, threats from vaccination had a significantly negative effect on self-efficacy (β=-0.15, p < .05) and vaccine adoption (β=-0.19, p < .001), respectively, which supports H4 and H6. Lastly, self-efficacy (β = 0.21, p < .001) and cues to adoption (β = 0.78, p < .001) produced significantly positive effects on vaccine adoption, respectively. Thus, both H7 and H8 were supported.
Figure 2.
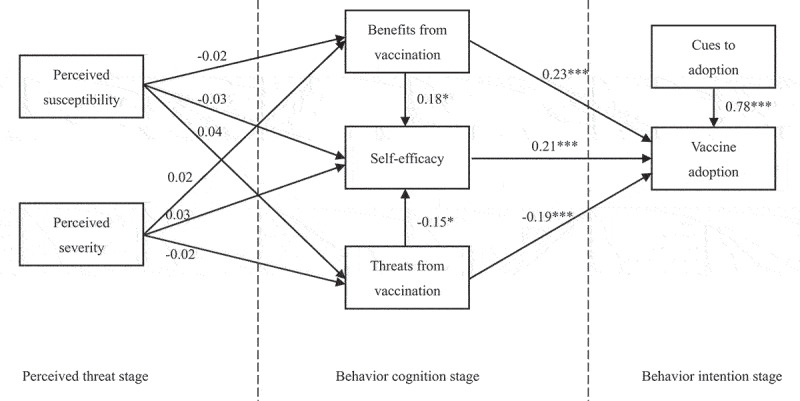
Hypothesis testing results.
Discussion
Conclusions
By combining HBM and valence theory, we produced a theoretical model that explores the impact process of vaccine adoption on COVID-19 and obtained four valuable conclusions. First, perceived threat does not have significant impact on the benefits from vaccination, threats from vaccination, and self-efficacy. Specifically, neither perceived susceptibility nor perceived severity has a significant effect on the benefits from vaccination, threats from vaccination, and self-efficacy. This insight is novel in public health research and distinct from existing research conclusions.24,27 This conclusion suggests that COVID-19 is indeed different from other diseases. The COVID-19 pandemic broke out at the end of 2019, and its impact continues to this day. However, this finding indicates that the public’s perceived threat of COVID-19 does not appear to be as serious as expected. We believe that the main reason for this observation is that COVID-19, which is a long-term threat, has been given attention by local governments after its outbreak. Given this continuous high attention, preventive and protective measures related to COVID-19 are especially important. In the long run, however, these efforts may cause public numbness and indifference. Vaccination is an effective technology that can largely prevent infection with COVID-19, but the public has not shown considerable appreciation for this technology. In terms of public opinion, there are serious doubts about vaccination technology. However, in this study, the empirical results indicate that the public’s perceived threat of COVID-19 does not affect their assessment of vaccination technology and their level of self-efficacy. This finding reflects that the public has become accustomed to COVID-19, and psychologically they are not afraid of its impact on their own health.
Second, benefits from vaccination have a significantly positive effect on individual self-efficacy and vaccine adoption. This finding is crucial for the development and improvement of vaccine technology in the context of COVID-19, and it can be considered a supplement to works of Raheli et al. (2020) and Valeeva et al. (2011).28,29 Despite being an effective measure against COVID-19, vaccine technology is not well known process. Currently, the benefits that this technology brings to public health are particularly important because its success largely determines the subjective evaluation of the public toward vaccines, and it affects the public’s behavior on its implementation. Similar to the research findings obtained in the fields of marketing and information systems, the empirical results of this study indicate that the benefits from vaccination not only mobilize the public’s self-efficacy, but they also promote the public’s adoption of vaccines; this suggests that positive valence can play a role in the management of COVID-19.
Third, threats from vaccination have a significant negative influence on self-efficacy and vaccine adoption. This conclusion is consistent with existing findings.52,53 According to the valence theory, any new technology, while it brings benefits, will also be accompanied by various potential risks and threats. This insight also applies to vaccines. As the negative valence of vaccination technology is concerned, the empirical results show that its negative effects on vaccine adoption and self-efficacy are not much smaller than the positive effects of positive valence of vaccination on the two variables. This demonstrates that for COVID-19, the public has serious doubts about vaccination technology. In this study, such doubts are reflected not only in the public’s psychological evaluation of vaccination, but also in the public’s behavioral intentions toward receiving the vaccine. From this perspective, the perceived threats posed by vaccines should be highly valued.
Fourth, both self-efficacy and cues to adoption produce a significant positive impact on vaccine adoption. This conclusion is similar to the evidence obtained from existing studies.32,35,36 In the face of possible disasters and other challenging conditions, self-efficacy determines an individual’s stress state, levels of anxiety, depression, and other psychosomatic response-processes. These emotional reactions in turn affect an individual’s activity and functions by changing the nature of the thinking process.54 Individuals with a strong sense of self-efficacy will respond to environmental pressures with a variety of protective behaviors. In the context of COVID-19, the empirical analysis indicates that the public has exerted a high level of self-efficacy, and they pursued vaccination to protect their health. Moreover, the path coefficient shows that the public’s self-efficacy plays a non-trivial role in vaccine adoption. This result further proves that the public is calm when facing the COVID-19 pandemic and has been rational when taking measures. In addition, based on the value of the path coefficient, policy-makers ought to pay attention to the effect of cues on vaccine adoption. In an environment where vaccination technology is questioned by the public at this stage of adoption, reliable knowledge, suggestions, and information are important guidelines for determining the intention of public behavior. The results of our analysis show that cues to adoption is an important element that affects the public’s behavioral intentions; in fact, the role of this element even exceeds the public’s own psychological hesitancy on vaccination technology.
Implications
We summarize our theoretical and practical contributions in this study. In theory, a model can be constructed to analyze the impact process of vaccine adoption in COVID-19 based on HBM and the valence theory. This theoretical contribution is ex-tremely important. In employing this model, governments can comprehend the response process of the public of adopting vaccines for COVID-19. The empirical results demonstrate that this model is convincing. On the one hand, our theoretical contribution points out the difference between COVID-19 and other diseases, and reveals the special aspect of COVID-19. Specifically, we demonstrated that the HBM is not fully applicable to the COVID-19. The main reason is that individual’s perceived threat to the COVID-19 does not have a significant impact on her/his behavioral cognition, which is different from what the HBM emphasizes. This contribution also points out the weakness of the HBM in explaining the COVID-19. COVID-19 has affected the life and work of the public, but at this stage, this virus no longer significantly affects the individual’s response to it. On the other hand, the public’s psychological evaluation of vaccination technology, and action cues can affect the public’s adoption of vaccines. The theoretical contribution demonstrates that the similarity between vaccination technology for COVID-19 and other technologies, and reveals the common aspect of the new technology. Moreover, we verified that the valence theory can be applied to the COVID-19 vaccine. Specifically, compared to other vaccines, we found that the COVID-19 vaccine adoption is also consistent with the valence theory’s assertion that individuals make decisions based on the benefits and threats of behavior. This finding can supplement the contributions of existing studies related to vaccine adoption, which suggests that vaccination technology, like technology adopted in other fields, is affected by its perceived subjective advantages and disadvantages, individual self-efficacy, and technology adoption cues.
In addition, the present study makes some practical contributions. First, the gov-ernments need to strengthen the publicity of vaccination technology. In this regard, relevant governmental departments should publicize the benefits of this technology through typical case interviews, comparative experimental reports, and so on, and emphasize its effectiveness in preventing COVID-19. Furthermore, it is necessary to eliminate the public’s perception of the risks of this technology as much as possible. For instance, the benefits of vaccination technology can be shown to the public through scientific experiments or live interaction via various sorts of media such as television channels, public service advertisements, and so on. In addition, the media can also be used to interview vaccinated people of different genders and different age groups on their physical reactions and changes over a period of time, which assists the public to reduce their perception of various potential risks of vaccination. Second, the governments and related policy-making institutions should give full play to the role of action cues to facilitate vaccine adoption. In this regard, medical and scientific research departments need to strengthen their clinical exploration of vaccination technology and continuously work to improve it. Through continuous research and development, relevant authorities can announce the progress in this area to the public in order to increase their cognition of vaccination. At the same time, the improvement of vaccination technology can also promote doctors’ recommendations for the public to adopt vaccination. These factors will have a positive influence on vaccine adoption.
Limitations and future research
First, a major limitation of this study is that we conducted data collection in China. COVID-19 in China is longer as serious as it was during the start of the pandemic. Moreover, vaccine development in this country is at the forefront of the world, according to the rates of vaccination. Therefore, the findings of this study may not be applicable to those countries where the epidemic is severe and vaccination technology is not as advanced, such as India. Second, an important reason for the public to adopt vaccination is the convenience of travel. Therefore, research related to this, such as the vaccine passport initiative, could be a future research direction. Third, the perceived barrier to vaccination is also a necessary precursor to behavior intention in the HBM. Researchers can explore this issue in the future. Fourth, this study did not investigate the unvaccinated population, and the individuals who participated in the online survey were relatively young. Hence, researchers can conduct empirical analyses on the unvaccinated populations and broader age populations to obtain novel and valuable conclusions.
Funding Statement
This paper was supported by the Natural Science Foundation of Shandong Province (ZR2021MH388), Qingdao Key Health Discipline Development Fund and Qingdao Clinical Research Center for Oral Diseases (22-3-7-lczx-7-nsh).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethics approval and consent to participate
A sample was selected to receive the invitation for the survey. An anonymous self-administered questionnaire was voluntarily answered. We didn’t ask for a separate written informed consent because of anonymity. Individual participation in the survey was considered as informed consent. This study was approved by the Ethics Committee of Qingdao University of Technology (QUT20210225) in China.
References
- 1.Dhama K, Sharun K, Tiwari R, Dadar M, Malik YS, Singh KP, Chaicumpa W.. COVID-19, an emerging coronavirus infection: Advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Hum Vaccin Immunother. 2020;16(6):1–10. doi: 10.1080/21645515.2020.1735227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu WL, Zou H, Song Y, Ren LL, Xu YJ. Understanding the continuous vaccination of the COVID-19 vaccine: an empirical study from China. Hum Vaccin Immunother. 2021;17(12):1–10. doi: 10.1080/21645515.2021.2013080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu FC, Guan XH, Li YH, Huang JY, Jiang T, Hou LH, Li JX, Yang BF, Wang L, Wang WJ. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2020;396(10249):479–488. doi: 10.1016/S0140-6736(20)31605-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JH, Marks F, Clemens JD. Looking beyond COVID-19 vaccine phase 3 trials. Nat Med. 2021;27(2):205–211. doi: 10.1038/s41591-021-01230-y. [DOI] [PubMed] [Google Scholar]
- 5.MedSci . Bulletin of global COVID-19 and vaccination on October 18, 2021. [accessed 2021 Oct 30]. https://www.medsci.cn/article/show_article.do?id=79a3218e95fd.
- 6.MedSci . Bulletin of global COVID-19 and vaccination on October 19, 2021. [accessed 2021 Oct 30]. https://www.medsci.cn/article/show_article.do?id=78b82188e0bc.
- 7.Chinadaily . COVID-19 vaccine: Answers to frequently asked questions. [accessed 2021 Oct 30]. http://www.chinadaily.com.cn/m/shanghai/jiading/2021-01/12/content_37542334.htm.
- 8.Papagiannis D, Rachiotis G, Malli F, Papathanasiou IV, Kotsiou O, Fradelos EC, Giannakopoulos K, Gourgoulianis KI. Acceptability of COVID-19 vaccination among Greek health professionals. Vaccines. 2021;9(3):200. doi: 10.3390/vaccines9030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Marc GP, Moreira ED, Zerbini C. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. New Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front Public Health. 2021;9:34. doi: 10.3389/fpubh.2021.632914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salmon D, Opel DJ, Dudley MZ, Brewer J, Breiman R. Reflections on governance, communication, and equity: challenges and opportunities in COVID-19 vaccination: article examines the engagement and communication steps necessary to strengthen the COVID-19 vaccine roll out by federal, state, and local governments. Health Affair. 2021;40(3):419–425. doi: 10.1377/hlthaff.2020.02254. [DOI] [PubMed] [Google Scholar]
- 12.Sah R, Shrestha S, Mehta R, Sah SK, Raaban AR, Dharma K, Rodriguez-Morales AJ. AZD1222 (Covishield) vaccination for COVID-19: experiences, challenges and solutions in Nepal. Travel Med Infect Di. 2021;40:101989. doi: 10.1016/j.tmaid.2021.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaur SP, Gupta V. COVID-19 vaccine: a comprehensive status report. Virus Res. 2020:198114. doi: 10.1016/j.virusres.2020.198114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ng N, Kankanhalli A, Xu YC. Studying users’ computer security behavior: a health belief perspective. Decis Support Syst. 2009;46(4):815–825. doi: 10.1016/j.dss.2008.11.010. [DOI] [Google Scholar]
- 15.Champion VL, Skinner CS. The health belief model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. Vol. 4. 4th ed. Jossey-Bass:San Francisco, USA; 2008. p. 45–65. [Google Scholar]
- 16.Sun Y, Wang N, Guo X, Peng Z. Understanding the acceptance of mobile health services: a comparison and integration of alternative models. J Electron Commer Re. 2013;14(2):183. doi: 10.1108/10662241311331781. [DOI] [Google Scholar]
- 17.Mukhtar S. Mental health and emotional impact of COVID-19: applying health belief model for medical staff to general public of Pakistan. Brain Behav Immun. 2020;87:28–29. doi: 10.1016/j.bbi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peter JP, Tarpey SL. A comparative analysis of three consumer decision strategies. J Consum Res. 1975;2(1):29–37. doi: 10.1086/208613. [DOI] [Google Scholar]
- 19.Goodwin NR. Economic meanings of trust and responsibility. Ann Arbor, MI: The University of Michigan Press; 1996. [Google Scholar]
- 20.Holbrook MB. Consumer value: a framework for analysis and research. London: Routledge Press; 1999. [Google Scholar]
- 21.Ozturk AB, Bilgihan A, Salehi-Esfahani S, Hua N. Understanding the mobile payment technology acceptance based on valence theory: a case of restaurant transactions. Int J Contemp Hosp M. 2017;29(8):2027–2049. doi: 10.1108/IJCHM-04-2016-0192. [DOI] [Google Scholar]
- 22.Ghasemaghaei M. The role of positive and negative valence factors on the impact of bigness of data on big data analytics usage. Int J Inform Manage. 2020;50:395–404. doi: 10.1016/j.ijinfomgt.2018.12.011. [DOI] [Google Scholar]
- 23.Tarkang EE, Zotor FB. Application of the health belief model (HBM) in HIV prevention: a literature review. Cent Afr J Public Health. 2015;1(1):1–8. doi: 10.11648/j.cajph.20150101.11. [DOI] [Google Scholar]
- 24.Ahadzadeh AS, Sharif SP, Ong FS, Khong KW. Integrating health belief model and technology acceptance model: an investigation of health-related internet use. J Med Internet Res. 2015. doi;17(2):e3564. doi: 10.2196/jmir.3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quart. 1989;13(3):319–340. doi: 10.2307/249008. [DOI] [Google Scholar]
- 26.Orji R, Vassileva J, Mandryk R. Towards an effective health interventions design: an extension of the health belief model. Online J Public Health Inform. 2012;4(3). doi: 10.5210/ojphi.v4i3.4321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenstock IM, Strecher VJ, Becker MH. The health belief model and HIV risk behavior change. Preventing AIDS: Springer; 1994. p. 5–24. [Google Scholar]
- 28.Raheli H, Zarifian S, Yazdanpanah M. The power of the health belief model (HBM) to predict water demand management: a case study of farmers’ water conservation in Iran. J Environ Manage. 2020;263:110388. doi: 10.1016/j.jenvman.2020.110388. [DOI] [PubMed] [Google Scholar]
- 29.Valeeva N, Van Asseldonk M, Backus G. Perceived risk and strategy efficacy as motivators of risk management strategy adoption to prevent animal diseases in pig farming. Prev Vet Med. 2011;102(4):284–295. doi: 10.1016/j.prevetmed.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Vakili M, Rahaei Z, Nadrian H, YarMohammadi P. Determinants of oral health behaviors among high school students in shahrekord, Iran based on health promotion model. J Am Dent Assoc. doi2011; 85(1):39–48. [PubMed] [Google Scholar]
- 31.Mou J, Shin D-H, Cohen J. Health beliefs and the valence framework in health information seeking behaviors. Inform Technol Peopl. 2016;29(4):876–900. doi: 10.1108/ITP-06-2015-0140. [DOI] [Google Scholar]
- 32.Buglar ME, White KM, Robinson NG. The role of self-efficacy in dental patients’ brushing and flossing: testing an extended health belief model. Patient Educ Couns. 2010;78(2):269–272. doi: 10.1016/j.pec.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 33.Schmutz JB, Lei Z, Eppich WJ, Manser T. Reflection in the heat of the moment: the role of in‐action team reflexivity in health care emergency teams. J Organ Behav. 2018;39(6):749–765. doi: 10.1002/job.2299. [DOI] [Google Scholar]
- 34.Aggarwal N, Albert LJ, Hill TR, Rodan SA. Risk knowledge and concern as influences of purchase intention for internet of things devices. Technol Soc. 2020;62:101311. doi: 10.1016/j.techsoc.2020.101311. [DOI] [Google Scholar]
- 35.Rezaei R, Mianaji S. Using the health belief model to understand farmers’ intentions to engage in the on-farm food safety practices in Iran. J Agr Sci Tech-Iran. doi2019; 21(3):561–574. [Google Scholar]
- 36.Koloseni DN, Lee CY, Gan M-L. Understanding information security behaviours of Tanzanian government employees: a health belief model perspective. Int J Technol Hum in. 2019;15(1):15–32. doi: 10.4018/IJTHI.2019010102. [DOI] [Google Scholar]
- 37.Times G China helps developing nations’ access to COVID-19 vaccines. [accessed 2020 Dec 14]. https://www.globaltimes.cn/content/1209942.shtml.
- 38.Lee E, Han S, Jo SH. Consumer choice of on-demand mHealth app services: context and contents values using structural equation modeling. Int J Med Inform. 2017;97:229–238. doi: 10.1016/j.ijmedinf.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 39.Lee AY, Aaker JL. Bringing the frame into focus: the influence of regulatory fit on processing fluency and persuasion. J Pers Soc Psychol. 2004;86(2):205. doi: 10.1037/0022-3514.86.2.205. [DOI] [PubMed] [Google Scholar]
- 40.Fragkaki I, Maciejewski DF, Weijman EL, Feltes J, Cima M. Human responses to Covid-19: the role of optimism bias, perceived severity, and anxiety. Pers Indiv Differ. 2021;176:110781. doi: 10.1016/j.paid.2021.110781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wong LP, Alias H, Wong P-F, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vacc Immunother. 2020;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen G, Sm G, Eden D. Validation of a new general self-efficacy scale. Organ Res Methods. 2001;4(1):62–83. doi: 10.1080/17538068.2019.1680038. [DOI] [Google Scholar]
- 43.Su Z, Chengbo Z, Mackert M. Understanding the influenza vaccine as a consumer health technology: a structural equation model of motivation, behavioral expectation, and vaccine adoption. J Commun Healthc. 2019;12(3–4):170–179. doi: 10.1080/17538068.2019.1680038. [DOI] [Google Scholar]
- 44.Li L, Li J. Factors affecting young Chinese women’s intentions to uptake human papillomavirus vaccination: an extension of the theory of planned behavior model. Hum Vaccin Immunother. 2020;16(12):3123–3130. doi: 10.1080/21645515.2020.1779518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhou M, Qu S, Zhao L, Campy KS, Wang S. Parental perceptions of human papillomavirus vaccination in central China: the moderating role of socioeconomic factors. Hum Vaccin Immunother. 2019;15(7–8):1688–1696. doi: 10.1080/21645515.2018.1547605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao M, Liu H, Qu S, He L, Campy KS. Factors associated with parental acceptance of influenza vaccination for their children: the evidence from four cities of China. Hum Vaccin Immunother. 2021;17(2):457–464. doi: 10.1080/21645515.2020.1771988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fan CW, Chen IH, Ko NY, Yen CF, Lin CY, Griffiths MD, Pakpour AH. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: an online survey study. Hum Vaccin Immunother. 2021;17(10):1–8. doi: 10.1080/21645515.2021.1933687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou M, Zhao L, Kong N, Campy KS, Wang S, Qu S. Predicting behavioral intentions to children vaccination among Chinese parents: an extended TPB model. Hum Vaccin Immunother. 2018;14(11):2748–2754. doi: 10.1080/21645515.2018.1496765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jongen VW, van der Loeff MFS, Boyd A, Petrignani M, Prins M, van der Wal M, Nielen A, de Melker H, Tgwm P, Alberts CJ. Human papillomavirus vaccination uptake: a longitudinal study showing ethnic differences in the influence of the intention-to-vaccinate among parent-daughter dyads. Hum Vaccin Immunother. 2021;17(4):990–999. doi: 10.1080/21645515.2020.1808411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoque R, Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: an extension of the UTAUT model. Int J Med Inform. 2017;101:75–84. doi: 10.1016/j.ijmedinf.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 51.Zhu WL, Mou J, Benyoucef M. Exploring purchase intention in cross-border e-commerce: a three stage model. J Retail Consum Serv. 2019;51:320–330. doi: 10.1016/j.jretconser.2019.07.004. [DOI] [Google Scholar]
- 52.Wei J, Vinnikova A, Lu L, Xu J. Understanding and predicting the adoption of fitness mobile apps: evidence from China. Health Commun. 2021;36(8):950–961. doi: 10.1080/10410236.2020.1724637. [DOI] [PubMed] [Google Scholar]
- 53.Deng Z. Understanding public users’ adoption of mobile health service. Int J Mob Commun. 2013;11(4):351–373. doi: 10.1504/IJMC.2013.055748. [DOI] [Google Scholar]
- 54.Benight CC, Bandura A. Social cognitive theory of posttraumatic recovery: the role of perceived self-efficacy. Behav Res Ther. 2004;42(10):1129–1148. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]


