ABSTRACT
Vaccination has proven to be the most effective tool in controlling the COVID-19 pandemic. While pregnant individuals are considered to be a high-risk population and are more likely to experience adverse effects from COVID-19, vaccination rates among pregnant individuals are significantly lower than in the general population. The Health Belief Model (HBM), Theory of Planned Behavior (TPB), 3C model, 5C model, and 5A model have been used to assess vaccination hesitancy behaviors. In this paper, we review the use of each of these models to address vaccine hesitancy, with a focus on the pregnant population and the COVID-19 vaccine. The HBM, TPB, 3C model, and 5C model have demonstrated great versatility in their ability to evaluate, explain, and modify vaccine hesitancy and behavior. Up to date, the HBM and 3C models appear to be the most effective models to study and address vaccination hesitancy within the pregnant persons.
KEYWORDS: Vaccine hesitancy, health belief model, theory of planned behavior, 3C model, 5C model, 5A model, pregnancy
Introduction
As the impact of the COVID-19 pandemic continues to evolve, it has become clear that our greatest tool in controlling the virus is vaccination. Fully vaccinated individuals have a decreased risk of contracting COVID-19, and if they do become infected, the risk of severe illness and hospitalization is substantially reduced.1 This is especially relevant for at-risk groups such as pregnant persons. Research has shown that pregnant persons diagnosed with COVID-19 are more likely to have higher maternal morbidity and mortality, including higher rates of preeclampsia, preterm birth, and maternal mortality.2 Additionally, newborns of persons with COVID-19 have significantly higher severe perinatal morbidity and mortality compared with newborns of persons without a COVID-19 diagnosis.2 Pregnant persons who were vaccinated against COVID-19 infection had a reduction in severe COVID-19 infection, if they got infected, and reduction in perinatal death, and in COVID-19-related hospitalization among infants of up to 6 months of age.3–7 According to the CDC, as of May 2022, over 205,000 pregnant persons were diagnosed with COVID-19, over 32,000 were hospitalized, and over 290 died from complications due to COVID-19.8 However, vaccination of this population remains low—only 69.5% of the pregnant persons are fully vaccinated.8 Additionally, Black pregnant persons, who have some of the highest rates of maternal and fetal morbidity and mortality,9 are the least protected, with only 54.2% fully vaccinated against COVID-19.1 Similar findings were seen in countries outside the US, with over 90% of COVID-19 infection-related hospitalizations and 98% of critical care admissions occurring in unvaccinated pregnant persons.10,11
The importance of understanding vaccination behavior and vaccine hesitancy, defined as delay in acceptance or refusal of vaccination despite the availability of vaccination services,12 has become more important now than ever. Various models have been used to assess vaccine hesitancy including the Health Belief Model, Theory of Planned Behavior, the 3C model, and
more.12–15 The aim of this paper is to review models that have been applied to research addressing vaccine hesitancy, with a focus on pregnant persons.
Models to address vaccine hesitancy
1. Health belief model
The Health Belief Model (HBM) (Figure 1) is one of the most widely employed theories to understand health behaviors and how they correlate with preventive behaviors.13 In its original form, the model aimed to explain the health behaviors of people failing to undergo screening tests for early detection of disease, as well as, the failure of people to take preventative measures such as vaccinations against disease.13 Since its creation, the model has been revised and expanded to include behavioral responses to health-related conditions and more fully explain conceptual relationships.16 The model assumes a perception that an adverse health condition can be avoided, that by following advice an adverse health condition can be averted, and that individuals are able to be convinced to adhere to a recommended behavior.17 The HBM also assumes that existing beliefs can predict future behaviors. When applied to disease prevention, it suggests that a future behavior can be predicted by the combination of an individual’s willingness to prevent an illness and their expectations of a specific action.13
Figure 1.
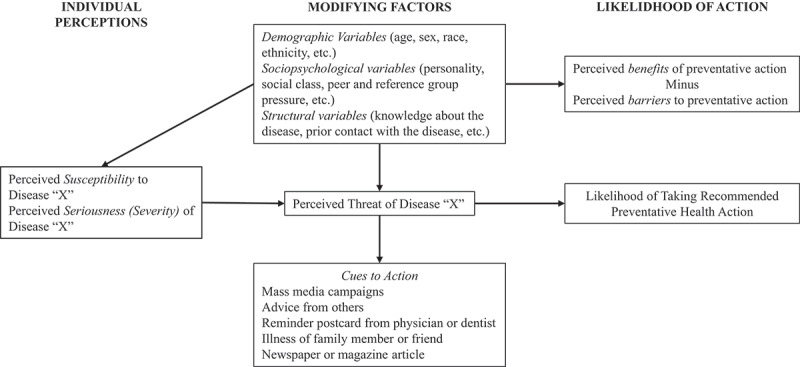
The “Health Belief Model.” Figure reproduced from Rosenstock, Health Education Monographs, 1974.13 Model details the individual perceptions and modifying factors that influence the likelihood of action regarding vaccination behaviors.
The HBM is composed of six constructs: perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy. Perceived susceptibility refers to an individual’s belief about their vulnerability to infection, i.e., the risk of acquiring COVID-19 infection. There is a wide variation in a person’s feelings of personal vulnerability to COVID-19 infection. Perceived severity refers to and individual’s belief that a disease is dangerous and has serious consequences. There is a wide variation in a person’s feelings of severity, and often a person considers the medical consequences (e.g., death and disability) and social consequences (e.g., family life and social relationships) when evaluating the severity of the possible COVID-19 infection on their life. Perceived benefits refer to an individual’s belief about the usefulness of a behavior and its ability to decrease the risk of severity of an adverse health outcome. The course of action a person takes in order to prevent COVID-19 infection is based on consideration and evaluation of perceived benefits of the COVID-19 vaccine. Perceived barriers refer to an individual’s belief about obstacles that may prevent individuals from performing a health behavior. In the case of COVID-19 vaccination, persons would weigh the effectiveness and safety of the vaccine, and the logistics, convenience, or discomfort of getting vaccinated. Cues to action refer to factors that may influence a behavior change. These factors may include information, people (obstetric provider recommending the vaccine), news (reading a new study about COVID-19 vaccination or COVID-19 illness in pregnancy), or events (friend of a family member getting severe COVID-19 infection). Self-efficacy refers to an individual’s trust in their ability to enact change and successfully perform the health behavior, in this case, vaccination against COVID-19.18–20 For change to be enacted, individuals must feel motivated to make change based off their perceived susceptibility/severity of the health treatment, their positive interactions with cues to action, and the benefits must outweigh the barriers.
Use of the HBM to promote vaccine uptake in non-pregnant individuals
The utility of the HBM in addressing vaccine hesitancy has been validated in diverse patient populations, vaccine types, countries, and modalities.16–18 The HBM has evaluated vaccine hesitancy in many subjects, including patients, physicians, and parents. In a study evaluating physician attitudes, HBM was used to evaluate physician likelihood of recommending vaccinations.21 It has also been used to assess pharmacists’ and other health-care workers’ vaccine acceptance and hesitancy.22–26 Studies have used the HBM to assess parent attitudes toward childhood vaccinations.27–32 Globally, the HBM has been used to assess general vaccine hesitancy in Nigeria,33 the United States,29 and Korea;30 measles and rubella vaccines in Romania and Japan;27,34 shingles vaccines in the United Kingdom;35 influenza vaccines in the United States,36–39 Japan,27 and Australia;40 human papilloma virus vaccines in the United States;28,31,41–48 and COVID-19 vaccines in the United States,21,44–46 China,47–53 Bangladesh,54–56 Turkey,22 Canada,23 Vietnam,57 France,58 Saudi Arabia,59 and Pakistan.60 Several other studies applied HBM to create interventions to increase vaccine knowledge and uptake,16 and to create new scales of vaccine attitudes and intentions to assess the effectiveness of health campaigns and advertising.21,30,31
Use of the HBM in pregnant individuals
The HBM has been applied to several studies investigating predictors of maternal vaccination to influenza,61 COVID-19,61 pertussis,62–65 Hepatitis B,66 Zika,67 Tdap,65,68 and H1N1.69,70 It was found that mothers were more likely to receive vaccinations in order to provide their newborn immunity and due to the provision of antibodies.49 Recommendation of vaccination from a provider was the most influential factor in increasing vaccination.71 When assessing the barriers to vaccination, pregnant individuals who believed that seasonal vaccination was not safe during pregnancy or not effective in protecting their fetus had lower levels of vaccine acceptance for both the influenza and pertussis vaccines.47,62 In addition, gestational age was identified as an important predictor of maternal vaccination and testing.64
Use of the HBM in COVID-19 vaccination uptake in non-pregnant individuals
The HBM has been used to study COVID-19 vaccination attitudes in a variety of populations. While it has been used to study the attitudes of the general population in a multitude of countries,46,53,54,58,59,72 it has also been used to evaluate various subpopulations. The most common subpopulation that has been evaluated has been health-care workers. Several studies have sought to identify and understand the beliefs of physicians, pharmacists, nurses, and health-care workers in general, in both their intent to get vaccinated themselves and their intent to recommend vaccination to others.22–26 One study compared health-care workers to different occupational groups of varying occupational risk of COVID-19 infection as classified by public health officials, and found that health-care workers (the high-risk group) had significantly higher scores for cue to action and lower scores for perceived barriers compared to the other groups.73 Another study compared the general population to health-care workers and found that health-care workers perceived significantly higher susceptibility and severity of the COVID-19 infection compared to the general population.26 In addition to health-care workers, the HBM has also been used to evaluate cultural and racial subgroups,45 health science students,57 and mothers.50,74 Between primarily African American and Latinx subgroups, mistrust, fear, and lack of information were the main themes regarding COVID-19 vaccine hesitancy.45 These themes were then contextualized within the HBM constructs in which mistrust was identified with perceived barriers, fear was identified with perceived susceptibility and severity, and lack of information was identified with perceived severity and barriers.41 In a study assessing health science students, vaccine intention was significantly related to perceived susceptibility, perceived severity, benefits of vaccination, and cues to action.53 In the studies exploring non-pregnant mothers’ willingness to vaccinate their children, hesitancy was found to be associated with decreased perceived susceptibility, benefit, and severity as well as increased perceived barriers.39 It was also found that previous vaccine behaviors and attitudes did not fully predict a mother’s willingness to vaccinate their children for COVID-19.71 The most commonly identified barrier to COVID-19 vaccination noted in the literature was concern for side effects or adverse effects.24,26,51,72,73 Concerns about vaccine safety and effectiveness were also noted as barriers in multiple studies.24,26,51,73 The most notable cues to action related to recommendation of the vaccine from the leading authorities or trustworthy individuals including the government,72,73 media,26,55,73 medical experts,26,73 and the World Health Organization.26
In the employment of the HBM in COVID-19 vaccination uptake, the model was used to hypothesize effective strategies to overcome vaccination hesitancy and influence behavioral change interventions.46 A study evaluating the ability of communication strategies to modify COVID-19 vaccination hesitancy suggested that willingness to be vaccinated is influenced by the media and public service messages, especially emotionally- and fear-centered public service messages.60 Multiple studies in which participants demonstrated a low level of perceived susceptibility to COVID-19 recommended efforts to enhance public education of the probability of outbreak resurgence and the real susceptibility to COVID-19.46,50,52,53 Another study highlighted the importance of physicians in the cue-to-action role and recommended that physicians promote vaccination uptake in targeted campaigns.54 Overall, the studies recommended that the HBM constructs may be used to develop targeted communication campaigns to increase vaccine behaviors.
Use of the HBM in COVID-19 vaccination uptake in pregnant individuals
The HBM has been explored in COVID-19 vaccine acceptance among pregnant Chinese individuals.48 Higher acceptance was associated with high knowledge score on COVID-19, high level of perceived susceptibility, low level of perceived barriers to vaccination, high level of perceived benefit, and high level of perceived cues to action.48 Individual’s reasoning for declining COVID-19 vaccination included concerns about side effects, safety, and efficacy of the COVID-19 vaccination both for themselves and their unborn child. This information was used to influence efforts to increase vaccination rates among the pregnant population.48 A recent study examined the performance of HBM among pregnant individuals in Iran found that perceived benefits and cues to action components of HBM had significant effects on vaccine hesitancy, while the perceived threat component has no significant effect on it.75
Performance of the HBM with annual vaccines versus vaccines given once or twice
The HBM has been used to explore vaccine attitudes about vaccinations with various schedules. The model has been used to assess annual vaccinations;36,40 vaccinations given a few times, such as the human papillomavirus vaccination;28,41 and the childhood vaccination schedule.29,32 While most studies analyze the behaviors of one method of vaccination schedule, a study in Japan explored attitudes toward both influenza and rubella vaccination in tandem.27 This study employed constructs of the HBM to assess how receiving risk information and advice from peers and family members influences individuals’ decision-making regarding vaccines. Regarding rubella vaccination, susceptibility information and minor risk information led to the greatest increase in intent to be vaccinated, while severe risk information decreased intent. Likewise, intent to receive influenza vaccination increased after participants were provided minor risk information, susceptibility information, and peer advice.27
The HBM has been used to explore vaccination beliefs about a variety of vaccinations that are given a few times. This includes but is not limited to measles,34 human papillomavirus,28,31,41–43 and shingles.35 Similar to its use in the COVID-19 literature, the HBM has been used to examine behaviors and attitudes that make an individual more or less likely to accept the HPV vaccine.28,41,42 These studies were able to identify the trend of social media content related to HPV vaccinations and the presence of HBM constructs within the content to inform efforts to improve vaccine understanding and intent.
The HBM has also been used to evaluate vaccine hesitancy in relation to annual vaccinations, such as influenza. As with all other vaccinations, the model has been used to predict and assess vaccine hesitancy and acceptance behaviors in addition to identifying barriers. Tweets from the 2018–2019 influenza season were also analyzed based on their inclusion of HBM constructs, similar to the social media analysis of the HPV vaccination. Interestingly, tweets in the early flu season were more likely to discuss vaccine uptake self-efficacy, while tweets in the peak flu season were more likely to mention susceptibility to the flu and barriers to vaccination.38
2. Theory of planned behavior model
The Theory of Planned Behavior (TPB) (Figure 2) is built upon the belief that an individual’s decision to engage in a behavior can be predicted by their intention to engage in that behavior.14 The theory suggests that attitudes, subjective norms, and perceived behavioral control predict an individual’s intention to engage in a health behavior.76 In succession, the intention to engage in a healthy behavior is the best predictor of an individual performing said behavior.14,77 The theory depends upon the assumption that people have the ability to practice self-control when moderating their behavior.14
Figure 2.
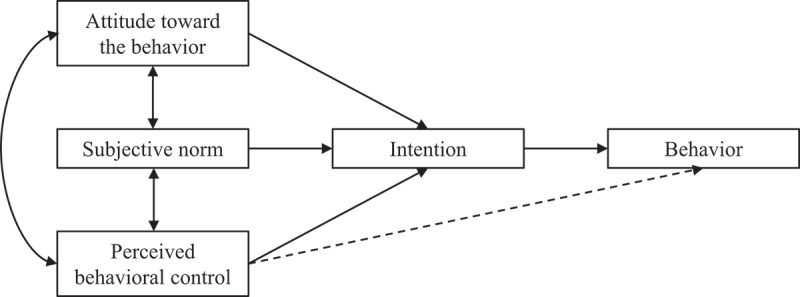
Theory of Planned Behavior. Figure reproduced from Ajzen, Organizational Behavior and Human Decision Processes, 1991.14 Figure details the relationship between various constructs and their ability to influence vaccination intention and overall behavior.
The TPB relies on three constructs: attitudes, subjective norms, and perceived behavioral control. Attitudes refer to an individual’s assessment of the favorableness of an action including its necessity, benefit, and effectiveness.78,79 Subjective norms refer to an individual’s measure of perceived social pressure to perform a behavior based on the opinion of others and how much value one places in other’s opinions.76 This construct may include family, friends, health-care professionals, social media, and mainstream media.78 Perceived behavioral control refers to an individual’s perception of their capability of performing a given behavior. Perceived behavioral control is a combination of both perceived control and self-efficacy and has both a direct and an indirect effect on behavior, through its effects on intentions.80,81 Altogether, the TPB assumes a positive correlation between an individual’s attitudes, social norms, and perceived behavior control and increased intention to perform a behavior, which in turn, results in greater health behavior performance.14,77
Use of the TPB to promote vaccine uptake in non-pregnant individuals
The TPB has been used as a tool to assess vaccine hesitancy in a multitude of vaccinations globally. The TPB has been used to evaluate general and childhood vaccine hesitancy in Italy,82 China,83 Canada,84 and the United States;85 influenza vaccination in the United States;74,86–88 HPV vaccination in the United States;41,89 Hepatitis B vaccination in Uganda;66 Swine Flu vaccination in the United Kingdom;90 the Boostrix-IPV vaccination in the United Kingdom;91 and COVID-19 vaccination in the United States,46,92 Bangladesh,54–56 Ireland,93 New Zealand,94 Pakistan,95 and Malta.96 While this list is not conclusive, it begins to illustrate the versatility and usability of the TPB.
In addition to informing and structuring study questionnaires, the TPB has been utilized diversely. It has provided the foundation for a behavioral analysis approach to examining vaccination acceptance and guided the development of research questions to evaluate vaccination behavior.56,97 In addition, the TPB has been used to develop interview questions for studies, including one study that used motivational interviewing techniques in attempts to decrease vaccine hesitancy.98 The TPB has also been used as a guide for literature reviews exploring vaccination intention.85
Use of the TPB model in pregnant individuals
The TPB has been used to assess pregnant individual’s vaccine intention and behaviors.66,71,90,91 In a literature review that explored predictors of maternal vaccination, the TPB model was used in eight of twelve reviewed studies that were theoretically based.71 The model is used to explore pregnant individual’s beliefs about the Boostrix-IPV,91 influenza,76 hepatitis B,66 and swine flu vaccinations.90
Repeatedly in the literature, the TPB is found to be a validated measure of pregnant individual’s intentions to get vaccinated. In a study exploring women’s hesitancy about the Boostrix-IPV vaccination, the TPB predicted 86% of the variance in vaccine intentions, with subjective norms and attitudes being the best predictors. In regard to vaccine behavior, the model accounted for 36% of the variance.91 In another study, which evaluated pregnant individual’s intent to receive the swine flu vaccination, the TPB explained 66% of the variance in intention to be vaccinated. In this study, attitude, subjective norm, and perceived control were all found to be predicative of vaccination intention.90
While the TPB has been found to be predictive of vaccination intention in pregnant individuals, multiple studies have expressed concerns about the model. One study highlighted that the theory was better at predicting vaccination intent than vaccination behavior and emphasized that public health interventions are more commonly built upon vaccination behavior.91 This same study also highlighted that the TPB does not account for all variables contributing to vaccine behavior and suggested that further work may need to be done to explore these variables.91
Use of the TPB model in COVID-19 vaccination uptake in non-pregnant individuals
Within the literature that explores the TPB and COVID-19, the relationship is bidirectional. The literature supports that the TPB is a validated measure to explore COVID-19 vaccine hesitancy.93 Conversely, the literature also supports that attitudes and behaviors toward the COVID-19 vaccine support the TPB.96 In multiple studies, attitudes, subjective norms, and perceived behavioral control were found to have a significant impact on vaccination intent and behavior.93–95 In one study, the constructs of the TPB accounted for 74% of variance in COVID-19 vaccination intention.95 In a study that evaluated multiple assessments of vaccination hesitancy, the TPB was found to have the highest predictive power of COVID-19 vaccination hesitancy.55
The authors suggested that the constructs of the TPB may be beneficial in the development of COVID-19 vaccination public health messages and efforts to improve vaccination uptake.46,93 While the TPB has been used to assess vaccination hesitancy, the application of TPB in promoting COVID-19 vaccine acceptance and uptake has not been tested.
Use of the TPB model in COVID-19 vaccination uptake in pregnant individuals
The use of the TPB model to address COVID-19 vaccine hesitancy and acceptance among pregnant individuals has not been investigated to-date in this review.
Performance of the TPB model with annual vaccines versus vaccines given once or twice
The TPB has been used to assess vaccination hesitancy related to vaccines given at various intervals, including both annuals and vaccines that are given a few times. While most studies analyze one type of vaccine schedule, one study analyzed both annual vaccinations and vaccines that are given once or twice. This study focused on the subjective norm construct from the TPB and found that subjective norms were associated with vaccination intention.97
For vaccines that are given on a few occasions, the TPB has been used to investigate vaccine hesitancy about the human papillomavirus vaccine.41,89 Both attitudes and subjective norms were found to be predictive of vaccination behavior.89 One study addressed how the constructs of TPB and behavioral intentions may vary based on patient knowledge regarding the HPV vaccination. The authors found that different types of knowledge about HPV and the vaccine (genders affected, HPV manifestations, vaccine efficacy, etc.) have different associations with the TPB constructs and ultimately the intention to be vaccinated.89 The other study exploring the TPB and HPV evaluated social media discussions in relation to the vaccination. The attitude construct from TPB was used to analyze social media posts and discussions and observe trends about the vaccination.41
The TPB has also been used to evaluate vaccination hesitancy for vaccines given annually, specifically the influenza vaccination. Attitude and subjective norms have both been found to be significant predictors of an individual’s intention to receive the influenza vaccination.87 In this study, a doctor’s influence was the strongest subjective norm identified.87 In a study that assessed barriers to receiving the influenza vaccination, the negative attitudes (a TPB construct) were amongst the most frequently reported barriers.88 The perception that receiving the influenza vaccination was not the norm in a peer group was also a frequently reported barrier.88
3. The 3C model
In 2012, the Strategic Advisory Group of Experts on Immunization (SAGE) established the SAGE Working Group on Vaccine Hesitancy in response to the globally low levels of vaccine uptake and the negative impacts of vaccine hesitancy.12 The group was tasked with establishing a definition for vaccine hesitancy as well as a working model of determinants. The Working Group created a model to explain the factors influencing vaccine hesitant behavior (Figure 3).99 The first model, the Working Group Matrix, is more comprehensive and better able to capture the complex factors influencing vaccine behavior. This model groups determinants of vaccine hesitancy into three categories: Contextual influences, Individual and Group influences, and Vaccine/Vaccination specific issues. This matrix was determined to be comprehensive as a systemic review of studies on vaccine hesitancy, and a survey of immunization managers found no other determinants.99,100
Figure 3.
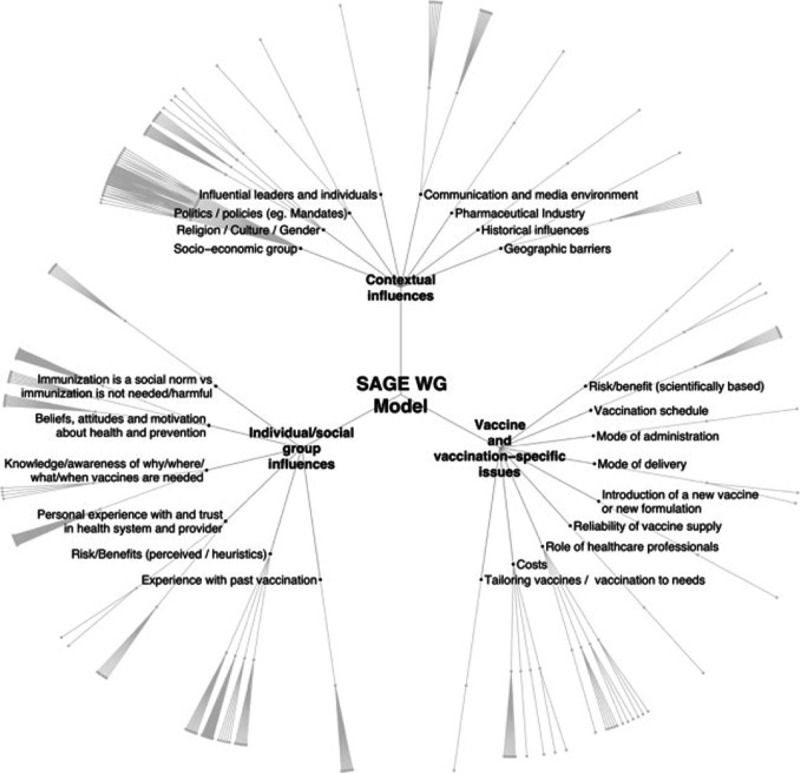
SAGE Working Group Matrix of Vaccine Hesitancy. Figure reproduced from Larson, Jarrett, Eckersberger, Smith, and Paterson, Vaccine, 2014.99 Figure demonstrates the determinants of vaccine hesitancy as laid out by the SAGE Working Group.
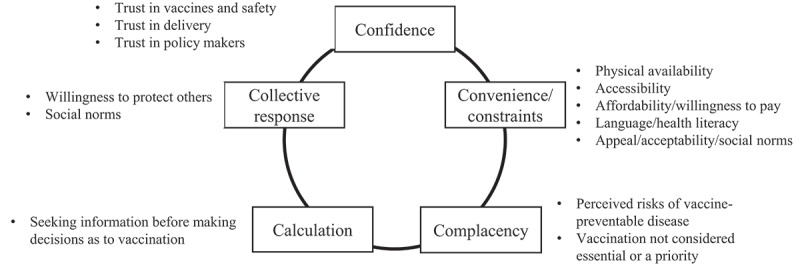
Subsequently, the group simplified the model for practical use and named it the 3C model, after Complacency, Convenience, and Confidence, the three factors most substantially contributing to vaccine behavior (Figure 4).12 Complacency is present when “perceived risks of vaccine-preventable diseases are low and therefore vaccination is not deemed a necessary preventative action.”12 Convenience measures the degree to which an individual’s ability to obtain vaccines is affected by “physical availability, affordability and willingness-to-pay, geographical accessibility, ability to understand (language and health literacy) and appeal of immunization service affect uptake.”12 Ineffective or inconvenient delivery of vaccination services was associated with increased vaccine hesitancy. Confidence is defined as “trust in (i) the effectiveness and safety of vaccines, (ii) the system that delivers them, including the reliability and competence of the health services and health professionals, and (iii) the motivations of policy-makers who decide on the need of vaccines.”5 Confidence is associated with low levels of vaccine hesitancy.
Figure 4.
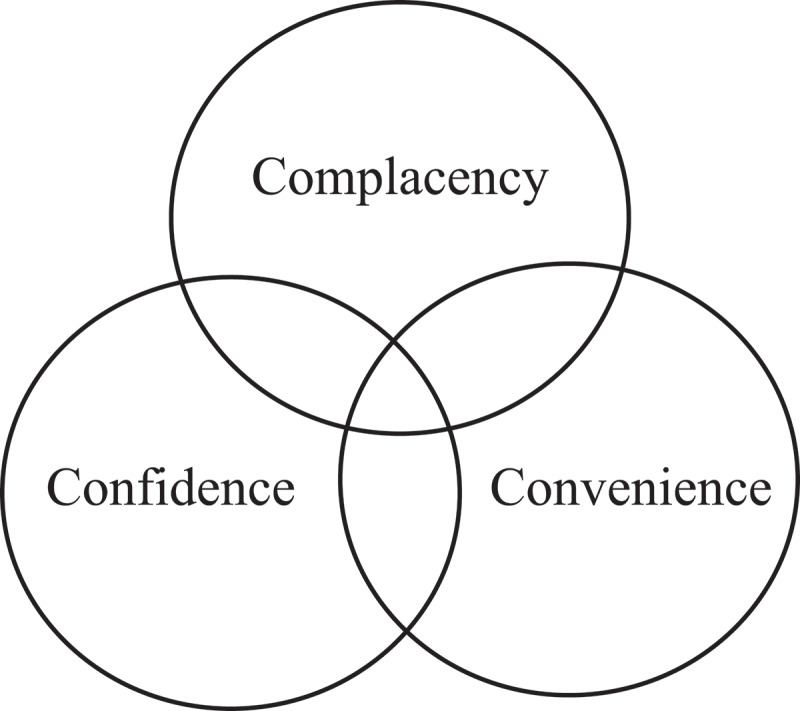
3C model. Figure reproduced from the World Health Organization’s SAGE vaccine hesitancy Working Group, Report of the SAGE working group on vaccine hesitancy, 2014.12 Figure demonstrates the factors that contribute to the 3C model.
With both models, the Working Group noted that vaccine hesitancy is complex and can vary depending on the contextual time and place.12,101 Additionally, while these models provide a framework through which to view vaccine behavior, there is no specific measure associated with the 3C model or the Working Group Matrix-outside of a metric for parental vaccine hesitancy.
Use of the 3C model to promote vaccine uptake in non-pregnant individuals
The establishment of the 3C model and the Working Group Matrix have been beneficial for interpreting vaccination intention and behavior. Application of the 3C model has also been used to better understand vaccine hesitancy globally and to formulate interventions aimed at targeting various aspects of confidence, complacency, and/or convenience. Research has applied this model to better understand hesitancy in measles vaccines,102,103 among health-care workers and students,104–107 as well as for general childhood vaccination in Tajikistan.108 There has also been research using the 3C model to create and analyze vaccine hesitancy interventions.109,110
A large systematic review of the 3C model use in vaccine hesitancy found that safety concerns, questions about vaccine effectiveness, and distrust in health-care authorities accounted for a large part of vaccine hesitancy reported throughout the literature, indicating that low levels of confidence likely play a significant role in vaccine behavior.88 A narrative review of vaccine hesitancy among health-care workers found similar trends in vaccine hesitancy as in the general population- low confidence and high complacency led to higher levels of hesitancy.111 Health-care workers with high hesitancy were less likely to be vaccinated and less likely to recommend vaccines to patients, highlighting the importance of decreasing vaccine hesitancy not only within patient populations, but the health-care system as well.111
Use of the 3C model in pregnant individuals
Systematic reviews of vaccine hesitancy within the pregnant and lactating population found that low vaccine confidence was a major barrier to receiving recommended vaccinations during pregnancy, with convenience playing a very limited role in attitudes toward vaccination.112,113 However, as highlighted in one of the reviews, the majority of research included in the reviews came from Western, high-income countries and may not be applicable globally.112
A qualitative study of high-risk groups in South America found that, across the board, low levels of vaccine confidence were a major contributor to vaccine hesitancy.114 However, in pregnant women, complacency also played a significant role. They found that many pregnant women did not consider themselves to be in a “high risk” group that contributed to complacency. A qualitative study of pregnant women’s perception of the Hepatitis B vaccine in Uganda found similar results.115 While low levels of confidence in health-care workers contributed to vaccine hesitancy, complacency due to limited knowledge of Hepatitis B also played a role.
The importance of geographical and cultural context when using the 3C model to understand vaccine hesitancy is highlighted here and emphasizes the need for more research into populations outside of the Western countries.
Use of the 3C model in COVID-19 vaccination uptake in non-pregnant individuals
The 3C model has also been used to a greater degree more recently in understanding COVID-19 vaccine attitudes. As with other vaccines, research has shown that low levels of confidence and convenience, and high levels of complacency, are associated with higher rates of COVID-19 vaccine hesitancy.116–120
While most of the studies on COVID-19 vaccine hesitancy used questionnaires to passively assess vaccine hesitancy,116–120 an experimental study in France found that they could decrease levels of complacency, and subsequently decrease levels of vaccine hesitancy, in the working age population by providing participants with information on herd immunity.21 Another study, looking at COVID-19,121*** explored the underpinnings of low confidence in health-care systems.122 Through their research, they found that health-care literacy was a key mediator in the relationship between health care distrust and vaccine hesitancy. Literature using the 3C model has also examined sociodemographic variations in COVID-19 vaccine hesitancy.123 Hesitancy due to low confidence and higher levels of circumspection (this study’s expansion on convenience) were primarily found in Black respondents- particularly in Black women who were found to have the highest rates of vaccine hesitancy of any group. However, this study also found that hesitancy among Black respondents declined faster than in other groups. While research into the COVID-19 vaccine has been rapidly carried out, as noted by the SAGE working group, vaccine hesitancy is complex. More research is needed in this area to better understand the needs of specific populations, such as pregnant and lactating individuals.
Use of the 3C model in COVID-19 vaccination uptake in pregnant individuals
Studies applying the 3C model to investigate COVID-19 vaccine acceptance among pregnant individuals have not been done to date of this review. However, research into COVID-19 vaccine hesitancy in the pregnant population has identified confidence in the vaccine as a key feature in vaccine acceptance in the US and UK.124,125
Performance of the 3C model with annual vaccines versus vaccines given once or twice
Research using the 3C model to compare general vaccine hesitancy to influenza-specific vaccine hesitancy found that one could not necessarily be substituted for the other.126 Looking at vaccination attitudes and behaviors of US adults, they found that high confidence and convenience and low complacency were associated with lower general vaccine hesitancy. High confidence in the flu-specific vaccine was associated with lower flu vaccine hesitancy and positively associated with rates of flu vaccination in the past year. However, higher general vaccine confidence was not associated with receiving the influenza vaccine for that given year, suggesting that general vaccine hesitancy or acceptance may be specific and unique to specific vaccines. Additional research into nursing home staff and influenza vaccinations suggest that the variability of influenza strains and misconceptions about the possible severity of infection can lead to low confidence and high complacency specific to this vaccine.105 These findings highlight the need for vaccine-specific analysis when utilizing this model.
4. The 5C model
The 5C model of vaccine hesitancy, proposed in 2018, expands the SAGE WHO’s 3C model to add Calculation and Collective Responsibility factors (Figure 5).127 The 5C model looks at psychological antecedents as a way to better understand an individual’s behavior, “going beyond confidence.”8 Calculation refers to information searching. Individuals engaging in information searching typically do so to conduct their own risk-benefit analysis and are assumed to be more risk averse. Due to the wide availability of vaccine misinformation, individuals with high levels of calculation have positive correlations with perceived vaccination risks and vaccine hesitancy.15 The calculation factor was added to the 3C model as a way to capture an individual’s motivation for thinking about and questioning vaccines.128 Collective responsibility is considered an individual’s “willingness to protect others by one’s own vaccination by means of herd immunity.”8 Individuals with high levels of collective responsibility will have higher levels of collectivism, communal orientation, and empathy. Those who have low levels of collective responsibility, either due to a lack of knowledge about herd immunity or unwillingness to protect others, will have positive correlations with vaccine hesitancy.
Figure 5.
The 5C Model. Figure reproduced from Turner, Larson, Dubé, and Fisher, Journal of Allergy and Clinical Immunology: In Practice, 2021.127 Figure details the five factors of the 5C model and the various elements that contribute to their composition.
The five factors uniquely interact in every individual to create a psychological state somewhere along the vaccine hesitancy spectrum. The authors of this model note that “the 5C antecedents provide insights in the individual, psychological antecedents and are not suitable to identify systems-related factors–beyond the effect they have on mental representations.”15 For example, low levels of confidence in one individual may be the result of their social environment, whereas for an individual in another country, it may be the result of mistrust in their health-care system. Therefore, the benefit of analyzing vaccination behavior through the 5C model is to better understand the psychological underpinnings behind an individual’s vaccine behavior. Further investigation is required to determine the factors informing that state. Doing so can help tailor strategies designed to promote vaccine uptake to specific individual groups by targeting a specific factor.
The 5C model provides both a short and long validated scale for assessing the psychological antecedents of vaccination behavior.15 While this model is available for adaptation and translation,129 some non-English speaking, low-income countries have found it difficult to adapt the scale.130
Use of the 5C model to promote vaccine uptake in non-pregnant individuals
Research using this model has explored the role of faith in one’s own intuition and the effects of decreasing complacency among target groups through the implementation of prosocial vaccination interventions.131,132 The 5C model has also been explored to understand the attitudes of physicians toward vaccination.133 Physicians with positive attitudes toward vaccine mandates have been found to generally have higher levels of confidence and collective responsibility. Physicians’ own vaccination behavior was also found to be significantly related to their recommendation of vaccines, with high levels of confidence in vaccines being associated with active recommendation.134 However, even within this group there were differences. Homeopathic physicians were found to have significantly lower confidence and higher complacency compared to other physicians, which influenced their vaccination recommendations.134 A qualitative study of health-care workers across Europe also found that confidence largely contributed to vaccine recommendation behavior but also noted that confidence varied widely across nations.135 The model has been applied to caregivers of children to assess willingness for vaccination against childhood diseases and Human Papilloma Virus in Malawi.130 The study found that confidence in vaccine safety was the strongest predictor of routine childhood immunization, followed by constraints due to everyday stress.130 In addition, a husband’s positive attitude increased childhood vaccination intention.130 This points to the importance of identifying local determinants of vaccine hesitancy to develop successful programs.
Use of the 5C model in pregnant individuals
Little research has been done using the 5C model as a means to understand vaccine hesitancy in pregnant and lactating individuals. Two studies were done using this model in pregnancy.136,137 Using the 5C model in the pregnant population was a proposal for a vaccine hesitancy intervention in the pregnant population in India.136 They propose administering the 5C scale at prenatal visits to identify individual patients’ unique behaviors and apply motivational interviewing techniques to address them in real time. However, the actual study has not yet been conducted. A study in Nigeria using the 5C model to understand drivers of vaccine hesitancy for themselves and their children concluded that the 5C model does not perform well in their population.137 Their intention to vaccinate unborn children was lower if they were Muslims, had lower confidence in the public health system, if husband approval was important, and if they believed in rumor. The authors concluded that the 5C scale needs a revision before being widely used in Nigeria.137
Use of the 5C model in COVID-19 vaccination uptake
The 5C model has been increasingly relevant in aiding our understanding of COVID-19 vaccine hesitancy. A technical report for the European Union on COVID-19 vaccine acceptance emphasized the importance of targeting different groups according to their specific needs in order to develop successful programs, using the 5C framework.138 Research using the 5C model in COVID-19 vaccination behavior has consistently shown that high confidence and collective responsibility were associated with lower levels of vaccine hesitancy, as is seen with other vaccinations.55,138–148 However, differences within groups were also found. For instance, for Japanese men specifically, constraints were significantly associated with COVID-19 vaccine intention, suggesting that convenience may be an important factor in their vaccination decisions.144 Additionally, a study of Israeli parents’ intent to vaccinate their children against COVID-19 found that in addition to higher confidence and collective responsibility, higher calculation was associated with vaccination intent.140
A recent study of Health Care Workers found that attitudes toward the COVID-19 vaccine were distinct from other vaccines, in that one could be generally accepting of vaccines but hesitant about the COVID-19 vaccine specifically.145
One study suggested using the 5C model to create profiles predicting COVID-19 vaccination intent and uptake to tailor interventions in nurses.147 The most likely to vaccinate were ‘Believers’ (high confidence and collective responsibility, low complacency, and constraint) and Contradictors (high on all 5C measures). In the middle were ‘Middlers’ (moderate on all 5C measures) and Outsiders (Low calculation and collective responsibility). Least likely were ‘Skeptics’ (low confidence and collective responsibility, high complacency, and constraint).
Use of the 5C model in COVID-19 vaccination uptake in pregnant individuals
Up to this date, no studies were done examining the 5C model for COVID-19 vaccine acceptance among pregnant individuals.
Performance of the 5C model with annual vaccines versus vaccines given once or twice
The 5 C model has been applied to both annual and single-dose vaccines.148,149 A study on the vaccination behaviors of the elderly population in the UK used this model to compare annual influenza vaccine to single pneumonia and shingles vaccines and found that low confidence, low collective responsibility, and high constraint and complacency predicted low uptake of the influenza vaccine.148 However, for the pneumonia and shingles vaccine, calculation was not a contributing factor in vaccine uptake. Another study looked specifically at the annual influenza vaccine among those with chronic respiratory conditions, finding that higher levels of collective responsibility and lower levels of constraints and complacency were associated with higher rates of vaccination.149
5. The 5A model
The 5A model was proposed by Thompson and colleagues in 2016 includes five barriers and facilitators of vaccine update: Access – the ability of individuals to be reached by or to reach the recommended vaccines; Affordability – the ability of individuals to afford the vaccine both from financial and non-financial aspect (e.g., time); Awareness – the degree to which individuals have knowledge of the need for the vaccine and vaccine’s objective benefits and risks; Acceptance – the degree to which individuals accept, question, or refuse the vaccine; and Activation – the degree to which individuals are nudged toward vaccination uptake.150
Use of the 5A model to promote vaccine uptake in non-pregnant individuals
A systematic review of vaccine uptake in the migrant population in Europe using the 5A model found multiple-access barriers to vaccination, including language, literary, and communication barriers.151 Acceptance barriers were mostly reported in easter European and Muslim migrants for HPV, MMR, and influenza vaccines. Another recent review examined the 5A model for non-COVID-19 vaccine uptake within Roma communities across Europe.152 In that study, access was identified as the greatest barrier to vaccination.
Use of the 5A model in pregnant individuals
Up-to-date, no studies were done examining the 5A model for vaccine acceptance among pregnant individuals.
Use of the 5A model in COVID-19 vaccination uptake
A mapping review of COVID-19 vaccine uptake among Adults 55 years and older in Africa with the 5A model taxonomy found that acceptance was the most commonly researched aspect of vaccine uptake (85%), followed by accessibility (25%), awareness (19%), and affordability (7%).153 Activation was examined in only one study as a factor affecting COVID-19 vaccine acceptance. The review concluded that more studies are needed to evaluate the impact of nudges (activation) to improve COVID-19 vaccine uptake in African nations.
Use of the 5A model in COVID-19 vaccination uptake in pregnant individuals
Up-to-date, no studies were done examining the 5A model for COVID-19 vaccine acceptance among pregnant individuals.
Conclusion
The HBM, TPB, 3C model, 5C model, and 5A model have demonstrated great versatility in their ability to evaluate, explain, and modify vaccine hesitancy and behavior. While each of these models have demonstrated success, the HBM and 3C models are the most effective for assessing vaccination hesitancy within pregnant individuals. Overall, the HBM is the most utilized model to address vaccination hesitancy. The 3C model is also widely used and has demonstrated great efficacy and thoroughness in its ability to assess vaccination hesitancy. These models have repeatedly proven their ability to holistically explain and create change within vaccination behaviors.
Multiple studies have expressed concern about the TPB’s ability to predict vaccination behavior in pregnant individuals. The model has been criticized for not fully accounting for all variables that may contribute to vaccination behavior. Additionally, the model is more likely to predict vaccination intent rather than actual vaccination behavior. Finally, the TPB has not been utilized to assess COVID-19 vaccination promotion and uptake; rather, it has only been used to assess vaccination hesitancy.
While the 5C model can be used to assess the psychological antecedents of vaccination behavior, it is not as efficacious as the HBM and 3C models. Some non-English speaking, low-income countries have found it difficult to adapt the scale used in the model even though it is available for adaptation and translation. Moreover, being a new model, 5C’s use and effectiveness has not been well investigated in pregnant individual.
We conclude that the HBM and 3C models are the most effective tools to study and address vaccination hesitancy within the pregnant population. As demonstrated in the literature, there is a need for increased vaccination within pregnant individuals. This is particularly important with the COVID-19 vaccine and boosters. Principles and constructs of the HBM and 3C models may be combined to create the most effective tool for assessing vaccine hesitancy in pregnant individuals. This tool could be used to both further understand vaccine hesitancy and promote vaccination behaviors within pregnant patients for a multitude of vaccinations. Since the vaccine roll out in December 2020, we have robust, high-quality data on tens of thousands of pregnancies confirming vaccine safety and benefits in protecting the mothers and their unborn children from severe COVID-19 illness. Promoting this evidence-based information to increase vaccine confidence and perceived benefits through HBM or 3C model is important next step to decrease COVID-19 vaccine hesitancy.
Funding Statement
Dr. Palatnik is supported by the American Heart Association [Career Development award 847482].
Highlights
Health Belief and 3C models are effective to study vaccine hesitancy in pregnancy
These models could be combined to address COVID-19 vaccine acceptance in pregnancy
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.COVID Data Tracker (CDC) . Centers for Disease control and prevention. 2020. [accessed 2022 Apr 4]. https://covid.cdc.gov/covid-data-tracker/#vaccinations-pregnant-women.
- 2.Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, Roggero P, Prefumo F, Silva Do Vale M, Cardona-Perez JA, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: the INTERCOVID multinational cohort study. JAMA Pediatr. 2021. Aug. [accessed 2021Dec 18];175(8):1–15. doi: 10.1001/jamapediatrics.2021.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fu W, Sivajohan B, McClymont E, Albert A, Elwood C, Ogilvie G, Money D.. Systematic review of the safety, immunogenicity, and effectiveness of COVID-19 vaccines in pregnant and lactating individuals and their infants. Int J Gynaecol Obstet. 2022. Mar;156(3):406–17. doi: 10.1002/ijgo.14008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipkind HS, Vazquez-Benitez G, DeSilva M, Vesco KK, Ackerman-Banks C, Zhu TG, Boyce TG, Daley MF, Fuller CC, Getahun D, et al. Receipt of COVID-19 vaccine during pregnancy and preterm or small-for-gestational-age at birth - eight integrated health care organizations, December 15, 2020-July 22, 2021. MMWR Morb Mortal Wkly Rep. 2022. Jan;71(1):26–30. doi: 10.15585/mmwr.mm7101e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgan JA, Biggio JR Jr, Martin JK, Mussarat N, Chawla HK, Puri P, Williams FB. Maternal outcomes after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in vaccinated compared with unvaccinated pregnant patients. Obstet Gynecol. 2022. Jan;139(1):107–09. doi: 10.1097/AOG.000000000000462. [DOI] [PubMed] [Google Scholar]
- 6.Goldshtein I, Steinberg DM, KUint J, Chodick G, Segal Y, Shapiro S, David B, Ben-Tov A. Association of BNT162b2 COVID-19 vaccination during pregnancy with neonatal and early infant outcomes. JAMA Pediatr. 2022. May;176(5):470–77. doi: 10.1001/jamapediatrics.2022.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halasa NB, Olson SM, Staat MA, Newhams MM, Price AM, Pannaraj PS, Boom JA, Sahni LC, Chiotos K, Cameron MA, et al. Maternal vaccination and risk of hospitalization for Covid-19 among infants. N Engl J Med. 2022. July;387(2):109–19. doi: 10.1056/NEJMoa2204399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cases, data, and surveillance (CDC) . Centers for Disease control and prevention. 2020. [accessed 2021 Dec 18]. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19/what-cdc-is-doing.html.
- 9.Anachebe NF, Sutton MY. Racial disparities in reproductive health outcomes. Am J Obstet Gynecol. 2003. Apr [accessed 2021 Dec 19];188(4):S37–S42. doi: 10.1067/mob.2003.245. [DOI] [PubMed] [Google Scholar]
- 10.Stock SJ, Carruthers J, Calvert C, Denny C, Donaghy J, Goulding A, Hopcroft LEM, Hopkins L, McLaughlin T, Pan J, et al. SARS-CoV-2 infection and COVID-19 vaccination rates in pregnant women in Scotland. Nat Med. 2022. Mar;28(3):504–12. doi: 10.1038/s41591-021-01666-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nachega JN, Sam-Agudu NA, Machekano RN, Rosenthal PJ, Schell S, de Waard L, Bekker A, Gachuno OW, Kinuthia J, Mwongeli N, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and pregnancy in Sub-Saharan Africa: a 6-country retrospective cohort analysis. Clin Infect Dis. 2022. Jun;8:294. doi: 10.1093/cid/ciac294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization . Report of the SAGE working group on vaccine hesitancy. 2014. Accessed Feb 1, 2022 https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf.
- 13.Rosenstock I. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–35. doi: 10.1177/109019817400200403. [DOI] [PubMed] [Google Scholar]
- 14.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 15.Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R, Angelillo IF. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018. Dec [accessed 2021Nov 16];13(12):e0208601. doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15(2):175–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 17.Botha E, van der Merwe D, Burnett RJ, Bester P. Predictors of parents’ infant vaccination decisions: a concept derivation. Health SA Gesondheid. 2021;26:1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shahrabani S, Benzion U, Yom Din G. Factors affecting nurses’ decision to get the flu vaccine. Eur J Heal Econ HEPAC Heal Econ Prev Care. 2009. May;10(2):227–31. doi: 10.1007/s10198-008-0124-3. [DOI] [PubMed] [Google Scholar]
- 19.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Heal Psychol Off J Div Heal Psychol Am Psychol Assoc. 2007. Mar;26(2):136–45. [DOI] [PubMed] [Google Scholar]
- 20.Rosenstock IM. Why people use health services. Milbank Q. 2005;83(4). doi: 10.3390/vaccines9050469. [DOI] [Google Scholar]
- 21.Poon PKM, Zhou W, Chan DCC, Kwok KO, Wong SYS. Recommending COVID-19 vaccines to patients: practice and concerns of frontline family doctors. Vaccines. 2021. Nov;9(11):1319. doi: 10.3390/vaccines9111319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Okuyan B, Bektay MY, Demirci MY, Ay P, Sancar M. Factors associated with Turkish pharmacists’ intention to receive COVID-19 vaccine: an observational study. Int J Clin Pharm. 2021. Nov:1–9. doi: 10.1007/s11096-020-01222-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toth-Manikowski SM, Swirsky ES, Gandhi R, Piscitello G. COVID-19 vaccination hesitancy among health care workers, communication, and policy-making. Am J Infect Control. 2022. Jan;50(1):20–25. doi: 10.1016/j.ajic.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spinewine A, Pétein C, Evrard P, Vastrade C, Laurent C, Delaere B, Henrard S . Attitudes towards COVID-19 vaccination among hospital staff-understanding what matters to hesitant people. Vaccines. 2021. May6;9(5):469. doi: 10.3390/vaccines9050469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maraqa B, Nazzal Z, Rabi R, Sarhan N, Al-Shakhra K, Al-Kaila M. COVID-19 vaccine hesitancy among health care workers in Palestine: a call for action. Prev Med. 2021. Aug;149:106618. doi: 10.1016/j.ypmed.2021.106618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al-Metwali BZ, Al-Jumaili AA, Al-Alag ZA, Sorofman B. Exploring the acceptance of COVID-19 vaccine among healthcare workers and general population using health belief model. J Eval Clin Pract. 2021. Oct;27(5):1112–22. doi: 10.1111/jep.13581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yasuhara N, Okamoto S, Hamada M, Uehara K, Obana N, Imamura T. Evaluation of Japanese people’s perception of risk information for making decisions to receive influenza and rubella vaccinations. Heal Expect an Int J Public Particip Heal Care Heal Policy. 2021. Dec;24(6):2013–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walker KK, Owens H, Zimet G. “We fear the unknown”: emergence, route and transfer of hesitancy and misinformation among HPV vaccine accepting mothers. Prev Med Rep. 2020. Dec;20:101240. doi: 10.1016/j.pmedr.2020.101240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dyda A, King C, Dey A, Leask J, Dunn AG. A systematic review of studies that measure parental vaccine attitudes and beliefs in childhood vaccination. BMC Public Health. 2020. Aug;20(1):1253. doi: 10.1186/s12889-020-09327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang K, Lee SY. Why do some Korean parents hesitate to vaccinate their children? Epidemiol Health. 2019;41:e2019031. doi: 10.4178/epih.e2019031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shapiro GK, Tatar O, Amsel R, Prue G, Zimet GD, Knauper B, Rosberger Z. Using an integrated conceptual framework to investigate parents’ HPV vaccine decision for their daughters and sons. Prev Med. 2018. Nov;116:203–10. doi: 10.1016/j.ypmed.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 32.Deas J, Bean SJ, Sokolovska I, Fautin C. Childhood vaccine attitudes and information sources among Oregon parents and guardians. Health Promot Pract. 2019. Jul;20(4):529–38. doi: 10.1177/1524839918778830. [DOI] [PubMed] [Google Scholar]
- 33.Onyeneho N, Igwe I, I’Aronu N, Okoye U. Compliance with regimens of existing vaccines in Orumba North local government area of Anambra state, Nigeria. Int Q Community Health Educ. 2015;35(2):120–32. doi: 10.1177/0272684X15569485. [DOI] [PubMed] [Google Scholar]
- 34.Cmeciu C, Coman I. Governmental and public thematic patterns on vaccination during a measles outbreak: the Romanian perspective. Glob Health Promot. 2021. Sep;28(3):23–31. doi: 10.1177/1757975920973000. [DOI] [PubMed] [Google Scholar]
- 35.Bricout H, Torcel-Pagnon L, Lecomte C, Almas MF, Matthews I, Lu X, Wheelock A, Sevdalis N, Angelillo IF. Determinants of shingles vaccine acceptance in the United Kingdom. PLoS One. 2019;14(8):e0220230. doi: 10.1371/journal.pone.0220230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hall CM, Northam H, Webster A, Strickland K. Determinants of seasonal influenza vaccination hesitancy among healthcare personnel: an integrative review. J Clin Nurs. 2022. Oct;31(15–16):2112–24. doi: 10.1111/jocn.16103. [DOI] [PubMed] [Google Scholar]
- 37.Mercadante AR, Law AV. Will they, or Won’t they? Examining patients’ vaccine intention for flu and COVID-19 using the Health Belief Model. Res Social Adm Pharm. 2021. Sep;17(9):1596–605. doi: 10.1016/j.sapharm.2020.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guidry JPD, Austin LL, O’Donnell NH, Coman IA, Lovari A, Messner M. Tweeting the #flushot: beliefs, barriers, and threats during different periods of the 2018 to 2019 flu Season. J Prim Care Community Health. 2020;11:2150132720932722. doi: 10.1177/2150132720932722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goss MD, Temte JL, Barlow S, Temte E, Bell C, Birstler J, Chen G. An assessment of parental knowledge, attitudes, and beliefs regarding influenza vaccination. Vaccine. 2020. Feb;38(6):1565–71. doi: 10.1016/j.vaccine.2019.11.040. [DOI] [PubMed] [Google Scholar]
- 40.Trent MJ, Salmon DA, MacIntyre CR. Using the health belief model to identify barriers to seasonal influenza vaccination among Australian adults in 2019. Influenza Other Respi Viruses. 2021. Sep;15(5):678–87. doi: 10.1111/irv.12843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Du J, Luo C, Shegog R, Bian J, Cunningham RM, Boom JA, Poland GA, Chen Y, Tuo C. Use of deep learning to analyze social media discussions about the human papillomavirus vaccine. JAMA Netw open. 2020. Nov;3(11):e2022025. doi: 10.1001/jamanetworkopen.2020.22025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luisi MLR. From bad to worse: the representation of the HPV vaccine Facebook. Vaccine. 2020. Jun;38(29):4564–73. doi: 10.1016/j.vaccine.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 43.Restivo V, Costantino C, Fazio TF, Casuccio N, D’Angelo C, Vitale F, Casuccio A. Factors associated with HPV vaccine refusal among young adult women after ten years of vaccine implementation. Int J Environ Res Public Health. 2018. Apr;15(4). doi: 10.3390/ijerph15040770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bronstein MV, Kummerfeld E, MacDonald A 3rd, Vinogradov S. Willingness to vaccinate against SARS-CoV-2: the role of reasoning biases and conspiracist ideation. Vaccine. 2022. Dec;40(2):213–22. doi: 10.1016/j.vaccine.2021.11.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bateman LB, Hall AG, Anderson WA, Cherrington AL, Helova A, Judd S, Kimberly R, Oates GR, Osborne T, Ott C, et al. Exploring COVID-19 vaccine hesitancy among stakeholders in African American and Latinx communities in the deep south through the lens of the Health Belief Model. Am J Health Promot. 2022 Feb;36(2):288–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Badr H, Zhang X, Oluyomi A, Woodard LD, Adepoju OE, Raza SA, Amos CI. Overcoming COVID-19 vaccine hesitancy: insights from an online population-based survey in the United States. Vaccines. 2021. Sep;9(10):1100. doi: 10.3390/vaccines9101100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang R, Tao L, Han N, Liu J, Yuan C, Deng L, Han C, Sun F, Chi L, Liu M, et al. Acceptance of seasonal influenza vaccination and associated factors among pregnant women in the context of COVID-19 pandemic in China: a multi-center cross-sectional study based on health belief model. BMC Pregnancy Childbirth. 2021. Nov;21(1):745. doi: 10.1186/s12884-021-04224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tao L, Wang R, Han N, Liu J, Yuan C, Deng L, Han C, Sun F, Liu M, Liu J. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: a multi-center cross-sectional study based on health belief model. Hum Vaccin Immunother. 2021. Aug;17(8):2378–88. doi: 10.1080/21645515.2021.1892432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yuen CYS, Dodgson JE, Tarrant M. Perceptions of Hong Kong Chinese women toward influenza vaccination during pregnancy. Vaccine. 2016. Jan;34(1):33–40. doi: 10.1016/j.vaccine.2015.11.032. [DOI] [PubMed] [Google Scholar]
- 50.Du M, Tao L, Liu J. The association between risk perception and COVID-19 vaccine hesitancy for children among reproductive women in China: an online survey. Front Med. 2021;8:741298. doi: 10.3389/fmed.2021.741298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen H, Li X, Gao J, Liu X, Mao Y, Wang R, Zheng P, Xiao Q, Jia Y, Hua F, et al. Health Belief Model perspective on the control of COVID-19 vaccine hesitancy and the promotion of vaccination in China: web-based cross-sectional study. J Med Internet Res. 2021. Sep;23(9):e29329. doi: 10.2196/29329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yan E, Lai DWL, Lee VWP. Predictors of intention to vaccinate against COVID-19 in the general public in Hong Kong: findings from a population-Based, cross-sectional survey. Vaccines. 2021. Jun;9(7):696. doi: 10.3390/vaccines9070696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020. Dec;14(12):e0008961. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Patwary MM, Bardhan M, Disha AS, Hasan M, Haque MZ, Sultana R, Hossain MR, Browning M, Alam MA, Sallam M. Determinants of COVID-19 vaccine acceptance among the adult population of Bangladesh using the Health belief model and the theory of planned behavior model. Vaccines. 2021. Nov;9(12):12. doi: 10.3390/vaccines9121393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hossain MB, Alam MZ, Islam MS, Sultan S, Faysal MM, Rima S, Hossain MA, Mamun AA. Health Belief Model, theory of planned behavior, or psychological antecedents: what predicts COVID-19 vaccine hesitancy better among the Bangladeshi adults? Front Public Health. 2021;9:711066. doi: 10.3389/fpubh.2021.711066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kalam MA, Davis TPJ, Shano S, Uddin MN, Islam MA, Kanwagi R, Islam A, Hassan MM, Larson HJ, Metwally AM. Exploring the behavioral determinants of COVID-19 vaccine acceptance among an urban population in Bangladesh: implications for behavior change interventions. PLoS One. 2021;16(8):e0256496. doi: 10.1371/journal.pone.0256496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Le An P, Nguyen HTN, Nguyen DD, Vo LY, Huynh G. The intention to get a COVID-19 vaccine among the students of health science in Vietnam. Hum Vaccin Immunother. 2021 Dec 2;17(12): 4823–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Guillon M, Kergall P. Factors associated with COVID-19 vaccination intentions and attitudes in France. Public Health. 2021. Sep;198:200–07. doi: 10.1016/j.puhe.2021.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mahmud I, Kabir R, Rahman MA, Alradie-Mohamed A, Vinnakota D, Al-Mohaimeed A. The Health Belief Model predicts intention to receive the COVID-19 vaccine in Saudi Arabia: results from a cross-sectional survey. Vaccines. 2021. Aug;9(8):864. doi: 10.3390/vaccines9080864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jin Q, Raza SH, Yousaf M, Zaman U, Siang JMLD. Can communication strategies combat COVID-19 vaccine hesitancy with trade-off between public service messages and public skepticism? Experimental evidence from Pakistan. Vaccines. 2021. Jul;9(7):757. doi: 10.3390/vaccines9070757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tao L, Wang R, Liu J. Comparison of vaccine acceptance between COVID-19 and seasonal influenza among women in China: a national online survey based on Health Belief Model. Front Med. 2021;8:679520. doi: 10.3389/fmed.2021.679520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zambri F, Perilli I, Quattrini A, Marchetti F, Colaceci S, Giusti A. Health Belief Model efficacy in explaining and predicting intention or uptake pertussis vaccination during pregnancy. Ann Ist Super Sanita. 2021;57(2):167–73. doi: 10.4415/ANN_21_02_09. [DOI] [PubMed] [Google Scholar]
- 63.Natan MB, El Kravchenko B, Sakashidlo K, Mor S. What drives pregnant women’s decisions to accept the pertussis vaccine? Appl Nurs Res. 2017. Dec;38:60–63. doi: 10.1016/j.apnr.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 64.Hayles EH, Cooper SC, Sinn J, Wood N, Leask J, Skinner SR. Pertussis vaccination coverage among Australian women prior to childbirth in the cocooning era: a two-hospital, cross-sectional survey, 2010 to 2013. Aust N Z J Obstet Gynaecol. 2016. Apr;56(2):185–91. doi: 10.1111/ajo.12429. [DOI] [PubMed] [Google Scholar]
- 65.Payakachat N, Hadden KB, Ragland D. Promoting Tdap immunization in pregnancy: associations between maternal perceptions and vaccination rates. Vaccine. 2016. Jan;34(1):179–86. doi: 10.1016/j.vaccine.2015.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nankya-Mutyoba J, Aizire J, Makumbi F, Ocama P, Kirk GD. Hepatitis B virus perceptions and health seeking behaviors among pregnant women in Uganda: implications for prevention and policy. BMC Health Serv Res. 2019. Oct;19(1):760. doi: 10.1186/s12913-019-4516-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wong LP, Alias H, Hassan J, AbuBakar S. Attitudes towards Zika screening and vaccination acceptability among pregnant women in Malaysia. Vaccine. 2017. Oct;35(43):5912–17. doi: 10.1016/j.vaccine.2017.08.074. [DOI] [PubMed] [Google Scholar]
- 68.Dempsey AF, Brewer SE, Sevick C, Pyrzanowski J, Mazzoni S, O’Leary ST. Tdap vaccine attitudes and utilization among pregnant women from a high-risk population. Hum Vaccin Immunother. 2016. Apr;12(4):872–78. doi: 10.1080/21645515.2015.1094594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fridman D, Steinberg E, Azhar E, Weedon J, Wilson TE, Minkoff H. Predictors of H1N1 vaccination in pregnancy. Am J Obstet Gynecol. 2011. Jun;204(6 Suppl 1):S124–7. doi: 10.1016/j.ajog.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 70.Fabry P, Gagneur A, Pasquier J-C. Determinants of A (H1N1) vaccination: cross-sectional study in a population of pregnant women in Quebec. Vaccine. 2011. Feb;29(9):1824–29. doi: 10.1016/j.vaccine.2010.12.109. [DOI] [PubMed] [Google Scholar]
- 71.Myers KL. Predictors of maternal vaccination in the United States: an integrative review of the literature. Vaccine. 2016. Jul;34(34):3942–49. doi: 10.1016/j.vaccine.2016.06.042. [DOI] [PubMed] [Google Scholar]
- 72.Hawlader MDH, Rahman ML, Nazir A, Ara T, Haque MMA, Saha S, SY Barsha, Hossian M, KF Matin, SR Siddiquea, et al. COVID-19 vaccine acceptance in South Asia: a multi-country study. Int J Infect Dis. 2021. Sep;114:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jiang T, Zhou X, Wang H, Dong S, Wang M, Akezhuoli H, Zhu H. COVID-19 vaccination intention and influencing factors among different occupational risk groups: a cross-sectional study. Hum Vaccin Immunother. 2021. Oct;17(10):3433–40. doi: 10.1080/21645515.2021.1930473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Walker KK, Head KJ, Owens H, Zimet GD. A qualitative study exploring the relationship between mothers’ vaccine hesitancy and health beliefs with COVID-19 vaccination intention and prevention during the early pandemic months. Hum Vaccin Immunother. 2021. Oct;17(10):3355–64. doi: 10.1080/21645515.2021.1942713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Firouzbakht M, Sharif NH, Kazeminavaei F, Rashidian P. Hesitancy about COVID-19 vaccination among pregnant women: a cross-sectional study based on the health belief model. BMC Pregnancy Childbirth. 2022. Aug;2(1):611. doi: 10.1186/s12884-022-04941-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Greyson D, Dubé È, Fisher WA, Cook J, Sadarangani M, Bettinger JA. Understanding influenza vaccination during pregnancy in Canada: attitudes, norms, intentions, and vaccine uptake. Health Educ Behav. 2021. Oct;48(5):680–89. [DOI] [PubMed] [Google Scholar]
- 77.Ajzen I. Attitudes, personality, and behavior. Chicago (IL): Dorsey Press; 1988. [Google Scholar]
- 78.Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021. Jan;9(1):42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guidry JPD, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, Ryan M, Fuemmeler BF, Carlyle KE. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021. Feb;49(2):137–42. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fishbein M, Ajzen I. Predicting and changing behavior: the reasoned action approach. New York (NY): Psychology Press; 2010. [Google Scholar]
- 81.Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol. 2001. Dec;40(Pt 4):471–99. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 82.Caso D, Capasso M, Fabbricatore R, Conner M. Understanding the psychosocial determinants of Italian parents’ intentions not to vaccinate their children: an extended theory of planned behaviour model. Psychol Health. 2022 Sep;37(9):1111–1131. [DOI] [PubMed] [Google Scholar]
- 83.Hu Y, Chen Y, Wang Y, Liang H. Measuring childhood vaccination acceptance of mother in Zhejiang province, East China. Hum Vaccin Immunother. 2019;15(2):287–94. doi: 10.1080/21645515.2018.1526557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dubé E, Gagnon D, Ouakki M, Bettinger JA, Witteman HO, MacDonald S, Fisher W, Saini V, Greyson D. Canadian immunization research network. measuring vaccine acceptance among Canadian parents: a survey of the Canadian immunization research network. Vaccine. 2018. Jan;36(4):545–52. doi: 10.1016/j.vaccine.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 85.Wheeler M, Buttenheim AM. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Hum Vaccin Immunother. 2013. Aug;9(8):1782–89. doi: 10.4161/hv.25959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Falope O, Vamos C, Izurieta R, Daley E, Kirby RS. The knowledge and perceptions of Florida pharmacists in administering inactivated influenza vaccines to pregnant women. Pharmacy (Basel). 2021. Apr 16;9(2):83.doi: 10.3390/pharmacy9020083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chu A, Gupta V, Unni EJ. Utilizing the theory of planned behavior to determine the intentions to receive the influenza vaccine during COVID-19: a cross-sectional survey of US adults. Prev Med Rep. 2021. Sep;23:101417. doi: 10.1016/j.pmedr.2021.101417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Schmid P, Rauber D, Betsch C, Lidolt G, Denker M-L. Barriers of influenza vaccination intention and behavior: a systematic review of influenza vaccine hesitancy, 2005-2016. PLoS One. 2017;12(1):e0170550. doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shah SFA, Ginossar T, Bentley JM, Zimet G, McGrail JP. Using the theory of planned behavior to identify correlates of HPV vaccination uptake among college students attending a rural university in Alabama. Vaccine. 2021. Dec;39(51):7421–28. doi: 10.1016/j.vaccine.2021.10.082. [DOI] [PubMed] [Google Scholar]
- 90.Myers LB, Goodwin R. Using a theoretical framework to determine adults’ intention to vaccinate against pandemic swine flu in priority groups in the UK. Public Health. 2012. Sep;126(Suppl):S53–6. doi: 10.1016/j.puhe.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 91.Ryan M, Marlow LAV, Forster A. Countering vaccine hesitancy among pregnant women in England: the case of Boostrix-IPV. Int J Environ Res Public Health. 2020. Jul;17(14):4984. doi: 10.3390/ijerph17144984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rountree C, Prentice G. Segmentation of intentions towards COVID-19 vaccine acceptance through political and health behaviour explanatory models. Ir J Med Sci. 2022 Oct;191(5):2369–2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Breslin G, Dempster M, Berry E, Cavanagh M, Armstrong NC, Gesser-Edelsburg A. COVID-19 vaccine uptake and hesitancy survey in Northern Ireland and Republic of Ireland: applying the theory of planned behaviour. PLoS One. 2021;16(11):e0259381. doi: 10.1371/journal.pone.0259381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Thaker J, Ganchoudhuri S. The role of attitudes, norms, and efficacy on shifting COVID-19 Vaccine Intentions: a longitudinal study of COVID-19 vaccination intentions in New Zealand. Vaccines. 2021. Oct;9(10):1132. doi: 10.3390/vaccines9101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Al-Wutayd O, Khalil R, Rajar AB. Sociodemographic and behavioral predictors of COVID-19 vaccine hesitancy in Pakistan. J Multidiscip Healthc. 2021;22:2847–56. doi: 10.2147/JMDH.S325529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cordina M, Lauri MA, Lauri J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm Pract (Granada). 2021;19(1):2317. doi: 10.18549/PharmPract.2021.1.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Winter K, Pummerer L, Hornsey MJ, Sassenberg K. Pro-vaccination subjective norms moderate the relationship between conspiracy mentality and vaccination intentions. Br J Health Psychol. 2021. Jul. doi: 10.1111/bjhp.12550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wermers R, Ostroski T, Hagler D. Health care provider use of motivational interviewing to address vaccine hesitancy in college students. J Am Assoc Nurse Pract. 2021. Jan;33(1):86–93. doi: 10.1097/JXX.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 99.Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014. Apr;32(19):2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 100.Dubé E, Gagnon D, Nickels E, Jeram S, Schuster M. Mapping vaccine hesitancy—Country-specific characteristics of a global phenomenon. Vaccine. 2014. Nov. [accessed 2021 Dec 18];32(49).6649–54. https://www.sciencedirect.com/science/article/pii/S0264410X14013073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015. Aug [accessed 2021 Nov 8];33(34):4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 102.Decouttere C, Banzimana S, Davidsen P, Van Riet C, Vandermeulen C, Mason E, Jalali MS, Vandaele N. Insights into vaccine hesitancy from systems thinking, Rwanda. Bull World Health Organ. 2021. Nov [accessed 2022 Apr 4];99(11):783–94. doi: 10.2471/BLT.20.285258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sabahelzain MM, Moukhyer M, Bosma H, van den Borne B. Determinants of measles vaccine hesitancy among Sudanese parents in Khartoum State, Sudan: a cross-sectional study. Vaccines. 2021. Dec [Accessed 2022 Apr 4];10(1):6. doi: 10.3390/vaccines10010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Siani A, Driscoll M, Hurst T, Coker T, Grantham AG, Bunet A. Investigating the determinants of vaccine hesitancy within undergraduate students’ social sphere. J Public Health (Bangkok). 2021. Apr. [accessed 2022 Apr 4]. doi: 10.1007/s10389-021-01538-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Moretti F, Visentin D, Bovolenta E, Rimondini M, Majori S, Mazzi M, Poli A, Tardivo S, Torri E. Attitudes of nursing home staff towards influenza vaccination: opinions and factors influencing hesitancy. Int J Environ Res Public Health. 2020. Mar [accessed 2022 Apr 4];17(6):1851. doi: 10.3390/ijerph17061851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lau LHW, Lee SS, Wong NS. The continuum of influenza vaccine hesitancy among nursing professionals in Hong Kong. Vaccine. 2020. Oct [accessed 2022 Apr 4];38(43):6785–93. doi: 10.1016/j.vaccine.2020.08.038. [DOI] [PubMed] [Google Scholar]
- 107.Zhou L, Wang J, Cheng P, Li Y, Liu G, Zhang X. HPV vaccine hesitancy among medical students in China: a multicenter survey. Front Public Heal. 2022. Feb. [accessed 2022 Apr 4];10:774767. https://www.frontiersin.org/articles/10.3389/fpubh.2022.774767/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Klassen AC, Milliron BJ, Reynolds L, Bakhtibekova Z, Mamadraimov S, Bahruddinov M, Shokamolova S, Shuster M, Mukhtar S, Gafurova M, et al. Formative research to address vaccine hesitancy in Tajikistan. Vaccine. 2021. Mar;39(10):1516–27. doi: 10.1016/j.vaccine.2021.01.033. [DOI] [PubMed] [Google Scholar]
- 109.Gianfredi V, Moretti M, Lopalco PL. Countering vaccine hesitancy through immunization information systems, a narrative review. Hum Vaccin Immunother. 2019. Nov. [accessed 2022 Apr 4];15(11):2508–26. https://www.tandfonline.com/doi/full/10.1080/21645515.2019.1599675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Taddio A, MacDonald N. Addressing vaccine hesitancy in travellers: the CARDTM system. J Travel Med. 2019;26(6). doi: 10.1093/jtm/taz056. [DOI] [PubMed] [Google Scholar]
- 111.Verger P, Botelho-Nevers E, Garrison A, Gagnon D, Gagneur A, Gagneux-Brunon A, Dubé E. Vaccine hesitancy in health-care providers in Western countries: a narrative review. Expert Rev Vaccines. 2022. Mar. [accessed 2022 Apr 4]:1–19. https://www.tandfonline.com/doi/full/10.1080/14760584.2022.2056026. [DOI] [PubMed] [Google Scholar]
- 112.Rosso A, Massimi A, Pitini E, Nardi A, Baccolini V, Marzuillo C, De Vito C, Villari P. Factors affecting the vaccination choices of pregnant women for their children: a systematic review of the literature. Hum Vaccin Immunother. 2020. Aug. [accessed 2022 Apr 4];16(8):1969–80. https://www.tandfonline.com/doi/full/10.1080/21645515.2019.1698901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wilson RJ, Paterson P, Jarrett C, Larson HJ. Understanding factors influencing vaccination acceptance during pregnancy globally: a literature review. Vaccine. 2015. Nov;33(47):6420–29. doi: 10.1016/j.vaccine.2015.08.046. [DOI] [PubMed] [Google Scholar]
- 114.González-Block MÁ, Pelcastre-Villafuerte BE, Knauth DR, Fachel-Leal A, Comes Y, Crocco P, Noboa L, Rodríguez Zea BR, Ruoti M, Díaz-Portillo SP, et al. Influenza vaccination hesitancy in large urban centers in South America. Qualitative analysis of confidence, complacency and convenience across risk groups. PLoS One. 2021. Aug. [accessed 2021 Dec 20];16(8):e0256040. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0256040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mutyoba JN, Surkan PJ, Makumbi F, Aizire J, Kirk GD, Ocama P, Atuyambe LM. Hepatitis B birth dose vaccination for newborns in Uganda: a qualitative inquiry on pregnant women’s perceptions, barriers and preferences. J Virus Erad. 2021. Jun [accessed 2022 Apr 4];7(2):100039. doi: 10.1016/j.jve.2021.100039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang J, Ji Q, Dong S, Zhao S, Li X, Zhu Q, Long S, Zhang J, Jin H. Factors influencing vaccine hesitancy in China: a qualitative study. Vaccines. 2021. Nov [accessed 2022 Apr 4];9(11):1291. doi: 10.3390/vaccines9111291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gerretsen P, Kim J, Caravaggio F, Quilty L, Sanches M, Wells S, Brown EE, Agic B, Pollock BG, Graff-Guerrero A. Individual determinants of COVID-19 vaccine hesitancy. PLoS One. 2021. Nov [accessed 2022 Apr 4];16(11):e0258462. doi: 10.1371/journal.pone.0258462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chan NN, Ong KW, Siau CS, Lee KW, Peh SC, Yacob S, Chia YC, Seow VK, Ooi PB. The lived experiences of a COVID-19 immunization programme: vaccine hesitancy and vaccine refusal. BMC Public Health. 2022. Dec [accessed 2022 Apr 4];22(1):296. doi: 10.1186/s12889-022-12632-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Luk TT, Zhao S, Wu Y, Wong JY, Wang MP, Lam TH. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: a population-based survey. Vaccine. 2021. Jun [accessed 2022 Apr 4];39(27):3602–07. doi: 10.1016/j.vaccine.2021.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Liu X, Dai J, Chen H, Li X, Chen S, Yu Y, Zhao Q, Wang R, Mao Y, Fu H, et al. Factors related to public COVID-19 vaccine hesitancy based on the 3C model: a cross-sectional study. Fudan Univ J Med Sci. 2021;48:307–12. http://jms.fudan.edu.cn. [Google Scholar]
- 121.Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021. Apr [accessed 2021 Dec 20];6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Turhan Z, Dilcen HY, Dolu İ. The mediating role of health literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Curr Psychol. 2022. Jul. [accessed 2021 Dec 20]; 41(11):8147–56. doi: 10.1007/s12144-021-02105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Liu R, Li GM. Hesitancy in the time of coronavirus: temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy. SSM Popul Health. 2021. Sep. [accessed 2022 Apr 4];15:100896. doi: 10.1016/j.ssmph.2021.100896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Skirrow H, Barnett S, Bell S, Riaposova L, Mounier-Jack S, Kampmann B, Holder B. Women’s views on accepting COVID-19 vaccination during and after pregnancy, and for their babies: a multi-methods study in the UK. BMC Pregnancy Childbirth. 2022. Jan;22(1):33. doi: 10.1186/s12884-021-04321-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Cui Y, Binger K, Palatnik A. Attitudes and beliefs associated with COVID-19 vaccination during pregnancy. JAMA Netw open. 2022. Apr;5(4):e227430. doi: 10.1001/jamanetworkopen.2022.7430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Quinn SC, Jamison AM, An J, Hancock GR, Freimuth VS. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: results of a national survey of White and African American adults. Vaccine. 2019. Feb [accessed 2021 Nov 16];37(9):1168–73. doi: 10.1016/j.vaccine.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 127.Turner PJ, Larson H, Dubé È, Fisher A. Vaccine hesitancy: drivers and how the allergy community can help. J Allergy Clin Immunol Pract. 2021. Oct;9(10):3568–74. doi: 10.1016/j.jaip.2021.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Betsch C, Böhm R, Chapman GB. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav Brain Sci. 2015. Oct. [accessed 2021 Dec 18]; 2(1):61–73. doi: 10.1177/2372732215600716. [DOI] [Google Scholar]
- 129.Betsch C, Bach Habersaat K, Deshevoi S, Heinemeier D, Briko N, Kostenko N, Kocik J, Böhm R, Zettler I, Wiysonge CS, et al. Sample study protocol for adapting and translating the 5C scale to assess the psychological antecedents of vaccination. BMJ Open. 2020. Mar. [accessed 2022 Apr 4];10(3):e034869. doi: 10.1136/bmjopen-2019-034869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Adeyanju GC, Sprengholz P, Betsch C, Essoh T-A. Caregivers’ willingness to vaccinate their children against childhood diseases and human papillomavirus: a cross-sectional study on vaccine hesitancy in Malawi. Vaccines. 2021. Oct [accessed 2022 Apr 4];9(11):1231. doi: 10.3390/vaccines9111231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Schindler J, Schindler S, Pfattheicher S. The role of intuition in vaccination attitudes. J Health Psychol. 2021. Dec. [accessed 2021 Dec 20]; 26(14):2950–57. doi: 10.1177/1359105320925160. [DOI] [PubMed] [Google Scholar]
- 132.Böhm R, Betsch C. Prosocial vaccination. Curr Opin Psychol. 2022. Feb. [accessed 2021 Dec 20];43:307–11. doi: 10.1016/j.copsyc.2021.08.010. [DOI] [PubMed] [Google Scholar]
- 133.Neufeind J, Betsch C, Zylka-Menhorn V, Wichmann O. Determinants of physician attitudes towards the new selective measles vaccine mandate in Germany. BMC Public Health. 2021. Mar;21(1):566. doi: 10.1186/s12889-021-10563-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Neufeind J, Betsch C, Habersaat KB, Eckardt M, Schmid P, Wichmann O. Barriers and drivers to adult vaccination among family physicians – insights for tailoring the immunization program in Germany. Vaccine. 2020. Jun [cited 2021 Dec 21];38(27):4252–62. doi: 10.1016/j.vaccine.2020.04.052. [DOI] [PubMed] [Google Scholar]
- 135.Karafillakis E, Dinca I, Apfel F, Cecconi S, Wűrz A, Takacs J, Suk J, Celetano LP, Kramarz P, Larson HJ. Vaccine hesitancy among healthcare workers in Europe: a qualitative study. Vaccine. 2016. Sep [accessed 2021 Dec 21];34(41):5013–20. doi: 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 136.Ransing R, Kukreti P, Raghuveer P, Puri M, Paranjape AD, Patil S, Hegde P, Padma K, Kumar P, Kishore J, et al. A brief psycho-social intervention for COVID-19 vaccine hesitancy among perinatal women in low-and middle-income countries: need of the hour. Asian J Psychiatr. 2022. Jan. [accessed 2021 Dec 19];67:102929. doi: 10.1016/j.ajp.2021.102929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Adeyanju GC, Sprengholz P, Betsch C. Understanding drivers of vaccine hesitancy among pregnant women in Nigeria: a longitudinal study. NPJ Vaccines. 2021. Mar;7(1):96. doi: 10.1038/s41541-022-00489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Nath R, Imtiaz A, Nath SD, Hasan E. Role of vaccine hesitancy, eHealth literacy, and vaccine literacy in young adults’ COVID-19 vaccine uptake intention in a lower-middle-income country. Vaccines. 2021. Nov [accessed 2022 Apr 4];9(12):1405. doi: 10.3390/vaccines9121405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Barello S, Palamenghi L, Graffigna G. Looking inside the ‘black box’ of vaccine hesitancy: unlocking the effect of psychological attitudes and beliefs on COVID-19 vaccine acceptance and implications for public health communication. Psychol Med. 2021. Mar. [accessed 2022 Apr 4]:1–2. doi: 10.1017/S003329172100101X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gendler Y, Ofri L. Investigating the influence of vaccine literacy, vaccine perception and vaccine hesitancy on Israeli parents’ acceptance of the COVID-19 vaccine for their children: a cross-sectional study. Vaccines. 2021. Nov [accessed 2022 Apr 4];9(12):1391. doi: 10.3390/vaccines9121391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hwang SE, Kim W-H, Heo J. Socio-demographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October-December 2020. Hum Vaccin Immunother. 2021. Oct. [accessed 2021 Dec 21]:1–8. doi: 10.1080/21645515.2021.1983389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kwok KO, Li -K-K, Wei WI, Tang A, Wong SYS, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021. Feb. [accessed 2021 Dec 20];114:103854. doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Machida M, Nakamura I, Kojima T, Saito R, Nakaya T, Hanibuchi T, Takamiya T, Odagiri Y, Fukusima N, Kikuchi H, et al. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccines. 2021. Mar. [accessed 2021 Dec 20];9(3):210. doi: 10.3390/vaccines9030210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Machida M, Nakamura I, Kojima T, Saito R, Nakaya T, Hanibuchi T, Takamiya T, Odagiri Y, Fukushima N, Kikuchi H, et al. Trends in COVID-19 vaccination intent from pre- to post-COVID-19 vaccine distribution and their associations with the 5C psychological antecedents of vaccination by sex and age in Japan. Hum Vaccin Immunother. 2021. Nov:1–9. doi: 10.1080/21645515.2021.1968217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Navin MC, Oberleitner LM-S, Lucia VC, Ozdych M, Afonso N, Kennedy RH, Keil H, Wu L, Matthew TA. COVID-19 vaccine hesitancy among healthcare personnel who generally accept vaccines. J Community Health. 2022. Mar. [accessed 2022 Apr 4]. https://link.springer.com/10.1007/s10900-022-01080-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wismans A, Thurik R, Baptista R, Dejardin M, Janssen F, Franken I, Delcea C. Psychological characteristics and the mediating role of the 5C Model in explaining students’ COVID-19 vaccination intention. PLoS One. 2021. Aug [accessed 2022 Apr 4];16(8):e0255382. doi: 10.1371/journal.pone.0255382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Leung CLK, Li -K-K, Wei VWI, Tang A, Wong SYS, Lee SS, Kwok KO. Profiling vaccine believers and skeptics in nurses: a latent profile analysis. Int J Nurs Stud. 2022. Feb. [accessed 2022 Apr 4];126:104142. doi: 10.1016/j.ijnurstu.2021.104142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Nicholls LAB, Gallant AJ, Cogan N, Rasmussen S, Young D, Williams L. Older adults’ vaccine hesitancy: psychosocial factors associated with influenza, pneumococcal, and shingles vaccine uptake. Vaccine. 2021. Jun;39(26):3520–27. doi: 10.1016/j.vaccine.2021.04.062. [DOI] [PubMed] [Google Scholar]
- 149.Williams L, Deakin K, Gallant A, Rasmussen S, Young D, Cogan N. A mixed methods study of seasonal influenza vaccine hesitancy in adults with chronic respiratory conditions. Influenza Other Respi Viruses. 2021. Sep [accessed 2022 Apr 4];15(5):625–33. doi: 10.1111/irv.12856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Thomson A, Robinson K, Vallée-Tourangeau G. The 5As: a practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016. Feb;34(8):1018–24. doi: 10.1016/j.vaccine.2015.11.065. [DOI] [PubMed] [Google Scholar]
- 151.Crawshaw AF, Farah Y, Deal A, Rustage K, Hayward SE, Carter J, Knights F, Goldsmith LP, Campos-Matos I, Wurie F, et al. Defining the determinants of vaccine uptake and undervaccination in migrant populations in Europe to improve routine and COVID-19 vaccine uptake: a systematic review. Lancet Infect Dis. 2022. Sept;22(9):e254–266. doi: 10.1016/s1473-3099(22)00066-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cronin A, Ibrahimm N. A scoping review of literature exploring factors affecting vaccine uptake within Roma communities across Europe. Expert Rev Vaccines. 2022. Aug;1:1–14. doi: 10.1080/14760584.2022.2104715. [DOI] [PubMed] [Google Scholar]
- 153.Kalu ME, Oyinlola O, Ibekaku MC, Adandom II, Iwuagwu AO, Ezulike CJ, Nwachukwu EC, Uduonu E. A mapping review on the uptake of the COVID-19 Vaccine among adults in Africa using the 5A’s vaccine taxonomy. Am J Trop Med Hyg. 2022. May 6;6:1688–97. doi: 10.4269/ajtmh.21-0515. [DOI] [PMC free article] [PubMed] [Google Scholar]


