ABSTRACT
The COVID-19 pandemic disproportionately impacted uninsured and minority populations, contributing to and reinforcing long-lasting health inequities. Clínica Esperanza/Hope Clinic (CEHC), a free clinic serving uninsured individuals, is one ‘safety-net’ clinic that improved access to COVID-19 testing and vaccinations for an at-risk population during the pandemic. A retrospective review was performed to quantify COVID-19 testing and vaccination rates for clinic participants, which were compared to rates in the general population. 51.7% of patients seeking COVID-related care at CEHC were uninsured, compared to 8% in Providence and 4.8% in Rhode Island. CEHC performed 5,623 COVID-19 tests for 4,498 unique individuals, a total of 15,783 vaccines were administered, and 10 to 20% of COVID-care participants reported food insecurity during the study period. The prevalence of COVID-19 in the uninsured population and the high demand for vaccines highlight the important role that free clinics can play in the pandemic setting.
KEYWORDS: COVID-19, vaccination, free clinic, disparities, uninsured
Introduction
Studies have repeatedly demonstrated that the COVID-19 pandemic disproportionately impacted uninsured, under-resourced populations in the United States, leading to a higher burden of health and psychosocial sequelae in these populations.1 FDA-approved COVID-19 vaccines and treatments significantly reduced morbidity and mortality, but unequal access contributed to disparities in health outcomes, exacerbating preexisting health disparities.2 It is critical to continue to identify approaches that expand access to and utilization of pandemic resources to under-served populations. Better understanding of these approaches will enable public health advocates to reduce barriers to care in future health crises.
One means of expanding access to COVID-19 prevention and treatment measures in the United States has been to support culturally attuned, free healthcare at free clinics like Clínica Esperanza/Hope Clinic (CEHC) in Rhode Island, that provide care to uninsured, Spanish-speaking immigrant populations. Since its establishment in 2010, CEHC has provided primary care appointments, specialty appointments, walk-in clinics, and health education programs to tens of thousands of uninsured community members. It is entirely grant-funded and operates with the help of volunteers who are local healthcare providers, neighborhood residents, and health professions students. CEHC’s innovative programs and comprehensive healthcare metrics have been described in several publications.3–7
COVID-19 testing and non-medical support services
CEHC previously reported that the prevalence of positive tests was two to three-fold higher at the CEHC COVID-19 testing site on the west side of Providence, as compared to the prevalence for the city of Providence in the same period.4 Beginning in April 2020, CEHC began offering testing at no cost to CEHC patients and residents of the surrounding west side neighborhoods in the city of Providence. As of 31 January 2022, 5,623 COVID-19 tests had been conducted for 4,498 unique individuals (Figure 1). The average positivity rate was 27% (1,517 tests) over this nearly two-year period. The positivity rate peaked at 66% during the first week of January, 2022, during the Omicron variant wave. A detailed breakdown of positive test rates over time, as compared to rates for the same time period in Providence,8 is provided in Figure 2. Twenty-eight of the testing participants reported having been hospitalized with COVID-19 at some point prior to their test.
Figure 1.
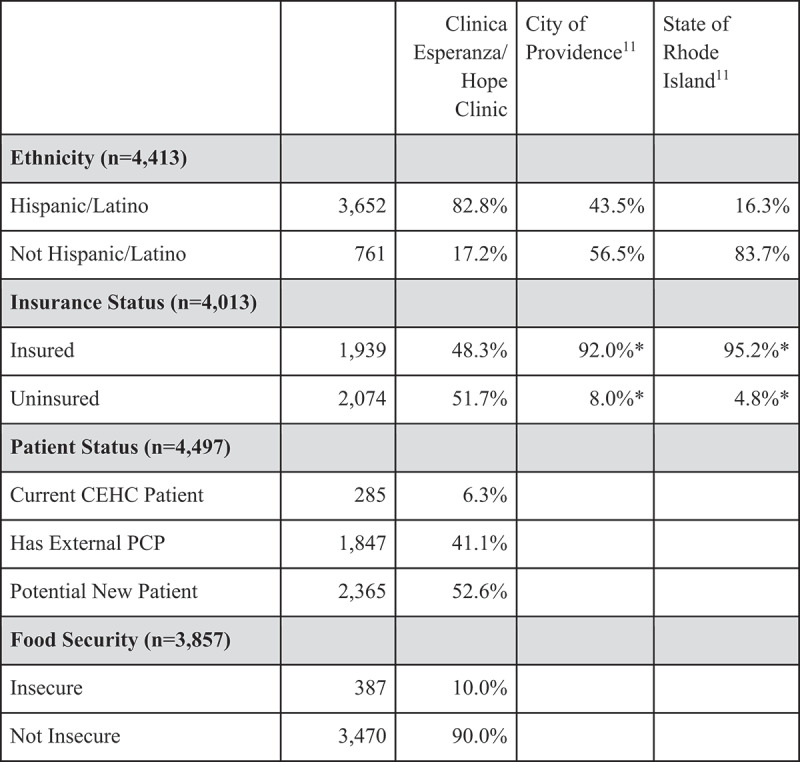
Demographics of participants in COVID-19 testing at CEHC (N = 4,498).
Note: * Uninsured under 65 years of age
Figure 2.
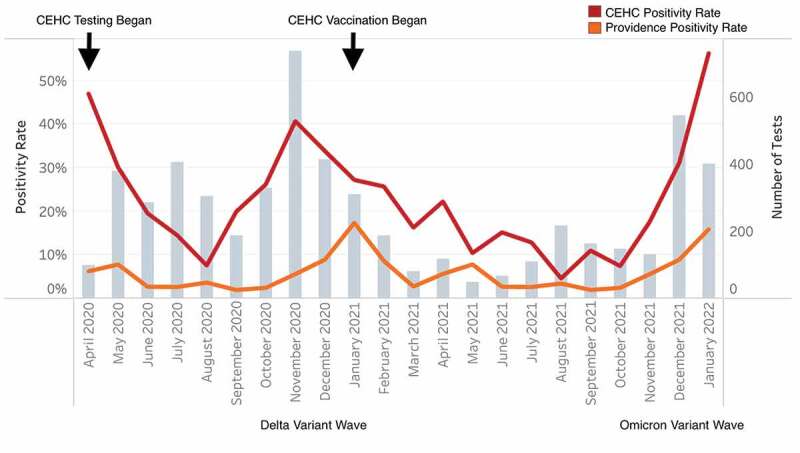
CEHC patients had higher test positivity rates than the city of Providence. Monthly testing rate and positivity are shown for Providence and the clinic.
Note: Number of tests completed (bars) and rate of positive tests (dots) by month.
Eighty-one percent of COVID-19 test participants were Hispanic/Latino and 57% were uninsured, which is consistent with the demographics of the Rhode Island community surrounding the clinic. Most of the individuals requesting COVID-19 tests were residents of the city of Providence’s high-density neighborhoods immediately surrounding CEHC, as determined by their ZIP code and demonstrated in Figure 3. Only 6% of tested patients were previously registered as patients of CEHC at the time of their first encounter for testing. While 47% of participants in testing reported that they had access to a primary care provider (PCP), 53% of patients were uninsured and lacked a PCP. Due to the need for appropriate follow-up after COVID-19 testing, CEHC staff and volunteers registered those individuals who were uninsured and lacked a PCP for continued care at CEHC. This led to a 105% increase in the registered patient population when comparing the CEHC patient population in the second half of 2019 to that of the second half of 2021. Since the volume of requested COVID-19 testing began to interfere with the day-to-day operation of the healthcare clinic, COVID-19 activities were moved to an empty storefront in a nearby shopping plaza, a location that also served as a vaccine site when vaccines became available.
Figure 3.
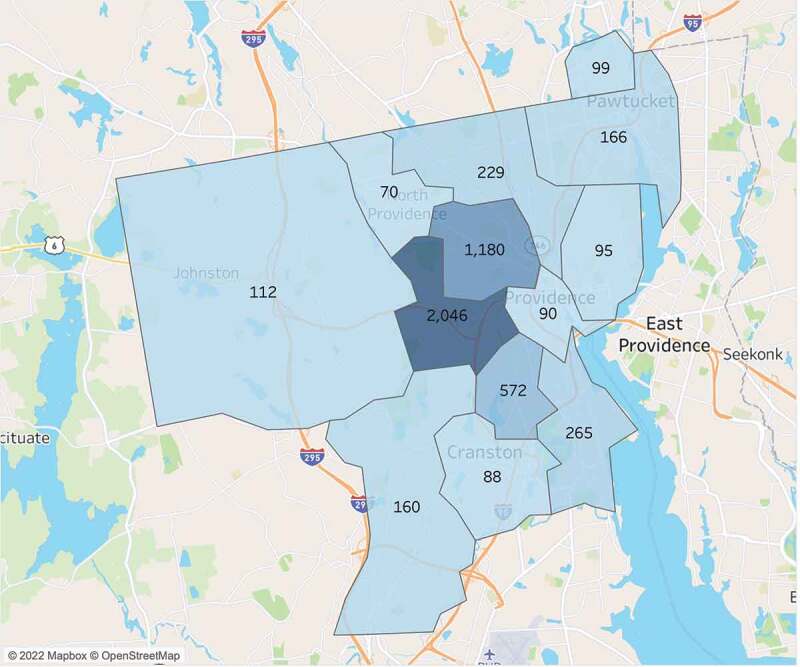
ZIP codes of individuals participating in COVID-19 testing at CEHC.
Note: Number of tests completed by patients living in each ZIP code (displayed for ZIP codes with >50 tests).
The COVID-19 pandemic had a significant impact on the economic stability of individuals who participated in testing at CEHC. On average, one-tenth of all testing participants reported food insecurity, a rate that increased during periods of high transmission. CEHC was able to partner with student volunteers from Brown University, with the City of Providence and with community organizations such as the Elisha Project and South Side Community Land Trust to distribute food boxes at the door of the clinic, to deliver food boxes to quarantined individuals in the neighborhood, and to provide direct financial support for uninsured and undocumented individuals who reported job loss.4
COVID-19 vaccination effort
Vaccine administration at CEHC began when vaccines were made available to community organizations in February 2021. The clinic participated in the City of Providence “High Density Clinic” collaborative, and vaccines were provided by the Rhode Island Department of Health. Volunteer pharmacists from the College of Pharmacy (University of Rhode Island), medical students from Brown University, and undergraduates from local colleges were mobilized and trained to vaccinate community members at the pop-up COVID-19 vaccine site. Permission was given to vaccinate all local residents aged 18 and up as soon as the EUA (Emergency Use Authorization) for that age group was approved, and later extended to residents ages 12 and up. More than 16,000 vaccine doses have been distributed by the clinic, to date.
The primary care clinic at CEHC shifted to telemedicine during the peak periods of COVID-19 transmission in the community, freeing up staff members to work at the COVID-19 vaccine and testing site. Strict protocols were in place to keep staff and volunteers safe, including “testing in to work” and distributing free at-home COVID-19 tests for family members. CEHC staff members who were quarantining due to exposure or infection worked from home if they were well enough, answering phone calls, scheduling patients, and assisting with follow up care for patients with positive COVID-19 tests. Managers “huddled” with the medical director and executive director by video call each morning during peak periods to coordinate and adapt CEHC’s approach to COVID.
Initially, CEHC participated in electronic scheduling on-demand through the Rhode Island’s online COVID-19 vaccine site. However, due to overwhelming demand from individuals residing outside the immediate neighborhood, scheduling for vaccines and testing became ‘private’ and by direct appointment only. Links to the internet-based registration site were provided directly to individuals who fit the geographic and demographic characteristics of the neighborhood served by the clinic. Despite these necessary limitations to scheduled appointments, demand for vaccination was extremely high in February, March, and April of 2021. During these months the vaccine site operated 12–14 hours per weekday and half days on Saturdays to accommodate the demand for vaccines.
The CEHC vaccine clinic was primarily staffed by volunteers, logging an estimated 3,000 volunteer hours during the initial vaccination period from 18 February 2021 – April 2021. Volunteers filled a wide range of roles, including but not limited to registering patients, interpreting, preparing, and administering vaccinations, monitoring patients after vaccination, arranging follow-up appointments, and managing vaccine and supply inventory. In large part due to the altruism of CEHC volunteers, the average cost of care (including infrastructure costs) per individual participant served during the pandemic period was less than $150.
CEHC efforts were primarily focused on vaccinating the low-income, Spanish-speaking, uninsured population living on the west side of Providence. To prioritize this population in scheduling vaccine appointments, clinic staff and volunteers used targeted Facebook advertisements and word-of-mouth to direct uninsured and undocumented individuals to contact the clinic by Facebook Messenger. Volunteers were trained to respond to Facebook Messenger with electronic links to the online appointment schedule. Eligibility was determined by zip code. Vaccinations were also available to individuals arriving in person without appointments, if capacity allowed. Uninsured and non-English-speaking neighborhood residents were also prioritized by providing insured individuals who spoke English and had the means to travel with information on alternative testing and vaccination locations. Individuals who had limited internet access and experience were registered for appointments by family members or by phone. The clinic recruited active social media users, such as younger family members or neighbors, to enable the registration and transportation of older members of the neighborhood.
From February 2021 to January 2022, a total of 15,783 doses of FDA-approved COVID-19 vaccine were administered at the pop-up vaccine clinic. This count includes first, second, third and booster doses of vaccine as was clinically indicated. Breakdown by vaccine brand and demographics can be found in Figure 4. Eighty-five percent of vaccine doses were administered to individuals from the city of Providence in “High Density (COVID) Clinic” zip codes, 78% were administered to uninsured individuals, and 81% were administered to individuals who self-identified as Hispanic/Latino.
Figure 4.
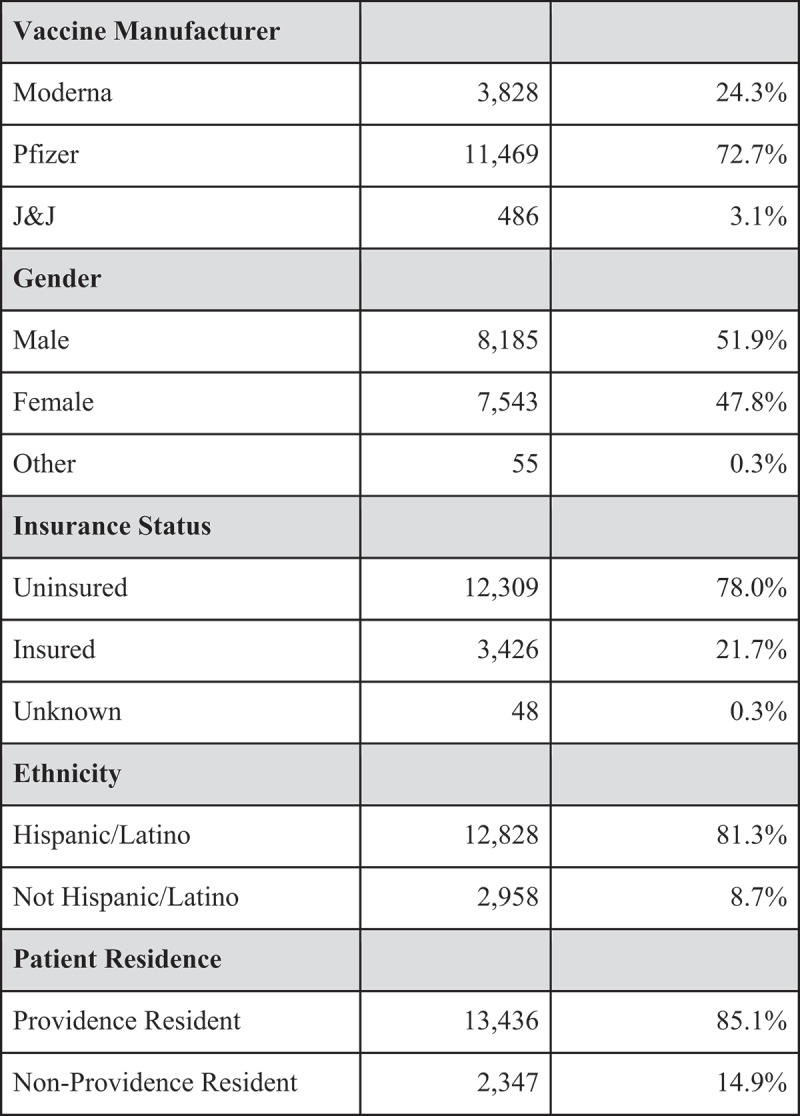
Vaccines administered by Clinica Esperanza/hope clinic volunteers and staff.
Note: Numbers and characteristics of doses of vaccine administered from 2/18/2021 through 1/31/2022. Data includes first, second, third, and booster doses. Total number of vaccine doses administered =15,783 for the study time period.
In July 2021, questions related to prior COVID-19 vaccination were added to COVID-19 testing intake interviews to better quantify the number of patients that had access to COVID-19 vaccines and to evaluate the number of individuals who were infected following vaccination. After that time, a total of 1,469 individuals were tested for COVID-19. Fifty-nine percent of these individuals reported that they were fully vaccinated, 6% reported that they were partially vaccinated and 18% reported that they had not received any FDA-approved COVID-19 vaccine. Of the 510 who were eligible for a booster dose at the time of their visit, 1/3 had received one. These findings are summarized in Figure 5.
Figure 5.
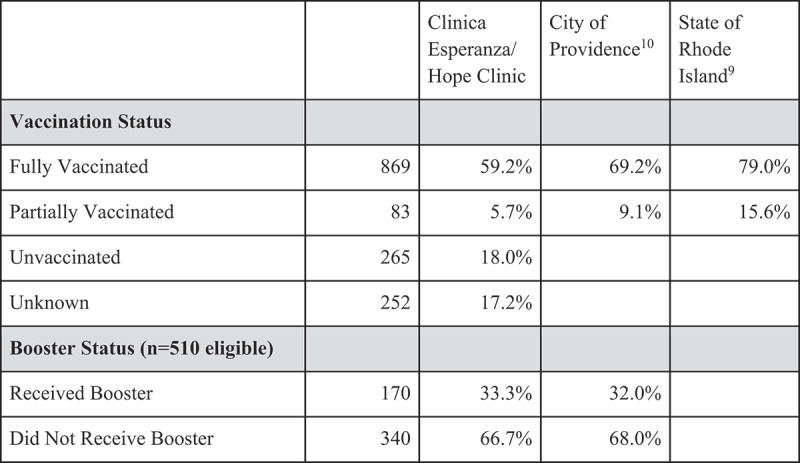
Vaccination rates at Clinica Esperanza/hope clinic’s test to treat site.
Note: Vaccination and booster status for patients who were tested on or after 7/1/2021 through 1/31/2022. Data provided for N=1,469 subjects.
Test to treat efforts
In May 2022, CEHC was chosen as the first federally funded COVID-19 Test to Treat site in the country. Test to Treat (T2T) is a federal program that supports wrap-around services at COVID-19 testing sites. CEHC’s T2T site provides testing, treatment for those who test positive, and vaccines for those who test negative, and in addition to telemedicine appointments for those who are prescribed antiviral medications, like Paxlovid, to treat their COVID-19 infection. This model is similar to CEHC’s COVID-19 testing program and was very easy to integrate into CEHC’s existing testing program. Prior to T2T, CEHC staff followed up with COVID positive patients in the days following their positive results to help patients monitor their symptoms and refer them to the hospital if they deteriorated.
Between May 25 and July 14, CEHC tested 499 individuals for COVID-19 at the T2T site. Of those tested, 92 tested positive and 74 were dispensed a course of Paxlovid. There are certain eligibility requirements individuals must meet in order to be prescribed Paxlovid for treatment which is why not every patient received a course. Of those patients who tested positive and were not prescribed Paxlovid, 15 were referred to other locations for treatment. Patients who were prescribed Paxlovid reported that the medication quickly improved their symptoms and shortened the amount of time they were symptomatic.
CEHC’s T2T site has filled a healthcare gap for the vulnerable community CEHC serves. Although Paxlovid and other antiviral medications have been readily available for some time for those with health insurance, uninsured individuals have had an extremely difficult time accessing these treatment courses due to cost. A single course of Paxlovid can cost more than $500,9 which would be an impossible financial burden on the low-income uninsured community members served by CEHC.
Conclusions
The high prevalence of COVID-19 infection and demand for vaccines in the population served by CEHC illustrate the important role that free clinics can play during health crises such as the recent COVID-19 pandemic. A limited sampling of eligible individuals in the population served by the clinic demonstrated that less than 60% were fully vaccinated. These rates are substantially lower than comparable statistics within the broader RI population. As of the end of January 2022, 79% of eligible individuals living in Rhode Island were reported to be fully vaccinated and 94.6% were at least partially vaccinated.10 In the study population, 33.3% of individuals eligible to receive a booster dose had received one. This is consistent with the corresponding statistic for the Providence population, which is 32%.11 These findings merit further investigation of potential barriers to access and underscore the need for continued support of free community clinics during health crises.
In conclusion, CEHC staff and volunteers pivoted during the pandemic from providing access to primary care to providing COVID-19 vaccines and COVID testing, making it possible for a large population of low-income, Spanish-speaking residents to get access to vaccines in a trusted, culturally attuned, bilingual clinical setting. Clinical care was shifted to telemedicine and all available volunteers were assigned to the COVID testing and vaccine site. Substantial funding for the vaccine effort was provided by the City of Providence and by other donors in early 2020, making it possible to expand from the limited space available at the main clinic site to a larger, dedicated testing and vaccination site. Clinic volunteers performed the brunt of the vaccine-related work at the clinic during the peak period in February and March 2021.
It is worth noting that the volume of work during the peak vaccination and testing periods meant that staff and volunteers were stretched thin. ‘Surge’ funding for hiring and training bilingual staff and/or cash reserves might have enabled the clinic to expand services and administer more vaccines. In retrospect, expanding hours during the weekend and opening for longer hours during the surge in vaccine demand could have enabled CEHC to provide even better access to COVID tests and vaccines for the at-risk population in the neighborhoods surrounding the clinic. Despite severe shortages of healthcare staff, CEHC was still able to recruit and train clinically-oriented volunteers and to deploy well-trained community health workers to sustain the important medical and social work that was required.
Lessons learned during the pandemic include the following: (1) Trusted providers of primary care such as free clinics can reach large populations of uninsured and unemployed community members who have limited resources due to their documentation status during a pandemic; (2) Access to free food and financial support may be distributed to individuals in need through the same trusted source; (3) Messages distributed by trusted healthcare providers through established social media networks can reach community members in need of critical access to tests and vaccines; (4) Volunteers and staff are willing to work long hours and put other activities on hold to respond to community needs in a crisis situation. CEHC team members and volunteers are proud of their contributions to improving access to healthcare during the COVID-19 pandemic and willing to share the lessons that were learned.
Acknowledgements
The authors appreciate the staff, volunteers, and funding supporters of CEHC, who collectively enabled access to testing, vaccines, and healthcare at CEHC throughout the COVID-19 pandemic for a population of Rhode Island residents that otherwise would have had limited access to care.
Funding Statement
Funding for the COVID pandemic programs described in this article was received from: The Rhode Island Department of Health; Providence City Council, Rhode Island Emergency Management (RIEMA), FEMA, Blue Cross Blue Shield of Rhode Island, Wend Foundation, BioReference Laboratories, Armory Management Company, Episcopal Charities Fund of Rhode Island, Tufts Health Plan Foundation (Point32Health Foundation), Rhode Island Foundation, TD Charitable Foundation, Centreville Bank, EpiVax VaxGivesBack Fund, Lifespan and the Elisha Project, and generous individual donors.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Khanijahani A, Iezadi S, Gholipour K, Azami-Aghdash S, Naghibi D.. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int J Equity Health. 2021;20(1):1. doi: 10.1186/s12939-021-01582-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller S, Wherry LR, Mazumder B. Estimated mortality increases during the covid-19 pandemic by socioeconomic status, race, and ethnicity: study examines COVID-19 mortality by socioeconomic status, race, and ethnicity. Health Aff (Millwood). 2021;40(8):1252–6. doi: 10.1377/hlthaff.2021.00414. [DOI] [PubMed] [Google Scholar]
- 3.Barry K, McCarthy M, Buckley J, Jacques S, Johnson H, Almeida-Monroe V, De Groot AS. Four years of CHEER: cost and QALY savings of a free nurse-run walk-in clinic serving an uninsured, predominantly Spanish-speaking immigrant population in providence. J Health Care Poor Underserved. 2019;30(2):806–19. doi: 10.1353/hpu.2019.0057. [DOI] [PubMed] [Google Scholar]
- 4.Barry K, McCarthy M, Melikian G, Almeida-Monroe V, Leonard M, De Groot AS. Responding to COVID-19 in an uninsured Hispanic/Latino community: testing, education and telehealth at a free clinic in Providence. R I Med J (2013). 2020. Nov 2;103(9):41–46. [PubMed] [Google Scholar]
- 5.Hindocha P, Nair NJ, Pigoga JL, Barry K, McCarthy M, Almeida-Monroe V, De Groot AS. Bridging the [health equity] gap at a free clinic for uninsured residents of Rhode Island. R I Med J (2013). 2018. Nov 1;101(9):27–31. [PubMed] [Google Scholar]
- 6.Suskin JA, Barry K, Satish E, Leonard M, De Groot AS. Meeting gynecologic needs and assuring adherence to screening guidelines at a student-run free clinic for uninsured, low-income women. R I Med J(2013). 2022. June 1;105(5):51–55. [PubMed] [Google Scholar]
- 7.McCarthy M, Barry K, Estrada C, Veliz B, Rosales D, Leonard M, De Groot AS. Recruitment, training, and roles of the bilingual, bicultural navegantes: developing a specialized workforce of community health workers to serve a low-income, Spanish-speaking population in Rhode Island. Front Public Health. 2021;9:666566. doi: 10.3389/fpubh.2021.666566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United States Census Bureau . Providence, Rhode Island. United States Government; 2021. https://www.census.gov/quickfacts/fact/table/providencecityrhodeisland,RI/RHI725220 [Google Scholar]
- 9.Gerencher K, Aungst C. How much do Paxlovid and Lagevrio cost? GoodRx health. Published May 3, 2022. [Accessed July 20, 2022]. https://www.goodrx.com/conditions/covid-19/covid-pill-cost-availability#costs
- 10.Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J, Macdonald B, Dattani S, Beltekian D, Ortiz-Ospina E et al, (2020) -“Coronavirus Pandemic (COVID-19)”. Published online at OurWorldInData.org. [Accessed Nov 06, 2022]. https://ourworldindata.org/coronavirus. [Google Scholar]
- 11.Rhode Island Department of Health . Rhode Island COVID-19 vaccine data. Rhode Island Department of Health. https://ri-department-of-health-covid-19-vaccine-data-rihealth.hub.arcgis.com/ [Google Scholar]


