ABSTRACT
Vaccine hesitancy has a significant impact on tackling infectious diseases as it has resulted in reemergence of vaccine-preventable diseases. This review aims to provide an up-to-date evaluation of COVID-19 vaccine hesitancy among the public in the Gulf Cooperation Council countries. We searched the PubMed and SCOPUS databases for manuscripts published on vaccine hesitancy and/or acceptance among the public in GCC countries up till April 1st, 2022. Forty-nine studies met the inclusion criteria and were reviewed. The average vaccine hesitancy rate across GCC countries was 43%. Concerns about vaccine safety (n = 32) and effectiveness (n = 26) were most frequently associated with hesitancy. Being male (n = 25) and having positive behavior regarding the influenza vaccine or vaccines in general (n = 22) were most frequently associated with acceptance. Collaborative efforts of governments, academic bodies, and the media to provide evidence of vaccines’ effectiveness throughout history and strictly manage the spread of the vaccine safety-related rumors are warranted.
KEYWORDS: Vaccine, hesitancy, rejection, acceptance, COVID-19, Gulf Cooperation Council
Introduction
Coronavirus disease (COVID-19) is an infectious respiratory disease caused by a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was identified at the end of 2019.1 The total number of COVID-19 cases among individual Gulf Cooperation Council (GCC) countries [(Saudi Arabia, Oman, the United Arab Emirates (UAE), Kuwait, Qatar, and Bahrain)] by late April, 2022, was more than 350,000 to 850,000 per country, with a mortality rate ranging between 0.19% and 1.21%.1
COVID-19 vaccination in the GCC countries commenced on November 4th, 2020, and was followed by a decline in the rate of new cases, hospitalization, intensive care unit admissions, and mortality.1–4 The most available COVID-19 vaccines in the GCC countries are those manufactured by Pfizer-BioNTech, Moderna, Johnson & Johnson, and Oxford-AstraZeneca. Tables 1 and 2 illustrate the available COVID-19 vaccines and the current vaccination status in each GCC country.1–8
Table 1.
The COVID-19 vaccines available in each GCC country.
| Vaccine | Saudi Arabia | UAE | Kuwait | Qatar | Oman | Bahrain |
|---|---|---|---|---|---|---|
| PfizerBioNTech – Comirnaty | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| Moderna – Spikevax | ✔ | ✔ | ✔ | ✔ | ✔ | |
| Janssen – Ad26.COV 2-S | ✔ | ✔ | ✔ | ✔ | ||
| AstraZeneca – Vaxzevria | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| Beijing CNBG – BBIBP-CorV | ✔ | ✔ | ✔ | |||
| Sinovac – CoronaVac | ✔ | |||||
| Gamaleya – Gam-COVID-Vac | ✔ | ✔ | ✔ | |||
| Gamaleya – Sputnik-Light | ✔ | ✔ | ||||
| SII – Covishield | ✔ | ✔ | ✔ | |||
| National Vaccine and Serum Institute – CHO Cell | ✔ | |||||
| Bharat Biotech – Covaxin | ✔ | |||||
| Valneva – VLA2001 | ✔ |
✔ the vaccine is available.
Table 2.
Vaccination status in each GCC country as of April 30th, 2022.
| Estimated vaccination status | Saudi Arabia | UAE | Kuwait | Qatar | Oman | Bahrain |
|---|---|---|---|---|---|---|
| Vaccination start date* | 01/06/21 | 12/14/20 | 12/28/20 | 12/23/20 | 12/29/20 | 11/04/20 |
| Total doses | 64,212,008 | 4,959,691 | 7,969,160 | 1,529,091 | 7,030,077 | 3,433,683 |
| Total doses per 100 population** | 184 | 50 | 187 | 53 | 138 | 202 |
*Date format: month/day/year.
**Rounded to whole numbers.
According to the World Health Organization’s (WHO) Strategic Advisory Group of Experts (SAGE) working group on immunization, vaccine hesitancy is defined as a “delay in acceptance or refusal of vaccines despite availability of vaccine services.”9 It has been reported as a global phenomenon due to various reasons, such as perceived risk versus benefit, psychosocial factors, and religious beliefs.10 Vaccine hesitancy can have detrimental consequences on an individual level, for those refusing or delaying vaccination, and on a public level. Vaccine hesitancy has resulted in reemergence of vaccine-preventable diseases, like measles and pertussis.11,12 According to the latest data from the WHO’s vaccine-preventable diseases monitoring system in 2019, vaccination rates among GCC countries for all the listed childhood vaccines exceed 90%.13
To the best of our knowledge, no previous review has evaluated vaccine hesitancy for the COVID-19 vaccines in the general public in the GCC countries. In this paper, we aim to summarize published data on the prevalence of vaccine hesitancy among the public in the GCC countries. We also explore some of the factors that might be associated with vaccine hesitancy and acceptance.
Search strategy
A literature search was performed using the PubMed and SCOPUS databases without language or date restrictions from January 1st, 2020 till April 1st, 2022. The following keywords were used: “COVID-19 vaccine” AND “hesitancy” OR “reluctance” OR “delay” OR “refusal” OR “acceptance” AND “Saudi Arabia” OR “Kuwait” OR “United Arab Emirates” OR “Qatar” OR “Oman” OR “Bahrain.” Papers discussing other vaccines and those assessing hesitancy among healthcare workers, students at schools of health sciences, or special populations were excluded as special populations would skew our study and would not be reflective of the general population.
Quality assurance and data synthesis
Given that this is a narrative review, we did not follow a particular quality assurance method. Articles that did not meet the inclusion criteria were excluded. The quality assurance of the included studies was assessed by looking into various variables, including sample size justification, target population, sampling frame, and statistics.
The evidence from the included studies was narratively summarized. Findings were not stratified by vaccine type or nationality as most of the included studies surveyed their population for COVID-19 vaccine acceptance in general regardless of that.
Results
A total of 298 papers was retrieved from both databases. After the removal of duplicates, a total of 214 titles and abstracts were screened for inclusion, 163 of which were excluded. The full texts of the remaining 51 studies were screened, and 49 of them met the eligibility criteria and were included. The reasons for exclusion are listed in the PRISMA flowchart in Figure 1. All the included studies were cross-sectional and survey-based and disseminated to adults through social media platforms (WhatsApp, Twitter, Facebook, and/or Instagram) or via e-mail.14–61 Most of the studies were conducted in Saudi Arabia (n = 32),14–45 followed by Kuwait (n = 6),29–46–50 the UAE (n = 6),51–56 Qatar (n = 4),57–60 and Oman (n = 1).61
Figure 1.
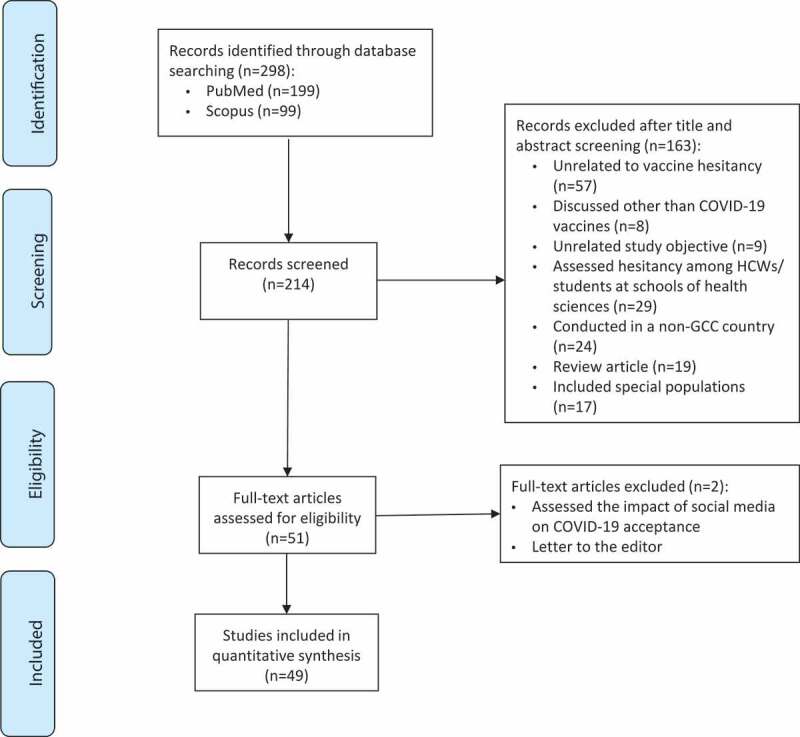
PRISMA flowchart of literature search and review.
All the studies were conducted during the period between March 2020 and August 2021, and 14 were conducted prior to the introduction of COVID-19 vaccines in the respective countries. Overall, the number of participants per study ranged between 154 and 8,056. Of the chosen studies, 24 included <1000 participants, 11 studies included 1000–2000 participants, 7 studies included 2000–3000 participants, and another 7 studies included >3000 participants. Table 3. summarizes the findings stratified per country.
Table 3.
COVID-19 vaccine hesitancy and acceptance rates and their associated variables per GCC country.
| Author (survey period) |
Reference no. | No. of participants | Hesitancy rate* | Factors associated with hesitancy** | Factors associated with acceptance** |
|---|---|---|---|---|---|
| Saudi Arabia | |||||
| Abu-Farha (Dec 2020) |
14 | 592 ⤓⤓ | 70% ⤒ |
|
|
| Alfageeh (Dec 2020) |
15 | 2,137 | 52% |
|
|
| Almaghaslah (Jan–Feb 2021) |
16 | 862 | 80% ⤒ |
|
|
| Al-Mohaithef (Jan–Mar 2021) | 17 | 658 | 47% |
|
|
| N. Alshahrani (Feb–Mar 2021) |
18 | 2,236 | 15% ⤒ |
|
|
| S. Alshahrani (Jan 2021) |
19 | 758 | 36% |
|
|
| Alzahrani (Dec 2020–Feb 2021) |
20 | 3,048 | 47% ⤒ |
|
|
| Fayed (Jan–Mar 2021) |
21 | 1,539 | 41% ⤒ | N/A |
|
| Magadmi (May 2020) |
22 | 3,101 | 55% |
|
|
| Mahmud (Jan–Mar 2021) |
23 | 1,387 | 73% ⤒ |
|
|
| Yahia (Jan–Mar 2021) |
24 | 531 | 38% |
|
|
| Zahid (Mar–Apr 2021) |
25 | 1,599 | 21% |
|
|
| Almalki (Jan–May 2021) |
26 | 407 | 6% |
|
|
| Al-Mohaithef and Padhi (Unspecified) |
27 | 992 | 35% ⤒ | N/A |
|
| Noushad (Feb–Mar 2021) |
28 | 879 | 44% ⤒ |
|
|
| Sallam (Dec 2020) |
29 | 154 ⤓ | 68% |
|
|
| Alduwayghiri and Khan (Jan 2021) |
30 | 1,713 | 45% |
|
N/A |
| Al-Mansour (Feb–Apr 2021) |
31 | 1935 | 31% ⤒ |
|
N/A |
| Al-Zalfawi (Mar–Apr 2021) |
32 | 2,022 | 36% | N/A |
|
| Alamer (July 2021) |
33 | 655 | 33% |
|
|
| Almalki (May 2020) |
34 | 597 | 15% | N/A |
|
| Almoayad (Jan 2021) |
35 | 487 | 53% |
|
|
| Alobaidi (Jan 2021) |
36 | 1,333 | 28% |
|
|
| Alqahtani (Unspecified) |
37 | 391 | 43% | N/A |
|
| Alrajeh (Unspecified) |
38 | 401 | 82% |
|
|
| Altulahi (Nov–Dec 2020) |
39 | 8,056 | 48% |
|
|
| Fadhel (Jul 2021) |
40 | 558 | 21% |
|
|
| Jan (Unspecified) |
41 | 756 | 22% |
|
NA |
| Khalafalla (Mar–Aug 2021) |
42 | 1,039 | 16% |
|
|
| Mubarak (Mar–May 2021) |
43 | 332 | 16% |
|
|
| Narapureddy (Apr–Jun 2021) |
44 | 782 | 34% |
|
|
| Othman (Jun 2021) |
45 | 504 | 5% |
|
N/A |
| Kuwait | |||||
| Sallam (Dec 2020) |
29 | 771 ⤓⤓ | 76% ⤒ |
|
|
| AlAwadhi (May–Sep 2020) |
46 | 7,241 | 33% |
|
|
| Alqudeimat (Aug 2020) |
47 | 2,368 | 73% ⤒ |
|
|
| Burhamah (Mar–Apr 2020) |
48 | 2,345 | 17% |
|
|
| Alibrahim and Awad (Mar–Apr 2021) |
49 | 4,147 | 26% |
|
|
| Al-Ayyadhi (Jan 2021) |
50 | 6,943 | 74% |
|
|
| UAE | |||||
| Albahri (Sep 2020) |
51 | 2,705 | 40% |
|
|
| Ahamed (Unspecified) |
52 | 1,003 | N/A |
|
|
| Saeed (Jan–Apr 2021) |
53 | 1,080 | 23% |
|
N/A |
| Niankara (Jul–Aug 2020) |
54 | 1,109 | 78% ⤒⤒ |
|
|
| Alzubaidi (Feb 2021) |
55 | 669 | 32% |
|
|
| Shahwan (Mar–Aug 2021) |
56 | 467 | 44% |
|
|
| Qatar | |||||
| Alabdulla (Oct–Nov 2020) |
57 | 7,821 | 40% ⤒ |
|
|
| Al-Mulla (Feb 2021) |
58 | 462 ⤓⤓⤓ | 37% |
|
|
| Khaled (Dec 2020–Jan 2021) |
59 | 1,038 | 57% ⤒⤒ |
|
|
| Hafizh (Unspecified) |
60 | 175 | N/A |
|
|
| Oman | |||||
| Al-Marshoudi (Dec 2020) |
61 | 3,000 | 43% |
|
|
N/A: not applicable, HCWs: healthcare workers.
*Rounded to whole numbers.
**Reported as statistically significant (P < 0.05).
⤒ After considering those who were unsure about receiving the vaccine as vaccine hesitant.
⤒⤒ After considering those who were vaccine resistant as vaccine hesitant.
⤓ Not tested for significance.
⤓⤓ Significance testing was based on the answers of the total study participants from the different countries (2,925 participants [25] and 3,414 participants [40]).
⤓⤓⤓ 454 participants answered questions related to their willingness to receive the vaccine.
Vaccine hesitancy by country
Figure 2 shows the median proportion of vaccine hesitancy reported by each GCC country. Figures 3 and 4 illustrate the most frequently reported predictors of COVID-19 vaccine acceptance and hesitancy per country, respectively.
Figure 2.
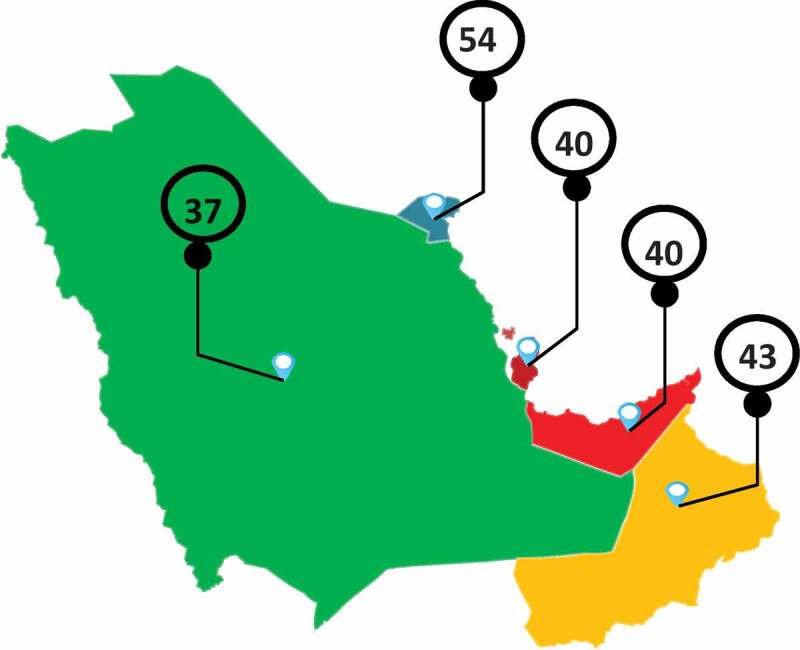
Medians of vaccine hesitancy rates (%) in each GCC country.
Figure 3.
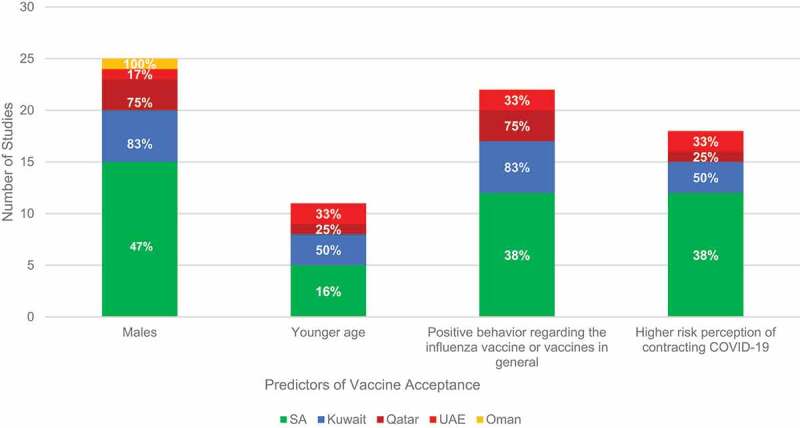
Predictors of COVID-19 vaccine acceptance.
The percentages are presented based on the total number of studies from each country (i.e., SA: 32, Kuwait: 6, UAE: 6, Qatar: 4, and Oman: 1).
Not all the findings reported in this figure were tested for significance.
Figure 4.
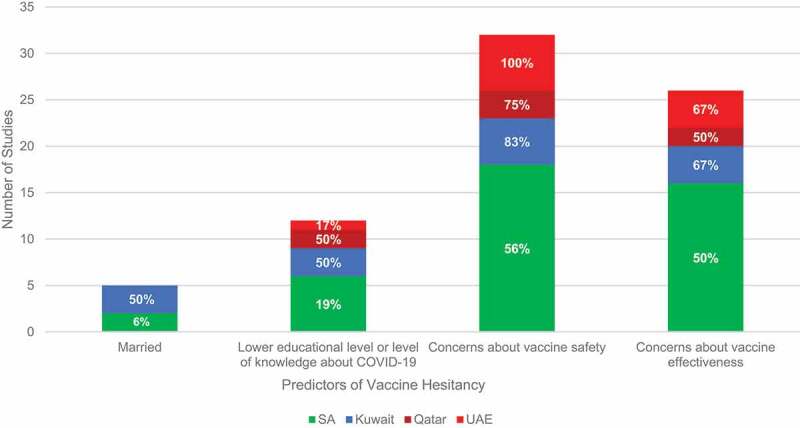
Predictors of COVID-19 vaccine hesitancy.
The percentages are presented based on the total number of studies from each country (i.e., SA: 32, Kuwait: 6, UAE: 6, and Qatar: 4).
Not all the findings reported in this figure were tested for significance.
Saudi Arabia
A total of 32 studies assessed COVID-19 vaccine hesitancy and acceptance among the general public in Saudi Arabia.14–45 Two studies additionally included participants from neighboring countries. Abu-Farha et al.14 included participants from Saudi Arabia, Jordan, Iraq, and Lebanon, and Sallam et al.29 included participants from Saudi Arabia, Kuwait, and Jordan. The dates of survey distribution ranged between May 2020 and August 2021. Most of the surveys were conducted during the first half of 2021 (19 of 32), when vaccination clinics were established in Saudi Arabia. Only seven studies were conducted before vaccines became available in Saudi Arabia.14,15,22,27,29,34,39
Certain sociodemographic variables were associated with vaccine acceptance (p < 0.05), including being male (n = 15),14–15-18–22-24–25-28–29-34–39-40–44 being younger (n = 5),18,22,24,32,39 and being married (n = 3).17,27,40 Other predictors of vaccine acceptance were positive behavior regarding the influenza vaccine or vaccines in general (n = 12),14,15,19,20,22,23,26,29,33,37,39,42 a high risk perception of contracting COVID-19 (n = 12),14–15-18–21-22–25-27–28-36–38-42 trust in the government/healthcare system (n = 7),17–25–27–33–37–43 a history of chronic illnesses (n = 4),28,29,36,39 being a healthcare worker (n = 2),14,23 and being a smoker (n = 2).21,39 In one study, being female was associated with better knowledge of, attitudes toward, and perception of the vaccine.32
Overall, the COVID-19 vaccine hesitancy rate in Saudi Arabia varied significantly between studies, ranging from 5% to 82%. The lowest hesitancy rates (<10%) were reported by 2 studies,26,45 whereas higher rates (>30%) were reported in 22 studies.14–17–19–24–27–33–35–37–39–44 Several factors were found to be associated with vaccine hesitancy, including concerns about vaccine safety (n = 18),16–20–22–26–29–31–36–38–40–42–45 concerns about vaccine effectiveness (n = 16),16–17-19–22-24–30-33–36-38–40-42–45 belief that the vaccine has not been tested sufficiently (n = 7),20–24–26–30,31–45 belief in conspiracy theories (n = 4),22,29,39,40 belief in natural immunity following COVID-19 infection (n = 2),30,39 a history of chronic illnesses (n = 2),31,45 a fear of injections (n = 2),30,44 and mistrust in pharmaceutical companies (n = 1).31
Alshahrani et al.18 assessed the intention of Saudi Arabian travelers to receive the COVID-19 vaccine prior to travel. A survey was distributed among domestic air travelers in waiting areas of airports. Of 2,236 participants, 36% thought that the COVID-19 vaccine should be obligatory, 49% thought it should be optional, and 15% described it as being unnecessary for travelers. Frequent travelers were significantly more willing to accept the vaccine. Similar results were reported in another study in which vaccine acceptance was more common among those who liked to travel internationally.19
One paper described responders’ suggestions to enhance vaccine acceptance.44 Most outlined the importance of providing enough evidence of safety and efficacy (45%) and of putting a government mandate in place (43%). Other responders emphasized peer pressure (5%), making it a requirement for travel (3%), physicians’ recommendations (3%), and employers making it mandatory (1%).
Kuwait
Overall, the COVID-19 vaccine hesitancy rate in Kuwait ranged between 17% and 76%, with a median of 54%.29–46–50 The survey periods took place between March 2020 and April 2021. Most of the studies (5 of 6) were conducted before the vaccine rollout in Kuwait.29–46–48 Burahmah et al.48 reported the lowest hesitancy rate (17%), as most participants (81%) had registered to receive the vaccine or had already received it. Interestingly, the vaccine hesitancy rate significantly increased over time as the policy regarding protective measures was relaxed.46 Males, younger adults, and those who had positive behavior regarding the influenza vaccine or vaccinations in general were more willing to receive the vaccine.29–46–50 On the contrary, those who were married or had children, nonsmokers, and those concerned about vaccine safety and effectiveness were more hesitant to receive the vaccine.29–46–50 Most participants considered social media their primary source for vaccine-related information (69%).49 Noteworthy, about one-third of respondents (32%) attributed their hesitancy to social media posts by physicians doubting the effectiveness of the COVID-19 vaccine.49 Similarly, Sallam et al.,29 who evaluated the negative impacts of belief in conspiracy theories, demonstrated significantly higher rates of vaccine hesitancy among those who believed in conspiracy theories and indicated social media as their primary source of information.
United Arab Emirates
Six studies assessed vaccine hesitancy in the UAE.51–56 Two of these were conducted before vaccine approval in the country and reported a hesitancy rate of 40% and 78%.51,54 The most frequently reported factors associated with COVID-19 vaccine hesitancy were concerns about vaccine safety and effectiveness, as well as the low risk perception of contracting COVID-19.51–56 Some participants were interested in developing immunity naturally through exposure rather than vaccination.51,56 In one study, more than half of the participants reported cost as a factor contributing to hesitancy. Religious or cultural convictions (11%) were reported as contributing factors in the study conducted by Niankara et al.54 Official government websites were seen to be the most trustworthy source of vaccine-related information.54 General internet websites were also commonly used as informative references.54 The main driver of receiving the vaccine among participants from the UAE was the intention to protect oneself and close relatives.
Qatar
The overall COVID-19 vaccine hesitancy rate in Qatar was 37%–57%, with a median of 40%.57–60 Only one study was conducted before the vaccine rollout in Qatar.57 Males were more likely to be willing to receive the vaccine.57–59 Similar to in other GCC countries, those who had positive behavior regarding the influenza vaccine were more likely to accept the COVID-19 vaccine.57,58,60 The most common reasons attributed to vaccine hesitancy were safety concerns and the belief that natural immunity conferred by contracting COVID-19 is safer.57–59In the study by Hafizh et al., respondents claimed that seeing public figures or heads of state accept the vaccine would encourage them to receive the vaccine.60 The local Ministry of Health (MOH), the WHO, and healthcare providers were deemed the primary sources for vaccine-related information.58,59
Oman
Only one study focused on Oman and explored hesitancy toward the COVID-19 vaccine in December 2020, before the vaccine was introduced for use in the country.61 In a cross-sectional, mobile-based survey conducted among 3,000 participants from the public, the overall vaccine hesitancy rate was 43%. The major concern raised by participants was the perception that the vaccine might be unsafe (23%). Interestingly, only 0.2% expressed religious convictions as a reason. Furthermore, among female participants, pregnant women were significantly more likely to be hesitant regarding the vaccine. Most participants referred to social media (67%) and mass media sources (56%) for vaccine-related information.
Discussion
This review summarizes COVID-19 vaccine hesitancy data from 49 papers across the GCC countries. Hesitancy rates ranged widely, from as low as 5% to as high as 82%. As shown in Figure 2, the median overall vaccine hesitancy rates in each country were 54%, 43%, 40%, and 37% for Kuwait, Oman, both the UAE and Qatar, and Saudi Arabia, respectively, with an average of 43%. This value is higher than that reported by Arce et al.62 among low- and middle-income countries (a median rate of 22%) and similar to that given for the United States (a median rate of 35%).62 Sallam et al.10 reported lower COVID-19 vaccine acceptance in Kuwait compared to other countries, which is inconsistent with our findings. This is probably because more studies from Kuwait were published at a later stage and included in our review; hence, the collective findings from all the studies published to date on Kuwait could be more reflective of the recent situation there.
The median hesitancy rate in individual countries ranged between 37–54%. Although the variation between the countries was not very wide, there might have been multiple factors contributing to this. The number of studies evaluated from individual countries varied widely from 32 in Saudi Arabia and only one in Oman. The timing of the individual studies varied between the countries as before and after the vaccine rollout. Furthermore, even after the introduction of vaccines for public use, the specific time of the study could have had an influence on the vaccine hesitancy rate depending on multiple factors. At the same time, inherently or genuinely the vaccine hesitancy rate might have varied between the countries depending on multiple factors including the trust of the people from each country in their health care system, their general belief and perception of vaccines, kind of information that is spread among the public, educational level, as well as other demographics of the participants.
Efforts taken by the individual countries’ regulatory bodies and health departments in tackling vaccine hesitancy might be different. This could differ in the way of sharing direct information among the public to improve vaccine acceptance through mass media and other means, addressing the concerns and rumors among the public on COVID-19 vaccine and measures taken to control infodemics including inaccurate information spread through social media and other means.
The included studies attempted to assess various factors likely influencing the willingness/unwillingness of the public to receive the COVID-19 vaccine. Although a specific and accurate interpretation of such findings cannot be obtained as there was no uniformity in the assessed/enquired-about factors, a general overview can be provided based on the results of the studies. The most frequently reported factors associated with COVID-19 vaccine acceptance across the GCC countries included being male (n = 25), positive behavior regarding the influenza vaccine or vaccines in general (n = 22), a higher risk perception of contracting COVID-19 (n = 18), and a younger age (n = 11). On the other hand, concerns about vaccine safety (n = 32) and vaccine effectiveness (n = 26), lower educational levels or levels of knowledge about COVID-19 (n = 12), and being married (n = 5) were frequently identified as factors associated with COVID-19 vaccine hesitancy. Other factors that contributed to hesitancy included the notion that the vaccines have not been tested sufficiently (n = 10), the idea that natural immunity is safer or sufficient (n = 6), and belief in conspiracy theories (n = 5). Figures 3 and 4 show the most common predictors of COVID-19 vaccine acceptance and hesitancy in each GCC country, respectively. Arce et al.62 reported similar predictors in low- and middle-income countries. In their study, concerns about vaccine safety were the most common predictor of hesitancy. Our results are also consistent with those reported by Sallam et al.,10 who conducted a systematic review to assess COVID-19 vaccine acceptance worldwide and reported higher COVID-19 vaccine acceptance among males. The association of gender and concerns about vaccine safety and effectiveness with vaccine hesitancy/acceptance was reported in other countries as well.63,64
While the source of vaccine information has been evaluated as a predictor for vaccine hesitancy in some studies, a correlation was not established. Social media and mass media sources were most commonly considered as the primary source of vaccine-related information, though official government websites and healthcare professionals were often referred to as well. Unlike traditional media, social media platforms do not undergo editorial curation or scientific evaluation. Such platforms allow users to create and share content and opinions quite rapidly, which may result in the fast spread of misinformation regarding COVID-19 vaccines. Such a process creates a major public health concern, which may be associated with lower vaccine acceptance among the general population.65
Implications and recommendations
Targeting factors associated with vaccine hesitancy might be the best place to start when aiming to increase vaccination rates. The WHO’s SAGE working group proposes three Cs to address when tackling vaccine hesitancy: confidence (i.e., trust in the vaccine, in the healthcare system, and in the policy makers), complacency (i.e., a low perception of risk regarding the disease), and convenience (i.e., the availability, accessibility, and affordability of the vaccine).9 Most of the GCC countries have targeted these three Cs in their efforts to enhance vaccine acceptance. Confidence in the vaccine and complacency were addressed by creating and distributing clear and continually updated resources in multiple languages. These resources included information about the heightened risk of the disease and its complications, methods for contracting and transmitting the disease, and the risk associated with not getting vaccinated. This information was widely disseminated via traditional channels (e.g., on television and street billboards) and social media. Additionally, some GCC governments created infographics and videos with information on COVID-19 vaccines in an effort to encourage the public to receive the vaccine. Quick hot lines were created by the MOH in each country to address any questions consumers might have regarding the vaccine or the virus. Important public figures, including the crown prince of Saudi Arabia, were vaccinated in public, and this was aired via different channels, again as a strategy to enhance confidence and trust in the vaccine and the healthcare system. Another method used to address complacency was the reporting of the number of cases, including those in critical condition, and death rates on a daily basis to increase awareness of the gravity of this disease.
The vaccination process in GCC countries was made easy and free of charge. At first, vaccination required downloading an application to a smart phone, being triaged according to one’s risk status, and traveling to a center that had the capacity to freeze the vaccines at very cold temperatures. As GCC countries acquired more doses, more and more vaccination centers were able to offer the vaccine with minimal waiting times. This made the process quite convenient and accessible. Finally, once individual countries had enough vaccine supplies for all their residents, a vaccine mandate was put in place in many of the countries. This mandate requires citizens and residents to demonstrate they have been vaccinated with two doses to be able to go pretty much anywhere: stores, universities, workplaces, movie theaters, airports, etc.
Potential future approaches
The following are additional recommendations that can be considered. One involves encouraging educational institutions (schools, colleges, and universities) to include classes/lectures on the pandemic disease, its dangers, and the benefits of the vaccine, as well as providing evidence on the effectiveness of vaccines throughout history. Furthermore, basic education on the drug development process, including the methods employed in assessing the efficacy and safety of medications, as well as vaccines, before their introduction for general use, could be considered. This could probably improve the trust of the public in terms of the drug/vaccine approval process and its efficacy and safety. The media (such as TV or radio) may host recovered COVID-19 patients or the relatives of individuals suffering from COVID-19 in order to emotionally influence people to get vaccinated to protect themselves and their loved ones.
Limitations
We believe this is the first review to summarize the data on COVID-19 vaccine hesitancy and acceptance among the public in the GCC countries. Nonetheless, this review has some limitations. First, all the included studies were cross-sectional, which means that our results cannot be generalized. Second, given that most of the included studies were from Saudi Arabia (32/49) and that no studies reported the situation in Bahrain, the distribution of the included studies is skewed, which makes our calculated average of vaccine hesitancy and the comparisons between GCC countries less reliable. Third, the included studies used different scales to assess vaccine hesitancy (e.g., some used a binary approach of yes/no questions, while others used a scale ranging from definitely/probably to unsure or from strongly agree to strongly disagree). Fourth, all the included studies utilized social media to distribute their web-based surveys. While this method allows for a larger reach of participants, it may be coupled with reliability and validity problems as part of the general population may not have access to such platforms or may need guidance while filling out the questionnaires.66 Fifth, although some studies did not consider those that were unsure/indecisive about receiving the vaccine as vaccine hesitant, we classified such individuals as hesitant as they fall under the WHO’s definition of a form of delaying the vaccination process.9 Sixth, as the included studies administered their surveys at different times, this could have been a confounder with regard to accurately mirroring vaccine hesitancy rates, especially with the fluctuations in the level of protective measures and/or in governmental/other organizations’ encouragement of vaccination over time. Lastly, one study included vaccinated individuals as study participants as the primary aim of the study was to assess vaccine safety.53 Lower vaccine hesitancy rates were reported, which is likely biased due to the fact that it included vaccinated individuals as study participants, who had obviously overcome their initial hesitancy, if any existed in the first place. The inclusion of this study might have affected the reflections on vaccine hesitancy in the respective country.
Conclusion
COVID-19 vaccine hesitancy is a common phenomenon among the public globally and in the GCC countries specifically, with concerns about vaccine safety and effectiveness being the most reported factors. This warrants collaborative efforts of governments, academic bodies, and the media to provide evidence on vaccines’ effectiveness throughout history and to strictly manage the spread of the vaccine safety-related rumors. Improving the health literacy of the public in general will also be beneficial. Such an approach is vital considering the potential emergence of similar situations in the future for which all stakeholders should be better prepared.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.World Health Organization (WHO) . Coronavirus disease (COVID-19) dashboard. [accessed 2022 Apr 30]. https://covid19.who.int/.
- 2.Ministry of Health . COVID-19 dashboard. Saudi Arabia; [accessed 2022 Apr 30]. https://covid19.moh.gov.sa/. [Google Scholar]
- 3.The Supreme Council for National Security . UAE Coronavirus (COVID-19) updates. United Arab Emirates: National Emergency Crisis and Disasters Management Authority; [accessed 2022 Apr 30]. https://covid19.ncema.gov.ae/en. [Google Scholar]
- 4.Government of Qatar . COVID-19 status in Qatar. Qatar: Qatar Open Data Portal; [accessed 2022 Apr 30]. https://www.data.gov.qa/pages/dashboard-covid-19-cases-in-qatar/. [Google Scholar]
- 5.World Health Organization (WHO) . COVID-19 vaccine tracker and landscape. [accessed 2022 Apr 30]. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.
- 6.Ministry of Health . COVID-19 & vaccine FAQs. Saudi Arabia; [accessed 2021 Oct 2]. https://www.moh.gov.sa/en/Ministry/HotTopics/Pages/COVID-19-Vaccine.aspx. [Google Scholar]
- 7.Ministry of Public Health . COVID-19 vaccine. Qatar; [accessed 2022 Apr 30]. https://covid19.moph.gov.qa/EN/Covid19-Vaccine/Pages/FAQ.aspx. [Google Scholar]
- 8.2022 VIPER Group COVID19 vaccine tracker team. COVID-19 vaccine tracker. [accessed 2022 Apr 30]. https://covid19.trackvaccines.org/trials-vaccines-by-country/.
- 9.World Health Organization (WHO) . Report of the SAGE working group on vaccine hesitancy. 2014. Oct; 1. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf.
- 10.Sallam M. Covid-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):1–15. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the United States. A review of measles and pertussis. Jama. 2016;315(11):1149–1158. doi: 10.1001/jama.2016.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jansen VAA, Stollenwerk N, Jensen HJ, Ramsay ME, Edmunds WJ, Rhodes CJ. Measles outbreaks in a population with declining vaccine uptake. Science. 2003;301(5634):804. doi: 10.1126/science.1086726. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization (WHO) . Vaccine-Preventable diseases: monitoring system. 2020 global summary. [accessed 2021 Dec 27].
- 14.Abu-Farha R, Mukattash T, Itani R, Karout S, Khojah HMJ, Abed Al-Mahmood A, Alzoubi KH. Willingness of Middle Eastern public to receive COVID-19 vaccines. Saudi Pharm J [Internet]. 2021;29(7):734–739. doi: 10.1016/j.jsps.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alfageeh EI, Alshareef N, Angawi K, Alhazmi F, Chirwa GC. Acceptability of a Covid-19 vaccine among the Saudi population. Vaccines. 2021;9(3):1–13. doi: 10.3390/vaccines9030226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almaghaslah D, Alsayari A, Kandasamy G, Vasudevan R. COVID-19 vaccine hesitancy among young adults in Saudi Arabia: a cross-sectional web-based study. Vaccines. 2021;9(4):1–8. doi: 10.3390/vaccines9040330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Mohaithef M, Padhi BK, Ennaceur S. Socio-Demographics correlate of COVID-19 vaccine hesitancy during the second wave of COVID-19 pandemic: a cross-sectional web-based survey in Saudi Arabia. Front Public Heal. 2021;9(June):698106. doi: 10.3389/fpubh.2021.698106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alshahrani NZ, Alshahrani SM, Farag S, Rashid H. Domestic Saudi Arabian travellers’ understanding about Covid-19 and its vaccination. Vaccines. 2021;9(8):1–10. doi: 10.3390/vaccines9080895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alshahrani SM, Dehom S, Almutairi D, Alnasser BS, Alsaif B, Alabdrabalnabi AA, Bin Rahmah A, Alshahrani MS, El-Metwally A, Al-Khateeb BF, et al. Acceptability of COVID-19 vaccination in Saudi Arabia: a cross-sectional study using a web-based survey. Hum Vaccines Immunother [Internet]. 2021;17(10):3338–3347. doi: 10.1080/21645515.2021.1936869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alzahrani SH, Baig M, Alrabia MW, Algethami MR, Alhamdan MM, Alhakamy NA, Asfour HZ, Ahmad T. Attitudes toward the SARS-CoV-2 vaccine: results from the Saudi residents’ intention to get vaccinated against Covid-19 (srigvac) study. Vaccines. 2021;9(7):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fayed AA, Al Shahrani AS, Almanea LT, Alsweed NI, Almarzoug LM, Almuwallad RI, Almugren WF. Willingness to receive the COVID-19 and seasonal influenza vaccines among the Saudi population and vaccine uptake during the initial stage of the national vaccination campaign: a cross-sectional survey. Vaccines. 2021;9(7):1–12. doi: 10.3390/vaccines9070765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Magadmi RM, Kamel FO. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health. 2021;21(1):1–8. doi: 10.1186/s12889-021-11501-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahmud I, Kabir R, Rahman MA, Alradie-Mohamed A, Vinnakota D, Al-Mohaimeed A. The health belief model predicts intention to receive the Covid-19 vaccine in Saudi Arabia: results from a cross-sectional survey. Vaccines. 2021;9(8):1–11. doi: 10.3390/vaccines9080864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yahia AIO, Alshahrani AM, Alsulmi WGH, Alqarni MMM, Abdulrahim TKA, Heba WFH, Alqarni TAA, Alharthi KAZ, Buhran AAA. Determinants of COVID-19 vaccine acceptance and hesitancy: a cross-sectional study in Saudi Arabia. Hum Vaccines Immunother [Internet]. 2021:1–6. doi: 10.1080/21645515.2021.1950506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zahid HM, Alsayb MA. Assessing the knowledge and attitude toward COVID-19 vaccination in Saudi Arabia. Int J Environ Res Public Health. 2021;18(15):1–9. doi: 10.3390/ijerph18158185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Almalki MJ, Alotaibi AA, Alabdali SH, Zaalah AA, Maghfuri MW, Qirati NH, Jandali YM, Almalki SM. Acceptability of the COVID-19 vaccine and its determinants among university students in Saudi Arabia: a cross-sectional study. Vaccines. 2021;9(9):1–13. doi: 10.3390/vaccines9090943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Mohaithef M, Padhi BK. Determinants of Covid-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657–1663. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noushad M, Nassani MZ, Koppolu P, Alsalhani AB, Samran A, Alqerban A, Abusalim GS, Barakat A, Alshalhoub MB, Rastam S. Predictors of Covid-19 vaccine intention among the Saudi Arabian population: a cross-sectional survey. Vaccines. 2021;9(8):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A, et al. High rates of Covid-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9(1):1–16. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alduwayghiri EM, Khan N. Acceptance and attitude toward COVID-19 vaccination among the public in Saudi Arabia: a cross-sectional study. J Contemp Dent Pract. 2021;22(7):730–734. doi: 10.5005/jp-journals-10024-3114. [DOI] [PubMed] [Google Scholar]
- 31.Al-Mansour K, Alyahya S, AbuGazalah F, Alabdulkareem K. Factors affecting Covid-19 vaccination among the general population in Saudi Arabia. Healthcare (Switzerland). 2021;9(9):1–9. doi: 10.3390/healthcare9091218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Zalfawi SM, Rabbani SI, Asdaq SM, Alamri AS, Alsanie WF, Ahomrani M, Mohzari Y, Alrashed AA, AlRifdah AH, Almagrabe T, et al. Public knowledge, attitude, and perception towards COVID-19 vaccination in Saudi Arabia. Int J Environ Res Public Health. 2021;18(19):1–15. doi: 10.3390/ijerph181910081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alamer E, Hakami F, Hamdi S, Alamer A, Awaf M, Darraj H, Abutalib Y, Madkhali E, Alamer R, Bakri N, et al. Knowledge, attitudes and perception toward COVID-19 vaccines among adults in Jazan province, Saudi Arabia. Vaccines. 2021;9(11):1–12. doi: 10.3390/vaccines9111259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Almalki MJ. Knowledge, attitudes, and practices toward COVID-19 among the general public in the border region of Jazan, Saudi Arabia: a cross-sectional study. Front Public Health. 2021;9(12):1–10. doi: 10.3389/fpubh.2021.733125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Almoayad F, Bin-Amer LA, Althubyani NT, Alajmi SM, Alshammari AA, Alsuwayal RA. The general public’s intent to receive a COVID-19 vaccine in Saudi Arabia. Int J Health Promot Educ Routledge. 2022:1–16. doi: 10.1080/14635240.2022.2047094. [DOI] [Google Scholar]
- 36.Alobaidi S. Predictors of intent to receive the COVID-19 vaccination among the population in the Kingdom of Saudi Arabia: a survey study. J Multidiscip Healthc. 2021;14:1119–1128. doi: 10.2147/JMDH.S306654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alqahtani YS. Acceptability of the COVID-19 vaccine among adults in Saudi Arabia: a cross-sectional study of the general population in the southern region of Saudi Arabia. Vaccines. 2022;10(1):1–13. doi: 10.3390/vaccines10010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alrajeh AM, Daghash H, Buanz SF. Altharman HA, Belal S. COVID-19 vaccine hesitancy among the adult population in Saudi Arabia. Cureus. 2021;13(12):1–10. doi: 10.7759/cureus.20197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Altulahi N, AlNujaim S, Alabdulqader A, Alkharashi A, AlMalki A, AlSiari F, Bashawri Y, Alsubaie S, AlShahrani D, AlGoraini Y. Willingness, beliefs, and barriers regarding the COVID-19 vaccine in Saudi Arabia: a multiregional cross-sectional study. BMC family practice. BioMed Central. 2021;22(1):247. doi: 10.1186/s12875-021-01606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Heard E. Intersectionality in practice. Health Promot Int. 2021;36(1):1–13. doi: 10.1093/heapro/daaa069. [DOI] [PubMed] [Google Scholar]
- 41.Jan M, Alqahtani M, Amer KA, Althubait B, Aldosari AAS, Al Mudawi AAM. COVID-19 and vaccine hesitancy: individual determinants among Saudis in Asir region. Cureus. 2022;14(2). doi: 10.7759/cureus.22331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khalafalla HE, Tumambeng MZ, Halawi MH, Masmali EM, Tashari TB, Arishi FH, Shadad RHM, Alfaraj SZA, Fathi SMA, Mahfouz MS, et al. COVID-19 vaccine hesitancy prevalence and predictors among the students of Jazan University, Saudi Arabia using the health belief model: a cross-sectional study. Vaccines. 2022;10(2):1–9. doi: 10.3390/vaccines10020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mubarak AS, Baabbad AS, Almalki NA, Alrbaiai GT, Alsufayni GA, Kabrah DK. Beliefs, barriers, and acceptance associated with COVID-19 vaccination among Taif University students in Saudi Arabia. J Family Med Prim Care. 2022;11(1):224–232. doi: 10.4103/jfmpc.jfmpc_1255_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Narapureddy BR, Muzammil K, Alshahrani MY, Alkhathami AG, Alsabaani A, AlShahrani AM, Dawria A, Nasir N, Kalyan Viswanath Reddy L, Alam MM, et al. COVID-19 vaccine acceptance: beliefs and barriers associated with vaccination among the residents of KSA. J Multidiscip Healthc. 2021;14(11):3243–3252. doi: 10.2147/JMDH.S340431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Othman SS, Alsuwaidi A, Aseel R, Alotaibi R, Bablgoom R, Alsulami G, Alharbi R, Ghamri R. Association between social media use and the acceptance of COVID-19 vaccination among the general population in Saudi Arabia – a cross-sectional study. BMC Public Health BioMed Central. 2022;22(1):1–11. doi: 10.1186/s12889-022-12757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alawadhi E, Zein D, Mallallah F, Haider NB, Hossain A. Monitoring COVID-19 vaccine acceptance in Kuwait during the pandemic: results from a national serial study. Risk Manag Healthc Policy. 2021;14:1413–1429. doi: 10.2147/RMHP.S300602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alqudeimat Y, Alenezi D, Alhajri B, Alfouzan H, Almokhaizeem Z, Altamimi S, Almansouri W, Alzalzalah S, Ziyab AH. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. 2021;30(3):262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Burhamah W, AlKhayyat A, Oroszlányová M, AlKenane A, Jafar H, Behbehani M, Almansouri A. The SARS-CoV-2 vaccine hesitancy among the general population: a large cross-sectional study from Kuwait. Cureus. 2021;13(7):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alibrahim J, Awad A. COVID-19 vaccine hesitancy among the public in Kuwait: a cross-sectional survey. Int J Environ Res Public Health. 2021;18(16):1–21. doi: 10.3390/ijerph18168836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Al-Ayyadhi N, Ramadan MM, Al-Tayar E, Al-Mathkouri R, Al-Awadhi S. Determinants of hesitancy towards COVID-19 vaccines in State of Kuwait: an exploratory internet-based survey. risk Manag Healthc Policy. 2021;14:4967–4981. doi: 10.2147/RMHP.S338520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Albahri AH, Alnaqbi SA, Alshaali AO, Alnaqbi SA, Shahdoor SM. COVID-19 vaccine acceptance in a sample from the United Arab Emirates general adult population: a cross-sectional survey, 2020. Front Public Heal. 2021;9:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ahamed F, Ganesan S, James A, Zaher WA. Understanding perception and acceptance of Sinopharm vaccine and vaccination against COVID-19 in the UAE. BMC Public Health. 2021;21(1):1–11. doi: 10.1186/s12889-021-11620-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saeed BQ, Al-Shahrabi R, Alhaj SS, Alkokhardi ZM, Adrees AO. Side effects and perceptions following Sinopharm COVID-19 vaccination. Int J Infect Dis. 2021. ;111:219–226. doi: 10.1016/j.ijid.2021.08.013. Epub 2021 Aug 9. PMID: 34384899; PMCID: PMC8351310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Niankara I, Muqattash R, Niankara A, Traoret RI. COVID-19 vaccine development in a quadruple helix innovation system: uncovering the preferences of the fourth helix in the UAE. J Open Innov Technol Mark Complex. 2020;6:1–25. [Google Scholar]
- 55.Alzubaidi H, Samorinha C, Saddik B, Saidawi W, Abduelkarem AR, Abu-Gharbieh E, Sherman SM. A mixed-methods study to assess COVID-19 vaccination acceptability among university students in the United Arab Emirates. Hum Vaccin Immunother. 2021;17(11):4074–4082. doi: 10.1080/21645515.2021.1969854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shahwan M, Suliman A, Abdulrahman Jairoun A, Alkhoujah S, Al-Hemyari SS, AL-Tamimi SK, Godman B, Mothana RA. Prevalence, knowledge and potential determinants of COVID-19 vaccine acceptability among university students in the United Arab Emirates: findings and implications. J Multidiscip Healthc. 2022;15(November 2021):81–92. doi: 10.2147/JMDH.S341700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alabdulla M, Reagu SM, Al-Khal A, Elzain M, Jones RM. COVID-19 vaccine hesitancy and attitudes in Qatar: a national cross-sectional survey of a migrant-majority population. Influenza Other Respi Viruses. 2021;15(3):361–370. doi: 10.1111/irv.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Al-Mulla R, Abu-Madi M, Talafha QM, Tayyem RF, Abdallah AM. Covid-19 vaccine hesitancy in a representative education sector population in Qatar. Vaccines. 2021;9(6):1–12. doi: 10.3390/vaccines9060665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Khaled SM, Petcu C, Bader L, Amro I, Al-Hamadi AMHA, Assi M, Ali AAM, Le Trung K, Diop A, Bellaj T, et al. Prevalence and potential determinants of Covid-19 vaccine hesitancy and resistance in Qatar: results from a nationally representative survey of Qatari nationals and migrants between December 2020 and January 2021. Vaccines. 2021;9(5):1–18. doi: 10.3390/vaccines9050471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hafizh M, Badri Y, Mahmud S, Hafez A, Choe P. COVID-19 vaccine willingness and hesitancy among residents in Qatar: a quantitative analysis based on machine learning. J Hum Behav Soc Environ. 2021:1–24. doi: 10.1080/10911359.2021.1973642. [DOI] [Google Scholar]
- 61.Al-Marshoudi S, Al-Balushi H, Al-Wahaibi A, Al-Khalili S, Al-Maani A, Al-Farsi N, Al-Jahwari A, Al-Habsi Z, Al-Shaibi M, Al-Msharfi M, et al. Knowledge, attitudes, and practices (Kap) toward the Covid-19 vaccine in Oman: a pre-campaign cross-sectional study. Vaccines. 2021;9(6):1–14. doi: 10.3390/vaccines9060602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Solís Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, Syunyaev G, Malik AA, Aboutajdine S, Adeojo O, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med [Internet]. 2021;27(8):1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kreps S, Prasad S, Brownstein JS, Hswen Y, Garibaldi BT, Zhang B, Kriner DL. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw Open. 2020;3(10):e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, Jit M. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet [Internet]. 2021;397(10278):1023–1034. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccines Immunother [Internet]. 2020;16(11):2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wright KB. Web-Based survey methodology. In: Liamputtong P, editor. Handbook of research methods in health social sciences. Singapore: Springer; 2017. doi: 10.1007/978-981-10-2779-6_18-1. [DOI] [Google Scholar]


