ABSTRACT
Influenza causes significant mortality and morbidity in the United States (US). Employees are exposed to influenza at work and can spread it to others. The influenza vaccine is safe, effective, and prevents severe outcomes; however, coverage among US adults (50.2%) is below Healthy People 2030 target of 70%. These highlights need for more effective vaccination promotion interventions. Understanding predictors of vaccination acceptance could inform vaccine promotion messages, improve coverage, and reduce illness-related work absences. We aimed to identify factors influencing influenza vaccination among US non-healthcare workers. Using mixed-methods approach, we evaluated factors influencing influenza vaccination among employees in three US companies during April–June 2020. Survey questions were adapted from the WHO seasonal influenza survey. Most respondents (n = 454) were women (272, 59.9%), 20–39 years old (n = 250, 55.1%); white (n = 254, 56.0%); had a college degree (n = 431, 95.0%); and reported receiving influenza vaccine in preceding influenza season (n = 297, 65.4%). Logistic regression model was statistically significant, X (16, N = 450) = 31.6, p = .01. Education [(OR) = 0.3, 95%CI = 0.1–0.6)] and race (OR = 0.4, 95%CI = 0.2–0.8) were significant predictors of influenza vaccine acceptance among participants. The majority had favorable attitudes toward influenza vaccination and reported that physician recommendation would influence their vaccination decisions. Seven themes were identified in qualitative analysis: “Protecting others” (109, 24.0%), “Protecting self” (105, 23.1%), “Vaccine accessibility” (94, 20.7%), “Education/messaging” (71, 15.6%), “Policies/requirements” (15, 3.3%), “Reminders” (9, 2.0%), and “Incentives” (3, 0.7%). Our findings could facilitate the development of effective influenza vaccination promotion messages and programs for employers, and workplace vaccination programs for other diseases such as COVID-19, by public health authorities.
KEYWORDS: Influenza, corporate employees, vaccination, health education
HIGHLIGHTS
Influenza causes significant mortality and morbidity in the United States (US).
The US working-age group (18–64-year-old) bears a huge burden of influenza annually.
Influenza vaccination coverage in the working-age group is low.
Physicians and employers can influence vaccine acceptance of working adults.
Employers can consider practical steps, e.g., incentivizing, or offering vaccine onsite.
Introduction
Millions of Americans are affected by seasonal influenza illness annually, resulting in a huge public health and economic burden.1 During the 2019–2020 influenza season alone, the influenza virus was associated with an estimated 38 million illnesses, resulting in 18 million medical visits, 400,000 hospitalizations, and 22,000 deaths.2 Employees (except maybe those who work remotely alone full time) may be exposed to influenza at workplaces and can spread it to their clients and families. Non-healthcare employees in the United States account for 86% of all US workers, according to the Census Bureau’s 2019 American Community Survey (ACS).3,4 The US working-age group (18–64-year-olds) bears a significant burden of influenza annually, and their influenza vaccination coverage is often low.2 Their rates of infections, medically attended illnesses, hospitalizations, and deaths were higher in 2019–2020 than during the 2017–2018 season. They had approximately 13 million cases of influenza in this population, the highest number of infections for this age group since the 2010–2011 season, with more than 75,000 hospitalizations, and the highest seasonal influenza case rates seen since the 2017–2018 season. They had an estimated 8,000 influenza-related deaths (39% of all deaths).2 Influenza-related illnesses and work absences have a ripple effect on productivity and the economy. Preventive measures such as vaccinations are critical to reducing the public health and economic impact of seasonal epidemics on the population and healthcare system.2
The Centers for Disease Control and Prevention (CDC) estimates that among adults aged 18 years and older, the percentage that has been vaccinated against the influenza range from 40.5% in 2010–2011 to 50.2% in 2020–2021 influenza seasons.5 By March, 2022, only an estimated 45.4% had received a dose of influenza vaccine.6 These rates are far below the Healthy People 2030 Immunization and Infectious Diseases target of 80% influenza vaccination coverage for all non-institutionalized adults aged 18–64 years.7
Corporate employees are socio-demographically distinct from other working groups regarding education level and financial independence.8 Therefore, extrapolating broader population-level influenza vaccine studies to this group may not effectively capture nuances in attitudes and predictors of influenza vaccine acceptance. Previous studies on influenza vaccine acceptance focused on individuals at high risk of influenza infection such as health-care workers,9 individuals with severe illness, such as the elderly population,10,11 or simply focused on the entire adult population.12 This highlights the need for more effective prevention interventions among this group, which is seldom studied.13
Furthermore, recent studies have found influenza vaccination coverage to be associated with reduced spread and risk of severe COVID-19.14,15 Getting vaccinated against influenza is now more important than ever because of the ongoing COVID-19 pandemic. The influenza vaccine prevents tens of thousands of hospitalizations16,17 and intensive care unit (ICU)18 admissions of US adults each year and can reduce the burden on the health-care system and conserve scarce health-care resources for the care of people with COVID-19.19 This highlights the need to improve influenza vaccination rates among the working-age population, particularly amidst the ongoing pandemic.
The objectives of this paper are to:1) understand US corporate employee influenza vaccination behaviors, and 2) explore attitudes toward influenza vaccination uptake and factors influencing employees’ decisions to get vaccinated against influenza. Our null hypothesis is that there is no relationship between the sociodemographic variables and influenza vaccination. The data were collected as part of a larger study on social mixing among employees in non-healthcare settings.20
Methods
We conducted a mixed-methods observational study, using qualitative and quantitative methods to analyze survey data collected among corporate non-healthcare employees during the early stages of the COVID-19 pandemic, from April-June 2020. Corporate non-healthcare employees primary duties relate to corporate-level activities rather than business group-level, education group-level, or campus-level activities.21 We recruited two US multinational consulting companies and one university administrative department.20 The two consulting companies (N1 = 275, N2 = 3000) have employees across all US states while the university administrative department (N3 = 560), is located in Atlanta, Georgia, USA (Ni represents number of employees per company). Company officials sent e-mails inviting all staff working in their US offices to participate. Following consent, participants enrolled into the study by completing a self-administered questionaire via Qualtrics, an online survey platform. We adapted the self-administered questionnaire from the Seasonal Influenza Vaccine Survey by the World Health Organization.22 We tested, adjusted, and validated the questionnaire through a focus group discussion, a cognitive interview, and a pilot study, carried out on a convenience sample of the target population. We used Cronbach’s alpha test to assess internal consistency of the survey.
We collected socio-demographic data (age, gender, education level, race, ethnicity, marital status, job title, and department) and influenza vaccination behavior trend data from 2018-to 2020. To assess attitudes toward influenza vaccination and factors influencing influenza vaccination decisions, we used questions with a 5-point Likert scale of “strongly agree” to “strongly disagree.” In addition, we used open-ended questions to elicit factors influencing their influenza vaccination decision-making. Force response option in Qualtrics, which requires the respondent to answer a question before continuing to the next question in the survey, was used to ensure participants responded to every question. We conducted a descriptive analysis of the variables and report the frequency, proportion, and 95% confidence intervals around the estimates using chi-square analyses, for quantitative variables. We conducted a logistic regression analysis to determine the sociodemographic factors (gender, age, educational level, job title, race, marital status, ethnicity) associated with influenza vaccination acceptance. Before the regression analysis, we collapsed the education-level variable into those with at least a 4-year bachelor’s degree (i.e., Bachelor’s degree in college (4-year), Master’s degree, and Doctoral or professional degree, e.g. (Ph.D., JD, MD)) and those with lower than a 4-year bachelor’s degree (High school or equivalent (GED), Associate degree in college (2-year), and Some college but no degree). Because of the small size, “Prefer not to answer” category was declared as missing for this analysis. Finally, we collapsed the race variable into white, black, and others (Asian, American Indian or Alaska Native, and others). Marital status variable was collapsed into “married or demostic partners” and others. The strength of association was measured by the odds ratio (OR) and 95% confidence intervals (CI). The level of statistical significance was set at alpha of 0.05. Quantitative data analyses were performed using SAS 9.4 statistical software (SAS Institute Inc., Cary NC).
We conducted qualitative data analysis by coding free-text responses to the open-ended questions into one of four themes and sub-themes. Responses that included multiple themes or sub-themes were coded under each relevant category. No response contained more than three themes or subthemes. Responses indicating “no other factors” influencing participants’ influenza vaccination decisions – such as “NA” or “None”—were excluded from the analysis. Frequency and proportion were measured for qualitative variables. This research activity was reviewed by the Yale University institutional review board (IRB# 2000026906) and conducted in compliance with applicable CDC policy for human subjects protections.
Results
Among 3,835 eligible participants from the three participating companies who received e-mail during the early pandemic period (April–June 2020) via our company contact persons, we enrolled 454 employees (12% response rate) (Table 1). The majority were women (272, 59.9%), aged 20–39 years (250, 55.1%), identified as white (254, 56.0%), and had a bachelors’ degree or higher (420, 92.5%). Most respondents (292, 64.3%) reported getting the influenza vaccine every year and 65.4% (297) stated they received the influenza vaccine during the “previous influenza season” (2019–2020). A majority of 50–59-year-old participants (70.3%) reported receiving influenza vaccination in the preceding season, while the youngest age group (20–29 years) reported the least (60.1%). Women (66.9%) were more likely than men (62.9%) to report having received an influenza vaccine in the 2019–20 season, though not statistically significant. Participants with doctoral or professional degrees made up 9.6% of the sample and a higher proportion of them (83.7%) (compared to others who do not have any doctoral or professional degrees) reported receiving the influenza vaccine in the 2019–2020 season. There was a significant association between education and influenza vaccine acceptance X2 (5, N = 454) = 25.5, p = .0001. Participants with higher education level were more likely than those with lower education level to accept influenza vaccination (Pearson’s = 0.2, CI: 0.1 to 0.3) (Table 1). Furthermore, there was a significant association between race and influenza vaccine acceptance X2 (4, N = 454) = 15.5, p = .0038. Black/African American employees had the lowest influenza vaccination rate (44.4%) compared to other race/ethnicity categories. Asian participants reported the highest influenza vaccination rate (73.0%), Logistic regression to determine association between sociodemographic factors and influenza vaccination acceptance was statistically significant, X2 (16, N = 450) = 31.6, p = .01 and further confirmed that education [(OR) = 0.3, 95%CI = 0.1–0.6)] and race (OR = 0.4, 95%CI = 0.2–0.8) were significant predictors of influenza vaccine acceptance. Holding all other predictor variables constant, participants with bachelor’s (4-year) degree or higher in college were 70% more likely to accept influenza vaccination compared to those with lower than bachelor’s (4-year) degree in college. Furthermore, African Americans were 60% less likely to accept influenza vaccination compared to other races (nonwhite). There was no significant association between seasonal influenza vaccination acceptance and other variables (Table 2).
Table 1.
Socio-Demographic characteristics of participants, April–June 2020*.
| Total |
No |
Yes |
CI | |||||
|---|---|---|---|---|---|---|---|---|
| No. 454 | (%) (100) |
No. 157 | (%) (34.6) |
No. 297 | (%) (65.4) | |||
| Age | 20–29 years | 133 | (29.3) | 53 | (39.9) | 80 | (60.1) | −0.03 to 0.15 |
| 30–39 years | 117 | (25.8) | 39 | (33.3) | 78 | (66.7) | ||
| 40–49 years | 85 | (18.7) | 28 | (32.9) | 57 | (67.1) | ||
| 50–59 years | 74 | (16.3) | 22 | (29.7) | 52 | (70.3) | ||
| 60–69 years | 40 | (8.8) | 13 | (32.5) | 27 | (67.5) | ||
| 70+ years | 5 | (1.1) | 2 | (40.0) | 3 | (60.0) | ||
| Gender | Women | 272 | (59.9) | 90 | (33.1) | 182 | (66.9) | −0.12 to 0.06 |
| Men | 178 | (39.2) | 66 | (37.1) | 112 | (62.9) | ||
| Prefer not to answer | 4 | (0.9) | 1 | (25.0) | 3 | (75.0) | ||
| Education | High school or equivalent (GED) | 4 | (0.9) | 2 | (50.0) | 2 | (50.0) | 0.10 to 0.28 |
| Associate degree in college (2-year) | 11 | (2.4) | 5 | (45.5) | 6 | (54.5) | ||
| Some college but no degree | 19 | (4.2) | 15 | (78.9) | 4 | (21.1) | ||
| Bachelor’s degree in college (4-year) | 169 | (37.2) | 63 | (37.3) | 106 | (62.7) | ||
| Master’s degree | 208 | (45.8) | 65 | (31.2) | 143 | (68.8) | ||
| Doctoral or professional degree, e.g. (Ph.D., JD, MD) | 43 | (9.6) | 7 | (16.3) | 36 | (83.7) | ||
| Race | Asian | 74 | (16.3) | 20 | (27.0) | 54 | (73.0) | −0.10 to 0.08 |
| Black/African American | 54 | (11.9) | 30 | (55.6) | 24 | (44.4) | ||
| American Indian or Alaska Native | 7 | (1.5) | 4 | (57.1) | 3 | (42.9) | ||
| White/Caucasian | 254 | (56.0) | 79 | (31.1) | 175 | (68.9) | ||
| Other | 65 | (14.3) | 24 | (36.9) | 41 | (63.1) | ||
| Hispanic/Latino | No | 426 | (93.8) | 147 | (34.5) | 279 | (65.5) | −0.10 to 0.09 |
| Yes | 28 | (6.2) | 10 | (35.7) | 18 | (64.3) | ||
| Marital | Married or domestic partnership | 234 | (51.5) | 76 | (32.5) | 158 | (67.5) | −0.15 to 0.03 |
| Divorced | 32 | (7.1) | 9 | (28.1) | 23 | (71.9) | ||
| Separated | 2 | (0.4) | 1 | (50.0) | 1 | (50.0) | ||
| Single or never married | 183 | (40.3) | 70 | (38.3) | 113 | (61.8) | ||
| Widowed | 3 | (0.7) | 1 | (33.3) | 2 | (66.7) | ||
| Job title | Manager | 108 | (23.8) | 38 | (35.2) | 70 | (64.8) | −0.09 to 0.10 |
| Consultant | 107 | (23.6) | 38 | (35.5) | 69 | (64.5) | ||
| Executive/C-Suite | 14 | (3.1) | 2 | (14.3) | 12 | (85.7) | ||
| Individual contributor | 97 | (21.4) | 38 | (39.2) | 59 | (60.8) | ||
| Leader | 36 | (7.9) | 7 | (19.4) | 29 | (80.6) | ||
| Other (specify) | 92 | (20.3) | 34 | (37.0) | 58 | (63.0) | ||
| Influenza shot frequency | Every year | 292 | (64.3) | 25 | (8.6) | 267 | (91.4) | −0.70 to −0.55 |
| Never | 66 | (14.5) | 64 | (97.0) | 2 | (3.0) | ||
| Occasionally | 96 | (21.2) | 68 | (70.8) | 28 | (29.2) | ||
*Participants are corporate employees in three US companies; CI = 95% confidence interval.
Table 2.
Factors associated with seasonal influenza vaccination acceptance.
| Variables | Odd Ratio | 95% Wald Confidence Limits | |
|---|---|---|---|
| 20 to 29 years old vs. >65 years old | 0.3 | 0.1 | 1.4 |
| 30 to 39 years old vs. >65 years old | 0.5 | 0.1 | 2.0 |
| 40 to 49 years old vs. >65 years old | 0.6 | 0.2 | 2.3 |
| 50 to 59 years old vs. >65 years old | 0.7 | 0.2 | 2.9 |
| 60 to 64 years old vs. >65 years old | 0.6 | 0.1 | 2.6 |
| Female vs. Male | 1.2 | 0.8 | 1.8 |
| Lower than a bachelor’s degree in college (4-year) vs. bachelor’s degree in college (4-year) or higher | 0.3 | 0.1 | 0.6 |
| White vs. Others | 1.0 | 0.6 | 1.5 |
| Black vs. Others | 0.4 | 0.2 | 0.8 |
| Non-Hispanic vs Hispanic | 1.0 | 0.4 | 2.3 |
| Married or domestic partnership vs. Others | 0.9 | 0.5 | 1.4 |
| Manager vs. Other | 0.8 | 0.4 | 1.5 |
| Consultant vs. Other | 0.9 | 0.5 | 1.6 |
| Executive/C-Suite vs. Other | 1.9 | 0.4 | 9.6 |
| Individual contributor vs. Other | 0.8 | 0.4 | 1.6 |
| Leader (looks after a region or business area) vs. Other | 1.6 | 0.6 | 4.4 |
N = 454; Testing Global Null Hypothesis: BETA = 0: Probability modeled is influenza shot in the past year=‘Yes;’ R-Square = 0.07; Chi-Square = 31.6; DF = 16; Pr > ChiSq = 0.01; Convergence criterion (GCONV = 1E–8) satisfied.
Attitudes toward influenza vaccination
Cronbach’s alpha reliability test showed a global value of Alpha = 0.71 for the Attitudes scale. This highlights the good internal consistency of the questionnaire, implying that the questionnaire actually measures what it’s intended to measure. Most of the respondents had favorable attitudes toward influenza vaccination. A majority reported that vaccination of employees against influenza is important, and the benefits of vaccination are greater than the risks. Furthermore, 73.6% disagree that influenza vaccination poses a risk to their health and 69.2% believed that if they were unvaccinated, exposure to influenza would be a risk to their health (Figure 1).
Figure 1.
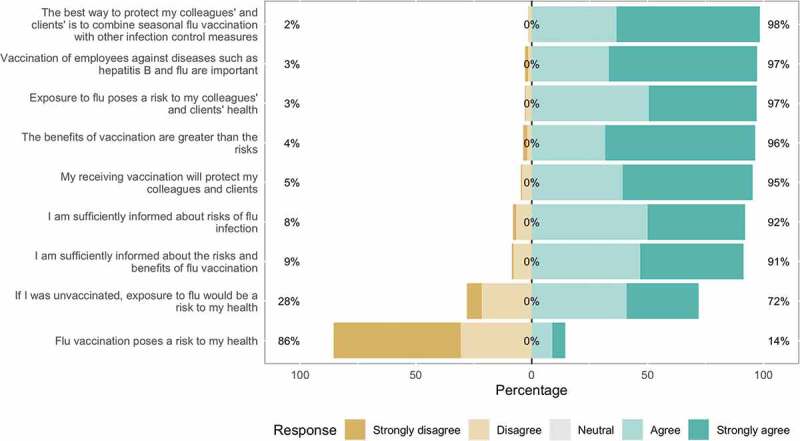
Participants’ attitudes towards influenza vaccination, April to June, 2020.
Factors that influence influenza vaccination decision-making
Cronbach’s alpha reliability test showed a global value of Alpha = 0.78 for the scale. Recommendation from a personal physician (89.4%) and contribution to pandemic preparedness (88.6%) were the top factors that would influence participants’ decision to accept influenza vaccination (Figure 2).
Figure 2.
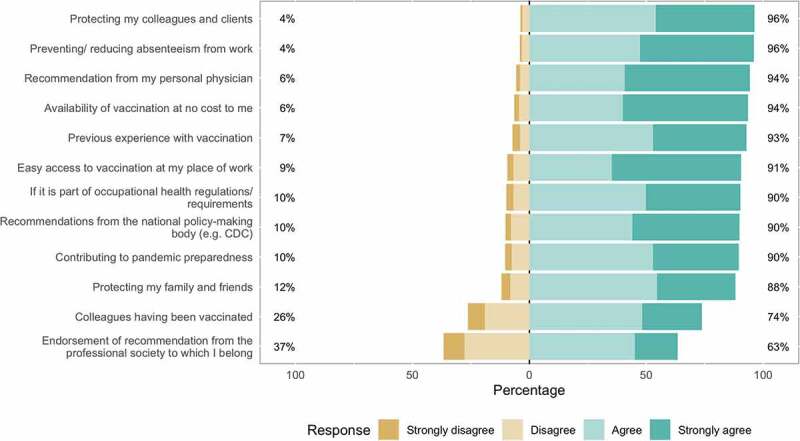
Factors that influence participants’ decision to accept influenza vaccination, April to June, 2020.
Qualitative responses
Seven themes emerged in the qualitative analysis of the responses to open-ended questions regarding factors that would influence the participants to receive the influenza vaccine (Figure 3). They include “Protecting others” (109, 24.0%), “Protecting self” (105, 23.1%), “Vaccine accessibility” (94, 20.7%), “Education and messaging” (71, 15.6%), “Policies/Requirements” (15 (3.3%), “Reminders” (9, 2.0%), and “Incentives” (3, 0.7%). The major themes were further classified by sub-themes identified during analysis (Table 3).
Figure 3.
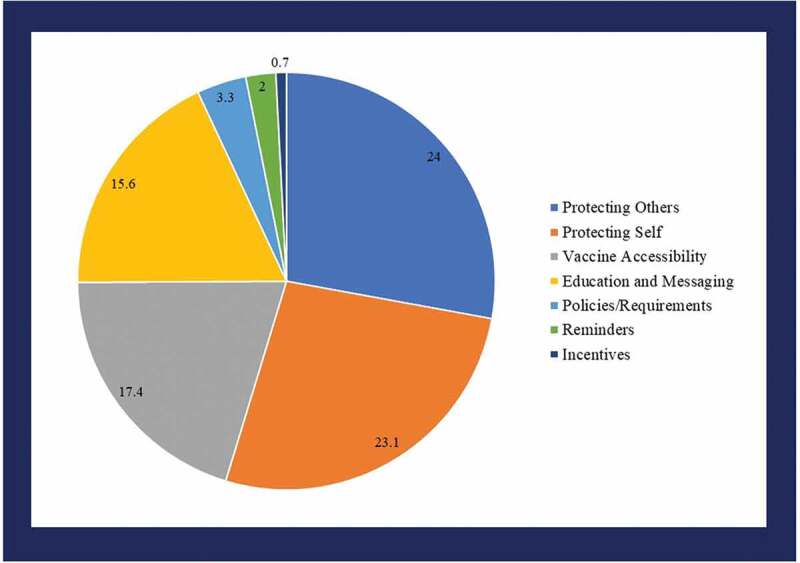
Themes identified from qualitative data: Factors that influence participants’ decision to accept influenza vaccination, April to June, 2020.
Table 3.
Qualitative results on factors influencing influenza vaccination decision-making, April–June 2020*.
| Themes sub-themes | No. (%) |
|---|---|
| Protecting Others | 109 (24.0) |
| Friends and family | 75 |
| Community | 17 |
| Peer effect | 17 |
| Protecting Self | 105 (23.1) |
| Personal health | 48 |
| Safety and side effects | 38 |
| Pro-vaccine | 16 |
| End COVID-19 pandemic | 3 |
| Vaccine Accessibility | 79 (17.4) |
| Convenience and accessibility | 62 |
| Cost of vaccine | 17 |
| Education and Messaging | 71 (15.6) |
| Information on vaccine efficacy | 37 |
| Content of vaccine messaging | 34 |
| Policies/Requirements | 15 (3.3) |
| Reminders | 9 (2.0) |
| Incentives | 3 (0.7) |
N = 454; *Participants are corporate employees in three US companies.
Protecting others
The most common theme identified among the participants as a factor that would influence their decision to get vaccinated against influenza was the desire to protect friends, family, community, and those in their direct social network from getting infected. One response falling into this category was, “The health of my family especially my parents and older relatives. I am conscientious of having had my flu shot before I visit them during the winter holiday time.” Another response indicating protection of the community as a factor stated –“I believe vaccines are the most effective way of preventing infectious diseases. By receiving a vaccination, I am contributing to society’s herd immunity for that particular viral disease.” Some participants mentioned that the desire to mitigate COVID-19 or the COVID-19 pandemic would influence them toward getting the influenza vaccine.
Protecting self
In addition to protecting others, the desire to protect self was also identified. These include participants’ comments that mentioned protection against personal health as a factor that would infleunce their decision to accept influenza vaccination. Participants who perceive themselves as being at high-risk for influenza infection stated positive attitudes toward influenza vaccine. One respondent wrote, “I spend significant amounts of time on airplanes, in hotels, and hospitals. I am exposed to lots of viruses and germs, so am a strong believer in flu vaccination. In addition, I hate to admit it, I am in my early 60‘s so I’m in a higher risk group.”
Vaccine accessibility
Access to vaccinations, the convenience of location, the time required to obtain a vaccination, or availability of a specified type of vaccine, e.g., the nasal route option were stated by some participants as factors that would influence them toward getting the influenza vaccine. Respondents mentioned that making vaccination coordination easy for them and their family members, would influence them toward getting the influenza vaccine. Examples of comments in this theme include - “Severe phobia of needles – can only get non-needle vaccinations. A nasal flu option is the only flu vaccine I have ever received, they are hard to find though.;” “Readily available – that it doesn’t take too much extra effort out of my routine to go get it. Especially having to consider the best way to get my family to also get it … it’s sometimes hard to coordinate everything.”
Education and messaging
Several participants mentioned that access to vaccine information such as the success rate and side effects, information from scientists and public figures, culturally appropriate facts, and targeted messaging would influence them toward getting the influenza vaccine. A respondent wrote, “If you want to have people more likely to take a vaccination, you need to get more buy-in starting at a young age. Targeted messaging to all age ranges. I work in healthcare and have been immersed in it, but there are people who just read headlines and think vaccines are bad. Peer pressure people with facts and supporting their fellow human beings.”
Policies/requirements
Other factors that would influence participants toward getting the influenza vaccine included requirements set by the workplace, government, or other organizations the participants are affiliated with. Some participants further stated that workplace, government, or organization policies and requirements would influence them toward accepting the influenza vaccine. An example is this statement from a participant: “The ONLY way I would consider accepting a flu vaccination is if it is REQUIRED by my employer in order to work on the property.”
Reminders
Reminders from employers, physicians, and other professionals would influence the decision to get vaccinated against influenza among participants. Some participants stated that certain messages from “extra-curricular groups we have at work” can be very influential with regard to them accepting influenza vaccination. A participant wrote: “I think the extra-curricular groups we have at work are very influential. The messaging we receive from them is very impactful.”
Incentives
Some participants mentioned that payment or other incentives such as cash or gift cards from their favorite stores would influence them toward accepting the influenza vaccination. One participant wrote: “Payment – Pay me $20 to get a flu shot and I’ll get one every year.” While another stated: “Gift card from store (Target) … ” More quotes from participants are presented in Table 4.
Table 4.
Qualitative results on factors influencing influenza vaccination decision-making, April–June 2020*.
| Themes | Sub-themes | No. (%) | |
|---|---|---|---|
| Protecting Others | 109 (24.0) | ||
| Friends and family | 17 | ||
| Community | 17 | ||
| Peer effect | 17 | ||
| Protecting Self | 105 (23.1) | ||
| Personal health | 48 | ||
| Safety and side effects | 38 | ||
| Pro-vaccine | 16 | ||
| End COVID-19 pandemic | 3 | ||
| Vaccine Accessibility | 79 (17.4) | ||
| Convenience and accessibility | 62 | ||
| Cost of vaccine | 17 | ||
| Education and Messaging | 71 (15.6) | ||
| Information on vaccine efficacy | 37 | ||
| Content of vaccine messaging | 34 | ||
| Policies/Requirements | 15 (3.3) | ||
| Reminders | 9 (2.0) | ||
| Incentives | 3 (0.7) |
[n = 454].
*Participants are corporate employees in three US companies.
Discussion
Most study participants had favorable attitudes toward influenza vaccination and reported that physician recommendation would influence their decision to accept influenza vaccination. Factors influencing acceptance of influenza vaccination included: protecting others, protecting self, vaccine accessibility, education/messaging, policies/requirements, reminders, and incentives. In this study, we found that over 65% of employees received their influenza vaccine in the past year (influenza season 2019–2020). While there are limited data specifically for US non-healthcare employees on this outcome, this rate is greater than the reported national influenza vaccination coverage (48.4% of adults aged 18 years and older) during the same season.13 This suggests that US non-healthcare employees have higher influenza vaccination coverage than the general US population. This higher-than-average vaccination rate could be due to the socio-demographic composition of corporate employees compared to the overall US population. However, there is still room for improvement, as coverage is still below the Healthy People 2030 objective.
Older participants were more likely to report getting their influenza vaccine in the past year, although our analysis did not show that this is statistically significant. Respondents aged 30 years and older reported higher influenza vaccination coverage (67.0% and higher) while those aged 29 year and younger reported coverage rate of 60.1%. This is similar to findings by O’Halloran et al., 2013, which showed younger (aged 18–49 years old) non-healthcare employees reported lower (24.6%) coverage versus those aged 50–64 years and 65 years or older who reported coverage rate of 36.3% and 53.3% respectively.23 These results are not surprising as individuals at higher risk for influenza complications include persons 65 years and older,24 which may partially explain why they are more likely to be vaccinated. Participants with higher educational attainment reported higher influenza vaccination coverage than thise with lower educational attainment. This may be because they are more knowledgeable about the benefits of vaccination.25 Public health authorities and employers need to identify and implement ways in which influenza vaccination rates may be increased for the younger population and those with lower educational attainment. They should focus more on encouraging younger age groups to reach the Health People 2030 influenza vaccination rate goal. In addition, vaccine messaging campaigns that target lower educational background populations must include simple language that is not based on scientific reasoning.
Influenza vaccination interventions at worksites during work hours have been shown to increase vaccination rates among employees.26–30 A study conducted in 2004 reported that 70% of U.S. companies offer influenza vaccination at the worksite;31 however, coverage has remained lower than Healthy People 2030 target.7 In a survey of 54 U.S. corporations, 96% of which employed 1000 full-timeworkers, only eight (15%) reported on-site influenza vaccination rates that were higher than 50%.31 The low vaccination rates highlight the importance of improving employee-site vaccination programs. Companies/employees should consider vaccination promotion initiatives offered with other worksite health promotion programs.32
Given that majority of the respondents had positive/favorable attitudes toward influenza vaccination, worksite vaccine programs may be a solution to increasing vaccination rates among the general US population. Previous studies among healthcare workers showed that higher vaccination rate was observed when influenza vaccine was offered for no cost at their worksite for more than one day.33 There are limited studies to show this effect among non healthcare workers. Additionally, there are many benefits of workplace vaccinations. For employers, increased vaccination coverage reduces illness and work absenteeism,34 maintains productivity, and improves morale. For employees, onsite vaccination to reduce vaccine-preventable diseases improves health, reduces absences due to sickness, and is generally convenient.
Our study found that most participants have positive attitudes toward vaccination, and 80% reported having easy access to vaccination at their workplace as a factor influencing their decision to accept vaccination. As the COVID-19 vaccine distribution is underway, employers should consider offering a free, on-site COVID-19 vaccination clinic during work hours. In addition to the benefits mentioned above, vaccination clinics may help save many lives, especially for employers whose employees are at increased risk for severe illness from COVID-19—including those 60 years and older and individuals with underlying medical conditions.29
On the other hand, 30% of our sample reported that exposure to influenza would not be a risk to their health if unvaccinated. We found that the recommendation from personal physicians (89%), desire to protect their colleagues and clients (80%) and wanting to contribute to pandemic preparedness (89%), would influence respondents’ influenza vaccination decision-making. Using these messages may be useful strategies for public health authorities and health-care providers in their vaccine promotion messaging campaigns. Additionally, to increase the vaccination rate, vaccine campaigns should include clear, concise language and personal narratives about protecting relatives/family members and coworkers.35 One of the sub-themes from our qualitative findings was that the reason for getting vaccinated was to protect ‘friends and family.’ Therefore, personal stories can be a powerful tool for increasing uptake of influenza vaccinations.
Furthermore, our results highlight demographic disparities in influenza vaccination rates in this sample, particularly racial and ethnic, age, and educational background. Black/African American employees had the lowest influenza vaccination rate (44%) compared to other racial groups. CDC reports similar disparities across the US population, with the influenza vaccine uptake within the non-Hispanic Black community being low at 41%.36 The vaccination rate disparity may be due to the persistent racial and ethnic inequities in access to affordable health-care services or the greater reluctance to trust medical professionals.37 Our finding is concerning considering that our entire study sample has a higher vaccination rate (65%) compared to the general US population (48.4%) and non-Hispanic Blacks have the highest overall age-adjusted rate of hospitalization (68.8%) and highest overall age-adjusted rate of intensive care unit admission (11.6%).38 This highlights the need for increased/improved promotion for vaccination coverage, especially for this group. Public health authorities must address this vaccination coverage gap by engaging with employers and community/local leaders to develop culturally specific messaging tailored to reach racial and ethnic communities when hosting employee-site vaccination clinics. Our study presents some limitations. Respondents self-reported their vaccination status, precluding any verification by health records. Furthermore, this is a voluntary survey. There is the risk of selection bias; those who participated may be more attentive to vaccination than the general employee population. We purposively selected individuals from job categorized as management occupations, business and financial operations occupations, computer and mathematical occupations, and life physical and social science occupations. While our sample size limits generalizability of our findings to the US non-healthcare population, nevertheless, the distribution of population by age and job category is similar to the overall distribution of US employees aged >16 years as given by the Bureau of Labor Statistics,1 thus we represent a diverse cross-section of the working population as shown in Table 1. The distribution of the study participants by age,39 gender, and race40 are similar to US employees’ overall distribution, thus, they represent a diverse cross-section of the working population with regard to these characteristics. Our study strengths includes the use of mixed-methods in that the qualitative research assessed the extent to which findings are supported and elaborated by evidence from respondents quotes.
In conclusion, given the findings of this study where certain age groups, races, and less knowledgeable groups are less likely to receive the influenza vaccination, corporate employers may benefit from targeted interventions to persuade vaccine-hesitant populations to receive it. Few studies have specifically focused on addressing US corporate workers – a unique socio-demographic group. Our findings could inform public health professionals/authorities planning annual influenza and COVID-19 immunization programs. They could facilitate the development of vaccination promotion messages for corporate employees and potentially guide future educational programs to improve immunization rates and health outcomes among the US working-age population. They may also provide helpful information for employers considering worksite vaccination clinics. Future research could assess predictors and barriers of influenza vaccination decision-making among specific groups within this population. It could also evaluate educational interventional studies implemented at workplaces aimed at increasing accurate knowledge of influenza vaccination to empower employees in their vaccination decision-making.
Acknowledgments
The authors thank the employees of the three companies that participated in this study. The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding Statement
This study was supported by the Centers for Diseases Control and Prevention (grant number - 5U01CK000572-02)
Disclosure statement
Dr. Inci Yildirim reports personal fees from Merck outside the submitted work. The authors list no other conflicts of interest. Alessia Melegaro acknowledges funding from the European Research Council (ERC) under Horizon 2020 research and innovation program (Grant agreement No. 101003183).
References
- 1.Centers for Disease Control and Prevention . Key facts about influenza (Flu) [Internet]. Centers for Disease Control and Prevention; 2020. [accessed 2021 Mar 18]. https://www.cdc.gov/flu/about/keyfacts.htm.
- 2.Centers for Disease Control and Prevention . Estimated influenza illnesses, medical visits, hospitalizations, and deaths in the United States—2019–2020 influenza season [Internet]. CDC; 2020. [accessed 2021 Apr 5]. https://www.cdc.gov/flu/about/burden/2019-2020.html.
- 3.US Census Bureau . 22 Million employed in health care fight against COVID-19 [Internet]. Census.gov; [accessed 2022 Mar 20]. https://www.census.gov/library/stories/2021/04/who-are-our-health-care-workers.html.
- 4.Statista . Number of employees in the U.S. by industry February 2022 [Internet]. Statista; 2022. [accessed 2022 Mar 20]. https://www.statista.com/statistics/978479/number-employees-united-states-industry/.
- 5.Centers for Disease Control and Prevention . Flu vaccination coverage, United States, 2020–21 influenza season [Internet]. Centers for Disease Control and Prevention; 2021. [accessed 2022 May 23]. https://www.cdc.gov/flu/fluvaxview/coverage-2021estimates.htm.
- 6.Centers for Disease Control and Prevention . Weekly Flu Vaccination Dashboard [Internet]. Centers for Disease Control and Prevention; 2022. [accessed 2022 May 23]. https://www.cdc.gov/flu/fluvaxview/dashboard/vaccination-dashboard.html.
- 7.Office of Disease Prevention and Health Promotion . Healthy people 2020 topics and objectives: immunization and infectious diseases [Internet]; 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives.
- 8.Department for Professional Employees . The professional and technical workforce: by the numbers [Internet]. Department for Professional Employees. AFL-CIO; 2019. [accessed 2021 Aug 18]. https://www.dpeaflcio.org/factsheets/the-professional-and-technical-workforce-by-the-numbers.
- 9.Dini G, Toletone A, Sticchi L, Orsi A, Bragazzi NL, Durando P.. Influenza vaccination in healthcare workers: a comprehensive critical appraisal of the literature. Hum Vacc Immunother [Internet]. 2017. [accessed 2021 Aug 18];14(3):1–9. doi: 10.1080/21645515.2017.1348442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smetana J, Chlibek R, Shaw J, Splino M, Prymula R. Influenza vaccination in the elderly. Hum Vacc Immunother [Internet]. 2017. [accessed 2021 Aug 18];14(3):540–49. doi: 10.1080/21645515.2017.1343226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trucchi C, Paganino C, Orsi A, De Florentis D, Ansaldi F. Influenza vaccination in the elderly: why are the overall benefits still hotly debated? J Prev Med Hyg [Internet]. 2015. [accessed 2021 Aug 18];56:E37–43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4718343/. [PMC free article] [PubMed] [Google Scholar]
- 12.Chapman GB, Coups EJ. Predictors of influenza vaccine acceptance among healthy adults. Prev Med [Internet]. 1999;29(4):249–62. doi: 10.1006/pmed.1999.0535. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention . Flu vaccination coverage, United States, 2019–20 influenza season | FluVaxview | Seasonal Influenza (Flu) | CDC [Internet]. Centers for Disease Control and Prevention; 2020. [accessed 2021 Mar 18]. https://www.cdc.gov/flu/fluvaxview/coverage-1920estimates.htm.
- 14.Conlon A, Ashur C, Washer L, Eagle KA, Bowman MAH. Impact of the influenza vaccine on COVID-19 infection rates and severity. Am J Infect Control [Internet]. 2021. [accessed 2021 Mar 18]. https://www.ajicjournal.org/article/S0196-65532100089-4/abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zanettini C, Omar M, Dinalankara W, Imada EL, Colantuoni E, Parmigiani G, Marchionni L. Influenza vaccination and COVID19 mortality in the USA. medRxiv [Internet]. 2020. [accessed 2021 Mar 18]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7325191/. [DOI] [PMC free article] [PubMed]
- 16.Centers for Disease Control and Prevention (CDC) . Benefits of flu vaccination during 2018-2019 flu season [Internet]. Centers for Disease Control and Prevention (CDC); 2020. [accessed 2021 Apr 5]. https://www.cdc.gov/flu/about/burden-averted/2019-2020.htm.
- 17.Rondy M, El Omeiri N, Thompson MG, Levêque A, Moren A, Sullivan SG. Effectiveness of influenza vaccines in preventing severe influenza illness among adults: a systematic review and meta-analysis of test-negative design case-control studies. J Infect [Internet]. 2017;75(5):381–94. doi: 10.1016/j.jinf.2017.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention . Study Shows Flu Vaccine Reduces Risk of Severe Illness [Internet]. Centers for Disease Control and Prevention; 2019. [accessed 2021 Aug 18]. https://www.cdc.gov/flu/spotlights/2017-2018/vaccine-reduces-risk-severe-illness.htm.
- 19.Centers for Disease Control and Prevention . Flu Vaccines Benefits [Internet]. Centers for Disease Control and Prevention; 2021. [accessed 2021 Mar 18]. https://www.cdc.gov/flu/prevent/vaccine-benefits.htm.
- 20.Kiti MC, Aguolu OG, Liu CY, Mesa AR, Regina R, Woody M, Willebrand K, Couzens C, Bartelsmeyer T, Nelson KN, et al. Social contact patterns among employees in 3 U.S. companies during early phases of the COVID-19 pandemic, April to June 2020. Epidemics [Internet]. 2021. [accessed 2021 Jun 18];100481. doi: 10.1016/j.epidem.2021.100481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Law Insider . Corporate employee definition [Internet]. Law Insider; 2021. [accessed 2021 Aug 18]. https://www.lawinsider.com/dictionary/corporate-employee.
- 22.World Health Organization . How to implement seasonal influenza vaccination of health workers [Internet]. WHO; 2019. [accessed 2021 Apr 16]. http://www.who.int/immunization/documents/ISBN_9789241515597/en/.
- 23.O’Halloran AC, Lu P, Williams WW, Schumacher P, Sussell A, Birdsey J, Boal WL, Sweeney MH, Luckhaupt SE, Black CL, et al. Influenza vaccination among workers—21 U.S. states, 2013. Am J Infect Control [Internet]. 2017. [accessed 2022 May 17];45(4):410–16. doi: 10.1016/j.ajic.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention . People at high risk of flu [Internet]. Centers for Disease Control and Prevention; 2021. [accessed 2021 Mar 20]. https://www.cdc.gov/flu/highrisk/index.htm.
- 25.Kempe A, Saville AW, Albertin C, Zimet G, Breck A, Helmkamp L, Vangala S, Dickinson LM, Rand C, Humiston S, et al. Parental hesitancy about routine childhood and influenza vaccinations: a national survey. Pediatrics [Internet]. 2020. [accessed 2021 Mar 20];146. https://pediatrics.aappublications.org/content/146/1/e20193852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ofstead CL, Sherman BW, Wetzler HP, Dirlam Langlay AM, Mueller NJ, Ward JM, Ritter DR, Poland GA. Effectiveness of worksite interventions to increase influenza vaccination rates among employees and families. J Occup Environ Med [Internet]. 2013;55(2):156–63. doi: 10.1097/JOM.0b013e3182717d13. [DOI] [PubMed] [Google Scholar]
- 27.Landwehr K, Trees WJ, Reutman S. A quality improvement project to improve influenza vaccination rates among employees at an onsite employer-based health clinic. Workplace Health Saf [Internet]. 2021. [accessed 2022 Mar 20];69:448–54. doi: 10.1177/21650799211016906. [DOI] [PubMed] [Google Scholar]
- 28.Baskin E. Increasing influenza vaccination rates via low cost messaging interventions. Plos One [Internet]. 2018. [accessed 2022 Mar 20];13(2):e0192594. doi: 10.1371/journal.pone.0192594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention . Workplace Vaccination Program [Internet]. Centers for Disease Control and Prevention. 2021. [accessed 2021 Mar 20]. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/essentialworker/workplace-vaccination-program.html.
- 30.D’Heilly SJ, Nichol KL. 2004. Work-site-based influenza vaccination in healthcare and non-healthcare settings. Infect Control Hosp Epidemiol. 25(11):941–45. doi: 10.1086/502324. [DOI] [PubMed] [Google Scholar]
- 31.Nowalk MP, Lin CJ, Toback SL, Rousculp MD, Eby C, Raymund M, Zimmerman RK. Improving Influenza Vaccination Rates in the Workplace: a Randomized Trial. Am J Prev Med [Internet]. 2010. [accessed 2021 Mar 20];38(3):237–46. doi: 10.1016/j.amepre.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention . Promoting Vaccination in the Workplace [Internet]. Centers for Disease Control and Prevention. 2021. [accessed 2021 Mar 20]. https://www.cdc.gov/flu/business/promoting-vaccines-workplace.htm.
- 33.Centers for Disease Control and Prevention . Influenza Vaccination Coverage Among Health Care Personnel — United States, 2018–19 Influenza Season | FluVaxview | Seasonal Influenza (Flu) [Internet]; 2019. [accessed 2022 May 17]. https://www.cdc.gov/flu/fluvaxview/hcp-coverage_1819estimates.htm.
- 34.Cancelliere C, Cassidy JD, Ammendolia C, Côté P. Are workplace health promotion programs effective at improving presenteeism in workers? a systematic review and best evidence synthesis of the literature. BMC Public Health [Internet]. 2011. [accessed 2021 Mar 20];11(1):395. doi: 10.1186/1471-2458-11-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention . CDC Digital Media Toolkit: 2020-21 Flu Season [Internet]. Centers for Disease Control and Prevention. 2020. [accessed 2021 Mar 20]. https://www.cdc.gov/flu/resource-center/toolkit/index.htm.
- 36.Centers for Disease Control and Prevention . Racial and Ethnic Minority Groups [Internet]. Cent Dis Control Prev. 2021. [accessed 2021 Mar 20]. https://www.cdc.gov/flu/highrisk/disparities-racial-ethnic-minority-groups.html. [Google Scholar]
- 37.Hill L, Artiga S, Haldar S. Key Facts on Health and Health Care by Race and Ethnicity [Internet]. KFF; 2019. [accessed 2021 Mar 20]. https://www.kff.org/report-section/key-facts-on-health-and-health-care-by-race-and-ethnicity-coverage-access-to-and-use-of-care/.
- 38.Centers for Disease Control and Prevention . Flu Disparities Among Racial and Ethnic Minority Groups [Internet]. Centers for Disease Control and Prevention. 2021. [accessed 2022 May 23]. https://www.cdc.gov/flu/highrisk/disparities-racial-ethnic-minority-group.html.
- 39.Bureau of Labor Statistics . Labor Force Statistics from the Current Population Survey [Internet]; 2019. https://www.bls.gov/cps/cpsaat18b.htm.
- 40.The Washington Post . The Washington Post’s Workforce Demographics [Internet]. Washington Post; 2021. [accessed 2022 Mar 21]. https://www.washingtonpost.com/pr/2021/07/28/workforce-demographics/.


