Abstract
Backgrounds:
Cardiovascular disease (CVD) remains the leading cause of deaths nationwide. However, little is understood about its temporal trend and corresponding influence on longevity improvements. We aimed to describe the updated tendency in CVD mortality and to quantify its impact on life expectancy (LE) increase in China.
Methods:
All-cause mortality rates were calculated with population sizes from the National Bureau of Statistics and death counts from the National Health Commission. We estimated CVD mortality rates by allocating age- and sex-based mortality envelopes to each CVD subtype based on its proportion derived from the Disease Surveillance Points system. The probability of CVD premature deaths and LE were calculated with life tables and we adopted Arriaga's method to quantitate age- and cause-specific contributions to LE gains.
Results:
During 2013 to 2018, the age-standardized mortality rate of CVD decreased from 289.69 (95% confidence interval [CI]: 289.03, 290.35)/100,000 to 272.37 (95%CI: 271.81, 272.94)/100,000, along with a decline in probability of CVD premature deaths from 9.05% (95%CI: 9.02%, 9.09%) to 8.13% (95%CI: 8.10%, 8.16%). The gap in CVD mortality across sexes expanded with more remarkable declines in females, especially for those aged 15 to 64 years. Among major subtypes, the probability of premature deaths from hemorrhage stroke declined fastest, while improvements of ischemic stroke and ischemic heart disease were limited, and there was an increase in stroke sequelae. LE in China reached 77.04 (95%CI: 76.96, 77.12) years in 2018 with an increase of 1.38 years from 2013. Of the total LE gains, 21.15% (0.29 years) were attributed to reductions of CVD mortality in the overall population, mostly driven by those aged >65 years.
Conclusions:
The general process in reducing CVD mortality has contributed to longevity improvements in China. More attention should be paid to prevention and control of atherosclerotic CVD and stroke sequelae, especially for the elderly. Working-age males also deserve additional attention due to inadequate improvements.
Keywords: Aged; Cardiovascular diseases; Causes of death; Hemorrhagic stroke; Ischemic stroke; Longevity; Mortality, premature; Myocardial ischemia; Life expectancy; China
Introduction
Under the process of urbanization and social transition, life expectancy (LE) of the Chinese population has reached 77.3 years in 2019 with a rapid increase of >42 years since 1949.[1] Meanwhile, there have been dramatic changes in the cause-specific death spectra, and the impact of population ageing has also gradually appeared, leading to a marked shift in the major contributor to LE increases. In the past China, longevity improvements were mainly promoted by reduced infant deaths and were largely attributed to constant declines in mortality from diarrhea, lower respiratory diseases, and other common infectious diseases. On the other hand, since the early 21st century, the contribution to LE has been centralized more on the elderly, and the predominant driving force of gains in LE has turned to reductions in mortality from non-communicable diseases (NCDs), among which cardiovascular diseases (CVDs) contributed the most.[2] However, it should never be ignored that CVDs are still the leading cause of nationwide mortality, accounting for approximately 4.6 million deaths in 2019.[3] In addition, a deteriorating situation of atherosclerotic CVDs has been observed in China, despite a downward trend in most developed countries.[4–6]
Taking population health as the top priority for national development, the Chinese government released a series of policies to promote health throughout the nation. In response to the Sustainable Development Goals, The Healthy China 2030 Initiative put forward targets for increasing LE to 79.0 years and reducing the probability of premature deaths from major NCDs by 30% relative to the 2015 levels.[7] Correspondingly, The Medium-to-Long Term Plan for the Prevention and Treatment of NCD (2017–2025) issued by the State Council reiterated the goal of reducing age-standardized mortality rates of CVDs in China. To achieve these national health project targets, it is indispensable to evaluate the temporal trend in CVD mortality and its impact on longevity promotion. However, current nationwide evidence is limited and dispersed in China. Previous studies only focused on the burden of CVDs without further consideration of its corresponding influence on LE.[8–10] Several studies have reported the impact of transitions in CVD epidemic on LE, whereas most of them were conducted at province-level or based on earlier epidemiological data.[11–14] In addition, the potentially heterogeneous impact of various CVD subtypes on LE improvement has not been well evaluated in China.[2]
Based on consecutive nationally representative cause-specific mortality data derived from the National Health Commission (NHC), the current study investigated the contemporary trend in mortality and the probability of premature deaths from total CVD and its subtypes during 2013 to 2018 in China, and further quantified its contributions to longevity improvement, both in overall and sex-specific Chinese population. Hong Kong, Macao, and Taiwan were excluded from the scope of this study due to insufficiency in data.
Methods
Data sources
We obtained annual population counts by age and sex in China from the National Bureau of Statistics (NBS), which were estimated based on National Population Censuses, Intercensal Surveys, and Annual Surveys on Population Changes. Information of all-cause mortality was primarily obtained from the death and population registration system of the NHC. To minimize the impact of death underreporting, mortality records from multiple administrative departments were also incorporated as supplementary data, including data from Ministry of Public Security, Ministry of Civil Affairs, and Ministry of Human Resources and Social Security. After cross-validation and de-duplication based on the unique Citizen Identification Number, the integrated mortality database contained more than 9 million death records annually, which covered most decedents in China.
Data on the underlying cause of deaths were available from China's Disease Surveillance Points (DSP) system, which was established in 1978 and enlarged several times in the last decades. Since 2013, the DSP system has expanded to 605 surveillance points across 31 province-level administrative units in China, which covers >24% of the entire population and provides nationally representative mortality statistics. In each DSP area (either an urban district or a rural county), causes of deaths are first determined by well-trained staff at local hospitals (for in-hospital mortality) or community health centers (for deaths outside hospitals) and coded according to the 10th version of the International Classification of Disease (ICD-10). Thereafter, all certifications are submitted online through the national Death Information System. The complete list of death is rechecked using the automatic coding software in the online system, and if necessary, by qualified staff at the National Center for Disease Control and Prevention.[15]
To avoid the potential influence of delayed death reports, the current analyses only covered deaths reported for calendar years 2013 to 2018. In addition, 10 out of the 605 DSP sites (3 sites in east China, 5 in central China, and 2 in west China) were excluded due to missing mortality data in any year during the study period to ensure consistency of sample population [Supplementary Table 1].
Statistical analyses
Overall and sex-specific estimates of all-cause mortality rates were primarily generated for the entire age span from 0 to ≥85 years in mostly 5-year age intervals, based on the aggregated data on population sizes from the NBS and death counts from the above-mentioned integrated mortality database. We further adopted the modified capture-recapture method to adjust for the underreported deaths for those <5 years and applied the Kannisto model to revise mortality rates at advanced ages.[16,17]
Based on the underlying cause of deaths coded with ICD-10, we arranged deaths caused by CVDs in a hierarchy with each level composed of causes mutually exclusive and collectively exhaustive [Supplementary Table 2]: The first level was a composite of CVDs; the second level was comprised of three major subsets classified as heart diseases, cerebrovascular diseases, and other CVDs; and the third level included four subtypes of heart diseases (ischemic heart diseases [IHD], hypertensive heart diseases [HHD], rheumatic heart diseases [RHD], and other heart diseases) and six subtypes of cerebrovascular diseases (hemorrhagic stroke [HS], ischemic stroke [IS], unspecific stroke, sequelae of stroke, hypertensive encephalopathy, and other cerebrovascular diseases).
CVD mortality rates were estimated by allocating all-cause mortality envelopes to each CVD subtype based on its proportion of total deaths from the annual DSP sample sites, stratified by sex and age. To enhance the validity of cause-specific mortality rates, deaths encoded as codes that should not be the underlying cause of deaths (often known as garbage codes) were reassigned before analyses. Deaths incorrectly classified as heart failure and other ill-defined CVD causes were redistributed pro-rata as deaths due to IHD and chronic obstructive pulmonary diseases (COPD) for people aged ≥50 years, and due to IHD, COPD, congenital heart anomalies, and other heart diseases for those aged <50 years, in accordance with the Global Health Estimates [Supplementary Tables 3 and 4].[18] Further, we reassigned all deaths coded as chronic cardiopulmonary diseases (I27.9) to COPD, in line with previous analyses conducted in China.[19,20]
To reduce the influence of population ageing, we calculated the age-standardized CVD mortality rate and its 95% confidence intervals (95% CIs) based on China's 2010 census population structure.[21] Using the age grouping criteria adopted by NBS (young population: <15 years; working-age population: 15–64 years; and elderly population: ≥65 years), the age-standardized mortality rates stratified by age at deaths were also calculated to explore the potential differences across age groups. The probability of premature deaths and its 95% CI due to total CVD and its subtypes were calculated with age-specific CVD mortality rates using the standard life table method, which reflected the unconditional probability of deaths from CVDs between exact ages 30 and 70.[22] To evaluate temporal trends in the age-standardized mortality rates and probability of premature deaths, we estimated the annual percentage change (APC) and its 95% CI by fitting log-linear regression models.
LE at birth was estimated based on period abridged life tables, assuming that a hypothetical cohort was subject throughout its lifetime to current age-specific death rates.[23] To further investigate the age- and cause-specific contributions to longevity improvement, we decomposed life gains during the study period with Arriaga's method.[24] Details on calculating the probability of premature deaths, APC, LE, and Arriaga decomposition have been provided in section II of the supplementary materials.
Statistical analyses were performed with SAS 9.4 (SAS Institute, Cary, NC) and R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Trends in the age-standardized mortality rates from CVDs
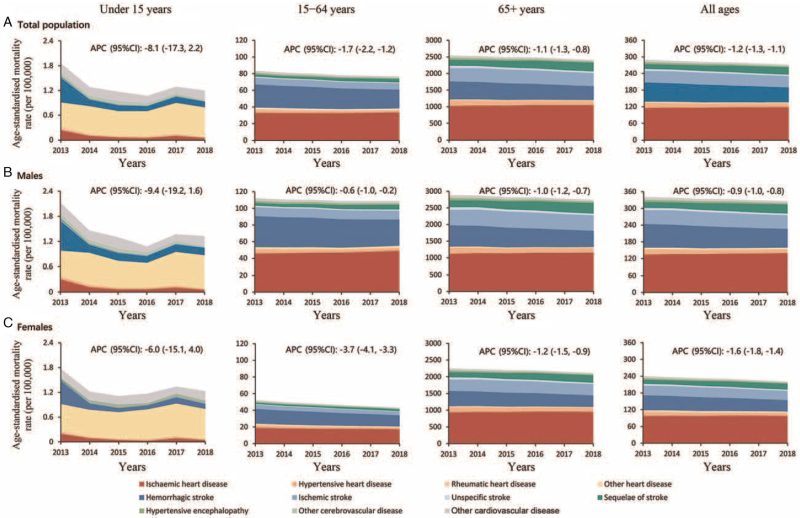
We observed a consistent downward tendency in the age-standardized mortality rates for total CVDs among overall Chinese population, from 289.69 (95% CI: 289.03, 290.35)/100,000 in 2013 to 272.37 (95% CI: 271.81, 272.94)/100,000 in 2018 [Table 1]. The age-standardized mortality rates declined remarkably for most subtypes of heart diseases, including HHD and RHD, while there was a slight increase (APC: 0.51% [95% CI: 0.27%, 0.76%]) for IHD, mostly driven by rises among the elderly [Figure 1]. In addition, we observed significant reductions in age-standardized mortality rates of cerebrovascular diseases, among which HS (APC: −5.04% [95% CI: −5.76%, −4.32%]) declined much rapidly than IS (APC: −0.70% [95% CI: −2.03%, 0.63%]). Nevertheless, a notable rise was observed in stroke sequelae, which increased from 17.97 (95% CI: 17.81,18.14)/100,000 to 26.92 (95% CI: 26.75, 27.10)/100,000 over the study period.
Table 1.
Trends in age−standardized mortality rates of total and each subtype of CVDs in overall Chinese population, 2013 to 2018.
| Age-standardized mortality rate (95% CI), per 100,000 | |||||||
| Diseases | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | APC (95% CI), % |
| Total CVD | 289.69 (289.03, 290.35) | 285.81 (285.19, 286.44) | 281.91 (281.29, 282.52) | 280.07 (279.47, 280.66) | 275.91 (275.32, 276.49) | 272.37 (271.81, 272.94) | −1.20 (−1.34, −1.07) |
| Heart disease | 138.35 (137.90, 138.80) | 138.04 (137.61, 138.47) | 135.97 (135.54, 136.39) | 136.15 (135.74, 136.56) | 136.02 (135.61, 136.42) | 136.08 (135.68, 136.49) | −0.36 (−0.7, −0.02) |
| Ischemic heart disease | 115.50 (115.09, 115.91) | 116.77 (116.37, 117.17) | 116.63 (116.24, 117.02) | 118.14 (117.76, 118.53) | 118.25 (117.87, 118.63) | 118.53 (118.15, 118.90) | 0.51 (0.27, 0.76) |
| Hypertensive heart disease | 16.83 (16.67, 16.99) | 14.92 (14.78, 15.06) | 13.56 (13.43, 13.69) | 12.66 (12.53, 12.78) | 12.39 (12.27, 12.51) | 12.20 (12.08, 12.32) | −6.39 (−9.38, −3.39) |
| Rheumatic heart disease | 3.59 (3.51, 3.66) | 3.66 (3.59, 3.74) | 3.24 (3.17, 3.31) | 2.97 (2.91, 3.03) | 2.98 (2.92, 3.05) | 2.97 (2.92, 3.04) | −4.72 (−7.75, −1.68) |
| Other heart disease | 2.44 (2.38, 2.50) | 2.69 (2.63, 2.75) | 2.54 (2.48, 2.6) | 2.38 (2.32, 2.43) | 2.40 (2.34, 2.45) | 2.38 (2.33, 2.44) | −1.52 (−4.44, 1.40) |
| Cerebrovascular disease | 145.56 (145.09, 146.02) | 142.22 (141.78, 142.66) | 141.19 (140.75, 141.62) | 139.52 (139.09, 139.94) | 135.84 (135.43, 136.25) | 132.22 (131.82, 132.62) | −1.80 (−2.30, −1.30) |
| Hemorrhagic stroke | 69.02 (68.70, 69.35) | 66.52 (66.21, 66.82) | 63.79 (63.49, 64.08) | 60.58 (60.30, 60.86) | 57.21 (56.94, 57.49) | 53.65 (53.39, 53.91) | −5.04 (−5.76, −4.32) |
| Ischemic stroke | 41.80 (41.55, 42.05) | 43.08 (42.84, 43.32) | 43.21 (42.97, 43.45) | 42.47 (42.24, 42.71) | 41.25 (41.02, 41.47) | 40.99 (40.77, 41.21) | −0.70 (−2.03, 0.63) |
| Unspecific stroke | 7.29 (7.19, 7.40) | 6.55 (6.45, 6.64) | 5.90 (5.81, 5.99) | 5.76 (5.68, 5.85) | 5.27 (5.19, 5.35) | 5.07 (4.99, 5.14) | −7.12 (−8.98, −5.26) |
| Sequelae of stroke | 17.97 (17.81, 18.14) | 17.96 (17.81, 18.12) | 20.76 (20.59, 20.92) | 23.88 (23.7, 24.05) | 25.8 (25.63, 25.98) | 26.92 (26.75, 27.10) | 9.28 (6.39, 12.17) |
| Hypertensive encephalopathy | 5.85 (5.75, 5.94) | 4.98 (4.90, 5.07) | 4.63 (4.55, 4.71) | 4.24 (4.16, 4.31) | 3.60 (3.53, 3.67) | 3.12 (3.06, 3.19) | −12.01 (−14.08, −9.95) |
| Other cerebrovascular disease | 3.62 (3.55, 3.69) | 3.13 (3.06, 3.19) | 2.91 (2.85, 2.97) | 2.59 (2.53, 2.64) | 2.71 (2.65, 2.77) | 2.47 (2.42, 2.53) | −7.03 (−10.58, −3.48) |
| Other CVD | 5.78 (5.69, 5.88) | 5.55 (5.47, 5.64) | 4.75 (4.67, 4.83) | 4.40 (4.33, 4.48) | 4.05 (3.98, 4.12) | 4.07 (4,4.14) | −7.93 (−10.82, −5.04) |
Age-standardized mortality rate was computed with the direct method using the standard population structure from China's 2010 census conducted by the National Bureau of Statistics. APC: Annual percentage change; CI: Confidence interval; CVD: Cardiovascular disease.
Figure 1.
Trends in age-standardized mortality rates of (A) total and each subtype of CVD by age at death in overall and (B,C) sex-specific Chinese population, 2013 to 2018. APC: Annual percent change; CI: Confidence interval; CVD: Cardiovascular disease.
The age-standardized mortality rates [95% CI] for CVDs from 2013 to 2018 were consistently higher in men (from 341.55 [340.51, 342.59]/100,000 in 2013 to 326.29 [325.37, 327.20]/100,000 in 2018) than women (from 240.00 [239.18, 240.82]/100,000 in 2013 to 220.93 [220.24, 221.62]/100,000 in 2018), and the differences between sexes were particularly pronounced for the working-age group [Supplementary Table 5]. Moreover, the annual decline was also much gentler in men (APC: −0.63% [95% CI: −1.04%, −0.21%]) than in women (APC: −3.74% [95% CI: −4.15%, −3.33%]) within the 15 to 64 age interval (P < 0.001). However, no such difference was observed between sexes for decedents aged <15 years (P = 0.64) and aged ≥65 years (P = 0.80).
Trends in the probability of premature deaths from CVDs
Along with changes in the age-standardized mortality rates, we observed a decline in the risk (95% CI) of dying from total CVDs in those aged 30 to 70 years, from 9.05% (9.02%, 9.09%) in 2013 to 8.13% (8.10%, 8.16%) in 2018 [Table 2]. Although premature deaths [95%CI] attributed to cerebrovascular diseases (4.89% [4.86%, 4.92%] in 2013 and 4.22% [4.19%, 4.24%] in 2018) remained greater than heart diseases (4.19% [4.17%, 4.22%] in 2013 and 3.94% [3.92%, 3.97%] in 2018), the gap was narrower due to a faster APC (95% CI) of declines in cerebrovascular diseases (−2.85% [−3.10%, −2.60%]) compared with heart diseases (−1.21% [−1.90%, −0.52%]). In the third level of cause hierarchy, probability of premature deaths (95%CI) for HS dropped significantly from 2.88% (2.86%, 2.91%) to 2.25% (2.24%, 2.27%) with an APC (95% CI) of −4.91% (−5.43%, −4.39%), whereas the decreasing trend was much slower for IS and there was even an increase in the sequelae of stroke. Among the major subtypes of heart diseases, the probability of premature deaths from IHD remained constant between 2013 and 2018, despite a remarkable increase in IHD mortality rates observed among the elderly. On the other hand, the probability of premature deaths attributed to HHDs (APC: −9.68% [95% CI: −14.11%, −5.25%]) and RHDs (APC: −6.78% [95% CI: −9.45%, −4.12%]) decreased rapidly.
Table 2.
Trends in probability of premature deaths due to total and each subtype of CVDs in overall and sex−specific Chinese population aged 30 to 70 years, 2013 to 2018.
| Probability of premature death (95% CI), % | |||||||
| Population | In 2013 | In 2014 | In 2015 | In 2016 | In 2017 | In 2018 | APC (95% CI), % |
| Overall population | |||||||
| Total CVD | 9.05 (9.02, 9.09) | 8.79 (8.75, 8.82) | 8.58 (8.55, 8.62) | 8.42 (8.38, 8.45) | 8.28 (8.25, 8.32) | 8.13 (8.10, 8.16) | −2.10 (−2.42, −1.77) |
| Heart disease | 4.19 (4.17, 4.22) | 4.09 (4.07, 4.12) | 4.00 (3.98, 4.02) | 3.96 (3.94, 3.98) | 3.95 (3.93, 3.97) | 3.94 (3.92, 3.97) | −1.21 (−1.90, −0.52) |
| Ischemic heart disease | 3.51 (3.49, 3.54) | 3.48 (3.45, 3.50) | 3.45 (3.42, 3.47) | 3.46 (3.44, 3.48) | 3.47 (3.45, 3.49) | 3.48 (3.46, 3 .50) | −0.14 (−0.54, 0.26) |
| Hypertensive heart disease | 0.46 (0.45, 0.47) | 0.38 (0.37, 0.39) | 0.33 (0.33, 0.34) | 0.03 (0.30, 0.31) | 0.29 (0.28, 0.29) | 0.28 (0.27, 0.28) | −9.68 (−14.11, −5.25) |
| Rheumatic heart disease | 0.15 (0.15, 0.16) | 0.15 (0.15, 0.16) | 0.14 (0.13, 0.14) | 0.12 (0.12, 0.13) | 0.12 (0.11, 0.12) | 0.11 (0.10, 0.11) | −6.78 (−9.45, −4.12) |
| Other heart disease | 0.10 (0.09, 0.10) | 0.11 (0.10, 0.11) | 0.10 (0.10, 0.11) | 0.09 (0.09, 0.10) | 0.09 (0.09, 0.10) | 0.10 (0.09, 0.10) | −2.02 (−6.93, 2.89) |
| Cerebrovascular disease | 4.89 (4.86, 4.92) | 4.72 (4.69, 4.75) | 4.62 (4.59, 4.64) | 4.49 (4.47, 4.52) | 4.37 (4.35, 4.40) | 4.22 (4.19, 4.24) | −2.85 (−3.10, −2.60) |
| Hemorrhagic stroke | 2.88 (2.86, 2.91) | 2.77 (2.75, 2.79) | 2.65 (2.63, 2.67) | 2.51 (2.50, 2.53) | 2.40 (2.38, 2.42) | 2.25 (2.24, 2.27) | −4.91 (−5.43, −4.39) |
| Ischemic stroke | 1.16 (1.14,1.17) | 1.17 (1.16,1.19) | 1.16 (1.14,1.17) | 1.11 (1.10,1.13) | 1.08 (1.07,1.10) | 1.07 (1.06,1.08) | −1.97 (−3.02, −0.91) |
| Unspecific stroke | 0.18 (0.18, 0.19) | 0.16 (0.16, 0.17) | 0.15 (0.14, 0.15) | 0.14 (0.13, 0.14) | 0.13 (0.12, 0.13) | 0.12 (0.12, 0.13) | −7.77 (−8.76, −6.78) |
| Sequelae of stroke | 0.41 (0.40, 0.42) | 0.41 (0.40, 0.42) | 0.47 (0.46, 0.48) | 0.56 (0.55, 0.57) | 0.62 (0.61, 0.63) | 0.64 (0.63, 0.65) | 10.41 (6.95, 13.86) |
| Hypertensive encephalopathy | 0.20 (0.20, 0.21) | 0.17 (0.17, 0.18) | 0.16 (0.16, 0.17) | 0.15 (0.15, 0.16) | 0.12 (0.12, 0.13) | 0.11 (0.10, 0.11) | −11.71 (−14.69, −8.73) |
| Other cerebrovascular disease | 0.12 (0.11, 0.12) | 0.10 (0.09, 0.10) | 0.09 (0.09, 0.09) | 0.08 (0.07, 0.08) | 0.08 (0.08, 0.09) | 0.08 (0.08, 0.08) | −8.04 (−12.97, −3.11) |
| Other CVD | 0.19 (0.19, 0.20) | 0.18 (0.18, 0.19) | 0.16 (0.16, 0.17) | 0.15 (0.15, 0.16) | 0.15 (0.14, 0.15) | 0.15 (0.14, 0.15) | −5.12 (−8.17, −2.08) |
| Males | |||||||
| Total CVD | 11.31 (11.25, 11.37) | 11.16 (11.1, 11.21) | 11.1 (11.05, 11.16) | 10.96 (10.91, 11.01) | 10.85 (10.8, 10.9) | 10.77 (10.72, 10.82) | −0.98 (−1.10, −0.85) |
| Heart disease | 5.27 (5.22, 5.31) | 5.23 (5.20, 5.27) | 5.22 (5.18, 5.26) | 5.19 (5.16, 5.23) | 5.21 (5.18, 5.25) | 5.30 (5.26, 5.33) | 0.03 (−0.54, 0.61) |
| Ischemic heart disease | 4.49 (4.45, 4.52) | 4.52 (4.49, 4.56) | 4.57 (4.54, 4.61) | 4.61 (4.57, 4.65) | 4.64 (4.6, 4.67) | 4.74 (4.70, 4.77) | 1.02 (0.74, 1.31) |
| Hypertensive heart disease | 0.56 (0.54, 0.57) | 0.47 (0.46, 0.49) | 0.42 (0.41, 0.43) | 0.38 (0.37, 0.39) | 0.37 (0.36, 0.38) | 0.36 (0.35, 0.37) | −8.65 (−12.62, −4.68) |
| Rheumatic heart disease | 0.13 (0.12, 0.14) | 0.13 (0.12, 0.14) | 0.12 (0.11, 0.12) | 0.11 (0.10, 0.11) | 0.11 (0.10, 0.11) | 0.10 (0.09, 0.10) | −5.43 (−7.31, −3.55) |
| Other heart disease | 0.13 (0.13, 0.14) | 0.14 (0.13, 0.15) | 0.14 (0.13, 0.15) | 0.13 (0.12, 0.13) | 0.13 (0.12, 0.13) | 0.13 (0.13, 0.14) | −0.85 (−3.43, 1.74) |
| Cerebrovascular disease | 6.15 (6.10, 6.19) | 6.04 (5.99, 6.08) | 6.01 (5.97, 6.06) | 5.89 (5.85, 5.93) | 5.76 (5.73, 5.80) | 5.59 (5.56, 5.63) | −1.83 (−2.36, −1.30) |
| Hemorrhagic stroke | 3.66 (3.63, 3.70) | 3.55 (3.52, 3.58) | 3.46 (3.42, 3.49) | 3.29 (3.26, 3.32) | 3.15 (3.12, 3.18) | 2.98 (2.96, 3.01) | −4.10 (−4.86, −3.35) |
| Ischemic stroke | 1.46 (1.43, 1.48) | 1.51 (1.49, 1.53) | 1.52 (1.50, 1.54) | 1.48 (1.46, 1.50) | 1.45 (1.43, 1.47) | 1.43 (1.41, 1.45) | −0.72 (−2.17, 0.73) |
| Unspecific stroke | 0.23 (0.22, 0.24) | 0.21 (0.20, 0.22) | 0.19 (0.19, 0.20) | 0.19 (0.18, 0.19) | 0.17 (0.16, 0.18) | 0.17 (0.16, 0.17) | −6.13 (−8.41, −3.85) |
| Sequelae of stroke | 0.52 (0.50, 0.53) | 0.53 (0.51, 0.54) | 0.62 (0.61, 0.64) | 0.74 (0.73, 0.76) | 0.83 (0.82, 0.85) | 0.87 (0.85, 0.88) | 11.70 (8.47, 14.93) |
| Hypertensive encephalopathy | 0.25 (0.24, 0.26) | 0.22 (0.22, 0.23) | 0.22 (0.21, 0.22) | 0.20 (0.19, 0.21) | 0.16 (0.15, 0.17) | 0.15 (0.14, 0.15) | −10.30 (−14.13, −6.47) |
| Other cerebrovascular disease | 0.15 (0.14, 0.15) | 0.13 (0.12, 0.13) | 0.11 (0.11, 0.12) | 0.10 (0.09, 0.10) | 0.11 (0.10, 0.11) | 0.10 (0.10, 0.11) | −7.50 (−13.27, −1.73) |
| Other CVD | 0.24 (0.23, 0.25) | 0.23 (0.22, 0.24) | 0.21 (0.20, 0.21) | 0.20 (0.20, 0.21) | 0.19 (0.18, 0.20) | 0.20 (0.19, 0.21) | −4.38 (−7.19, −1.57) |
| Females | |||||||
| Total CVD | 6.44 (6.40, 6.49) | 6.14 (6.09, 6.18) | 5.93 (5.89, 5.98) | 5.75 (5.71, 5.79) | 5.58 (5.54, 5.62) | 5.31 (5.27, 5.35) | −3.66 (−4.10, −3.23) |
| Heart disease | 2.97 (2.94, 3.01) | 2.84 (2.81, 2.87) | 2.74 (2.71, 2.77) | 2.68 (2.65,2.71) | 2.64 (2.61, 2.66) | 2.52 (2.50, 2.55) | −3.04 (−3.71, −2.37) |
| Ischemic heart disease | 2.41 (2.38, 2.44) | 2.33 (2.30, 2.36) | 2.28 (2.25, 2.31) | 2.27 (2.25, 2.30) | 2.26 (2.23, 2.28) | 2.16 (2.14, 2.19) | −1.84 (−2.67, −1.00) |
| Hypertensive heart disease | 0.34 (0.33, 0.36) | 0.28 (0.27, 0.29) | 0.25 (0.24, 0.25) | 0.22 (0.21, 0.23) | 0.20 (0.20, 0.21) | 0.19 (0.18, 0.20) | −11.56 (−14.51, −8.61) |
| Rheumatic heart disease | 0.17 (0.17, 0.18) | 0.17 (0.17, 0.18) | 0.16 (0.15, 0.17) | 0.14 (0.13, 0.14) | 0.13 (0.12, 0.13) | 0.12 (0.11, 0.13) | −7.66 (−10.12, −5.19) |
| Other heart disease | 0.06 (0.06, 0.07) | 0.07 (0.06, 0.07) | 0.06 (0.06, 0.07) | 0.06 (0.06, 0.06) | 0.06 (0.05, 0.06) | 0.06 (0.05, 0.06) | −1.32 (−5.62, 2.97) |
| Cerebrovascular disease | 3.44 (3.41, 3.48) | 3.27 (3.23, 3.30) | 3.17 (3.14, 3.21) | 3.05 (3.02, 3.08) | 2.93 (2.90, 2.96) | 2.77 (2.74, 2.80) | −4.15 (−4.62, −3.67) |
| Hemorrhagic stroke | 2.01 (1.98, 2.03) | 1.91 (1.89, 1.94) | 1.83 (1.80, 1.85) | 1.72 (1.69, 1.74) | 1.62 (1.60, 1.65) | 1.49 (1.47, 1.51) | −5.87 (−6.76, −4.97) |
| Ischemic stroke | 0.82 (0.80, 0.84) | 0.80 (0.78, 0.82) | 0.79 (0.77, 0.80) | 0.74 (0.73, 0.76) | 0.71 (0.70, 0.73) | 0.70 (0.68, 0.71) | −3.47 (−4.47, −2.47) |
| Unspecific stroke | 0.13 (0.12, 0.14) | 0.11 (0.11, 0.12) | 0.10 (0.09, 0.10) | 0.09 (0.09, 0.10) | 0.08 (0.08, 0.09) | 0.08 (0.07, 0.08) | −9.97 (−13.03, −6.91) |
| Sequelae of stroke | 0.29 (0.28, 0.30) | 0.29 (0.28, 0.30) | 0.32 (0.31, 0.33) | 0.38 (0.37, 0.39) | 0.40 (0.39, 0.41) | 0.41 (0.40, 0.42) | 8.19 (4.96, 11.43) |
| Hypertensive encephalopathy | 0.15 (0.14, 0.16) | 0.11 (0.11, 0.12) | 0.11 (0.10, 0.12) | 0.10 (0.10, 0.11) | 0.08 (0.08, 0.09) | 0.07 (0.07, 0.07) | −13.89 (−18.80, −8.98) |
| Other cerebrovascular disease | 0.08 (0.08, 0.09) | 0.07 (0.06, 0.07) | 0.06 (0.06, 0.07) | 0.05 (0.05, 0.06) | 0.06 (0.05, 0.06) | 0.05 (0.05, 0.06) | −8.56 (−15.51, −1.60) |
| Other CVD | 0.14 (0.13, 0.15) | 0.13 (0.13, 0.14) | 0.12 (0.11, 0.12) | 0.10 (0.10, 0.11) | 0.10 (0.10, 0.11) | 0.10 (0.09, 0.10) | −7.58 (−11.38, −3.77) |
APC: Annual percentage change; CI: Confidence interval; CVD: Cardiovascular disease.
Males showed consistent higher risks of premature mortality [95%CI] from CVDs (11.31% [11.25%, 11.37%] in 2013 to 10.77% [10.72%, 10.82%] in 2018) compared with females (6.44% [6.40%, 6.49%] in 2013 to 5.31% [5.27%, 5.35%] in 2018) during the observation period. Although there was a decline in premature mortality from most CVD subtypes in both sexes, the extent of decrease varied (APC: −0.98% [95% CI: −1.10%, −0.85%]) in men and −3.66% [−4.10%, −3.23%] in women, P < 0.001). Notably, we observed steady reductions in probability of premature deaths due to IS and IHD among women, whereas for men, the probability remained unchanged for IS (APC: −0.72% [95% CI: −2.17%, 0.73%]) and even increased for IHD (APC:1.02% [95% CI: 0.74%, 1.31%]).
Decomposition of LE by age and CVD causes
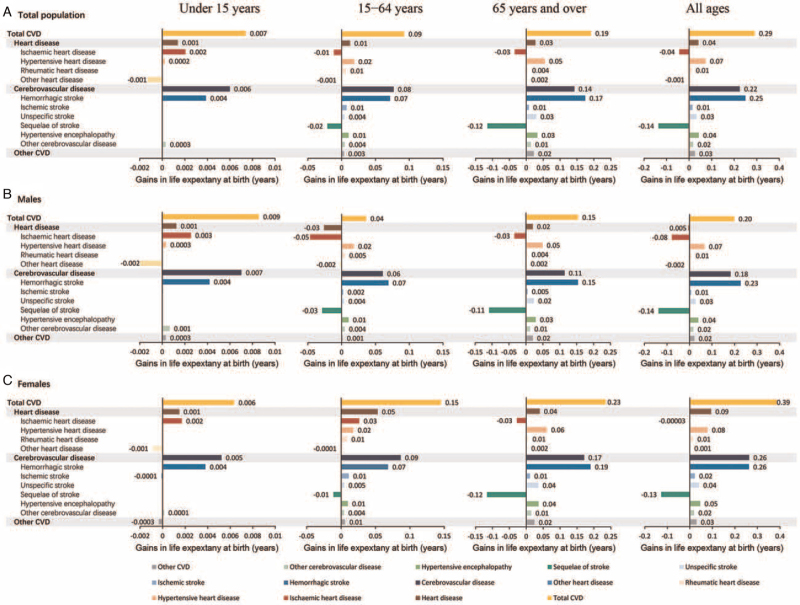
LE at birth in China increased from 75.66 (75.56, 75.77) years in 2013 to 77.04 (76.96, 77.12) years in 2018, of which 25.08% were attributed to youths under 15 years, 32.60% to working-age adults, and 42.32% to the elderly. Generally, a remarkable reduction in CVD mortality accounted for 0.29 years (21.15%) increase in longevity in the overall Chinese population, which is predominantly attributable to declines in cerebrovascular diseases (0.22 years, 16.32%). In the third level of cause hierarchy, approximately 18.14%, 5.34%, and 3.11% of the gains in LE during 2013 to 2018 came from reductions in mortality from HS, HHD, and hypertensive encephalopathy, respectively, which accounted for most of the contributions from CVDs. Contrastingly, the contribution of IS was quite limited (0.01 years, 1.08%), and the relative impact of IHD (−0.04 years, −3.16%) and stroke sequelae (−0.14 years, −9.90%) was even found to be negative during 2013 to 2018 [Supplementary Table 6; Table 3]. Similar patterns were observed across age structures, whereas the contribution of CVDs to longevity improvements increased remarkably with age. For the population aged < 15 years, only 2.14% (0.007 years) of gains in LE were achieved by a reduction in CVD mortality, whereas it accounted for 20.60% (0.09 years) in the working-age and 32.83% (0.19 years) in the elderly population [Supplementary Table 7; Figure 2].
Table 3.
Age-and cause-specific contributions to life expectancy at birth in overall and sex-specific Chinese population, 2013 to 2018.
| Contributions to gains in life expectancy at births from 2013 to 2018, years (%) | |||
| Parameters | Overall population | Males | Females |
| Total | 1.38 | 1.30 | 1.43 |
| By age groups | |||
| Under 15 years | 0.35 (25.08) | 0.38 (29.30) | 0.30 (21.18) |
| 15–64 years | 0.45 (32.60) | 0.48 (36.99) | 0.39 (27.27) |
| 65 years and over | 0.58 (42.32) | 0.44 (33.71) | 0.74 (51.54) |
| By causes | |||
| Total CVD | 0.29 (21.15) | 0.20 (15.27) | 0.39 (27.01) |
| Heart disease | 0.04 (2.95) | −0.005 (−0.37) | 0.09 (6.58) |
| Ischemic heart disease | −0.04 (−3.16) | −0.08 (−6.01) | 0 (−0.002) |
| Hypertensive heart disease | 0.07 (5.34) | 0.07 (5.15) | 0.08 (5.49) |
| Rheumatic heart disease | 0.01 (0.79) | 0.01 (0.65) | 0.01 (0.98) |
| Other heart disease | −0.001 (−0.06) | −0.002 (−0.19) | 0.001 (0.06) |
| Cerebrovascular disease | 0.22 (16.32) | 0.18 (13.97) | 0.26 (18.37) |
| Hemorrhagic stroke | 0.25 (18.14) | 0.23 (17.44) | 0.26 (18.32) |
| Ischemic stroke | 0.01 (1.08) | 0.01 (0.55) | 0.02 (1.54) |
| Unspecific stroke | 0.03 (2.44) | 0.03 (2.09) | 0.04 (2.80) |
| Sequelae of stroke | −0.14 (−9.90) | −0.14 (−10.59) | −0.13 (−8.89) |
| Hypertensive encephalopathy | 0.04 (3.11) | 0.04 (2.98) | 0.05 (3.20) |
| Other cerebrovascular disease | 0.02 (1.33) | 0.02 (1.33) | 0.02 (1.32) |
| Other CVD | 0.03 (1.88) | 0.02 (1.66) | 0.03 (2.06) |
CVD: Cardiovascular disease.
Figure 2.
Age- and cause-specific contributions to life expectancy at births in (A) overall and (B,C) sex-specific Chinese population, 2013 to 2018. CVD: Cardiovascular disease.
Heterogeneous age- and cause-specific contribution patterns were observed between sexes. On average, women in China (from 78.69 [95%CI: 78.58, 78.79] years in 2013 to 80.12 [95%CI: 80.03, 80.20] years in 2018) were expected to live >5 years longer compared to men (from 72.99 [95%CI: 72.90, 73.11] years in 2013 to 74.29 [95%CI: 74.21, 74.39] years in 2018), and this disparity has persisted with a greater increase of LE in female individuals. In terms of cause-specific decomposition, 27.01% (0.39 years) of gains in LE was attributed to declines in CVD mortality in females, nearly double the corresponding contribution in males (0.20 years, 15.27%). This difference was even more pronounced within the working-age population. Decreased CVD mortality in females of that age has made obvious contributions to LE improvements (0.15 years, 37.22%), much larger than their male counterparts (0.04 years, 7.51%).
Discussion
In this paper, we provided up-to-date evidence on the temporal trend in CVD mortality and its corresponding impact on LE increase in China, with particular attention paid to variations across age, sex, and CVD subtypes. Between 2013 and 2018, significant declines were observed for both the age-standardized mortality rates and probability of premature deaths due to CVDs, which accounted for 21.25% of the total LE gains in China. In general, the relative contribution of CVDs to longevity improvement significantly increased with age, and it was relatively lower for males than females due to slower decreases in CVD mortality. Remarkable declines in HS accounted for the greatest improvements in CVD mortality, along with reductions in most CVD subtypes. By contrast, the decrease in IS mortality and its contribution to longevity improvement was quite limited, and an upward trend in mortality of IHD and stroke sequelae were observed, which stunted the increase in LE over the study period.
Substantial reduction of 22.3% in the age-standardized mortality rate of HS, consistent with the recent Global Burden of Disease (GBD) study and the 2017 nationwide retrospective survey in China,[8,25] accounted for a major decline in CVD mortality over the observation period. This improvement could be attributed to both progress in the control of risk factors and advances in health care coverage and medical technology. For instance, benefiting from the implementation of several nationwide projects, including the community-based standardized blood pressure management programs, the awareness and control rates of hypertension improved greatly over the last decade in China.[26] Moreover, stroke screening and the intervention of high-risk population programs and nationwide stroke center network set up by the government have provided strong support for early diagnosis and timely treatment, thus greatly reducing case fatality.[27] The age-standardized mortality rate of RHDs continued its steady downward trend through the past decades, which to some extent reflected the improvement in life quality, accessibility of appropriate care, and consistent supply of quality-assured antibiotics in China.
By contrast, there was no such significant decline in the age-standardized mortality rates of IS and IHD. Reasons for this less optimistic situation of atherosclerotic CVD in China were manifold, of which lifestyle transformation and the consequent increased metabolic risk factors might be the two key drivers.[28] During the past decade, the average intake of whole grain and fresh vegetables continuously decreased in China, whereas the consumption of animal-based food and oil grew tremendously. Prevalence of hypercholesteremia and diabetes also elevated rapidly, accompanied by low awareness, treatment, and control rates, as well as declined physical activity levels and increased rates of obesity.[29–31] In addition to the inadequate control of risk factors for atherosclerosis, a high proportion of out-of-hospital IHD deaths due to delay of seeking medical treatment and inadequate pre-hospital care remained an issue of concern in China, which also hindered the reduction in IHD mortality to a certain degree.[32,33]
Consistent with previous provincial findings, we observed a notable increase in mortality rates from stroke sequelae, which indicated an insufficient rehabilitation service in China.[34] The importance of early rehabilitation has still not been commonly understood by the general Chinese population. Only 38.9% of stroke patients and their family members were reported to realize the necessity of rehabilitation after suffering a stroke.[35] On the other hand, although the Chinese government has launched a three-stage rehabilitation network for stroke patients and gradually established stroke units nationwide since the early 2000s, a stereoscopic rehabilitation system, including hospitals, communities, and nursing services, is not yet well established.[36] It has been reported that about 30% to 60% of stroke patients had no access to rehabilitation in hospitals and that only 20% of patients received rehabilitation after hospital discharge.[27] More qualified post-stroke rehabilitation institutions and well-trained rehabilitation therapists are urgently needed in China, as well as better public health education for the general population.
Furthermore, we noticed a sex difference in the declining rate of CVD burden, which was most pronounced among the working-age population. Despite the similar percentage reduction among the young and the elderly, CVD mortality rates in females aged 15 to 64 years decreased perceptibly by 17.57% over the study period, compared to a 3.12% reduction observed in their male contemporaries. The probability of premature CVD deaths declined by 3.66%/year among females, >3.5 times the rate of decline of males, which indicates a higher unmet need for males to achieve the target proposed by The Healthy China 2030 Initiative. This slower improvement in the CVD health of working-age males was consistent with findings from previous studies conducted in China[4,8,37,38] and world-wide,[39] largely driven by unhealthy lifestyles and subsequent metabolic disorders. In China, larger proportions of males indulge in cigarette smoking and harmful use of alcohol in comparison with females; the prevalence of hypertension as well as diabetes is also higher among males, and the gap is likely to expand further.[40–42] Besides, longer working hours and increasing work stress accompanied by rapid social and economic develop-ment,[43] which seems to be more harmful to CVD health in men, has also partly contributed to the disparity in CVD mortality between sexes among the young and middle-aged population.[44,45]
Nationwide studies on age- and cause-specific contributions to LE are quite limited in China. The most recent study based on the data from GBD 2016 reported that people aged ≥65 years contributed 37.4% to the increased LE during 2007 to 2016 in China, and the most prominent driving force was reductions in mortality from CVD (24.1%).[2] Consistently, our findings reflected the accelerated demographic and epidemiological transition taking place in China and unprecedentedly illustrated the heterogeneity across CVD subtypes in relative contributions to longer lives. During 2013 to 2018, remarkable declines in mortality from HS played an important role in improvements of LE for both sexes, while the persistently high mortality rates from IHD stunted improvements in longevity, especially for males. It can be simply estimated that if the probability of premature CVD deaths maintains the current decline rather than remaining unchanged, an extra gain in LE of 0.27 years for males and 0.50 years for females would be achieved by 2030, mostly attributable to declines in HS mortality. Moreover, if the probability of premature CVD deaths could further decrease by 30% in 2030 in comparison with 2015 levels, males would obtain an additional gain of 0.31 years over maintaining the current APC, largely driven by more remarkable improvements in IHD and stroke sequelae [Supplementary Table 8].[46]
To the best of our knowledge, this study provided the most recent and detailed estimates of burdens of CVD mortality and their impacts on longevity in China. Based on the integrated mortality database verified through multiple sources of administrative records, we have made every effort to avoid potential bias due to missing or delayed death reports and estimated the rates of mortality with higher accuracy. Furthermore, the consecutive and detailed cause-specific mortality data derived from the DSP system made it possible for us to depict a nationwide picture representing the burden of total CVD and its subtypes, providing more specific information on resource allocation and priority setting in the healthcare system. Additionally, previous studies have used cause-eliminated life tables to evaluate the life-shortening effect of CVDs under the assumption that all CVD deaths were avoided.[14] This method, however, does not actually reflect the potential influence of contemporary changes in mortality from other causes. Instead, we adopted a more comparative decomposition method, which quantified the relative contributions of CVDs to LE improvements in the real situation where changes in mortality from other causes were also taken into consideration.[47]
This study also has some limitations. To date, the Chinese government has yet to establish a complete vital registration system for its entire population. Although we adopted the most comprehensive available data, the CVD specific mortality rates reported in our study were still approximately estimated using the death distribution method, consistent with previous publications.[20,48] The exclusion of 10 out of 605 DSP sites with incomplete data could also result in a biased estimation. Further, death certificate data were subject to miscoding and misclassification, and thus the temporal trends might be affected by improvement in quality of registry on mortality causes. However, no significant changes were observed in the sensitivity analyses conducted for all 605 sites. Moreover, each certification was checked by both qualified health workers and the automatic online coding system, and the garbage codes were redistributed before analyses; hence, it is unlikely to substantially alter the general CVD mortality trends over the observation period. Besides, the absence of valid historical data limited our ability to further explore longer temporal patterns of CVD mortality. Studies based on more recent evidence are also needed to evaluate the influence of the latest measurements on CVD prevention and control, including the establishment of a pre-hospital medical emergency network and the continuous improvement of stroke and chest pain centers.[49]
In conclusion, we observed a stable decline in the burden of overall CVD mortality during 2013 to 2018 in China, catalyzed by a remarkable reduction in HS, a decreased predominance of HS over IS, an unimproved trend for IHD, and a rapid increase in stroke sequelae. Although the general CVD mortality reduction has led to more than one-fifth of the total increase in LE over the study period, the annual rates of decline are still inadequate to meet the targets for CVD mortality reduction, which indicates a pressing need to improve CVD health of the Chinese population, especially for working-age males. Given the rapid process of population ageing, special concerns should also be given to health maintenance for the elderly to ensure a sustainable increase in LE. Controlling modifiable lifestyle and metabolic risk factors of CVDs, improving pre-hospital emergency care for IHD, and strengthening rehabilitation therapy for stroke survivors are critical interventions in addressing the worrisome CVD burdens in China.
Funding
This study was supported by grants from the Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (No. 2021-I2M-1-010, No. 2017-I2M-1-004), the the National Natural Science Foundation of China (No. 12126602, No. 82030102) and the National Key R&D Program of China (No. 2017YFC0211700).
Conflicts of interest
None.
Supplementary Material
Footnotes
How to cite this article: Xia X, Cai Y, Cui X, Wu R, Liu F, Huang K, Yang X, Lu X, Wu S, Gu D. Temporal trend in mortality of cardiovascular diseases and its contribution to life expectancy increase in China, 2013 to 2018. Chin Med J 2022;135:2066–2075. doi: 10.1097/CM9.0000000000002082
Xue Xia and Yue Cai contributed equally to this work.
Supplemental digital content is available for this article.
References
- 1.National Health Commission. Yearbook of Health Statistics of China (in Chinese). Beijing, China: Peking Union Medical College Press; 2020. [Google Scholar]
- 2.Chen H, Qian Y, Dong Y, Yang Z, Guo L, Liu J, et al. Patterns and changes in life expectancy in China, 1990–2016. PLoS One 2020; 15:e0231007.doi: 10.1371/journal.pone.0231007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME); 2020. Available at: http://ghdx.healthdata.org/gbd-results-tool. Accessed July 17, 2021. [Google Scholar]
- 4.Liu J. New characteristics of cardiovascular disease epidemic trend in China (in Chinese). Chin J Cardiol 2015; 43:295–296. doi: 10.3760/cma.j.issn.0253-3758.2015.04.003. [Google Scholar]
- 5.Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol 2019; 16:203–212. doi: 10.1038/s41569-018-0119-4. [DOI] [PubMed] [Google Scholar]
- 6.Shah NS, Molsberry R, Rana JS, Sidney S, Capewell S, O’Flaherty M, et al. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999-2018: observational analysis of vital statistics. BMJ 2020; 370:m2688.doi: 10.1136/bmj.m2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Xinhua News Agency. Outline of healthy China 2030 Plan (in Chinese). 2016. Available at: http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm. Accessed December 6, 2020. [Google Scholar]
- 8.Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, et al. Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 Global Burden of Disease Study. JAMA Cardiol 2019; 4:342–352. doi: 10.1001/jamacardio.2019.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang X, Khan AA, Haq EU, Rahim A, Hu D, Attia J, et al. Increasing mortality from ischaemic heart disease in China from 2004 to 2010: disproportionate rise in rural areas and elderly subjects. 438 million person-years follow-up. Eur Heart J Qual Care Clin Outcomes 2017; 3:47–52. doi: 10.1093/ehjqcco/qcw041. [DOI] [PubMed] [Google Scholar]
- 10.Chen Z, Jiang B, Ru X, Sun H, Sun D, Liu X, et al. Mortality of stroke and its subtypes in China: results from a Nationwide Population-Based Survey. Neuroepidemiology 2017; 48:95–102. doi: 10.1159/000477494. [DOI] [PubMed] [Google Scholar]
- 11.Su JT, Gao YL, Wei ZH, Wang J. Decomposition of life expectancy among permanent residents of Beijing, 2000-2010 (in Chinese). Chin J Epidemiol 2013; 34:250–253. doi: 10.3760/cma.j.issn.0254-6450.2013.03.011. [PubMed] [Google Scholar]
- 12.Zheng Y, Chang Q, Yip PSF. Understanding the increase in life expectancy in Hong Kong: contributions of changes in age- and cause-specific mortality. Int J Environ Res Public Health 2019; 16:1959.doi: 10.3390/ijerph16111959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang YH, Li LM. Evaluation of impact of major causes of death on life expectancy changes in China, 1990-2005. Biomed Environ Sci 2010; 22:430–441. doi: 10.1016/s0895-3988 (10)60022-0. [DOI] [PubMed] [Google Scholar]
- 14.Fan J, Li GQ, Liu J, Wang W, Wang M, Qi Y, et al. Impact of cardiovascular disease deaths on life expectancy in Chinese population. Biomed Environ Sci 2014; 27:162–168. doi: 10.3967/bes2014.037. [DOI] [PubMed] [Google Scholar]
- 15.Liu S, Wu X, Lopez AD, Wang L, Cai Y, Page A, et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ 2016; 94:46–57. doi: 10.2471/BLT.15.153148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang R, Xue M, Lin Q, Zhou X, Cai Y. The methodology study of realizing the full coverage of vital registration in China through multisource data comparison (in Chinese). Chin J Health Inform Manage 2019; 16:192–197. doi: 10.3969/j.issn.1672-5166.2019.01.16. [Google Scholar]
- 17.Zeng Y, Vaupel JW. Chinese oldest old mortality and its comparison with Sweden and Japan (in Chinese). Popul Econ 2004. 8–16. https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD2004&filename=RKJJ200403001&uniplatform=NZKPT&v=cePJurkR1irsGCJd-kbAWFrdieFm33rEoUaba5_0bjrf6ePeGe6zeVkd1K9NFCH2 [Google Scholar]
- 18.World Health Organization. WHO methods and data sources for country-level causes of death 2000-2019. 2020. [Google Scholar]
- 19.Wan X, Yang GH. Is the mortality trend of ischemic heart disease by the GBD2013 study in China real? Biomed Environ Sci 2017; 30:204–209. doi: 10.3967/bes2017.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wan X, Ren H, Ma E, Yang G. Mortality trends for ischemic heart disease in China: an analysis of 102 continuous disease surveillance points from 1991 to 2009. BMC Public Health 2017; 18:52.doi:10.1186/s12889-017-4558-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aragon TJ. epitools: Epidemiology tools. R package version 0.5-10. 2017. Available at: https://CRAN.R-project.org/package=epitools. Accessed November 20, 2020. [Google Scholar]
- 22.World Health Organization. Global status report on noncommunicable diseases 2014. 2016. Available at: http://www.who.int/nmh/publications/ncd-status-report-2014/en/. Accessed November 20, 2020. [Google Scholar]
- 23.Chiang CL. The Life Table and its Applications. Malabar, FL: Robert E Krieger Publ Co; 1984. [Google Scholar]
- 24.Arriaga EE. Measuring and explaining the change in life expectancies. Demography 1984; 21:83–96. https://pubmed.ncbi.nlm.nih.gov/6714492/ [PubMed] [Google Scholar]
- 25.Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a Nationwide Population-Based Survey of 480 687 adults. Circulation 2017; 135:759–771. doi: 10.1161/CIRCULATIONAHA.116.025250. [DOI] [PubMed] [Google Scholar]
- 26.Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012-2015. Circulation 2018; 137:2344–2356. doi: 10.1161/CIR-CULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 27.Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol 2019; 18:394–405. doi: 10.1016/s1474-4422(18)30500-3. [DOI] [PubMed] [Google Scholar]
- 28.Liu F, Li J, Chen J, Hu D, Li Y, Huang J, et al. Predicting lifetime risk for developing atherosclerotic cardiovascular disease in Chinese population: the China-PAR project. Sci Bull 2018; 63:779–787. doi:10.1016/j.scib.2018.05.020. [DOI] [PubMed] [Google Scholar]
- 29.Jile C, Yu W. A Comprehensive Report on the Nutrition and Health Status of Chinese Residents, 2010–2013. Beijing: Peking University Medical Press; 2016. [Google Scholar]
- 30.Liu M, Liu SW, Wang LJ, Bai YM, Zeng XY, Guo HB, et al. Burden of diabetes, hyperglycaemia in China from to 2016: findings from the 1990 to 2016, global burden of disease study. Diabetes Metab 2018; 45:286–293. doi: 10.1016/j.diabet.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 31.Pan L, Yang Z, Wu Y, Yin RX, Liao Y, Wang J, et al. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis 2016; 248:2–9. doi: 10.1016/j.atherosclero-sis.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 32.Guan W, Venkatesh AK, Bai X, Xuan S, Li J, Li X, et al. Time to hospital arrival among patients with acute myocardial infarction in China: a report from China PEACE prospective study. Eur Heart J Qual Care Clin Outcomes 2019; 5:63–71. doi: 10.1093/ehjqcco/qcy022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou T, Li X, Lu Y, Murugiah K, Bai X, Hu S, et al. Changes in ST segment elevation myocardial infarction hospitalisations in China from 2011 to 2015. Open Heart 2021; 8:e001666.doi: 10.1136/openhrt-2021-001666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yihe H, Yan L, Linchi W, Chunyan H, Yujie H. Strategies analysis on prevention and control of cerebrovascular diseases based on the data of 10-year mortality and 8-year morbidity in Suzhou (in Chinese). Chin J Cerebrovasc Dis 2020; 17:446–454. doi: CNKI:SUN:NXGB.0.2020-08-005. [Google Scholar]
- 35.Zhang X, Chen Y, Liu Y, Gu W, Wang C, Bi Z. Survey of the cognition and requirements of the community stroke rehabilitation (in Chinese). Shanghai Med Pharm J 2015; 36:58–60. doi: CNKI:SUN:SYIY.0.2015-18-024. [Google Scholar]
- 36.Asakawa T, Zong L, Wang L, Xia Y, Namba H. Unmet challenges for rehabilitation after stroke in China. Lancet 2017; 390:121–122. doi:10.1016/s0140-6736(17)31584-2. [DOI] [PubMed] [Google Scholar]
- 37.Zeng XY, Li YC, Liu SW, Wang LJ, Liu YN, Liu JM, et al. Subnational analysis of probability of premature mortality caused by four main non-communicable diseases in China during 1990-2015 and “Health China 2030” reduction target (in Chinese). Chin J Prev Med 2017; 51:209–214. doi: 10.3760/cma.j.issn.0253-9624.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 38.Lv J, Ni L, Liu K, Gao X, Yang J, Zhang X, et al. Clinical characteristics, prognosis, and gender disparities in young patients with acute myocardial infarction. Front Cardiovasc Med 2021; 8:720378.doi: 10.3389/fcvm.2021.720378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang W, Hu M, Liu H, Zhang X, Li H, Zhou F, et al. Global Burden of Disease Study 2019 suggests that metabolic risk factors are the leading drivers of the burden of ischemic heart disease. Cell Metab 2021; 33:1943–1956. doi: 10.1016/j.cmet.2021.08.005. [DOI] [PubMed] [Google Scholar]
- 40.The State Council Information Office. Report on Nutrition and Chronic Diseases in China (in Chinese). 2021. Available at: http://www.gov.cn/xinwen/2020-12/24/content_5572983.htm. Accessed April 8, 2021. [Google Scholar]
- 41.Chinese Center for Disease Control and Prevention. China Chronic Disease and Risk Factor Surveillance 2013 (in Chinese). Beijing, China: Military Medical Science Press; 2016. [Google Scholar]
- 42.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021; 398:957–980. doi: 10.1016/s0140-6736(21)01330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pega F, Nafradi B, Momen NC, Ujita Y, Streicher KN, Pruss-Ustun AM, et al. Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000-2016: a systematic analysis from the WHO/ILO joint estimates of the work-related burden of disease and Injury. Environ Int 2021; 154:106595.doi: 10.1016/j.envint.2021.106595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Akizumi Tsutsumi KK, Kazuomi K, Shizukiyo I. Prospective study on occupational stress and risk of stroke. Arch Intern Med 2009; 169:56–61. doi: 10.1001/archinternmed.2008.503. [DOI] [PubMed] [Google Scholar]
- 45.Rosengren A, Hawken S, Ôunpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:953–962. doi: 10.1016/s0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 46.Cao B, Bray F, Ilbawi A, Soerjomataram I. Effect on longevity of one-third reduction in premature mortality from non-communicable diseases by 2030: a global analysis of the Sustainable Development Goal health target. Lancet Glob Health 2018; 6:e1288–e1296. doi:10.1016/s2214-109x(18)30411-x. [DOI] [PubMed] [Google Scholar]
- 47.Beltran-Sanchez H, Preston SH, Canudas-Romo V. An integrated approach to cause-of-death analysis: cause-deleted life tables and decompositions of life expectancy. Demogr Res 2008; 19:1323.doi:10.4054/DemRes.2008.19.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019; 394:1145–1158. doi: 10.1016/s0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Information Professional Committee of Chinese Hospital Association. Notice on the issuance of guidelines on further improving pre-hospital emergency medical services (in Chinese). 2021. Available at: https://www.chima.org.cn/Html/News/Articles/6111.html. Accessed July 11, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.