Abstract
Objective:
Determine crash risk in adults with a history of childhood ADHD and persistent ADHD symptoms.
Method:
Participants with (n = 441) and without (n = 239; local normative comparison group, LNCG) childhood ADHD from the Multimodal Treatment Study of ADHD (MTA) were included. Participants provided self-reports on the total number of motor vehicle crashes (MVCs) they had been involved in and the time of licensure. Driving experience was estimated as the number of months since licensure. Total number of MVCs by adulthood was regressed on baseline ADHD status adjusting for sex, age at follow-up, driving experience, baseline ODD/CD comorbidity, baseline household income level, adult ODD/CD symptoms, adolescent and adult substance use, and adult antisocial personality disorder symptoms. We repeated the analysis using adult ADHD status (persistent vs. desistant vs. LNCG) and symptom level as the predictor variable. Results are presented as Incidence Rate Ratios (IRR) and Confidence Intervals (CI).
Results:
Childhood ADHD was associated with a higher number of crashes (IRR = 1.45, CI = 1.15 to 1.82) and adult ADHD symptom persistence was associated with more crashes than desistence (IRR = 1.46, CI = 1.14 to 1.86). ADHD desistence was not associated with a significantly increased risk for crashes compared to the LNCG (IRR = 1.24, CI = 0.96 to 1.61). Concurrent symptoms of inattention and hyperactivity/impulsivity predicted MVC risk.
Conclusion:
Adult ADHD persistence is a stronger predictor of motor vehicle crash risk than childhood-limited ADHD.
Keywords: Attention-Deficit/Hyperactivity Disorder (ADHD), driving, motor vehicle crashes, ADHD persistence, comorbidity
LAY ABSTRACT
This study compares the risk of motor vehicle crashes in adult drivers with persistent Attention-Deficit/Hyperactivity Disorder (ADHD) symptoms versus adults with childhood-limited (desistent) ADHD. Our results show that adults with a childhood diagnosis of ADHD have a higher risk for car crashes than adult drivers without childhood ADHD (incidence rate ratio = 1.45). We also found that adults with persistent ADHD (incidence rate ratio = 1.81), but not desistant ADHD, had a high risk for car crashes compared to adults without any childhood ADHD.
INTRODUCTION
Attention Deficit/Hyperactivity Disorder (ADHD) is characterized by developmentally inappropriate levels of inattention and hyperactivity/impulsivity that significantly impair daily life functioning.1 Once considered a disorder exclusive to childhood, it has become increasingly clear that ADHD often persists into adulthood. Estimates of childhood cases persisting into adulthood vary significantly, ranging from 5-75% across studies.2 A meta-analysis reported that full persistence of childhood ADHD (i.e., meeting full diagnostic criteria for the disorder as an adult) occurs in about 15% of cases, but that as many 65% of individuals with childhood ADHD partially meet diagnostic criteria for ADHD in adulthood.3
Recently, data from the Multimodal Treatment Study of ADHD (MTA) was used to examine the functional impairment experienced by individuals with persistent ADHD in comparison to individuals whose symptoms remit or “desist” in adulthood as well as a community control group, consisting of individuals who did not meet criteria for ADHD as children.4 The groups exhibited a pattern in which the community control group was the least impaired, while the persisters were the most impaired across several areas of functioning assessed (educational, occupational, emotional, substance use, legal problems and sexual behavior). Desisters’ functioning fell in-between the two groups with their impairment being significantly less than that of their peers whose ADHD persisted. Although, driving was not examined as an area of impairment in this MTA follow-up study,4 the consequences of being involved in motor vehicle crashes (MVC) can be potentially life-threatening.
MVCs are a leading cause of death among individuals ages 18-25, the age range of the MTA follow-up sample, and accounted for nearly half of all unintentional injury-related deaths in this age range in 2017.5 What is of concern is that prior studies consistently show a risk for MVCs in individuals with ADHD that is approximately 30% higher than in those without ADHD.6 Individuals with ADHD often report greater numbers of traffic violations, speeding violations, and license suspensions, 6 and also report engaging in significantly greater levels of risky driving on psychometrically valid measures of risky driving (e.g., Driving Behavior Questionnaire7) than do individuals without ADHD.8 Impairments in driving also extend to problems with basic driving abilities. For example, simulated driving studies suggest that individuals with ADHD exhibit problems with maintaining control of their cars as indicated by greater variability in steering and lane position of the car in comparison to individuals without ADHD.9–11
The distinction between childhood ADHD and persistent/desistent adult ADHD has not been made when examining ADHD-MVC risk, but there is reason to believe that this distinction is important. Concurrent symptom levels are a strong predictor of risky driving in ADHD.12–13 Studies involving individuals who met diagnostic criteria for ADHD symptoms at the time of assessment find impairments in outcomes (e.g., repeated MVCs and moving violations)12 and driving abilities (e.g., problems with maintaining lane position)13–14 in comparison to controls. Conversely, studies that did not assess concurrent symptom levels, and instead examined the effect of childhood ADHD on adult MVC risk, failed to find some differences in driving in individuals with childhood ADHD in comparison to controls (e.g., Molina et al.15). Differences in study findings suggest that it is important to consider childhood ADHD versus ADHD persistence when examining the ADHD-MVC risk association. Longitudinal studies, such as the MTA, offer the opportunity to examine the impact of both childhood ADHD and ADHD persistence and desistence on MVC risk.
The literature examining the ADHD-MVC association contains several limitations calling into question the extent to which ADHD increases MVC risk. Several early studies contained small sample sizes consisting of convenience samples drawn from ADHD specialty assessment clinics. These study findings may have limited generalizability since the samples might have represented cases of ADHD that are more severe than would be found in community-based samples and therefore could result in overestimates of this risk. Recently, population-based studies have addressed these limitations and suggest that ADHD is associated with increased MVC risk. For example, the association between ADHD diagnosis and MVC risk was assessed in one study by linking medical records from primary care clinics, not ADHD specialty clinics, to state driving records in a sample of adolescents and young adults.16 Study findings indicated that ADHD increased risk of crash significantly for both males and females (Hazard Ratio = 1.42 and 1.25 for males and females, respectively). This study was particularly strong as it did not rely on self-report of MVC involvement, which can be biased due to problems with recall and social desirability. A study using a Swedish longitudinal population-based registry reported a similar ADHD hazards ratio of 1.47 for MVCs involving emergency hospital visits or death (based on administrative records) after adjusting for covariates.17 Finally, a longitudinal prospective study of over 3,000 drivers examined the relationship between ADHD status at the beginning of the study and self-reported MVC involvement 3 years later, reporting a significant odds ratio of 2.21 after accounting for demographic variables for individuals meeting diagnostic criteria for ADHD.12 Using the same sample as Aduen et al.,15 similar results were reported when analyses were run using recordings of naturalistic driving to measure MVC involvement.18 While these studies offer stronger evidence for the ADHD-MVC risk, their study designs did not allow for an analysis of the ADHD persister and desister distinction.
Obtaining a valid epidemiologic measure of the true ADHD-MVC risk also requires accounting for appropriate confounding variables in analytical models. A meta-analysis of 16 studies examining differences in MVC involvement across samples of individuals with and without ADHD identified two variables that attenuate, but do not eliminate, the ADHD-MVC association when accounted for in analyses. First, individuals with ADHD consistently reported driving more miles than their non-ADHD counterparts across studies, which Vaa6 conceptualized as differences in “exposure” to driving. Accounting for this effect reduced the relative risk estimate from 1.36 to 1.23. While self-report of miles driven is one method of assessing exposure, there may be problems with this approach given that individuals with ADHD exhibit difficulties with estimation.19 Using months since licensure as an indicator of exposure might be less subject to problems with estimation. The second confounding variable identified in the meta-analysis was ODD/CD comorbidity and removing the effect of ODD/CD reduced the relative risk estimate for the ADHD effect from 1.86 to 1.31 (Vaa6). Since research supports a theoretical model in which individuals with comorbid childhood ADHD/ODD exhibit a developmental pathway to antisocial behavior in adulthood,20 we argue that current symptoms of antisocial personality disorder (ASPD) are another important confounding variable to account for when examining the ADHD-MVC association. In fact, driving research has linked ASPD symptoms to important driving related behaviors and outcomes including road rage and MVC-related deaths. Socioeconomic status, which predisposes to a high risk for negative outcomes in ADHD, also increases risk for MVCs and can affect access to driving and likelihood of licensure.21–24 Thus, socioeconomic status may too confound the ADHD-MVC association. Finally, substance use is another potentially important confounding variable to account for in analyses given that adults with ADHD engage in higher frequency substance use in comparison to adults without ADHD and that alcohol use increases MVC risk in adults with ADHD.25
The present study uses the MTA sample to examine the risk of MVCs involving drivers diagnosed with ADHD in childhood. Here we assess the risk of MVC involvement, accounting for variables that may confound the true risk of ADHD status on crash involvement, including months driving experience, childhood and adult ODD/CD comorbidity, socioeconomic status, adult ASPD symptoms, and substance use. We also assess the effects of adult ADHD persistence versus desistence on MVC.
METHODS
Sample
This study uses data from the National Institute of Mental Health (NIMH) Multimodal Treatment Study of Children with ADHD (MTA). The MTA was a 14-month randomized clinical trial of 579 children with ADHD, aged 7-10 years, with a 10 month follow-up at 24 months after baseline. The MTA then continued as an observational study with assessments in childhood (3 years after baseline), adolescence (6, 8 and 10 years after baseline), and adulthood (12, 14 and 16 years after baseline). An age- and sex-matched comparison group of 272 children (LNCG, Local Normative Comparison Group) was recruited 2 years after baseline and followed at the same intervals as the original MTA group. Further details on the MTA cohort and LNCG are available in previous publications.15,26–29
The current study is based on participants who were assessed at least once in adulthood (either the 12, 14, or 16 year follow-up). This included 453 participants with ADHD (ADHD group) and 241 without baseline ADHD (the LNCG).30 Of these 694 participants, 12 were driving without a license (n(ADHD) = 11, n(LNCG) = 1). Driving experience could not be calculated for these participants and they were excluded from further analyses. In addition, information on age at licensure was missing for two participants (n(ADHD) = 1, n(LNCG) = 1) who were also excluded from analyses. This led to a final sample size of 680 (n(ADHD) = 441, n(LNCG) = 239). Table 1 compares baseline characteristics of participants from the original MTA (n = 579) who were included in this study (n = 441) versus those not included (n = 138). We found no differences in baseline age, baseline ADHD symptom severity, and baseline ODD/CD status between participants included and those lost to follow-up. However, significant differences in baseline socioeconomic status were present between the two groups. Median household income at baseline in the current subsample ranged from $40,000 to $50,000 per annum, but ranged from $30,000 to $40,000 in those lost to follow-up. Parental educational attainment levels, maternal age, participants’ sex, and ethnicity also differed between the two groups.
Table 1.
Baseline Characteristics of Participants with Childhood ADHDa
| Participants with baseline ADHD included in this study (n = 441) |
Participants with baseline ADHD not included (n = 138) |
||
|---|---|---|---|
|
| |||
| Mean(SD) | Mean(SD) | p | |
| Age (in years) | 7.79 (0.83) | 7.73 (0.75) | .43 |
|
| |||
| ADHD symptom severity (Swanson, Nolan, and Pelham scale) | 1.99 (0.44) | 2.03 (0.42) | .26 |
|
| |||
| Mother’s age (in years) | 38.08 (7.19) | 35.88 (7.14) | .002 |
|
| |||
| Father’s age (in years) | 40.42 (7.25) | 38.79 (7.72) | .052 |
| n (%) | n (%) | p | |
|
| |||
| Sex | |||
| Female | 96 (21.8%) | 18 (13%) | .024 |
| Male | 345 (78.2%) | 120 (87%) | |
|
| |||
| Ethnicity | |||
| Caucasian | 285 (64.6%) | 67 (48.6%) | .006 |
| Black | 80 (18.1%) | 35 (25.4%) | |
| Non-black Hispanic | 29 (6.6%) | 11 (8%) | |
| Black Hispanic | 3 (0.7%) | 6 (4.3%) | |
| Asian | 4 (0.9%) | 2 (1.4%) | |
| Mixed | 37 (8.4%) | 16 (11.6%) | |
| Other | 3 (0.7%) | 1 (0.7%) | |
|
| |||
| Randomized treatment group assignment | |||
| Community Care | 106 (24%) | 40 (29%) | .18 |
| Combined treatment | 118 (26.8%) | 27 (19.6%) | |
| Medication only | 104 (23.6%) | 40 (29.6%) | |
| Psychosocial only | 113 (25.6%) | 31 (22.5%) | |
|
| |||
| Grade | |||
| 1st | 71 (16.1%)) | 18 (13%) | .76 |
| 2nd | 179 (40.6%) | 60 (43.5%) | |
| 3rd | 132 (29.9%) | 45 (32.6%) | |
| 4th | 58 (13.2%) | 15 (10.9%) | |
| 5th | 1 (0.2%) | 0 | |
|
| |||
| Mother’s educational level | |||
| Eighth grade or less | 3 (0.7%) | 1 (0.7%) | .003 |
| Some high school | 18 (4.1%) | 11 (8.1%) | |
| High school graduate | 85 (19.4%) | 35 (25.7%) | |
| Some college or post-high school | 152 (34.6%) | 59 (43.4%) | |
| College graduate | 105 (29.9%) | 19 (14.0%) | |
| Advanced graduate or professional degree | 76 (17.3%) | 11 (8.1%) | |
|
| |||
| Father’s educational level | |||
| Eighth grade or less | 5 (1.4%) | 5 (5%) | .001 |
| Some high school | 21 (6%) | 13 (12.9%) | |
| High school graduate | 80 (22.8%) | 33 (32.7%) | |
| Some college or post-high school | 105 (29.9%) | 28 (27.7%) | |
| College graduate | 68 (19.4%) | 12 (11.9%) | |
| Advanced graduate or professional degree | 72 (20.5%) | 10 (9.9%) | |
|
| |||
| Household income | |||
| < $10,000 | 36 (8.3%) | 15 (11.2%) | .036 |
| $10,000 to $20,000 | 48 (11.1%) | 20 (14.9%) | |
| $20,000 to $30,000 | 58 (13.4%) | 28 (20.9%) | |
| $30,000 to $40,000 | 59 (13.6%) | 24 (17.9%) | |
| $40,000 to $50,000 | 55 (12.7%) | 12 (9%) | |
| $50,000 to $60,000 | 48 (11.1%) | 12 (9%) | |
| $60,000 to $70,000 | 43 (9.9%) | 6 (4.5%) | |
| $70,000 to $75,000 | 22 (5.1%) | 2 (1.5%) | |
| ≥ $75,000 | 64 (14.8%) | 15 (11.2%) | |
|
| |||
| Receiving welfare/public assistance/social security income | .06 | ||
| Yes | 75 (17%) | 33 (24%) | |
| No | 366 (83%) | 104 (76%) | |
|
| |||
| Conduct /Oppositional Defiant Disorder diagnosis | |||
| Yes | 178 (42%) | 53 | .53 |
| No | 246 (58%) | 83 | |
Attention-Deficit/Hyperactivity Disorer
The MTA was approved by Institutional Review Boards and all procedures were carried out in accordance with the Declaration of Helsinki. Participants were informed of the study procedures and provided written consent/assent.
Outcome
Our driving outcome was number of MVCs. Information on MVCs was available via self-reports from the 6-year follow-up onwards. Participants reported ‘the total number of times they were the driver of a vehicle that was involved in an accident regardless of whether they were judged to be at fault or not’. We calculated the total number of (i.e., cumulative) crashes between licensure and the last available adult assessment time-point. That is, one crash outcome measure was available for each participant.
Adult ADHD
Adult ADHD persistence and desistence was defined as in Sibley et al.30 Briefly, we used the Conners’ Adult ADHD Rating Scale (CAARS), using both self and parent reports, to determine ADHD symptoms. Presence of an ADHD symptom was defined as an item score of 2 (“Pretty much, often”) or 3 (“Very much, very frequently”) on the 0-3 scale endorsed by either self or parent, with the requirement that both self and parent measures be available. Impairment was considered positive with a score of 3 or more on either self or parent ratings of the Impairment Rating Scale (IRS) summary item. We used DSM 5 symptom count (≥ 5 symptoms), age of onset (before 12 years of age), and impairment criteria to classify participants as diagnostic persisters or desisters. Participants meeting the DSM criteria at any adult follow-up were classified as persisters. With this algorithm, 220 participants from our study sample were classified as persisters and 221 as desisters.
Driving experience
Between adolescence and adulthood, participants reported on several driving behaviors including whether or not they possessed a driver’s license. Based on the first assessment point at which they reported having obtained a license (participant’s response was required on, first “I currently do not have a driver’s license (YES/NO)”, and second, if answered ‘YES’ to previous question, “I currently have a driver’s license for ‘n’ months out of the past two years”, with two years being the interval between two MTA assessments), we determined age at licensure. We approximated driving experience by subtracting age at licensure from age at the last available assessment in adulthood. Thus, our driving experience variable represents the total number of months between licensure and the adult assessments. Note, however, that our measure ‘driving experience’ does not estimate true experience, as frequency of driving may differ between participants.
Income levels
Baseline household income levels were assessed via parent-reports. We included household income as a proxy for socioeconomic status.
Oppositional defiant and conduct disorders
Comorbid oppositional defiant disorder (ODD) and conduct disorder (CD) were determined at baseline according to DSM-III-R criteria as assessed by the Diagnostic Interview Schedule for Children – Parent version or DISC-P.31 A baseline diagnosis of either ODD or CD was included as a covariate in our analyses.
ODD/CD in adulthood was operationalized as the mean of ODD and CD symptoms across all three adult assessment waves, assessed via the DISC-P. Adult ODD/CD was also included as a covariate.
Substance use
Substance use was assessed in adolescence and adulthood with the Substance Use Questionnaire32 adapted for the MTA.33 Substance use variables were comparable to measures of substance use in other longitudinal studies published previously.33 Participants reported the frequency of alcohol and marijuana use in the past year on an 11-point scale, or, for adolescents, in the past 6 months. The response scales were harmonized to ensure comparability of rating scales from the adolescent and adulthood questionnaires.34 The highest reported past year frequencies across adolescence and adulthood for each of alcohol and marijuana were used in analyses.
Antisocial personality disorder
The Wisconsin Personality Disorders Inventory (WISPI-IV)35 was administered at the 16-year follow-up. The WISPI-IV is a 214-item self-report questionnaire with participants rating each item on a scale of 1-10. Items are combined to provide scores for 11 personality disorder subscales. Adequate convergent and discriminant validity has been demonstrated for the WISPI.36 We included mean scores from the antisocial personality disorder subscale of the WISPI.
Analysis
We used robust Poisson regressions to assess for ADHD-related differences in car crashes rates while controlling for relevant covariates. Our outcome ‘car crashes’ was a count variable (calculated by totalling all car crashes between licensure and the last available assessment point for each participant) and to account for the variation in driving experience between participants, we included driving experience as an offset in the Poisson regression model. That is, ‘car crashes’ was regressed on diagnosis at baseline (ADHD or LNCG) and we included the natural log of driving experience with a fixed coefficient of one as an offset variable in the model. We also controlled for the following variables: sex (sex was added as a covariate as sex-based differences in driving may be seen, both in the general population, as well as specific to populations with ADHD37), age at follow-up (we adjusted for age at follow-up as higher age may be associated with improvements in driving behaviors), baseline diagnosis of oppositional defiant disorder (ODD) or conduct disorder (CD), baseline household income levels, the highest frequency of alcohol and highest frequency of marijuana use, adult ODD/CD symptom scores and adult antisocial personality disorder (ASPD).
We repeated the regression using adult ADHD status (persister or desister or LNCG) as the grouping variable. We also examined associations between dimensional adult ADHD symptom levels and total crashes.
Results are presented as Incidence Rate Ratios (IRR), Confidence Intervals (CI), and p-values. P-values were adjusted using the Benjamini-Hochberg False Discovery Rate (FDR) to account for multiple testing.38 Analyses employed R software, version 3.5.2. (©The R Foundation for Statistical Computing, 2018), and IBM SPSS Statistics for Windows, Version 24 (© IBM Corporation 1989, 2016).
RESULTS
Table 2 presents a comparison of the ADHD group and the LNCG across a few key variables. Total car crashes per subject and alcohol use were comparable in the two groups. Age at licensure, marijuana use, ASPD symptom scores and adult ODD/CD symptom scores were higher in the ADHD group than the LNCG. Licensure rates and baseline annual household income levels (median income LNCG = $50,000 to $60,000; median income ADHD = $40,000 to $50,000) were lower in the ADHD group than the LNCG.
Table 2.
Characteristics of the ADHDb Group and the Local Normative Comparison Group (LNCG)
| ADHD group (n=441) |
LNCG (n=239) |
||
|---|---|---|---|
|
| |||
| Mean(SD) | Mean(SD) | p | |
| Age at follow-up (in years) | 24.79 (1.46) | 24.36 (1.38) | <.001 |
|
| |||
| Car crashes in adulthood | 1.49 (1.72) | 1.34 (1.68) | .30 |
|
| |||
| Driving experience (in months) | 60.74 (29.25) | 71.0 (28.5) | <.001 |
|
| |||
| Age at licensure (in years) | 18.69 (2.2) | 17.75 (1.82) | <.001 |
|
| |||
| Adult Inattentive symptoms | 1.01 (.58) | .44(.43) | <.001 |
|
| |||
| Adult Hyperactive/Impulsive symptoms | .85 (.53) | .39 (.35) | <.001 |
|
| |||
| Alcohol use | 6.92 (2.41) | 6.93 (2.10) | .93 |
|
| |||
| Marijuana use | 5.72 (4.45) | 4.97 (3.91) | .023 |
|
| |||
| Anti-social Personality Disorder symptoms | 1.66 (.89) | 1.37 (.75) | <.001 |
|
| |||
| Adult Conduct Disorder/Oppositional Defiant Disorder symptoms | 1.42 (1.31) | 1.11 (.99) | .001 |
| n (%) | n (%) | p | |
|
| |||
| Sex | |||
| Female | 96 (21.8%) | 48 (20.1%) | .60 |
| Male | 345 (78.2%) | 191 (79.9%) | |
|
| |||
| License obtained | |||
| Yes | 352 (79.8%) | 208 (87%) | .019 |
| No | 89 (20.2%) | 31 (13%) | |
|
| |||
| Baseline household income | |||
| < $10,000 | 36 (8.3%) | 8 (3.5%) | <.001 |
| $10,000 to $20,000 | 48 (11.1%) | 19 (8.3%) | |
| $20,000 to $30,000 | 58 (13.4%) | 23 (10%) | |
| $30,000 to $40,000 | 59 (13.6%) | 30 (13%) | |
| $40,000 to $50,000 | 55 (12.7%) | 28 (12.2%) | |
| $50,000 to $60,000 | 48 (11.1%) | 20 (8.7%) | |
| $60,000 to $70,000 | 43 (9.9%) | 16 (7%) | |
| $70,000 to $75,000 | 22 (5.1%) | 14 (6.17%) | |
| ≥ $75,000 | 64 (14.8%) | 72 (31.3%) | |
|
| |||
| Baseline | |||
| Conduct/Oppositional | 178 (42%) | 3 (1.3%) | <.001 |
| Defiant Disoders | 246 (58%) | 234 (98.7%) | |
| Yes | |||
| No | |||
Attention-Deficit/Hyperactivity Disorder
Table 3 presents a comparison of the persistent and the desistant groups. Age at licensure and licensure rates did not differ between persisters and desisters. Significant differences were found between the two groups in marijuana use, ASPD symptom scores and adult ODD/CD symptom scores (Table 3).
Table 3.
Characteristics of the Persister and Desister groups
| Persisters (n=220) |
Desisters (n=221) |
||
|---|---|---|---|
|
| |||
| Mean(SD) | Mean(SD) | p | |
| Age at follow-up (in years) | 24.79 (1.42) | 24.80 (1.51) | .94 |
|
| |||
| Car crashes in adulthood | 1.54 (1.60) | 1.45 (1.84) | .62 |
|
| |||
| Driving experience (in months) | 55.94 (28.84) | 65.30 (28.99) | .002 |
|
| |||
| Age at licensure (in years) | 18.91 (2.14) | 18.48 (2.25) | .07 |
|
| |||
| Adult Inattentive symptoms | 1.42 (.48) | .60 (.34) | <.001 |
|
| |||
| Adult Hyperactive/Impulsive symptoms | 1.17 (.49) | .54 (.35) | <.001 |
|
| |||
| Alcohol use | 7.03 (2.39) | 6.81 (2.44) | .35 |
|
| |||
| Marijuana use | 6.70 (4.42) | 4.75 (4.27) | <.001 |
|
| |||
| Anti-social Personality Disorder symptoms | 1.86 (.98) | 1.46 (.75) | <.001 |
|
| |||
| Adult Conduct Disorder/Oppositional Defiant Disorder symptoms | 1.62 (1.40) | 1.22 (1.19) | .002 |
| n (%) | n (%) | p | |
|
| |||
| Sex | |||
| Female | 48 (21.8%) | 48 (21.7%) | .98 |
| Male | 172 (78.2%) | 173 (78.3%) | |
|
| |||
| License obtained | |||
| Yes | 173 (78.6%) | 179 (81%) | .54 |
| No | 47(21.4%) | 42 (19%) | |
|
| |||
| Baseline household income | |||
| < $10,000 | 19 (8.8%) | 17 (7.8%) | .47 |
| $10,000 to $20,000 | 24 (11.2%) | 24 (11%) | |
| $20,000 to $30,000 | 29 (13.5%) | 29 (13.3%) | |
| $30,000 to $40,000 | 30 (14%) | 29 (13.3%) | |
| $40,000 to $50,000 | 32 (14.9%) | 23 (10.6%) | |
| $50,000 to $60,000 | 18 (8.4%) | 30 (13.8%) | |
| $60,000 to $70,000 | 25 (11.6%) | 18 (8.3%) | |
| $70,000 to $75,000 | 8 (3.7%) | 14 (6.4%) | |
| ≥ $75,000 | 30 (14.0%) | 34 (15.6%) | |
|
| |||
| Baseline | |||
| Conduct/Oppositional | 93 (44.3%) | 85 (39.7%) | .98 |
| Defiant Disorders | 117 (78.2%) | 129 (60.3%) | |
| Yes | |||
| No | |||
We carried out Poison regressions to determine associations of baseline and adult ADHD status with MVC risk, adjusting for driving experience, sex, age at follow-up, baseline comorbid ODD/CD, baseline household income levels, the highest frequency of alcohol and highest frequency of marijuana use, adult ODD/CD symptom scores and adult ASPD scores. Results from these fully adjusted models showed that a diagnosis of ADHD at baseline was associated with a higher number of MVCs by adulthood (IRR = 1.45, CI = 1.15 to 1.82, p = .006). Comparisons of persisters, desisters and the LNCG showed that the persistent group was associated with a higher rate of MVCs than the desistant group (IRR = 1.46, CI = 1.14 to 1.86, p = .007) or the LNCG (IRR = 1.81, CI = 1.40 to 2.36, p = .0004). MVC rates in the desister group was comparable to that of the LNCG (IRR = 1.24, CI = 0.96 to 1.61, p = .17). Figure 1 presents an overview of IRRs and CIs for baseline and adult ADHD groups. Mean ADHD symptom levels in adulthood (within the baseline ADHD group only) showed a significant association with MVCs (IRR = 1.71, CI = 1.31 to 2.23, p = .001). Both adult inattention (IRR = 1.51, CI = 1.20 to 1.91, p =.003) and hyperactive/impulsive symptom levels (IRR = 1.54, CI = 1.20 to 1.98, p = .005) were associated with MVCs.
Figure 1.
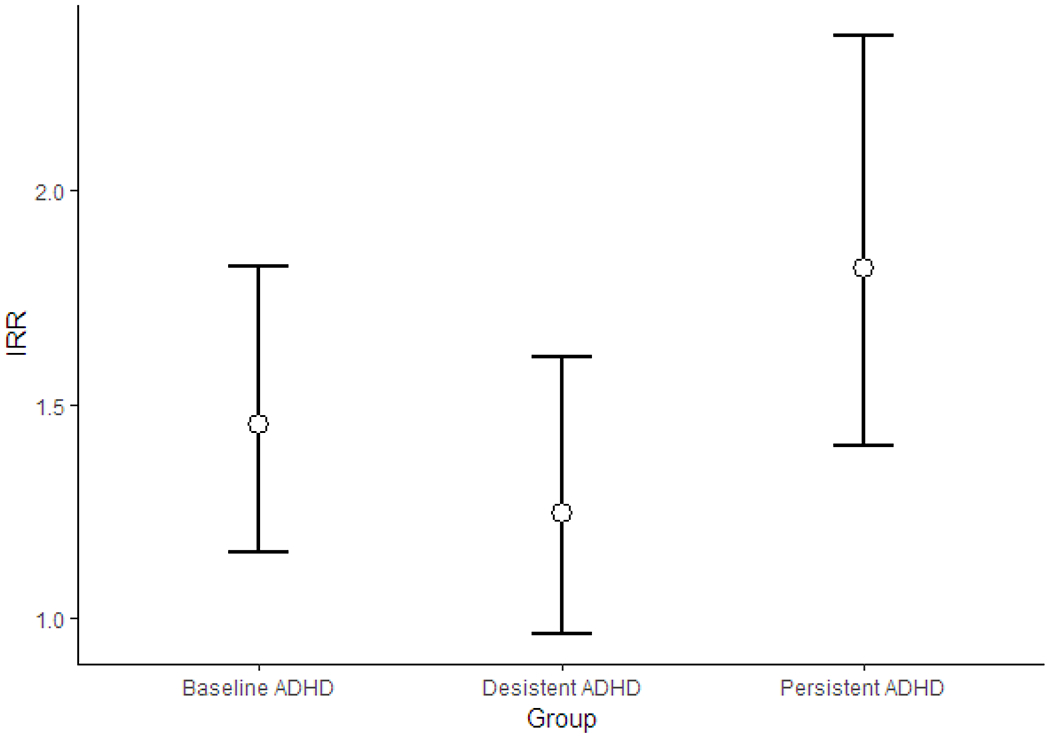
Incidence Rate Ratios (IRR) and their confidence intervals for motor vehicle crash risk in the baseline and adult ADHD groups compared to the Local Normative Comparison Group (LNCG).
To explore the role of driving experience in crash risk, we first ran a regression model including only baseline ADHD status as our predictor, without adjusting for any covariate (unadjusted model). Next, we added driving experience to the regression model (partly adjusted model; did not include any other covariate) to compare the effects of adjusting for driving experience as opposed to not adjusting for driving experience in the associations between ADHD and MVCs. In the unadjusted model, we found no association between baseline ADHD and MVCs (unadjIRR = 1.11, unadjCI = 0.95 to 1.30, unadjp = .18). However, adjustment for driving experience revealed a significant association of baseline ADHD status with MVCs (adjIRR = 1.32, adjCI = 1.13 to 1.54, adjp = .0004). Similarly, we found no differences in MVCs between persisters and the LNCG (unadjIRR = 1.11, unadjCI = .93 to 1.34, unadjp = .25) or between persisters and the desisters (unadjIRR = 1.11, unadjCI = .92 to 1.35, unadjp = .27) in the unadjusted model. Adjustment for driving experience resulted in significant differences in MVCs between persisters and LNCG (adjIRR = 1.59, adjCI = 1.32 to 1.90, adjp < .001) and between persisters and desisters (adjIRR = 1.48, adjCI = 1.22 to 1.78, adjp < .001).
DISCUSSION
We found that adult drivers with childhood ADHD were at a higher risk for MVCs after accounting for driving experience as months since licensure, sex, age at follow-up, baseline ODD/CD comorbidity status, baseline household income, adult ODD/CD symptoms, alcohol and marijuana use, and adult ASPD symptoms. The present study contributes to the literature by making the distinction between those whose childhood ADHD persisted and desisted in adulthood when examining the ADHD-MVC association. We found that within the ADHD group, persisters, but not desisters had an increased MVC risk in comparison to individuals who have never met diagnostic criteria for ADHD.
A previous MTA study demonstrated that although persisters had the worst functional outcomes, desisters also performed poorly in educational and occupational domains.3 In the present study, however, we did not find any increased crash risk among desisters. The low crash risk associated with desistence appears to be explained by differences in ADHD symptom severity and highlight that concurrent, rather than childhood ADHD, increases risk of an MVC. Consistent with this explanation, our results showed that both adult inattention symptom levels and hyperactivity/impulsivity symptom levels were associated with car crashes. The higher risk of MVCs in persisters could also be related to the timing of driving skill development. Driving abilities are gained later in life (mid-to-late adolescence), when desisters may already see a reduction in their ADHD symptom levels. This, unlike educational and occupational outcomes, which are dependent on skills gained throughout childhood, adult driving outcomes may only be impaired if ADHD persists. This may explain why the continuation of ADHD symptoms, either inattentive or hyperactive/impulsive, is predictive of MVCs.
The associations between ADHD and MVC in adult drivers (1.45to1.81) were stronger than that reported in previous population-based studies (1.25 to 1.47) (Curry et al.16; Chang et al.17). Estimates in our study were strongest when comparing ADHD persisters to controls. Notably, these population-based studies utilized objective measures of MVCs including state driving records (Curry et al.16), hospital visits, and video-camera recordings (Aduen et al.12) and yet our findings, which relied on self-report of MVCs, are only somewhat greater than theirs. We also examined the ADHD symptom dimension-MVC risk association within the childhood ADHD group. Our dimensional analysis results are similar to those reported by Aduen et al.,18 in which total ADHD symptom severity significantly predicted crashes and near-crashes. While significant, their reported IRR’s (1.05 and 1.06 for crashes and near-crashes, respectively) were lower than the estimates we found in our study (1.51 and 1.54). Thus, the ADHD-MVC association appears to be strongest when using self-report, as we did, than when using administrative records (Chang et al.17; Curry et al.16), and is even less pronounced when using real-world measures of MVC involvement (Aduen et al.18).
Clinicians will need to walk a delicate tightrope between the need to impart necessary safety information to families and the general public, and the need to avoid contributing to stigma that individuals with ADHD already face.39 Stigma occurs when the population at large accepts negative stereotypes about a group, applying it, accurately or not, to each and every member of that group.40 When the public stigma includes stereotypes that individuals present a safety risk to themselves or others, the consequences can be particularly damaging.40 Mueller and colleagues (2012)40 warned that individuals with ADHD may face public stigma because, as a group, they have been reported to be at greater risk for socially unacceptable behavior such as illicit substance use. Our findings suggest that those with a childhood history of ADHD also are at increased risk for MVC, on average. Hence, increasing awareness among drivers with ADHD, their families, and clinicians who work with them is an important step in preventing MVCs among drivers with ADHD. However, it is important that these findings are discussed in a balanced way so they do not contribute to perceptions of individuals with ADHD as universally presenting a safety risk to those around them. One way to do this is to place this information in the context of our findings related to ADHD persistence versus desistence: MVC risk appears to be specific to individuals whose childhood ADHD persists into adulthood, with symptoms of inattention and hyperactivity/impulsivity being predictive of MVC risk. This finding suggests that continuous management of ADHD symptoms in adulthood may prevent MVCs. Such information could motivate individuals with ADHD to continue treatments for ADHD symptoms or to seek interventions that target specific impairments. For example, there is some evidence to suggest that training with driving simulators may improve driving abilities in the short term (Fabiano et al., 2016). While, additional studies on driving simulator based training are needed to estimate their long-term utility and before such training is routinely implemented, providing such information may help youth with ADHD understand the complex pathways leading to an MVC risk, stay abreast of developments in the field, and consequently feel empowered and in charge of their lives. Moreover, some youth with ADHD may decide (or their parents may decide for them) to postpone obtaining a driver’s license until they mature further, and it is important to discuss the implications of such delays. That is, delaying licensure may not improve outcomes41 perhaps because driving is an acquired skill that improves with practice,42 and licensure delays beyond adolescence could lead to a loss of opportunities to train under safe conditions (such as with the graduated driver’s licensing or GDL for adolescents). For this reason, some experts recommend that parents and adolescents elect to delay obtaining a full, independent license and keep their adolescent with ADHD in a graduated driver’s license stage that has restrictions in place meant to keep adolescent driver’s safe (e.g., restriction on number of passengers).43 Finally, youth with ADHD may benefit from special driving training such as via a certified driving rehabilitation specialist. However, we severely lack studies that assess if, and to what extent, training from specialized driving instructors attenuates driving problems and MVC risk. Especially, research is needed to understand if development of special, more intensive driver training programs for those with ADHD could be an effective intervention. In sum, discussing all these facets of the ADHD-MVC risk in a balanced and truthful manner is an important beginning in raising awareness without unnecessarily contributing to public stigma of ADHD.
Our study findings highlight an important methodological issue when examining MVC-risk, namely how to account for driving exposure since individuals who spend more time on the road have higher opportunities for MVC involvement. In previous studies, researchers have defined driving exposure as number of miles driven and have used this measures as a control variable in analyses. Miles driven has been found to be an important confounding variable that when controlled for in analyses attenuates the ADHD-MVC association (Vaa6). Except for naturalistic studies, which can calculate the number of miles driven using in-car technology, researchers rely on self-report estimates of the average number of miles driven per week by participants. We calculated the time since licensure as the indicator of driving exposure as we felt this was a more objective estimate and less prone to errors than self-report of miles driven. Rather than attenuating the ADHD-MVC risk this association was only present when experience was included in the model. Thus, in the present sample it appears that ADHD does increase risk for MVCs and that individuals with ADHD accumulate similar rates of MVCs as do their peers without ADHD, but in a shorter period. The differential influence of months driving experience in our study and miles driven in other studies on the ADHD-MVC association highlights the complex nature of the construct of driving exposure. Individuals with childhood ADHD are likely to drive without a license43–45 and may drive more frequently than controls,6 both of which can affect MVC risk and miles driven, but not time since licensure. Since retrospective recall of ‘total miles driven’ may be poor and biased,47 future studies can combine this measure with information about time since licensure to estimate driving exposure.
A notable limitation of this study is that we could not assess the effects of medication on crash risk in adult drivers.48 We did not have information on the timing of medication use with respect to driving, so we could not evaluate the acute pharmacological effect on driving and crash timing. Moreover, less than 10% of the ADHD group reported any use of medication in adulthood when most of the driving would have been occurring. Thus, the statistical power to evaluate protective effects of medication would be low. A second important limitation of our study is the use of self-reports to assess crashes. Retrospective recall of car crashes may be poor. Further, our questionnaire asked for information on any car crash that the participant may have been involved in. This can be interpreted in multiple ways and while some participants may have reported only the most serious car crashes, others may have also reported minor collisions, which may be considered unimportant from a public health perspective. Moreover, ADHD is associated with positive illusory bias for a subset of individuals.49 Particularly, self-assessments of driving capabilities in individuals with ADHD tend to be positively biased.47 This may have led to underreporting of car crashes in the ADHD group. We also did not assess driving frequency, which may affect the likelihood of crashing. Driving exposure in this study was calculated as time since licensure. However, true driving exposure depends on the actual frequency of driving and the total number of miles driven since licensure. Thus, participants with comparable time since licensure in this study may or may not be comparable in terms of actual miles driven. Participants with ADHD who were driving without a license were excluded from analyses since driving experience could not be calculated. However, their inclusion could alter crash risk. Finally, a comparison of baseline characteristics of the study sample compared to those not followed-up showed notable differences in socioeconomic status. Median paternal educational level and household income were higher in the study sample. Inclusion of the participants lost to follow-up may have resulted in a different picture of the ADHD-car crash association.
To summarize, we found that adult ADHD persistence, but not desistence, is associated with car crashes in adult drivers, accounting for childhood ODD/CD comorbidity, childhood socioeconomic status, adult ODD/CD, substance use, and ASPD. Thus, we suggest that compared to childhood ADHD, adult ADHD status is a stronger predictor of car crashes in adult drivers.
CLINICAL POINTS:
Long term, continuous treatment of ADHD, and management of adult persistent ADHD symptoms can reduce adult car crash risk
In adulthood, presence of either inattention or hyperactivity/impulsivity symptoms are sufficient to increase a risk for motor vehicle crashes
Risk for motor vehicle crashes in adult drivers with ADHD can only be understood in the context of driving experience
Footnotes
Presentation information:
This study was presented at the American Academy of Child and Adolescent Psychiatry’s 65th Annual Meeting, October 22-27, 2018, in Seattle, WA, and at the Nineteenth Biennial Scientific Meeting of the International Society for Research in Child and Adolescent Psychopathology, June 26-29, in Los Angeles, California
Text for social media promotion: Adult persistent #ADHD related to motor vehicle #crash risk, shows new study @JAACAP
Contributor Information
Arunima Roy, The Royal’s Institute of Mental Health Research, University of Ottawa.
Annie A. Garner, Department of Psychology, Saint Louis University.
Jeffery N. Epstein, Department of Pediatrics, University of Cincinnati College of Medicine; Division of Behavioral Medicine and Clinical Psychology, Cincinnati Children’s Hospital Medical Center.
Betsy Hoza, Department of Psychological Science, University of Vermont.
J. Quyen Nichols, Department of Psychological Science, University of Vermont.
Brooke S. G. Molina, Departments of Psychiatry, Psychology & Pediatrics, University of Pittsburgh School of Medicine.
James M. Swanson, Child Development Center, School of Medicine, University of California, Irvine.
L. Eugene Arnold, Department of Psychiatry & Behavioral Health, Nisonger Center, Ohio State University.
Lily Hechtman, Division of Child Psychiatry, McGill University, Montreal Children’s Hospital.
REFERENCES
- 1.Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (5th edition). 2014. [Google Scholar]
- 2.Caye A, Spadini AV, Karam RG et al. Predictors of persistence of ADHD into adulthood: a systematic review of the literature and meta-analysis. Eur Child Adolesc Psychiatry. 2016;25(11):1151–1159. [DOI] [PubMed] [Google Scholar]
- 3.Faraone S, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2005;36(02):159. [DOI] [PubMed] [Google Scholar]
- 4.Hechtman L, Swanson JM, Sibley MH, et al. Functional Adult Outcomes 16 Years After Childhood Diagnosis of Attention-Deficit/Hyperactivity Disorder: MTA Results. J Am Acad Child Adolesc Psychiatry. 2016;55(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) [online]. 2005. [2019 Mar. 21]. Available from URL: www.cdc.gov/injury/wisqars
- 6.Vaa T ADHD and relative risk of accidents in road traffic: A meta-analysis. Accid Anal Prev. 2014;62:415–425. [DOI] [PubMed] [Google Scholar]
- 7.Reason J, Manstead A, Stradling S, Baxter J, Campbell K. Errors and violations on the roads: a real distinction? Ergonomics. 1990;33(10-11):1315–1332. [DOI] [PubMed] [Google Scholar]
- 8.Graziano P, Reid A, Slavec J, Paneto A, McNamara J, Geffken G. ADHD Symptomatology and Risky Health, Driving, and Financial Behaviors in College. J Atten Disord. 2014;19(3):179–190. [DOI] [PubMed] [Google Scholar]
- 9.Barkley RA, Murphy KR, & Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996; 98(6): 1089–1095. [PubMed] [Google Scholar]
- 10.Fischer M, Barkley R, Smallish L, Fletcher K. Hyperactive children as young adults: Driving abilities, safe driving behavior, and adverse driving outcomes. Accident Analysis & Prevention. 2007;39(1):94–105. [DOI] [PubMed] [Google Scholar]
- 11.Narad M, Garner AA, Brassell AA, et al. Impact of Distraction on the Driving Performance of Adolescents With and Without Attention-Deficit/Hyperactivity Disorder. JAMA Pediatr. 2013;167(10):933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aduen P, Kofler M, Cox D, Sarver D, Lunsford E. Motor vehicle driving in high incidence psychiatric disability: Comparison of drivers with ADHD, depression, and no known psychopathology. J Psychiatr Res. 2015;64:59–66. [DOI] [PubMed] [Google Scholar]
- 13.Barkley RA, Murphy KR, Dupaul GJ, Bush T. Driving in young adults with attention deficit hyperactivity disorder: Knowledge, performance, adverse outcomes, and the role of executive functioning. J Int Neuropsychol Soc. 2002;8(05). [DOI] [PubMed] [Google Scholar]
- 14.Narad ME, Garner AA, Antonini TN, et al. Negative Consequences of Poor Driving Outcomes Reported by Adolescents With and Without ADHD. J Atten Disord. 2015:108705471557506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Molina BS, Hinshaw SP, Swanson JM, et al. The MTA at 8 Years: Prospective Follow-up of Children Treated for Combined-Type ADHD in a Multisite Study. J Am Acad Child Adolesc Psychiatry. 2009;48(5):484–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curry AE, Metzger KB, Pfeiffer MR, Elliott MR, Winston FK, Power TJ. Motor Vehicle Crash Risk Among Adolescents and Young Adults With Attention-Deficit/Hyperactivity Disorder. JAMA Pediatr. 2017;171(8):756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang PD, Lichtenstein P, D’Onofrio BM, Sjölander A, Larsson H. Serious transport accidents in adults with attention-deficit/hyperactivity disorder and the effect of medication: A population-based study. JAMA Psychiatry. 2014;71(3):319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aduen P, Kofler M, Sarver D, Wells E, Soto E, Cox D. ADHD, depression, and motor vehicle crashes: A prospective cohort study of continuously-monitored, real-world driving. J Psychiatr Res. 2018;101:42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prevatt F, Proctor B, Baker L, Garrett L, Yelland S. Time Estimation Abilities of College Students With ADHD. J Atten Disord. 2010;15(7):531–538. [DOI] [PubMed] [Google Scholar]
- 20.Storebø O, Simonsen E. The Association Between ADHD and Antisocial Personality Disorder (ASPD). J Atten Disord. 2016;20(10):815–824. [DOI] [PubMed] [Google Scholar]
- 21.Russell A, Ford T, Russell G. Socioeconomic Associations with ADHD: Findings from a Mediation Analysis. PLoS ONE. 2015;10(6):e0128248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rowland A, Skipper B, Rabiner D et al. Attention-Deficit/Hyperactivity Disorder (ADHD): Interaction between socioeconomic status and parental history of ADHD determines prevalence. Journal of Child Psychology and Psychiatry. 2017;59(3):213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shults R, Banerjee T, Perry T. Who’s not driving among U.S. high school seniors: A closer look at race/ethnicity, socioeconomic factors, and driving status. Traffic Inj Prev. 2016;17(8):803–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harper S, Charters T, Strumpf E. Trends in Socioeconomic Inequalities in Motor Vehicle Accident Deaths in the United States, 1995–2010. Am J Epidemiol. 2015;182(7):606–614. [DOI] [PubMed] [Google Scholar]
- 25.Wymbs BT, Molina BSG, Belendiuk KA, et al. Motorsports Involvement Among Adolescents and Young Adults with Childhood ADHD. J Clin Child Adolesc Psychol. 2013;42(2):220–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jensen PS. A 14-Month Randomized Clinical Trial of Treatment Strategies for Attention-Deficit/Hyperactivity Disorder. Arch Gen Psychiatry. 1999;56(12):1073. [DOI] [PubMed] [Google Scholar]
- 27.Jensen PS, Arnold LE, Swanson JM, et al. 3-Year Follow-up of the NIMH MTA Study. J Am Acad Child Adolesc Psychiatry. 2007;46(8):989–1002. [DOI] [PubMed] [Google Scholar]
- 28.National Institute of Mental Health Multimodal Treatment Study of ADHD Follow-up: 24-Month Outcomes of Treatment Strategies for Attention-Deficit/Hyperactivity Disorder. Pediatrics. 2004;113(4):754–761. doi: 10.1542/peds.113.4.754. [DOI] [PubMed] [Google Scholar]
- 29.Wells KC, Epstein JN, Hinshaw SP, et al. Parenting and family stress treatment outcomes in attention deficit hyperactivity disorder (ADHD): An empirical analysis in the MTA study. J Abnorm Child Psychol. 2000;28(6):543–53. [DOI] [PubMed] [Google Scholar]
- 30.Sibley MH, Swanson JM, Arnold LE, et al. Defining ADHD symptom persistence in adulthood: optimizing sensitivity and specificity. J Child Psychol Psychiatry. 2016;58(6):655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, Differences From Previous Versions, and Reliability of Some Common Diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. [DOI] [PubMed] [Google Scholar]
- 32.Molina BSG, Pelham WE. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J Abnorm Psychol. 2003;112(3):497–507. [DOI] [PubMed] [Google Scholar]
- 33.Molina BS, Hinshaw SP, Arnold LE, et al. Adolescent Substance Use in the Multimodal Treatment Study of Attention-Deficit/Hyperactivity Disorder (ADHD) (MTA) as a Function of Childhood ADHD, Random Assignment to Childhood Treatments, and Subsequent Medication. J Am Acad Child Adolesc Psychiatry. 2013;52(3): [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Molina BS, Howard AL, Swanson JM, et al. Substance use through adolescence into early adulthood after childhood-diagnosed ADHD: findings from the MTA longitudinal study. J Child Psychol Psychiatry. August 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klein MH, Benjamin LS, Rosenfeld R, Treece C, Husted J, Greist JH. The Wisconsin personality disorders inventory: Development, reliability, and validity. J Pers Disord.1993;7(4):285–303. [Google Scholar]
- 36.Smith T, Klein M, Benjamin L. Validation of the Wisconsin Personality Disorders Inventory-IV with the SCID-II. J Pers Disord. 2003;17(3):173–187. [DOI] [PubMed] [Google Scholar]
- 37.Bron TI, Bijlenga D, Breuk M, Michielsen M, Beekman AT, Kooij JS. Risk factors for adverse driving outcomes in Dutch adults with ADHD and controls. Accid Anal Prev. 2018;111:338–344. [DOI] [PubMed] [Google Scholar]
- 38.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;1:289–300. [Google Scholar]
- 39.Mueller AK, Fuermaier ABM, Koerts J, Tucha L. Stigma in attention deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2012:4(3):101–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corrigan PW, Shapiro JR. Measuring the impact of programs that challenge the public stigma of mental illness. Clin Psychol Rev. 2010:30(8);907–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Curry AE, Yerys BE, Metzger KB, Carey ME, Power TJ. Traffic crashes, violations, and suspensions among young drivers with ADHD. Pediatrics. 2019;43(6), e20182305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keating DP. Understanding adolescent development: Implications for driving safety. J Safety Res. 2007;38(2):147–157. doi: 10.1016/j.jsr.2007.02.002 [DOI] [PubMed] [Google Scholar]
- 43.Aduen PA, Cox DJ, Fabiano GA, Garner AA, & Kofler MJ (2019). Expert Recommendations for Improving Driving Safety for Teens and Adult Drivers with ADHD. The ADHD Report, 27(4), 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barkley RA, Guevremont DC, Anastopoulos AD, DuPaul GJ, Shelton TL. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: a 3-to 5-year follow-up survey. Pediatrics. 1993;1;92(2):212–8. [PubMed] [Google Scholar]
- 45.Hoza B, Mcquade JD, Murray-Close D, et al. Does childhood positive self-perceptual bias mediate adolescent risky behavior in youth from the MTA study? J Consult Clin Psychol. 2013;81(5):846–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thompson AL, Molina BS, Pelham W, Gnagy EM. Risky Driving in Adolescents and Young Adults with Childhood ADHD. J Pediatr Psychol. 2007;32(7):745–759. [DOI] [PubMed] [Google Scholar]
- 47.Fabiano GA, Schatz NK, Hulme KF et al. Positive bias in teenage drivers with ADHD within a simulated driving task. J Atten Disord. 2018;22(12):1150–1157. [DOI] [PubMed] [Google Scholar]
- 48.Chang Z, Quinn PD, Hur K, et al. Association between medication use for attention-deficit/hyperactivity disorder and risk of motor vehicle crashes. JAMA psychiatry. 2017;74(6):597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM. A Critical Review of Self-perceptions and the Positive Illusory Bias in Children with ADHD. Clin Child Fam Psychol. 2007;10(4):335–351. [DOI] [PubMed] [Google Scholar]


