Highlights
-
•
Tested effect of rural identity on virtual human clinician (VHC) appearance.
-
•
Participants with high rural identity rated VHCs as more attractive.
-
•
Black adults with high rural belonging rated VHCs as more attractive.
-
•
Black adults with high rural identity rated a Black VHC as more attractive.
Abbreviations: VHC, virtual human clinician; ALEX, Agent Leveraging Empathy for eXams
Keywords: Cancer screening disparities, Health communication, Rural health, Virtual human technology
Abstract
Rural adults experience disparities in colorectal cancer screening, a trend even more distinct among rural Black adults. Healthcare disruptions caused by COVID-19 exacerbated inequities, heightening attention on virtual communication strategies to increase screening. Yet little is known about how rural adults perceive virtual human clinicians (VHCs). Given that identifying as rural influences perceived source credibility often through appearance judgments, the goal of this pilot was to explore how to develop VHCs that individuals highly identified with rurality find attractive. Between November 2018 and April 2019, we tested a culturally tailored, VHC-led telehealth intervention delivering evidence-based colorectal cancer prevention education with White and Black adults (N = 2079) in the United States recruited through an online panel who were non-adherent to screening guidelines and between 50 and 73 years of age. Participants were randomized on three factors (VHC race-matching, VHC gender-matching, Intervention type). Ordinal logistic regression models examined VHC appearance ratings. Participants with a high rural identity (AOR = 1.12, CI = [1.02, 1.23], p =.02) rated the VHCs more attractive. High rural belonging influenced VHC attractiveness for Black participants (AOR = 1.22, CI = [1.03, 1.44], p =.02). Also, Black participants interacting with a Black VHC and reporting high rural self-concept rated the VHC as more attractive (AOR = 2.22, CI = [1.27, 3.91], p =.01). Findings suggest adults for whom rural identity is important have more positive impressions of VHC attractiveness. For patients with strong rural identities, enhancing VHC appearance is critical to tailoring colorectal cancer prevention interventions.
1. Introduction
Colorectal cancer is the second leading cause of cancer death in the United States. In 2022, it is estimated that 151,030 people will be diagnosed with colorectal cancer, and 52,580 people will die from the disease ((American Cancer Society, 2022). Colorectal cancer mortality can be reduced by timely screening (Loomans-Kropp and Umar, 2019); unfortunately, due in part to structural challenges (e.g., access, cost), rural adults are less likely to get screened and experience disproportionate disease burden (Anderson et al., 2013: Henley et al., 2017, Moreno et al., 2020, Zahnd et al., 2021). Colorectal cancer disparities are even more distinct among rural Black adults (Rogers et al., 2020, Zahnd et al., 2021). As singular communication strategies are ineffective in meeting the needs of diverse subgroups, there is an urgent need to develop screening interventions that deliver culturally tailored messaging to rural adults to close gaps in the prevention and early detection of colorectal cancer.
Advancements in telehealth delivery through virtual human technology offer a cutting-edge opportunity to provide evidence-based colorectal cancer prevention messaging. Using virtual human clinicians (VHCs), computer-based conversational agents that interact with patients by presenting human attributes (e.g., facial expressions, hand gestures, speech), screening education can be provided in a consistent manner that reduces barriers (Bickmore et al., 2009). Prior research on virtual agents has found them effective in addressing various health behaviors, including alcohol consumption, personal fitness, and nutrition (Lisetti et al., 2013, Lucas et al., 2018, Olafsson et al., 2020) . VHCs can serve as social models and offer customizable interactions that match patient characteristics (e.g., race, gender, language) (Baylor and Kim, 2004, Krieger et al., 2021, Provoost et al., 2017, Zalake et al., 2021).
VHC-led interventions can be tailored to patient preferences, impacting message processing and relevance (Hawkins et al. 2008). Rural patients have unique needs, given the lack of medical workforce diversity and clinician shortages. VHCs in telehealth offer a low-cost alternative to face-to-face care that reduces travel constraints while improving access and choice for rural patients, contributing to increased satisfaction (Bernardo et al., 2018, Kamran et al., 2022, Orlando et al., 2019). Prior work has shown tailored virtual agents to be effective in educating rural populations about cancer (Mendu et al., 2018). Further, patients with low health literacy, which is increasingly likely among rural adults, often find VHC-led interventions acceptable and easy to use (Bickmore et al., 2009). In sum, current literature on VHCs suggests they are an appropriate communication strategy for rural patients to increase the utilization of colorectal cancer screening.
Perceived clinician credibility can influence patient response to recommendations (Polinski et al., 2014) . One way to enhance credibility in face-to-face encounters is racial concordance between patient and clinician (Street et al., 2008, Thornton et al., 2011) . In the telehealth context, VHC credibility has a positive influence on colorectal cancer screening intention (Cooks et al., 2022). Matching patients with a race-concordant VHC can also positively influence screening intentions due to increased credibility (Cooks et al., 2022, Griffin et al., 2019, Hung et al., 2020, Krieger et al., 2021, Shen et al., 2018, ter Stal et al., 2020). Intentions to screen are often positively associated with screening completion (Brumbach et al., 2017, Birmingham et al., 2015). However, knowledge of how rural adults perceive VHC credibility is lacking, limiting the ability to tailor effective interventions.
One key dimension of credibility is attractiveness; message sources rated as more attractive are often more persuasive and generate increased behavioral motivation (Baylor et al., 2009; Cialdini, 2001, Cialdini and Goldstein, 2004, Chaiken, 1979, Ohanian, 1990, Wilson-Howard et al., 2021). The flexibility of VHCs allows for systematic enhancements to appearance. Recent findings in developing culturally appropriate VHCs for rural Black adults suggest credibility is influenced by technical quality and appearance (Vilaro et al., 2021a, Wilson-Howard et al., 2021). Simply put, VHC appearance is an indicator of credibility, particularly among rural adults, which influences colorectal cancer screening intentions. Thus, the appearance of a message source is an important factor for enhancing the credibility of interventions to encourage screening in rural populations.
There is, however, a lack of consistency in how rurality is measured; it is frequently defined geographically, yet the strength with which an individual identifies themselves as being rural can significantly influence behavior (Ratcliffe et al., 2016). Like other forms of group-based membership, such as racial and ethnic identity, rural identity functions to reduce uncertainty, specifically within a social “place” as members accept cultural norms and behavior (Tajfel, 1979, Twigger-Ross et al., 2003). This “sense of place” suggests a relationship between individuals and their environment where bonds with places, including their value and meaning, are continuously reconstructed (Lengen and Kistemann, 2012). The four-item rural identity scale first used by Krok-Schoen et al. (2015) taps four dimensions: (1) place identity (e.g., bond generated with places through observation of values, thoughts, and ideas [Qazimi, 2014]), (2) self-concept (e.g., personal identification as “rural”), (3) similarity (e.g., alignment with rural culture and values), and (4) sense of belonging (e.g., community connection). However, the scale performance in capturing rurality has not been explored within virtual cancer screening interventions.
This pilot study tested a VHC-led intervention entitled Meet “ALEX” (Agent Leveraging Empathy for eXams), providing evidence-based colorectal cancer prevention education(Griffin et al., 2019, Zalake et al., 2021) . A challenge to communicating the importance of colorectal cancer screening to a rural audience is the perception that a message source is a cultural “outsider,” which can be reduced through appearance adjustments (e.g., clothing, accessories, etc.) to increase message acceptance (Palmer-Wackerly et al., 2014, Hardy et al., 2019). The importance of VHC appearance for credibility and acceptability among rural adults was also a consistent theme during user-centered ALEX development. One tester commented, “Like I say, being as that he was a brother-doctor look, it was more acceptable to listen to it opposed to another type,” while another mentioned, “I don’t want to go to nobody looking all weird and start asking me questions” (Vilaro et al., 2021b, Wilson-Howard et al., 2021). Given the importance of VHC appearance, the purpose of this pilot was to explore how to develop VHCs that rural adults would find attractive. Considering that tailoring health interventions involves attending to the influence of cultural norms and beliefs (Kreuter et al., 2003) and that sociocultural aspects of rurality (e.g., cultural values, perceptions) can influence user experiences with technology (Hardy et al., 2019), the role of rural identity was examined. Several research questions were investigated:
RQ1a: Is rural identity associated with evaluations of VHC appearance?
RQ1b: How do rural identity and race interact to influence evaluations of VHC appearance?
RQ2: How do rural identity and VHC race-matching interact to influence evaluations of VHC appearance among Black adults?
RQ3: How do the different dimensions of rural identity relate directly and intersect with race and VHC race-matching to influence evaluations of VHC appearance?
2. Materials and methods
Meet ALEX was developed as part of a National Cancer Institute-funded project (1R01CA207689-01) and approved for human-subjects research by a local institutional review board. Development is described below and more thoroughly elsewhere (Griffin et al., 2019, Zalake et al., 2021).
2.1. Design
After consenting, participants were randomized to one of eight treatments based on VHC race-matching (matched, not-matched), VHC gender-matching (matched, not-matched), and intervention type (interactive, static). This study focuses on rural identity effects related to VHC race-matching. Statistical models did not consider VHC gender-matching and intervention type and have been reported elsewhere (Cooks et al., 2022, Krieger et al., 2021).1
2.2. Intervention
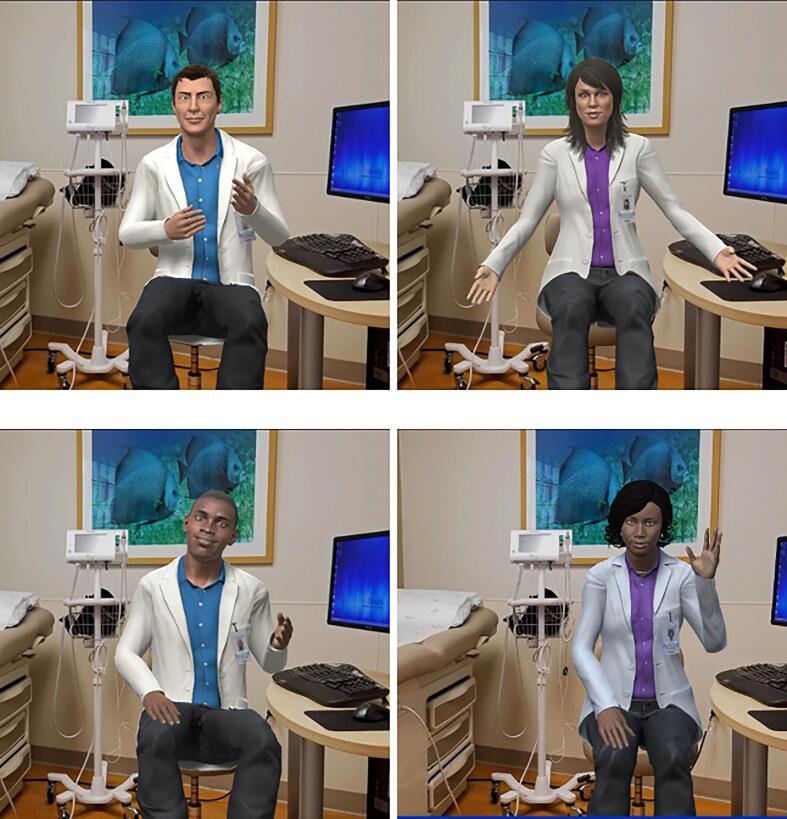
Using computer-generated characters to engage patients in a one-one conversation about colorectal cancer prevention, ALEX is a VHC located in a digital exam room that can be matched to patient race and gender (see Fig. 1). ALEX was developed to address colorectal cancer screening disparities through a cross-disciplinary partnership of communication, cancer, and computer scientists, clinicians, and community members. Focus groups and think-aloud interviews with over 120 diverse community members within the research team’s largely rural catchment area informed the iterative user-centered design process, including enhancements to VHC appearance. Phase 1 collected information on user preferences and needs before prototype development. In Phase 2, users tested the prototype and commented on character details that informed refinement (e.g., added white coat, changed lighting, removed gray hair). Phase 3 included additional feedback on VHC appearance (e.g., added smile, focused eye gaze, changed hairstyle), leading to final modification (see Vilaro et al., 2020, Wilson-Howard et al., 2021). Efforts were made to reduce the health literacy for engagement (i.e., visuals of stool sample collection rather than words). The interactive ALEX provides colorectal cancer screening information verbally with closed captioning, asks closed-ended questions, and uses nonverbal behaviors; users receive personalized prevention messaging based on responses (see supplement for link). The static ALEX provides identical content in text and still photos. ALEX is a patient-centered intervention that addresses various screening modalities (e.g., colonoscopy, Cologuard, FIT) (For more information on the ALEX intervention, see Cooks et al., 2022, Krieger et al., 2021).
Fig. 1.
Images of the Meet ALEX virtual clinicians.
2.3. Sample selection and data collection
Between November 2018 and April 2019, a total of 2,267 participants recruited from a nationally representative Qualtrics panel of individuals who agreed to research participation were randomized into this online experiment; 201 did not complete the post-intervention questionnaire and were excluded from analysis, leaving a final sample of 2,066 participants. Qualtrics was selected for recruitment to pilot this intervention before moving into a clinical population. Panel members were emailed an invitation link and completed eligibility questions. A total of 24,732 individuals began the survey, and more than 22,000 were screened out (due primarily to being within screening guidelines). Eligibility criteria included: (a) United States residents aged 50–73, (b) able to read in English, (c) self-identifying race as Black or White Non-Hispanic,2 (d) non-adherent with colorectal cancer screening guidelines, and (e) providing informed consent. Although colorectal cancer screening is currently recommended for individuals aged 45 to 75 years, at the time of this study, screening guidelines had not been revised to include patients 45–49 years of age.3 Further, we set the upper limit to 73 to ensure eligibility for the study duration.
2.4. Measures
The primary outcome measured was VHC appearance quality measured as attractiveness (McCroskey and Teven, 1999). Using a 5-point semantic differential (labeled “unattractive-attractive”), the item read, “ALEX was your virtual healthcare assistant who provided you the health information during your virtual appointment. ALEX is….”. (M = 4.6, SD = 0.7). Rural identity was assessed using a four-item measure (α = 0.92, M = 2.7, SD = 1.3), capturing different facets of deriving a sense of self from social group memberships (Krok-Schoen et al., 2015). Specifically, on a 5-point Likert scale, the items measure rural place identity (“How much is being from a rural community a part of who you are?” M = 2.5, SD = 1.4), self-concept (“How much do you identify with people who live in rural communities?” M = 2.9, SD = 1.3), belonging (“How much do you see yourself as belonging to a rural community?” M = 2.6, SD = 1.5), and similarity (“To what extent do you feel your general attitudes and opinions are similar to people who live in rural communities?” M = 3.0, SD = 1.3).
2.5. Analysis plan
Statistical analyses were conducted using R 4.0.1 (R Core Team, 2018). Ordinal logistic regression models were implemented with the clm function in the ordinal package. An ordinal logistic regression model with a logit link function is called a proportional-odds model. We implemented five ordinal regression models corresponding to the median of the rural identity measure along with each of its four items. To evaluate the proportional odds assumption, we conducted a Brant Test using the “brant” package in R; this assumption was supported (p = 0.89). The estimated regression coefficients of each model represent log-odds ratios, which were transformed into odds ratios through exponentiation (see Stoltzfus, 2011 for a review). Models used perceived VHC attractiveness as a dependent variable and contained up to three-way interactions between participant race, rural identity, and VHC race-matching4 as features. Rural identity was coded as a continuous variable. The mean absolute error was formulated to assess model fit, with the value between the predicted and observed perceived VHC attractiveness being 0.88.
Analyses were conducted to determine the influence of rural identity on the relationship between VHC race-matching and VHC attractiveness. We used two 2-sided Z-tests to identify the main effects of participant race, rural identity, and VHC race-matching. We also used Z-tests to determine whether rural identity influenced the relationship between VHC race-matching and VHC attractiveness based on participant race. To do this, we conducted four hypothesis tests that required examining linear combinations of regression coefficients (see technical supplement for more information). We tested the effect of VHC race-matching against race-mismatching amongst Black participants with high rural identity. A similar test was conducted with Black adults with low rural identity and among White participants based on rural identity identification. High identification was defined as an item response of ‘5′, and low identification as a response of ‘1′. All hypothesis tests were conducted at a 0.05 significance level. We provide adjusted odds ratios (AOR) and 95 % confidence intervals for each tested effect.
3. Results
3.1. Sample characteristics
Table 1 describes sample demographics. Participants were primarily female (59.9 %), with an average age of 58.7 (SD = 6.2). Among this sample, 37.1 % (n = 840) identified as Black or African American. Further, over 60 % had at least some post-secondary education, and income level displayed a fairly even distribution. Table 2 presents responses at each scale level for rural identity items overall and by participant race/VHC race-matching interaction.
Table 1.
Sample characteristics (N = 2267).
| Characteristic | |
|---|---|
| Age, mean (SD) | 58.7 (6.2) |
| Gender, No. (%) | |
| Man | 908 (40.1 %) |
| Woman | 1359 (59.9 %) |
| Race, No. (%) | |
| Black | 840 (37.1 %) |
| White | 1427 (62.9 %) |
| Educational Attainment | |
| College graduate | 475 (22.8 %) |
| Technical, trade or vocational school AFTER high school | 559 (26.9 %) |
| High school incomplete (completed grades 1–8) | 41 (2.0 %) |
| Post-graduate training/professional school after college (MA, Ph.D., JD, or MD) | 195 (9.4 %) |
| Some college | 809 (38.9 %) |
| Income | |
| Less than $10,000 | 142 (6.8 %) |
| $10 – $20,000 | 298 (14.3 %) |
| $20 – $30,000 | 338 (16.3 %) |
| $30 – $40,000 | 246 (11.8 %) |
| $40 – $50,000 | 198 (9.5 %) |
| $50 – $75,000 | 336 (16.2 %) |
| $75 – $100,000 | 204 (9.8 %) |
| $100,000 or more | 158 (7.6 %) |
Table 2.
Proportion of responses across items, overall and by race/virtual human clinician (VHC) race-matching.
| Overall % (n) |
Participant Race/Race-Matching % (n) |
||||
|---|---|---|---|---|---|
| Study variable | Black/Matched | Black/Mis-matched | White/Matched | White/Mis-matched | |
| Belonging | |||||
| 1 | 33.5 (6 9 7) | 39.6 (1 3 3) | 42.4 (1 3 4) | 33.6 (1 7 9) | 28.0 (2 5 1) |
| 2 | 14.9 (3 1 0) | 13.7 (46) | 13.0 (41) | 15.2 (81) | 15.9 (1 4 2) |
| 3 | 21.3 (4 4 2) | 21.4 (72) | 19.3 (61) | 19.4 (1 0 3) | 23.0 (2 0 6) |
| 4 | 13.9 (2 8 9) | 11.3 (38) | 13.6 (43) | 15.8 (84) | 13.9 (1 2 4) |
| 5 | 16.4 (3 4 1) | 14.0 (47) | 11.7 (37) | 16.0 (85) | 19.2 (1 7 2) |
| Place identity | |||||
| 1 | 36.9 (7 6 7) | 46.1 (1 5 5) | 44.3 (1 4 0) | 37.8 (2 0 1) | 30.3 (2 7 1) |
| 2 | 14.5 (3 0 1) | 11.6 (39) | 16.1 (51) | 13.9 (74) | 15.3 (1 3 7) |
| 3 | 20.5 (4 2 6) | 18.5 (62) | 16.1 (51) | 19.2 (1 0 2) | 23.6 (2 1 1) |
| 4 | 14.7 (3 0 6) | 10.4 (35) | 13.3 (42) | 17.5 (93) | 15.2 (1 3 6) |
| 5 | 13.4 (2 7 9) | 13.4 (45) | 10.1 (32) | 11.7 (62) | 15.6 (1 4 0) |
| Self-concept | |||||
| 1 | 20.4 (4 2 5) | 22.9 (77) | 25.0 (79) | 21.4 (1 1 4) | 17.3 (1 5 5) |
| 2 | 17.5 (3 6 4) | 15.8 (53) | 19.3 (61) | 16.7 (89) | 18.0 (1 6 1) |
| 3 | 27.2 (5 6 6) | 29.3 (98) | 25.6 (81) | 25.4 (1 3 5) | 28.2 (2 5 2) |
| 4 | 20.0 (4 1 5) | 15.5 (52) | 18.4 (58) | 22.6 (1 2 0) | 20.7 (1 8 5) |
| 5 | 14.9 (3 0 9) | 16.7 (56) | 11.7 (37) | 13.9 (74) | 15.9 (1 4 2) |
| Similarity | |||||
| 1 | 17.0 (3 5 3) | 19.9 (67) | 20.6 (65) | 16.9 (90) | 14.6 (1 3 1) |
| 2 | 17.2 (3 5 8) | 18.2 (61) | 17.8 (56) | 17.1 (91) | 16.8 (1 5 0) |
| 3 | 31.8 (6 6 0) | 32.1 (1 0 8) | 33.0 (1 0 4) | 30.8 (1 6 4) | 31.7 (2 8 4) |
| 4 | 21.3 (4 4 3) | 18.8 (63) | 17.5 (55) | 22.2 (1 1 8) | 23.1 (2 0 7) |
| 5 | 12.7 (264) | 11.0 (37) | 11.1 (35) | 13.0 (69) | 13.7 (1 2 3) |
| VHC attractiveness | |||||
| 1 | (1.9) 40 | 1.2 (4) | 1.9 (6) | 3.4 (18) | 1.3 (12) |
| 2 | (2.9) 60 | 2.1 (7) | 1.9 (6) | 3.4 (18) | 3.3 (29) |
| 3 | (43.0) 889 | 30.0 (1 0 0) | 38.3 (1 2 0) | 52.4 (2 7 8) | 43.9 (3 9 1) |
| 4 | (25.0) 516 | 23.1 (77) | 25.2 (79) | 25.6 (1 3 6) | 25.1 (2 2 4) |
| 5 | (27.2) 563 | 43.5 (1 4 5) | 32.6 (1 0 2) | 15.3 (81) | 26.4 (2 3 5) |
3.2. RQ1: Are rural identity and race associated with evaluation of VHC appearance?
RQ1 explored the relationship between rural identity and VHC appearance and whether participant race influenced this association (Table 3). Individuals with high rural identity rated the ALEX VHC as significantly more attractive (AOR = 1.12, CI = [1.02, 1.23], p =.02) compared to those with low rural identity; race did not have a significant influence on this effect (AOR = 1.19, CI = [0.99, 1.44], p =.07).
Table 3.
Effect sizes of rural identity, participant race, and VHC race-matching on VHC attractiveness.
| VHC Attractiveness |
||||
|---|---|---|---|---|
| Predictor Variable |
AOR |
95 % CI |
P* |
|
| Main Effects | Interactions | |||
| Overall Rural Identity | 1.12 | [1.02, 1.23] | 0.02 | |
| x Participant Race (White – ref) | 1.19 | [0.99, 1.44] | 0.07 | |
| x VHC Race-Matching (Not-matching – ref) | 1.91 | [1.02, 3.56] | 0.04 | |
| Belonging | 1.06 | [0.98, 1.16] | 0.15 | |
| x Participant Race (White – ref) | 1.22 | [1.03, 1.44] | 0.02 | |
| x VHC Race-Matching (Not-matching – ref) | 1.75 | [0.95, 3.21] | 0.07 | |
| Place identity | 1.09 | [1.00, 1.19] | 0.05 | |
| x Participant Race (White – ref) | 1.14 | [0.96, 1.35] | 0.13 | |
| x VHC Race-Matching (Not-matching – ref) | 1.78 | [0.96, 3.31] | 0.07 | |
| Self-concept | 1.12 | [1.01, 1.22] | 0.03 | |
| x Participant Race (White – ref) | 1.09 | [0.91, 1.32] | 0.33 | |
| x VHC Race-Matching (Not-matching – ref) | 2.22 | [1.27, 3.91] | 0.01 | |
| Similarity | 1.14 | [1.03, 1.26] | 0.01 | |
| x Participant Race (White – ref) | 1.20 | [0.98, 1.46] | 0.07 | |
| x VHC Race-Matching (Not-matching – ref) | 1.57 | [0.87, 2.83] | 0.13 | |
Abbreviation: VHC, virtual human clinician.
Note: The interactions with VHC race-matching are a within-race analysis among Black participants.
3.3. RQ2: Are rural identity and VHC race-matching associated with evaluations of VHC appearance among Black adults?
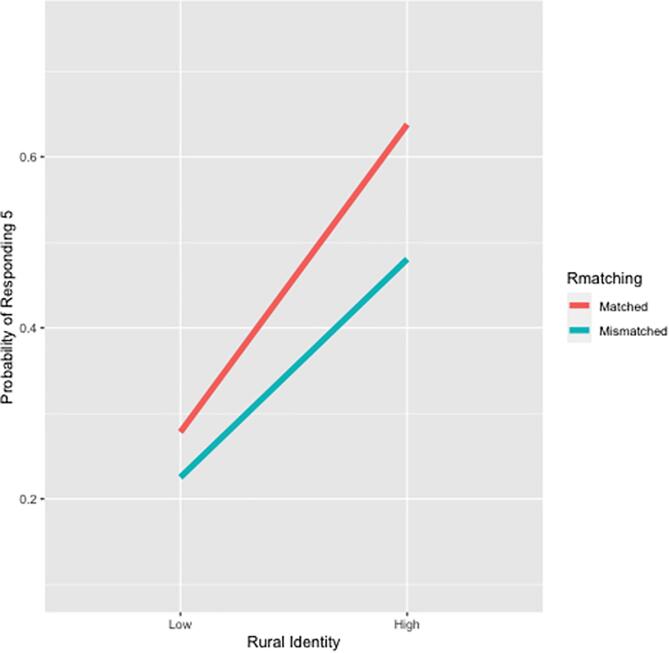
RQ2 considered whether the association between VHC race-matching and VHC attractiveness is affected by differences in rural identity among Black adults (Table 3). This interaction effect was statistically significant; for Black adults with high rural identity, being matched with a Black VHC was associated with higher attractiveness ratings (AOR = 1.91, [1.02, 3.56], p = 0.04). In other words, the odds of a 1 unit increase in perceived VHC attractiveness is 1.91 times larger than a 1 unit decrease in attractiveness for race-matched Black participants with high rural identity, compared to race-mismatched Black participants who also identify strongly with rurality (Fig. 2).
Fig. 2.
Interaction effect of virtual human clinician (VHC) race-matching and rural identity on evaluation of VHC attractiveness.
3.4. RQ3: How do the different dimensions of rural identity relate directly and intersect with race and VHC race-matching to influence evaluations of VHC appearance?
3.4.1. Main effects of identity and attractiveness
RQ3 assessed each item of the rural identity measure separately to explore whether these factors function differently (Table 3). Three of the four dimensions displayed a significant relationship with VHC attractiveness. Regardless of their race, participants with high perceived similarity with rural communities (AOR = 1.14, CI = [1.03, 1.26], p =.01) rated the VHC as more attractive. Also, a high rural self-concept (AOR = 1.12, CI = [1.01, 1.22], p =.03), and place identity (AOR = 1.09, CI = [1.00, 1.19], p =.05) with rural communities were positively associated with VHC attractiveness. Sense of belonging to a rural community had little effect (AOR = 1.06, CI = [0.98, 1.16], p =.15).
3.4.2. Identity and race interaction
However, the analysis revealed that rural belonging was important to VHC perceptions for Black participants, as those with a high sense of belonging rated the VHC more attractive than similar Whites (AOR = 1.22, CI = [0.95, 1.03, 1.44], p =.02).
3.4.3. Identity and race-matching interaction
Lastly, the influence of rural identity on the VHC race-matching effect among Black adults was significant for only one dimension of identity; matching Black participants with a Black VHC was a cue for increased attractiveness only when rural self-concept was high (AOR = 2.22, CI = [1.27, 3.91], p = 0.01).
4. Discussion
How a patient perceives the appearance of a health message source can influence credibility, and rural adults often rely on appearance cues to make judgments on trustworthiness. This study explored how differences in rural identity and related components influenced VHC appearance ratings. Participants with high rural identity rated the VHCs as more attractive, regardless of their race or VHC type. However, participant race had a meaningful effect when rural belonging was high, as Black adults with high belonging saw the VHCs as more attractive than Whites. Further, being matched with a Black VHC led to higher attractiveness ratings for Black adults with high rural identity. Yet, this relationship was more nuanced as only a high rural self-concept had a significant effect.
These findings support the importance of rural identity in user experience with VHC-delivered interventions and inform intervention tailoring. Also, the intersection of race and rural identity underscores the need to account for rural identity as part of efforts to address racial cancer health disparities. Appearance evaluations are critical in this digital context, given source attractiveness positively influences acceptance of cancer prevention messaging and colorectal cancer screening intentions (Baylor, 2009, Cooks et al., 2022, Liao et al., 2019, Patzer, 1983, Valinatajbahnamiri and Siahtiri, 2021). Therefore, it is imperative that digital colorectal cancer screening interventions targeting rural disparities allocate resources to develop culturally appropriate VHCs that optimize appearance.
4.1. Rural identity and VHC appearance
Regardless of the VHC they interacted with, individuals with a higher rural identity had more positive impressions of appearance. Prior work suggests rural adults prefer VHCs seen as calm and with a smiling and inviting face (Vilaro et al., 2021a). The current study suggests adults with high rural identity may be even more attuned to VHC appearance, possibly due to sociocultural norms for rurality that value virtual agents being similar to community members as a credibility indicator (Mendu et al., 2018). This finding could also result from intergroup categorization and identity priming through intervention engagement. Humans have many identities (e.g., ethnicity, class, religion) that cannot all be psychologically active, and high identification increases access to these identities; therefore, individuals with higher rural identity may be more easily primed to engage with this piece of their self-concept (Gaertner and Dovidio, 2000). A strong, salient rural identity would then contribute to VHC evaluations compatible with group norms.
4.2. Race, rural identity, and VHC appearance
Black adults face structural challenges such as access and cost that contribute to racial disparities in colorectal cancer screening (Geiger, 2003, Muthukrishnan et al., 2019), and for rural Black adults, these challenges are even more pronounced (Caldwell et al., 2016, James et al., 2017, Zahnd et al., 2021) , . VHCs offer a low-cost option for prevention education; this capacity to minimize screening challenges highlights the importance of developing tailored experiences for diverse populations.
In this study, Black participants with a higher sense of rural belonging rated the VHCs as more attractive. A strong sense of belonging creates strong bonds of trust and obligation (Hogg, 2010). It can be reasoned that shared negative experiences with rural healthcare systems (e.g., structural racism, discrimination) foster a strong sense of rural belonging among Black adults (Fowler-Brown et al., 2006, Hammonds and Reverby, 2019). More specifically, rural Black adults may attend more closely to VHC features such as clothing and perceived professionalism (Vilaro et al., 2021a). This differential effect based on race may be explained by the fact that identifying as both Black and rural represents two stigmatized identities, creating a novel intervention response.
4.3. VHC race-matching and VHC appearance
Rural identity also influenced VHC attractiveness ratings for Black participants matched with a Black VHC. Because social groups seek a positive self-image, they often rate other members more favorably (Hornsey et al., 2008). Therefore, Black adults may rate Black VHCs as more attractive given perceived similarity, an effect enhanced by increased rurality (Joyce and Harwood, 2014). Item analysis revealed that VHC race-matching for Black participants was a significant cue for attractiveness only when rural self-concept was high, suggesting racial concordance maybe even more important for these individuals. Response to lack of diversity in the medical workforce may also explain this finding (Winkfield et al., 2021); Black adults who see rural identity as central to who they are may rate Black VHCs as more attractive because of their novelty and presentation of a non-traditional source of medical information.
4.4. Strengths and limitations
Findings of this pilot study are building blocks to more precisely tailored VHC-led cancer screening interventions for rural adults. Given the established relationship between source attractiveness and message persuasiveness, the positive association between rural identity and VHC attractiveness implies screening interventions targeting rural adults should maximize the appearance of these conversational agents. Further, the fact that race concordance served as a strong cue for VHC attractiveness among Black adults with high rural identity suggests that race-matching is a vital intervention component for this group. Lastly, these findings provide a novel contribution to the study of VHC-led interventions by exploring the association between rural identity and perceived attractiveness across four factors of identity.
This study is not without limitations. A national panel was used for recruitment; these individuals may be more familiar with online platforms. However, online panels such as Qualtrics can recruit diverse samples for cancer research (Miller et al., 2020). It takes many years to fully disseminate a telehealth intervention, increasing the utility of piloting with early adopters. This pilot study aimed to explore patient experience with this intervention before moving into a clinical population. Also, given the use of a national panel, some participants may have increased access to technology. While over 70 % of rural communities have access to broadband service (Federal Communications Commission, 2020), there is a portion of this population that does not. As with all interventions, dissemination of Meet ALEX is not a one-size-fits-all approach.
Further, there are promising policies (e.g., the “ReConnect” program [usda.gov/broadband]) that will expand broadband in the United States, indicating the importance of identifying evidence-based interventions that are ready for broad deployment. Finally, a potential limitation is that rurality is a social construction and can be defined differently. Yet, the fact that these relationships with rural identity were found across a national sample suggests commonalities that inform intervention development.
5. Conclusion
This study is a next step in the line of research showing VHC appearance matters. With the COVID-19 pandemic disrupting cancer screening, there are significant opportunities to leverage VHCs to minimize challenges to screening uptake. VHC-led screening interventions to address rural disparities should invest adequate resources to maximize VHC appearance, particularly when targeting Black adults with an increased sense of belonging to a rural community. Further, VHC race-matching may be even more critical for Black adults who strongly identify with rurality, especially those with a greater rural self-concept. As the use of VHCs to deliver care grows, the examination of intergroup behavior in this context will only increase in importance. These findings resonate with the call to action for tailored strategies communicating the “why,” “when,” and “what” of colorectal cancer screening from preferred message sources. By focusing on the experiences of individuals highly identified with rurality, this study pushes the boundaries of our understanding of the role of group identity in VHC-led interventions.
Ethics. The study was approved by the University of Florida Institutional Review Board. Informed consent was obtained from all individual participants included in the study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Role of Funding Source
The research presented in this paper is that of the authors and does not reflect the official policy of the NIH.
Funding
This research was supported by the University of Florida Opportunity Seed Fund (PI: Krieger), a grant from the National Institutes of Health (R01CA207689; PI: Krieger), and a grant from the National Cancer Institute (T32CA257923; PI:Siemann). The study was approved by the University of Florida Institutional Review Board (#201801473) and the University of Florida Health Cancer Center Scientific Review and Monitoring Committee.
Footnotes
Participants assigned to the interactive VHC had higher intentions to screen and greater perceptions of VHC credibility. No main effects for VHC gender were found.
The current iteration of Meet ALEX can be customized on race only for Black and White patients. Future plans include additional research to test ALEX with an expanded patient population.
The recommended age for colorectal cancer screening was adjusted in May 2021 to include patients 45–49 years of age.
Separate models were analyzed for the composite rural identity score along with each of the four individual items.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2022.102034.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- American Cancer Society Colorectal Cancer Facts & Figures 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf
- Anderson A.E., Henry K.A., Samadder N.J., Merrill R.M., Kinney A.Y. Rural vs Urban Residence Affects Risk-Appropriate Colorectal Cancer Screening. Clinical Gastroenterology and Hepatology. 2013;11(5):526–533. doi: 10.1016/j.cgh.2012.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor A.L. Promoting motivation with virtual agents and avatars: role of visual presence and appearance. Philosophical Transactions of the Royal Society B: Biological Sciences. 2009;364(1535):3559–3565. doi: 10.1098/rstb.2009.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor A.L., Kim Y. International conference on intelligent tutoring systems. Springer; 2004. Pedagogical agent design: The impact of agent realism, gender, ethnicity, and instructional role; pp. 592–603. [Google Scholar]
- Bernardo B.M., Gross A.L., Young G., Baltic R., Reisinger S., Blot W.J., Paskett E.D. Predictors of Colorectal Cancer Screening in Two Underserved U.S. Populations: A Parallel Analysis. Frontiers in Oncology. 2018:230. doi: 10.3389/fonc.2018.00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickmore T.W., Pfeifer L.M., Jack B.W. Taking the Time to Care: Empowering Low Health Literacy Hospital Patients with Virtual Nurse Agents. In Proceedings of the SIGCHI conference on human factors in computing systems. 2009:1265–1274. [Google Scholar]
- Birmingham W.C., Hung M., Boonyasiriwat W., Kohlmann W., Walters S.T., Burt R.W., Kinney A.Y. Effectiveness of the extended parallel process model in promoting colorectal cancer screening. Psycho-Oncology. 2015;24(10):1265–1278. doi: 10.1002/pon.3899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brumbach B.H., Birmingham W.C., Boonyasiriwat W., Walters S., Kinney A.Y. Intervention mediators in a randomized controlled trial to increase colonoscopy uptake among individuals at increased risk of familial colorectal cancer. Annals of Behavioral Medicine. 2017;51(5):694–706. doi: 10.1007/s12160-017-9893-1. [DOI] [PubMed] [Google Scholar]
- Caldwell J.T., Ford C.L., Wallace S.P., Wang M.C., Takahashi L.M. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. American journal of public health. 2016;106(8):1463–1469. doi: 10.2105/AJPH.2016.303212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaiken S. Communicator physical attractiveness and persuasion. Journal of personality and social psychology. 1979;37(8):1387. [Google Scholar]
- Cialdini R.B. The science of persuasion. Scientific American. 2001;284(2):76–81. [Google Scholar]
- Cialdini R.B., Goldstein N.J. SOCIAL INFLUENCE: Compliance and Conformity. Annu. Rev. Psychol. 2004;55:591–621. doi: 10.1146/annurev.psych.55.090902.142015. [DOI] [PubMed] [Google Scholar]
- Federal Communications Commission. 2020 Broadband Deployment Report. Adopted April 20, 2020, released April 24, 2020, https://docs.fcc.gov/public/attachments/FCC-20-50A1.pdf.
- Cooks E.J., Duke K.A., Neil J.M., Vilaro M.J., Wilson-Howard D., Modave F., Krieger J.L. Telehealth and racial disparities in colorectal cancer screening: A pilot study of how virtual clinician characteristics influence screening intentions. Journal of clinical and translational science. 2022;6(1) doi: 10.1017/cts.2022.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler-Brown A., Ashkin E., Corbie-Smith G., Thaker S., Pathman D.E. Perception of racial barriers to health care in the rural South. Journal of Health Care for the Poor and Underserved. 2006;17(1):86–100. doi: 10.1353/hpu.2006.0022. [DOI] [PubMed] [Google Scholar]
- Gaertner S.L., Dovidio J.F. Psychology Press; Philadelphia PA: 2000. Reducing Intergroup Bias: The Common Ingroup Identity Model. [Google Scholar]
- Geiger H.J. In: Unequal treatment: Confronting racial and ethnic disparities in health care. Smedley B., Stith A., Nelson A., editors. National Academies Press; 2003. Racial and ethnic disparities in diagnosis and treatment: a review of the evidence and a consideration of causes; pp. 417–454. [PubMed] [Google Scholar]
- Griffin L., Lee D., Jaisle A., Carek P., George T., Laber E., Lok B., Modave F., Paskett E., Krieger J. Creating an mHealth app for colorectal cancer screening: user-centered design approach. JMIR human factors. 2019;6(2):e12700. doi: 10.2196/12700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammonds E.M., Reverby S.M. Toward a historically informed analysis of racial health disparities since 1619. American journal of public health. 2019;109(10):1348–1349. doi: 10.2105/AJPH.2019.305262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy, J., Wyche, S., & Veinot, T., 2019. Rural HCI research: Definitions, distinctions, methods, and opportunities. Proceedings of the ACM on Human-Computer Interaction, 3(CSCW), 1-33.
- Hawkins R.P., Kreuter M., Resnicow K., Fishbein M., Dijkstra A. Understanding tailoring in communicating about health. Health education research. 2008;23(3):454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henley S.J., Anderson R.N., Thomas C.C., Massetti G.M., Peaker B., Richardson L.C. Invasive cancer incidence, 2004–2013, and deaths, 2006–2015, in nonmetropolitan and metropolitan counties—United States. MMWR Surveillance Summaries. 2017;66(14):1. doi: 10.15585/mmwr.ss6614a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogg M.A. In: Trust in Risk Management. Siegrist M., Earle T.C., Gutscher H., editors. Routledge; 2010. Social identity and the group context of trust: Managing risk and building trust through belonging; pp. 67–87. [Google Scholar]
- Hornsey M.J., Robson E., Smith J., Esposo S., Sutton R.M. Sugaring the pill: Assessing rhetorical strategies designed to minimize defensive reactions to group criticism. Human communication research. 2008;34(1):70–98. [Google Scholar]
- Hung P., Deng S., Zahnd W.E., Adams S.A., Olatosi B., Crouch E.L., Eberth J.M. Geographic disparities in residential proximity to colorectal and cervical cancer care providers. Cancer. 2020;126(5):1068–1076. doi: 10.1002/cncr.32594. [DOI] [PubMed] [Google Scholar]
- James C.V., Moonesinghe R., Wilson-Frederick S.M., Hall J.E., Penman-Aguilar A., Bouye K. Racial/ethnic health disparities among rural adults—United States, 2012–2015. MMWR Surveillance Summaries. 2017;66(23):1. doi: 10.15585/mmwr.ss6623a1. https://www.cdc.gov/mmwr/volumes/66/ss/ss6623a1.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce N., Harwood J. Improving intergroup attitudes through televised vicarious intergroup contact: Social cognitive processing of ingroup and outgroup information. Communication Research. 2014;41(5):627–643. [Google Scholar]
- Kamran S.C., Winkfield K.M., Reede J.Y., Vapiwala N. Intersectional Analysis of US Medical Faculty Diversity over Four Decades. New England Journal of Medicine. 2022;386(14):1363–1371. doi: 10.1056/NEJMsr2114909. [DOI] [PubMed] [Google Scholar]
- Kreuter M.W., Lukwago S.N., Bucholtz D.C., Clark E.M., Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Education & Behavior. 2003;30(2):133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- Krieger J.L., Neil J.M., Duke K.A., Zalake M.S., Tavassoli F., Vilaro M.J., Wilson-Howard D.S., Chavez S.Y., Laber E.B., Davidian M. A pilot study examining the efficacy of delivering colorectal cancer screening messages via virtual health assistants. American journal of preventive medicine. 2021 doi: 10.1016/j.amepre.2021.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krok-Schoen J.L., Palmer-Wackerly A.L., Dailey P.M., Krieger J.L. The conceptualization of self-identity among residents of Appalachia Ohio. Journal of Appalachian Studies. 2015;21(2):229–246. [Google Scholar]
- Lengen C., Kistemann T. Sense of place and place identity: Review of neuroscientific evidence. Health & place. 2012;18(5):1162–1171. doi: 10.1016/j.healthplace.2012.01.012. [DOI] [PubMed] [Google Scholar]
- Liao G.-Y., Cheng T., Teng C.-I. How do avatar attractiveness and customization impact online gamers’ flow and loyalty? Internet Research. 2019 [Google Scholar]
- Lisetti C., Amini R., Yasavur U., Rishe N. I Can Help You Change! An Empathic Virtual Agent Delivers Behavior Change Health Interventions. ACM Trans. Manage. Inf. Syst. 2013;4(4):19:1–19:28. [Google Scholar]
- Loomans-Kropp H.A., Umar A. Cancer prevention and screening: the next step in the era of precision medicine. NPJ precision oncology. 2019;3(1):1–8. doi: 10.1038/s41698-018-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas G.M., Krämer N., Peters C., Taesch L., Mell J., Gratch J. Effects of Perceived Agency and Message Tone in Responding to a Virtual Personal Trainer. In Proceedings of the 18th International Conference on Intelligent Virtual Agents. 2018:247–254. [Google Scholar]
- McCroskey J.C., Teven J.J. Goodwill: A reexamination of the construct and its measurement. Communications Monographs. 1999;66(1):90–103. [Google Scholar]
- Mendu, S., Boukhechba, M., Gordon, J. R., Datta, D., Molina, E., Arroyo, G., ... & Barnes, L. E. (2018, May). Design of a culturally-informed virtual human for educating Hispanic women about cervical cancer. In Proceedings of the 12th EAI International Conference on Pervasive Computing Technologies for Healthcare, 360-366. [DOI] [PMC free article] [PubMed]
- Miller C.A., Guidry J.P., Dahman B., Thomson M.D. A Tale of Two Diverse Qualtrics Samples: Information for Online Survey Researchers A Tale of Two Diverse Qualtrics Samples. Cancer Epidemiology, Biomarkers & Prevention. 2020;29(4):731–735. doi: 10.1158/1055-9965.EPI-19-0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno C.C., Duszak R., Yee J., Horny M. Geographic dispersion and rural versus urban utilization of CT colonography in the United States. Journal of the American College of Radiology. 2020;17(4):475–483. doi: 10.1016/j.jacr.2019.10.002. [DOI] [PubMed] [Google Scholar]
- Muthukrishnan M., Arnold L.D., James A.S. Patients' self-reported barriers to colon cancer screening in federally qualified health center settings. Preventive medicine reports. 2019;15 doi: 10.1016/j.pmedr.2019.100896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohanian R. Construction and validation of a scale to measure celebrity endorsers' perceived expertise, trustworthiness, and attractiveness. Journal of advertising. 1990;19(3):39–52. [Google Scholar]
- Olafsson S., O’Leary T.K., Bickmore T.W. Motivating health behavior change with humorous virtual agents. In Proceedings of the 20th ACM international conference on intelligent virtual agents. 2020:1–8. [Google Scholar]
- Orlando J.F., Beard M., Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PloS one. 2019;14(8):e0221848. doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer-Wackerly A.L., Krok J.L., Dailey P.M., Kight L., Krieger J.L. Community engagement as a process and an outcome of developing culturally grounded health communication interventions: An example from the DECIDE project. American journal of community psychology. 2014;53(3):261–274. doi: 10.1007/s10464-013-9615-1. [DOI] [PubMed] [Google Scholar]
- Patzer G.L. Source credibility as a function of communicator physical attractiveness. Journal of business research. 1983;11(2):229–241. [Google Scholar]
- Polinski J.M., Kesselheim A.S., Frolkis J.P., Wescott P., Allen-Coleman C., Fischer M.A. A matter of trust: patient barriers to primary medication adherence. Health Education Research. 2014;29(5):755–763. doi: 10.1093/her/cyu023. [DOI] [PubMed] [Google Scholar]
- Provoost S., Lau H.M., Ruwaard J., Riper H. Embodied conversational agents in clinical psychology: a scoping review. Journal of medical Internet research. 2017;19(5):e151. doi: 10.2196/jmir.6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qazimi S. Sense of place and place identity. European Journal of Social Science Education and Research. 2014;1(1):306–310. [Google Scholar]
- R Core Team, 2018. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/.
- Ratcliffe M., Burd C., Holder K., Fields A. Defining rural at the US Census Bureau. American community survey and geography brief. 2016;1(8) [Google Scholar]
- Rogers C.R., Moore J.X., Qeadan F., Gu L.Y., Huntington M.S., Holowatyj A.N. Examining factors underlying geographic disparities in early-onset colorectal cancer survival among men in the United States. American journal of cancer research. 2020;10(5):1592. [PMC free article] [PubMed] [Google Scholar]
- Shen M.J., Peterson E.B., Costas-Muñiz R., Hernandez M.H., Jewell S.T., Matsoukas K., Bylund C.L. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. Journal of racial and ethnic health disparities. 2018;5(1):117–140. doi: 10.1007/s40615-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltzfus J.C. Logistic regression: a brief primer. Academic emergency medicine. 2011;18(10):1099–1104. doi: 10.1111/j.1553-2712.2011.01185.x. [DOI] [PubMed] [Google Scholar]
- Street R.L., O’Malley K.J., Cooper L.A., Haidet P. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. The Annals of Family Medicine. 2008;6(3):198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tajfel H. Individuals and groups in social psychology. British Journal of Clinical Psychology. 1979;18(2):183–190. [Google Scholar]
- ter Stal S., Tabak M., op den Akker, H., Beinema, T., & Hermens, H. Who do you prefer? The effect of age, gender and role on users’ first impressions of embodied conversational agents in eHealth. International Journal of Human-Computer Interaction. 2020;36(9):881–892. [Google Scholar]
- Twigger-Ross C., Bonaiuto M., Breakwell G. In: Psychological Theories for Environmental Issues. Bonnes M., Lee T., Bonaiuto M., editors. Routledge; 2003. Identity theories and environmental psychology; pp. 203–233. [Google Scholar]
- Thornton R.L.J., Powe N.R., Roter D., Cooper L.A. Patient–physician social concordance, medical visit communication and patients’ perceptions of health care quality. Patient education and counseling. 2011;85(3):e201–e208. doi: 10.1016/j.pec.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valinatajbahnamiri M., Siahtiri V. Flow in computer-mediated environments: A systematic literature review. International Journal of Consumer Studies. 2021 [Google Scholar]
- Vilaro M.J., Wilson-Howard D.S., Griffin L.N., Tavassoli F., Zalake M.S., Lok B.C., Modave F.P., George T.J., Carek P.J., Krieger J.L. Tailoring virtual human-delivered interventions: A digital intervention promoting colorectal cancer screening for Black women. Psycho-Oncology. 2020;29(12):2048–2056. doi: 10.1002/pon.5538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilaro M.J., Wilson-Howard D.S., Neil J.M., Tavassoli F., Zalake M.S., Lok B.C., Modave F.P., George T.J., Odedina F.T., Carek P.J. A Subjective Culture Approach to Cancer Prevention: Rural Black and White Adults’ Perceptions of Using Virtual Health Assistants to Promote Colorectal Cancer Screening. Health Communication. 2021:1–12. doi: 10.1080/10410236.2021.1910166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilaro M.J., Wilson-Howard D.S., Zalake M.S., Tavassoli F., Lok B.C., Modave F.P., George T.J., Odedina F., Carek P.J., Krieger J.L. Key changes to improve social presence of a virtual health assistant promoting colorectal cancer screening informed by a technology acceptance model. BMC medical informatics and decision making. 2021;21(1):1–9. doi: 10.1186/s12911-021-01549-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson-Howard D., Vilaro M.J., Neil J.M., Cooks E.J., Griffin L.N., Ashley T.T.…Krieger J.L. Development of a Credible Virtual Clinician Promoting Colorectal Cancer Screening via Telehealth Apps for and by Black Men: Qualitative Study. JMIR Formative Research. 2021;5(12) doi: 10.2196/28709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkfield K.M., Levit L.A., Tibbits M., Melnick E., Schenkel C., Kirkwood K., Green S., Pierce L. Addressing equity, diversity, and inclusion of Black physicians in the oncology workforce. JCO Oncology Practice. 2021;17(5):224–226. doi: 10.1200/OP.21.00079. [DOI] [PubMed] [Google Scholar]
- Zahnd W.E., Murphy C., Knoll M., Benavidez G.A., Day K.R., Ranganathan R., Eberth J.M. The intersection of rural residence and minority race/ethnicity in cancer disparities in the United States. International Journal of Environmental Research and Public Health. 2021;18(4):1384. doi: 10.3390/ijerph18041384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalake M., Tavassoli F., Duke K., George T., Modave F., Neil J., Krieger J., Lok B. Internet-based tailored virtual human health intervention to promote colorectal cancer screening: design guidelines from two user studies. Journal on Multimodal User Interfaces. 2021:1–16. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.