Abstract
Objectives
To assess changes in duration, timing, and social jetlag in adolescent sleep during the COVID-19 pandemic and evaluate the impact of mood, physical activity, and social interactions on sleep.
Study Design
An online survey queried adolescents’ sleep before (through retrospective report) and during the initial phase of COVID-19 in May 2020. Adolescents (N = 3,494), 13–19 years old, in the United States (U.S.) answered questions about their current and retrospective (prior to COVID-19) sleep, chronotype, mood, and physical and social activities. Linear regression models were fit for time in bed, reported bed and wake times, and social jetlag during COVID-19, accounting for pre-COVID-19 values.
Results
Total reported time in bed (a proxy for sleep duration) increased on weekdays by an average of 1.3 ± 1.8 hours (p < 0.001) during COVID-19, compared to retrospective report of time in bed prior to COVID-19. During COVID-19, 81.3% of adolescents reported spending 8 hours or more in bed on weekdays compared to only 53.5% prior to COVID-19. On weekdays, bedtimes were delayed on average by 2.5 hours and wake times by 3.8 hours during COVID-19 compared to prior to COVID-19. On weekends, bedtimes were delayed on average by 1.6 hours and waketimes by 1.5 hours (all p’s < 0.001). Social jetlag of > 2 hours decreased to 6.3% during COVID-19 compared to 52.1% prior to COVID-19. Anxiety and depression symptoms and a decline in physical activity during COVID-19 were associated with delayed bed and wake times during COVID-19.
Conclusions
During COVID-19, adolescents reported spending more time in bed, with most adolescents reporting 8 hours of sleep opportunity and more consistent sleep schedules. As schools return to in-person learning, additional research should examine how sleep schedules may change due to school start times and what lessons can be learned from changes that occurred during COVID-19 that promote favorable adolescent sleep.
Keywords: circadian rhythm, sleep timing, adolescents, pediatrics, COVID-19
Introduction
The COVID-19 pandemic significantly disrupted routines and schedules for both youth and adults but the impact on sleep in United States (U.S.) adolescents is not fully known. Adolescence is a developmental period marked by multiple biological, environmental, and social factors contributing to high rates of insufficient and delayed sleep (Crowley, Wolfson, Tarokh, & Carskadon, 2018). According to Youth Risk Behavior survey data pre-pandemic, 75% of 12th grade students reported obtaining < 8 hours of sleep per night and up to 25% report < 6 hours of sleep per night (Centers for Disease Control and Prevention, 2019) As evidence is emerging about the impacts of a pandemic on sleep, it has been posited that the COVID-19 pandemic may have both positive and negative effects on adolescents’ sleep (Becker & Gregory, 2020; Stearns, Ievers-Landis, McCrae, & Simon, 2021).
School closures and the implementation of virtual learning during the early months of the pandemic caused changes to school start times and academic demands for many adolescents. Many high schools in the U.S. have start times prior to 8:30AM, which, in combination with a physiological delay in circadian rhythms that results in later sleep onset, limits sleep opportunity for adolescents (Adolescent Sleep Working Group, Committee on Adolescence, & Council on School Health, 2014; Crowley et al., 2018). Additionally, this can create an increase in social jetlag, defined as a > 2-hour difference in sleep timing from weekdays to weekends, which may result in daytime tiredness or fatigue (Mindell & Owens, 2015). In adolescence, this often looks like going to bed later and waking up later on weekends compared to weekdays. A shift to a more flexible or delayed school schedule may provide the opportunity for adolescents, particularly those with an evening chronotype, or later sleep timing preference, to obtain significantly more sleep and reduce social jetlag (Becker & Gregory, 2020). Indeed, in a Canadian study of qualitative phone interviews during COVID-19, adolescents reported increased sleep duration (primarily due to later wake times), improved sleep quality, and less daytime sleepiness (Gruber, Saha, Somerville, Boursier, & Wise, 2020). Adolescents attributed these changes to not having to wake at a set time to attend school and reduced school stress (Gruber et al., 2020).
Overall, results from adolescent- and parent-reported online surveys and qualitative interviews consistently report sleep duration increased and bed/wake times delayed during COVID-19 compared to retrospective reports prior to COVID-19 (Bruni et al., 2021; Illingworth, Mansfield, Espie, Fazel, & Waite, 2022; Lim et al., 2021; López-Bueno et al., 2020; Lu et al., 2020; Meltzer, Saletin, et al., 2021; Zhou et al., 2020). Across studies, risk factors for poor sleep (elevated insomnia symptoms, delayed sleep/wake schedule) included depression and anxiety symptoms, including COVID-19 specific sadness, fears, and worries (Becker et al., 2021; Bruni et al., 2021; Lim et al., 2021; López-Bueno et al., 2020; Lu et al., 2020; Zhou et al., 2020). Factors associated with better sleep included physical activity and social support (Becker et al., 2021; Bruni et al., 2021; Lim et al., 2021; López-Bueno et al., 2020; Lu et al., 2020; Zhou et al., 2020). However, many of these studies are limited by reliance on parent report rather than direct adolescent report, mixed quality of the measures used to assess sleep, and comparison of assessments taken during COVID-19 to other samples evaluated prior to the pandemic.
While COVID-19 likely led to improved sleep opportunity and duration for adolescents, other factors such as increased mood symptoms, decreased social support and reduced physical activity may have negatively impacted sleep in adolescents during COVID-19. Pandemic-related stress and social isolation may increase anxiety and depression symptoms; social distancing measures and limited extracurricular activities may reduce social interactions with peers; and closures of sports teams and restrictions on use of outdoor spaces may have reduced physical activity of adolescents. Two online surveys of adolescents and young adults in China found high rates of insomnia symptoms in respondents during the COVID-19 pandemic, with depression and anxiety symptoms being risk factors for sleep disturbance (Lu et al., 2020; Zhou et al., 2020). However, no prior studies have evaluated risk and protective factors for multiple dimensions of sleep in a large sample of U.S. adolescents.
The objectives of the current study were to: 1) examine changes in time in bed, sleep timing, and social jetlag during the COVID-19 pandemic compared to pre-COVID-19 sleep; and 2) evaluate the impact of mood, sleep timing preference, insomnia symptoms, physical activity, and social interactions during COVID-19 as they relate to time in bed, bed and wake times, and social jetlag during the COVID-19 pandemic. We hypothesized that adolescents would report longer time in bed, delayed bed and wake times, and have reduced social jetlag during COVID-19 compared to pre-COVID-19. Additionally, we hypothesized that increased physical activity and social interactions during COVID-19 would be protective for sleep (increased time in bed and reduced social jetlag), while greater mood symptoms would be a risk factor for unfavorable sleep (shorter time in bed and greater social jetlag).
Methods
An online self-report survey was completed by U.S. high school students between the ages of 13- and 19-years old. Adolescents were recruited through social media ads on Facebook during a two-week period in May 2020. The ads linked to a description of the study and a screening and consent page on the Research Electronic Data Capture (REDCap; (Harris et al., 2009) platform through the University of Colorado Denver. Participants answered several screening questions and if they met inclusion criteria and provided informed consent (if over age 18) or assent, attesting to parent/guardian permission to participate (if under age 18) then participants completed the survey electronically. If participants did not provide consent or assent to participate or did not meet inclusion criteria, they were redirected to a page informing them they were not eligible to take the survey and thanking them for their time. Participants were allowed to opt out of any item and withdraw from the survey at any time. No compensation was provided. Study procedures were consistent with the Colorado Multiple Institutional Review Board guidelines and IRB approval was obtained prior to adolescent participation and completion of study measures.
The survey used a combination of previously validated measures and items derived by the authors for the purpose of the study to assess sleep (time in bed, timing, and social jetlag), mood, and behaviors currently (during the COVID-19 pandemic) and retrospectively (prior to COVID-19). Participants were asked to complete a range of measures based on their current functioning during the COVID-19 pandemic and to think retrospectively on their functioning before the COVID-19 pandemic began. Specifically, participants were asked to report their bedtime and waketime on weekdays and weekends currently and prior to COVID-19, which was used to describe sleep timing. Time in bed was calculated as the difference between bed and wake times and was used as a proxy for sleep duration. This is a common approach utilized in pediatric sleep research (Paruthi et al., 2016). Social jetlag was calculated as the difference between weekend and weekday midpoints. Social jetlag of > 2 hours was used as a cut off based on commonly reported oversleep in adolescents and previous research indicating healthy sleepers have variability of 60 minutes or less in their sleep times and regularity in sleep contributes to overall sleep health (DeSantis et al., 2019, Mindell & Owens, 2015; Okun et al., 2011). Sleep midpoints were calculated as the midpoint between reported bedtime and waketime.
The Pediatric Insomnia Severity Index (PISI) (Byars, Simon, Peugh, & Beebe, 2017) was used to assess insomnia symptoms both currently (during COVID-19) and retrospectively (prior to COVID-19). Items are rated on a 6-point scale from 0 = never to 5 = always and higher scores indicate more problems with sleep. Chronotype, assessed during COVID-19 only, was evaluated with the Morningness/Eveningness Scale for Children (MESC) (Carskadon, Vieira, & Acebo, 1993). Scores range from 10–42 with higher scores indicating greater morningness preference. MESC scores were categorized into eveningness, morningness, and intermediate preference for descriptive purposes. A MESC score of ≤ 23 indicates evening preference, ≥ 24 and ≤ 27 indicates intermediate preference, and ≥ 28 indicates a morning preference (Díaz-Morales, 2015). Current anxiety and depression symptoms during COVID-19 were measured with the PROMIS Anxiety and Depression short form measures (Irwin et al., 2012). Each item is rated on a 5-point scale based on symptoms over the past week and raw scores are summed and converted to T-scores. Descriptive categories were defined by the PROMIS developers, with T-scores of 50 and below described as “within normal limits,” 50–55 as “mild,” 55–65 as “moderate,” and 65 and above as “severe” (Northwestern University, 2020).
Participants were asked to estimate whether their participation in various activities either increased, decreased, or stayed the same during COVID-19 compared to pre-COVID-19 (e.g., physical activity, social interactions, electronics use, time in bed during the day). Demographic information (e.g., age, gender identity, race/ethnicity), school participation (e.g., grade, in-person vs virtual), and current local COVID-19 prevention measures (e.g., stay-at-home orders) were queried. To determine socioeconomic status, participants were asked to provide their zip code and this was categorized according to the Economic Innovation Group’s Distressed Communities Index (DCI; www.eig.org/dci). The complete questionnaire is available in Appendix A.
Analyses
Self-reported demographic, clinical, and sleep characteristics were summarized using frequencies and percentages for categorical variables and means with standard deviations. Difference in sleep outcomes from pre-COVID-19 to during COVID-19 were assessed using paired t-test, with effect sizes calculated as the mean difference divided by the standard deviation of the difference. McNemar’s tests were used to compare pre- and during COVID-19 proportions of subjects who had time in bed ≥ 8 hours, social jetlag > 2 hours, bedtimes after midnight, and wake times before 7:00 AM.
Separate linear regression models were fit for each sleep outcome during COVID-19 (time in bed on weekdays and weekends, bedtimes on weekdays and weekends, wake times on weekdays and weekends, and social jetlag). For each of the outcomes, three models were fit including three different sets of variables: 1) change in physical activity and social interactions (self-reported as either an increase or same amount versus a decrease or never participating in the activity from pre-COVID to during COVID-19) and PISI score during COVID-19, 2) MESC score during COVID-19 and school type during COVID-19 (self-reported as either in-person or not in-person), and 3) depression and anxiety diagnoses and current PROMIS score categories (categorized as Severe versus Moderate or below). The groupings of variables were chosen based on clinical reasoning. For each of the 21 models fit, the self-reported baseline (pre-COVID-19) sleep outcome variable was included in the model as a covariate. For a given model, only individuals with complete data specific to that model were included. As a measure of effect size, partial R2 attributable to each sleep outcome variable are reported for each model.
A significance level of 0.05 was used to determine statistical significance. Data were visualized using boxplots. Data cleaning, analysis, and visualization was done in RStudio (version 2021.09.0.351, R version 4.1.2) (RStudio Team, 2020).
Results
Participant Characteristics
A total of 7,186 survey responses were received. Of those, 1,099 did not agree to consent for the study, and 854 did not meet age requirements and thus did not go on to answer survey questions. Additionally, 1,739 responses were excluded due to missing answers for bed and wake times, which are required to calculate the sleep variables. Data from a total of 3,494 adolescents with average age 16.2 ± 1.1 years old from 48 states in the U.S. were analyzed (see Table 1). Most participants identified as female (65.4%) and White (72.7%). Twenty-seven percent of respondents came from at-risk or distressed communities based on the DCI. Prior to COVID-19 shutdowns, 94.9% of participants reported attending a traditional, in-person high school, with the remainder attending online school, home-school, or another type of school. During COVID-19, 80.7% of participants reported their local community was on stay-at-home orders and only 7.3% stated they were still attending in person school.
Table 1.
Participant Demographic and Clinical Characteristics at Time of Survey Response
| N=3,494 | |
|---|---|
| Gender | |
| Female | 2,029 (65.4%) |
| Male | 905 (29.2%) |
| Other | 167 (5.4%) |
| Race | |
| American Indian or Alaska Native | 26 (0.744%) |
| Asian | 69 (1.97%) |
| Black | 47 (1.35%) |
| More than one race | 369 (10.6%) |
| Native Hawaiian or Pacific Islander | 2 (0.0572%) |
| Unknown | 442 (12.7%) |
| White | 2539 (72.7%) |
| Ethnicity (% Hispanic) | 331 (9.5%) |
| Age (M±SD) | 16.24 ± 1.09 |
| Reported Diagnosis of Depression | 1162 (33.3%) |
| Reported Diagnosis of Anxiety | 1399 (40.0%) |
| PROMIS Depression T-score (M±SD) | 64.37 ±11.48 |
| PROMIS Depression Categories | |
| Moderate and Below (T-score < 65) | 1494 (47.4%) |
| Severe (T-score > 65) | 1660 (52.6%) |
| PROMIS Anxiety T-score (M±SD) | 57.85 ±13.50 |
| PROMIS Anxiety Categories | |
| Moderate and Below (T-score < 65) | 2165 (68.6%) |
| Severe (T-score > 65) | 990 (31.4%) |
| MESC Score (M±SD) | 21.08 ±5.37 |
| MESC Categories | |
| Morning Type (MESC ≥ 28) | 803 (25.7%) |
| Evening Type (MESC ≤ 23) | 1551 (49.7%) |
| Intermediate Type (24 ≤ MESC ≤ 27) | 768 (24.6%) |
| PISI Score (M±SD) | |
| Before COVID-19 | 11.69 (5.91) |
| During COVID-19 | 13.71 (6.68) |
| School Type Pre-COVID-19 | |
| In-person | 3317 (94.9%) |
| Online | 88 (2.5%) |
| Home-school | 68 (1.9%) |
| Other | 21 (0.6%) |
| DCI Quantiles | |
| Prosperous | 1024 (32.5%) |
| Comfortable | 712 (22.6%) |
| Mid-Tier | 564 (17.9%) |
| At-Risk | 535 (17.0%) |
| Distressed | 320 (10.1%) |
Note: PROMIS T-scores have a mean of 50 and SD of 10. T-scores of 50 and below = within normal limits, 50–55 = mild, 55–65 = moderate, and 65 and above = severe. DCI, Distressed Communities Index; MESC, Morningness Eveningness Scale for Children, scores range from 10–42, a score of ≤ 23 indicates evening preference, ≥ 24 and ≤ 27 indicates intermediate, and ≥ 28 indicates a morning preference; PISI, Pediatric Insomnia Severity Index, range 0–30, higher scores indicate greater insomnia symptoms.
Half of respondents endorsed an Evening chronotype (49.7%). During COVID-19, half of participants (52.6%) endorsed PROMIS Depression scores in the Severe range (M=64.37 ±11.48), and one-third (31.4%) endorsed PROMIS Anxiety scores in the Severe range (M=57.85 ±13.50). During COVID-19, two-thirds (66.9%) of participants endorsed spending no time or less time engaging in social interactions and half (52.2%) reported engaging in no physical activity or less physical activity compared to before COVID-19.
Change in Time in Bed
During COVID-19, total reported time in bed increased on weekdays by an average of 1.35 ± 1.78 hours (p < 0.001) and decreased on weekends by an average of 0.18 ± 1.76 hours (p < 0.001) compared to retrospective report of before COVID-19 (see Table 2). Prior to COVID-19, 53.5% of adolescents reported more than 8 hours of sleep per night on weekdays and 88.2% on weekends, and this increased to 81.3% on weekdays and stayed relatively consistent at 82% on weekends during COVID-19 (both p’s < 0.001).
Table 2.
Change in Sleep Variables from Pre-COVID to During COVID-19
| Before COVID-19 | During COVID-19 | Change | Effect Size | p-value | |
|---|---|---|---|---|---|
| Bedtime | |||||
| Weekday | 10:37 PM (1.11) | 1:10 AM (2.10) | 2.51 (1.91) hours | 1.32 | < 0.001 |
| Weekend | 12:07 AM (1.42) | 1:46 AM (2.10) | 1.65 (1.79) hours | 0.93 | < 0.001 |
| Waketime | |||||
| Weekday | 6:24 AM (0.97) | 10:18 AM (2.34) | 3.85 (2.40) hours | 1.60 | < 0.001 |
| Weekend | 9:27 AM (1.55) | 10:56 AM (2.30) | 1.47 (2.07) hours | 0.72 | < 0.001 |
| Sleep Duration (hours) | |||||
| Weekday | 7.79 (1.08) | 9.13 (1.66) | 1.35 (1.78) hours | 0.75 | < 0.001 |
| Weekend | 9.34 (1.40) | 9.17 (1.67) | −0.18 (1.76) hours | −0.10 | < 0.001 |
| Social Jetlag (hours) | 2.23 (1.11) | 0.62 (0.98) | −1.61 (1.33) hours | −1.21 | < 0.001 |
Note: Means with Standard Deviations are used to summarize continuous data and compared using a paired t-test.
Change in Bedtimes
During COVID-19, bedtimes were delayed on weekdays by an average of 2.51 ± 1.91 hours (p < 0.001) and on weekends by 1.65 ± 1.79 hours (p < 0.001) compared to retrospective report of before COVID-19 (see Table 2 and Figure 1). Prior to COVID-19, 5.7% of adolescents reported a bedtime after midnight on weekdays and 37.2% on weekends, and this increased to 60.6% on weekdays and 71.6% on weekends during COVID-19 (both p’s < 0.001).
Figure 1.
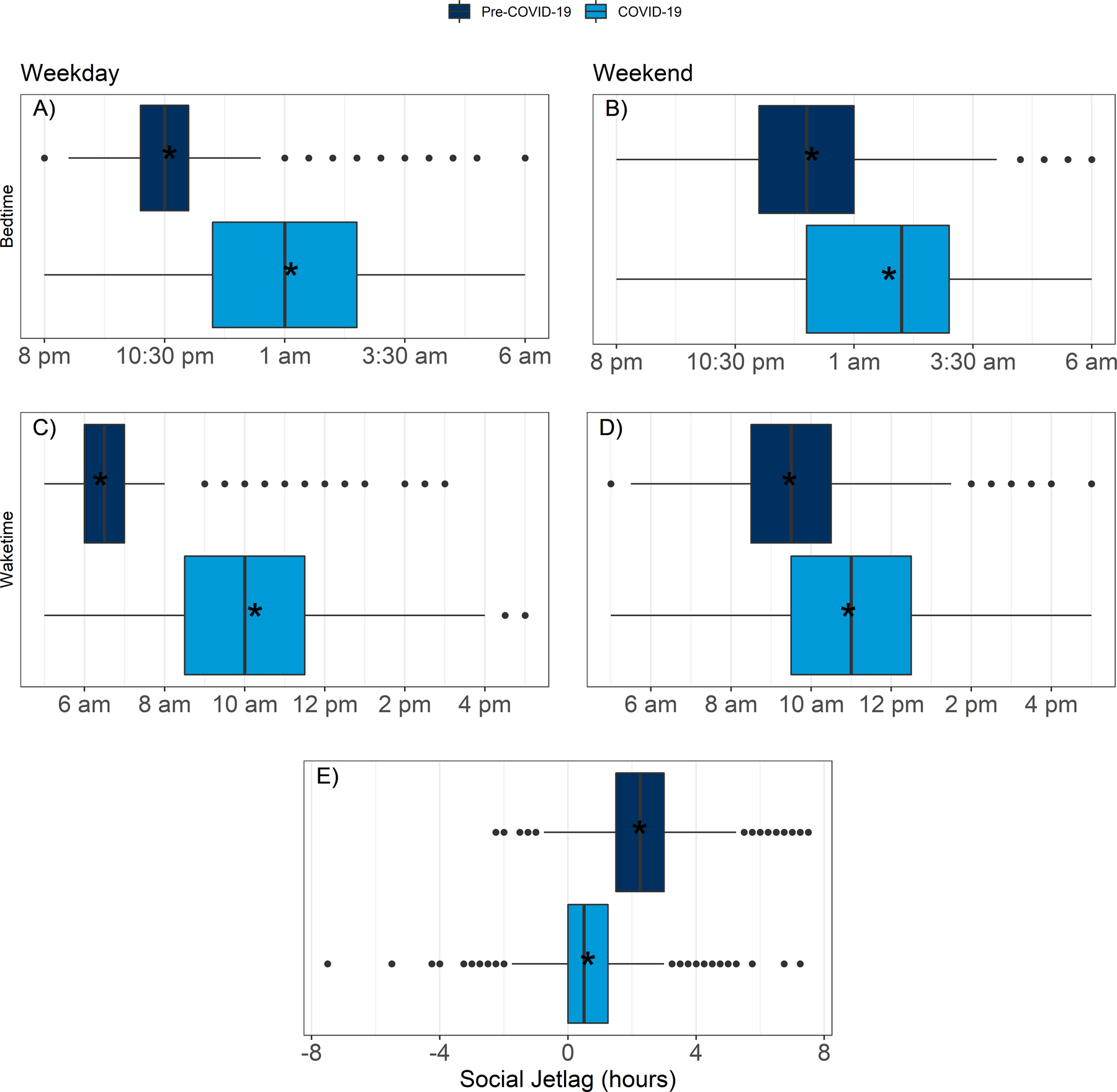
Bed and wake times during COVID-19 and before COVID-19 on weekdays and weekends. Box plots represent medians and first and third quartiles of bed and wake times with outliers expressed as dots. Mean times are expressed as stars. Bedtimes were delayed on weekdays by 2.51 ± 1.91 hours (A) and weekends and by 1.65 ± 1.79 hours (B) during COVID-19 (light grey) compared to pre-COVID-19 (dark grey; all p’s < 0.001). Waketimes were delayed on weekdays by 3.85 ± 2.40 hours (C) and weekends and by 1.47 ± 2.07 hours (D) during COVID-19 (light grey) compared to pre-COVID-19 (dark grey; all p’s < 0.001). Social jetlag during COVID-19 and before COVID-19. Social jetlag was calculated as the difference in sleep times on weekends and weekdays. Box plots represent medians and first and third quartiles of bed and wake times with outliers expressed as dots. Mean times are expressed as stars. Social jetlag was 2.2 ± 1.1 hours pre-COVID-19 (dark grey), and this decreased to 0.6 ± 0.9 hours on average during COVID-19 (light grey; p < 0.001).
Change in Waketimes
During COVID-19, waketimes were delayed on weekdays by 3.85 ± 2.40 hours (p < 0.001) and on weekends by 1.47 ± 2.07 hours (p < 0.001) during COVID-19 compared to retrospective report of before COVID-19 (see Table 2 and Figure 1). Prior to COVID-19, 73.2% of adolescents reported a waketime before 7:00 AM on weekdays and 3.2% on weekends, and this decreased to 4.4% on weekdays (p < 0.001) and 2.7% on weekends (p = 0.12) during COVID-19.
Change in Social Jetlag
Prior to COVID-19, 52.1% of adolescents retrospectively endorsed social jetlag >2 hours, which decreased to 6.3% during COVID-19 (p < 0.001). During COVID-19, social jetlag was reduced to an average of 0.6 ± 0.98 hours from 2.2 ± 1.1 hours before COVID-19 (p < 0.001) (see Table 2 and Figure 1).
Factors Associated with Changes in Time in Bed, Sleep Timing, and Social Jetlag
Change in Physical Activity, Social Interactions, and PISI Scores.
Models were fit for each sleep variable based on the following predictors: change in physical activity, change in social interactions, and PISI scores, controlling for pre-COVID-19 sleep.
Physical Activity.
Adolescents who reported no physical activity or a decrease in physical activity during COVID-19 had an estimated shift in bedtime of 24 minutes later (95% CI: 16.5, 31.6, p < 0.001) during weekdays and 25.3 minutes later during weekends (95% CI: 18.3, 32.3, p < 0.001), compared to those engaging in the same or more physical activity during COVID-19 (Tables B.1 and B.2). Similarly, adolescents who reported no physical activity or a decrease in physical activity during COVID-19 had an estimated shift in waketime of 31 minutes later (95% CI: 21.8, 40.2, p < 0.001) during the weekdays and 28.8 minutes later during the weekends (95% CI: 20.8, 36.7, p < 0.001), compared to those engaging in the same or more physical activity during COVID-19 (Tables B.7 and B.8). Change in physical activity was not significantly associated with change in time in bed or change in social jetlag (Tables B.13, B.14, and B.19).
Social Interactions.
Adolescents who reported no social interactions or a decrease in social interactions during COVID-19 had an estimated shift in waketime of 10 minutes later (95% CI: −19.8, −0.3, p-value = 0.44) on weekdays (Table B.7). Change in social interactions was not significantly associated with bedtime, weekend waketime, time in bed, or social jetlag during COVID-19 (Tables B.1, B.2, B.8, B.13, B.14, and B.19).
PISI Score.
During COVID-19, PISI scores were significantly higher by 2.06 ± 6.06 points, indicating greater insomnia symptoms compared to retrospective report prior to COVID-19 (p < 0.001) (see Table 1). For each 1-point increase in current PISI score during COVID-19, indicating greater insomnia symptoms, bedtime was delayed by 1.4 minutes (95% CI: 0.8, 1.9, p-value < 0.001) on weekdays and 1.6 minutes (95% CI: 1.1, 2.2, p-value < 0.001) on weekends (Tables B.1 and B.2). Similarly, during COVID-19 waketimes were delayed by 1.3 minutes (95% CI 0.6, 2, p-value < 0.001) on weekdays and 1.9 minutes (95% CI: 1.3, 2.5, p-value < 0.001) on weekends (Tables B.7 and B.8). An increase in PISI score during COVID-19 was significantly associated with greater during COVID-19 social jetlag, but only by 0.5 minutes (95% CI: 0.2, 0.8, p-value = 0.001) (Table B.19). PISI score during COVID-19 was not significantly associated with time in bed during COVID-19 while adjusting for change in physical activity, change in social interactions, and pre-COVID-19 time in bed (Tables B.13 and B.14).
Anxiety and Depression Symptoms and Diagnoses.
Models were fit for each sleep variable based on the following predictors: PROMIS Anxiety and Depression score categories and anxiety and depression diagnoses, controlling for pre-COVID-19 sleep.
Anxiety Symptoms.
Adolescents who scored in the Severe range on the PROMIS Anxiety scale during COVID-19 had a delay in weekday bedtimes by an estimated 15.9 minutes (95% CI: 6.2, 25.5, p-value = 0.001) and weekend bedtimes by 15.2 minutes (95% CI: 6.2, 24.2, p-value = 0.001) compared to adolescents with Moderate or below levels of anxiety (Tables B.3 and B.4). A score in the Severe range on the PROMIS Anxiety measure was associated with a delay in waketime of 14.7 minutes on weekends (95% CI: 4.4, 25, p = 0.005), but there was no statistically significant change on weekdays (p-value = 0.286) (Tables B.9 and B.10). Anxiety PROMIS score was not significantly associated with time in bed or social jetlag during COVID-19 (Tables B.15, B.16, and B.20).
Depression Symptoms.
Participants with a score in the Severe range on the PROMIS Depression scale during COVID-19 delayed their weekday bedtimes by an estimated 21.8 minutes (95% CI: 12.8, 30.8, p-value < 0.001) and their weekend bedtimes by 21.6 minutes (95% CI: 13.1, 30, p-value < 0.001) compared to adolescents with Moderate or below levels of depression (Tables B.3 and B.4). Adolescents who scored in the Severe range on the PROMIS Depression measure had a greater delay in wake time on weekdays by an estimated 19.8 minutes (95% CI: 8.7, 30.9, p < 0.001) and weekends by 23.8 minutes (95% CI: 14.1, 33.5, p < 0.001) compared to those in the Moderate or below range (Tables B.9 and B.10). Depression PROMIS score was not significantly associated with time in bed or social jetlag during COVID-19 (Tables B.15, B.16, and B.20).
Anxiety and Depression Diagnoses.
A diagnosis of depression prior to COVID-19 was associated with a greater delay in wake time on weekdays during COVID-19 by an estimated 15.1 minutes (95% CI: 1.1, 29, p = 0.034) compared to those without a prior diagnosis of depression (Table B.9). A diagnosis of anxiety was significantly associated with an estimated increase in weekday time in bed of 9.7 minutes during COVID-19 (95% CI: 0.2, 19.1, p-value = 0.045) (Table B.15).
MESC Score.
Models were fit to predict each sleep variable based on MESC score during COVID-19, adjusting for school type during COVID-19 (in-person or online) and pre-COVID-19 sleep. For every 1-point increase in the MESC score (indicating greater morningness preference) bedtimes shifted earlier on weekdays by 6.9 minutes (95% CI: −7.6, −6.2, p-value < 0.001) and on weekends by 5.7 minutes (95% CI: −6.4, −5, p-value < 0.001) (Tables B.5 and B.6). A 1-point increase in MESC score was also associated with an earlier wake time of 10 minutes on weekdays (95% CI: −10.8, −9.2, p-value < 0.001) and 6.8 minutes on weekends during COVID-19 (95% CI: −7.6, −5.9, p-value < 0.001) (Tables B.11 and B.12). There was a significant decrease in time in bed on the weekdays, but only by 1.4 minutes (95% CI: −2, −0.8, p-value < 0.001) for every 1-point increase in MESC score. MESC score was not significantly associated with weekend time in bed or social jetlag during COVID-19.
Discussion
In our sample of almost 3,500 adolescents from across the U.S. in the early months of the COVID-19 pandemic, we found that adolescents increased their time in bed, shifted their bed and wake times later, and had less social jetlag during COVID-19 compared to retrospective report of their behaviors prior to COVID-19. Prior to COVID-19, only 53.5% of adolescents reported ≥ 8 hours in bed on weekdays while 81.3% of adolescents reported ≥ 8 hours in bed on weekdays during COVID-19. This increased sleep opportunity was due to a notable delay in waketimes, averaging nearly 4 hours later on weekdays compared to pre-pandemic patterns. Prior to COVID-19, 52.1% of adolescents reported social jetlag with a > 2-hour difference between weekday and weekend sleep times but this reduced to just 6.3% of respondents during COVID-19, suggesting a more regular sleep/wake schedule. Unsurprisingly, without an enforced start time for in-person school, adolescents tended to sleep on a delayed sleep schedule which may align with the tendency for a circadian phase delay in adolescence. Significantly later wake times allowed for more sleep opportunity during COVID-19 and most adolescents reported time in bed in line with recommendations for their age during this time.
The current findings seem comparable to the limited extant research on adolescent sleep patterns during COVID-19: both adolescent and parent report of youth sleep behaviors during COVID-19 indicate an increase in sleep duration and delay in bed/wake times compared to either retrospective report or other samples assessed prior to the pandemic (Bruni et al., 2021; Illingworth et al., 2022; Lim et al., 2021; López-Bueno et al., 2020; Lu et al., 2020; Meltzer, Saletin, et al., 2021; Zhou et al., 2020). Despite changes to schedules and stressors related to COVID-19 (e.g., changes in school, reduced opportunities for physical activity and social interaction) that may have impacted sleep, the majority of adolescents reported improvements in sleep during COVID-19 with reduced social jetlag as well as increased time in bed. These findings support recent research that supports later school start times as a means of providing increased sleep opportunity for teens (Meltzer, Saletin, et al., 2021; Meltzer, Shaheed, & Ambler, 2016; Meltzer, Wahlstrom, Plog, & Strand, 2021; Ziporyn et al., 2022).
Physical activity level during COVID-19 was associated with some aspects of sleep. Specifically, adolescents who endorsed a decrease or not participating in physical activity during COVID-19 had greater delays in bedtimes and waketimes during COVID-19 compared to those adolescents that reported engaging in physical activity. Physical activity has been found to be protective for and associated with longer sleep duration, better sleep quality, and less variability in sleep duration and timing in adolescents prior to COVID-19 (Hrafnkelsdottir et al., 2020; Lang et al., 2016; Xu, Adams, Cohen, Earp, & Greaney, 2019). In a study conducted prior to COVID-19 that implemented an intervention promoting physical activity in adolescents (adding 30 minutes of moderate-intensity physical activity every weekday for 3 weeks), youth obtained longer sleep duration, shorter sleep onset latency, and improved sleep efficiency (Chennaoui, Arnal, Sauvet, & Léger, 2015). Thus, encouraging physical activity in adolescents may be a promising strategy to promote sleep health.
Contrary to hypotheses, engagement in social interactions was not significantly associated with change in time in bed, bedtime, or social jetlag during COVID-19. Participants that decreased or did not engage in social interactions during COVID-19 had a slight delay (~10 minutes) in their waketimes, though the clinical significance of this change is unclear. This is in contrast to research in adults that found high levels of social support during COVID-19 reduced risk for poor sleep quality compared to individuals with low levels of social support (Grey et al., 2020). In adolescents prior to COVID-19, those with higher levels of social support had better sleep quality and less insufficient sleep, and social support moderated the effects of stress on sleep (van Schalkwijk, Blessinga, Willemen, Van Der Werf, & Schuengel, 2015). Thus, social support may be helpful for promoting sleep during times of high stress, such as during the COVID-19 pandemic. It may be that our item querying social interactions was not fully able to capture the ways that adolescents were obtaining social support during COVID-19 (e.g., via online interactions). Further examination of how adolescents obtain social support and association with sleep is needed.
Adolescents with symptoms of depression and anxiety in the Severe range significantly shifted bed and wake times later during COVID-19, compared to those with symptoms in the Moderate or below range. Additionally, a reported diagnosis of depression before COVID-19 was also associated with greater delay in waketimes, and a reported diagnosis of anxiety was associated with an increase in time in bed during COVID-19. A large, nationally representative survey of over 10,000 adolescents in the U.S., conducted prior to COVID-19, found that later weeknight bedtime, shorter weeknight sleep duration, greater bedtime delay on weekends, and weekend oversleep were associated with higher odds of depressed mood and anxiety disturbance, substance use, and behavior disorders, as well as increased suicidality (Zhang et al., 2017). Delays in bedtime may lead to shorter weeknight sleep opportunity when adolescents are attending school in person. They may also exacerbate previous mood symptoms leading to further sleep problems. These factors should be considered when determining appropriate school start times for adolescents.
Findings should be considered within the limitations of the study, which include a reliance on current and retrospective self-report of sleep, mood, and behaviors which may be subject to error and bias. However, this methodology is similar to other studies that also took place early in the pandemic and allows for more precise examination of individual change in sleep behaviors than other studies that used a different sample assessed prior to the pandemic as comparison. Because we did not account for sleep onset latency or night wakings, our values of time in bed are not true estimates of total sleep duration but more accurately reflect sleep opportunity. Additionally, chronotype was not assessed retrospectively before COVID-19 and participants may have responded differently on the MESC during COVID-19 than they would have prior to COVID-19. Indeed, their behaviors during COVID-19 may have impacted their responses regarding how easy it is to wake in the morning, how alert they are when they wake up, and the flexibility to complete assignments at different times when engaged in online or remote learning. A strength of our study was inclusion of a large sample of adolescents across the U.S. While the sample demographics did not precisely match that of the U.S., perhaps limited by the diversity of users of the social media platforms that we recruited from, our sample was geographically and economically diverse. Moreover, the survey used validated measures and content-specific questions to assess both current and retrospective assessment of sleep both before and during COVID-19. Finally, the current results should be interpreted within the time frame of survey administration, which was limited to the early months of the COVID-19 pandemic (May 2020). While limitations in research conducted during this time are understandable given the restrictions, safety concerns, and significant stressors that occurred (Stearns et al., 2021), the current findings may not be applicable or comparable to sleep behaviors at later times in the pandemic.
Future research, clinical care, and policy decisions should take into consideration the changes in sleep that appear to have occurred during COVID-19, such as increased sleep opportunity and decreased social jetlag that have been shown to have positive implications for physical and mental health as well as academic achievement in adolescents. The increase in time in bed combined with delayed bed and wake times suggests that measures such as delaying high school start times may be valuable for allowing adolescents to obtain sufficient sleep. Yet, more research is needed on the potential consequences of late sleep timing for youth. Clinicians working with adolescents should consider assessing and promoting physical activity and social interactions, as well as adequate screening and treatment for mental health symptoms as a strategy to improve sleep.
Conclusion
Results of this study reinforce prior observations indicating that adolescent sleep patterns are significantly impacted by academic and social schedules. Stay at home restrictions during the COVID-19 pandemic allowed adolescents to significantly improve time in bed by choosing their own bed and wake times. It is imperative to consider lessons learned during COVID-19 that may optimize and continue to promote sleep in adolescents.
Supplementary Material
Grant Funding:
This work was supported by the following funding sources: Department of Pediatrics, University of Colorado Anschutz Medical Campus; NIH K23DK117021; and NIH/NCATS Colorado CTSA UL1 TR002535. Dr. Honaker’s time was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K23HL150299. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure Statement: No conflicts of interest are reported for any of the authors.
References
- Adolescent Sleep Working Group, Committee on Adolescence, & Council on School Health. (2014). School start times for adolescents. Pediatrics, 134(3), 642–649. doi: 10.1542/peds.2014-1697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Dvorsky MR, Breaux R, Cusick CN, Taylor KP, & Langberg JM (2021). Prospective Examination of Adolescent Sleep Patterns and Behaviors Before and During COVID-19. Sleep doi: 10.1093/sleep/zsab054 [DOI] [PMC free article] [PubMed]
- Becker SP, & Gregory AM (2020). Editorial Perspective: Perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. J Child Psychol Psychiatry, 61(7), 757–759. doi: 10.1111/jcpp.13278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni O, Malorgio E, Doria M, Finotti E, Spruyt K, Melegari MG, . . . Ferri R (2021). Changes in sleep patterns and disturbances in children and adolescents in Italy during the Covid-19 outbreak. Sleep Med doi: 10.1016/j.sleep.2021.02.003 [DOI] [PMC free article] [PubMed]
- Byars KC, Simon SL, Peugh J, & Beebe DW (2017). Validation of a Brief Insomnia Severity Measure in Youth Clinically Referred for Sleep Evaluation. J Pediatr Psychol, 42(4), 466–475. doi: 10.1093/jpepsy/jsw077 [DOI] [PubMed] [Google Scholar]
- Carskadon MA, Vieira C, & Acebo C (1993). Association between puberty and delayed phase preference. Sleep, 16(3), 258–262. doi: 10.1093/sleep/16.3.258 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019). Youth Risk Behavior Survey Data Retrieved from https://www.cdc.gov/healthyyouth/data/yrbs/index.htm
- Chennaoui M, Arnal PJ, Sauvet F, & Léger D (2015). Sleep and exercise: a reciprocal issue? Sleep Med Rev, 20, 59–72. doi: 10.1016/j.smrv.2014.06.008 [DOI] [PubMed] [Google Scholar]
- Crowley SJ, Wolfson AR, Tarokh L, & Carskadon MA (2018). An update on adolescent sleep: New evidence informing the perfect storm model. J Adolesc, 67, 55–65. doi: 10.1016/j.adolescence.2018.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSantis AS, Dubowitz T, Ghosh-Dastidar B, Hunter GP, Buman M, Buysse DJ, . . . Troxel WM (2019). A preliminary study of a composite sleep health score: associations with psychological distress, body mass index, and physical functioning in a low-income African American community. Sleep Health, 5(5), 514–520. doi: 10.1016/j.sleh.2019.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz-Morales JF (2015). Morningness–Eveningness Scale for Children (MESC): Spanish normative data and factorial invariance according to sex and age. Personality and Individual Differences, 87, 116–120. doi: 10.1016/j.paid.2015.07.027 [DOI] [Google Scholar]
- Grey I, Arora T, Thomas J, Saneh A, Tohme P, & Abi-Habib R (2020). The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res, 293, 113452. doi: 10.1016/j.psychres.2020.113452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber R, Saha S, Somerville G, Boursier J, & Wise MS (2020). The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med, 76, 33–35. doi: 10.1016/j.sleep.2020.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 42(2), 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hrafnkelsdottir SM, Brychta RJ, Rognvaldsdottir V, Chen KY, Johannsson E, Gudmundsdottir SL, & Arngrimsson SA (2020). Less screen time and more physical activity is associated with more stable sleep patterns among Icelandic adolescents. Sleep Health, 6(5), 609–617. doi: 10.1016/j.sleh.2020.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illingworth G, Mansfield KL, Espie CA, Fazel M, & Waite F (2022). Sleep in the time of COVID-19: findings from 17000 school-aged children and adolescents in the UK during the first national lockdown. Sleep Adv, 3(1), zpab021. doi: 10.1093/sleepadvances/zpab021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin DE, Gross HE, Stucky BD, Thissen D, DeWitt EM, Lai JS, . . . DeWalt DA (2012). Development of six PROMIS pediatrics proxy-report item banks. Health Qual Life Outcomes, 10, 22. doi: 10.1186/1477-7525-10-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang C, Kalak N, Brand S, Holsboer-Trachsler E, Pühse U, & Gerber M (2016). The relationship between physical activity and sleep from mid adolescence to early adulthood. A systematic review of methodological approaches and meta-analysis. Sleep Med Rev, 28, 32–45. doi: 10.1016/j.smrv.2015.07.004 [DOI] [PubMed] [Google Scholar]
- Lim MTC, Ramamurthy MB, Aishworiya R, Rajgor DD, Tran AP, Hiriyur P, . . . Goh DYT (2021). School closure during the coronavirus disease 2019 (COVID-19) pandemic - Impact on children’s sleep. Sleep Med, 78, 108–114. doi: 10.1016/j.sleep.2020.12.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Bueno R, López-Sánchez GF, Casajús JA, Calatayud J, Gil-Salmerón A, Grabovac I, . . . Smith L (2020). Health-Related Behaviors Among School-Aged Children and Adolescents During the Spanish Covid-19 Confinement. Front Pediatr, 8, 573. doi: 10.3389/fped.2020.00573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C, Chi X, Liang K, Chen ST, Huang L, Guo T, . . . Zou L (2020). Moving More and Sitting Less as Healthy Lifestyle Behaviors are Protective Factors for Insomnia, Depression, and Anxiety Among Adolescents During the COVID-19 Pandemic. Psychol Res Behav Manag, 13, 1223–1233. doi: 10.2147/prbm.S284103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ, Saletin JM, Honaker SM, Owens JA, Seixas A, Wahlstrom KL, . . . Carskadon MA (2021). COVID-19 instructional approaches (in-person, online, hybrid), school start times, and sleep in over 5,000 U.S. adolescents. Sleep doi: 10.1093/sleep/zsab180 [DOI] [PMC free article] [PubMed]
- Meltzer LJ, Shaheed K, & Ambler D (2016). Start Later, Sleep Later: School Start Times and Adolescent Sleep in Homeschool Versus Public/Private School Students. Behav Sleep Med, 14(2), 140–154. doi: 10.1080/15402002.2014.963584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ, Wahlstrom KL, Plog AE, & Strand MJ (2021). Changing school start times: impact on sleep in primary and secondary school students. Sleep, 44(7). doi: 10.1093/sleep/zsab048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell JA, & Owens JA (2015). A clinical guide to pediatric sleep: Diagnosis and management of sleep problems (3rd ed). Wolters Kluwer. [Google Scholar]
- Northwestern University. (2020). PROMIS Score Cut Points Retrieved from https://staging.healthmeasures.net/score-and-interpret/interpret-scores/promis/promis-score-cut-points. https://staging.healthmeasures.net/score-and-interpret/interpret-scores/promis/promis-score-cut-points
- Okun ML, Reynolds CF 3rd, Buysse DJ, Monk TH, Mazumdar S, Begley A, & Hall M (2011). Sleep variability, health-related practices, and inflammatory markers in a community dwelling sample of older adults. Psychosom Med, 73(2), 142–150. doi: 10.1097/PSY.0b013e3182020d08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, Lloyd RM, . . . Wise MS (2016). Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J Clin Sleep Med, 12(11), 1549–1561. doi: 10.5664/jcsm.6288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- RStudio Team. (2020). RStudio: Integrated Development for R Boston, MA: PBC. Retrieved from www.rstudio.com [Google Scholar]
- Stearns MA, Ievers-Landis CE, McCrae CS, & Simon SL (2021). Sleep across childhood during the COVID-19 pandemic: a narrative review of the literature and clinical case examples. Children’s Health Care, 1–23. doi: 10.1080/02739615.2021.2016407 [DOI]
- van Schalkwijk FJ, Blessinga AN, Willemen AM, Van Der Werf YD, & Schuengel C (2015). Social support moderates the effects of stress on sleep in adolescents. J Sleep Res, 24(4), 407–413. doi: 10.1111/jsr.12298 [DOI] [PubMed] [Google Scholar]
- Xu F, Adams SK, Cohen SA, Earp JE, & Greaney ML (2019). Relationship between Physical Activity, Screen Time, and Sleep Quantity and Quality in US Adolescents Aged 16⁻19. Int J Environ Res Public Health, 16(9). doi: 10.3390/ijerph16091524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Paksarian D, Lamers F, Hickie IB, He J, & Merikangas KR (2017). Sleep Patterns and Mental Health Correlates in US Adolescents. J Pediatr, 182, 137–143. doi: 10.1016/j.jpeds.2016.11.007 [DOI] [PubMed] [Google Scholar]
- Zhou SJ, Wang LL, Yang R, Yang XJ, Zhang LG, Guo ZC, . . . Chen JX (2020). Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med, 74, 39–47. doi: 10.1016/j.sleep.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziporyn TD, Owens JA, Wahlstrom KL, Wolfson AR, Troxel WM, Saletin JM, . . . Carskadon MA (2022). Adolescent sleep health and school start times: Setting the research agenda for California and beyond. A research summit summary. Sleep Health, 8(1), 11–22. doi: 10.1016/j.sleh.2021.10.008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


