Abstract
Aim
The aims of the study were to synthesize the role of technology‐based healthcare interventions (TBIs) and to identify the most effective interventions for the best functional maternal and child health (MCH) outcomes among low‐risk pregnant women in low‐ and middle‐income countries (LMICs).
Design
A systematic review and network meta‐analysis (NMA).
Methods
We will perform a comprehensive search in electronic databases and other resources to identify relevant randomized controlled trials. Two reviewers will independently perform study selection, data extraction and quality assessment. Our primary outcomes include proportion of recommended antenatal care visits, skilled delivery care, postnatal care visits and exclusive breastfeeding practices. We will use pairwise random‐effects meta‐analysis and NMAs to estimate direct, indirect and relative effects using the relevant intervention classifications for each outcome separately. We plan to assess hierarchy of interventions, statistical inconsistency and certainty of evidence.
Results
This review will compare the effectiveness of different form of TBIs on a comprehensive range of MCH outcomes and will provide the outcome‐specific reliable evidence of the most effective interventions on improving MCH in LMICs. The review findings will guide researchers, stakeholders or policymakers on the potential use of TBIs in the given contexts that could achieve the best functional MCH outcomes in LMICs.
Keywords: antenatal care, delivery care, exclusive breastfeeding, healthcare service utilization, LMICs, maternal and child health, network meta‐analysis, perinatal care, postnatal care, systematic review
1. INTRODUCTION
Despite continuing efforts on improving maternal and child health (MCH), global maternal and child mortality remains unacceptably high. Low‐ and middle‐income countries (LMICs), particularly sub‐Saharan Africa and central and southern Asia, had account for most deaths (WHO, 2019a, 2021a, 2021c). An estimated 94% of maternal deaths occur in LMICs, and these two regions contain around 86% of the global maternal deaths in 2017 (WHO, 2019a, 2021c). Of the global childhood deaths occurring in 2019, more than 80% died in these regions (WHO, 2021a). Most of the deaths occurred from the causes of complications during pregnancy, childbirth or postpartum period that could be prevented in most cases as the healthcare solutions to manage or prevent complications are well known. Timely management and treatment and essential maternal healthcare service practice such as recommended antenatal care (ANC), skilled delivery and postnatal care (PNC) including exclusive breastfeeding (EBF) practice, can reduce the complications and may result in preventing maternal and child mortality. Prior evidence has confirmed the ability of recommended ANC visits, skilled birth attendance (SBA) at the time of the labour and delivery, facility delivery, PNC visits and EBF practice on reducing maternal and child mortality (Campbell et al., 2006; Tolossa et al., 2020; Victora et al., 2016; WHO, 2019a; Yakoob et al., 2011). However, the coverage of these services is quite low in LMICs, resulting in higher maternal and child mortality in these settings (UNICEF, 2019).
In LMICs, providing essential healthcare services throughout the pregnancy cycle are quite complex, and may not feasible in low‐resource settings, as integrated and multiple interventions are needed throughout the antenatal, delivery and postnatal pathways. As LMICs have a shortage of health personnel and high clinic volume, information and communication technology (ICT) may support the uptake of essential healthcare services effectively by strengthening health systems as it requires no additional or less human resources.
In the last two decades, technology‐based healthcare interventions (TBIs) that utilize ICT to address health needs are being considered as a promising solution to strengthen health service uptake effectively at individual, organizational and community levels. TBIs include electronic health (eHealth), mobile health (mHealth), telehealth, telemedicine or digital health interventions. Such interventions are being used for improving health behaviours among antepartum and postpartum women by providing healthcare reminder, health advice, health education, health information sharing or communication that may result on improving MCH outcomes in LMICs. In 2018 Seventy‐First World Health Assembly (WHA), all member states of World Health Organization (WHO) demonstrated a collective recognition of the value of digital technologies to contribute to advancing universal health coverage (UHC) and other health aims of the sustainable development goals (SDGs) (WHO, 2019b). In that assembly, all WHO member states approved a resolution on digital health, in which it has been urged to assess the use of digital technologies for health and to prioritize the development, evaluation, implementation, scale‐up and greater use of digital technologies.
Over the last decade, evidence about eHealth, mHealth, telehealth, telemedicine or digital health interventions is being systematically studied to evaluate their role in improving MCH, particularly in promoting essential healthcare utilization during pregnancy and postpartum period (Amoakoh‐Coleman et al., 2016; Ashford et al., 2016; Chan & Chen, 2019; Chen et al., 2018; Colaci et al., 2016; Daly et al., 2018; Feroz et al., 2017; Hussain et al., 2020; Lamont et al., 2016; Lee et al., 2016; Nair et al., 2018; Palmer et al., 2020; Rivera‐Romero et al., 2018; Sondaal et al., 2016; Van Den Heuvel et al., 2018; Vodopivec‐Jamsek et al., 2012; Wagnew et al., 2018). These studies are limited to assessing an isolated range of interventions (such as mHealth only) or limited range of outcomes (such as uptake of health services but not perinatal outcomes). Moreover, there has been no consensus on the effectiveness of TBIs on improving MCH outcomes. A comprehensive systematic review reported an increasing trend of mHealth interventions with diversified functions used in improvement of reproductive, maternal, newborn and child health. However, they urged rigorous evaluation to draw consistent conclusions on effectiveness of these interventions with their functions as they noticed negative or unclear results from around half of their included randomized controlled trials (RCTs) (Chen et al., 2018). Therefore, a rigorous evaluation considering all forms of TBIs is urgently required to generate evidence and promote the appropriate integration and use of technologies into the existing health systems to improve MCH outcomes in resource‐limited settings.
1.1. Review questions
This systematic review and network meta‐analysis (NMA) will address the following review questions:
What is the role of TBIs on improving MCH outcomes, including essential maternal healthcare service utilization among low‐risk pregnant women in LMICs;
What is the efficacy of single and complex TBIs on improving selected MCH outcomes with regard to target populations; and
Which kinds of TBIs are the most effective interventions that could achieve the best functional MCH outcomes in these resource‐limited settings?
2. METHODS AND ANALYSIS
2.1. Review design
This is a systematic review and NMA aimed to assess and synthesize the role of TBIs on improving antenatal, delivery and postnatal care service utilization, with a comprehensive range of MCH outcomes, in low‐risk pregnant women in LMICs. Our NMAs will estimate direct, indirect and relative effects of TBIs on the MCH outcomes and will identify the most effective interventions that could achieve the best functional MCH outcomes in LMICs.
2.2. Protocol registration and review guideline
The review protocol is registered in the “International Prospective Register for Systematic Reviews” (PROSPERO) database (PROSPERO registration number‐ CRD42021239185) (Schiavo, 2019). This protocol adheres to the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., 2019). We will report the review findings according to the guideline of Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) extension statement for reporting of systematic reviews incorporating network meta‐analyses (NMA) of healthcare interventions (Hutton et al., 2015).
2.3. Data sources
We will perform a comprehensive search to identify randomized controlled trials (RCTs), including Cluster‐RCTs and quasi‐RCTs, in the following electronic resources with no limit of languages, date or types of publication: APA PsycINFO, British Nursing Index, CINAHL PLUS, EMBASE, EmCare, MEDLINE, PubMed, PubMed Central, ScienceDirect, Scopus, The Cochrane Library and Web of Science. Reference lists of included articles and relevant systematic reviews, including grey literature, citation tracking and reference snowballing, and handsearching in key journals, will also be checked for identifying additional potential studies for inclusion. We will also search clinical trial registries in order to identify additional registered studies that are not captured by the above searches.
2.4. Search strategy
An extensive search strategy addressing the review questions has been developed to search the electronic databases. The search strategy of PubMed described in Table 1 has been piloted on 8 December 2020, and then validated with an expert librarian. The strategy will be fed to each electronic database based on their own controlled vocabulary. The search terms consist of Medical Subject Headings (MeSH), title/abstract/keywords (ti/ab/kw) and text words (tw). Our search strategy focuses on eHealth, mHealth, telehealth and digital health. The search results will be updated before publication. We will report the detailed search strategies for all electronic databases in the full review.
TABLE 1.
Search strategy of PubMed database
| SL | Query |
|---|---|
| 1. | expectant mother[Text Word] OR “pregnant women”[MeSH Terms] OR pregnant women[Text Word] OR pregnant mother[Text Word] OR “pregnancy”[MeSH Terms] OR pregnancy[Text Word] |
| 2. | computer[Text Word] OR tablet[Text Word] OR phone[Text Word] OR mobile[Text Word] OR mobile phone[Text Word] OR mobile device[Text Word] OR smartphone[MeSH Terms] OR smartphone[Text Word] OR smart‐phone[Text Word] OR “cell phone”[MeSH Terms] OR cell phone[Text Word] OR cellphone[Text Word] OR cellular phone[Text Word] OR web[Text Word] OR website[Text Word] OR “Internet”[MeSH Terms] OR Internet[Text Word] OR online[Text Word] OR on‐line[Text Word] OR “technology”[MeSH Terms] OR technology[Text Word] OR digital technology[Text Word] OR mobile technology[Text Word] OR health technology[Text Word] OR “wireless technology”[MeSH Terms] OR wireless technology[Text Word] OR wireless device[Text Word] OR iPhone[Text Word] OR i‐Phone[Text Word] OR iPad[Text Word] OR i‐Pad[Text Word] OR iPod[Text Word] OR i‐Pod[Text Word] |
| 3. | SMS[Text Word] OR short message service[Text Word] OR short messaging[Text Word] OR mobile phone messaging[Text Word] OR MMS[Text Word] OR multimedia message service[Text Word] OR multi‐media message[Text Word] OR SMS advice[Text Word] OR SMS reminder[Text Word] OR text message[Text Word] OR “text messaging”[MeSH Terms] OR text messaging[Text Word]OR texting[Text Word] |
| 4. | mobile call[Text Word] OR mobile calling[Text Word] OR mobile communication[Text Word] OR voice call[Text Word] OR voice calling[Text Word] OR voice message[Text Word] OR video conference[Text Word] |
| 5. | “mobile applications”[MeSH Terms] OR mobile applications[Text Word] OR mobile apps[Text Word] OR mobile app[Text Word] OR smartphone app[Text Word] OR app[Text Word] OR apps[Text Word] OR email[Text Word] OR “electronic mail”[MeSH Terms] OR electronic mail[Text Word] OR e‐mail[Text Word] OR personal digital assistant[Text Word] OR PDA[Text Word] |
| 6. | #2 OR #3 OR #4 OR #5 |
| 7. | eHealth[Text Word] OR e‐Health[Text Word] OR electronic health[Text Word] OR digital health[Text Word] OR telehealth[Text Word] OR “telemedicine”[MeSH Terms] OR telemedicine[Text Word] OR “telecommunications”[MeSH Terms] OR telecommunication[Text Word] OR mHealth[Text Word] OR m‐Health[Text Word] OR mobile health[Text Word] OR mobile medicine[Text Word] OR mcare[Text Word] OR m‐care[Text Word] OR mobile care[Text Word] OR mHealth messaging[Text Word] OR mobile telehealth[Text Word] OR mobile telehealth care[Text Word] OR m‐Edu[Text Word] OR medu[Text Word] OR m‐education[Text Word] OR mobile education[Text Word] OR mLearning[Text Word] OR eLearning[Text Word] |
| 8. | #6 AND #7 |
| 9. | (randomized controlled trial[Publication Type] OR controlled clinical trial[Publication Type] OR randomized[Title/Abstract] OR placebo[Title/Abstract] OR clinical trials as topic[MeSH Major Topic] OR randomly[Title/Abstract] OR trial[Title]) NOT (animals[MeSH Terms] NOT humans[MeSH Terms]) |
| 10. | #1 AND #8 AND #9 |
2.5. Criteria for considering studies for this review
The study eligibility criteria have been defined by following PICOS framework (P‐Participants, I‐interventions, C‐Comparator, O‐Outcomes and S‐Study design/settings). A study will be included if the study meets all of the following criteria:
Participants: We will include studies if the study was conducted on reproductive aged low‐risk women who were in antenatal and postnatal period. If the participants are high‐risk population such as pregnant/postpartum women with HIV/AIDS, heart diseases, diabetes and preeclampsia at the baseline, we will exclude those studies due to having higher medical adherence before the commencement of the intervention provision among these groups. We will include the studies in which only a subgroup of participants is eligible for the review only if it is possible to extract relevant data specific to that subgroup from the publication. Otherwise, we will exclude those studies.
Interventions: We intend to include all types of TBIs (e.g. eHealth intervention, mHealth intervention, telehealth intervention or digital health) in this review, that focus on improving MCH outcomes, including essential healthcare services utilization during antenatal or postnatal period.
Comparator: We will include studies that compare the effectiveness of TBIs with standard care or non‐TBIs. If the study compares different forms of TBIs, it will be eligible for inclusion.
Study designs: We will include individual RCTs, cluster‐RCTs, and quasi‐RCTs that evaluate the effectiveness of TBIs on improving MCH. We will exclude qualitative studies, observational studies, cross‐sectional studies, review studies, case studies, commentaries, editorials, expert opinions and symposium proceedings if they have insufficient information to assess the eligibility.
Study settings: We will include studies conducted in LMICs. We will follow World Bank country classification at the time of study implementation to identify LMICs (World Bank, 2019).
2.6. Outcomes to be reported in this review
This systematic review will cover a comprehensive range of MCH outcomes reported in the studies. The primary and secondary outcome variables are classified as below:
- Primary outcomes:
- Proportion of ANC visits
- Proportion of skilled delivery care utilization such as facility delivery, and skilled birth attendance (SBA) during delivery
- Rate of PNC utilization
- Rate of exclusive breastfeeding practice
Secondary outcomes:
Maternal health outcomes:
Rate of micronutrients intake during pregnancy (Iron, Folic acid, Vitamin D, Vitamin K)
Tetanus vaccine coverage during pregnancy
Maternal mortality/death
Maternal anaemia during pregnancy
Postpartum haemorrhage
Preterm birth
Preeclampsia
Child health outcomes:
Low birthweight
Small for gestational age
Large for gestational age
Stillbirth
Perinatal death
Neonatal mortality/death
2.7. Operational definitions
2.7.1. Low‐risk/healthy pregnant women
A pregnant women is considered as low‐risk/healthy pregnant women if she does not have any diseases of HIV/AIDS, cancer, heart diseases, preeclampsia, diabetes or other severe diseases at the baseline or before the commencement of the intervention provision.
2.7.2. High‐risk pregnant women
A pregnant women having HIV/AIDS, cancer, heart diseases, preeclampsia, diabetes or other severe diseases at the baseline or before the commencement of the intervention provision is considered as high‐risk pregnant women.
2.7.3. Skilled care
The cares provided by skilled health personnel such as doctors, nurses and midwives.
2.7.4. Technology‐based healthcare interventions
Technology‐based healthcare interventions (TBIs) include all forms of technologies (e.g. mobile, telephone, computer, Internet, Web and social media) that are being used to support strengthening health system. It covers eHealth, mHealth, telehealth or digital health.
2.7.5. eHealth
Electronic health (eHealth) refers to the application of information and communication technologies (ICT) in support of health and health‐related fields, including health surveillance, healthcare services, health literature and health education, knowledge and research (WHO, 2021b).
2.7.6. mHealth
Mobile health (mHealth) is the use of mobile communication technology for healthcare practice. It covers all forms of mobile phone‐based healthcare interventions using voice calling, text message, voice message, mobile video and mobile apps (WHO, 2011).
2.7.7. Telehealth
It includes remote clinical (telemedicine) or non‐clinical care and services using electronic and telecommunication technologies (e.g. real‐time two‐way communication between the patient and the healthcare provider).
2.7.8. Digital health
It refers to the use of digital technologies in healthcare utilization (WHO, 2019b).
2.7.9. One‐way communication intervention
It involves the transfer of information, either health education/advice and/or upcoming healthcare reminder, from healthcare providers to the study participants, but the participants do not have any access to healthcare providers between the health visits.
2.7.10. Two‐way communication intervention
In the two‐way communication intervention, a healthcare provider delivers the tailored information to the study participants, and the participants have also an access to reach healthcare providers if they have any health issue raised between the health visits.
2.8. Study selection process
EndNote reference management software and Rayyan QCRI tool (an online tool to study screening) will be utilized in the study selection process (Ouzzani et al., 2016). In the first stage, all articles retrieved from the electronic databases will be stored in EndNote and then duplicates will be identified and deleted. After removing the duplicates, the combined articles will be screened through Rayyan QCRI tool.
Two reviewers will independently screen the titles and abstracts of all retrieved studies and will exclude irrelevant studies based on study eligibility criteria. Then, all potentially relevant studies will undergo full‐text screening to assess the eligibility in detail. In the full‐text screening, two reviewers will also critically review the selected studies based on the predefined inclusion and exclusion criteria. Any disagreements between reviewers will be resolved through discussion. If the agreement is not reached, a third reviewer will review and make the final decision. We will note the reasons of all studies excluded in full‐text screening. After full‐text screening, we will recheck the duplicate studies. If we identify multiple reports from a single study, we will select the study that has the most relevant information, or we will combine all reports in a single study if required. The flow of study selection will be shown in a PRISMA flow diagram (Figure 1).
FIGURE 1.
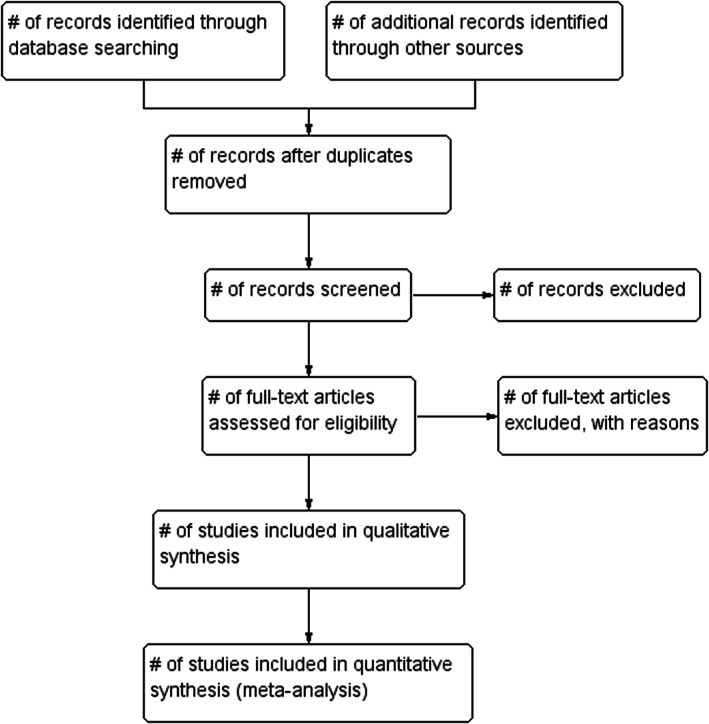
PRISMA study flow diagram
2.9. Data extraction
Two reviewers will independently extract data from all the included studies using a predesigned data extraction form. The data extraction form will be finalized through a series of trial of pilot data extraction forms. Any disagreement will be resolved through discussion or by a third reviewer. If the third reviewer cannot resolve the disagreement, we will contact the authors of the studies. For the unsolved cases, we will report the disagreement in the review.
We will extract a standard set of data from each of the selected studies such as study characteristics, participant characteristics, intervention characteristics and outcomes. We will also report key characteristics of the included studies in a separate table. The characteristics data will include, but will not be limited to author information, year of publication, study location, study setting, study design, study name, sample size, study year, targeted participants, age of participants, gestational age at recruitment, comparator, types, function, mode and duration of interventions, intervention provider and reported outcomes.
2.10. Dealing with non‐English studies and missing data
Articles written in languages other than English (Spanish, Chinese, German, Italian and others) will be read and extracted data with the assistance of colleagues who were native speakers in these languages. If we do not have native speakers in a language and cannot be translated in English, we will prepare a list of these studies not included in the review. When the information is unclear/missing or full‐text articles are not available, we will contact the authors of the studies to collect our required information. For continuous outcomes, if standard deviation (SD) data are missing in the reports, we will mathematically calculate SD or will measure it from the figure data. If the study reports only medians, we will use median as the mean and the interquartile range (IQR3‐IQR1)/1.35 as the standard deviation (Follmann et al., 1992).
2.11. Risk of bias (study quality) assessment
We will use the Cochrane Collaboration's risk of bias assessment tool to assess risk of bias in the randomized controlled studies (Higgins et al., 2011). Following the guideline of the Cochrane handbook, two independent reviewers will evaluate the following components of Cochrane Collaboration's risk of bias assessment tool: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias (e.g. intention to treat analysis, baseline imbalance (Higgins et al., 2019)). Any disagreement will be resolved through discussion or by a third reviewer.
2.12. Strategy for data synthesis
We will narratively synthesize study characteristics, participant characteristics, intervention characteristics and key findings of primary and secondary outcomes among all included studies. We will present the structure of a network of interventions, direct, indirect and relative effects for each primary outcome separately, as NMA aims to combine the direct and indirect evidence into a single effect size (Higgins et al., 2019; Song et al., 2009). While pooling the effect size, we will use risk ratios for dichotomous outcomes and mean differences for continuous outcomes, and their 95% confidence interval will also be reported. If the study provided odds ratio, we will convert into risk ratio. If the odds ratio or risk ratio is unavailable in any study, we will calculate crude risk ratio from raw data reported in the studies. If we find different measurement unit of an outcome, we will convert it to a unique measurement unit. If the conversion is not possible and have sufficient number of studies to conduct meta‐analysis separately, we will perform the analysis for each measurement unit of that outcome. Otherwise, we will narratively synthesize the results. All meta‐analysis results will be presented in forest plots or tabular formats. Heterogeneity will be assessed by visual inspection of forest plots or tested using I‐square statistic, and we will consider I‐square value greater than 50% as substantial heterogeneity (Higgins et al., 2019). Along with I‐square statistic, we will also consider Tau‐square statistic and Cochrane Q test (chi‐square statistic) to check the statistical heterogeneity. The ranking probability of interventions will be depicted in a graphical rankogram, and publication bias will be presented in funnel plots for each outcome. Statistical significance will be defined as p‐value <.05 for all analyses. In addition, we will present a summary of findings for our primary outcomes.
2.13. Data analysis
We will first conduct a pairwise random‐effects meta‐analysis to summarize the effect size of all direct evidence for each outcome separately. If we find low heterogeneity in the pairwise meta‐analysis, we will use a fixed effect model. Then, we will evaluate our primary and secondary outcomes in separate NMAs using the relevant intervention classifications, as NMA can estimate direct, indirect and relative effect size in a single model (Higgins et al., 2019; Song et al., 2009). We will stratify meta‐analyses according to study population, study regions, logistics of intervention provision, intervention content or study quality, if we have a minimum number of studies. We will also use meta‐regression to adjust confounding factors such as socio‐demographic index (SDI), maternal mortality ratio, neonatal mortality rate, prevalence of anaemia in pregnant women, country/region and risk of bias of studies. We plan to use funnel plots and Egger test to assess publication bias in the pairwise meta‐analysis. We will use comparison‐adjusted funnel plot to identify possible‐small study effects in a network meta‐analysis (Chaimani et al., 2013; Chaimani & Salanti, 2012). The minimum number of studies for the meta‐analysis will be two. We will perform all statistical analyses using Stata, RevMan, and/or R‐studio.
2.14. Ranking interventions
To identify the most effective intervention, we will rank interventions separately for each outcome. We will use the surface under the cumulative ranking curve (SUCRA) for ranking probabilities of interventions. A larger SUCRA value indicates a better rank of intervention (Chaimani et al., 2013; Salanti et al., 2011).
2.15. Statistical inconsistency assessment
We plan to use local and global approaches to evaluate the inconsistencies between direct and indirect evidence (Higgins et al., 2012; White et al., 2012). To evaluate for global inconsistencies in the entire network, we will use the design by treatment interaction model. This approach takes into account different sources of inconsistency that can occur when studies with different designs give different results or for disagreements between direct and indirect evidence. Using this method, we will infer the presence of inconsistency from any sources in the entire network based on a chi‐square test. To evaluate local inconsistency, the side‐splitting method will be utilized. This method can separate evidence on a particular comparison into direct and indirect evidence. We will evaluate the disagreement between direct and indirect evidence using the restricted maximum likelihood method. Statistical significance will be defined as p‐value <.05 for all analyses.
2.16. Certainty of evidence assessment
We will check the certainty of evidence only for our primary outcomes using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) method (Puhan et al., 2014). GRADE includes five components for evaluating evidence based on RCT studies: (i) risk of bias, (ii) heterogeneity, (iii) indirectness, (iv) imprecision, and (v) publication bias. Based on the judgement of each component of GRADE assessment (Guyatt et al., 2011; Guyatt et al., 2011; Guyatt, Oxman, Kunz, et al., 2011; Guyatt, Oxman, Montori, et al., 2011; Guyatt, Oxman, Vist, et al., 2011), we will classify our evidence as either: (a) high certainty evidence (further research is extremely unlikely to change the credibility of the pooled results); (b) moderate certainty evidence (further research is likely to change the credibility of the pooled results and may change the estimate); (c) low certainty evidence (further research is extremely likely to change the credibility of the pooled results and likely to change the estimate); or (d) very low certainty evidence (the pooled results have extreme uncertainty).
The GRADE ratings will be down in the following cases: (i) risk of bias: high risk of bias exists in more than one‐third studies; (ii) heterogeneity of estimates across trials: I 2‐value is greater than 50%; (iii) indirectness: we define indirectness as intransitivity; (iv) publication bias: Egger test is positive (p‐value is <.05); and (v) imprecision: the pooled estimate shows a wide confidence interval or a single trial in that comparison.
We will appraise direct and indirect evidence based on the GRADE assessment. For the certainty of indirect evidence, we will use the most dominant first order loop that contributed to the network estimates and chose the lower confidence rating among two direct comparisons as the rating of indirect comparison.
If only direct or indirect evidence is available for a given comparison, we will consider their rating as the network rating. When both direct and indirect evidence are available, we will consider the higher of the two ratings as the network rating. We will downgrade the rating if inconsistency exists between direct and indirect evidence. Inconsistency is defined as p‐value <.05 using the slide‐splitting method.
3. STRENGTHS AND LIMITATIONS OF THIS REVIEW
This review has several strengths and limitations:
To the best of our knowledge, this is the first comprehensive systematic review and network meta‐analyses (NMA) of randomized controlled trials that will estimate direct, indirect and relative effects of TBIs on a comprehensive range of MCH outcomes and will identify the most effective interventions that could achieve the best functional MCH outcomes in LMICs.
Robust analytical approaches such as network meta‐analyses, surface under the cumulative ranking curve (SUCRA), local and global approaches for statistical inconsistency between direct and indirect evidences, and GRADE approach for NMA will be used to minimize bias and to provide more accuracy of the estimates.
Adhering to stringent methodology, comprehensive search of multiple electronic databases and other resources (without any limit of language, date or types of publication), and a transparent and systematic approach to study selection, data extraction and study quality assessment will be the strengths of this review.
There may be high heterogeneity due to complex interventions and a limited number of studies that could limit summarizing the effects of the intervention.
ETHICAL APPROVAL
As this study will be a review of published paper/data, no ethical approval is required to conduct this review. We will submit the findings of this review to peer‐reviewed journals for publication and also present at national and international health conferences that will guide researchers for conducting further research or guide relevant stakeholders/funders, policymakers and health authorities for targeting appropriate TBIs to strengthen their health system or to promote healthcare utilization in their given contexts.
AUTHOR CONTRIBUTIONS
MOR: conceptualized this review. MOR, EO: designed the review protocol. MOR: developed the search strategy and wrote the manuscript. EO, DY, NY, KS: critically reviewed its intellectual contents. All authors approved the final version of the manuscript for publication.
All authors have agreed on the final version and meet at least one of the following criteria [recommended by the ICMJE (http://www.icmje.org/recommendations/)]:
• substantial contributions to conception and design, acquisition of data or analysis and interpretation of data;
• drafting the article or revising it critically for important intellectual content.
FUNDING INFORMATION
This work was supported by JST, PRESTO Grant Number JPMJPR21RC, Japan.
CONFLICT OF INTEREST
The authors have no conflict of interest.
Supporting information
Appendix S1
ACKNOWLEDGEMENTS
We would like to thank St. Luke's International University and the University of Tokyo for providing access to their library for database searching and acquisition of articles. We are thankful to the Japanese Ministry of Education, Culture, Sports, Science and Technology (MEXT) to provide MEXT doctoral programme scholarship to Md. Obaidur Rahman that partially support this research as a partial fulfilment of the doctoral programme. We thank Japan Science and Technology Agency for supporting this research (JST PRESTO Grant Number JPMJPR21RC). We would also express our gratitude to Dr Sarah E Porter, PhD, RN, academic advisor, St. Luke's International University, for the final checking and editing of the manuscript.
Rahman, M. O. , Yamaji, N. , Sasayama, K. , Yoneoka, D. , & Ota, E. (2023). Technology‐based innovative healthcare solutions for improving maternal and child health outcomes in low‐ and middle‐income countries: A network meta‐analysis protocol. Nursing Open, 10, 367–376. 10.1002/nop2.1310
PROSPERO registration number: CRD42021239185
DATA AVAILABILITY STATEMENT
No additional data available
REFERENCES
- Amoakoh‐Coleman, M. , Borgstein, A. B.‐J. , Sondaal, S. F. , Grobbee, D. E. , Miltenburg, A. S. , Verwijs, M. , Ansah, E. K. , Browne, J. L. , & Klipstein‐Grobusch, K. (2016). Effectiveness of mHealth interventions targeting health care workers to improve pregnancy outcomes in low‐and middle‐income countries: A systematic review. Journal of Medical Internet Research, 18(8), e226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashford, M. T. , Olander, E. K. , & Ayers, S. (2016). Computer‐or web‐based interventions for perinatal mental health: A systematic review. Journal of Affective Disorders, 197, 134–146. [DOI] [PubMed] [Google Scholar]
- Campbell, O. M. , Graham, W. J. , & Lancet Maternal Survival Series steering group . (2006). Strategies for reducing maternal mortality: Getting on with what works. Lancet, 368(9543), 1284–1299. [DOI] [PubMed] [Google Scholar]
- Chaimani, A. , Higgins, J. P. , Mavridis, D. , Spyridonos, P. , & Salanti, G. (2013). Graphical tools for network meta‐analysis in STATA. PLoS One, 8(10), e76654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaimani, A. , & Salanti, G. (2012). Using network meta‐analysis to evaluate the existence of small‐study effects in a network of interventions. Research Synthesis Methods, 3(2), 161–176. [DOI] [PubMed] [Google Scholar]
- Chan, K. L. , & Chen, M. (2019). Effects of social media and mobile health apps on pregnancy care: Meta‐analysis. JMIR mHealth and uHealth, 7(1), e11836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, H. , Chai, Y. , Dong, L. , Niu, W. , & Zhang, P. (2018). Effectiveness and appropriateness of mHealth interventions for maternal and child health: Systematic review. JMIR mHealth and uHealth, 6(1), e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colaci, D. , Chaudhri, S. , & Vasan, A. (2016). mHealth interventions in low‐income countries to address maternal health: A systematic review. Annals of Global Health, 82(5), 922–935. [DOI] [PubMed] [Google Scholar]
- Daly, L. M. , Horey, D. , Middleton, P. F. , Boyle, F. M. , & Flenady, V. (2018). The effect of mobile app interventions on influencing healthy maternal behavior and improving perinatal health outcomes: Systematic review. JMIR mHealth and uHealth, 6(8), e10012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feroz, A. , Perveen, S. , & Aftab, W. (2017). Role of mHealth applications for improving antenatal and postnatal care in low and middle income countries: A systematic review. BMC Health Services Research, 17(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Follmann, D. , Elliott, P. , Suh, I. , & Cutler, J. (1992). Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology, 45(7), 769–773. [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H. , Oxman, A. D. , Kunz, R. , Brozek, J. , Alonso‐Coello, P. , Rind, D. , Devereaux, P. J. , Montori, V. M. , Freyschuss, B. , Jaeschke, R. , Williams, J. W., Jr. , Murad, M. H. , Sinclair, D. , Falck‐Ytter, Y. , Meerpohl, J. , Whittington, C. , Thorlund, K. , Andrews, J. , Schünemann, H. J. , & Vist, G. (2011). GRADE guidelines 6. Rating the quality of evidence—Imprecision. Journal of Clinical Epidemiology, 64(12), 1283–1293. [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H. , Oxman, A. D. , Kunz, R. , Woodcock, J. , Brozek, J. , Helfand, M. , Alonso‐Coello, P. , Falck‐Ytter, Y. , Jaeschke, R. , Akl, E. A. , Post, P. N. , Norris, S. , Meerpohl, J. , Shukla, V. K. , Nasser, M. , Schünemann, H. J. , Vist, G. , & GRADE Working Group . (2011). GRADE guidelines: 8. Rating the quality of evidence—Indirectness. Journal of Clinical Epidemiology, 64(12), 1303–1310. [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H. , Oxman, A. D. , Kunz, R. , Woodcock, J. , Brozek, J. , Helfand, M. , Alonso‐Coello, P. , Glasziou, P. , Jaeschke, R. , Norris, S. , Vist, G. , Dahm, P. , Shukla, V. K. , Higgins, J. , Falck‐Ytter, Y. , Schünemann, H. J. , Akl, E. A. , & GRADE Working Group . (2011). GRADE guidelines: 7. Rating the quality of evidence—Inconsistency. Journal of Clinical Epidemiology, 64(12), 1294–1302. [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H. , Oxman, A. D. , Montori, V. , Vist, G. , Kunz, R. , Brozek, J. , Alonso‐Coello, P. , Djulbegovic, B. , Atkins, D. , Williams, J. W., Jr. , Meerpohl, J. , Norris, S. L. , Akl, E. A. , Schünemann, H. J. , & Falck‐Ytter, Y. (2011). GRADE guidelines: 5. Rating the quality of evidence—Publication bias. Journal of Clinical Epidemiology, 64(12), 1277–1282. [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H. , Oxman, A. D. , Vist, G. , Kunz, R. , Brozek, J. , Alonso‐Coello, P. , Montori, V. , Akl, E. A. , Djulbegovic, B. , Norris, S. L. , Williams, J. W., Jr. , Atkins, D. , Meerpohl, J. , Schünemann, H. J. , & Falck‐Ytter, Y. (2011). GRADE guidelines: 4. Rating the quality of evidence—Study limitations (risk of bias). Journal of Clinical Epidemiology, 64(4), 407–415. [DOI] [PubMed] [Google Scholar]
- Higgins, J. , Jackson, D. , Barrett, J. , Lu, G. , Ades, A. , & White, I. (2012). Consistency and inconsistency in network meta‐analysis: Concepts and models for multi‐arm studies. Research Synthesis Methods, 3(2), 98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M. J. , & Welch, V. A. (2019). Cochrane handbook for systematic reviews of interventions. John Wiley & Sons. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T. , Altman, D. G. , Gøtzsche, P. C. , Jüni, P. , Moher, D. , Oxman, A. D. , Savovic, J. , Schulz, K. F. , Weeks, L. , Cochrane Bias Methods Group, Cochrane Statistical Methods Group , & Sterne, J. A. C. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ, 343, d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain, T. , Smith, P. , & Yee, L. M. (2020). Mobile phone–based behavioral interventions in pregnancy to promote maternal and fetal health in high‐income countries: Systematic review. JMIR mHealth and uHealth, 8(5), e15111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton, B. , Salanti, G. , Caldwell, D. M. , Chaimani, A. , Schmid, C. H. , Cameron, C. , Ioannidis, J. P. , Straus, S. , Thorlund, K. , Mulrow, C. , Catalá‐López, F. , Gøtzsche, P. C. , Dickersin, K. , Boutron, I. , Altman, D. G. , Moher, D. , & Jansen, J. P. (2015). The PRISMA extension statement for reporting of systematic reviews incorporating network meta‐analyses of health care interventions: Checklist and explanations. Annals of Internal Medicine, 162(11), 777–784. [DOI] [PubMed] [Google Scholar]
- Lamont, K. , Sliwa, K. , Stewart, S. , Carrington, M. , Pretorius, S. , Libhaber, E. , Wiysonge, C. S. , Adebayo, E. F. , & Klipstein‐Grobusch, K. (2016). Short message service (SMS) as an educational tool during pregnancy: A literature review. Health Education Journal, 75(5), 540–552. [Google Scholar]
- Lee, S. H. , Nurmatov, U. B. , Nwaru, B. I. , Mukherjee, M. , Grant, L. , & Pagliari, C. (2016). Effectiveness of mHealth interventions for maternal, newborn and child health in low–and middle–income countries: Systematic review and meta–analysis. Journal of Global Health, 6(1), 10401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair, U. , Armfield, N. R. , Chatfield, M. D. , & Edirippulige, S. (2018). The effectiveness of telemedicine interventions to address maternal depression: A systematic review and meta‐analysis. Journal of Telemedicine and Telecare, 24(10), 639–650. [DOI] [PubMed] [Google Scholar]
- Ouzzani, M. , Hammady, H. , Fedorowicz, Z. , & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer, M. J. , Henschke, N. , Bergman, H. , Villanueva, G. , Maayan, N. , Tamrat, T. , Mehl, G. L. , Glenton, C. , Lewin, S. , Free, C. , & Fønhus, M. S. (2020). Targeted client communication via mobile devices for improving maternal, neonatal, and child health. Cochrane Database of Systematic Reviews, 8(8), CD013679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhan, M. A. , Schünemann, H. J. , Murad, M. H. , Li, T. , Brignardello‐Petersen, R. , Singh, J. A. , Kessels, A. G. , Guyatt, G. H. , & GRADE Working Group . (2014). A GRADE working group approach for rating the quality of treatment effect estimates from network meta‐analysis. BMJ, 349, g5630. [DOI] [PubMed] [Google Scholar]
- Rivera‐Romero, O. , Olmo, A. , Muñoz, R. , Stiefel, P. , Miranda, M. L. , & Beltrán, L. M. (2018). Mobile health solutions for hypertensive disorders in pregnancy: Scoping literature review. JMIR mHealth and uHealth, 6(5), e130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salanti, G. , Ades, A. , & Ioannidis, J. P. (2011). Graphical methods and numerical summaries for presenting results from multiple‐treatment meta‐analysis: An overview and tutorial. Journal of Clinical Epidemiology, 64(2), 163–171. [DOI] [PubMed] [Google Scholar]
- Schiavo, J. H. (2019). PROSPERO: An international register of systematic review protocols. Medical Reference Services Quarterly, 38(2), 171–180. [DOI] [PubMed] [Google Scholar]
- Sondaal, S. F. V. , Browne, J. L. , Amoakoh‐Coleman, M. , Borgstein, A. , Miltenburg, A. S. , Verwijs, M. , & Klipstein‐Grobusch, K. (2016). Assessing the effect of mHealth interventions in improving maternal and neonatal care in low‐and middle‐income countries: A systematic review. PLoS One, 11(5), e0154664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, F. , Loke, Y. K. , Walsh, T. , Glenny, A.‐M. , Eastwood, A. J. , & Altman, D. G. (2009). Methodological problems in the use of indirect comparisons for evaluating healthcare interventions: Survey of published systematic reviews. BMJ, 338, b1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolossa, T. , Fekadu, G. , Mengist, B. , Mulisa, D. , Fetensa, G. , & Bekele, D. (2020). Impact of antenatal care on neonatal mortality among neonates in Ethiopia: A systematic review and meta‐analysis. Arch Public Health, 78(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF (2019). Healthy mothers, healthy babies: Taking stock of maternal health.
- Van Den Heuvel, J. F. , Groenhof, T. K. , Veerbeek, J. H. , Van Solinge, W. W. , Lely, A. T. , Franx, A. , & Bekker, M. N. (2018). eHealth as the next‐generation perinatal care: An overview of the literature. Journal of Medical Internet Research, 20(6), e202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora, C. G. , Bahl, R. , Barros, A. J. , França, G. V. , Horton, S. , Krasevec, J. , Murch, S. , Sankar, M. J. , Walker, N. , Rollins, N. C. , & Lancet Breastfeeding Series Group . (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387(10017), 475–490. [DOI] [PubMed] [Google Scholar]
- Vodopivec‐Jamsek, V. , de Jongh, T. , Gurol‐Urganci, I. , Atun, R. , & Car, J. (2012). Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews, 12(12), CD007457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagnew, F. , Dessie, G. , Alebel, A. , Mulugeta, H. , Belay, Y. A. , & Abajobir, A. A. (2018). Does short message service improve focused antenatal care visit and skilled birth attendance? A systematic review and meta‐analysis of randomized clinical trials. Reproductive Health, 15(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, I. R. , Barrett, J. K. , Jackson, D. , & Higgins, J. P. (2012). Consistency and inconsistency in network meta‐analysis: Model estimation using multivariate meta‐regression. Research Synthesis Methods, 3(2), 111–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2011). mHealth: New horizons for health through mobile technologies. World Health Organization. [Google Scholar]
- WHO . (2019a). Trends in maternal mortality 2000 to 2017: Estimates by WHO. UNICEF, UNFPA, World Bank Group and the United Nations Population Division. [Google Scholar]
- WHO . (2019b). WHO guideline: Recommendations on digital interventions for health system strengthening. World Health Organization. [PubMed] [Google Scholar]
- WHO . (2021a). Children: Improving survival and well‐being. World Health Organization. https://www.who.int/news‐room/fact‐sheets/detail/children‐reducing‐mortality [Google Scholar]
- WHO . (2021b). eHealth. World Health Organization. https://www.who.int/ehealth/about/en/ [Google Scholar]
- WHO . (2021c). Maternal mortality. World Health Organization. https://www.who.int/news‐room/fact‐sheets/detail/maternal‐mortality [Google Scholar]
- World Bank . (2019). Country and lending groups. World Bank. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519‐world‐bank‐country‐and‐lending‐groups [Google Scholar]
- Yakoob, M. Y. , Ali, M. A. , Ali, M. U. , Imdad, A. , Lawn, J. E. , Van Den Broek, N. , & Bhutta, Z. A. (2011). The effect of providing skilled birth attendance and emergency obstetric care in preventing stillbirths. BMC Public Health, 11(3), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
No additional data available


