Abstract
Background
Western parents swaddle infants to promote sleep and reduce night-waking, however recent evidence of the effects of swaddling on the sleep of healthy infants has not been systematically reviewed.
Objective
To investigate the effect of swaddling on the sleep of infants up to 1 year of age using a narrative synthesis approach.
Data Sources
We systematically searched five academic databases, including the Cochrane trial registry (Pubmed, PsycINFO, Embase, the Cochrane library, and Blackwell Synergy). We manually searched reference lists and citations of included studies and reference lists of existing reviews.
Study Selection
Studies of any type, published since 2007, reporting primary data whose subjects were humans up to 12 months of age with outcome measures relating to the impact of swaddling on sleep and arousal.
Data Extraction
By hand using a customized template. A narrative synthesis is used to present the results.
Results
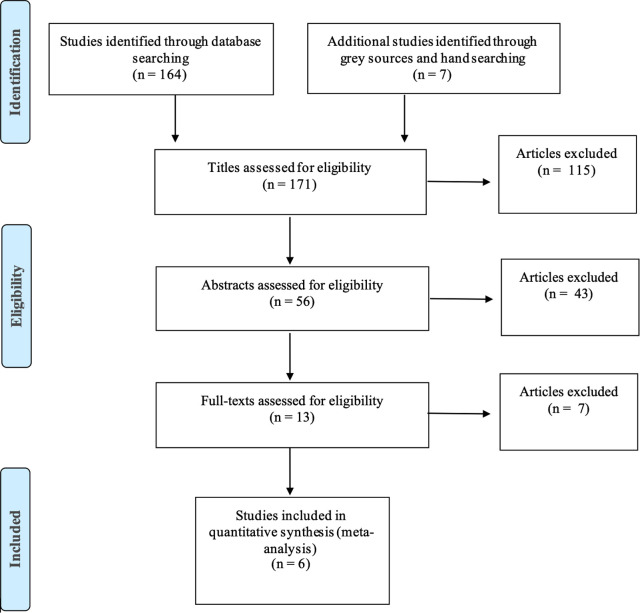
In total 171 studies were retrieved with 115 studies discarded at title. A further 43 were discarded at abstract, and six were discarded at full text. Two papers were combined as they reported on the same study giving a total of 6 studies that met the inclusion criteria for the review. An evidence hierarchy was used to assess Risk of Bias in the included studies; the results are presented via a narrative synthesis. Swaddling was associated with increased duration of quiet sleep in infants and a significantly reduced number of sleep state changes among infants naïve to the intervention.
Limitations
The integrity of the intervention (swaddling) including its baseline characteristics, was defined broadly across the included studies limiting the interpretation and transferability of the results of this review.
Conclusions
Swaddling appears to increase quiet sleep duration in infants and reduces the number of sleep state changes among infants naïve to the intervention. Parents should be made aware that implementing conditions unfavorable to arousability may increase SUDI risk among infant who have not previously been swaddled. This review has relevance for informing future practice recommendations and parent advice as well as in designing future studies.
Keywords: infant care [methods], infant sleep, parenting (MeSH), sleep duration, arousal
Introduction
To explore the effect of swaddling on infant sleep and arousal in infants under 12 months of age we conducted a systematic review of the evidence published over the past 15 years since the review of van Sleuwen et al. (1). This previous review concluded that swaddling infants above the waist increased sleep duration, reduced motor activity and startles, and lowered heart rate, however swaddling was not found to affect the capacity of the infant to respond to stimulation with less-intense auditory stimulation arousing swaddled infants more effectively than non-swaddled infants. The previous review highlighted “the difference in the physiologic effect of swaddling in QS [quiet sleep] and AS [active sleep]” as an avenue requiring more research (1: e1106). Nelson (2) also conducted a systematic review of swaddling to inform nursing practice, however this did not examine effects on infant sleep and arousal. In their meta-analysis, Pease et al. (3) found evidence to suggest risk of SIDS (a subset of SUDI) increases with infant age when infants are swaddled. They identified a twofold risk for infants aged >6 months. However, their review was limited to “SIDS” as an outcome measure, with no measure of sleep and/or arousal processes. The present review sought to fill these knowledge deficits by answering the question, what is the effect of swaddling on infant sleep and arousal? In developing the literature search strategy, we used the PICO framework to ensure comprehensive and bias-free searches.
POPULATION: Infants aged < 1 year.
INTERVENTION: Swaddling.
COMPARISON: Not swaddling.
OUTCOMES: Effects on sleep and arousal.
Review protocol
Our search aimed to identify studies of any type reporting primary data for human infants <1 year of age, whose outcome measures included information on the impact of swaddling on sleep and arousal. Abstracts were screened by both authors. Studies were excluded if they only examined infants born prematurely (gestational age < 37 weeks), featured a primary intervention other than swaddling, were published before 2007, or were not published in English. To maximise inclusion of relevant studies qualitative and quantitative studies from a range of disciplines were included. This mixed-methods approach is thought to provide a more complete basis for complex clinical and policy decision-making than that currently offered by single method reviews (4). It was particularly appropriate for the present review question, as swaddling is not only a physiological intervention but also a social one; its application differs across and within cultures according to numerous diverse factors such as tradition, health professional advice, policy recommendations, fashion and personality (5–8). The objective of this mixed-methods approach is therefore to integrate a quantitative estimation of swaddling's “effectiveness” via measures of infant sleep duration and arousal, with a more qualitative understanding from the perspective of the implementers of the intervention (usually parents), increasing the relevance of the review for policy and practice.
Search strategy
Our systematic search identified studies published from 2007 to March 2022 covering the same electronic databases as the 2007 review: Pubmed, PsycINFO, Embase, the Cochrane library, and Blackwell Synergy. The search terms used are shown in Table 1. Following standard guidelines for systematic reviews (9) leading journals were hand searched as were the reference lists of those studies meeting the inclusion criteria. Due to lack of resources to undertake translation searches were restricted to English language material. We included all papers that identified any effects of swaddling on infant sleep and arousal even if this topic was not the primary purpose of the paper.
Table 1.
Search terms used in systematically searching the literature.
| Terms and truncations | Terms to be captured in search |
|---|---|
| infan* OR baby* OR babies OR newborn* OR neonat* | to include infant, infants, baby, baby's, babies, newborn, newborns, neonate, neonatal |
| AND sleep* OR arous* | sleep, sleeping, arouse, arousal, arousing |
| AND swaddl* OR restrain* OR wrap* | swaddle, swaddling, swaddled, restrain, restrained, restraining, wrap, wrapping, wrapped |
Data extraction and appraisal
After screening, the first author worked independently to extract data from the included papers. All papers that met the inclusion criteria were read in full, with data extracted by hand using a customized template (Supplementary Appendix 1) (10). Mindful that “the effect of swaddling may be somehow mediated through the modified sleep characteristics in the infants” (11, 12) the data extraction template included factors associated with modified sleep behaviour, such as environmental temperature (9, 13, 14), nocturnal or diurnal setting (15–17) and feeding method (18). Study authors were contacted in cases where information was missing. An appraisal form was used (Supplementary Appendix 2) to assess the quality of each study in terms of internal and external validity.
Results (narrative synthesis)
In reporting the findings of a systematic mixed-methods review narrative synthesis is an effective approach for explaining potentially conflicting outcomes. Where contradictions arose, our goal was to ascertain epistemological explanations.
Preliminary synthesis
An initial list of 171 studies was retrieved from the initial searches. Studies were assessed against the inclusion criteria with 115 discarded following title review. A further 43 were discarded following a review of abstracts, and 7 were discarded following review of full text. At each stage reviews were conducted by the first author and verified by the second author with discussion of any discrepancies. Where two publications reported on the same study (19, 20) (confirmed by contacting authors) the information extracted was combined as a single study (20), meaning 6 studies met the inclusion criteria (see Figure 1).
Figure 1.
PRISMA flow diagram.
The six studies that met the inclusion criteria all used swaddling as their primary intervention and measured infant sleep and arousal outcomes, but varied in their approach to study design and setting. Richardson et al. (20), Meyer and Erler (21), and Narangerel et al. (22) each sought to evaluate the effects of swaddling on different stages of infant arousability, although Narangerel et al. (22) narrowed their focus to respiratory rate and oxygen saturation. The remaining studies, sought to ascertain the effects of swaddling on the temporal nature of infant sleep and arousal. Three studies (20–22) used clinical measures such as polysomnography to assess sleep and arousal while the other three studies (11, 23, 24) were conducted in a home setting and used participant self-report instruments (see Table 2).
Table 2.
Summary of study designs and key variables.
| Richardson et al 2010 | Narangerel et al 2007 | Meyer and Erler 2011 | McRury and Zolotor 2010 | Kelmanson 2013 | Öztürk and Bayik 2019 | |
|---|---|---|---|---|---|---|
| Randomised controlled trial | X | X | ||||
| Quasi-experimental | X | X | X | X | ||
| Outcomes assessed by | Objective measurement | Objective measurement | Objective measurement | Self report | Self report | Self report |
| Period of sleep (nocturnal or diurnal) stated | X | X | X | X | X | |
| Study environment | Lab | Home | Lab | Home | Home | Home |
| Swaddle technique detailed | X | X | ||||
| Environmental temperature detailed | X | X | ||||
| Feeding method detailed | X | X | ||||
| Swaddle tightness measured |
The main findings identified from two clinical studies (20, 21) and one self-report study (24) were that swaddling of infants naïve to the intervention was associated with decreased arousal and increased sleep duration. These findings were consistent across nocturnal and diurnal sleep periods. However, two self-report studies did not report any difference in duration of crying or sleeping as a result of swaddling (23) or of any effect of swaddling upon “infant sleep disturbances” (11). The remaining clinical study (22) did not report any measurable effect of swaddling on SaO2 or respiratory rates. The authors of two studies (22, 23) cited Type II Errors as explanations for not reporting significant outcomes.
Discrepancies between studies
A key factor explaining the discrepancy between study outcomes is the study environment. Two of the three studies detecting measurable outcomes for swaddling (20, 21) were conducted in the controlled environments of sleep laboratories. Those studies that did not report measurable outcomes were conducted in home settings. The only home study to report a measurable outcome (24) did not isolate swaddling but combined it with other interventions simultaneously (holding on side or stomach, shushing, and swinging).
Study population characteristics may also explain the heterogeneity in findings. Narangerel et al. (22) compared swaddled to non-swaddled infants, but did not report whether the swaddled infants were habituated or naïve (unaccustomed) to swaddling. While Richardson et al. (20) found significant outcomes for sleep and arousal in infants naïve to swaddling, this study did not report a significant outcome for routinely swaddled infants. Kelmanson (11) focused only on routinely swaddled infants and did not report significant sleep outcomes. The habituated vs. naïve dichotomy may also explain why McRury and Zolotor (23) did not report significant outcomes, however the latter study did not verify whether the intervention was actually applied. Mothers in the intervention group may have decided against using the intervention, while those who implemented it may have done so using different techniques.
Differences in data collection methods (physiological vs. self-report measures) may also account for the inconsistent outcomes. The self-report studies used bespoke questionnaires (11) and diary methods (23, 24). These are vulnerable to the subjective perceptions of the participants, making it difficult to combine and synthesise the results with those of the other studies. They highlighted a strong discrepancy between maternal perceptions of swaddling effectiveness and physiological markers of effectiveness. Thus, if a sensitivity analysis was conducted in which self-report studies were excluded from the review, swaddling would appear to have an impact upon sleep and arousal in naïve infants. That Narangerel et al. (22), a physiological study whose sample consisted entirely of routinely swaddled infants, did not report significant outcomes would support this hypothesis.
Robustness of the synthesis
Evidence hierarchy is often used to assess the quality of intervention studies (25). The first author independently applied the hierarchy to determine the appropriateness of study designs for assessing questions of “effectiveness”. In applying this approach to the question of swaddling effectiveness, two studies (11, 23) would be designated “poor quality” in terms of measures of effectiveness, being qualitative studies considered more susceptible to bias than the quasi-experimental studies (20, 22). The randomized trial (21), designated at the top of the hierarchy, would be deemed most robust. However, the objectives of each study are too dissimilar to synthesize in this manner. Narangerel et al. (22) is a particular outlier, focusing specifically on respiratory rate and oxygen saturation, while the other studies examined sleep and arousal more broadly, including maternal perception of swaddling effectiveness.
Varying degrees of confounding were evident across all studies. Only Richardson et al. (20) and Narangerel et al. (22) reduced contamination by accounting for environmental temperature, for instance, which is known to significantly modify an infant's cardiorespiratory and autonomic parameters (26). Moreover, only two studies (20, 24) ascertained infant feeding method. Whether an infant is breast or bottle fed is considered a strong moderating variable with regard to sleep fragmentation (27–29). Potential differences in such important baseline characteristics reduce internal validity (30).
The weakest study in relation to confounding was that of Narangerel et al. (22) which not only failed to allocate participants randomly but also failed to ascertain infant feeding method and whether the sleep studied was nocturnal, diurnal or both. An investigation of sleep and arousal cannot be effective when analyzed in isolation from these key factors (31, 32).
Selection bias
For most of the included studies it was unclear whether true randomization had been conducted reflecting previous critiques that randomization is inadequately described in most published studies (33–36). Additionally two studies (23, 24) used a recruitment technique that biased the pool of participants towards certain demographics, namely educated, western mothers giving birth in a hospital setting. One study (23) required participants to have “the resources to play a VHS tape/CD at home” and to “contact a research assistant by phone” before being discharged from hospital. Further, mothers who did not speak English or were unable to fill out a diary themselves were excluded. The generalizability of McRury and Zolotor (23) was further weakened by the relatively high attrition rate of 31%. The tendency to drop-out has been associated with ethnicity and low academic achievement (37–39).
Allocation bias
With regard to allocation bias, those studies which utilized randomization (20, 21, 23, 24) also used comparison groups that were balanced at baseline and thus distributed possible confounding factors evenly. McRury and Zolotor (23) was the strongest study in this respect, being the only one to blind the researchers to control and intervention groups, and to compare demographic and baseline characteristics of the intervention and control participants.
Two studies (11, 22) allocated infants to predefined “natural” intervention and control groups. The outcomes of these studies cannot be confidently attributed to the intervention as their non-randomized nature may have encouraged a tendency to over-estimate effect sizes (40).
However, the greatest threat to the robustness of the synthesis involves the integrity of the intervention. This was problematic across all studies, and it is unclear whether the interventions were similar enough to synthesize: Narangerel et al. (22) for instance, gave a very brief description of the swaddle technique used, namely “two or three layers of cloth that enclosed the trunk and arms up to infant's neck”. Where swaddle technique was described, three (20–22) enclosed the infants' arms within the swaddle. This detail is important as previous research suggests infants swaddled with arms free experience the same startle frequency as unswaddled infants (7). Arm restraint therefore appears to be integral to the effectiveness of the swaddling intervention. The weakest studies, and those most at risk of Type III error, were those lacking any description of swaddle technique (11, 23). While Richardson et al. (20) and Meyer and Erler (21) describe their swaddle techniques in some detail, they along with all other studies, failed to measure or control for swaddle tightness–another important moderating variable discussed below. Richardson et al. (20) merely stated that the infants were “firmly” wrapped.
Discussion and recommendations
The most contentious factors arising from this review are habituation, sleep stages, sleep environment, swaddle technique and swaddle tightness.
Habituation (routine vs. non-routine swaddling)
Significant outcomes for swaddling were only detected in non-routinely swaddled infants (20, 21). When samples involved only routinely swaddled infants significant changes in sleep and arousal were not detected (11). The application of routine vs. non-routine sleep interventions has important implications for infant physiology, and therefore health policy. In support of this finding non-routinely swaddled infants have been shown to exhibit higher arousal thresholds (41) and less spontaneous arousability in AS (20), both considered risk factors for SIDS (42). Future studies should further explore habituation to swaddling.
Sleep states
To date, a largely neglected area of infant sleep research is the interaction between interventions and sleep architecture (changes in sleep states). This review indicates that swaddling significantly reduces the frequency of infant sleep state changes, promoting quiet sleep and sleep efficiency (21).
Previous research has associated a deficiency in acethecholine brain receptors with insufficient arousal (43, 44). It is possible that swaddling, by decreasing the type and number of arousals, may exacerbate this. Furthermore, the arousal threshold from quiet sleep is greater than that from active sleep (21). By promoting greater duration of quiet sleep at a time when arousal mechanisms are underdeveloped, swaddling may impair an infant's ability to handle a regulatory crisis, such as prolonged apnea. Future research should therefore examine the effect of swaddling on the sequence and duration of infant sleep states.
Sleep environment
Both studies conducted in sleep laboratories (20, 21) found swaddling to have measurable outcomes, and there is evidence from other sleep studies that the study environment is an important moderating variable (45). For instance, swaddled infants have been shown to demonstrate increased responsiveness to environmental auditory stress compared to the unswaddled condition (46). Another facet of environment, bedsharing, has also been shown to influence infant sleep and arousal (28, 29, 47). Bedsharing infants experience significantly less time in deep sleep and significantly more shifts in sleep stages than solitary sleeping infants (48). Despite these factors, none of the studies in the present review detailed whether bedsharing or co-sleeping (parent sharing room with infant) was a factor considered in their analysis.
Swaddle tightness
Motor restraint is a key component of swaddling, fundamental to the intervention. It has been suggested that the sedative effects of swaddling are “triggered by very specific stimuli delivered above a certain threshold” (37, 49). This threshold may, in part, be determined by tightness. Indeed, the decreased arousability procured through swaddling is unlikely to be explained merely by the material's constant stimulation of the skin and thermal receptors, as one study in the review (20) controlled for these factors and still found decreased arousability in swaddled infants. Yet despite the potential importance of swaddle tightness, none of the studies attempted to measure or control it, weakening the value of the studies reviewed. Swaddle tightness is an elusive variable, not only across swaddling studies, but also within health policy. Australian guidelines (12) advise that swaddles “should be firm, to prevent loose wrapping becoming loose bedding. However, the wrap should not be too tight and must allow for hip and chest wall movement.” “New guidance from the American Academy of Pediatrics does not mention tightness at all (50). Earlier guidance provided slightly more detail: The swaddle should not be too tight or make it hard for your baby to breathe or move their hips” (51).
That swaddled infants demonstrate heightened responsiveness to environmental auditory stress (26, 46) supports the hypothesis that tightness may be an important factor in the effectiveness of swaddling. It is possible, for instance, that the tightness of the swaddle numbs tactile sensory receptors prompting a compensatory increase in auditory sensory reception.
There is also evidence to suggest that swaddle tightness may impact cardiorespiratory function. This has implications for SIDS, as abnormalities in cardiorespiratory function have been shown to impact the arousal response needed to regulate breathing (41, 52, 53). Unless very loose, swaddling increases thoracic compression (54) which leads to a reduction in oxygen saturation and a consequent increase in respiratory rate and cardiac activity (21). These physiological changes may explain why swaddling has been associated with an increased risk of acute respiratory infection (1, 55). The finding that swaddling has little or no effect on respiratory rate applies only to routinely swaddled infants (22) contrasting with earlier studies (56) and with the previous review (1). The implications of this are important as impaired respiratory and heart rates are associated with arousal difficulties, a key mechanism proposed in the triggering of SIDS (41). An investigation which explicitly examines swaddle tightness would therefore be of benefit, particularly with regard to the formation of policy guidelines for cardio-respiratory compromised infants.
Limitation of review
Only six studies met the inclusion criteria, and no consistent outcomes were revealed. As the integrity of the intervention varied across all studies reviewed, including baseline characteristics, interpretation and transferability of the results should be treated with caution.
Conclusions
Swaddling was a complex intervention to systematically review due to the variable nature of its application, and the considerable heterogeneity across studies regarding participant characteristics (e.g., feeding method), environment (e.g., laboratory or home) and outcomes measured (e.g., sleep, arousal, or facets of both). By combining physiological and self-report studies, this review provides an understanding of swaddling under differing research conditions.
This review supports the possibility that, by producing conditions unfavorable to arousability, swaddling may increase SIDS risk in infants that are naïve to the experience (3, 20). This argument is strengthened by the finding that swaddling significantly reduces the frequency of sleep state transitions and promotes quiet sleep. Given that swaddling is typically used during the critical period in which infants are most vulnerable to SIDS, namely <6 months of age (52, 57) further research into the effect of swaddling on infant sleep and arousal, particularly for swaddle-naïve infants, is strongly recommended.
Funding
This study was funded by an Economic and Social Research Council Doctoral Studentship to the first author (Grant Ref: ES/J500082/1).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
AD conceptualised the study, AD & HB obtained funding, AD designed and conducted the review, HB verified inclusion, AD & HB discussed outcomes, drafted and edited manuscript, and approved the final version. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fped.2022.1000180/full#supplementary-material.
References
- 1.Van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TW, L'Hoir MP. Swaddling: a systematic review. Pediatrics. (2007) 120(4):e1097–106. 10.1542/peds.2006-2083 [DOI] [PubMed] [Google Scholar]
- 2.Nelson AM. Risks and benefits of swaddling healthy infants: an integrative review. MCN: Am J Matern/Child Nurs. (2017) 42(4):216–25. 10.1097/NMC.0000000000000344 [DOI] [PubMed] [Google Scholar]
- 3.Pease AS, Fleming PJ, Hauck FR, Moon RY, Horne RS, L’Hoir MP, et al. Swaddling and the risk of sudden infant death syndrome: a meta-analysis. Pediatrics. (2016) 137(6):e20153275. 10.1542/peds.2015-3275 [DOI] [PubMed] [Google Scholar]
- 4.Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth. (2020) 18(10):2108–18. 10.11124/JBISRIR-D-19-00169 [DOI] [PubMed] [Google Scholar]
- 5.Garg P, Eastwood J, Liaw S, Jalaludin B, Grace R. A case study of well child care visits at general practices in a region of disadvantage in Sydney. PLoS One. (2018) 11(10):e0205235. 10.1371/journal.pone.0205235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LeVine RA. Anthropology and child development: A cross-cultural reader. London: Blackwell; (2008). [Google Scholar]
- 7.Lipton EL. Swaddling, A child care practice: historical, cultural, and experimental observations. Pediatrics. (1965) 35(3):521–67. 10.1542/peds.35.3.521 [DOI] [PubMed] [Google Scholar]
- 8.Moss J. Swaddling then, there and now: historical, anthropological and current practices. Matern Child Nurs J. (1979) 8(3):137–51. [PubMed] [Google Scholar]
- 9.Anders TF. Infant sleep, nighttime relationships, and attachment. Psychiatry. (1994) 57(1):11–21. 10.1080/00332747.1994.11024664 [DOI] [PubMed] [Google Scholar]
- 10.Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. (2012) 22(10):1435–43. 10.1177/1049732312452938 [DOI] [PubMed] [Google Scholar]
- 11.Kelmanson I. Swaddling: maternal option and sleep behaviour in two-month-old infants. Child Care Pract. (2013) 19(1):36–48. 10.1080/13575279.2012.712035 [DOI] [Google Scholar]
- 12.Red Nose. National Scientific Advisory Group. Information Statement: Wrapping or swaddling babies. Melbourne, Red Nose. https://rednose.org.au/downloads/Wrapping_Babies-Safe_Sleeping-Information_Statement_Nov_2017_WEB.pdf (2017).
- 13.Franco P, Szliwowski H, Dramaix M, Kahn A. Influence of ambient temperature on sleep characteristics and autonomic nervous control in healthy infants. Sleep. (2000) 23(3):401–7. [PubMed] [Google Scholar]
- 14.McGraw K, Hoffmann R, Harker C, Herman JH. The development of circadian rhythms in a human infant. Sleep. (1999) 22(3):303–10. 10.1093/sleep/22.3.303 [DOI] [PubMed] [Google Scholar]
- 15.Freudigman K, Thoman EB. Ultradian and diurnal cyclicity in the sleep states of newborn infants during the first two postnatal days. Early Hum Dev. (1994) 38(2):67–80. 10.1016/0378-3782(94)90218-6 [DOI] [PubMed] [Google Scholar]
- 16.Henderson JM, France KG, Blampied NM. The consolidation of infants’ nocturnal sleep across the first year of life. Sleep Med Rev. (2011) 15(4):211–20. 10.1016/j.smrv.2010.08.003 [DOI] [PubMed] [Google Scholar]
- 17.Thoman EB, Whitney MP. Sleep states of infants monitored in the home: individual differences, developmental trends, and origins of diurnal cyclicity. Infant Behav Dev. (1989) 12(1):59–75. 10.1016/0163-6383(89)90053-2 [DOI] [Google Scholar]
- 18.Elias MF, Nicholson NA, Konner M. Two sub-cultures of maternal care in the United States. In: Taub DM, King FA, editors. Current perspectives in primate social dynamics. New York: Van Nostrand Reinhold; (1986). p. 37–50. [Google Scholar]
- 19.Richardson HL, Walker AM, Horne RS. Minimizing the risks of sudden infant death syndrome: to swaddle or not to swaddle? J Pediatr. (2009) 155(4):475–81. 10.1016/j.jpeds.2009.03.043 [DOI] [PubMed] [Google Scholar]
- 20.Richardson HL, Walker AM, Horne RS. Influence of swaddling experience on spontaneous arousal patterns and autonomic control in sleeping infants. J Pediatr. (2010) 157(1):85–91. 10.1016/j.jpeds.2010.01.005 [DOI] [PubMed] [Google Scholar]
- 21.Meyer LE, Erler T. Swaddling: a traditional care method rediscovered. World J Pediatr. (2011) 7(2):155–60. 10.1007/s12519-011-0268-6 [DOI] [PubMed] [Google Scholar]
- 22.Narangerel G, Pollock J, Manaseki-Holland S, Henderson J. The effects of swaddling on oxygen saturation and respiratory rate of healthy infants in Mongolia. Acta Paediatr. (2007) 96(2):261–5. 10.1111/j.1651-2227.2007.00123.x [DOI] [PubMed] [Google Scholar]
- 23.McRury JM, Zolotor AJ. A randomized, controlled trial of a behavioral intervention to reduce crying among infants. J Am Board Fam Med. (2010) 23(3):315–22. 10.3122/jabfm.2010.03.090142 [DOI] [PubMed] [Google Scholar]
- 24.Öztürk Dönmez R, Bayik Temel A. Effect of soothing techniques on infants’ self-regulation behaviors (sleeping, crying, feeding): a randomized controlled study. Randomized Control Trial Jpn J Nurs Sci. (2019) 16(4):407–19. 10.1111/jjns.12250 [DOI] [PubMed] [Google Scholar]
- 25.Cuyatt GH, Haynes MRB, Cook DJ, Green ML, Wilson MC, Richardson WS. Users’ guides to the medical literature XXV. Evidence-based medicine: principles for applying. JAMA. (2000) 284(10):1290–6. 10.1001/jama.284.10.1290 [DOI] [PubMed] [Google Scholar]
- 26.Franco P, Seret N, Van Hees JN, Scaillet S, Groswasser J, Kahn A. Influence of swaddling on sleep and arousal characteristics of healthy infants. Pediatrics. (2005) 115(5):1307–11. 10.1542/peds.2004-1460 [DOI] [PubMed] [Google Scholar]
- 27.Horne RSC, Parslow PM, Ferens D, Watts AM, Adamson TM. Comparison of evoked arousability in breast and formula fed infants. Arch Dis Child. (2004) 89(1):22–5. [PMC free article] [PubMed] [Google Scholar]
- 28.McKenna JJ, Mosko S, Dungy C, McAninch J. Sleep and arousal patterns of co-sleeping human mother/infant pairs: a preliminary physiological study with implications for the study of sudden infant death syndrome (SIDS). Am J Phys Anthropol. (1990) 83(3):331–47. 10.1002/ajpa.1330830307 [DOI] [PubMed] [Google Scholar]
- 29.Quillin SI, Glenn LL. Interaction between feeding method and co-sleeping on maternal-newborn sleep. J Obstet Gynecol Neonatal Nurs. (2004) 33(5):580–8. 10.1177/0884217504269013 [DOI] [PubMed] [Google Scholar]
- 30.Clarke M, Oxman A. Cochrane reviewers’ handbook. The Cochrane Collaboration (2003). version 4.2. 0. https://www.iecs.org.ar/cochrane/guias/Handbook_4-2-2.pdf [Google Scholar]
- 31.McKenna J. Sudden infant death syndrome: infant sleep, breastfeeding, and infant sleeping arrangements. In: Ember CR, Ember M, editors. Encyclopedia of medical anthropology. Health and illness in the World's Cultures. New York: Kluver Academic (Plenum Publishers) (2004). p. 506–17. [Google Scholar]
- 32.McKenna JJ, Ball HL, Gettler LT. Mother–infant cosleeping, breastfeeding and sudden infant death syndrome: what biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Am J Phys Anthropol. (2007) 134(S45):133–61. 10.1002/ajpa.20736 [DOI] [PubMed] [Google Scholar]
- 33.Altman DG, Dore CJ. Randomisation and baseline comparisons in clinical trials. Lancet. (1990) 335(8682):149–53. 10.1016/0140-6736(90)90014-V [DOI] [PubMed] [Google Scholar]
- 34.Meade MO, Richardson WS. Selecting and appraising studies for a systematic review. Ann Intern Med. (1997) 127(7):531–7. 10.7326/0003-4819-127-7-199710010-00005 [DOI] [PubMed] [Google Scholar]
- 35.Schulz KF, Chalmers I, Grimes DA, Altman DG. Assessing the quality of randomization from reports of controlled trials published in obstetrics and gynecology journals. Jama. (1994) 272(2):125–8. 10.1001/jama.1994.03520020051014 [DOI] [PubMed] [Google Scholar]
- 36.Williams DH, Davis CE. Reporting of assignment methods in clinical trials. Control Clin Trials. (1994) 15(4):294–8. 10.1016/0197-2456(94)90045-0 [DOI] [PubMed] [Google Scholar]
- 37.Krishnan E, Murtagh K, Bruce B, Cline D, Singh G, Fries JF. Attrition bias in rheumatoid arthritis databanks: a case study of 6346 patients in 11 databanks and 65,649 administrations of the Health Assessment Questionnaire. J Rheumatol. (2004) 31(7):1320–6. [PubMed] [Google Scholar]
- 38.Matthews FE, Chatfield M, Freeman C, McCracken C, Brayne C, Cfas MRC. Attrition and bias in the MRC cognitive function and ageing study: an epidemiological investigation. BMC Public Health. (2004) 4(1):1–10. 10.1186/1471-2458-4-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Siddiqui O, Flay BR, Hu FB. Factors affecting attrition in a longitudinal smoking prevention study. Prev Med. (1996) 25(5):554–60. 10.1006/pmed.1996.0089 [DOI] [PubMed] [Google Scholar]
- 40.NHS Centre for Reviews and Dissemination,. Undertaking systematic reviews of research on effectiveness: CRD's guidance for those carrying out or commissioning reviews. CRD report Number 4 (2001).
- 41.Harper R, Kinney HC. Potential mechanisms of failure in the sudden infant death syndrome. Curr Pediatr Rev. (2010) 6(1):39–47. 10.2174/157339610791317214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harper RM. Sudden infant death syndrome: a failure of compensatory cerebellar mechanisms? Pediatr Res. (2000) 48(2):140–2. 10.1203/00006450-200008000-00004 [DOI] [PubMed] [Google Scholar]
- 43.Harrington CT, Al Hafid N, Waters KA. Butyrylcholinesterase is a potential biomarker for sudden infant death syndrome. EBioMedicine. (2022) 80:104041. 10.1016/j.ebiom.2022.104041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mosko S, Richard C, McKenna J, Drummond S. Infant sleep architecture during bedsharing and possible implications for SIDS. Sleep. (1996) 19(9):677–84. 10.1093/sleep/19.9.677 [DOI] [PubMed] [Google Scholar]
- 45.Baddock SA, Purnell MT, Blair PS, Pease AS, Elder DE, Galland BC. The influence of bed-sharing on infant physiology, breastfeeding and behaviour: a systematic review. Sleep Med Rev. (2019) 43:106–17. 10.1016/j.smrv.2018.10.007 [DOI] [PubMed] [Google Scholar]
- 46.Franco P, Scaillet S, Groswasser J, Kahn A. Increased cardiac autonomic responses to auditory challenges in swaddled infants. Sleep. (2004) 27(8):1527–32. 10.1093/sleep/27.8.1527 [DOI] [PubMed] [Google Scholar]
- 47.Worthman CM, Brown RA. Companionable sleep: social regulation of sleep and cosleeping in Egyptian families. J Fam Psychol. (2007) 21(1):124. 10.1037/0893-3200.21.1.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McKenna JJ, Bernshaw NJ. Breast-feeding and infant–parent co-sleeping as adaptive strategies: are they protective against SIDS? In: Stuart-Macadam P, Dettwyler K, editors. Breastfeeding: Biocultural Perspectives. New York: Aldine de Gruyter; (1995) p. 265–305. [Google Scholar]
- 49.Karp H. The fourth trimester and the calming reflex: novel ideas for nurturing young infants. Midwifery Today Int Midwife. (2012) 102:25–6. [PubMed] [Google Scholar]
- 50.Moon RY, Carlin RF, Hand I, Task force on sudden infant death syndrome. Sleep-related infant deaths: updated 2022 recommendations for reducing infant deaths in the sleep environment. Pediatrics. (2022) 150(1):e2022057990. 10.1542/peds.2022-057990 [DOI] [PubMed] [Google Scholar]
- 51.Moon RY. How to keep your sleeping baby safe: AAP policy explained. URL = https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/A-Parents-Guide-to-Safe-Sleep.aspx (2019).
- 52.Byard R, Krous H. Sudden infant death syndrome: problems, progress and possibilities. London, UK: Arnold Hodder Headline PLC/Oxford University Press; (2001). [Google Scholar]
- 53.Kinney HC, Filiano JJ, Sleeper LA, Mandell F, Valdes-Dapena M, White WF. Decreased muscarinic receptor binding in the arcuate nucleus in sudden infant death syndrome. Science. (1995) 269(5229):1446–50. 10.1126/science.7660131 [DOI] [PubMed] [Google Scholar]
- 54.Kahn A, Rebuffat E, Sottiaux M. Effects of body movement restraint on cardiac response to auditory stimulation in sleeping infants. Acta Paediatr. (1992) 81(12):959–61. 10.1111/j.1651-2227.1992.tb12153.x [DOI] [PubMed] [Google Scholar]
- 55.Yurdakok K. Swaddling and acute respiratory infections. Am J Public Health. (1990) 80:873–5. 10.2105/AJPH.80.7.873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gerard CM, Harris KA, Thach BT. Spontaneous arousals in supine infants while swaddled and unswaddled during rapid eye movement and quiet sleep. Pediatrics. (2002) 110(6):e70. 10.1542/peds.110.6.e70 [DOI] [PubMed] [Google Scholar]
- 57.Ariagno RL, Giotzbech SF. Sudden infant dealth syndrome. In: Rudolph AM, editor. Pediatrics (19th ed). Norwalk CT (Connecticut): Appleton & Lange Norwalk; (1981). p. 850–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.