Abstract
BACKGROUND
Hypertension is the most modifiable factor associated with cardiovascular events and complications. The conventional blood pressure (BP) meter method is simple but is limited in terms of real-time monitoring abnormal BP. Therefore, the development of a multifunction smartwatch (HUAWEI WATCH D) sphygmomanometer could significantly improve integrated BP monitoring.
METHODS
We enrolled 361 subjects from Chinese PLA General Hospital, Beijing, China to validate the accuracy of the smartwatch versatile sphygmomanometer using ISO 81060-2:2018. Resting and ambulatory BP accuracy of the smartwatch were compared with gold standard clinical sphygmomanometers using ISO 81060-2:2018 guidelines, the accuracy of 24 h systolic blood pressure (SBP) circadian rhythm monitoring, and diurnal high SBP alert for this smartwatch were assessed using a confusion matrix approach. Additionally, we analyzed online users of different ages for compliance.
RESULTS
Eighty-five subjects underwent resting BP measurements; the mean resting BP differences between two devices were −0.683 ± 6.203 mmHg (SBP) (P = 0.723) and 1.628 ± 5.028 mmHg (diastolic blood pressure, DBP) (P = 0.183). In 35 subjects’ ambulatory BP measurements, the mean differences of ambulatory BP were −1.943 ± 5.475 mmHg (SBP) (P = 0.923) and 3.195 ± 5.862 mmHg (DBP) (P = 0.065). All data complied with ISO 81060-2:2018 guidelines (mean ≤ ±5 mmHg and standard deviation ≤ ±8 mmHg) with no significant differences. Positive predictive values (PPV) of resting SBP and DBP were 0.635 and 0.671, respectively. The PPV of ambulatory SBP and DBP were 0.686. Also, 24 h SBP circadian rhythm monitoring was performed in 107 subjects: accuracy = 0.850, specificity = 0.864, precision/PPV = 0.833, sensitivity = 0.833, and F1-measure (F1) = 0.833. The accuracy, specificity, precision, sensitivity, and F1 values in 85 subjects undergoing diurnal high SBP alerting were 0.858, 0.876, 0.706, 0.809, and 0.754, respectively.
CONCLUSIONS
When compared with the gold standard clinical sphygmomanometer, smartwatch results were consistent and accurate. Online user feedback showed that elderly individuals cared more about BP monitoring accuracy, with better compliance.
Hypertension is a severe chronic disease, one of the leading causes of death.[1] Globally, approximately 25% of the population over 20 years old have hypertension.[2] However, most individuals are generally unaware of hypertension and its management. In China, hypertension awareness rate is approximately 51.5%, the treatment rate is 46.1%, and the control rate is only 16.9%.[3] As multiple hypertension management guidelines have advocated clinical blood pressure (BP) measurements, out-of-office BP monitoring and BP-regulated management should be integrated.[4,5,6] However, the shortcomings of some common clinical or home sphygmomanometers cannot be neglected, e.g., they cannot continuously and automatically monitor long-term BP levels, especially during sleep, nor can they monitor masked hypertension. Also, conventional 24 h clinical automated sphygmomanometers are not convenient for frequent monitoring. As BP variability and home management are important for individualized healthcare, more comfortable, convenient, and efficient BP monitoring devices are required.[7]
The HUAWEI WATCH D is a multifunction sphygmomanometer smartwatch that is intended to measure and record BP values at resting or activity times using oscillometry technology. The smartwatch can also senselessly monitor 24 h SBP circadian rhythm, alerts users when abnormal SBP surges appear via photoplethysmogram (PPG), this non-invasive technology can detect BP senselessly on the wrist, and provide real-time BP monitoring during daily life.[8] A smartwatch providing four BP measurement approaches can help users to avoid potential cardiovascular accidents and recognize hidden hypertension.[9] A preliminary offline study of 5,000 subjects by HUAWEI confirmed algorithms based on ISO 81060-2:2018 and YY0670-2008 guidelines. Additionally, the smartwatch provides repeated heart rate, oxygen saturation, respiratory rate, and calorie measurements. Its small size and easy-to-use operation increase the requirement compliance, especially in aged populations.
In this study, we sought to validate the accuracy of four applications: (1) resting BP measurements; (2) ambulatory BP measurements; (3) 24 h SBP circadian rhythm monitoring; and (4) diurnal high SBP alerts. Moreover, 156 online users were randomly selected to review and provide feedback for this novel sphygmomanometer.
METHODS
Subjects
Subjects were enrolled at the Chinese PLA General Hospital. Subjects’ characteristics for studies were: (1) at least 85 subjects (35 in the ambulatory BP measurement study); (2) age range 18–80 years old; and (3) male/female subjects’ percentages ≥ 30%. The following were excluded: (1) individuals with arrhythmia diseases; (2) individuals with shock (BP < 90/60 mmHg); (3) individuals wearing heart-lung machines; (4) individuals with infections and bleeding tendencies in upper limbs; (5) individuals with anxiety/depression; and (6) individuals with wrist tattoos. Subjects voluntarily signed informed consent sheets before studies commenced.
Validation investigations were approved by the Ethics Committee of the Chinese PLA General Hospital, Beijing, China, and conducted according to ISO 81060-2:2018 and 2020 Chinese Hypertension League guidelines. Studies were conducted in a quiet environment and at room temperature (25 °C ± 2 °C). Written consent for studies and data use in clinical analyses was obtained from each subject.
Devices
The smartwatch (HUAWEI WATCH D) is compatible with oscillometry and PPG technologies and designed to measure BP values on the wrist using oscillometry technology. In China, the smartwatch was granted a national registration class II medical device certificate. Pressure and heart rate ranges are 0–300 mmHg and 40–180 beats/min, respectively. Both 24 h SBP circadian rhythm monitoring and diurnal high SBP alert studies were supported by PPG senseless technology. Two wrist cuff models were available: models for a wrist circumference = 13–16 cm (small) and 16.1–20 cm (medium). Data could be stored and viewed using an associated HUAWEI WATCH D application and a smartphone.
Studies
Resting BP measurement study
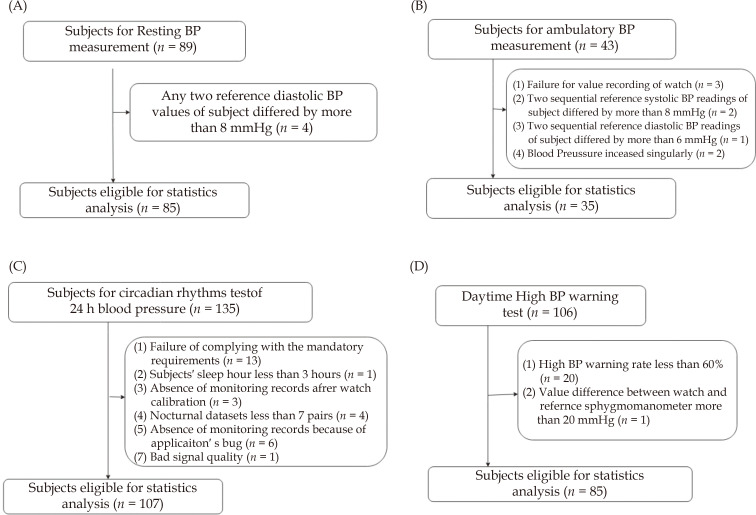
Resting BP measurement is a conventional clinical and out-of-office method. According to ISO 81060-2:2018 guidelines, 89 subjects were enrolled (Figure 1A) and measured in a sitting position. Their BP values were sequentially and alternately measured using mercury sphygmomanometers and smartwatch oscillometric measurements on the same arm at 1–3 min intervals. Two independent observers simultaneously recorded BP values using a double stethoscope mercury sphygmomanometer. Observers were blinded to each others’ BP values. Sequential processes were repeated at least 2–3 times and three valid BP data pairs from the reference and smartwatches were generated for one subject. Average values were used for accuracy analysis.
Figure 1.
Study flow diagram.
BP: blood pressure.
Ambulatory BP measurement study
According to ISO 81060-2:2018 guidelines, for a sphygmomanometer to be used in ambulatory monitoring, an additional clinical study of 35 subjects’ ambulatory BP measurements is essential. During the study, 39 subjects were enrolled (Figure 1B) and an exercise bike used to increase subject heart rates by > 15% (of resting heart rate). BP in the same arm was sequentially and alternately measured three times using mercury sphygmomanometers and smartwatch oscillometric measurements according to sequential processes in ISO 81060-2:2018 guidelines (Figure 1B). The average values of three data pairs were used for accuracy analysis.
Posture during measurements: the arm and feet were in a stable position and the watch maintained at heart level. Fingertips were gently rested on the opposite shoulder. On the exercise bike, subjects were told not to move or bend fingers during measurements. [10-12] Resting and ambulatory BP value measurements were based on smartwatch oscillometric and double stethoscope mercury sphygmomanometer measurements.
24 h SBP circadian rhythm monitoring study
Several studies have suggested that abnormal BP circadian rhythms are linked to cardiovascular diseases and cause organ damage.[13] Normally, average BP declines by 10%–20% when transitioning from waking to sleeping. This phenomenon is normal and is called “dipper”, and the nocturnal BP fall is blunted by 0%–10% called “non-dipper”. The 24 h BP circadian rhythm monitoring process was proven as a crucial clinical target forecasting the occurrence and risk of cardiovascular and renal diseases, besides office BP. [8] We enrolled 135 subjects (Figure 1C), a reference sphygmomanometer (automatic oscilliometric sphygmomanometer on the right upper arm) and smartwatch (left wrist) were used to simultaneously measure resting BP (2–3 times). The sphygmomanometer and smartwatch were worn for 24 h and automatically detected SBP at 20 min and 30 min diurnal and nocturnal intervals, respectively. The smartwatch detected 24 h SBP circadian rhythms using PPG technology and was calibrated twice a day.
Diurnal high SBP alert study
Factors influencing BP surges include exercise, emotions, and morning awakening, the sudden BP rises trigger stroke and heart failure. [8,14-17] Thus, constant BP monitoring and identifying abnormally high BP are critical. We recruited 106 volunteers to this study (Figure 1D). A reference automatic oscilliometric sphygmomanometer (right upper arm) and a smartwatch (left wrist) were used to simultaneously measure individual resting BPs (2–3 times); the mean BP value was assigned as the first data point. After standing heart rates were increased by exercises under observer guidance, post-exercise BP measurements were immediately recorded at 1 min and were designated the second data point. After 3-5 mins rest, the resting BPs were measured and termed as the third data point. This trial was repeated 1-2 times. Five paired datasets were recorded for each individual analysis. The smartwatch alert signals (via PPG) were compared to reference readings (reference sphygmomanometer SBP). SBP variations were automatically monitored (once/minute) by the smartwatch throughout the study.
Feedback analysis from online users of different ages
Growing evidence has shown that digital information and communication technologies influence universal BP diagnosis and management. Thanks to the potential benefits of digital BP management, monitoring BP variability using smartwatches, transmitting to phones, and analyzing via the internet have been proposed.[18] We randomly collected 7226 online users since the smartwatch was launched and analyzed feedback from 156 users over different age ranges.
Statistics Analyses
Resting and ambulatory BP measurement study
After resting and ambulatory BP tests, the differences of SBP and DBP were calculated separately using criteria 1 and 2 of ISO 81060-2:2018 guidelines.[19] The percentage of absolute BP differences within 5, 10, 15, and > 15 mmHg were calculated.[20] Bland-Altman plots were used to assess consistency between reference and test BPs.
24 h SBP circadian rhythm monitoring study
Valid paired smartwatch and reference sphygmomanometer datasets were generated at least once an hour, diurnal valid readings > 20 times, and nocturnal readings > 7 times. If valid readings were recorded < 20 + 7 times, then 24 h monitoring was repeated. SBP circadian rhythm calculations were performed as follows:
 |
1 |
When nocturnal SBP decline rate ≥ 10%, the rhythm was called “dipper”; when nocturnal SBP decline rate < 10%, the rhythm was called “non-dipper”. According to formula (1), we used the confusion matrix approach to estimate accuracy, precision (positive predictive value (PPV)), specificity, sensitivity, and F1 values of the Huawei smartwatch SBP circadian rhythm classification, the reference sphygmomanometer was the gold standard.[21]
Diurnal high SBP alert study
Diurnal high SBP alerts were recorded by the smartwatch when the SBP increased to 160 mmHg via exercise. Valid paired datasets were defined as the reference SBP values and smartwatch alert came out within 2 min intervals. A confusion matrix was used to estimate the accuracy, precision, specificity, sensitivity, and F1 values for this diurnal high SBP alert application.
RESULTS
Validating the Accuracy of Resting BP Measurements
Four subjects were excluded according to exclusion criteria (Figure 1A). Thus, resting BP was measured in 85 subjects with a mean age of 37 ± 14 years (range 21–70 years); and 48 males (56.5%) and 37(43.5%) males were included (Table 1S). SBP and DBP measurements were in line with ISO 81060-2:2018 guidelines, and the mean wrist circumference was 164.1 ± 17.2 mm (within the 130.0 – 196.0 mm range).
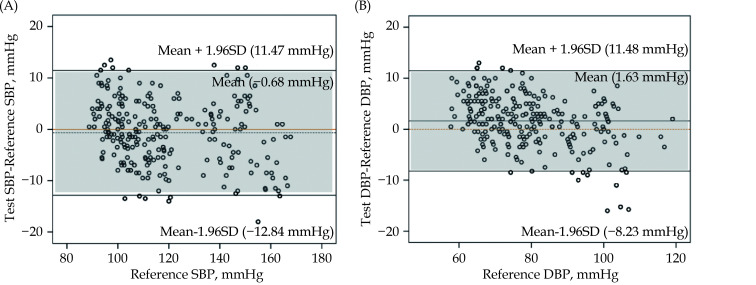
The SBP distribution of 85 subjects included SBP ≥ 160 mmHg, SBP ≥ 140mmHg, and SBP ≤ 120 mmHg, their percentages were 7.06%, 22.35%, and 62.35%, respectively. The DBP distribution of 85 subjects included DBP ≥ 100 mmHg, DBP ≥ 90 mmHg, and DBP < 80 mmHg, their percentages were 9.41%, 24.71%, and 61.18%, respectively. The mean differences and SD in resting BPs as measured by a smartwatch sphygmomanometer versus a mercury sphygmomanometer were –0.683 ± 6.203/203 mmHg (SBP, P = 0.723) and 1.628 ± 5.028 mmHg (DBP, P = 0.183) (Table 1; Criterion 1). The mean differences in resting BPs as measured by a smartwatch sphygmomanometer versus a mercury sphygmomanometer were −0.683 ± 5.364 (SBP, P = 0.838) and 1.628 ± 4.468 for (DBP, P = 0.440) according to criterion 2. The standard deviation for SBP was < 6.90 mmHg and for DBP, it was < 6.73 mmHg. These values satisfied ISO 81060-2:2018 guidelines. The PPV for resting SBP was 0.635 and 0.671 for resting DBP. The percentage of absolute BP differences within 5, 10, 15 and > 15 mmHg between the smartwatch and references in the resting BP study are shown in Table 2. Bland-Altman plots of mean differences in resting SBP and DBP by both devices are shown in Figure 2, the smartwatch demonstrated good consistency with the reference mercury sphygmomanometer.
Table 1. Mean differences and standard deviation (SD) of differences between the smartwatch and the reference in the resting and ambulatory BP tests.
| Overall | Resting BP study n = 85 |
Ambulatory BP study n = 35 |
||||
| SBP (mmHg) | DBP (mmHg) | SBP (mmHg) | DBP (mmHg) | |||
| aThis criterion is fulfilled if the mean value of the difference is within or equal to ± 5 mmHg, and the standard deviation is < 8 mmHg. bThis criterion is fulfilled if the SDs of the subjects are below 6.9 and 6.73 mmHg, respectively. Criterion 2 is not required for ambulatory measurement study. Abbreviations: BP, Blood Pressure; DBP, diastolic blood pressure; SBP, systolic blood press. | ||||||
| Criterion 1a | MD ± SD | −0.683 ± 6.203 | 1.628 ± 5.028 | −1.943 ± 5.475 | 3.195 ± 5.862 | |
| P | 0.723 | 0.183 | 0.923 | 0.065 | ||
| Criterion 2b | MD ± SD | −0.683 ± 5.3642 | 1.628 ± 4.468 | - | - | |
| P | 0.838 | 0.440 | - | - | ||
Table 2. Percentage of absolute blood pressure differences between the smartwatch and the reference in the resting and ambulatory BP studies.
| Subjects | Resting BP study n = 85 |
Ambulatory BP study n = 35 |
|||
| SBP (mmHg) | DBP (mmHg) | SBP (mmHg) | DBP (mmHg) | ||
| DBP: diastolic blood pressure; SBP: systolic blood pressure. | |||||
| ≤ 5 mmHg | 55.69% | 67.06% | 61.90% | 60.00% | |
| ≤ 10 mmHg | 89.41% | 96.08% | 89.52% | 85.71% | |
| ≤ 15 mmHg | 99.61% | 98.82% | 100% | 98.10% | |
| > 15 mmHg | 0.39% | 1.18% | 0 | 1.90% | |
Figure 2.
Bland-Altman plot of the differences between the test BPs with reference BPs in the ambulatory BP measurement study. (A): SBP; (B): DBP.
DBP: diastolic blood pressure; SBP: systolic blood pressure.
Validating the Accuracy of Ambulatory BP Measurements
We screened 43 subjects for additional ambulatory BP measurement study, 8 subjects were excluded by the criteria specified in the ISO 81060-2:2018 (Figure 1B). The 35 available subjects included 13 male (37.1%), 22 female (62.9%), had a mean age of 40 ± 13 years (range from 23 to 62 years), and their mean wrist circumference was 159.6 ± 15.2 mm (from 133.0–186.0 mm), (Table 2S).
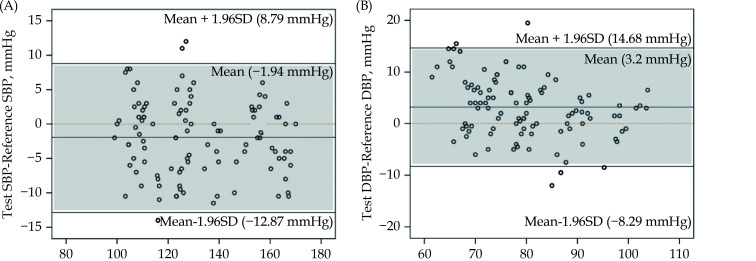
SBP ≥ 140 mmHg, and < 140 mmHg percentages were 27.1% and 62.9%, respectively. Mean differences in ambulatory BP, as measured by the smartwatch and mercury sphygmomanometer, were −1.943 ± 5.475 mmHg (SBP, P = 0.923) and 3.195 ± 5.862 mmHg (DBP, P = 0.065) (Table 1 Criterion 1). These results agreed with ISO 81060-2:2018 guidelines. The PPV for ambulatory SBP and DBP were separately 0.686. The percentages of absolute BP differences within 5, 10, 15 and > 15 mmHg between the smartwatch and reference in the ambulatory BP study are shown in Table 2. Additionally, Bland-Altman plots for SBP and DBP are shown in Figure 3. The 95% distribution interval of the mean difference for SBP was 8.79 mmHg and –12.87 mmHg, and for DBP, it was 14.68 mmHg and –8.29 mmHg.
Figure 3.
Bland-Altman plots of the differences between the test BPs with reference BPs in the ambulatory BP group. (A): SBP; (B): DBP.
DBP: diastolic blood pressure; SBP: systolic blood pressure.
Validating the accuracy of 24 h SBP circadian rhythm monitoring
In the dataset distributions of the 135 subjects, 13 subjects failed to comply with mandatory requirements, 1 subject slept < 3 h, 3 subjects’ watches did not have records after calibration, 4 subjects’ nocturnal datasets were less than seven pairs (14.3%), 6 subjects’ data were not recorded due to a bug, and 1 subject’s smartwatch got bad quality signals. Data from these 28 subjects were not included in statistical analysis (Figure 1C).
The 107 subjects included 44 males (41.1%) and 63 females (58.9%), with an average age of 40.1 ± 13.5 years (23–79 years) and average height = 165.6 ± 8.3 cm (148.0–186.0 cm). The average body weight was 63.7 ± 11.4 kg (41.0–90.0 kg) and the average wrist circumference was 162.3 ± 15.9 mm (130.0–193.0 mm) (Table 3S).
SBP ≥ 160 mmHg, SBP ≥ 140 mmHg (≥ 160 mmHg included), and SBP ≤ 120 mmHg percentages were 4.67%, 18.69%, and 62.62%, respectively. Fifty-nine subjects (55.1%) had a dipper-type SBP circadian rhythm, and 48 subjects (44.9%) had a non-dipper-type rhythm. Smartwatch SBP circadian rhythm was consistent with reference sphygmomanometer results: accuracy = 0.850, specificity = 0.864, precision/PPV = 0.833, sensitivity = 0.833, and F1 = 0.833 (Table 3).
Table 3. Accuracy of 24-h SBP circadian rhythms and diurnal high SBP alert.
| Evaluation | Recall/Sensitivity | Specificity | Precision/ PPV | F1 | Accuracy |
| SBP: systolic blood pressure; PPV: the positive predictive value. | |||||
| 24-h SBP circadian rhythms | 0.833 | 0.864 | 0.833 | 0.833 | 0.850 |
| Diurnal high SBP alert | 0.809 | 0876 | 0.706 | 0.754 | 0.858 |
Validating the accuracy of diurnal high SBP alert
In the 106 subjects, 20 were excluded for application alert rates of < 60%, and one subject was excluded as the difference between two devices > 20 mmHg (Figure 1D). Thus, 85 subjects were included. There were 38 males (44.7%) and 47 females (55.3%), with an average age of 38.5 ± 12.9 years (23–67 years), average height = 166.0 ± 7.9 cm (148.0–186.0 cm), average weight = 64.0 ± 11.0 kg (41.0–90.0kg), and wrist circumference = 161.7 ± 15.2 mm (130.0–196.0 mm) (Table 4S).
SBP ≥ 160 mmHg, SBP ≥ 140 mmHg (≥ 160 mmHg included), and SBP ≤ 120 mmHg percentages were 5.88%, 24.71%, and 64.71% respectively. Accuracy = 0.858, specificity = 0.876, precision/PPV = 0.706, sensitivity = 0.809, and F1 = 0.754 (Table 3), thereby indicating the smartwatch was highly consistent with the reference sphygmomanometer.
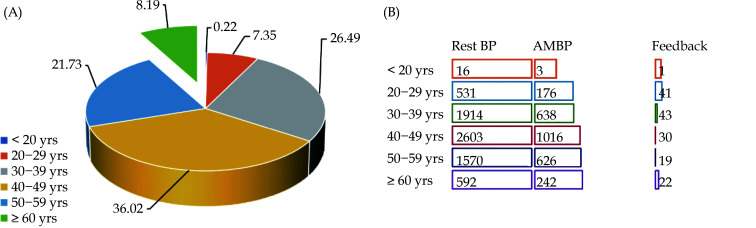
Feedback analysis of users of different ages
Smartwatch sphygmomanometer use in elderly populations has been questioned due to cognitive abilities and vision decline in these groups. Our analyses showed that 8.19% of subjects > 60 years old used smartwatch sphygmomanometers to monitor BP (Figure 4A). Further analyses showed that when compared with 30–39 years old, the proportion of elderly participants who completed ambulatory monitoring of blood pressure (AMBP) and feedbacks on the use of problems was higher, accounting for 40.87% vs. 33.33%, 3.7% vs. 2.24%, respectively.
Figure 4.
Age distribution of resting blood pressure, AMBP, and user feedback.
(A): Age distribution of all online user; (B): proportion of completed resting state blood pressure measurement, AMBP and use of feedback in different age groups. AMBP: ambulatory monitoring of blood pressure; BP: blood pressure.
DISCUSSION
Oscillometry-based resting and ambulatory BP measurement accuracy satisfied criteria 1 and 2 of ISO 81060-2:2018 guidelines (Table 1), and smartwatch accuracy met ambulatory sphygmomanometer ISO standards.
Our 24 h SBP circadian rhythm data indicated, even the invalid datasets percentage is striking in this small sample study, it was 20.7% (28 of 135 subjects), most of the reasons were application’s bugs and operation problems. After reviewing valid datasets, the sensitivity, accuracy, specificity, and precision were reassuring, which meant that SBP trend monitoring was able to fulfill the accuracy requirements when procedures and applications ran properly.
Our data showed that the diurnal high SBP alert application was capable of real-time alerting when an abnormally high SBP appeared, thereby potentially preventing hypertension risks. An anticipated purpose is that the device will highlight links between an individuals’ daily habits and BP surges, moreover, it can be used to filter out masked and abnormal high BP. The development of such smartwatch with hybrid BP measurements will benefit individuals’ private healthcare.
We randomly surveyed 7226 online users since the smartwatch was launched. As shown in Table 4 and Figure 4, among the users age distribution, the percentage of age 40–49 was higher than others (36.02% of 7226), among their SBP distributions, SBP ≥ 135 mmHg or DBP ≥ 85 mmHg percentage was correspondingly the highest 34.97%. The aged population (≥ 60 years old) percentage was 8.19% and SBP ≥ 135 or DBP ≥ 85 percentage was 6.0%. Users ≥ 60-year-old (8.96% of 2701) used AMBP. We collected 156 customers feedback between December 27th 2021 to February 13th 2022, the age distribution was shown in Figure 4, users ≥ 50 years old percentage was 29.92%. Approximately 14.1% of the aged users (≥ 60 years old) paid more attention to BP and relevant parameter measurement, 4.55% of them chose insensibly BP monitoring applications, 4.55% chose ABPM, 22.73% chose resting BP measurements, and 13.64% left questions about cardiovascular disease on the feedback, however, 31.82% could not get used to use this smartwatch. Moreover, 9.09% users provided personal advice after measurements; some compared the multi-measurement method with conventional home sphygmomanometers, because most of them had health issues (heart, cardiovascular, and liver diseases), and BP measurement was an important part of their daily routine. These positively questions and trials meant most users are willing to try these novel BP measurements by using smartwatch, and moreover, they are willing to accept a new mode of digital BP measurement.
Table 4. Distribution of 7226 online customers’ blood pressure.
| Age range | People | SBP ≥ 160 | SBP ≥ 135 (≥ 160 included) | SBP < 120 | DBP ≥ 85 |
| Data are presented as n (%). DBP: diastolic blood pressure; SBP: systolic blood pressure. | |||||
| < 20 yrs | 16 (0.22%) | 0 (0.00%) | 0 (0.00%) | 8 (0.11%) | 4 (0.06%) |
| 20-29 yrs | 531 (7.35%) | 3 (0.04%) | 111 (1.54%) | 235 (3.25%) | 231 (3.20%) |
| 30-39 yrs | 1914 (26.49%) | 49 (0.68%) | 649 (8.98%) | 595 (8.23%) | 1203 (16.65%) |
| 40-49 yrs | 2603 (36.02%) | 56 (0.77%) | 886 (12.26%) | 740 (10.24%) | 1641 (22.71%) |
| 50-59 yrs | 1570 (21.73%) | 28 (0.39%) | 532 (7.36%) | 478 (6.62%) | 822 (11.38%) |
| 60 yrs | 592 (8.19%) | 19 (0.26%) | 240 (3.32%) | 176 (2.44%) | 194 (2.68%) |
| Total | 7226 (100%) | 155 (2.15%) | 2418 (33.46%) | 2232 (30.89%) | 4095 (56.67%) |
Our study provided a holistic approach to BP monitoring. The non-invasive PPG technology can detect abnormal BP circadian rhythms and surges as early-warnings of hypertension, while resting and ambulatory BP measurements are useful in hypertension diagnoses. Thus, the system might provide an effective hypertension screening platform for public health campaigns. Hypertension awareness, and control rates might be improved using this multifunctional wrist device.
Study strengths and limitations
A study limitation was that the monitoring of 24 h SBP circadian rhythms based on PPG could only divide SBP variations into dippers and non-dippers, however, the categorization of extreme dippers (decline ≥ 20%) and risers or reverse dippers (decline < 0) have been assessed in previous studies.[22,23] With a higher prevalence of riser patterns in some specific cohorts (resistant hypertension individuals, ≥ 65% in elderly, and type 2 diabetes), more precise categorizations must be identified for 24 h SBP circadian rhythm applications in the future.[23-26]
Equipped with a PPG and oscillometry cuff, the HUAWEI WATCH D measured BP levels from different dimensions. It can connect to cell phones and provided reports for users. The device may be developed as an assisting prospective diagnostic device for remote telemedicine, and help individuals to have a better understanding of their health.
Conclusions
Our comparative BP estimation study highlighted excellent smartwatch accuracy and reliability. Versatile BP measurements showed the device was superior to conventional BP meters in terms of precise and objective BP evaluations. This multifunctional smartwatch provided a long-term, senseless, and straightforward approach for daily BP monitoring, and was especially convenient for elderly populations in reducing their time and financial costs when monitoring their health.
Acknowledgments
This study was supported by the National Key Research and Development Program of China (2020 YFC1512305), All authors have no conflicts of interest to disclose.
Contributor Information
Shan-Shan ZHOU, Email: a_339@126.com.
Yun-Dai CHEN, Email: cyundai@vip.163.com.
References
- 1.Kumar M Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aekplakorn W, Suriyawongpaisal P, Tansirisithikul R, et al Effectiveness of self-monitoring blood pressure in primary care: a randomized controlled trial. J Prim Care Community Health. 2016;7:58–64. doi: 10.1177/2150131915614069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joint Committee for Guideline Revision 2018 Chinese Guidelines for Prevention and Treatment of Hypertension-A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol. 2019;16:182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin H J, Wang T D, Chen M Y C, et al 2020 consensus statement of the taiwan hypertension society and the taiwan society of cardiology on home blood pressure monitoring for the management of arterial hypertension. Acta Cardiologica Sinica. 2020;36:537. doi: 10.6515/ACS.202011_36(6).20201106A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stergiou GS, Palatini P, Parati G, et al 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39:1293–1302. doi: 10.1097/HJH.0000000000002843. [DOI] [PubMed] [Google Scholar]
- 6.Shimbo D, Artinian NT, Basile JN, et al Self-measured blood pressure monitoring at home: a joint policy statement from the American Heart Association and American Medical Association. Circulation. 2020;142:e42–e63. doi: 10.1161/CIR.0000000000000803. [DOI] [PubMed] [Google Scholar]
- 7.Hansen TW, Thijs L, Li Y, et al International database on ambulatory blood pressure in relation to cardiovascular outcomes investigators. prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension. 2010;55:1049–1057. doi: 10.1161/HYPERTENSIONAHA.109.140798. [DOI] [PubMed] [Google Scholar]
- 8.Fabbian F, Smolensky MH, Tiseo R, et al Dipper and non-dipper blood pressure 24-hour patterns: circadian rhythm-dependent physiologic and pathophysiologic mechanisms. Chronobiol Int. 2013;30:17–30. doi: 10.3109/07420528.2012.715872. [DOI] [PubMed] [Google Scholar]
- 9.Kario K, Ferdinand KC, O’Keefe JH Control of 24-hour blood pressure with SGLT2 inhibitors to prevent cardiovascular disease. Prog Cardiovasc Dis. 2020;63:249–262. doi: 10.1016/j.pcad.2020.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Unger T, Borghi C, Charchar F, et al 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982–1004. doi: 10.1097/HJH.0000000000002453. [DOI] [PubMed] [Google Scholar]
- 11.Williams B, Mancia G, Spiering W, et al 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041. doi: 10.1097/HJH.0000000000001940. [DOI] [PubMed] [Google Scholar]
- 12.Whelton PK, Carey RM, Aronow WS, et al 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 13.Chokesuwattanaskul A, Cheungpasitporn W, Thongprayoon C, et al Impact of circadian blood pressure pattern on silent cerebral small vessel disease: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9:e016299. doi: 10.1161/JAHA.119.016299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh JP, Larson MG, Manolio TA, et al Blood pressure response during treadmill testing as a risk factor for new-onset hypertension. The Framingham heart study. Circulation. 1999;99:1831–1836. doi: 10.1161/01.CIR.99.14.1831. [DOI] [PubMed] [Google Scholar]
- 15.Ragueneau I, Michaud P, Démolis JL, et al Effects of cigarette smoking on short-term variability of blood pressure in smoking and non smoking healthy volunteers. Fundam Clin Pharmacol. 1999;13:501–507. doi: 10.1111/j.1472-8206.1999.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 16.Kawano Y Physio-pathological effects of alcohol on the cardiovascular system: its role in hypertension and cardiovascular disease. Hypertens Res. 2010;33:181–191. doi: 10.1038/hr.2009.226. [DOI] [PubMed] [Google Scholar]
- 17.Xu D, Zhang Y, Wang B, et al Acute effects of temperature exposure on blood pressure: An hourly level panel study. Environ Int. 2019;124:493–500. doi: 10.1016/j.envint.2019.01.045. [DOI] [PubMed] [Google Scholar]
- 18.Yatabe J, Yatabe MS, Ichihara A The current state and future of internet technology-based hypertension management in Japan. Hypertens Res. 2021;44:276–285. doi: 10.1038/s41440-020-00591-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.No-invasive sphygmomanometers. Part 2: Clinical validation of automated measurement type. American National Standards Institute 2018. ANSI/AAMI/ISO 81060-2. http://webstore.ansi,org. (assessed on Nov 9, 2021).
- 20.O’Brien E, Atkins N, Stergiou G, et al Working Group on Blood Pressure Monitoring of the European Society of Hypertension. European Society of Hypertension International Protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press Monit. 2010;15:23–38. doi: 10.1097/MBP.0b013e3283360e98. [DOI] [PubMed] [Google Scholar]
- 21.Sammut C, and Geoffrey I. W. Encyclopedia of machine learning; Springer: New York, NY, the USA, 2011.
- 22.Mancia G, Fagard R, Narkiewicz K, et al 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 23.Hermida RC, Smolensky MH, Ayala DE, Portaluppi F 2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. Chronobiol Int. 2013;30:355–410. doi: 10.3109/07420528.2013.750490. [DOI] [PubMed] [Google Scholar]
- 24.Ríos MT, Domínguez-Sardia M, Ayala DE, et al Prevalence and clinical characteristics of isolated-office and true resistant hypertension determined by ambulatory blood pressure monitoring. Chronobiol Int. 2013;30:207–220. doi: 10.3109/07420528.2012.701135. [DOI] [PubMed] [Google Scholar]
- 25.Hermida RC, Ayala DE, Crespo JJ, et al Influence of age and hypertension treatment-time on ambulatory blood pressure in hypertensive patients. Chronobiol Int. 2013;30:176–191. doi: 10.3109/07420528.2012.701131. [DOI] [PubMed] [Google Scholar]
- 26.Ayala DE, Moyá A, Crespo JJ, et al Circadian pattern of ambulatory blood pressure in hypertensive patients with and without type 2 diabetes. Chronobiol Int. 2013;30:99–115. doi: 10.3109/07420528.2012.701489. [DOI] [PubMed] [Google Scholar]